Abstract
Depression is a significant mental health challenge globally. While traditional antidepressants are effective, they often have unwanted side effects. Saffron, a natural spice derived from Crocus sativus L., has emerged as a potential alternative therapy for depression. Researchers have found that its components such as crocin, crocetin, and safranal have been found to mitigate depressive symptoms through neurotransmitter regulation, anti-inflammatory effects, and neuroprotection. Clinical trials suggest that the effectiveness of saffron in treating mild to moderate depression is comparable to that of standard medications, and animal studies support these results, showing behavioral improvements with saffron treatment. Saffron is particularly appealing due to its safety and lower incidence of side effects, making it suitable for those sensitive to conventional drugs. Additionally, its antioxidant properties may offer further health benefits. However, challenges such as determining the appropriate dosage, prohibitive cost, and the limited availability of quality saffron need to be addressed. Most research on saffron’s efficacy is short-term; thus, long-term studies are essential to understand its full therapeutic potential and ongoing antidepressant effects. While saffron is safe in terms of its culinary value, higher therapeutic doses require careful monitoring for drug interactions and side effects. In summary, saffron represents a promising direction in depression treatment, with benefits potentially matching those of standard treatments and a better safety profile. However, further research is necessary to establish clear guidelines for its use, optimize dosing, and assess long-term outcomes. Saffron offers a natural treatment path for depression, but its use must be controlled and supported by scientific evidence.
Keywords: Depression, saffron, phytoconstituents, crocin, antidepressant
Introduction
Depression is a major psychological condition characterized by a chronic sense of hopelessness, low mood, cognitive impairment, and loss of interest. It affects the ability of a person to operate on an individual, biological, and societal level. It is characterized by profound sadness, emptiness, grief, despair, and despondency. Over time, it may also lead to neurological dysfunction, difficulties concentrating, altered eating and sleeping habits, an inability to experience joy, and suicidal ideation. Studies have shown that the majority of individuals have experienced at least one depressive episode during their lifetime, with women being twice as likely to suffer from depression compared to men. Despite the availability of other therapeutic modalities, pharmacotherapy has become the most common inpatient therapy for treating depression [1].
The International Classification of Diseases (ICD), which is released by the World Health Organization (WHO), includes depression in a large category of diverse disorders [2]. A few depressive disorders are distinguished by the current ICD-11 version: recurrent depressive disorder (current episode moderate, without psychotic symptoms, or severe, with or without such symptoms, or recurrent depressive disorder currently in full recovery, or unspecified frequent depressive disorder) and single episode depressive disorder (moderate, without psychotic symptoms, or serious, with or without such symptoms) [3].
According to the WHO, depression is a significant mental health disorder that impacts millions of individuals worldwide, irrespective of their age and geographic location. According to the most recent approximations, approximately 251 to 310 million individuals around the globe are struggling with depression. According to the Global Health Data Exchange, depression affects approximately 3.4% of the world’s population, with a possible margin of error that could expand this range between 2% and 6%. WHO offers a more moderate evaluation, estimating that approximately 5% of adults globally suffer from depression, with a higher prevalence among women [4]. The COVID-19 pandemic has had a significant impact, leading to a rise in depression and anxiety worldwide by more than 25% in year 2020. This increase highlights the pandemic’s negative impact on mental health. During this period, researchers identified women and young people as particularly vulnerable groups [5].
The results of the National Mental Health Survey conducted between 2015 and 2016 indicate that almost 15% of adults in India require active intervention for one or more mental health issues. Additionally, it was found that one in 20 Indians was found to suffer from depression. Unfortunately, a considerable number of individuals who are affected by mental health issues do not receive adequate treatment due to various obstacles, such as, a lack of resources, trained healthcare providers, and the social stigma that is associated with mental disorders [6,7].
The discovery of antidepressants in the 1950s significantly transformed depression treatment, leading to a marked decrease in suicide rates among those affected [8]. However, antidepressants come with several drawbacks, such as low remission rates (over 30% of patients do not achieve remission despite multiple treatments) [9] and poor tolerability, with many patients discontinuing their medication within the first few months [10]. Earlier antidepressants, like tricyclic antidepressants (TCAs) and MAO inhibitors (MAOI), were commonly used but are now rarely prescribed due to their adverse health effects [11]. Although newer antidepressants have fewer severe side effects, issues like sexual dysfunction, gastrointestinal problems, and discontinuation syndrome remain concerns [12].
Various pharmacological strategies for treating depression, including increasing the dose of selective serotonin reuptake inhibitors (SSRIs) or TCAs, or combining these with lithium or atypical antipsychotic drugs, have shown encouraging results. However, these findings require further validation [13].
The primary use of ketamine, an antagonist of the N-methyl-D-aspartate (NMDA) receptor for glutamate, is as an anesthetic. However, it has also demonstrated a rapid and significant antidepressant effect. Its addictive properties have been raised about its potential for abuse [14].
Therefore, the need for safe and effective depression therapies has become an increasingly urgent safety concern, and the side effects associated with many antidepressant medications have resulted in an increased focus on herbal psychopharmacology research [8,9]. In recent years, herbal treatments have gained popularity as alternatives to prescription pharmaceuticals for treating major depressive disorder (MDD). The increasing interest in herbal remedies for mental health treatment reflects a broader trend towards integrative and holistic approaches to healthcare. This is because they offer potential benefits such as fewer side effects, lower costs, and alternative options when conventional drugs are ineffective or inaccessible. The WHO has acknowledged the importance of traditional medicine, noting that an estimated 80% of the world’s population relies on herbal medicine for primary healthcare. Numerous studies examining the efficacy of various herbs in treating depression mirror this growing acceptance [15].
Various studies have reported that saffron is associated with fewer side effects than conventional antidepressants, making it an attractive option for patients who may be sensitive to the adverse effects of standard medications [16].
Recent clinical trials have demonstrated that saffron, a spice derived from the plant Crocus sativus L., which is native to Southwest Asia, has emerged as a promising alternative medicine for depression treatment. Iran stands out as the world’s primary saffron producer, accounting for 90% of global saffron output. Moreover, the country has explored the potential therapeutic applications of saffron, including its antidepressant, cardioprotective, and chemopreventive effects. These marked effects are attributed to the presence of potent phytochemicals and bioactive compounds in saffron, such as crocin, crocetin, and safranal. Studies have also highlighted its potential in various medical areas, demonstrating its efficacy in treating conditions such as depression and Alzheimer’s disease and even as an anti-inflammatory and antitumor agent [17,18]. In depression, it has an impact by altering brain chemicals such as serotonin, which is responsible for boosting mood. However, the exact mechanism through which Saffron increases serotonin levels in the brain is still unclear. More precisely, saffron extract may inhibit serotonin reuptake in synapses. By preventing neuronal serotonin reuptake, serotonin remains in the brain for an extended period, thus amplifying its antidepressant effects [19-21].
This comprehensive review aims to explore the potential of phytotherapeutics in comparison to currently available pharmaceutical medications and to identify a safe and effective alternative treatment for depression using saffron, based on recent research findings. The ultimate goal of this effort is to promote patient benefit and alleviate the high global burden of depression.
Major Symptoms and Risk Factors
Depression can cause a range of physical, social, and psychological symptoms that have a significant impact on a person’s quality of life.
The treatment landscape for depression has long been dominated by conventional pharmacological interventions, primarily antidepressants such as SSRIs and serotonin-norepinephrine reuptake inhibitors (SNRIs). While these medications have been effective for many patients, they are not without limitations. Common side effects, including weight gain, sexual dysfunction, and gastrointestinal disturbances, often lead to non-compliance and treatment discontinuation. Additionally, the delayed onset of therapeutic effects, often taking several weeks, can leave patients in distress during the initial treatment phase. As a result, there is a growing recognition of the need for alternative treatment options that can provide effective relief from depressive symptoms without the associated drawbacks of traditional medications.
Additional side effects, such as persistent sadness, a central feature within the intricate network models of psychiatric syndromes, encapsulate a myriad of debilitating symptoms. Anhedonia, the haunting loss of interest or pleasure in once-enjoyable activities, stands as a poignant marker of depressive states, accompanied by cognitive impairments, casting shadows on decision-making and concentration, consequently diminishing productivity. Unfortunately, physical manifestations, such as unexplained aches, headaches, and digestive woes emerge, evading clear medical elucidation. Sleep becomes a battleground, plagued by insomnia or hypersomnia, entwined with the chains of fatigue and depression. Appetite and weight vacillate, mirroring the illness’s disruptive impact on bodily equilibrium. Psychomotor agitation or retardation disrupts the flow of existence, blurring the boundaries of restlessness and inertia. Fatigue, a relentless specter, looms over every endeavor, resisting the solace of rest. Mood variability casts its turbulent shadow, heralding irritability and erratic swings that strain social bonds. Hopelessness and pessimism shroud the psyche, painting life and the future in bleak hues, often accompanied by the suffocating weight of worthlessness. In the dark, whispers of suicidal ideation emerge, demanding immediate clinical intervention to tether the fragile thread of existence (Figure 1) [22-24].
Figure 1.
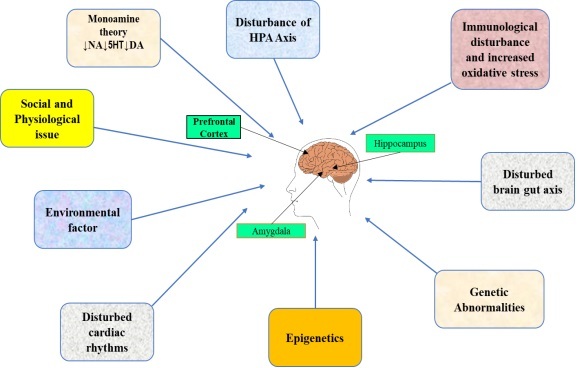
The main pathomechanisms of depression. The main structures associated with the pathogenesis of depression are the prefrontal cortex and limbic system (including the hippocampus and the amygdala) according to the comprehensive, immuno-endocrinological theory of the development of depression, this disease results from the action of multiple exogenous and endogenous factors. Details are given in the text. HPA, hypothalamic-pituitary-adrenal axis; 5HT, 5-hydroxytryptamine; NA, noradrenaline; DA, dopamine.
Current Therapeutics and Their Limitations
A combination of therapies and medications can treat depression. There are several evidence-based options available for treating depression in the therapeutic landscape. Psychotherapy is often the primary treatment for depression. Different forms of psychotherapy have been proven to be effective, including cognitive-behavioral therapy (CBT), which concentrates on modifying negative thought patterns and behaviors. Interpersonal psychotherapy (IPT) aims to enhance problematic personal relationships and social functioning [25]. Psychodynamic therapy addresses unconscious thoughts and feelings and past experiences. Mindfulness-based cognitive therapy (MBCT) combines cognitive therapy with mindfulness techniques [26,27]. Behavioral therapy involves activities that increase pleasure and accomplishments [28]. Neuromodulation techniques such as transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT) are used, especially in treatment-resistant patients [29]. Lifestyle modifications, such as changes in diet, exercise, and sleep patterns can also play a supportive role in managing depression, customized to meet the individual’s needs and preferences [30,31].
When treating moderate to severe depression, doctors typically use a combination of medication and therapy. One common medication prescribed for depression is SSRIs, which have a favorable side-effect profile. SNRIs are also effective in treating both depression and anxiety [32,33]. TCAs are effective in treating depression, but they are less commonly used due to their side effects. MAOIs are reserved for specific types of depression that are resistant to other treatments. Atypical antidepressants are a diverse group of medications that offer alternative options to traditional antidepressants. NMDA receptor antagonists represent a new class of medication that can be used to treat treatment-resistant depression. Research has demonstrated that combining medication with therapy can improve treatment outcomes for individuals with depression [34-36].
Recent studies have shown significant progress in treating depression. One promising treatment for treatment-resistant depression is Stanford’s accelerated intelligent neuromodulation therapy (SAINT), which has had a high remission rate [37]. Physical activities, such as walking, jogging, yoga, and strength training, have been identified as effective ways to alleviate symptoms of depression. Further research is underway to explore innovative treatments such as psychedelics and rapid-acting antidepressants, which will expand the range of therapeutic options available to those suffering from depression. These advancements highlight the personalized nature of depression treatment and the importance of close collaboration between patients and healthcare providers to develop a tailored and effective treatment plan that considers each individual’s unique circumstances (Figure 2) [38,39].
Figure 2.
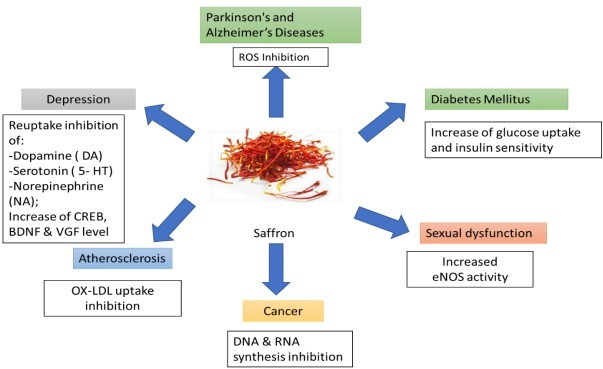
Potential therapeutic applications of saffron.
Current Challenges
The impediments encountered by current therapeutics for depression include a high occurrence of spontaneous recovery and placebo effects, variations in treatment efficacy, side effects affecting compliance, challenges in anticipating treatment results, economic and socio-cultural impacts on clinical protocols, restricted availability of healthcare due to geographical and health inequalities, and deficiencies in clinical supervision [40,41]. Establishing saffron’s efficacy as an antidepressant is challenging due to the variability in study designs and methodologies across clinical trials. Variations in dosages, formulations, and treatment durations have led to conflicting findings. Some trials used standardized saffron extracts, while others used non-standardized saffron powder, making it challenging to compare results and draw definite conclusions about saffron’s effectiveness.
Moreover, many clinical trials had small sample sizes, which limited the statistical power of the findings. For example, a meta-analysis of 12 studies found that while saffron showed significant improvements in depressive symptoms compared to placebo, the overall effect sizes varied widely among the trials. Larger, multi-center studies including diverse populations are necessary to confirm saffron’s efficacy and establish its effectiveness across different demographic groups. These obstacles emphasize the complexity of effectively addressing depression and the need for individualized strategies, pioneering therapies, and increased healthcare accessibility. Overcoming these barriers necessitates a thorough comprehension of patient-specific elements influencing treatment response, advancements in prognostic methodologies such as machine learning, and a comprehensive approach to clinical oversight that integrates awareness, screening, diagnosis, treatment, and monitoring [42,43].
Saffron as a Potential Candidate for Depression Treatment
Saffron (C. sativus) is considered one of the most ancient and highly respected spices, with a diverse range of uses that have been utilized across distinct cultures and periods. According to historical records, the use of saffron in art dates back to approximately 1600-1700 BC, indicating its importance in early civilizations. Initially, grown in the Middle East, the cultivation and trade of saffron spread to regions such as India, China, and the Mediterranean, highlighting its global significance, and it is a quintessential terroir product in Morocco, contributing significantly to the nation’s wealth [44,45].
Research suggests that saffron has potential as a treatment for depression due to its capacity to regulate neurotransmitters such as serotonin, dopamine, and noradrenaline. The proposed mechanism involves inhibiting serotonin reuptake in synapses, thereby prolonging elevated levels and enhancing its positive impact on mood regulation. Numerous clinical trials have demonstrated that saffron possesses antidepressant properties comparable to those of conventional antidepressant medications like fluoxetine, imipramine, and citalopram. A meta-analysis revealed that saffron exhibited a substantial positive effect compared to a placebo for both depression and anxiety outcomes. Additionally, it possesses strong antioxidant properties, which can protect against oxidative stress and inflammation which are the main factors implicated in depression [46-48]. More extensive, well-controlled trials are required to validate the promising existing evidence and confirm the effectiveness, safety profile, and mechanism of action of saffron in the treatment of MDD. The standardization and characterization of active ingredients are also important for advancing research and optional clinical applications [47,48].
Botanical Description
C. sativus is a perennial geophyte from the Iridaceae family and is commonly referred to as saffron. It is known for its crimson stigmas, which are harvested as the world’s most valuable spice. The plant grows from corms and reaches a height of 10-25 cm, with each corm wrapped by numerous concentric spathes that give rise to thin, fibrous roots. The saffron plant is famous for its beautiful flowers, which have six purple tepals, three golden stamens, and red stigmas that are highly prized. These stigmas are long and thread-like and are responsible for the unique color and flavoring properties of saffron [49,50]. The plant’s life cycle is characterized by a reverse growth pattern, where it flowers in autumn, particularly in October and November, and then undergoes vegetative growth until the following spring. The saffron is widely cultivated in the Mediterranean basin and southwest Asia and is not only a botanical wonder but also a cultural symbol that is deeply ingrained in the culinary and medicinal traditions of these regions. Its growth requires specific climatic conditions, with a preference for dry, warm summers and cool autumns. Saffron’s appeal lies not only in its culinary applications but also in its medicinal properties, which can be attributed to its rich composition of bioactive compounds such as crocin, picrocrocin, and safranal which are responsible for saffron’s unique color, taste, and aroma (Figure 3) [51,52].
Figure 3.
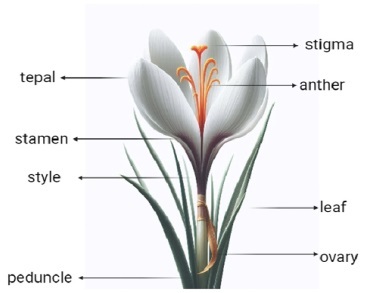
Structure of different parts of the saffron plant.
Phytochemical Constituents and Therapeutic Mechanisms of Saffron
Scientific studies have recently investigated the chemical composition of C. sativus and its associated medicinal properties. The bioactive constituents of saffron include crocin, crocetin, and safranal [53,54], whose vibrant color comes from crocin, a potent antioxidant that has been linked to cardioprotective benefits by safeguarding the heart against various stressors. Crocetin, another significant compound, enhances memory and cognitive functions, contributing to the therapeutic efficacy of saffron. Safranal, which gives saffron its distinctive aroma, has been studied for its antidepressant and anxiolytic effects. It is also known for its role in neuroprotection, particularly in the context of neurodegenerative diseases [55,56]. The characteristic bitter taste of safranin comes from picrocrocin, the precursor of safranal. Picrocrocin also possesses medicinal qualities, although its specific therapeutic effects are less well documented than those of crocin and safranal. The complex chemical composition of saffron includes approximately 10% water, 12% protein, 5% fat, 5% minerals (including essential elements like calcium, phosphorus, potassium, sodium, zinc, and manganese), 5% crude fiber, and 63% carbohydrates. These carbohydrates include starch, reducing sugars, pentosans, gums, pectin, and dextrins, contributing to the nutritional value of saffron. Saffron also contains more than 160 volatile and aromatic compounds, such as terpenes, terpene alcohol, and their esters, which contribute to its unique fragrance and pharmacological profile. The medicinal potential of saffron is supported by its complex array of bioactive compounds. Therapeutic applications of these compounds are vast, ranging from their use in cardiovascular protection to their role in mental health and neuroprotection. Ongoing research continues to unveil the full scope of saffron’s healing capabilities (Table 1) [57,58].
Table 1. Amounts of Active Ingredients Present in Saffron Petals.
| Compound | Amount | Reference |
| Protein | 10.20% | [87] |
| Fat | 5.3% | [88] |
| Ash | 7% | [89] |
| Fiber | 8.80% | [90] |
| Sodium | 25.75 mg/100g | [91] |
| Potassium | 542.13 mg/100g | [92] |
| Calcium | 486.25mg/100g 54213 mg/100g | [93] |
| Copper | 0.87 mg/100g | [94] |
| Iron | 17.99 mg/100g | [95] |
| Magnesium | 2.93 mg/100g | [19] |
| Zinc | 1.80 mg/100g | [96] |
| Phosphorus | 209.90 mg/100g | [97] |
| Kaempferol | 12.6%w/w | [98] |
| Crocin | 0.6%w/w | [99] |
| Anthocyanins | 1712 mg/1 extract | [100] |
| Phenolic compound | 3.42mg | [101] |
Recent studies have examined the complex range of bioactive elements that are found in C. sativus and their multifaceted biological activities. It has a lot of carotenoids, like lycopene, α- and β-carotene, and zeaxanthin, along with the water-soluble apocarotenoid crocetin and its glycosyl esters, which are called crocin. These compounds are primarily responsible for the unique color of saffron and are also associated with a variety of medicinal properties. The therapeutic potential of saffron is extensive, with research emphasizing its antioxidant, anti-inflammatory, anti-cancer, and neuroprotective effects [59,60]. Saffron’s constituents, especially crocin, and crocetin, play a significant role in scavenging free radicals and protecting cells from oxidative stress, thus reducing the risk of genotoxicity and neoplastic transformations in cells. Additionally, saffron and its bioactive components have been linked to chemopreventive effects, indicating a potential role in cancer prevention strategies. The anti-genotoxic effects of saffron help to protect cellular DNA from harmful mutations that could lead to cancer. Considering these properties, saffron remains a topic of interest because of its potential applications in various therapeutic and preventive healthcare settings. Its bioactive compounds, particularly crocin, and crocetin, are currently being investigated for their ability to reduce the risk of chronic diseases and improve overall health outcomes [21,61].
Chemical Composition of Stigma
Studies have delved deeper into the chemical makeup of the saffron stigma, confirming its intricate and diverse profile. The dry red stigma and yellowish style that make up commercial saffron were carefully collected from the C. sativus flower, with each stigma weighing approximately 2 mg. The saffron stigma comprises a fusion of both lipophilic and hydrophilic substances. It comprises carbohydrates, proteins, amino acids, and minerals, which contribute to its nutritional value. Moreover, it is abundant in mucilage, starch, and gums, which enrich its textural properties. Vitamins, such as riboflavin and thiamine, are also present, augmenting their health benefits [62]. The pigments found in saffron, which include crocin, alpha and beta carotenes, mangicrocin, xanthone-carotenoid glycosidic conjugates, anthocyanin, lycopene, flavonoids, and zeaxanthin, provide its vibrant color and antioxidant properties. These pigments, along with alkaloids and saponins, contribute to the medicinal qualities of saffron. Crocetin, its glycosidic derivative (crocin), picrocrocin, and safranal are the primary bioactive ingredients of the stigma. Crocetin and crocin are recognized for their powerful antioxidant capabilities, whereas picrocrocin and safranal add to the distinctive taste and aroma of saffron. These components not only confer saffron with its characteristic attributes but also support its use in various therapeutic applications, including its cardioprotective, neuroprotective, and chemopreventive properties. The ongoing research into chemical composition of saffron continues to reveal its potential as a valuable natural resource for health and nutrition (Figure 4) [63,64].
Figure 4.
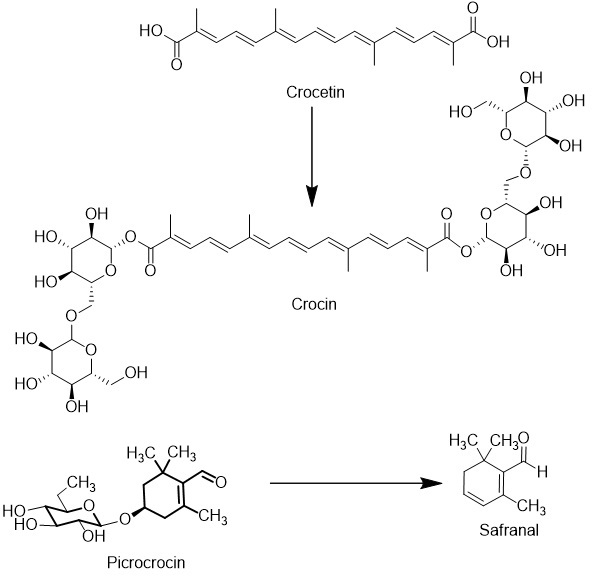
Chemical structures of major components in saffron.
Pharmacological and Biological Activity of Saffron
Saffron exhibits a wide range of pharmacological effects, including strong antioxidant activity, anti-inflammatory, anti-atherogenic, anti-apoptotic, antihypertensive, and hypolipidemic effects, which can reduce oxidative stress and inflammation, both of which are principal factors in central nervous system (CNS) pathologies. These effects are attributed to its bioactive ingredients, and it may be a potent candidate for developing new drugs for cardiovascular diseases. Preclinical studies have demonstrated the anticancer, neuroprotective, and immunomodulatory effects of saffron [65-67]. In 2024, a study revealed the stress-relieving properties of saffron extract, suggesting its potential to enhance resilience to occasional stress. While these studies suggest that saffron may have potential benefits for various health conditions, they also highlight the need for further clinical research to fully establish its efficacy and safety profiles [68].
1. Antioxidant Effects: Saffron exhibits potent antioxidant and free radical scavenging activities due to the presence of carotenoids such as crocin and crocetin. It inhibits lipid peroxidation and enhances antioxidant enzyme activities and helps protect cells from oxidative stress-induced damage, preserving cellular integrity and function. A study revealed that after saffron supplementation, the active compound crocin significantly reduced levels of oxidative stress markers, malondialdehyde (MDA), and total antioxidant capacity (TAC) [65,69,70].
2. Anti-inflammatory Effects: It exerts anti-inflammatory effects by inhibiting proinflammatory cytokines and enzymes such as Cyclooxygenase-2 (COX-2) and intercellular Nitrogen Oxygen Species (iNOS), reducing inflammatory conditions at the cellular level. Saffron and crocin exert neuroprotective effects by reducing oxidative stress and inflammatory responses, which shows their potential for mitigating inflammation-related damage in patients with brain injury [71].
3. Anti-Atherogenic Effects: In saffron, compounds such as crocetin help decrease the levels of cardiac markers such as Lactate dehydrogenase (LDH), Creatine kinase (CK), and MDA, which are the indicators of cardiovascular risk factors. These effects contribute to the potential of saffron in preventing atherosclerosis and cardiovascular diseases. Saffron extract has a plaque-stabilizing effect in both the early and advanced stages of atherosclerosis [72,73].
4. Anti-Apoptotic Effects: The bioactive constituents of safranin help prevent programmed cell death, thereby promoting cell survival and tissue integrity. This antiapoptotic activity is crucial in various disease conditions where excessive cell death occurs [65].
5. Antihypertensive Effects: Safranal and crocetin help control blood pressure by modulating cellular mechanisms involved in vascular tone and blood pressure regulation. Saffron may exert its antihypertensive effects through various mechanisms, including increasing nitric oxide (NO) concentrations, enhancing antioxidant properties, regulating endothelial function, and attenuating the NF-kappa B pathway, through which its supplementation is potentially useful for blood pressure regulation [65,74].
6. Hypolipidemic Effects: Hypolipidemic effects help reduce triglycerides and cholesterol levels within the cells, thereby improving lipid profiles and reducing the risk of cardiovascular diseases associated with dyslipidemia. In 2024, researchers conducted a systematic review and meta-analysis to investigate the effects of saffron supplementation on glycemic outcomes in patients with diabetes. The study revealed that saffron was effective in reducing fasting plasma glucose (FPG) and hemoglobin A1c (HbA1c), indicating that it may be useful in controlling blood sugar levels in diabetic patients. However, the study noted that there was significant variation in the quality of the methodology used, indicating that more well-designed clinical trials are needed to further investigate the potential benefits of saffron. Another review published in 2024 focused on the effects of saffron on the CNS, particularly its potential as a nutraceutical for treating common CNS diseases [20,53].
However, further clinical evidence and meta-analyses are needed to validate its therapeutic potential in various disorders. While promising as a treatment for depression, saffron comes with potential side effects, contraindications, and drug interactions that warrant careful consideration. Common side effects include gastrointestinal issues like nausea and vomiting, drowsiness, and, in rare cases, allergic reactions. Saffron is contraindicated in pregnancy due to its potential to cause uterine contractions and in individuals with known allergies to saffron or related plants. It may also exacerbate symptoms in people with bipolar disorder or cause hypotension in those with low blood pressure. Saffron can interact with various medications, such as antidepressants (increasing the risk of serotonin syndrome), antihypertensives (potentially causing low blood pressure), anticoagulants (raising bleeding risk), and sedatives (enhancing sedation). Therefore, it is important for individuals to consult healthcare providers before using saffron, especially if they have existing health conditions or are on medication. Saffron has emerged as a promising natural treatment for depression and anxiety, with recommended dosages varying based on duration and intensity of use.
Research indicates that a daily dosage of 30 mg is generally safe and effective, while short-term use may extend to 60 mg with caution. For long-term treatment, a dosage of 15-30 mg is advisable. Always consult with a healthcare provider before starting saffron, especially at higher dosages or for long-term use (Figure 5) [75,76].
Figure 5.
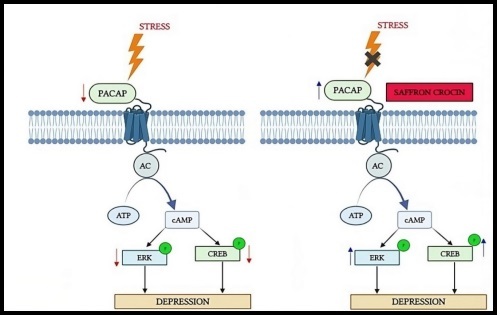
Adenylate cyclase-activating polypeptide (PACA), extracellular regulated protein kinase (ERK), response element binding protein (CREB), cyclic adenosine monophosphate (cAMP), adenosine triphosphate (ATP), and adenylyl cyclase (AC) are the mechanisms by which saffron crocin exhibits neuroprotection activation (B) and reduces the effects of stress (A).
Mechanism of Action and Broader Therapeutic Landscape of Saffron
Saffron has emerged as a promising alternative to standard antidepressants, with mechanisms of action that parallel those of conventional treatments. While standard antidepressants primarily target neurotransmitter systems, saffron’s multifaceted effects on various pathways contribute to its therapeutic potential in depression. Standard antidepressants primarily target neurotransmitter systems. SSRIs, like fluoxetine, sertraline, and escitalopram, inhibit the reuptake of serotonin, increasing its availability in the synaptic cleft and enhancing serotonergic signaling crucial for mood regulation. SNRIs, like venlafaxine and duloxetine, inhibit the reuptake of both serotonin and norepinephrine, leading to increased levels of these neurotransmitters in the brain, which can be beneficial for patients with severe depressive symptoms or those who do not respond adequately to SSRIs. TCAs block the reuptake of norepinephrine and serotonin and also affect various other neurotransmitter systems, leading to a broader range of side effects. Due to their side effect profile, TCAs are generally considered second-line treatments for depression [77,78].
Saffron’s active components, crocin and safranal, modulate several neurotransmitter systems involved in mood regulation, particularly serotonin and dopamine. Saffron inhibits the serotonin transporter (SERT), similar to SSRIs, increasing the availability of serotonin in the synaptic cleft. This leads to improved mood and alleviation of depressive symptoms. Animal studies have shown that saffron extracts and their constituents, such as safranal and crocin, can reduce immobility time and increase swimming time in the forced swimming test, similar to the effects of fluoxetine, a commonly prescribed SSRI. Saffron promotes dopamine release, which is associated with pleasure and reward, potentially contributing to its antidepressant effects. Saffron increases levels of brain-derived neurotrophic factor (BDNF), crucial for neurogenesis and synaptic plasticity. Researchers have linked elevated BDNF levels to improved mood and cognitive function, therefore supporting saffron’s role as a therapeutic agent in depression. Additionally, saffron influences the kynurenine pathway, reducing the production of harmful metabolites associated with brain inflammation and mental health disorders. By inhibiting enzymes in this pathway, especially through crocin, saffron lowers the production of harmful metabolites. This may help keep neurotransmitter levels in balance, protect against neurodegenerative diseases, and boost mood [79]. Saffron possesses strong antioxidant and anti-inflammatory properties, potentially further contributing to its antidepressant effects by reducing inflammation and oxidative stress to protect neuronal health and enhance mood stability [80,81].
In several clinical trials, researchers compared the efficacy of saffron with standard antidepressants. In a randomized controlled trial, it was found that saffron (30 mg/day) and fluoxetine (20 mg/day) were equally effective in reducing depressive symptoms. The study also revealed that saffron demonstrated fewer side effects. Another study showed that over a 6-week period, saffron (30 mg/day) was as effective as imipramine (100 mg/day) in reducing depressive symptoms. Moreover, saffron exhibited a more favorable side effect profile.
Saffron offers a natural alternative that can complement existing treatment protocols for depression. It can be used as a standalone therapy for individuals seeking natural alternatives to conventional antidepressants or as an adjunct therapy alongside traditional medications, potentially enhancing overall treatment efficacy and reducing side effects. The integration of saffron into treatment protocols aligns with the emphasis on personalized medicine, ensuring that treatment plans are tailored to individual patient needs. Saffron’s ability to address both depressive and anxiety symptoms makes it an attractive option for a holistic approach to mental health care. While current evidence supports saffron’s efficacy in mild to moderate depression, larger, well-designed trials are needed to confirm its long-term effects and safety profile (Figure 6) [45,78-81].
Figure 6.
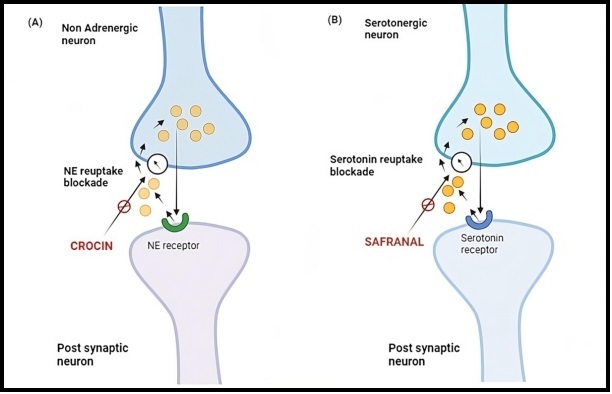
Illustration of the mechanism of inhibiting norepinephrine (NE) reuptake and serotonin-reuptake by (A) crocin and (B) safranal, respectively.
Experimental Evidence
Experimental research conducted on animals has revealed that saffron and its phytochemicals such as crocin, crocetin, and safranal have the potential to be effective antidepressants. The following are some of the key discoveries made:
Affron®, a standardized extract of saffron that contains bioactive compounds such as safranal and crocin isomers, was assessed for its impact on depressive-like behaviors in a rat model over 21 days, with 10 rats per group. The rats were administered 200 mg/kg of Affron® orally, 50 mg/kg via intraperitoneal injection, or saline as a control. The results revealed that oral administration of Affron® significantly increased sucrose preference, indicating reduced anhedonia, and decreased immobility time in the forced swim test, suggesting antidepressant-like effects. However, no significant changes were observed in anxiety-related behaviors in the elevated plus maze test. Statistical analysis validated these findings, underscoring Affron®’s potential as a treatment for depressive symptoms, though it showed limited effects on anxiety [82].
Another study reviewed the neuroprotective effects of saffron (C. sativus) in a rat model of cerebral ischemia/reperfusion. A total of 40 rats were divided into four groups, with two groups receiving saffron extract (100 mg/kg and 200 mg/kg) for 3 weeks prior to inducing ischemia. Behavioral assessments, including latency to move and fall, were conducted post-treatment. Results indicated that saffron significantly reduced latency to move and fall compared to the control group, while also decreasing oxidative stress markers (MDA, NO) and increasing antioxidant levels, like glutathione (GSH). Additionally, saffron treatment led to improved neurological scores, suggesting its efficacy in mitigating ischemic damage [15,46,58].
A 6-week trial in 66 patients with MDD and anxiety found saffron 30 mg/day had anxiolytic effects comparable to citalopram 40 mg/day, with no severe side effects. Another trial in 80 adults found saffron extract (Affron®) 28 mg/day for 4 weeks significantly improved anxiety symptoms [3]. The primary outcome measure in these studies was change in depressive symptoms, which were assessed using validated depression rating scales such as:
• Hamilton Depression Rating Scale (HDRS)
• Beck Depression Inventory (BDI)
• Montgomery-Åsberg Depression Rating Scale (MADRS)
Some trials also measured anxiety using the Hamilton Anxiety Rating Scale (HARS). Adverse events were monitored in all trials to assess safety and tolerability [83].
Clinical trials have also compared the effects of saffron with those of conventional antidepressants such as citalopram. The trials showed improvements in both depression and anxiety over 6 weeks, indicating that saffron could be a viable alternative for treating mild to moderate symptoms of depression [44].
Researchers included two placebo-controlled trials with a total of 40 patients in 2015 meta-analysis. The analysis revealed a large effect size for saffron supplementation compared to placebo in reducing depressive symptoms (mean effect size = 1.62, p<0.001). This indicates that saffron was significantly more effective than placebo in alleviating depression [4,5]. A study of 40 elderly patients (>60 years) with MDD found that saffron 30 mg/day had similar antidepressant effects to sertraline 50 mg/day after 6 weeks. This suggests saffron may be an effective option for treating depression in older adults. [84].
These studies provide promising evidence that saffron and its phytochemicals have the potential to be beneficial in treating depressive states, supporting their potential use as natural antidepressants. However, further research, including human clinical trials, is necessary to fully understand their efficacy and safety profile [85,86]. Effects of saffron in treatment of depression in clinical trials are summarized in Table 2.
Table 2. Effect of Saffron in Clinical Trials for Depression Therapy.
| S. No. | Type of study | Population | Sample Size | Intervention | Compared with | Duration | Results | References |
| 1 | Double Blind Randomized Controlled trial | Patient with Depression | 40 | Petals of Crocus sativus (15 mg bid) | Fluoxetine (10 mg bid) | 8 weeks | Effect similar to fluoxetine | [102] |
| 2 | Placebo controlled Double Blind Randomized Controlled trial | Patient with Depression | 40 | Capsules of Crocus sativus petals (30 mg bid) | Placebo | 6 weeks | A better outcome than placebo | [103] |
| 3 | Single Centre controlled Placebo controlled Double Blind Randomized Controlled trial | Patient with Depression | 40 | Capsules of Crocus sativus petals (30 mg bid) | Placebo | 6 weeks | A better outcome than placebo | [104] |
| 4 | Double Blinded | Medical Students | 50 | Drank tea containing saffron 3 times a day | Pre-test Post test | 4 weeks | Decreasing of the mean score (P<0.0001) | [18] |
| 5 | Double Blind Randomized Controlled trial | Patient with Depression | 70 | Crocus sativus capsules (100 mg/day) | Placebo | 12 weeks | The BDI score of depression group reduced by 2 times than placebo | [105] |
| 6 | Single center Double Blind Randomized Controlled trial | Patient with Depression | 40 | Hydroalcoholic extract of saffron (30 mg/day) | Fluoxetine (20 mg bid) | 6 weeks | Effect similar to fluoxetine | [106] |
Future Prospects
Future research on saffron’s role in treating depression should prioritize exploring its biological mechanisms, particularly how its active compounds influence neurotransmitter systems and inflammation. Large-scale clinical trials across diverse populations are essential to confirm its effectiveness and compare it with standard antidepressants. Investigations should also focus on determining optimal dosages and formulations, as well as examining the genetic factors that may impact individual responses to saffron. Furthermore, studies should evaluate the potential advantages of combining saffron with other therapies and its efficacy in treating specific depression subtypes, such as treatment-resistant or postpartum depression. These efforts will help clarify saffron’s role in clinical practice and improve treatment strategies for depression.
Conclusion
Saffron is a natural antidepressant with a strong safety profile and efficacy comparable to standard treatments for MDD. Its diverse mechanisms, including modulation of neurotransmitter systems, enhancement of neurotrophic factors, and reduction of oxidative stress and inflammation, make it a valuable addition to mood disorder treatment. Incorporating saffron into comprehensive treatment plans allows healthcare providers to offer patients a broader range of options, fostering a more personalized approach to mental health care. Integrating saffron into existing treatment protocols could offer a more comprehensive and holistic approach to managing depression. Saffron can be used alone by individuals seeking natural alternatives to conventional antidepressants or as a complementary therapy alongside traditional treatments, potentially enhancing overall efficacy and improving patient outcomes. The increasing interest in herbal and dietary supplements for mental health indicates a broader trend in integrative approaches to psychiatric care. Combining saffron with lifestyle interventions, such as exercise and dietary modifications, can offer a more comprehensive approach to managing depression. Identifying specific patient characteristics that may predict a favorable response to saffron treatment could help healthcare providers tailor interventions to individual needs, improving treatment adherence and overall effectiveness. Long-term sustainability of saffron as an antidepressant treatment requires further research, guidelines for saffron use, and training programs to educate professionals about natural therapies.
Glossary
- ICD
International Classification of Disease
- WHO
World Health Organization
- MDD
Major Depressive disorder
- SSRIs
selective serotonin reuptake inhibitors
- SNRIs
Serotonin-norepinephrine reuptake inhibitors
- TCA
Tricyclic antidepressants
- MAOIs
Monoamine oxidase inhibitors
- NMDA
N-methyl-D-aspartate
- MDA
malondialdehyde
- NO
Nitric Oxide
- CNS
Central Nervous System
- BDNF
Brain-derived neurotrophic factors
Author Contributions
SC conceived the topic of the review. PCG, SC, and AV contributed to the writing and editing of the review. AT, PKP, and SV critically revised the manuscript.
Funding
This article was not supported by any funding source.
References
- Klein DN, Calentino AE. Depressive disorders. Encycl Ment Heal. Third Ed Vol 1-3. 2023. Jan 1;1:V1-608-V1-616. https://doi.org/ 10.1016/B978-0-323-91497-0.00182-X. [DOI] [Google Scholar]
- Clack S, Ward T. The Classification and Explanation of Depression. Behav Chang [Internet]. 2019. Apr 1 [cited 2024 May 17];36(1):41–55. Available from: https://www.cambridge.org/core/journals/behaviour-change/article/abs/classification-and-explanation-of-depression/9C06BBD2D616CD6996CA70313AF384D2 https://doi.org/ 10.1017/bec.2019.4 [DOI]
- Dawson-Squibb JJ, Davids EL, Viljoen M, Rice K, Stein DJ. The WHO International Classification of Diseases 11th Revision (ICD-11). 2023;53–78. [Google Scholar]
- Liu X. The global burden of depressive disorder from 1990 to 2019: a systematic analysis for the global burden of disease study 2019. [Internet]. 2023 Mar 24 [cited 2024 May 21];12611:1366–74. Available from: https://www.spiedigitallibrary.org/conference-proceedings-of-spie/12611/126115E/The-global-burden-of-depressive-disorder-from-1990-to-2019/10.1117/12.2669550.full
- Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. COVID-19 Mental Disorders Collaborators . Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic [Internet]. Lancet. 2021. Nov;398(10312):1700–12. [cited 2024 May 20] Available from: http://www.thelancet.com/article/S0140673621021437/fulltext 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017. Sep;219:86–92. 10.1016/j.jad.2017.05.003 [DOI] [PubMed] [Google Scholar]
- Sachan N, Yadav N, Masih P, Spencer P, Gautam R, Rawat R, et al. Depression, Anxiety and Stress among Nursing Students [Internet]. Asian J Nurs Educ Res. 2022. Feb;12(1):70–4. [cited 2024 May 27] Available from: https://ajner.com/AbstractView.aspx?PID=2022-12-1-14 10.52711/2349-2996.2022.00014 [DOI] [Google Scholar]
- Hall WD, Mant A, Mitchell PB, Rendle VA, Hickie IB, McManus P. Association between antidepressant prescribing and suicide in Australia, 1991-2000: trend analysis [Internet]. BMJ. 2003. May;326(7397):1008–1008. [cited 2024 Sep 4] Available from: http://www.bmj.com/ 10.1136/bmj.326.7397.1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ. STAR*D: what have we learned? [Internet]. Am J Psychiatry. 2007. Feb;164(2):201–4. [cited 2024 Sep 4]. 10.1176/ajp.2007.164.2.201 [DOI] [PubMed] [Google Scholar]
- Cassano P, Fava M. Tolerability issues during long-term treatment with antidepressants [Internet]. Ann Clin Psychiatry. 2004;16(1):15–25. [cited 2024 Sep 4]. 10.1080/10401230490281618 [DOI] [PubMed] [Google Scholar]
- Brown C, Taniguchi G, Yip K. The monoamine oxidase inhibitor-tyramine interaction [Internet]. J Clin Pharmacol. 1989. Jun;29(6):529–32. [cited 2024 Sep 4]. 10.1002/j.1552-4604.1989.tb03376.x [DOI] [PubMed] [Google Scholar]
- Khawam EA, Laurencic G, Malone DA Jr. Side effects of antidepressants: an overview [Internet]. Cleve Clin J Med. 2006. Apr;73(4):351–3. [cited 2024 Sep 4]. 10.3949/ccjm.73.4.351 [DOI] [PubMed] [Google Scholar]
- Edwards SJ, Hamilton V, Nherera L, Trevor N. Lithium or an atypical antipsychotic drug in the management of treatment-resistant depression: a systematic review and economic evaluation [Internet]. Health Technol Assess. 2013. Nov;17(54):1–190. [cited 2024 Sep 4]. 10.3310/hta17540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Song Y, Zhang X, Zhao W, Ma T, Liu Y, et al. Ketamine relieves depression-like behaviors induced by chronic postsurgical pain in rats through anti-inflammatory, anti-oxidant effects and regulating BDNF expression [Internet]. Psychopharmacology (Berl). 2020. Jun;237(6):1657–69. [cited 2024 Sep 4]. 10.1007/s00213-020-05490-3 [DOI] [PubMed] [Google Scholar]
- Varshney S, Alam MA, Kaur A, Sharma S. A Comprehensive Review on the Neuropharmacological Effects ofAntidepressants in Various Prospects [Internet]. Curr Psychopharmacol. 2023. Jul;12(1):1–21. [cited 2024 May 20] Available from: https://www.eurekaselect.com/article/132801 [Google Scholar]
- Munir N, Qamar A, Hasnain M, Waqif H, Hanif M, Sarwar Z, et al. Medicinal Plants and Phytochemicals against Depression. Phytochem Drug Discov Cent Nerv Syst Disord [Internet]. 2023. Aug 14 [cited 2024 May 17];203–17. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/9781119794127.ch8 https://doi.org/ 10.1002/9781119794127.ch8 10.1002/9781119794127.ch8 [DOI]
- Mir TG, Wani AK, Singh J, Shukla S. Mir T ul G, Wani AK, Singh J, Shukla S. Therapeutic application and toxicity associated with Crocus sativus (saffron) and its phytochemicals. Pharmacol Res Mod Chin Med. 2022. Sep;4:100136. 10.1016/j.prmcm.2022.100136 [DOI] [Google Scholar]
- Moshiri M, Vahabzadeh M, Hosseinzadeh H. Clinical Applications of Saffron (Crocus sativus) and its Constituents: A Review [Internet]. Drug Res (Stuttg). 2015. Jun;65(6):287–95. [cited 2024 May 17]. [DOI] [PubMed] [Google Scholar]
- Amini S, Mohseni H, Abiri B, Jafarirad S. The role of saffron (Crocus sativus L) on testosterone and depression in andropause middle-aged and elderly men: a systematic review. Nutr Food Sci. 2023. Nov;53(8):1419–36. 10.1108/NFS-03-2023-0071 [DOI] [PubMed] [Google Scholar]
- Irani M, Rahmanian A, Soltani N. Efficacy of Saffron (Crocus sativus L.) in Premenstrual Syndrome, Labor, Childbirth, and Menopause: A Systematic Review of Clinical Trials. Mod Care J. [Internet]. 2023. May 9 [cited 2024 May 20];20(3). Available from: https://brieflands.com/articles/mcj-134533.html [Google Scholar]
- Yang W, Qiu X, Wu Q, Chang F, Zhou T, Zhou M, et al. Active constituents of saffron (Crocus sativus L.) and their prospects in treating neurodegenerative diseases (Review) [Review] [Review]. Exp Ther Med. 2023. Apr;25(5):235. 10.3892/etm.2023.11934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varsha MS, Shaikh AZ, Pawar SP. Depression: As a Risk Factor for Coronary Heart Disease. Res J Pharmacol Pharmacodyn [Internet]. 2022. Aug 10 [cited 2024 May 27];14(3):139–45. [Google Scholar]
- Sharma I, Kaur M, Parashar B, Kainth MA. Depression. An Overview ABSTRACT. 2014;4(1):28–31. [Google Scholar]
- Cai H, Chen MY, Li XH, Zhang L, Su Z, Cheung T, et al. A network model of depressive and anxiety symptoms: a statistical evaluation [Internet]. Mol Psychiatry. 2024. Mar;29(3):767–81. [cited 2024 May 20] 10.1038/s41380-023-02369-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Z. Why psychotherapy can treat depression. [Internet]. 2023. Mar 24 [cited 2024 May 20];12611:928–33. Available from: https://www.spiedigitallibrary.org/conference-proceedings-of-spie/12611/126113L/Why-psychotherapy-can-treat-depression/10.1117/12.2669677.full https://doi.org/ 10.1117/12.2669677 10.1117/12.2669677 [DOI]
- Li D. Treatment of depression from both biological and psychological aspects. [Internet]. 2022. Dec 6 [cited 2024 May 20];12458:336–42. Available from: https://www.spiedigitallibrary.org/conference-proceedings-of-spie/12458/124581G/Treatment-of-depression-from-both-biological-and-psychological-aspects/10.1117/12.2660405.full https://doi.org/ 10.1117/12.2660405 10.1117/12.2660405 [DOI]
- Vijayalakshmi KK. Assessment of Depression among Cancer Patients [Internet]. Asian J Nurs Educ Res. 2018. Mar;8(1):11–4. [cited 2024 May 27] Available from: https://ajner.com/AbstractView.aspx?PID=2018-8-1-4 10.5958/2349-2996.2018.00004.6 [DOI] [Google Scholar]
- Ertezaee B, Asghari K, Oreizi H, Ghasemi N. The Mediating Role of Pleasant Activities in Cognitive Behavioral Therapy for Depressed Adolescents. Int J Behav Sci. 2019;13(1):33–9. [Google Scholar]
- Tariq S, Alwetayan S, O’neill-Kerr A. Exploring the Trend in the Use of Electroconvulsive Therapy (ECT), Modified ECT and Transcranial Magnetic Stimulation (TMS) in Northamptonshire Healthcare Trust Enhancing Medical Governance of Care Within an EIP Service. 2023. [cited 2024 May 20]; Available from: https://doi.org/ 10.1192/bjo.2023.392. [DOI]
- Cuijpers P, Miguel C, Ciharova M, Quero S, Plessen CY, Ebert D, et al. Psychological treatment of depression with other comorbid mental disorders: systematic review and meta-analysis. Cogn Behav Ther. 2023. May;52(3):246–68. 10.1080/16506073.2023.2166578 [DOI] [PubMed] [Google Scholar]
- Kamdem GB, Silva Teixeira A, Senchyna A, Junod Peron N, Benzakour L, Durieux-Paillard S, et al. [Latest developments in the non-pharmacological treatment of depression - A more integrative approach]. Rev Med Suisse. 2022. Sep;18(797):1809–11. [cited 2024 May 20] Available from: https://europepmc.org/article/med/36170135 10.53738/REVMED.2022.18.797.1809 [DOI] [PubMed] [Google Scholar]
- Dalrymple KL. Combined Treatments (Medications plus Psychotherapy). Encycl Clin Psychol [Internet]. 2015. Jan 23 [cited 2024 May 20];1–6. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/9781118625392.wbecp083
- Licinio AW, Wong ML, Licinio J. Biological and behavioural antidepressant treatment responses with the selective serotonin reuptake inhibitor fluoxetine can be determined by the environment. Mol Psychiatry. [Internet]. 2017. Mar 23 [cited 2024 May 20];22(4):484–484. Available from: https://www.nature.com/articles/mp201768 https://doi.org/ 10.1038/mp.2017.68 [DOI] [PubMed] [Google Scholar]
- Kaulage SR, Aldar KT, Jadhav RP, Jadhav PD, Yadhav VD. Review on Antidepressant Medication. 2019. [cited 2024 May 20]; Available from: https://doi.org/ 10.32628/IJSRST1962118. [DOI] [Google Scholar]
- Mann JJ, Rizk MM. Rethinking the medication management of major depression [Internet]. Expert Rev Neurother. 2023. Apr;23(4):331–63. [cited 2024 Sep 4]. 10.1080/14737175.2023.2190886 [DOI] [PubMed] [Google Scholar]
- Kaur M, Kaur S, Kaur R. Correlation of Depression and Quality of life among rural elderly. Int J Adv Nurs Manag. 2016;4(4):323. 10.5958/2454-2652.2016.00072.X [DOI] [Google Scholar]
- Kalin NH. Insights and Advances Into Treatments for Major Depression [Internet]. Am J Psychiatry. 2023. Mar;180(3):173–6. [cited 2024 May 20]. 10.1176/appi.ajp.20230041 [DOI] [PubMed] [Google Scholar]
- Kochar Kaur K. Therapeutic applications of recent advancements in insight regarding mechanisms of development of Anorexia Nervosa: implications in the management and development of biomarkers for early detection besides avoidance of neonatal malformations-A Short C. J Intern Med Heal Aff. 2022. Dec 19;1(1):01–6. [Google Scholar]
- Yao J, Chen C, Guo Y, Yang Y, Liu X, Chu S, et al. A Review of Research on the Association between Neuron–Astrocyte Signaling Processes and Depressive Symptoms. Int J Mol Sci. 2023, Vol 24, Page 6985 [Internet]. 2023 Apr 10 [cited 2024 May 20];24(8):6985. Available from: https://www.mdpi.com/1422-0067/24/8/6985/htm. https://doi.org/ 10.3390/ijms24086985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert U, Tomasetti C, Marra C, Neviani F, Pirani A, Taddeo D, et al. Treating depression in clinical practice: new insights on the multidisciplinary use of trazodone. Front Psychiatry [Internet]. 2023. [cited 2024 May 20];14. Available from: /pmc/articles/PMC10466041/ https://doi.org/ 10.3389/fpsyt.2023.1207621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkin JM, Golani LK, Smith JL. Clinical pharmacological innovation in the treatment of depression [Internet]. Expert Rev Clin Pharmacol. 2023. Apr;16(4):349–62. [cited 2024 May 20] Available from: https://www.tandfonline.com/doi/abs/10.1080/17512433.2023.2198703 10.1080/17512433.2023.2198703 [DOI] [PubMed] [Google Scholar]
- Goldberg JF. Perspectives on the success rate of current antidepressant pharmacotherapy [Internet]. Expert Opin Pharmacother. 2022. Nov;23(16):1781–91. [cited 2024 May 20] Available from: https://www.tandfonline.com/doi/abs/10.1080/14656566.2022.2138333 10.1080/14656566.2022.2138333 [DOI] [PubMed] [Google Scholar]
- Stachowicz K, Sowa-Kućma M. The treatment of depression - searching for new ideas. Front Pharmacol. 2022. Oct;13:988648. 10.3389/fphar.2022.988648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson PA, Forster J, Khan J, Pouchieu C, Dubreuil S, Gaudout D, et al. Effects of Saffron Extract Supplementation on Mood, Well-Being, and Response to a Psychosocial Stressor in Healthy Adults: A Randomized, Double-Blind, Parallel Group, Clinical Trial [Internet]. Front Nutr. 2021. Feb;7:606124. [cited 2024 May 20] Available from: https://pubmed.ncbi.nlm.nih.gov/33598475/ 10.3389/fnut.2020.606124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausenblas HA, Saha D, Dubyak PJ, Anton SD. Saffron (Crocus sativus L.) and major depressive disorder: a meta-analysis of randomized clinical trials [Internet]. J Integr Med. 2013. Nov;11(6):377–83. [cited 2024 Aug 31]. 10.3736/jintegrmed2013056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafiee M, Arekhi S, Omranzadeh A, Sahebkar A. Saffron in the treatment of depression, anxiety and other mental disorders: current evidence and potential mechanisms of action [Internet]. J Affect Disord. 2018. Feb;227:330–7. [cited 2024 May 17]. 10.1016/j.jad.2017.11.020 [DOI] [PubMed] [Google Scholar]
- Marx W, Lane M, Rocks T, Ruusunen A, Loughman A, Lopresti A, et al. Effect of saffron supplementation on symptoms of depression and anxiety: a systematic review and meta-analysis [Internet]. Nutr Rev. 2019. Aug;77(8):557–71. [cited 2024 May 20]. 10.1093/nutrit/nuz023 [DOI] [PubMed] [Google Scholar]
- José Bagur M, Alonso Salinas GL, Jiménez-Monreal AM, Chaouqi S, Llorens S, Martínez-Tomé M, et al. Saffron: An Old Medicinal Plant and a Potential Novel Functional Food. Mol. 2018, Vol 23, Page 30 [Internet]. 2017 Dec 23 [cited 2024 May 17];23(1):30. Available from: https://www.mdpi.com/1420-3049/23/1/30/htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dave PH, Vishnupriya V, Gayathri R. Herbal Remedies for Anxiety and Depression- A Review. Res J Pharm Technol [Internet]. 2016. Aug 28 [cited 2024 May 27];9(8):1253–6. Available from: https://rjptonline.org/AbstractView.aspx?PID=2016-9-8-46 [Google Scholar]
- Cicco N. Crocus sativus (L.) Grown in Pots with High Volume Capacity: From a Case of Study to a Patent. Agric 2022, Vol 12, Page 1813 [Internet]. 2022 Oct 31 [cited 2024 May 21];12(11):1813. Available from: https://www.mdpi.com/2077-0472/12/11/1813/htm
- Irfan M, Nasseer S, Rashid U, Wani MA, Khan MH, Bhat RA, et al. Studies of Phenotypic and Genotypic Variation for Morphological Traits in Saffron (Crocus sativus L.). Int J Environ Clim Chang [Internet]. 2022. Oct;12(11):3311–20. [cited 2024 May 20] Available from: https://journalijecc.com/index.php/IJECC/article/view/1381 10.9734/ijecc/2022/v12i111381 [DOI] [Google Scholar]
- Rasmi Y, Salazar E, Gupta E, Daei-Hasani B, Calderón-Juárez M. Saffron. Mol Mech Funct Food [Internet]. 2022. Nov 16 [cited 2024 May 20];453–84. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/9781119804055.ch14 [Google Scholar]
- Christodoulou E, Kadoglou NP, Kostomitsopoulos N, Valsami G. Saffron: a natural product with potential pharmaceutical applications [Internet]. J Pharm Pharmacol. 2015. Dec;67(12):1634–49. [cited 2024 May 20]. 10.1111/jphp.12456 [DOI] [PubMed] [Google Scholar]
- Nemtsov A, Kirshkov P. The Study of Precision of ISO 3632-2 Method for Analysis of Herbal Medicines. Asian J Pharm Anal [Internet]. [cited 2024 May 27];10(3):2231–5675. Available from: www.anvpublication.orgwww.asianpharmaonline.orgHomepagewww.ajpaonline.com
- Akowuah GA, Htar TT. Therapeutic properties of saffron and its chemical constituents [Internet]. J Nat Prod. 2014;7:5–13. [cited 2024 May 20] Available from: https://research.monash.edu/en/publications/therapeutic-properties-of-saffron-and-its-chemical-constituents [Google Scholar]
- Zouagui R, Sbabou L. Saffron in Phytotherapy: Pharmacological Properties and Medicinal Uses. 2022. [cited 2024 May 20];253–72. Available from: https://link.springer.com/chapter/10.1007/978-3-031-10000-0_15
- Avila-Sosa R, Nevárez-Moorillón GV, Ochoa-Velasco CE, Navarro-Cruz AR, Hernández-Carranza P, Cid-Pérez TS. Detection of Saffron’s Main Bioactive Compounds and Their Relationship with Commercial Quality. Foods. 2022, Vol 11, Page 3245 [Internet]. 2022 Oct 18 [cited 2024 May 20];11(20):3245. Available from: https://www.mdpi.com/2304-8158/11/20/3245/htm https://doi.org/ 10.3390/foods11203245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohajeri SA, Sepahi S, Ghorani Azam A. Antidepressant and antianxiety properties of saffron. Saffron Sci Technol Heal. 2020. Jan 1;431–44. https://doi.org/ 10.1016/B978-0-12-818638-1.00028-9. [DOI] [Google Scholar]
- Long Y, Tao H, Wang S, Xing B, Wang Z, Liu K, et al. Identification and Functional Validation of Two Novel Antioxidant Peptides in Saffron [Internet]. Antioxidants. 2024. Mar;13(3):378. [cited 2024 May 21] Available from: https://www.mdpi.com/2076-3921/13/3/378/htm 10.3390/antiox13030378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo MR. Analytical Profiling of Saffron (Crocus sativus) using 1H-NMR and FTIR based Metabolomics approach and UV-Vis, HPTLC and TLC Chromatography Fingerprinting. Res J Pharmacogn Phytochem [Internet]. 2023. Aug 5 [cited 2024 May 27];15(3):191–7.
- Sami M, Rashid A, Akram M, Ibadi AK, Mbaye EH, Sami M, et al. Phytochemical analysis and therapeutic properties of medicinal plants Crocus sativus: saffron. https://wjarr.com/sites/default/files/WJARR-2022-1277.pdf [Internet]. 2022. Nov 30 [cited 2024 May 20];16(2):1117–22. Available from: https://wjarr.com/content/phytochemical-analysis-and-therapeutic-properties-medicinal-plants-crocus-sativus-saffron
- Naim N, Bouymajane A, Oulad El Majdoub Y, Ezrari S, Lahlali R, Tahiri A, et al. Flavonoid Composition and Antibacterial Properties of Crocus sativus L. Petal Extracts [Internet]. Molecules. 2022. Dec;28(1):186. [cited 2024 May 20]. 10.3390/molecules28010186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karimi E, Oskoueian E, Hendra R, Jaafar HZ, Stigma Phenolic and Flavonoid Compounds and Its Antioxidant Activity . Evaluation of Crocus sativus L. stigma phenolic and flavonoid compounds and its antioxidant activity [Internet]. Molecules. 2010. Sep;15(9):6244–56. [cited 2024 May 20]. 10.3390/molecules15096244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long Y, Tao H, Wang S, Xing B, Wang Z, Liu K, et al. Identification and Functional Validation of Two Novel Antioxidant Peptides in Saffron [Internet]. Antioxidants. 2024. Mar;13(3):378. [cited 2024 May 20] 10.3390/antiox13030378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaffari S, Roshanravan N. Saffron; An updated review on biological properties with special focus on cardiovascular effects. Biomed Pharmacother. 2019. Jan;109:21–7. 10.1016/j.biopha.2018.10.031 [DOI] [PubMed] [Google Scholar]
- Zamani M, Zarei M, Nikbaf-Shandiz M, Gholami F, Hosseini AM, Nadery M, et al. The effects of saffron supplementation on cardiovascular risk factors in adults: A systematic review and dose-response meta-analysis. Front Nutr. 2022. Dec;9:1055517. 10.3389/fnut.2022.1055517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mzabri I, Addi M, Berrichi A. Traditional and Modern Uses of Saffron (Crocus Sativus). Cosmet. 2019, Vol 6, Page 63 [Internet]. 2019 Oct 25 [cited 2024 May 18];6(4):63. Available from: https://www.mdpi.com/2079-9284/6/4/63/htm [Google Scholar]
- Sut S, Gherardi G, Ruzza F, Caudullo G, Shrestha SS, Sorrenti V, et al. Saffron the “Red Gold” and Its CNS Activity: A Challenge for Future Applications in Nutraceuticals. J Food Biochem. 2024;2024. [Google Scholar]
- Abedi A, Ghobadi H, Sharghi A, Iranpour S, Fazlzadeh M, Aslani MR. Effect of saffron supplementation on oxidative stress markers (MDA, TAC, TOS, GPx, SOD, and pro-oxidant/antioxidant balance): an updated systematic review and meta-analysis of randomized placebo-controlled trials. Front Med (Lausanne). 2023. Feb;10:1071514. 10.3389/fmed.2023.1071514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahmani AH, Khan AA, Aldebasi YH. Saffron (Crocus sativus) and its active ingredients: role in the prevention and treatment of disease. Pharmacogn J. 2014;9(6):873–9. 10.5530/pj.2017.6.137 [DOI] [Google Scholar]
- Salem M, Shaheen M, Tabbara A, Borjac J. Saffron extract and crocin exert anti-inflammatory and anti-oxidative effects in a repetitive mild traumatic brain injury mouse model. Sci Reports. [Internet]. 2022. Mar 23 [cited 2024 May 18];12(1):1–14. https://doi.org/ 10.1038/s41598-022-09109-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butnariu M, Quispe C, Herrera-Bravo J, Sharifi-Rad J, Singh L, Aborehab NM, et al. The Pharmacological Activities of Crocus sativus L.: A Review Based on the Mechanisms and Therapeutic Opportunities of its Phytoconstituents [Internet]. Oxid Med Cell Longev. 2022. Feb;2022(11):8214821. [cited 2024 May 18]. 10.1155/2022/8214821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasim NA, Rahim IN, Omar E, Muid SA, Nawawi HM. Plaque-stabilizing effect of saffron extract in early and advanced atherosclerotic New Zealand white rabbits [Internet]. Atherosclerosis. 2023. Aug;379:S37. [cited 2024 May 18] Available from: http://www.atherosclerosis-journal.com/article/S0021915023042624/fulltext 10.1016/j.atherosclerosis.2023.06.170 [DOI] [Google Scholar]
- Setayesh L, Ashtary-Larky D, Clark CC, Rezaei Kelishadi M, Khalili P, Bagheri R, et al. The Effect of Saffron Supplementation on Blood Pressure in Adults: A Systematic Review and Dose-Response Meta-Analysis of Randomized Controlled Trials [Internet]. Nutrients. 2021. Aug;13(8):2736. [cited 2024 May 18]. 10.3390/nu13082736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafiee A, Jafarabady K, Seighali N, Mohammadi I, Rajai Firouz Abadi S, Abhari FS, et al. Effect of Saffron Versus Selective Serotonin Reuptake Inhibitors (SSRIs) in Treatment of Depression and Anxiety: A Meta-analysis of Randomized Controlled Trials. Nutr Rev [Internet]. 2024. Jun 24 [cited 2024 Aug 31]. [DOI] [PubMed] [Google Scholar]
- Bandaru S, Alivelu A, Bai KS, Yendluri P. Safety and efficacy of desvenlafaxine with escitalopram among the patients of depression associated with anxiety: A randomized, open-labeled, comparative study. Natl J Physiol Pharm Pharmacol [Internet]. 2024 [cited 2024 Aug 31];74(2024):1. Available from: www.njppp.com
- Alex K, Zhao Y, Ding X, Fayzullaeva L, Ge A, O’Donnell M, et al. Abstract 2436 Molecular Interactions of SERT and Escitalopram in Serotonin Modulation [Internet]. J Biol Chem. 2024;300(3):107192. 10.1016/j.jbc.2024.107192 [DOI] [Google Scholar]
- Yue JK, Burke JF, Upadhyayula PS, Winkler EA, Deng H, Robinson CK, et al. Selective serotonin reuptake inhibitors for treating neurocognitive and neuropsychiatric disorders following traumatic brain injury: an evaluation of current evidence. Brain Sci. 2017. Jul;7(8):93. 10.3390/brainsci7080093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monchaux de Oliveira C, Morael J, Guille A, Amadieu C, Vancassel S, Gaudout D, et al. Saffron extract interferes with lipopolysaccharide-induced brain activation of the kynurenine pathway and impairment of monoamine neurotransmission in mice [Internet]. Front Nutr. 2023. Oct;10:1267839. [cited 2024 Sep 4]. 10.3389/fnut.2023.1267839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bian Y, Zhao C, Lee SM. Neuroprotective Potency of Saffron Against Neuropsychiatric Diseases, Neurodegenerative Diseases, and Other Brain Disorders: From Bench to Bedside [Internet]. Front Pharmacol. 2020. Oct;11:579052. [cited 2024 May 20]. 10.3389/fphar.2020.579052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui MJ, Saleh MS, Basharuddin SN, Zamri SH, Mohd Najib MH, Che Ibrahim MZ, et al. Saffron (Crocus sativus L.): as an Antidepressant [Internet]. J Pharm Bioallied Sci. 2018;10(4):173–80. [cited 2024 Sep 3]. 10.4103/JPBS.JPBS_83_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orio L, Alen F, Ballesta A, Martin R, De Heras RG. Antianhedonic and Antidepressant Effects of Affron®, a Standardized Saffron (Crocus Sativus L.) Extract. Molecules [Internet]. 2020. Jul 1 [cited 2024 May 20];25(14). Available from: /pmc/articles/PMC7397008/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guizzaro L, Morgan DD, Falco A, Gallo C. Hamilton scale and MADRS are interchangeable in meta-analyses but can disagree at trial level [Internet]. J Clin Epidemiol. 2020. Aug;124:106–17. [cited 2024 Sep 2] Available from: http://www.jclinepi.com/article/S0895435619310522/fulltext 10.1016/j.jclinepi.2020.04.022 [DOI] [PubMed] [Google Scholar]
- Omidkhoda SF, Hosseinzadeh H. Saffron and its active ingredients against human disorders: A literature review on existing clinical evidence. Iran J Basic Med Sci [Internet]. 2022. Aug 1 [cited 2024 Aug 31];25(8):913. Available from: /pmc/articles/PMC9464341/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahmansouri N, Farokhnia M, Abbasi SH, Kassaian SE, Noorbala Tafti AA, Gougol A, et al. A randomized, double-blind, clinical trial comparing the efficacy and safety of Crocus sativus L. with fluoxetine for improving mild to moderate depression in post percutaneous coronary intervention patients [Internet]. J Affect Disord. 2014. Feb;155(1):216–22. 10.1016/j.jad.2013.11.003 [DOI] [PubMed] [Google Scholar]
- Matraszek-Gawron R, Chwil M, Terlecki K, Skoczylas MM. Current Knowledge of the Antidepressant Activity of Chemical Compounds from Crocus sativus L. Pharm. 2023, Vol 16, Page 58 [Internet]. 2022 Dec 30 [cited 2024 May 21];16(1):58. Available from: https://www.mdpi.com/1424-8247/16/1/58/htm [DOI] [PMC free article] [PubMed]
- Jadouali SM, Atifi H, Mamouni R, Majourhat K, Bouzoubaâ Z, Laknifli A, et al. Chemical characterization and antioxidant compounds of flower parts of Moroccan crocus sativus L. J Saudi Soc Agric Sci. 2019;18(4):476–80. 10.1016/j.jssas.2018.03.007 [DOI] [Google Scholar]
- Mangione G, Caccamo M, Marino VM, Marino G, Licitra G. Characterization of artisanal saffron ricotta cheese produced in Sicily: Physicochemical, microbiological, sensory, and antioxidant characteristics. J Dairy Sci. 2023. Dec;106(12):8375–88. 10.3168/jds.2023-23612 [DOI] [PubMed] [Google Scholar]
- Naim N, Madani I, Ennahli S, Lahlali R Chemical Composition Profiling and Antifungal Activity of Saffron Petal Extract. Molecules. 2022;8742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceccopieri C, Skonieczna J, Madej JP. Modification of a haematoxylin, eosin, and natural saffron staining method for the detection of connective tissue. J Vet Res (Pulawy). 2021. Jan;65(1):125–30. 10.2478/jvetres-2021-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modaghegh MH, Shahabian M, Esmaeili HA, Rajbai O, Hosseinzadeh H. Safety evaluation of saffron (Crocus sativus) tablets in healthy volunteers. Phytomedicine. 2008. Dec;15(12):1032–7. 10.1016/j.phymed.2008.06.003 [DOI] [PubMed] [Google Scholar]
- Chaouqi S, Moratalla-López N, Alonso GL, Lorenzo C, Zouahri A, Asserar N, et al. Effect of Soil Composition on Secondary Metabolites of Moroccan Saffron (Crocus sativus L.). Plants. 2023. Feb;12(4):711. 10.3390/plants12040711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badihi L, Gerami M, Akbarinodeh D, Shokrzadeh M, Ramezani M. Physio-chemical responses of exogenous calcium nanoparticle and putrescine polyamine in Saffron (Crocus sativus L.). Physiol Mol Biol Plants. 2021. Jan;27(1):119–33. 10.1007/s12298-020-00923-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fathi M, Samadi M, Abbaszadeh S, Nourani MR. Fabrication and characterization of multifunctional bio-safe films based on Carboxymethyl Chitosan and Saffron Petal Anthocyanin Reinforced with Copper Oxide Nanoparticles for sensing the meat freshness. J Polym Environ. 2022;30(11):4538–49. 10.1007/s10924-022-02490-6 [DOI] [Google Scholar]
- Asil h. Effects of chelated iron (eddha-fe) treatments on corm and stigma quality in saffron (Crocus sativus l.). Bangladesh J Bot. 2023;52(1). [Google Scholar]
- Hamdi E, Muñiz-Gonzalez AB, Hidouri S, Bermejo AM, Sakly M, Venero C, et al. Prevention of neurotoxicity and cognitive impairment induced by zinc nanoparticles by oral administration of saffron extract. J Anim Physiol Anim Nutr (Berl). 2023. Nov;107(6):1473–94. 10.1111/jpn.13848 [DOI] [PubMed] [Google Scholar]
- Abbasi MR, Sepaskhah AR. Nitrogen leaching and groundwater N contamination risk in saffron/wheat intercropping under different irrigation and soil fertilizers regimes. Sci Rep. 2023. Apr;13(1):6587. 10.1038/s41598-023-33817-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kianmehr M, Khazdair MR. Possible therapeutic effects of Crocus sativus stigma and its petal flavonoid, kaempferol, on respiratory disorders. Pharm Biol. 2020. Dec;58(1):1140–9. 10.1080/13880209.2020.1844762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammadi Y, Rezaei Farimani A, Beydokhti H, Riahi SM. Comparison of the effect of saffron, crocin, and safranal on serum levels of oxidants and antioxidants in diabetic rats: A systematic review and meta-analysis of animal studies. Food Sci Nutr. 2023. Mar;11(6):2429–39. 10.1002/fsn3.3302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alizadeh-Sani M, Tavassoli M, McClements DJ, Hamishehkar H. Multifunctional halochromic packaging materials: saffron petal anthocyanin loaded-chitosan nanofiber/methyl cellulose matrices. Food Hydrocoll. 2021;111:111. 10.1016/j.foodhyd.2020.106237 [DOI] [Google Scholar]
- Cortez MV, Perovic NR, Soria EA, Defagó MD. Effect of heat and microwave treatments on phenolic compounds and fatty acids of turmeric (curcuma longa l.) and saffron (Crocus sativus L.). Braz J Food Technol. 2020;23:23. 10.1590/1981-6723.20519 [DOI] [Google Scholar]
- Akhondzadeh Basti A, Moshiri E, Noorbala AA, Jamshidi AH, Abbasi SH, Akhondzadeh S. Comparison of petal of Crocus sativus L. and fluoxetine in the treatment of depressed outpatients: a pilot double-blind randomized trial [Internet]. Prog Neuropsychopharmacol Biol Psychiatry. 2007. Mar;31(2):439–42. [cited 2024 Sep 5]. 10.1016/j.pnpbp.2006.11.010 [DOI] [PubMed] [Google Scholar]
- Akhondzadeh S, Tahmacebi-Pour N, Noorbala AA, Amini H, Fallah-Pour H, Jamshidi AH, et al. Crocus sativus L. in the treatment of mild to moderate depression: a double-blind, randomized and placebo-controlled trial [Internet]. Phytother Res. 2005. Feb;19(2):148–51. [cited 2024 Sep 5] Available from: https://pubmed.ncbi.nlm.nih.gov/15852492/ 10.1002/ptr.1647 [DOI] [PubMed] [Google Scholar]
- Moshiri E, Basti AA, Noorbala AA, Jamshidi AH, Hesameddin Abbasi S, Akhondzadeh S. Crocus sativus L. (petal) in the treatment of mild-to-moderate depression: a double-blind, randomized and placebo-controlled trial [Internet]. Phytomedicine. 2006. Nov;13(9-10):607–11. [cited 2024 Sep 5]. 10.1016/j.phymed.2006.08.006 [DOI] [PubMed] [Google Scholar]
- Mazidi M, Shemshian M, Mousavi SH, Norouzy A, Kermani T, Moghiman T, et al. A double-blind, randomized and placebo-controlled trial of Saffron (Crocus sativus L.) in the treatment of anxiety and depression [Internet]. J Complement Integr Med. 2016. Jun;13(2):195–9. Available from: https://www.degruyter.com/document/doi/10.1515/jcim-2015-0043/html 10.1515/jcim-2015-0043 [DOI] [PubMed] [Google Scholar]
- Noorbala AA, Akhondzadeh S, Tahmacebi-Pour N, Jamshidi AH. Hydro-alcoholic extract of Crocus sativus L. versus fluoxetine in the treatment of mild to moderate depression: a double-blind, randomized pilot trial [Internet]. J Ethnopharmacol. 2005. Feb;97(2):281–4. [cited 2024 Sep 5]. 10.1016/j.jep.2004.11.004 [DOI] [PubMed] [Google Scholar]


