Abstract
Childhood bereavement is an adverse event, yet children demonstrate considerable variability in health outcomes. Bereaved children are at risk of lower lifelong educational attainment, though the contribution of neurocognitive performance is yet to be investigated. Using data from the population-based Generation R Study wherein nearly 10,000 pregnant mothers were recruited between 2002 and 2006, we estimated the association of bereavement by age 10 years with four subtests of cognitive function and academic achievement at 13 years. Bereavement by 10 years of age was experienced by n = 796 (37.3%) of youth and was associated with a 1.12-point (SD = 0.55; p-value = 0.04) lower full-scale IQ at 13 years, which was mainly driven by lower matrix reasoning scores (βadjusted = −0.27, SE = 0.11, p < 0.02). There were no differences in academic achievement or other subtests of neurocognitive function between bereaved and non-bereaved children. Secondary analyses adjusting for pre-bereavement nonverbal cognitive ability and mental health problems revealed an overall association between bereavement and subsequent full-scale IQ and matrix reasoning, but only among those youth whose caregivers reported that the loss had an emotional influence on the child. These novel findings leveraging prospective assessments in a population-based birth cohort highlight risk and resilience mechanisms warranting further research.
Keywords: Bereavement, Cognitive ability, Academic achievement, Child development, Mental health
Subject terms: Risk factors, Trauma
Introduction
Approximately 4–7% of children will experience the death of a parent by the age of 181, and up to 62% of children are bereaved of a parent, sibling, grandparent, or other close family member by the age of 102. Bereavement in childhood is associated with an elevated risk for adverse health outcomes3, yet there is substantial variability in this association. While the majority of bereaved children do not experience clinically significant psychopathology following the death of a loved one4, studies do show that a smaller proportion of bereaved youth are at higher risk of poor health and social outcomes relative to their non-bereaved counterparts, including elevated anxiety and depression symptoms, lower lifelong educational attainment5,6, and reduced developmental competence7.
The association between childhood bereavement and subsequent lower educational attainment is well characterized, but risk pathways are yet to be identified. One study found that young adults who experienced the death of a family member during their college years have 43% lower odds of obtaining a college degree8. Additional work has shown that bereaved youth achieved fewer years of educational attainment, and reported more difficulties at work and less well-elaborated plans for career development compared to non-bereaved peers9. While social and structural factors influence educational attainment among bereaved individuals6, highly disruptive traumatic experiences can also affect neurocognitive processes9. Yet this association is yet to be investigated among bereaved children in datasets with prospective measurements of cognitive ability, as well as adequate measurement of potential confounders to adjust for the many sociodemographic and structural factors that elevate mortality risk among adults10,11.
While studies of neurocognitive function among bereaved youth are scarce, work investigating the association between bereavement and neurocognition among adults is more developed. Prior studies among adults have noted an association between bereavement and neurocognitive deficits in the specific domains of attention and executive functioning12, memory and learning13,14, language and processing speed, and verbal fluency15. Work from a life course perspective has shown that experiencing parental death in childhood is longitudinally associated with an elevated risk of cognitive impairment in later life16,17, consistent with perspectives suggesting that life course stressors may impede neurocognitive development, elevating vulnerability to later-life cognitive impairment18. However, work examining more proximate interruptions to neurocognitive development among bereaved youth is yet to be carried out. Identified associations, if found, could pinpoint targeted opportunities to remediate the effects of bereavement on neurocognitive development and thereby facilitate the acquisition of educational targets among bereaved children.
Longitudinal birth cohorts with repeated measures over time provide the necessary framework to prospectively estimate the associations between bereavement and neurocognitive and academic performance. The present investigation aims to evaluate a hypothesized relationship between childhood bereavement and lower academic and neurocognitive performance. We leverage a longitudinal study design to address confounding by baseline characteristics evident before the death by adjusting for neurocognitive performance and mental health problems assessed at ages 5–6, before bereavement. Secondary models characterize the contribution of pre-loss neurocognitive performance and mental health symptoms in attenuating the hypothesized association between bereavement and reduced academic and neurocognitive performance.
Methods
Study population
This study is nested with the Generation R Study, a population-based birth cohort study on child and maternal health that enrolled mothers with a delivery date from April 2002 until January 2006 in Rotterdam, The Netherlands. The Generation R study design and procedures are extensively described in prior publications19,20. All study protocols were approved by the Medical Ethical Committee of the Erasmus Medical Center (EMC) in Rotterdam, the Netherlands. All methods were carried out in accordance with the Declaration of Helsinki of the World Medical Association. Written informed consent was obtained from all participants. If a child was less than 12 years old, legal guardians gave consent on behalf of the child. When a child was 12 years or older, written informed consent was obtained from both legal guardians and the child.
From the full Generation R cohort, we included 5862 participants who consented to participate in the research visit when the study child was 10 years of age, at which time exposure to bereavement was assessed. We excluded 315 participants with unreliable life events responses due to language barriers, missingness in one or both bereavement questions, missingness in age at or influence of loss, a reported age at loss greater than their age at the visit around age 10 years, or exposure to both parent and “other” loss. Finally, we excluded 3412 individuals who were missing cognitive or academic test outcome data around ages 12 and 13 years. Thus, our final analytic sample included 2135 individuals with both exposure and outcomes ascertained. Secondary analyses further filtered this analytic sample based on age at and influence of loss, as detailed below. See Fig. 1 for the analytic sample flow chart.
Fig. 1.
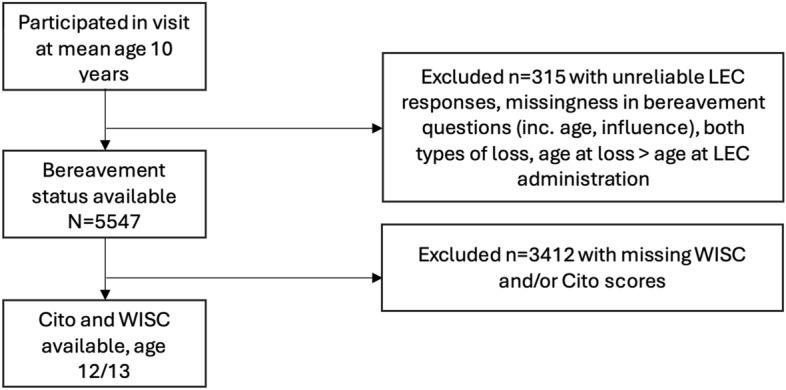
Flow chart of study population.
Measures
Bereavement
Bereaved children were identified based on caregivers' responses (95.4% mother reported) through an interview about the occurrence of adverse life events when the child was on average 10 years old. The assessment was based on a previous assessment in a similar cohort, including several questionnaires, such as the Stressful Life Events Questionnaire21. Specifically, caregivers were asked, “Has the father/mother or other caretaker of your child died?” and “Has someone else, who your child cared a lot about, died?” It is unknown who this person and what their relationship with the child was. Caregivers also specified the age of the child at bereavement, as well as caregiver perceived influence of the death on the child at the time of reporting (1 = no influence, 2 = a little, 3 = moderate, 4 = a lot of influence). Positive responses to either question were combined into one bereavement category, as the prevalence of parental loss was too low to investigate separately. All categorizations of perceived lasting influence were included in our primary analyses, as detailed below.
Cognition
At 13 years of age, children were administered four sub-tests from the Wechsler Intelligence Scale for Children-Fifth Edition (WISC-V). The WISC-V is designed to assess individual cognitive functioning in 6- to 16-year-olds. In collaboration with Pearson (Pearson Clinical Assessment, San Antonio, TX, USA), four core subtests were selected from the WISC-V to derive an estimated full scale IQ (FSIQ). The four subtests included vocabulary, matrix reasoning, digit span and coding, corresponding to measurement of verbal comprehension, fluid reasoning, working memory and processing speed, respectively. All four subtests were administered by trained research assistants. The detailed method of administering the four subtests is described in a previous study22. Raw scores from the subtests were first converted to age-standardized T-scores (ranging from 1 to 19) based on Dutch norm scores and were summed and converted to an estimated FSIQ.
Academic performance
School performance was measured with the end-of-primary-school test created by the Central Institute for Test Development (Cito, www.cito.com). The Cito test is the most widely used test in primary schools in the Netherlands, comprising 85% of all children23 and broadly assesses learning achievement of 12-year-olds. Test scores range from 501 to 550 and these scores are converted to a secondary school recommendation. The scores are left-skewed and have a ceiling effect. The Cito test comprises two subscales: language and mathematics. The language subscale included writing, reading comprehension, spelling, grammar, punctuation, and vocabulary. The mathematics subscale consisted of dealing with numbers, money and time, mental arithmetic, proportions, fractions and percentages, and geometry24 (Van Boxtel, Engelen, & de Wijs, 2011). As raw subscale scores are not easily comparable across test administration years, percentile rank scores are recommended by the publishers, as was done in previous work using Generation R data25.
Academic underachievement
Based on earlier work26, Cito test scores (standard scale from 501 to 550) were regressed on FSIQ scores in a linear regression model without any additional variables to quantify the academic underachievement. Standardized residuals were obtained, which were used as a continuous score to indicate academic achievement not explained by FSIQ As such, this score is expressed as a standardized z-score, with negative values representing the number of standard deviations that academic achievement is lower than expected (i.e. underachievement).
Covariates
Child sex, parental national origin, maternal education level, maternal marital status, household income, and maternal psychopathology were included as covariates. Date of birth and child sex were obtained from medical records. Information on parental national origin was collected through maternal self-report on parental national origin, and it was categorized according to the classification of Statistics Netherlands, i.e. Dutch, non-Dutch European, and non-Dutch non-European27. Maternal education level was assessed through self-report and classified into low (primary school or lower), middle (lower and intermediate vocational training) or high (higher vocational education and university). Maternal marital status was assessed through self-report and classified as married or living together vs. no partner or not living together. Household income was assessed using maternal self-report at child age 5 years and was categorized using poverty levels thresholds of Statistics Netherlands: < €1400/month, between €1400–2200/month, and ≥ €2200/month20,28. Maternal psychopathology was measured at child age 3 years using the validated Brief Symptom Inventory29. For analyses pertaining to Cito test score or academic (under)achievement, Cito test administration year (2014, 2015, 2016, 2017) and age at Cito assessment were included as covariates26. For analyses pertaining to Cito sub-scale percentile scores, age at Cito assessment but not Cito test year was included, given that the percentile scores (unlike the overall score) are comparable across test administration years. For secondary analyses restricting to bereavement after IQ assessment at age 5 years, IQ at age 5 and a continuous score of emotional and behavioral problems at age 5 years assessed using the Child Behavior Checklist30 were included as covariates as well. At mean age 5 years, children completed an assessment for nonverbal IQ using two subtests of the validated Dutch ‘Snijders-Oomen’ nonverbal intelligence test—Revised (SON-R,31. The test assessed intelligence without overreliance on language skills, thus suitable for this young and multi-ethnic cohort in which children of non-Dutch national origin were less likely to be exposed to the Dutch language. Non-verbal IQ was only adjusted for in secondary analyses restricted to bereavement occurring after the nonverbal IQ assessment. In the full sample, the correlation between FSIQ assessed at age 13 and nonverbal IQ assessed at age 5–6 was r = 0.40, and in the analytic sample, it was r = 0.48.
Statistical analysis
We first compared sociodemographic characteristics of bereaved and non-bereaved participants across the following variables: type of loss (parental vs. other), age at loss, child’s sex and parental national origin, mother’s marital status, education and psychopathology, and household income. Next, to carry out our primary objective regarding assessing hypothesized associations between bereavement by age 10 and neurocognitive outcomes at ages 12–13, we conducted a series of linear regressions. First, we specified unadjusted models, regressing each neurocognitive outcome at ages 12–13 on bereavement status before the age of 10, regardless of maternal assessment of the influence of the loss on the child. Note, however, that the “unadjusted” models for Cito test score and academic underachievement included Cito test administration year and age at Cito assessment as covariates, and the unadjusted models for Cito sub-scale percentile scores included age at Cito assessment as a covariate25,26. Second, we specified adjusted models that introduced baseline covariates (child sex, parental national origin, maternal psychopathology, household income, maternal education, and maternal marital status), without removing the aforementioned Cito-specific covariates. Third, we performed a few sensitivity analyses. To explore the impact of maternally perceived lasting influence of the loss on the child on our study results, we filtered bereaved individuals based on at least some (> 1) lasting influence of the loss on the child and then based on at least moderate (> 2) lasting influence. To address the Cito test ceiling effect, we repeated all analyses in the supplement with the Cito test score after removing the bottom and top 25% of Cito test scores.
Finally, to address potential reverse causation and confounding by early childhood IQ and mental health symptoms, we performed secondary analyses on outcomes that were significantly associated with bereavement in primary analyses. In primary analyses, we could not simply adjust for pre-bereavement IQ and mental health symptoms at age 5 because some individuals were bereaved before the age of baseline assessment. In these secondary analyses, we restricted the bereaved cohort to those bereaved after their IQ and mental health assessment at around age 5, while adjusting for these assessments. Similar sensitivity analyses were performed for these secondary results, filtering bereaved individuals based on at least some (> 1) lasting influence of the loss on the child and then based on at least moderate (> 2) lasting influence.
We addressed missingness in our covariates by applying multiple imputation (MI) within our analytic sample using MICE, generating 20 imputed datasets each with a maximum of 20 iterations. While all children in our analytic sample had bereavement status observed, n = 42 had missing data on their specific age at their loss. For secondary analyses that involved restricting the bereaved sample to those with an age of loss greater than their age at the IQ assessment around age 5 years, we excluded these n = 42 individuals as well. All analyses were performed in R, version 4.3.2.
Results
Comparisons of sociodemographic characteristics across bereaved and non-bereaved participants are reported in Table 1. Of the n = 2135 children in our analytic sample, 796 (37.3%) experienced the death of a parent/caregiver or other loved one between the ages of 0 and 10, according to maternal report. Of those bereaved, 11 (1.4%) experienced the death of a parent or caregiver. Approximately 50% of bereaved children experienced the loss in question after the age of 5. There were hardly any average group differences between bereaved and non-bereaved children according to child and maternal sociodemographic characteristics. Comparison of bereaved individuals according to the timing of loss (before vs. after age 5) likewise revealed no meaningful between-group differences (Table S1).
Table 1.
Analytic sample characteristics by bereavement status.
| Variable | Complete case | Multiple imputation | |||||
|---|---|---|---|---|---|---|---|
| Not bereaved (N = 1339) | Bereaved (N = 796) | Total (N = 2135) | Not bereaved (N = 1339) | Bereaved (N = 796) | Total (N = 2135) | ||
| Type of loss | Other | – | 785 (98.6%) | 785 (98.6%) | – | 785 (98.6%) | 785 (98.6%) |
| Parent | – | 11 (1.4%) | 11 (1.4%) | – | 11 (1.4%) | 11 (1.4%) | |
| N missing | – | 0 | 0 | – | - | - | |
| Age at loss | Before IQ@5 assessment | – | 359 (47.6%) | 359 (47.6%) | – | 359 (47.6%) | 359 (47.6%) |
| After IQ@5 assessment | – | 395 (52.4%) | 395 (52.4%) | – | 395 (52.4%) | 395 (52.4%) | |
| N missing | – | 42 | 42 | – | 42 | 42 | |
| Child’s sex | Female | 712 (53.2%) | 436 (54.8%) | 1148 (53.8%) | 712 (53.2%) | 436 (54.8%) | 1148 (53.8%) |
| Male | 627 (46.8%) | 360 (45.2%) | 987 (46.2%) | 627 (46.8%) | 360 (45.2%) | 987 (46.2%) | |
| N missing | 0 | 0 | 0 | – | – | – | |
| Mother’s marital status | Married or living with partner | 1140 (90.5%) | 688 (91.7%) | 1828 (90.9%) | 1211 (90.4%) | 731 (91.8%) | 1942 (91.0%) |
| No partner | 120 (9.5%) | 62 (8.3%) | 182 (9.1%) | 128 (9.6%) | 65 (8.2%) | 193 (9.0%) | |
| N missing | 79 | 46 | 125 | – | – | – | |
| Parental national origin | Dutch | 888 (67.0%) | 537 (68.2%) | 1425 (67.4%) | 897 (67.0%) | 542 (68.1%) | 1439 (67.4%) |
| Non-Dutch non-European | 336 (25.3%) | 188 (23.9%) | 524 (24.8%) | 338 (25.2%) | 191 (24.0%) | 529 (24.8%) | |
| Non-Dutch European | 102 (7.7%) | 62 (7.9%) | 164 (7.8%) | 104 (7.8%) | 63 (7.9%) | 167 (7.8%) | |
| N missing | 13 | 9 | 22 | – | – | – | |
| Household income | < 1400 | 154 (14.2%) | 85 (12.8%) | 239 (13.7%) | 224 (16.7%) | 116 (14.6%) | 340 (15.9%) |
| 1400–2200 | 172 (15.9%) | 115 (17.3%) | 287 (16.4%) | 209 (15.6%) | 139 (17.5%) | 348 (16.3%) | |
| > 2200 | 758 (69.9%) | 463 (69.8%) | 1221 (69.9%) | 906 (67.7%) | 541 (68.0%) | 1447 (67.8%) | |
| N missing | 255 | 133 | 388 | – | – | – | |
| Mother’s education | Low | 62 (4.9%) | 26 (3.5%) | 88 (4.4%) | 69 (5.2%) | 26 (3.3%) | 95 (4.4%) |
| Medium | 456 (36.0%) | 300 (40.0%) | 756 (37.5%) | 486 (36.3%) | 326 (41.0%) | 812 (38.0%) | |
| High | 749 (59.1%) | 424 (56.5%) | 1173 (58.2%) | 784 (58.6%) | 444 (55.8%) | 1228 (57.5%) | |
| N missing | 72 | 46 | 118 | – | – | – | |
| Mother’s psychopathology score | Mean (SD) | 0.2 (0.3) | 0.2 (0.3) | 0.2 (0.3) | 0.2 (0.3) | 0.2 (0.3) | 0.2 (0.3) |
| Range | 0.0–2.6 | 0.0–2.3 | 0.0–2.6 | 0.0–2.6 | 0.0–2.3 | 0.0–2.6 | |
| N missing | 312 | 166 | 478 | – | – | – | |
For MI, summary statistics come from the first multiply imputed dataset. Age at loss was not imputed.
Results from primary analyses of the relationship between bereavement between ages 0 and 10 with neurocognitive outcomes at ages 12–13 are displayed in Table 2. Overall, effect estimates between unadjusted and adjusted models were similar. Bereaved individuals, on average, demonstrated 1.12-point (SD = 0.55; p-value = 0.04) lower FSIQ scores than their non-bereaved counterparts, conditional on child and maternal sociodemographic factors. Among the WISC sub-tests, only matrix reasoning demonstrated a statistically significant relationship with bereavement, conditional on child and maternal sociodemographic factors (β = −0.27; SD = 0.11; p-value = 0.02). Note, however, that associations are nominally significant at the α = 0.05 level when accounting for the fact that multiple tests were conducted. In totality, we do find evidence that estimates for all outcomes are negative, even as the size of the estimate varies by outcome. That the direction of effects is consistent suggests a lower likelihood that observed associations are due to chance and a higher likelihood that a reduction in p-value after correcting for multiple tests could reflect sample size limitations rather than associations arising simply due to chance32. The relationship of bereavement status with coding, vocabulary, and digit span WISC sub-tests, and with academic underachievement, Cito test score, and Cito percentile scores, was null—there were no differences in these mean outcomes between bereaved and non-bereaved children. Additional adjustment for paternal educational level and paternal psychopathology resulted in similar model estimates (data available upon request, which are not shown here due to > 30% missingness in these covariates, making them less suitable for multiple imputation). We found that inclusion of these paternal covariates resulted in the observed associations of bereavement with FSIQ and WISC-MR becoming nonsignificant due to larger standard errors, as expected, but given the instability that inclusion of these covariates introduced to the model, results are difficult to interpret.
Table 2.
Association between bereavement before age 10 and neurocognitive outcomes at ages 12–13 (N = 2135).
| Outcome | Model | Estimate | SE | p-value |
|---|---|---|---|---|
| CITO language percentile score | Unadjusted | −1.10 | 1.21 | 0.36 |
| Adjusted | −1.28 | 1.13 | 0.26 | |
| CITO math percentile score | Unadjusted | −1.44 | 1.22 | 0.24 |
| Adjusted | −1.34 | 1.16 | 0.25 | |
| CITO test score | Unadjusted | −0.40 | 0.40 | 0.31 |
| Adjusted | −0.44 | 0.37 | 0.24 | |
| WISC CD T-score | Unadjusted | −0.14 | 0.15 | 0.34 |
| Adjusted | −0.16 | 0.14 | 0.27 | |
| WISC DS T-score | Unadjusted | −0.18 | 0.12 | 0.12 |
| Adjusted | −0.17 | 0.12 | 0.14 | |
| WISC MR T-score | Unadjusted | −0.27 | 0.12 | 0.02* |
| Adjusted | −0.27 | 0.11 | 0.02* | |
| WISC Vocab T-score | Unadjusted | −0.04 | 0.13 | 0.78 |
| Adjusted | −0.04 | 0.12 | 0.74 | |
| WISC Estimated FSIQ | Unadjusted | −1.10 | 0.57 | 0.05* |
| Adjusted | −1.12 | 0.55 | 0.04* | |
| Academic underachievement | Unadjusted | 0.011 | 0.04 | 0.80 |
*Associations are nominally significant at the .05 level accounting for the fact that multiple tests were conducted. CITO = primary school test; WISC = Weschler Intelligence Scale for Children; FSIQ = full scale intelligence quotient; CD = Coding; DS = Digit-span; MR = Matric reasoning. Unadjusted models for CITO test score and academic underachievement include CITO test administration year and age at CITO assessment as covariates. Unadjusted models for CITO sub-scale percentile scores include age at CITO assessment as a covariate. All adjusted models include the following covariates, in addition to any CITO-specific covariates mentioned: child sex, parental national origin, maternal psychopathology, household income, maternal education, and maternal marital status.
Significant values in bold.
Sensitivity analyses, excluding bereaved individuals for whom the loss was rated as ‘no influence’ on the child by the caregiver, resulted in similar conclusions (Table S2, S3). Further excluding bereaved individuals for whom the loss was rated as ‘little influence’ by the primary caregiver changed primary results (Table S4). Namely, bereavement was no longer significantly associated with FSIQ (β = −1.37; SD = 1.31; p-value = 0.30), but the magnitude of the relationship between bereavement and the matrix reasoning sub-test became considerably larger (β = −0.68; SD = 0.27; p-value = 0.01). Cito test scores and Cito math percentile scores were also now significantly associated with bereavement status. However, excluding the top and bottom 25% of Cito test scores in sensitivity analyses resulted in a non-significant relationship between bereavement and Cito test score (Table S5).
Secondary analyses explored the relationship of bereavement between ages 5 and 10 with WISC FSIQ and matrix reasoning outcomes, excluding those who were bereaved before the age of 5 (Table 3). Models that adjusted for pre-bereavement IQ and mental health symptoms, in addition to sociodemographic characteristics, revealed no significant associations between bereavement and these two neurocognitive outcomes. However, in sensitivity analyses that filtered the bereaved sample based on maternal-reported influence of death, bereaved children who were substantially impacted by the loss demonstrated significantly lower matrix reasoning scores than their non-bereaved counterparts, even after adjusting for pre-bereavement IQ and mental health symptoms (Tables S6, S7).
Table 3.
Association between bereavement ages 5–10 and neurocognitive outcomes at ages 12–13 (N = 1734) after adjustment for potential confounders.
| Outcome | Model | Estimate | SE | p-value |
|---|---|---|---|---|
| WISC MR T-score | Adjusted + IQ | −0.22 | 0.15 | 0.13 |
| Adjusted + CBCL | −0.25 | 0.15 | 0.09* | |
| Adjusted + CBCL + IQ | −0.22 | 0.15 | 0.13 | |
| WISC Estimated FSIQ | Adjusted + IQ | −0.32 | 0.66 | 0.63 |
| Adjusted + CBCL | −0.60 | 0.70 | 0.39 | |
| Adjusted + CBCL + IQ | −0.35 | 0.66 | 0.59 |
*Associations are nominally significant at the .05 level, accounting for the fact that multiple tests were conducted. WISC = Weschler Intelligence Scale for Children; FSIQ = full scale intelligence quotient; MR = Matric reasoning. Models include the following covariates: child sex, parental national origin, maternal psychopathology, household income, maternal education, and maternal marital status. As specified, models also include IQ and/or CBCL scores at age 5.
Discussion
We found that among bereaved youth in this birth cohort, 11 (1.4%) experienced the death of a parent or caregiver, a proportion consistent with prior prevalence estimates in a general Scottish population, where 1.3% of children had experienced the death of a parent by age 1033. Although bereavement was not associated with school performance or academic underachievement, we did find that bereaved children had an on average 1.12 point lower FSIQ score than their non-bereaved counterparts, which was largely driven by lower fluid reasoning scores as indexed by a test of visual-spatial reasoning, the matrix reasoning subtest of the WISC. Interestingly, estimates remained similar after adjustment for sociodemographic characteristics. Estimates dropped below the level of statistical significance after adjusting for earlier nonverbal IQ and mental health problems, consistent with prior findings33, but only when bereavement was of no or little influence on the current functioning of the child (as rated by a caregiver). However, when caregivers reported that the bereavement was still of considerable influence on the child, these children had lower FSIQ and matrix reasoning scores even after adjustment for pre-bereavement nonverbal IQ and mental health problems. Building on a growing body of literature about the effects of bereavement in early life, these novel findings shed light on the effect of bereavement on cognitive development in a general population sample of Dutch youth.
These findings are consistent with previous studies in pediatric samples showing that bereavement was associated with subsequently elevated depressive and anxiety symptoms, lower lifelong educational attainment, and reduced general developmental competence5–7. Although studies in adults have previously shown that experiencing bereavement was associated with lower odds of obtaining a college degree, fewer years of education, and worse neurocognitive function8,14,16,34, this study is the first to observe a relationship between bereavement and cognitive functioning—in particular fluid reasoning—in childhood. This is in line with research on childhood adversities more generally and their effects on later cognitive functioning38.
While we had hypothesized an effect of bereavement on school performance, we did not find an association in the present study. We propose two possible explanations. First, the most robust evidence in the literature addresses educational attainment5, yet educational attainment and academic performance are not exchangeable. Children may complete fewer years of schooling for reasons not associated with academic performance. Therefore, the mechanisms underlying the association between bereavement and reduced educational attainment may be independent of academic performance. Second, the existing research on academic performance among bereaved youth has yielded mixed results. While a recent systemic review noted an association between bereavement and reduced educational performance, results from other studies have been mixed37. For example, one study found that the effects of bereavement on educational performance varied by child sex38. Other studies have shown that in the event of maternal suicide, the effects on reduced academic performance among youth were null when controlling for maternal depression39. Therefore, we suggest that while our results here are somewhat unexpected, in the context of a mixed literature base it may be that there are unmeasured associations that have yet to be identified and should be a focus of future research.
While speculative, results may be used to inform future research focused on mechanisms of risk for adverse health outcomes, as well as protective factors, among bereaved youth. Previous studies have shown that bereavement itself is prospectively associated with more mental health problems, which could result in poorer attention span at school, and hence, reduced cognitive stimulation and lower lifelong educational attainment. Future studies are needed to disentangle these and other potential mechanisms of risk. For example, longitudinal repeated assessments of cognitive function are needed to examine the issue of timing of bereavement in relation to normative development of cognitive functions, such as fluid reasoning. In addition, it will be important to study the immediate and long-term effects of bereavement, also considering that the current diagnostic classification criteria for prolonged grief disorder specify that a year must have passed before this DSM-5-TR disorder can be classified. Previous studies have shown that pre-trauma psychopathology is related to worse post-trauma effects among adults40, our findings suggest a somewhat different pattern. We found that youth bereavement rated by parents as moderate to severe was associated with poorer cognitive functioning even when adjusting for pre-bereavement mental health problems and cognitive ability. It may be that the developmental perspective is especially salient in accurately identifying risk factors for post-bereavement psychopathology given the rapid neurodevelopment context relevant to children and youth. Second, our results suggest further research targeting visual spatial functioning may be warranted. Visual spatial development accelerates between the ages of 10 and 13 among typically developing children41, so it may be a sensitive period when youth might be vulnerable to adverse effects of interpersonal loss. Finally, our results suggest further research on a protective effect of nonverbal cognitive ability, emerging as early as 5 years of age, against adverse effects of childhood bereavement.
Clinically, childcare professionals such as healthcare workers, social workers, and teachers, should be mindful of the cognitive development of bereaved children. Even though prior research has shown that most children do not develop mental health problems following bereavement4, a subset of bereaved youth who experience the long-term negative impact of bereavement could potentially benefit from careful monitoring of cognitive, social, and physical development. Our results are in line with a broader literature42 documenting the relationship between stressful life events and cognitive development, suggesting that educational experts and childcare providers may also consider screening for educational support among bereaved youth. It should, however, be borne in mind that the estimates from this study were small, would not survive correction for multiple testing, and that many other factors not considered in the current investigation likely play a role in cognitive development following bereavement.
Our study was characterized by a relatively large sample size, a prospective design that allowed us to determine the directionality of effects, as well as adjust for several important confounders including early childhood cognition and mental health problems. Despite these strengths, there were also several limitations to consider. First, selective loss to follow-up before the study assessment of experiencing bereavement could have biased our estimates, limiting the generalizability of our study. However, very similar proportions of bereaved and non-bereaved youth had data available on neurocognitive and scholastic functioning outcomes (40% vs. 38%) mitigating the potential bias of our observed associations. Second, although we had data on parental bereavement, we did not have information on the type of relationship that the child had with the deceased loved one. These could have included grandparents, siblings, other family members or friends, and yet were not able to stratify our analyses by relationship type to investigate the potential differential association between the type of relationship and the effect of that loss on the child. Further, the quality of the relationships or the extent of caregiving provided in the child’s life was not measured relative to the identified deceased loved one, which could be relevant with respect to the impact of the bereavement. Third, although we adjusted for several covariates, we cannot rule out the potential effects of genetic and unmeasured environmental confounding. Although we adjusted for parental psychopathology in our models, parental negative affect could have biased their assessment of the impact of bereavement on their child. Finally, the correlation between nonverbal cognitive ability at age 5/6 and 13 was moderate in this sample (r = 0.48), suggesting caution interpreting findings. However, it should be noted that these were quite different tests and subtests (e.g. non-verbal vs. combined verbal/non-verbal cognitive), therefore lower correlations would be expected.
In summary, leveraging prospective data from a population-based sample of children, we found that bereavement was to a small extent associated with poorer cognitive functioning, in particular fluid reasoning. Bereavement was not associated with poorer school performance or academic underachievement. These results contribute to a growing body of literature dedicated to characterizing the association between bereavement on physical and mental health in population-based datasets.
Supplementary Information
Acknowledgements
CAD is supported by the National Institute of Mental Health (K23MH117278). ALED is supported by the National Institute of Mental Health (T32 MH 017119).
Author contributions
Conceptualization (C.A.D., H.T.); Methodology (C.A.D., K.B., A.L.E.D.); Investigation (A.L.E.D., K.B., C.A.D.); Data Curation (K.B., A.L.E.D.); Writing—Original Draft (C.A.D., A.L.E.D., K.B.); Writing—Review and Editing (P.J., H.T., C.A.D., A.L.E.D., K.B.); Supervision (C.A.D., P.J., H.T.); Project Administration (C.A.D., K.B., P.J.).
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: K. Bolhuis and A. L. Espinosa Dice.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-72178-5.
References
- 1.Burns, M., Griese, B., King, S. & Talmi, A. Childhood bereavement: Understanding prevalence and related adversity in the United States. Am. J. Orthopsychiatry90(4), 391–405 (2020). 10.1037/ort0000442 [DOI] [PubMed] [Google Scholar]
- 2.Paul, S. & Vaswani, N. The prevalence of childhood bereavement in Scotland and its relationship with disadvantage: the significance of a public health approach to death, dying and bereavement. Palliat. Care Soc. Pract.14, 2632352420975043 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaplow, J. B., Saunders, J., Angold, A. & Costello, E. J. Psychiatric symptoms in bereaved versus nonbereaved youth and young adults: A longitudinal epidemiological study. J. Am. Acad. Child Adolesc. Psychiatry49(11), 1145–1154 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Espinosa Dice, A. L. et al. Correction: Resilient phenotypes among bereaved youth: A comparison of trajectory, relative, and cross-domain approaches. Child Adolesc. Psychiatry Ment. Health.17(1), 39 (2023). 10.1186/s13034-023-00582-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burrell, L. V., Mehlum, L. & Qin, P. Educational attainment in offspring bereaved by sudden parental death from external causes: A national cohort study from birth and throughout adulthood. Soc. Psychiatry Psychiatr. Epidemiol.55(6), 779–788 (2020). 10.1007/s00127-020-01846-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prix, I. & Erola, J. Does death really make us equal? Educational attainment and resource compensation after paternal death in Finland. Soc. Sci. Res.64, 171–183 (2017). 10.1016/j.ssresearch.2016.10.012 [DOI] [PubMed] [Google Scholar]
- 7.Brent, D. A., Melhem, N. M., Masten, A. S., Porta, G. & Payne, M. W. Longitudinal effects of parental bereavement on adolescent developmental competence. J. Clin. Child Adolesc. Psychol.41(6), 778–791 (2012). 10.1080/15374416.2012.717871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thyden, N. H., Schmidt, N. M. & Osypuk, T. L. The unequal distribution of sibling and parent deaths by race and its effect on attaining a college degree. Ann. Epidemiol.45, 76–82 (2020). 10.1016/j.annepidem.2020.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wade, M., Wright, L. & Finegold, K. E. The effects of early life adversity on children’s mental health and cognitive functioning. Transl. Psychiatry.12(1), 244 (2022). 10.1038/s41398-022-02001-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonough, P., Duncan, G. J., Williams, D. & House, J. Income dynamics and adult mortality in the United States, 1972 through 1989. Am. J. Public Health.87(9), 1476–1483 (1997). 10.2105/AJPH.87.9.1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bosma, H., van de Mheen, H. D., Borsboom, G. J. & Mackenbach, J. P. Neighborhood socioeconomic status and all-cause mortality. Am. J. Epidemiol.153(4), 363–371 (2001). 10.1093/aje/153.4.363 [DOI] [PubMed] [Google Scholar]
- 12.Hall, C. A. et al. Cognitive functioning in complicated grief. J. Psychiatr. Res.58, 20–25 (2014). 10.1016/j.jpsychires.2014.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Connor, M. F. & Arizmendi, B. J. Neuropsychological correlates of complicated grief in older spousally bereaved adults. J. Gerontol. B Psychol. Sci. Soc. Sci.69(1), 12–18 (2014). 10.1093/geronb/gbt025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xavier, F. M. F., Ferraz, M. P. T., Trentini, C. M., Freitas, N. K. & Moriguchi, E. H. Bereavement-related cognitive impairment in an oldest-old community-dwelling Brazilian sample. J. Clin. Exp. Neuropsychol.24(3), 294–301 (2002). 10.1076/jcen.24.3.294.983 [DOI] [PubMed] [Google Scholar]
- 15.Saavedra Pérez, H. C. et al. Cognition, structural brain changes and complicated grief. A population-based study. Psychol. Med.45(7), 1389–1399 (2015). 10.1017/S0033291714002499 [DOI] [PubMed] [Google Scholar]
- 16.Liu, H., Lin, Z. & Umberson, D. Parental death and cognitive impairment: An examination by gender and race-ethnicity. J. Gerontol. B Psychol. Sci. Soc. Sci.10.1093/geronb/gbab125 (2021). 10.1093/geronb/gbab125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel, P. & Oremus, M. The association between adverse childhood experiences and late-life cognition: A systematic review of cross-sectional and case-control studies. Gerontologist.63(6), 1087–1103 (2023). 10.1093/geront/gnac041 [DOI] [PubMed] [Google Scholar]
- 18.Glymour, M. M. & Manly, J. J. Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychol. Rev.18(3), 223–254 (2008). 10.1007/s11065-008-9064-z [DOI] [PubMed] [Google Scholar]
- 19.Jaddoe, V. W. V. et al. The Generation R Study: design and cohort update 2012. Eur. J. Epidemiol.27(9), 739–756 (2012). 10.1007/s10654-012-9735-1 [DOI] [PubMed] [Google Scholar]
- 20.Kooijman, M. N. et al. The Generation R Study: design and cohort update 2017. Eur. J. Epidemiol.31(12), 1243–1264 (2016). 10.1007/s10654-016-0224-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amone-P’Olak, K. et al. Life stressors as mediators of the relation between socioeconomic position and mental health problems in early adolescence: The TRAILS study. J. Am. Acad. Child Adolesc. Psychiatry48(10), 1031–1038 (2009). 10.1097/CHI.0b013e3181b39595 [DOI] [PubMed] [Google Scholar]
- 22.Blok, E. et al. Cognitive performance in children and adolescents with psychopathology traits: A cross-sectional multicohort study in the general population. Dev. Psychopathol.35(2), 926–940 (2023). 10.1017/S0954579422000165 [DOI] [PubMed] [Google Scholar]
- 23.van der Lubbe M. The End of Primary School Test. Cito; 2007.
- 24.de Wijs A. VBHER&. Wetenschappelijke Verantwoording van de Eindtoets Basisonderwijs 2010. Cito; 2011.
- 25.Steenkamp, L. R. et al. Psychotic experiences and future school performance in childhood: a population-based cohort study. J. Child Psychol. Psychiatry62(3), 357–365 (2021). 10.1111/jcpp.13281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schuurmans, I. K. et al. Child mental health problems as a risk factor for academic underachievement: A multi-informant, population-based study. Acta Psychiatr. Scand.145(6), 578–590 (2022). 10.1111/acps.13426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Netherlands S. Immigrants in the Netherlands (Allochtonen in Nederland). Statistics Netherlands (Centraal Bureau voor de Statistiek); 2004.
- 28.Centraal Bureau voor de Statistiek (CBS)/Sociaal en Cultureel Planbureau (SCP). Armoedesignalement [Poverty Survey 2013].; 2013.
- 29.Derogatis, L. R. & Melisaratos, N. The Brief Symptom Inventory: an introductory report. Psychol. Med.13(3), 595–605 (1983). 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- 30.Achenbach TM, Rescorla L. Manual for the ASEBA School-Age Forms & Profiles: An Integrated System of Multi-Informant Assessment. ABESA; 2001.
- 31.Tellegen, P.J., Winkel, M., Wijnberg-Williams, B.J., & Laros, J.A. Snijders-Oomen Niet-Verbale Intelligentietest SON-R 2, 5–7. Boom Testuitgevers; 2005.
- 32.Li, D. et al. Assessment of treatment effect with multiple outcomes in 2 clinical trials of patients with duchenne muscular dystrophy. JAMA Netw. Open.3(2), e1921306 (2020). 10.1001/jamanetworkopen.2019.21306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Denckla, C. A., Espinosa Dice, A. L., Slopen, N., Koenen, K. C. & Tiemeier, H. Mental health among bereaved youth in the ALSPAC birth cohort: Consideration of early sociodemographic precursors, cognitive ability, and type of loss. Dev. Psychopathol.2023, 1–12 (2023). 10.1017/S0954579423000512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Høeg, B. L. et al. Does losing a parent early influence the education you obtain? A nationwide cohort study in Denmark. J. Public Health.41(2), 296–304 (2019). 10.1093/pubmed/fdy070 [DOI] [PubMed] [Google Scholar]
- 35.Su, Y., D’Arcy, C., Yuan, S. & Meng, X. How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. J. Affect. Disord.252, 278–293 (2019). 10.1016/j.jad.2019.04.026 [DOI] [PubMed] [Google Scholar]
- 36.Lund, J. I., Toombs, E., Radford, A., Boles, K. & Mushquash, C. Adverse childhood experiences and executive function difficulties in children: A systematic review. Child Abuse Negl.106, 104485 (2020). 10.1016/j.chiabu.2020.104485 [DOI] [PubMed] [Google Scholar]
- 37.Elsner, T. L., Krysinska, K. & Andriessen, K. Bereavement and educational outcomes in children and young people: A systematic review. Sch. Psychol. Int.25, 01430343211057228 (2021). [Google Scholar]
- 38.Abdelnoor, A. & Hollins, S. The effect of childhood bereavement on secondary school performance. Educ. Psychol. Pract.20(1), 43–54 (2004). 10.1080/0266736042000180401 [DOI] [Google Scholar]
- 39.Geulayov, G., Metcalfe, C. & Gunnell, D. Parental suicide attempt and offspring educational attainment during adolescence in the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort. Psychol. Med.46(10), 2097–2107 (2016). 10.1017/S0033291716000556 [DOI] [PubMed] [Google Scholar]
- 40.Gradus, J. L. et al. Pre-trauma predictors of severe psychiatric comorbidity 5 years following traumatic experiences. Int. J. Epidemiol.51(5), 1593–1603 (2022). 10.1093/ije/dyac030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mous, S. E. et al. The association of gender, age, and intelligence with neuropsychological functioning in young typically developing children: The Generation R study. Appl. Neuropsychol. Child6(1), 22–40 (2017). 10.1080/21622965.2015.1067214 [DOI] [PubMed] [Google Scholar]
- 42.Denckla, C. A. et al. Patterning of individual variability in neurocognitive health among South African women exposed to childhood maltreatment. Sci. Rep.11(1), 6669 (2021). 10.1038/s41598-021-85979-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


