Abstract
Spondyloarthritis (SA) is a chronic inflammatory disease that predominantly affects the spinal column. SA-related pain can be intense, persistent, and disabling. Studies with cannabis have been conducted involving patients with refractory epilepsy, multiple sclerosis, Parkinson’s disease, sleep disorders, and chronic pain. Cannabidiol is the major non-psychotropic component of cannabis, has anti-inflammatory and analgesic properties, and exerts anxiolytic and mood-stabilizing effects. This paper reports a case of a 72-year-old male with SA, with mild stenoses of the spinal canal at C4-C5 and C5-C6 and stenoses of the left neural foramina at C3-C4, C4-C5, C5-C6, and C6-C7. The use of cannabidiol in our patient achieved satisfactory results in the control of pain related to cervical spondyloarthritis.
Keywords: spondyloarthritis, pain management, chronic pain, cannabis medicine, prescribed cannabis
Introduction
Spondyloarthritis (SA) is a chronic inflammatory disease that predominantly affects the spinal column. SA generally begins in young adulthood and is associated with accentuated physical impairment and a significant reduction in quality of life [1]. SA-related pain can be intense, persistent, and disabling [2].
The treatment of patients with chronic pain can be a therapeutic challenge for physicians, as it consists of the use of analgesics and physiotherapy, with variable responses and short-lasting results [3]. Cannabinoids are relevant in this context, as these substances affect all pain pathways responsible for the transmission, modulation, or perception of pain [4,5]. Cannabidiol (CBD) is a cannabinoid that has significant analgesic, anti-inflammatory, anticonvulsant, and anxiolytic properties that can be useful in the treatment of patients with chronic pain and is considered relatively safe, with few side effects [6-8].
This paper describes a case of the use of cannabidiol as a therapeutic option for pain related to cervical spondyloarthritis and improvement in quality of life.
Case presentation
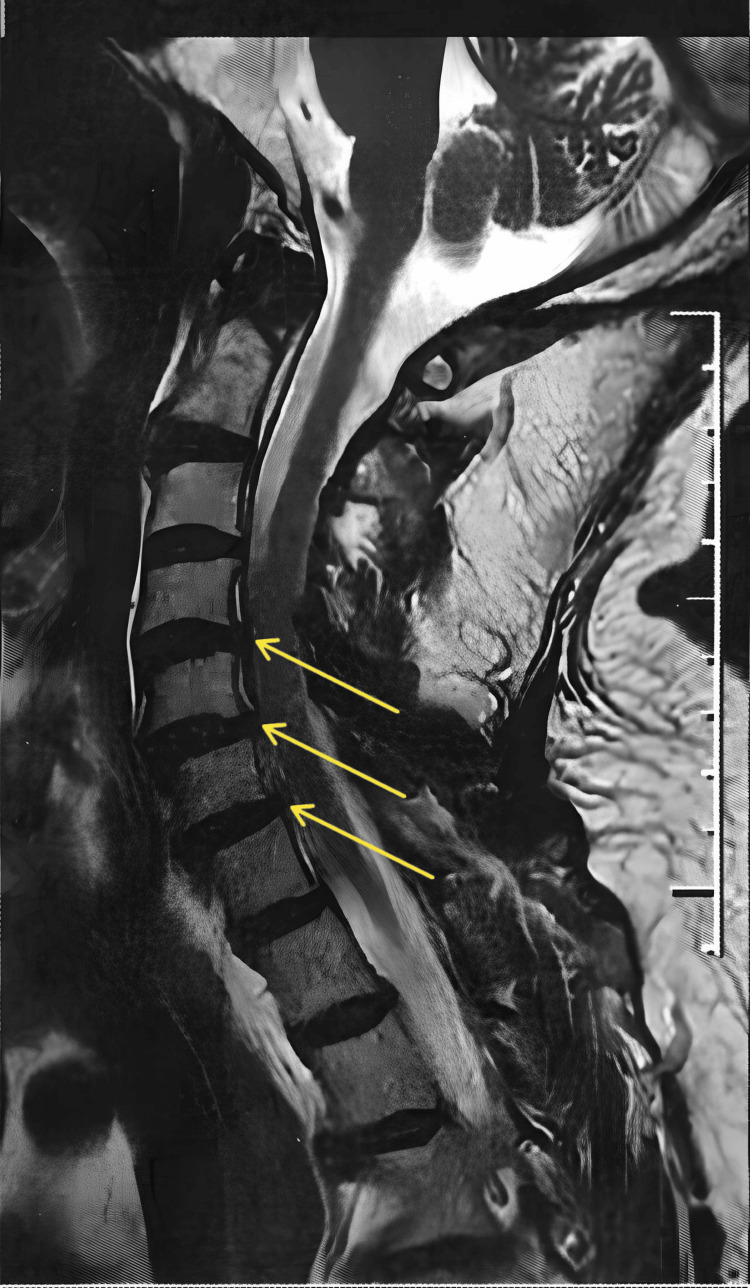
A 72-year-old, white, male, diabetic, hypertensive, and retired physician with spondyloarthritis and mild stenoses of the spinal canal at C4-C5 and C5-C6 and stenoses of the left neural foramina at C3-C4, C4-C5, C5-C6, and C6-C7 (Figure 1) presented with constant neuropathic pain in the cervical spine and left shoulder and arm for more than one year, numbness on the left side of the face, diminished muscle strength, and pain intensity of 8 on the visual analog scale (VAS) of 1 to 10.
Figure 1. Magnetic resonance imaging of the cervical spine showing spondyloarthrosis, highlighting mild stenosis of the spinal canal at C4-C5 and C5-C6 and stenoses of the left neural foramina at C3-C4, C4-C5, C5-C6, and C6-C7.
Electroneuromyography for an analysis of upper limb pain showed a chronic neurogenic pattern in muscles corresponding to the myotomes on the right at C7 and the left at C7/T1, without acute denervation, compatible with cervical radiculopathy on the right at C7 and the left at C7/TI, moderate on the right and severe on the left. The patient made continual use of olmesartan 40 mg + amlodipine besylate 5 mg, dapaglifosin 10 mg, analgesics (tramadol, dipyrone, ibuprofen), and physiotherapy sessions (a duration of 3 weeks without clinical improvement). Physical activity (karate, walking, and swimming) was interrupted and labor was not possible due to pain, leading to retirement.
Treatment involved full-spectrum medicinal cannabis oil 6000 mg (200 mg of CBD/mL and 0.3% tetrahydrocannabinol). The dose began at 8 mg every 12 h, with an increase every four days to 100 mg every 12 h. Signs of improvement emerged after 20 days of use (approximate dose of 50 mg every 12 h). After 90 days of treatment, the patient reported the absence of pain, the return of physical activity (walking and swimming), and the suspension of the use of analgesics. Muscle strength increased considerably and tremors in the left arm had diminished by 90%. The transient side effect was sleepiness only at the onset of treatment. The patient has been taking cannabidiol for one year, with adjustments to lower the dose (currently 144 mg a day).
Discussion
Chronic pain exerts an enormous personal and economic impact, affecting more than 30% of individuals throughout the world [9]. According to the Centers for Disease Control and Prevention (CDC), approximately 20.4% of adults in the United States had chronic pain in 2019 [10].
Various studies have been conducted on the use of cannabis as a therapeutic option in cases of chronic pain. Current standard treatment involves opioids, which have side effects such as severe constipation, nausea, sleepiness, respiratory depression, and opiate dependence [11]. In this case, the patient took an opioid continually but suspended the use of all analgesics, including the opioid, after 90 days of treatment with CBD due to the absence of pain. The only side effect reported by the patient was mild sleepiness at the onset of treatment.
Treatment with CBD should be based on the control of pain and consequent improvement in quality of life. In the present case, the pain was relieved, the opioid was suspended, and the patient returned to the practice of physical activity, all of which contributed to an improvement in quality of life. This clinical outcome indicates that the therapeutic conduct was adequate, which is in agreement with the findings described in the literature. In a longitudinal prospective study involving 751 patients with chronic pain, Safakish et al. investigated the effects of medicinal cannabis and found significant improvements in both pain and health-related quality of life [12].
Randomized, placebo-controlled, double-blind, clinical trials are needed to prove the effectiveness of CBD in patients with spondyloarthritis-related pain, including different lines of CBD-enriched Cannabis extracts, different doses, and different lengths of treatment to investigate the effectiveness, safety, and tolerance.
Conclusions
The use of cannabidiol in our patient achieved satisfactory control of pain related to cervical spondyloarthritis. Based on this result and considering scientific evidence of the effectiveness of CBD in the treatment of patients with chronic pain due to different illnesses, this therapeutic option may be beneficial to such patients when conventional medicinal treatment is unsatisfactory. However, clinical trials are needed to confirm the effectiveness of CBD in patients with spondyloarthritis-related pain.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Valdecir C. Tadei
Acquisition, analysis, or interpretation of data: Valdecir C. Tadei
Drafting of the manuscript: Valdecir C. Tadei
Critical review of the manuscript for important intellectual content: Valdecir C. Tadei
Supervision: Valdecir C. Tadei
References
- 1.Van der Heijde D, Landewé R. Ankylosing Spondylitis and the Spondyloarthropathies. Vol. 12. Philadelphia, Pennsylvania: Mosby Elsevier; 2006. Assessment of disease activity, function and quality of life; pp. 206–213. [Google Scholar]
- 2.Chronic widespread pain in the spectrum of rheumatological diseases. Atzeni F, Cazzola M, Benucci M, Di Franco M, Salaffi F, Sarzi-Puttini P. Best Pract Res Clin Rheumatol. 2011;25:165–171. doi: 10.1016/j.berh.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 3.The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Raja SN, Carr DB, Cohen M, et al. Pain. 2020;161:1976–1982. doi: 10.1097/j.pain.0000000000001939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Endocannabinoids: a unique opportunity to develop multitarget analgesics. Maione S, Costa B, Di Marzo V. Pain. 2013;154 Suppl 1:0–93. doi: 10.1016/j.pain.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 5.Practical considerations in medical cannabis administration and dosing. MacCallum CA, Russo EB. Eur J Intern Med. 2018;49:12–19. doi: 10.1016/j.ejim.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Effectiveness of cannabidiol to manage chronic pain: a systematic review. Mohammed SY, Leis K, Mercado RE, Castillo MM, Miranda KJ, Carandang RR. Pain Manag Nurs. 2024;25:0–86. doi: 10.1016/j.pmn.2023.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Efficacy, safety, and regulation of cannabidiol on chronic pain: a systematic review. Villanueva MR, Joshaghani N, Villa N, et al. Cureus. 2022;14:0. doi: 10.7759/cureus.26913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cannabis versus neuromodulators in chronic pain. Cecilio SAJ, de Oliveira Júnior JO. BrJP. 2023;6:146–152. [Google Scholar]
- 9.Chronic pain: an update on burden, best practices, and new advances. Cohen SP, Vase L, Hooten WM. Lancet. 2021;397:2082–2097. doi: 10.1016/S0140-6736(21)00393-7. [DOI] [PubMed] [Google Scholar]
- 10.Chronic pain and high-impact chronic pain among U.S. Adults, 2019. Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. https://www.cdc.gov/nchs/data/databriefs/db390-H.pdf. Adults, 2019. NCHS Data Brief. 2020;1:33151145. [PubMed] [Google Scholar]
- 11.Medical cannabis for chronic nonmalignant pain management. Hameed M, Prasad S, Jain E, et al. Curr Pain Headache Rep. 2023;27:57–63. doi: 10.1007/s11916-023-01101-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medical cannabis for the management of pain and quality of life in chronic pain patients: a prospective observational study. Safakish R, Ko G, Salimpour V, Hendin B, Sohanpal I, Loheswaran G, Yoon SY. Pain Med. 2020;21:3073–3086. doi: 10.1093/pm/pnaa163. [DOI] [PubMed] [Google Scholar]