Abstract
Aspergillosis is a vicious fungal infection that can develop in immunosuppressed patients. The presence of aspergillosis in the ureter or elsewhere in the genito-urinary tract is highly uncommon and rarely reported in the literature. Here, we present a 54-year-old gentleman, with uncontrolled diabetes, who presented with urosepsis. Right hydronephrosis and ureteric stricture with urinary extravasation were seen on imaging. Right percutaneous nephrostomy was done, with drainage and analysis of the pus revealing the growth of Aspergillus fumigatus species. On open exploration, a ureteric abscess cavity, which was adherent to the duodenum, was drained and uretero-ureterostomy along with feeding jejunostomy was performed. Histopathological examination and special staining confirmed the growth of aspergillosis. The patient was treated with antifungal agents and responded well with an uneventful post-operative recovery.
Keywords: liposomal amphotericin b, invasive aspergillosis, immunocompromised hosts, ureteral aspergillosis, ureterectomy, double-j stent, voriconazole therapy, ureteric stricture, feeding jejunostomy
Introduction
Aspergillosis is a vicious fungal infection that is known to develop in immunosuppressed patients. Commonly occurring in lungs, the presence of aspergillosis in the ureter or elsewhere in the genito-urinary tract is uncommon and rarely reported in the literature [1]. The diagnosis and treatment of the disease are challenging owing to the poor concentration of antifungal agents in the urine [2]. Prompt recognition and an early initiation of therapy can reduce the associated morbidity and mortality drastically. We present a case of a 54-year-old male with isolated invasive aspergillosis of the ureter along with urosepsis and ureteric obstruction. Despite a turbulent course of treatment, the patient responded well after urinary diversion, supported by adequate antifungal therapy.
Case presentation
A 54-year-old gentleman, with uncontrolled diabetes mellitus for 25 years, presented with fever and right loin pain for five days. He had an associated history of passing turbid and foul-smelling urine. No history of hematuria or other urinary symptoms was noted. No other systemic illnesses were present. He had a history of left percutaneous nephrolithotripsy for left renal calculus five years back as well as a history of spine stabilization surgery done one year back. Later, he was admitted twice with urosepsis with bilateral hydroureteronephrosis for which he underwent bilateral ureteroscopy which showed extensive papillary necrosis on both sides. Hence, he was taken up twice for bilateral ureteric stenting followed by subsequent stent removals 6 months back. On examination, the patient was found to be febrile with severe tenderness over the right loin.
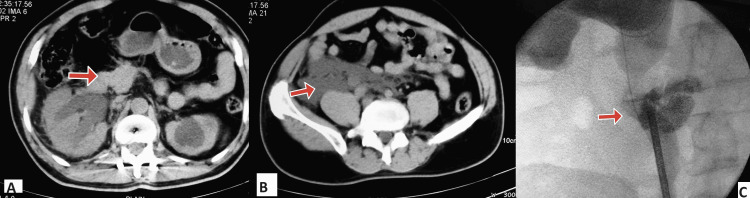
Blood investigations revealed a rise in the total leucocyte count of 18,200 cells/cu mm (normal range: 5,000-11,000 cells/cu mm), due to the prevailing infection and inflammation. His creatinine was found to be 3.2 mg/dl (normal range: 0.7 - 1.2 mg/dl) attributing to an obstructive uropathy. Urine culture revealed the growth of Aspergillus fumigatus species. Ultrasound and non-contrast computed tomography (CT) of the abdomen were done and showed right hydroureteronephrosis and urine extravasation in the upper ureter as shown in Figures 1A, 1B.
Figure 1. Computed tomography images with axial cuts showing (A) right hydronephrosis with (B) urinary extravasation. (C) Retrograde pyelogram (antero-posterior view) showing extravasation of contrast, as marked by the arrows.
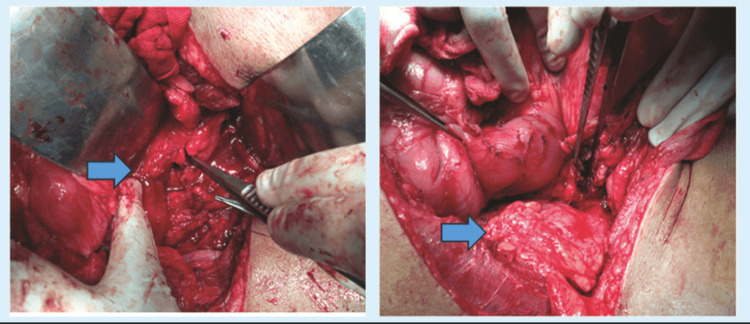
He was subjected to right percutaneous nephrostomy (PCN) and retrograde pyelogram, which showed contrast extravasation in the lower ureter, as shown in Figure 1C. Purulent drainage of around 2000 ml/day was noted from the PCN while the patient was passing clear and adequate amount of urine via the urethra. Urine culture showed growth of fungal elements. Hence, the patient was kept under an antifungal cover of intravenous amphotericin. Post drainage, the serum creatinine dropped from 3.7 mg/dl to 1.3 mg/dl. The patient was then evaluated and taken for open exploration of the right ureter. A dilated upper ureter with a lower half stricture leading to an abscess cavity was noted, which was adherent to the wall of the second part of the duodenum. Hence, the stricture segment of the ureter was resected and the abscess cavity was drained followed by uretero-ureterostomy and feeding jejunostomy as shown in Figure 2. A double J (DJ) ureteral stent was placed across the anastomosis site.
Figure 2. Intraoperative images showing intra-abdominal (A) ureteral abscess cavity adherent with duodenum and (B) Omental wrapping around the anastomosis site and intact dissected duodenum, as marked by the arrows.
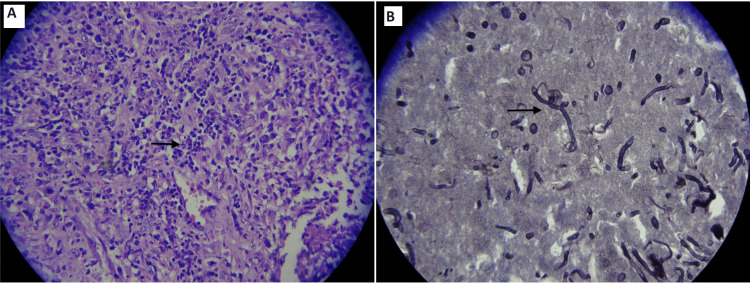
The histopathological examination (HPE) report showed an acute or chronic inflammation in the ureteric stricture segment. The abscess cavity was found to show necrosis with mixed inflammation and fungal elements suggestive of invasive aspergillosis. Culture revealed the growth of Aspergillus fumigatus, which was resistant to fluconazole. Gomori methanamine silver (GMS) stain, the special stain for detecting fungal elements, was found to be positive as well, as shown in Figure 3.
Figure 3. (A) Histopathological examination showing few isolated hyphae-like structures with narrow septae and acute angular branching. (B) Gomori methanamine silver (GMS) stain detecting Aspergillus fungal hyphae (100x, GMS stain).
Postoperatively, the patient had an uneventful stay. After the HPE report, the patient was maintained on oral voriconazole 200mg twice daily for three months. After six weeks, urine culture revealed no growth after which DJ stent removal was done. The patient improved significantly during the follow-up period.
Discussion
Aspergillus is a filamentous fungus isolated from air, soil, decaying vegetables, or dust. The most common variants of Aspergillus involved are Aspergillus fumigatus and Aspergillus flavus. Mortality associated with systemic aspergillus infection is around 40 to 50%, while the mortality associated with genitourinary aspergillosis is shown to be around 28% [1,3]. Genitourinary infection is highly uncommon and usually involves hematogenous spread, ascending infection, or obstructive uropathy. Infection by aspergillosis occurs more commonly among patients with immunocompromised status such as diabetes mellitus, malignancy, and post-organ transplantation status [4-6]. Ureteral aspergillosis can commonly present with fever, flank pain, nausea, vomiting, hematuria, or dysuria along with nephromegaly or obstruction of the ureters, which may even lead to death [7,8]. The diagnosis is confirmed by the isolation of the fungus from the tissue or fluid. The recommended treatment is treatment with antifungal agents, with intravenous amphotericin B being the most effective drug along with oral fluconazole. Among all the azoles, only fluconazole has the unique property of urinary excretion while the other drugs such as voriconazole and posaconazole, are metabolized in the liver, with poor urinary excretion [4,9]. Treatment of a fungal ball can be benefited by an excision prior to antifungal therapy. This can be achieved via open or endoscopic antegrade or retrograde approaches [10,11]. Usage of isolated medical therapy in cases of associated urinary obstruction is not proven to be beneficial, needing surgical bypass of the obstruction [2,9,12]. In diabetics, achieving simultaneous sugar control plays an important role in controlling the infection.
Our patient presented with urosepsis due to ureteric obstruction, which was initially controlled with urinary diversion and intravenous amphotericin B and antibiotics. This was essential in controlling the sepsis. On further surgical exploration, the obstruction was found to be due to an abscess cavity arising from the lower ureter causing a stricture. Urine culture was found to be positive for the growth of Aspergillus fumigatus, which was resistant to fluconazole. Complete abscess drainage along with excision of the stricture under the cover of intravenous antibiotics and oral voriconazole was a key factor in having an uneventful postoperative recovery. There have been attempts to treat localized genitourinary aspergillosis with local irrigation of amphotericin B, which has seen little success. Although controversial, it should be kept among the various treatment options available in the treatment of localized disease [13].
Conclusions
Whenever a patient with immunosuppression and sepsis presents, aspergillosis of the genito-urinary tract is considered an important part of the differential diagnosis. An early initiation of treatment along with an appropriate urological intervention can speed up the course of recovery, reducing the associated high morbidity and mortality rate.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Balaji Subramaniam, Senthil Kumar T, Saravanan Jambunathan, Shantanu Chandrashekhar, Saravanan K
Acquisition, analysis, or interpretation of data: Balaji Subramaniam, Senthil Kumar T, Saravanan Jambunathan, Shantanu Chandrashekhar, Saravanan K
Drafting of the manuscript: Balaji Subramaniam, Senthil Kumar T, Saravanan Jambunathan, Shantanu Chandrashekhar, Saravanan K
Critical review of the manuscript for important intellectual content: Balaji Subramaniam, Senthil Kumar T, Saravanan Jambunathan, Shantanu Chandrashekhar, Saravanan K
References
- 1.Isolated renal and urinary tract aspergillosis: a systematic review. Bongomin F, Morgan B, Ekeng BE, et al. Ther Adv Urol. 2023;15:17562872231218621. doi: 10.1177/17562872231218621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Urinary tract aspergillosis in a patient with chronic kidney disease. Zhou L, Zhao H, Chen Z, Zhu L. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2017-221638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epidemiology and sites of involvement of invasive fungal infections in patients with haematological malignancies: a 20-year autopsy study. Lewis RE, Cahyame-Zuniga L, Leventakos K, et al. Mycoses. 2013;56:638–645. doi: 10.1111/myc.12081. [DOI] [PubMed] [Google Scholar]
- 4.Practice guidelines for the diagnosis and management of aspergillosis: 2016 Update by the Infectious Diseases Society of America. Patterson TF, Thompson GR 3rd, Denning DW, et al. Clin Infect Dis. 2016;63:0. doi: 10.1093/cid/ciw326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aspergillosis of the urinary tract: ascending route of infection and evolving patterns of disease. Flechner SM, McAninch JW. J Urol. 1981;125:598–601. doi: 10.1016/s0022-5347(17)55119-8. [DOI] [PubMed] [Google Scholar]
- 6.Aspergillus mycetoma of the renal pelvis associated with ureteropelvic junction obstruction. Eisenberg RL, Hedgcock MW, Shanser JD. J Urol. 1977;118:466–467. doi: 10.1016/s0022-5347(17)58063-5. [DOI] [PubMed] [Google Scholar]
- 7.Sivasubramanian G, Sobel JD: . Netherlands. From Diagnosis to Prevention. Dordrecht: Springer; 2009. Urinary tract infections caused by Aspergillus species. [Google Scholar]
- 8.Invasive aspergillosis arising from ureteral aspergilloma. Choi H, Kang IS, Kim HS, Lee YH, Seo IY. Yonsei Med J. 2011;52:866–868. doi: 10.3349/ymj.2011.52.5.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Posaconazole as salvage therapy for zygomycosis. Greenberg RN, Mullane K, van Burik JA, et al. Antimicrob Agents Chemother. 2006;50:126–133. doi: 10.1128/AAC.50.1.126-133.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Synchronous endoscopic management of bilateral kidney and ureter fungal bezoar. Modi P, Goel R. Urol Int. 2007;78:374–376. doi: 10.1159/000100847. [DOI] [PubMed] [Google Scholar]
- 11.Case report: bilateral ureteral obstruction secondary to Aspergillus bezoar. Smaldone MC, Cannon GM, Benoit RM. J Endourol. 2006;20:318–320. doi: 10.1089/end.2006.20.318. [DOI] [PubMed] [Google Scholar]
- 12.Aspergillus infection limited to renal allograft: case report and review of literature. Linden E, Restrepo D, Dikman S, Murphy B, Huprikar S. Transpl Infect Dis. 2006;8:177–181. doi: 10.1111/j.1399-3062.2006.00134.x. [DOI] [PubMed] [Google Scholar]
- 13.Bladder irrigation with amphotericin B and fungal urinary tract infection--systematic review with meta-analysis. Tuon FF, Amato VS, Penteado Filho SR. Int J Infect Dis. 2009;13:701–706. doi: 10.1016/j.ijid.2008.10.012. [DOI] [PubMed] [Google Scholar]