Abstract
Abstract
Objective
This paper aims to evaluate the literature on the prevalence of psychological distress and its associated factors in patients with breast cancer.
Design
Systematic review and meta-analysis.
Data sources
PubMed, Web of Science, Embase, the Cochrane Library, China National Knowledge Infrastructure and Wanfang were searched from inception to 11 June 2024.
Eligibility criteria
Studies reported data on the prevalence and correlates of psychological distress were included. Review, letter, conference abstracts and articles not available in English and Chinese were excluded.
Data extraction and synthesis
Two researchers independently conducted literature screening, data extraction and bias risk assessment. Meta-analysis was employed to estimate the prevalence and correlates of psychological distress in patients with breast cancer. The Agency for Healthcare Research and Quality and the Newcastle-Ottawa Scale were used for quality assessment. Meta-analysis was performed by using the R V.4.1.1 software.
Results
In total, 34 studies representing 13 828 patients with breast cancer were included in the study. Most of the studies were cross-sectional study (n=25, 73.53%%). The pooled prevalence of psychological distress was 50% (95% CI 42% to 58%, I2=98%). Results showed that psychological distress was positively correlated with younger age (z=0.13, 95% CI 0.07 to 0.20), having children (z=0.39, 95% CI 0.11 to 0.61), poor financial situation (z=0.12, 95% CI −0.03 to 0.26), short time since diagnosis (z=0.19, 95% CI 0.01 to 0.36), previous treatment (z=0.15, 95% CI 0.03 to 0.27), distant metastasis (z=0.31, 95% CI 0.07 to 0.52), chemotherapy (z=0.22, 95% CI 0.05 to 0.38), prior emotional status (z=0.40, 95% CI 0.29 to 0.50), body image damaged (z=0.10, 95% CI −0.01 to 0.21), negative coping (z=0.12, 95% CI −0.11 to 0.34), communication avoidance (z=0.32, 95% CI 0.24 to 0.39) and negatively correlated with married (z=−0.25, 95% CI 0.45 to −0.02), high education level (z=−0.19, 95% CI −0.40 to 0.05), having insured (z=−0.04, 95% CI −0.15 to 0.08), full employment (z=−0.40, 95% CI −0.61 to −0.14), time of completion of treatment (z=−0.12, 95% CI −0.30 to −0.06), surgery (z=−0.05, 95% CI −0.53 to 0.45), social support (z=−0.18, 95% CI −0.29 to −0.06), post-traumatic growth (z=−0.19, 95% CI −0.34 to −0.03), good physical conditions (z=−0.17, 95% CI −0.29 to −0.04), positive coping (z=−0.22, 95% CI −0.53 to 0.15).
Conclusion
Our findings indicated that the prevalence of psychological distress in patients with breast cancers was 50% and 21 correlates of psychological distress. Screening and evidence-based interventions are urgent and essential to address this public concern and promote the health of patients with breast cancer.
PROSPERO registration number
CRD42023397109.
Keywords: breast tumours, mental health, nursing care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We conducted a comprehensive search strategy to screen all eligible studies.
Our findings reveal disparities in psychological distress across different geographic areas, underscoring the need for targeted interventions.
We used subgroup analysis and sensitivity analysis to assess potential heterogeneity.
Heterogeneity was observed in some associated factors.
Restriction of publication language to English and Chinese is a limitation of this meta-analysis.
Introduction
Breast cancer is the most common malignancy among women worldwide.1 2 Owing to the recent advances in screening and treatment, the survival rate and survival period of patients with breast cancer have been significantly improved. The 5-year survival rate of breast cancer in the USA, Australia and some European countries has reached 85%–90%.3 Breast cancer survivors have become a significant and unique group. Surgery, chemotherapy, radiation therapy and hormone therapy are considered to be the main treatments for breast cancer.4 For most patients with breast cancer, such modalities can lead to adverse outcomes such as changes in body image (such as breast loss, scarring, hair loss and skin changes), drug toxicity, sexual dysfunction and other adverse outcomes.5 6 It also leads to a long-term state of chronic psychological stress, prone to a variety of adverse emotions and psychological distress has become a prominent emotional characteristic of survivors after breast cancer surgery.7
The National Comprehensive Cancer Network defines psychological distress as an unpleasant emotional state caused by various factors affecting the patient’s effective response to cancer and physical symptoms.8 It can cover all psychological, spiritual and social problems of patients with cancer and negatively impact their quality of life (QoL), treatment effect, recovery and survival time.9
Given the importance of the relationship between psychological distress and health outcomes in patients with breast cancer, evaluating it has received considerable attention. However, the prevalence of psychological distress reported among patients with breast cancer has varied widely. For example, psychological distress rates of 49.0% in China were reported in 20229 and 47% were reported in Germany.10 In contrast, the prevalence was low in Jordan (36.3%)11 and Spain (24.5%).12 In addition, many studies have explored the correlates associated with the psychological distress of patients with breast cancer, but the results are inconsistent among studies. For instance, older age has been considered as one positive predictor for psychological distress in patients with breast cancer.13 However, Alfonsson et al found that being younger was correlated with psychological distress.14 However, several potential factors contributing to the variance in estimates have been hypothesised, including variations in economic growth, evaluation tools and sample size. Nevertheless, a systematic review of these issues has not been performed.
Therefore, we performed a systematic review and meta-analysis to explore the prevalence and correlates of psychological distress among patients with breast cancer and provide recommendations for further research and policy-making.
Methods
This systematic review was registered on the Prospective International Register for Systematic Reviews (PROSPERO, 11 June 2024, registration number CRD42023397109).
Search strategy
Two researchers independently searched for published studies, including PubMed, Cochrane Library, Web of Science, Embase, China National Knowledge Infrastructure and Wanfang from inception to 11 June 2024. The search terms were “breast neoplasms OR breast cancer OR breast tumour” AND " psychological distress OR distress OR psychological status OR emotional distress OR emotional status.” The search strategy was adjusted to fit the specifications of different databases. We also manually checked the list of references included in the study for additional relevant articles. The search strategy is shown in online supplemental table 1.
Study selection
The inclusion criteria of the study were as follows: (1) patients (age ≧18 years) with breast cancer; (2) studies reporting the prevalence or correlates of psychological distress in patients with breast cancer; (3) measured the prevalence or correlates of psychological distress using standardised, validated instruments and questionnaires (If more than two assessment tools were selected in one study, the results should be reported using one tool) and (4) studies with cross-sectional and cohort designs. Studies were excluded if (1) the sample size was less than 100; (2) inaccessible or incomplete full texts; (3) review, letter and conference abstracts; (4) provided insufficient information to calculate aggregate prevalence and correlates and (5) non-Chinese and non-English literature.
Data extraction
We used EndNote V.X9 software to manage the retrieved literature. Two authors independently extracted the data from the included studies, screened the literature and cross-checked it, and the third author assisted in judgement in case of disagreement. First, the literature that was inconsistent with the inclusion criteria was excluded after reviewing the title and abstract. Then, the full text was reviewed and screened to determine the literature that meets the criteria. The content of data extraction included the first author of the literature, publication time, region, study type, sample size, assessment tools, sample size, the prevalence of psychological distress, correlates of psychological distress and quality score. Any disagreements were resolved by discussion with the third author (KJ).
Quality assessment
The quality evaluation of cross-sectional studies adopted the evaluation criteria recommended by the Agency for Healthcare Research and Quality (AHRQ),15 which included 11 items, and each item has three choices: ‘yes’, ‘no’ and ‘unclear’. It includes selecting research objects, controlling and treating confounding factors, and statistical analysis. Prospective cohort studies were evaluated by the Newcastle-Ottawa Scale (NOS), each containing three blocks with eight items, specifically for population selection, comparability, exposure or outcome evaluation.16 The star rating method is used to evaluate the literature quality in this scale. One star in line with the evaluation criteria represents 1 point, and the total score is nine stars (9 points). Study quality was assessed according to the total score. The higher score indicating the better the quality of the article. Two authors carried out literature quality evaluation independently, and differences were resolved through discussion.
Statistical analysis
The meta-analyses were conducted by using R programming (V.4.1.1), with p<0.05 as statistically significant. Data on the proportion of patients with breast cancer with psychological distress and the total sample size were extracted from individual studies to generate pooled estimates using accurate binomial tests and associated 95% CIs. The Pearson correlation coefficient (r) was used as an indicator of the effect size of correlates of psychological distress. Pooled associations were calculated such that values above 0 reflected positive associations between the correlation variables and psychological distress. In contrast, a value less than 0 reflects the negative association between correlation variables and psychological distress. According to Cohen’s recommendations, correlations are considered small when r=0.10–0.29, moderate when r=0.30–0.49 and vital when r=0.50 and above.17
The heterogeneity of the data was tested using the I2 statistic. If p<0.1, I2≥50%, the random effects model was used.18 Otherwise, a fixed effect model was used. Descriptive analysis was used for studies that could not combine effect sizes. The stability and reliability of the results were investigated using sensitivity. When the number of articles was over 10, the funnel plot was used to assess whether publication bias existed. When the number of literature is less than ten, publication bias was identified by using the Egger test (p<0.5 is considered as significant).19
Patient and public involvement
There is no public and patient involvement.
Results
Study selection
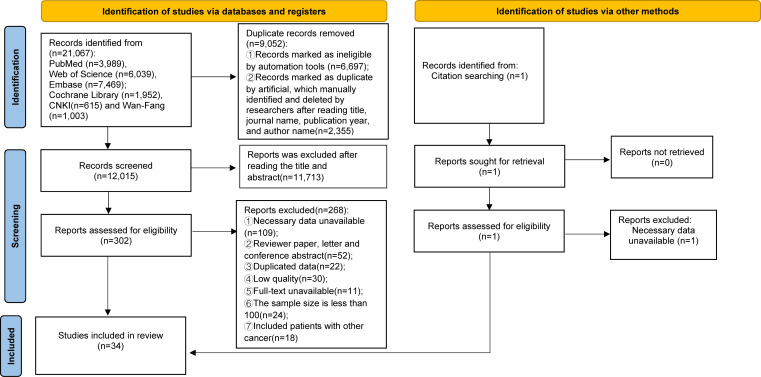
We identified 21 067 potentially eligible articles through a database search and 1 study from citation searching, with 12 015 remaining after removing 9052 duplicates. Following the evaluation of article titles and abstracts, 302 articles met the criteria for full-text review. According to the inclusion criteria, 268 publications that did not meet the criteria were excluded, resulting in the final inclusion of 34 studies. 25 were cross-sectional studies, and 9 were cohort studies (figure 1).
Figure 1. The flow diagram of studies selection.
Basic characteristic of the included studies
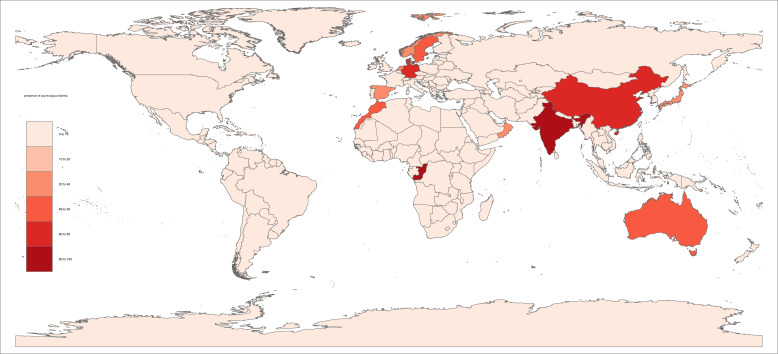
The basic characteristics of the included studies are presented in table 1. The 34 included studies involved a total of 13 828 participants.12,1420 Among the included 34 studies, 14 were conducted in Asian countries, 10 in Europe, 4 in Africa, 3 in North America and 3 in Oceania. Most were cross-sectional studies (n=25, 73.53%), and there were nine cohort studies (26.47%). The most commonly used scale for assessing psychological distress was the Distress Thermometer (n=13, 38.24%), followed by the Hospital Anxiety and Depression Scale (n=10, 29.42%), Depression, Anxiety and Stress Scale (n=4, 11.76%), The problem list (n=3, 8.82%), Generalised Anxiety Disorder Scale-7 (n=2, 5.88%), the Brief Symptom Inventory 18 (BSI-18) (n=1, 2.94%), Kessler Psychological Distress Scale (n=1, 2.94%), The 10-item Centre for Epidemiologic Studies Depression Scale (n=1, 2.94%), the 9-item Patient Health Questionnaire (n=1, 2.94%), Connor-Davidson Resilience Scale-10 (n=1, 2.94%) and Self-Rating Depression Scale (n=1, 2.94%).
Table 1. Characteristics of the included literature.
| First author, year | Region | Study design | Sample size | Tool | Prevalence (%) | Correlates | Quality assessment score |
| Alfonsson, 201614 | Sweden | Cross-sectional | 833 | HADS | 42 | 1, 2, 5, 10, 12, 15, 22 | 6 |
| Andreu, 201112 | Spain | Cohort study | 102 | BSI-18 | 24.5 | 12, 15, 23 | 7 |
| Berhili, 201721 | Morocco | Cross-sectional | 446 | DT | 46.6 | 1, 5, 11, 13, 15 | 7 |
| Berhili, 201922 | Morocco | Cross-sectional | 122 | HADS | 33.6 | 2, 5 | 9 |
| Bidstrup, 201523 | Denmark | Cross-sectional | 426 | DT | 76 | 1, 2, 3, 12, 24 | 8 |
| Bjerkeset, 202024 | Norway | Cross-sectional | 834 | HADS | 30 | 1, 2, 7, 11 | 10 |
| Faller, 201725 | Germany | Cross-sectional | 897 | GAD-7 | – | 15 | 7 |
| Holger, 202226 | Germany | Cohort study | 1400 | DT | 67.3 | 1, 8 | 6 |
| Jørgensen, 201627 | Denmark | Cohort study | 1024 | DT | 68.9 | 1, 4, 8, 10, 14, 25 | 7 |
| Liu, 201328 | China | Cohort study | 120 | DT | 46.7 | 16 | 8 |
| Lim, 202329 | Singapore | Cohort study | 1386 | DT, PL | 36.8 | 1, 8, 14, 17 | 9 |
| Liu, 202130 | USA | Cohort study | 171 | DT, PL | 21.3 | 13, 26 | 7 |
| Nsondé Malanda, 202131 | Congo | Cross-sectional | 150 | DT | 82 | 7, 11, 27, 28 | 7 |
| Thakur, 202232 | India | Cross-sectional | 165 | DASS | 84.1 | 1, 9, 18 | 10 |
| Lo-Fo-Wong, 201633 | Netherlands | Cohort study | 746 | DT, PL | 22 | 29, 30, 31, 32 | 7 |
| Park, 201713 | Korea | Cohort study | 117 | DT | 18.8 | 1, 14, 33, 34 | 8 |
| Schubart, 201435 | USA | Cross-sectional | 149 | DT | 68 | 1 | 9 |
| Wevers, 202036 | Netherlands | Cross-sectional | 238 | HADS | 61.4 | 4, 14 | 8 |
| Shen, 201837 | China | Cohort study | 216 | DT | 78.2 | 1, 3, 5, 8, 15, 19, 20, 35 | 8 |
| Soo, 201538 | Australia | Cross-sectional | 185 | DASS | 52.4 | 1, 2, 3, 8, 9, 11, 14, 15, 16, 17, 36 | 6 |
| Taira, 201439 | Japan | Cross-sectional | 497 | HADS | 42 | 37 | 9 |
| Akechi, 201040 | Japan | Cross-sectional | 408 | HADS | 35 | 38 | 9 |
| Yang, 201641 | China | Cross-sectional | 100 | DT | 71 | 1, 3, 6 | 6 |
| Ying, 202042 | China | Cross-sectional | 273 | K10 | – | 19, 20, 21 | 8 |
| Warmoth, 202043 | USA | Cross-sectional | 136 | CES-D | – | 39 | 6 |
| Yu, 201544 | Australia | Cross-sectional | 338 | DASS | 41.8 | 17, 21 | 7 |
| Younis, 202045 | Jordan | Cross-sectional | 200 | HADS | – | 1, 6 | 6 |
| Su, 202247 | China | Cross-sectional | 200 | PHQ-9, GAD-7 | 39.5 | 40 | 10 |
| Alcorso, 201520 | Australia | Cross-sectional | 166 | DASS | – | 1, 17, 18 | 7 |
| Phoosuwan, 202134 | Sweden | Cross-sectional | 481 | HADS | – | 1, 15, 17 | 6 |
| Yu, 201846 | China | Cross-sectional | 400 | IES-R | – | 16 | 7 |
| Al-Fahdi, 202348 | Oman | Cross-sectional | 171 | HADS | 21.6 | 1, 3 | 9 |
| Gu, 202349 | China | Cross-sectional | 522 | SDS | 71.6 | 15, 41 | 8 |
| Omari, 202350 | Morocco | Cross-sectional | 209 | HADS | 65.1 | 1, 42, 43 | 8 |
Correlates: 1. Age (younger); 2. Marital status (married); 3. Education (short or unknown); 4. Having children; 5. Poor financial situation; 6. Having insured; 7. Full employment; 8. Time since diagnosis; 9. Time of completion of treatment; 10. Previous treatment for psychological states;11. Distant metastasis; 12. Chemotherapy; 13. Surgery; 14. Prior emotional status; 15. Social support; 16. Post-traumatic growth; 17. Physical conditions; 18. Body image damage; 19. Positive coping; 20. Negative coping; 21. Communication avoidance; 22. High levels of fatigue; 23. Helplessness; 24. Radiotherapy; 25. Feelings regarding femininity and attractiveness; 26. Status of cancer at time of screening; 27. BMI; 28. Sleep; 29. Lack of muscle strength; 30. Experience of a low level of life satisfaction; 31. More frequent cancer worry; 32. Neuroticism; 33. Nervousness; 34. Pain; 35. Family history of breast cancer; 36. In treatment; 37. Breast trial outcome index; 38. Patient’s perceived need; 39. Self-stigma; 40. Symptom burden; 41. Self-efficiency; 42. Lymph node status; 43. Chronic illness.
BMIbody mass indexBSI-18Brief Symptom Inventory 18CES-D10-item Center for Epidemiologic Studies Depression ScaleDASSDepression, Anxiety and Stress ScaleDTThe Distress ThermometerGAD-7Generalised Anxiety Disorder ScaleHADSThe Hospital Anxiety and Depression ScaleIES-RImpact of Event Scale-RevisedK10Kessler Psychological Distress ScalePHQ-9The 9-item Patient Health QuestionnairePLproblem listSDSSelf-Rating Depression Scale
The prevalence of psychological distress in patients with breast cancer ranged from 18.8% to 84.1%. The quality of included cross-sectional articles was evaluated by the AHRQ, and the scores ranged between 6 and 10; the quality of included cohort studies was evaluated using the NOS, with scores ranging from 6 to 9 (online supplemental tables 2–3).
Pooled prevalence of psychological distress
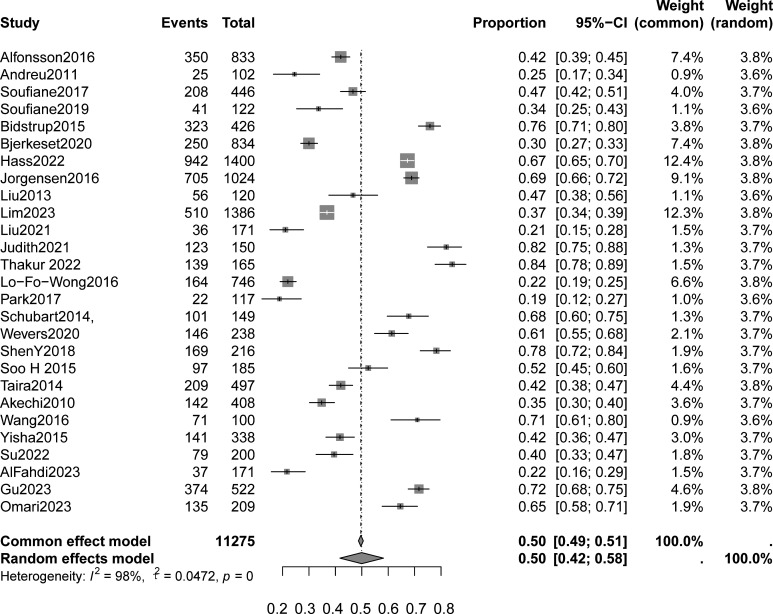
Using the random effect model, the pooled prevalence of psychological distress in patients with breast cancer was 50% (95% CI 42% to 58%) (figure 2). There was substantial heterogeneity in studies (p<0.01), with an I2 values of 98%. The prevalence of psychological distress varied among studies using different assessment tools, ranging from 27% to 63% and those from different samples ranged from 49% to 51% (table 2, online supplemental figure 1). In addition, the prevalence of psychological distress after the COVID-19 period (53%) was higher than before (48%) (table 2, online supplemental figure 2). With regard to the ranges of prevalence data of the entire study sample by geographical area, the pooled prevalence of psychological distress in developed countries is 47% and 53% in developing countries (table 2, online supplemental figure 3). The geographical distribution of studies can be seen in figure 3.
Figure 2. The forest plot of the pooled prevalence of psychological distress in patients with breast cancer.
Table 2. Subgroup analyses of prevalence of psychological distress in patients with breast cancer.
| Subgroup | No of included studies | Prevalence (%) | 95%CI | I2 (%) | P value |
| Tool | |||||
| DT | 10 | 63 | 0.50 to 0.74 | 97 | <0.01 |
| HADS | 8 | 41 | 0.31 to 0.52 | 96 | <0.01 |
| DT+PL | 3 | 27 | 0.17 to 0.37 | 97 | <0.01 |
| DASS | 3 | 60 | 0.34 to 0.84 | 98 | <0.01 |
| Country | |||||
| Developed country | 15 | 47 | 0.37 to 0.58 | 98 | <0.01 |
| Developing country | 11 | 53 | 0.40 to 0.66 | 99 | <0.01 |
| Sample | |||||
| ≥400 | 11 | 49 | 0.38 to 0.60 | 99 | <0.01 |
| <400 | 16 | 51 | 0.39 to 0.62 | 97 | <0.01 |
| Period | |||||
| Before COVID-19 | 16 | 48 | 0.38 to 0.58 | 98 | <0.01 |
| After COVID-19 | 11 | 53 | 0.38 to 0.67 | 99 | <0.01 |
DTDistress ThermometerHADSHospital Anxiety and Depression ScalePLproblem list
Figure 3. World geographical distribution of prevalence of psychological distress in the included studies.
Correlates of psychological distress
Factors that correlate with psychological distress among patients with breast cancer are presented in table 3. For sociodemographic characteristics, only having children and full employment was moderately associated with psychological distress. All clinical correlates of psychological distress were significant, and effect sizes ranged from small to medium effect sizes. The most significant effect size was observed for distant metastasis. Among psychological characteristics, only prior emotional status was a significant correlate, except for communication avoidance. Psychological characteristics had a small-to-medium effect size.
Table 3. Correlates of psychological distress among patients with breast cancer.
| Correlates | Ka | No. of individuals | Z (95% CI) | P value | I2 |
| Sociodemographic correlates | |||||
| Age (younger) | 18 | 8508 | 0.13 (0.07 to 0.20) | <0.01 | 88 |
| Marital status (married) | 5 | 2724 | −0.25 (0.45 to −0.02) | <0.01 | 97 |
| Higher education | 5 | 1098 | −0.19 (−0.40 to 0.05) | <0.01 | 93 |
| Having children | 2 | 1262 | 0.39 (0.11 to 0.61) | <0.01 | 94 |
| Poor financial situation | 2 | 662 | 0.12 (−0.03 to 0.26) | 0.07 | 69 |
| Having insured | 2 | 300 | −0.04 (−0.15 to 0.08) | 0.75 | 0 |
| Full employment | 2 | 984 | −0.40 (−0.61 to −0.14) | <0.01 | 90 |
| Clinical correlates | |||||
| The short time since diagnosis | 5 | 4211 | 0.19 (0.01 to 0.36) | <0.01 | 97 |
| The time of completion treatment | 2 | 350 | −0.12 (−0.30 to 0.06) | 0.07 | 69 |
| The previous treatment for psychology | 2 | 1857 | 0.15 (0.03 to 0.27) | <0.01 | 86 |
| Distant metastasis | 4 | 1615 | 0.31 (0.07 to 0.52) | <0.01 | 95 |
| Chemotherapy | 3 | 1361 | 0.22 (0.05 to 0.38) | <0.01 | 90 |
| Surgery | 2 | 617 | −0.05 (−0.53 to 0.45) | <0.01 | 97 |
| Physical and psychological correlates | |||||
| Poor prior emotional status | 5 | 2950 | 0.40 (0.29 to 0.50) | <0.01 | 94 |
| Social support | 8 | 3682 | −0.18 (−0.29 to −0.06) | <0.01 | 92 |
| Post-traumatic growth | 3 | 705 | −0.19 (−0.34 to −0.03) | 0.02 | 73 |
| Physical conditions | 5 | 2556 | −0.17 (−0.29 to −0.04) | <0.01 | 88 |
| Body image damaged | 2 | 331 | 0.10 (−0.01 to 0.21) | 0.76 | 0 |
| Positive coping | 2 | 489 | −0.22 (−0.53 to 0.15) | <0.01 | 94 |
| Negative coping | 2 | 489 | 0.12 (−0.11 to 0.34) | <0.01 | 85 |
| Communication avoidance | 2 | 611 | 0.32 (0.24 to 0.39) | 0.81 | 0 |
Ka:The number of articles reported
Sociodemographic correlates
The most reported correlate was age (younger), and it was proved to be positively correlated with psychological distress among breast cancer (z=0.13, 95% CI 0.07 to 0.20) (online supplemental figure 4).13 14 20 21 23 24 26 27 29 32 34 35 37 38 41 45 48 50 The meta-analysis was run after removing each study individually; however, this did not suggest that any one study had a significant effect on the z value (online supplemental figure 5). Meanwhile, funnel plots showed no quality bias in the included literature (online supplemental figure 6). Marital status (married) was negatively correlated with psychological distress (z=−0.25, 95% CI −0.45 to −0.02; online supplemental figure 7)1422,24 38 and the result of sensitivity analysis showed that the z value of excluded studies had no significant change (online supplemental figure 8). Highly educated was also found to be negatively correlated with psychological distress (z=−0.19, 95% CI −0.40 to 0.05; online supplemental figure 9).23 37 38 41 48 The result of sensitivity analysis showed that the z value of excluded studies had no significant change (online supplemental figure 11).
Moreover, having children (z=0.39, 95% CI 0.11 to 0.61; online supplemental figure 11)27 36 and poor financial situation (z=0.12, 95% CI −0.03–0.26; online supplemental figure 12)21 37 were positively associated with psychological distress. Having insured was positively correlated with psychological distress (z=−0.04, 95% CI −0.15 to 0.08; online supplemental figure 13).41 45 Additionally, two studies24 31 assessed the association between full employment and psychological distress, and the results showed a negative correlation between the two variables (z=−0.40, 95% CI −0.61 to −0.14; online supplemental figure 14).
Clinical correlates
The pooled analysis identified six potential clinical factors associated with psychological distress in breast cancer: the time since diagnosis, the time of completion of treatment, the previous treatment for psychology, distant metastasis, chemotherapy and surgery. The short time since diagnosis (z=0.19, 95% CI 0.01 to 0.36),26 27 29 37 38 the previous treatment for psychology (z=0.15, 95% CI 0.03 to 0.27),14 27 distant metastasis (z=0.31, 95% CI 0.07 to 0.52),21 24 31 38 and chemotherapy (z=0.22, 95% CI 0.05 to 0.38)12 14 23 were positive related with psychological distress. Patients with longer time of completion treatment (z=−0.12, 95% CI −0.30 to 0.06)32 38 or surgery (z=−0.05, 95% CI −0.53 to 0.45)21 30 were less likely to have psychological distress. Clinical factors associated with psychological distress are presented in online supplemental figures 15–23.
Physical and psychological correlates
Five studies were included in the meta-analysis examining the correlation between psychological distress and prior emotional status.13 27 29 36 38 Results of the meta-analysis suggest that poor prior emotional status had a statistically significant moderate, positive correlation with psychological distress (z=0.40, 95% CI 0.29 to 0.50; online supplemental figure 24). The sensitivity analysis results indicated no significant change in z value after removing literature one by one (online supplemental figure 25). The result of Egger’s test (t=0.38, df=3, p=0.727) indicates that a publication bias is unlikely. In addition, seven studies examined the correlation between psychological distress and social support.12 14 21 25 34 37 38 49 Results showed that social support had a small, negative correlation with psychological distress (z=−0.18, 95% CI −0.29 to −0.06; online supplemental figure 26). The meta-analysis was run after removing each study individually, and it suggests that any one study had a significant effect on the z value (online supplemental figure 27). The Egger test results (t=−0.15, df=5, p=0.888) showed that publication bias did not exist.
Post-traumatic growth (z=−0.19, 95% CI −0.34 to −0.03; online supplemental figures 28 and 29)28 38 46 and physical conditions (z=−0.17, 95% CI −0.29 to −0.04; online supplemental figures 30 and 31)20 29 34 38 44 were proved to be negative correlation with psychological distress. Body image damage was significant, with a small positive association with psychological distress (z=0.10, 95% CI −0.01 to 0.21; online supplemental figure 32).20 32 Positive coping (z=−0.22, 95% CI −0.53 to 0.15; online supplemental figure 33) and negative coping (z=0.12, 95% CI −0.11 to 0.34; online supplemental figure 34) were found to be negatively and positively correlated with psychological distress.37 42 Communication avoidance was associated with psychological distress with a moderate positive effect size (z=0.32, 95% CI 0.24 to 0.39; online supplemental figure 35).42 44
Descriptive analysis
Since the following correlates were identified in only one study, we used descriptive analysis to present the association between correlates and psychological distress. Breast cancer-related psychological distress was positively correlated with fatigue (r=0.454),14 hopelessness(r=0.719),12 radiotherapy (r=0.333),23 feelings regarding femininity and attractiveness (r=0.486),27 status of cancer at time of screening (r=0.182),30 body mass index (r=0.291),31 poor sleep quality (r=0.302),31 lack of muscle strength(r=0.163),33 more frequent cancer worry (r=0.092),33 neuroticism (r=0.024),33 nervousness (r=0.547),13 pain (r=0.466),13 family history of breast cancer (r=0.014),37 in treatment (r=0.16),38 patient’s perceived need (r=0.63),40 self-stigma (r=0.50)43 and symptom burden(r=0.53).47 While negative correlations were the experience of a low level of life satisfaction (r=−0.072),33 breast trial outcome index (r=−0.129),39 self-efficiency(r=−0.388),49 lymph node status(r=0.234)50 and chronic illness (r=0.271).50
Discussion
The available evidence estimates that the pooled prevalence of breast cancer-related psychological distress was 50%. As we all know, a cancer diagnosis may induce psychological distress. However, it is under‐recognised within clinical oncology practice, which can result in undesirable or severe consequences.51 Therefore, it is essential to address the psychological distress associated with breast cancer. In addition, our study verified that eleven factors were positively related to psychological distress, including age, having children, poor financial situation, the time since diagnosis, the previous treatment for psychology, distant metastasis, chemotherapy, poor prior emotional status, body image damaged, negative coping and communication avoidance; 10 factors were negatively associated with psychological distress, including marital status, higher education, having insured, full employment, the time of completion treatment, surgery, social support, post-traumatic growth, physical conditions and positive coping. Those correlates mentioned above should be fully considered by clinical staff when developing strategies to prevent and intervene in psychological distress in patients with breast cancer.
Previous studies have assessed psychological distress in patients with breast cancer.52 53 Nevertheless, Chen et al only examined the factors connected to psychological distress in patients with breast cancer during the COVID-19 pandemic.54 Lyu et al only explored the relationship between psychological distress and QoL in Chinese early patients with breast cancer under chemotherapy.9 Lam et al described trajectories of psychological distress and their determinants only among patients with advanced breast cancer.55 Our study systematically reviewed published articles on the prevalence of psychological distress among patients with breast cancer. Meanwhile, we also conducted a subgroup analysis of the prevalence of psychological distress and explored correlates in patients with breast cancer, which were not evaluated in other studies. Thus, our study has made significant progress over previous studies and could provide more information.
In a subgroup analysis, our study found that the prevalence of psychological distress varied by the socioeconomic level of the country, with a higher incidence of psychological distress in developing countries, possibly due to the fact that patients with breast cancer in developing countries face not only the stress of the disease but also economic stress.56 In addition, poor quality and under-resourced medical resources have resulted in less access to early supportive services.57 The COVID-19 pandemic may affect the mental health of patients with breast cancer. Our findings suggest that the prevalence of psychological distress is still higher in the aftermath of the COVID-19 outbreak, possibly because there is a long period of isolation, limited access to medical resources and a lack of social support.54 58 Furthermore, it should be noted that extensive sample studies are rated, and larger sample and multicentre studies should be conducted to evaluate psychological distress and correlates in patients with breast cancer.
This meta-analysis showed that all included literature assessed psychological distress symptoms in patients with breast cancer using a self-report tool rather than a structured clinical interview. Therefore, the results only suggested that patients with breast cancer had psychological distress symptoms, not psychiatric or other disorders. However, a self-reported tool is convenient to operate, sensitive to psychological distress symptoms and has high clinical application value. Our results suggest that there are significant differences in the assessment of psychological distress symptoms in patients with breast cancer by different scales, and which scale is more suitable for the assessment of psychological distress in patients with breast cancer needs to be further investigated.
For sociodemographic correlates, seven factors were confirmed to be associated with psychological distress. Younger patients with breast cancer experienced higher levels of psychological distress, which may be due to younger patients’ concerns about the impact of cancer on their job development, loss of financial ability and marital life, which is consistent with the study of Adjei Boakye et al.59 In contrast to the current research results, Park et al found that older age was a predictor of consistently high psychological distress,13 mainly because older crises are linked to postmenopausal symptoms like hot flashes and night sweats.60 However, more research is warranted to confirm the age difference. Marital status was negatively associated with psychological distress, as married patients may receive emotional, financial and life support from their partners.61 Our study further confirmed that higher education was related to lower levels of psychological distress. They engage socially and live healthier, longer lives because they have higher cognitive and vital decision-making skills.62 A previous study from Sweden indicated that higher education is positively linked to less psychological distress, which might be related to a better job and financial security.63 In addition, our study identified that having children was a risk factor for psychological distress related to their concern for their children’s future upbringing and education.64 Furthermore, financial situation and employment were also associated with psychological distress. Patients with poor economic conditions are worried about missing the best opportunity for diagnosis and treatment and are prone to negative psychological emotions. In contrast, patients with good financial status or full-time employment could get more access to better medical and social resources and thus have lower psychological distress.65 Additionally, having insured is a protective correlate of psychological distress, consistently indicating a higher prevalence of psychological distress among patients with medical insurance.66
Among clinical correlates, the short time since diagnosis, the previous treatment for psychology or psychology illness, distant metastasis and chemotherapy are positive for psychological distress. Patients with a short time since diagnosis are prone to have psychological distress, which may be related to the fact that patients will worry about their lives due to the uncertainty of the future after cancer diagnosis.13 37 The previous treatment for psychology is a significant factor that needs to be addressed related to higher psychological distress. Patients with a history of psychological treatment suffer from poorer mental health, diminished psychological tolerance and decreased psychological adaptability compared with patients without a history of psychiatric disease.67 The present review found that patients with distant metastases had higher levels of psychological distress, consistent with previous studies62 68; this remains a substantial risk to consider. Chemotherapy is a potential risk factor for psychological distress in breast cancers and should be considered; such findings have also been reported by other researchers, although with a smaller sample size (<100 patients) than the studies evaluated in the present review.69 Furthermore, the completion time of treatment and surgery were all significant indicators of psychological distress. The time of treatment completion was negatively associated with psychological distress, suggesting that psychological distress appears to lessen with time, a finding consistent with other studies.70 Interestingly, in our meta-analysis, having surgery was associated with lower psychological distress scores, which may be due to the fact that patients who undergo surgery can gain emotional relief from physically removing the tumour and receiving potentially curative treatment.30 However, such a finding was inconsistent with a previous study.71 Therefore, additional high-quality, large-sample studies are needed to assess the association between surgery and psychological distress.
Some studies suggest that individuals with a history of poor prior emotional status could be more likely to develop psychological distress,62 72 consistent with our findings. The traumatic nature of breast cancer can trigger initial symptoms or exacerbate pre-existing symptoms, thereby exacerbating psychological stress in these vulnerable individuals. Future work is necessary to examine other potential correlates. In contrast, post-traumatic growth refers to positive changes in individual psychology, a better predictor of psychological status among patients with chronic illnesses.73 In addition, social support and good physical conditions appear to be protective factors against psychological distress, suggesting that social support and good physical conditions can both act as buffer mediators for psychological distress.74 75 The results also showed that body image damage increased the likelihood of psychological distress, which may be due to the negative perception of their body image from others.76 Several included studies also focused on the relationship between coping strategies and psychological distress, with positive coping strategies that could alleviate stress and facilitate positive psychological outcomes, while negative coping strategies are the opposite.77 Moreover, communication avoidance may induce psychological distress as patients show alienation from positive emotional information, which is one of the negative coping strategies. Therefore, medical staff should guide patients to adopt positive coping strategies to alleviate their inner experience of psychological distress and improve their mental health.
However, this study has several limitations. First, different psychological distress assessment tools were integrated into this meta-analysis, and different studies had different definitions and assessment tools for psychological distress, resulting in high heterogeneity. Second, the limited number of included studies may introduce bias. Although we conducted a comprehensive search of studies on psychological distress, we may still need to include some relevant published and unpublished studies. Finally, the literature search was limited to studies published in English and Chinese, with the possibility of additional research published in the language of the country under investigation. Nevertheless, to our knowledge, this is the first quantitative analysis of psychological distress in patients with breast cancer, integrating studies from around the globe. This meta-analysis may provide evidence for the prevention and management of psychological distress in patients with breast cancer.
Conclusion
In summary, this systematic review and meta-analysis indicate that patients with breast cancer experience varying levels of psychological distress. Several sociodemographic, clinical, physical and psychological factors are linked to the prevalence of psychological distress among patients with breast cancer. We believe that the psychological state of patients with breast cancer is a vital public health priority, and psychological distress in breast cancer should receive adequate attention from healthcare professionals. Therefore, there is an essential need for patients with breast cancer to proactively screen for their psychological status during the illness journey. Appropriate management is also needed to improve their QoL and reduce the exposure of patients with breast cancer to psychological distress as a mental health problem.
supplementary material
Acknowledgements
We are special grateful to all researchers who participated in this study during the study period.
Footnotes
Funding: This study was supported by Guangxi medical and health appropriate technology development and application project (No. S2023064), Self-raised project of Guangxi Health Commission (Z-A20220499) and Self-established Cultivation Project of the First Affiliated Hospital of Guangxi Medical University—Nursing Clinical Research Climbing Plan (No. YYZS2022011).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-077067).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Wen-Zhen Tang, Email: tangwenzhen0416@163.com.
Ernest Mangantig, Email: e.mangantig@usm.my.
Yulita Hanum P Iskandar, Email: yulita@usm.my.
Shi-li Cheng, Email: chengshili@student.usm.my.
Azlina Yusuf, Email: azlinayusuf@usm.my.
Kui Jia, Email: jiakui2024@163.com.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin . 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin . 2019;69:438–51. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 3.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–75. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gradishar WJ, Anderson BO, Abraham J, et al. Breast Cancer, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:452–78. doi: 10.6004/jnccn.2020.0016. [DOI] [PubMed] [Google Scholar]
- 5.Villarreal-Garza C, López-Martínez EA, Martínez-Cannon BA, et al. Medical and information needs among young women with breast cancer in Mexico. Eur J Cancer Care (Engl) 2019;28:e13040. doi: 10.1111/ecc.13040. [DOI] [PubMed] [Google Scholar]
- 6.Esser P, Mehnert A, Johansen C, et al. Body image mediates the effect of cancer‐related stigmatization on depression: A new target for intervention. Psychooncology. 2018;27:193–8. doi: 10.1002/pon.4494. [DOI] [PubMed] [Google Scholar]
- 7.Maass SWMC, Boerman LM, Verhaak PFM, et al. Long-term psychological distress in breast cancer survivors and their matched controls: A cross-sectional study. Maturitas. 2019;130:6–12. doi: 10.1016/j.maturitas.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Distress Management Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2003;1:344. doi: 10.6004/jnccn.2003.0031. [DOI] [PubMed] [Google Scholar]
- 9.Lyu D, Lan B, Sun XY, et al. Relationship between dynamic changes of psychological distress and quality of life in Chinese early breast cancer patients. Zhonghua Zhong Liu Za Zhi. 2022;44:1119–24. doi: 10.3760/cma.j.cn112152-20210412-00308. [DOI] [PubMed] [Google Scholar]
- 10.Hass HG, Herzberger A, Wöckel A, et al. Male Breast Cancer: Therapy-Induced Toxicities, Psychological Distress, and Individual Patient Goals during Oncological Inpatient Rehabilitation. Oncol Res Treat. 2022;45:736–43. doi: 10.1159/000526704. [DOI] [PubMed] [Google Scholar]
- 11.Al-Ghabeesh SH, Al-Kalaldah M, Rayan A, et al. Psychological distress and quality of life among Jordanian women diagnosed with breast cancer: The role of trait mindfulness. Eur J Cancer Care (Engl) 2019;28:e13082. doi: 10.1111/ecc.13082. [DOI] [PubMed] [Google Scholar]
- 12.Andreu Y, Galdón MJ, Durá E, et al. A longitudinal study of psychosocial distress in breast cancer: prevalence and risk factors. Psychol Health. 2012;27:72–87. doi: 10.1080/08870446.2010.542814. [DOI] [PubMed] [Google Scholar]
- 13.Park J-H, Chun M, Jung Y-S, et al. Predictors of Psychological Distress Trajectories in the First Year After a Breast Cancer Diagnosis. Asian Nurs Res (Korean Soc Nurs Sci) 2017;11:268–75. doi: 10.1016/j.anr.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Alfonsson S, Olsson E, Hursti T, et al. Socio-demographic and clinical variables associated with psychological distress 1 and 3 years after breast cancer diagnosis. Support Care Cancer . 2016;24:4017–23. doi: 10.1007/s00520-016-3242-y. [DOI] [PubMed] [Google Scholar]
- 15.Rostom A, Dubé C, Cranney A, et al. Celiac disease. Evid Rep Technol Assess (Summ) 2004;2004:1–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
- 17.Cohen J. A power primer. Psychol Bull. 1992;112:155–9. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–55. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 20.Alcorso J, Sherman KA. Factors associated with psychological distress in women with breast cancer-related lymphoedema. Psychooncology. 2016;25:865–72. doi: 10.1002/pon.4021. [DOI] [PubMed] [Google Scholar]
- 21.Berhili S, Kadiri S, Bouziane A, et al. Associated factors with psychological distress in Moroccan breast cancer patients: A cross-sectional study. The Breast . 2017;31:26–33. doi: 10.1016/j.breast.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 22.Berhili S, Ouabdelmoumen A, Sbai A, et al. Radical Mastectomy Increases Psychological Distress in Young Breast Cancer Patients: Results of A Cross-sectional Study. Clin Breast Cancer. 2019;19:e160–5. doi: 10.1016/j.clbc.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 23.Bidstrup PE, Christensen J, Mertz BG, et al. Trajectories of distress, anxiety, and depression among women with breast cancer: Looking beyond the mean. Acta Oncol. 2015;54:789–96. doi: 10.3109/0284186X.2014.1002571. [DOI] [PubMed] [Google Scholar]
- 24.Bjerkeset E, Röhrl K, Schou-Bredal I. Symptom cluster of pain, fatigue, and psychological distress in breast cancer survivors: prevalence and characteristics. Breast Cancer Res Treat. 2020;180:63–71. doi: 10.1007/s10549-020-05522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Faller H, Brähler E, Härter M, et al. Unmet needs for information and psychosocial support in relation to quality of life and emotional distress: A comparison between gynecological and breast cancer patients. Pat Educ Couns. 2017;100:1934–42. doi: 10.1016/j.pec.2017.05.031. [DOI] [PubMed] [Google Scholar]
- 26.Holger GH, Marianne S, Achim W, et al. Psychological distress in breast cancer patients during oncological inpatient rehabilitation: incidence, triggering factors and correlation with treatment-induced side effects. Arch Gynecol Obstet. 2022 doi: 10.1007/s00404-022-06657-3. [DOI] [PubMed] [Google Scholar]
- 27.Jørgensen L, Laursen BS, Garne JP, et al. Prevalence and predictors of distress in women taking part in surgical continuity of care for breast cancer: A cohort study. Eur J Oncol Nurs. 2016;22:30–6. doi: 10.1016/j.ejon.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 28.Liu J, Wang H, Wang M, et al. Posttraumatic growth and psychological distress in Chinese early‐stage breast cancer survivors: a longitudinal study. Psychooncology. 2014;23:437–43. doi: 10.1002/pon.3436. [DOI] [PubMed] [Google Scholar]
- 29.Lim SY, Ke Y, Mok NK-M, et al. Factors associated with distress and the impact of distress on acute health-care service utilization among patients diagnosed with breast and gynecological cancers. Pall Supp Care . 2023:1–8. doi: 10.1017/S1478951522001444. n.d. [DOI] [PubMed] [Google Scholar]
- 30.Liu JK, Kaji AH, Roth KG, et al. Determinants of Psychosocial Distress in Breast Cancer Patients at a Safety Net Hospital. Clin Breast Cancer. 2022;22:43–8. doi: 10.1016/j.clbc.2021.06.011. [DOI] [PubMed] [Google Scholar]
- 31.Nsondé Malanda J, Loukibou Ngouari F, Salam Ngouaka B, et al. The Psychological Distress of Patients with Breast Cancer at University Teaching Hospital of Brazzaville. IJCOCR . 2021;6:22. doi: 10.11648/j.ijcocr.20210601.14. [DOI] [Google Scholar]
- 32.Thakur M, Sharma R, Mishra AK, et al. Psychological distress and body image disturbances after modified radical mastectomy among breast cancer survivors: A cross-sectional study from a tertiary care centre in North India. Lancet Reg Health SE Asia. 2022;7:100077. doi: 10.1016/j.lansea.2022.100077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lo-Fo-Wong DNN, de Haes HCJM, Aaronson NK, et al. Predictors of enduring clinical distress in women with breast cancer. Breast Cancer Res Treat. 2016;158:563–72. doi: 10.1007/s10549-016-3896-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Phoosuwan N, Lundberg PC. Psychological distress and health-related quality of life among women with breast cancer: a descriptive cross-sectional study. Support Care Cancer . 2022;30:3177–86. doi: 10.1007/s00520-021-06763-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schubart JR, Emerich M, Farnan M, et al. Screening for Psychological Distress in Surgical Breast Cancer Patients. Ann Surg Oncol. 2014;21:3348–53. doi: 10.1245/s10434-014-3919-8. [DOI] [PubMed] [Google Scholar]
- 36.Wevers MR, Schou-Bredal I, Verhoef S, et al. Psychological distress in newly diagnosed breast cancer patients: an observational study comparing those at high risk of hereditary cancer with those of unknown risk. J Psychosoc Oncol Res Pract. 2020;2:e18. doi: 10.1097/OR9.0000000000000018. [DOI] [Google Scholar]
- 37.Shen Y, Zhang J, BU Q, et al. A longitudinal study of psychological distress and its related factors in patients with breast cancer. Chin Nurs Manag. 2018;18:617–22. [Google Scholar]
- 38.Soo H, Sherman KA. Rumination, psychological distress and post-traumatic growth in women diagnosed with breast cancer. Psychooncology. 2015;24:70–9. doi: 10.1002/pon.3596. [DOI] [PubMed] [Google Scholar]
- 39.Taira N, Iwata H, Hasegawa Y, et al. Health-related quality of life and psychological distress during neoadjuvant endocrine therapy with letrozole to determine endocrine responsiveness in postmenopausal breast cancer. Breast Cancer Res Treat. 2014;145:155–64. doi: 10.1007/s10549-014-2935-5. [DOI] [PubMed] [Google Scholar]
- 40.Akechi T, Okuyama T, Endo C, et al. Patient’s perceived need and psychological distress and/or quality of life in ambulatory breast cancer patients in Japan. Psychooncology. 2011;20:497–505. doi: 10.1002/pon.1757. [DOI] [PubMed] [Google Scholar]
- 41.Yang W, Shan-hong FAN, Lei C. Psychological distress and related factors in patients with breast cancer. Chin J Gen Pract. 2016;14:1912–4. doi: 10.16766/j.cnki.issn.1674-4152.2016.11.039. [DOI] [Google Scholar]
- 42.Ying W, Zhengwen PAN, Annuo LIU, et al. Mediating Role of Coping Style in Adult Attachment and Psychological Distress in Breast Cancer Patients. Nurs J Chin PLA. 2020;37 [Google Scholar]
- 43.Warmoth K, Wong CCY, Chen L, et al. The role of acculturation in the relationship between self-stigma and psychological distress among Chinese American breast cancer survivors. Psychology, Health & Medicine. 2020;25:1278–92. doi: 10.1080/13548506.2020.1734638. [DOI] [PubMed] [Google Scholar]
- 44.Yu Y, Sherman KA. Communication avoidance, coping and psychological distress of women with breast cancer. J Behav Med. 2015;38:565–77. doi: 10.1007/s10865-015-9636-3. [DOI] [PubMed] [Google Scholar]
- 45.Younis MAR, Norsa’adah B, Othman A, et al. Psychological distress impact and associated factors among Jordanian women diagnosed with breast cancer. Med Sci. 2020;24:2610–9. [Google Scholar]
- 46.Yu WJ, Zhang AH, Xia C, et al. Mediating role of resilience in posttraumatic growth and miserable emotion among breast cancer patients. Mod Prev Med. 2018;45:1827–31. [Google Scholar]
- 47.Su Z, Zhou Y, Han X, et al. Symptom burden in advanced breast cancer patients and its association between death anxiety and psychological distress. Chin J Cancer Res. 2022;34:298–308. doi: 10.21147/j.issn.1000-9604.2022.03.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Al-Fahdi A, Chan MF, Al-Siyabi W, et al. Prevalence of psychological distress and associated factors among Omani women diagnosed with breast cancer: a single-centre, cross-sectional study. BMJ Open. 2023;13:e073967. doi: 10.1136/bmjopen-2023-073967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gu Z, Li M, Liu L, et al. The moderating effect of self-efficacy between social constraints, social isolation, family environment, and depressive symptoms among breast cancer patients in China: a cross-sectional study. Support Care Cancer. 2023;31 doi: 10.1007/s00520-023-08063-0. [DOI] [PubMed] [Google Scholar]
- 50.Omari M, Amaadour L, Zarrouq B, et al. Evaluation of psychological distress is essential for patients with locally advanced breast cancer prior to neoadjuvant chemotherapy: baseline findings from cohort study. BMC Womens Health . 2023;23:445. doi: 10.1186/s12905-023-02571-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ostovar S, Modarresi Chahardehi A, Mohd Hashim IH, et al. Prevalence of psychological distress among cancer patients in Southeast Asian countries: A systematic review. Eur J Cancer Care (Engl) 2022;31:e13669. doi: 10.1111/ecc.13669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cicero G, De Luca R, Dorangricchia P, et al. Risk Perception and Psychological Distress in Genetic Counselling for Hereditary Breast and/or Ovarian Cancer. J Genet Couns. 2017;26:999–1007. doi: 10.1007/s10897-017-0072-0. [DOI] [PubMed] [Google Scholar]
- 53.Guangju C, Ruyan X, Miu M. Analysis of influencing factors of psychological distress in patients with breast cancer radiotherapy. Chin J Mod Nurs. 2022;28:805–8. [Google Scholar]
- 54.Chen X, Wang L, Liu L, et al. Factors associated with psychological distress among patients with breast cancer during the COVID-19 pandemic: a cross-sectional study in Wuhan, China. Support Care Cancer . 2021;29:4773–82. doi: 10.1007/s00520-021-05994-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lam WWT, Soong I, Yau TK, et al. The evolution of psychological distress trajectories in women diagnosed with advanced breast cancer: a longitudinal study. Psychooncology. 2013;22:2831–9. doi: 10.1002/pon.3361. [DOI] [PubMed] [Google Scholar]
- 56.Kola L, Kohrt BA, Hanlon C, et al. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;8:535–50. doi: 10.1016/S2215-0366(21)00025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cimino T, Said K, Safier L, et al. Psychosocial distress among oncology patients in the safety net. Psychooncology. 2020;29:1927–35. doi: 10.1002/pon.5525. [DOI] [PubMed] [Google Scholar]
- 58.Cohen M, Yagil D, Aviv A, et al. Cancer patients attending treatment during COVID-19: intolerance of uncertainty and psychological distress. J Cancer Surviv . 2022;16:1478–88. doi: 10.1007/s11764-021-01126-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Adjei Boakye E, Polednik KM, Deshields TL, et al. Emotional distress among survivors of adolescent and young adult cancer or adult cancer. Ann Epidemiol. 2022;72:48–56. doi: 10.1016/j.annepidem.2022.03.014. [DOI] [PubMed] [Google Scholar]
- 60.Hong KM. Understanding of middle-aged women’s crisis and Christian counseling. Gosp Prax. 2012;25:217–44. [Google Scholar]
- 61.Alnazly E, Khraisat OM, Al-Bashaireh AM, et al. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16:e0247679. doi: 10.1371/journal.pone.0247679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Thapa S, Sun H, Pokhrel G, et al. Performance of Distress Thermometer and Associated Factors of Psychological Distress among Chinese Cancer Patients. J Oncol. 2020;2020:3293589. doi: 10.1155/2020/3293589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brännlund A, Hammarström A. Higher education and psychological distress: a 27-year prospective cohort study in Sweden. Scand J Public Health. 2014;42:155–62. doi: 10.1177/1403494813511559. [DOI] [PubMed] [Google Scholar]
- 64.O’leimat AS, Alhussami M, Rayan A. The correlates of psychological distress among parents of children with psychiatric disorders. J Child Adolesc Psychiatr Nurs . 2019;32:24–32. doi: 10.1111/jcap.12223. [DOI] [PubMed] [Google Scholar]
- 65.Altice CK, Banegas MP, Tucker-Seeley RD, et al. Financial Hardships Experienced by Cancer Survivors: A Systematic Review. J Natl Cancer Inst. 2017;109:djw205. doi: 10.1093/jnci/djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tu C, He Y, Ma X. Factors influencing psychological distress and effects of stepwise psychological care on quality of life in patients undergoing chemotherapy after breast cancer surgery. Am J Transl Res. 2022;14:1923–33. [PMC free article] [PubMed] [Google Scholar]
- 67.Christensen S, Zachariae R, Jensen AB, et al. Prevalence and risk of depressive symptoms 3–4 months post-surgery in a nationwide cohort study of Danish women treated for early stage breast-cancer. Breast Cancer Res Treat. 2009;113:339–55. doi: 10.1007/s10549-008-9920-9. [DOI] [PubMed] [Google Scholar]
- 68.Tian X, Jin Y, Tang L, et al. Predicting the Risk of Psychological Distress among Lung Cancer Patients: Development and Validation of a Predictive Algorithm Based on Sociodemographic and Clinical Factors. Asia Pac J Oncol Nurs. 2021;8:403–12. doi: 10.4103/apjon.apjon-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pok-Ja O, Jung-Ran C. Changes in Fatigue, Psychological Distress, and Quality of Life After Chemotherapy in Women with Breast Cancer: A Prospective Study. 43 doi: 10.1097/NCC.0000000000000689. n.d. [DOI] [PubMed] [Google Scholar]
- 70.Ganz PA, Kwan L, Stanton AL, et al. Physical and Psychosocial Recovery in the Year After Primary Treatment of Breast Cancer. JCO . 2011;29:1101–9. doi: 10.1200/JCO.2010.28.8043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schnur JB, Montgomery GH, Hallquist MN, et al. Anticipatory psychological distress in women scheduled for diagnostic and curative breast cancer surgery. Int J Behav Med. 2008;15:21–8. doi: 10.1007/BF03003070. [DOI] [PubMed] [Google Scholar]
- 72.Nguyen TQ, Do TM, Pham TA. Screening for Psychological Distress in Vietnamese Cancer Patients: An Evaluation of the Distress Thermometer. Cancer Med. 2021;10:7793–803. doi: 10.1002/cam4.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vescovelli F, Minotti S, Ruini C. Exploring Post-traumatic Growth in Parkinson’s Disease: A Mixed Method Study. J Clin Psychol Med Settings. 2021;28:267–78. doi: 10.1007/s10880-020-09713-9. [DOI] [PubMed] [Google Scholar]
- 74.Adar T, Davidof M, Elkana O. Social Support Mediates the Association between Attachment Style and Psychological Distress during COVID-19 in Israel. Viruses. 2022;14:693. doi: 10.3390/v14040693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Oryan Z, Avinir A, Levy S, et al. Risk and protective factors for psychological distress during COVID-19 in Israel. Curr Psychol . 2023;42:2448–59. doi: 10.1007/s12144-021-02031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Amini-Tehrani M, Zamanian H, Daryaafzoon M, et al. Body image, internalized stigma and enacted stigma predict psychological distress in women with breast cancer: A serial mediation model. J Adv Nurs. 2021;77:3412–23. doi: 10.1111/jan.14881. [DOI] [PubMed] [Google Scholar]
- 77.Mozid NE. Association between psychological distress and coping strategies among students engaged in online learning. PLoS One. 2022;17:e0270877. doi: 10.1371/journal.pone.0270877. [DOI] [PMC free article] [PubMed] [Google Scholar]