Abstract
Background
Childhood abuse and neglect pose important risk factors for the development of psychopathology during pregnancy. However, only a few studies have assessed the effects of a specific type of abuse during the perinatal period, namely, psychological maltreatment, which includes emotional abuse and neglect. These studies have found that women who have experienced psychological maltreatment exhibit higher levels of antenatal depressive symptoms and greater difficulties forming attachment with their babies than women who have not experienced this kind of adversity. The aim of this study was to examine how emotional abuse and neglect experiences may favor the occurrence of psychological distress in pregnant women, and whether prenatal attachment might explain this association.
Methods
Participants comprised 128 Italian pregnant women ranging in age from 21 to 46 years (Mage = 33.4; SD = 6.10). Women responded to the following self-report instruments: CECA.Q and CTQ-SF, for the assessment of psychological maltreatment experiences; MAAS, for the evaluation of prenatal attachment; and PAMA, for the assessment of perinatal psychological distress.
Results
Pearson correlations revealed a positive association between childhood neglect and perinatal psychological distress and a negative association between childhood neglect and prenatal attachment scores. No significant correlations were found for emotional abuse. Perinatal psychological distress was negatively associated with prenatal attachment. Mediation analyses showed significant associations between childhood neglect and the dimensions of perinatal affectivity and prenatal maternal attachment. Prenatal maternal attachment mediated the relationship between neglect and perinatal psychological distress.
Conclusions
The transition to motherhood is a sensitive period, particularly for women who have experienced abuse and neglect during childhood. These experiences may negatively impact a woman’s disposition to emotionally and behaviorally engage in the formation of a bond with their unborn baby. These results may have important prevention and clinical implications and thus warrant further exploration.
Keywords: Pregnancy, Perinatal period, Childhood psychological maltreatment, Emotional abuse, Neglect, Prenatal Attachment, Maternal psychological distress
Background
Pregnancy is a vulnerable period in which the negative consequences of adverse previous experiences may occur, as becoming a mother can activate emotional responses related to childhood experiences of abuse and neglect [67]. Literature has shown that women with histories of childhood trauma reported higher levels of depression [23], post-traumatic stress disorder, personality disorders, and dissociation during pregnancy [11] and postpartum [52] compared to non-exposed women. However, these studies have focused mainly on cumulative childhood maltreatment, and research on the effects of childhood maltreatment in the perinatal period has on centered on sexual and physical abuse, and not specifically on psychological maltreatment, which includes emotional abuse (EA) and/or neglect.
EA refers to the inability to provide children with an emotional environment that adequately supports their psychological and physical development [24]. It is characterized by the parents ‘hostility and intention to scare and humiliate the child, constantly disapproving, reprimanding, and yelling at him, suggesting that he is without value [15]. Neglect, in contrast, is commonly described as an omissive abuse in which the environment neither confirms nor meets the child’s basic needs (emotional and/or developmental) and is not capable of providing emotional support or warmth to the child [56]. Bifulco [13] adds and specifies that neglect also includes parents’ disinterest in their child’s material care, health, social functions, and schoolwork.
EA and neglect are particular forms of maltreatment that rather than being point-like as physical and sexual abuse, represent relational modes of a chronically dysfunctional family atmosphere characterized by episodes of abuse or omission, which are pervasive, occur daily, and contribute to structuring the quality of the relationship. EA and neglect create a chronically dysfunctional family atmosphere that negatively impacts the construction and representation of themselves and significant others.
Having a history of childhood neglect and EA exposes women to psychological distress during pregnancy [46] and the postpartum period [14], possibly affecting their emotional and caregiving abilities as mothers [57]. Perinatal psychological distress is a condition that arises from a maladaptive response to stressors related to the transition to motherhood [18]. It is a state of maternal emotional suffering that encompasses a wide range of psychological dimensions, such as anxiety, depressive symptoms, anger, stress, and somatization [4]. Although this condition is not among the recognized mental disorders, it may expose a woman to several negative psychopathological outcomes during the postpartum period [55].
Regarding the association between adverse childhood experiences and psychological distress, the literature has mostly focused on perinatal depressive symptoms. For instance, findings from a longitudinal study conducted by Li [46] revealed that women who had encountered neglect or EA demonstrated significantly elevated symptoms of antenatal depression in comparison to women with no history of physical or emotional neglect.
Experiences of neglect in childhood have also been linked to mothers experiencing significantly greater difficulties in bonding with their children compared to women who have not experienced maltreatment [54]. A recent longitudinal study [68] confirmed that exposure to childhood neglect, in particular, has an important influence on women’s experiences of attachment to their babies and that these maternal difficulties predict postpartum depression.
Attachment between mother and infant starts during pregnancy and continues to increase daily after birth. Although most literature has examined this bond after the infant’s birth, recent studies have revealed that this bond starts during pregnancy when women begin to develop both a cognitive and affective a mental representation of their unborn children [21]. Prenatal attachment refers to this specific bond between the mother and her fetus [25]. The concept of prenatal attachment originally focused on maternal behavior during pregnancy. Cranley [27], however, was the first to define this concept as the mother’s interest in establishing a relationship with her unborn child, which manifests through behaviors that demonstrate emotional investment and bonding. Later, some authors also emphasized the emotional aspect [26], and Doan and Zimmerman [31] focused on both components of the concept, redefining prenatal attachment as the emotional bond between a parent and fetus that is connected to the cognitive and emotional capacity to understand and connect with another person. This bond evolves within a larger environmental context.
Recent studies have consistently shown that the quality of prenatal attachment is closely and positively related to the quality of postnatal mother–child attachment [64]. Specifically, evidence suggests that a suboptimal prenatal attachment is associated with a lack in a mother’s care of herself and her baby during pregnancy, which can result in potential complications and risks during pregnancy and delivery [47]. These findings align with literature reporting that the quality of prenatal attachment is also strongly correlated with the quality of maternal adult attachment. Indeed, mothers that demonstrate a secure adult state of mind with respect to their childhood experiences with their caregivers have a better and early occurring prenatal attachment during pregnancy [30]. Notably, maternal attachment security has also been strongly correlated with maternal distress [53], sensitive parenting [40], and improved developmental outcomes in children [2]. In light of this literature, it might be hypothesized that prenatal attachment could act as a pivotal protective factor for several maternal and dyadic unfavorable outcomes, thus warranting further investigation.
In this framework, it is not surprising that a suboptimal prenatal attachment is also linked with maternal psychological distress, particularly prenatal depressive symptoms [38, 50, 63]. However, the direction of this link between prenatal depressive symptoms and prenatal attachment remains unclear. Studies have suggested that prenatal depressive symptoms may constitute a risk factor for a lack of maternal attachment and depressive symptoms during the postpartum period [32, 38]. The direction of this relationship might also be reversed, especially if symptoms are measured prenatally. Indeed, insecure adult attachment representations, whether attachment is measured prenatally or not, derive from the perceived quality of childhood experiences [49]. In the context of childhood trauma, the literature has shown that specific memories of inadequate parenting as well as rejection, violence, and neglect, may result in the mother fearing the repeating of a painful past and a perception of the “child-as-threat” [62]. These feelings, in turn, might potentially be associated with feelings of inadequate parenting abilities, low self-esteem and, ultimately, reduced psychological well-being.
Models of the relationship between childhood trauma, prenatal attachment, and psychological distress have been proposed. Berthelot et al. [11] proposed that mental health levels could buffer the relationship between childhood abuse and neglect experiences of future mothers and the quality of their prenatal attachment. Although they did not find a direct relationship between childhood maltreatment and prenatal attachment, they did find pairwise associations between poor mental health and childhood maltreatment or between poor mental health and prenatal attachment.
Given:
that this hypothesis-driven model does not support the existence of a mediation role of mental health between childhood trauma and prenatal attachment;
the paucity of literature on prenatal attachment;
the unclear direction of the relationship between mental health and prenatal attachment;
that childhood trauma has been rarely investigated in its sub-dimensions;
Building on extant literature (Bertherlot et al., 2019), the aim of the present study was to test complementary models of the relationship between childhood trauma, psychological distress, and prenatal attachment by investigating (i) the relationship between two specific and diverse childhood trauma experiences (namely, EA and neglect) and the presence of psychological distress in pregnant women, and (ii) whether prenatal attachment might act as a potential protective factor within this relationship. We hypothesized the following:
Pregnant women’s childhood experiences of EA and neglect are positively associated with prenatal psychological distress.
Pregnant women’s childhood experiences of EA and neglect are negatively associated with prenatal maternal attachment.
Prenatal maternal attachment is negatively associated with prenatal psychological distress.
Antenatal maternal attachment mediates the relationship between EA and neglect and psychological distress.
Methods
Participants
A total of 128 pregnant women ranging between 21 and 46 years of age (M = 33.4; SD = 6.10) participated in the study. The participants were recruited at the ARNAS Civico Hospital of Palermo, thanks to a research agreement protocol with the Department of Psychology, Educational Science and Human Movement, University of Palermo, Italy. The participants completed the questionnaires during their first hospital visit. The visits involved routine check-ups or pregnancy traces. In this hospital, psychological distress evaluation, conducted by trained psychologists, was a standard component of a comprehensive assessment of general women’s health during pregnancy. Data for this study were collected from November 2023 to February 2024.
Inclusion criteria were: a) being pregnant; b) being at least age 18; and c) able to understand and speak the Italian language. Participation in the research was voluntary, and all participants gave informed consent prior to inclusion in the study. Participants completed self-report questionnaires on either their smartphone, computer, or tablet.
A total of 91.4% of participants had a romantic relationship and lived with a partner. Most participants (64.1%) were in the third trimester of pregnancy, had no other children (78%), and had planned the currently pregnancy (80.3%). Detailed information on demographic and clinical characteristics is reported in Table 1.
Table 1.
Characteristics of the study population (N = 128)
| Variable | ||
|---|---|---|
| n | % | |
| Age | ||
| < 29 years old | 36 | 28.12 |
| 36–30 years old | 70 | 54.69 |
| 45–37 years old | 22 | 17.19 |
| Education | ||
| Primary School | 3 | 2.34 |
| Hight School | 40 | 31.25 |
| University degree | 47 | 36.72 |
| Post-degree | 38 | 29.69 |
| Employment status | ||
| Unemployed | 8 | 6.25 |
| Housewife | 8 | 6.25 |
| Student | 3 | 2.34 |
| Precarious employment | 27 | 21.1 |
| Stable employment | 82 | 64.06 |
| Marital status | ||
| Single | 11 | 8.59 |
| Married/Cohabitant | 117 | 91.41 |
| Economic status | ||
| Low | 18 | 14.06 |
| Middle | 71 | 55.47 |
| Medium–high | 39 | 30.47 |
| Gestational age | ||
| First trimester | 9 | 7.03 |
| Second trimester | 42 | 32.81 |
| Third trimester | 77 | 60.16 |
| Pregnancy | ||
| Planned pregnancy | 102 | 80.31 |
| Unplanned pregnancy | 25 | 19.69 |
| First pregnancy | ||
| Yes | 59 | 46.46 |
| No | 68 | 53.54 |
| Other children | ||
| Yes | 28 | 22.05 |
| No | 99 | 77.95 |
| High-risk pregnancy | ||
| Yes | 37 | 28.91 |
| No | 91 | 71.09 |
| Medically Assisted Procreation | ||
| Yes | 9 | 7.09 |
| No | 118 | 92.91 |
| Psychopharmacological treatment | ||
| Yes | 0 | 0 |
| No | 128 | 100 |
Ethical approval for this study was obtained from the Bioethics Committee at the University of Palermo (prot.n.153791–2023 of 26/10/2023), and the procedures used adhere to the principles of the Declarations of Helsinki.
Measures
Participants underwent a psychological assessment consisting of the following instruments:
Questionnaire on sociodemographic characteristics and pregnancy-related variables
This questionnaire is suitable for gathering sample information such as age, educational and economical status, marital status, and pregnancy details such as primiparity, month of pregnancy, and single versus twin pregnancy.
Childhood Experience of Care and Abuse Questionnaire (CECA.Q) [12]
This is a self-report measure whose purpose is to collect objective information relating to adverse experience in childhood, before age 17. More specifically, CECA.Q assesses antipathy (defined as coldness, rejection, or hostility) and neglect (defined in terms of parents’ disinterest in material care, health, friendships, and schoolwork) expressed by parents toward the child, parental physical abuse, sexual abuse by any adult. In this study, we considered only the subscales antipathy (8 items) and neglect (8 items), assessed using a 5-point Likert scale ranging from (1) ‘yes definitely’ to (5) ‘no, not at all’. We considered the antipathy and neglect scores of both parents, which were input into the calculation of an overall emotional abuse and neglect score, as described below. The questionnaire shows high reliability and validity, achieving satisfactory internal scale consistency for the antipathy (α = 0.81) and neglect (α = 0.80) scales.
This 28-item self-report questionnaire on childhood trauma was developed to assess five types of early maltreatment experiences [10]. The five type of abuse are emotional abuse, physical abuse, emotional neglect, physical neglect, and sexual abuse [9]. Each type corresponds to a subscale, and each subscale is composed of five questions that are rated on a 5-point Likert Scale (from 1 = Never true to 5 = Very often true). The total possible score is 125, with cutoff points suggested by Aas et al. [1] of ≥ 10 for physical abuse, ≥ 8 for sexual abuse, ≥ 13 for emotional abuse, ≥ 15 for emotional neglect, and ≥ 10 for physical neglect. High scores suggest more severe abuse experiences. The emotional abuse and neglect subscale scores obtained from this instrument were entered into the calculation of an overall emotional abuse and neglect score, described below. The Italian version of the CTQ-SF questionnaire has adequate psychometrics properties. Internal consistence is excellent in each subscale: emotional abuse (α = 0.88), physical abuse (α = 0.95), emotional neglect (α = 0.91), physical neglect (α = 0.87), and sexual abuse (α = 0.96) [58].
This self-report questionnaire assesses maternal prenatal attachment. It is a 19-item questionnaire that uses a 5-point Likert Scale to analyze what the mother felt and thought about her unborn child and her daily behaviors towards the child/fetus. The total possible score is 95 and the minimum possible score is 19. Higher scores suggest a stronger bonding. The MAAS has two subscales that assess the intensity and quality of attachment. Specifically, the Quality of Attachment subscale measures the mother’s emotional experiences toward the fetus (i.e., closeness, pleasure, tenderness, and distress over imagined loss), while the Intensity of Concern subscale measures the extent of time spent dreaming about, talking to, or palpating the fetus. We used the Italian version of the questionnaire, which demonstrated good internal consistency for the scale of MAAS total score (α = 0.71) and Intensity of Concern subscale (α = 0.62). The Quality of Attachment subscale, however, exhibited poor internal consistency, with an α of 0.57 [17]. In this study we used both the scores of Quality of Attachment (MAAS-QA) and Intensity of Concern (MAAS-IC), and the overall score (MAAS-TOT), obtained by summing the MAAS-QA and MAAS-IC scores.
The Perinatal Assessment of Maternal Affectivity (PAMA) [4]
PAMA is an 11-item self-reported screening measure that assesses perinatal maternal distress. The first eight items correspond to eight subscales. These eight subscales correspond to a dimension: anxiety, depression, perceived stress, irritability/anger (excitability, anger attacks, disputes with others), relationship problems, psychosomatic reaction, physiological problems (with sleeping or eating), addictions (smoking, taking drugs, drinking alcohol), and other risky behaviors (such as driving fast after drinking alcohol). The last three items are open-ended questions relating to motherhood and cultural factors. The PAMA scores range from 0 to 3. The higher scores indicate a greater risk of developing symptoms related to psychological distress. In this study we used the total score (PAMA_TOT), given by the sum of the subscale scores, which allows a global assessment of maternal affectivity during the perinatal period. PAMA scores showed adequate internal consistency reliability (α = 0.76).
Descriptive statistics for all the variables of interest are shown in Table 2
Table 2.
Descriptive statistics of the variables of interest
| Mean | SD | Range | |
|---|---|---|---|
| PAMA-TOT | 6.98 | 4.24 | 0—22 |
| MAAS-QA | 46.56 | 2.75 | 38—50 |
| MAAS-IC | 29.92 | 3.84 | 18—38 |
| MAAS-TOT | 81.11 | 5.75 | 64—92 |
| CTQ Emotional Abuse | 6.3 | 3.28 | 5–21 |
| CTQ Emotional Neglect | 10.48 | 4.1 | 5–25 |
| CTQ Physical Neglect | 6.64 | 2.33 | 5–16 |
| CECA-Q Antipathy Mother | 8.48 | 3.9 | 4–22 |
| CECA-Q Antipathy Father | 3.74 | 4.27 | 0—16 |
| CECA-Q Neglect Mother | 3.59 | 4.51 | 0—24 |
| CECA-Q Neglect Father | 5.75 | 6.42 | 0—25 |
Statistical analysis
To evaluate childhood experiences of emotional abuse and neglect, we assessed 61 (48%) pregnant women with the CECA.Q, and the remaining 67 (52%) with the CTQ.
To integrate the scores of both questionnaires, the overall emotional abuse score (EAS) was calculated by considering, for participants who had completed the CECA.Q, a Z-score-standardized sum of the maternal and paternal antipathy scores, whereas for participants who had completed the CTQ, the emotional abuse subscale scores, standardized in Z points. Similarly, to obtain the overall neglect score (NS), we used the scores of maternal and paternal neglect for the CECA.Q and the physical and emotional neglect subscales of the CTQ and transformed all scores into Z scores.
To facilitate comparison among all the variables included in the study, we standardized each variable into Z-scores, subsequently transforming them into T-scores. All variables were tested for the possible presence of outliers using Grubb’s test (p < 0.05). We identified one outlier for the variable NS and one outlier for the variable PAMA-TOT. Both values were removed from the dataset and were not used in subsequent analyses. Skewness and kurtosis were used to assess the normality of the variables. We adopted the conservative criterion of skewness and kurtosis < 2 [36] to identify deviations from normality. All variables showed acceptable normality except NS, which showed marked kurtosis (NS: skewness = 1.8; kurtosis = 3.8). Given the effectiveness of the Log10 transformation for variables with marked kurtosis [41], we computed the Log10 transformations of the NS obtaining acceptable distribution parameters (skewness = 1.1; kurtosis = 1.3).
To assess the potential impact of confounding factors, we tested the association between the variables of interest and age using Pearson correlation (p < 0.05), as well as the association between the variables of interest and the trimester of pregnancy at the time of the survey using ANOVA statistics (p < 0.05).
Using Pearson correlation (p < 0.05), we investigated the possible association between childhood experiences of neglect and EA, as measured by the NS and EAS scores, and the dimensions of perinatal affectivity and prenatal maternal attachment as measured by the PAMA and MAAS scales. In addition, also using Pearsons correlation (p < 0.05), we explored the possible association between the PAMA and MAAS scales. All correlations were corrected for multiple comparisons using the False Discovery Rate procedure (Benjamini–Hochberg method) [7].
The possible relationships between childhood experiences of neglect and EA, and the dimensions of perinatal affectivity and prenatal maternal attachment were further analyzed with mediation analysis to explore the potential mediating role of prenatal maternal attachment [6]. For this purpose, separate models were created using the measure of exposure to childhood experiences of neglect and EA (NS and EAS) as the predictor, the total score on the Perinatal Affectivity Scale (PAMA) as the outcome, and the measures of perinatal affectivity (MAAS-TOT, MAAS-QA, MAAS-IC) as the mediator. All models were bootstrapped for 1000 repetitions. The statistical significance of the mediation models was set at p < 0.05.
Results
Correlation analyses between exposure to childhood of neglect and EA and the dimensions of perinatal affectivity and prenatal maternal attachment showed a positive correlation between NS and PAMA-TOT (r = 0. 22, FDRp = 0.02), as well as a negative correlation between NS and the measures of MAAS-TOT (r = -0.28, FDRp = 0.004), MAAS-QA (r = -0.31, FDRp = 0.004) and MAAS-IC (r = -0.19, FDRp = 0.03). There was no significant correlation for the EAS (p > 0.05). The PAMA-TOT was also negatively associated with the dimensions of MAAS-TOT (r = -0.27, FDRp = 0.002) and MAAS-QA (r = -0.43, FDRp = 0.002). Analyses of the potential effect of age and trimester of pregnancy on the variables of interest indicated no effect of these variables (Table 3).
Table 3.
Results of correlation analyses
| PAMA-TOT | MAAS-TOT | MAAS-QA | MAAS-IC | |||||
| r | p-value | r | p-value | r | p-value | r | p-value | |
| NS | 0. 22 | 0.02* | -0.28 | 0.004* | -0.31 | 0.004* | -0.19 | 0.03* |
| EAS | 0. 11 | 0.2 | -0.17 | 0.054 | -0.1 | 0.27 | -0.15 | 0.09 |
| MAAS-TOT | MAAS-QA | MAAS-IC | ||||||
| r | p-value | r | p-value | r | p-value | |||
| PAMA-TOT | - | - | -0.27 | 0.002* | -0.43 | 0.002* | -0.08 | 0.36 |
*FDR p-value
Mediation analyses performed on the variables showed significant associations between childhood exposure to neglect and abuse and the dimensions of perinatal affectivity and prenatal maternal attachment, which is in line with the Baron e Kenny (1986) assumptions.
Specifically, we found a total mediation of the MAAS-TOT on the relationship between NS and PAMA-TOT (direct effect Z: 1.8, p = 0.7; indirect effect Z: 2, p = 0.04; total effect Z: 2.6, p = 0.01, Fig. 1a). Similarly, the MAAS-QA scale was also found to fully mediate the relationship between NS and PAMA-TOT (direct effect Z: 1.3, p = 0.2; indirect effect Z: 2.9, p = 0.004; total effect Z: 2.6, 0.008, Fig. 1b). In contrast, no mediation was detected for the MAAS-IC scale.
Fig. 1.
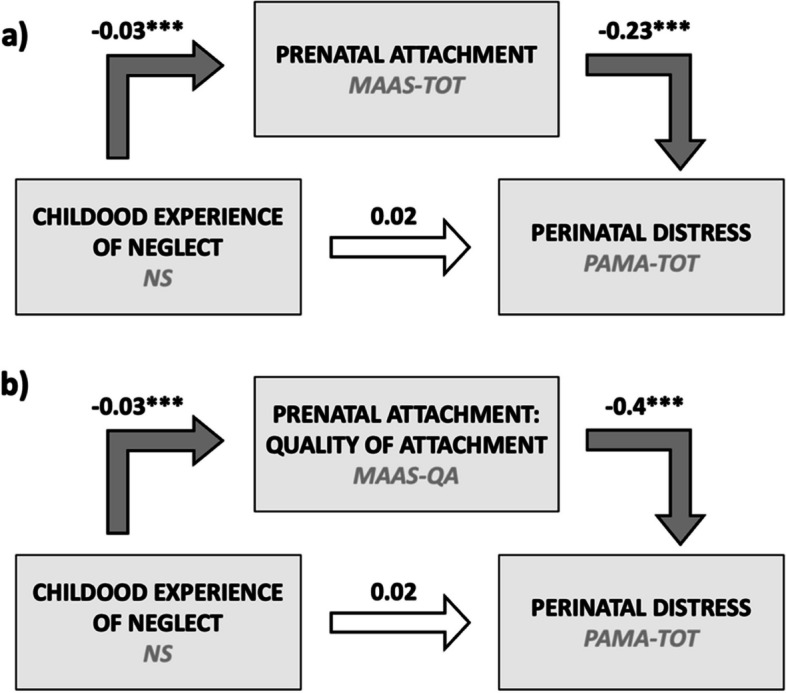
Mediating role of prenatal attachment (a: total score; b: quality of attachment) on the relationship between maternal exposure to neglect in childhood and perinatal maternal distress. Note. The solid arrows between the blocks indicate the statistical significance of the path coefficient, while the values above each arrow indicate the standardized path coefficient estimates
Discussion
This study aimed to investigate the association between experiences of childhood EA and neglect, prenatal maternal attachment, and psychological distress in a non-clinical sample of pregnant women, also testing the mediating effect of prenatal attachment in the link between childhood EA and neglect and psychological distress.
Results first showed that participants who experienced childhood maltreatment were more likely to report psychological distress during pregnancy than non-exposed participants. Regarding the association between experiences of childhood EA and neglect, and psychological distress (hypothesis 1), we found that childhood neglect, but not EA, was positively associated with increased levels of perinatal psychological distress. This finding corroborates results from previous research which observed that experiences of physical or psychological neglect during childhood represented a significant risk factor for psychological distress during the perinatal period, particularly for depressive symptoms [14, 46]. The transition to motherhood involves a process in which women tend to recall memories of care that they experienced with their own parents during childhood. When these early experiences are marked by interpersonal adversities, such as neglect by a caregiver, traumatic memories may be reactivated and prompt the onset of negative affective responses, along with the intensification of underlying feelings of vulnerability [19]. Pregnancy is a particularly sensitive period characterized by an increase of a woman’s physiological and emotional needs, such as those of care, support, and attention [44]. Pregnant women with histories of childhood neglect may expect that significant others will be unable to respond to these demands, as previous negative caregiving experiences may have conveyed a representation of others as being inherently unavailable, unreliable, and detached [70]. In turn, this belief may promote feelings of loneliness, favoring the appearance of perinatal signals of psychological distress.
Results from our study highlight that childhood neglect is negatively associated with all the prenatal attachment scores (MAAS-QA, MAAS-IC, MAAS-TOT) (hypothesis 2), suggesting that having experienced this kind of childhood adversity may have deleterious effects on a woman’s disposition to emotionally and behaviorally invest in the creation of a bond with her unborn baby. This result aligns with previous studies that found that childhood neglect [23, 66], as well as childhood maltreatment and early interpersonal trauma globally [19, 60, 62], were associated with lower maternal–fetal attachment. One possible explanation is that previous life events, particularly those occurring during childhood with one’s own caregivers, shape the acceptance of and the adaptation to the experience of motherhood. Indeed, women start to forge their novel identities as mothers during gestation, developing specific expectations regarding their ability to effectively assume and adjust to this new role [48, 65]. Women who have grown up in warm, nurturing, and supportive family environments have more opportunities to develop a positive perception of self and an adequate sense of maternal efficacy, which in turn may positively affect their emotional investment towards their babies [68]. These feelings may favor protective, sensitive, and caring mother-fetus interactions, with documented benefits for mothers’ and children’s physical and psychological well-being both during pregnancy and the postnatal period [19, 59]. Conversely, women who have lived in negligent families, in which their material and emotional needs as children were not recognized, may acquire a defective sense of self and thus perceive themselves as scarcely effective in responding to the demands of their new role, which can potentially have negative effects on their relationships with the fetus [68]. These women may also feel that they lack the emotional resources to fulfill their children’s needs, and that may cause them to experience feelings of frustration and resentment towards the baby [16].
Our results show a negative association between prenatal attachment and psychological distress, specifically that lower levels of prenatal attachment are associated with higher levels of psychological distress in mothers. This finding is consistent with previous studies showing that distress experienced by mothers can negatively affect the establishment of adequate prenatal attachment bonding and the development of appropriate parenting attitudes [5, 11], although the literature is not fully consistent [37, 51]. Indeed, some studies report increased perinatal distress in mothers with greater sensitivity to the child’s needs and richer bonding experiences [22, 43], while others point out that perceived good prenatal attachment bonding positively affects the dimensions associated with psychological well-being, such as self-care [34, 45], body self-perception [20], or self-efficacy [29]. The complexity of the scenario therefore justifies the adoption of specific, hypothesis-based statistical models, like mediation analyses. Through this analysis, we showed that prenatal attachment acts as a full mediator within the relationship between exposure to adverse events in childhood—particularly neglect—and perinatal distress. Given that prenatal attachment is negatively associated with both exposure to neglect in infancy and perinatal distress, it is conceivable that this mediation describes a potential protective role of prenatal attachment on prenatal distress from the harmful effects of exposure to childhood neglect.
Interestingly, this mediation emerged selectively with both general and quality of attachment MAAS dimensions rather than with the intensity of concerned MAAS dimension. This finding reflects the absence of an association between neglect dimensions and measures of perinatal distress in our dataset. Moreover, this finding is in line with previous work showing a stronger relationship with psychological distress dimensions for the attachment quality scale than for the worry intensity scale [42, 61, 69].
We believe that our mediation findings might have important clinical implications, especially when considered in the context of existing findings. Indeed, it should be noted that the relationship between prenatal distress and attachment has been more frequently investigated in terms of the influence of distress on attachment during pregnancy, although a full mediation of distress between childhood trauma and prenatal distress has not been found (see Berthelot et al., [11]). On the one hand, this existing literature has pointed out that prenatal distress might be a relevant proximal factor buffering the potential negative effects of childhood trauma on the parent–child relationship. On the other hand, we demonstrated that if the terms are reversed, prenatal attachment might also buffer the maladaptive effects of childhood trauma on prenatal distress, therefore potentially acting as a distal factor on the parent–child relationship. In this framework, our findings complement extant literature and point out the urgency of considering not only prenatal distress, but also prenatal attachment as relevant correlated protecting factors for postnatal psychological wellbeing of mothers and, in turn, of a secure mother–child relationship.
However, the lack of association with emotional abuse, which was consequently not investigated further in the mediation analysis, is surprising. Previous work suggested an effect of emotional abuse on prenatal attachment, albeit to a lesser degree than neglect [66], but the literature on this issue remains substantially sparse. Within this framework, our findings differentiating the effects of neglect and emotional abuse on prenatal attachment represent a point of novelty that deserves further study. Many works investigating parental adversity in childhood do not differentiate the dimensions of neglect and emotional abuse (e.g., Berthelot [11]), possibly underestimating the specific contribution of each dimension.
Limitations
Several limitations should be considered when interpreting the results of this study. First, the data were cross-sectional, so it was not possible to examine causal inferences between EA and neglect and psychological distress. Indeed, the experiences of EA and neglect and prenatal emotional distress were measured concurrently, precluding temporal conclusions. Thus, our cross-sectional mediation findings should not be interpreted in absolute causal terms, and are therefore intrinsically limited in their impact by the nature of our data and by our research design. Future research should employ a longitudinal design to elucidate how experienced EA and neglect during childhood may impact women emotional distress during pregnancy and whether our findings can be generalized to a different temporal design. Furthermore, data about women’s experiences of emotional abuse and neglect were collected retrospectively. Participants were required to recall experiences from their childhood, but the literature has demonstrated a good agreement between adverse childhood experiences and recall in adulthood [33]. Furthermore, the measures used in the present study were self-reported, which could be influenced by social desirability bias. Future research should adopt a multi-method approach, including qualitative interviews. It should be also noted that childhood trauma was assessed with two different instruments (namely, CECA Q and CTQ) across all the enrolled women. To maximize the sample size, neglect and abuse composite scores were derived based on Z-scores from both questionnaires obtained from subscales measuring overlapping constructs. These findings should therefore be replicated in larger and more consistent samples in which childhood trauma is univocally assessed with a single instrument.
Another important limitation of this study is the fact that that the literature has reported several other variables and circumstances which characterize the pregnancy period and may affect perinatal distress, psychological and physical health of future parents (e.g., social support, personal attributes, pregnancy complications, stressful life events during pregnancy, marital satisfaction, psychiatric history (for a full review, see Alipour et al., [3]). Although our study specifically focused on childhood trauma, it cannot be ruled out that these factors might intervene in the relationship between childhood trauma, prenatal attachment, and prenatal distress, for example, as potential mediators. Future studies are warranted to test this hypothesis.
As a last relevant limitation issue, it must be pointed that our sample was mainly composed of women with a low-risk status. The participants were characterized by their higher education, higher economic status, stable marital situation, and lack of any pregnancy complications. In more heterogeneous samples, variability in such socio-demographic conditions might have affected the results. Thus, on the one hand, our findings should be considered as being related mainly to low-risk samples. On the other hand, future studies could be conducted in higher vs. lower socio-demographic risk status women employing a statistical design allowing control for such heterogeneity to fully understand the generalizability of our findings.
Strengths and clinical implications
The major strength of this study is that it addresses a gap in the current literature concerning the knowledge of the clinical consequences of EA and neglect. Previous studies largely concentrated on the outcomes of sexual and physical abuse and have thus not paid attention to the specific effects of these types of maltreatment. Additionally, our study focused on a specific sample, namely, pregnant women. To our knowledge, only a few studies have specifically explored a variety of traumatic childhood experiences in pregnant women and how these experiences influence a woman’s emotional distress during pregnancy.
Our findings show that neglect represents a significant risk factor for psychological symptoms during pregnancy. For this reason, clinicians working with pregnant women should consider that routinely asking about childhood family environment could provide crucial prognostic understanding for their assessment. It is relevant to implement prevention strategies to reduce the risk of depression and other emotional symptoms in pregnant women.
Another strength of the study is the comprehensive evaluation of women’s emotional distress. In contrast to other studies that focused only on the risk of depression during pregnancy, our study examined the risk of psychological distress in pregnant women using PAMA, an instrument that is capable of assessing perinatal maternal affective disorders [4] through numerous psychological dimensions (e.g., anxiety, depressive symptoms, stress, anger, somatization). This may allow for a more extensive understanding of the general psychological distress experienced by women during pregnancy that could result in more severe psychopathological outcomes in the post-partum period. The assessment of psychological distress during pregnancy, in particular, may be crucial to preventing depression and psychopathology in the postpartum period. Indeed, several studies have found that among women with high depression scores in late pregnancy, almost half carried the symptoms with them into the postpartum period [39]. Moreover, a recent umbrella review revealed that antenatal depression is widespread, with a prevalence ranging from 15 to 65% [28].
Research has highlighted the need for more accurate information regarding specific risk factors for antenatal depression and psychological distress. With this information, we could target and prioritize healthcare expenditures more efficiently and thereby optimize preventive interventions [8, 35].
Acknowledgements
We are grateful to Dr. Antonio Maiorana and to all HCU Obstetrics and Gynecology’s medical team, ARNAS Civico Di Cristina-Benfratelli Hospital of Palermo, for contributing to data collection and to all women who took part in this research
Authors’ contributions
MRI: conception and design of the work, interpretation of data, manuscript drafting; LF and LAA: analysis and interpretation of data, critical revision of the manuscript; EB and GC: data acquisition, manuscript drafting; AM: support for data acquisition, critical revision of the manuscript; GF and FG: supervision, critical revision of the manuscript. All authors have approved the submitted version of the manuscript.
Funding
This study was supported by PRIN 2022 Initiative from the Italian Minister of Education (CUP Project: B53D23014870006), awarded to MRI and LAA, and by internal funding of the University of Palermo. The funding bodies had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 20213 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants included in the study. The study protocol has been approved by the Bioethics Committee at the University of Palermo (167/2023). Written informed consent has been obtained by each individual who took part in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aas M, Steen NE, Agartz I, Aminoff SR, Lorentzen S, Sundet K, Andreassen OA, Melle I. Is cognitive impairment following early life stress in severe mental disorders based on specific or general cognitive functioning? Psychiatry Res. 2012;198(3):495–500. 10.1016/j.psychres.2011.12.045. [DOI] [PubMed] [Google Scholar]
- 2.Alhusen JL, Hayat MJ, Gross D. A longitudinal study of maternal attachment and infant developmental outcomes. Arch Womens Ment Health. 2013;16:521–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alipour Z, Kheirabadi GR, Eslami AA, Kazemi A. Psychological profiles of risk for antenatal depression and anxiety in Iranian sociocultural context. J Educ Health Promot. 2018;7:160. 10.4103/jehp.jehp_201_17. [DOI] [PMC free article] [PubMed]
- 4.Baldoni F, Agostini F, Terrone G, Casu G, Giannotti M. A Psychometric Study of the Perinatal Assessment of Maternal Affectivity (PAMA) for the Screening of Perinatal Affective Disorders in Mothers. Healthcare. 2023;11(6):907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baltacı N, Koç E, Doğan Yüksekol Ö, Çokyeter B. The Effects of Listening to Lullabies and Self-selected Music on Distress and Maternal Attachment in Pregnant Women: A Randomized Controlled Study. Altern Ther Health Med. 2023;29(7):46–51. [PubMed] [Google Scholar]
- 6.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173. [DOI] [PubMed] [Google Scholar]
- 7.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B. 1995;57(1):289–300. [Google Scholar]
- 8.Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Depression during Pregnancy : Overview of Clinical Factors. Clin Drug Investig. 2004;24(3):157–79. 10.2165/00044011-200424030-00004. [DOI] [PubMed]
- 9.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–6. 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 10.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–90. 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 11.Berthelot N, Lemieux R, Garon-Bissonnette J, Muzik M. Prenatal Attachment, Parental Confidence, and Mental Health in Expecting Parents: The Role of Childhood Trauma. J Midwifery Womens Health. 2020;65(1):85–95. 10.1111/jmwh.13034. [DOI] [PubMed]
- 12.Bifulco A, Bernazzani O, Moran PM, Jacobs C. The childhood experience of care and abuse questionnaire (CECA.Q): Validation in a community series. Br J Clin Psychol. 2005;44(4):563–81. 10.1348/014466505X35344. [DOI] [PubMed] [Google Scholar]
- 13.Bifulco A, Brown GW, Harris TO. Childhood Experience of Care and Abuse (CECA): a retrospective interview measure. J Child Psychol Psychiatry. 1994;35(8):1419–35. 10.1111/j.1469-7610.1994.tb01284.x. [DOI] [PubMed]
- 14.Bränn E, Shen Q, Lu D. Perinatal depression and its health impact. BMJ. 2024;384. 10.1136/bmj.p2777. [DOI] [PubMed]
- 15.Briere J, Jordan CE. Childhood maltreatment, intervening variables, and adult psychological difficulties in women: an overview. Trauma Violence Abuse. 2009;10(4):375–88. 10.1177/1524838009339757. [DOI] [PubMed]
- 16.Brown RH, Eisner M, Walker S, Tomlinson M, Fearon P, Dunne MP, et al. The impact of maternal adverse childhood experiences and prenatal depressive symptoms on foetal attachment: preliminary evidence from expectant mothers across eight middle-income countries. J Affect Disord. 2021;295:612–9. 10.1016/j.jad.2021.08.066. [DOI] [PubMed] [Google Scholar]
- 17.Busonera A, Cataudella S, Lampis J, Tommasi M, Zavattini GC. Investigating validity and reliability evidence for the maternal antenatal attachment scale in a sample of Italian women. Arch Womens Ment Health. 2016;19:329–36. [DOI] [PubMed] [Google Scholar]
- 18.Button S, Thornton A, Lee S, Shakespeare J, Ayers S. Seeking help for perinatal psychological distress: A meta-synthesis of women’s experiences. Br J Gen Pract. 2017;67(663):e692–9. 10.3399/bjgp17X692549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caglayan ISC, Cicek AU, Yilmaz Y, Sahin AE. The Role of Childhood Trauma on Prenatal Attachment: A Cross-Sectional Study. J Nerv Ment Dis. 2023;211(4):281–8. [DOI] [PubMed] [Google Scholar]
- 20.Canlı A, Demirtaş B. Prenatal Attachment and the Relationship With Body Self-Perception. J Obstet Gynecol Neonatal Nurs. 2022;51(1):e1–12. 10.1016/j.jogn.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Cannella BL. Maternal-fetal attachment: an integrative review. J Adv Nurs. 2005;50(1):60–8. 10.1111/j.1365-2648.2004.03349.x. [DOI] [PubMed] [Google Scholar]
- 22.Chang HC, Chen SY, Chen CH. Predictors of Antenatal Psychosocial Stress in Taiwanese Women. J Nurs Res. 2016;24(3):193–200. 10.1097/jnr.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 23.Christie H, Talmon A, Schäfer SK, et al. The transition to parenthood following a history of childhood maltreatment: a review of the literature on prospective and new parents’ experiences. Eur J Psychotraumatol. 2017;8(sup7):1492834. 10.1080/20008198.2018.1492834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cicchetti D, Toth SL. Child Maltreatment. Annu Rev Clin Psychol. 2005;1(1):409–38. 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- 25.Condon JT. The assessment of antenatal emotional attachment: Development of a questionnaire instrument. Br J Med Psychol. 1993;66(2):167–83. 10.1111/j.2044-8341.1993.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 26.Condon JT, Corkindale C. The correlates of antenatal attachment in pregnant women. Br J Med Psychol. 1997;70(4):359–72. [DOI] [PubMed] [Google Scholar]
- 27.Cranley MS. Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res. 1981;30(5):281–4. [PubMed] [Google Scholar]
- 28.Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. 2020;20(1):173. 10.1186/s12889-020-8293-9. [DOI] [PMC free article] [PubMed]
- 29.Delavari M, Mohammad-Alizadeh-Charandabi S, Mirghafurvand M. The relationship between maternal-fetal attachment and maternal self-efficacy in Iranian women: a prospective study. J Reprod Infant Psychol. 2018;36(3):302–11. 10.1080/02646838.2018.1436753. [DOI] [PubMed] [Google Scholar]
- 30.Doan H, Zimerman A. Prenatal attachment: A developmental model. Int J Prenat Perinat Psychol Med. 2008;20(1–2):20–8. [Google Scholar]
- 31.Doan HM, Zimerman A. Conceptualizing prenatal attachment: Toward a multidimensional view. J Prenat Perinat Psychol Health. 2003;18:109–30. [Google Scholar]
- 32.Dubber S, Reck C, Müller M, Gawlik S. Postpartum bonding: the role of perinatal depression, anxiety and maternal–fetal bonding during pregnancy. Arch Womens Ment Health. 2015;18(2):187–95. 10.1007/s00737-014-0445-4. [DOI] [PubMed] [Google Scholar]
- 33.Dube SR, Anda RF, Whitfield CL, et al. Long-term consequences of childhood sexual abuse by gender of victim. Am J Prev Med. 2005;28(5):430–8. 10.1016/j.amepre.2005.01.015. [DOI] [PubMed]
- 34.Eltomy EH, Essa RM, Fathalla NF. Relationship between Maternal Fetal Attachment and Self-Care Practices among Pregnant Women. Alexandria Sci Nurs J. 2020;22(2):19–26. 10.21608/asalexu.2020.206110. [Google Scholar]
- 35.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–83. 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed]
- 36.George D, Mallery P. Spss for Windows Step by Step: a Simple Guide and Reference, 17.0 Update. 10th ed. Boston: Allyn & Bacon; 2010.
- 37.Gioia MC, Cerasa A, Muggeo VMR, et al. The relationship between maternal-fetus attachment and perceived parental bonds in pregnant women: Considering a possible mediating role of psychological distress. Front Psychol. 2023;13:1095030. 10.3389/fpsyg.2022.1095030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goecke TW, Voigt F, Faschingbauer F, et al. The association of prenatal attachment and perinatal factors with pre- and postpartum depression in first-time mothers. Arch Gynecol Obstet. 2012;286(2):309–16. 10.1007/s00404-012-2286-6. [DOI] [PubMed] [Google Scholar]
- 39.Green JM. Postnatal depression or perinatal dysphoria? Findings from a longitudinal community-based study using the Edinburgh Postnatal Depression Scale. J Reprod Infant Psychol. 1998;16(2-3):143–55.
- 40.Gross JT, Stern JA, Brett BE, Fitter MH, Cassidy J. Mothers’ attachment style predicts response to child distress: The role of maternal emotions and attributions. J Child Fam Stud. 2023;32(3):876–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hammouri HM, Sabo RT, Alsaadawi R, Kheirallah KA. Handling skewed data: A comparison of two popular methods. Appl Sci. 2020;10(18):6247. [Google Scholar]
- 42.Hart R, McMahon CA. Mood state and psychological adjustment to pregnancy. Arch Womens Ment Health. 2006;9(6):329–37. 10.1007/s00737-006-0141-0. [DOI] [PubMed] [Google Scholar]
- 43.Hsu TL, Chen CH. Stress and maternal-fetal attachment of pregnant women during their third trimester. Kaohsiung J Med Sci. 2001;17(1):36–45. [PubMed] [Google Scholar]
- 44.Infurna MR, Bevacqua E, Costanzo G, Falgares G, Giannone F. Psychosocial Risk Factors and Psychopathological Outcomes: Preliminary Findings in Italian Pregnant Women. Women. 2023;3(1):121–31. [Google Scholar]
- 45.Laxton-Kane M, Slade P. The role of maternal prenatal attachment in a woman’s experience of pregnancy and implications for the process of care. J Reprod Infant Psychol. 2002;20(4):253–66. 10.1080/0264683021000033174. [Google Scholar]
- 46.Li Y, Long Z, Cao D, Cao F. Maternal history of child maltreatment and maternal depression risk in the perinatal period: A longitudinal study. Child Abuse Negl. 2017;63:192–201. 10.1016/j.chiabu.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 47.Lindgren K. Relationships among maternal–fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health. 2001;24(3):203–17. 10.1002/nur.1023. [DOI] [PubMed] [Google Scholar]
- 48.Maas AJBM, Vreeswijk CMJM, de Cock ESA, Rijk CHAM, van Bakel HJA. ‘Expectant Parents’: Study protocol of a longitudinal study concerning prenatal (risk) factors and postnatal infant development, parenting, and parent-infant relationships. BMC Pregnancy Childbirth. 2012;12:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Main M, Hesse E. Parents’ unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? In: Greenberg MT, Cicchetti D, Cummings EM, editors. Attachment in the preschool years: Theory, research, and intervention. The University of Chicago Press; 1990. p. 161–82. [Google Scholar]
- 50.McFarland J, Salisbury AL, Battle CL, et al. Major depressive disorder during pregnancy and emotional attachment to the fetus. Arch Womens Ment Health. 2011;14(5):425–34. 10.1007/s00737-011-0237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McNamara J, Townsend ML, Herbert JS. A systemic review of maternal wellbeing and its relationship with maternal fetal attachment and early postpartum bonding. PLoS ONE. 2019;14(7): e0220032. 10.1371/journal.pone.0220032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meltzer-Brody S, Larsen JT, Petersen L, et al. Adverse life events increase risk for postpartum psychiatric episodes: A population-based epidemiologic study. Depress Anxiety. 2018;35(2):160–7. 10.1002/da.22697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moe V, Von Soest T, Fredriksen E, Olafsen KS, Smith L. The multiple determinants of maternal parenting stress 12 months after birth: The contribution of antenatal attachment style, adverse childhood experiences, and infant temperament. Front Psychol. 2018;9:1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Muzik M, Bocknek EL, Broderick A, et al. Mother-infant bonding impairment across the first six months postpartum: The primacy of psychopathology in women with childhood abuse and neglect histories. Arch Womens Ment Health. 2013;16(1):29–38. 10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Obrochta CA, Chambers C, Bandoli G. Psychological distress in pregnancy and postpartum. Women Birth. 2020;33(6):583–91. 10.1016/j.wombi.2020.01.009. [DOI] [PubMed] [Google Scholar]
- 56.Proctor LJ, Dubowitz H. Child Neglect: Challenges and Controversies. In: Korbin JE, Krugman RD, editors. Handbook of Child Maltreatment. Netherlands: Springer; 2014. p. 27–61. 10.1007/978-94-007-7208-3_2. [Google Scholar]
- 57.Rodriguez VJ, Are F, Madden A, Shaffer A, Suveg C. Intergenerational Transmission of Childhood Maltreatment Mediated by Maternal Emotion Dysregulation. J Child Fam Stud. 2021;30(8):2068–75. 10.1007/s10826-021-02020-3. [Google Scholar]
- 58.Sacchi C, Vieno A, Simonelli A. Italian validation of the Childhood Trauma Questionnaire—Short Form on a college group. Psychol Trauma. 2018;10(5):563. 10.1037/tra0000333. [DOI] [PubMed]
- 59.Şahin M, Erbil N. Relationship between maternal antenatal attachment and traumatic childbirth perception among pregnant women. Int J Gynecol Obstet. 2024;165(1):288–97. 10.1002/ijgo.15154. [DOI] [PubMed]
- 60.Sancho-Rossignol A, Schilliger Z, Cordero MI, et al. The association of maternal exposure to domestic violence during childhood with prenatal attachment, maternal-fetal heart rate, and infant behavioral regulation. Front Psychiatry. 2018;9:358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schmidt D, Seehagen S, Vocks S, et al. Predictive Importance of Antenatal Depressive Rumination and Worrying for Maternal-Foetal Attachment and Maternal Well-Being. Cogn Ther Res. 2016;40:565–76. 10.1007/s10608-016-9759-z. [Google Scholar]
- 62.Schwerdtfeger KL, Goff BS. Intergenerational transmission of trauma: exploring mother-infant prenatal attachment. J Traumatic Stress. 2007;20(1):39–51. 10.1002/jts.20179. [DOI] [PubMed] [Google Scholar]
- 63.Seimyr L, Sjögren B, Welles-Nyström B, Nissen E. Antenatal maternal depressive mood and parental–fetal attachment at the end of pregnancy. Arch Womens Ment Health. 2009;12(5):269–79. 10.1007/s00737-009-0079-0. [DOI] [PubMed] [Google Scholar]
- 64.Smorti M, Ponti L, Ghinassi S, Rapisardi G. The mother-child attachment bond before and after birth: The role of maternal perception of traumatic childbirth. Early Hum Dev. 2020;142: 104956. 10.1016/j.earlhumdev.2020.104956. [DOI] [PubMed] [Google Scholar]
- 65.Stern DN. The Motherhood Constellation: A Unified View of Parent-Infant Psychotherapy. Abington: Routledge; 1995. [Google Scholar]
- 66.Stigger RS, Martins CDSR, de Matos MB, et al. Is Maternal Exposure to Childhood Trauma Associated With Maternal-Fetal Attachment? Interpersona. 2020;14(2):200–10. [Google Scholar]
- 67.Stöckl H, Gardner F. Women’s perceptions of how pregnancy influences the context of intimate partner violence in Germany. Cult Health Sex. 2013;15(10):1206–20. 10.1080/13691058.2013.813969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Talmon A, Horovitz M, Shabat N, Haramati OS, Ginzburg K. «Neglected moms» - The implications of emotional neglect in childhood for the transition to motherhood. Child Abuse Negl. 2019;88:445–54. 10.1016/j.chiabu.2018.12.021. [DOI] [PubMed] [Google Scholar]
- 69.White O, McCorry NK, Scott-Heyes G, Dempster M, Manderson J. Maternal appraisals of risk, coping and prenatal attachment among women hospitalised with pregnancy complications. J Reprod Infant Psychol. 2008;26(2):74–85. 10.1080/02646830801918455. [Google Scholar]
- 70.Widom CS, Czaja SJ, Kozakowski SS, Chauhan P. Does adult attachment style mediate the relationship between childhood maltreatment and mental and physical health outcomes? Child Abuse Negl. 2018;76:533–45. 10.1016/j.chiabu.2017.05.002. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
No datasets were generated or analysed during the current study.


