Abstract
Midlife, beginning at 40 years and extending to 65 years, a range that encompasses the late reproductive to late menopausal stages, is a unique time in women’s lives, when hormonal and physical changes are often accompanied by psychological and social evolution. Access to sexual health and sexual well-being (SHSW) services, which include the prevention and management of sexually transmitted infections, contraception and the support of sexual function, pleasure and safety, is important for the health of midlife women, their relationships and community cohesion. The objective was to use the socio-ecological model to synthesise the barriers and enablers to SHSW services for midlife women in high-income countries. A systematic review of the enablers and barriers to women (including trans-gender and non-binary people) aged 40–65 years accessing SHSW services in high-income countries was undertaken. Four databases (PubMed, PsycINFO, Web of Science and Google Scholar) were searched for peer-reviewed publications. Findings were thematically extracted and reported in a narrative synthesis. Eighty-one studies were included; a minority specifically set out to study SHSW care for midlife women. The key barriers that emerged were the intersecting disadvantage of under-served groups, poor knowledge, about SHSW, and SHSW services, among women and their healthcare professionals (HCPs), and the over-arching effect of stigma, social connections and psychological factors on access to care. Enablers included intergenerational learning, interdisciplinary and one-stop women-only services, integration of SHSW into other services, peer support programmes, representation of minoritised midlife women working in SHSW, local and free facilities and financial incentives to access services for under-served groups. Efforts are needed to enhance education about SHSW and related services among midlife women and their healthcare providers. This increased education should be leveraged to improve research, public health messaging, interventions, policy development and access to comprehensive services, especially for midlife women from underserved groups.
Keywords: access, women, middle age, sexual health, sexual well-being
Plain language summary
Sexual health and sexual wellbeing services for midlife women in high income countries
Midlife, beginning at 40 years and extending to 65 years, a range that encompasses the late reproductive to late menopausal stages, is a unique time in women’s lives. Access to Sexual Health and Sexual Wellbeing (SHSW) services, which include the prevention and management of sexually transmitted infections, contraception and the support of sexual function, pleasure and safety, is important for the health of midlife women, their relationships and community cohesion. The objective of this systematic review was to use the socio-ecological model to synthesise the barriers and enablers to SHSW services for midlife women in high income countries. Eighty-one studies were included; a minority specifically set out to study SHSW care for midlife women. The key barriers that emerged were the intersecting disadvantage of under-served groups, poor knowledge, about SHSW, and SHSW services, among women and their HealthCare Professionals (HCPs), and the over-arching effect of stigma, social connections, and psychological factors on access to care. Enablers included intergenerational learning, interdisciplinary and one-stop women-only services, integration of SHSW into other services, peer support programmes, representation of minoritised midlife women working in SHSW, local and free facilities, and financial incentives for under-served groups to access services. The appetite for education about SHSW and SHSW services among midlife women and their HCPs should be capitalised upon, and utilised to improve research, public health messaging, interventions and access to holistic services, particularly for midlife women from under-served groups.
Introduction
The publication of the UK government’s first Women’s Health Strategy in 2022 1 coincided with the welcome and long overdue global recognition of the necessity for more multi-disciplinary research in both women’s2 –5 and older people’s sexual health and sexual well-being (SHSW).6 –8 Public health approaches to sexuality focus on adverse biomedical outcomes, 9 despite the growing evidence for the importance of a holistic approach when evaluating sexual health,8,9 and the inclusion of positive sexuality and sexual experiences in the World Health Organization’s definition of sexual health. 10 In this review, we have followed Mitchell’s framework, which separates SHSW into two separate, inter-linked foci of public health enquiry. 11 Sexual health is defined as encompassing the prevention and management of sexually transmitted infections (STIs) including HIV, sexual violence prevention, support of sexual function, desire and arousal and fertility management. Sexual well-being is a multi-dimensional concept,12,13 which comprises sexual safety and security, sexual respect, sexual self-esteem, resilience in relation to sexual experience, forgiveness of past sexual experience, comfort with sexuality and self-determination in one’s sexual life. 11 SHSW services are often combined and offered in primary care, secondary care (sexual health and gynaecology services), health services which look after physical and mental health conditions interlinked with SHSW, and community and charitable services. Midlife is defined as beginning at 40 years and extending to 65 years, 14 a time when hormonal, physical and psychological changes in the lives of women 15 are often accompanied by evolution in their relationships,16,17 and social developments. 18 This stage can be a positive transition point for women, 19 empowering them to determine how they envision spending the latter half of their years, and can result in varied sexual experiences. 20
Midlife women are a growing population, often responsible for being both primary caretakes of children and elders, and major economic contributors.21,22 Increasing societal demands impact on their sexual experiences. 23 Cultural shifts in relationship patterns, 24 and population changes due to the stretching of mid years, 25 mean that SHSW services are an increasingly important part of the lives of midlife women, integral to the physical and mental health of many.26,27 Intimate partner violence and sexual assault are major public health issues, which have long-term effects on the health and functioning of many midlife women. 28 Prompt, effective diagnosis and treatment of STIs and gynaecological diseases, and the provision to support midlife women in having enjoyable, safe sex, has wide-ranging benefits to individuals, partnerships 29 and communities. 30 Indeed, the provision of sexual and reproductive health services is related to multiple human rights and should be available in adequate numbers, physically and economically accessible without discrimination and of good quality for everybody, including all midlife women. 31 Studies are often framed in a male, hetero-normative 32 perspective and the heterogeneous needs of midlife women are sometimes stereotyped by ageist and sexist misconceptions, or forgotten, 24 squeezed between the higher prevalence of STIs in adolescents and the increasingly apparent high prevalence of sexual dysfunction in older adults. 33
General health issues, such as diabetes, cardiovascular disease and arthritis, begin to emerge during the latter half of midlife and operate both to impact on sexual experience, with implications for the need for help-seeking, and should also provide opportunities for issues relating to sexual matters to be raised in routine healthcare. 8 However, many healthcare professionals (HCPs) are reserved about, and ill equipped to discuss SHSW with midlife women.5,6,15,32,34 –37 Stigma and negative attitudes about women’s sexuality, and sexuality at older ages, may inhibit discussion with HCPs. 38 Embarrassment may inhibit women from accessing help when symptomatic, 15 and SHSW services are not designed in a way that encourage midlife adults to seek help.5,6,15,32,34 –37 Health policies about ageing often omit sexuality, further contributing to the lack of research and services available. 39 Technology has not been sufficiently harnessed; the only evidence available for improving access to SHSW services for midlife women lies in the menopause field, but many menopause apps lack a credible evidence base. 40
In addition to the health inequalities related to identifying as female gender, 41 including the diminishing healthy life expectancy despite a longer life expectancy of women, 42 and the historical default of medical research being carried out on men, 43 there are also significant disparities in access to, and engagement with, healthcare services among women, largely due to the social determinants of health. 44 Within globally privileged settings, there is already a high disparity in access to services. The review was therefore restricted to high-income countries to improve the specificity of findings. It has enabled us to disentangle the impact of different strands of marginalisation within the context of affluent economies, which have separate challenges from low- and middle-economic locales. The World Bank’s definition of high-income countries was employed; high-income countries had a gross national income per capita of US$13,845 or more in 2022, calculated using the Atlas method. 45
This review evaluated the research that identified the enablers and barriers to midlife women’s access to SHSW services and established whether any groups of midlife women were particularly disadvantaged. It thereby delineated the key foci for policy and strategy change to improve quality and equity of SHSW care for midlife women in high-economic countries. The socio-ecological model (SEM) recognises the multiple and dynamic factors that can affect the barriers and enablers to accessing healthcare by considering the complex interplay between individual, interpersonal, organisational, community and public policy factors. 46 These factors affect SHSW decision-making for an individual and can both enable and inhibit healthy sexual behaviours. 47 The SEM approach has been successfully employed to interrogate many aspects of SHSW services for different populations, for example SHSW services for female sex workers, 48 adolescents49,50 and migrant Asian women, 51 and has enabled a holistic consideration of the different SHSW needs of midlife women within the complex context of the societies in which they live.
Objectives
The objectives of this review were to identify the barriers and enablers to SHSW services for midlife women in high-income countries 45 using the SEM, 52 and to identify the groups of midlife women in high-income countries who found accessing these services particularly challenging.
Method
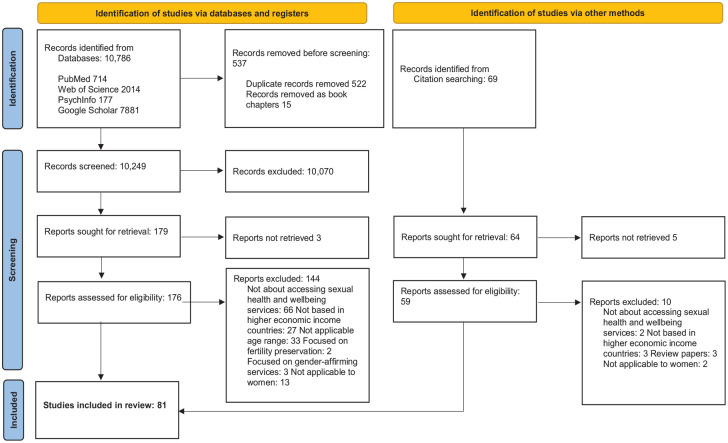
Reporting of the review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) recommendations (Figure 1). The protocol was Registered with the PROSPERO database on 8 June 2023, registration number: CRD42023433812.
Figure 1.
PRISMA flow diagram. The barriers and enablers to accessing sexual health and well-being services for midlife women (aged 40–65 years) in high-income countries: A mixed-methods systematic review. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Source: Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. Doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Eligibility criteria
The inclusion criteria (Table 1) were studies that had been published between November 1993 and November 2023, peer-reviewed, employed any methodology to capture primary data and investigated barriers to, or enablers of, access to SHSW care for midlife women (40–65 years old) who resided in high-income countries, 45 grouped into intrapersonal, HCP relationship, community and organisation perspectives. Studies on anyone who identified as a woman, gender diverse and non-conformist to either gender were included in this review. Transgender women and non-binary people (TGNB) experience different levels of stigma and discrimination than their cisgender counterparts, 53 but can share more in common with cisgender women than they do with men who have sex with men, 54 a group with whom they are often aggregated in SHSW research. 55 The review states when conclusions were drawn from TGNB-specific studies.
Table 1.
Inclusion and exclusion criteria for the barriers and enablers to accessing sexual health and sexual well-being services for midlife women (aged 40–65 years) in high-income countries: A mixed-methods systematic review.
| Study characteristic | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Sample | Studies which were composed of self-identifying women aged 40–65 years (studies which included men and women were included if women aged 40–65 years (or whose mean age was between 40 and 65) represented 50% or more of the study population, or women aged 40–65 were analysed separately). Studies which were composed of HCPs who worked in, or sign-posted midlife women to, SHSW services. |
Studies which were composed of less than 50% self-identifying women aged 40–65 (or whose mean age was not between 40 and 65) or studies in which women aged 40–65 were not analysed separately. Studies which were composed of HCPs who did not work with or sign post-midlife women to SHSW services. |
| Design | Empirical research. | Review/Meta-analysis articles. Theoretical articles. Book chapters. Unpublished manuscripts. Conference abstracts. |
| Publication | Peer-reviewed. Published between November 1993 and October 2023. | Not peer-reviewed. Published prior to November 1993 or after October 2023. |
| Language | English. | Any other language. |
| Duration of follow-up | All. | Not applicable. |
| Focus | Studies that assessed intra-personal-based factors, for example, age, sexuality, ethnicity, knowledge, psychological factors, other priorities, that may have affected midlife women’s access to SHSW services. Studies which evaluated the impact of interactions with HCPs on access to SHSW services. Studies which investigated the impact of organisational factors (hospital policies) on access to SHSW services. Studies which investigated community factors, for example, social stigma, which impacted on access to SHSW services. Studies which investigated public policy, for example health insurance coverage, guidelines, which impacted on access to SHSW services. |
Studies which investigated interventions, for example, treatment for menopause, sexual dysfunction, HIV testing, adherence to HIV pre-exposure prophylaxis, adherence to antiretrovirals, if not directly related to improving access to existing services. Studies which investigated the enablers and barriers to fertility technology techniques. Studies which investigated the enablers and barriers to accessing male-related sexual dysfunction services. Studies which assessed access to gender-affirming therapy for transpeople. Studies which investigated the impact of COVID-19 or other natural disasters on barriers/facilitators to services unless it included barriers/facilitators applicable to ongoing care. Studies with a focus on enablers and barriers to accessing SHSW care for men who have sex with men and non-binary and/ or transpeople unless there was a separate analysis for midlife non-binary and/ or transpeople, or midlife transpeople represented at least 50% of the studied population. |
HCP, healthcare professionals; SHSW, sexual health and sexual well-being.
Exclusion criteria (Table 1) comprised studies which investigated fertility technology techniques, as this was felt to widen the scope of the review too much and warrant a separate analysis. Male-related sexual dysfunction services were excluded, as although these would affect some women as partners in a relationship, women would not be the primary focus of the services. Studies addressing enablers and barriers to care for midlife TGNB people were only included in the review if they met the criteria of including at least 50% TGNB people and did not focus solely on gender-affirming therapy, a subject that warrants a separate review. COVID-19 may have had a significant impact on access to SHSW services 48 ; studies were only included if enablers and barriers that could be attributed to the COVID-19 pandemic had not yet reverted back to their state prior to the pandemic.
Search strategy
The search strategy was devised by KS with the assistance of CI, CL and SB. PubMed, PsycINFO, Web of Science and Google Scholar databases were searched between 23 April 2023 and 1 August 2023. The search strategy (Figure 2) was based on the SPIDER tool. 56 Sample: Women aged 40–65 years (and their HCPs); Phenomenon of Interest: Barriers and enablers to SHSW services; Design: Peer-reviewed research (qualitative/quantitative/mixed-methods); Evaluation: Critical Appraisal Checklists (CASP) criteria 57 ; Research type: Systematic review to optimise identification of relevant articles. The detailed search strategy is documented in Figure 2. Search limits included: English language and adults and middle-aged adults. No date or country of setting limits were applied. The included articles’ reference lists were hand-searched for additional relevant articles. Articles identified in the search were exported to EndNote. After removal of duplicates, 45 the remaining articles were exported to Excel.
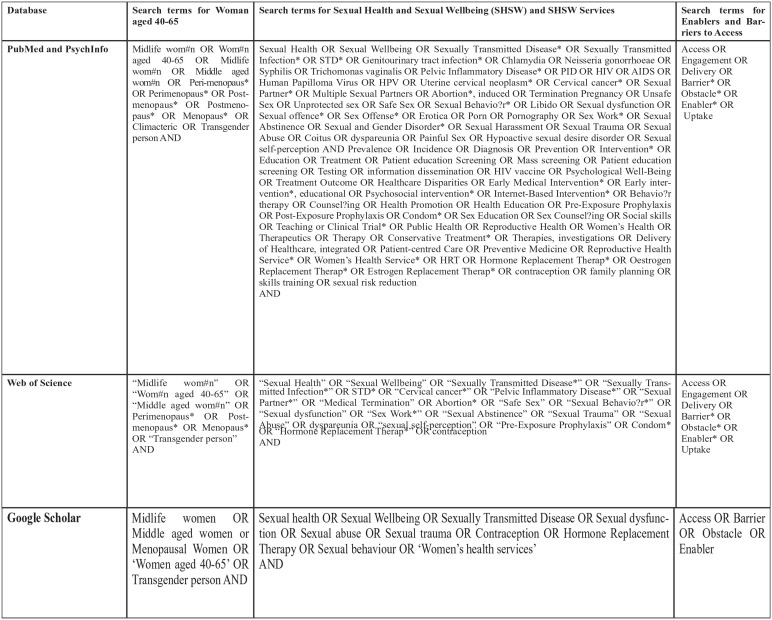
Figure 2.
Detailed search strategy criteria for the barriers and enablers to accessing sexual health and well-being services for midlife women (aged 40–65 years) in high-income countries: a mixed-methods systematic review.
Selection
Titles and abstracts were screened for relevance by KS and articles that did not meet the inclusion criteria were removed. Full texts of the remaining articles were reviewed independently in Microsoft Excel by KS and CN. Any disagreements were resolved through discussion between KS, CN and CI to reach a final decision.
Data extraction
Study characteristics were extracted by KS using a pre-set proforma on Excel (author, title, year published, participant characteristics, study aim.) Further study characteristics were then extracted by hand by KS onto a table in Microsoft Word (participant characteristics: sample, age range, gender of participants, relationship status, sexual orientation, language requirements, education level, ethnicity, study design and study findings).
Quality assessment
The CASPs 57 were used to systematically assess the trustworthiness, relevance and results of the articles. The appropriate checklist was used for each study, for example the qualitative checklist was used for qualitative studies. The reporting of the results of the study were assessed for validity, what the results were, and whether the methodology was sound. KS rated the studies (high, moderate or low quality) using the checklists as guides. About 10% were randomly selected and rated by a second author (CI, SB, CL, CN) to ensure validity. Any discrepancy in the rating was discussed, and if required, a third or fourth author would have been consulted to ensure unanimity. However, there were no discrepancies, resulting in a Cohen’s Kappa rating 51 of 1. Eligibility of articles was not determined by quality rating.
Data synthesis
The socio-ecological model (SEM) 52 was used to conceptualise and organise the findings into the enablers and barriers to accessing SHSW care, in terms of intra-personal factors, interactions with providers, organisational factors, community factors and public policy. The use of the SEM model has precedence in contextualising the complex levels of socioecology in which individuals are embedded, and the social, structural and cultural influences on behaviours affecting access to SHSW care. In the past, it has proved valuable in the analysis of the barriers and enablers to SHSW care for female sex workers, 58 adolescents, 59 urban men 49 and migrant Asian women. 50 Narrative synthesis was used to explore relationships within and between study findings. This method was employed because characteristics of the study designs and outcomes were too heterogenous to yield a meaningful summary of findings using a meta-analysis. The main findings and conclusions were grouped and coded inductively into descriptive themes that emerged from the data within the categories of ‘barriers to’ and ‘enablers of’ access to SHSW care, as defined by the inclusion criteria (Table 1). Data were further grouped and coded to iteratively develop and refine descriptive themes, with each study contributing new themes, using the SEM. Generation of higher-level analytical themes was undertaken.
Results
Study characteristics and main findings
Eighty-one studies were included in the final selection (Table 2).
Table 2.
Quality assessment of studies for the barriers and enablers to accessing sexual health and sexual well-being services for midlife women (aged 40–65 years) in high-income countries: A mixed-methods systematic review.
| Author (year of publication), study location | Study population characteristics (sample, age range, gender of participants, relationship status, sexual orientation, education level, ethnicity) | Study design and methodology | Aim of study | CASP quality | What are the results? |
|---|---|---|---|---|---|
| Auerbach et al. (2020), USA 54 | 43, 55.6% were aged 41–55 years, 25 women who identified as cisgender, 10 women who identified as transgender, 3 women who identified as ‘other’, 55.5% more than high-school education, 71% Black/African/Afro-Caribbean, 5 HCPs (one identified as a transwoman, two as cisgender women, two as cisgender men) | Qualitative. Focus groups. Convenience sampling. | Barriers and facilitators to including transwomen in HIV treatment and support services traditionally focused on cisgender women. | High, good mix of participants. | Histories of trauma, need for space safe away from men, unique challenge of being a woman in the world. Lack of understanding that many cisgender women are receptive to education, with a low barrier to improving their knowledge. Drawn to women’s care spaces out of desire for community, care tailored to specifically meet women’s needs, and a space that feels free of stigma and harm. Inclusive all-women care environment would disentangle transwomen demographically from men who have sex with men, foster community and understanding, affirm gender. |
| Bass et al. (2022), USA 60 | 34, age 18–52, mean age 34–46, 21% identified as female, 82% identified as transwoman, 6% identified as queer, 2.9% identified as ‘additional’, 56% some college education and above, 44% African American, 41% White, 21% Latinx, 12% other races | Quantitative. Cross-sectional study. Convenience sampling. | Barriers and facilitators to HIV PrEP use in transgender women. | High. | Knowledge of HIV PrEP is low. Persistent beliefs about effect of PrEP on hormone use. Need for culturally appropriate trans-specific messages in HIV prevention interventions and communications. |
| Benyamini et al. (2008), Israel 61 | 814, Aged 45–64, women, gender not specified, presumed cisgender, 540 long-term Jewish resident women, 151 Russian immigrants, 123 Arab women | Quantitative. Cohort. Questionnaire. Stratified random sampling. | Assess rates of primary and preventive healthcare use among midlife women from different cultural origins to identify socio-demographic and health characteristics that could explain differences in healthcare use. | High. | Long-term residents reported more preventive visits and screening tests compared with immigrants and Arab women. Cultural group, education, self-rated health and health motivation were significantly associated with use of primary and preventive care. Ethnic/origin group differences were mostly related to cultural rather than financial barriers. Arab women’s low use of preventive gynaecologic care related to lack of physicians of same culture and gender. |
| Blackstock et al. (2021), USA 62 | 52, Mean age 44.7 years, 11.5% transgender women, 88.5% gender identity not specified, presumed cisgender, 34.6% less than a high school education, 86.5% Latina or non-Latina Black | Quantitative. Cohort study. Pilot intervention. Convenience sampling. | Evaluate HIV PrEP outreach and navigation intervention. | Moderate (Study aim not completely clear). | 50% Aware of HIV PrEP. Gap between PrEP interest and connecting to PrEP care. Importance of peer-outreach. |
| Bullington et al. (2022), USA 63 | 578, Aged 25–60 (35 experienced menopause aged under 41, 101 experienced menopauses aged 41–45, 442 experienced menopause aged 46–50), women, gender not specified, presumed cisgender, majority Black ethnicity but mixed ethnicity study (e.g. 9% White) | Quantitative. Cohort. Convenience sample. | Description of premature and early menopause and subsequent hormonal treatment in women living with or at risk of HIV. | Moderate (significant confounding factors as to why older women received less hormonal therapy). | 51% of women who experienced menopause before 41, 24% of women 41–45, 7% of women between 46 and 50 received menopausal hormonal therapy or hormonal contraception. Women Living with HIV are less likely to access hormone therapy for menopause than other women. |
| Bush et al. (2007), USA 64 | 22, Physicians | Qualitative. In-depth interviews. Convenience sampling. | Physician’s perceptions on HRT and counselling strategies. | High. | Many felt that women should oversee HRT decision. Decision aids are needed to guide discussions with women. |
| Cahill et al. (2020), USA 65 | 19, Mean age 42, 72% had high-school or less education, identify as transgender women, mixed ethnicity study | Qualitative. Focus groups. Convenience sampling. | Explore barriers to HIV PrEP uptake. | High. | Some had not heard of HIV PrEP, some reported their HCPs had not told them about PrEP, some had questions about side-effects, some expressed medical distrust. Expressed need for gender-affirming healthcare services, concerns about interactions between feminising hormones and PrEP, these interactions need to be made clear in health education campaigns. Clinicians should be trained in providing gender-affirming care. |
| Cannon et al. (2018), USA 66 | 68, Ages 18–50 but ages 35–50 analysed separately, women, gender identity not specified, presumed cisgender, 59% African-American, 25% White, 14.9% other | Quantitative. Cross-sectional study: survey with multiple-choice close-ended questions administered via interview. Convenience sampling. | Risk of unintended pregnancy among newly incarcerated women. | Moderate (small study). | Poor knowledge about emergency contraception safety, when and how to take. About 58.8% aged 35–50 used no contraception at intake, but 63.2% would accept free contraception at release. |
| Cappiello and Boardman (2021), USA 67 | 35, Nurse practitioners in their first 2 years of community-based practice | Qualitative. Interviews. Convenience sampling. | Exploration of perceived competency in providing sexual and reproductive healthcare. | High but small study. | More preparation needed to discuss STIs, dyspareunia and pelvic pain. Interest in discussion of sexuality across the lifespan and postmenopausal sexual concerns. |
| Clarke (2009), USA 68 | 6 Magazines, 3 for middle-aged women, all 3 have circulation of >2,000,000 | Qualitative. Exploratory content analysis. | Portrayal of sexuality, sexual health and sexual disease. | High. | Major themes: sex depicted as a woman’s work and responsibility in a marriage; accountable for husband’s sexual fulfilment, and happiness. Fear-mongering in refusing husband’s request for sex. Idea that sex can be viewed as a workout and beneficial for women’s health. |
| Cronin et al. (2023), England, Finland, Denmark, New Zealand, Australia and USA 22 | 48 Nurses, ages 37–65 (majority over 40 years) | Qualitative. Focus groups and interviews. | Perspectives of nurses (wide range of clinical settings) on digital interventions as strategies to support menopausal women. To understand the requirements for designing health interventions for support in the workplace. | High. | Women were frustrated by the stigma and lack of recognition and awareness at work about menopause. Without awareness, women felt uncertain of the validity of their own experiences, often questioning themselves and their concerns. Colleagues were judgemental, lacked insight, tiredness related to menopause symptoms was not socially acceptable. Participants from many countries felt that many women were unprepared and there was a lack of knowledge about the menopause. Mothers had not prepared them – no detail/depth in explanations. ‘You just get on with it, that sort of thing’. ‘I talk to mums everyday about everything to do with their bodies and their bleeding, babies and everything . . . there are so many variations on how it is for premenopausal women, like maybe we don’t really understand enough’. Participants preferred to select from a range of interventions available across different formats (to meet individual needs). Participants had spent a long time looking for information, with poor results. They felt that due to the widespread use of smart phones, it should be possible to have quick, easy access at any time and anonymously, to a private, secure platform with evidence-based information. They felt that digital resources should be culturally sensitive, with podcasts, videos, virtual reality, mindfulness, expert blogs. |
| Dakshina et al. (2014), UK 69 | 202, Ages 16–60, Median age 41, IQR 35–49 years, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Purposive sampling. | Ascertain proportion of women with a documented discussion about their family planning needs within a 12-month period. | High. | Contraception only documented to have been offered to 15% of women who required it. |
| Dalrymple et al. (2017), Scotland 70 | 31 (18 Women, 13 men), ages 45–65, women, gender not specified, presumed cisgender, most had been divorced, most from deprived areas as per Scottish Index of Multiple Deprivation areas | Qualitative. Interviews. Convenience sample. | Psychosocial factors that influence risk-taking. | High (but small study and may not have been representative due to recruitment from clinics and sporting centres and limited ethnic diversity). | Reassured if new partner had few previous partners, long previous relationships, or had recently spent time alone. Very few used condoms or tested for STIs. Unwanted pregnancy shaped risk perceptions through life-course. Prioritisation of intimacy above risk of STIs. Feelings of reassurance and safety from STIs were associated with intimacy. Motivation to seek intimate and monogamous relationships, and a sense of emotional connection with new partner, lent safety to actual exposure to STIs. Vulnerability associated with relationship transitions – guilt and loss of self-esteem leading to prioritisation of emotional rather than health needs (safe sex). Social norms relating to age-appropriate sexual and health seeking behaviours – older people ‘should know better’, ashamed to seek help. Distancing from young people’s risky behaviour. Felt had to adjust to new sexual culture – fast progression to sex in new relationships. Sense of freedom linked with feeling young, encouraging more risk taking. |
| Dietz et al. (2018), USA 71 | 30, Aged 45–60, women, gender identity not specified, presumed cisgender | Qualitative study. Focus groups. Convenience sample. | Women’s knowledge of menopause, preferred sources of information, barriers to treatment. | High (but not generalisable). | Feel insufficiently informed about hormone therapy. Prefer older female providers. |
| Doblecki-Lewis et al. (2015), USA 72 | 8, Aged 40–59 (analysed separately from other women in study aged 18 to >60), women, gender identity/education/ethnicity not separated out for this age group, but study included predominantly Black and Hispanic participants and 77% of total participants were heterosexual) | Quantitative. Cross-sectional study. Purposive sampling. | Self-reported sexual risk behaviour, awareness and perception of HIV Pre exposure Prophylaxis (PrEP) and HIV Post exposure Prophylaxis (PEP) in a sheltered population (women experiencing homelessness). | High (but although analysed separately, small sample of midlife women). | Women who reported that they would ‘definitely consider’ or ‘might consider’ PrEP or PEP were significantly younger (mean age = 29.3 years) compared with those who reported they would ‘definitely not consider’ these strategies (mean age = 41.5 years; p = 0.004 for difference). |
| Donati et al. (2009), Italy 73 | 720, Aged 45–60 years, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Purposive sampling. | Women’s attitude, knowledge and practice regarding menopause and HRT. | High. | Minority received information about menopause, those who did found it poor and contrasting. |
| Duff et al. (2018), Canada 74 | 109, Aged 44–53, women, gender identity not specified, presumed cisgender, 33% Lesbian, gay, bisexual, queer, two-spirit, 90% high school graduate, 56% Indigenous, 7% African/Black/Caribbean, 36% White | Quantitative. Cohort study. Convenience sampling. | Correlates of antiretroviral adherence among perimenopausal and menopausal women living with HIV. | High. | Severe menopausal symptoms, injecting drug use and physical/sexual gender-based violence associated with <95% antiretroviral adherence. |
| Du Mont et al. (2021), Canada 75 | 27, HCPs who look after people who have been sexually assaulted | Quantitative. Cross-sectional. Convenience recruitment. | Evaluation of networks’ capacity to address needs of trans-sexual assault survivors. | High. | Barriers to providing care: lack of knowledge, discriminatory attitudes, limited training opportunities. About 100% felt would benefit from further training to help trans-people. Hospital policies not trans-sensitive. Paucity of trans-positive services for referral/collaboration. Facilitators: efforts to promote trans-positive environments, trans-positive hospital policies, partnership building with other services. |
| Ejegi-Memeh et al. (2021), UK 76 | 10 (4 Aged 40–65, results separated out), aged 50–83, women, gender identity not specified, presumed cisgender | Qualitative. Interviews. Convenience sampling. | Barriers and facilitators to sexual discussions in primary care in women with type 2 diabetes mellitus. | High quality but small number. | Problematic changes to sexual health and well-being, attributed to diabetes, menopause, ageing and changes in intimate relationship, tended not to be discussed with HCPs. Women assumed HCPs did not broach topic of sex due to embarrassment, ageism, social taboos around older women and sex. Facilitators: professional-patient rapport, female HCPs, instigation of conversation by HCP. |
| Erens et al. (2019), UK 8 | 23 (5 Women aged 40–65 years, results separated out), aged 55–74, women, gender identity not specified, presumed cisgender, 3 married, 1 widowed, 1 co-habiting, 30,503,880 (9,751,175 women aged 40–65 years, results separated out) | Mixed methods. Qualitative. Interviews. Purposive sampling from nationally representative sample (Natsal-3). Quantitative. Cross-sectional (nationally representative sample from private residential addresses, Natsal-3). | To explore how older people see their health status as having influenced their sexual activity and satisfaction; and to further understanding of how they respond and deal with the consequences. | High. | Where help had been received, it was in the form of sildenafil for men. No participants in the qualitative component mentioned any other form of help. Women described continuing to have sex despite a health-related reduction in their own sexual desire to ensure the continued stability of the relationship. ‘You get used to what you like and because I can’t have what I like I’m not really bothered’. After adjusting for age and relationship status, the odds for being sexually active were much lower for those who saw themselves as being in bad/very bad health compared with those in very good health. For women in a steady or cohabiting relationship, after adjusting for age, satisfaction with their sex life was associated with feeling happy in the relationship. |
| Erickson et al. (2019), Canada 77 | 292, mean age 43, 10% transgender women, 90% cisgender women, 48% had completed high-school, 58% indigenous, 34% White, 4% Afro-Caribbean, 5% other | Quantitative. Cross-sectional. Convenience sample. | How incarceration affects HIV treatment outcomes. | High. | Exposure to recent incarceration independently associated with reduced odds of HIV virological suppression. |
| Esposito (2005), USA 78 | 56 (40 Women, 6 HCPs), ages 39–62, women, gender identity not specified, presumed cisgender, 38% married or cohabiting, 6, HCPs, ages 34–56, all White and European American | Qualitative. Focus groups. Convenience and snowball sampling. | Immigrant Hispanic and Healthcare Providers expectations of healthcare encounters in the Menopause. | High. | Linguistic ability. Cultural inhibitions to not bringing up topic. Dealing with American providers required higher level of assertiveness than previously needed. Lack of access to advice – some knowledgeable relatives were now dead, others never talked about menopause/could not remember it/denied symptoms. Brochures and videos nonspecific – unsure if applied to them, failed to address intensity of symptoms. Women wanted provider-initiated, individualised, anticipatory guidance for menopause. Providers felt other challenges (diabetes, heart disease, HIV prevention) were more important. Providers did not have time to assess their needs. Need for better mainstream medical relief from menopause symptoms. HCPs questioned whether menopause an issue for immigrant Hispanic women. Symptoms were not important because women were socialised to minimise their gynaecological discomforts in context of competing family needs. May manage symptoms effectively through alternative health resources such as local medicine woman. HCPs wanted patients to be informed and clear about what they wanted. Frustrated with lack of continuity in care, for example, when international mobility complicated care. Cultural expectations of stoicism around gendered issues such as menopause. |
| Ettinger et al. (2000) and Ettinger and Pressman (1999), USA79,80 | 749, Aged 50–65, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional. Convenience sampling. | Predictors of women receiving HRT counselling. | High. | Higher level of education and higher level of income associated with increased likelihood of HRT counselling being obtained. |
| Fox-Young et al. (1995), Australia 81 | 40, Aged 45–55, women, gender identity not specified, presumed cisgender | Qualitative. Focus groups. Convenience sampling. | Women’s perceptions and experiences of menopause, HRT, doctor–patient relationships. | High (but not generalisable). | Lack of reliable and accurate information about menopause. Need to foster open discussion between women and HCPs, need for equal partnership. |
| Gazibara et al. (2022), Spain and Serbia 82 | 461 from Madrid, 513 from Belgrade, 40–65, Women, gender not specified, presumed cisgender | Quantitative. Cross-sectional study. Convenience sampling. | Compare climacteric symptoms associated with health-related quality of life. | High (unclear whether similar level of contra-indications in two different populations). | Similar ratings of somatic and urogenital complaints. Serbian women of higher education were more likely to use HRT. |
| Gkrozou et al. (2019), UK 40 | 22 Apps | Review analysis of menopause apps. | Identify mHealth apps that address the menopause with a focused view on the degree of medical professional involvement and evidence base practice in their design. | High (but limited due to small number). | Only 22.7% of the apps analysed had documented evidence-based practice in the form of guidelines or treatment protocols. |
| Gleser (2015), UK 83 | 62, Specialist trainee doctors | Quantitative. Cross-sectional study. Questionnaire. Convenience sampling. | Determine views and attitudes of specialist trainee doctors towards sexual health in the (peri)menopause. | Moderate. (Did not look at confounders such as ethnicity, sexuality). | Do not believe that women proactively raise their concerns regarding menopausal symptoms affecting sexual health without being asked. Reported lack of consultation time as main barrier to address sexual health and sexual problems in menopausal women. Some reported perceived unease from patient’s side, poor coverage of topic in curriculum, lack of training. |
| Gomez-Acebo et al. (2020), Spain 84 | 2038, Ages 20–85 (1031 women born before 1950 had average age of 70, 1007 women born after 1950 had average age of 48), women, gender not specified, presumed cisgender, majority with low level of education, 12 Spanish provinces | Quantitative. Cross-sectional design. Purposive sampling. | Influence of individual and contextual socio-economic levels on reproductive factors. | Moderate (did not stratify by ethnicity). | For women born before 1950: more educated women double use of HRT, women living in less vulnerable areas double use of HRT. But socio-economic inequalities in HRT not true for women born after 1950. |
| Goparaju et al. (2015), USA 85 | 39, Median age 49, women, gender identity not specified, presumed cisgender, Majority Black/African American or Latina/Hispanic, mixed level of education, 50% married | Qualitative. Focus groups. Purposive sampling. | Women’s knowledge, attitudes and potential behaviours regarding HIV PrEP. | High. | PrEP awareness was extremely low and the HIV-negative women urged publicity: they wanted to use and recommend it to others despite potential side effects, and difficulties with access, duration and frequency of use. Women’s reactions to PrEP differed based on their sero-status: HIV-negative women expressed much enthusiasm while the HIV-positive women voiced caution and concerns based on their experience with ARVs. |
| Guo and Sims (2021), USA 86 | 498, Aged 42–65, women, gender identity not specified, presumed cisgender, Chinese American women | Quantitative. Cohort study. Purposive recruitment. | Patient-level factors associated with Pap uptake. | High. | Having a female healthcare provider positively associated with Pap test uptake. Not having a primary healthcare provider and not having time to go to the doctor negatively associated with Pap test uptake. |
| Heinemann et al. (2008), USA 87 | 10,297, Age: 40–70, women, gender not specified, presumed cisgender, education level: over 60% were low/medium, majority married/stable relationships, 9 countries on 4 continents | Quantitative. Cross-sectional. Validated survey. National representative population panes and quota sampling. | Prevalence of menopausal women’s symptoms, motivations for hormone therapy. | Moderate (ethnicity not described). | Self-reported symptoms did not differ significantly among women in Europe, North America, Latin America and Indonesia. Prevalence range of hormone therapy from 50% to 1.8%. Acceptance of HRT affected by: worry about side effects. |
| Hendren et al. (2019), Canada 88 | 154, Median age 41–45, 53% women (Adult nephrologists) | Quantitative. Cohort. Convenience sampling. | Adult nephrologists training in, exposure to and confidence in managing women’s health. | High. | 65% lacked confidence in women’s health issues, 89% felt that interdisciplinary clinics and continuing education seminars would improve their knowledge. |
| Hillman et al. (2020), UK 89 | 142,919,989, Aged over 40 (2,677,613 HRT prescriptions), women, gender identity not specified, presumed cisgender, from 6478 practices | Quantitative. Cross-sectional study. Purposive sampling. | General practice HRT prescription trends and their association with markers of socio-economic deprivation. | High. | HRT prescribing rate 39% lower in practices from most deprived quintile compared to most affluent. After adjusting for cardiovascular risks/outcomes, 18% lower. More deprived practices have significantly higher tendency to prescribe oral HRT (should be avoided if high cardiovascular risk). |
| Hinchliff et al. (2021), UK 90 | 23 (12 Women, 11 men), ages 58–75, women, gender identity not specified, presumed cisgender, majority married | Qualitative. Interviews. Purposive sampling. | Explore why older adults do, or do not, seek help for sexual difficulties. | High. | Both women and men framed help-seeking in relation to erectile dysfunction. Reluctance/inability to talk about sex with partner stopped them getting help. Feeling embarrassed to talk about sexual difficulties – considered taboo. Dealing with other health conditions more important. Significant barrier was concern about interaction of medicines prescribed for the sexual difficulty with those already taken for health conditions. Spent a long time, sometimes years, thinking about whether to get help. Patient fear of not being taken seriously and doctor reticence to ask. Help-seeking journeys often ended without resolution. Most were not asked about sexual well-being even though had conditions known to affect sex life. Doctors prioritised general health over sexual health. Having access to approachable doctor facilitated help-seeking. Patients saw help-seeking only appropriate up to a certain age. |
| Howells et al. (2019), UK 91 | 73, Women, gender identity not specified, presumed cisgender, 56% Black African, 5% Black Caribbean, 5% Black British, 3% White British, 10% White other | Quantitative. Cross-sectional study. Retrospective case note review. Purposive sampling. | Assess uptake and effectiveness of HRT in postmenopausal women living with HIV. | High. | Good symptom control (91%) in those of Black ethnicity who started HRT but low uptake (52%). |
| Huang et al. (2009), USA 92 | 1977, Aged 45–80 (77% between 45 and 64), women, gender identity not specified, presumed cisgender, 67% currently married/living as married, 44% White, 29% African American, 18% Latina, 19% Asian | Quantitative. Cohort study. Purposive sampling. | Factors influencing sexual activity and functioning. | High. | 43% Reported moderate to very high sexual desire or interest, decreased with increasing age varied according to race/ethnicity/co-habitation. Sexual desire and interest strongly associated with sexual satisfaction. About 40% reported problems with sexual activity. Physical and mental health strongly associated with sexual desire and interest. Lack of partner capable of or interested in sex important. |
| Huynh et al. (2022), USA 93 | 87, Ages <45 (40%), 45–65 (44.8%), >65 (12.6%), women, gender identity not specified, presumed cisgender, 85% Heterosexual, 72% married or partnered, 82% Caucasian, 5.7% Asian, 4.6% Black or African American, 1% Latina, 1% American Indian or Alaskan, 4.6%, Other/prefer not to say, Focus groups: 13, Individual interviews: 3 | Mixed methods. Cross-sectional study and Qualitative (interviews and focus groups). Convenience sampling. | Characterise education that patients with breast cancer receive about potential sexual health effects of treatment, and preferences in format, content, timing. | Moderate quality (? Selection bias and homogenous population, and qualitative element very small). | Few women received information about sexual health effects of treatment. Patients in favour of multiple options of education being offered, with emphasis on in-person options and support groups. |
| Jacobs et al. (2014), USA 94 | 3258, aged 42–52, women, gender not specified, presumed cisgender, 7 US sites, 68% married, 76% had some form of college education, 28% African American, 7% Chinese, 8% Japanese, 7% Hispanic, 50% Caucasian | Quantitative. Cohort. Mixed recruitment methods. | Relationship between perceived everyday multi-ethnic/multiracial and other discrimination and receipt of cervical (and breast) screening. | High (but difficulty with concept of ‘reported discrimination’). | Reported discrimination owing to physical appearance and gender associated with reduced receipt of Pap smear regardless of race. Perceived discrimination much higher in African American women. |
| Kerkhoff et al. (2006), Ireland 95 | 58, Age 22–81, median age 46, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Convenience sample. | Assess female renal transplant recipient’s awareness of gynaecological issues, and to assess uptake of screening services. | High (but not generalisable). | 84% Aware as to why they should have regular cervical smears. |
| Kingsberg et al. (2013), USA 34 | 3046, Age: postmenopausal, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Questionnaire. Purposive sampling. | Characterise postmenopausal women’s experiences with vulvar-vaginal atrophy and interactions with HCPs about it. | High. | 24% Attributed symptoms to menopause, 65% had discussed symptoms with HCP, 40% using treatment (62% who had consulted HCP were using treatment). Concerns about side effects and cancer risks limited access to treatment. |
| Levin et al. (2023), Israel 96 | 252, Mean age 54, women, gender not specified, presumed cisgender | Quantitative. Cross-sectional study. Convenience sample. | Compare stage and survival of cervical cancer of Jewish and Arab women. | Moderate- (many more Jewish women in study, unsure re. power, and many confounders). | Arab women at higher risk to be diagnosed with advanced cervical cancer than Jewish women. |
| Lewis et al. (2020), UK 24 | 19 (10 Women, 9 men), ages 40–59, women, gender not specified, presumed cisgender | Qualitative. Face-to-face interviews. Purposive selection from NATSAL-3. | Identify factors shaping STI risk perceptions and practices among individuals contemplating or having sex with new partners following end of long-term relationship. | High (but small number). | Loss of fertility reduces motivation to prioritise safe sex. Inadequate indicators to assess STI status of partners, for example, demeanour, appearance. Self-perception as low risk even if have come out of long-term relationship. Constraints on the navigation of sexual safety include self-perceived STI risk rooted in past. Perceived dominance of ‘couple culture’ pressure to re-partner. Perceived norms vary between social networks – normalisation of condomless sex with new partners, paying for sex, ‘othering’ of those at risk of STIs/HIV. Intersecting gender-age dynamics in negotiation of risk prevention strategies – association with youth, lack of familiarity, concerns about erectile dysfunction. Enablers: peers and younger relatives’ influences. Age-related barriers to accessing condoms; disconnection from safe sex messaging and services (men who have sex with men and youth focused). Greater public discussion about sexuality and more positive representation of sexuality in mid-life in tension with sensationalised media coverage. Age-gender barriers to accessing condoms in shops/pharmacies. |
| Lippman et al. (2016), USA 97 | 50 (11 Gave in-depth interviews), median age 42, transgender women 56% post high-school education, 30% Black African-American, 22% White/Caucasian, 20% Hispanic/Latino, 8% Asian/Pacific Islander, 8% Native American, 12% multi-racial |
Mixed. Quantitative. Cross-sectional. Qualitative interviews. Convenience sampling. | Feasibility and acceptability of HIV self-testing. | High. | 68% Prefer HIV self-testing to attendance at clinic. Emotional support embedded into service very important. |
| Maar et al. (2013), Canada 98 | 18, HCPs | Qualitative. Interviews. Convenience sampling. | Structural barriers to cervical screening. | High. | Shortage of HCPs, lack of recall system, geographic/transportation barriers, health literacy, socio-economic inequalities, generational effects, colonial legacy. |
| Maiorana et al. (2021), USA 99 | 67, 36 Staff, 31 participants in interventions, average age 44 (range 21–63), all participants identified as transgender women of colour, 77% of staff identified as transgender women of colour | Qualitative. Interviews. Convenience sampling. | Identify commonalities amongst intervention services for Transgender Women of Colour (addressing unmet basic needs, facilitating engagement in HIV care, health system navigation, improving health literacy and support) and relationships formed during implementation. | High. | Interplay of transphobia, sexism and racism. Transgender women have low self-esteem, feel defensive and socially excluded due to stigma, and previous experiences of marginalisation in community and healthcare system. Gender-affirming services and caring relationships help to engage transwomen of colour in care. Intervention services need to be complex, and HCPs need to be able to perform many roles. Services that address basic unmet needs such as food, housing before addressing other barriers to engaging in HIV care. |
| Moro et al. (2010), Canada 100 | 4, Age 46–72, women, gender-identity not specified, presumed cisgender | Qualitative. Focus group. Convenience sampling. | Enablers and barriers to obtaining bioidentical hormones and how to improve the access path. | Poor (small number). | Seek information from friends/books/websites/HCPs. Quality of available information a barrier to making informed decision. Internet a confusing medium-wide range of quality. HCP with supportive/trustworthy/ample information seen as key enabler to care. Some physicians did not listen to their needs. Some made unilateral decisions favouring HRT without consulting patient. Struggle to access physicians who would prescribe HRT. Cost of bioidentical HRT big barrier. Suggestions: continuing education for physicians, comprehensive website with risks and benefits of HRT, regular seminars for menopausal women, policy change to allow other health professionals to prescribe HRT, women-only clinics. |
| Munro et al. (2017), Canada 101 | 14 Women (8 aged over 40) and 10 HCPs, women who identify as transgender women | Qualitative. Interviews. Convenience sampling. | Dynamics of healthcare utilisation by transwomen living with HIV. | High, but small study. | Importance of coordinating HIV services and transition-related care. Importance of training service providers. |
| Nappi and Kokot-Kierepa (2010), USA 102 | 4246, Aged 55–65, women, gender identity not specified, presumed cisgender, Sweden, Finland, UK, USA, Canada | Quantitative. Cross-sectional. Interviews using structured questionnaire. Purposive sampling. | Issues related to vaginal atrophy via an international survey. | Moderate (purposive sampling but not sampled to be representative). | Different needs in different countries (51% in US versus 10% in Finland aware of local treatment); country-specific approaches to improve uptake of treatment for vaginal atrophy. About 77% believe women uncomfortable discussing vaginal atrophy, 42% not aware that local treatment is available. |
| Nemoto et al. (2021), USA 103 | 60 in Cohort study (34 enrolled in HIV care and 26 who had never enrolled), 12 interviews, age range 19–60, average age 41, transgender women (78% gender identity transgender woman, 21% female), 32% college or above level education, 80% African American, 13% Hispanic, 2% Asian, 5% Multiracial | Mixed study: Cohort and qualitative. Interviews. Convenience sample. | Describe access to HIV primary care for African American transwomen living with HIV. | High. | Transphobia and community stigma are strong barriers to enrolling in HIV care; 44% who had enrolled in HIV care had not received anti-retroviral treatment (ART); 50% of those on ART had poor adherence. If engaged in sex work, sold drugs, or experienced higher levels of transphobia less likely to have enrolled in HIV care. |
| Nusbaum et al. (2004), USA 104 | 1196, 54% aged <45, 15% 45–54 years, 32% aged over 54, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Survey. Convenience sampling. | Self-reported sexual concerns and interest and experience in discussing these concerns with physicians. | High. | 96% of ‘middle aged’ women showed interest in discussing with HCP. Women who discussed concerns found it helpful. Felt that discussing would be easier if physician broached topic. Having female physician would facilitate discussion. Most women had never had topic raised by physicians. |
| Okhai et al. (2020), UK 105 | 6455 Women (1595 aged 40–50, analysed separately, 607 aged >50, analysed separately), women, gender identity not specified, presumed cisgender, all acquired HIV via sex with men, 14% White, 5.7% Black Caribbean, 70.6% Black African, 3.6% Black other, 2.7% South Asian, 3.4% Mixed | Quantitative. Cross-sectional study. Purposive sampling. | Investigate whether association between menopausal age and engagement in HIV care. | High, large study. | Postmenopausal aged women less likely to be engaged in HIV care than younger ages differs from previous studies? Due to different definitions of engagement in care. However, suggestion that better adherence to antiretrovirals among 40–50 years than younger women. |
| Ong et al. (2022), Australia 106 | 3 Suburban GP practices, qualitative: 33, 17 doctors, 7 nurses, 9 administrative staff | Mixed methods. Quantitative. Cross-sectional. Qualitative. Interviews. Convenience sample. | Hub and spoke model: primary care HIV/STI testing and treatment with support of specialist SH centre hub. | High. | Early and sustained increase in chlamydia, gonorrhoea, syphilis, HIV testing. Many training needs identified by GPs, nurses and admin staff, for example, taking a non-judgemental sexual history, using culturally appropriate terms, approaching partner notification, legal requirements, how to invite patients to talk, work flow in the clinic, to provide flexible time for lectures, routine refresher training-enthusiasm to upskill, rarely provided consultations with ‘priority’ populations (LGBTQ, sex workers, people who inject drugs, certain ethnicities, incarcerated, refugees). |
| Parkes et al. (2020), UK 107 | 7019, Ages 16–74 but approximately 50% over 40, and ages analysed in groups, women, gender identity not specified, presumed cisgender, 88% White | Quantitative. Latent class analysis from NATSAL-3. Purposive sampling. | Identify clusters of sexual health markers with their socio-demographic, health and lifestyle correlates. | High. | 6 Classes found for women, for example, 7% ‘unwary STI risk takers’. |
| Politi et al. (2009), USA 108 | 40, Mean age 55, women, gender identity not specified, presumed cisgender, unmarried women, 73% college degree, 98% White | Qualitative. Interviews. Convenience sampling. | Describe the experience of middle aged and older aged unmarried women’s communication with HCPs about Sexual Health. | Moderate (not generalisable). | Sexual minority women hesitant to share information due to previous negative experiences when disclosing sexuality. Unmarried women more likely to disclose information about sexual health if perceive HCP does not make assumptions and appears non-judgemental. Unmarried women more comfortable talking to female providers about sexual health. |
| Reese et al. (2020), USA 109 | 144, Mean age 56, women, gender identity not specified, presumed cisgender, 62% partnered, 67% White, 27% Black/African American, 4% Hispanic/Latina | Quantitative. Cross-sectional study. Web-based baseline self-report surveys. Convenience sample. | How commonly women sought help for sexual health concerns after breast cancer treatment and from whom, and whether help-seeking was associated with sexual function/activity/self-efficacy. | High. | Women seeking help were younger and more likely to be partnered; 42% sought help from intimate partners, family/friends; 24% from HCPs, 19% from online/print materials. Women seeking help from outlets other than HCPs had significantly lower self-efficacy than those who did not. |
| Roberts and Sibbald (2000), UK 110 | 181 General practitioners, 147 Practice nurses | Quantitative. Cross-sectional study. Purposive sampling. | Knowledge and views about HRT. | Moderate | 57% of GPs and 85% of practice nurses wanted more knowledge about HRT. |
| Rostom et al. (2002), Canada 111 | 51, Ages 40–70, women, gender-identity not specified, presumed cisgender, 75% had college or University degree | Quantitative. Randomised trial. | Perceptions of HRT associated risks, barriers to HRT, knowledge of menopause symptoms, decision aids for HRT/menopause. | High. | Realistic expectations score of risk perceptions (heart disease, hip fractures, breast cancer): 35%. Baseline knowledge score: 77%. |
| Samuel et al. (2014), UK 112 | 124, Age range 50–75 years, mean age 52, women, gender identity not specified, presumed cisgender, 83% Black ethnicity | Quantitative. Cross-sectional study. Notes review. Purposive sampling. | Review of care provided to HIV-positive women aged over 50. | High. | 71% Late diagnoses, 42% with advanced/very advanced HIV, 22.6% documented missed opportunities for early diagnosis. |
| Sangaramoorthy et al. (2017), USA 113 | 35, Age: 40–71, 88% between 40 and 59 years, women, gender not specified, presumed cisgender, 32% college or higher education, 28 native-born African Americans, 7 Black African participants | Qualitative. Interviews. Purposive and snowball recruitment. | Perceptions and experiences of HIV-related stigma. | High. | Intersectional stigma is a central feature in lives, at interpersonal, familial/community and institutional/structural levels. Negative responses to gender, age, race and disease. |
| Schneider (1997), France, Germany, Spain, UK 114 | 929, Aged 40–65, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional. Convenience sampling. | Attitudes towards and use of HRT. | High. | Use of HRT: 18% Spain, 55% France; 38%–61% of women had not discussed menopause or symptoms with HCP; 66% women believed they needed more information about HRT. |
| Sevelius et al. (2014), USA 115 | 58, 20 interviewees, 38 focus group participants, 85% aged 40–59, women who identified as transgender women, 85% African-American/Black, 5% Pacific Islander, 5% Multiracial, 5% Caucasian | Qualitative. Interviews and focus groups. Convenience sample. | Barriers and facilitators to engagement in HIV care among transgender women. | High (triangulation across methods). | Mental health problems, substance use, poverty, transphobia, barriers to care. Avoidance of healthcare due to stigma and past negative experiences, prioritisation of hormone therapy, concern about interactions between hormone therapy and anti-retroviral. Culturally competent, transgender sensitive healthcare powerful facilitator. |
| Sillence et al. (2023), UK 116 | 18 Menopause apps | Qualitative and quantitative. Review analysis. | Quality, feature and written review analysis of menopause apps. | High. | Data reports and visualisations empowered app users to seek out help and facilitated conversations with HCPs. Apps with clear links to HCP support, were viewed positively by app reviewers and all three apps with HCP support had ‘good’ quality scores. Few of the menopause apps were explicitly supported by HCPs. Many apps scored poorly in relation to the credibility of the source. |
| Simon et al. (2013), USA 117 | 3530, Age 55–65 years, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Convenience sample. | Postmenopausal women’s knowledge of, and attitudes towards, vaginal atrophy. | High. | 63% Associated vaginal symptoms with menopause; 80% considered vaginal atrophy to negatively affect their lives; 40% Waited 1 year before consulting HCP. |
| Sinko and Saint Arnault (2020), USA 118 | 21, Aged 20–81 (9 aged over 41–50+ and 4 aged 31–40), women, gender identity not specified, presumed cisgender, 78% college degree or higher, 86% Caucasian, 11% African American, 1% Asian | Qualitative. Survivor narratives. Convenience sampling. | Explore nature of Gender-based violence healing. | High. | Contextual factors that influence healing: societal expectations, social reactions to self-disclosure, normalisation of violence. Internal themes of shame, self-doubt, self-blame, fear of judgement. Healing: reconnecting with self (reclaiming identity, managing symptoms, regaining control); reconnecting with others (sense of belonging, relating to others); reconnecting with world (releasing negativity, living a purposeful life). |
| Solomon et al. (2021), UK 119 | 661, Aged 45–60, median age 49, women, gender identity not specified, presumed cisgender, 44% completed University, 72% Black African, 8.4% White UK, 19.4% other | Quantitative. Cross-sectional study. Convenience sampling. | Association between HIV clinic attendance and ART adherence and menopausal symptoms. | High, large study, majority Black African. | Severe menopausal symptoms associated with suboptimal ART adherence and HIV clinic attendance. |
| Strohl et al. (2015), USA 120 | 215, Age range 18–70, average age 50, women, gender not specified, presumed cisgender, 22% married, 38% college graduate or above education, 100% African American/Black | Quantitative. Cross-sectional study: survey. Convenience sampling. | HPV knowledge and awareness. | High (but not generalisable (100% African American/Black)). | Knowledge of HPV, cervical cancer and HPV vaccination was low. |
| Studts et al. (2012), USA 121 | 345, Aged 40–64, women, gender identity not specified, presumed cisgender, 61.2% married, 95.1% White | Quantitative. Randomised controlled trial, single-blind, two-arm. | Effectiveness of faith-based lay health advisor intervention to improve cervical screening rates in an area of low screening rates. | High (but homogenous study population). | Significantly more likely to have smear if baseline report of recent prior smear. |
| Studts et al. (2013), USA 122 | 345, Ages 40–64, mean age 51, women, gender not specified, presumed cisgender, 64% High-school education or less, 61% Married, 95% Non-Hispanic Caucasian | Quantitative. Cross-sectional study: 88-Item questionnaire (built using qualitative research). Recruited from Churches. Convenience sampling. | Barriers to cervical cancer screening. | Moderate (results not generalisable as recruited from churches and homogeneous ethnicity). | Fear, worry and embarrassment prevented screening. Erroneous beliefs (that a person who has cervical cancer would have symptoms) prevented screening. Lowest perceived income adequacy, lowest perceived health status more likely to report fear of cancer being detected (significant emotional barrier). Access to healthcare facilities, health insurance coverage, cost of testing, limited transport options, lack of physician recommendation/interaction. More likely to screen if could use home kit. |
| Taylor et al. (2017), USA 123 | 50, Ages 50–69, mean age 56, women, gender identity not specified, presumed cisgender, 48% more than high school education, 90% Black or African American | Qualitative. Interviews and focus groups. Convenience sampling. | Explore importance of sex and sexuality among women living with HIV to identify their sexual health and HIV prevention needs. | High. | Sexual pleasure increases with age. Sexual freedom (from the fear of pregnancy and traditional gender norms – expectations of being in a committed relationship or needing financial support, have more partners, sex when they like). Less pleasurable due to partner and relationship characteristics (partner’s inability to perform, unhappiness with relationships, trapped in sexless relationship). Changes in sexual abilities (physical limitations, increase or decrease in desire, ageing as barrier/improvement to orgasm experience, impact of comorbidities). Sexual risk behaviours (many condomless sex, relationship dynamics important for not practising safe sex). Ageist assumptions about sex lives and serostatus (belief older women should not be sexually active, younger men perceive sex with older women is lower risk behaviour-expectation they can have condomless sex) many fought against these stereotypes. STI prevention for older women living with HIV should promote ways to maintain satisfying and safe sex lives. |
| Thames et al. (2018), USA 124 | 45, Ages 50–80 years, African-American, women, gender not specified, presumed cisgender | Qualitative. Focus groups, followed by community-based conference. Convenience sampling. | Community-based participatory research approach to analyse sexual health behaviours and mental health. | High. | Depression, loneliness and self-esteem issues reasons for engaging in high-risk sexual behaviours. Women did not feel comfortable discussing sexual practices with their physicians, partners, or friends. |
| Tortolero-Luna et al. (2006), USA 125 | 235, 35–61 Years (62% aged between 40 and 61), women, gender not specified, presumed cisgender, 58% less than high school education, 80% married or co-habiting, Hispanic women (92% from Mexico) | Quantitative. Cross-sectional. Survey questions. Univariate and multivariate analysis. Convenience sampling. | Assess how English language use by Hispanic women affects their preferences for participating in decision-making and information seeking regarding medical care. | Moderate (difficult to distinguish between effect of language and effect of culture). | Decreased use of English language associated with less desire to participate in medical decision making. Increased use of English language may influence Hispanic women’s preferences for participating in medical decisions and their information-seeking behaviour. |
| Valanis et al. (2000), USA 126 | 93, 311, Aged 50–79, women, gender not specified, presumed cisgender, 40 study centres with range of geographic and ethnic diversity, 85% White but attempted to recruit mixed ethnicity | Quantitative. Cohort study. Questionnaire. Convenience sample. | Compare heterosexual and non-heterosexual women on demographic characteristics, psychosocial risk factors, screening practices, health-related behaviours associated with increased risk of diseases. | Moderate (quality-lower proportion of non-heterosexuals than ideal). | In bisexual and homosexual women: lower cancer screening rates. Lesbian and bisexual women had more risk factors for reproductive cancers. Women reporting never having had sex as adults had lower Pap screening rates and lower rates of HRT use. |
| Van Dommelen et al. (2022), USA 127 | 220, Physicians and advanced practice providers (182 OBGYN, 38 family/internal medicine) | Quantitative. Cross-sectional. Questionnaire. Convenience sampling. | Identify barriers to screening for sexual dysfunction among HCPs. | High. | Primary barrier for OBGYNs time constraints, for primary care provider not having enough knowledge. |
| Vazquez et al. (2007), USA 146 | 440, 43% Over age of 45, 32% aged 35–44, women, gender identity not specified, presumed cisgender | Quantitative. Cross-sectional study. Survey. Convenience sample. | Women’s perceptions of issues they face with diagnosis of epilepsy. | High (but not generalisable). | 31% of Women with epilepsy knowledgeable about menopause; 28% Discussed menopause with HCP but 52% wanted more info; 48% very concerned about impact of antiepileptic drugs on menopause. |
| Walter et al. (2004), UK 128 | 40, Aged 50–55, women, gender identity not specified, presumed cisgender | Qualitative. Focus groups and interviews. Convenience sampling. | Women’s understanding of risk associated with menopause and HRT. | High (but not generalisable). | Women request unbiased, truthful, summarised, personalised, information. Barriers to optimal risk communication and decision making were lack of HCP time, GP attitudes and poor communication. |
| Walters et al. (2021), USA 129 | 35, 31% Aged 36–50, 50% aged over 50, 32 cisgender, 3 transgender, 37% Heterosexual, 31% some college or more (education), 46% Hispanic/Latina, 46% Non-Hispanic Black, 9% Non-Hispanic White | Qualitative, interviews. Purposive recruitment. | Barriers and facilitators to HIV PrEP education intervention. | High. | 51% Had previously heard about HIV PrEP (although many had behaviours that would put them at risk of HIV). Facilitators: offering other health and social services as well, women-focused approach, peer-outreach and navigation. Barriers: concerns about side-effects or interactions, concurrent health-related conditions or appointments, insecure housing and travel, caring responsibilities. |
| Watts and Jen (2023), USA 130 | 27, Aged 39–57, women, gender identity not specified, presumed cisgender, 70% in long-term relationship, 74% heterosexual, 7% lesbian, 11% bi- or pan-sexual, 4% gender fluid, 4% asexual, 80% bachelor or postgraduate degree, 59% White ethnicity, 11% White Jewish, 15% mixed ethnicity, 1% Asian, 1% Latina, 1% no race given | Qualitative. Interviews. Purposive and snowballing recruitment. | Investigate perceptions and interpretations of midlife women’s sexual experiences and changes about sexual engagement, unwanted sexual experiences, body image, sexual healthcare. | High. | Increasing age and sexual-minority group associated with worse healthcare experiences. New lack of sexual desire: sometimes loss, sometimes relief. Relieved to no longer feel like sexual objects. After divorce-renewed sense of autonomy over sexual experiences, renewed interest in sex with new partners. Interdependence between their sexual experiences and other important people in their lives. Growth in sexual expression-increasing awareness of own sexual needs. Legacy of unwanted sexual experiences. Overwhelmingly negative healthcare experiences, felt dismissed, ageist, sexist or heterosexist attitudes – deep scepticism of HC system’s ability to meet needs. Representation matters – want more women and more minorities as providers. Those who also worked as HCPs expressed concern that there is very little training for HCPs about needs of midlife women. Positive experience if provider normalised age-related changes and provided honest and direct communication. |
| Weng et al. (2001), UK 131 | 581, Aged 45–54, women, gender not specified, presumed cisgender | Quantitative. Cross-sectional study. Convenience sample. | Factors associated with physician recommendation of HRT. | High. | Black women significantly less likely than White women to report being advised about HRT. |
| Wigfall et al. (2011), USA 132 | 2027, Aged 50–64, women, gender identity not specified, presumed cisgender, 6 deep-South States, majority had college or higher education level, majority Non-Hispanic White, but good Non-Hispanic Black representation | Quantitative. Cohort study. Convenience sample. | HIV testing uptake among postmenopausal women. | High. | 26% Had ever had HIV test (excluding blood donation testing); 14% had most recent test during post-reproductive years. Women aged 50–54 were 25% as likely to have been tested for HIV as women 60–64. Non-Hispanic White women were half as likely as Non-Hispanic Black women, and rural women 30% as likely as urban women, to have had most recent test during post-reproductive years. |
| Wilson et al. (2013), USA 133 | 10, Ages 28–55 years, women who identify as transwomen, African-American | Qualitative. In-depth interviews. Convenience sampling. | Barriers and facilitators to HIV care and support services. | Moderate(demographic details (age in particular) unclear, all participants same ethnicity). | Gender-related stigma: socially excluded and isolated; peer distrust; institutional distrust-negative experiences in HIV care system. Facilitators: instrumental support (incentives to meet their basic needs), emotional and informational support, access to gender-related care. Transportation and safe and anonymous location of services. Social connectedness. |
| Wong et al. (2018), Hong Kong 29 | 40, Age 42–65 years, gender identity not specified, presumed cisgender, Chinese Cantonese | Qualitative. Interviews. Convenience sampling. | Impact of menopause on sexual health. | High. | Lack of information – suggestion to give information specifically about sexual health (how physical and emotional changes influence sex life and strategies) instead of general menopause symptoms. Cultural taboos – lack of open dialogue about sex and menopause – unsure what is ‘normal’. Seminars, pamphlets for women, documentaries, storytelling programmes, adverts, newspapers/magazines useful sources of information. Financial constraints to seeking healthcare. |
CASP, Critical Appraisal Checklists; HCP, healthcare professionals; HPV, human papilloma virus; HRT, hormone replacement therapy; SHSW, sexual health and sexual well-being; STI, sexually transmitted infection.
Study locations
Most of the studies were conducted in the United States (46), and the United Kingdom (17), with the remaining being conducted in Canada (7), Australia (2), Hong Kong (1), Israel (2), Spain (1), Italy (1), Ireland (1), Spain and Serbia (1), England, Finland, Denmark, New Zealand, Australia and United States (1) and Europe (1).
Design of included studies
Studies included in the review were quantitative (45), qualitative (30) and mixed methods (six). Of those using qualitative methods, nine employed focus group discussions, 16 used interviews, four used both focus group discussions and interviews and one was a qualitative content analysis. Of those employing quantitative methods, one was a review analysis, 10 were cohort studies, 32 were cross-sectional studies and two were randomised trials. Mixed methods trials included cross-sectional studies linked with interviews (three) or interviews (one) and focus groups (one), a cohort study linked with interviews (one) and a mixed quantitative and qualitative content analysis (one).
Study samples
Most studies (60) were presumed to have been conducted on cisgender women, although this was not specifically documented. Ten studies were conducted on transgender women. Three studies were conducted on both transgender and cisgender women. Eight studies were conducted on HCPs.
Recruitment methods
Convenience sampling was the most common method of recruitment (51), followed by purposive sampling (20). Four studies used a mixture of purposive and snowballing sampling, one study used convenience and snowballing sampling, four studies used randomised sampling, one study used ‘mixed recruitment’.
Quality assessment
The CASP checklists 57 were used to critically appraise the studies with systematic consistency (Table 2). Studies were assessed for validity and methodological reliability. Sixty-five of the studies were deemed to be of high quality, 15 of moderate quality and one of poor quality.
Type of SHSW areas examined
The enablers and barriers to accessing different SHSW services were examined. The SHSW services investigated included: sexual experience and function services, cervical screening, human papilloma virus (HPV) and cervical cancer care, HIV and STI testing, primary and preventive care, HIV care, HIV pre-exposure and post-exposure prophylaxis, menopause care, Hormone Replacement Therapy (HRT), gender-based violence services, contraceptive care and women’s health services in general. Thematic extraction of findings (Table 3).
Table 3.
Thematic extraction of findings, based on the socio-ecological model. (specific to people who identify as trans and non-binary in italics)
| Main themes | Sub themes: Barriers | Sub themes: Enablers |
|---|---|---|
|
Intra-personal Intersecting disadvantage of marginalised groups Knowledge and awareness, and behaviourPsychological factor Competing priorities |
Age. Sexuality. Physical appearance. Gender. Gender identity. Immigration status. Language. Cultural group. Racial and ethnic groups. Linguistic ability. Colonial legacy. Level of education. Income. Level of deprivation of area of residence. Area of residence (rurality). Unstable housing. Living with HIV. Sex work. Selling drugs. Previous incarceration. Accuracy, depth and breadth. Use inadequate indicators to assess STI status of partners, for example, demeanour, appearance. Difficulty in differentiating between credible and non-credible information. Internet deemed a confusing medium. Brochures and videos not specific enough and fail to address intensity of symptoms. Repetition of learned unhelpful behaviour, for example, only using condoms if worried about pregnancy. Learned fear: older women have seen women who left the community to get help not returning. Lack of familiarity with condoms. Lack of access to advice for younger women-older relatives are dead/cannot remember/will not talk about menopause. Depression. Loneliness. Poor self-esteem. Self-silencing. Low levels of sexual assertiveness. Felt defensive. Fear. Worry. Embarrassment. Less self-efficacy meant less likely to seek help from HCPs. Prioritising of intimacy over risk. Feelings of intimacy falsely associated with feelings of safety from STIs. Vulnerability of relationship transitions. New lack of desire felt as a relief. Sense of freedom linked with feeling young, resulting in more risk taking. Impact of traumaPhysical changes. Comorbidities (impact of physical and mental health and perceived health status). Stage of the menopause. Fear of side-effects and contra-indications to treatments. Concerned about effect of condoms on erectile dysfunction. Prioritised gender-affirming therapy. Lack of time. Care-giving responsibilities. |
Age. Level of education. More likely to use condoms compared to when younger. Multi-format educational material, for example, consumer decision aids, seminars, pamphlets, documentaries, storytelling programmes, adverts, newspapers/magazines, comprehensive website. In-person options. Support groups. Need for specific information about sexual health during menopause. Peer out-reach. Making accessing services a habitual behaviour, for example, regular smear tests. Mobile health, for example, with podcasts, videos, virtual reality, mindfulness, expert blogs (anonymous, quick to access, evidence-based). No longer felt like sexual objects. Renewed sense of autonomy. Growth In sexual expression and awareness of own needs. Renewed interest in sex. New lack of desire sometimes felt as a loss (prompting help-seeking). Impact of trauma (prompting help-seeking). Stage of the menopause (severity of symptoms may prompt utilisation of other SHSW services). |
|
Intra-personal Interactions with providers Women’s perceptions of HCPs HCP Knowledge and Beliefs Representation in healthcare |
Made to feel dismissed. Ageist. Sexist. Heterosexist. Transphobic. Racist. Embarrassed. HCPs influenced by social taboos. More training required. HCPs reticent to initiate conversations. Uncertainty as to which HCPs could best answer their questions. Descriptions of physicians who make unilateral decisions. Need for better training. Prioritise general over sexual health. Do not ask about sexual well-being even if patients have conditions affecting sex life. Question whether menopause an issue for immigrant women. HCPs prefer women to enter consultations clear and informed about what they want. Women’s Initiative study. |
Knowledgeable, approachable physicians. Supportive and trustworthy. Caring relationships. Holistic care. Personalised. Preventive care. Multi-skilled HCPs. HCPs who broach sexual health topics. HCPs normalise age-related changes. Honest and direct communication. Non-judgemental and do not make assumptions. Appetite for better training. Women should oversee decisions. Women who consulted HCPs found them useful. Decision aids could enable discussions More women. Better cultural and minority group representation. |
|
Organisation factors Perception of HC systems Format of HC systems |
Institutional distrust. Sceptical of system’s ability to meet needs. | Integrated educational and emotional support. Interdisciplinary clinics. Organisations incorporating many different services: One-stop, Gender-affirming. STI services incorporated into other healthcare service. Self-testing. Self-service. Women-only clinics. Multiple options of healthcare education. Culturally competent systems. Anonymous locations. Policy change to allow HCPs other than physicians to prescribe HRT. Trans-positive hospital policies. |
|
Community factors Cultural factors Social connection Intergenerational factors |
Stigma. Social norms (age and sex), for example age-gender barriers to accessing condoms in shops/pharmacies. Women view help-seeking appropriate only up to a certain age. Normalisation of condomless sex. ‘Othering’ those at risk of STIs. Paying for sex. Older people should ‘know better’-ashamed to seek help. Normalisation of violence. Mainly women’s responsibilities. Women socialised to minimise discomforts. ‘Couple culture’ – pressure to re-couple. Workplace expectations, minimisation by employees and colleagues. Reluctance to talk about sex with partner prevents help-seeking. Lack of understanding from partner. Sex less pleasurable due to partner or relationship characteristics, for example, partner’s inability to perform, unhappiness in relationship. Lack of recognition and awareness at work about menopause. Without awareness, women felt uncertain of the validity of their own experiences, often questioning themselves and their concerns. Distancing from young people’s risky behaviour yet pressure to adjust to new sexual culture fast. Ageist assumptions from younger men, for example, expectation that midlife women are lower risk so can have condomless sex. Fast progression to sex in new relationships. Condoms associated with youth. Mothers not discussing details of menopause with daughters. |
Social norms: sex as a work-out, sex as beneficial to women’s health. Reconnecting with world. Educating others in community. Interdependence between their sexual experiences and important people in life. More likely to seek help if partnered. Gender-age dynamics on sexual risk negotiation: influence of young relatives on understanding of sexual safety. Fighting against stereotypes of older women not being sexually active. |
|
Public policy Public health messages Material barriers/enablers |
Disconnection from safe sex messaging. Sensationalised media coverage. Excluded by adverts. Cost of services. Transport options. Shortage of appropriate HCPs. Shortage of HCP time. Poor treatment options/lack of research. |
Greater public discussion about sexuality and more positive mid-life representation. PrEP should be advertised all over the city, on the buses, metro stations (subways), on doors everywhere, in doctors’ offices, social media-everywhere possible, with phone numbers to contact, particularly on streets and public places because ‘I learn my information from the street’. Create identifying profile markers to improve focus of strategies. Focus on predictors of risk behaviour rather than predictors of risk status. Country-specific approach required. Facilities closer to home. Insurance coverage. Expertise and skills and range of tests available outside sexual health services. Recall-based screening systems. Incentives (financial) to meet basic needs. Mobile technology, for example, Apps. |
The barriers and enablers to accessing sexual health and well-being services for midlife women (aged 40–65 years) in high-income countries: A mixed-methods systematic review. HC, healthcare; HCP, healthcare professionals; PrEP, pre-exposure prophylaxis; SHSW, sexual health and sexual well-being; STI, sexually transmitted infection.
Intra-personal themes
Intersecting disadvantage of marginalised groups
Twenty-eight studies revealed the intersecting disadvantage of being a midlife woman and belonging to other marginalised groups with relation to accessing SHSW services. There is evidence that age,72,90,108,113,130,134 sexuality,108,130 ‘physical appearance’ as a cause of perceived discrimination, 135 gender,90,134 gender identity,75,99,136 race,99,113,137 ethnicity,96,131,137 immigration status, 61 cultural group,61,78 nationality,87,114 colonial legacy, 98 linguistic ability,78,125 level of deprivation, 89 income, 79 perceived income inadequacy, 121 area of residence, 84 level of education79,82,84,138 and belonging to a stigmatised group,63,74,77,103,113 impact on the ability of midlife women to access SHSW care. This intersecting marginalisation was demonstrated by an Australian study which investigated whether a ‘hub and spoke’ model would improve access to testing for STIs. Primary HCPs reported that they ‘rarely’ provided sexual health consultations for the most marginalised communities, which were identified as lesbian, gay, queer and transexual people, sex workers, people who inject drugs, certain ethnicities, the incarcerated, and refugees. 106
Older age, within the midlife range, often inhibited access to SHSW services:63,66,130,134,109 increased age was associated with worse sexual healthcare experiences, 130 being less likely to consider HIV pre- and post-exposure prophylaxis for HIV, older women who had experienced a premature menopause were less likely to receive treatment than their younger counterparts, 63 and younger women were more likely to seek sexual health help following breast cancer than their older counterparts. 109 Although older age inhibited access to some services, perhaps due to a combination of discrimination, self-advocacy and lack of current knowledge, the wisdom acquired with age, sometimes resulted in improved access to services. Confounding factors such as ethnicity, family poverty status, urbanisation and HIV exposure risk, may have affected the results, but a large cohort study in the United States demonstrated that women aged 60–64 were more likely to have been screened for HIV than women aged 50–54. 132 Similarly, one small study, which investigated the sexual behaviour of midlife women who had experienced incarceration, suggested that (older) women were more likely to use precautions to protect against STIs than when they were younger, and were more likely to co-test with new partners pre-sex compared to when they were younger. 139
Non-heterosexual women faced more barriers to accessing SHSW services than heterosexual women. They described hesitancy seeking help due to negative past experiences after disclosing their sexuality, 108 and worse sexual healthcare experiences. 130 Bisexual and homosexual women in the United States had lower cervical screening rates than heterosexual women; 140 proposed reasons were difficult past experiences, 141 and poor HCP knowledge about when screening was required. 142 One study in the United States found that perceived discrimination due to ‘physical appearance’ (not defined), and gender, were associated with the reduced receipt of cervical smears; 94 the authors suggested that the discrimination that these women perceived to be present may have inhibited their access to screening. The gender imbalance in sexual relationships remains an ongoing issue: two different UK studies found that both women and men frame the necessity to seek help for sexual difficulties predominantly in relation to erectile dysfunction.8,90 It can be postulated that this minimises the importance that women face on seeking help for their own sexual dysfunction. Gender identity also affects midlife women’s access to care:99,103,115,136,143 three studies demonstrated that transphobia was a strong barrier to enrolling in,115,144 and engaging in, 99 HIV care. Transwomen also faced unique challenges when accessing care following sexual assault. 75
Six studies demonstrated that race99,113,132 and ethnicity61,131,137 affected use of preventive healthcare, 60 HIV-testing, 132 HIV-related stigma, 113 HIV care for transwomen, 99 and awareness of HIV PrEP for transwomen. 137 Similarly, Black women were significantly less likely than White women to report being offered HRT, 131 and a study in Israel revealed that Arab women were more likely than Jewish women to present at an advanced stage of cervical cancer. 96 Although, in contrast, one study found that perceived racial discrimination was not found to be associated with receipt of cervical smears, 94 this research had many limitations including the unusually frequent exposure that the study participants had to healthcare services.
Access to HRT varied significantly depending on country of residence.87,114 Despite the fact that self-reported menopausal symptoms did not differ significantly among women of different nationalities, there was a marked difference in the utilisation of hormone therapy, for example with much higher use in France compared to Spain. 87 An analogous finding was that linguistic ability was a barrier to accessing menopause care for Hispanic women in the United States, 78 and affected women’s desire to participate in medical decision-making around menopause issues. 125 Cultural inhibitions and the need for a higher level of assertiveness than previously required when dealing with American providers limited women’s access to menopause care, 78 and an Australian study described the legacy of colonialism as a barrier to women accessing cervical smears. 98
The social determinants of health, 145 including income,79,89,121,122 area of residence, 84 and level of education,79,82,84,138 have been associated with access to SHSW services for midlife women. Sexual and reproductive health behaviour was associated with socio-economic indicators in Spanish women who were born before the 1950s. 84 Both socio-economic inequity in Canada, 98 and lowest perceived income adequacy as an emotional barrier in the United States (higher fear of cancer being detected), 122 have been associated with decreased access to cervical screening. Similarly, in the United States, higher level of income was associated with an increased likelihood of HRT counselling being obtained by women, although the results may be out-dated, as the study was conducted in 1998. 80 A UK-based study found a strong association between HRT prescription rate and socio-economic deprivation. After adjusting for cardiovascular risks, there was an 18% lower HRT prescription rate in the most deprived practices compared with the least deprived. 89 Poverty has also been cited as a major barrier to transgender midlife women accessing HIV care. 115 Likewise, area of residence has been associated with access to SHSW services: American women living in urban areas were much more likely to have been screened for HIV than those living in rural areas. 132 Level of education, a significant factor influencing access to public services, was found to impact on access to SHSW care.61,79,82,98,134 Five studies, investigating HRT, 82 preventive healthcare use, 61 STI testing, 134 cervical screening 98 and likelihood to receive HRT counselling, 80 found positive associations between the level of a woman’s education and their ability to access SHSW services.
Belonging to a stigmatised group, such as being a sex worker, 144 selling 144 and using recreational drugs, 74 having been recently imprisoned, 77 and living with a condition such as HIV,63,113 negatively impacted on access to SHSW for midlife women. For example, engagement in sex work and selling drugs were identified as prohibiting factors for women who required HIV care in the United States. 103 A Canadian study demonstrated that injecting drugs was associated with worse adherence to antiretroviral therapy for midlife women living with HIV. 74 Recent incarceration was found to be independently associated with not achieving HIV virological suppression in a cohort study of women living with HIV in Canada. 77 Although there are many reasons, apart from belonging to a minoritised group, why these women found accessing care challenging, establishing where care is most needed is the first step in disentangling where services should be focused.
Knowledge, awareness and behaviour
Twenty-five studies exploring knowledge about STI risks,24,70 HPV, 120 cervical cancer,95,121 menopause,22,29,34,117,146 HRT,91,111,114,147 contraception, 66 HIV PrEP62,65,85 and HIV Treatment as Prevention,129,148 revealed a poor depth and breadth of SHSW knowledge among midlife women, which was a barrier to accessing services. The incorporation of different formats of education into healthcare systems64,93,100,109 was viewed as an enabler to accessing SHSW services.
Interviews with mid-lifers in the United Kingdom, following the end of long-term relationships, found that participants used indicators such as demeanour and appearance to assess the STI status of new partners. 24 Similarly, very few heterosexual mid-lifers in Scotland used condoms or co-tested with new partners for STIs if their new partners reassured them that they were ‘low-risk’ (few previous partners, recently had a long previous relationship). 70 Indeed, some women cited freedom from the risk of pregnancy as a reason not to use condoms, simultaneously (and perhaps unknowingly) increasing their exposure to STIs.70,123 Unfamiliarity, or inexperience, with condoms after not using them for a long time, also prevented their use. 24 Women in the United States, as recently as 2018, demonstrated disappointing knowledge about contraception and emergency contraception 66 and had poor knowledge about HPV, cervical cancer and HPV vaccination. 120 In focus groups about HIV Pre-exposure Prophylaxis in the United States, women were surprised and angry that they had never heard about it; they advocated for educational campaigns. 85 More reassuringly, although still in need of improvement, an Irish study found that 84% of women were aware of why they should have regular cervical smears. 95 Reflecting the need for access to evolving health education at different stages of women’s lives, a study in the United States in the year 2000 found that women who reported never having had sex as adults had lower cervical screening rates and lower rates of HRT use. 140
Middle aged women’s knowledge about menopause symptoms and management was disappointing.22,34,73,81,126,146 Focus groups in the United States reported a need for (more) reliable, accessible and current information about the menopause. 81 In one study of women living with epilepsy, only 31% had confidence that they were knowledgeable about the menopause; the authors attributed this to inadequate patient–physician communication. 146 An Italian survey found that a minority of midlife women received information about the menopause, and possible therapies, and those who did found it of poor quality. 73 Of 3046 postmenopausal women with vulvar-vaginal atrophy, only 24% attributed their symptoms to the menopause. 34 Breast cancer survivors with menopausal symptoms, in a study in 2013, described difficulty distinguishing between credible and non-credible sources of information, and uncertainty about which HCPs to approach for advice. 147
The importance of multiple formats of SHSW educational resources for midlife women was highlighted,22,64,93,109 regarding sexual health following cancer treatment,64,93 sexual health concerns, 109 the menopause22,78 and HRT. 100 Women attributed the poor quality of information available about HRT as a barrier to making informed decisions, described the internet as confusing, 100 and suggested a comprehensive HRT website, with regular seminars for menopausal women 100 and consumer decision aids summarising the evidence about HRT. 100 Hispanic women were disappointed that brochures and videos were non-specific and failed to address the intensity of their menopausal symptoms. They called for better tailored, individualised information and described a lack of access to advice due to the death of matriarchs, and cultural challenges with asking elders to educate them. 78 Women in Hong Kong felt that information about the physical and emotional changes in the menopause which can affect sexual function should be specifically addressed by HCPs, and suggested seminars and pamphlets, documentaries, storytelling programmes, adverts, newspapers and magazines as useful sources of information. 29 It must be acknowledged that historically limited research about the management of menopause compounded the lack of access to good information and may have influenced the findings of these studies. 149 In a more recent study, nurses in the menopause transition described spending a long time looking for information, with poor results. Due to the widespread use of smart phones, they felt that it should be possible to have quick, easy access at any time in an anonymous way, secure platform with evidence-based information. They described the necessity for digital resources to be culturally sensitive, with podcasts, videos, virtual reality, mindfulness, and expert blogs. 22 Survivors of breast cancer who requested education about sexual dysfunction had a preference for in-person options and support groups. 93 Similarly, women (cisgender and transgender) who were consulted about how to improve their engagement with PrEP education advocated for learning from peers. 129
A facilitator to accessing SHSW services was when women made visiting services into a habitual behaviour. Midlife women in the United States, where there was not a universal screening recall system, were significantly more likely to have a cervical smear if they had one previously. 121 However, not re-assessing personal changes in risk with time and circumstance may have resulted in adverse outcomes for some women. One study found that women’s self-perceived STI risk was sometimes rooted in past long-term relationships: even if they were taking chances with their SHSW, they still viewed themselves as at the same exposure as when they were in a long-term monogamous relationship. 24
Psychological factors
Midlife is a particularly vulnerable phase for experiencing mental health problems. 150 In the United States, rates of depression are highest in women in their midlife, compared to men, and women of other ages. 151 Sexual health problems can be interlinked with mental health challenges, 152 and poor mental health can significantly impact on a woman’s ability to access SHSW care.70,99,102,121,122,124 In addition, poor self-confidence has been associated with holding stigmatising beliefs, 135 and risk-taking behaviour. 124 Midlife women with low levels of self-esteem and sexual assertiveness, and high levels of self-silencing, were more likely to report HIV-stigmatising beliefs than women with higher levels of self-confidence. 135 It can be postulated that holding such views prevented them from accessing services. Women in the United States cited depression, loneliness, low self-esteem and defensiveness, as reasons for engaging in high-risk sexual behaviours.99,124 Similarly in the United Kingdom, feelings of guilt and loss of self-esteem influenced sexual risk taking, and experiencing intimacy was prioritised, and seen as exclusive, to self-protection from STIs. 70 Breast cancer survivors who had lower self-efficacy were more likely to seek help for sexual dysfunction from outlets other than HCPs. 109 Discomfort with thinking about and discussing SHSW, can sometimes be attributed to culturally embedded psychological hurdles to accessing services. Fear, worry and embarrassment have been identified as barriers to cervical screening, 121 two-thirds of postmenopausal women in one study were uncomfortable discussing vaginal atrophy, 102 and discomfort with the topic of sexuality made it hard for cancer patients to seek psychosexual help. 153 The impact of trauma can also pervade healthcare choices, for example one study demonstrated that the experience of trauma was a barrier for adherence to antiretroviral therapy for midlife women. 74
However, some psychological factors, for example the sexual liberation often associated with ageing, have been shown to enable access to SHSW care.123,130 Older women living with HIV in the United States described many different elements which may have prompted them to seek SHSW services: aging was associated with sexual freedom, a growth in sexual expression and increased self-awareness. 123 They described respite from feeling like sexual objects, articulated a renewed sense of autonomy over sexual experiences after divorce and conflicting feelings over a new lack of sexual desire. 130
Competing priorities
Midlife women have many competing priorities. Lack of time to look after themselves,86,153 care-giving responsibilities, 129 increasing prevalence of comorbidities8,61,92,123 and worries about the side effects of treatment and interactions with other medications60,87,90,115,146 can present challenges to accessing SHSW services. Priorities also change with age and circumstance, for example as the risk of pregnancy diminishes, 70 or the need for support with children decreases, 123 factors that have had an impact on SHSW help-seeking, such as the balance of risks versus pleasure, may change.
Stage of the menopause journey was shown to be both a barrier and an enabler to accessing care.74,105 Women aged 40–50 years had better adherence to antiretrovirals than women aged less than 40; the authors suggested that in seeking help for menopausal symptoms, women were exposed to services more often. 105 In contrast, symptoms could interfere with the ability to access care. Two studies found an association between severe menopausal symptoms and suboptimal antiretroviral adherence,74,119 and one study found an association between intensity of menopausal symptoms and reduced HIV clinic attendance. 119
The fear of side effects from treatments (HRT,60,87 HIV PrEP60,85) worry about medication interactions (HIV PrEP on hormone use, 60 hormones on antiretrovirals, 115 antiepileptic drugs and HRT, 146 comorbidity medications on sexual dysfunction treatment 90 ) and other health issues sometimes took precedence over SHSW concerns.76,129 Women described the negative impact of comorbidities on their sex life, physical limitations in sexual activity, and changes in the experience of orgasm, factors which increased their need for, but complicated their access to, SHSW services. 123 Poor self-rated health was associated with less use of preventive care. 61 Women living with HIV were less likely to access hormone therapy for premature menopause than other women. 63 In a UK study, the odds for being sexually active were lower for women who saw themselves as being in bad or very bad health compared with those in very good health. 8 It can be postulated that poor health not only affects the ability to have and enjoy sex, but also to access SHSW services if more sexual activity or satisfaction is desired. Transwomen identified mental health problems as a significant barrier to accessing HIV care63,115 and prioritised gender affirming therapy over HIV PrEP.99,115 Midlife women in the United Kingdom sometimes spent years considering whether to access professional help for sexual difficulties, 90 and 40% of women with vaginal atrophy in one study in the United States waited more than 1 year before consulting a HCP 117 ; this could be attributed to many factors, including competing priorities for their time, attention and health.
Interaction with providers
Four themes emerged about the barriers and enablers imposed by HCPs: women’s perceptions of the knowledge and beliefs of HCPs, the objective knowledge of HCPs, beliefs of HCPs about their own knowledge, and representation of midlife women in SHSW services.
Women’s perceptions of HCPs
Negative encounters with HCPs, including being made to feel dismissed, 130 not taken seriously 90 and encountering ageist, 130 sexist, 130 heterosexist, 130 transphobic, 99 racist 99 and HCP attitudes, fostered an ongoing distrust amongst midlife women of SHSW services. Women in one study in the United States, some of whom also worked as HCPs, felt that HCPs needed more training about the needs of midlife women. 130 Women described poor access to competent physicians, as a barrier to accessing: sexual health following oncological treatment, 93 sexual health in primary care, 76 sexual health concerns, 104 menopause care, 78 sexual dysfunction services for postmenopausal women, 154 transgender competent HIV PrEP care 65 and transgender competent HIV care. 101 In contrast, knowledgeable physicians were described by women as having enabled them to access HRT. 100 The importance of multi-skilled HCPs who could deliver tailored care was highlighted by three studies: women described aspirations to receive personalised, preventative, truthful, unbiased menopause care78,128 and transwomen felt that HCPs should be competent in performing many different roles. 99 Women felt that HCPs should provide more holistic care,30,123 for example they felt that physical activity should have been offered as a possible treatment for the menopause, 30 and sexual satisfaction should have been discussed at the same time that STI care had been offered. 123 Women felt that HCP’s prioritisation of general health over sexual health 34 was a barrier to SHSW services.
Behaviour, such as communication skills, 128 displayed by HCPs influenced midlife women’s access to SHSW care. Women wanted to feel equal in the decision making relationship, 81 and physicians who made unilateral decisions 100 were viewed as barriers to care. Approachable HCPs, who were non-judgemental and did not make assumptions about them, 108 and who were able to develop a good rapport, 76 and normalise age-related changes, 130 encouraged them to access services. Physicians across primary and secondary care and a range of specialties were reticent to initiate conversations about sexual health,76,90,154 yet women stated that they would have preferred physicians to broach sexual health topics.55,102,105,108,124,150 Women surmised that HCPs did not broach sexual health topics due to embarrassment, ageism and social taboos around older women and sex 76 ; it was not specified whether the gender of the HCP made any difference to women’s assumptions.
HCP’s knowledge and beliefs
A range of HCPs support the SHSW of midlife women; the review found there was a need for better training in this subject across this group of professionals.69,75,90,106,112,146 In one study, 52% of women living with epilepsy who had discussed the menopause with their HCP still wanted more information. 146 In the United Kingdom, there were too many missed opportunities to test women for HIV, which had resulted in (preventable) irreversible consequences. 112 Similarly, a different study found that contraception had only been documented to have been offered to 15% of eligible women living with HIV. 69 HCPs questioned whether menopause was even an issue for immigrant Hispanic women, indicated that socialisation to minimise gynaecological discomforts limited the significance of their symptoms, and believed (without any evidence) that women were managing their symptoms through local medicine women. 78 The majority of women in one study, despite having conditions which were known to affect sexual function, had never been asked by their GP about sexual well-being. 90 Furthermore, a large survey in the United States which explored sexual concerns, found that most women wanted to discuss these with a HCP (but had not managed to), but encouragingly the discussion had proved helpful for those who had done so. 104
Compelling evidence demonstrated an appetite among HCPs for better, wider-ranging training.67,75,83,88,106,110,127 A questionnaire for community HCPs about HRT, 110 a questionnaire eliciting nephrologists’ confidence in SHSW for women, 88 a questionnaire investigating barriers to sexual dysfunction screening, 127 interviews exploring competence in sexual healthcare, 67 a questionnaire which determined HCP trainees’ views in delivering perimenopausal care, 83 a study of HCPs caring for survivors of sexual assault 75 and an evaluation of a hub-spoke model, 106 verified lack of HCP confidence in SHSW issues, and a desire for further education among HCPs. Training needs identified included taking a non-judgemental sexual history, using culturally appropriate terms, and management of work flow in the clinic. 106 The initial findings of the Women’s Health Initiative, a large-scale national trial, influenced the professional and public health narrative about the dangers of HRT, 64 and thereby controversially continues to negatively impact on practitioner’s HRT prescribing rates. 155 However, a positive fall-out of the study was that many HCPs expressed the feeling that patients should be the main decision-maker with regard to HRT. 64
Representation in healthcare
A UK-based study which explored women’s midlife transitions, 130 and a study in the United States which investigated unmarried midlife women’s sexual health-seeking behaviour, 108 found that midlife women welcomed more female representation in healthcare. Women in the United States expressed a preference for an older female provider when discussing menopause treatment. 71 Correspondingly, women with type 2 diabetes viewed female HCPs as facilitators to them accessing sexual healthcare discussions, 76 and having a female physician correlated with women having had a cervical smear. 86 Arab women’s low use of preventative healthcare was related to a lack of physicians of the same culture and gender. 61
Organisational factors
Perceptions of healthcare systems
Institutional distrust was a barrier to healthcare services 130 within the remits of: access to HRT, 100 HIV care for women, 113 and HIV care for transwomen.115,123,133,143 Systems which offered emotional and information support together with clinical care were viewed as enablers to accessing care for transwomen.133,156
Format of healthcare systems
Strategies to make healthcare systems more accessible that were proposed centred around combining expertise 88 and services,106,133 and establishing women-only clinics.54,123 Nephrologists suggested that interdisciplinary clinics could improve their ability to manage women’s SHSW needs. 88 Similarly, combining SHSW services,53,54,99,101,129,133,135 co-locating SHSW services within other existing healthcare services, 99 and self-service and self-testing possibilities,97,122 were suggested as possibilities to improve access. HCPs in one study felt that a recall-based system, employed in many other countries, would have improved cervical screening rates among an Aboriginal community in Canada. 98 Canadian women in this study also advocated policy change to allow health professionals other than physicians to prescribe HRT. 100 This would improve access, by increasing the availability of services. Enablers for access to SHSW services that were suggested for transwomen included creating trans-positive environments and services with trans-positive policies, 75 co-location of gender-affirming and other SHSW services,54,99,101,133 and including social care provision. 129 Transwomen preferred services in a safe space away from men,54,123 and valued anonymous services. 133
Community factors
Cultural factors
Although stigma is a cross-cutting theme which affects all levels of the SEM, 157 here we concentrate on the effect of stigma in the community as a barrier to SHSW care. Fourteen studies attributed community-based stigma to be a barrier to midlife women accessing a wide range of SHSW care: sexual function care, 90 postmenopausal sexual healthcare, 154 menopause care,22,29,78 HIV care, 113 preventive sexual health services 135 and specific to transwomen: sexual health,54,133 HIV PrEP 60 and HIV care.99,103,115,133
Social norms influenced SHSW care-seeking behaviour. For example, normalisation of condomless sex with new partners, paying for sex and ‘othering’ of those at risk of STIs, were barriers to SHSW services. 24 Women experienced age-gender barriers to accessing condoms in shops and pharmacies 24 and described seeking help for sexual difficulties as only being appropriate up to a certain age. 90 Cultural expectations of stoicism around menstruation and menopause prevented Hispanic women from seeking help. 78 Similarly, it can be postulated that the stigma and lack of understanding from healthcare colleagues prevented nurses in the menopause transition in one study from seeking help. They described how ‘tiredness related to menopause symptoms was not socially acceptable’, and one woman described how (at work) ‘you just get on with it, that sort of thing’. 22
Evolving cultural landscapes may have complicated women’s ability to access SHSW services. A study which investigated gender-based violence described how the (increasing) normalisation of violence affected the healing process, 118 and this cultural norm may have been a significant barrier to accessing care for some women. At the conclusion of a long-term relationship, some women felt pressured to re-partner to fit into (current) ‘couple culture’, 24 whereas others described how sexual liberation from the fear of pregnancy, and from the traditional gender norms of when they were younger, such as the expectations of being in a committed relationship and needing financial support, 123 meant that they had chosen more partners and sex whenever they wanted, compared to in their younger years. 123 These changes in cultural expectations may have contributed to midlife women struggling to identify when to use SHSW services. However, prevalent social ideas may have prompted some women to seek SHSW care. For example, a content analysis of women’s magazines in the United States found the portrayal of sex as good exercise which benefitted the health of women, and the implication that a woman was responsible for her husband’s sexual fulfilment, as recurring themes, 68 both of which may have encouraged women to access SHSW services.
Social connection
Relationship dynamics and communication affected whether safe sex was practised. 123 Women who were partnered were more likely to seek help for sexual health concerns after breast cancer treatment than those without a partner, 109 but partnership with somebody not interested in (or capable of) sex significantly contributed to sexual inactivity.8,92 One woman described ‘missing the closeness of cuddles before and after’ but also ‘feeling sorry for my husband’ (beta-blockers and arthritis affected his ability to have sex). 8 Another woman explained that because the sex practices she had previously enjoyed with her partner were no longer possible, they did not want to explore alternatives. 8 In a different study, women described sex as less pleasurable compared with when they were younger due to their partner’s impaired sexual performance, and unhappiness and the feeling of being trapped in sexless relationships. 123 These relationship complexities may have made accessing help challenging, even though it may have been desired. Conversely, women in a UK study described continuing to have sex despite a health-related reduction in their own sexual desire for the benefit of their partner. 8 This highlights the need for holistic SHSW services for older couples, which include relationship counselling. Anxiety about communicating with intimate partners had a negative impact on access to services. One study demonstrated how inhibitions relating to conversations about sex with their partner prevented older adults from seeing professional help for sexual difficulties. 90
Studies which investigated the nature of healing from gender-based violence, 118 the repercussions of trauma experienced by transwomen living with HIV, 54 and the legacy of unwanted sexual experiences on midlife women, 123 highlighted themes which encompassed the need to learn how to reconnect with others, and the importance of belonging to a community in terms of facilitating access to SHSW services. Similarly, an exploration of the inclusion of transwomen in HIV services found that ciswomen’s openness to education about trans issues was much better than the trans community expected. If their receptivity had been recognised, social connection and enhanced inclusivity in services may have been accomplished more successfully. 54 Without awareness and understanding from colleagues, nurses in the menopause transition felt judged and uncertain of the validity of their own experiences. 22 It is likely that if women working in healthcare settings are sometimes expected to minimise their menopause symptoms, women in other workplaces may also be discouraged from accessing care by the expectations of employers and other employees.
Intergenerational factors
Midlife women matured in a context of different sexual norms, sex education and SHSW campaigns. Midlife nurses in one study explained how female relatives had not helped to prepare them for the menopause by not discussing their experiences in any detail or depth. 22 In contrast, one study demonstrated that younger relatives positively influenced midlife women’s understanding of sexual safety, and thereby enabled access to care. 24 Women in a study in the United States railed against ageist stereotypes about their sex lives. They narrated how younger generations thought older women should not be sexually active, and how younger men perceived sex with older women as lower risk behaviour, and therefore expected condomless sex. 123 Their ability to challenge this fallacy may have empowered them to access appropriate SHSW services. In contrast, other studies depicted midlife women as othering themselves from young people’s behaviour, despite engaging in similar risks. While midlife women perceived condoms as associated with youth, 24 they also described pressure to adjust to a new sexual culture quickly, leading to rapid progression to sex in new relationships. 70
Public policy
Public health messages
In a study about risk taking in 40–65 year olds, participants described disconnection from safe sex promotional services. 24 The study identified a discrepancy between the positive broader public discussion about sexuality, and the sensationalised media coverage of sex in older women. 24 These confusing messages may have contributed to increased stigma and discomfort around sex in the midlife and may have affected women’s decisions to access SHSW services. When discussing HIV PrEP campaigns, there was a concern that information was not available in the places that midlife women would frequent: they advocated for it to be advertised all over the city on the buses, metro stations, on doors, in doctors’ offices and social media, with phone numbers to contact. 85 Transwomen described the need for better quality of public health campaigns. They worried about the need for clarity in messages about the lack of interactions between feminising hormones and HIV PrEP 65 and felt that HIV PrEP adverts needed to include trans-specific messages 60 in order to begin to tackle some of the barriers to uptake.
Although there are many barriers and enablers to SHSW care that are uniform across high-income countries, public health messages may benefit from being country specific. An international survey of four high-income countries found marked differences between the nations: 51% of postmenopausal women in the United States compared to 10% in Finland were aware of local treatment options for vaginal atrophy. 158 There was a similar significant discrepancy between high-income nations in a study which examined HRT prescription rates. 87 The identification of risk behaviours and group or nation-specific problems could help to target messages, for example, Parkes’s latent class analysis of NATSAL-3, which identified six classes for women, including ‘unwary STI risk takers’. 107
Material barriers
The material barriers to accessing SHSW which were identified included: financial challenges,121,133 transport difficulties,121,129 shortage of both HCPs and the time that they can offer78,83,98,100,127,128 and poor mainstream treatment options. 78 Cost of care was found to be a barrier to accessing cervical screening 122 and HIV care 133 in the United States, SHSW services during the menopause in Hong Kong, 29 and bioidentical HRT in Canada. 100 Transwomen living with HIV proposed that financial incentives to meet their basic needs would be a facilitator to accessing HIV care. 133 Similarly, some women discussing HIV PrEP in focus groups in the United States felt that financial incentives should be attached, although others felt that preventing HIV itself should be the incentive. 85 Limited transport options were found to be barriers to accessing cervical screening in Canada 98 and the United States,98,122 and HIV care in the United States. 133 Both women and HCPs felt that better availability of HCPs would improve access to SHSW services. A shortage of appropriate HCPs 98 and not having a primary care physician 86 were associated with worse cervical smear uptake in the United States. HCPs felt that lack of consultation time was a significant barrier to providing good SHSW services,78,83,127 particularly in relation to menopause care78,83 and sexual dysfunction care. 127 The lack of treatment options available for conditions affecting midlife women’s SHSW, such as sexual dysfunction, 90 and menopause,34,87 may inhibit women from seeking, and HCP from offering, some SHSW services. A woman in one study expressed ‘I talk to mums everyday about babies and everything . . . there are so many variations on how it is for premenopausal women, like maybe we don’t really understand enough’. 22 The lack of prioritisation for research into treatment options for conditions that affect midlife women means that even for those women who are able to access care, it can often feel fruitless.
Mobile technology, for example, applications have been used to improve access to menopause services. 116 An analysis of 18 menopause applications found that data reports and visualisations encouraged application users to seek out help and facilitated conversations with HCPs. 116 In particular, applications with clear links to HCP support were viewed positively by application reviewers, and all of the three applications with HCP support had ‘good’ quality scores. 116 Importantly, however, few of the menopause applications were explicitly supported by HCPs, and many scored poorly in relation to the credibility of the source. 116 A different study corroborated this: only 22.7% of the applications analysed had documented evidence-based practice in the form of guidelines or treatment protocols. 41
Discussion
To our knowledge, this is the first systematic review of the evidence that addresses the barriers and enablers to SHSW care for women aged 40–65 years in high-income countries. The gender disparity in healthcare research, 159 the ethical challenges of conducting SHSW studies 160 and the sociocultural pressures of the midlife phase, 18 together with the increasing prevalence of general health issues which may both impact on sexual health and facilitate increased access to HCPs, 24 resulted in limited, evolving and sometimes conflicted evidence with regard to the factors affecting access to services. Most research to date has identified the barriers and enablers that cisgender women encounter in accessing sexual health services. Encouragingly, there is increasing representation of transwomen in the literature and a developing recognition of the importance of sexual well-being.
The limited number of interventions that have been trialled to improve access to SHSW services for midlife women have mostly been found to be efficacious. 161 The majority of successful interventions have included education or knowledge sharing (including health literacy and support and healthcare system navigation), been tailored to the specific population or sub-population (e.g. cancer survivors) and have included a diversity of methods of communication with which to engage participants.162 –168 Studies indirectly exploring interventions to improve access to SHSW care in midlife women living with and surviving cancer provide valuable insights to guide future research. Examples include evidence for readily accessible self-treatments such as comparison between vaginal lubricants in breast cancer, 169 physical activity to improve sexual well-being in endometrial cancer 170 and technological psychoeducational interventions for breast, colorectal and gynaecological cancer survivors (telephone, text and internet approaches) which were found to reduce geographical barriers and confer convenience (ill health, competing care giving/work responsibilities) and privacy advantages.166,171
Consistent evidence has emerged about the wide disparity in access to care within the high-income setting. The intersecting disadvantage of being a midlife woman from an under-resourced group provides a clear indication as to where services should be focused. There is compelling evidence, and appetite for, multi-format, updated, education about SHSW issues and services for midlife women, their communities and their HCPs (across specialties166,172), not least so that improved, more equitable care can be advocated for. Mobile technology has been employed to democratise menopause education, but information on applications must be evidence-based 40 and extended to other SHSW issues. We must capitalise on both intergenerational and peer-led learning and targeted community action 173 to address unacceptable norms such as the socialisation of women to minimise discomfort, the framing of sexual dysfunction from a solely male perspective and to destigmatise and improve inclusivity of sexual health and well-being services for all midlife women.167,174 Public health messages focusing on predictors of risk behaviour, offering more evidence-based self-care interventions175 –177 and steering the cultural discourse to positive, safe, enjoyable midlife sex for women are required. The impact of poor mental health provision on access to SHSW services should not be underestimated.162,165,178 The false economy of denying midlife women the holistic, free, easily accessible and integrated SHSW services that they deserve must be recognised.
Strengths and limitations of the systematic review
The variety of study designs, comprising of qualitative, quantitative and mixed methods studies, prevented meta-analysis of findings. However, the inclusion of a wide range of methodologically diverse studies, and the narrative synthesis, enabled the emergence of complex themes, providing an in-depth understanding of the barriers and enablers to SHSW care for midlife women. The qualitative evidence complemented the quantitative results. For example, cohort and cross-sectional studies identified the more marginalised groups of women, and qualitative findings helped to describe the barriers faced by those women in their own words or the words of their HCPs.
SHSW services are deliberately combined in this review in an effort to support the World Health Organization’s approach of acknowledging positive sexuality and sexual experiences as key public health outcomes that are intrinsically linked with sexual health. 11 However, SHSW services are inconsistently conceptualised. Although the review sought to include all SHSW services as per Mitchell’s 2021 framework, 11 SHSW services in high-income countries that have been defined in different ways may not have been captured. Many of the included studies excluded an important group of transgender and gender non-binary people who have SHSW needs and experiences that are similar in some ways, but also unique, to those of cisgender women. 179 Research lags behind our understanding of the imperative necessity to recognise and distinguish between the needs of women with non-binary and transgender identities. Most studies included in the review are presumed to have been conducted on cisgender women, but we are unable to differentiate women who were not asked, and those who did not want to reveal their gender identities. Therefore, we are unable to judge whether the review reflects access to care for non-binary and transwomen.
The exclusion of non-English language articles may have resulted in the lack of representation from important national and cultural perspectives. Furthermore, most studies were conducted in English-speaking countries, which impacts on the generalisability of the results for women living in non-English speaking countries. Although this review investigated the barriers and enablers to accessing care for women in high-income countries, only a small number of studies specifically addressed access to care for women resident, but who had not been born in, these countries. These women have unique needs, and further research is required to elucidate how to distinguish their challenges in accessing care from women resident in the countries in the high-income countries in which they were born.
Strengths and limitations of the included studies
Overall, the quality of the reporting of the studies was high, with sound methodology and valid results. Studies addressed clearly focused issues. Study methodologies were appropriate for the aims of the studies, and closely aligned with the outcome measures. Half of the studies did not include the race or ethnicity of the participants, which may have had a significant bearing on the barriers and enablers to accessing care. When race or ethnicity was specified, most studies attempted to include women of different races and ethnicities, with mixed results.
Strong theoretical foundations for the work were clearly elaborated in most studies. Many studies used convenience sampling strategies, which may have resulted in an overrepresentation of women who were better able to overcome barriers to accessing care, and women who were already seeking care. Qualitative studies used focus groups, interviews or a mixture of both methods considered appropriate for eliciting views on sensitive topics such as SHSW. 180 However, few of the qualitative studies reported on the quality assessment criteria of ‘reflexivity’, the acknowledgement of cultural bias in the researcher–participant relationship. Many of the quantitative studies were cross-sectional studies, either cross-sectional designs or cross-sections from other research samples. Most surveys were administered individually and verbally, modes considered most accessible for those with low literacy. 180 However, some surveys required computer literacy, which will have excluded more marginalised and women in the older bracket of midlife, rendering the findings less generalisable.
Implications for clinical practice and future research
Clinical practice
SHSW is interlinked with many aspects of mental and physical health and should therefore be provided as an important component of holistic care. Midlife can be viewed as a time of opportunity, where education about positive links between the adoption of sexual health and well-being behaviours can promote a healthier older age. HCPs with a range of roles and responsibilities, require and desire better training in delivering, and signposting, midlife women to SHSW services, and should therefore be offered appropriate training to give them the confidence and ability to do so in an inclusive, sensitive manner.
Policy
Maintaining an active, satisfying and fulfilling sexual life as women age is positively linked with life satisfaction. 182 It is evident that policies which optimise SHSW as integral parts of holistic healthcare benefit women and the societies in which they live. There is a crucial need to advocate for policy change and social campaigns aimed at raising awareness among policymakers, workplaces and communities about the SHSW needs of midlife women. Such initiatives are essential for ensuring that appropriate resources and support are allocated to address the unique challenges faced by this demographic. This review demonstrates that midlife women can enjoy the changes that midlife brings to their SHSW but that they face many barriers to accessing research and services. Policies to educate the public and de-stigmatise SHSW and SHSW services are overdue. Women, especially those from the most under-served groups, must have access to high-quality information; this will help to address other barriers to care such as gender-age dynamics and harmful social norms. The competing priorities that midlife women juggle must be acknowledged within policies, by ensuring flexible appointment times, childcare options, knowledgeable employers and considering accessible one-stop or integrated and interdisciplinary services, with innovative delivery such as self-service and self-testing. Inadequate consultation time and lack of skilled HCPs are pervasive issues, and in countries where women pay for SHSW services, cost is a barrier to vital services.
Future research
Research about how to best enable the participation of midlife women, particularly those who belong to under-resourced groups, in SHSW research is needed. Midlife women’s voices can then be used to prioritise management strategies, including treatment options, education, use of technology and implementation of accessible services. Future research should include longitudinal cohort studies for in-depth examination of the sexual health and well-being challenges of midlife women, randomised controlled trials, with implementation science elements, to test service designs, for example women-only services, and targeted public health messages, as well as qualitative research such as in-depth interviews, focus group discussions and co-creation of education and policies, to ensure that midlife women’s voices are always at the forefront of new policies.
Conclusion
The advent of the physiological and psychological changes that midlife brings to women can serve as an opportunity for workplaces, HCPs, communities, healthcare organisations and women themselves to evaluate, improve access to and co-create essential sexual health and well-being services. Implementation of changes must be evidence-based, and address the wide disparities in access, and the intersecting disadvantages of under-served groups.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057241277723 for The barriers and enablers to accessing sexual health and sexual well-being services for midlife women (aged 40–65 years) in high-income countries: A mixed-methods systematic review by Kiersten Simmons, Carrie Llewellyn, Stephen Bremner, Yvonne Gilleece, Claire Norcross and Collins Iwuji in Women’s Health
Acknowledgments
We would like to thank the Public Participant Involvement group for their advice, Dr Johann McGavin for his ongoing support, and Scott Innes, Senior Library Assistant at Sussex Health Knowledge and Libraries, for working extremely hard to source some of the articles.
Footnotes
ORCID iDs: Kiersten Simmons  https://orcid.org/0009-0005-2481-5380
https://orcid.org/0009-0005-2481-5380
Carrie Llewellyn  https://orcid.org/0000-0002-9107-8473
https://orcid.org/0000-0002-9107-8473
Stephen Bremner  https://orcid.org/0000-0003-0790-7070
https://orcid.org/0000-0003-0790-7070
Collins Iwuji  https://orcid.org/0000-0003-2045-1717
https://orcid.org/0000-0003-2045-1717
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contribution(s): Kiersten Simmons: Conceptualisation; Investigation; Writing – original draft; Methodology; Validation; Visualisation; Writing – review & editing; Formal analysis; Project administration; Data curation; Resources.
Carrie Llewellyn: Supervision; Writing – review & editing; Validation.
Stephen Bremner: Validation; Writing – review & editing; Supervision.
Yvonne Gilleece: Writing – review & editing.
Claire Norcross: Validation.
Collins Iwuji: Validation; Supervision; Writing – review & editing.
Third-party submission: Not applicable.
Writing assistance: Not applicable.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Not applicable.
References
- 1. Department of Health and Social Care. Women’s Health Strategy for England. Updated August 2022. https://www.gov.uk/government/publications/womens-health-strategy-for-england/womens-health-strategy-for-england#introduction. (n.d.).
- 2. Womersley K, Hockham C, Mullins E. The Women’s Health Strategy: ambitions need action and accountability. BMJ 2022; 378: o2059. [DOI] [PubMed] [Google Scholar]
- 3. Jen S. Sexuality of midlife and older women: a review of theory use. J Women Aging 2018; 30(3): 204–226. [DOI] [PubMed] [Google Scholar]
- 4. Kwiatkowski K, Coe K, Bailar JC, et al. Inclusion of minorities and women in cancer clinical trials, a decade later: have we improved? Cancer 2013; 119(16): 2956–2963. [DOI] [PubMed] [Google Scholar]
- 5. Carvalho AOd, Andrade LBd, Ruano FFLO, et al. Knowledge, practices and barriers to access sexual health of women in the menopausal stages: a cross-sectional study with Brazilian gynecologists. BMC Womens Health 2024; 24(1): 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haesler E, Bauer M, Fetherstonhaugh D. Sexuality, sexual health and older people: a systematic review of research on the knowledge and attitudes of health professionals. Nurse Educ Today 2016; 40: 57–71. [DOI] [PubMed] [Google Scholar]
- 7. Sinković M, Towler L. Sexual aging: a systematic review of qualitative research on the sexuality and sexual health of older adults. Qual Health Res 2019; 29(9): 1239–1254. [DOI] [PubMed] [Google Scholar]
- 8. Erens B, Mitchell KR, Gibson L, et al. Health status, sexual activity and satisfaction among older people in Britain: a mixed methods study. PLoS One 2019; 14(3): e0213835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wellings K, Johnson AM. Framing sexual health research: adopting a broader perspective. Lancet 2013; 382(9907): 1759–1762. [DOI] [PubMed] [Google Scholar]
- 10. Douglas JM, Jr., Fenton KA. Understanding sexual health and its role in more effective prevention programs. Public Health Rep 2013; 128 Suppl 1(Suppl 1): 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mitchell KR, Lewis R, O'Sullivan LF, et al. What is sexual wellbeing and why does it matter for public health? Lancet Public Health 2021; 6(8): e608–e613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martin KM, Woodgate RL. Concept analysis: the holistic nature of sexual well-being. Sex Relationsh Ther 2020; 35(1): 15–29. [Google Scholar]
- 13. Lorimer K, DeAmicis L, Dalrymple J, et al. A rapid review of sexual wellbeing definitions and measures: should we now include sexual wellbeing freedom? J Sex Res 2019; 56(7): 843–853. [DOI] [PubMed] [Google Scholar]
- 14. Harlow SD, Gass M, Hall JE, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Menopause 2012; 19(4): 387–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kingsberg SA, Schaffir J, Faught BM, et al. Female sexual health: barriers to optimal outcomes and a roadmap for improved patient-clinician communications. J Womens Health 2019; 28(4): 432–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thomas AJ, Mitchell ES, Woods NF. The challenges of midlife women: themes from the Seattle midlife Women’s health study. Womens Midlife Health 2018; 4(1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hartmann U, Philippsohn S, Heiser K, et al. Low sexual desire in midlife and older women: personality factors, psychosocial development, present sexuality. Menopause 2004; 11(6 Pt 2 of 2): 726–740. [DOI] [PubMed] [Google Scholar]
- 18. Infurna FJ, Gerstorf D, Lachman ME. Midlife in the 2020s: opportunities and challenges. Am Psychol 2020; 75(4): 470–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Qin P, Syeda S, Canetto SS, et al. Midlife suicide: A systematic review and meta-analysis of socioeconomic, psychiatric and physical health risk factors. J Psychiatr Res 2022; 154: 233–241. [DOI] [PubMed] [Google Scholar]
- 20. Thomas HN, Hamm M, Hess R, et al. Changes in sexual function among midlife women: ‘I’m older . . . and I’m wiser’. Menopause 2018; 25(3): 286–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harper S. Understanding the implications of population ageing for mid-life women. J Br Menopause Soc 2003; 9(4): 147–150. [DOI] [PubMed] [Google Scholar]
- 22. Cronin C, Bidwell G, Carey J, et al. Exploring digital interventions to facilitate coping and discomfort for nurses experiencing the menopause in the workplace: an international qualitative study. J Adv Nurs 2023; 79(10): 3760–3775. [DOI] [PubMed] [Google Scholar]
- 23. Wellings K, Gibson L, Lewis R, et al. ‘We’re Just Tired’: influences on sexual activity among male-partnered women in midlife; A mixed method study. J Sex Res 2023; 60(9): 1304–1317. [DOI] [PubMed] [Google Scholar]
- 24. Lewis R, Mitchell KR, Mercer CH, et al. Navigating new sexual partnerships in midlife: a socioecological perspective on factors shaping STI risk perceptions and practices. Sex Transm Infect 2020; 96(4): 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Office for National Statistics. Living longer: is age 70 the new 65?. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglongerisage70thenewage65/2019-11-19. 2019.
- 26. von Hippel C, Adhia A, Rosenberg S, et al. Sexual function among women in midlife: findings from the Nurses’ Health Study II. Womens Health Issues 2019; 29(4): 291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thomas HN, Chang CC, Dillon S, et al. Sexual activity in midlife women: importance of sex matters. JAMA Intern Med 2014; 174(4): 631–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gibson CJ, Huang AJ, McCaw B, et al. Associations of intimate partner violence, sexual assault, and posttraumatic stress disorder with menopause symptoms among midlife and older women. Jama Intern Med 2019; 179(1): 80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wong ELY, Huang F, Cheung AWL, et al. The impact of menopause on the sexual health of Chinese Cantonese women: a mixed methods study. J Adv Nur 2018; 74(7): 1672–1684. [DOI] [PubMed] [Google Scholar]
- 30. Thomas A, Daley AJ. Women’s views about physical activity as a treatment for vasomotor menopausal symptoms: a qualitative study. BMC Womens Health 2020; 20(1): 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. World Health Organisation. Sexual and Reproductive Health and Rights. https://www.who.int/health-topics/sexual-and-reproductive-health-and-rights#tab=tab_1. 2014.
- 32. Levkovich I, Gewirtz-Meydan A, Karkabi K, et al. Views of family physicians on heterosexual sexual function in older adults. BMC Fam Pract 2018; 19(1): 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Athey RA, Kershaw V, Radley S. Systematic review of sexual function in older women. Eur J Obstet Gynecol Reprod Biol 2021; 267: 198–204. [DOI] [PubMed] [Google Scholar]
- 34. Kingsberg SA, Wysocki S, Magnus L, et al. Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women's VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. J Sex Med 2013; 10(7): 1790–1799. [DOI] [PubMed] [Google Scholar]
- 35. Fileborn B, Thorpe R, Hawkes G, et al. Sex, desire and pleasure: considering the experiences of older Australian women. Sex Relationsh Ther 2015; 30(1): 117–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Simon JA, Davis SR, Althof SE, et al. Sexual well-being after menopause: an International Menopause Society White Paper. Climacteric 2018; 21(5): 415–427. [DOI] [PubMed] [Google Scholar]
- 37. Hinchliff S, Gott M. Seeking medical help for sexual concerns in mid- and later life: a review of the literature. J Sex Res 2011; 48(2–3): 106–117. [DOI] [PubMed] [Google Scholar]
- 38. Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med 2007; 357(8): 762–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kirkman L, Fox C, Dickson-Swift V. A case for sexual health policy that includes midlife and older adult sexuality and sexual health. Int J Aging Soc 2016; 6(2): 17–27. [Google Scholar]
- 40. Gkrozou F, Tsonis O, Godden M, et al. Mobile Health (mHealth) apps focused on menopause: are they any good? Post Reprod Health 2019; 25(4): 191–198. [DOI] [PubMed] [Google Scholar]
- 41. Allen J, Sesti F. Health inequalities and women – addressing unmet needs. London, United Kingdom: British Medical Association, 2018. [Google Scholar]
- 42. Baum F, Musolino C, Gesesew HA, et al. New perspective on why women live longer than men: an exploration of power, gender, social determinants, and capitals. Int J Environ Res Public Health 2021; 18(2): 661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nordell J. The bias that blinds: why some people get dangerously different medical care. The Guardian. 2021. [Google Scholar]
- 44. Short SE, Zacher M. Women’s health: population patterns and social determinants. Annu Rev Sociol 2022; 48(1): 277–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. The World Bank. World Bank Country and lending groups, https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. 2021.
- 46. Sallis JF, Owen N, Fisher E. Ecological models of health behavior. In: Glanz K, Rimmer BK, Viswanath K. (eds) Health behavior and health education: theory, research and practice. San Francisco: Jossey-Bass. 2008, pp. 465–482. [Google Scholar]
- 47. Skovdal M. Theory guiding change at the community level. Maidenhead: Open University Press. 2013.
- 48. Hannah V, Hamsadvani K, Elin CL, et al. Impact of the COVID-19 pandemic on access to and utilisation of services for sexual and reproductive health: a scoping review. BMJ Global Health 2022; 7(10): e009594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Marcell AV, Morgan AR, Sanders R, et al. The socioecology of sexual and reproductive health care use among young urban minority males. J Adolesc Health 2017; 60(4): 402–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gray C, Crawford G, Maycock B, et al. Socioecological factors influencing sexual health experiences and health outcomes of migrant Asian women living in ‘western’ high-income countries: a systematic review. Int J Environ Res Public Health 2021; 18(5): 2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012; 22(3): 276–282. [PMC free article] [PubMed] [Google Scholar]
- 52. Kilanowski JF. Breadth of the socio-ecological model. J Agromed 2017; 22(4): 295–297. [DOI] [PubMed] [Google Scholar]
- 53. Hibbert M, Wolton A, Crenna-Jennings W, et al. Experiences of stigma and discrimination in social and healthcare settings among trans people living with HIV in the UK. AIDS Care 2018; 30(7): 836–843. [DOI] [PubMed] [Google Scholar]
- 54. Auerbach JD, Moran L, Watson C, et al. We are all women: barriers and facilitators to inclusion of transgender women in HIV treatment and support services designed for cisgender women. AIDS Patient Care STDs 2020; 34(9): 392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Long JE, Montaño M, Cabello R, et al. Brief report: comparing sexual risk behavior in a high-risk group of men who have sex with men and transgender women in Lima, Peru. J Acquir Immune Defic Syndr 2019; 80(5): 522–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res 2012; 22(10): 1435–1443. [DOI] [PubMed] [Google Scholar]
- 57. CASP UK. CASP systematic review checklist [Internet]. Oxford: CASP UK, 2018. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Systematic-Review-Checklist_2018.pdf [Google Scholar]
- 58. Ma PHX, Chan ZCY, Loke AY. The socio-ecological model approach to understanding barriers and facilitators to the accessing of health services by sex workers: a systematic review. AIDS Behav 2017; 21(8): 2412–2438. [DOI] [PubMed] [Google Scholar]
- 59. Sidamo NB, Kerbo AA, Gidebo KD, et al. Socio-ecological analysis of barriers to access and utilization of adolescent sexual and reproductive health services in Sub-Saharan Africa: a qualitative systematic review. Open Access J Contracept 2023; 14: 103–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bass SB, Kelly PJ, Brajuha J, et al. Exploring barriers and facilitators to PrEP use among transgender women in two urban areas: implications for messaging and communication. BMC Public Health 2022; 22(1): 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Benyamini Y, Blumstein T, Boyko V, et al. Cultural and educational disparities in the use of primary and preventive health care services among midlife women in Israel. Womens Health Issues 2008; 18(4): 257–266. [DOI] [PubMed] [Google Scholar]
- 62. Blackstock OJ, Platt J, Golub SA, et al. A pilot study to evaluate a novel pre-exposure prophylaxis peer outreach and navigation intervention for women at high risk for HIV infection. AIDS Behav 2021; 25(5): 1411–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bullington BW, Edmonds A, Ramirez C, et al. Premature and early menopause among US women with or at risk for HIV. Menopause 2022; 29(6): 741–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bush TM, Bonomi AE, Nekhlyudov L, et al. How the Women’s Health Initiative (WHI) influenced physicians’ practice and attitudes. J Gen Intern Med 2007; 22(9): 1311–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cahill SR, Keatley J, Wade Taylor S, et al. ‘Some of us, we don’t know where we’re going to be tomorrow.’ Contextual factors affecting PrEP use and adherence among a diverse sample of transgender women in San Francisco. AIDS Care 2020; 32(5): 585–593. [DOI] [PubMed] [Google Scholar]
- 66. Cannon R, Madrigal JM, Feldman E, et al. Contraceptive needs among newly incarcerated women in a county jail in the United States. Int J Prison Health 2018; 14(4): 244–253. [DOI] [PubMed] [Google Scholar]
- 67. Cappiello JD, Boardman MB. Did I learn enough to practice? Reflections of new nurse practitioner graduates in providing sexual and reproductive health care. J Am Assoc Nurse Pract 2021; 34(1): 109–118. [DOI] [PubMed] [Google Scholar]
- 68. Clarke J. Women’s work, worry and fear: the portrayal of sexuality and sexual health in US magazines for teenage and middle-aged women, 2000–2007. Cult Health Sexual 2009; 11(4): 415–429. [DOI] [PubMed] [Google Scholar]
- 69. Dakshina S, Tariq S, Lovatt N, et al. Provision of family planning care to women living with HIV attending two large London HIV clinics. HIV Med 2014; 15: 61. [Google Scholar]
- 70. Dalrymple J, Booth J, Flowers P, et al. Psychosocial factors influencing risk-taking in middle age for STIs. Sex Transm Infect 2017; 93(1): 32–38. [DOI] [PubMed] [Google Scholar]
- 71. Dietz NA, Mijares-Cantrell T, Acevedo D, et al. Women veterans and menopause: knowledge and preferences. Women Health 2018; 58(8): 898–914. [DOI] [PubMed] [Google Scholar]
- 72. Doblecki-Lewis S, Lester L, Schwartz B, et al. HIV risk and awareness and interest in pre-exposure and post-exposure prophylaxis among sheltered women in Miami. Int J STD AIDS 2015; 27(10): 873–881. [DOI] [PubMed] [Google Scholar]
- 73. Donati S, Cotichini R, Mosconi P, et al. Menopause: knowledge, attitude and practice among Italian women. Maturitas 2009; 63(3): 246–252. [DOI] [PubMed] [Google Scholar]
- 74. Duff PK, Money DM, Ogilvie GS, et al. Severe menopausal symptoms associated with reduced adherence to antiretroviral therapy among perimenopausal and menopausal women living with HIV in Metro Vancouver. Menopause. 2018; 25(5): 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. DuMont J, Kosa SD, Abavi R, et al. Toward affirming care: an initial evaluation of a sexual violence treatment network’s capacity for addressing the needs of trans sexual assault survivors. J Interpers Viol 2021; 36(21–22): NP12436–NP12455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Ejegi-Memeh S, Hinchliff S, Johnson M. Sexual health discussions between healthcare professionals and midlife-older women living with type 2 diabetes: an interpretative phenomenological study. J Adv Nurs 2021; 77(3): 1411–1421. [DOI] [PubMed] [Google Scholar]
- 77. Erickson M, Pick N, Ranville F, et al. Recent incarceration as a primary barrier to virologic suppression among women living with HIV: results from a longitudinal community-based cohort in a Canadian setting. AIDS Behav 2020; 24(4): 1243–1251. [DOI] [PubMed] [Google Scholar]
- 78. Esposito N. Agenda dissonance: immigrant hispanic women’s and providers’ assumptions and expectations for menopause healthcare. Clin Nurs Res 2005; 14(1): 32–56. [DOI] [PubMed] [Google Scholar]
- 79. Ettinger B, Woods NF, Barrett-Connor E, et al. The North American Menopause Society 1998 menopause survey: part II. Counseling about hormone replacement therapy: association with socioeconomic status and access to medical care. Menopause 2000; 7(3): 143–148. [DOI] [PubMed] [Google Scholar]
- 80. Ettinger B, Pressman A. Continuation of postmenopausal hormone replacement therapy in a large health maintenance organization: transdermal matrix patch versus oral estrogen therapy. Am J Manag Care 1999; 5(6): 779–785. [PubMed] [Google Scholar]
- 81. Fox-Young S, Sheehan M, O’Connor V, et al. Women’s perceptions and experience of menopause: a focus group study. J Psychosom Obstet Gynecol 1995; 16(4): 215–221. [DOI] [PubMed] [Google Scholar]
- 82. Gazibara T, López-Picado A, Larroy C, et al. A comparative study of climacteric symptoms among two populations of mid-aged women. J Obstet Gynaecol 2022; 42(6): 2178–2184. [DOI] [PubMed] [Google Scholar]
- 83. Gleser H. Sex, women and the menopause: are specialist trainee doctors up for it? A survey of views and attitudes of specialist trainee doctors in Community Sexual & Reproductive Health and Obstetrics & Gynaecology around sexuality and sexual healthcare in the (peri)menopause. Post Reprod Health 2015; 21(1): 26–33. [DOI] [PubMed] [Google Scholar]
- 84. Gomez-Acebo I, Dierssen-Sotos T, Palazuelos C, et al. Changes in individual and contextual socio-economic level influence on reproductive behavior in Spanish women in the MCC-Spain study. BMC Womens Health 2020; 20(1): 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Goparaju L, Experton LS, Praschan NC, et al. Women want pre-exposure prophylaxis but are advised against it by their hiv-positive counterparts. J AIDS Clin Res 2015; 6(11): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Guo YQ, Sims OT. A longitudinal analysis of patient-level factors associated with pap test uptake among Chinese American women. J Racial Ethn Health Disparities 2021; 8(3): 756–762. [DOI] [PubMed] [Google Scholar]
- 87. Heinemann K, Rubig A, Strothmann A, et al. Prevalence and opinions of hormone therapy prior to the Women’s Health Initiative: a multinational survey on four continents. J Womens Health 2008; 17(7): 1151–1166. [DOI] [PubMed] [Google Scholar]
- 88. Hendren EM, Reynolds ML, Mariani LH, et al. Confidence in women’s health: a cross border survey of adult nephrologists. J Clin Med 2019; 8(2): 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hillman S, Shantikumar S, Ridha A, et al. Socioeconomic status and HRT prescribing: a study of practice-level data in England. Br J Gen Pract 2020; 70(700): e772–e777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Hinchliff S, Lewis R, Wellings K, et al. Pathways to help-seeking for sexual difficulties in older adults: qualitative findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Age Ageing 2021; 50(2): 546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Howells P, Modarres M, Samuel M, et al. Experience of hormone replacement therapy in postmenopausal women living with HIV. Post Reprod Health 2019; 25(2): 80–85. [DOI] [PubMed] [Google Scholar]
- 92. Huang AJ, Subak LL, Thom DH, et al. Sexual function and aging in racially and ethnically diverse women. J Am Geriatr Soc 2009; 57(8): 1362–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Huynh V, Vemuru S, Hampanda K, et al. No one-size-fits-all: sexual health education preferences in patients with breast cancer. Ann Surg Oncol 2022; 29(10): 6238–6251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Jacobs EA, Rathouz PJ, Karavolos K, et al. Perceived discrimination is associated with reduced breast and cervical cancer screening: the Study of Women’s Health Across the Nation (SWAN). J Womens Health (Larchmt) 2014; 23(2): 138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kerkhoff BA, O’Connor TC, Plant WD, et al. Poor uptake of reproductive health screening services by female renal transplant recipients. Ir Med J 2006; 99(3): 78–80. [PubMed] [Google Scholar]
- 96. Levin G, Cohen L, Brandt B, Kogan L, et al. Ethnic disparity in cervical cancer stage at diagnosis: a retrospective study in an Israeli referral-center. Int J Gynecol Obstet 2023; 161(3): 769–774. [DOI] [PubMed] [Google Scholar]
- 97. Lippman SA, Moran L, Sevelius J, et al. Acceptability and feasibility of HIV self-testing among transgender women in San Francisco: a mixed methods pilot study. AIDS Behav. 2016; 20(4): 928–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Maar M, Burchell A, Little J, et al. A qualitative study of provider perspectives of structural barriers to cervical cancer screening among first nations women. Womens Health Issues 2013; 23(5): e319–e325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Maiorana A, Sevelius J, Keatley J, et al. ‘She is like a sister to me’. Gender-affirming services and relationships are key to the implementation of HIV care engagement interventions with transgender women of color. AIDS Behav 2021; 25(Suppl 1): 72–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Moro D, Young W, Stein R, et al. Menopausal women’s access path to bioidentical hormone replacement therapy: an exploratory. Int J Pharm Compd 2010; 14(2): 165–169. [PubMed] [Google Scholar]
- 101. Munro L, Marshall Z, Bauer G, et al. (Dis)integrated care: barriers to health care utilization for trans women living with HIV. J Assoc Nurs AIDS Care 2017; 28(5): 708–722. [DOI] [PubMed] [Google Scholar]
- 102. Nappi RE, Kokot-Kierepa M. Women’s voices in the menopause: results from an international survey on vaginal atrophy. Maturitas 2010; 67(3): 233–238. [DOI] [PubMed] [Google Scholar]
- 103. Nemoto T, Iwamoto M, Suico S, et al. Sociocultural Contexts of Access to HIV Primary Care and Participant Experience with an Intervention Project: African American transgender women living with HIV in Alameda County, California. AIDS Behav. 2021; 25(1): 84–95. [DOI] [PubMed] [Google Scholar]
- 104. Nusbaum MRH, Helton MR, Ray N. The changing nature of women’s sexual health concerns through the midlife years. Maturitas 2004; 49(4): 283–291. [DOI] [PubMed] [Google Scholar]
- 105. Okhai H, Tariq S, Burns F, et al. Associations of menopausal age with virological outcomes and engagement in care among women living with HIV in the UK. HIV Res Clin Pract 2020; 21(6): 174–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Ong JJ, Fairley CK, Fortune R, et al. Improving access to sexual health services in general practice using a Hub-and-Spoke Model: a mixed-methods evaluation. Int J Environ Res Public Health 2022; 19(7): 3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Parkes A, Waltenberger M, Mercer C, et al. Latent class analysis of sexual health markers among men and women participating in a British probability sample survey. BMC Public Health 2020; 20(1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Politi MC, Clark MA, Armstrong G, et al. Patient-provider communication about sexual health among unmarried middle-aged and older women. J Gen Intern Med 2009; 24(4): 511–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Reese JB, Sorice KA, Pollard W, et al. Understanding sexual help-seeking for women with breast cancer: what distinguishes women who seek help from those who do not? J Sex Med 2020; 17(9): 1729–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Roberts PJ, Sibbald B. Hormone replacement therapy: the views of general practitioners and practice nurses. Br J Gen Pract. 2000; 50(461): 986. [PMC free article] [PubMed] [Google Scholar]
- 111. Rostom A, O’Connor A, Tugwell P, et al. A randomized trial of a computerized versus an audio-booklet decision aid for women considering post-menopausal hormone replacement therapy. Patient Educ Couns 2002; 46(1): 67–74. [DOI] [PubMed] [Google Scholar]
- 112. Samuel MI, Welch J, Tenant-Flowers M, et al. Care of HIV-positive women aged 50 and over – can we do better? Int J STD AIDS 2014; 25(4): 303–305. [DOI] [PubMed] [Google Scholar]
- 113. Sangaramoorthy T, Jamison A, Dyer T. Intersectional stigma among midlife and older Black women living with HIV. Cult Health Sexual 2017; 19(12): 1329–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Schneider HPG. Cross-national study of women’s use of hormone replacement therapy (HRT) in Europe. Int J Fertil Womens Med 1997; 42: 365–375. [PubMed] [Google Scholar]
- 115. Sevelius JM, Patouhas E, Keatley JG, et al. Barriers and facilitators to engagement and retention in care among transgender women living with human immunodeficiency virus. Ann Behav Med 2014; 47(1): 5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Sillence E, Hardy C, Kemp E. ‘This App Just Gets Me’: assessing the quality, features and user reviews of Menopause Smartphone Apps. J Cons Health Internet 2023; 27(2): 156–172. [Google Scholar]
- 117. Simon JA, Kokot-Kierepa M, Goldstein J, et al. Vaginal health in the United States: results from the Vaginal Health: insights, views & attitudes survey. Menopause 2013; 20(10): 1043–1048. [DOI] [PubMed] [Google Scholar]
- 118. Sinko L, Saint Arnault D. Finding the strength to heal: understanding recovery after gender-based violence. Violence Against Women 2020; 26(12–13): 1616–1635. [DOI] [PubMed] [Google Scholar]
- 119. Solomon D, Sabin CA, Burns F, et al. The association between severe menopausal symptoms and engagement with HIV care and treatment in women living with HIV. AIDS Care 2021; 33(1): 101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Strohl AE, Mendoza G, Ghant MS, et al. Barriers to prevention: knowledge of HPV, cervical cancer, and HPV vaccinations among African American women. Am J Obstet Gynecol 2015; 212(1): 65.e1–65.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Studts CR, Tarasenko YN, Schoenberg NE, et al. A community-based randomized trial of a faith-placed intervention to reduce cervical cancer burden in Appalachia. Prev Med 2012; 54(6): 408–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Studts CR, Tarasenko YN, Schoenberg NE. Barriers to cervical cancer screening among middle-aged and older rural Appalachian women. J Commun Health 2013; 38(3): 500–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Taylor TN, Munoz-Plaza CE, Goparaju L, et al. ‘The pleasure is better as I’ve gotten older’: Sexual health, sexuality, and sexual risk behaviors among older women living with HIV. Arch Sex Behav 2017; 46(4): 1137–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Thames AD, Hammond A, Nunez RA, et al. Sexual health behavior and mental health among older African American women: the Sistahs, Sexuality, and Mental Health Well-Being Project. J Womens Health 2018; 27(9): 1177–1185. [DOI] [PubMed] [Google Scholar]
- 125. Tortolero-Luna G, Byrd T, Groff JY, et al. Relationship between English language use and preferences for involvement in medical care among Hispanic women. J Womens Health (Larchmt) 2006; 15(6): 774–785. [DOI] [PubMed] [Google Scholar]
- 126. Valanis B, Bowen D, Bassford T, et al. Sexual orientation and health: comparisons in the women’s health initiative sample. Arch Fam Med 2000; 9: 843–853. [DOI] [PubMed] [Google Scholar]
- 127. VanDommelen K, Kasper R, McCarter M, et al. What’s preventing healthcare providers from screening for female sexual dysfunction? J Sex Med 2022; 19(Suppl_3): S23. [Google Scholar]
- 128. Walter FM, Emery JD, Rogers M, et al. Women's views of optimal risk communication and decision making in general practice consultations about the menopause and hormone replacement therapy. Patient Educ Couns 2004; 53(2): 121–128. [DOI] [PubMed] [Google Scholar]
- 129. Walters SM, Platt J, Anakaraonye A, et al. Considerations for the design of pre-exposure prophylaxis (PrEP) interventions for women: lessons learned from the implementation of a Novel PrEP Intervention. AIDS Behav 2021; 25(12): 3987–3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Watts A, Jen S. Context-dependent sexual changes during women’s midlife transitions. J Women Aging 2023; 35(6): 542–556. [DOI] [PubMed] [Google Scholar]
- 131. Weng HH, McBride CM, Bosworth HB, et al. Racial differences in physician recommendation of hormone replacement therapy. Prev Med 2001; 33(6): 668–673. [DOI] [PubMed] [Google Scholar]
- 132. Wigfall LT, Richter DL, Torres ME, et al. HIV testing among midlife women in the Deep South: an analysis of the 2008 Behavioral Risk Factor Surveillance System Survey data. J Womens Health 2011; 20(6): 933–941. [DOI] [PubMed] [Google Scholar]
- 133. Wilson EC, Arayasirikul S, Johnson K. Access to HIV care and support services for African American transwomen living with HIV. Int J Transgend 2013; 14(4): 182–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Trujillo D, Arayasirikul S, Xie H, et al. Disparities in sexually transmitted infection testing and the need to strengthen comprehensive sexual health services for trans women. Transgend Health 2022; 7(3): 230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Jacobs RJ, Kane MN. HIV-related stigma in midlife and older women. Soc Work Health Care 2010; 49(1): 68–89. [DOI] [PubMed] [Google Scholar]
- 136. DuMont J, Kosa SD, Hemalal S, et al. Formation of an intersectoral network to support trans survivors of sexual assault: a survey of health and community organizations. Int J Transgend Health 2021; 22(3): 243–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Holder CL, Perez-Gilbe HR, Fajardo FJ, et al. Disparities of HIV risk and PrEP use among transgender women of color in South Florida. J Natl Med Assoc 2019; 111(6): 625–632. [DOI] [PubMed] [Google Scholar]
- 138. Richters J, Grulich AE, de Visser RO, et al. Sex in Australia: contraceptive practices among a representative sample of women. Aust N Z J Public Health 2003; 27(2): 210–216. [DOI] [PubMed] [Google Scholar]
- 139. Emerson A, Valleroy E, Knittel A, et al. Sex and aging: perspectives of older adult women with experience of incarceration. J Women Aging 2023; 35(5): 487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Valanis BG, Bowen DJ, Bassford T, et al. Sexual orientation and health – comparisons in the Women’s Health Initiative sample. Arch Fam Med 2000; 9(9): 843–853. [DOI] [PubMed] [Google Scholar]
- 141. Rankow EJ, Tessaro I. Cervical cancer risk and Papanicolaou screening in a sample of lesbian and bisexual women. J Fam Pract 1998; 47(2): 139–143. [PubMed] [Google Scholar]
- 142. White JC, Dull VT. Health risk factors and health-seeking behavior in lesbians. J Womens Health 1997; 6(1): 103–112. [DOI] [PubMed] [Google Scholar]
- 143. Sevelius JM, Keatley J, Calma N, et al. ‘I am not a man’: trans-specific barriers and facilitators to PrEP acceptability among transgender women. Global Public Health 2016; 11(7–8): 1060–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Nemoto T, Cruz TM, Iwamoto M, et al. A tale of two cities: access to care and services among African-American transgender women in Oakland and San Francisco. LGBT Health 2015; 2(3): 235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014; 129 Suppl 2(Suppl 2): 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Vazquez B, Gibson P, Kustra R. Epilepsy and women’s health issues: unmet needs–survey results from women with epilepsy. Epilepsy Behav 2007; 10(1): 163–169. [DOI] [PubMed] [Google Scholar]
- 147. Balneaves LG, Panagiotoglou D, Brazier AS, et al. Qualitative assessment of information and decision support needs for managing menopausal symptoms after breast cancer. Support Care Cancer 2016; 24(11): 4567–4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Zalazar V, Aristegui I, Socías ME, et al. Ethics and the treatment as prevention strategy among transgender women living with HIV in Argentina. Cult Health Sex 2021; 23(5): 674–689. [DOI] [PubMed] [Google Scholar]
- 149. MacLellan J, Dixon S, Bi S, et al. Perimenopause and/or menopause help-seeking among women from ethnic minorities: a qualitative study of primary care practitioners’ experiences. Br J Gen Pract 2023; 73(732): e511–e518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Gondek D, Bann D, Patalay P, et al. Psychological distress from early adulthood to early old age: evidence from the 1946, 1958 and 1970 British birth cohorts. Psychol Med 2022; 52(8): 1471–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief 2018(303): 1–8. [PubMed] [Google Scholar]
- 152. Montejo AL. Sexuality and mental health: the need for mutual development and research. J Clin Med 2019; 8(11): 1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Decker CL, Pais S, Miller KD, et al. A brief intervention to minimize psychosexual morbidity in dyads coping with breast cancer. Oncol Nurs Forum 2012; 39(2): 176–185. [DOI] [PubMed] [Google Scholar]
- 154. Ling DCY, Wong WCW, Ho SC. Are post-menopausal women ‘Half-a-Man’?: sexual beliefs, attitudes and concerns among midlife Chinese women. J Sex Marital Ther 2008; 34(1): 14–28. [DOI] [PubMed] [Google Scholar]
- 155. Cagnacci A, Venier M. The controversial history of hormone replacement therapy. Medicina (Kaunas) 2019; 55(9): 602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Lippman SA, Sevelius JM, Saggese GSR, et al. Peer navigation to support transgender women’s engagement in HIV care: findings from the Trans Amigas Pilot Trial in São Paulo, Brazil. AIDS Behav 2022; 26(8): 2588–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Stangl AL, Earnshaw VA, Logie CH, et al. The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med 2019; 17(1): 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Nappi RE, Krychman ML. The American-European difference in vulvar and vaginal atrophy views: a lesson from the REVIVE Survey. Climacteric 2016; 19(3): 252–255. [DOI] [PubMed] [Google Scholar]
- 159. Merone L, Tsey K, Russell D, et al. Sex inequalities in medical research: a systematic scoping review of the literature. Womens Health Rep (New Rochelle) 2022; 3(1): 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Stenson AL, Kapungu CT, Geller SE, et al. Navigating the challenges of global reproductive health research. J Womens Health (Larchmt) 2010; 19(11): 2101–2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Tyndall I, Hartland T, Banerjee M, et al. Tailoring sexual health interventions for middle-aged and older adults, including vulnerable populations: a scoping review. Int J Sex Health 2022; 34(4): 593–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Lovejoy TI, Heckman TG. Depression moderates treatment efficacy of an HIV secondary-prevention intervention for HIV-positive late middle-age and older adults. Behav Med 2014; 40(3): 124–133. [DOI] [PubMed] [Google Scholar]
- 163. Echenique M, Illa L, Saint-Jean G, et al. Impact of a secondary prevention intervention among HIV-positive older women. AIDS Care 2013; 25(4): 443–446. [DOI] [PubMed] [Google Scholar]
- 164. DeMarco RF, Chan K. The Sistah Powah structured writing intervention: a feasibility study for aging, low-income, HIV-positive Black women. Am J Health Promot 2013; 28(2): 108–118. [DOI] [PubMed] [Google Scholar]
- 165. Arcos-Romero AI, Calvillo C. Sexual health and psychological well-being of women: a systematic review. Healthcare (Basel) 2023; 11(23): 3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Sopfe J, Pettigrew J, Afghahi A, et al. Interventions to improve sexual health in women living with and surviving cancer: review and recommendations. Cancers (Basel) 2021; 13(13): 3153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Thomas HN, Brotto LA, de Abril Cameron F, et al. A virtual, group-based mindfulness intervention for midlife and older women with low libido lowers sexual distress in a randomized controlled pilot study. J Sex Med 2023; 20(8): 1060–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Seav SM, Dominick SA, Stepanyuk B, et al. Management of sexual dysfunction in breast cancer survivors: a systematic review. Womens Midlife Health 2015; 1(1): 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Hickey M, Marino JL, Braat S, et al. A randomized, double-blind, crossover trial comparing a silicone- versus water-based lubricant for sexual discomfort after breast cancer. Breast Cancer Res Treat 2016; 158(1): 79–90. [DOI] [PubMed] [Google Scholar]
- 170. Armbruster SD, Song J, Bradford A, et al. Sexual health of endometrial cancer survivors before and after a physical activity intervention: a retrospective cohort analysis. Gynecol Oncol 2016; 143(3): 589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Brotto LA, Dunkley CR, Breckon E, et al. Integrating quantitative and qualitative methods to evaluate an online psychoeducational program for sexual difficulties in colorectal and gynecologic cancer survivors. J Sex Marital Ther 2017; 43(7): 645–662. [DOI] [PubMed] [Google Scholar]
- 172. Winkley K, Kristensen C, Fosbury J. Sexual health and function in women with diabetes. Diabet Med 2021; 38(11): e14644. [DOI] [PubMed] [Google Scholar]
- 173. Lomax N, Wheeler H, Anaraki S, et al. Management of a syphilis outbreak in street sex workers in east London. Sex Transm Infect 2006; 82(6): 437–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Metusela C, Ussher J, Perz J, et al. ‘In my culture, we don’t know anything about that’: sexual and reproductive health of migrant and refugee women. Int J Behav Med 2017; 24: 836–845. [DOI] [PubMed] [Google Scholar]
- 175. Yeh PT, Kennedy CE, de Vuyst H, et al. Self-sampling for human papillomavirus (HPV) testing: a systematic review and meta-analysis. BMJ Global Health 2019; 4(3): e001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Ogale Y, Yeh PT, Kennedy CE, et al. Self-collection of samples as an additional approach to deliver testing services for sexually transmitted infections: a systematic review and meta-analysis. BMJ Global Health 2019; 4(2): e001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Courtenay T, Baraitser P. Improving online clinical sexual and reproductive health information to support self-care: a realist review. Digit Health 2022; 8: 20552076221084465. [Google Scholar]
- 178. Moghalu O, Hotaling J, Pastuszak A. Psychiatric comorbidities and sexual health. Curr Sex Health Rep 2020; 12: 91–100. [Google Scholar]
- 179. Moseson H, Zazanis N, Goldberg E, et al. The imperative for transgender and gender nonbinary inclusion: beyond women's health. Obstet Gynecol 2020; 135(5): 1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Liamputtong P. Focus group methodology: principles and practice. London, https://methods.sagepub.com/book/focus-group-methodology (2011, Accessed 1 March 2024). [Google Scholar]
- 181. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf) 2005; 27(3): 281–291. [DOI] [PubMed] [Google Scholar]
- 182. Vasconcelos P, Paúl C, Serruya SJ, et al. A systematic review of sexual health and subjective well-being in older age groups. Rev Panam Salud Publica 2022; 46: e179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057241277723 for The barriers and enablers to accessing sexual health and sexual well-being services for midlife women (aged 40–65 years) in high-income countries: A mixed-methods systematic review by Kiersten Simmons, Carrie Llewellyn, Stephen Bremner, Yvonne Gilleece, Claire Norcross and Collins Iwuji in Women’s Health