Highlights
-
•
Residents of Puerto Rico have experienced multiple adverse events in recent years.
-
•
We interviewed over 1,300 adults in Puerto Rico before and during the COVID-19 pandemic.
-
•
We found that higher resilience and coping were linked with better quality diet, sleep, and physical activity.
-
•
These relationships were stronger among participants interviewed during the COVID-19 pandemic.
-
•
We did not find relationships between higher resilience and coping and alcohol use or smoking.
Keywords: Resilience, Coping, Trauma, Natural disasters, Pandemic, Health behaviors
Abstract
Objective: Residents of Puerto Rico have recently experienced multiple adverse events, including hurricanes, earthquakes, and political unrest. Such adversity is associated with worse mental and physical health. Psychological resilience and effective coping may mitigate these relations by fostering positive health behaviors, like consuming a high-quality diet and being physically active. However, empirical evidence for these relationships is limited. Methods: We assessed psychological resilience, resilient coping, and health behaviors among two groups of adults in Puerto Rico, before and during the pandemic, in 2019–2023 (total N = 1,342). Resilience and resilient coping were assessed using the Brief Resilience Scale and Brief Resilient Coping Scale. Diet quality was defined by the Alternate Healthy Eating Index from a food frequency questionnaire. We collected data on sleep, physical activity, alcohol intake, and tobacco use using validated questionnaires. Results: Adjusting for confounders, higher resilience z-scores were associated with being in the highest category of diet quality [OR: 1.25, 95 % CI: 1.04, 1.50]; getting 7–8 h of sleep per night [OR: 1.15, 95 % CI: 1.02,1.30]; and reporting moderate or heavy physical activity (vs. light or sedentary) [OR: 1.17, 95 % CI: 1.02,1.34]. The same patterns were observed for higher resilient coping z-scores, and for categorical measures of resilience and resilient coping. These relationships were stronger among participants interviewed during (vs. before) the COVID-19 pandemic, suggesting that resilience and resilient coping may be particularly relevant during an ongoing stressor. Conclusion: Identifying supportive strategies to cultivate resilience and effective coping mechanisms may contribute to healthier behaviors, particularly in a vulnerable population.
1. Introduction
Traumatic societal events can adversely influence health (Lantz et al., 2005, Pietrzak et al., 2012a). Society-wide trauma can range from persistent financial scarcity or violence to less predictable events like economic shocks or climate-related disasters. For example, high-income nations saw a decline in self-rated health and increased morbidity and psychological distress after the 2007–2009 Great Recession (Margerison-Zilko et al., 2016). Political events of vast magnitude (e.g., presidential elections) also have negative health effects, particularly in communities that have been marginalized or oppressed (Williams & Medlock, 2017).
Systematic reviews suggest that individuals with higher psychological resilience or positive coping strategies have better mental and physical health (Avila et al., 2017, Cal et al., 2015 Park et al., 2022, Taylor and Stanton, 2007). Population-based studies have shown that most individuals demonstrate resilience after trauma (Bonanno, 2004, Bonanno et al., 2006, Pietrzak et al., 2012b), by engaging core aspects of resilience, e.g., personal control, a sense of coherence, and use of resources, which guide effective stress responses (Reich, 2006). Resilience can also be defined as positive psychological functioning, the absence of significant psychopathology despite experiencing of trauma, or the ability to cope effectively after adversity (Bonanno, 2004, Bonanno and Diminich, 2013, Luthar et al., 2000). Investigators speculate that resilience and coping may buffer negative health outcomes partly through a health behavior pathway (Krok et al., 2023). Although some studies have found that health behaviors influence later resilience and coping levels (Segovia et al., 2013, Wister et al., 2022), the bulk of the literature suggests that the directionality of this association proceeds from resilience to health behaviors. For example, in the NutriNet-Santé study, participants with higher resilience reported better overall diet quality, including a greater intake of seafood and whole-grain foods and lower intake of ultra-processed foods and confectionery products (Robert et al., 2022). Similarly, higher resilience among Australian adolescents was associated with higher physical activity levels, independent of psychological distress (To et al., 2022). In the Women’s Health Initiative, higher resilience was associated with higher odds of adhering to a better diet and recommended physical activity, sleeping 7–9 h per night, and consuming alcohol moderately (Springfield et al., 2020).
Despite data suggesting a connection between resilience and health behaviors, few studies on this topic have been conducted in the context of population-level adversity, instead primarily focusing on individual-level experiences like childhood trauma (Hughes et al., 2017, Nishimi et al., 2022). Furthermore, scant research in this area is conducted among vulnerable communities who already experience disproportionate social inequities that increase their risk for unhealthy behaviors and disease (OHCHR, United Nations, n.d.).
Residents of Puerto Rico, a territory of the United States, are a vulnerable population with documented social and health inequities (Previdi & Vega, 2020) who have recently experienced multiple society-wide traumas. In the past seven years, Puerto Rico has faced Hurricanes Irma and María (2017), earthquakes in 2019–2020, Hurricane Fiona (2022), sociopolitical unrest, an enduring economic crisis, and the COVID-19 pandemic (Ezell et al., 2021). Studies have documented adverse physical, mental, and behavioral health outcomes, including higher sedentarism and binge drinking, after these events (Ezell et al., 2021, Garciá et al., 2021, Hernádez-Torres et al., 2023, Llibre-Guerra et al., 2020, López-Cepero et al., 2022, Mattei et al., 2022, Scaramutti et al., 2019). Simultaneously, these events sparked narratives of resilience, unity, crafting a ‘new normal’, and rebuilding, as individuals shifted their outlook, especially among underserved groups (Marrero et al., 2022, Petrun Sayers et al., 2023, Sato et al., 2022, Yabe et al., 2021). Meaning-making (the meaning that individuals give to a difficult event) is likely to be a key process here, as it was shown to be a primary mediator in the relationship between resilience and health behaviors in a serial mediation analysis of data collected among recovered COVID-19 patients in a different geographic setting (Krok et al., 2023).
Based on a meaning-making theoretical model positing that reframing negative experiences may help people adopt healthy behaviors (Krok et al., 2023), and on the existing literature above, we hypothesized that higher psychological resilience and resilient coping in the context of these events in Puerto Rico would be associated with better diet quality, more physical activity, healthier sleep duration, moderate or no alcohol use, and no tobacco use. We further hypothesized that the relationships between psychological resilience and health behaviors would be strongest (i.e., most evident) among participants interviewed during the COVID-19 pandemic, an additional stressful event that began in the middle of our recruitment period, contributing to worsening health behaviors in other populations (Du et al., 2021, Knell et al., 2020) and plausibly operating as an effect modifier in the relationships between resilience or resilient coping and health behaviors.
2. Methods
2.1. Sample
This study used cross-sectional data from the Puerto Rico Observational Study of Psychosocial, Environmental, and Chronic Disease Trends (PROSPECT), an ongoing study beginning in 2019 (Mattei et al., 2021). See Appendix for recruitment details. Briefly, adults aged 30–75 who had lived in Puerto Rico for at least the prior year and were able to answer questions without assistance were recruited using multiple sampling strategies. Eligible participants were invited to an interview administered by trained research assistants at partner clinics, following standardized procedures. Participants provided written, informed consent. The Harvard T.H. Chan School of Public Health Institutional Review Board approved this study. All procedures were performed in compliance with relevant laws and institutional guidelines.
At the time of analysis, 1,367 individuals were interviewed. After removing 25 incomplete or inaccurate interviews, 1,342 individuals were included in this study. Analyses considering diet quality as an outcome used a smaller sample of 738 participants whose food frequency questionnaires were processed by the time of analysis.
2.2. Resilience and resilient coping
Self-rated resilience was measured with the Spanish Brief Resilience Scale (BRS), which assesses the ability to rebound from stressful events (Rodríguez-Rey et al., 2016). Self-reported resilient coping was measured with the Spanish Brief Resilient Coping Scale (BRCS), which assesses perceived competence and coping tactics (Limonero et al., 2014). Both measures have been shown to be reliable in other Spanish-speaking populations. The BRS includes six items (e.g., “I tend to bounce back quickly after hard times”), each rated on a scale from 1 to 5 (“totally disagree” to “totally agree”). The overall score is calculated as the mean of the individual responses. The mean score was categorized into low resilience (1.0–2.9), medium resilience (3.0–4.2), and high resilience (4.3–5.0) for clearer interpretations, and based on prior work (Smith et al., 2013). The BRCS includes four items (e.g., “I look for creative ways to alter difficult situations”), each rated on a scale from 1 to 5 (“does not describe me at all” to “describes me very well”). The total score is calculated as the sum of the individual responses. The total score ranges from 4 to 20, with pre-defined categories of low (4–13), medium (14–16), and high resilient coping (17–20), based on prior work (Brief Resilient Coping Scale (BRCS), (n.d.), Limonero et al., 2014, Sinclair and Wallston, 2004). Cronbach’s alpha was 0.79 for the BRS and 0.84 for the BRCS. The Pearson correlation between the two standardized scores was 0.40 (P < 0.0001), suggesting that the two scales share variance but are distinct. Thus, each variable was included as an exposure in separate models (i.e., no models included both exposures simultaneously). Further, each was modeled as both a continuous, standardized variable and a categorical variable in separate models.
2.3. Health behaviors
We considered diet quality, sleep duration, physical activity, alcohol use, and smoking (tobacco use) as outcomes. Diet was measured with a food frequency questionnaire, culturally adapted for this population and validated against biomarkers of intake (Palacios et al., 2015, Tucker et al., 1998, Tucker et al., 2010). The Minnesota Nutritional Data System (NDS-R, version 5.0_35) was used for food and nutrient analyses, and the Alternate Healthy Eating Index (AHEI) was used to classify diet quality (McCullough & Willett, 2006). We tertiled the overall AHEI scores to create three categories of diet quality, relative to the sample, as done in the Multiethnic Cohort to determine association with type 2 diabetes and cardiometabolic factors (Jacobs et al., 2017).
Physical activity at work, outside, or at home was measured using a modified version of the Paffenbarger questionnaire from the Harvard Alumni Activity Survey, which was validated against objective activity measures and tested in Puerto Rican adults (Paffenbarger et al., 1978, Paffenbarger et al., 1993, Tucker et al., 2010). A physical activity score was calculated as the sum of hours spent on typical daily activities, multiplied by weighting factors that parallel the rate of oxygen consumption associated with each activity. Physical activity levels were defined as sedentary, light, moderate, and vigorous/heavily active, using cutoffs previously established among Puerto Rican adults to reflect physical activity guidelines (Sotos-Prieto et al., 2015). For regressions, a binary variable was created to combine sedentary and light activity vs. moderate/vigorous physical activity.
Sleep duration, alcohol intake, and tobacco use information was collected using questions previously asked in this and similar populations (Li et al., 2014, Tucker et al., 2010). Usual hours of sleep per 24-hour period were classified as short (≤6 h), healthy (7–8 h), or long duration (≥9 h). For the regressions, we created a binary variable of extreme sleep (short or long) vs. healthy sleep, based on evidence of association with both short and long sleep duration and overall mortality and incidence of various chronic diseases (Cappuccio et al., 2010, Chaput et al., 2020, Jike et al., 2018). Alcohol use was probed for frequency of intake of common alcoholic beverages; responses were categorized into heavy drinking (≥8 drinks per week for women or ≥ 15 drinks per week for men) vs. moderate or no drinking; we also ran a sensitivity analysis excluding non-drinkers. Tobacco use was categorized as being a never, former, or current smoker; a binary variable was created to define non-smoker vs. current or former smoker for regressions.
2.4. Covariates
The Supplemental Methods (Appendix) details the covariates. Briefly, participants provided information on sex at birth, ethnicity, marital status, education, income, area of residence, household size, health insurance, and personal and family history of major chronic diseases (Choi et al., 2019, Garg et al., 2022). A physical morbidity index was created by summing responses to 25 self-reported chronic health conditions ever diagnosed by a health professional (Appendix Table 1).
A “mental health index” was considered as an additional potential covariate in sensitivity analyses, given the relationships between other aspects of mental health and both resilience/resilient coping and health behaviors (Walsh et al., 2013, Weitzel et al., 2022). See Appendix for more details. Briefly, the index was calculated by summing probable disorders based on screeners of depression (Center for Epidemiologic Studies-Depression Scale (Falcón and Tucker, 2000, González et al., 2017, Radloff, 1977)), anxiety (Generalized Anxiety Disorder-7 (García-Campayo et al., 2010, Löwe et al., 2008, Spitzer et al., 2006)), and post-traumatic stress syndrome (Eisenman et al., 2003, Lang and Stein, 2005), or self-reported current or past medical diagnosis of depression, anxiety, and “other mental or psychological diagnosis”. Other psychosocial covariates considered in sensitivity analyses were short-term stress (14-item Perceived Stress Scale (Cohen et al., 1983, Falcon et al., 2009, Perera et al., 2017)); loneliness (3-item UCLA Loneliness Scale (Hughes et al., 2004)); and social support (Interpersonal Support Evaluation List-12 (Merz et al., 2014, Sarason and Sarason, 1985)).
2.5. Effect modifier
We stratified analyses into two groups of participants by date of completing the interview in relation to the COVID-19 pandemic: participants who completed interviews between March 21, 2019-March 16, 2020 were considered pre-pandemic. Those who completed interviews between May 12, 2020-April 4, 2023 were considered “during pandemic.” These were two separate groups of individuals, based on interview timing; no longitudinal within-person data was available.
2.6. Statistical analyses
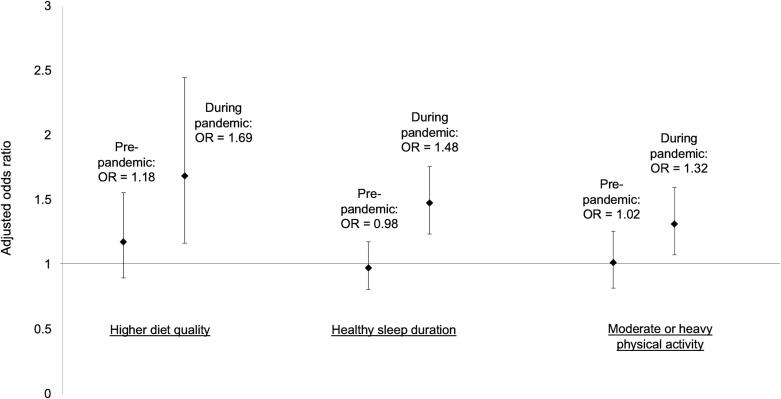
We assessed the distribution of participants' sociodemographic, psychosocial, and health factors, overall, and by levels of resilience or resilient coping (Table 1). We assessed the distributions of the five health behavior outcomes, overall and by levels of resilience or resilient coping, before dichotomizing the outcomes for regressions (Table 2). Separate logistic models estimated odds ratios (95 % confidence intervals) of engaging in high diet quality, healthy sleep duration, moderate or heavy physical activity, non-heavy alcohol use, and being a non-smoker, with BRS and BRCS separately entered as a continuous score (z-score) or as categories (Table 3). Outcomes were dichotomized for comparability across models and practical interpretation. Models were adjusted for the potential confounders listed above. Given correlations among health behaviors (Saint Onge and Krueger, 2017, Sotos-Prieto et al., 2015), we also adjusted for the health behaviors other than the outcome of interest in our primary models (e.g., when modeling diet quality as the outcome, we adjusted for sleep duration, physical activity, alcohol use, and smoking status). We further adjusted models for mental health and psychosocial indicators listed above as a sensitivity analysis (Table 3). Finally, we stratified the primary models by pre-pandemic timing vs. during the pandemic (Fig. 1, Appendix).
Table 1.
Descriptive characteristics, overall and by levels of resilience and resilient coping, among 1,342 adults interviewed in 2019–2023 in Puerto Rico.
|
Resilience (BRS; total score range: 1–5;mean: 3.7) |
Resilient coping (BRCS; total score range: 4–20; mean: 17.9) |
||||||
|---|---|---|---|---|---|---|---|
| Low resilience (1.0–2.9) | Medium resilience (3.0–4.2) | High resilience (4.3–5.0) | Low coping (4–13) | Medium coping (14–16) |
High coping (17–20) | ||
| n (%) or mean (SD) | n (%) or mean (SD) | n (%) or mean (SD) | |||||
| Age | 52.1 (11.6) | 50.9 (11.1) | 52.3 (11.6) | 52.7 (12.0) | 50.0 (10.9) | 50.5 (11.2) | 52.9 (11.8) |
| Sex at birth | |||||||
| Male | 344 (26.5) | 58 (26.2) | 139 (25.4) | 127 (27.4) | 27 (30.3) | 70 (27.7) | 226 (25.5) |
| Female | 956 (73.5) | 163 (73.8) | 408 (74.6) | 337 (72.6) | 62 (69.7) | 183 (72.3) | 660 (74.5) |
| Ethnicity | |||||||
| Puerto Rican | 1219 (93.8) | 205 (92.8) | 514 (94.0) | 437 (94.2) | 87 (97.8) | 237 (93.7) | 828 (93.5) |
| Dominican | 36 (2.8) | 4 (1.81) | 19 (3.5) | 10 (2.2) | 1 (1.1) | 4 (1.6) | 29 (3.3) |
| Other | 45 (3.46) | 12 (5.4) | 14 (2.6) | 17 (3.7) | 1 (1.1) | 12 (4.7) | 29 (3.3) |
| Marital status | |||||||
| Married or partnered | 617 (47.6) | 93 (42.3) | 264 (48.4) | 235 (50.7) | 39 (44.3) | 129 (51.2) | 423 (47.7) |
| Divorced, separated, or widowed | 321 (24.8) | 61 (27.7) | 127 (23.3) | 113 (24.4) | 20 (22.7) | 55 (21.8) | 225 (25.4) |
| Single | 358 (27.6) | 66 (30.0) | 155 (28.4) | 116 (25.0) | 29 (33.0) | 68 (27.0) | 238 (26.9) |
| Education | |||||||
| Less than high school | 85 (6.6) | 24 (10.9) | 39 (7.1) | 16 (3.46) | 16 (18.2) | 20 (7.9) | 44 (5.0) |
| High school graduate or GED | 228 (17.6) | 47 (21.4) | 93 (17.0) | 75 (16.2) | 17 (19.3) | 46 (18.3) | 152 (17.2) |
| Some college or Associates degree | 325 (25.1) | 68 (30.9) | 135 (24.7) | 106 (22.9) | 21 (23.9) | 68 (27.0) | 217 (24.6) |
| College degree | 364 (28.1) | 47 (21.4) | 147 (26.9) | 152 (32.9) | 22 (25.0) | 69 (27.4) | 253 (28.6) |
| Graduate degree | 292 (22.6) | 34 (15.5) | 132 (24.2) | 113 (24.5) | 12 (13.6) | 49 (19.4) | 218 (24.7) |
| Yearly income | |||||||
| ≤$10,000 | 359 (28.6) | 88 (41.3) | 142 (27.1) | 102 (22.3) | 35 (40.2) | 85 (34.3) | 209 (24.5) |
| $10,001–20,000 | 328 (26.1) | 56 (26.3) | 142 (27.1) | 117 (25.6) | 27 (31.0) | 62 (25.0) | 223 (26.1) |
| $20,001–50,000 | 427 (34.0) | 56 (26.3) | 186 (35.4) | 169 (37.0) | 18 (20.7) | 83 (34.3) | 308 (36.1) |
| >$50,000 | 141 (11.2) | 13 (6.10) | 55 (10.5) | 69 (15.1) | 7 (8.1) | 16 (6.5) | 114 (13.4) |
| Area of residence | |||||||
| Urban | 866 (66.7) | 144 (65.8) | 373 (68.2) | 302 (65.1) | 58 (65.2) | 181 (71.8) | 577 (65.2) |
| Rural | 330 (25.4) | 58 (26.5) | 135 (24.7) | 126 (27.2) | 26 (29.2) | 55 (21.8) | 237 (26.8) |
| Peri-urban | 102 (7.9) | 17 (7.8) | 39 (7.1) | 36 (7.8) | 5 (5.6) | 16 (6.4) | 71 (8.2) |
| Household family size | 2.49 (1.2) | 2.47 (1.2) | 2.45 (1.3) | 2.56 (1.3) | 2.22 (1.0) | 2.62 (1.3) | 2.49 (1.2) |
| Survey timing | |||||||
| Completed during COVID-19 | 784 (60.3) | 138 (62.4) | 279 (51.0) | 323 (69.6) | 51 (57.3) | 115 (45.5) | 572 (45.6) |
| Completed before COVID-19 | 516 (39.7) | 83 (37.6) | 268 (49.0) | 141 (30.4) | 38 (42.7) | 138 (54.6) | 314 (35.4) |
| Health insurance | |||||||
| No health insurance | 51 (3.9) | 8 (3.6) | 25 (4.6) | 17 (3.7) | 7 (7.9) | 5 (2.0) | 38 (4.3) |
| Health insurance | 1246 (96.1) | 212 (96.4) | 522 (95.4) | 447 (96.3) | 82 (92.1) | 247 (98.0) | 848 (95.7) |
| Family history of chronic conditions | |||||||
| <5 of 8 conditions in family history | 725 (56.4) | 100 (45.7) | 325 (59.7) | 259 (56.2) | 54 (60.7) | 151 (59.7) | 477 (54.3) |
| ≥5 of 8 conditions in family history | 561 (43.6) | 119 (54.3) | 219 (40.3) | 202 (43.8) | 35 (39.3) | 102 (40.3) | 401 (45.7) |
| Physical morbidity Index | 3.3 (2.6) | 3.8 (2.7) | 2.5 (1.3) | 2.6 (1.3) | 3.7 (2.7) | 3.2 (2.6) | 3.3 (2.5) |
| Mental health morbidity index | 1.4 (1.7) | 3.1 (1.8) | 1.4 (1.6) | 0.7 (1.1) | 2.8 (2.0) | 1.7 (1.8) | 1.2 (1.5) |
| Loneliness scale | 4.5 (1.7) | 5.5 (2.2) | 4.5 (1.6) | 3.9 (1.3) | 5.9 (2.1) | 4.7 (1.7) | 4.2 (1.6) |
| Social support scale | 27.8 (8.5) | 23.0 (10.2) | 27.2 (7.5) | 31.0 (7.3) | 19.8 (9.5) | 26.0 (7.3) | 29.2 (8.1) |
| Perceived Stress Scale | 17.0 (10.4) | 25.0 (10.8) | 18.2 (9.3) | 11.7 (8.4) | 27.1 (10.5) | 20.5 (8.7) | 14.9 (10.0) |
BRS = Brief Resilience Scale (higher score = higher resilience), BRCS = Brief Resilient Coping Scale (higher score = higher coping). Physical morbidity index: sum of 25 self-reported conditions ever diagnosed by a health professional (see Appendix). Mental health index: sum of endorsements of probable depression, anxiety, or post-traumatic stress disorder, as well as self-reported current or past medical diagnosis of depression, anxiety, or “other mental or psychological diagnosis” (range: 1–6). Loneliness: 3-item UCLA Loneliness Scale (higher score = more loneliness). Social support: Interpersonal Support Evaluation List-12 (higher score = more social support).
Table 2.
Prevalence of health behaviors, overall and by levels of resilience and resilient coping, among 1,342 adults, 2019–2023, Puerto Rico.
| AHEI tertiled (n (%)) |
Average sleep hours (3 categories)(n (%)) |
|||||
|---|---|---|---|---|---|---|
| Bottom AHEI tertile | Middle AHEI tertile | Top AHEI tertile | 6 or fewer hours per night | 7–8 h per night | 9 or more hours per night | |
| Total sample | 246 (33.3) | 246 (33.3) | 246 (33.3) | 509 (40.3) | 675 (53.4) | 79 (6.3) |
| By level of resilience (BRS): | ||||||
| Among those with low resilience | 44 (38.6) | 43 (37.7) | 27 (23.7) | 109 (49.6) | 94 (42.7) | 17 (7.7) |
| Among those with medium resilience | 108 (33.8) | 106 (33.1) | 106 (33.1) | 221 (40.5) | 297 (54.4) | 28 (5.1) |
| Among those with high resilience | 78 (29.8) | 83 (31.7) | 101 (38.6) | 162 (35.1) | 270 (58.4) | 30 (6.5) |
| By level of resilient coping (BRCS): | ||||||
| Among those with low resilient coping | 32 (65.3) | 8 (16.3) | 9 (18.4) | 49 (55.7) | 33 (37.5) | 6 (6.8) |
| Among those with medium resilient coping | 57 (38.8) | 53 (36.1) | 37 (25.2) | 110 (43.5) | 128 (40.6) | 15 (5.9) |
| Among those with high resilient coping | 142 (28.5) | 171 (34.3) | 186 (37.3) | 333 (37.7) | 496 (56.2) | 54 (6.1) |
| Physical Activity (n (%)) | Heavy drinking (n (%)) | Smoking status (n (%)) | ||||||
|---|---|---|---|---|---|---|---|---|
| Sedentary/ Lightly active | Moderately active | Heavily active | Heavy drinking | Non-heavy drinking | Never smoker | Former smoker | Current smoker | |
| Total sample | 897 (69.0) | 286 (22.0) | 117 (9.0) | 135 (13.2) | 891 (86.8) | 869 (68.6) | 244 (19.3) | 153 (12.1) |
| By level of resilience (BRS): | ||||||||
| Among those with low resilience | 159 (72.0) | 48 (21.7) | 14 (6.3) | 20 (11.3) | 157 (88.7) | 152 (68.8) | 38 (17.2) | 31 (14.0) |
| Among those with medium resilience | 403 (73.7) | 96 (17.6) | 48 (8.8) | 49 (10.8) | 403 (89.2) | 377 (69.1) | 107 (19.6) | 62 (11.4) |
| Among those with high resilience | 284 (61.2) | 128 (27.6) | 52 (11.2) | 63 (16.8) | 311 (83.2) | 320 (69.0) | 92 (19.8) | 52 (11.2) |
| By level of resilient coping (BRCS): | ||||||||
| Among those with low resilient coping | 65 (73.0) | 15 (16.9) | 9 (10.1) | 7 (10.9) | 57 (89.1) | 60 (67.4) | 13 (14.6) | 16 (18.0) |
| Among those with medium resilient coping | 188 (74.3) | 46 (18.2) | 19 (7.51) | 24 (11.3) | 188 (88.7) | 176 (69.6) | 52 (20.6) | 25 (9.9) |
| Among those with high resilient coping | 589 (66.5) | 211 (23.8) | 86 (9.71) | 101 (14.0) | 623 (86.1) | 609 (68.8) | 171 (19.3) | 105 (11.9) |
BRS = Brief Resilience Scale, BRCS = Brief Resilient Coping Scale, AHEI = Alternative Healthy Eating Index.
Table 3.
Adjusted logistic models estimating odds (95% confidence interval) of engaging in health behaviors by continuous z-scores or categories of resilience or resilient coping, among 1,342 adults, 2019–2023, Puerto Rico.
| Top AHEI tertile vs. middle or low | Healthy sleep hours vs. extreme sleep hours | Moderate or heavy physical activity vs. sedentary or light activity | Non-heavy drinking vs. heavy drinking | Non-smoker vs. current or former smoker | |
|---|---|---|---|---|---|
| Odds ratio (95 % confidence interval) | |||||
| Model 1 | |||||
| Resilience (BRS) score, standardized | 1.25 (1.04, 1.50) | 1.15 (1.02, 1.30) | 1.17 (1.02, 1.34) | 0.83 (0.67, 1.03) | 1.01 (0.84, 1.22) |
| BRS categorical: | |||||
| Medium resilience vs. low resilience | 1.58 (0.93, 2.68) | 1.39 (0.99, 1.95) | 0.95 (0.65, 1.39) | 1.20 (0.66, 2.19) | 1.02 (0.61, 1.70) |
| High resilience vs. low resilience | 1.87 (1.08, 3.22) | 1.68 (1.19, 2.38) | 1.62 (1.11, 2.37) | 0.79 (0.44, 1.43) | 0.96 (0.57, 1.64) |
| Resilient coping (BRCS) score, standardized | 1.31 (1.07, 1.60) | 1.25 (1.10, 1.41) | 1.19 (1.04, 1.37) | 0.83 (0.66, 1.05) | 0.91 (0.75, 1.10) |
| BRCS categorical: | |||||
| Medium resilient coping vs. low resilient coping | 1.34 (0.57, 3.15) | 1.65 (0.98, 2.79) | 0.83 (0.46, 1.48) | 0.86 (0.32, 2.28) | 1.47 (0.68, 3.17) |
| High resilient coping vs. low resilient coping | 2.02 (0.92, 4.46) | 2.05 (1.27, 3.31) | 1.32 (0.78, 2.23) | 0.72 (0.29, 1.76) | 0.97 (0.49, 1.89) |
| Model 2 | |||||
| Resilience (BRS) score, standardized | 1.28 (1.03, 1.59) | 0.97 (0.84, 1.12) | 1.17 (0.99, 1.37) | 0.83 (0.65, 1.07) | 0.84 (0.66, 1.06) |
| BRS categorical: | |||||
| Medium resilience vs. low resilience | 1.54 (0.87, 2.71) | 1.16 (0.80, 1.67) | 0.98 (0.65, 1.47) | 1.02 (0.53, 1.97) | 0.72 (0.41, 1.28) |
| High resilience vs. low resilience | 1.89 (1.03, 3.49) | 1.13 (0.75, 1.69) | 1.66 (1.07, 2.58) | 0.81 (0.41, 1.62) | 0.59 (0.31, 1.13) |
| Resilient coping (BRCS) score, standardized | 1.35 (1.07, 1.70) | 1.09 (0.95, 1.26) | 1.18 (1.01, 1.38) | 1.02 (0.78, 1.33) | 0.83 (0.67, 1.04) |
| BRCS categorical: | |||||
| Medium resilient coping vs. low resilient coping | 1.35 (0.56, 3.23) | 1.27 (0.74, 2.19) | 0.77 (0.43, 1.40) | 1.13 (0.41, 3.10) | 1.12 (0.49, 2.57) |
| High resilient coping vs. low resilient coping | 2.08 (0.90, 4.81) | 1.40 (0.84, 2.34) | 1.23 (0.71, 2.16) | 1.24 (0.46, 3.32) | 0.70 (0.32, 1.50) |
BRS = Brief Resilience Scale, BRCS = Brief Resilient Coping Scale, AHEI = Alternative Healthy Eating Index.
Model 1: adjusted for age, sex, income, marital status, rural vs. urban residence, health insurance, morbidity index, family history of chronic conditions, household family size, and the health behaviors other than the outcome (e.g., for the diet quality model, the following covariates were included: healthy sleep, physical activity level, heavy drinking, and smoking status).
Model 2: Model 1 covariates + mental health index (including probable depression, anxiety, and post-traumatic stress disorder), social support score, perceived stress score, and loneliness score.
Fig. 1.
Odds ratios for engaging in health behaviors by continuous BRCS z-score, stratified by pandemic timing, among 1,342 adults, 2019–2023, Puerto Rico. BRCS = Brief Resilient Coping Scale (higher score = higher resilience). OR = odds ratio. Vertical bars indicate 95% confidence intervals. Pre-pandemic: interviewed between March 21, 2019 − March 16, 2020. During pandemic: interviewed between May 12, 2020 − April 4, 2023. Higher diet quality: in the top tertile of Alternative Healthy Eating Index in the sample compared to middle or lowest tertile. Healthy sleep duration: 7–8 h on average compared to ≥9 h on average. Moderate or heavy physical activity: compared to sedentary and light activity. All models are adjusted for age, sex, income, marital status, rural vs. urban residence, health insurance, morbidity index, family history of chronic conditions, household family size, and the health behaviors other than the outcome (e.g., for the diet quality model, the following covariates were included: healthy sleep, physical activity level, heavy drinking, and smoking status).
Missing data information is included in the Appendix.
3. Results
The mean BRS score in this sample was 3.7 (standard deviation (SD) = 0.9). The mean BRCS score was 17.9 (SD = 2.9). For the BRS categories, participants had low (17.9 %), medium (44.4 %), and high resilience (37.7 %). For the BRCS, participants had low (7.3 %), medium (20.6 %), and high (72.2 %) coping.
The mean age was 52.1 years (SD = 11.6; Table 1). Participants were predominantly female at birth and of Puerto Rican ethnicity. Participants in the high BRS category were more likely to be married, have higher educational attainment, report higher income, and report fewer mental health conditions, compared to the low and medium BRS groups. Similar trends were observed for BRCS categories.
Participants in the high (vs. low or medium) BRS category were more likely to be in the top tertile for total AHEI score, have healthy sleep hours, and engage in moderate/vigorous physical activity; similar patterns were observed for BRCS (Table 2). There were also more current smokers in the low BRS (14.0 %) and BRCS (18.0 %) categories, compared to only 12.1 % in the overall sample. Finally, there were more heavy drinkers in the high BRS (16.8 %) and BRCS (14.0 %) groups, compared to 13.2 % in the total sample.
After adjusting for potential confounders, we observed positive associations for both resilience and resilient coping with better diet quality, healthier sleep hours, and more physical activity, when modeling either the standardized scores or the categorical variables as predictors (Table 3). For example, participants in the highest BRS category had higher odds of being in the healthiest diet quality group [OR: 1.87, 95 % CI: 1.08, 3.22]. Similarly, those in the highest BRCS category had higher odds of reporting healthy sleep hours compared to extreme sleep hours [OR: 2.05, 95 % CI: 1.27, 3.31]. Neither resilience nor resilient coping were clearly or meaningfully associated with alcohol use or smoking status. Findings were similar in analyses with alcohol use that excluded non-drinkers (not shown).
Across outcomes, after additionally adjusting for the mental health index and other psychosocial factors, results remained consistent, albeit with wider confidence intervals and slightly attenuated estimates for healthy sleep hours (e.g., OR for standardized BRCS: 1.09 [95 % CI: 0.95, 1.26] in Model 2 compared to OR: 1.25 [95 % CI: 1.10, 1.41] in Model 1, Table 3). Across outcomes, consistent results were also observed in analyses that did not adjust for other health behaviors (see Appendix Table 2).
In our analyses stratified by date of interview in relation to the pandemic, associations between BRS and BRCS with higher diet quality, healthy sleep duration, and more physical activity were consistently stronger among individuals interviewed during COVID-19, compared to those interviewed pre-pandemic (Fig. 1 and Appendix Table 3). For example, no relationship was observed between standardized BRCS and healthy sleep duration among those interviewed pre-pandemic [OR: 0.98, 95 % CI: 0.81, 1.18], whereas the magnitude of the estimate was substantially stronger among those interviewed during the pandemic [OR: 1.48, 95 % CI: 1.24, 1.76], with non-overlapping confidence intervals (Fig. 1, Appendix Table 3).
4. Discussion
In this cross-sectional study of adults in Puerto Rico who experienced multiple adversities, we found higher self-rated resilience and resilient coping were associated with healthier quality diet, physical activity, and sleep duration after adjusting for confounders, including physical and mental health conditions and other health behaviors. These positive associations were stronger among individuals interviewed during the COVID-19 pandemic, suggesting that resilience and resilient coping may be particularly relevant for health behaviors during an ongoing, collective stressor.
Some ways in which resilience and coping may influence health behaviors like diet and physical activity are through meaning-making, self-efficacy, and effective use of resources—skills or processes that individuals may have relied on during prior instances of trauma as well (Choi et al., 2023). As noted in our theoretical model based on Krok et al. (Krok et al., 2023), meaning-making can help re-frame negative experiences and promote positive health behaviors.
The finding that observed associations were stronger among participants interviewed during the COVID-19 pandemic points to the unique nature of this protracted, collective stressor. The pandemic led to strict lockdown policies that affected behaviors for many people, for example the closing of gyms and social gathering spaces, in addition to limited supermarket access (Du et al., 2021, Knell et al., 2020). Given this unique and unprecedented situation, participants may have had to utilize coping skills and resilience more strongly than before the pandemic. Furthermore, coping and resilience themselves can change over time and may be situation-dependent (Nielsen and Knardahl, 2014, Stewart and Schwarzer, 1996), and thus may be activated or enhanced during extremely stressful periods. However, it is important to note that these stratified analyses compared two different groups of individuals interviewed at different times. Given the lack of longitudinal data, we could not assess changes over time within the same individuals.
The unique context of Puerto Rico adds nuance to the observed relationships. The political and economic colonialism and oppression that the population has faced for more than a century, on top of individual trauma, undoubtedly shape resilience and behaviors (Marín and Marín, 1991, Rodríguez-Madera et al., 2021). Additionally, the island has faced numerous challenges including natural disasters, which have further tested the resilience of its residents (Rodríguez-Madera et al., 2021). At the same time, there is a strong cultural history, identity, and a sense of community that may buffer some trauma, promote greater resilience, and influence health behaviors (Gallo et al., 2009, Marín and Marín, 1991, Petrun Sayers et al., 2023). Thus, the community's cohesion and cultural history may serve as protective factors against the negative impacts of stressors on health behaviors. This sense of belonging and shared identity may foster support networks and encourage healthier coping mechanisms among individuals (Idalí Torres et al., 2008, Ramos-Olazagasti et al., 2013).
Despite differences in populations and context, results from our study are consistent with findings in other populations, including a study of older US women from the Women’s Health Initiative (WHI), which found that higher resilience was associated with better quality diet, recommended physical activity, and 7–9 h of sleep per night, with estimates of similar magnitude to those found here (Springfield et al., 2020). The WHI study also found a null relationship between resilience and smoking status, consistent with ours. However, unlike in their study, we did not observe an association between higher resilience and moderate (non-heavy) alcohol use. This could be because moderate or non-heavy alcohol use was defined differently across the two studies, or because our study included both men and women, or because the WHI data were collected before COVID-19. Importantly, when we adjusted for loneliness and social support, we did not see large changes in these results, even though individuals who socialize frequently may report higher resilience and consume more alcohol (Sudhinaraset et al., 2016). One potential reason for the null relationships we observed between resilience/resilient coping and smoking could be the relative stability of smoking patterns over time compared to other behaviors; smoking may not be as responsive to stressful events and resulting resilience, particularly for individuals without a smoking history, which comprised most of our sample. Moreover, individuals may consider smoking or alcohol use to be forms of coping (Park & Iacocca, 2014) and, therefore, may rate themselves higher on resilient coping, even though the BRCS aims to measure psychological coping strategies rather than broader coping behaviors. The absence of clear associations with smoking status and alcohol use could also suggest that additional factors, such as cultural norms and individual histories, may influence these behaviors differently within this context.
Future directions include assessing longitudinal relationships between resilience and resilient coping with physical health outcomes such as cardiometabolic factors, with potential mediation by the health behaviors assessed here. Extending these findings to other communities vulnerable to multiple societal traumas would also be useful. Furthermore, although resilience manifests at the individual level, it is not necessarily an individual trait or characteristic; many contextual level factors may relate to or help define ultimate resilience (Park et al., 2022). Future work should therefore seek to understand contextual factors that ultimately lead to certain individuals and populations demonstrating high resilience. A deeper understanding of the complexities of Puerto Rico's socio-cultural context could enrich our interpretation of the study findings, highlighting the interplay between historical, cultural, and environmental factors in shaping resilience, coping, and health behaviors among its residents. It is also important not to overly promote the idea of resilience to the point of encouraging individuals to “stay strong” at all times throughout multiple adversities, which can deplete reserves; this idea has been termed a hidden “cost” of resilience (De France et al., 2022, Suslovic and Lett, 2023).
There are some limitations to our study. First, this analysis was cross-sectional, so we cannot disentangle whether resilience and coping preceded health behaviors; these relationships may be reciprocal, as indicated in other studies (Segovia et al., 2013, Windle, 2012, Wister et al., 2022). Future work should assess health behaviors with repeated measures to understand longitudinal and longer-term effects. Second, selection bias may have resulted from our recruitment; individuals who enrolled in the study may be healthier or more interested in health and may report greater psychological resilience than the general population of Puerto Rico. Although our multi-prong sampling design included probabilistic household sampling through census blocks, this process proved to be less fruitful than initially anticipated, given outdated Census data and several vacant and unresponsive households, largely due to the destructive 2017 hurricanes (Mattei et al., 2021). Third, we could not account specifically for recent individual traumatic and stressful events (outside the context of the recent hurricanes), which likely affected self-rated resilience, resilient coping, and health behaviors. However, for this study, we were primarily interested in the relationship between these variables in the context of collective, widespread trauma. Finally, misclassification of variables is a potential limitation in this study, given that they were all self-reported. Our use of validated measures reduces this limitation.
To sum, we found consistent relationships between resilience and resilient coping with three health behaviors that are strongly linked to conditions like type 2 diabetes and cardiovascular disease. Our results suggest practical public health implications, including assessing resilience in communities that are vulnerable to disasters or other negative events to gauge their level of preparedness before disasters occur, and leveraging or strengthening population-level resilience for disaster preparation and response. For example, programs that generate social connectedness or rempower people’s sense of control or cohesion during an event may benefit both resilience and healthy behaviors, in addition to established post-disaster interventions like Psychological First Aid (Hobfoll et al., 2008, Sandifer and Walker, 2018). Ultimately, given Puerto Rico’s susceptibility to adversity and the already high prevalence of chronic health conditions (Mattei et al., 2018), identifying supportive strategies to build and maintain resilience and resilient coping mechanisms in Puerto Rico may contribute to better cardiovascular health over the life course.
Funding
This study was supported by the US National Institutes of Health’s National Heart Lung and Blood Institute (R01 HL143792 to JM) and National Institute on Minority Health and Health Disparities (R21 MD013650 to JM) as well as a Robert Wood Johnson Foundation Culture of Health Leaders Award (to JM). L Sampson and M Tamez were supported by the National Institutes of Health grant T32 HL098048. Additional support in community engagement was received from the Hispanic Alliance for Clinical and Translational Research (Alliance), National Institute of General Medical Sciences, National Institutes of Health (U54GM133807). These funding sources were not involved in the research.
CRediT authorship contribution statement
Laura Sampson: Writing – original draft, Methodology, Formal analysis, Conceptualization. Ariel H. Kim: Writing – review & editing, Formal analysis. H. June O’Neill: Writing – review & editing, Formal analysis. Martha Tamez: Writing – review & editing, Formal analysis. Luis M. Falcon: . Katherine L. Tucker: Writing – review & editing, Investigation. Edna Acosta-Pérez: Writing – review & editing, Investigation. Jose F. Rodriguez Orengo: Writing – review & editing, Investigation. Laura D. Kubzansky: Writing – review & editing, Investigation, Writing – review & editing, Conceptualization. Karestan C. Koenen: . Josiemer Mattei: Writing – review & editing, Supervision, Project administration, Investigation, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Dr. Koenen has been a paid consultant in the past three years for the US Department of Justice and Covington and Burling, LLP. She receives royalties from Guilford Press and Oxford University Press. Dr. Kubzansky receives royalties from Oxford University Press. The other authors have no competing interests to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2024.102874.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Avila M., Lucchetti A., Lucchetti G. Association between depression and resilience in older adults: a systematic review and meta-analysis. Int. J. Geriatr. Psychiatry. 2017;32(3):237–246. doi: 10.1002/GPS.4619. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Diminich E.D. Annual Research Review: Positive adjustment to adversity–trajectories of minimal-impact resilience and emergent resilience. J. Child Psychol. Psychiatry. 2013;54(4):378–401. doi: 10.1111/JCPP.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Galea S., Bucciarelli A., Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychol. Sci. 2006;17(3):181–186. doi: 10.1111/J.1467-9280.2006.01682.X. [DOI] [PubMed] [Google Scholar]
- Brief Resilient Coping Scale (BRCS). Lee Kum Sheung Center for Health and Happiness. Harvard T.H. Chan School of Public Health. (n.d.). Retrieved June 15, 2023, from https://www.hsph.harvard.edu/health-happiness/brief-resilient-coping-scale-brcs/.
- Cal S.F., de Sá L.R., Glustak M.E., Santiago M.B. Resilience in chronic diseases: A systematic review. Cogent Psychology. 2015;2(1):1024928. doi: 10.1080/23311908.2015.1024928. [DOI] [Google Scholar]
- Cappuccio F.P., D’Elia L., Strazzullo P., Miller M.A. Sleep Duration and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. Sleep. 2010;33(5):585. doi: 10.1093/SLEEP/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput J.P., Dutil C., Featherstone R., Ross R., Giangregorio L., Saunders T.J., Janssen I., Poitras V.J., Kho M.E., Ross-White A., Carrier J. Sleep duration and health in adults: an overview of systematic reviews. Applied Physiology, Nutrition, and Metabolism = Physiologie Appliquee, Nutrition et Metabolisme. 2020;45(10):S218–S231. doi: 10.1139/APNM-2020-0034/SUPPL_FILE/APNM-2020-0034SUPPLB.DOCX. [DOI] [PubMed] [Google Scholar]
- Choi J., Choi J.Y., Lee S.A., Lee K.M., Shin A., Oh J., Park J., Song M., Yang J.J., Lee J.K., Kang D. Association between family history of diabetes and clusters of adherence to healthy behaviors: cross-sectional results from the Health Examinees-Gem (HEXA-G) study. BMJ Open. 2019;9(6):25477. doi: 10.1136/BMJOPEN-2018-025477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K.W., Nishimi K., Jha S.C., Sampson L., Hahn J., Kang J.H., Koenen K.C., Kubzansky L.D. Pre-pandemic resilience to trauma and mental health outcomes during COVID-19. Soc. Psychiatry Psychiatr. Epidemiol. 2023;58(3):453. doi: 10.1007/S00127-022-02367-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- De France K., Evans G.W., Brody G.H., Doan S.N. Cost of resilience: Childhood poverty, mental health, and chronic physiological stress. Psychoneuroendocrinology. 2022;144 doi: 10.1016/J.PSYNEUEN.2022.105872. [DOI] [PubMed] [Google Scholar]
- Du C., Zan M.C.H., Cho M.J., Fenton J.I., Hsiao P.Y., Hsiao R., Keaver L., Lai C.C., Lee H., Ludy M.J., Shen W., Swee W.C.S., Thrivikraman J., Tseng K.W., Tseng W.C., Doak S., Folk S.Y.L., Tucker R.M. The Effects of Sleep Quality and Resilience on Perceived Stress, Dietary Behaviors, and Alcohol Misuse: A Mediation-Moderation Analysis of Higher Education Students from Asia, Europe, and North America during the COVID-19 Pandemic. Nutrients. 2021;13(2):1–22. doi: 10.3390/NU13020442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenman D.P., Gelberg L., Liu H., Shapiro M.F. Mental health and health-related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. JAMA. 2003;290(5):627–634. doi: 10.1001/JAMA.290.5.627. [DOI] [PubMed] [Google Scholar]
- Ezell J.M., Salari S., Rooker C., Chase E.C. Intersectional trauma: COVID-19, the psychosocial contract, and America’s racialized public health lineage. Traumatology. 2021;27(1):78. doi: 10.1037/TRM0000302. [DOI] [Google Scholar]
- Falcon L.M., Todorova I., Tucker K. Social Support, Life Events and Psychological Distress among the Puerto Rican Population in the Boston area of the United States. Aging Ment. Health. 2009;13(6):863. doi: 10.1080/13607860903046552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falcón L.M., Tucker K.L. Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. The Journals of Gerontology. Series b, Psychological Sciences and Social Sciences. 2000;55(2) doi: 10.1093/GERONB/55.2.S108. [DOI] [PubMed] [Google Scholar]
- Gallo L.C., Penedo F.J., De Los E., Monteros K., Arguelles W. Resiliency in the Face of Disadvantage: Do Hispanic Cultural Characteristics Protect Health Outcomes? J. Pers. 2009;77(6):1707–1746. doi: 10.1111/J.1467-6494.2009.00598.X. [DOI] [PubMed] [Google Scholar]
- Garciá C., Rivera F.I., Garcia M.A., Burgos G., Aranda M.P. Contextualizing the COVID-19 Era in Puerto Rico: Compounding Disasters and Parallel Pandemics. The Journals of Gerontology: Series B. 2021;76(7):e263–e267. doi: 10.1093/GERONB/GBAA186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Campayo J., Zamorano E., Ruiz M.A., Pardo A., Pérez-Páramo M., López-Gómez V., Freire O., Rejas J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual. Life Outcomes. 2010;8:8. doi: 10.1186/1477-7525-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg A., Vora K.S., Ali M.K., Kondal D., Deepa M., Staimez L.R., Kadir M.M., Mohan V., Tandon N., Shivashankar R. Association of family history of cardiometabolic diseases (CMDs) and individual health behaviours: Analysis of CARRS study from South Asia. Indian Heart J. 2022;74(4):307–313. doi: 10.1016/J.IHJ.2022.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González P., Nuñez A., Merz E., Brintz C., Weitzman O., Navas E.L., Camacho A., Buelna C., Penedo F.J., Wassertheil-Smoller S., Perreira K., Isasi C.R., Choca J., Talavera G.A., Gallo L.C. Measurement Properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): Findings from HCHS/SOL. Psychol. Assess. 2017;29(4):372. doi: 10.1037/PAS0000330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernádez-Torres R., Martínez M., Id L., Torres I., Rosario-Herná Ndezid E., Ramos-Pibernusid A., Sotoid A., Ortiz L., Mascayano F., Rivera-Segarraid E. The impact of the Covid-19 pandemic and previous natural disasters on the mental health of healthcare workers in Puerto Rico. PLOS Global Public Health. 2023;3(5):e0001784. doi: 10.1371/journal.pgph.0001784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll S.E., Watson P., Bell C.C., Bryant R.A., Brymer M.J., Friedman M.J., Friedman M., Gersons B.P.R., De Jong J.T.V.M., Layne C.M., Maguen S., Neria Y., Norwood A.E., Pynoos R.S., Reissman D., Ruzek J.I., Shalev A.Y., Solomon Z., Steinberg A.M., Ursano R.J. Five Essential Elements of Immediate and mid-Term Mass Trauma Intervention: Empirical Evidence. Https://doi.org/10.1521/psyc.2007.70.4.283. 2008;70(4):283–315. doi: 10.1521/PSYC.2007.70.4.283. [DOI] [PubMed] [Google Scholar]
- Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C., Jones L., Dunne M.P. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res. Aging. 2004;26(6):655. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idalí Torres M., Marquez D.X., Carbone E.T., Stacciarini J.M.R., Foster J.W. Culturally responsive health promotion in puerto rican communities: a structuralist approach. Health Promot. Pract. 2008;9(2):149–158. doi: 10.1177/1524839907307675. [DOI] [PubMed] [Google Scholar]
- Jacobs S., Boushey C.J., Franke A.A., Shvetsov Y.B., Monroe K.R., Haiman C.A., Kolonel L.N., Le Marchand L., Maskarinec G. A priori-defined diet quality indices, biomarkers and risk for type 2 diabetes in five ethnic groups: the Multiethnic Cohort. Br. J. Nutr. 2017;118(4):312–320. doi: 10.1017/S0007114517002033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jike M., Itani O., Watanabe N., Buysse D.J., Kaneita Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 2018;39:25–36. doi: 10.1016/J.SMRV.2017.06.011. [DOI] [PubMed] [Google Scholar]
- Knell G., Robertson M.C., Dooley E.E., Burford K., Mendez K.S. Health Behavior Changes During COVID-19 Pandemic and Subsequent “Stay-at-Home” Orders. Int. J. Environ. Res. Public Health. 2020;17(17):1–16. doi: 10.3390/IJERPH17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krok, D., Telka, E., Szcześniak, M., & Falewicz, A. (2023). Threat Appraisal, Resilience, and Health Behaviors in Recovered COVID-19 Patients: The Serial Mediation of Coping and Meaning-Making. International Journal of Environmental Research and Public Health 2023, Vol. 20, Page 3649, 20(4), 3649. https://doi.org/10.3390/IJERPH20043649. [DOI] [PMC free article] [PubMed]
- Lang A.J., Stein M.B. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav. Res. Ther. 2005;43(5):585–594. doi: 10.1016/J.BRAT.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Lantz P.M., House J.S., Mero R.P., Williams D.R. Stress, life events, and socioeconomic disparities in health: results from the Americans’ Changing Lives Study. J. Health Soc. Behav. 2005;46(3):274–288. doi: 10.1177/002214650504600305. [DOI] [PubMed] [Google Scholar]
- Li Y., Zhang X., Winkelman J.W., Redline S., Hu F.B., Stampfer M., Ma J., Gao X. The Association between Insomnia Symptoms and Mortality: A Prospective Study of US Men. Circulation. 2014;129(7):737. doi: 10.1161/CIRCULATIONAHA.113.004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limonero J.T., Tomás-Sábado J., Gómez-Romero M.J., Maté-Méndez J., Sinclair V.G., Wallston K.A., Gómez-Benito J. Evidence for validity of the brief resilient coping scale in a young Spanish sample. Span. J. Psychol. 2014;17(2) doi: 10.1017/SJP.2014.35. [DOI] [PubMed] [Google Scholar]
- Llibre-Guerra J.J., Jiménez-Velázquez I.Z., Llibre-Rodriguez J.J., Acosta D. The impact of COVID-19 on mental health in the Hispanic Caribbean region. Int. Psychogeriatr. 2020;32(10):1143–1146. doi: 10.1017/S1041610220000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Cepero A., O’Neill H.J., Marrero A., Falcon L.M., Tamez M., Rodríguez-Orengo J.F., Mattei J. Association between adverse experiences during Hurricane María and mental and emotional distress among adults in Puerto Rico. Soc. Psychiatry Psychiatr. Epidemiol. 2022;57(12):2423. doi: 10.1007/S00127-022-02355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care. 2008;46(3):266–274. doi: 10.1097/MLR.0B013E318160D093. [DOI] [PubMed] [Google Scholar]
- Luthar S.S., Cicchetti D., Becker B. The Construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margerison-Zilko C., Goldman-Mellor S., Falconi A., Downing J. Health Impacts of the Great Recession: A Critical Review. CurrentEpidemiology Reports. 2016;3(1):81. doi: 10.1007/S40471-016-0068-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín G., Marín B.V. Sage Publications Inc.; 1991. Research with Hispanic populations. [Google Scholar]
- Marrero A., Lόpez-Cepero A., Borges-Méndez R., Mattei J. Narrating agricultural resilience after Hurricane María: how smallholder farmers in Puerto Rico leverage self-sufficiency and collaborative agency in a climate-vulnerable food system. Agric. Hum. Values. 2022;39(2):555–571. doi: 10.1007/S10460-021-10267-1/METRICS. [DOI] [Google Scholar]
- Mattei, J., Tucker, K. L., Falcón, L. M., Ríos-Bedoya, C. F., Kaplan, R. M., O’neill, H. J., Tamez, M., Mendoza, S., Díaz-Álvarez, C. B., Orozco, J. E., Acosta Pérez, E., & Rodríguez-Orengo, J. F. (2021). Design and Implementation of the Puerto Rico Observational Study of Psychosocial, Environmental, and Chronic Disease Trends (PROSPECT). Am J Epidemiol, 190(5), 707–717. https://doi.org/10.1093/aje/kwaa231. [DOI] [PMC free article] [PubMed]
- Mattei J., Tamez M., Ríos-Bedoya C.F., Xiao R.S., Tucker K.L., Rodríguez-Orengo J.F. Health conditions and lifestyle risk factors of adults living in Puerto Rico: A cross-sectional study. BMC Public Health. 2018;18(1):1–12. doi: 10.1186/S12889-018-5359-Z/FIGURES/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei J., Tamez M., O’Neill J., Haneuse S., Mendoza S., Orozco J., Lopez-Cepero A., Ríos-Bedoya C.F., Falcón L.M., Tucker K.L., Rodríguez-Orengo J.F. Chronic Diseases and Associated Risk Factors Among Adults in Puerto Rico After Hurricane Maria. JAMA Netw. Open. 2022;5(1):e2139986–e. doi: 10.1001/JAMANETWORKOPEN.2021.39986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough M.L., Willett W.C. Evaluating adherence to recommended diets in adults: the Alternate Healthy Eating Index. Public Health Nutr. 2006;9(1A):152–157. doi: 10.1079/phn2005938. [DOI] [PubMed] [Google Scholar]
- Merz E.L., Roesch S.C., Malcarne V.L., Penedo F.J., Llabre M.M., Weitzman O.B., Navas-Nacher E.L., Perreira K.M., Gonzalez F., Ponguta L.A., Johnson T.P., Gallo L.C. Validation of Interpersonal Support Evaluation List-12 (ISEL-12) scores among English- and Spanish-Speaking Hispanics/Latinos from the HCHS/SOL Sociocultural Ancillary Study. Psychol. Assess. 2014;26(2):384. doi: 10.1037/A0035248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen M.B., Knardahl S. Coping strategies: A prospective study of patterns, stability, and relationships with psychological distress. Scand. J. Psychol. 2014;55(2):142–150. doi: 10.1111/SJOP.12103. [DOI] [PubMed] [Google Scholar]
- Nishimi K.M., Koenen K.C., Coull B.A., Kubzansky L.D. Association of Psychological Resilience with Healthy Lifestyle and Body Weight in Young Adulthood. J. Adolesc. Health. 2022;70(2):258. doi: 10.1016/J.JADOHEALTH.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paffenbarger R.S., Wing A.L., Hyde R.T. Physical activity as an index of heart attack risk in college alumni. Am. J. Epidemiol. 1978;108(3):161–175. doi: 10.1093/OXFORDJOURNALS.AJE.A112608. [DOI] [PubMed] [Google Scholar]
- Paffenbarger R.S., Hyde R.T., Wing A.L., Lee I.-M., Jung D.L., Kampert J.B. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N. Engl. J. Med. 1993;328(8):538–545. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- Palacios C., Trak M.A., Betancourt J., Joshipura K., Tucker K.L. Validation and reproducibility of a semi-quantitative FFQ as a measure of dietary intake in adults from Puerto Rico. Public Health Nutr. 2015;18(14):2550–2558. doi: 10.1017/S1368980014003218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C.L., Iacocca M.O. A stress and coping perspective on health behaviors: theoretical and methodological considerations. Anxiety Stress Coping. 2014;27(2):123–137. doi: 10.1080/10615806.2013.860969. [DOI] [PubMed] [Google Scholar]
- Park J.W., Mealy R., Saldanha I.J., Loucks E.B., Needham B.L., Sims M., Fava J.L., Dulin A.J., Howe C.J. Multilevel resilience resources and cardiovascular disease in the United States: A systematic review and meta-analysis. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association. 2022;41(4):278–290. doi: 10.1037/HEA0001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera M.J., Brintz C.E., Birnbaum-Weitzman O., Penedo F.J., Gallo L.C., Gonzalez P., Gouskova N., Isasi C.R., Navas-Nacher E.L., Perreira K.M., Roesch S.C., Schneiderman N., Llabre M.M. Factor Structure of the Perceived Stress Scale-10 (PSS) Across English and Spanish Language Responders in the HCHS/SOL Sociocultural Ancillary Study. Psychol. Assess. 2017;29(3):320. doi: 10.1037/PAS0000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrun Sayers E.L., Anthony K.E., Tom A., Kim A.Y., Armstrong C. ‘We will rise no matter what’: community perspectives of disaster resilience following Hurricanes Irma and Maria in Puerto Rico. J. Appl. Commun. Res. 2023;51(2):126–145. doi: 10.1080/00909882.2022.2069473. [DOI] [Google Scholar]
- Pietrzak R.H., Goldstein R.B., Southwick S.M., Grant B.F. Physical Health Conditions Associated with Posttraumatic Stress Disorder in U.S. Older Adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J. Am. Geriatr. Soc. 2012;60(2):296. doi: 10.1111/J.1532-5415.2011.03788.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak R.H., Tracy M., Galea S., Kilpatrick D.G., Ruggiero K.J., Hamblen J.L., Southwick S.M., Norris F.H. Resilience in the face of disaster: Prevalence and longitudinal course of mental disorders following Hurricane Ike. PLoS One. 2012;7(6) doi: 10.1371/JOURNAL.PONE.0038964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Previdi I.L., Vega C.M.V. Health Disparities Research Framework Adaptation to Reflect Puerto Rico’s Socio-Cultural Context. Int. J. Environ. Res. Public Health. 2020;17(22):1–11. doi: 10.3390/IJERPH17228544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977;1(3):385–401. [Google Scholar]
- Ramos-Olazagasti M.A., Shrout P.E., Yoshikawa H., Canino G.J., Bird H.R. Contextual Risk and Promotive Processes in Puerto Rican Youths’ Internalizing Trajectories in Puerto Rico and New York. Dev. Psychopathol. 2013;25(3):755. doi: 10.1017/S0954579413000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich J.W. Three psychological principles of resilience in natural disasters. Disaster Prevention and Management: an International Journal. 2006;15(5):793–798. doi: 10.1108/09653560610712739/FULL/PDF. [DOI] [Google Scholar]
- Robert M., Shankland R., Bellicha A., Kesse-Guyot E., Deschasaux-Tanguy M., Andreeva V.A., Srour B., Hercberg S., Touvier M., Leys C., Péneau S. Associations between Resilience and Food Intake Are Mediated by Emotional Eating in the NutriNet-Santé Study. J. Nutr. 2022;152(8):1907–1915. doi: 10.1093/JN/NXAC124. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Madera S.L., Varas-Díaz N., Padilla M., Grove K., Rivera-Bustelo K., Ramos J., Contreras-Ramirez V., Rivera-Rodríguez S., Vargas-Molina R., Santini J. The impact of Hurricane Maria on Puerto Rico’s health system: post-disaster perceptions and experiences of health care providers and administrators. Global Health Research and Policy. 2021;6(1):1–11. doi: 10.1186/S41256-021-00228-W/TABLES/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Rey R., Alonso-Tapia J., Hernansaiz-Garrido H. Reliability and validity of the Brief Resilience Scale (BRS) Spanish Version. Psychol. Assess. 2016;28(5):e101–e110. doi: 10.1037/PAS0000191. [DOI] [PubMed] [Google Scholar]
- Saint Onge J.M., Krueger P.M. Health lifestyle behaviors among U.S. adults. SSM - Population Health. 2017;3:89–98. doi: 10.1016/J.SSMPH.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandifer P.A., Walker A.H. Enhancing disaster resilience by reducing stress-associated health impacts. Front. Public Health. 2018;6(DEC) doi: 10.3389/FPUBH.2018.00373/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarason I.G., Sarason B.R., editors. Social Support: Theory. Martinus Nijhoff Publishers; Research and Applications: 1985. [Google Scholar]
- Sato M., Horner P.S., Vélez Ortiz D., Nelson A. The role of spirituality in family adjustment and resilience among Puerto Rican families post-Hurricane Maria. J. Relig. Spiritual. Soc. Work Soc. Thought. 2022;41(1):90–103. doi: 10.1080/15426432.2021.2000553. [DOI] [Google Scholar]
- Scaramutti C., Salas-Wright C.P., Vos S.R., Schwartz S.J. The Mental Health Impact of Hurricane Maria on Puerto Ricans in Puerto Rico and Florida. Disaster Med. Public Health Prep. 2019;13(1):24–27. doi: 10.1017/DMP.2018.151. [DOI] [PubMed] [Google Scholar]
- Segovia F., Moore J.L., Linnville S., Hoyt R.E., Hain R.E. Sleep and Resilience: A Longitudinal 37-Year Follow-up Study of Vietnam Repatriated Prisoners of War. Mil. Med. 2013;178(2):196–201. doi: 10.7205/MILMED-D-12-00227. [DOI] [PubMed] [Google Scholar]
- Sinclair V.G., Wallston K.A. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment. 2004;11(1):94–101. doi: 10.1177/1073191103258144. [DOI] [PubMed] [Google Scholar]
- Smith, B. W., Epstein, E. M., Ortiz, J. A., Christopher, P. J., & Tooley, E. M. (2013). The Foundations of Resilience: What Are the Critical Resources for Bouncing Back from Stress? 167–187. https://doi.org/10.1007/978-1-4614-4939-3_13.
- Sotos-Prieto M., Bhupathiraju S.N., Falcón L.M., Gao X., Tucker K.L., Mattei J. A Healthy Lifestyle Score Is Associated with Cardiometabolic and Neuroendocrine Risk Factors among Puerto Rican Adults. J. Nutr. 2015;145(7):1531. doi: 10.3945/JN.114.206391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/ARCHINTE.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Springfield S., Qin F., Hedlin H., Eaton C.B., Rosal M.C., Taylor H., Staudinger U.M., Stefanick M.L. Resilience and CVD-protective health behaviors in older women: Examining racial and ethnic differences in a cross-sectional analysis of the women’s health initiative. Nutrients. 2020;12(7):1–18. doi: 10.3390/nu12072107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart S.M., Schwarzer R. Stability of coping in Hong Kong medical students: a longitudinal study. Pers. Individ. Differ. 1996;20(2):245–255. doi: 10.1016/0191-8869(95)00162-X. [DOI] [Google Scholar]
- Sudhinaraset M., Wigglesworth C., Takeuchi D.T. Social and Cultural Contexts of Alcohol Use: Influences in a Social-Ecological Framework. Alcohol Res. 2016;38(1):35. /pmc/articles/PMC4872611/ [PMC free article] [PubMed] [Google Scholar]
- Suslovic B., Lett E. Resilience is an Adverse Event: A Critical Discussion of Resilience Theory in Health Services Research and Public Health. Https://Doi.Org/10.1177/2752535X231159721. 2023;2752535X2311597 doi: 10.1177/2752535X231159721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E., Stanton A.L. Coping Resources, Coping Processes, and Mental Health. Https://Doi.Org/10.1146/Annurev.Clinpsy.3.022806.091520. 2007;3:377–401. doi: 10.1146/ANNUREV.CLINPSY.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- The impact of climate change on the rights of people in vulnerable situations. OHCHR, United Nations. (n.d.). Retrieved December 7, 2023, from https://www.ohchr.org/en/climate-change/impact-climate-change-rights-people-vulnerable-situations.
- To Q.G., Vandelanotte C., Cope K., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., Fenning A.S., Stanton R. The association of resilience with depression, anxiety, stress and physical activity during the COVID-19 pandemic. BMC Public Health. 2022;22(1):1–8. doi: 10.1186/S12889-022-12911-9/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker K.L., Bianchi L.A., Maras J., Bermudez O.I. Adaptation of a Food Frequency Questionnaire to Assess Diets of Puerto Rican and Non-Hispanic Adults. Am. J. Epidemiol. 1998;148(5):507–518. doi: 10.1093/oxfordjournals.aje.a009676. [DOI] [PubMed] [Google Scholar]
- Tucker K.L., Mattei J., Noel S.E., Collado B.M., Mendez J., Nelson J., Griffith J., Ordovas J.M., Falcon L.M. The Boston Puerto Rican Health Study, a longitudinal cohort study on health disparities in Puerto Rican adults: challenges and opportunities. BMC Public Health. 2010;10:107. doi: 10.1186/1471-2458-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh J.L., Senn T.E., Carey M.P. Longitudinal associations between health behaviors and mental health in low-income adults. Transl. Behav. Med. 2013;3(1):104–113. doi: 10.1007/S13142-012-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzel E.C., Löbner M., Glaesmer H., Hinz A., Zeynalova S., Henger S., Engel C., Reyes N., Wirkner K., Löffler M., Riedel-Heller S.G. The Association of Resilience with Mental Health in a Large Population-Based Sample (LIFE-Adult-Study) Int. J. Environ. Res. Public Health. 2022;19(23) doi: 10.3390/IJERPH192315944/S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Medlock M.M. Health Effects of Dramatic Societal Events — Ramifications of the Recent Presidential Election. N. Engl. J. Med. 2017;376(23):2295–2299. doi: 10.1056/NEJMMS1702111/SUPPL_FILE/NEJMMS1702111_DISCLOSURES.PDF. [DOI] [PubMed] [Google Scholar]
- Windle G. The contribution of resilience to healthy ageing. Perspect. Public Health. 2012;132(4):159–160. doi: 10.1177/1757913912449572. [DOI] [PubMed] [Google Scholar]
- Wister A., Li L., Whitmore C., Ferris J., Klasa K., Linkov I. Multimorbidity resilience and health behaviors among older adults: A longitudinal study using the Canadian Longitudinal Study on Aging. Front. Public Health. 2022;10 doi: 10.3389/FPUBH.2022.896312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yabe T., Rao P.S.C., Ukkusuri S.V. Regional differences in resilience of social and physical systems: Case study of Puerto Rico after Hurricane Maria. Environment and Planning b: Urban Analytics and City Science. 2021;48(5):1042–1057. doi: 10.1177/2399808320980744/ASSET/IMAGES/LARGE/10.1177_2399808320980744-FIG5.JPEG. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.