Abstract
Background
While SARS-CoV2 infection has been shown to be a significant risk-factor for several secondary bacterial, viral and Aspergillus infections, its impact on intensive care unit (ICU)-acquired candidemia (ICAC) remains poorly explored.
Method
Using the REA-REZO network (French surveillance network of ICU-acquired infections), we included all adult patients hospitalized for a medical reason of admission in participating ICUs for at least 48 h from January 2020 to January 2023. To account for confounders, a non-parsimonious propensity score matching was performed. Rates of ICAC according to SARS-CoV2 status were compared in matched patients. Factors associated with ICAC in COVID-19 patients were also assessed using a Fine-Gray model.
Results
A total of 55,268 patients hospitalized at least 48 h for a medical reason in 101 ICUs were included along the study period. Of those, 13,472 were tested positive for a SARS-CoV2 infection while 284 patients developed an ICAC. ICAC rate was higher in COVID-19 patients in both the overall population and the matched patients’ cohort (0.8% (107/13,472) versus 0.4% (173/41,796); p < 0.001 and 0.8% (93/12,241) versus 0.5% (57/12,241); p = 0.004, respectively). ICAC incidence rate was also higher in those patients (incidence rate 0.51 per 1000 patients-days in COVID-19 patients versus 0.32 per 1000 patients-days; incidence rate ratio: 1.58 [95% CI:1.08–2.35]; p = 0.018). Finally, patients with ICAC had a higher ICU mortality rate (49.6% versus 20.2%; p < 0.001).
Conclusion
In this large multicenter cohort of ICU patients, although remaining low, the rate of ICAC was higher among COVID-19 patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-024-05104-w.
Keywords: Candidaemia, COVID-19, ICU, Healthcare associated infection
Background
The clinical spectrum of severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) infections can lead to severe acute respiratory distress syndrome (ARDS), responsible for numerous hospitalizations in intensive care units (ICUs) with prolonged mechanical ventilation and high mortality [1]. Since the beginning of the SARS-CoV2 pandemic, critically ill patients have emerged as a population at high risk for secondary infections. Primarily studies focused on bacterial [2–4] (notably ventilator associated pneumonia and bloodstream infections) and on coronavirus disease 2019 (COVID-19) associated pulmonary aspergillosis [5, 6], evidencing a negative impact of such ICU-acquired infections on patients’ prognosis [7–10]. However, ICU-acquired candidemia (ICAC) has also been shown to have a high incidence in severe COVID-19 patients [5, 11–13]. Candida digestive colonization, occurring in about one-half of ICU patients [14, 15], is frequently reported to precede candidemia. In addition, the assessment of fecal mycobiome of severe COVID-19 patients showed an enrichment with members of the genus Candida along with prolonged decreased mycobiota diversity [16, 17]. Beyond the digestive manifestation of COVID-19 [18, 19], the high proportion of severe patients receiving broad spectrum antibiotics (either on initial case-management of severe COVID-19 patients or to treat bacterial secondary infection) may contribute to such a higher Candida colonization and could favor ICAC. In addition, the over-occupation of ICUs and compromised infection control measures during the SARS-CoV2 pandemic might have contributed to subsequent high incidence of ICAC and global higher incidence of candidemia cases along with the emergence of fluconazole-resistant Candida species [20, 21].
However, although Candida sp. is the most common fungal infection in ICU patients [22, 23], its incidence in ICU patients remains low making it challenging to investigate. We therefore sought to assess the relationship between SARS-CoV2 infection and the rate of ICAC in a large-scale multicenter nationwide cohort study.
Method
Study setting
This study was conducted using the REA-REZO prospective continuous multicenter cohort surveillance. This patient-based surveillance focusing on ICU-acquired infections is carried out on a voluntary basis by collecting data of all adult patients hospitalized for more than 48 h in any of the contributing ICUs to the REA-REZO network for more than 15 years using a standardized form completed for each patient. Detailed protocol for data collection and monitoring is available at: https://rearezo.chu-lyon.fr/. All patients received specific information about the potential use of their personal data for research purposes and were given the opportunity to refuse it. The study was carried out in accordance with the ethical standards of the Declaration of Helsinki, and the database was approved by the National Data Protection Commission (Commission nationale de l'informatique et des libertés, Number 919149) and by the institutional review board (CPP SUD ESTdIRB 00009118).
Study population and surveillance data
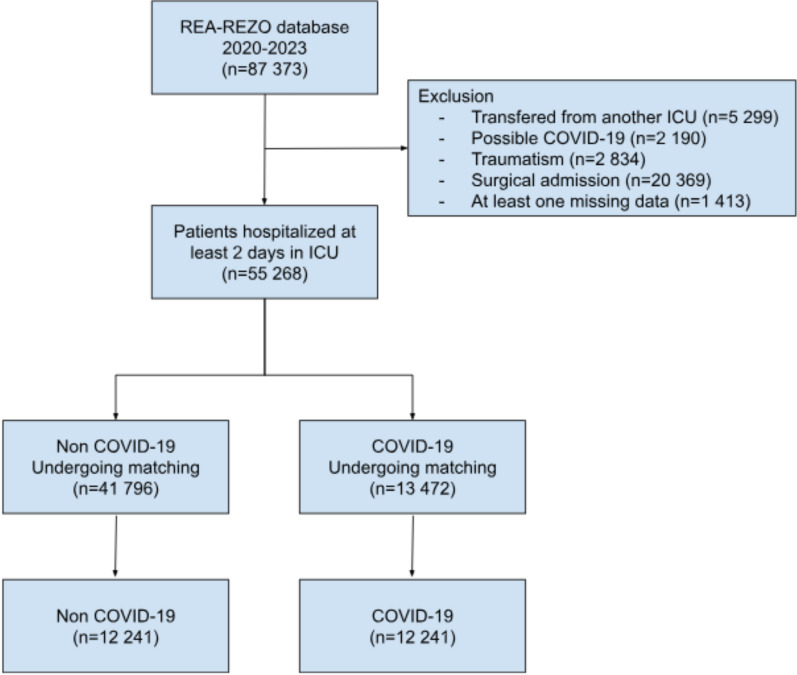
For the present analysis, all patients hospitalized for at least 2 days between January 2020 and January 2023 were included. Patients transferred from another ICU, patients having missing variable data needed for analysis, with a traumatic or nonmedical reason of admission (either elected or urgent surgery) as well as patients with possible COVID-19 (since at the beginning of the pandemic tests were not systematically available) were excluded (Fig. 1). Patients were prospectively evaluated and followed until ICU discharge or death. General patient characteristics analyzed included: age, sex severity assessed by the Simplified Acute Physiological Score II [24], antibiotherapy ± 2 days before or after ICU admission, origin of the patient (community or long term-care versus nosocomial), immunosuppression according to the Acute Physiology and Chronic Health Evaluation II definition [25], exposition to central venous catheter before ICAC onset, type of ICU and whether ExtraCorporeal Membrane Oxygenation was performed in the ICU (ECMO center).
Fig. 1.
Flow Chart
Definitions
COVID-19 was diagnosed with a positive RT-PCR (nasopharyngeal swabs, sputum, endotracheal aspiration, bronchoalveolar lavage). ICAC was defined by at least one positive blood culture positive for Candida sp. sampled after more than 48 h of ICU stay [26].
ICU were classified as medical when > 80% of patients admitted to the ICU had a medical reason for admission, surgical when > 80% of patients admitted to the ICU had a surgical reason for admission, and medical-surgical when > 80% of admissions were neither surgical nor medical.
Objectives
Our primary objective was to compare the rate of candidemia according to the exposure to SARS-CoV2 infection.
Secondary objectives included the comparison of clinical outcomes including the cumulative incidence of ICAC up to day-90 after ICU admission, ICU length of stay, duration of mechanical ventilation, the development of ventilator associated pneumonia (VAP) or bacterial bloodstream infection (BSI) as well as ICU mortality rate according to SARS-CoV2 infection status. Finally, we aimed to assess the risk -factors for ICAC in COVID-19 patients.
Statistical analysis
Data were reported as numbers (percentages) for categorical variables or medians (interquartile ranges: 25th–75th percentiles) for continuous variables. A propensity score (PS) matched analysis with a 1:1 ratio was performed to account for intergroup imbalance between COVID-19 and non-COVID-19 patients. PS was calculated using a non-parsimonious logistic regression model including every variable available during the period at risk for candidemia. Therefore, the following variables were included in PS calculation: Year of ICU admission, age, sex, SAPS II, type of ICU (Medical, Surgical or Medical-Surgical), ECMO center, provenance from community/nursing home, immunosuppression (both neutropenia and other kinds of immunosuppression), early treatment with antibiotics, use of central venous catheter and ICU length of stay before ICAC. Matching was performed based on a nearest-neighbor matching procedure with a 1:1 ratio and a caliper of 0.1 using the “MatchIt” package. Satisfactory matching was defined as an absolute value of the standardized mean difference (SMD) < 0.1 for all variables. In the matched population, we also estimated and compared the incidence rate (expressed as number of events per 1000 patients × ICU days) of ICAC during the first 90 days after ICU admission according to the COVID-19 status using ICU length-of-stay (censored at 90 days) as offset variable. In addition, competing risk analysis was used to estimate the cumulative incidence of the first episodes of ICAC between study groups considering death within 90 days and ICU discharge as competing events in order to take into account the time-dependent nature of ICAC. Curves until day 90 after ICU admission were compared using the gray test and hazard ratio (HR) with their 95% confidence interval (95%CI) was estimated using the fine and gray subdistribution hazard function. Patients with missing data needed were excluded from the analysis (n = 1413).
Finally, the fine-gray competing risk regression was also used to assess factors associated with the occurrence of ICAC in COVID-19 patients. Covariables achieving a p value < 0.2 in the univariable analysis were entered in the multivariable analysis.
Statistical analyses were performed with the statistical software R 4.1.1. All tests were two-sided, and p < 0.05 was considered statistically significant. The design of this study followed the Strengthening in Reporting of Observational Studies in Epidemiology (STROBE) guidelines [27].
Results
Entire cohort characteristics
During the study period, 55,268 patients admitted to 101 different ICUs for medical reasons were included in the present analysis (Fig. 1). The median age was 66 years old (IQR:56–74) and 35.7% were female. The epidemiological and clinical features of COVID-19 patients and non-COVID-19 patients are displayed in Table 1.
Table 1.
Characteristics of patients according to COVID-19 status
| Before propensity score matching | After propensity score matching | |||||
|---|---|---|---|---|---|---|
| Non-COVID-19 n = 41,796 |
COVID-19 n = 13,472 |
SMD | Non-COVID-19 n = 12,241 |
COVID-19 n = 12,241 |
SMD | |
| Baseline characteristics | ||||||
| Age (years) | 66 [55–74] | 66 [57–73] | 0.0444 | 67 [56–74] | 66 [56–73] | − 0.0118 |
| Male sex | 26,382 (63.1) | 9132 (67.8) | 0.0998 | 8166 (66.7) | 8221 (67.2) | 0.0096 |
| Immunosuppression | ||||||
| No immunodepression | 35,161 (84.1) | 11,513 (85.5) | 0.0378 | 10,360 (84.6) | 10,432 (85.2) | 0.0167 |
| Neutropenia | 1034 (2.5) | 117 (0.9) | − 0.1730 | 119 (1.0) | 115 (0.9) | − 0.003 |
| Other immunosuppression | 5601 (13.4) | 1842 (13.7) | 0.0079 | 1762 (14.4) | 1694 (13.8) | − 0.0162 |
| Simplified acute physiology score II | 46 [34–60] | 37 [29–48] | − 0.5473 | 38 [29–50] | 37 [29–48] | − 0.0164 |
| Year of ICU admission | ||||||
| 2020 | 15,398 (36.8) | 3284 (24.4) | − 0.2903 | 3135 (25.6) | 3218 (26.3) | 0.0158 |
| 2021 | 11,974 (28.6) | 7169 (53.2) | 0.4923 | 6286 (51.4) | 6107 (49.9) | − 0.0293 |
| 2022 | 14,424 (34.5) | 3019 (22.4) | − 0.2902 | 2820 (23.0) | 2916 (23.8) | 0.0188 |
| Type of ICU | ||||||
| Medical-surgical | 12,979 (31.1) | 4302 (31.9) | 0.0189 | 3919 (32.0) | 3923 (32.0) | 0.0007 |
| Medical | 28,502 (68.2) | 9085 (67.4) | − 0.0162 | 8232 (67.2) | 8237 (67.3) | 0.0009 |
| Surgical | 315 (0.8) | 85 (0.6) | − 0.0155 | 460 (3.7) | 471 (3.8) | − 0.0093 |
| ECMO Center | 38,683 (92.6) | 12,375 (91.9) | − 0.0254 | 11,211 (91.6) | 11,267 (92.0) | 0.0167 |
| Provenance from community or nursing home | 27,649 (66.1) | 7210 (53.5) | − 0.2533 | 6698 (54.7) | 6739 (55.1) | 0.0067 |
| ICU management | ||||||
| Need for mechanical ventilation | 22,801 (54.6) | 7119 (52.8) | − 0.0343 | 6084 (49.7) | 6214 (50.8) | 0.0213 |
| Antibiotherapy ± 2 days before or after ICU admission | 25,662 (61.4) | 8485 (63.0) | 0.0328 | 7813 (63.8) | 7686 (62.8) | − 0.0215 |
| Central venous catheter before ICAC | 27,391 (65.5) | 8069 (59.9) | − 0.1151 | 7005 (57.2) | 7160 (58.5) | 0.0258 |
| ICU length of stay before ICAC (days) | 5 [3–10] | 9 [5–19] | 0.4082 | 6 [3–14] | 9 [5–17] | 0.0554 |
Data are presented as median (IQR: interquartiles), n (%)
COVID-19: Coronavirus disease 2019; ICU: Intensive Care Unit; ICAC: ICU-acquired candidaemia; SMD: Standardized Mean Difference
At least one episode of ICAC occurred in 280 patients (0.5%) at a median delay from ICU admission of 12 days (IQR:7–24). The crude rate of ICAC was higher in COVID-19 patients (0.8% vs. 0.4%; p < 0.001). The most common Candida species identified from blood culture was Candida albicans accounting for 62.9% of all Candida species (176/280). Catheter related ICAC was the source of candidemia observed in 31.9% of all ICAC cases.
Patients with ICAC also experienced VAP and BSI more frequently compared to those without ICAC (55.7% versus 12.1%; p < 0.001 and 48.2% vs. 4.5%; p < 0.001, respectively). Noteworthy, among patients with ICAC, the proportion of VAP and BSI preceding ICAC were 61.5% (96/156) and 60.7% (82/135), respectively. The median time from the diagnosis of ICAC to catheter removal in patients with catheter-related ICAC was 2 (IQR 0.5–11) days. Finally, patients with ICAC had a higher ICU mortality rate (49.6% versus 20.2%; p < 0.001) as presented in Supplementary Table 1.
Propensity score matched analysis
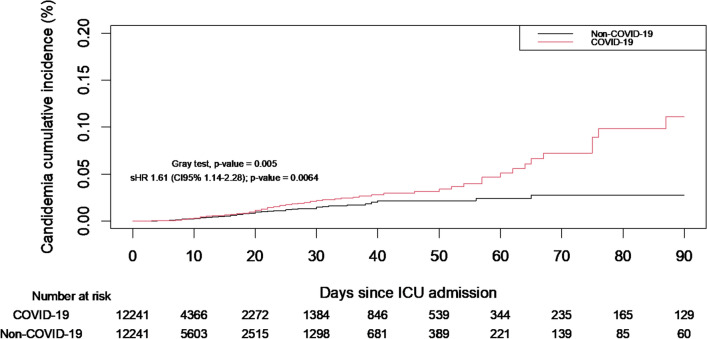
In order to overcome baseline differences between groups, a propensity score matched analysis was performed. The density plot of the propensity score of included patients is presented in Supplementary Fig. 1. Of the 55 268 included patients, 12 241 patients among non-COVID-19 patients were matched with 12 241 COVID-19 patients. The baseline characteristics between the two groups were reassessed after propensity score matching and appeared well balanced (SMD < 0.1) as displayed in Table 1 and in Supplementary Fig. 2. In the matched population, the rate of ICAC was higher in COVID-19 patients as compared to non-COVID-19 patients (0.8% vs. 0.5%; p = 0.004) as presented in Table 2. The distribution of Candida species as well as sources of ICAC were comparable between groups (Table 2). The delay between ICU admission and ICAC did not differ between COVID-19 patients and non-COVID-19 patients (20 days (IQR 11–31) versus 16 days (IQR 8–25); p = 0.067). In addition, the proportion of patients developing either VAP or bacterial BSI was higher in COVID-19 patients (7.7% versus 5.5%; p < 0.001 and 22.3% versus 13.1%; p < 0.001). Veno-venous ECMO were also more frequent in COVID-19 patients (2.7% versus 1.1%; p < 0.001). Cumulative incidence analysis also showed an increased incidence of ICAC in COVID-19 patients (gray test p = 0.005) (Fig. 2). Furthermore, when performing competing risk analysis to take into account the time dependent nature of ICAC, such an association between COVID-19 and the increased incidence of ICAC was also observed (sdHR = 1.61 [95% CI:1.14–2.28]; p = 0.006). Notably, COVID-19 patients had a higher ICU mortality rate (21.9% versus 15.7%; p < 0.001). Finally, the incidence rate of ICAC was higher in COVID-19 patients (incidence rate 0.51 per 1000 patients-days versus 0.32 per 1000 patients-days; incidence rate ratio: 1.58 [95% CI:1.08–2.35]; p = 0.018).
Table 2.
Clinical course and outcomes of patients according to COVID-19 status
| Before propensity score matching | After propensity score matching | |||||
|---|---|---|---|---|---|---|
| Non-COVID-19 n = 41,796 |
COVID-19 n = 13,472 |
p-value | Non-COVID-19 n = 12,241 |
COVID-19 n = 12,241 |
p-value | |
| Clinical outcomes | ||||||
| Candidaemia | 173 (0.4) | 107 (0.8) | < 0.001 | 57 (0.5) | 93 (0.8) | 0.004 |
| Candida species isolated | 0.126 | 0.804 | ||||
| Candida albicans | 109 (63.0) | 67 (62.6) | 38 (66.7) | 60 (64.5) | ||
| Candida parapsilosis | 14 (8.1) | 19 (17.8) | 7 (12.3) | 16 (17.2) | ||
| Candida glabrata | 24 (13.9) | 12 (11.2) | 5 (8.8) | 8 (8.6) | ||
| Candida krusei | 6 (3.5) | 1 (0.9) | 0 (0.0) | 1 (1.1) | ||
| Candida tropicalis | 4 (2.3) | 1 (0.9) | 2 (3.5) | 1 (1.1) | ||
| Other Candida species | 16 (9.2) | 7 (6.5) | 5 (8.8) | 7 (7.5) | ||
| Suspected sources of candidaemia* | 0.113 | 0.669 | ||||
| Catheter | 51 (29.5) | 36 (33.6) | 15 (26.3) | 30 (32.2) | ||
| Digestive | 25 (14.5) | 5 (4.7) | 3 (5.3) | 4 (4.3) | ||
| Pleuro-pulmonary | 16 (9.2) | 15 (14.0) | 6 (10.5) | 14 (15.1) | ||
| Urinary | 7 (4.0) | 5 (4.7) | 2 (3.5) | 4 (4.3) | ||
| Skin/soft tissue | 2 (1.2) | 0 (0.0) | 1 (1.8) | 0 (0.0) | ||
| Other | 5 (2.9) | 1 (0.9) | 2 (3.5) | 1 (1.1) | ||
| Unknown | 67 (38.7) | 45 (42.1) | 28 (49.1) | 40 (43.0) | ||
| Median delay of candidaemia | 9 [6–18] | 21 [11–35] | < 0.001 | 16 [8–25] | 20 [11–31] | 0.067 |
| Need for a dialysis catheter | 4202 (10.1) | 1077 (8.0) | < 0.001 | 1118 (9.1) | 907 (7.4) | < 0.001 |
| Bacteremia | 1364 (3.3) | 1230 (9.1) | < 0.001 | 669 (5.5) | 945 (7.7) | < 0.001 |
| Ventilator associated pneumonia | 3411 (8.2) | 3423 (25.4) | < 0.001 | 1603 (13.1) | 2729 (22.3) | < 0.001 |
| Venoarterial ECMO | 172 (0.4) | 33 (0.2) | 0.005 | 40 (0.3) | 29 (0.2) | 0.185 |
| Venovenous ECMO | 382 (0.9) | 385 (2.9) | < 0.001 | 130 (1.1) | 332 (2.7) | < 0.001 |
| Duration of mechanical ventilation | 1 [0–5] | 2 [0–14] | < 0.001 | 0 [0–8] | 0 [1–11] | < 0.001 |
| ICU case fatality | 8283 (19.8) | 2970 (22.0) | < 0.001 | 1923 (15.7) | 2683 (21.9) | < 0.001 |
Data are presented as median (IQR: interquartiles), n (%)
Abbreviations: COVID-19: Coronavirus disease 2019; ICU: Intensive Care Unit; OR: Odds Ratio; 95%CI: 95% confidence interval
* Source of candidemia was assessed when colonization with the same Candida Spp was identified as causative pathogen
Fig. 2.
Cumulative incidence of candidaemia in matched patients according to COVID-19 status
Of note, among unmatched non-COVID-19 patients, the ICAC rate was 0.4% (116/29 555).
Sensitivity analysis
When analysing variables associated with ICAC in COVID-19 patients, need for mechanical ventilation (sdHR 5.11 [95%CI:1.16–22.43; p = 0.03]) and bacteremia before ICAC onset (sdHR 2.25 [95%CI:1.52–3.32; p < 0.001]) were the only variables that remained independently associated with the occurrence of ICAC while immunosuppression (either neutropenia or other kind of immunosuppression) was not found to be a risk-factor for ICAC as exposed in Supplementary Table 2.
Discussion
This large cohort study including adult patients admitted to ICUs for a medical reason evidenced an increased rate of ICAC in COVID-19 patients.
The SARS-CoV2 pandemic has changed the global medical landscape, resulting in severe illness and millions of deaths worldwide with large populations of patients needing ICU supportive care and prolonged mechanical ventilation [1, 28]. Beyond direct viral lethality and the initial management of patients with COVID-19, clinicians have had to contend with high rates of secondary infections with a high proportion of ICU-related deaths attributable to those secondary infections.
In the present study, the rate of ICAC appeared increased in COVID-19 patients compared to non-COVID-19 patients. Similarly, high rates of bacterial VAP were previously observed in COVID-19 patients. Such an increased risk for acquired infections might have been promoted by several factors. Firstly, the SARS-COV2 virus drives a myriad of immune disorders that could contribute to higher susceptibility and severity of secondary infections [29]. Secondly, although therapeutic interventions initially focused on treatments to reduce the viral load of SARS-COV2[30], the most effective drugs for preventing severe forms of COVID-19 proved to be immunosuppressive treatments (namely corticosteroids and interleukin-6 receptor antagonists) [31, 32]. Those treatments which aim to control the consequences of immune activation caused by SARS-CoV2 tissue invasion, may also increase the risk of secondary infections by reducing the ability of patients' immune systems to prevent and eliminate the microorganisms involved in secondary infections [5, 33–35]. Thirdly, severe COVID-19 patients are often placed under prolonged mechanical ventilation, needing prolonged central venous and urinary catheters. The use of these invasive procedures can also increase the penetration of microorganisms, and consequently the risk of nosocomial infection [36, 37]. Along these lines COVID-19 patients appeared to require veno-venous ECMO more frequently than non-COVID-19 patients. This could be due to the clinical presentation of critically ill patients with common severe ARDS in COVID-19 patients, making them more likely to require veno-venous ECMO assistance. Conversely, veno-arterial ECMO was less frequent in COVID-19 patients, and SAPS II scores prior to propensity score matching appeared lower in these patients.
The present study using an extensive surveillance network, confirms the conclusions of other smaller cohort studies [5, 11–13]. Furthermore, the large cohort of patients included in the present analysis allows us to compare the risk of ICAC between COVID-19 and non-COVID-19 patients. The increased rate of ICAC in COVID-19 patients is noteworthy. Although being uncommon, affecting less than 1% of severe COVID-19 patients, the consequences of these infections deserve to be emphasized with a survival rate dropping from 79.8% to 50.7% in patients developing ICAC. Such an impact on patients’ outcomes makes it necessary to explore potentially avoidable risk factors. Nonetheless, the direct impact of ICAC on patient’s survival should be interpreted with caution as patients with ICAC also often developed other ICU-acquired infections (namely BSI and VAP) which preceded ICAC in nearly 60% of cases and may have also contributed to the mortality rate in these critically ill patients. Previous studies reported increased ICU mortality related to bacterial VAP and invasive pulmonary aspergillosis [5, 7, 38] which could encourage clinicians to prevent them whether by reinforcing hygiene measures or through other preventive measures such as selective digestive decontamination given its effect on the occurrence of ICU-acquired infections (either bacterial or fungal) [39–41]. Beyond the increase in incidence, the emergence of fluconazole-resistant Candida species, already highlighted, could contribute to a crucial change in the ICAC landscape in the COVID-19 era, underlining the need for constant vigilance [20, 21]. It should be noted that when assessing risk-factors for ICAC in COVID-19 patients, neither immunosuppression nor SAPS II score were identified as independent predictors. While previous studies have shown these covariates to be independent predictors of candidemia in non-COVID-19 patients [42, 43], investigations in COVID-19 patients have consistently found no association between ICU admission severity, immunosuppression and candidemia [42, 43], in the context of COVID-19 patients, investigations of risk factors for ICAC have already found no association between severity on ICU admission or immunosuppression and candidemia [44–46]. This lack of association warrants particular attention to candidemia, even in non-severe, non-immunocompromised COVID-19 patients.
Although several other cohort studies have already attempted to decipher the ICAC landscape in the COVID-19 era, most were retrospective, and involved smaller sample sizes, which may affect their ability to control for confounding bias [11, 13, 35, 47]. In contrast, the present study accounted for both the time-dependent nature of ICAC and competing events (enabling to control for events “competing” with the event of interest). In ICU patients, failing to account for these competing events when assessing the relationship between COVID-19 status and ICAC could result in biased estimates [48, 49].
Interestingly, in the assessment of independent risk factors for ICAC in COVID-19 patients, common risk factors such as central venous catheter, immunosuppression, antibiotic therapy or severity on ICU admission were not identified as significant [42, 43]. However, antibiotic therapy tended to be associated with ICAC, while mechanical ventilation and bacteremia prior to ICAC were the only covariates that remained independent risk factors for ICAC in multivariable analysis. The need for mechanical ventilation may increase the likelihood of receiving corticosteroids and interleukin-6 receptor antagonists, which have been previously linked to ICAC in COVID-19 patients [45, 46]. Furthermore, bacteremia prior to ICAC might have favored antimicrobial use as well as sepsis-induced immune dysfunction that could promote the development of ICAC [42, 43, 50, 51].
Although being the largest study to explore ICAC in COVID-19 and non-COVID-19 patients our study suffers from limitations that must be acknowledged.
Firstly, despite performing a non-parsimonious propensity score in order to overcome baseline differences between groups, residual confounding factors are inherent to the observational nature of our study which may limit conclusions from being drawn. Secondly, the surge of ICU that was promoted by the SARS-CoV2 pandemic might have resulted in significant changes in care practice with increased workload that may have prevented strict and thorough implementation of preventive bundles. However, when comparing the different years of ICU admission, we did not notice an increased risk of ICAC during the first waves of the SARS-CoV2 pandemic. Thirdly, due to limited data availability, we were unable to assess several relevant covariates that could be risk factors for ICAC such as the need for vasopressors, Charlson’s comorbidity index, abdominal surgery, and the use of interleukin-6 receptor antagonists or corticosteroids. Consequently, residual confounding factors may remain, making it challenging to draw definitive conclusions. In addition, although only patients admitted to the ICU for a medical reason were included, sensitivity analyses based on the different medical reasons for ICU admission could not be performed. Such analyses would have added greater homogeneity to the patient groups. Conversely, our results cannot be generalized to surgical or trauma patients. Fourthly, as diagnosing the sources of ICAC can be difficult (with the exception of catheter-related candidiasis), uncertainties may remain when evaluating this parameter. As a result, a significant number of ICAC cases had an unknown suspected source, which could have limited the assessment of source control in this specific pathology. Finally, by limiting the follow-up of included patients to ICU stay, the long-term impact of COVID-19 on ICAC occurrence could not be assessed.
In conclusion, although our study has several limitations, through this large exploratory cohort we observed an increased risk of ICAC in COVID-19 patients although crude incidence remained low.
Supplementary Information
Acknowledgements
The authors would like to thank Alison Mac Lean, Medical Librarian, Hospital Center of Vannes, for her help in drafting the article.
REAREZO study group
Serge Alfandari, Alexandra Allaire, Antonio Alvarez, Ammenouche Nacim, Laurent Argaus, Gérard Audibert, Caroline Aurel, Odile Bajolet, Frédéric Barbut, Genevieve Barjon, Patricia Baune, Sébastien Beague, Bassam Beilouny, Nicolas Bele, Nicolas Belin, Cécile Bernerd, Yasmina Berrouane, Aziz Berrouba, Julie Bertrand, Claire Bianchi, Sandrine Biangoma, Fabienne Birot Jaulin, Severine Bonjean, Stéphanie Bordes-Couecou, Abdenour Bouhara, Philippe Bouillard, Céline Bourigault, Sylvie Bourzeix, Sébastien Boutreux, Hanene Bouzidi, Julie Brochart, Stéphanie Bulyez, Marie Callanquin, Nathalie Canu, Matthieu Capron, Daniel Carbognani, Vincent Castelain, Vincent Catanese, Isabelle Cattaneo, Vanessa Chartier, Guillaume Chassaing, Robert Chausset, Mélanie Chauvet, Fabrice Chopin, Catherine Chubilleau, Céline Clayer, Agnès Cohen, Sylvie Comparot, Philippe Corne, Marie-Elisabeth Cornesse, Gaelle Corno, Esther Cortes, Patricia Courouble, Christian Crombe, Véronique Curnier, Monzer Dabbachi, Cédric Dananché, Abla Daroukh, Damien Dassant, Martine Daumas, Aurélien Daurat, Dominique Deffarges, Fanny Delanghe, Olivier Delastre, Joel Delhomme, Jean Paul Délias, Martine Delorme, Fabienne Derramond, Frédérique Diaw, Isabelle Dijols, Kamel Djedaini, Loic Dopeux, Sophie Duhoo, Thierry Dulac, Clarisse Dupin, Laurène Dupont, Michel Durand, Isabelle Durand Joly, Jean-Yves Dusseau, Pierre Yves Egreteau, Carole Eldin, Florence Espinasse, Eric Farfour, Abdelhamid Fatah, Yannick Fedun, Luis Ferreira, Pierre Fillatre, Toufic Finge, Véronique Fleurial, Arnaud Florentin, Agnès Fribourg, Severine Gallais-Hoff, Claude Galland, Richard Galliot, Sylvain Garnier, Gaelle Gasan, Julien Gaubert-Duclos, Valérie Gauzere, Thomas Geffriaud, Isabelle Geneau, Hughes Georges, Solweig Gerbier Colomban, Christophe Giacardi, Sebastien Gibot, Audrey Glanard, Marion Gleize, Marieline Goret, Michele Gourgues, Delphine Grau, Béatrice Grisi, Clotilde Groleau, Liliane Grolier-Bois, Catherine Guignabert, Fethi Hadj-Slimane, Emmanuelle Hammad, Catherine Haond, Marie Hélène Hausermann, Francoise Hayo, Christophe Henry, Alexandre Herbland, Julien Huntzinger, Hervé Hyvernat, Alexandre Jean, Boris Jolibois, Sylvie Joron, Gauthier Julien, Jean Kempf, Lyes Knani, Béatrice La Combe, Marie Labruyere, Sandrine Lacroix, Bruno Lafon, Katia Lamant, Peggy Larroudé, Anne Launoy, Bernadette Laurent, Thierry Lavigne, Christine Lawrence, Quoc Vien Le, Muriel Le Coq, Anne-Sophie Le Floch, Fanny Le Fall, Brigitte Le Tallec, Lucie Lecoutre, Stanislas Ledochowski, Rusel Leon, Claire Lepouse, Thomas Lescot, Mélanie Levrard, Marie Laure Lier, Anne Lignereux, Benjamin Louart, Claire Maheu, Aurélie Maindron, Francois Mallard, Marie Reine Mallaret, Bernard Mankikian, Christiane Manzon, Philippe Mardrus, Jacques Mariot, Audry Martin, Emmanuelle Martin, Maelle Martin, Pascale Martres, Virginie Maxime, Olivier Meunier, Ella-Pauline Meyer, Ferhat Meziani, Sébastien Moschietto, Céline Muller, Elodie Munier-Marion, Caroline Neulier, François Nicolas, Jacques-Yves Nizou, Christine Palitta, Michel Pascal, Olivier Passouant, René-Gilles Patrigeon, Frédérique Pavillard, Sabine Peghaire, Christophe Perdrix, Jean-Sebastien Petit, Judith Pibre, Walter Picard, Sylvie Picault, Santiago Picos Gil, Jérôme Pillot, Patrick Pina, Rémi Plattier, Laurent Poiron, Christian Pommier, Gaël Pradel, Cristian Prelipcean, Paul-Simon Pugliesi, Vincent Quenee, Olga Raposo, Eve Remy, Sabine Reynaud Deforges, Jean-Christophe Richard, Sylvie Ricome, Thomas Rimmele, Adrien Robine, Anne-Claude Roche, Laetitia Rohr, Gwenaël Rolland-Jacob, Adrien Roques, Catherine Rougier, Jérôme Roustan, Mélanie Saint-Leger, Faouzi Saliba, Dominique Sechaud, Amine Si-Ali, Catherine Simac, Georges Simon, Michel Sirodot, Vincent Stoeckel, Philippe Tagawa, Marine Tasle, Fabrice Thiollière, Benoit Thiphagne, Aurélie Thomas-Hervieu, François Tinturier, Alexandre Tonnelier, Alexandre Toro, David Tranvan, Dominique Trivier, Gilles Troché, Rémi Trusson, Lionel Ursulet, Marie Laure Valdeyron, Catherine Vallet, Vanessa Van Rossem, Laurence Vasse, Myriam Venelle, Christine Venot, Antoine Vieillard-Baron, Jean-François Vincent, Michel Vitris, Hussein Yassine, Lassane Zanre, Cecile Zylberfajn.
Author contributions
F.R., N.M., Al.M, A.F. and A.L. conceived, designed, coordinated the data collection and supervised the study. F.R., N.M., Al.M., Y.F., C.H.V., A.S., A.F., A.F. and A.L. collected and interpreted the data. F.R. performed the statistical analysis. F.R. wrote the first draft of the article. All authors revised the manuscript and approved the final version of the manuscript.
Funding
No funding was received for this work.
Availability of data and materials
The datasets from this study are available from the corresponding author on request.
Ethics approval and consent to participate
All patients received specific information about the potential use of their personal data for research purposes and were given the opportunity to refuse it. The study was carried out in accordance with the ethical standards of the Declaration of Helsinki, and the database was approved by the National Data Protection Commission (Commission nationale de l'informatique et des libertés, Number 919149) and by the institutional review board (CPP SUD ESTdIRB 00009118).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Florian Reizine, Email: florian.reizine@gmail.com.
the REAREZO study group:
Serge Alfandari, Alexandra Allaire, Antonio Alvarez, Ammenouche Nacim, Laurent Argaus, Gérard Audibert, Caroline Aurel, Odile Bajolet, Frédéric Barbut, Genevieve Barjon, Patricia Baune, Sébastien Beague, Bassam Beilouny, Nicolas Bele, Nicolas Belin, Cécile Bernerd, Yasmina Berrouane, Aziz Berrouba, Julie Bertrand, Claire Bianchi, Sandrine Biangoma, Fabienne Birot Jaulin, Severine Bonjean, Stéphanie Bordes-Couecou, Abdenour Bouhara, Philippe Bouillard, Céline Bourigault, Sylvie Bourzeix, Sébastien Boutreux, Hanene Bouzidi, Julie Brochart, Stéphanie Bulyez, Marie Callanquin, Nathalie Canu, Matthieu Capron, Daniel Carbognani, Vincent Castelain, Vincent Catanese, Isabelle Cattaneo, Vanessa Chartier, Guillaume Chassaing, Robert Chausset, Mélanie Chauvet, Fabrice Chopin, Catherine Chubilleau, Céline Clayer, Agnès Cohen, Sylvie Comparot, Philippe Corne, Marie-Elisabeth Cornesse, Gaelle Corno, Esther Cortes, Patricia Courouble, Christian Crombe, Véronique Curnier, Monzer Dabbachi, Cédric Dananché, Abla Daroukh, Damien Dassant, Martine Daumas, Aurélien Daurat, Dominique Deffarges, Fanny Delanghe, Olivier Delastre, Joel Delhomme, Jean Paul Délias, Martine Delorme, Fabienne Derramond, Frédérique Diaw, Isabelle Dijols, Kamel Djedaini, Loic Dopeux, Sophie Duhoo, Thierry Dulac, Clarisse Dupin, Laurène Dupont, Michel Durand, Isabelle Durand Joly, Jean-Yves Dusseau, Pierre Yves Egreteau, Carole Eldin, Florence Espinasse, Eric Farfour, Abdelhamid Fatah, Yannick Fedun, Luis Ferreira, Pierre Fillatre, Toufic Finge, Véronique Fleurial, Arnaud Florentin, Agnès Fribourg, Severine Gallais-Hoff, Claude Galland, Richard Galliot, Sylvain Garnier, Gaelle Gasan, Julien Gaubert-Duclos, Valérie Gauzere, Thomas Geffriaud, Isabelle Geneau, Hughes Georges, Solweig Gerbier Colomban, Christophe Giacardi, Sebastien Gibot, Audrey Glanard, Marion Gleize, Marieline Goret, Michele Gourgues, Delphine Grau, Béatrice Grisi, Clotilde Groleau, Liliane Grolier-Bois, Catherine Guignabert, Fethi Hadj-Slimane, Emmanuelle Hammad, Catherine Haond, Marie Hélène Hausermann, Francoise Hayo, Christophe Henry, Alexandre Herbland, Julien Huntzinger, Hervé Hyvernat, Alexandre Jean, Boris Jolibois, Sylvie Joron, Gauthier Julien, Jean Kempf, Lyes Knani, Béatrice La Combe, Marie Labruyere, Sandrine Lacroix, Bruno Lafon, Katia Lamant, Peggy Larroudé, Anne Launoy, Bernadette Laurent, Thierry Lavigne, Christine Lawrence, Quoc Vien Le, Muriel Le Coq, Anne-Sophie Le Floch, Fanny Le Fall, Brigitte Le Tallec, Lucie Lecoutre, Stanislas Ledochowski, Rusel Leon, Claire Lepouse, Thomas Lescot, Mélanie Levrard, Marie Laure Lier, Anne Lignereux, Benjamin Louart, Claire Maheu, Aurélie Maindron, Francois Mallard, Marie Reine Mallaret, Bernard Mankikian, Christiane Manzon, Philippe Mardrus, Jacques Mariot, Audry Martin, Emmanuelle Martin, Maelle Martin, Pascale Martres, Virginie Maxime, Olivier Meunier, Ella-Pauline Meyer, Ferhat Meziani, Sébastien Moschietto, Céline Muller, Elodie Munier-Marion, Caroline Neulier, François Nicolas, Jacques-Yves Nizou, Christine Palitta, Michel Pascal, Olivier Passouant, René-Gilles Patrigeon, Frédérique Pavillard, Sabine Peghaire, Christophe Perdrix, Jean-Sebastien Petit, Judith Pibre, Walter Picard, Sylvie Picault, Santiago Picos Gil, Jérôme Pillot, Patrick Pina, Rémi Plattier, Laurent Poiron, Christian Pommier, Gaël Pradel, Cristian Prelipcean, Paul-Simon Pugliesi, Vincent Quenee, Olga Raposo, Eve Remy, Sabine Reynaud Deforges, Jean-Christophe Richard, Sylvie Ricome, Thomas Rimmele, Adrien Robine, Anne-Claude Roche, Laetitia Rohr, Gwenaël Rolland-Jacob, Adrien Roques, Catherine Rougier, Jérôme Roustan, Mélanie Saint-Leger, Faouzi Saliba, Dominique Sechaud, Amine Si-Ali, Catherine Simac, Georges Simon, Michel Sirodot, Vincent Stoeckel, Philippe Tagawa, Marine Tasle, Fabrice Thiollière, Benoit Thiphagne, Aurélie Thomas-Hervieu, François Tinturier, Alexandre Tonnelier, Alexandre Toro, David Tranvan, Dominique Trivier, Gilles Troché, Rémi Trusson, Lionel Ursulet, Marie Laure Valdeyron, Catherine Vallet, Vanessa Van Rossem, Laurence Vasse, Myriam Venelle, Christine Venot, Antoine Vieillard-Baron, Jean-François Vincent, Michel Vitris, Hussein Yassine, Lassane Zanre, and Cecile Zylberfajn
References
- 1.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rouzé A, Martin-Loeches I, Povoa P, Makris D, Artigas A, Bouchereau M, et al. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: a European multicenter cohort study. Intensive Care Med. 2021;47:188–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lepape A, Machut A, Bretonnière C, Friggeri A, Vacheron C-H, Savey A, et al. Effect of SARS-CoV-2 infection and pandemic period on healthcare-associated infections acquired in intensive care units. Clin Microbiol Infect. 2023;29:530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massart N, Maxime V, Fillatre P, Razazi K, Ferré A, Moine P, et al. Characteristics and prognosis of bloodstream infection in patients with COVID-19 admitted in the ICU: an ancillary study of the COVID-ICU study. Annals of Intensive Care [Internet]. 2021 [cited 2023 Oct 26];11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8708508/ [DOI] [PMC free article] [PubMed]
- 5.Gangneux J-P, Dannaoui E, Fekkar A, Luyt C-E, Botterel F, De Prost N, et al. Fungal infections in mechanically ventilated patients with COVID-19 during the first wave: the French multicentre MYCOVID study. Lancet Respir Med. 2022;10:180–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White PL, Dhillon R, Cordey A, Hughes H, Faggian F, Soni S, et al. A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICU. Clin Infect Dis. 2020; [DOI] [PMC free article] [PubMed]
- 7.Vacheron C-H, Lepape A, Savey A, Machut A, Timsit JF, Comparot S, et al. Attributable mortality of ventilator-associated pneumonia among patients with COVID-19. Am J Respir Crit Care Med. 2022;206:161–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nseir S, Martin-Loeches I, Povoa P, Metzelard M, Du Cheyron D, Lambiotte F, et al. Relationship between ventilator-associated pneumonia and mortality in COVID-19 patients: a planned ancillary analysis of the coVAPid cohort. Crit Care. 2021;25:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buetti N, Ruckly S, de Montmollin E, Reignier J, Terzi N, Cohen Y, et al. COVID-19 increased the risk of ICU-acquired bloodstream infections: a case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med. 2021;47:180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buetti N, Tabah A, Loiodice A, Ruckly S, Aslan AT, Montrucchio G, et al. Different epidemiology of bloodstream infections in COVID-19 compared to non-COVID-19 critically ill patients: a descriptive analysis of the Eurobact II study. Crit Care. 2022;26:319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alessandri F, Ceccarelli G, Migliara G, Baccolini V, Russo A, Marzuillo C, et al. High incidence of candidemia in critically Ill COVID-19 patients supported by veno-venous extracorporeal membrane oxygenation: a retrospective study. J Fungi (Basel). 2023;9:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nucci M, Barreiros G, Guimarães LF, Deriquehem VAS, Castiñeiras AC, Nouér SA. Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses. 2021;64:152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mastrangelo A, Germinario BN, Ferrante M, Frangi C, Li Voti R, Muccini C, et al. Candidemia in coronavirus disease 2019 (COVID-19) patients: incidence and characteristics in a prospective cohort compared with historical non-COVID-19 controls. Clin Infect Dis. 2021;73:e2838–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alenazy H, Alghamdi A, Pinto R, Daneman N. Candida colonization as a predictor of invasive candidiasis in non-neutropenic ICU patients with sepsis: a systematic review and meta-analysis. Int J Infect Dis. 2021;102:357–62. [DOI] [PubMed] [Google Scholar]
- 15.Blot S, Vandewoude K. Management of invasive candidiasis in critically ill patients. Drugs. 2004;64:2159–75. [DOI] [PubMed] [Google Scholar]
- 16.Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Zhan H, et al. Alterations in gut microbiota of patients With COVID-19 during time of hospitalization. Gastroenterology. 2020;159:944-955.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maeda Y, Motooka D, Kawasaki T, Oki H, Noda Y, Adachi Y, et al. Longitudinal alterations of the gut mycobiota and microbiota on COVID-19 severity. BMC Infect Dis. 2022;22:572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elmunzer BJ, Spitzer RL, Foster LD, Merchant AA, Howard EF, Patel VA, et al. Digestive manifestations in patients hospitalized with coronavirus disease 2019. Clin Gastroenterol Hepatol. 2021;19:1355-1365.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El Moheb M, Naar L, Christensen MA, Kapoen C, Maurer LR, Farhat M, et al. Gastrointestinal complications in critically Ill patients with and without COVID-19. JAMA. 2020;324:1899–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Najafzadeh MJ, Shaban T, Zarrinfar H, Sedaghat A, Hosseinikargar N, Berenji F, et al. COVID-19 associated candidemia: from a shift in fungal epidemiology to a rise in azole drug resistance. Med Mycol. 2024;62:myae031. [DOI] [PubMed] [Google Scholar]
- 21.Siopi M, Georgiou P-C, Paranos P, Beredaki M-I, Tarpatzi A, Kalogeropoulou E, et al. Increase in candidemia cases and emergence of fluconazole-resistant. Euro Surveill. 2024;2024(29):2300661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vincent J-L, Sakr Y, Singer M, Martin-Loeches I, Machado FR, Marshall JC, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 2020;323:1478–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tabah A, Buetti N, Staiquly Q, Ruckly S, Akova M, Aslan AT, et al. Epidemiology and outcomes of hospital-acquired bloodstream infections in intensive care unit patients: the EUROBACT-2 international cohort study. Intensive Care Med. 2023;49:178–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63. [DOI] [PubMed] [Google Scholar]
- 25.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 26.Plachouras D, Lepape A, Suetens C. ECDC definitions and methods for the surveillance of healthcare-associated infections in intensive care units. Intensive Care Med. 2018;44:2216–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. [DOI] [PubMed] [Google Scholar]
- 28.COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73. [DOI] [PMC free article] [PubMed]
- 29.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19—final report. N Engl J Med. 2020;383:1813–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384:693–704. [DOI] [PMC free article] [PubMed]
- 32.REMAP-CAP Investigators, Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, Nichol AD, et al. Interleukin-6 receptor antagonists in critically Ill patients with Covid-19. N Engl J Med. 2021;384:1491–502 [DOI] [PMC free article] [PubMed]
- 33.Lamouche-Wilquin P, Souchard J, Pere M, Raymond M, Asfar P, Darreau C, et al. Early steroids and ventilator-associated pneumonia in COVID-19-related ARDS. Crit Care. 2022;26:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khan S, Bilal H, Khan MN, Fang W, Chang W, Yin B, et al. Interleukin inhibitors and the associated risk of candidiasis. Front Immunol. 2024;15:1372693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kayaaslan B, Eser F, Asilturk D, Oktay Z, Hasanoglu I, Kalem AK, et al. Development and validation of COVID-19 associated candidemia score (CAC-Score) in ICU patients. Mycoses. 2023;66:128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ford D, Reveles K, Hoban C, Koutoubi S, Cadena J. Effects of COVID-19 hospitalization rates on the incidence of hospital-acquired Candida central line-associated bloodstream infection. Am J Infect Control. 2024;52:387–91. [DOI] [PubMed] [Google Scholar]
- 37.Arastehfar A, Ünal N, Hoşbul T, Alper Özarslan M, Sultan Karakoyun A, Polat F, et al. Candidemia among coronavirus disease 2019 patients in Turkey admitted to intensive care units: a retrospective multicenter study. Open Forum Infect Dis. 2022;9:ofac078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schauwvlieghe AFAD, Rijnders BJA, Philips N, Verwijs R, Vanderbeke L, Van Tienen C, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med. 2018;6:782–92. [DOI] [PubMed] [Google Scholar]
- 39.Buil JB, Schouten JA, Wauters J, van de Hoeven H, Verweij PE, CAC-SDD study group. Absence of candidemia in critically ill patients with COVID-19 receiving selective digestive decontamination. Intensive Care Med. 2022;48:611–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Jonge E, Schultz MJ, Spanjaard L, Bossuyt PMM, Vroom MB, Dankert J, et al. Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet. 2003;362:1011–6. [DOI] [PubMed] [Google Scholar]
- 41.Hurley JC. ICU-acquired candidemia within selective digestive decontamination studies: a meta-analysis. Intensive Care Med. 2015;41:1877–85. [DOI] [PubMed] [Google Scholar]
- 42.Poissy J, Damonti L, Bignon A, Khanna N, Von Kietzell M, Boggian K, et al. Risk factors for candidemia: a prospective matched case-control study. Crit Care. 2020;24:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas-Rüddel DO, Schlattmann P, Pletz M, Kurzai O, Bloos F. Risk factors for invasive candida infection in critically Ill patients: a systematic review and meta-analysis. Chest. 2022;161:345–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kazancioglu S, Bodur H, Mumcuoglu I, Bastug A, Ozbay BO, Aydos O, et al. Candidemia in critically ill COVID-19 patients: risk factors and impact on mortality. Heliyon. 2024;10: e28033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dixit D, Jen P, Maxwell TD, Smoke S, McCracken JA, Cardinale-King M, et al. Risk factors and clinical outcomes of Candidemia Associated with severe COVID-19. Crit Care Explor. 2022;4: e0762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beştepe Dursun Z, Sipahioğlu H, Civan Yüksel R, Sav H, Çelik İ. Risk factors and lethality associated with Candidemia in severe COVID-19 patients. Curr Med Mycol. 2022;8:32–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Papadimitriou-Olivgeris M, Kolonitsiou F, Kefala S, Spiliopoulou A, Aretha D, Bartzavali C, et al. Increased incidence of candidemia in critically ill patients during the coronavirus disease 2019 (COVID-19) pandemic. Braz J Infect Dis. 2022;26: 102353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dautzenberg MJD, Wekesa AN, Gniadkowski M, Antoniadou A, Giamarellou H, Petrikkos GL, et al. The association between colonization with carbapenemase-producing enterobacteriaceae and overall ICU mortality: an observational cohort study. Crit Care Med. 2015;43:1170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolkewitz M, Vonberg RP, Grundmann H, Beyersmann J, Gastmeier P, Bärwolff S, et al. Risk factors for the development of nosocomial pneumonia and mortality on intensive care units: application of competing risks models. Crit Care. 2008;12:R44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Venet F, Monneret G. Advances in the understanding and treatment of sepsis-induced immunosuppression. Nat Rev Nephrol. 2018;14:121–37. [DOI] [PubMed] [Google Scholar]
- 51.Davis CG, Chang K, Osborne D, Walton AH, Dunne WM, Muenzer JT. Increased susceptibility to candida infection following cecal ligation and puncture. Biochem Biophys Res Commun. 2011;414:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets from this study are available from the corresponding author on request.