Abstract
Background
Poor diet quality contributes to morbidity and mortality and affects environmental sustainability. The EAT-Lancet reference diet offers a healthy and sustainable solution. This study aimed to estimate the association between diet cost and dietary quality, measured with an EAT-Lancet Index.
Methods
An EAT-Lancet index was adapted to assess adherence to this dietary pattern from 24-h recalls data from the 2012 and 2016 Mexican National Health and Nutrition Surveys (n = 14,242). Prices were obtained from the Consumer Price Index. We dichotomized cost at the median (into low- and high-cost) and compared the EAT-Lancet index scores. We also used multivariate linear regression models to explore the association between diet cost and diet quality.
Results
Individuals consuming a low-cost diet had a higher EAT-Lancet score than those consuming a high-cost diet (20.3 vs. 19.4 from a possible scale of 0 to 42; p < 0.001) due to a lower intake of beef and lamb, pork, poultry, dairy, and added sugars. We found that for each one-point increase in the EAT-Lancet score, there was an average decrease of MXN$0.4 in the diet cost (p < 0.001). This association was only significant among low- and middle-SES individuals.
Conclusions
Contrary to evidence from high-income countries, this study shows that in Mexico, adhering to the EAT-Lancet reference diet is associated with lower dietar costs, particularly in lower SES groups. These findings suggest the potential for broader implementation of healthier diets without increasing the financial burden.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12937-024-01002-7.
Keywords: EAT-Lancet diet, Dietary quality, Planetary healthy diet, Diet costs, Mexico
Background
Poor-quality diets are the leading cause of morbidity and mortality worldwide and contribute to undernutrition, overweight, obesity, and persistent micronutrient deficiencies [1]. Globally, 149 million children are stunted, 45 million children are wasted [2], 2.6 billion people are overweight or obese [3], and 372 million preschool children and 1.2 billion nonpregnant women of reproductive age have one or more micronutrient deficiencies [4]. Furthermore, food production profoundly impacts the planet’s health. Food systems account for a third of global greenhouse gas emissions [5], while agriculture is the greatest driver of global deforestation and is a major cause of soil degradation, water pollution, and loss of biodiversity [6, 7].
To address these challenges, the EAT-Lancet Commission proposed the EAT-Lancet reference diet, an evidence-based framework for a healthy and sustainable diet [8]. The EAT-Lancet reference diet is rich in fruits, vegetables, whole grains, legumes, nuts and seeds, and unsaturated oils and includes limited amounts of red meat, refined grains, and added sugars. Combined with improved and sustainable food production practices and food waste reduction, the Commission estimated that this diet would allow feeding 10 billion people within planetary boundaries by 2050 [8].
Affordability is one of the four key components of sustainable diets and food systems, alongside food promotion, advertising and information, and food quality [9]. However, 750 million people, or 10% of the world population, face severe food insecurity, and more than 3 billion people, or 38%, are unable to afford a healthy diet [10]. As expected, there are wide variations in affordability across and within countries. Across countries, healthy and sustainable diets are more affordable in high-income countries than in low-income countries. Hirvonen and colleagues estimated that the median cost of an EAT-Lancet reference diet in 2011 was of $2.84 international dollars, with the cost being higher in high-income countries ($2.66) than in low-income countries ($2.42) [11]. However, this diet was more affordable in high-income countries, representing 6.1% of daily household income, compared to low-income countries, where it represented 89.1% of daily household income.
Within countries, extensive research from high-income countries has shown that unhealthy foods have a lower cost than healthy foods [12, 13]. Similarly, low-quality diets, as measured by various diet quality indexes including the Mediterranean diet score, the Healthy Eating Index, and the DASH score, among others, cost less than high-quality diets [13–18]. Despite the higher incomes in these countries, which theoretically enable better affordability of healthy diets, significant dietary disparities persist, as individuals with higher incomes tend to consume higher quality diets compared to those with lower incomes. This disparity can largely be attributed to the cost of healthy foods, which poses a substantial barrier for low-income households, as price remains one of the main drivers influencing food purchases, especially in low-income households where budgetary constraints narrow the range of food choices [12].
In middle-income countries, such as Mexico, there is limited evidence about the relationship between diet quality and cost. Previous studies indicated that, on average, the intake of whole grains and legumes was higher, and the intake of discretionary processed foods was lower in individuals with low socioeconomic status (SES) compared to those with high SES [19]. Therefore, the relationship between diet quality and diet cost might differ between Mexico and high-income countries. Curi-Quinto et al. reported that diet quality estimated with the Healthy Eating Index 2015 was positively associated with cost in Mexican urban areas, but there was no association in rural areas [20]. Clark a et al. derived dietary patterns with principal component analysis among Mexican children and adolescents and found that there was no difference in cost between healthy, transition, and nonhealthy patterns [21]. However, no previous study in Mexico has evaluated the association between cost and adherence to a healthy and sustainable diet, such as the EAT-Lancet recommendations. Batis et al. modeled baskets following the EAT-Lancet reference diet and the current Mexican intake and found that the EAT-Lancet baskets were less expensive [22]. Modeling baskets is an option for monitoring the food environment, independent of people’s choices. Nonetheless, it is also of interest to study the intersection between these choices and diet costs because individuals who adhere to a healthy diet might choose more expensive foods or vice versa; alternatively, depending on the culinary traditions of each context, inexpensive foods could be either healthy or unhealthy. Moreover, the association between adherence to a healthy diet and cost could differ according to socioeconomic characteristics. In this regard, evaluating the association between the healthfulness of the diets consumed by individuals and their costs can provide important insights into food behavior and the costs of healthy diets. Thus, this study aimed to estimate the association between diet cost and dietary quality, measured with an EAT-Lancet Indexamong all individuals and by socioeconomic status.
Methods
Design and sample
The 2012 and 2016 Mexican National Health and Nutrition Surveys (ENSANUT 2012 and 2016, for its acronym in Spanish) are probabilistic population-based surveys with a multistage, stratified sampling design, representative at the national and regional levels and for rural and urban areas [23, 24]. Briefly, ENSANUT 2012 was conducted between October 2011 and May 2012, and information was collected from 50,528 households, for a household response rate of 87% [24]. ENSANUT 2016 was conducted between May and September 2016, and information was collected from 9,479 households, for a household response rate of 77.9% [23].
Detailed dietary information was obtained for random subsamples in both surveys using 24-h recalls (n = 10,885 for ENSANUT 2012 and n = 4,341 for ENSANUT 2016). For the present analysis, we excluded children younger than one year of age (n = 420), children older than one year of age who were being breastfed (n = 109), pregnant and lactating women (n = 245), and individuals with implausible intake (n = 183). Plausible intake was defined as energy intake between ± 3 standard deviations of the ratio of energy intake and energy requirement, estimated using the Institute of Medicine equations for body weight maintenance. A detailed description of the methods used to identify implausible intake is described elsewhere [25, 26]. Furthermore, we also excluded individuals who consumed less than 50 kcal (n = 3) or more than 6,000 kcal (n = 24) per day to account for slight variations in dietary collection and cleaning methods between the surveys. Only those with intakes greater than 6,000 kcal were recorded for 2012, and those with intakes less than 50 kcal were recorded for 2016. Thus, the study sample included 14,242 individuals, composed of preschool children (1–4 y), school-aged children (5–11 y), adolescent (12–19 y) and adult (≥ 20 y) men, and nonpregnant, nonlactating adolescent and adult women with complete socioeconomic information (n = 10,062 for ENSANUT 2012 and n = 4,180 for ENSANUT 2016).
Dietary assessment
The 24-h recall was collected by trained interviewers between Monday and Sunday using an automated 5-step multiple-pass method [27]. Participants ≥ 15 years old were asked to report all foods and beverages consumed the previous day. For children and adolescents younger than 15 years, the person responsible for food preparation in the household was asked to provide information regarding their intake, with children or adolescents complementing the interview by reporting food eaten away from home. Interviewers assisted participants to avoid omissions and were provided with a food scale, measuring cups and serving spoons to help with the estimation of portion sizes. Tortilla and other typical foods of specific regions were weighted to capture variability from different regions of the country. Intake could be reported as individual foods or beverages (e.g., chips or water) or mixed dishes/beverages (e.g., stew or coffee with sugar). Mixed dishes and beverages could be either disaggregated to their ingredients if the participant knew the amounts used in their preparation or recorded as a standard preparation if eaten away from home or if the amounts used were unknown. For the purposes of this analysis, standard preparations were disaggregated to their ingredient level. For instance, a beef stew was disaggregated to beef, potato, carrot, tomato, etc. Energy and nutrient content was estimated using the 2016 food composition table compiled by the National Institute of Public Health (Nutrient Database, Compilation of the Mexican National Institute of Public Health, unpublished material, 2016).
EAT-Lancet diet quality index
We used an EAT-Lancet index, developed by Stubbendorff et al., to assess adherence to the EAT-Lancet reference diet, with some minor adaptations [28]. A total of 14 components were included in the index construction, including components that should be consumed in adequate amounts or “emphasized intake” and components that should be consumed in moderation or “limited intake”. The emphasized components were 1) vegetables, 2) fruits, 3) whole grains, 4) legumes, 5) seafood, 6) nuts, and 7) unsaturated oils. The limited components were 1) beef and lamb, 2) pork, 3) poultry, 4) eggs, 5) dairy, 6) potatoes and 7) added sugar. Scores between 3 and 0 were assigned for each component, with 3 indicating compliance and 0 indicating noncompliance. Hence, the score ranged from 0 to 42 points. Whole grains were defined as grains with ≥ 10 g of total fiber per 100 g of carbohydrates and refined otherwise [29].
Stubbendorff's EAT-Lancet index considered intake in grams as recommended by the EAT-Lancet reference diet. For example, compliance for vegetables consisted of 300 g, which would result in 3 points. The amount of grams per food group from the EAT-Lancet reference diet was only estimated for an intake of 2,500 kcal/day, representing the diet of an average adult male. However, since we included all age and sex groups, we recalculated the amounts of grams from Stubbendorff's EAT-Lancet index to a percent of contribution to total daily energy intake to account for lower energy requirements of children and women. For instance, 300 g of vegetables would represent a 3.2% contribution.
Furthermore, the EAT-Lancet reference diet recommends an added sugars intake from 0 to 31 g (< 5% kcal). The EAT-Lancet index by Stubbendorff et al. assigns 3 points for less than 31 g of added sugars, 2 points from 31 to 62 g, 1 point from 62 to 124 g, and 0 points for more than 124 g. We considered these criteria to be too permissive, given that 1 point (62 to 124 g) would represent a contribution between 10 and 20%; therefore, we modified the cutoff points for added sugars as follows: < 5%, 3 points; 5 to 7.5%, 2 points; 7.5 to 10%, 1 point; and > 10%, 0 points (Supplemental Table 1).
Food and beverage prices
We retrieved monthly nominal prices of food and beverages from the National System of Statistical and Geographical Information (INEGI, for its acronym in Spanish), which are used as the imput to calculate the Consumer Price Index (CPI). The CPI measures average weighted price changes of a basket of goods and services that are commonly purchased by urban households [30]. INEGI collected prices from 46 cities distributed across the 32 Mexican states between 2011 and 2016. These cities have a population of > 20,000 inhabitants, including the ten most populated urban zones in the country, representing ~ 66% of the Mexican population. In each city, prices were obtained from a sample of 16,000 sales points (stores, markets, and other vendors), excluding food services. Food and beverage prices are collected byweekly and reported on a monthly basis throughout the year from the different points of sale, and monthly averages are reported on the INEGI website.
Given that INEGI provides data with greater detail about most food and beverage items (e.g., brand and package size) than does the ENSANUT food composition table, many INEGI items were linked to a single food code from ENSANUT. The exception was a few categories from ENSANUT, which were collected at the brand level; thus, these items were matched with a specific item from INEGI (e.g., ready-to-eat cereals). The INEGI data reported prices for unprocessed foods per kilogram of gross weight; thus, we adjusted for refusal to match the net intake in grams. Moreover, some items are reported in other units, such as pieces, a handful, and liters. For those items, we estimated the weight using ENSANUT’s portion and weights table and the density of liquids. To bring food and beverage nominal prices to their equivalent in real prices, we used rthe CPI provided by INEGI whose reference month is July 2018.
Matching of prices with ENSANUT items
We started with 2,133,141 unique prices from 2011 to 2016. For water, we only took prices from 20-L jugs, excluding prices from water bottles (n = 20,342), to consider water intake within households [31]. We also identified items which prices per year had a coefficient of variation above 80, and reviewed them individually. A total of 976 unique prices were excluded for possible errors. Thus, the remaining 2,111,823 unique prices were used to estimate average prices.
To account for seasonal and regional variability, we estimated average prices at four levels: 1) quarterly averages at the regional level according to the four regions used in ENSANUT (north, center, south, and Mexico City), 2) annual averages at the regional level, 3) national annual averages, and 4) national total average from 2011 to 2016. Any average that had fewer than five observations was excluded. Of all the foods and beverages reported in ENSANUT, 85.8% were matched with quarterly averages at the regional level, 3.5% were matched with annual averages at the regional level, 6.4% with national annual averages, and 3.7% with national total averages. The remaining 0.6% of the reported items in the ENSANUT lacked a direct match, so these items were instead matched to a group or subgroup average.
Statistical analysis
We estimated proportions and 95% confidence intervals (95% CIs) to describe the sample by sociodemographic characteristics, including age group, sex, SES, region, place of residence, and survey. The SES index was determined through principal component analysis, considering household characteristics and assets. Subsequently, households were classified into tertiles. Region was divided into North, Central, Mexico City, and South. Place of residence was categorized as rural if the location had fewer than 2,500 inhabitants and urban otherwise. To adjust the cost by total energy intake, we estimated the cost residuals centered at the mean by regressing the diet cost on energy intake and then calculated the residual of the regression, followed by adding the mean of the diet cost to the calculated residual, hereafter referred to as diet cost residuals. This way the cost comparison is not influenced by differences in total energy intake that can be observed between age, sex, or socioeconomic groups.
We dichotomized the diet cost residuals at the median to define a low-cost and a high-cost diet. Then, we used multivariate linear regression models to compare the EAT-Lancet index and its 14 components between individuals consuming a low-cost diet and those consuming a high-cost diet. Similarly, we compared the energy intake and cost per 100 kcal among consumers of the index components by diet cost categories. The previous models were adjusted by age group, self-reported sex, SES tertile, region, place of residence, survey, and total energy intake (except for the energy intake comparison). In the tables, we present the predicted means of the EAT-Lancet index, energy intake and cost per 100, which were estimated using the Stata’s margins command.
Finally, we assessed the association between diet cost residuals and the EAT-Lancet index using a pooled multivariate linear regression model. To further assess whether the relationship differed by SES, we repeated the same model but included an interaction term between the EAT-Lancet index and SES tertiles. All analyses were conducted in Stata version 14.1 (College Station, TX: StataCorp LLC) and were weighted to be nationally representative and to account for the complex survey design.
Results
Sociodemographic characteristics of the sample are presented in Table 1. The mean EAT-Lancet index score was 19.9, with a range from 0 to 35 on a possible scale from 0 to 42 (a higher score reflecting a higher adherence to the EAT-Lancet reference diet). The limited intake components had a higher score than the emphasized intake components. The EAT-Lancet index was higher among adults, low-SES individuals, those living in the southern region, and those living in rural areas compared to their respective counterparts. The mean cost of the diet was MXN $52.9 (equivalent to $2.95 USD). Diet cost was higher among adolescents and adults, men, high-SES individuals, and individuals from urban areas compared to their counterparts. Diet cost was also higher among individuals living in Mexico City and the North than among those living in the South. Differences in diet cost adjusted by energy (cost residuals) remained statistically significant for SES, region, and place of residence (Table 1).
Table 1.
EAT-Lancet index score and diet cost by sociodemographic characteristics
| Samplea | EAT-Lancet Index score | Emphasized intake score | Limited intake score | Energy intake (kcal) | Costb (MXN$) |
Cost residualsc (MXN$) |
|||
|---|---|---|---|---|---|---|---|---|---|
| n | % [95%CI] | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | ||
| All | 14,242 | 19.9 (19.7,20) | 5.7 (5.6,5.9) | 14.1 (14,14.2) | 1833 (1801,1865) | 52.9 (51.6,54.3) | 52.9 (52.0,53.9) | ||
| Age groupsd | |||||||||
| Preschool | 2,626 | 7.8 [7.3,8.4] | 18.1 (17.9,18.4) | 4.6 (4.4,4.8) | 13.6 (13.4,13.8) | 1245 (1200,1289) | 37.6 (36.0,39.2) | 53.2 (52.3,54.1) | |
| School-aged children | 3,837 | 15.4 [14.6,16.3] | 18.9 (18.6,19.1) | 5.2 (5,5.3) | 13.7 (13.5,13.9) | 1721 (1676,1766) | 48.7 (47.0,50.4) | 51.7 (50.7,52.7) | |
| Adolescents | 3,281 | 15.7 [14.8,16.6] | 19.2 (18.9,19.4) | 5.3 (5.2,5.5) | 13.9 (13.7,14.1) | 2019 (1970,2069) | 57.6 (55.8,59.5) | 52.7 (51.3,54.0) | |
| Adults | 4,498 | 61.1 [59.7,62.5] | 20.5 (20.2,20.8) | 6.1 (6,6.3) | 14.4 (14.2,14.5) | 1889 (1840,1938) | 54.8 (52.8,56.8) | 53.3 (52.0,54.6) | |
| Sex | |||||||||
| Men | 6,759 | 49.1 [47.2,50.9] | 19.8 (19.5,20.0) | 5.7 (5.5,5.8) | 14.1 (13.9,14.2) | 2024 (1975,2073) | 57.0 (54.8,59.1) | 51.9 (50.3,53.5) | |
| Women | 7,483 | 50.9 [49.1,52.8] | 19.9 (19.7,20.2) | 5.8 (5.6,5.9) | 14.1 (14,14.3) | 1649 (1608,1690) | 49.1 (47.5,50.7) | 54.0 (53.0,54.9) | |
| Socioeconomic status | |||||||||
| Low | 6,109 | 33.1 [31.1,35.2] | 20.8 (20.6,21.1) | 6 (5.8,6.1) | 14.9 (14.7,15) | 1799 (1750,1847) | 45.1 (43.7,46.5) | 46 (45.2,46.9) | |
| Middle | 4,761 | 32.2 [30.4,34.1] | 19.7 (19.5,20) | 5.7 (5.5,5.8) | 14 (13.9,14.2) | 1791 (1745,1838) | 51.3 (49.7,53) | 52.4 (51.3,53.6) | |
| High | 3,372 | 34.6 [32.1,37.2] | 19.1 (18.7,19.4) | 5.6 (5.4,5.9) | 13.4 (13.2,13.7) | 1905 (1838,1972) | 61.9 (59,64.8) | 60 (58.1,61.9) | |
| Geographical region | |||||||||
| North | 3,318 | 19.6 [17.6,21.8] | 18.5 (18.2,18.8) | 5.1 (4.9,5.3) | 13.4 (13.2,13.6) | 1823 (1748,1898) | 54.4 (51.7,57.2) | 54.7 (53.1,56.3) | |
| Central | 5,011 | 31.7 [29.5,34.1] | 20.1 (19.7,20.4) | 5.9 (5.7,6.1) | 14.1 (14,14.3) | 1836 (1773,1898) | 53.3 (50.2,56.4) | 53.2 (51.1,55.3) | |
| Mexico City | 905 | 17.4 [15.3,19.7] | 19.1 (18.7,19.6) | 5.5 (5.2,5.8) | 13.6 (13.4,13.9) | 1829 (1743,1914) | 57.9 (54.7,61.2) | 58.0 (56.0,60.1) | |
| South | 5,008 | 31.2 [29.1,33.5] | 20.9 (20.5,21.3) | 6.1 (5.9,6.3) | 14.8 (14.6,15) | 1839 (1791,1887) | 48.9 (47.3,50.6) | 48.8 (47.5,50.1) | |
| Place of residence | |||||||||
| Urban | 8,248 | 73.9 [72.2,75.6] | 19.3 (19.1,19.6) | 5.6 (5.4,5.7) | 13.8 (13.6,13.9) | 1845 (1803,1887) | 55.7 (54.0,57.4) | 55.4 (54.3,56.5) | |
| Rural | 5,994 | 26.1 [24.4,27.8] | 21.3 (21.1,21.5) | 6.2 (6.1,6.4) | 15.1 (14.9,15.2) | 1799 (1759,1838) | 45.1 (43.8,46.4) | 46.0 (45.0,46.9) | |
| Survey | |||||||||
| 2012 | 10,062 | 52.1 [49.4,54.8] | 19.9 (19.7,20.1) | 5.7 (5.6,5.8) | 14.2 (14.1,14.3) | 1883 (1850,1915) | 51.8 (50.7,52.9) | 50.5 (49.8,51.2) | |
| 2016 | 4,180 | 47.9 [45.2,50.6] | 19.8 (19.5,20.2) | 5.8 (5.6,6) | 14.0 (13.8,14.2) | 1779 (1721,1838) | 54.2 (51.7,56.7) | 55.6 (54.0,57.3) | |
Data are from the Encuesta Nacional de Salud y Nutrición de Medio Camino 2016 (Ensanut 2016), and the Encuesta Nacional de Salud y Nutrición 2012
aValues are unweighted sample size, weighted percentages and 95% confidence interval
bExchange rate (July 2024): $1 USD = $17.95 MXN
cCalculated cost residuals adjusted by energy intake, centered at the mean cost
dSchool-aged children: 5 to 11 years; adolescents: 12 to 19 years; adults: ≥ 20 years
When comparing the mean EAT-Lancet index scores between individuals classified as having a low-cost diet versus a high-diet cost, those with a low-cost diet had higher scores compared to those with a high-cost diet (score: 20.3 vs. 19.4, p < 0.001) (Table 2). The limited intake score accounted for the overall score difference (14.6 vs. 13.7, p < 0.001). No significant difference was observed in the emphasized intake score. However, there were differences in all the individual components. Vegetables, fruits, seafood, and nuts had higher scores due to higher intake, and eggs and potatoes had higher scores due to lower intake for individuals in the high-cost category compared to those with a low-cost diet. In contrast, whole grains, legumes, and unsaturated oils had higher scores due to higher intake, and beef and lamb, pork, poultry, dairy, and added sugars had higher scores due to lower intake for individuals in the low-cost diet compared to those in the high-cost diet. Notably, the cost per 100 kcal among consumers in the high-cost diet group was higher for nearly all food groups compared to the low-cost diet group, except for nuts and potatoes. This implies that individuals with a high-cost diet opted for more expensive options within the same food group than those with a low-cost diet (Table 2).
Table 2.
EAT-Lancet index, energy intake, and cost of food groups by diet costa
| Index score | Energy intake, kcal (per capita) | Cost per 100 kcal, MXN$ (per consumer) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low cost | High cost | p value | Low cost | High cost | p value | Low cost | High cost | p value | ||
| EAT-Lancet Indexb | 20.4 (20.2, 20.6) | 19.3 (19.1, 19.6) | < 0.001 | |||||||
| Energy, kcal | 1847 (1805, 1889) | 1819 (1775, 1862) | 0.3 | |||||||
| Average cost per 100 kcal | 2.19 (2.17, 2.21) | 3.67 (3.62, 3.72) | < 0.001 | |||||||
| Emphasized intake | 5.75 (5.63, 5.88) | 5.74 (5.56, 5.92) | 0.9 | |||||||
| Vegetables | 1.15 (1.10, 1.20) | 1.47 (1.41, 1.54) | < 0.001 | 36.9 (35.0, 38.7) | 53.6 (50.6, 56.6) | < 0.001 | 7.62 (7.44, 7.8) | 8.15 (7.99, 8.31) | < 0.001 | |
| Fruits | 0.81 (0.75, 0.87) | 1.41 (1.33, 1.49) | < 0.001 | 42.7 (38.3, 47.0) | 86.8 (80.2, 93.4) | < 0.001 | 5.91 (5.66, 6.17) | 6.9 (6.69, 7.11) | < 0.001 | |
| Whole grains | 1.91 (1.86, 1.96) | 1.25 (1.20, 1.31) | < 0.001 | 505 (489, 522) | 328 (316, 341) | < 0.001 | 0.66 (0.64, 0.68) | 0.83 (0.79, 0.87) | < 0.001 | |
| Legumes | 0.87 (0.81, 0.92) | 0.45 (0.41, 0.05) | < 0.001 | 94.3 (87.3, 101.3) | 46.9 (41.7, 52.2) | < 0.001 | 0.94 (0.91, 0.97) | 1.05 (1, 1.11) | < 0.001 | |
| Seafood | 0.15 (0.12, 0.18) | 0.36 (0.31, 0.42) | < 0.001 | 4.0 (2.7, 5.3) | 19.0 (14.0, 23.9) | < 0.001 | 9.57 (8.97, 10.17) | 12.2 (11.15, 13.25) | < 0.001 | |
| Nuts | 0.02 (0.01, 0.02) | 0.05 (0.02, 0.08) | 0.02 | 3.0 (1.8, 4.2) | 6.3 (3.4, 9.2) | 0.023 | 4.58 (4.34, 4.82) | 4.58 (4.18, 4.98) | 0.7 | |
| Unsaturated oils | 0.85 (0.80, 0.90) | 0.73 (0.66, 0.80) | 0.003 | 112 (104, 120) | 98 (85, 111) | 0.03 | 0.8 (0.75, 0.86) | 1.12 (1.01, 1.22) | < 0.001 | |
| Limited intake | 14.6 (14.5, 14.8) | 13.6 (13.5, 13.7) | < 0.001 | |||||||
| Beef and lamb | 2.37 (2.31, 2.43) | 1.91 (1.84, 1.99) | < 0.001 | 39.8 (33.6, 46.0) | 106 (93.5, 119) | < 0.001 | 6.18 (5.74, 6.62) | 7.25 (6.88, 7.62) | < 0.001 | |
| Pork | 2.10 (2.04, 2.16) | 1.94 (1.85, 2.02) | 0.001 | 58.7 (51.6, 65.8) | 87.4 (72.1, 102.7) | < 0.001 | 4.64 (4.48, 4.8) | 5.23 (5.08, 5.37) | < 0.001 | |
| Poultry | 2.47 (2.43, 2.52) | 2.02 (1.95, 2.10) | < 0.001 | 49.8 (44.7, 54.9) | 108 (98.9, 117) | < 0.001 | 4.75 (4.52, 4.99) | 6.25 (6, 6.5) | < 0.001 | |
| Eggs | 1.74 (1.67, 1.81) | 2.17 (2.10, 2.23) | < 0.001 | 60.1 (55.6, 64.7) | 36.2 (33.0, 39.4) | < 0.001 | 2.71 (2.7, 2.73) | 2.75 (2.72, 2.79) | 0.03 | |
| Dairy | 2.13 (2.08, 2.19) | 1.94 (1.89, 2.00) | < 0.001 | 169 (157, 181) | 190 (180, 201) | 0.01 | 2.98 (2.92, 3.05) | 3.5 (3.43, 3.57) | < 0.001 | |
| Potatoes | 2.65 (2.60, 2.70) | 2.74 (2.71, 2.77) | 0.003 | 22.8 (18.1, 27.5) | 16.3 (13.9, 18.7) | 0.02 | 2.82 (2.77, 2.86) | 2.87 (2.81, 2.93) | 0.2 | |
| Added sugars | 1.16 (1.09, 1.22) | 0.88 (0.82, 0.95) | < 0.001 | 211 (202, 221) | 246 (237, 256) | < 0.001 | ||||
Values are predicted means and 95% confidence intervals (in parenthesis) estimated with Stata’s -margins-command. Total energy intake model was adjusted by age group, sex, socioeconomic status, geographical region, place of residence and survey year. All other models adjusted by the same covariates plus energy intake
aLow-cost diet defined as cost residuals below the median (n = 8,056), and high-cost diet above the media (n = 6,186). Median: $50.84 MXN
bRange for EAT-Lance score goes from 0 to 42 points, with each component going from 0 to 3 points
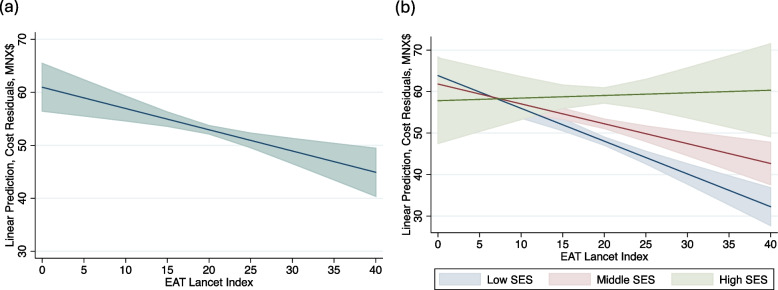
We observed a negative and statistically significant association between the EAT-Lancet score and diet cost. For each increase in one point of the EAT-Lancet score, there was an average decrease of MXN$0.4 in the diet cost (p < 0.001), holding covariates constant (Fig. 1A). Interestingly, this relationship held only for those in the low- and middle-SES categories (Fig. 1B). Among those in the low-SES category, a one-point increase in the EAT-Lancet score was associated with an MXN$0.8 lower diet cost (p < 0.001), holding covariates constant. Similarly, for those in the middle SES category, a one-point increase in the score was associated with an MXN$0.5 lower diet cost (p < 0.001). There was no association between the EAT-Lancet score and diet cost for those in the high-SES category.
Fig. 1.
Adjusted prediction (with 95% CI) estimating the association between diet cost* and the EAT-Lancet index.* Diet cost estimated as calculated cost residuals adjusted by energy intake, centered at the mean cost (A) Estimations are based on an ordinary least squares regression model of diet cost (as cost residuals) and the EAT-Lancet index, adjusted by age group, sex, socioeconomic status (SES), geographical region, place of residence and survey year. B Same model as panel A, plus an interaction term between diet cost and socioeconomic status (SES) level.
Discussion
We estimated the association between diet cost and adherence to the EAT-Lancet reference diet in the Mexican population using two different approaches. First, we dichotomized the cost into low- and high-cost and compared the scores of the EAT-Lancet index. We found that those who consumed a low-cost diet had, on average, a diet quality score 0.9 points higher (out of 42 points) than those who consumed a high-cost diet. This difference was due to the limited intake components, including a lower intake of beef and lamb, pork, poultry, dairy, and added sugars. Second, we estimated the association between diet cost and diet quality using both variables as continuous. We found that for each one-point increase in the EAT-Lancet score, there was an average decrease of MXN$0.4 in the diet cost. Interestingly, when we assessed the effect of measure modification by SES, this relationship was observed only for low- and middle-SES individuals. In contrast, the diets of high-SES individuals had the same cost, regardless of adherence to the EAT-Lancet score. It should be noted that the difference in the diet quality score between the low-cost and the high-cost diet is small (0.9 points) because the population was divided only in two groups, and we are not comparing extreme costs (e.g., lowest vs highest quintiles). The linear relation can give a better sense of the magnitude of the association, the one-point increase in the EAT-Lancet score associated with a decrease of MXN$0.4 is equal to a decrease of 2.5 points in the diet quality score for each MXN$1 increase (equivalent to $0.05 USD), which is an important difference in diet quality.
The finding in our study is contrary to what has been previously observed in high-income countries, where a higher diet quality score was associated with higher diet costs. For instance, a higher cost was associated with higher Healthy Eating Index (HEI) 2010 scores in adults from the United States. When divided into cost quintiles, individuals in the highest diet-cost quintile had 22.4 points more (out of 100) in the HEI score than those in the lowest diet-cost quintile. This difference was mainly explained by a greater intake of vegetables, fruits, whole grains, and seafood and a lower intake of refined grains, solid fats, alcohol, and added sugars [32]. In contrast, in our study, a high-cost diet was associated with a lower intake of whole grains and a higher intake of added sugars. In a study with Spanish participants aged 2 to 24 years, a higher adherence to the Mediterranean diet was associated with an increase of 0.71 Euros per day compared to those in the lower adherence group [33]. Results in the same direction were estimated in Malaysian and Belgian adults using the Malaysian Healthy Eating Index and the Mediterranean Diet Score, respectively [34, 35], and in Swedish and Chinese children using the HEI 2005 and the Chinese Children Dietary Index, respectively [15, 36].
Previous results might not be entirely comparable with our results due to the use of different indexes. For instance, the HEI 2010 score adds points to higher intakes of total protein foods and dairy [37], while the EAT-Lancet index adds points to lower intakes of these food groups. These differences might explain why, contrary to our findings, Curi-Quinto et al. reported a positive association between cost and adherence to the HEI 2015 among Mexicans living in urban areas [20]. Yet, as in our study, they found that the association was not the same across the Mexican population, as in the rural population, they found a null association. Likewise, the HEI 2010 considers food groups and nutrients such as refined grains, sodium, and empty calories (solid fats, alcohol, and added sugar). Thus, the HEI 2010 might be more comprehensive in describing the intake of ultra-processed foods, which the EAT-Lancet index does not include. Although the EAT-Lancet index includes added sugar as a nutrient recommended for limited intake, it probably does not capture the intake of the wide range of ultra-processed products consumed by the Mexican population [38], and that has been extensively associated with negative health outcomes [39, 40]. However, to our knowledge, this is the only analysis that has explored the association of diet cost using an index that measures adherence to the EAT-Lancet recommendations.
We also compared the cost per 100 kcal within the 13 food groups between those who consumed a high- and a low-cost diet. We found that those who consumed a low-cost diet opted for options that were, on average, less expensive than those selected by individuals who consumed a high-cost diet for most food groups. Thus, even though much of the literature has explained diet-related inequities due to the higher price of healthy foods [41, 42], at least in Mexico, there are options within healthy food groups, such as vegetables, fruits, whole grains, legumes, and seafood, that are more affordable.
When we compared across food groups, similar to previous studies [12], we found that the cost of vegetables, fruits, and animal products per 100 kcal was higher than that for other food groups. As discussed by Jones, the higher cost largely depends on the unit of analysis since foods with low energy density seem more expensive when the unit of analysis is the cost per 100 kcal, whereas the cost per weight will reflect the contrary [43]. Moreover, similar to other studies [12, 13, 15], a high-cost diet was associated with a higher intake of fruits and vegetables. Therefore, subsidies for fruits and vegetables could be an effective policy to increase their consumption. A meta-analysis of experimental and prospective observational studies estimated that a 10% decrease in price or subsidy for healthy foods increased consumption by 12% [44].
We also found that a higher-quality diet among those who consumed a low-cost diet was explained by a higher intake of whole grains, legumes, and unsaturated oils and a lower intake of beef and lamb, pork, poultry, dairy, and added sugars. However, even among individuals who consumed a low-cost diet, the average intake of added sugars was 11.4% of total energy intake, 1.4 percentage points above the WHO recommendation [45]. In Mexico, several policy measures have been implemented to address the public health issue of obesity and to improve dietary quality. Among these measures, an MXN$1 tax per liter (approximately a 10% price increase) on sugar-sweetened beverages and an 8% tax on nonessential energy-dense foods were implemented in 2014 [46]. Starting in 2020, all packaged products with high content of calories, added sugars, sodium, saturated fat, and trans-fat are required to display a front-of-pack warning label disclosing their content to consumers [47]. Results from the tax evaluation showed decreases in purchases of sugar-sweetened beverages and taxed foods [48, 49]. We examined whether the relationship between diet cost and diet quality differed by survey year, considering that taxes were implemented between 2012 and 2016. However, we found no evidence of effect measure modification. Thus, a higher tax or a redesign toward a sugar-based design (rather than the existing per-unit tax) could have more meaningful effects on total sugar intake [50]. We also explored effect measure modification by sex, without evidence of a difference in the relationship between men and women.
As previously mentioned, the association between diet cost and diet quality differed by SES. Specifically, the dietary cost was the same for high-SES individuals regardless of adherence to the EAT-Lancet index; for low- and middle-SES individuals, greater adherence was associated with a lower diet cost. Within the high SES stratum, higher adherence to the EAT-Lancet is driven by a higher intake of expensive options such as fruits and seafood, and lower adherence is also driven by expensive options such as red meats, poultry and dairy. Therefore, both higher and lower adherence end up with similar costs. In the lower- and middle-SES strata, greater adherence is driven mainly by less expensive options such as whole grain and legumes (Supplemental Table 2). This finding is in line with what Batis et al. reported in a modeling study in which they generated diet baskets that followed the EAT-Lancet reference diet and compared it with the current diet [22]. Their main finding was that the cost of the EAT-Lancet baskets was lower than that of the current diet baskets due to the savings associated with lower amounts of animal products, sugar-sweetened beverages, and other discretionary foods. However, there was a great overlap in the distribution of diet baskets, suggesting that a diet with specific characteristics could have a wide range of costs.
Several limitations need to be acknowledged. First, as with any data that rely on self-reports, measurement error may affect intake estimates obtained from 24-h dietary recalls. Recall bias and selective underreporting, particularly of foods perceived as unhealthy by the participants, are common issues that affect 24-h recalls [51, 52]. However, 24-h recalls provide very detailed information on food and beverage consumption, which allowed us to match each food to a specific cost. Second, the methodology we used to match food and beverage costs to dietary intake might not reflect the actual cost paid by individuals [53]. We estimated regional and quarterly average prices using data from urban areas and assumed to reflect the cost individuals from a nationally representative sample would pay for food. Nevertheless, large variations could exist within regions, between rural and urban areas, and across individuals. For instance, there could be variations between food prepared at home and purchased away from home or between brand foods and generic or low-cost options. Moreover, there could be differences across SES groups given that low-income families tend to buy in smaller shops with higher costs, while high-income families can afford to buy in bulk, facing lower costs per unit. Third, our cost estimation does not take into account the time and other costs associated with food preparation, given that ready-to-eat foods might have a higher cost but would minimize the time and costs associated with preparation. In contrast, other foods, such as dry legumes, might have lower costs but would need time plus gas or electricity for cooking.
Nevertheless, our study also has several strengths. Although we cannot estimate the actual cost paid by individuals in the sample, the CPI and the ENSANUT data allowed us to consider temporal and spatial variations in food and beverage costs. Our methodology also considered yield factors, increasing the precision of actual costs. Seasonal variation in food prices are not very large in Mexico [22], but still it is an strength that by using ENSANUT data from 2012 and 2016, which were collected in non-overlapping months, all months of the year were represented in our analysis. Having a nationally representative sample allowed us to compare across SES groups. Moreover, the EAT-Lancet index that we used was validated by Stubbendorff et al. in a Swedish cohort with a mean of 20 years of follow-up, showing that higher adherence to the index was associated with lower all-cause mortality, cancer mortality, and cardiovascular mortality [28].
Conclusions
Our results show that a higher adherence to the EAT-Lancet reference diet was associated with lower diet costs in the Mexican population. Thus, contrary to evidence from high-income countries, a healthier diet might not imply higher expenditures on food. However, there is still an urgent need to improve dietary quality in the Mexican population, which requires joint actions to make healthier options more accessible, affordable, and available while limiting access to and marketing of ultra-processed foods and beverages.
Supplementary Information
Acknowledgements
The authors would like to thank ENSANUT’s team and participants.
Abbreviations
- SES
Socioeconomic status
- ENSANUT 2012
Mexican National Health and Nutrition Survey 2012
- ENSANUT 2016
Mexican National Health and Nutrition Survey 2012
- CPI
Consumer Price Index
- INEGI
National System of Statistical and Geographical Information
- CI
Confidence Interval
- MXN
Mexican peso
- HEI
Healthy Eating Index
Authors’ contributions
TCA and CBR had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization: TCA and CBR. Acquisition, analysis, or interpretation of data: TCA and CBR. Writing of the original draft: TCA. Writing, critical review and editing: JCS, SRR, JAR, SB, CBR. Funding acquisition: JAR, SB.
Funding
This study was funded by Bloomberg Philanthropies. Funders had no role in the study design, analysis, data interpretation or writing.
Availability of data and materials
The datasets supporting the conclusions of this article are available on the National Health and Nutrition Survey (ENSANUT) website through https://ensanut.insp.mx/ and on the National System of Statistical and Geographical Information (INEGI) website through https://www.inegi.org.mx/temas/inpc/.
Declarations
Ethics approval and consent to participate
The Research, Biosafety, and Ethics Committees of the National Insitute of Public Health approved the ENSANUT surveys. Informed consent for adults and assent for minors was obtained from all subjects involved in the ENSANUT. For this analysis, ethical review and approval were waived as it used publicly available data for research and publication.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Malnutrition. 2021. https://www.who.int/news-room/fact-sheets/detail/malnutrition. Accessed 1 Sep 2024.
- 3.Lobstein T, Brinsden H, Neveux M. World Obesity Atlas 2023. 2023. https://www.worldobesityday.org/assets/downloads/World_Obesity_Atlas_2023_Report.pdf. Accessed 1 Sep 2024.
- 4.Stevens GA, Beal T, Mbuya MN, Luo H, Neufeld LM, Addo OY, et al. Micronutrient deficiencies among preschool-aged children and women of reproductive age worldwide: a pooled analysis of individual-level data from population-representative surveys. Lancet Glob Health. 2022;10:e1590–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crippa M, Solazzo E, Guizzardi D, Monforti-Ferrario F, Tubiello FN, Leip A. Food systems are responsible for a third of global anthropogenic GHG emissions. Nat Food. 2021;2:198–209. [DOI] [PubMed] [Google Scholar]
- 6.Food and Agriculture Organization. COP26: Agricultural expansion drives almost 90 percent of global deforestation. 2021. https://www.fao.org/newsroom/detail/cop26-agricultural-expansion-drives-almost-90-percent-of-global-deforestation/en. Accessed 1 Sep 2024.
- 7.Mbow H-OP, Reisinger A, Canadell J, O’Brien P. Special Report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems (SR2). Ginevra IPCC; 2017. p. 650. [Google Scholar]
- 8.Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. The Lancet. 2019;393:447–92. [DOI] [PubMed] [Google Scholar]
- 9.HLPE. Nutrition and food systems. A report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. 2017. [Google Scholar]
- 10.FAO, IFAD, UNICEF, WFP, WHO. The State of Food Security and Nutrition in the World 2020: Transforming food systems for affordable healthy diets. Rome, FAO; 2020. [Google Scholar]
- 11.Hirvonen K, Bai Y, Headey D, Masters WA. Affordability of the EAT–Lancet reference diet: a global analysis. Lancet Glob Health. 2020;8:e59-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73:643–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rao M, Afshin A, Singh G, Mozaffarian D. Do healthier foods and diet patterns cost more than less healthy options? A systematic review and meta-analysis. BMJ Open. 2013;3:e004277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alves RM, Lopes CMM, Rodrigues SSP, Perelman J. Adhering to a Mediterranean diet in a Mediterranean country: an excess cost for families? Br J Nutr. 2022;128:1393–400. [DOI] [PubMed] [Google Scholar]
- 15.Rydén PJ, Hagfors L. Diet cost, diet quality and socio-economic position: how are they related and what contributes to differences in diet costs? Public Health Nutr. 2011;14:1680–92. [DOI] [PubMed] [Google Scholar]
- 16.Monsivais P, Rehm CD, Drewnowski A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern Med. 2013;173:1922–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris MA, Hulme C, Clarke GP, Edwards KL, Cade JE. What is the cost of a healthy diet? Using diet data from the UK Women’s Cohort Study. J Epidemiol Community Health. 2014;68:1043–9. [DOI] [PubMed] [Google Scholar]
- 18.Beydoun MA, Fanelli-Kuczmarski MT, Allen A, Beydoun HA, Popkin BM, Evans MK, et al. Monetary value of diet is associated with dietary quality and nutrient adequacy among urban adults, differentially by sex, race and poverty status. PLoS ONE. 2015;10:e0140905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aburto TC, Batis C, Pedroza-Tobías A, Pedraza LS, Ramírez-Silva I, Rivera JA. Dietary intake of the Mexican population: comparing food group contribution to recommendations, 2012–2016. Salud Pública México. 2022;64:267–79. [DOI] [PubMed] [Google Scholar]
- 20.Curi-Quinto K, Unar-Munguía M, Rodríguez-Ramírez S, Röös E, Willett WC, Rivera JA. Diet cost and quality using the Healthy Eating Index-2015 in adults from urban and rural areas of Mexico. Public Health Nutr. 2022;25:2554–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark P, Mendoza-Gutiérrez CF, Montiel-Ojeda D, Denova-Gutiérrez E, López-González D, Moreno-Altamirano L, et al. A healthy diet is not more expensive than less healthy options: cost-analysis of different dietary patterns in Mexican children and adolescents. Nutrients. 2021;13:3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Batis C, Marron-Ponce JA, Stern D, Vandevijvere S, Barquera S, Rivera JA. Adoption of healthy and sustainable diets in Mexico does not imply higher expenditure on food. Nat Food. 2021;2:792–801. [DOI] [PubMed] [Google Scholar]
- 23.Romero-Martinez M, Shamah-Levy T, Cuevas-Nasu L, Gomez-Humaran IM, Gaona-Pineda EB, Gomez-Acosta LM, et al. Methodological design of the National Health and Nutrition Survey 2016. Salud Publica Mex. 2017;59:299–305. [DOI] [PubMed] [Google Scholar]
- 24.Romero-Martinez M, Shamah-Levy T, Franco-Nunez A, Villalpando S, Cuevas-Nasu L, Gutierrez JP, et al. National Health and Nutrition Survey 2012: design and coverage. Salud Publica Mex. 2013;55(Suppl 2):S332–40. [PubMed] [Google Scholar]
- 25.Lopez-Olmedo N, Carriquiry AL, Rodriguez-Ramirez S, Ramirez-Silva I, Espinosa-Montero J, Hernandez-Barrera L, et al. Usual Intake of Added Sugars and Saturated Fats Is High while Dietary Fiber Is Low in the Mexican Population. J Nutr. 2016;146:1856S-S1865. [DOI] [PubMed] [Google Scholar]
- 26.Ramírez-Silva I, Rodríguez-Ramírez S, Barragán-Vázquez S, Castellanos-Gutiérrez A, Reyes-García A, Martínez-Piña A, et al. Prevalence of inadequate intake of vitamins and minerals in the Mexican population correcting by nutrient retention factors, Ensanut 2016. Salud Pública México. 2020;62:521–31. [DOI] [PubMed] [Google Scholar]
- 27.Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77:1171–8. [DOI] [PubMed] [Google Scholar]
- 28.Stubbendorff A, Sonestedt E, Ramne S, Drake I, Hallström E, Ericson U. Development of an EAT-Lancet index and its relation to mortality in a Swedish population. Am J Clin Nutr. 2022;115:705–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mozaffarian RS, Lee RM, Kennedy MA, Ludwig DS, Mozaffarian D, Gortmaker SL. Identifying whole grain foods: a comparison of different approaches for selecting more healthful whole grain products. Public Health Nutr. 2013;16:2255–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Instituto Nacional de Estadística y Geografía. Índice Nacional de Precios al Consumidor: documento metodológico. México: Instituto Nacional de Estadística y Geografía; 2018.
- 31.Pedraza LS, Popkin BM, Salgado JC, Taillie LS. Mexican households’ purchases of foods and beverages vary by store-type, taxation status, and SES. Nutrients. 2018;10:1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rehm CD, Monsivais P, Drewnowski A. Relation between diet cost and Healthy Eating Index 2010 scores among adults in the United States 2007–2010. Prev Med. 2015;73:70–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schröder H, Gomez SF, Ribas-Barba L, Pérez-Rodrigo C, Bawaked RA, Fíto M, et al. Monetary diet cost, diet quality, and parental socioeconomic status in Spanish youth. PLoS ONE. 2016;11:e0161422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pondor I, Gan WY, Appannah G. Higher dietary cost is associated with higher diet quality: A cross-sectional study among selected Malaysian adults. Nutrients. 2017;9:1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pedroni C, Castetbon K, Desbouys L, Rouche M, Vandevijvere S. The cost of diets according to nutritional quality and sociodemographic characteristics: A population-based assessment in Belgium. J Acad Nutr Diet. 2021;121(2187–2200):e4. [DOI] [PubMed] [Google Scholar]
- 36.Zhang X, Gong Y, Jia P, Zhang J, Xue H, Quan L, et al. Monetary diet cost is positively associated with diet quality and obesity: an analysis of school-aged children in Southwest China. J Public Health. 2019;41:250–8. [DOI] [PubMed] [Google Scholar]
- 37.Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, et al. Update of the healthy eating index: HEI-2010. J Acad Nutr Diet. 2013;113:569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marrón-Ponce JA, Sánchez-Pimienta TG, da Costa Louzada ML, Batis C. Energy contribution of NOVA food groups and sociodemographic determinants of ultra-processed food consumption in the Mexican population. Public Health Nutr. 2018;21:87–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pagliai G, Dinu M, Madarena M, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125:308–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suksatan W, Moradi S, Naeini F, Bagheri R, Mohammadi H, Talebi S, et al. Ultra-processed food consumption and adult mortality risk: a systematic review and dose–response meta-analysis of 207,291 participants. Nutrients. 2021;14:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee JH, Ralston RA, Truby H. Influence of food cost on diet quality and risk factors for chronic disease: a systematic review. Nutr Diet. 2011;68:248–61. [Google Scholar]
- 42.Robertson A, Loring B. Guidance for addressing inequities in overweight and obesity. World Health Organization; 2014. [Google Scholar]
- 43.Jones NRV, Monsivais P. Comparing prices for food and diet research: the metric matters. J Hunger Environ Nutr. 2016;11:370–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Afshin A, Penalvo JL, Del Gobbo L, Silva J, Michaelson M, O’Flaherty M, et al. The prospective impact of food pricing on improving dietary consumption: a systematic review and meta-analysis. PLoS ONE. 2017;12:e0172277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization. Guideline: sugars intake for adults and children. World Health Organization; 2015. [PubMed] [Google Scholar]
- 46.Barrientos-Gutiérrez T, Colchero MA, Sánchez-Romero LM, Batis C, Rivera-Dommarco J. Position paper on taxes to nonessential energy-dense foods and sugar-sweetened beverages. Salud Pública México. 2018;60:586b-b591. [DOI] [PubMed] [Google Scholar]
- 47.White M, Barquera S. Mexico adopts food warning labels, why now? Health Syst Reform. 2020;6:e1752063. [DOI] [PubMed] [Google Scholar]
- 48.Salgado Hernández JC, Ng SW, Colchero MA. Changes in sugar-sweetened beverage purchases across the price distribution after the implementation of a tax in Mexico: a before-and-after analysis. BMC Public Health. 2023;23:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Batis C, Rivera JA, Popkin BM, Taillie LS. First-Year Evaluation of Mexico’s Tax on Nonessential Energy-Dense Foods: An Observational Study. PLoS Med. 2016;13:e1002057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hernández JCS, Basto-Abreu A, Junquera-Badilla I, Moreno-Aguilar LA, Barrientos-Gutiérrez T, Colchero MA. Building upon the sugar beverage tax in Mexico: a modelling study of tax alternatives to increase benefits. BMJ Glob Health. 2023;8(Suppl 8):e012227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Willett W. Nutritional epidemiology. Oxford University Press; 2012. [Google Scholar]
- 52.Bailey RL, Mitchell DC, Miller C, Smiciklas-Wright H. Assessing the effect of underreporting energy intake on dietary patterns and weight status. J Am Diet Assoc. 2007;107:64–71. [DOI] [PubMed] [Google Scholar]
- 53.Monsivais P, Perrigue MM, Adams SL, Drewnowski A. Measuring diet cost at the individual level: a comparison of three methods. Eur J Clin Nutr. 2013;67:1220–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets supporting the conclusions of this article are available on the National Health and Nutrition Survey (ENSANUT) website through https://ensanut.insp.mx/ and on the National System of Statistical and Geographical Information (INEGI) website through https://www.inegi.org.mx/temas/inpc/.