Abstract
Progress toward racial health equity cannot be made if we cannot measure its fundamental driver: structural racism. As in other epidemiologic studies, the first step is to measure the exposure. But how to measure structural racism is an ongoing debate. To characterize the approaches epidemiologists and other health researchers use to quantitatively measure structural racism, highlight methodological innovations, and identify gaps in the literature, we conducted a scoping review of the peer-reviewed and gray literature published during 2019–2021 to accompany the 2018 published work of Groos et al., in which they surveyed the scope of structural racism measurement up to 2017. We identified several themes from the recent literature: the current predominant focus on measuring anti-Black racism; using residential segregation as well as other segregation-driven measures as proxies of structural racism; measuring structural racism as spatial exposures; increasing calls by epidemiologists and other health researchers to measure structural racism as a multidimensional, multilevel determinant of health and related innovations; the development of policy databases; the utility of simulated counterfactual approaches in the understanding of how structural racism drives racial health inequities; and the lack of measures of antiracism and limited work on later life effects. Our findings sketch out several steps to improve the science related to structural racism measurements, which is key to advancing antiracism policies.
Keywords: structural racism, health equity, measurement
Introduction
Racial health inequities persist despite decades of efforts to eliminate them.1‑3 Even in the face of medical advances, increased access to health care, and improvements in nutrition, racialized communities often have worse health than their White counterparts.4 In this article, we use the term racialized people/communities to affirm that race is socially constructed by those in power (ie, White people) to maintain their superior position in the social hierarchy while exploiting those deemed “other” (ie, non-White people) by way of creating the meaning of “race.”5 Evidence of persistent racial inequities has been observed as far back as the data have been collected. For example, Black and Indigenous communities often suffer from the most adverse birth outcomes, highest rates of chronic diseases, and have a shortened life expectancy.6 To address these persistent inequities, health research has begun to consider the role of social determinants,7 which affect a wide range of health risks and outcomes.8,9 Yet, after close to 1 million lives were lost to COVID-19, with Black and Indigenous people at a much higher mortality risk compared with their White counterparts,10 we must move even farther upstream to consider the structural factors shaping the distribution of those social determinants of health. One critical upstream factor is structural racism.
Structural racism is “the totality of ways in which societies foster racial discrimination, through mutually reinforcing inequitable systems (in housing, education, employment, earnings, benefits, credit, media, health care, criminal justice, and so on) that in turn reinforce discriminatory beliefs, values, and distribution of resources, which together affect the risk of adverse health outcomes.”11 White supremacy refers to “a society-wide system that removes power from non-white people through means both blatant and invisible; from the daily pangs of interpersonal racism to the subterranean harms of implicit bias in our schools and hospitals to the disparate accumulation of wealth that began in slavery and dispossession, continued in redlining and segregation, and echoes still in unequal household wealth and access to capital.”12 Together, structural racism and White supremacy operate to shape cultural beliefs, institutional and systemwide policies, and interpersonal rules and behaviors creating advantages for White people while producing cumulative and chronic adverse outcomes for racialized communities. Research has begun to link structural racism to racial health inequities, with further theoretical and conceptual support where empirical evidence is lacking, yet it is still in its early stages.1,4,6,13‑15
A key challenge of research linking structural racism and health inequities lies in operationalizing and measuring structural racism.15 In 2018, Groos et al.16 published a scoping review in which they identified 20 articles on structural racism and health published in the past 30 years. Since the murders of George Floyd, Jr., Ahmaud Arbery, Breonna Taylor, and many other members of the Black community whose lives were stolen too soon either at the hands of police or due to the disproportionate exposure to COVID-19 and the disparate access to vaccines and treatments, the United States has been forced to acknowledge its racist history and to explore how it has contributed to entrenched racial health inequities by collective action and uprisings across the country and the world.17 A flood of “new” research has come after an increase in attention to how structural racism and White supremacy operate in the United States and how they create deleterious health risks for racialized people.17‑19 Despite this progress, there is much we still do not know about the mechanisms connecting structural racism to health or how to accurately capture structural racism with quantitative measurements.14
The goal of epidemiologists and other health researchers is to conduct research that contributes to dismantling structural racism, building a more equitable society, and eliminating health inequities. But we cannot change what we cannot measure.14 Reliable, replicable, and theoretically informed structural racism measures are required to improve our understanding of structural racism and health inequities.14,16,20 Thus, we conducted a scoping review to understand the current knowledge, highlight interdisciplinary innovations, and identify gaps in the literature on structural racism measurement. We reviewed the most recent academic, peer-reviewed, and gray literature on structural racism measurement during 2019–2021. Our objective in writing this article is to describe the state of structural racism measurement in epidemiology and other health research and establish steps to improve structural racism measures. We synthesized the study findings to inform our recommendations for future efforts to better understand the complex mechanisms linking structural racism and racial health inequities.
Methods
Scoping reviews are quasi-systematic reviews used to aid understanding research on emerging topics that are distributed across published peer-reviewed and gray literature or located in different academic disciplines.21 Gray literature includes, but is not limited to, the following materials: reports (eg, preprints, preliminary progress and advanced reports, technical reports, statistical reports, memoranda, state-of-the-art reports, market research reports), theses and dissertations, conference proceedings, technical specifications and standards, noncommercial translations, bibliographies, technical and commercial documentation, and official documents not published commercially (primarily government reports and documents).22 The inclusion of gray literature in our search allows us to highlight new innovations and/or those intended for broader audiences beyond academic researchers. The scoping review for this study was focused on literature published from January 1, 2019, through December 31, 2021, to avoid duplicating the work already done by Groos et al., which explored peer-reviewed literature published during 2007–2017.16 For this review, we included only literature about structural racism in the United States that was published in English. We purposely excluded literature published in 2018 to avoid potential overlaps between the search conducted by Groos et al.16 and our search.
Literature search and management
Two graduate research assistants (GRAs) conducted an extensive literature search under the supervision of 2 doctorate-level researchers (referred to here as “lead authors” and who were blinded for the review). We also received assistance in literature search strategies across various online databases from a public health librarian who also was blinded for the review.
Our search had 2 parts. The first part focused on peer-reviewed literature. The search strategy was built and tested for sensitivity in Ovid MEDLINE using Medical Subject Heading terms and keywords. After reflection and feedback from the lead authors, the public health librarian applied the search strategies to 3 additional databases: PsycINFO, Academic Search Premier, and Race Relations Abstracts. Two conceptual domains were used to build the list of relevant search terms: the strategy for structural racism was designed to be specific rather than sensitive, due to large numbers of irrelevant records during the test phase, and the strategy for tools and indices was inclusive. Our full search strategies are listed in Appendix S1.
The second part of our search focused on gray literature. Appendix S2 shows the databases and specific search terms we used to conduct this part of our review. The gray literature was found through Google Scholar, Google (google.com), ProQuest Dissertations and Theses (proquest.libguides.com/PQDT), MedRxiv (medrxiv.org/), and Open Science Framework Preprints (https://osf.io/). The first 25 pages of returned search results were retained, and the first 5 pages in 1 case (MedRxiv), because an initial scan of the results with the given search term indicated there were no truly relevant articles listed in the few previous or subsequent pages. For the dissertation and theses search, we included all results from our search. We also included the “anywhere except full text” filter to only search for studies in which structural racism was central to the study, as indicated by inclusion in the article metadata, rather than just mentioned in other sections of the articles.
Throughout the literature search, we used Zotero (https://www.zotero.org), a citation manager that allowed us to sort all articles into “included,” “maybe included,” and “excluded” folders; document the search engine through which each article was found and which search terms were used; and remove duplicated articles that were present in multiple databases.
Inclusion and exclusion criteria
Article selection was an iterative process. First, we used the search strategies described above to identify peer-reviewed and gray literature that focused on the development of structural racism measures and/or the application of such measures to elucidate racial health inequities. Next, the GRAs reviewed the article titles and abstracts, then sorted each article into “included,” “excluded,” or “maybe included.” Included literature mentioned measures of structural racism, institutional racism, or systemic racism for use with any racialized group. Excluded literature focused primarily on interpersonal racism or discrimination, other forms of racism (eg, cultural racism), literature published before 2019, and literature that did not allude to or mention any aspect of measurement of racism. The GRAs met with the lead authors weekly to report their progress and discuss issues that came up (eg, whether articles that only mentioned structural racism as an explanation in the discussion should be included, how to handle studies that were both published in a dissertation and subsequently published in a peer-reviewed journal), and both progress and issues that arose, as well as how to standardize decisions around these issues for all reviewing parties. When the GRAs were unsure if articles should be included or excluded, the lead authors made the final determination.
Once an initial set of articles was identified, the lead authors reviewed the abstracts of articles labeled as “include” and “maybe include.” Differences in opinion for the “maybe include” articles were discussed until the 2 lead authors reached a consensus. Once this first abstract review was completed, the lead authors double reviewed the full text of every article and further excluded those that did not meet inclusion criteria or were duplicates.
Data extraction
During the full-text review, the lead authors extracted the following: title, authors, year of publication, measure development or application, use of a single or multidimensional measure, data used, and outcomes. Subsequently, 2 additional reviewers (who did not supervise the GRAs) repeated the same full-text reviewing process described above. Finally, these 4 reviewers convened to discuss key themes, innovations, gaps, and future opportunities and directions.
Results
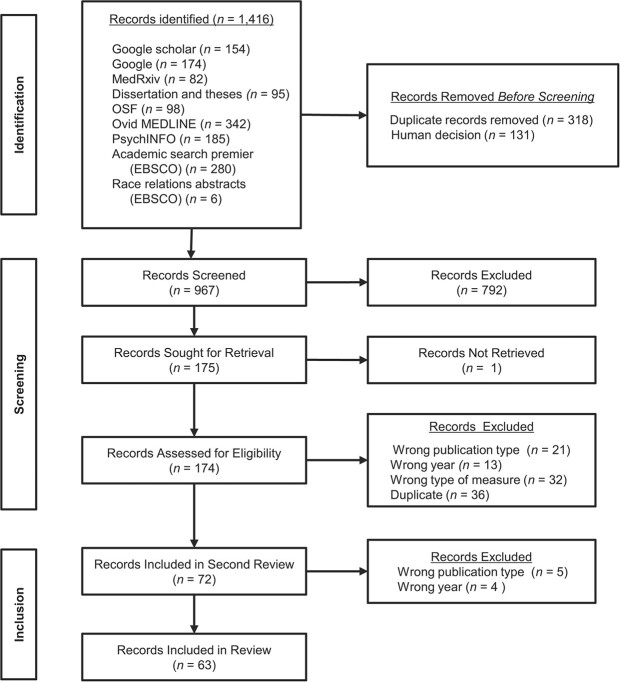
Of the 1416 articles identified, 63 fit our inclusion criteria and were reviewed (Figure 1). Table 1 summarizes the included studies, the domains of structural racism (ie, sectors in which structural racism manifest), and the measures these studies used. The number of studies included in our scoping review covering 2019–2021 tripled the number of studies that Groos et al.16 identified over a 10-year period.
Figure 1.
Identification of studies via databases and other methods.
Table 1.
Description of included articles.
| First Author, Year, Reference No. | Article Title | Domains | Racial Comparisons | Measures of Structural Racism |
|---|---|---|---|---|
| Agénor, 202187 | “Developing a database of structural racism–related state laws for health equity research and practice in the United States” | Electoral, judicial, carceral, immigration, housing, banking, education, policing | N/A | Typology of contemporary legal domains pertaining to state-level structural racism |
| Allgood, 202131 | “Equal protection under the law: the measurement of structural racism and health disparities” | Environment, police exposure, residential segregation, school segregation | Black-White | Pre-post racialized event (a situation in which marginalized groups are more affected; vicarious exposure, ie, Flint Water Crisis Declaration); number of police encounters; index of dissimilarity; index of isolation; ICE (race) in census tract and in school |
| Bell, 201928 | “Associations between obesity, obesogenic environments, and structural racism vary by county-level racial composition” | Socioeconomics | Black-White | County-level Black-White ratios for median income, percentage living below the poverty line, percentage who completed a 4-year college degree, percentage who were unemployed, and percentage who were homeowners. Split into quartiles (low, medium, medium-high, high) |
| Bell, 202032 | “Self-rated health and structural racism indicated by county-level racial inequalities in socioeconomic status: the role of urban–rural classification” | Education, housing, economics | Black-White | Median income; percentage who completed a 4-year college degree; percentage who were unemployed; percentage among Black people and non-Hispanic White people who were homeowners; dissimilarity index |
| Bishop-Royce, 202133 | “Structural racism, socioeconomic marginalization, and infant mortality” | Socioeconomic segregation | Black-White | ICE |
| Blanco, 202134 | “The impact of residential segregation on pancreatic cancer diagnosis, treatment, and mortality” | Residential segregation | Black-White | Index of dissimilarity |
| Blebu, 201972 | “An examination of preterm birth and residential social context among Black immigrant women in California, 2007–2010″ | Residential context, segregation | Black immigrants | Neighborhood co-ethnic density (the proportion of foreign-born Black people per total tract population), Black racial concentration as the proportion of Black residents (per total tract population) in each tract for segregation, neighborhood deprivation index |
| Brown, 202035 | “Structural factors and racial disparities in severe maternal morbidity: an examination of state- level indicators of structural racism and severe maternal morbidity among Black and White persons in the U.S., 2009–2011” | Criminal justice, political participation, education, and employment | Black-White | Criminal justice: the incarcerated proportion of the state’s adult population. Political participation: the proportion of the state’s citizen population registered to vote, and the proportion of the state’s citizen population who voted. Education: the proportion of the state’s population aged 25 years or older with a bachelor’s degree or higher, and the state’s 4-year adjusted cohort high school graduation rate. Each measure was constructed separately for the state’s Black and White populations. |
| Butler, 202065 | “Generational impacts of 1930s housing discrimination and the imperative need for the healthy start initiative to address structural racism” | Housing | Black | HOLC assessed categories and redlining. |
| Chambers, 202066 | “Exposures to structural racism and racial discrimination among pregnant and early post-partum Black women living in Oakland, California” | Socioeconomic segregation | Black | ICE (race plus income) |
| Chambers, 201936 | “Using index of concentration at the extremes as indicators of structural racism to evaluate the association with preterm birth and infant mortality–California, 2011–2012” | Residential segregation | Black-White | ICE (race; income; race plus income) |
| Chantarat, 202137 | “The intricacy of structural racism measurement: a pilot development of a latent- class multidimensional measure” | Housing, education, socioeconomics | Black-White | Dissimilarity index, disproportional index for education, employment, and ownership, ICE (income). |
| Collin, 202038 | “Neighborhood-level redlining and lending bias are associated with breast cancer mortality in a large and diverse metropolitan area” | Redlining, banking | Black-White | Redlining, lending bias |
| Diaz, 202139 | “Association of historic housing policy, modern day neighborhood deprivation and outcomes after inpatient hospitalization” | Housing | Black-White | HOLC assessment |
| Dougherty, 202027 | “Measuring structural racism and its association with BMI” | Education, housing, employment, criminal justice, health care | Black-White | Housing dissimilarity index; school dissimilarity index; ratios of Black-White high school graduates, incarceration, poverty, primary care, and ambulatory care |
| Dyer, 202140 | “The index of concentration at the extremes (ICE) and pregnancy-associated mortality in Louisiana 2016–2017” | Socioeconomic, housing segregation | Black-White | ICE (race plus income) |
| Dyer, 201967 | “Mass incarceration and public health: the association between Black jail incarceration and adverse birth outcomes among Black women in Louisiana” | Housing | Black | HOLC assessment, ICE (income, homeownership) |
| English, 2021,41 | “Intersecting structural oppression and Black sexual minority men’s health” | Residential segregation, incarceration, education, economics | Black-White | State racism index, Human Rights Campaign’s 2018 state equality index |
| Farhad, 202142 | “Association between disparities in intergenerational economic mobility and cause-specific mortality among Black and White persons in the United States” | Economics | Black-White | Economic mobility gap |
| Fernandez-Esquer, 202173 | “Structural racism and immigrant health: exploring the association between wage theft, mental health, and injury among Latino day laborers” | Economics | Latino | Wage theft |
| Graetz, 202130 | “Historical redlining and contemporary racial disparities in neighborhood life expectancy” | Housing, education | Black-White | Census tract–level HOLC redlining grades; county-level total urban renewal projects; school segregation at the district-level; ICE (race, class); tract-level home values; tract-level race-class segregation |
| Hollenbach, 202143 | “Associations between historically redlined districts and racial disparities in current obstetric outcomes” | Redlining | Black-White | HOLC assessment |
| Homan, 202144 | “Structural intersectionality as a new direction for health disparities research” | Structural intersectionality (racism plus sexism) across economic, educational, judicial, political, and segregation | Black-White | Ratios (Black people to White people) of the following: incarceration; disproportionate level of disenfranchisement of Black people; proportion with a bachelor’s degree; unemployed rate; poverty rate; proportion who are homeowners; proportion who voted in 2008; and level of Black peoples’ political underrepresentation in state legislatures; state-level dissimilarity index (Black-White) of residential segregation |
| Houghton, 202145 | “Firearm Homicide Mortality is Influenced by Structural Racism in US Metropolitan Areas” | Residential segregation, socioeconomics | Black-White | Dissimilarity index, percentage of the metropolitan area that is Black, population density, poverty rates, measures of educational attainment, crime rates, and a measure of state firearm legislation strength |
| Ibragimov, 202168 | “Police killings of Black people and rates of sexually transmitted infections: a cross-sectional analysis of 75 large US metropolitan areas, 2016″ | Policing | Black | Number of police killings of non-Hispanic Black people in 2015 |
| Janevic, 202146 | “Racial and economic neighborhood segregation, site of delivery, and morbidity and mortality in neonates born very preterm” | Residential segregation | Black-White | ICE (race plus income) |
| Kihlström and Kirby, 202129 | “We carry history within us: anti-Black racism and the legacy of lynching on life expectancy in the U.S. South” | Direct violence/lynching | Black | Population adjusted rate of historic lynching 1877–1950 |
| Knopov, 201947 | “The role of racial residential segregation in Black-White disparities in firearm homicide at the state level in the United States, 1991–2015” | Residential segregation | Black-White | Index of dissimilarity |
| Krieger, 202048 | “Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017″ | Housing, economic | Black-White | HOLC assessment, ICE (race plus income; race plus homeowner) |
| Larimore, 2019,49 | “Routes to low birth (or not): local, cultural racism in exceptional communities” | Socioeconomics, power, freedom | Black-White | Percentage of each racial group in a managerial position; Black-White ratios of the following: median household income; proportion with a bachelor’s degree or higher; proportion between the ages of 16 and 64 years who are currently unemployed; proportion of each racial group with incomes below 100% of the federal poverty line; social connection; isolation index; sex ratios by race and age to capture the population removal of lack men due to incarceration, index of spatial proximity, Black-White jail population gap for each MSA |
| Leos, 202074 | “Examining the effect of state- and individual-level structural racism on Latino adolescent sexual risk behaviors: an intergroup and intragroup analysis” | Education, criminal justice | Black-White Latino-White |
State-level structural racism (disparities in high school completion rates, disparities in bachelor’s degree completion rates, disparities in juvenile commitment rates) |
| Linton, 202075 | “Mortgage discrimination and racial/ethnic concentration are associated with same-race/ethnicity partnering among people who inject drugs in 19 US cities” | Residential segregation, housing | Black-White; Latino-White | ICE, mortgage loan denial |
| Liu, 201950 | “Structural racism and severe maternal morbidity in New York State” | Education, employment, criminal justice | Black-White | Disproportionality measure in female educational attainment, female employment, and incarceration |
| Lundberg, 202176 | “Quantifying the contribution of occupational segregation to racial disparities in health: a gap-closing perspective” | Occupational segregation | Black-White Hispanic-White Other race-White |
No measure; use a counterfactual method to measure the effect of equalizing occupational opportunity on racial health disparity |
| Lynch, 202151 | “The legacy of structural racism: associations between historic redlining, current mortgage lending, and health” | Redlining | Black-White | Historical redlining, contemporary lending discrimination |
| Martz, 202169 | “Pathways linking census tract typologies with subjective neighborhood disorder and depressive symptoms in the Black Women’s Experiences Living with Lupus (BeWELL) Study” | Residential segregation | Black | Evenness dimension of racial residential segregation |
| Matoba, 2019,52 | “Mortgage discrimination and preterm birth among African American women: an exploratory study” | Residential segregation | Black-White | Redlining index |
| Mitchell, 202183 | “Tract level associations between historical residential redlining and contemporary fatal encounters with police” | Redlining | N/A | HOLC assessment |
| Mujahid, 202177 | “Historical redlining and cardiovascular health: The Multi-Ethnic Study of Atherosclerosis” | Housing/redlining | Black-White Hispanic-White Chinese-White |
HOLC assessment |
| O’Brien, 202053 | “Structural racism, economic opportunity, and racial health disparities: evidence from US counties” | Economics | Black-White | Racial opportunity gap |
| Owens-Young, 2020,63 | “Structural racial inequities in socioeconomic status, urban–rural classification, and infant mortality in US counties” | Socioeconomics, education, housing | Black-White | Black-White ratios in median income, the percentage who completed a 4-year college degree, percentage who were unemployed, and percentage who were homeowners; dissimilarity index |
| Pabayo, 2019,54 | “Structural racism and odds for infant mortality among infants born in the United States 2010″ | Electoral, employment, criminal justice | Black-White | Prison incarceration and juvenile custody rates; sentencing rates; capital punishment; ratios of the proportion of the population aged ≥25 years with bachelor’s degree or higher, the proportion of civilian labor force not currently employed, proportion employed in management, business, science, and arts occupations, median household income |
| Pohl, 202178 | “Relationship between residential segregation, later-life cognition, and incident dementia across race/ethnicity” | Residential segregation | Black-White Hispanic-White |
Index of dissimilarity, index of isolation, index of interaction |
| Poulson, 202155 | “Residential racial segregation and disparities in breast cancer presentation, treatment, and survival” | Residential segregation | Black-White | Index of dissimilarity |
| Poulson, 202156 | “The role of racial segregation in treatment and outcomes among patients with hepatocellular carcinoma” | Residential segregation | Black-White | Index of dissimilarity |
| Poulson 202157 | “The impact of racial residential segregation on prostate cancer diagnosis and treatment” | Residential segregation | Black-White | Index of dissimilarity |
| Poulson, 202158 | “The impact of racial residential segregation on colorectal cancer outcomes and treatment” | Residential segregation | Black-White | Index of dissimilarity |
| Poulson, 202182 | “Historic redlining, structural racism, and firearm violence: a structural equation modeling approach” | Housing | N/A | HOLC assessment |
| Richardson, 202070 | “Reparations for Black American descendants of persons Enslaved in the US and their estimated impact on SARS-CoV-2 transmission” | Economics | Black | Gini coefficient: a hypothetical program of reparations for Black American descendants of persons enslaved in the United States |
| Samari, 202185 | “Measuring structural xenophobia: US state immigration policy climates over ten years” | Immigration | All races | Immigration Policy Climate Index, which quantifies and tracks policies enacted by US states that have differential impacts on residents, based on immigration or legal status |
| Samari, 202184 | “The Muslim ban and preterm birth: analysis of US vital statistics data from 2009 to 2018″ | Immigration | Women born in 1 of the countries included in the Executive Order 13769 Muslim ban | No measure, instead used counterfactual analysis that removes the effect of the Executive Order 13769 Muslim ban |
| Sewell, 202159 | “Political economies of acute childhood illnesses: measuring structural racism as meso level mortgage risks” | Housing and banking | Black-White | Neighborhood credit refusals, racialized credit refusals, neighborhood credit privateness, racialized credit privateness |
| Shim, 2021110 | “Race and ethnicity of editorial board members and editors as an indicator of structural racism in psychiatry and neuroscience journals” | Education and publishing | Black, Asian, Hispanic/Latinx, White | Participation in the editorial team (editor-in-chief, editorial board members) in psychiatry journals |
| Siegel, 202123 | “Racial/ethnic disparities in state-level COVID-19 vaccinations rates and their association with structural racism” | Economics, employment, incarceration, education, housing | Black-White Hispanic-White |
State racism index |
| Siegel, 202124 | “Actual racial/ethnic disparities in COVID-19 mortality for the non-Hispanic Black compared to non-Hispanic White population in 35 US states and their association with structural racism” | Economics, employment, incarceration, education, housing | Black-White | State racism index |
| Siegel, 202160 | “The relationship between racial residential segregation and Black-White disparities in fatal police shootings at the city level, 2013–2017” | Residential segregation | Black-White | Dissimilarity index |
| Stermon and Lukinbeal, 202180 | “Institutionalized racism: redlined districts then and now in Boston, Detroit, and Los Angeles” | Residential segregation | Non-White compared with White | Proportion of non-White people in the census tract, dissimilarity index, HOLC assessment |
| Sudhinaraset, 202186 | “Analysis of state-level immigrant policies and preterm births by race/ethnicity among women born in the US and women born outside the US” | Immigration | White, Asian, Black, Hispanic (for the outcome, not the measure) | Criminalizing and integration of immigrant policies variables |
| Tackett, 202071 | “Structural racism and its influence on the severity of atopic dermatitis in African American children” | Residential segregation | Black-White Latino-White |
Dissimilarity index |
| Tan, 202161 | “Structural racism and COVID-19 in the USA: a county-level empirical analysis” | Residential segregation | Black-White | Black-White spatial exposure, P~* score; Spatial Information Theory Index; the following Black-White ratios: poverty; employment; county-level jail incarceration rate |
| Treuhaft, 202081 | “The racial equity tool index: a new data tool to drive local efforts to dismantle structural racism” | Economics, educational, environmental | Compare “population” with each race: White, Black, Latino, API, Native American, mixed race | Racial equity index; prosperity score |
| Vilda, 202162 | “Structural racism, racial inequities, and urban–rural differences in infant mortality in the US” | Jail incarceration | Black-White | Parish-level jail incarceration prevalence |
| Volpe, 202164 | “State- and provider- level racism and health care in the US” | Socioeconomic, judicial, political | Black-White | State-level structural racism using political participation, employment and job status, educational attainment, and judicial treatment modeled after Lukachko, Hatzenbuehler, and Keyes (2014). |
| White, 202126 | “Residential racial segregation and social Distancing in the United States during COVID-19″ | Residential segregation | Black-White | Dissimilarity index |
Abbreviations: API, Asian and Pacific Islander; Black-White, Black and White (as with Latino-White, Hispanic-White, and so forth); HOLC, Home Owners’ Loan Corporation; ICE, index of concentration at the extremes; MSA, Metropolitan Statistical Area; N/A, not applicable.
Table 2 summarizes structural racism measures and their derivation strategies, the data required for their derivation, and the health outcomes these measures explain. Two commonly used data sources were the Home Owners’ Loan Corporation (HOLC) and the Home Mortgage Disclosure Act data to measure redlining. Decennial Census data and American Community Survey data were also used extensively to create ratios between measures for Black or other racialized populations relative to the White population. The HOLC, Home Mortgage Disclosure Act , decennial Census, and American Community Survey data are publicly available. The health outcomes most often analyzed with any of the included measures in Table 2 were measures that examined infant and maternal health outcomes (eg, preterm, low-birthweight birth, maternal morbidity), which made up most of the studies we identified. Examples of other outcomes examined included COVID-19–related behaviors and outcomes,23‑26 body mass index,27,28 and life expectancy.29,30 Our review revealed 8 key themes in how epidemiologists and other health researchers are operationalizing and measuring structural racism.
Table 2.
Structural racism measures derivation.
| Structural Racism Measure | Data Sources | Methodology for Estimation | Health Outcome | First Author, Year, Reference No. |
|---|---|---|---|---|
| Residential dissimilarity index | American Community Survey |
Where: ai = the population of group A in the ith area (eg, census tract) A = the total population in group A in the large geographic entity for which the index of dissimilarity is being calculated bi = the population of group B in the ith area B = the total population in group B in the large geographic entity for which the index of dissimilarity is being calculated n = number of large geographic entities |
Atopic dermatitis Firearm homicides Self-reported health Cardiovascular risk Pancreatic adenocarcinoma Firearm homicides Cognitive performance incident dementia Breast cancer Hepatocellular carcinoma Prostate cancer Colorectal cancer Fatal police shootings No health outcome Black-White county-level mobility ratio |
Tackett, 202071 Houghton, 202145 Owens-Young and Bell, 202032 Allgood, 202131 Blanco, 202134 Knopov, 201947 Pohl, 202178 Pouslon, 2021a55 Poulson, 2021b56 Poulson, 2021c57 Poulson, 2021d58 Siegel, 201960 Stermon, 202180 White, 202126 |
| School dissimilarity index | Department of Education Common Core of Data | Similar to above for the residential dissimilarity index but the smaller and large units of measurement in the equation are school and school district, respectively For more information, see Reardon and Townsend27 |
Body mass index | Dougherty, 202027 |
| Isolation index | US Census of Population and Housing |
Where: n = the number of areas (census tracts) in the metropolitan area, ranked smallest to largest by land area xi = the minority population of area i X = the sum of all xi (the total minority population) ti = the total population of area i |
Cardiovascular risk Cognitive performance incident dementia |
Allgood, 202131 Pohl, 202178 |
| Interaction index | American Community Survey Data |
Where: n = the number of areas (census tracts) in the metropolitan area, ranked smallest to largest by land area xi = the minority population of area i X = the sum of all xi (the total minority population) yi = the majority population (non-Hispanic white) of area i ti = the total population of area i |
Cognitive performance incident dementia | Pohl, 202178 |
| Evenness | US Census data | Evenness was assessed using divergence scores that quantify the difference between Black-White racial composition at the tract-level to the broader Atlanta, GA, metropolitan statistical area. | Systemic lupus erythematosus | Martz, 202169 |
| ICE | American Community Survey (for census tract measure) Elementary/Secondary Information System (for school district measure) |
Can be used for race, income, and race plus income, in various geographic unit (e.g., census tract, school district) Where: A = number of white households with income of $100 000 or higher (privileged group) P = number of Black households with income lower than $25 000 (deprived group) T = total number of Black and White households in the PUMA ICE ranges from −1 (all households are in the deprived group) to 1 (all households are in the privileged group). |
Infant mortality Preterm birth Infant mortality Pregnancy-associated mortality Discrimination life expectancy Cardiovascular risk Neonatal mortality and morbidity Characteristics of sexual partner |
Bishop-Royse, 202133 Krieger, 202048 Chambers, 201936 Dyer, 202140 Chambers, 202066 Graetz and Esposito, 202130 Allgood, 202131 Janevic, 202146 Linton, 202075 |
| School-district-level ICE | The average ICE in the school districts overlapping with each Census tract.
|
Cardiovascular risk Life expectancy |
Allgood, 202131 Graetz and Esposito, 202130 |
|
| Black-White spatial exposure score (P*) | American Community Survey |

Where:  = weighted proportion of White individuals within census tract q’s local environment = weighted proportion of White individuals within census tract q’s local environment = total number of Black individuals within county = total number of Black individuals within county = total number of Black individuals within census tract = total number of Black individuals within census tractq = each census tract |
COVID-19 cases at a county level | Tan, 202125 |
| Spatial Information Theory Index, H | American Community Survey |
Where: E = overall county entropy of the total population calculated as   =population density at q =population density at qT = total population in county |
COVID-19 cases at a county level | Tan, 202161 |
| ISP | American Community Survey |
Where:  and (g,G) = (x,X), (y,Y), (t,T) and (g,G) = (x,X), (y,Y), (t,T)n = number of areas in the metropolitan areas, ranked smallest to largest by land area xi = the minority population of area i X = the sum of all xi yi = the majority population of area i Y = the sum of all yi ti = the total population of area i T = the sum of all ti P = the ratio of X to T |
Low birthweight | Larimore, 201949 |
| Black-White disproportionality ratios | American Community Survey Robert Wood Johnson Foundation County Health Rankings Vera Institute of Justice (consolidation of data from the US Department of Justice Bureau of Justice Statistics Census of Jails and the Annual Survey of Jails, National Prisoner Statistics) |
Ratios span measures of socioeconomic status, political participation, ambulatory care, and incarceration rates. Ratio = rate for Black people to rate for White people |
Obesity and obesogenic environment Self-rated health Low birthweight Infant mortality rate Neonatal mortality Preterm birth COVID-19 cases at a county level Severe maternal morbidity Early sexual initiation, multiple sex partners No health outcome |
Bell, 201928 Bell, 202032 Larimore, 201949 Owens-Young, 202032 Pabayo, 201954 Pabayo, 201954 Blebu, 201972 Tan, 202161 Brown, 202035 Liu, 201950 Leos, 202074 Stermon, 202180 |
| Multidimensional measure of structural racism | American Community Survey | Multidimensional typologies derived from 5 structural racism measures: (1) Black-white residential segregation (measured with a dissimilarity index); (2) Black-white education inequity; (3) Black-white employment inequity; (4) Black-white homeownership; (5) Income equity (measured by the index of concentration at the extremes). Multidimensional typologies are identified with the latent class analysis model. |
COVID-19 vaccination rate | Chantarat, 202137 |
| State racism index | American Community Survey Vera Institute of Justice Jail Incarceration |
Average of segregation index, incarceration index, education index, economic index, and employment index—all measured at the state level. See Siegel et al.23 (Table 2) for the equations for all the measures. | Black-White proportion of COVID-19 vaccination rate | Siegel, 202123 |
| State racism index (adapted from Mesic et al. J Natl Med Assoc. 2018;110(2):106–16) | US Census data, US Bureau of Justice Statistics and US Census data | Each individual indicator, other than the dissimilarity index and isolation index, consisted of the state Black-White ratio. For each indicator, ratios were converted into a scale from 0 to 100. To derive an overall racism index for each dimension, scores for each component within that dimension were averaged. Then, to obtain a single, overall state racism index, scores for each of the 5 dimensions were averaged together. Then, each score across the years was averaged. Indicators used included: dissimilarity index, isolation index, incarceration rate, educational attainment, poverty status, median annual household income, rental housing percentage, nonlabor force participation, and unemployment. | Psychological and behavioral outcomes (depression, burdensomeness as a proximal cause of suicidal desire, alcohol use disorder, HIV testing) | English, 202141 |
| Structural intersectionality (state-level) | US Census Bureau data, Bureau of Labor Statistics Center for American women and Politics Guttmacher Institute |
Summation of the score from the following measures: Black-White ratios of incarceration, proportion with a bachelor’s degree, unemployed rate, poverty rate, proportion who are homeowners, proportion who voted in 2008 Blacks’ disproportionate level of disenfranchisement Level of political underrepresentation of Black people in state legislatures State-level dissimilarity index (Black-White) of residential segregation |
Self-rated health | Homan, 202144 |
| IPC Index | The Urban Institute Center for Health Journalism Kaiser Family Foundation Medicaid.gov National Immigration Law Center Georgetown University Health Policy Institute uLEAD National Council of State Legislatures FindLaw Law Logix Homeland Security Today Department of Homeland Security Immigration Forum Immigration and Customs Enforcement |
Fourteen policies were included across 5 domains (Wallace et al. SSM Popul Health. 2019;7:016–016): public health and welfare benefits (5 policies), higher education (2 policies), labor and employment (2 policies), driver’s license and identification (2 policies), and immigration enforcement (3 policies). The research team coded the values in the IPC index, in alignment with the Young and Wallace (Am J Public Health. 2019;109:1171–1176) framework, considering “-1 = exclusionary,” “0 = neither,” and “1 = inclusionary” to capture both exclusive and inclusive state environments. The IPC index was then calculated by summing the values for all 14 policies, with more-negative scores indicating exclusionary contexts and positive scores indicating inclusive environments. | No health outcome | Samari, 202185 |
| Criminalizing and integration immigrant policies variables | National Council of State Legislatures Health care coverage maps National Immigration Law Center National Employment Law Project US Department of Agriculture, Food and Nutrition Service National Health Law Program |
Six criminalizing immigrant policies, categorized as such because they create mechanisms of surveillance and immigration enforcement across the following 3 sectors: work authorization, immigration enforcement and criminal justice, and identification and licensing, and 14 inclusive immigrant policies across the following 4 sectors: health and social service benefits, education, labor and employment, and language access. States were coded “1” if the policy was in effect and “0” if not. These values were then summed to create continuous criminalizing (0–6) and inclusive immigrant policy indices (0–14) for each state. | Preterm birth | Sudhinaraset, 202186 |
| County structural racism | Census of jail inmates Department of Education Common Core of Data American Community Survey Dartmouth Atlas of Health Care |
A factor score from confirmatory factor analysis combining the following measures: Ratios of Black-White jail incarceration, high school graduation, poverty, ratio of proportion of Medicare beneficiaries discharged from a hospital for an ambulatory care sensitive condition, average annual proportion of Medicare enrollees having at least 1 ambulatory visit to a primary care clinician School dissimilarity index H entropy index |
Body mass index | Dougherty, 202027 |
| County Structural Racism score | American Community Survey Vera Institute of Justice Jail Incarceration data |
Summation of 3 dichotomizing county-level structural racism measures. For each measure, the value higher than the 75th percentile of all US counties is considered “high” (score 1), or “low” (score 0) otherwise The 3 structural racism measures that make up the county structural racism score are: Black-White ratios in proportions of the population age 25 years and older with a bachelor’s degree or higher, median household income, and jail incarceration |
Infant mortality rate | Vilda, 202162 |
| Overall measure of state structural racism | US Decennial Census Current population survey US Department of Justice, Bureau of Justice Statistics data |
Summation of 8 dichotomized state-level structural racism measures. For each measure, the value higher than the median of all US states is considered “high” (score 1), or “low” (score 0) otherwise. The 8 structural racism measures that make up the state structural racism score are: Black-White ratios in proportions of the population who: earned a bachelor’s degrees or higher, registered to vote, voted, are in civilian labor force, are employed, hold executive position, have a professional specialty, and incarceration |
Health care access | Volpe, 202164 |
| Agénor’s typology of structural racism policies | Westlaw Next, LexisNexis, Hein Online, 2010–2013 | “Typology of contemporary legal domains pertaining to state level structural racism.” 10 domains: voting rights, stand-your-ground laws, racial profiling laws, mandatory minimum prison sentencing laws, immigrant protections, fair-housing laws, minimum-wage laws, predatory lending laws, laws concerning punishment in schools, and stop-and-identify laws. The scholars then identified the scope and features (eg, population covered or affected, length of related sentence, exceptions, enforcement mechanisms) of each law using primary and secondary (ie, law review articles, legal reports) sources. The authors then characterized each law using a set of mutually exclusive categories (assigned a numeric value) and compiled the categories into a preliminary coding scheme, and used the scheme to assign a numerical value to each state for each law in that year. The coding scheme was then revised and finalized on the basis of this process. The authors developed a guide defining each law and its categories and outlining key questions to consider when assigning a numerical value to each state and the District of Columbia for each law using the scheme. | No health outcome | Agénor, 202187 |
| Dual mortgage market political economies measures | Project of Human Development in Chicago Neighborhoods Home Mortgage Disclosure Act Neighborhood Change Database |
A set of 4 measures includes: Neighborhood credit refusals: Ratio of the rate of access to the mortgage market for ethnoracially marginalized applicants (Black people and Latinx people) to the rate for ethnoracially privileged applicants (White people) for a specific area. Racialized credit refusals: Ratio of the rate of access to the mortgage market for ethnoracially marginalized applicants (Black people and Latinx people) to the rate for ethnoracially privileged applicants (White people) across areas. Neighborhood credit privateness: Ratio of the rate of the federal oversight of originated loans for ethnoracially marginalized applicants (Black people and Latinx people) to the rate for ethnoracially privileged applicants (White people) for a specific area. Racialized credit privateness: Ratio of the rate of the federal oversight of originated loans for ethnoracially marginalized applicants (Black people and Latinx people) to the rate for ethnoracially privileged applicants (White people) across areas. |
Acute illnesses of cold or flu, sinus trouble, sore throat or tonsils, headache, upset stomach, bronchitis, skin infection, pneumonia, urinary tract infections, fungal disease, mononucleosis | Sewell, 202159 |
| HOLC-assessed redlining measure | HOLC data Richmond Mapping Project |
1930s HOLC neighborhood grading map | Life expectancy Preterm birth Healthy Start initiative participation Fatal police shootings Firearm homicides Breast cancer deaths Ideal cardiovascular health, health behaviors, and health factors No health outcome Mortality |
Graetz and Esposito, 202130 Krieger, 202048 Matoba, 201952 Hollenbach, 202143 Butler, 202065 Mitchell, 202183 Poulson, 202182 Collin, 202038 Mujahid, 202177 Stermon, 202180 Diaz, 202139 |
| Lending bias or denial | Home Mortgage Disclosure Act data | The odds of denial of a mortgage application from a non-Hispanic Black or Hispanic applicant compared with denial of a non-Hispanic White applicant desiring to move in the same census tract, controlling for applicant sex and the ratio of the loan amount to applicants reported annual income | Breast cancer deaths Characteristics of sexual partner |
Collin, 202138 Linton, 202075 |
| Parish-level jail incarceration prevalence among Black individuals | Vera Institute of Justice (jail incarceration data) | Count of Black individuals aged 16 to 64 years in jail per 1000 Black, nonincarcerated residents. | Preterm birth and low birthweight | Dyer, 201967 |
| Racialized event (ie, Flint Water Crisis) | N/A | Vicarious exposure to structural racism-related events. Residency in the areas after the racialized event occurs is treated as an exposure in a quasi-experimental model (eg, difference-in-difference). | Birthweight, gestational age, size for gestational age | Allgood, 202131 |
| No. of police encounters | AddHealth | Response to survey question: “How many times have you been stopped or detained by the police for questioning about your activities? Do not count minor traffic violations.” This 5-level categorical variable includes response options ranging from 0 (never) to 6 or more times. |
Cardiovascular risk | Allgood, 202131 |
| No. of police killings | The Guardian’s The Counted Database | The number of police killings of non-Hispanic Black people in 2015 | Syphilis, gonorrhea, chlamydia | Ibragimov, 201968 |
| Lynching | Equal Justice Initiative lynching database | Population adjusted rate of historic lynchings 1877–1950 | Life expectancy | Kihlström, 202129 |
| Economic mobility gap | Opportunity Atlas | Intergenerational gap in upward economic mobility conditional on parental income for Black adults and White adults For details, see Chetty et al. National Bureau of Economic Research working paper 25 147; 2019. |
All-cause mortality gap Racial mortality gap |
Farhad, 202142 O’Brien, 202053 |
| Racial opportunity gap | Opportunity Insights Data Library | The difference in the average national income percentile ranking in adulthood achieved between White individuals and Black individuals in the same county born to parents at the 25th percentile of the national income distribution | Racial mortality gap | O’Brien, 202053 |
| County-level urban renewal projects | Richmond Renewing Project | The average of urban renewal projects in the counties overlapping with each Census tract | Life expectancy | Graetz and Esposito, 202130 |
| Tract-level home values | Zillow Home Value Index | See detailed description at https://www.zillow.com/research/zhvi-methodology-2019-highlights-26221/ | Life expectancy | Graetz and Esposito, 202130 |
| Racial equity index | National Equity Atlas | Uses an inclusion score and a prosperity score, also uses a formula for index of disparity (Pearcy and Keppel. Public Health Rep. 2022;117(3):273–280). | N/A | |
| Wage theft | Survey question | “In your last full day as a day laborer, would you say you were paid what was promised/agreed upon?” Responses ranged from 1 = strongly disagree to 4 = strongly agree. Responses for the wage-theft item were reverse scored so that higher scores indicated greater disagreement with the statement that the participant was paid what was promised or agreed upon. | Depression, isolation, alcohol use, severe injury, deportation stress | Fernandez-Esquer, 202173 |
| Participation on editorial team | Survey of editors-in-chief | Participation in editorial team (editor-in-chief, editorial board members) in psychiatry journals by race and ethnicity | None | Shim, 2021110 |
Abbreviations: Black-White, Black and White (as with Latino-White, Hispanic-White, and so forth); HOLC, Home Owners’ Loan Corporation; ICE, index of concentration at the extremes; IPC, Immigration Policy Climate; ISP, Index of Spatial Proximity; N/A, not applicable; PUMA, public use microdata area.
Focus on anti-Black and contemporary racism
Nearly two-thirds of the identified studies focused on anti-Black structural racism (ie, comparing the experiences of Black populations with those of White populations), with 3824,26‑28,30‑64 of 63 studies using either measures of Black and White (hereafter, Black-White) mixing in a specific spatial unit or Black-White disproportionality ratios (eg, rates of access to employment for Black compared with White county residents) to examine structural racism. Most studies used a between-group framework and used 1 or more anti-Black structural racism measures to elucidate Black-White health inequities. Of those that examined within-group effects of structural racism on Black health, 9 studies focused on how anti-Black racism drives poor health among US-born Black people,29,52,65‑71 and 1 study examined how co-ethnic density is associated with the health of foreign-born Black people (eg, African-born, Caribbean-born Black immigrants).72 Decentering White populations in analytical models allowed these researchers to examine heterogeneity in both exposure and the health effects of anti-Black structural racism for Black populations and to further understand why certain subgroups within this population are affected by structural racism more or less than others. Findings from a within-group framework like these studies further demonstrate that racism, not race, drives poor health among Black people.
Although the literature predominantly focuses on Black-White health inequities, we recognize that all racialized groups are affected by structural racism. Although it is unclear whether the oppression experienced by the non-Black racialized group (eg, Asian, Latinx, Native Americans) is a product of anti-Black and/or racialized group–specific structural racism (eg, xenophobia regarding Asian Americans, wage theft for Latinx people), the operationalization and measurement of structural racism for non-Black racialized groups are limited compared with the number of anti-Black structural racism measures available. Our search identified only 1 study that measured wage theft as a proxy for anti-Latinx structural racism.73 Another 10 studies applied anti-Black structural racism measures (eg, Black-White dissimilarity index) to investigate the impact of structural racism on health inequities between non-Black racialized groups and White people.23,74‑81
Segregation-driven measures
We identified 23 studies that use residential segregation measures, including the dissimilarity index (n = 15),26,31,34,41,45,47,55‑58, 60,63,71,78,80 index of concentration at the extremes (ICE; n = 9),30,31, 33,36,46,48,66,67,75 isolation index (n = 3),31,41,78 evenness (n = 1),69 and index of interaction (n = 1)78 to operationalize and measure structural racism. Although the dissimilarity index captures the distribution of racialized groups within a defined spatial unit, ICE can capture both racial residential segregation and income inequality, highlighting the distribution of privilege (white race and high income) and deprivation (Black race and low income) within a spatial unit.36
Beyond residential segregation
In addition to using residential segregation as a proxy of structural racism, various domains of structural racism were singularly measured, meaning they were investigated without any additional measure of another domain of structural racism. We identified the following domains in included studies: occupational segregation (n = 1)76; socioeconomic and economic inequities (n = 6)28,41,42,53,70,73 housing, home loans, and redlining (n = 9)38,39,43,51,59,65,77,82,83; incarceration (n = 1)67; policing (n = 1)68; publishing (n = 1)79; direct violence and lynching (n = 1)29; and immigration (n = 3).84‑86 Several studies also examined some combination of structural racism in education, housing, economic, environmental, judicial, civic, carceral, and health care measures (n = 21).23,24,27,30‑32,35,41,44,45,48‑50,54,63,64,72,74,75,81,87 Compared with articles that Groos et al. identified up to June 2017,17 more structural racism domains are measured in the present review. For example, 4 studies included measures of political participation,35,44,64,87 12 included measures of incarceration,23,24,27,35,41,44,49,50,54,61,62,67 and 4 examined racialized police encounters.31,68,83,87
Despite measuring several domains of structural racism, the above-mentioned group of studies23,24,27,30‑32,35,41,44,45,48‑50,54,63,64,72,74,75,81,87 examined the health effects of various domains of structural racism independently. For example, Brown35 and Liu et al.50 examined the association between structural racism in criminal justice, political participation, education, and employment relative to Black-White inequity in the rate of maternal morbidity in the United States. Neither study, however, examined how structural racism across these domains may interact and how the whole system generates poor health for racialized people relative to that of their White counterparts.
Structural racism as a spatial exposure
We identified 11 studies that measured structural racism at the state level,23,24,35,41,44,47,54,64,74,85,86 14 at the county level,26‑29,32,34,42,50,53,56,58,61‑63 6 at the metropolitan statistical area or city level,37,45,49,60,68,81 23 at a smaller neighborhood level (eg, census tract or block, zip code, community-area),24,30,33,36,38‑40 ,43,46,48,52,59,65,66,69‑72,77,78,80,82,83 and 5 at the individual exposure level.31,73,76,79,84 One study examined structural racism across 2 levels: Linton et al.75 examined the ICE for zip codes nested within counties, with mortgage loan denial measured at the county-level. However, most of the studies we identified examined area-level measures of racism at 1 level and did not examine how structural racism interacts across different levels.
Another consideration for structural racism measures tied to geographic units is how those measures perform in urban areas compared with rural areas. We found 3 studies that, using moderation in regression analyses, examined how county-level structural racism measures were performed in more rural versus more urban counties.28,32,62 The associations between structural racism and health varied by county rural–urban classification in this studies. Among these few studies, Bell and Owens-Young32 and Vilda et al.62 found nonsignificant associations between structural racism and self-reported health and infant mortality rates in rural areas. Both studies used the Black-White disproportionality ratios, operationalizing the rate of access to socioeconomic resources to measure structural racism among Black and White sampled populations.
Development of multidimensional measures
Of the 63 studies we identified, 42 examined single domains of structural racism (eg, residential segregation alone) and the other 21 considered the effect of various domains of structural racism (eg, residential segregation and education inequity) on the health of racialized people. Several studies estimated the independent effects of the various domains of structural racism on health. However, many studies used measures of structural racism in housing and socioeconomic status, putting 1 measure of each in a regression model, and discussing their relative association to a particular health outcome. With this approach, researchers demonstrate the independent effect of each domain of structural racism on health but cannot characterize the extent to which various domains of structural racism interact and their potential reinforcing effects on health.
We identified 9 studies23,24,27,37,41,44,47,62,64 that examined how 3 or more domains of structural racism interact with one another. In these studies, researchers used different methodologies to characterize the interconnection among various domains of structural racism and operationalize structural racism as a multidimensional, system-like determinant of health. Three studies we identified used the state racism index. This multidimensional index is the average of the standardized value of 5 state-level measures: (1) segregation index, (2) economic disparity index, (3) employment disparity index, (4) incarceration gap index, and (5) education attainment gap index. Dougherty et al.27 (the county structural racism measure) and Chantarat et al.37 (the multidimensional measure of structural racism) both followed the latent-construct approach used commonly among psychometricians for data reduction to consolidate multiple correlated characteristics. Unlike the state racism index, the 2 latent-construct measures in these 2 studies only were applied to 1 data set each (Dougherty et al.27 used the Behavioral Risk Factor Surveillance System data; Chantarat et al.37 used COVID-19 vaccination data from New York City).
In addition to examining structural racism, Homan et al.44 introduced a structural intersectionality measure that examined the intersection among multidimensional structural racism, structural sexism, and classism. By simply “adding up” various forms of oppression that racialized people may experience simultaneously, Homan et al.44 demonstrated the additive negative impact of forms of oppression on self-reported health status.
Policy databases
We identified 3 studies that cataloged policies into databases. Two, that of Samari et al.85 and Sudhinaraset et al.,86 focused primarily on immigration-related policies. Sudhinaraset et al.86 surveyed state-level immigration policies that either include immigrants in social services (eg, health care and social service benefits, education, employment) or criminalize and surveil immigrants (eg, legal status inquiry, requiring a social security number to obtain a driver’s license). Samari et al.85 examined 14 policies across 5 domains (public health and welfare benefits, higher education, labor and employment, driver’s licenses and identification, and immigration enforcement) to categorize each as inclusionary, exclusionary, or neither to create an immigration policy index. Agénor et al.87 searched expansively beyond immigration policies across judicial, economic, and civic domains to include stand-your-ground, mandatory minimum sentencing, racial profiling, minimum wage, and voting rights. The effort required to identify these racist policies from various government and nongovernment sources was immense, spanning disciplines, specialties, and databases. Once constructed, these policy databases are invaluable and can be made publicly available for continued research on how racist policies influence health.
Non-x variable measures of structural racism
Three studies we identified did not derive structural racism measures to be included as explanatory variables in regression models. Instead, they used simulated, counterfactual approaches (ie, comparing the difference between the effect observed in data and that in simulated, counterfactual scenarios in which a particular characteristic is made absent) to characterize the effect of structural racism on health inequities. Lundberg76 estimated the effect of occupational segregation (ie, racially patterned access to work and occupations) on racial inequity in work-limited disability. Instead of deriving an exposure variable (ie, the x variable in regression equations), as in a large majority of the studies we identified, Lundberg76 simulated the counterfactual labor market in which Black workers and White workers can access work and occupations equitably and examined change in the prevalence of work-related disability compared with the observed data. Graetz and Esposito30 used a similar simulated counterfactual approach to examine the extent to which redlining grades influence life expectancy and disparity in predominantly Black neighborhoods and White neighborhoods. Samari et al.84 also used a simulated counterfactual approach to examine the effect of the 2017 ban on travel for people from Muslim-majority countries on infant health outcomes born to women from banned countries in the United States. This use of this counterfactual approach offers a useful alternative to estimate what could have happened had a racist event or policy not occurred.
Development of an antiracism or equity measure
We identified 1 measure that focused on the progress toward racial equity and antiracism. Created by the National Equity Atlas, the racial equity index measured the progress toward equity rather than characterizing the evidence of racial inequities in society. The method is published elsewhere.81 Briefly, the racial equity index is a composite of 9 measures grouped into 3 domains: (1) economic vitality (wages, unemployment, poverty), (2) readiness (educational attainment, disconnected youth, school poverty), and (3) connectedness (air pollution exposure, commute time, housing burden). The racial equity index can be calculated at the city, state, and region levels. Compared with structural racism measures, which focus on how far apart the experiences between White and racialized groups are in accessing resources, the racial equity index evaluates how close the experiences of all racial groups (including White people) are to the population average—what the creator of the racial equity index operationalized as the state of equity.
Limited focus beyond the early life stage
All identified studies examined the relationship between structural racism and health outcomes in early and mid-life; only 1 study investigated how structural racism drives inequities in older age and late life, and another 3 examined mortality and life expectancy.29,30,42 We found 16 studies31,33,36,40,43,46,48,49,51,52,54,62,63,72,84,86 that focused on maternal and infant health, 3 that focused on populations of children,59,65,71 and 5 that did not predict health.79‑81,85,87 All others focused on adult health.
Discussion
Our scoping review characterizes the current state of the literature on operationalizing and measuring structural racism. This review highlights several innovations that may revolutionize future antiracist research and notes the gaps in the research and what should be done moving forward. Advancements can be made in both the measurement of structural racism and the methods used to determine how structural racism affects health. On the basis of our review, we identified several common measurement approaches and opportunities for future research.
Our review makes 1 point clear: no 1 definition or measurement of structural racism exists; rather, there is a great deal of heterogeneity in how the concept is used and enacted.17 Dean and Thorpe17 argue that to actually move toward measurement of structural racism that captures the systemic nature of this phenomenon, these measures must be multidimensional. Furthermore, they argue that if a measure uses only 1 domain, it is a measure of institutional racism, not structural racism. We observed this tension between multidimensional and unidimensional measures, and between structural and institutional racism, in the studies we reviewed, and agree with Dean and Thorpe17 in their assessment that to measure all the ways structural racism manifests, a multidimensional measure is required.
This heterogeneity of definition and measurement17 plagued both peer-reviewed literature and gray literature. In fact, across all the themes we discuss here, there was no noticeable distinction in measurement between types of literature. Both types relied primarily on using ratios or comparisons that generate disparities as indicators of structural racism, and relied on unidimensional measures, were cross-sectional, and examined anti-Black structural racism.
The large majority of structural-racism-measurement literature we reviewed focused on anti-Black structural racism. Structural racism in the United States is often studied in relation to the history of slavery, subsequent Jim Crow laws, and overall disproportionate harm inflicted upon Black Americans. Given this history, it follows that most of the research examining structural racism would interrogate how that history has contributed to the enduring health inequities between Black people and White people. Foundational literature on structural racism and health inequities sheds light on the effects of racist policies and practices that physically separate the racialized communities from White people.1,4,13 From primarily measuring residential segregation or racial mixing (eg, index of dissimilarity, isolation index, interaction index), contemporary work also operationalizes and measures structural racism as differential access to socioeconomic resources (e.g., high-quality school, employment, home loan) that are driven by residential segregation. Our review identified only a few articles reporting on studies in which these approaches were adapted to measure structural racism and assess health inequities for Latinx people, Asian and Pacific Islanders, Muslims, Native Americans, and Alaska Native Americans. It is possible that some anti-Black structural racism measures could be universally applied to assess health inequities for other racialized populations. However, given the unique historical and contemporary forms of structural racism that plague each racialized group, new structural racism measures are needed to specifically capture the ways in which structural racism affects specific racialized populations. For example, given increasing evidence of xenophobia and anti-immigrant acts, especially against Asian groups during the COVID-19 pandemic, special attention must be given to measuring anti-Asian (or specific Asian subgroups [eg, anti-Chinese]) and anti-immigrant structural racism.
Segregation was the most common domain measured with the dissimilarity index, ICE, and others. As with other unidimensional measures, the full impact of structural racism on health cannot be understood without examination of how segregation interacts with other domains such as housing quality, education, and environment. Given the lack of studies that consider the dynamic nature of segregation and how these interactions may compound to influence health, we suggest that more multidimensional and longitudinal measures be used to understand the mechanisms through which segregation shapes health.
Geographic considerations are crucial for structural racism measurements. When conducting structural racism research, we must ask, What is the most meaningful scale for the exposure and outcome we are measuring? Structural racism is often operationalized and measured as exposure at various spatial levels. Most prominently, Nancy Krieger, in her ecosocial theory,88 and Arline Geronimus, in her weathering effect,89 theorize that individuals embody racism and various forms of oppression around them, and that oppression can get “under the skin” and have negative impacts on the health of historically oppressed groups. Thus, a critical decision when deriving structural racism measures is what spatial unit to ground the measure in. Whereas studies of interpersonal and internalized racism use the individual as the unit of measurement, structural racism measures are often estimated at the census tract, county, or state levels. In some of the studies, researchers argued that they used county-level measures because racist laws are made at the county level. For example, preclearance coverage under the Voting Rights Act to monitor discrimination at the polls was issued at the county level; thus, a logical study design could then examine counties covered and not covered by preclearance to examine the effect of this coverage on voting rates and health outcomes. Because of data availability, studies may be limited in the geographic level they can analyze. For example, the American Community Survey 1-year estimates may only be available publicly at the county level for areas with a population of more than 65 000.90 The use of each spatial unit depends on the research question, and there is no gold standard for a spatial unit that is best for all questions. One potential approach has been proposed by Chantarat et al.37 and Riley,91 who argue that a specific domain of structural racism should be measured at the spatial unit consistent with the mechanism that gives rise to it. For example, if studying how incarceration policies influence health, a state-level analysis would be most appropriate because carceral policies are often created at the state level. For employment inequity, in which the corrupted job-search process is the main mechanism driving structural racism in the labor market, this form of structural racism should be measured at the labor market spatial unit, like the community zone or metropolitan statistical area, which expands beyond the neighborhood in which one lives.92 Discussion on how to best select the spatial unit to ground structural racism measures in is warranted.
Since the publication of the report by Groos et al. in 2018,16 there has been growth in the diversity of domains of structural racism being measured. In addition to residential segregation, inequities in education, employment, homeownership, and home loan access, researchers also examine racial inequities in incarceration, political participation, reparations, and occupational mobility. Although most measures still rely on population estimates from sources like the Home Mortgage Disclosure Act, American Community Survey, and County Health Ranking database, newly released databases like those of the Vera Institute of Justice,93 Pew Research Center,94 Global Burden of Disease Collaboration Network,95 Eviction Lab,96 National Conference of State Legislatures,97 and the Stanford Open Policing Project98 are new resources that may be used for operationalizing and measuring structural racism. Researchers may capitalize on the rich information from these new, publicly available data sources to measure structural racism beyond residential segregation to capture a more complete picture of this multidimensional determinant of health.
Many measures of structural racism are contemporary, examining structural racism in the 21st century, and some reach back to the 1950s and 1960s to examine the impact of Civil Rights advances on health. Yet, few structural racism measures focus on the period after emancipation and through Jim Crow. Of the articles reviewed, 9 studies used historical data to predict contemporary health outcomes, with 8 of those using historic redlining data,30,39,43,48,51,77,82,83 and 1 using historic lynching data.29 Notably, the study on historic lynching used data from 1877 to 1950 and demonstrated how historic lynching rates are negatively associated with life expectancy in 2019–2020.29 However, more historical data are needed to understand how the long arm of historical oppression shapes population health today. For example, 1 study published in 2015 (and so not a part of our review) found that places with slavery in the 1860s continue to have lower rates of voting to this day.99 Furthermore, a key characteristic of structural racism is that it evolves: slave patrols became the modern-day police force, poll taxes and literacy tests became voter identification laws and poll closures. These historic and contemporary power disparities translate to health inequities.100 Understanding how structural racism manifests in various periods can provide further insight into how structural racism transforms, adapts along with societal changes, and influences the health of racialized communities over time. More research that uses historical data is needed to understand how historic structural racism drives contemporary structural racism and health inequities. We also need historical data to track this evolution, expansion, and contraction across domains. In seeing this story over centuries, we can identify which interventions were most successful and see how structural racism evolves when facing different barriers. This insight may inform future interventions and provide a better understanding of how to dismantle structural racism.
Because structural racism can transform over time, methods used to measure it should also evolve. Structural racism operates as a system; thus, a systems approach is required to assess its affect on health and well-being. Some scholars have suggested a systems-science approach, as is used in fields such as engineering, as a new method for racism research.101 Others have incorporated methods from other social science disciplines, such as simulated counterfactual approaches, latent class, and confirmatory factor models, to create a body of knowledge that is grounded in theory and driven by policy.76,92 Many measures consider ratios of socioeconomic, political, carceral, and other measures for Black and White county or state populations. Although ratios do highlight inequities in these outcomes by racialized groups, these measures are often used in isolation or used in the same regression model, but a cumulative or interactive effect of these measures on health is not examined. Our search identified 2 studies that aim to change this through the innovative use of a latent-construct approach to operationalize and measure structural racism as a multidimensional determinant of health.27,92 This approach represents a novel and critical leap toward accurately measuring structural racism and its many complexities.102,103 Yet, the external validity for both newly proposed measures and their effectiveness in capturing structural racism (ie, do they both capture the same things) have not been tested. In addition to multidimensional structural racism, future measures should consider how different forms of structural racism and other forms of structural oppression (eg, structural sexism, classism) work in tandem to affect health. This could look like the measure of structural intersectionality put forth by Homan et al.44 Although these innovative approaches are considered a leap and push the frontier of structural racism measurements, studying external validation (eg, using the measure with other data sets) and improving these multidimensional measures should also be prioritized. To operationalize these joint effects, databases that link racist policies and other forms of structural racism are necessary.
Last, we found no studies that used a life-course framework and examined how structural racism drives racial health inequities among older adults. Because much of the work concerning structural racism is done with populations younger than 50–55 years, many aging and long-term services and supports researchers are not consuming this literature and applying these relevant frameworks to their equity work, although some note the connection between racism and inequities in aging.104 Focusing on older populations is important to understand the connections between historical and contemporary experiences with structural racism and current health inequities. Our population is aging and requires increased use of long-term care; these services continue to be among the most segregated institutions today.105 Thus, using the life-course exposure to structural racism and aging (eg, the risk of Alzheimer’s disease,106,107 gerontological services use101,104) should be prioritized in future research.
Limitations
This scoping review has some limitations. First, although we consulted with the librarian to develop the literature search strategies—consistent with the Cochrane literature search guideline—it is likely that some literature on this topic was not included. This is particularly true for gray literature, which is not cataloged systematically like peer-review literature, and we had to rely on search engines like Google Scholar to identify them. Second, our search focused on literature conducted in the United States and written in English. Some literature from countries with colonial history (eg, Australia, New Zealand) was identified in our initial search. Past literature suggested that structural racism manifests differently by locale; regional differences within the United States (eg, lynching in the South, racial covenants in the North) and internationally (eg, structural racism in Brazil is grounded on colorism rather than racial differences) have been documented.108 We encourage researchers to expand their search to incorporate literature from non-US countries to develop comprehensive insight on how structural racism affects health. Finally, given the new funding opportunities in structural racism research and an increasing concern about health-equity tourism, publication bias is a concern in our review. Unlike in meta-analyses, where methods to examine the extent of publication bias are available,109 no such methods exist for scoping reviews. Thus, we caution readers that there may be other studies with null results that are not published, which is beyond the scope of our search.
A path forward
From our review, 1 thing is clear: measuring structural racism is difficult. As such, the utility of the measures we have discussed is generally for a very narrow audience of researchers. At the current stage, individuals interested in studying multiple domains of structural racism still need to separately extract data from multiple databases. These steps are cumbersome and time consuming, especially for individuals outside the academic setting—who actively engage with the community directly affected by structural racism to identify antiracist strategies—who may not have the skill set and resources to do so. A significant shift in the data infrastructure aimed at measuring structural racism should be prioritized but, understandably, will take time. In the interim, research institutions should support scholars and activists who have shown dedication and have experienced the consequences of structural racism in their lives and communities. These efforts may help protect against health-equity tourism.19 This support could take the form of providing free data management, consultation, and analytic services to such scholars. In the long run, creating a data repository linking all the aforementioned databases together will make the extraction of data needed to create structural racism measures easier for those interested in advancing this work.
Conclusion
Operationalizing and measuring structural racism are crucial steps toward understanding and dismantling the link between structural racism and health inequities. Our analysis of the state of the literature on structural racism measurement during 2019–2021 in the epidemiology and other health literature identified gaps and highlighted opportunities. This article can serve as a resource to guide researchers and shape an antiracist path forward.
Acknowledgments
The authors thank Raquel Motachwa and Ceron Ford for their assistance in the preliminary screening of the literature, Miamon Queeglay for project coordination and supervision of the graduate research assistants, and Keelia Silvis and Marian Candil Escobar for copyediting the original manuscript.
Supplementary material
Supplementary material is available at Epidemiologic Reviews online.
Funding
This work was supported by the Robert Wood Johnson Foundation Evidence for Action (ID: 79238).
Conflict of interest
The authors declare no conflicts of interest.
Disclaimer
The contents of this work are of the authors and do not necessarily represent the official views of the funder.
Data availability
All articles reviewed were available online or through University of Minnesota Libraries.
Supplementary Material
Contributor Information
Anna K Hing, Division of Health Policy and Management, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Center for Antiracism Research for Health Equity, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Minnesota Population Center, Institute for Social Research and Data Innovation, University of Minnesota, Minneapolis, MN, United States.
Tongtan Chantarat, Division of Health Policy and Management, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Minnesota Population Center, Institute for Social Research and Data Innovation, University of Minnesota, Minneapolis, MN, United States.
Shekinah Fashaw-Walters, Division of Health Policy and Management, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Center for Antiracism Research for Health Equity, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Minnesota Population Center, Institute for Social Research and Data Innovation, University of Minnesota, Minneapolis, MN, United States.
Shanda L Hunt, University Libraries, University of Minnesota, Minneapolis, MN, United States.
Rachel R Hardeman, Division of Health Policy and Management, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Center for Antiracism Research for Health Equity, School of Public Health, University of Minnesota, Minneapolis, MN, United States; Minnesota Population Center, Institute for Social Research and Data Innovation, University of Minnesota, Minneapolis, MN, United States.
References
- 1. Gee GC, Hicken MT. Structural racism: the rules and relations of inequity. Ethn Dis. 2021;31:293‑300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hardeman RR, Hardeman-Jones SL, Medina EM. Fighting for America’s paradise: the struggle against structural racism. J Health Polit Policy Law. 2021;46(4):563‑575. [DOI] [PubMed] [Google Scholar]
- 3. Gee GC, Ford CL. Structural racism and health inequities. Bois Rev Soc Sci Res Race. 2011;8:115‑132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention . Racism and Health. Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/minorityhealth/racism-disparities/ [Google Scholar]
- 5. Bonilla-Silva E. Rethinking racism: toward a structural interpretation. Am Sociol Rev. 1997;62:465‑480. [Google Scholar]
- 6. Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105‑125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization . Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health. Accessed March 2, 2022.
- 8. Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015;41:311‑330. Accessed March 2, 2022. [Google Scholar]
- 9. Robert Wood Johnson Foundation . Understanding the Social Determinants of Health. Robert Wood Johnson Foundation. n.d.. https://www.rwjf.org/en/our-focus-areas/topics/social-determinants-of-health.html. Accessed March 2, 2022. [Google Scholar]
- 10. Ndugga N, Hill L, Artiga S. COVID-19 cases and deaths by race/ethnicity: current data and changes over time. KFF. November 17, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/
- 11. Bailey ZD, Krieger N, Agénor M, et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453‑1463. [DOI] [PubMed] [Google Scholar]
- 12. Anku K, Barrows A, Bernhard K, et al. We need a new social contract to undo a system of White supremacy. The Aspen Institute. July 9, 2020. https://www.aspeninstitute.org/blog-posts/undo-a-system-of-white-supremacy/ [Google Scholar]
- 13. Reskin B. The race discrimination system. Annu Rev Sociol. 2012;38:17‑35. [Google Scholar]
- 14. Hardeman RR, Homan PA, Chantarat T, et al. Improving the measurement of structural racism to achieve antiracist health policy. Health Aff (Millwood). 2022;41:179‑186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90:1212‑1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Groos M, Wallace M, Hardeman R, et al. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Dispar Res Pract. 2018;11(2):Article 13. [Google Scholar]
- 17. Dean LT, Thorpe RJ. What structural racism is (or is not) and how to measure it: clarity for public health and medical researchers. Am J Epidemiol. 2022;191:1521‑1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hardeman RR, Medina EM, Boyd RW. Stolen breaths. N Engl J Med. 2020;383(3):197‑199. [DOI] [PubMed] [Google Scholar]
- 19. Lett E, Adekunle D, McMurray P, et al. Health equity tourism: ravaging the justice landscape. J Med Syst. 2022;46:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hardeman RR, Murphy KA, Karbeah J, et al. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep. 2018;133(3):240‑249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Taylor J, Pagliari C. Comprehensive scoping review of health research using social media data. BMJ Open. 2018;8:e022931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alberani V, De Castro PP, Mazza AM. The use of grey literature in health sciences: a preliminary survey. Bull Med Libr Assoc. 1990;78:358‑363. [PMC free article] [PubMed] [Google Scholar]
- 23. Siegel M, Critchfield-Jain I, Boykin M, et al. Racial/ethnic disparities in state-level COVID-19 vaccination rates and their association with structural racism. J Racial Ethn Health Disparities. 2021;9:2361‑2374. 10.1007/s40615-021-01173-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Siegel M, Critchfield-Jain I, Boykin M, et al. Actual racial/ethnic disparities in COVID-19 mortality for the non-Hispanic Black compared to non-Hispanic White population in 35 US states and their association with structural racism. J Racial Ethn Health Disparities. 2021;9:886‑898. 10.1007/s40615-021-01028-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tan SB, deSouza P, Raifman M. Structural racism and COVID-19 in the USA: a county-level empirical analysis. J Racial Ethn Health Disparities. 2022;9:236‑246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. White A, Hao L, Yu X, et al. Residential racial segregation and social distancing in the United States during COVID-19. EClinicalMedicine. 2021;35:100840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dougherty GB, Golden SH, Gross AL, et al. Measuring structural racism and its association with BMI. Am J Prev Med. 2020;59:530‑537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bell CN, Kerr J, Young JL. Associations between obesity, obesogenic environments, and structural racism vary by county-level racial composition. Int J Environ Res Public Health. 2019;16:861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kihlström L, Kirby RS. We carry history within us: anti-Black racism and the legacy of lynchings on life expectancy in the U.S. South Health Place. 2021;70:102618. [DOI] [PubMed] [Google Scholar]
- 30. Graetz N, Esposito M. Historical redlining and contemporary racial disparities in neighborhood life expectancy. Social Forces. 2023;102(1):1‑22. 10.1093/sf/soac114 [DOI] [Google Scholar]
- 31. Allgood KL. Equal Protection Under the Law: The Measurement of Structural Racism and Health Disparities. Dissertation: University of Michigan; 2021. [Google Scholar]
- 32. Bell CN, Owens-Young JL. Self-rated health and structural racism indicated by county-level racial inequalities in socioeconomic status: the role of urban-rural classification. J Urban Health. 2020;97:52‑61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bishop-Royse J, Lange-Maia B, Murray L, et al. Structural racism, socio-economic marginalization, and infant mortality. Public Health. 2021;190:55‑61. [DOI] [PubMed] [Google Scholar]
- 34. Blanco BA, Poulson M, Kenzik KM, et al. The impact of residential segregation on pancreatic cancer diagnosis, treatment, and mortality. Ann Surg Oncol. 2021;28:3147‑3155. [DOI] [PubMed] [Google Scholar]
- 35. Brown J. Structural Factors and Racial Disparities in Severe Maternal Morbidity: An Examination of State-Level Indicators of Structural Racism and Severe Maternal Morbidity Among Black and White Persons in the U.S., 2009–2011. Thesis. University of Washington; 2020. [Google Scholar]
- 36. Chambers BD, Baer RJ, McLemore MR, et al. Using index of concentration at the extremes as indicators of structural racism to evaluate the association with preterm birth and infant mortality—California, 2011–2012. J Urban Health. 2019;96:159‑170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chantarat T, Van Riper DC, Hardeman RR. The intricacy of structural racism measurement: a pilot development of a latent-class multidimensional measure. eClinicalMedicine. 2021;40:101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Collin LJ, Gaglioti AH, Beyer KM, et al. Neighborhood-level redlining and lending bias are associated with breast cancer mortality in a large and diverse metropolitan area. Cancer Epidemiol Biomark Prev. 2021;30:53‑60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Diaz A, O’Reggio R, Norman M, et al. Association of historic housing policy, modern day neighborhood deprivation and outcomes after inpatient hospitalization. Ann Surg. 2021;274:985‑991. [DOI] [PubMed] [Google Scholar]
- 40. Dyer L, Chambers BD, Crear-Perry J, et al. The index of concentration at the extremes (ICE) and pregnancy-associated mortality in Louisiana, 2016–2017. Matern Child Health J. 2021;26:814‑822. 10.1007/s10995-021-03189-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. English D, Carter JA, Boone CA, et al. Intersecting structural oppression and Black sexual minority men’s health. Am J Prev Med. 2021;60:781‑791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Islami F, Fedewa SA, Thomson B, et al. Association between disparities in intergenerational economic mobility and cause-specific mortality among Black and White persons in the United States. Cancer Epidemiol. 2021;74:101998. [DOI] [PubMed] [Google Scholar]
- 43. Hollenbach SJ, Thornburg LL, Glantz JC, et al. Associations between historically redlined districts and racial disparities in current obstetric outcomes. JAMA Netw Open. 2021;4:e2126707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Homan P, Brown TH, King B. Structural intersectionality as a new direction for health disparities research. J Health Soc Behav. 2021;62:350‑370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Houghton A, Jackson-Weaver O, Toraih E, et al. Firearm homicide mortality is influenced by structural racism in US metropolitan areas. J Trauma Acute Care Surg. 2021;91:64‑71. [DOI] [PubMed] [Google Scholar]
- 46. Janevic T, Zeitlin J, Egorova NN, et al. Racial and economic neighborhood segregation, site of delivery, and morbidity and mortality in neonates born very preterm. J Pediatr. 2021;235:116‑123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Knopov A, Rothman EF, Cronin SW, et al. The role of racial residential segregation in Black-White disparities in firearm homicide at the state level in the United States, 1991–2015. J Natl Med Assoc. 2019;111:62‑75. [DOI] [PubMed] [Google Scholar]
- 48. Krieger N, van Wye G, Huynh M, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. Am J Public Health. 2020;110:1046‑1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Larimore SH. Routes to Low Birth Weight (Or Not): Local, Cultural Racism in Exceptional Communities. Dissertation. University of Washington; 2019. [Google Scholar]
- 50. Liu SY, Fiorentini C, Bailey Z, et al. Structural racism and severe maternal morbidity in New York state. Clin Med Insights Womens Health. 2019;12:1179562X1985477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lynch EE, Malcoe LH, Laurent SE, et al. The legacy of structural racism: associations between historic redlining, current mortgage lending, and health. SSM Popul Health. 2021;14:100793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Matoba N, Suprenant S, Rankin K, et al. Mortgage discrimination and preterm birth among African American women: an exploratory study. Health Place. 2019;59:102193. [DOI] [PubMed] [Google Scholar]
- 53. O’Brien R, Neman T, Seltzer N, et al. Structural racism, economic opportunity and racial health disparities: evidence from U.S. counties. SSM Popul Health. 2020;11:100564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pabayo R, Ehntholt A, Davis K, et al. Structural racism and odds for infant mortality among infants born in the United States 2010. J Racial Ethn Health Disparities. 2019;6:1095‑1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Poulson MR, Beaulieu-Jones BR, Kenzik KM, et al. Residential racial segregation and disparities in breast cancer presentation, treatment, and survival. Ann Surg. 2021;273:3‑9. [DOI] [PubMed] [Google Scholar]
- 56. Poulson MR, Blanco BA, Geary AD, et al. The role of racial segregation in treatment and outcomes among patients with hepatocellular carcinoma. HPB (Oxford). 2021;23:854‑860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Poulson MR, Helrich SA, Kenzik KM, et al. The impact of racial residential segregation on prostate cancer diagnosis and treatment. BJU Int. 2021;127:636‑644. [DOI] [PubMed] [Google Scholar]
- 58. Poulson M, Cornell E, Madiedo A, et al. The impact of racial residential segregation on colorectal cancer outcomes and treatment. Ann Surg. 2021;273:1023‑1030. [DOI] [PubMed] [Google Scholar]
- 59. Sewell AA. Political economies of acute childhood illnesses: measuring structural racism as mesolevel mortgage market risks. Ethn Dis. 2021;31:319‑332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Siegel M, Sherman R, Li C, et al. The relationship between racial residential segregation and Black-White disparities in fatal police shootings at the city level, 2013–2017. J Natl Med Assoc. 2019;111:580‑587. [DOI] [PubMed] [Google Scholar]
- 61. Tan SB, deSouza P, Raifman M. Structural racism and COVID-19 in the USA: a county-level empirical analysis. J Racial Ethn Health Disparities. 2021;9:236‑246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Vilda D, Hardeman R, Dyer L, et al. Structural racism, racial inequities and urban–rural differences in infant mortality in the US. J Epidemiol Community Health. 2021;75:788‑793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Owens-Young J, Bell CN. Structural racial inequities in socioeconomic status, urban-rural classification, and infant mortality in US counties. Ethn Dis. 2020;30:389‑398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Volpe VV, Schorpp KM, Cacace SC, et al. State- and provider-level racism and health Care in the U.S. Am J Prev Med. 2021(61):338‑347. [DOI] [PubMed] [Google Scholar]
- 65. Butler B, Outrich M, Roach J, et al. Generational impacts of 1930s housing discrimination and the imperative need for the healthy start initiative to address structural racism. J Health Disparities Res Pract. 2020;13. [Google Scholar]
- 66. Chambers BD, Arabia SE, Arega HA, et al. Exposures to structural racism and racial discrimination among pregnant and early post-partum Black women living in Oakland. California. Stress Health. 2020;36:213‑219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Dyer L, Hardeman R, Vilda D, et al. Mass incarceration and public health: the association between Black jail incarceration and adverse birth outcomes among Black women in Louisiana. BMC Pregnancy Childbirth. 2019;19:525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ibragimov U, Beane S, Friedman SR, et al. Police killings of Black people and rates of sexually transmitted infections: a cross-sectional analysis of 75 large US metropolitan areas, 2016. Sex Transm Infect. 2020;96:429‑431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Martz CD, Hunter EA, Kramer MR, et al. Pathways linking census tract typologies with subjective neighborhood disorder and depressive symptoms in the Black Women’s Experiences Living with Lupus (BeWELL) study. Health Place. 2021;70:102587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Richardson ET, Malik MM, Darity WA Jr, et al. Reparations for Black American descendants of persons enslaved in the U.S. and their estimated impact on SARS-CoV-2 transmission. Soc Sci Med. 2021;276:113741. 10.1016/j.socscimed.2021.113741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Tackett KJ, Jenkins F, Morrell DS, et al. Structural racism and its influence on the severity of atopic dermatitis in African American children. Pediatr Dermatol. 2020;37:142‑146. [DOI] [PubMed] [Google Scholar]
- 72. Blebu BE, Ro A, Kane JB, et al. An examination of preterm birth and residential social context among black immigrant women in California, 2007–2010. J Community Health. 2019;44:857‑865. [DOI] [PubMed] [Google Scholar]
- 73. Fernandez-Esquer ME, Ibekwe LN, Guerrero-Luera R, et al. Structural racism and immigrant health: exploring the association between wage theft, mental health, and injury among Latino day laborers. Ethn Dis. 2021;31:345‑356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Leos C. Examining the Effect of State- and Individual-Level Structural Racism on Latino Adolescent Sexual Risk Behaviors: An Intergroup and Intragroup Analysis. Dissertation. University of North Carolina, Chapel Hill; 2019. [Google Scholar]
- 75. Linton SL, Cooper HLF, Chen YT, et al. Mortgage discrimination and racial/ethnic concentration are associated with same-race/ethnicity partnering among people who inject drugs in 19 US cities. J Urban Health. 2020;97:88‑104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lundberg I. 202. Quantifying the contribution of occupational segregation to racial disparities in health: a gap-closing perspective. SocArXiv. 10.31235/osf.io/x9evk. Preprint: not peer reviewed. [DOI] [Google Scholar]
- 77. Mujahid MS, Gao X, Tabb LP, et al. Historical redlining and cardiovascular health: the Multi-Ethnic Study of Atherosclerosis. Proc Natl Acad Sci U S A. 2021;118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Pohl DJ, Seblova D, Avila JF, et al. Relationship between residential segregation, later-life cognition, and incident dementia across race/ethnicity. Int J Environ Res Public Health. 2021;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Shim RS. Dismantling structural racism in psychiatry: a path to mental health equity. Am J Psychiatry. 2021;178:592‑598. [DOI] [PubMed] [Google Scholar]
- 80. Stermon M, Lukinbeal C. Institutionalized racism: redlined districts then and now in Boston, Detroit, and Los Angeles. Yearb Assoc Pac Coast Geogr. 2021;83:81‑97. [Google Scholar]
- 81. Treuhaft S, Langston A, Scoggins J, Lee J, Pastor M. The Racial Equity Index: a new data tool to drive local efforts to dismantle structural racism. National Equity Atlas 2020. https://nationalequityatlas.org/research/index-findings
- 82. Poulson M, Neufeld MY, Dechert T, et al. Historic redlining, structural racism, and firearm violence: a structural equation modeling approach. Lancet Reg Health Am. 2021;3:100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Mitchell J, Chihaya GK. Tract level associations between historical residential redlining and contemporary fatal encounters with police. Soc Sci Med. 2022;302:114989. [DOI] [PubMed] [Google Scholar]
- 84. Samari G, Catalano R, Alcalá HE, et al. The Muslim ban and preterm birth: analysis of U.S. vital statistics data from 2009 to 2018. Soc Sci Med. 2020;265:113544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Samari G, Nagle A, Coleman-Minahan K. Measuring structural xenophobia: US state immigration policy climates over ten years. SSM Popul Health. 2021;16:100938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Sudhinaraset M, Woofter R, Young MEDT, et al. Analysis of state-level immigrant policies and preterm births by race/ethnicity among women born in the US and women born outside the US. JAMA Netw Open. 2021;4:e214482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Agénor M, Perkins C, Stamoulis C, et al. Developing a database of structural racism–related state laws for health equity research and practice in the United States. Public Health Rep. 1974;2021(136):428‑440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102:936‑944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2:207‑221. [PubMed] [Google Scholar]
- 90. US Census Bureau . Data suppression. https://www.census.gov/programs-surveys/acs/technical-documentation/data-suppression.html. Accessed March 2, 2022.
- 91. Riley AR. Neighborhood disadvantage, residential segregation, and beyond—lessons for studying structural racism and health. J Racial Ethn Health Disparities. 2018;5:357‑365. [DOI] [PubMed] [Google Scholar]
- 92. Chantarat T, Mentzer KM, Van Riper DC, et al. Where are the labor markets?: examining the association between structural racism in labor markets and infant birth weight. Health Place. 2022;74:102742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Kang-Brown J. Incarceration Trends. Vera Institute of Justice. 2022. https://www.vera.org/projects/incarceration-trends. Accessed April 3, 2022. [Google Scholar]
- 94. Bertoni N, Keeter S. How to access Pew Research Center survey data. Pew Research Center. 2021. https://www.pewresearch.org/fact-tank/2021/10/22/how-to-access-pew-research-center-survey-data/. Accessed April 3, 2022. [Google Scholar]
- 95. Global Burden of Disease Collaborative Network . Global Burden of Disease Collaborative Network 2022. https://ghdx.healthdata.org/organizations/global-burden-disease-collaborative-network. Accessed April 3, 2022.
- 96. Eviction Lab . Eviction Map and Data. Eviction Lab. https://evictionlab.org/map/. Accessed April 3, 2022. [Google Scholar]
- 97. National Conference of State Legislatures . Resources and tools for legislators and staff. https://www.ncsl.org/. Accessed April 3, 2022.
- 98. The Stanford Open Policing Project . The Open Policing Project. https://openpolicing.stanford.edu/. Accessed April 3, 2022.
- 99. Acharya A, Blackwell M, Sen M. A culture of disenfranchisement: how American slavery continues to affect voting behavior. https://scholar.harvard.edu/files/msen/files/slavery-voting.pdf. Accessed April 3, 2022.
- 100. Hing A. The right to vote, the right to health: voter suppression as a determinant of racial health disparities. J Health Dispar Res Pract. 2019;12(6):article 5. https://digitalscholarship.unlv.edu/jhdrp/vol12/iss6/5 [Google Scholar]
- 101. LaFave SE, Bandeen-Roche K, Gee G, et al. Quantifying older black Americans’ exposure to structural racial discrimination: how can we measure the water in which we swim? J Urban Health. 2022;99(5):794‑802. 10.1007/s11524-022-00626-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Szanton SL, SE LF, Thorpe RJ Jr. Structural racial discrimination and structural resilience: measurement precedes change. J Gerontol Ser A. 2022;77:402‑404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Brown TH, Homan PA. Frontiers in measuring structural racism and its health effects. Health Serv Res. 2022;57(3):443‑447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Shippee TP, Fabius CD, Fashaw-Walters S, et al. Evidence for action: addressing systemic racism across long-term services and supports. J Am Med Dir Assoc. 2022;23:214‑219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Fashaw-Walters SA, Rahman M, Gee G, et al. Out of reach: inequities in the use of high-quality home health agencies. Health Aff. (Millwood). 2022;41:247‑255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Jang E. Contextual understanding of literacy skills of language-minoritized bilinguals: a cross-country comparative study. Diss Abstr Int Sect Humanit Soc Sci. 2021;82: No-Specified. [Google Scholar]
- 107. Zeki Al Hazzouri A, Jawadekar N, Kezios K, et al. Racial residential segregation in young adulthood and brain integrity in middle age: can we learn from small samples? Am J Epidemiol. 2022;191:591‑598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Telles EE. Race in Another America: The Significance of Skin Color in Brazil. Princeton University Press; 2004. 10.2307/j.ctt6wpzpb [DOI] [Google Scholar]
- 109. Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- 110. Shim RS, Tully LM, Yu G, et al. Race and ethnicity of editorial board members and editors as an indicator of structural racism in psychiatry and neuroscience journals. JAMA Psychiatry. 2021;78:1161‑1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Reardon SF, Townsend JB. SEG: Stata module to compute multiple-group diversity and segregation indices. Revised April 18, 2018. https://EconPapers.repec.org/RePEc:boc:bocode:s375001
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All articles reviewed were available online or through University of Minnesota Libraries.