Abstract
BACKGROUND:
Eliminating financial barriers and improving healthcare accessibility pertain to be key elements of the United Nation’s sustainable development goals. These have directed health policymakers to advocate private health insurance as a health promotion strategy to enable patients to obtain absolute and affordable medical care when needed. Against this backdrop, the current study investigates the coverage trend and financial risk-protective nature of private health insurance plans.
MATERIALS AND METHOD:
We examined 12 months’ hospital billing data of private health insurance holders with cancer, cardiac, neurological, and renal diseases. The billing and insurance claim data of 5002 patients were extracted from the billing section of a tertiary care teaching hospital located in southern India from April 2022 through March 2023. Five per cent of patients from each disease condition were selected through proportionate random sampling for analysis (n = 250). The cost incurred and reimbursement trend under various cost heads were investigated by examining the cost incurred by the patient during the hospitalization and comparing it with the amount reimbursed by the insurance company.
RESULTS:
The scrutiny exhibits that private health insurance fails to provide comprehensive coverage, resulting in under-insurance among subscribers. Reimbursement received for each cost category is also discussed. To the best of our knowledge, this is the first study that has used institutional data instead of large survey data or patient data.
CONCLUSION:
The research concludes by soliciting policymakers, healthcare providers, and insurers to develop strategies to enhance the affordability and accessibility of healthcare to promote health and wellness.
Keywords: Cost of disease, health promotion, out-of-pocket expenditure, under-insurance, private health insurance
Introduction
Global demand for health insurance coverage is increasing rapidly[1] across lower-middle-income countries (LMICs)[2,3] owing to the catastrophic financial repercussions of ill health. Additionally, the economic burden of disease conditions[4,5,6,7] and partial insurance coverage[8,9] warrant immediate action to expand health insurance coverage to prevent the likely financial catastrophe. However, LMICs, which largely depend on private health expenditure (PHE) as a share of total health expenditure, are still far from attaining universal health coverage (UHC). PHE has a significant contribution from private health insurance (PHI), which entails a regressive type of pre-payment with a compromised risk-sharing strategy compared to Government Sponsored Health Insurance (GSHI).[10,11,12] Hence, PHI is not considered a suitable means for achieving UHC for countries with a huge economic burden of chronic ailments.[4,6,10] On the contrary, scholars have endorsed PHI as a health promotion strategy to enable patients to obtain absolute and affordable medical care when needed.[13,14,15] Against this backdrop, the current study investigates the reimbursement pattern and impact of PHI in chronic ailments by analyzing the hospital’s billing data.
The existing literature is skewed toward GSHI. Such insights, inter alia, cover the assessment of the economic burden of chronic ailments[4,6,7,10] and the impact of health insurance.[3,8,9,16,17,18,19,20] Severe financial toxicity has been observed among cancer patients with larger family members, undergoing multiple chemotherapy cycles and accessing private healthcare facilities.[6] A recent review has also pointed out the prevalence of health coverage disruption among the low-income quintiles with cancer adversely affecting the continuum of care.[17]
Evidence from India, regarding the role of GSHI among cancer and cardiac conditions, has reported a minimal reduction in out-of-pocket cost (OOPC).[20] They have suggested the broadening of coverage owing to the soaring out-patient costs. Bodhisane[18] and Ma et al.[19] highlighted the dual outcome of health insurance, which reflected an increase in healthcare accessibility among cardiovascular patients, while financial protection remains questionable.
Discussing the inefficiency of GSHI in preventing financial calamity, among healthcare seekers with chronic ailments, researchers have investigated the outcome of multiple strategies in containing healthcare costs.[18,21,22,23] Likewise, Wu et al.[22] have hinted at the potential of PHI as a supplementary aid in financial risk protection across high-income countries. Sugunan et al.’s[23] qualitative literature synthesis reveals that the effectiveness of PHI, in providing financial protection against healthcare costs, is not well-researched across LMICs. Though Sonymol[3] scrutinized the cost components of GSHI and PHI from the patient’s perspective, the study failed to assess the financial risk-protective nature of PHI. This demands a fresh insight into the role of PHI in reducing costs across chronic ailments by investigating institutional-level data. Hence, the current study answers the following research questions:
What is the reimbursement pattern toward healthcare costs incurred by PHI holders with chronic diseases?
What is the disease-specific impact on insurance coverage?
This study makes a few contributions to the literature. The first is its innovative methodology to evaluate the role of PHI using institutional data. Despite significant contributions to the outcomes of private health insurance, methodological concerns are extant due to the limitation of data collection techniques used in large-scale surveys. Scholars have challenged the credibility of primary data obtained through surveys owing to its inherent recall bias.[24,25,26,27,28] Berete et al.[27], Sinha[29] and Wagstaff[30] also have questioned this obscurity in information extracted from large-scale national surveys. This demands a fresh insight into the role of private health insurance in allaying healthcare costs by evaluating data available at the institutional level. The current study is an earnest endeavor in this regard. Second, disclosure of reimbursement patterns under different cost categories may aid health policymakers in designing optimized health plans for their subscribers. Third, from a consumer perspective, insights from this study could help understand the dynamics of reimbursement, which, in turn, can nudge the choice of an optimal healthcare plan in the future. This paper also adds to the body of knowledge in sustainable development goal 3 (Global health and wellbeing) in addressing UHC.
Materials and Methods
Study design and settings
This was a cross-sectional study where 1-year billing information of PHI holders, hospitalized with cardiac, cancer, renal, and neurological ailments, was investigated. The billing and insurance claims of patients hospitalized during 2022–2023 in a multi-speciality tertiary care teaching hospital located in a coastal district of South India were extracted. The selected institution is a 2000-bed multi-speciality teaching hospital with out-patient visits of more than six lakh in a year. Moreover, the hospital delivers multiple and diverse partnerships with insurance companies, providing services to more than 15 health insurance companies. The billing data of insured patients were extracted from the health information system and the insurance database of the hospital.
Study participants and sampling
The hospital had 5002 in-patients with chronic disease conditions subscribed to PHI during the study period. Hence, the sampling frame consisted of 5002 patients. Five per cent of the sampling frame (n = 250) was considered for the analysis. The sampling design was proportionate random sampling. Details are given in Table 1.
Table 1.
Number of patients subscribed to PHI and the selected cases
| Disease conditions | Total cases | Selected cases (5% of total) |
|---|---|---|
| Cardiac ailments | 1497 | 75 |
| Cancer ailments | 1727 | 86 |
| Renal ailments | 1418 | 71 |
| Neurological ailments | 360 | 18 |
| Total | 5002 | 250 |
Source: Present study
Data collections tools and technique
The study’s data were extracted from the billing and insurance records of the hospital between April 2022 to March 2023. These records encompass detailed information about reimbursements issued by health insurance companies across specific cost categories. They also conferred comprehensive insights into costs accrued and reimbursements associated with patient services, pharmacy charges, consumables utilized during in-patient care, and room rent. The data acquisition process occurred in two distinct phases, ensuring a comprehensive exploration of the financial dynamics within the specified period, as indicated below [Figure 1].
Figure 1.
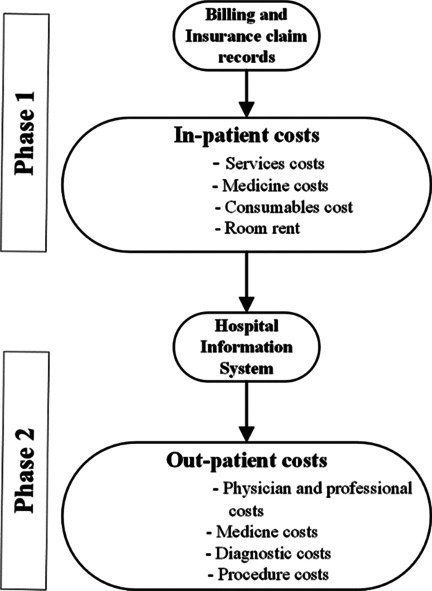
Phases of data collection
Phase 1: In-patient cost: The in-patient costs consisted of the expenses incurred by the patients during the period of hospitalization categorized into four cost categories (services, medicine, consumables, and room rent), where the reimbursed amount and patient’s share were detailed.
Phase 2: Out-patient cost: The in-patient costs excluded information on patients’ spending on services received on an out-patient basis. We extracted the data from the hospital information system using patients’ unique identification codes. This included the cost incurred for the purchase of medicine, diagnostic services, interventions or procedures accessed, and physician and other professional charges.
Definition of terms
Total hospital cost (THC): The in-patient and out-patient expenditure incurred by the patient during the period of hospitalization. This information was collected for a period of 4 months, including 1 month before the admission and 3 follow-up months.[31]
OOPC: The cost incurred by the in-patient after receiving reimbursement from the health insurance company.[32]
-
Total in-patient costs (TICs): The cost incurred for service availed as in-patient was categorized into four sub-costs [Table 2].[33]
Package cost: The cost of the pre-defined package of services tailored for the treatment of a particular ailment. Predominantly packages for cardiac ailments.
Service cost: This mainly involved administrative and equipment costs such as admission charges, diagnostic and laboratory charges, and physicians and other professional charges.
Consumables cost: The cost charged by the hospitals for the utilization of consumable items such as personal protective equipment, bedpans, gauze pieces, and so on.
Pharmacy costs: The amount charged by the hospitals for the medicines consumed by the patient during the period of hospitalization on an in-patient basis. Here, the medicine purchased by the patient on an out-patient basis is not considered.
Room cost: The cost charged by the hospital for the utilization of bed facilities by the patient. This covered the cost incurred for the utilization of patient beds in general wards, emergency rooms, semi-special rooms, and special and deluxe rooms.
Reimbursed amount: This included the cost reimbursed by the health insurance company under different cost heads.[32]
Table 2.
Calculation of healthcare expenditure
| Total Hospital Costs | Out-patient cost + Total in-patient Cost |
|---|---|
| Out-of-Pocket Cost | Total Hospital Costs – Reimbursed amount |
| Total In-patient Costs | Package cost + Service cost + Consumable cost + Pharmacy cost + Room cost |
Source: present study
We used R (V.2.4.0) for coding and analysis of the captured data. The expenditures incurred were presented in mean and median estimates. The data of 250 patients were used to estimate the reimbursement provided by the insurance company and patient share toward the expenditure incurred. The cost incurred was calculated as follows:
Ethical consideration
The study received the required ethics approval from the “Institutional Ethics Committee, Kasturba Hospital and Kasturba Medical College”, Karnataka, India, with ethics code number IEC: 346/2021.
Results
Private health insurance reimbursement pattern among chronic ailment patients
This section outlines the total in-patient cost and reimbursement received for PHI holders hospitalized with chronic ailments. The highest in-patient cost experienced by patients hospitalized is with renal ailments (median = $880) and cardiac ailments (median = $775), respectively. The median expenditure for patients with cancer and neurological ailments is $267 and $658, respectively. The PHI reimburses the in-patient costs incurred by the patient’s plans under five cost heads: “Packages”, “Services”, “Consumables”, “Medicine,” and “Room”. The highest coverage is accorded to the services received for renal ailments (median = $685). Similarly, regarding the cost incurred for medicine, PHI holders received a median coverage of $79, where the patient share is $25. Looking at the total in-patient cost, the PHI holders received a median reimbursement of $815 for renal ailments [Table 3].
Table 3.
Private health insurance reimbursement pattern against in-patient expenditure (amount in $)
| Disease Conditions | Packages |
Services |
Pharmacy |
Consumables |
Room |
Total In-patient cost |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reimbursed amount | Patient share | Reimbursed amount | Patient share | Reimbursed amount | Patient share | Reimbursed amount | Patient share | Reimbursed amount | Patient share | Reimbursed amount | Patient share | Total | |
| Cardiac | |||||||||||||
| Min | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 172.06 |
| Median (Mean) | 179 (467) | 0 (4) | 407 (667) | 0 (150) | 90 (322) | 51 (193) | 21 (64) | 0 (43) | 0 (25) | 7 (57) | 697 (1545) | 58 (447) | 775 (1992) |
| Max | 1274 | 192 | 4510 | 5121 | 3142 | 2071 | 654 | 1259 | 543 | 1968 | 10419 | 5572 | 12040 |
| SD | 433 | 24 | 853 | 754 | 473 | 337 | 130 | 161 | 83 | 230 | 1631 | 703 | 1922 |
| Cancer | |||||||||||||
| Min | - | - | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 32 | 0 | 44 |
| Median (Mean) | - | - | 165 (424) | 2 (46) | 81 (215) | 9 (64) | 0.66 (25) | 0.048 (13) | 0 (12) | 10 (34) | 246.66 (676) | 21 (157) | 267 (833) |
| Max | - | - | 2586 | 1167 | 2656 | 1035 | 227 | 21 | 264 | 477 | 5019 | 2406 | 5496 |
| SD | - | - | 582.78 | 165.26 | 419.47 | 156.03 | 38.41 | 42.78 | 34.08 | 64.02 | 847.63 | 348.40 | 971 |
| Renal | |||||||||||||
| Min | - | - | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 63.23 | 0 | 7.21 |
| Median (Mean) | - | - | 685 (428) | 7 (18) | 79 (113) | 25 (76) | 51 (77) | 0 (17) | 0 (19) | 33 (55) | 815 (637) | 65 (227) | 880 (864) |
| Max | - | - | 2600 | 142 | 778 | 1365 | 884 | 223 | 161 | 332 | 3774 | 1582 | 1969 |
| SD | - | - | 444 | 28 | 131 | 197 | 131 | 34 | 39 | 66 | 619 | 233 | 444 |
| Neurological | |||||||||||||
| Min | - | - | 143 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | 0 | 12 | 187 |
| Median (Mean) | - | - | 400 (539) | 3 (14) | 132 (273) | 0 (77) | 15 (64) | 0 (24) | 54 (99) | 46 (68) | 601 (972) | 57 (183) | 658 (1155) |
| Max | - | - | 2475 | 126 | 1759 | 466 | 334 | 255 | 722 | 240 | 3753 | 846 | 4599 |
| SD | - | - | 542 | 3 | 132 | 0 | 15 | 0 | 54 | 46 | 905 | 224 | 1069 |
Source: the present study (₹1=$ 0.012)
For cancer conditions, the highest coverage is provided for the cost incurred for services (median = $165), followed by medicine (median = $81). Coverage is significantly low for consumables and beds, where the patient’s share remains higher with a median cost of $10. Most cardiac cases are provided with treatment packages where PHI plans provide full coverage. However, this pattern is not followed in other disease conditions. The median reimbursement received under the package category for cardiac patients is $697, and the median expenditure incurred is estimated at $58. The insurance has covered a major share incurred for services (median = $407), medicines (median = $90), and consumables (median = $21). A similar pattern is observed for patients hospitalized with neurological ailments where health insurance has reimbursed a larger share of the cost incurred for services (median = $400) and medicines ($132). In a nuanced examination of the data, it has been ascertained that despite the minimal coverage offered against bed-related expenses, the patient’s financial burden continues to soar across all disease conditions.
Disease-based out-patient cost, THC, and insurance coverage
This section deals with the THC incurred by the patients, including the out-patient cost. The out-patient cost is calculated based on the payment done by the patients for diagnosis, purchase of medicine, or procedures related to the ailment on an out-patient basis. The data divulge that the patients have chosen health insurance premiums that have limited or no coverage over out-patient costs. This has resulted in a huge impact on the THC and OOPC for the patients. The median out-patient cost incurred for the patient is estimated at $109.
Patients with cancer ailments have reported the highest median out-patient cost ($356), followed by patients with neurological ailments ($149). The lowest out-patient cost is reported by patients who underwent treatment for cardiac ailments ($48) [Table 4]. Likewise, patients hospitalized for renal conditions have reported out-patient costs of $113.
Table 4.
Total healthcare cost and insurance coverage (amount in $)
| Disease Conditions | Numerical Summaries | Out-patient cost | In-patient cost | Total Hospital Cost (OPC + IPC) | Reimbursed Amount | OOPC |
|---|---|---|---|---|---|---|
| Cardiac | Min | 0 | 172.06 | 200 | 0 | 9 |
| Median (Mean) | 48 (79) | 775 (1992) | 823 (2071) | 697 (1545) | 129 (526) | |
| Max | 838 | 12040 | 12040 | 10419 | 5718 | |
| SD | 123 | 1922 | 1919 | 1631 | 714 | |
| Cancer | Min | 31 | 44 | 200 | 32 | 37 |
| Median (Mean) | 356 (518) | 267 (833) | 623 (1351) | 247 (676) | 376 (675) | |
| Max | 3132 | 5496 | 5920 | 5019 | 3170 | |
| SD | 533 | 971 | 1160 | 847.63 | 695 | |
| Renal | Min | 7 | 7.21 | 116 | 63.23 | 41 |
| Median (Mean) | 113 (276) | 880 (864) | 993 (1140) | 815 (637) | 178 (503) | |
| Max | 1967 | 1969 | 5417 | 3774 | 2574 | |
| SD | 444 | 444 | 944 | 619 | 520 | |
| Neurological | Min | 11 | 187 | 277 | 0 | 85 |
| Median (Mean) | 169 (333) | 658 (1155) | 827 (1488) | 601 (972) | 226 (516) | |
| Max | 2950 | 4599 | 4863 | 3753 | 2989 | |
| SD | 661 | 1069 | 1236 | 905 | 661 |
Source: the present study
Table 4 depicts the median insurance coverage for THC with respect to the identified disease conditions. It is to be noted that despite being insured, the OOPC is prevalent. It varies from $129 for patients with cardiac ailments to $376 for patients hospitalized due to cancer conditions. Patients with renal ailments have experienced the least OOPC (median = $178), while patients with neurological ailments have an OOPC of $226. The results highlight that the insurance coverage opted by the patients has limited reimbursement of out-patient costs. Therefore, under-insurance is observed among PHI holders. Hence, the burden of expenditure for healthcare seeking of private insurance holders is discerned to be substantially high.
Discussion
One of the key findings of this research is the unraveling of the reimbursement pattern received by patients with cardiac, cancer, renal, and neurological ailments and who have subscriptions with PHI. This helps health policymakers design optimum health insurance plans based on utilization and reimbursement trends. Our argument is consistent with Baione’s[34] observation regarding the role of various “reimbursement rules” in designing optimal health insurance plans. The total health expenditure and out-patient costs experienced by PHI holders with chronic disorders were also depicted. The results disclosed that when the costs for services and medicines received significant coverage, the costs for consumables and room rent received minimal weightage, resulting in a major contribution to total healthcare costs. These observations are consistent with past studies which underscore the role of room cost and other non-medical costs in escalating the economic burden among insurance holders with chronic ailments.[20,26,35,36] However, Stadhouders[37] ascribe only an insignificant role to room cost in healthcare cost escalation. Another possibility of high patient share toward bed cost is increased utilization of intensive care units and the upgradation of in-patient bed facilities from general wards to deluxe or super deluxe rooms, which is not covered in the health insurance plans opted. This trend has been previously reported among healthcare seekers with chronic ailments in different research settings.[38]
In our study, the highest in-patient costs were reported by PHI holders with renal, cardiac, and neurological disorders. We retrospect similar findings reported in India[28,39] and a few developed nations.[40,41] Though the PHI has covered the cost incurred under “packages” for cardiac patients, the OOPC is prevalent due to lower coverage for other cost heads. For other diseases, partial coverage was provided toward the costs incurred for services, consumables, and medicine.
The analysis of the out-patient costs revealed that cancer conditions outweighed all other disease conditions, followed by neurological ailments. Similar findings have been widely reported irrespective of geographical boundaries, emphasizing the burden of out-patient costs among chronic ailments.[42,43,44] However, these studies did not report the insurance status of the study participants. Also, the pernicious effects of out-patient charges have been proclaimed by Sabermahani[36] and Ayogu et al.[45] with a focus on uninsured or insured by not-for-profit health plans.
Though PHI provides minimal protection for in-patient expenditure, low coverage toward out-patient costs and non-medical expenditures (consumables and room costs) in total healthcare costs are highlighted in our study. This can be related to the findings of Peng[26] and Gambhir et al.,[46] which have depicted the inefficiency of PHI in providing out-patient coverage to the increasing demand. Our findings have validated the past observations regarding the unsuitability of PHI as a solution to achieve UHC.[4,6,12] Moreover, our findings reiterate Gambhir et al.’s[46] and Balqis-Ali NZ et al.’s[47] argument about the quantitative welfare gains of top-up insurance as the standard full-coverage policy will be ineffective in covering the anticipated highly expensive treatment options for chronic illness.
Limitations and recommendation
This study is not free from limitations. We did not include the costs incurred by patients to visit other healthcare settings. For example, a patient is likely to seek medical support from other service providers. This might have underestimated the total healthcare cost and share of health insurance. The present study could not capture the full episodes of hospitalization pertaining to a disease condition but rather only part thereof. Therefore, the total expenditure and reimbursement received are not captured. However, to the best of our knowledge, this is the first study that assessed the reimbursement trends received by PHI holders hospitalized with chronic diseases using institutional data. Second, only a few PHI policies provide minimal coverage for out-patient services at higher premiums, which are not considered.
We would like to make a few suggestions for the direction of future research from the following perspectives. Despite minimal coverage, PHI holders report OOPC among patients with chronic diseases. Low coverage toward the room costs raises a concern regarding the health insurance literacy of PHI holders. Though health insurance awareness is high, health insurance literacy requires further investigation. We propose a few research questions to set the path for future scholarly engagements. What is the intensity of OOPC faced by PHI? How far is the viability of having a top-up plan to safeguard expensive treatment options for chronic illness? Is there any association between the premium paid, sum insured, and degree of OOPC? Do the subscribers face catastrophic health expenditure (CHE) or impoverishment? Are PHI holders insurance literate? Is there any available source to improve the literacy? Is there any association between health insurance literacy and choice of PHI plans?
Conclusion
The study examined the role of PHI in alleviating financial burden among patients with chronic disease conditions. Billing information of PHI holders with cancer, renal, cardiac, and neurological disease conditions was extracted from the hospital information system and analyzed to uncover the reimbursement pattern of PHI under various cost categories. As per the author’s knowledge, this is the first attempt to showcase the contribution of PHI to healthcare costs using billing data from a healthcare setting.
Our results have affirmed the phenomenon of under-insurance among PHI holders. Inadequate coverage, coupled with unexpected health events and the resultant inevitable healthcare-seeking episodes, will have a substantial toll on patients’ economic security. Hence, this necessitates the indispensability of an auxiliary mechanism, in terms of embedded add-ons to health insurance policies, to ward off any probable financial catastrophe due to unaffordable healthcare expenses. We also appeal to an integrated solution by policymakers, insurance companies, and healthcare service providers to design a comprehensive solution to mitigate the under-insurance problem and thereby promote affordable and equitable access to health and wellness in response to the global call for universal health coverage (MDG # 3).
Ethics statement and funding
The research was rolled out after obtaining necessary institutional approval from the Institutional Ethics Committee, Kasturba Hospital and Kasturba Medical College, Manipal Academy of Higher Education, Manipal, India, vide ethics code No. 346/2021). This research has not received any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Financial support and sponsorship
The authors did not receive any financial support from any organization for the submitted work.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank the hospital administration for their invaluable support and guidance.
References
- 1.Prinja S, Bahuguna P, Gupta I, Chowdhury S, Trivedi M. Role of insurance in determining utilization of healthcare and financial risk protection in India. PLoS One. 2019;14:e0211793. doi: 10.1371/journal.pone.0211793. doi: 10.1371/journal.pone. 0211793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James N, Acharya Y. Increasing health insurance enrollment in low- and middle-income countries: What Works, What Does Not, and Research Gaps: A scoping review. Inquiry. 2022;59:469580221090396. doi: 10.1177/00469580221090396. doi: 10.1177/00469580221090396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sonymol K, Shankar R. Healthcare cost reduction and health insurance policy improvement. Value health reg Issues. 2022;29:93–99. doi: 10.1016/j.vhri.2021.10.001. doi: 10.1016/j.vhri. 2021.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P, et al. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: A systematic review. BMC Public Health. 2018;18:975. doi: 10.1186/s12889-018-5806-x. doi: 10.1186/s12889-018-5806-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kazibwe J, Tran PB, Annerstedt KS. The household financial burden of non-communicable diseases in low- and middle-income countries: A systematic review. Health Res Policy Syst. 2021;19:96. doi: 10.1186/s12961-021-00732-y. doi: 10.1186/s12961-021-00732-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donkor A, Atuwo-Ampoh VD, Yakanu F, Torgbenu E, Ameyaw EK, Kitson-Mills D, et al. Financial toxicity of cancer care in low- and middle-income countries: A systematic review and meta-analysis. Support Care Cancer. 2022;30:7159–90. doi: 10.1007/s00520-022-07044-z. doi: 10.1007/s00520-022-07044-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jabbari A, Hadian M, Mazaheri E, Jelodar ZK. The economic cost of cancer treatment in Iran. J Educ Health Promot. 2023;12:32. doi: 10.4103/jehp.jehp_928_21. doi: 10.4103/jehp.jehp_928_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Etemadi M, Shiri M, Rostami E, Mohseni M, Seyedi M. Financial burden imposed on the insured patients for private treatment: Evidence from a state of Iran. J Educ Health Promot. 2019;8:243. doi: 10.4103/jehp.jehp_285_19. doi: 10.4103/jehp.jehp_285_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Musonge-Effoe JE, Alema-Mensah E, Effoe VS, Akinnawo F, Caplan L. The association between health care coverage and prevalence of cardiovascular diseases and diabetes over a 10-year period. Prev Med. 2020;132:105983. doi: 10.1016/j.ypmed.2020.105983. doi: 10.1016/j.ypmed. 2020.105983. [DOI] [PubMed] [Google Scholar]
- 10.Kwon KN, Chung W. Effects of private health insurance on medical expenditure and health service utilization in South Korea: A quantile regression analysis. BMC Health Serv Res. 2023;23:1219. doi: 10.1186/s12913-023-10251-x. doi: 10.1186/s12913-023-10251-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Achdut L. Private expenditures on healthcare: Determinants, patterns and progressivity aspects. Isr J Health Policy Res. 2019;8:87. doi: 10.1186/s13584-019-0356-y. doi: 10.1186/s13584-019-0356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okoro R. N. Cushioning the economic burden of chronic kidney disease for patients in LMICs: The heightened need for a government-driven financial support policy. Health Policy Technol. 2021;10:100507. [Google Scholar]
- 13.Khoo J, Hasan H, Eagar K. Private versus public? Examining hospital use by a privately insured population in New South Wales, Australia, using data linkage. Aust Health Rev. 2021;45:14–21. doi: 10.1071/AH19274. doi: 10.1071/AH19274. [DOI] [PubMed] [Google Scholar]
- 14.Balqis-Ali NZ, Jailani AS, Fun WH, Jawahir S, Sararaks S, Lee GHY. Effect of supplementary private health insurance on inpatient utilisation: Evidence from Malaysia. Heliyon. 2023;9:e14025. doi: 10.1016/j.heliyon.2023.e14025. doi: 10.1016/j.heliyon. 2023.e14025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inkoom L, Ansu-Mensah M, Bawontuo V, Kuupiel D. Mapping evidence on the use of health promotion and disease prevention interventions as a strategy to sustaining pro-poor health insurance schemes: A scoping review protocol. Syst Rev. 2022;11:70. doi: 10.1186/s13643-022-01942-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sriravindrarajah A, Kotwal SS, Sen S, McDonald S, Jardine M, Cass A, et al. Impact of supplemental private health insurance on dialysis and outcomes. Intern Med J. 2020;50:542–9. doi: 10.1111/imj.14375. doi: 10.1111/imj. 14375. [DOI] [PubMed] [Google Scholar]
- 17.Yabroff KR, Reeder-Hayes K, Zhao J, Halpern MT, Lopez AM, Bernal-Mizrachi L, et al. Health insurance coverage disruptions and cancer care and outcomes: Systematic Review of Published Research. J Natl Cancer Inst. 2020;112:671–87. doi: 10.1093/jnci/djaa048. doi: 10.1093/jnci/djaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bodhisane S, Pongpanich S. The influence of the National Health Insurance scheme of the Lao People’s Democratic Republic on healthcare access and catastrophic health expenditures for patients with chronic renal disease, and the possibility of integrating organ transplantation into the health financing system. Health Res Policy Syst. 2022;20:71. doi: 10.1186/s12961-022-00869-4. doi: 10.1186/s12961-022-00869-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma M, Tian W, Kang J, Li Y, Xia Q, Wang N, et al. Does the medical insurance system play a real role in reducing catastrophic economic burden in elderly patients with cardiovascular disease in China? Implication for accurately targeting vulnerable characteristics. Global Health. 2021;17:36. doi: 10.1186/s12992-021-00683-7. doi: 10.1186/s12992-021-00683-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta R, Makkar JS, Sharma SK, Agarwal A, Sharma KK, Bana A, et al. Association of health insurance status with coronary risk factors, coronary artery disease, interventions and outcomes in India. Int J Cardiol Cardiovasc Risk Prev. 2022;14:200146. doi: 10.1016/j.ijcrp.2022.200146. doi: 10.1016/j.ijcrp. 2022.200146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jalali FS, Bikineh P, Delavari S. Strategies for reducing out of pocket payments in the health system: A scoping review. Cost Eff Resour Alloc. 2021;19:47. doi: 10.1186/s12962-021-00301-8. doi: 10.1186/s12962-021-00301-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu R, Li N, Ercia A. The effects of private health insurance on universal health coverage objectives in China: A systematic literature review. Int J Environ Res Public Health. 2020;17:2049. doi: 10.3390/ijerph17062049. doi: 10.3390/ijerph 17062049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sugunan A, Rajasekharan Pillai K, George A. Effectiveness of interventions to contain out-of-pocket-expenditure in lower-middle income countries: A systematic review and synthesis. Int J Health Plann Manage. 2023;38:918–35. doi: 10.1002/hpm.3642. doi: 10.1002/hpm. 3642. [DOI] [PubMed] [Google Scholar]
- 24.Chhabra KR, Sheetz KH, Nuliyalu U, Dekhne MS, Ryan AM, Dimick JB. Out-of-Network bills for privately insured patients undergoing elective surgery with in-network primary surgeons and facilities. JAMA. 2020;323:538–47. doi: 10.1001/jama.2019.21463. doi: 10.1001/jama. 2019.21463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez-Acevedo AJ, Chan RJ, Olsen CM, Pandeya N, Whiteman DC, Gordon LG. Out-of-pocket medical expenses compared across five years for patients with one of five common cancers in Australia. BMC Cancer. 2021;21:1055. doi: 10.1186/s12885-021-08756-x. doi: 10.1186/s12885-021-08756-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peng Z, Zhu L. The impacts of health insurance on financial strain for people with chronic diseases. BMC Public Health. 2021;21:1012. doi: 10.1186/s12889-021-11075-2. doi: 10.1186/s12889-021-11075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berete F, Demarest S, Charafeddine R, De Ridder K, Van Oyen H, Van Hoof W, Bruyère O, Van der Heyden J. Linking health survey data with health insurance data: methodology, challenges, opportunities and recommendations for public health research. An experience from the HISlink project in Belgium. Arch Public Health. 2023;81:198. doi: 10.1186/s13690-023-01213-0. doi: 10.1186/s13690-023-01213-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moreno-Serra R, Anaya-Montes M, León-Giraldo S, Bernal O. Addressing recall bias in (post-) conflict data collection and analysis: Lessons from a large-scale health survey in Colombia. Confl Health. 2022;16:14. doi: 10.1186/s13031-022-00446-0. doi: 10.1186/s13031-022-00446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sinha RK. Impact of publicly financed health insurance scheme (Rashtriya Swasthya Bima Yojana) from equity and efficiency perspectives. Vikalpa. 2018;43:191–206. [Google Scholar]
- 30.Wagstaff A, Eozenou P, Smitz M. Out-of-pocket expenditures on health: a global stocktake. The World Bank Res. Obser. 2020;35:123–57. [Google Scholar]
- 31.Catapano JS, Ducruet AF, Srinivasan VM, Rumalla K, Nguyen CL, Rutledge C, et al. Radiographic clearance of chronic subdural hematomas after middle meningeal artery embolization. J Neurointerv Surg. 2022;14:1279–1283. doi: 10.1136/neurintsurg-2021-018073. doi: 10.1136/neurintsurg-2021-018073. [DOI] [PubMed] [Google Scholar]
- 32.Sriram S, Khan MM. Effect of health insurance program for the poor on out-of-pocket inpatient care cost in India: Evidence from a nationally representative cross-sectional survey. BMC Health Serv Res. 2020;20:839. doi: 10.1186/s12913-020-05692-7. doi: 10.1186/s12913-020-05692-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kapinos KA, Peters RM, Jr, Murphy RE, Hohmann SF, Podichetty A, Greenberg RS. Inpatient Costs of Treating Patients With COVID-19. JAMA Netw Open. 2024;7:e2350145. doi: 10.1001/jamanetworkopen.2023.50145. doi: 10.1001/jamanetworkopen. 2023.50145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baione F., Biancalana D., Menzietti M. Optimal reimbursement limitation for a health plan. Ann Oper Res. 2023;1:20. [Google Scholar]
- 35.Hobbins AP, Barry L, Kelleher D, Shah K, Devlin N, Ramos Goni JM, et al. Do people with private health insurance attach a higher value to health than those without insurance? Results from an EQ-5D-5 L valuation study in Ireland. Health Policy. 2020;124:639–646. doi: 10.1016/j.healthpol.2020.03.005. doi: 10.1016/j.healthpol. 2020.03.005. [DOI] [PubMed] [Google Scholar]
- 36.Sabermahani A, Sirizi MJ, Zolala F, Nazari S. Out-of-Pocket costs and importance of nonmedical and indirect costs of inpatients. Value Health Reg Issues. 2021;24:141–147. doi: 10.1016/j.vhri.2020.05.004. doi: 10.1016/j.vhri. 2020.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Stadhouders N, Kruse F, Tanke M, Koolman X, Jeurissen P. Effective healthcare cost-containment policies: A systematic review. Health Policy. 2019;123:71–79. doi: 10.1016/j.healthpol.2018.10.015. doi: 10.1016/j.healthpol. 2018.10.015. [DOI] [PubMed] [Google Scholar]
- 38.Zheng B, Reardon PM, Fernando SM, Webber C, Thavorn K, Thompson LH, et al. Costs and Outcomes of Patients Admitted to the Intensive Care Unit With Cancer. J Intensive Care Med. 2021;36:203–10. doi: 10.1177/0885066619899653. doi: 10.1177/0885066619899653. [DOI] [PubMed] [Google Scholar]
- 39.Kumar A, Siddharth V, Singh SI, Narang R. Cost analysis of treating cardiovascular diseases in a super-specialty hospital. PLoS One. 2022;17:e0262190. doi: 10.1371/journal.pone.0262190. doi: 10.1371/journal.pone. 0262190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Darba S, Safaei N, Mahboub-Ahari A, Nosratnejad S, Alizadeh G, Ameri H, et al. Direct and Indirect Costs Associated with Coronary Artery (Heart) Disease in Tabriz, Iran. Risk Manag Healthc Policy. 2020;13:969–78. doi: 10.2147/RMHP.S261612. doi: 10.2147/RMHP.S261612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanco B, Mora T, Trapero-Bertran M. Direct health care costs associated to neurological diseases and different degrees of malnutrition. Clin Nutr ESPEN. 2021;44:297–305. doi: 10.1016/j.clnesp.2021.05.028. doi: 10.1016/j.clnesp. 2021.05.028. [DOI] [PubMed] [Google Scholar]
- 42.Hajat C, Siegal Y, Adler-Waxman A. Clustering and Healthcare Costs With Multiple Chronic Conditions in a US Study. Front Public Health. 2020;8:607528. doi: 10.3389/fpubh.2020.607528. doi: 10.3389/fpubh. 2020.607528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prinja S, Sharma Y, Dixit J, Thingnam SKS, Kumar R. Cost of Treatment of Valvular Heart Disease at a Tertiary Hospital in North India: Policy Implications. Pharmacoecon Open. 2019;3:391–402. doi: 10.1007/s41669-019-0123-6. doi: 10.1007/s41669-019-0123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lucas-Noll J, Clua-Espuny JL, Lleixà-Fortuño M, Gavaldà-Espelta E, Queralt-Tomas L, Panisello-Tafalla A, et al. The costs associated with stroke care continuum Figure: A systematic review. Health Econ Rev. 2023;13:32. doi: 10.1186/s13561-023-00439-6. doi: 10.1186/s13561-023-00439-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ayogu EE, Mosanya AU, Onuh JC, Adibe MO, Ubaka CM, Ukwe CV. Direct medical cost of treatment of uncomplicated malaria after the adoption of artemisinin-based combination therapy in Nigeria. J Appl Pharm Sci. 2021;11:029–034. [Google Scholar]
- 46.Gambhir RS, Malhi R, Khosla S, Singh R, Bhardwaj A, Kumar M. Out-patient coverage: Private sector insurance in India. J Family Med Prim Care. 2019;8:788–792. doi: 10.4103/jfmpc.jfmpc_101_19. doi: 10.4103/jfmpc.jfmpc_101_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balqis-Ali NZ, Anis-Syakira J, Fun WH, Sararaks S. Private health insurance in malaysia: Who Is Left Behind? Asia Pac J Public Health. 2021;33:861–9. doi: 10.1177/10105395211000913. doi: 10.1177/10105395211000913. [DOI] [PMC free article] [PubMed] [Google Scholar]


