Abstract
Background
Thrombotic thrombocytopenic purpura (TTP) is a rare hematological disorder. The occurrence of TTP subsequent to an emergent aortic valve replacement after a TAVR procedure is exceedingly uncommon with only a few reported cases worldwide.
Case Presentation
We report the case of a 70-year-old female patient diagnosed with aortic insufficiency. Following a transcatheter aortic valve replacement, she underwent emergency aortic valve replacement under cardiopulmonary bypass on the subsequent day due to heart valve displacement. The postoperative diagnosis revealed TTP and symptomatic treatment involving plasma exchange was administered. After demonstrating steady improvement, the patient was eventually discharged.
Conclusion
Aortic valve replacement after TAVR is a high-risk procedure and increases susceptibility for developing secondary TTP. The diagnosis and treatment of secondary TPP is considerably challenging, and early diagnosis with symptomatic treatment including plasma exchange can increase patient survival.
Keywords: Thrombotic thrombocytopenic purpura (TTP), Aortic valve replacement after TAVR, Plasma exchange
Introduction
Thrombotic thrombocytopenic purpura (TTP) is a type of thrombotic microangiopathy (TMA) [1]. The incidence rate of TTP is low; however, it is a critical condition and often presents with sudden onset, making it prone to initial misdiagnoses due to its atypical symptoms. Without timely treatment, it can lead to a high mortality rate [2, 3]. Common triggers include inflammation, infection and pregnancy [4, 5]. Diagnosing TTP can be challenging as well, requiring the evaluation of the protease ADAMTS13 (a disintegrin and metalloproteinase with thrombospondin motifs 13) which can serve as a disease monitor for TTP [2, 6].
TAVR (transcatheter aortic valve replacement) is becoming increasingly common, but it is not without complications [7]. Aortic valve replacement after TAVR is a high-risk procedure. TPP following emergent aortic valve replacement after a complicated TAVR procedure has never been reported.
Case presentation
A 70-year-old female patient was referred to our hospital on August 1, 2022 due to a 4-month history of chest congestion, which had notably intensified over the past 2 months. She was diagnosed with aortic insufficiency. The patient had a history of hypertension for 4 years, and her blood pressure had been effectively controlled through antihypertensive treatment. Upon admission, the patient underwent a series of relevant examinations. She subequently received a cardiac transcatheter aortic valve replacement (TAVR) under local anesthesia on August 5, 2022. During this procedure, two Taurus Elite 29 mm valves were implanted due to the displacement of the first valve. The following morning after surgery, the patient developed chest tightness and dyspnea with occasional premature ventricular beats. Her systolic blood pressure was 90 mmHg and her diastolic blood pressure was between 50 and 60mmHg. Her urine output volume also gradually decreased. The patient showed no signs of improvement after being treated with oxygen and diuretics. In the afternoon, echo findings revealed a shift in the position of the prosthetic valve, with it being positioned lower and closer to the anterior leaflet of the mitral valve. Additionally, there was an observed increase in forward flow rate across the mitral valve (Vmax = 2.2 m/s), indicative of mitral valve stenosis. A complication of valve displacement following TAVR was suspected. Consequently, she underwent emergency cardiopulmonary bypass (CPB) aortic valve replacement on August 6th (the first day after TAVR), which also included replacement of the mitral valve and removal of a cardiac foreign body. During the operation, it was noted that the first implanted valve was situated in the left ventricle and the mitral valve was damaged, with rupture of the anterior and posterior chordae tendineae. The patient’s own aortic valve was thick and misaligned, leading to severe aortic valve insufficiency. Two Taurus Elite valves were removed during the procedure. The native aortic and mitral valves were resected, and a 27# biofuncture valve was implanted into the mitral valve position, while a 23# biofuncture valve was implanted into the aortic valve position. During the surgery, the crossclamp time was 85 min, and the CPB time lasted 126 min. Intraoperative esophageal ultrasound showed no significant perivalvular leakage of the aortic or mitral valves. Postoperatively, the patient was admitted to the extracardiac intensive care unit.
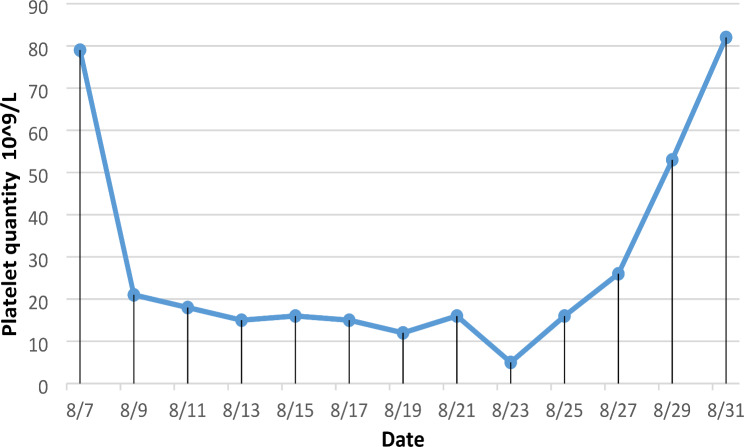
Following the surgery, the patient presented with oliguria and abnormalities in her routine blood test indicators. In response, we promptly initiated continuous renal replacement therapy (CRRT). Subsequently, the patient exhibited reduced hemoglobin and platelet levels, which were accompanied by minor bleeding spots on the skin (Fig. 1). Multiple consultations with relevant departments were obtained. She was administered corticosteroid therapy (August 7 - August 11), human immunoglobulin therapy (August 16 - August 20), along with rhTPO (recombinant human thrombopoietin) to promote platelet accumulation. She received multiple transfusions of platelets, plasma, and red blood cells. Despite all these therapies, no significant improvement was noted in the patient’s condition.
Fig. 1.

Locations of the bleeding spots in the patient
On August 23, the patient’s condition had deteriorated and the minimum PLT count dropped to 5*109/L. Consultation with the hematology department indicated that TTP should be suspected. We utilized the PLASMIC score, as shown in Table 1, for further assessment [8, 9]. The test results showed a platelet count of 16*109/L, a creatinine level of 1.03 mg/dL and an elevated reticulocyte count of 9.06%. The patient had neither active cancer nor recent solid organ or stem cell transplant. The INR (international normalized ratio) was 1.23. A PLASMIC SCORE of 6 points further indicated an increased risk of TTP [10]. These findings collectively suggested a diagnosis of TTP. In response, we immediately initiated plasmapheresis. Measurement of plasma ADAMTS13 activity was at 29.66% and ADAMTS13 inhibitory antibody levels were negative. Plasma exchange (PE) treatments were conducted daily from August 23 to August 26 and on August 28. Concurrently, the patient received an infusion of human immunoglobulin (August 23 to August 28) and glucocorticoids (August 23 to August 30). The platelet-elevating drug hetrombopag olamine (non-peptide thrombopoietin receptor (TPOR) agonist) was administered. Following these interventions, the patient’s hemoglobin and platelet count gradually increased and returned to normal levels (Fig. 2). By August 27, ADAMTS13 activity had increased to 37.43% and ADAMTS13 inhibitory antibody levels were negative. On August 29, the patient’s platelet levels had risen to 53*109/L, and a tracheotomy was performed. On September 8th, ADAMTS13 activity was 43.97% and the ADAMTS13 inhibitory antibody test was negative. Throughout this treatment course, the patient’s kidney function progressively improved as well. After her condition had stabilized, the patient was weaned from the ventilator and discharged from the hospital on September 27. The patient is currently able to live independently now one year and ten months after the surgical aortic valve replacement.
Table 1.
The PLASMIC score stratifies patients into low-risk (0–4), intermediate-risk (5), and high-risk (6–7) categories
| Parameter | Points | |
|---|---|---|
| Platelet count | < 30*109/L | 1 |
| Creatinine level | < 2 mg/dL: | 1 |
| Combined hemolysis parameter |
Reticulocyte count > 2.5%, or Haptoglobin undetectable, Or indirect bilirubin > 2 mg/dL |
1 |
| No active cancer | 1 | |
| No history of solid-organ or hematopoietic stem cell transplant: | 1 | |
| MCV | < 90 fL | 1 |
| INR | < 1.5 | 1 |
Fig. 2.
The patient’s PLT trends. The platelet count decreased rapidly after the operation, and the effect of conventional treatment and platelet transfusion was poor. However, the platelet count increased significantly after plasma exchange
Discussion
TTP falls within a group of microvascular thrombohemorrhagic syndromes. Acquired TMA also includes Shiga toxin–mediated TMA (ST-HUS), complement-mediated TMA, and drug-mediated TMA [1]. A diagnosis of TTP includes evaluating the age of onset, clinical manifestations, laboratory test results, and genetic information [1]. The onset and progression of TTP is rapid, hence early diagnosis is crucial. Multiple scoring systems such as the PLASMIC score, Bentley score, and French TMA score are used to guide the diagnosis and initiate effective treatment following confirmation [8, 10, 11]. Recently, a relationship between decreased ADAMTS13 activity and TTP morbidity has been identified, providing strong evidence for the effectiveness of PE treatment. Moreover, measuring ADAMTS13 activity and antibodies in plasma can help determine the therapeutic effect. Previous studies demonstrated that patients with a severe deficiency in ADAMTS13 activity (< 10%) can be diagnosed with TTP if they have an intermediate to high-risk PLASMIC score, even in low-risk patients. Slightly higher levels of ADAMTS13 activity (10-30%) is not sufficient to exclude TTP in intermediate to high-risk patients, and in such cases, plasma exchange should be continued for at least 7 days to evaluate a possible clinical response [12]. ADAMTS13 activity should also be tested using a different test method before initiating plasma exchange, as the results can vary between methods [12, 13]. At this stage, the patient should also be tested for antibodies, VWF: Ag and complement Factor H. Since ADAMTS13 activity results are not immediately available, the empiric initiation of plasma exchange while awaiting the final result is necessary and recommended [12, 14], and can reduce the mortality rate of TTP patients from approximately 90–10%~20% [6]. At the same time, in patients with moderate to high clinical suspicion of TTP or in confirmed cases, corticosteroid therapy should be initiated immediately, and combination therapy with rituximab may be considered [3, 15]. The treatment should be adjusted according to the patient’s ADAMTS13 activity levels and the results of the inhibitory or IgG antibody tests. Relevant literature indicates that plasma exchange is the preferred treatment for TTP. The mechanism involves the removal of ADAMTS13 inhibitors, IgG antibodies and other pathogenic factors in the blood. Supplementation of ADAMTS13 can also be used to treat ADAMTS13 deficiency. Early treatment with PE is associated with rapid relief of symptoms and improved outcomes [16].
TTP following a emergent aortic valve replacement after a TAVR procedure is rare. In the presented case, on the first day after a complicated TAVR, the patient developed chest tightness and dyspnea with echo findings revealing a shift in the position of the prosthetic valve. Immediate emergency CPB and surgical aortic valve replacement was performed. Intraoperative esophageal ultrasound showed no significant perivalvular leakage of the aortic or mitral valves. High traumatic stress in this patient resulted in the abnormal release of vWF from vascular endothelial cells, which subsequently led to decreased ADAMTS13 activity, increase of vascular endocrine polymers (vWF) and formation of platelet thrombi in the microvessels, all leading to TTP [17]. After acute heart failure and CPB surgery, factors such as renal ischemia, reperfusion, inflammation, and hemolysis likely contributed to the development of acute renal dysfunction [13]. CPB can cause platelet aggregation, adhesion and even destruction, with an extended CPB time being associated with more pronounced postoperative thrombocytopenia [18, 19]. Moreover, postoperative bleeding can exacerbate the consumption of peripheral blood platelets and obscure the symptoms of TTP. Clinicians may also lack sufficient awareness of the characteristics of TTP, resulting in delayed or missed diagnoses of TMA. After major cardiac surgery, TTP should be suspected if a patient presents with hemolytic anemia, thrombocytopenia, neuropsychiatric symptoms, and acute renal failure within 24 to 72 h. In this case, the patient exhibited all of the symptoms. Early administration of corticosteroids and immunoglobulin therapy were carried out due to the patient’s suspected immune-related disease. These actions may have led to the changes in the patient’s ADAMTS13 activity and IgG antibody levels. Using results from the PLASMIC score, plasma exchange therapy was given immediately after the suspected diagnosis of TTP was made. The patient’s ADAMTS13 activity levels increased significantly along with clinical improvement after plasma exchange. The effectiveness of plasma exchange also supports the diagnosis of TTP.
Conclusion
Emergent aortic valve replacement after complicated TAVR is a high-risk procedure. When a patient presents with hemolytic anemia, thrombocytopenia, acute renal failure or neuropsychiatric symptoms after complicated cardiac surgery, TTP should be suspected. Perform ADAMTS13 testing promptly, and initiate plasma exchange and corticosteroids to reduce mortality. Further research should collect and evaluate TTP cases post-cardiac surgery to advance diagnosis and treatment.
Author contributions
Xia Shao and Xiaobin Xu gathered data, performed a literature review and wrote the main manuscript text, Ruying Hu prepared Figs. 1 and 2. Xia Shao and Weijun Yang were directly involved in the care of this patient and helped review the final manuscript. Qingju Li, Kaiyu Tao and Aiqiang Dong reviewed and revised the manuscript.
Funding
This work has no funding.
Data availability
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.George JN, Nester CM. Syndromes of thrombotic microangiopathy. N Engl J Med. 2014;371(7):654–66. [DOI] [PubMed] [Google Scholar]
- 2.Joly BS, Coppo P, Veyradier A. An update on pathogenesis and diagnosis of thrombotic thrombocytopenic purpura. Expert Rev Hematol. 2019;12(6):383–95. [DOI] [PubMed] [Google Scholar]
- 3.Zheng XL, Vesely SK, Cataland SR, Coppo P, Geldziler B, Iorio A, Matsumoto M, Mustafa RA, Pai M, Rock G, et al. ISTH guidelines for treatment of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terrell DR, Williams LA, Vesely SK, LÄMmle B, Hovinga JAK, George JN. The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS‐13 deficiency. J Thromb Haemost. 2005;3(7):1432–6. [DOI] [PubMed] [Google Scholar]
- 5.Miller DP, Kaye JA, Shea K, Ziyadeh N, Cali C, Black C, Walker AM. Incidence of Thrombotic Thrombocytopenic Purpura/Hemolytic uremic syndrome. Epidemiology. 2004;15(2):208–15. [DOI] [PubMed] [Google Scholar]
- 6.Scully M, Hunt BJ, Benjamin S, Liesner R, Rose P, Peyvandi F, Cheung B, Machin SJ. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323–35. [DOI] [PubMed] [Google Scholar]
- 7.Thomas F, Lüscher M FESC. TAVI is on the move! How it compares with surgery and what complications we still have to consider. Eur Heart J 2019. [DOI] [PubMed]
- 8.Park SH, Kim H-K, Jeong J, Lee S-H, Lee YJ, Kim YJ, Jo J-C, Lim J-H. Performance validation of three Scoring systems for the prediction of thrombotic Microangiopathy due to severe ADAMTS13 Deficiency and the response to therapeutic plasma exchange: first study in Korea. Annals Lab Med. 2023;43(5):485–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orhan B, Özkocaman V, Akdemir Ç, Ersal T, Pınar İE, Yalçın C, Candar Ö, Çubukçu S, Koca TG, Ambarcıoğlu P, et al. Potential modifications of the PLASMIC scoring system for predicting thrombotic thrombocytopenic purpura: sometimes, less is more. Int J Lab Hematol. 2023;45(5):751–7. [DOI] [PubMed] [Google Scholar]
- 10.Okoli S, Jenkins KA, Bojanowski CM. Current Intensive Care Management of Thrombotic Thrombocytopenic Purpura: a Case Report and updated literature review. J Intensive Care Med. 2023;38(7):592–7. [DOI] [PubMed] [Google Scholar]
- 11.Makar R, Marques M, Sun L, Upadhyay V, Bendapudi P. Clinical Scoring systems in thrombotic microangiopathies. Semin Thromb Hemost. 2017;43(05):540–8. [DOI] [PubMed] [Google Scholar]
- 12.Chiasakul T, Cuker A. Clinical and laboratory diagnosis of TTP: an integrated approach. Hematology. 2018;2018(1):530–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Neal JB, Shaw AD, Billings FT. Acute kidney injury following cardiac surgery: current understanding and future directions. Crit Care 2016, 20(1). [DOI] [PMC free article] [PubMed]
- 14.Soares Ferreira Junior A, Pinheiro Maux Lessa M, Boyle SH, Sanborn K, Kuchibhatla M, Onwuemene OA. In patients with suspected immune TTP, admission source impacts hospital length of stay and time to therapeutic plasma exchange impacts clinical outcomes. Thromb Res. 2023;227:34–9. [DOI] [PubMed] [Google Scholar]
- 15.Long B, Bridwell RE, Manchanda S, Gottlieb M. Evaluation and management of Thrombotic Thrombocytopenic Purpura in the Emergency Department. J Emerg Med. 2021;61(6):674–82. [DOI] [PubMed] [Google Scholar]
- 16.Darmon M, Azoulay E, Thiery G, Ciroldi M, Galicier L, Parquet N, Veyradier A, Le Gall J-R, Oksenhendler E, Schlemmer B. Time course of organ dysfunction in thrombotic microangiopathy patients receiving either plasma perfusion or plasma exchange*. Crit Care Med. 2006;34(8):2127–33. [DOI] [PubMed] [Google Scholar]
- 17.Tellez-Hinojosa C, Vazquez-Mellado A, Gómez-Almaguer D. Thrombotic thrombocytopenic purpura. Med Universitaria. 2015;17(69):234–9. [Google Scholar]
- 18.Van Poucke S, Stevens K, Wetzels R, Kicken C, Verhezen P, Theunissen M, Kuiper G, van Oerle R, Henskens Y, Lancé M. Early platelet recovery following cardiac surgery with cardiopulmonary bypass. Platelets. 2016;27(8):751–7. [DOI] [PubMed] [Google Scholar]
- 19.Ding J, Chen Z, Niu S, Zhang J, Mondal NK, Griffith BP, Wu ZJ. Quantification of Shear-Induced platelet activation: high shear stresses for short exposure time. Artif Organs. 2015;39(7):576–83. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.