Abstract
Background
This study explored the association between emotion word repertoire (EWR), attachment, reflective functioning and personality organization (PO) and suicidal behavior in borderline personality disorder (BPD) patients.
Methods
The current study performed a secondary data analysis from a randomized control trial for BPD patients (all female; n = 87; age: m = 27; SD = 7.42). EWR was assessed via machine-scoring transcripts of Adult Attachment Interviews (AAI) for affective words using the VETA electronic scoring software for the Levels of Emotional Awareness Scale (LEAS). Generated scores were related to impairments in PO (Structured Interview for Personality Organization; STIPO), attachment organization (AAI) and mentalization (Reflective Functioning Scale), general symptom severity (Brief Symptom Inventory; BSI-53), self-harm and suicidal behavior. Independent effects of the investigated predictors were studied using Bayesian path analysis.
Results
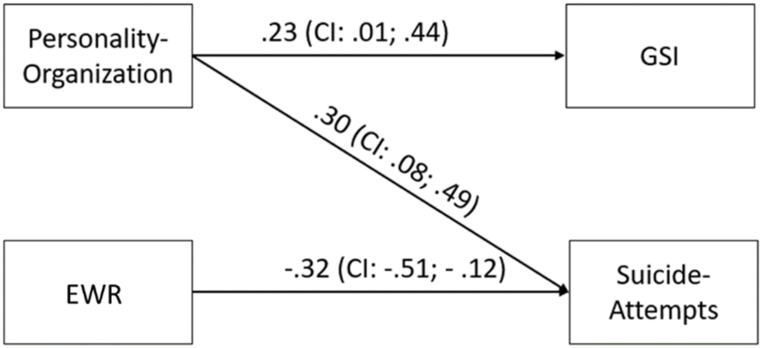
Corrected for education, findings in Bayesian path analysis suggest an independent negative association between EWR and suicide attempts (BE = −.32; 95 % CI [-.51, −.12]) and positive associations of deficits in PO with psychiatric symptoms (BE = .23; 95 % CI [.01, .44]) as well as suicide attempts (BE = .30; 95 % CI [.08, .49]).
Discussion
The findings underscore the potential role of high EWR and PO as a protective factor for suicidal behavior in individuals with BPD.
Keywords: Emotion word repertoire, Emotional awareness, Suicidal behavior, Personality organization, Adult attachment interview, Machine scoring
1. Introduction
With a prevalence of 1.7 % in the general population, Borderline Personality Disorder (BPD) is a significant challenge for mental health care [1]. Characterized by a high degree of comorbidity and severe functional impairment, one of the most challenging aspects for health professionals dealing with this disorder is the recurrent pattern of suicidal ideation, threats, and behavior [[2], [3], [4]]. In fact, several studies suggest that incidence of completed suicide in BPD ranges up to 10 %, often occurring before the age of 40 [3]. Efforts to identify risk-factors for suicidal behavior concluded sexual and physical abuse in childhood, impulsivity, comorbidity – especially comorbid depression – and substance abuse as significant predictors of suicide attempts [2,[5], [6], [7], [8]].
Regarding general psychopathology, previous research has established an association between suicidal behavior and alexithymia [9], defined as the inability to express or identify emotions [10]. A related but distinct concept to alexithymia is emotional awareness which denotes an individual's ability to describe and recognize emotions in oneself and others [11]. Most measurements of emotional processing can be either categorized as self-report measures or emotional intelligence ability tests. In contrast, the Levels of Emotional Awareness Scale (LEAS; [12]) consists of 10 or 20 hypothetical scenarios designed to evoke anger, fear, happiness and sadness. Participants are then asked “How would you feel?” and “How would the other person feel?“. Based on the open-end answers, emotional awareness can be differentiated in five levels including (1) awareness of physical sensations, (2) action tendencies, (3) single emotions, (4) blends of emotions (i.e., feeling multiple emotions at once), and (5) blends of blends of emotional experience [13]. Surprisingly, previous research suggests only small to non-significant overlaps between the LEAS and measures of alexithymia or emotional intelligence [[14], [15], [16], [17]].
Research on emotional awareness and suicide is limited. Ciarrochi, Scott, Deane and Heaven [14] did not find significant associations with suicidal ideation, while Baer, LaCroix, Browne, Hassen, Perera, Weaver, Soumoff and Ghahramanlou-Holloway [18] suggest a lack of emotional awareness as associated with acquired suicide capability in military personnel. However, no data have been acquired in regard to emotional awareness and suicide attempts. Yet, it has been argued that a concrete action towards ending one's own life might be fostered by a lack of the capability to symbolize intensely painful [19], but often highly ambivalent affects [20]. This deficit is typically associated with an incapacity to find suitable social support or experience emotional relief in the context of intimate conversations with close friends or professional health care personnel [21,22].
Recent advances in the operationalization of emotional awareness regarding computerized scoring procedures opened up the potential for its application to large text bodies originating from sources other than the traditional LEAS scenarios [[23], [24], [25]]. At present, the semi-structured adult attachment interview (AAI; [26]) was tested regarding its abilities to serve as raw material for extracting information about levels of emotional awareness. Previous studies applying the Linguistic Inquiry Word Count (LIWC) program to the AAI suggested interesting possibilities of machine-scoring text analysis of these interview narratives [27,28]. In a similar vein, the eLEAS algorithm was applied to transcripts of AAI interviews in order to extract scores of the sum of uniquely used affective level 3 words (“All-Sum-unique-3” see Lane [12]), with higher values indicating an increased emotion word repertoire (EWR). As the AAI delves into often painful memories of early attachment, including experiences of separation and abuse, higher EWR in this interview might indicate more differentiated processing of emotions. This, in turn, could be linked to a more effective regulation of challenging affects [11,17], serving as a potential protective factor against suicidal behavior.
Previous empirical research associated deficits in personality organization (PO) and attachment security with suicide attempts [29,30]. PO was conceptually outlined by Kernberg [31]. Theoretically anchored within object relations theory, Kernberg based the degree of PO on the stability of internalized self- and object representations. In correspondence to this, PO can be understood as the robustness of self-regulating functions needed to deal with intra- and interpersonal conflicts [32]. With regard to suicide attempts in BPD patients, Baus, Fischer-Kern, Naderer, Klein, Doering, Pastner, Leithner-Dziubas, Plener and Kapusta [29] observed more severe impairments of PO in patients with a history of suicide attempts. This relationship was particularly driven by an increased level of aggression and self-directed aggression.
Considering its close theoretical and empirical ties to affect regulation and the capacity to cope with interpersonal problems [[33], [34], [35], [36], [37]], it is not surprising that insecure adult attachment was repeatedly identified as a risk factor for suicidal behavior [30,38]. Unresolved attachment, which is closely linked to BPD [[39], [40], [41]], is characterized by a global breakdown in discourse strategy around themes of loss or trauma. The Cannot Classify category, is characterized by a lack of any consistent discourse style or by two distinct but diverse patterns. Both attachment categories pose the most severe expression of insecure attachment, summarized as disorganized attachment representation. A disorganized attachment representation is a clinically significant risk factor for suicidal behavior [38] and possibly eligible to differentiate within a group of BPD patients regarding past suicide attempts.
1.1. Research aims
In this report, we examine the EWR-scored AAI transcripts in relation to the frequency of suicide attempts in a sample of BPD patients, as well as their general psychiatric symptom burden and self-harm behavior. The results are compared to expert-rated reflective functioning capacities, attachment organization based on the AAI and PO assessed through the Structured Interview of Personality Organization (STIPO). We anticipated that higher EWR scores would be correlated with increased reflective functioning, enhanced PO, and an organized attachment representation. To assess the independent effects of all variables of interest simultaneously, the Bayesian structural equation modeling (BSEM) technique was applied.
2. Methods
2.1. Participants and procedure
The study reinvestigates baseline data of a previous randomized trial which studied 104 BPD patients (NCT00714311; see Ref. [42] for further details). Inclusion criteria for the present sample were an age >18, diagnosis of BPD via Structured Clinical Interview for DSM‐IV Axis II disorders (SCID II; [43]), female gender and completion of the AAI. The latter criteria lead to the exclusion of 17 participants whose AAI transcripts were lost due to poor audio quality of their interviews.
2.2. Psychometric assessment
The Adult Attachment Interview (AAI; [26]) is a 20-item semi-structured interview aiming to evoke feelings, memories and thoughts about early attachment relationships. This includes experiences of separation, rejection, loss and abuse. Within the interview, there are various ways for the interviewee to elaborate on, contradict, or fail to support earlier assertions. After the transcription of verbatim protocols, trained (within a two-week training workshop conducted by Mary Main and Erik Hesse) coders scored the transcripts according to one of five primary attachment classfications, namely: Secure/autonomous (F), dismissive (Ds), preoccupied (E), unresolved (U), and cannot classify (CC). For the present study, these categories were dichotomized into organized (F, D & E) and disorganized (U, CC) attachment representations. Raters were blind to all identifying attributes of participants and the nature and purpose of the study. Interrater agreement on categorical classifications was 86 % (κ = .80, t = 6.11, p = .001).
The Reflective Functioning Scale (RF; [44]) was scored based on the AAI transcripts by trained blinded coders. Individual differences in RF pertaining to the ability to mentalize in the context of attachment bonds are scored according to an 11-point scale, ranging from −1 (interviews are completely devoid of mentalization or severely distorting the mental states of others) to 9 (very high RF, interviews show exceptionally complex, elaborate, or original reasoning about mental states). The total RF score is given based on questions of the AAI that probe for reflection (so called demand questions). All RF coders were trained by certified instructors. Patients were scored as hypermentalizing (HM) if they exhibited excessively deep and detailed yet unconvincing accounts of the mental states related to observable behaviors of both self and important attachment figures.
Emotion Word Repertoire scores were assessed via the Verbal Emotion in Text Assessment Python Package (VETA; [24]) which was adapted to score and analyze EWR survey data. For the aims of this study the software analyzed AAI transcripts. Only the participants' verbal responses to AAI probes were scored. The EWR score was generated with the “allsum-unique-3” algorithm, which sums level three words eliminating duplicates in accordance with the multilevel approach of emotional awareness [12]. This was a modification of the established allsumunique metric which includes level 1 and 2 as well as level 3 words. Unlike responses to LEAS scenarios, in which the respondent is asked to describe their feelings, AAI questions are more general inquiries that do not specifically address feelings; therefore, incidental use of level 1 (somatic) or level 2 (action tendencies or valenced non-specific words) in response to AAI probes were excluded as their use could not be assumed to be part of a description of feelings. The analysis was based upon the first 16 items of the AAI, which had a completion rate of 84 % and are comparable between subjects with or without children [26]. Cronbach's α for EWR was estimated as very good with α = .86.
Structured Interview of Personality Organization (STIPO; [45]) was used to measure deficits in personality functions crucial for the regulation of the self and relationships with others. The interview consists of 100 items and enables trained raters to assess six levels of personality functioning ranging from 1 (high) to 6 (low). For an extensive description see Ref. [46].
Brief Symptom Inventory (BSI-53; [47]) operationalizes the amount of psychological distress in the last seven days and is comprised of 53 items rated on a 5-point Likert scale ranging from 0 (“absolutely not”) to 4 (“very strong”). The total score Global Severity Index (GSI) provides a measure for the total psychiatric symptom burden.
Suicide attempts and self-harm were assessed with the Cornell Interview for Suicidal and Self-harming Behavior – Self Report (CISSB; [48]), which is an adapted questionnaire originating from the Parasuicidal History Interview [49]. For the analysis absolute frequencies in the last year were investigated.
DSM-IV criteria for borderline personality disorder and comorbid Axis I and II diagnoses were assessed by the German version of the SCID-I and -II [43,50].
2.3. Statistical analysis and analysis strategy
SPSS 29.0 was used for data management, descriptive statistics and bivariate correlations. As the STIPO total score is ordinally scaled and due to the severe non-normality of the suicide attempts variable, Spearman-Rank correlation was used. Bayesian structural equation modeling (BSEM) was conducted via AMOS 29. BSEM has several advantages over traditional frequentist SEM approaches and allows for missing data, nonlinearity, small sample sizes and has no normal distribution assumption [51,52].
With regard to the novel approach of operationalizing emotional awareness based on AAI interviews non-informative priors were used as provided by the default settings of AMOS. Posterior distributions for investigated parameters were estimated via Markov Chain Monte Carlo (MCMC; Metropolis algorithm see Ref. [53] for more details). MCMC techniques generate a sequence of samples in which each new sample depends on the previous one, thus forming a Markov Chain. This property enables the algorithm to converge toward the desired target distribution. In AMOS, the MCMC algorithm stochastically samples parameter values as if they were variables, thus propagating the posterior distribution. Posterior mean values are approximated by calculating the averages of the samples generated during the MCMC process [54]. A convergence statistic = 1 and a posterior predictive p value (PPP) close to .5 was assumed as indicator for an excellent fit [55]. Bayesian analysis does not use a traditional p value to test for significant results of the Bayesian Estimations (BE) regression weights but employ so called credibility intervals (CI). Comparable to the traditional “significant” p-value approach, estimated distributions that do not include zero within the lower and upper 95 % bounds are regarded as credible.
Only variables that showed significant zero-order correlations with the investigated criteria were included in the initial model. After the initial fitting of the first model, a second model was constructed, which excluded all paths which did include zero within the lower and upper 95 % bounds.
3. Results
3.1. Descriptive results
Patients had a mean age of 27 years (SD = 7.4). Most patients reported a general qualification for university entrance as their highest degree of education. 26.4 % (n = 23) patients reported at least one suicide attempt in the last year. According to SKID I and II interviews 81.6 % were diagnosed with a DSM-IV axis I comorbidity and 71 % with at least one comorbid personality disorder.
3.2. Correlation analysis
As shown in Table 1 both uncorrected (for total word count) (r = −.31; p < .01) and corrected EWR (r = −.22; p < .05) variables were significantly correlated with fewer suicide attempts in the year before treatment. Furthermore, uncorrected and corrected EWR were linked to increased reflective functioning (r = .34 & .28; both p < .01) and hypermentalization (r = .48 & .35; both p < .001). Only the uncorrected EWR score was correlated with higher education (r = .30; p < .01) and increased self-harm in the last year (r = .24; p < .05).
Table 1.
Spearman Rank zero-order correlations between EWR Scores, STIPO, AAI and psychiatric symptoms.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. EWR | – | |||||||||
| 2. EWR/Vocabulary | .81** | – | ||||||||
| 3. STIPO | .08 | .05 | – | |||||||
| 4. AAI Organized | −.08 | 0 | −.43** | – | ||||||
| 5. RF | .34** | .28** | −.15 | .17 | – | |||||
| 6. HM | .48** | .35** | .22* | −.16 | .10 | – | ||||
| 7. Education | .30** | .14 | −.26* | .16 | .30** | .06 | – | |||
| 8. GSI | .16 | .20 | .26* | −.18 | .00 | −.04 | −.04 | – | ||
| 9. Self-harm (last year) | .24* | .10 | .28** | −.19 | .13 | .06 | .05 | .18 | – | |
| 10. Suicide Attempts (last year) | −.31** | −.22* | .28** | −.14 | −.10 | −.20 | −.24* | .06 | .04 | – |
| Mean or Frequency | 133.59 | .12 | 4.86 | 40 | 2.74 | 9 | 3.60 | 1.41 | 30.38 | 23 |
| SD or % | 65.45 | .04 | .57 | 46 | 1.11 | 10.30 | 1.11 | .65 | 70.07 | 26.40 |
Note. *p < .05; **p < .01; N = 87; EWR = Emotion Word Repertoire; EWR/Vocabulary = Emotion Word Repertoire divided by Vocabulary; STIPO = Structured Interview of Personality Organization; AAI Organized = Organized Attachment Representation in the Adult Attachment Interview; RF = Reflective Functioning; HM = Hypermentalizing; GSI = Global Severity Index.
Neither PO nor organized attachment representation correlated with the EWR variables (p > .05). However, lower PO was linked to less education (r = −.26; p < .05), a disorganized attachment (p = −.43; p < .001) and generally higher symptom load including increased GSI (r = .26; p < .05), self-harm (r = .28; p < .01) and suicide attempts (r = .28; p < .01). Finally, reflective functioning correlated with higher education (r = .30; p < .01).
3.3. Path analysis
Based on the significant results of the zero-order correlations the data were fitted to an initial path model that included the following regression paths: PO to GSI, self-harm and suicides attempts in the last year; EWR to GSI, self-harm and suicide attempts. The model was controlled for the effects of education. After the trimming step, self-harm and the path from EWR to GSI had to be deleted. This resulted in a model with an excellent model fit (PPP = .5; Convergence statistics = 1). As shown in Fig. 1, EWR was negatively associated with suicide attempts in the last year (BE = −.32; 95 % CI [-.51, −.12]), while deficits in PO were linked to increased GSI (BE = .23; 95 % CI [.01, .44]) and more frequent suicide attempts (BE = .30; 95 % CI [.08, .49]). In sum, PO and EWR were able to explain 22 % of the variance of suicide attempts, while PO explained 7 % of the variance of GSI.
Fig. 1.
Trimmed BSEM path model of the associations between EWR and impairments in Personality Organization with Global Severity Index (GSI) and Suicide Attempts (corrected for education; CI: 95 %).
4. Discussion
Utilizing a novel approach to measure EWR based on AAI transcripts, this study investigated risk factors for suicide attempts in patients with BPD. The findings indicate that impairments in both personality organization (PO) and EWR are independently linked to a higher incidence of past suicide attempts. Specifically, greater impairment in PO corresponds to more frequent suicide attempts, while a larger EWR demonstrates protective effects in this context. Notably, the machine-derived EWR score exhibited no correlation with PO or attachment organization. However, the EWR scores did display associations with the patients' educational levels and reflective functioning, aligning with expectations based on previous research on levels of emotional awareness [[56], [57], [58]]. The primary finding, indicating a significantly reduced incidence of suicidal behavior in patients with higher EWR during AAI interviews, underscores the clinical importance of verbalization skills concerning painful affective states and memories.
One plausible explanation for the negative association between suicide attempts and EWR lies in its link to seeking social support. Patients with an increased ability to verbalize emotions have been found to be more likely to communicate, request and consequently receive suitable social support [59]. In turn, it is known from meta-analytic evidence that both support from health professionals as well as from informal social networks are effective in decreasing suicidal tendencies [21,22].
Another possible explanation is that suicide attempts may be preceded by a kind of “tunnel vision” in which the range of emotional experiences is narrow and highly aversive, lacking differentiation and complexity, resulting in hopelessness. A greater EWR may enable a broader range of experiences including hope and thus a greater willingness to continue on. From a constructivist perspective, the ability to know or construct what one is experiencing requires access to a repertoire of emotion concepts captured in words [13]. As such, EWR is closely related to, but not identical with, emotional awareness.
In this context, a larger EWR might also be associated with less impulsivity, in parallel to increased emotional awareness [[60], [61], [62]]. In turn, negative urgency, a personality predictor of externalizing behavior involving the tendency to act rashly when distressed, has been associated with suicide risk [[63], [64], [65]]. Consistent with the retained ability to experience hope, it is reasonable to hypothesize that greater EWR and higher emotional awareness may be associated with less negative urgency. However, additional research will be needed to test these hypotheses.
Moreover, our results suggest that EWR is a function of verbal abilities, which is further underscored by the observed significant association with education. However, considering that the relationship between EWR and suicide attempts remained significant after controlling for the patients’ education and scope of vocabulary (total word count) used in the AAI, the ability to mentally perceive and report emotions seems to be uniquely connected to resilience against suicidal behavior. Along these lines, EWR scores, generally associated with increased reflective functioning, were notably higher in patients rated as hypermentalizers. Hypermentalizers exhibit excessively rich yet unconvincing narratives laden with pseudopsychological jargon [44]. However, in contrast to EWR, neither reflective functioning in general, nor a specific overanalyzing/hypermentalizing narrative style, was significantly associated with suicidal behavior.
Considering Schneidman's [19] theory on the role of mental pain in suicides, it is conceivable that the ability to articulate affects is linked to an attenuation of the painful aspects of these emotions. Limitations in the ability to experience and express emotion, particularly in individuals exposed to early life adversity, may result in the tendency to experience distressing emotions in social contexts as physical pain [66]. Experiencing emotional distress as a bodily sensation rather than an emotional feeling may contribute to an increased experience of emotionally painful distress and compromise the ability to recognize and regulate it. Previous research - using the original LEAS procedure - which observed lower LEAS scores in psychosomatic patients compared to other psychiatric groups, support this line of reasoning [16]. However, further empirical research on the connection between emotional awareness, psychosomatic conditions and mental pain will be necessary.
In line with our expectations and previous literature [29], increased deficits in PO were associated with more suicide attempts. However, the observed lack of a significant relationship between EWR and PO seem to be contraindicative. This is even more puzzling as both constructs explain significant – although seemingly independent – proportions of the variance of past suicidal behavior. In psychodynamic literature, EWR-related concepts like alexithymia are usually seen as part of personality functioning or organization [67]. Yet, to date, concrete empirical data on the relationship between PO, as measured with the STIPO, and alexithymia or emotional awareness has not been collected. Given that this study investigated a relatively homogeneous sample of female BPD patients, one might speculate that the lack of significant correlation might relate back to a scarcity of interindividual variance regarding PO. Thus, future studies would have to investigate more diverse samples to test this explanatory model.
Furthermore, in comparison to Fischer-Kern et al. [68] the present study observed a slight reduction in the correlation between RF and PO, which, in combination with the reduced sample size, lead to a non-significant result regarding this relationship. The generally relatively small correlations observed between both constructs in BPD patient samples seem surprising at first glance. However, again the most plausible explanation for this may be found in the relatively homogenous sample, which showed rather small standard deviations regarding both RF and PO. A previous study by Atanassov and Savov [69] which investigated a mixed sample of healthy participants and heroin addicted patients observed moderate to strong correlations between the STIPO and mentalization, using the Verbal Elaboration of Affect Scale [70]. Moreover, findings by Müller, Wendt, Spitzer, Masuhr, Back and Zimmermann [71] indicated significant associations between self-rate measures of personality organization and reflective functioning.
4.1. Limitations and future directions
The present study breaks new ground in automating the operationalization of an important ingredient of emotional awareness using linguistic narratives that differ from the original hypothetical scenarios used in standard LEAS measurement. However, it is essential to note that only female patients diagnosed with BPD were examined in this study. Therefore, further validation is needed to generalize the observations to the broader population. Additionally, future studies should compare computer scoring methods of AAI-narratives against hand-scored results obtained from the standard LEAS. Moreover, given that all participants in this study were patients with borderline personality disorder, the addition of a control group of healthy volunteers would permit more comprehensive examination of the association between EWR and PO.
Another issue is the recurring question [24] of whether emotional awareness scores should be corrected for word count. Lane and Smith [13] have argued against controlling for word count or vocabulary, suggesting that doing so might result in the loss of important variance within the emotional awareness variable, as awareness and reporting are inseparable [72]. Moreover, affective verbal output might not only be a result of emotional awareness but also contribute to its construction [73].
4.2. Conclusion
The initial results with this exploratory approach to the measurement of EWR as an ingredient of emotional awareness hold promise for further investigations in connection to psychopathological phenomena as well as psychotherapeutic outcome research. While more research will be needed to deepen the understanding of the relation between emotional awareness and suicidal behavior, our results highlight the suicide-specific vulnerability of patients with BPD who are impaired in their verbal ability to talk about painful, attachment-related affects. Thus, it might be a promising path for psychotherapeutic interventions to foster this ability, especially in patients with suicidal tendencies.
Ethics statement
This study was carried out in accordance with the recommendations of the ethics committee of the Medical University of Vienna which approved the protocol under the signature 207/2004. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
Funding statement
The original RCT was supported by grant number 10636 from the Jubilaeumsfonds of the Austrian National Bank. The secondary analysis received no external funding.
Availability of Data
Due to the European General Data Protection Regulation (GDPR), the data is not publicly available.
CRediT authorship contribution statement
J. Fuchshuber: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Conceptualization. S. Doering: Writing – review & editing, Writing – original draft, Supervision, Project administration, Funding acquisition, Conceptualization. S. Schmitz-Riol: Writing – review & editing, Formal analysis, Data curation. J. Herpertz: Writing – review & editing, Software. S. Hörz-Sagstetter: Writing – review & editing, Investigation. M. Rentrop: Writing – review & editing, Investigation. M. Fischer-Kern: Writing – review & editing, Investigation. P. Buchheim: Writing – review & editing, Investigation. J. Taylor: Writing – review & editing, Software. A. Tmej: Writing – review & editing, Investigation. K. Weihs: Writing – review & editing, Conceptualization. R.D. Lane: Writing – review & editing, Writing – original draft, Supervision, Project administration, Conceptualization.
Declaration of competing interest
Richard D. Lane has disclosed an outside interest in the Electronic Levels of Emotional Awareness Scale to the University of Arizona. Conflicts of interest resulting from this interest are being managed by The University of Arizona in accordance with its policies.
Acknowledgments
Richard D. Lane participated in this study as the Fulbright-Freud Visiting Lecturer of Psychoanalysis 2023 sponsored by Fulbright Austria and the Sigmund Freud Museum in Vienna, Austria.
References
- 1.Gunderson J.G., Herpertz S.C., Skodol A.E., Torgersen S., Zanarini M.C. Borderline personality disorder. Nat. Rev. Dis. Prim. 2018;4:1–20. doi: 10.1038/nrdp.2018.29. [DOI] [PubMed] [Google Scholar]
- 2.Soloff P.H., Lynch K.G., Kelly T.M., Malone K.M., Mann J.J. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am. J. Psychiatr. 2000;157:601–608. doi: 10.1176/appi.ajp.157.4.601. [DOI] [PubMed] [Google Scholar]
- 3.Black D.W., Blum N., Pfohl B., Hale N. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J. Pers. Disord. 2004;18:226–239. doi: 10.1521/pedi.18.3.226.35445. [DOI] [PubMed] [Google Scholar]
- 4.Bohus M., Stoffers-Winterling J., Sharp C., Krause-Utz A., Schmahl C., Lieb K. Borderline personality disorder. Lancet. 2021;398:1528–1540. doi: 10.1016/S0140-6736(21)00476-1. [DOI] [PubMed] [Google Scholar]
- 5.Yang F., Tong J., Zhang S.F., Zhang J., Zhong B.L. Prevalence and correlates of suicide attempts in Chinese individuals with borderline personality disorder. Front. Psychiatr. 2022;13 doi: 10.3389/fpsyt.2022.942782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brodsky B.S., Malone K.M., Ellis S.P., Dulit R.A., Mann J.J. Characteristics of borderline personality disorder associated with suicidal behavior. Am. J. Psychiatr. 1997;154:1715–1719. doi: 10.1176/ajp.154.12.1715. [DOI] [PubMed] [Google Scholar]
- 7.Friedman R.C., Aronoff M.S., Clarkin J.F., Corn R., Hurt S.W. History of suicidal behavior in depressed borderline inpatients. Am. J. Psychiatr. 1983;140:1023–1026. doi: 10.1176/ajp.140.8.1023. [DOI] [PubMed] [Google Scholar]
- 8.Grilo C.M., Udo T. Association of borderline personality disorder criteria with suicide attempts among US adults. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.9389. ARTNe21938910.1001/jamanetworkopen.2021.9389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemming L., Taylor P., Haddock G., Shaw J., Pratt D. A systematic review and meta-analysis of the association between alexithymia and suicide ideation and behaviour. J. Affect. Disord. 2019;254:34–48. doi: 10.1016/j.jad.2019.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sifneos P.E. The prevalence of 'alexithymic' characteristics in psychosomatic patients, Psychother. Psychosom. 1973;22:255–262. doi: 10.1159/000286529. [DOI] [PubMed] [Google Scholar]
- 11.Lane R.D., Weihs K.L., Herring A., Hishaw A., Smith R. Affective agnosia: expansion of the alexithymia construct and a new opportunity to integrate and extend Freud's legacy. Neurosci. Biobehav. Rev. 2015;55:594–611. doi: 10.1016/j.neubiorev.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Lane R.D., Quinlan D.M., Schwartz G.E., Walker P.A., Zeitlin S.B. The levels of emotional awareness scale: a cognitive-developmental measure of emotion. J. Pers. Assess. 1990;55:124–134. doi: 10.1080/00223891.1990.9674052. [DOI] [PubMed] [Google Scholar]
- 13.Lane R.D., Smith R. Levels of emotional awareness: theory and measurement of a socio-emotional skill. J. Intell. 2021;9:42. doi: 10.3390/jintelligence9030042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ciarrochi J., Scott G., Deane F.P., Heaven P.C. Relations between social and emotional competence and mental health: a construct validation study. Pers. Indiv. Differ. 2003;35:1947–1963. doi: 10.1016/S0191-8869(03)00043-6. [DOI] [Google Scholar]
- 15.Maroti D., Lilliengren P., Bileviciute-Ljungar I. The relationship between alexithymia and emotional awareness: a meta-analytic review of the correlation between TAS-20 and LEAS. Front. Psychol. 2018;9:453. doi: 10.3389/fpsyg.2018.00453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Subic-Wrana C., Bruder S., Thomas W., Lane R.D., Kohle K. Emotional awareness deficits in inpatients of a psychosomatic ward: a comparison of two different measures of alexithymia. Psychosom. Med. 2005;67:483–489. doi: 10.1097/01.psy.0000160461.19239.13. [DOI] [PubMed] [Google Scholar]
- 17.Lane R.D., Solms M., Weihs K.L., Hishaw A., Smith R. Affective agnosia: a core affective processing deficit in the alexithymia spectrum. Biopsychosoc. Med. 2020;14:1–14. doi: 10.1186/s13030-020-00184-w. [DOI] [Google Scholar]
- 18.Baer M.M., LaCroix J.M., Browne J.C., Hassen H.O., Perera K.U., Weaver J., Soumoff A., Ghahramanlou-Holloway M. Lack of emotional awareness is associated with thwarted belongingness and acquired capability for suicide in a military psychiatric inpatient sample, suicide life threat. Beyond Behav. 2019;49:1395–1411. doi: 10.1111/sltb.12530. [DOI] [PubMed] [Google Scholar]
- 19.Shneidman E.S. Suicide as psychache, J. Nerv. Ment. Dis. 1993;181:145–147. doi: 10.1097/00005053-199303000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Kernberg O.F. The suicidal risk in severe personality disorders: differential diagnosis and treatment. J. Pers. Disord. 2001;15:195–208. doi: 10.1521/pedi.15.3.195.19203. ; discussion 209-115. [DOI] [PubMed] [Google Scholar]
- 21.Miller A.B., Esposito-Smythers C., Leichtweis R.N. Role of social support in adolescent suicidal ideation and suicide attempts. J. Adolesc. Health. 2015;56:286–292. doi: 10.1016/j.jadohealth.2014.10.265. [DOI] [PubMed] [Google Scholar]
- 22.Heerde J.A., Hemphill S.A. Examination of associations between informal help-seeking behavior, social support, and adolescent psychosocial outcomes: a meta-analysis. Dev. Rev. 2018;47:44–62. doi: 10.1016/j.dr.2017.10.001. [DOI] [Google Scholar]
- 23.Lane R.D. The construction of emotional experience: state-related emotional awareness and its application to psychotherapy research and practice. Counsell. Psychother. Res. J. 2020;20:479–487. doi: 10.1002/capr.12331. [DOI] [Google Scholar]
- 24.Herpertz J., Taylor J., Allen J.J.B., Herpertz S., Opel N., Richter M., Subic-Wrana C., Dieris-Hirche J., Lane R.D. Development and validation of a computer program for measuring emotional awareness in German-The geLEAS (German electronic Levels of Emotional Awareness Scale) Front. Psychiatr. 2023;14 doi: 10.3389/fpsyt.2023.1129755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barchard K.A., Bajgar J., Leaf D.E., Lane R.D. Computer scoring of the levels of emotional awareness scale. Behav. Res. Methods. 2010;42:586–595. doi: 10.3758/BRM.42.2.586. [DOI] [PubMed] [Google Scholar]
- 26.George C., Main M., Kaplan N. An International Journal on Personal Relationships; 1996. Adult Attachment Interview, Interpersona. [Google Scholar]
- 27.Cassidy J., Sherman L.J., Jones J.D. What's in a word? Linguistic characteristics of Adult Attachment Interviews. Am. J. Bioeth. 2012;14:11–32. doi: 10.1080/14616734.2012.636649. [DOI] [PubMed] [Google Scholar]
- 28.Waters T.E., Steele R.D., Roisman G.I., Haydon K.C., Booth-LaForce C. A linguistic Inquiry and word count analysis of the adult attachment interview in two large corpora. Can. J. Behav. Sci. 2016;48:78–88. doi: 10.1037/cbs0000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baus N., Fischer-Kern M., Naderer A., Klein J., Doering S., Pastner B., Leithner-Dziubas K., Plener P.L., Kapusta N.D. Personality organization in borderline patients with a history of suicide attempts. Psychiatr. Res. 2014;218:129–133. doi: 10.1016/j.psychres.2014.03.048. [DOI] [PubMed] [Google Scholar]
- 30.Green J., Berry K., Danquah A., Pratt D. The role of psychological and social factors in the relationship between attachment and suicide: a systematic review. Clin. Psychol. Psychother. 2020;27:463–488. doi: 10.1002/cpp.2445. [DOI] [PubMed] [Google Scholar]
- 31.Kernberg O.F. In: Major Theories of Personality Disorder. Clarkin J.F., Lenzenweger M.F., editors. Guilford Press; New York City: 1996. A psychoanalytic theory of personality disorders; pp. 106–140. [Google Scholar]
- 32.Rudolf G., Grande T., Henningsen P. Die Struktur der Persönlichkeit: Theoretische Grundlagen zur psychodynamischen Therapie struktureller Störungen. first ed. Klett-Cotta; 2018. [Google Scholar]
- 33.Zhang X., Li J.H., Xie F., Chen X., Xu W.J., Hudson N.W. The relationship between adult attachment and mental health: a meta-analysis. Journal of Personality and Social Psychology. 2022;123:1089–1137. doi: 10.1037/pspp0000437. [DOI] [PubMed] [Google Scholar]
- 34.Cooke J.E., Kochendorfer L.B., Stuart-Parrigon K.L., Koehn A.J., Kerns K.A. Parent-child attachment and children's experience and regulation of emotion: a meta-analytic review. Emotion. 2019;19:1103–1126. doi: 10.1037/emo0000504. [DOI] [PubMed] [Google Scholar]
- 35.Mikulincer M., Shaver P.R. In: Handbook of Attachment: Theory, Research, and Clinical Applications. Cassidy J., Shaver P.R., editors. Guilford Press; New York City: 2008. Adult attachment and affect regulation; pp. 503–531. [Google Scholar]
- 36.Schore J.R., Schore A.N. Modern attachment theory: the central role of affect regulation in development and treatment. Clin. Soc. Work. J. 2008;36:9–20. doi: 10.1007/s10615-007-0111-7. [DOI] [Google Scholar]
- 37.Candel O.S., Turliuc M.N. Insecure attachment and relationship satisfaction: a meta-analysis of actor and partner associations. Pers. Indiv. Differ. 2019;147:190–199. doi: 10.1016/j.paid.2019.04.037. [DOI] [Google Scholar]
- 38.Zortea T.C., Gray C.M., O'Connor R.C. The relationship between adult attachment and suicidal thoughts and behaviors: a systematic review. Arch. Suicide Res. 2021;25:38–73. doi: 10.1080/13811118.2019.1661893. [DOI] [PubMed] [Google Scholar]
- 39.Fonagy P., Target M., Gergely G. Attachment and borderline personality disorder - a theory and some evidence. Psychiatr. Clin. 2000;23:103–122. doi: 10.1016/S0193-953x(05)70146-5. [DOI] [PubMed] [Google Scholar]
- 40.Buchheim A., Hörz-Sagstetter S., Doering S., Rentrop M., Schuster P., Buchheim P., Pokorny D., Fischer-Kern M. Change of unresolved attachment in borderline personality disorder: RCT study of transference-focused psychotherapy. Psychother. Psychosom. 2017;86:314–316. doi: 10.1159/000460257. [DOI] [PubMed] [Google Scholar]
- 41.Buchheim A., Diamond D. Attachment and borderline personality disorder. Psychiatr. Clin. 2018;41:651–668. doi: 10.1016/j.psc.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Doering S., Horz S., Rentrop M., Fischer-Kern M., Schuster P., Benecke C., Buchheim A., Martius P., Buchheim P. Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: randomised controlled trial. Br. J. Psychiatry. 2010;196:389–395. doi: 10.1192/bjp.bp.109.070177. [DOI] [PubMed] [Google Scholar]
- 43.Fydrich T., Renneberg B., Schmitz B., Wittchen H.-U. Hogrefe; 1997. SKID-II: Strukturiertes Klinisches Interview für DSM-IV, Achse II: Persönlichkeitsstörungen [SCID-II: Structured Clinical Interview for DSM-IV, Axis II: Personality disorders] [Google Scholar]
- 44.Fonagy P., Target M., Steele H., Steele M. University College London; London: 1998. Reflective-functioning Manual Version 5 for Application to Adult Attachment Interviews. [Google Scholar]
- 45.Clarkin J.F., Caligor E., Stern B., Kernberg O.F. Weill Medical College of Cornell University; 2004. Structured Interview of Personality Organization (STIPO) [Google Scholar]
- 46.Stern B.L., Caligor E., Clarkin J.F., Critchfield K.L., Horz S., MacCornack V., Lenzenweger M.F., Kernberg O.F. Structured Interview of Personality Organization (STIPO): preliminary psychometrics in a clinical sample. J. Pers. Assess. 2010;92:35–44. doi: 10.1080/00223890903379308. [DOI] [PubMed] [Google Scholar]
- 47.Derogatis L.R., Melisaratos N. The brief symptom inventory: an introductory report. Psychol. Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 48.Clarkin J. vol. 21. Weill Medical College of Cornell University; 1998. (Cornell Revised Treatment History Inventory (CRITH)). [Google Scholar]
- 49.Linehan M., Wagner A., Cox G. University of Washington; 1989. Parasuicide History Interview: Comprehensive Assessment of Parasuicidal Behavior. [Google Scholar]
- 50.Wittchen H.-U., Zaudig M., Fydrich T. Hogrefe; 1997. SKID-I: Strukturiertes Klinisches Interview für DSM-IV, Achse I [SCID–I: Structured Clinical Interview for DSM-IV, Axis I] [Google Scholar]
- 51.Hoyle R.H. Guilford press; New York City: 2012. Handbook of Structural Equation Modeling. [Google Scholar]
- 52.Muthen B., Asparouhov T. Bayesian structural equation modeling: a more flexible representation of substantive theory. Psychol. Methods. 2012;17:313–335. doi: 10.1037/a0026802. [DOI] [PubMed] [Google Scholar]
- 53.Lee S.-Y. John Wiley & Sons; 2007. Structural Equation Modeling: A Bayesian Approach. [Google Scholar]
- 54.Byrne B.M. Routledge; Abingdon: 2010. Structural Equation Modeling with Amos: Basic Concepts, Applications, and Programming. [Google Scholar]
- 55.Garnier-Villarreal M., Jorgensen T.D. Adapting fit indices for Bayesian structural equation modeling: comparison to maximum likelihood. Psychol. Methods. 2020;25:46. doi: 10.1037/met0000224. [DOI] [PubMed] [Google Scholar]
- 56.Lane R.D., Sechrest L., Reidel R., Weldon V., Kaszniak A., Schwartz G.E. Impaired verbal and nonverbal emotion recognition in alexithymia. Psychosom. Med. 1996;58:203–210. doi: 10.1097/00006842-199605000-00002. [DOI] [PubMed] [Google Scholar]
- 57.Nandrino J.L., Baracca M., Antoine P., Paget V., Bydlowski S., Carton S. Level of emotional awareness in the general French population: effects of gender, age, and education level. Int. J. Psychol. 2013;48:1072–1079. doi: 10.1080/00207594.2012.753149. [DOI] [PubMed] [Google Scholar]
- 58.Lane R.D., Sechrest L., Riedel R. Sociodemographic correlates of alexithymia. Compr. Psychiatr. 1998;39:377–385. doi: 10.1016/s0010-440x(98)90051-7. [DOI] [PubMed] [Google Scholar]
- 59.Yeung N.C.Y., Chow T.S. Coping with my own way: mediating roles of emotional expression and social support seeking in the associations between individual differences and posttraumatic growth. Health Psychol. Open. 2019;6 doi: 10.1177/2055102919846596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bréjard V., Bonnet A., Pedinielli J.-L. Développement cognitivo-émotionnel, régulation des émotions et comportements à risques: une étude exploratoire chez l'adolescent, Neuropsychiatr. Enfances Adolesc. 2005;53:395–400. doi: 10.1016/j.neurenf.2005.09.018. [DOI] [Google Scholar]
- 61.Bréjard V., Bonnet A., Pedinielli J.-L. Rôle du tempérament et de la conscience émotionnelle dans la prise de risque chez des adolescents. L'Encéphale. 2012;38:1–9. doi: 10.1016/j.encep.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 62.Bréjard V., Pasquier A., Bonnet A., Pedinielli J. Comparative study of the subjective emotional experience among adolescents showing depressive symptoms associated or not with risk-taking behavior. L'encephale. 2011;37:257–265. doi: 10.1016/j.encep.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 63.Beach V.L., Gissandaner T.D., Schmidt A.T. The UPPS model of impulsivity and suicide: a systematic literature review. Arch. Suicide Res. 2022;26:985–1006. doi: 10.1080/13811118.2021.1892002. [DOI] [PubMed] [Google Scholar]
- 64.Millner A.J., Lee M.D., Hoyt K., Buckholtz J.W., Auerbach R.P., Nock M.K. Are suicide attempters more impulsive than suicide ideators? Gen. Hosp. Psychiatr. 2020;63:103–110. doi: 10.1016/j.genhosppsych.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 65.Anestis M.D., Joiner T.E. Examining the role of emotion in suicidality: negative urgency as an amplifier of the relationship between components of the interpersonal–psychological theory of suicidal behavior and lifetime number of suicide attempts. J. Affect. Disord. 2011;129:261–269. doi: 10.1016/j.jad.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 66.Lane R.D., Anderson F.S., Smith R. Biased competition favoring physical over emotional pain: a possible explanation for the link between early adversity and chronic pain. Psychosom. Med. 2018;80:880–890. doi: 10.1097/PSY.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 67.Wagner-Skacel J., Matzer F., Kohlhammer-Dohr A., Dalkner N., Jauk E. Assessment of personality functioning in psychosomatic medicine. Wien Klin. Wochenschr. 2022;134:602–610. doi: 10.1007/s00508-021-01993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fischer-Kern M., Buchheim A., Hörz S., Schuster P., Doering S., Kapusta N.D., Taubner S., Tmej A., Rentrop M., Buchheim P. The relationship between personality organization, reflective functioning, and psychiatric classification in borderline personality disorder, Psychoanal. Psychol. 2010;27:395. doi: 10.1037/a0020862. [DOI] [Google Scholar]
- 69.Atanassov N., Savov S. Mentalization and personality organization in heroin addicted patients: a narrative analysis. Language and Psychoanalysis. 2016;5:14–30. [Google Scholar]
- 70.Lecours S., Sanlian N., Bouchard M.A. Assessing verbal elaboration of affect in clinical interviews: exploring sex differences. Bull. Menninger Clin. 2007;71:227–247. doi: 10.1521/bumc.2007.71.3.227. Full text linksCite. [DOI] [PubMed] [Google Scholar]
- 71.Müller S., Wendt L.P., Spitzer C., Masuhr O., Back S.N., Zimmermann J. A critical evaluation of the reflective functioning questionnaire (RFQ) J. Pers. Assess. 2022;104:613–627. doi: 10.1080/00223891.2021.1981346. [DOI] [PubMed] [Google Scholar]
- 72.Weiskrantz L. Consciousness lost and found: a neuropsychological exploration. first. Oxford University Press; 1997. [Google Scholar]
- 73.Satpute A.B., Nook E.C., Cakar M.E. In: Neuroscience of Enduring Change: Implications for Psychotherapy. Lane R., D, editors. Oxford University Press; Oxford: 2020. The role of language in the construction of emotion and memory: a predictive coding view; pp. 56–88. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the European General Data Protection Regulation (GDPR), the data is not publicly available.