The usefulness of telemedicine has been acknowledged because of coronavirus disease 2019, which highlighted it as a prominent and expedient method of delivering healthcare support while ensuring safety.1 The implementation of telemedicine can be traced to nearly every corner of the globe, from advanced economies like the USA and Europe to the most remote African villages. Today, telemedicine is widely used in developed nations, although its popularity remains limited in many lower-income and middle-income countries (LMICs).2 3
Calculated estimates put Pakistan’s population at 210 million, with a 2% annual growth rate, making it the sixth most populous country in the world. The availability of mental health therapy is hindered by a shortage of both treatment facilities and professionals with the required education and experience. Currently, the country’s psychiatrist count is merely 400–500, translating to approximately 2–3 per million population.4 Mental health illnesses affect 4% of Pakistan’s population, with women making up the majority of those affected.5
LMICs face significant health inequities, with remote populations bearing the brunt of limited access. Telemedicine offers a promising solution, particularly for mental healthcare. In these settings, tele-mental health holds immense potential to improve access to quality services by enabling remote care delivery, expanding the reach of qualified personnel, enhancing supervision and training, promoting cost-effectiveness, and streamlining clinical workflows.6
A comprehensive analysis of available literature provides prevalence figures for depression and anxiety, as well as examines the related factors contributing to these conditions. The research revealed that the average overall prevalence of depressive disorders and anxiety was 34%, with a range of 29%–66% for women and 10%–33% for men. The factors linked to anxiety and depressive disorders include being female, middle-aged, having a poor level of education, experiencing financial hardship, being a housewife and having marital problems.7
A game-changer in healthcare, telemedicine has helped people, regardless of location or schedule, to get the high-quality care they need at a fraction of the cost. Telemedicine can step in when resources are few and the doctor-to-patient ratio is low.2 Online telemedicine portals like Sehat Kahani have been around since 2017 and offer mental health and general healthcare teleconsultations. For a more pleasant and stress-free telehealth experience, the Sehat Kahani platform pairs female practitioners with female patients, allowing women to choose their preferred providers.5 Pakistan possesses a distinctive advantage in constructing its telemedicine infrastructure. The telemedicine paradigm enhances the quality of medical care and promotes the efficient utilisation of medical resources.8
Mental health services are becoming increasingly important in the country’s health delivery system, which is encouraging despite many challenges and problems. Many sectors of Pakistan’s mental health treatment system are seeing significant improvement.9
This research aimed to bridge a gap in our understanding of the experiences of those who use mental health services by shedding light on obstacles to treatment. The use of e-health services in treating mental health difficulties can be demonstrated by disseminating real-time data collected from telemedicine platforms such as Sehat Kahani. This study used retrospective data obtained from the electronic health records compiled by Sehat Kahani, an e-health platform that has been actively promoting Sustainable Development Goal 3 since its establishment in 2017; through its telemedicine application and 63 e-health facilities, it has made healthcare more accessible in Pakistan.
The data set spans 8 months, starting on 1 March 2023 and ending on 31 October 2023. The sample comprises both men and women. However, the majority of patients seeking care for mental health difficulties were women who visited Sehat Kahani e-clinics in their local area during the 8-month period. A total of 5200 consultations were conducted via the Sehat Kahani platform and recorded in electronic health records by nurses assisting in the telehealth clinics. A random sample of patient medical records was selected from 10 Sehat Kahani clinics offering mental health services. To ensure data quality, a two-step screening process was implemented. First, our data software effectively randomised and selected 5200 patient medical records collected over 8 months. Second, records were manually screened for completeness, resulting in the exclusion of 344 records (105 with missing information and 239 of minors under 18 years of age). This rigorous approach yielded a final sample of 4856 medical records for analysis (see online supplemental figure 1).
These data sets consist of records from six clinics located in Sindh province. Specifically, there are two clinics in Karachi (Bilawal Goth and Korangi Zia), two in Hyderabad (Gidu and Hala Naka), one in Larkana, and one in Moro. The Punjab clinic is located in Kasur, while the Balochistan clinic is situated in Quetta. Additionally, there are two clinics in Khyber Pakhtunkhwa, specifically in Kaab and Loharbanda. The study assessed the patients' Patient Health Questionnaire 9 (PHQ-9) Scores and certain demographic factors. Only patients aged 18 years and above were included in the study, while those under 18 years or those receiving treatments other than mental health from Sehat Kahani clinics were excluded. Adherence to ethical principles was ensured throughout the study. Patients attending Sehat Kahani clinics provided informed consent, which explicitly acknowledged the potential use of anonymised data for commercial purposes and publications that promote the telemedicine approach to mental healthcare. This transparent approach protects patient privacy while allowing the research to contribute to the advancement of telemedicine in mental health service delivery.
The data collection instrument used in this study was PHQ-9. PHQ-9 is a highly used and validated instrument for screening and evaluating symptoms of depression. The tool offers a comprehensive and consistent method for gathering patient information during telepsychiatry consultations. The questionnaire was expanded to include supplementary inquiries regarding demographics and the referral mechanism system. PHQ-9 was administered by mental health practitioners providing mental health services at Sehat Kahani e-health centres. The data were analysed using the Statistical Package for Social Sciences V.22. The frequencies and percentages were computed to ascertain the descriptive statistics of the sociodemographic variables. The χ2 test was used to examine the correlations between the scores of categorical variables. A value of p≤0.05 was used as the threshold for statistical significance.
The findings of the current study show that mental health difficulties in Pakistan are on the rise. Urgent measures need to be taken in response to this issue. Of the 4856 patients, only 24 were male, while all the others seeking assistance from Sehat Kahani e-health solutions were female. Additional data analysis indicates that 3332 patients had follow-up appointments, while 1524 were new registrations. Of all the participants who visited Sehat Kahani, only 1302 patients were referred to the clinics; the other 3554 willingly came to seek mental health-related e-health services. Patients' follow-up recommendations were determined based on their PHQ-9 Scores; 2200 patients were instructed to schedule a follow-up appointment after their session. Patients aged 29–39 years comprised the majority of the participants visiting the clinic, as shown in table 1.
Table 1. Patient demographics and clinic visit information.
| Patient variables | Frequency | Per cent |
| Gender | ||
| Female | 4832 | 99.5 |
| Male | 24 | 0.5 |
| Type of registration | ||
| Follow-up visit | 3332 | 68.6 |
| New visit | 1524 | 31.4 |
| Symptomatic | ||
| Yes | 687 | 14.1 |
| No | 4169 | 85.9 |
| Referred to Sehat Kahani e-health solutions | ||
| Yes | 1302 | 26.8 |
| No | 3554 | 73.2 |
| Follow-up is required | ||
| Yes | 2200 | 45.3 |
| No | 2656 | 54.7 |
| Age categories | ||
| 18–28 years | 826 | 17.0 |
| 29–39 years | 2611 | 53.8 |
| 40–50 years | 1049 | 21.6 |
| 51–61 years | 282 | 5.8 |
| 62+ years | 88 | 1.8 |
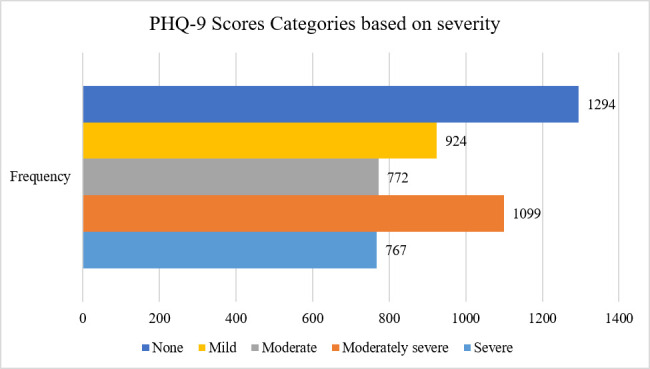
A total of 2638 patients were identified as having depression through PHQ-9 screening; the remaining patients either displayed symptoms that were not connected to depression, had mild symptoms or none at all. As shown in figure 1, based on the PHQ-9 Scale, there were approximately 772 patients in the moderate category, 1099 in the moderately severe category and 767 in the severe category.
Figure 1. Patient Health Questionnaire 9 (PHQ-9) Depression Score categories for patients at Sehat Kahani clinics.
Values of p were statistically significant for the type of registration (p=0.020), patients’ referral status (p=0.020) and severity of PHQ-9 Scores (p=0.011) (see online supplemental table 1). This suggests that patients who visit Sehat Kahani e-health solutions are highly motivated by the platform’s provision of excellent mental health services and its efforts to decrease the stigma associated with accessing mental healthcare.
In online supplemental table 1, we employed the χ2 test as the statistical methodology for data analysis. The patients’ type of registration, referral status and severity of the PHQ-9 Score are strongly associated with the age of patients seeking mental health treatment at Sehat Kahani e-health solutions. This association is considered statistically significant when variables have values less than 0.05.
The national surveys of Pakistan do not sufficiently address mental health, leading to a scarcity of reliable data and contradictions in outcomes. Establishing a robust mental health surveillance system is greatly enhanced by providing high-quality information at the national level.10 The Pakistani community seems to have a restricted comprehension and sparse terminology to articulate their internal psychological and emotional encounters. Despite this, to tackle mental health concerns, the community displays a range of responses and reactions influenced by distinct social, cultural and religious variables.11 The prevalence of mental health disorders is higher among women than men, a consistent trend observed globally. Women globally experience inferior overall health, heightened levels of despair and more psychological suffering compared with men.12 13
Aligning with prior research,14 our findings suggest that telepsychiatry offers a valuable approach to addressing the rising prevalence of depression among Pakistani women. The high proportion of women in both studies (98.4% and 99.5%, respectively) further supports this. Our data with 4856 participants revealed a significant number of individuals with moderate (772) and severe depression (767) diagnoses. This result mirrors the findings of the study conducted in the e-health clinics of Dadar Mansehra14 with 2660 participants, of which 449 and 554 participants scored within the categories of moderate and severe depression, respectively. These results collectively highlight the potential of telepsychiatry to impact mental healthcare delivery in Pakistan significantly.
Furthermore, the results of our study are inconsistent with prior research conducted at Shifa International Hospital’s outpatient psychiatry clinic, which found that 86.5% of the participants (n=260) expressed a preference for future consultations by telepsychiatry.15 In contrast, our study, which had a larger sample size of 4856 participants, found that 68.6% of patients at Sehat Kahani e-clinic were willing to return for mental healthcare treatments, as shown by the follow-up rate. This suggests that although there is a strong demand for telepsychiatry, a considerable number of patients prioritise the consistency of therapy offered by inperson follow-up appointments.
This study highlights the increasing mental health concerns in Pakistan, specifically among women. Sehat Kahani’s e-health solutions reveal a significant disparity in the utilisation of mental health services between genders, with men being less likely to seek such care. The platform’s services are highly valued, as indicated by the strong follow-up rates and the large number of patients actively seeking e-health solutions. The study findings underscore the significance of promptly addressing mental health concerns in Pakistan. An effective surveillance system is essential for comprehending and managing mental health. It would enhance the collection and analysis of mental health data nationwide. The community’s diverse mental health responses are influenced by cultural and socioeconomic issues, underscoring the importance of employing culturally sensitive approaches.
Our study has some limitations. First, the study’s sample comprises individuals who use Sehat Kahani’s telemedicine e-health solutions. It is possible that they do not reflect the entire population, particularly those with little knowledge of or access to telemedicine services in their area. Second, most participants were female, indicating a possible gender bias in the sample. This may restrict the applicability of the results. Finally, there is a chance of bias in the study because it uses self-reported data. People may exaggerate or understate their symptoms depending on what society expects of them.
Based on our findings, we suggest that to address the gender disparity, it is advisable to execute focused outreach initiatives to enhance male understanding of mental health and telemedicine services. Community leaders, social media and traditional communication routes should be employed to guarantee a more inclusive and diverse sample. Also, by granting individuals in rural regions the opportunity to receive healthcare, telemedicine could alleviate the scarcity of mental health professionals in Pakistan. Finally, telemedicine might additionally mitigate the social disapproval linked to mental health conditions by facilitating individuals’ access to therapy without necessitating a visit to a physical clinic.
supplementary material
Acknowledgements
We are deeply grateful to the British Asian Trust for its incredible support of integrated mental health care. We are grateful to Muhammad Sumair Khan, Lead Clinical Operations at Sehat Kahani, for providing essential EHR data from the cloud, which significantly enriched this research.
Biography
Sara Saeed Khurram embarked on her journey in healthcare by graduating with an MBBS degree from DOW University of Health Sciences, Karachi, Pakistan, in 2010. Building upon this foundation, she furthered her education by earning a Master's degree in health policy and management from The Aga Khan University of Health Sciences, Karachi, Pakistan, in 2018. In 2014, her commitment to improving global health led her to become the CEO and co-founder of Sehat Kahani, a digital health platform that aligns with Sustainable Development Goal 3, advocating for universal access to quality healthcare. As a CEO, Dr Sara Saeed Khurram has demonstrated remarkable leadership in leveraging technology to enhance healthcare delivery. Her impactful contributions extend to mental health research, public health, and improving access to healthcare in marginalized communities, reflecting her current research activities and interests. Her visionary leadership and advocacy for accessible healthcare highlight her ongoing commitment to transformative change in these critical areas.

Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Collaborators: Not Applicable.
Ethics approval: This study involves human participants. Community Innovation Hub, Sehat Kahani approved the study (reference no: IRB-0021/CIH/2024). Participants gave informed consent to participate in the study before taking part.
Contributor Information
Sara Saeed Khurram, Email: sara@sehatkahani.com.
Iffat Zafar Aga, Email: iffatzaga@gmail.com.
Mahek Karim, Email: mpethani.17@gmail.com.
Muhammad Muzzamil, Email: muzzamilrao21@gmail.com.
Alina Lakhani, Email: alina@sehatkahani.com.
Sanaa Ahmed, Email: sanaa.ahmad@britishasiantrust.org.
References
- 1.Kay M, Santos J, Takane M. Telemedicine: opportunities and developments in member states. Glob Obs eHealth series. 2010:8–9. [Google Scholar]
- 2.Kumar G, Shardha HK, Tariq W, et al. Assessment of knowledge and attitude of healthcare professionals regarding the use of telemedicine: a cross-sectional study from rural areas of Sindh, Pakistan. Front Public Health. 2022;10:967440. doi: 10.3389/fpubh.2022.967440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biruk K, Abetu E. Knowledge and attitude of health professionals toward telemedicine in resource-limited settings: a cross-sectional study in North West Ethiopia. J Healthc Eng. 2018;2018:2389268. doi: 10.1155/2018/2389268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siddiqui F. Barriers and challenges to mental health care in Pakistan. PJNS. 2021;16:1–2. [Google Scholar]
- 5.Farooqui AT, Karim S, Karim N. Role of digital health tools in improving maternal and adolescent mental health services in Pakistan: a way forward. J Coll Physicians Surg Pak. 2023;33:957–8. doi: 10.29271/jcpsp.2023.09.957. [DOI] [PubMed] [Google Scholar]
- 6.Acharibasam JW, Wynn R. Telemental health in low-and middle-income countries: a systematic review. Int J Telemed Appl. 2018;2018:9602821. doi: 10.1155/2018/9602821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. BMJ. 2004;328:794. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ullah N, Khan P, Sultana N. A telemedicine network model for health applications in Pakistan: current status and future prospects. JDCTA. 2009;3:149–55. doi: 10.4156/jdcta.vol3.issue3.19. [DOI] [Google Scholar]
- 9.Javed A, Khan MS, Nasar A, et al. Mental healthcare in Pakistan. Taiwan J Psychiatry. 2020;34:6. doi: 10.4103/TPSY.TPSY_8_20. [DOI] [Google Scholar]
- 10.Alvi MH, Ashraf T, Naz F, et al. Burden of mental disorders by gender in Pakistan: analysis of global burden of disease study data for 1990–2019. BJPsych Bull. 2023;29:1–8. doi: 10.1192/bjb.2023.76. [DOI] [PubMed] [Google Scholar]
- 11.Shafiq S. Perceptions of Pakistani community towards their mental health problems: a systematic review. Global Psychiatry. 2020;3:28–50. doi: 10.2478/gp-2020-0001. [DOI] [Google Scholar]
- 12.World Health Organization . Depression and other common mental disorders: global health estimates. Geneva: World Health Organization; 2017. [Google Scholar]
- 13.Boerma T, Hosseinpoor AR, Verdes E, et al. A global assessment of the gender gap in self-reported health with survey data from 59 countries. BMC Public Health. 2016;16:675. doi: 10.1186/s12889-016-3352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aga IZ, Khurram SS, Karim M, et al. Employing telepsychiatry services to assess the prevalence and identify mental health disorders using the PHQ-9 and GAD-7 in resource-constrained regions of Dadar Mansehra, Pakistan: an observational cross-sectional study. BMJ Open. 2023;13:e078976. doi: 10.1136/bmjopen-2023-078976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yousafzai AW, Khan SA, Bano S, et al. Patient satisfaction with telepsychiatry consultations in the time of COVID-19: data from a tertiary care hospital in Pakistan. KMUJ. 2022;14:33–7. doi: 10.35845/kmuj.2022.21719. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


