Abstract
Background
The path of a complaint and patient satisfaction with complaint resolution is often dependent on the responses of healthcare professionals (HCPs). It is therefore important to understand the influences shaping HCP behaviour. This systematic review aimed to (1) identify the key actors, behaviours and factors influencing HCPs’ responses to complaints, and (2) apply behavioural science frameworks to classify these influences and provide recommendations for more effective complaints handling behaviours.
Methods
A systematic literature review of UK published and unpublished (so-called grey literature) studies was conducted (PROSPERO registration: CRD42022301980). Five electronic databases [Scopus, MEDLINE/Ovid, Embase, Cumulated Index to Nursing and Allied Health Literature (CINAHL) and Health Management Information Consortium (HMIC)] were searched up to September 2021. Eligibility criteria included studies reporting primary data, conducted in secondary and tertiary care, written in English and published between 2001 and 2021 (studies from primary care, mental health, forensic, paediatric or dental care services were excluded). Extracted data included study characteristics, participant quotations from qualitative studies, results from questionnaire and survey studies, case studies reported in commentaries and descriptions, and summaries of results from reports. Data were synthesized narratively using inductive thematic analysis, followed by deductive mapping to the Theoretical Domains Framework (TDF).
Results
In all, 22 articles and three reports met the inclusion criteria. A total of 8 actors, 22 behaviours and 24 influences on behaviour were found. Key factors influencing effective handling of complaints included HCPs’ knowledge of procedures, communication skills and training, available time and resources, inherent contradictions within the role, role authority, HCPs’ beliefs about their ability to handle complaints, beliefs about the value of complaints, managerial and peer support and organizational culture and emotions. Themes mapped onto nine TDF domains: knowledge, skills, environmental context and resources, social/professional role and identity, social influences, beliefs about capability, intentions and beliefs about consequences and emotions. Recommendations were generated using the Behaviour Change Wheel approach.
Conclusions
Through the application of behavioural science, we identified a wide range of individual, social/organizational and environmental influences on complaints handling. Our behavioural analysis informed recommendations for future intervention strategies, with particular emphasis on reframing and building on the positive aspects of complaints as an underutilized source of feedback at an individual and organizational level.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12961-024-01209-4.
Keywords: Patient safety, Complaints, Quality of healthcare, Behavioural response, Systematic review
Introduction
National health organizations aim to provide high-quality healthcare and promote public health and well-being while ensuring equitable access to medical services for all their residents. Patient complaints are increasingly considered as a resource to assess quality of service provision by health organizations [2–5]. Healthcare complaints are defined as grievances often attributed to errors in professional practice, or a failure within the healthcare setting or a specific service, and sometimes the source can be a combination of these factors [6]. Complaints received from patients can provide a valuable source of information about satisfaction levels and safety practices within a service or healthcare organization [7–10]. In addition to measuring patient satisfaction, mechanisms for recording patient complaints can provide information about gaps in service provision [11, 12] and organizational issues [5, 13] that might otherwise be difficult to obtain. The information obtained from monitoring patient complaints can be helpful, not only in addressing the immediate issue but also preventing them from reoccurring again [7, 14–16].
Patient complaints arise for various reasons, including being a vehicle for expressing emotional responses about care received [17, 18]. They can also arise from genuine patient–practitioner miscommunications or be an indication of a mismatch in expectations about how the healthcare service operates [19, 20]. Complaints are usually categorized as formal, defined as a written complaint raised by a patient or a carer, most often to the chief executive or the organization that requires an investigation to be carried out and a written response to be given [21], or ‘informal’, defined as instances where the complainant directly communicates their concerns to the HCP involved. If resolution is not achieved at the local level, the complaint can be escalated [21]. The categorization of a formal or informal complaint usually depends on the nature of the complaint, its severity and the way the complainant chooses to pursue the complaint [22, 23]. Whether a concern or informal complaint can be resolved without escalating to a formal complaint can also depend on how healthcare practitioners respond to the complaint in the first instance. Resolving a complaint before it escalates to the formal route is generally considered beneficial for both parties involved (for example, less stressful and time-consuming for complainants and organizations), although there may be cases where the formal resolution is necessary or unavoidable, particularly for complex or serious malpractice issues [6].
In the United Kingdom, all National Health Service (NHS) hospitals have been required to set up a complaints procedure, based on the Hospital Complaints Procedure Act 1985, with additional revisions in the following years [28]. In the last few decades, the patient complaints procedure for patients and healthcare organizations in the UK has become publicly available, along with reporting rates of complaints for transparency [29]. In 2021, a new process was announced for the management of NHS patient complaints, whereby healthcare organizations in the UK are supported by the Parliamentary and Health Service Ombudsman, to provide faster and more effective handling of patient complaints [30, 31]. In 2017, a campaign called Say Sorry was introduced to help translate patient complaints into learning and improvements in quality of care, and resolve complaints before they escalate into civil action [32]. Despite these efforts to reform policies and improve complaints management systems, public inquiries conducted after significant incidents, such as the Mid-Staffordshire Hospital trust and the review of maternity services at the Shrewsbury and Telford Hospital NHS trust from 2000 to 2019 [33, 34], have revealed persistent failings in handling complaints. Moreover, the substantial increase in clinical negligence claims over the last decade indicates patient dissatisfaction with the initial handling of concerns or complaints [35] and suggests a relatively limited implementation of these reforms to date [29, 36].
Whilst there is an extensive literature on factors influencing patients to raise a complaint about healthcare received [12, 22, 23], comparatively less research has examined how health professionals respond to complaints [41, 42]. Responding as well as handling complaints can be classified as a cluster of behaviours typically referring to the processes of receiving and responding to complaints [41], such as communicating with the complainant to gather additional information, providing an explanation or an apology or directing complaints to Patient Advice and Liaison Services (PALS). The two terms “responding to complaints” and “complaint handling” will be used interchangeably henceforth, whilst “complaint management” encompasses a broader set of activities beyond just responding, including assessing, monitoring and resolving complaints or establishing procedures and policies to facilitate the handling of complaints, although there may be variations in the way these terms are used in different organizations [27, 41]. Identifying the factors that influence the way HCPs respond to complaints and the context in which these responses occur is the first step in intervening to change ineffective practices, as these initial responses can impact the path of a complaint [36]. HCP responses and overall handling of complaints can be understood and have a greater probability of being changed using the methodologies, principles and insights offered by behavioural science. Behavioural science is an umbrella term for a selection of disciplines (such as psychology and sociology) and refers to an evidence-based understanding of human behaviour and the factors influencing behaviour in individuals, communities and populations [43–45]. Essentially, behavioural science examines how people behave, why they behave as they do and in what context. Behavioural science theories and frameworks can guide the development of more targeted, and likely effective, interventions. The WHO highlights that leveraging behavioural evidence on what influences behaviours at the individual, community and population level can improve the design of policies, programmes and services aimed at achieving better health outcomes for all [46]. A widely used behavioural framework to synthesize influences on behaviours in a number of systematic reviews (for example, [47–49]) is the Theoretical Domains Framework (TDF [50]). The TDF synthesizes constructs from 33 behaviour change theories into 14 domains representing cognitive, affective, social and environmental influences on behaviour. The TDF is a theoretical approach for analysing behaviour change in complex systems, making it particularly well suited for analysing the multifaceted nature of complaints handling behaviours in healthcare [51]. A strength of using the TDF is that it can be mapped onto comprehensive frameworks representing influences on behaviour and different types of behaviour change intervention strategies using published matrices including the Behaviour Change Wheel (BCW) [52] and the Behaviour Change Technique (BCT) Taxonomy v1 [53]. This enables more systematic identification of intervention strategies that are likely to be more relevant in addressing specific influences on behaviour, thus making recommendations more likely to be effective.
Review aims and objectives
This review aimed to apply behavioural science frameworks to identify and synthesize existing evidence on the responses of healthcare practitioners to patient complaints in a public healthcare system, specifically the NHS in the UK. Our primary focus was on responding to and handling complaints at the point of receipt, as these initial behaviours can significantly influence the trajectory of the complaint resolution process [54]. Through the application of behavioural science, we aimed to synthesize available evidence to generate recommendations for behavioural interventions addressing issues underlying poor complaint handling and thus mitigate escalation, where appropriate. The specific objectives of this study were to identify:
Actors and their behaviours that are relevant to initial responses to complaints within secondary and tertiary care;
Influences on the identified behaviours and categorize these using the TDF;
Use the BCW and BCTv1 taxonomy to propose recommendations for intervention strategies likely to target these influences to achieve behaviour change.
Methods
A systematic review was conducted of published peer-reviewed and grey literature studies, available up to September 2021. The review protocol was registered on the international Prospective Register of Systematic Reviews (PROSPERO; Registration Number CRD42022301980). Presentation of the following sections is aligned with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines for systematic reviews [55].
Search strategy and study selection criteria
The electronic databases Scopus, MEDLINE/Ovid, Embase, Cumulated Index to Nursing and Allied Health Literature (CINAHL), Health Management Information Consortium (HMIC), the Cochrane library and National Institute for Health and Care Excellence (NICE) index were searched. Search strategies for each database were designed in consultation with an information retrieval specialist based in the Evidence Synthesis Team in the Population Health Sciences Institute at [removed for peer-review] University. The strategies prioritized sensitivity to capture all studies relevant to the research aims and objectives, but a restriction on the basis of language (English), location (UK setting) or time relevance of the study (published within the last 20 years) was applied. A filter for the geographical location was also applied to enhance geographical specificity of the search [56]. A 20-year time limit was applied, with the rationale being that the health service would have changed quite substantially in the past 20 years and therefore papers older than this would be less relevant to informing our findings and current recommendations. The search strategy per database is provided in an additional file (Supplementary File 1).
Any study reporting empirical data (qualitative and/or quantitative research and systematic review articles) on a wide range of patient complaints (that is, relationship, clinical or management problems) either verbally or in writing, based in tertiary or secondary care services in the UK was included. Specifically, the criteria related to participants/population, intervention (exposure), comparison groups, outcomes, and study design [PI(E)COS] – participants/population: any type of healthcare professional; intervention (exposure): any studies examining responses to complaints; comparator(s): not applicable; outcome(s): any type of response to complaints; and study design: any. Studies from primary care, mental health, forensic, paediatric or dental care services were excluded because the types of complaints and complaints processes in these services are very different to those in secondary and tertiary care. Studies not reporting empirical data (that is, commentary articles) were also excluded.
Procedure
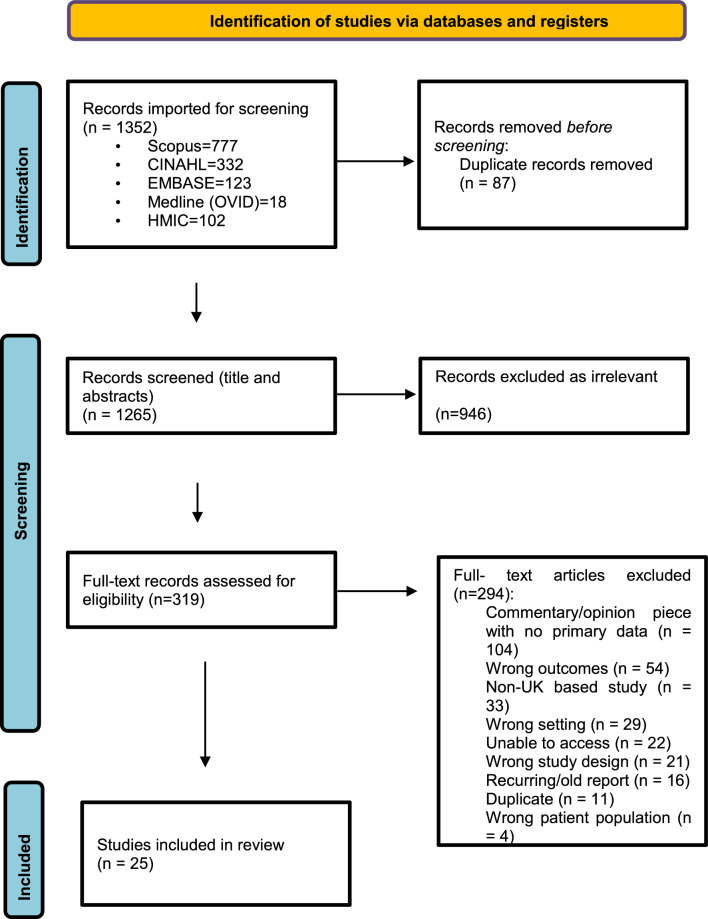
All titles and abstracts were imported and managed using Endnote version 12. We first checked and removed duplicates in Endnote, and the remaining articles were exported into the review management programme Covidence (Covidence, 2020) for screening. Articles were reviewed by four authors (P.C., V.A., C.M. and B.G.) for title and abstract screening. Double-screening was done by two authors (P.C. and V.A.) on a proportion of the retrieved articles (30%) with 97% agreement. Full-text screening of the resulting articles was undertaken by four authors (V.A., B.G., C.M. and L.G.), who double-screened each article, and resolved discrepancies together, or with an additional author (P.C.). The selection process was recorded, and the PRISMA flow diagram was completed.
Quality appraisal
One author (B.G.) individually conducted a quality appraisal of the included studies using the Mixed Methods Appraisal Tool (MMAT) [57, 58] and the Joanna Briggs Institute Critical Appraisal Checklist (JBI) [59]. Two authors (V.A. and C.M.) jointly conducted a second quality appraisal of the included articles and discussed any disagreements with B.G. As per recommendations for use, the tools were not used to score individual studies and exclude on this basis, but rather were used as a broad guide to provide a context in which to interpret findings. In addition, the priority for the review was to capture breadth of data regarding actors, behaviours and relevant influences.
Data extraction
The data extraction form was specifically developed for this review and informed by previous methods and tools [for example, the Healthcare Complaints Analysis Tool (HCAT) [25]]. The data extraction form was first piloted by author B.G. and reviewed and refined by the researchers (V.A., C.M. and B.G.). The final data extraction form included the following: (1) study characteristics (that is, title, authors, year, and setting), (2) study aims, (3) design (including measures and study population), (4) description of actors involved with the complaint (that is, healthcare practitioner, family members, and carers), (5) behaviours (for example, apologizing/not apologizing, showing active listening, and type of follow-up response), (6) behavioural influences (for example, workload and attitudes) and (7) consequences (for example, positive or negative complaint outcome). All articles were double-extracted by two groups of reviewers (V.A. and B.G.) and (C.M. and B.G.), with all three reviewers independently extracting information from the articles. Consensus meetings were regularly held to discuss discrepancies between the reviewers, and any unresolved disagreements during the main data extraction process were discussed with an additional fourth reviewer (P.C.).
Data analysis and synthesis
A narrative synthesis (Mays et al., 2005) of the findings from the included studies was conducted involving a two-stage process: an inductive thematic analysis combined with a deductive framework analysis approach [60–62]. Specifically:
Inductive thematic analysis: Three authors (V.A., C.M. and B.G.) thematically analysed the identified influences on behaviour by grouping similar data points and inductively generating themes in the final list of 25 articles. During the analysis and synthesis process, we identified actors, behaviours and influences relating to first responses of HCPs after receiving a complaint.
Deductive framework analysis: The themes were deductively mapped using the TDF [50]. The TDF was deemed most suited to our behavioural analysis, as it encompasses varying levels of behavioural influences ranging from individual through to broader social/organizational factors. V.A., C.M. and B.G. classified the themes according to the TDF domains in a Microsoft Excel spreadsheet. Consensus meetings were held to resolve disagreements. The final mapping was also reviewed by authors F.L. and A.C. Mapping the inductive codes onto the TDF framework allowed us to synthesize a vast amount of data extracted from the included papers and evidence sources and categorize these as barriers or enablers or both [63]. Following identification of barriers and enablers, we consulted published matrices linking the TDF to the intervention strategies of the BCW to generate suggestions for potential interventions to address reported barriers and enablers.
Results
Study selection and characteristics
The search results are presented in the PRISMA diagram (Fig. 1). In total, 25 studies were included, of which 18 were empirical studies with primary data, 3 were commentaries presenting case studies, 3 were government articles and 1 was a conference abstract (see Table 1 for a summary of the included studies). From the list of included studies, 14 studies contained qualitative data [26, 64–76], 7 studies included quantitative data [21, 77–82] and 4 studies included mixed methods data [83–86]. Research aims of the studies varied, including processes that practitioners followed when resolving complaints (n = 17), the psychosocial impact of patient complaints on healthcare practitioners (n = 2), identification of patient motives during the complaints process (n = 1), the ways that experienced healthcare practitioners navigated performance (n = 1), practitioner experiences of healthcare regulation practices (n = 1), language used in patient complaints (n = 1) and patient-centred processes in the complaints procedure (n = 1).
Fig. 1.
PRISMA diagram of study selection and exclusion
Table 1.
Characteristics of studies included in the systematic review
| Author/year | Study type/method | Setting | Participants |
|---|---|---|---|
| Abbott [64] | Qualitative interviews and workshop | Acute hospital, mental health, primary care (acute hospital only reported in this study) | 15 PALSa service users, 15 members of local user/carer organizations, representatives of 14 user/carer organizations (N = 44 in total) |
| Abraham [65] | Case studies, commentary | Hospital | Patients (N = 3) |
| Adams et al. [26] | Mixed methods (article reports on qualitative data only) | Hospital, community | N = 41 (eight services: emergency admissions, midwifery, older peoples’ acute medicine, in-patient haematology, adult community nursing, community matron service, intermediate care service and an adult community and palliative care nursing services) |
| Allan et al. [66] | Action research, qualitative interviews and discussion groups | Hospital | Service users (N = 5), key stakeholders in 3 NHS trusts (N = 6), midwifery and nursing reflective discussion groups (n = 6) |
| Allan et al. [67] | Action research, qualitative interviews and discussion groups | Hospital | Midwives (N = 6) |
| Balasubramaniam et al. [77] | Online quantitative survey | NHS trust | Junior doctors (N = 50) |
| Behavioural insights [83] | Surveys and interviews, government article | Not applicable | Survey: patients (N = 728), interviews: patients/past claimants (N = 20) |
| Bolton and Goldsmith [78] | Cross-sectional, quantitative survey | Hospital | Neurologists (N = 58) |
| Bourne et al. [21] | Cross-sectional, quantitative survey | Not applicable | Doctors/members of the BMA (N = 6144) |
| Bourne et al. [68] | Qualitative, analysis of open-ended responses to a cross-sectional survey | Not applicable | Doctors/members of the BMA (N = 3417) |
| Bourne et al. [79] | Cross-sectional, quantitative survey | Not applicable | Doctors/members of the BMA (N = 7926) |
| Burr [84] | Government report, mixed methods | NHS trusts | Questionnaire to NHS trusts (N = 382) and follow-up interviews with 18 NHS trusts, questionnaire to service users (N = 229) |
| Cooke [69] | Qualitative, informal interviewing and observational/documentary data | Hospital | N = 144 (total) including ward nurses, ward sisters/charge nurses, clinical nurse specialists, directorate managers, quality assurance and risk managers, human resource managers, union representatives and trust board members |
| Hutchinson et al. [85] | Mixed methods, interviews and postal survey | NHS trusts | N = 18 in total – (8 GPs, 4 psychiatrists, 3 medical regulators, 1 patient organization representative, 1 professional representative, 1 psychologist rehabilitating), 457 survey responses from NHS trusts and LMCs |
| McCreadie et al. [70] | Qualitative interviews | Hospital | Doctors (N = 59) |
| McGivern and Fischer [71] | Qualitative interviews | Not specified | N = 18 in total: patient organization representative (N = 1), medical regulators (N = 3), psychiatrists (N = 4 GPs (n = 8), psychologist (N = 1) |
| NHS [112] | Quantitative, national statistics, government report | Hospital and community | N = 117,836 (not specified) |
| Odelius et al. [72] | Mixed methods (article reporting interviews and focus groups) | Hospital | N = 11 (n = 6 midwives and n = 5 service users who had logged written complaints regarding aspects of their care or that of a family member) |
| Robinson et al. [81] | Quantitative, retrospective study of data records related to complaints | Hospital |
Complaints managers (N = 27) (n = 20 fertility services, n = 7 PCT funding-related issues) |
| Scott [73] | Case studies | Not specified | Complaints manager (N = 1) |
| Siyambalapitiya et al. [82] | Quantitative, retrospective study with analysis of computerized data related to complaints | Hospital | Hospital management (N = 85) |
| Tingle [74] | Mixed methods, survey and telephone interviews, commentary | Not specified | Patients (N = 728) |
| Treanor [86] | Qualitative survey | Hospital | Hospital management (N = 1456) |
| Xanthos [76] | Qualitative interviews | Hospital | Complaints managers (N = 21) |
| Xanthos [75] | Qualitative interviews, commentary | Hospital | Complaints managers (N = 30) |
BMA British Medical Association, GP general practitioner, LMCs local medical committees, PCT primary care trust
aPatient Advice and Liaison Service (PALS) provides a point of contact for patients and their families and can help to resolve issues and concerns and provide information and support about the complaints procedure (Robinson et al. [81])
Quality assessment of included studies
As described in the relevant section above, we used the MMAT for 21 studies to assess research quality for qualitative, quantitative and mixed methods studies. We used the JBI tool to assess quality of the four commentaries included in the review. In the quality appraisal, the qualitative studies (n = 14), as assessed with the MMAT, met all the assessment criteria. The majority of the commentary studies (n = 3) met all the assessment criteria with the exception of one study not making explicit reference to additional literature. The majority of the quantitative studies (n = 4), as assessed by the MMAT, met the assessment criteria, but it was not possible to determine the risk of nonresponse bias from the information provided in three studies, and similarly, the statistical analyses performed were not described in sufficient detail in three studies. Two of the mixed methods studies, as assessed by the MMAT, met all assessment criteria, while one study presenting NHS data did not provide additional information on the data collection methods, and another study did not provide sufficient information to assess congruence between quantitative and qualitative results. Details of the methodological quality criteria assessed within each category are provided in the Supplementary File 2.
Actors and behaviours
Resulting from the analysis, we identified eight actors and 22 behaviours (Table 2). There were four groups of actors identified: patients and carers; health practitioners such as consultants, midwives and nurses; patient liaison service (PALS) officers, including complaints managers; and organizations such as the NHS.
Table 2.
Behaviours and actors identified in the systematic review of the evidence, and indicative quotes/excerpts from studies featuring these behaviours and actors
| Behaviour | Definition | Actor(s) | Source(s) | Quotes |
|---|---|---|---|---|
| 1. Raising a concern or complaint | Expressing dissatisfaction about the care received from healthcare professionals | Patient | Allan et al. [66] | “This example had given rise to an angry informal complaint by the mother of the postnatal woman who, on overhearing that the antenatal woman’s visitor was allowed to stay, did not understand why she was unable to stay as well” (p. 12) |
| Odelius et al. [72] | “Frontline staff such as nurses and midwives are often the first to be approached) by patients or carers with concerns or informal complaints” (p. 2) | |||
| McCreadie [70] | “Accordingly, a complaint is initiated with the primary aim of preventing the same problem re-occuring while seeking accountability” (p. 8) | |||
| 2. Stops pursuing complaint | Deciding to not take the complaint further | Patient | Treanor [86] | “Following the hospital’s response, I chose not to continue as I felt it was not taken seriously” (p. 25) |
| Xanthos [75] | “Patients are still left feeling very vulnerable and, at the end of the day, they haven’t got the answers or the explanations that they require. I think a lot of people don’t pursue them because they think ‘it’s getting me nowhere’, and it’s just a long complicated process that is going to cause more stress and upset for them. The patients don’t get a very good deal” (p. 15) | |||
| 3. Escalates complaint/makes repeated complaints | Taking the complaint further to ensure action will be taken | Patient/patient representative | Abraham [65] | “Requested an independent review (IR) of the complaint” (case 2; p. 352) |
| Adams [26] | “Well, it wasn’t the best [1] … so we can all learn from that one … but it’s the way he did it [complained] … why would he do it like that [go to the Head of Department] and not come to us? That’s the thing that really threw us all … and now we all think that it’s about how they felt about us really … that’s the really difficult thing” (p. 609) | |||
| 4. Active listening and understanding, validating the patients’ perspective | Giving attention to what the patient is saying and understanding and acknowledging their point of view | Midwives | Odelius [72] | “Participants nonetheless saw most complaints they had come across as justified and understandable” (p. 9) |
| Patient And Liaison Service (PALS)a | Abbott [64] | “I think I just wanted somebody to confirm to me that I wasn’t going mad. And that is what she did.” (p. 131) | ||
| Healthcare professionals (HCPs) | Adams [26] | “‘Complaints should give you an indication of how things are going … like what we should be addressing and can’t see for ourselves …’ (eau:int.2)” (p. 609) | ||
| 5. Dealing with aggressive comments/de-escalation | Dealing with angry patients by using de-escalation skills to defuse the situation |
Nurses (midwifes) Nurses |
Odelius et al. [72] Cooke [69] |
“7I find an aggressive person difficult, that’s something we all find difficult, which probably reflects that we don’t have a lot of skills given to us doing that [previous] training, to deal with that sort of thing’ (Midwife 7)” (p. 9) “We had an angry relative – he complained about everything. […]. I was called to answer him and he came on to the ward aggressive, shouting, squared up to me. I felt intimidated and threatened. I got no response from the complaints manager.” (Ward sister/charge nurse HC26) (p. 159) |
| 6. Responding to/resolving complaint | Showing acknowledgement and replying to patients who are dissatisfied with their care | Midwives | Allan [66] | “This results in an informal or formal complaint that is difficult for staff to untangle and address.” (p. 2110) |
| HCPs (general) | Burr [84] | “Our survey found that 59 per cent of people who made a formal complaint considered that it had been received in an open and constructive manner. Over a third (36 per cent), however, considered that their complaint had not been received in an open and constructive manner and five per cent did not know” (p. 23) | ||
| Complaints manager | McCreadie [70] |
“Although X acted with the best of intentions I am sorry for the upset you experienced [3934] “In short, the complaint-responder ascribes a moral incentive to the actions of the staff involved, thereby effectively closing down further criticism” (p. 5) |
||
| Odelius [72] | “As a result of receiving your letter we are reviewing Health Visitor training in relation to infants presenting with symptoms of acute illness, staff will learn from this event” (p. 6) | |||
| PALS | Abbott [64] | “Most PALS users spoke appreciatively of the fast response that they had received. What’s good, I think, is the instant response you get. At least within 24 h. That is fantastic. (SU, PALS: acute hospital)” (p. 131) | ||
| NHS trust | Robinson [81] | “Out of 27 complaints, 26 were resolved at Trust level. None were referred to the PHSO in this time period compared with three throughout the rest of the trust” (p. 47) | ||
| Chief executive | Cooke [69] | “Chief executives read all complaints letters and detailed attention was given to complaints at the Trust board meetings which I observed. ‘I see every complaint and sign all replies …’” (p. 14) | ||
| 7. Apologizing/not apologizing to complainant | Expressing regret on behalf of the healthcare professional, or system, that caused the patient to complain | HCPs (general) | Burr [84] | “In its first Spotlight on Complaints report, the Healthcare Commission stated that one of the frequent problems in the way that complaints are handled locally is the failure to apologize, even when shortcomings have been identified. It also reported that obtaining an apology was cited as the desired outcome for ten per cent of complainants amongst 10,950 completed independent reviews” (p. 8) |
| Treanor [86] | “They neither acknowledged nor apologized for the suffering they inflicted on my husband and the anguish to me for seeing him suffer and losing him prematurely” (p. 27) | |||
| Complaints manager | Xanthos [76] | “One complaints manager reported staff resistance to incorporating an apology into the ‘acknowledgement letter’ to complainants. She, personally, felt strongly that the letter should include an apology, and insisted on its inclusion, despite staff objections” (p. 9) | ||
| NHS trust | Abraham [65] | “The trust apologised and agreed to remind all staff of the importance of keeping relatives and carers fully informed” (p. 352) | ||
| Behavioural insights [83] | “Explanations or apologies were deemed to be rare or insufficient when they were given” (p. 19) | |||
| Robinson [81] | “Out of 27 complaints, 18 (67%) were settled with an apology alone.” (p. 47) | |||
| Tingle [74] | “Money is not the main driver or motivator to sue, it is more the quest for a reasoned explanation and apology” (p. 1339) | |||
| 8. Avoiding/delaying response to complaint | Preventing oneself from dealing with the complaint or deciding to respond later than would be typically expected | HCPs- Junior staff | Allan [66] | “The junior staff actually encourage patients to go to PALS and I’m like ‘no’. (Senior ward manager)” (p. 2111) |
| Complaints manager | Scott [73] | “He was stunned by having to wait weeks for a reply that said there was nothing wrong with David’s care” (p. 44) | ||
| PALS | Treanor [86] | “‘My complaint was ignored three times by PALS.’ And a third pointed out: ‘Unless someone tells you who to contact, there is nowhere to go’” (p. 26) | ||
| NHS trust | Abraham [65] | “Mr B did not receive a reply to his complaint to the trust for almost 10 months and he waited for over a year to receive a reply to his request for an IR [independent review]” (p.352) | ||
| GMC | Bourne [68] | “Nevertheless the GMC took an inordinate amount of time to deal with the complaint and provided no feedback whatsoever while their internal processes were continuing” (p.3) | ||
| 9. Dismissing patient complaints | Dismissing the patients’ reasons for making a complaint | Consultant | Bolton [78] | “Many respondents described an ‘inevitability’ and a ‘lack of surprise’ at receiving complaints from patients with functional neurological disorders.” (p. 4) |
| HCPs (general) | Adams [26] | “Half the patients that we see, we make a massive difference to their health. We stop them arresting. And it’s not being dramatic, we really do and half the patients are oblivious to what you’ve done and they’re more bothered about, ‘they haven’t even offered me a bloody cup of tea for five hours …’ and you think, ‘oh, my God, if only you knew’” (p. 614) | ||
| Doctor | Treanor [86] | “The outcome of the complaint was upsetting as I know the doctor lied. He told my husband he had cancer by letter but the response said he didn’t” (p.26) | ||
| 10. Accepting/not accepting complainant’s point of view | The act of perceiving a situation or understanding a concept from the patients’ perspective |
HCPs (general) Complaints Managers |
Adams [26] Xanthos [75] |
“Other staff in hospital and community services described their work as ‘fielding’ and ‘diffusing’, ‘just apologising and finding it [the apology] easy to say’ and ‘letting [complainants] get it out of their system’. This ‘listening’ work, as described by several interviewees, often involved simply accepting the version of events given by complainants” (p. 616) “Respondents rarely mentioned accepting the complainant’s point of view”; “‘This is what our staff are saying, and we are sorry if you are saying something different’ – but we have to represent our staff as well as the patient – we work for the hospital” (p. 14) |
| Bolton [78] | “Respondents described cases in which patients appeared manipulative, repeatedly complaining despite input from senior managers on a regular basis.” (p. 4) | |||
| 11. Providing explanation to patients or updates throughout the process | Informing patients about the reasons why the standard of care was unsatisfactory or about the progress of their complaint throughout the process | HCPs (general) | Siyambalapitiya [82] | “A total of 99% of patients were satisfied with an explanation or apology provided, but one complaint went to litigation.” (p. 108) |
| Tingle [111] | “Almost two thirds (63%) of survey respondents felt that no explanation was given to them.” (p. 1339) | |||
| Complaints managers | Treanor [86] | “The complaint manager was excellent. Showing compassion and remaining in regular touch. I really felt supported.” (p. 26) | ||
| 12. Seeking help from other staff/managers | Requesting help from others to allow oneself to perform a task more easily | Midwives | Allan [67] |
“Midwives referred to calling the security team to support them in dealing with aggressive behaviour. Bella: If you decide this is a potentially really aggressive person who could cause harm to staff or whatever then it’s, then you just get the security in” (p. 13) “…very nervous about doing that. I was young – I put consultants and doctors up on a pedestal – I thought, ‘this is awful – I can’t do it.’” (p. 13) |
| Nurses | Cooke [69] | “I felt intimidated and threatened. I got no response from the complaints manager” (p. 17) | ||
| Complaints Manager | Xanthos [76] | “If it was a complaint about the attitude of one of the consulting staff, I would definitely go to the Medical Director. I would not confront them at all. Attitude and communication issues I find are the touchiest complaints to discuss … when I was first here … I would go and speak to staff about it directly. If you put yourself in my shoes, they had this young girl coming to talk to them about their attitude – and I would be pissed off with someone doing that to me. I just became very nervous about doing that. I was young – I put consultants and doctors up on a pedestal – I thought, ‘this is awful – I can’t do it.’” (p. 8) | ||
| 13. Defensive practice | Deviating from good practice for the purpose of protecting oneself from complaints or criticism. For example, overtreatment; ordering tests and procedures rather than diagnosing the patient | HCPs (general) | Bourne [21] |
“Avoidance behaviour (eg, abandoning procedures early) was more common when negative process or behavioural issues were reported ” (p. 8) “….psychological morbidity increased when complaints were associated with a dysfunctional team, whistleblowing and bullying. Conversely, evidence of good process such as being kept well-informed and accurate minute taking was associated with improved psychological welfare and less defensive practice. […]” |
| Consultants | Bourne [79] | “84.7% of doctors with a recent and 79.9% with a past complaint reported changing the way they practised medicine as a result of the complaint; 72.7% of doctors with no previous complaint reported changing their practise after having observed a colleague’s experience of a complaint” (p. 6) | ||
| 14. Defensive behaviour/attitude | Showing a lack of care or feeling for others who have received a complaint | HCPs (general) | Burr [84] | “In our interviews with complaints managers and chief executives, who recognized that the attitude of operational staff towards complaints could sometimes be defensive” (p. 24) |
| Complaints Managers | Xanthos [3] |
One complaints manager commented: “… There’s still a couple [of consultants] who are defensive and do bury their head in the sand – and I have terrible trouble actually getting a response out of them.” (Complaints Manager) |
||
| 15. Lack of sympathy to complained about staff | Showing a lack of care or feeling for others who have received a complaint | Complaints managers | Cooke [69] | “Complaints brought nurses under unprecedented and often unsympathetic scrutiny” (p. 16) |
| Ward manager | “There was a man on the ward who was quite poorly, his family were anxious, accused staff of not washing him. It was documented, it had been done, I’d done it myself. They ended up going to the manager’s office, she came down and marched past me – ‘I’ll speak to you later’ she said. She was quite aggressive really – I explained the abuse we’d had from the family, there’s a sign on the wall about the Trust not tolerating abuse of staff but I was told ‘Tough, you’ve got to put up with it’” (p. 18) | |||
| 16. Being more attentive to angry complainants | Paying more attention to patients who are displaying angry behaviour compared to those who are not displaying anger | Nurses | Cooke [69] | “Nurses also felt that the pressure to prevent complaints forced them to prioritise by decibels and that this compromised their own professional judgement. The patient or, more often, relative who ‘shouted the loudest’ got the most attention” (p. 17) |
| 17. Showing support to other staff | The act of helping other colleagues to perform in their job and protecting each other from complaints and criticism | Medical director, doctors | Hutchinson [85] | “A medical director discussed the difficulties of reporting colleagues and the perception of ‘whistle-blowing’ and a DPH suggested that ‘it’s almost impossible to make a complaint against a doctor’. One respondent demonstrated defensiveness: ‘it’s us against the world and we close ranks to protect each other’” (p. 48) |
| 18. Denial/denying responsibility | Refusing to accept that one’s actions resulted in the patient to make a complaint | Complaints manager | Scott [73] | “He was stunned by having to wait weeks for a reply that said there was nothing wrong with David’s care” (p. 22) |
| Treanor [86] | “They [the hospital] considered it closed, the answer was that no person was found to take responsibility” (p. 25) | |||
| 19. Reluctance to provide feedback to senior staff about poor complaint handling | Showing unwillingness to advise staff at a higher hierarchical level to change their practice | Complaints manager | Xanthos [75] | “How do you go to a 60-year-old consultant and say, ‘I think you ought to go on a customer care course’? You may be quite a young manager – a lot of managers are” (p. 14) |
| Xanthos [76] | “If you put yourself in my shoes, they had this young girl coming to talk to them about their attitude – and I would be pissed off with someone doing that to me. I just became very nervous about doing that. I was young – I put consultants and doctors up on a pedestal – I thought, ‘this is awful – I can’t do it’” | |||
| 20. Asking for an independent investigation | Attempting to obtain information about the complaint independently of the trust | Complaints managers | Xanthos [76] | “I’ve had a couple of differences with say the Director of Nursing … a couple of times when I’ve said, ‘I think this ought to go out for an independent investigation to whoever’, and she’s disagreed with me and overruled me – but that’s OK – it happens. There was one particular one I was very concerned about – I wasn’t happy at all – and I said to the Director of Nursing … ‘I would like an independent report from such and such a person.’ She said, ‘no, I don’t think we need to do that …’” |
| 21. Assessing patient needs and expectations from complaints | Consulting patients to understand the nature of the complaint and how they wish to resolve the complaint | NHS trust |
Burr [84] Robinson [81] |
“Seventy per cent of trusts consulted complainants in the early stages of the complaints process to establish the reasons for their complaint and 62 per cent of trusts consulted complainants to establish the kind of resolution they were seeking. Around a third of trusts therefore dealt with complaints without assessing the expectations of complainants” (p. 26) “Eight complainants requested funding for treatment as part of their settlement but only one was offered funding” (p. 47) |
| 22. Audit/review of policy | NHS trust | Robinson [81] | “A further 8 (30%) were resolved with an apology and audit or review of policy; for example, following a complaint regarding waiting times in clinic it was agreed that such an audit would be carried out” (p. 47) |
Thematic analysis
Ten themes were identified from the data relating to responses to complaints: (1) knowledge of complaints procedures and training, (2) interpersonal skills, (3) concerns about time and resources, (4) inherent contradictions within the role, (5) role authority. (6) beliefs about ability to handle complaints, (7) beliefs about the value/consequences of complaints, (8) managerial and peer support, (9) organizational culture and leadership, and (10) negative emotions. The themes accompanied by a summary description, relevant actors and corresponding mapping to TDF domains, the sources (that is, studies) and supporting quotes are presented in Table 3.
Table 3.
Summary of themes, description of each theme and relevant actors and corresponding TDF domains, and categorized as barrier, enabler or both
| Theme | Summary description of theme and relevant actors | TDF domains and definitions | Barrier, enabler or mixed | Sources | Example quote(s)/ Excerpt(s) |
|---|---|---|---|---|---|
| 1. Knowledge of complaints procedures and training |
Having up-to-date knowledge and training about formal and informal complaints procedures Actors: HCPs, complaints managers, PALS officers |
Knowledge (An awareness of the existence of something) Skills (An ability or proficiency acquired through practice) |
Barrier |
Allan et al., [66] Balasubramaniam et al., [77] NHS Digital: Data on written complaints in the NHS [112] Odelius et al., [72] Scott [73] |
“Some staff seem unaware of the mechanisms for resolving informal and formal complaints” (Allan et al., [66], p. 2111) “Only 15 (30%) had any training in handling the complaints. This was even less among overseas graduates, only four (15%) had any training.” (Balasubramaniam et al., [77], p. 28) |
| 2. Interpersonal skills |
Having appropriate cognitive and communication skills in complaints handling Actors: HCPs, complaints managers, PALS officers |
Skills (An ability or proficiency acquired through practice) |
Mixed |
Abbott et al., [64] Abraham [65] Allan et al., [66] Allan et al., [67] BIT report [83] Burr [84] Hutchinson [85] Odelius et al., [72] Robinson et al., [81] Scott [73] Siyambalapitiya et al., [82] Tingle [74] Treanor [86] |
“[…] 99% of patients were satisfied with an explanation and an apology indicating that almost all have been due to a lack of good communication than due to real deficiencies in the clinical care.” (Siyambalapitiya et al., [82], p. 109) “The development of interpersonal skills will help staff establish and maintain effective relationships with patients and their carers, and understand complainants’ behaviour, rather than make unconscious assumptions about it.” (Scott, [73], p. 23) |
| 3. Concerns about time and resources |
Lack of time and resources to handle complaints appropriately, overlapping tasks and responsibilities Actors: HCPs, PALS officers, complaints managers |
Environmental context/resources (Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence and adaptive behaviour) |
Barrier |
Abbott et al., [64] Adams et al., [26] Allan et al., [67] Treanor, [86] Burr [84] |
“You’ve got to have time and we just sometimes, if you have to weigh up between doing that and giving care to a woman, it’s clearly quite right you go with the giving clinical care, that’s a constant balance that you’ve always got, how much time do I give to both? (SG 25/06/12)” (Allan et al., [67], p. 23) “There are so many people doing the same job now, just slightly overlapping with the next one. People do get very confused as to exactly what we are there for.” (Community Organization Representative, older people, PALS; Abbott et al., [64], p. 134) |
| 4. Inherent contradictions within the role |
Duties and responsibilities of role entails inherent contradictions when handling complaints Actors: PALS officers, complaints managers |
Social/professional role and identity (A coherent set of behaviours and displayed personal qualities of an individual in a social or work setting) |
Barrier |
Abbott et al., [64] Xanthos [75] Xanthos [76] |
“In this situation, complaints managers are confronted with significant dilemmas in that they are coordinating complaints investigations while being a member of the organisation complained about.” (Xanthos [76], p. 10) “You are complaining in the hospital to another person in the hospital. It might not be as confidential as you think. (SU, PALS: acute hospital)” (Abbott et al., [64], p. 133) |
| 5. Role authority |
Role divisions and power dynamics between clinical and non-clinical staff undermine authority Actors: HCPs, PALS officers, complaints managers |
Social/professional role and identity (A coherent set of behaviours and displayed personal qualities of an individual in a social or work setting) Social influences (Those interpersonal processes that can cause individuals to change their thoughts, feelings or behaviours) |
Barrier |
Burr [84] Xanthos [75] Xanthos [76] |
“I don’t have direct line authority over any department or members of staff – all I can do is point out the area/make the manager aware of the problem … there are occasions when you feel that a manager is not really going to tackle a particular problem, or a clinical director is not really going to tackle the problem.” (Xanthos [75], p. 14) “The relationship with the chief executive on complaints handling does, however, vary. Just 12 per cent of chief executives maintained regular dialogue with complaints managers as a way of ensuring action had been taken on complaints, and just five per cent reported that serious complaints were escalated to senior management as a way of ensuring action was taken” (Burr [84], p. 24) |
| 6. Beliefs about ability to handle complaints |
Variability in confidence levels for handling complaints and intention to engage in complaint handling Actors: HCPs |
Beliefs about capabilities (Acceptance of the truth, reality or validity about an ability, talent or facility that a person can put to constructive use) Intentions (A conscious decision to perform a behaviour or a resolve to act in a certain way) |
Mixed |
Allan et al., [66] Allan et al., [67] Odelius et al., [72] Scott [73] |
“And I think I’m pretty good at handling a complaint you know, if someone comes up to me and they are aggressive I can diffuse it and I know others that will actually add fuel to that fire. They will make that situation worse. (Ward nurse)” (Allan et al., [66], p. 2110) “For Ruth, the solution is to manage expectations rather than change the system to avoid complaints: ‘Ruth: It’s managing their expectations isn’t it…hopefully it stops them from making those informal complaints…we know it’s a problem all the time’ (SG17/05/12)” (Allan et al., [67], p.24) |
| 7. Beliefs about the value/consequences of complaints |
Variability in the beliefs about the value complaints in improving patient care/beliefs about negative consequences Actors: HCPs, complaints managers |
Beliefs about consequences (Acceptance of the truth, reality or validity about outcomes of a behaviour in a given situation) |
Mixed |
Adams et al., [26] Bolton & Goldsmith, [78] Bourne [79] Bourne [68] McCreaddie et al., [70] Odelius [72] Scott [73] Xanthos, [75] |
“Participants nonetheless saw most complaints they had come across as justified and understandable” (Odelius et al., [72], p. 9) “Fauxpology imputes the cause of distress to the subjective (and possibly misguided) impressions of the complainant, implying that their feelings do not align with the facts, and in this way evades blame or responsibility for the complainable action” (McCreaddie et al. [70], p. 8) “You get the people who are frankly out for money! And we get quite a lot of those actually, proportionally.” (complaints manager; [75], p. 15) |
| 8. Managerial and peer support |
Varying levels of support provided by managers and colleagues to those receiving complaints Actors: HCPs |
Social influences (Those interpersonal processes that can cause individuals to change their thoughts, feelings or behaviours) |
Mixed |
Abbott, [64] Odelius et al., [72] Bourne et al. [68] Bourne et al. [21] Burr [84] Cooke [69] Hutchinson[85] McGivern & Fischer, [71] Scott [73] |
“Nurse also felt that they were often left to deal alone with irate members of the public in the absence of management support and often under conditions of extreme pressure” (Cooke [69], p. 17) “[…] it’s sort of, sort of re-affirmed that fact that I think in some situations where you’re dealing with [aggression], you don’t get the support from colleagues that you might wish that you had and that’s, maybe that’s come to light a bit, when we’ve been looking at this” (Midwife). (Odelius et al. [72], p. 9) |
| 9. Organizational culture and leadership |
Leadership and culture in organizations driving staff complaints’ handling approaches Actors: HCPs, PALS officers, complaints managers |
Social influences (Those interpersonal processes that can cause individuals to change their thoughts, feelings or behaviours) |
Mixed |
Abbott, [64] Abraham [65] Burr [84] Cooke [69] Hutchinson [85] McGivern & Fischer, [71] Tingle [74] Treanor [86] |
“The majority of complaints managers (56 per cent) and chief executives (51 per cent) consider that overall there is an open and fair culture of complaints handling within their trust. A significant proportion of complaints managers (40 per cent) and chief executives (46 per cent), however, felt that pockets existed where there was a tendency towards a blaming and closed culture” (Burr, [84], p. 24) “However, a trust medical director suggested that the culture was slowly changing and doctors were more able to accept reporting poor practice as a professional responsibility” ([85], p. 48) |
| 10. Negative emotions: stress and anxiety, frustration and fear |
Stress and anxiety, frustration and fear of legal consequences experienced by those receiving a complaint Actors: HCPs, PALS officers, complaints managers |
Emotions (A complex reaction pattern, involving experiential, behavioural and physiological elements, by which the individual attempts to deal with a personally significant matter or event) |
Barrier |
Allan et al. [66] Allan et al. [67] Adams et al. [26] Bolton & Goldsmith, [78] Bourne et al. [79] Bourne et al. [68] Bourne et al. [21] Cooke, [69] Burr [84] McGivern & Fischer, [71] Scott [73] Treanor [86] Xanthos [75] |
“Nurses were fearful of complaints. Many felt that any complaint, however unreasonable, would expose them to criticism by managers. Thus complaints frequently made them feel that they were being attacked on all sides.” (Cooke [69], p.161) “And it’s tiring and stressful because you want to be giving care to patients and sometimes all you’re doing is fighting fires and apologising.” (Allan [67], p. 21) “The complaints procedure is a big pressure. People complain about things people wouldn’t have complained about before. I am strict about visiting, I see stressed out staff nurses, visitors demanding attention – moither, moither – they can’t see the staff nurse is pushed already, they want attention now. When you’re out there, you’re on a stage; because of litigation we’re all aware of it; trying to keep three steps in front” ([69], p. 18) |
Bold letters were used to visually highlight the themes and the TDF domains in the table among all other information
Influences on behaviour: behavioural analysis using the TDF
Theme 1: knowledge of complaints’ procedures and training
TDF domain: knowledge, skills
It was recognized that all HCPs needed to know the established complaints procedures to effectively respond to patients’ complaints (NHS Digital: Data on written complaints in the NHS, [112]; Scott [73]). However, knowledge of the appropriate mechanisms for resolving formal or informal complaints, and up-to-date knowledge about how to deal with complaints was highlighted as an issue (Odelius et al. [72]). Knowledge of procedures was found to be low in ward managers and reported as a barrier:
Reflective Discussion (RD) groups, service user and stakeholder interviews showed that some staff seem unaware of the mechanisms for resolving informal and formal complaints (Allan et al. [66], p. 2111).
It was reported that a high proportion of HCPs, particularly those early in their career, had not received the necessary training to deal with complaints as part of their professional education and training (Balasubramaniam et al. [77]). Lack of adequate training, for example, dealing with aggression and de-escalation skills, was particularly a problem when patients and relatives displayed aggressive behaviour (Odelius et al. [72]). In addition, lack of assessment of the staff training needs about how to respond to complaints within their organization was also highlighted as an issue by ward staff:
Staff members have not been asked for their training needs around responding to informal and formal complaints. (Allan et al., [66], p. 2111).
Theme 2: interpersonal skills
TDF domains: skills, social/professional role and identity
Cognitive and interpersonal skills, particularly communication skills, were one of the most commonly reported themes among the included studies reflecting their integral role in complaints handling (for example, [65, 73, 74, 81, 86]). HCPs’ ability to communicate well with patients and their families was an enabler to deal with complaints effectively. In one of the papers, good communication was highlighted as the single most important factor leading to complaints resolution (Siyambalapitiya et al. [82]). In a report produced for the government, the complaints process was seen to be “opaque, impersonal and lacked compassion for some” [83]. Importantly, the report noted that from the patients’ perspective staff reactions fell below the standards expected, as described in the following excerpt:
Explanations or apologies were deemed to be rare or insufficient when they were given. Several interviewees remarked that, had these initial processes been handled better, they may not have pursued their claim (Behavioural Insights Team Report, [83], p. 19).
Theme 3: concerns about time and resources
TDF domain: environmental context and resources
A number of environmental factors and concerns about resources (for example, lack of time and staff shortages) were cited by healthcare personnel as issues that have a negative impact on competing job demands, role uncertainty, time and availability for dealing with complaints, as illustrated in the following quote:
[…] staff described the time-consuming work of negotiation over available resources in order to prevent patients from formalising a complaint that took “time away from other patients”. (Adams et al., p. 617).
In relation to PALS in particular, it was reported that, although PALS was set up to support the more vulnerable and “hard-to-reach” population groups, some PALS officers expressed the concern that the specific resources needed for this service to function well had not been released. Lack of adequate resources such as job posts that need to be covered and time management issues, particularly as complex cases require more time for effective management, put staff in PALS under pressure to perform different roles at work, as illustrated in the quote below:
The workshop participants were concerned that PALS were being expected to do too much. There was a suspicion that such a catch-all service has been set up to fail. (Workshop participants, Hospital setting) (Abbott et al. [64], p. 134).
Overlapping responsibilities among staff or lack of clarity about what is expected at work due to overlapping responsibilities and combined concerns about time and resources, were frequently found to be barriers to effective complaints handling. Lack of role clarity and responsibilities were cited as causing confusion to both HCPs and also to patients about who is responsible for handling complaints, as pointed out in this quote:
There are so many people doing the same job now, just slightly overlapping with the next one. People do get very confused as to exactly what we are there for. (Community Organization Representative, older people, PALS) (Abbott et al. [64], p. 134).
In addition, it was reported that a high number of organizations had complaints procedures that did not involve an assessment of the complainants’ expectations when making a complaint, although assessing expectations was a critical factor in resolving complaints satisfactorily, as highlighted in this excerpt:
Whilst direct early contact with the complainant is one of the most important factors in resolving complaints satisfactorily, one third of trusts deal with complaints without assessing the expectations of the complainants. (Burr [84], p. 8).
Theme 4: inherent contradictions within the role
TDF domain: social/professional role and identity
Data from complaints manager interviews and PALS officers indicated that there was an inherent contradiction in their role in terms of investigating complaints, whilst being an employee of the complained-about organization. Complaints managers oversee the complaints management and resolution process. They investigate and address complaints from patients or their caregivers regarding any aspect of their healthcare experience, and if appropriate, liaising with or referring patients to PALS. PALS are the point-of-contact in the hospital setting to provide information and advice to patients about the complaints procedure, resolve informal concerns and receive complaints [41]. Formal or informal complaints that PALS cannot resolve are addressed by the complaint management team in the hospital [81]. Professionals in these roles, such as complaints managers and PALS officers, articulated role conflict arising from acknowledging that staff are working hard with limited resources (Abbott et al. [64]), whilst understanding the patient’s point of view during the complaints process [75]. These inherent conflicts are critical to the initial response behaviour in complaints management, as they create internal tensions and pressures:
Actually there is friction from both sides – I always say you are the “meat in the sandwich”. You receive the complaint and obviously you’ve got to go to the person who has been complained about, or the department that has been complained about – and here’s a department that have been working very, very hard, under very difficult circumstances, with limited resources, feeling they are doing the very best they can – and someone’s complained, you know, and obviously they get defensive – so obviously you have to take the right approach when you deal with the staff too. (Xanthos, [75], p. 14).
Theme 5: role authority
TDF domains: social/professional role and identity, social influences
Role divisions and power dynamics between those not having a clinical role versus those having a clinical role often put complaints managers (especially younger complaints managers) in a position of lacking the authority to advise clinical staff at a high level within the organization. Thus, complaints managers tended to avoid advising or confronting clinical staff, particularly those in senior clinical roles, about issues raised in complaints:
How do you go to a 60-year-old consultant and say, “I think you ought to go on a customer care course”? You may be quite a young manager – a lot of managers are. (Complaints Manager) (Xanthos, [75], p. 14).
The highly hierarchical structures within the organization, and the division between those in non-clinical roles versus those in clinical roles who viewed complaints as a low priority task when busy with clinical duties, contributed to organizational marginalization and separateness of complaints management as described in the following excerpt:
Respondents offered a range of reasons for this, including the bureaucracy of the NHS, a lack of resources, local trust policy, difficulties emanating from the fact that complaints managers were generally not part of any directorate or department, and the relatively low status of most complaints managers in NHS organisations (Xanthos, [75], p. 14).
It was also reported that complaints managers often had differences of opinion with senior clinical management, for example, the director of nursing and the medical director on handling particular complaints, with ultimate decision-making authority typically resting with senior clinical management. The following quote highlights these dynamics:
… I’ve had a couple of differences with say the Director of Nursing … a couple of times when I’ve said, “I think this ought to go out for an independent investigation to whoever”, and she’s disagreed with me and overruled me – but that’s OK – it happens. (Xanthos, [76], p. 31).
Theme 6: beliefs about ability to handle complaints
TDF domains: beliefs about capabilities, intentions
HCPs varied in their level of confidence to handle complaints effectively. It was reported that a high majority of junior doctors as well as some more experienced professionals reported low confidence levels when it came to dealing with complaints (Allan et al. [66]). Previous experience in complaint handling, as well as the complexity of the issue or not being directly involved in the event leading to the complaints, made staff reluctant or unsure about their ability to resolve issues (Allan et al. [67]), and this increased referrals to services such as PALS:
I don’t know why … whether that’s our age and we’re older now in a job and we know what it’s like to research, to pull someone’s notes and have a look, see who the nurse was, see what happened (Senior ward manager) (Odelius et al. [72], p. 14).
In contrast, having confidence in their ability to deal with complaints made staff more willing to actively deal with complaints rather than referring to PALS:
The junior staff actually encourage patients to go to PALS and I’m like “no”. (Nursing focus group) (Allan et al. [66], p. 2111).
Theme 7: beliefs about the value/consequences of complaints
TDF domains: beliefs about consequences, social influences
While in one of the studies, HCPs reported viewing complaints as justified and understandable, arising mostly from misaligned expectations between patients and healthcare personnel (Odelius et al. [72]), participants in other studies reported believing that the complaint was unfair, unjustified or viewed it as a personal attack – “vexatious complaint” (Scott, [73]) – and despite offering help to the patient, the patient continued to complain, as indicated in the excerpt below:
58% thought the complaint was unjustified. Many clinicians explained they had already taken extra time and effort to explain the diagnosis and explore management options, and despite this, the patient still complained (Bolton & Goldsmith, [78], p. 4).
Importantly, some HCPs interpreted complaints as a poor appreciation of their efforts to provide care (Adams et al. [26]). Negative perceptions about the value of complaints were a barrier to responding effectively to complaints (McCreaddie et al. [70]), as they were often interpreted as indications of loss of trust and a breakdown in the clinician–patient relationship:
One respondent described the situation as “irretrievable” once the patient had “turned against you”. (Neurologist) (Bolton & Goldsmith, [78], p. 4).
In some cases, HCPs rationalized complaints by locating the cause of the complaints within the patient due to their medical condition or personality type (for example, vindictive or personally critical):
The notion that “some people complain about just about anything” was another way in which interviewees rationalized patients’ complaining (Adams et al. [26], p. 615).
In other cases, HCPs dismissed complaints because they believed patients were complaining for personal benefits, such as compensation (Xanthos, [75], p.15).
Theme 8: managerial and peer support
TDF domain: social influences, social/professional role and identity
Social influences were common themes among the included studies and reported both as a barrier and as an enabler (for example, [21, 68, 72, 84]). Clinical staff in the included studies stated that they mostly felt supported by their colleagues, but often lacked support from management, believing this was due to managers wishing to avoid escalation of the complaint:
The managers do not care about finding out the truth or supporting their staff. They only wish to avoid escalation of the complaint […]. They do not support staff at all. (Bourne et al. [68], p. 3).
On the contrary, some managers felt the obligation to take the HCPs side, as they did not want to be seen not supporting staff who work in the organization:
I suppose at the end of the day we would come down on the side of staff. You don’t want to be seen to not be backing up your staff. Sounds awful that – doesn’t it? (Burr [84], p. 14).
The majority of HCPs stated in the included papers that they received support from their colleagues (Bourne et al. [21]). Conversely, some doctors felt unable to criticise other staff or be a “whistle blower”, as they had a mutual understanding of how it feels to be on the receiving end of a complaint (Bourne et al. [79]) and therefore felt the moral obligation to show collegiality and protect each other. The following excerpts highlight these perspectives:
A medical director discussed the difficulties of reporting colleagues and the perception of “whistle-blowing” and a Director of Public Health suggested that “it’s almost impossible to make a complaint against a doctor”. One respondent demonstrated defensiveness: “it’s us against the world and we close ranks to protect each other” (Burr, [84], p. 48).
Theme 9: organizational culture and leadership
TDF domain: social influences
Organizational culture is the set of shared beliefs, values, attitudes and norms of behaviour that guide and inform the actions of all employees [87]. While it was acknowledged that there were “pockets” of blaming culture in some teams, often leading to defensive practices as a way to avoid patients’ complaints or having to deal with them [71, 85], leadership was found to be the critical factor setting the tone for complaints management and governance:
Chief executives and senior managers determine the culture of the organisation and need to convey to staff that complaints handling is an integral part of safety and quality and that all staff have a responsibility to respond openly and constructively to complaints (Burr, [84], p. 44).
Organizational position and policies about how complaints should be responded to cascaded from the top (that is, the chief executive) and guided the way complaints were examined and handled by frontline staff, as indicated in the quote below:
“I don’t just sign the complaint; I read every single line of every complaint in this organisation”. “Complaints are a learning opportunity and it provides a role model for the organisation that the chief executive’s interested in the process and interested in the outcome” (Burr, [84], p. 24).
Theme 10: negative emotions
TDF domains: emotions, beliefs about consequences
Another frequently emerging theme within the data was negative emotions (for example, [66, 67, 69, 86). HCPs experienced feelings of stress and anxiety, and also feelings of betrayal and hurt after receiving a complaint, which influenced how they viewed complaints:
I still find it very hard that a patient’s family could be so vindictive and unpleasant. (Doctor) (Bourne et al. [68], p. 3).
In some instances, HCPs also felt frustrated and betrayed that the patient did not come to them first and pursued a formal complaint against them (Adams et al. [26]). Several participants felt vulnerable and intimidated by patients and their families, which resulted in feeling unable to address a concern in case the problem escalated further:
Several interviewees discussed the same examples of senior consultants being intimidated by families and unable to respond to this because “you’d be frowned upon about being assertive and dealing with it in case they actually do raise a complaint” (Adams, [26], p. 616).
Surveys examining HCPs’ anxiety, stress and depression found that complaints investigations were associated with greater anxiety and depression [78, 79]. Perceiving that normal process was not being followed was also associated with increased anxiety and depression (Bourne et al. [21]). In addition, legal liability concerns or fear were often cited as a driver for staff reluctance to offer an apology and to acknowledge responsibility or errors to reduce perceived legal risks, and costs or compensations associated with legal processes. It was reported that, although the NHS Litigation Authority’s official position was that apologies could be offered as a way to resolve a complaint, the legal complexities of offering an apology in combination with the lack of clear guidance about what HCPs could do on the ground was a source of confusion:
Trusts frequently told the Healthcare Commission that they had not apologized for fear of admitting legal liability. The medical defence organisations and the NHS Litigation Authority, however, have consistently made it clear that apologies can be given to try to resolve matters without admitting liability (Burr, [84], p. 28).
Recommended intervention strategies using the BCW approach
Contextually appropriate strategies are necessary to address individual practice behaviours, as well as wider organizational practices for effective complaints management. The BCW can guide the development of interventions that would be best suited to address the identified barriers to effective complaints handling. In the BCW, all TDF domains are directly mapped to a broader, complimentary model comprising six constructs that guide behaviour – the capability, opportunity, motivation and behaviour (COM-B) model: (1) psychological capability, (2) physical capability, (3) physical opportunity, (4) social opportunity, (5) reflective motivation and (6) automatic motivation. The COM-B model has been found particularly useful to intervention designers and policy-makers [88, 89]. Using the BCW approach [52], the relevant TDF/COM-B components were mapped on to intervention types, subsequently to policy categories and, lastly, to behaviour change techniques through which the intervention could be implemented [53]. We identified six intervention types, six policy categories and 16 behavioural changes techniques. Table 4 presents the suggested strategies/recommendations for improving health professionals’ ability to respond constructively to complaints structured around the BCW.
Table 4.
TDF influences as factors mapped to proposed interventions using the Behaviour Change Wheel and recommendations for practice changes
| Factors influencing complaint management | TDF (and corresponding COM-B) | Intervention type | Policy categories | Behaviour change technique(s) | Recommendations for practice |
|---|---|---|---|---|---|
|
Knowledge of complaints procedures Lack of training |
Knowledge Skills (Psychological capability) |
Education Training Enablement |
Communication/marketing Service provision |
-Information about social and environmental consequences -Feedback on behaviour -Feedback on outcomes of behaviour -Demonstration of behaviour -Self-monitoring of behaviour -Prompts/cues |
-Increase knowledge of the procedures for handling formal and informal complaints within the organization -Assess staff training needs and offer tailored training for developing communication skills and “perspective taking” abilities (for example, show active listening, understanding and empathy and avoid fauxpology) -Remind HCPs of the complexities of the system for patients and their families and the difficulties around navigating it |
| Interpersonal skills for example, de-escalation skills | |||||
| Time and resources |
Environmental context and resources (Physical opportunity) |
Environmental restructuring Enablement |
Environmental/social planning Fiscal measures |
-Restructuring the physical environment -Restructuring the social environment -Problem-solving -Action planning |
-Increase resources for patient care to match demand (for example, increased staff) or more effective management of demand issues/PALS to be appropriately resourced to allow for learnings from complaint management to feed into patient care -Assess patients’ expectations for effective resolution and plan actions accordingly |
|
Inherent contradictions within the role Authority of the role Managerial and collegial support Organizational support/blaming culture and defensive attitudes |
Social/professional role and identity Social influences (Social opportunity) |
Environmental restructuring Persuasion Modelling |
Environmental/social planning Regulation |
-Restructuring the social environment -Demonstration of the behaviour -Social support (emotional) -Information about social and environmental consequences -Credible source |
-Address role divisions by intervening at multiple levels of the system/organization to emphasise responding to complaints as part of the HCPs’ role -Set the expectation for senior clinical managers to be open to constructive feedback and lead by example -Address organizational culture to overcome blaming and defensiveness |
| Beliefs about ability to deal with complaints/difficult situations |
Beliefs about capabilities Beliefs about consequences Intention (Reflective motivation) |
Persuasion Education Modelling Enablement |
Communication/marketing Service provision |
-Verbal persuasion about capability -Framing/reframing -Feedback on behaviour -Feedback on outcomes of behaviour -Focus on past success |
-Audit and give feedback on behaviour to increase staff confidence in complaints handling and provide training where needed -Reframe the complaints process from a policing function to an improvement function, taking care to involve clinical staff in the positioning of this change -Increase managerial and collegiate support for health professionals who have complaints raised against them to help them manage negative emotions associated with receiving complaints to minimize defensive responses and practice -Provide emotional support (for example, counselling and/or supervision) to HCPs as needed -Reframe organizational narratives around the meaning of patient complaints (for example, an opportunity to learn vs a vexatious attack) and communicate learnings across the organization |
| Belief that complaints have negative consequences | |||||
| Negative emotions: stress, anxiety, frustration and fear |
Emotion (Automatic motivation) |
Modelling Enablement |
Communication/marketing Service provision Legislation |
-Social support (emotional) -Framing/reframing -Identification of self as role model -Credible source -Problem-solving -Action planning |
|
| Fear of litigation |
Discussion
The aim of this review was to understand HCPs’ response to complaints at the initial point of receipt. The data presented here show that HCPs’ responses and wider organizational responses are complex, involving a wide range of influences, that is, psychological, social and environmental. Drawing on the TDF [50], the identified influences mapped onto nine domains, and subsequently, recommendations for future potential interventions in healthcare organizations were generated using the BCW approach. Although the analysis focuses on the British healthcare system in detail, the findings and recommendations have broader implications for public healthcare organizations globally.
The first key finding of this systematic review is the identified gaps in the evidence base for HCPs’ response behaviours at initial receipt. The majority of the included papers relate to the management of complaints that are made post-incident, and associated organizational processes and consequences, rather than HCPs’ initial response to a complaint, that is, in-the-moment. However, it was clear that post-incident management has an effect on in-the-moment responding, so the two were considered together. Similarly, there was no clear distinction in the literature for the management of informal versus formal complaints.
The nature of HCPs’ beliefs about the consequences of patients’ complaints was identified as an important theme. The belief that complaints compete for time and attention as an additional task on top of other clinical priorities, which are more central to their professional identity, was reported as an important barrier to effective complaints management. Similarly, the belief that complaints are not beneficial for the healthcare professional–patient relationship or that complaints do not always reflect quality of care shaped how complaints were viewed and responded to. When complaints were viewed in this way, HCPs often attributed complaints to the complainants’ personality type or to personal/materialistic benefits and therefore responded unhelpfully. In turn, unresolved complaints exacerbated the frustration and lack of trust for both patients and HCPs [36, 90].
Other commonly cited barriers to effective complaints handling included overlapping responsibilities, and lack of time and resources to spend on examining the particular circumstances or causes for each complaint, lack of assessment of patient expectations [91] and lack of appropriate training to respond to particular types of patient communications (for example, communications aggressive in tone). Although PALS was set up to support the more vulnerable and hard-to-reach population groups, PALS officers were concerned about the lack of adequate resources (for example, staffing issues) necessary for quality service provision [92, 93].
Another key theme was the role of organizational structure and culture in shaping individual response behaviours, and in particular, the role of managerial-organizational support for staff. Clinical managers can help increase awareness of policy and procedure among staff, but they can also support staff who receive complaints to respond constructively and manage the emotional burdens of complaints, as also indicated in previous studies (for example, [17]). Importantly, role divisions and the organizational – seemingly blaming – culture within which these actors (clinical managers and HCPs) operate was found to be a determining factor leading to defensive practice with the aim to avoid litigation [1, 38, 94]. However, it was clear that leadership set the tone for key priorities and strategic direction and articulating a coherent set of values can guide individual actions [95, 96].
In line with research in patient-centred care and communication [6, 97, 98], frequently reported enablers were skills such as active listening, reflections and empathizing with the patient. The need for authenticity (not offering “fake apologies”), acceptance of the patient perspective and accountability in responding to informal or formal complaints was acknowledged in the majority of the included studies. However, there was relatively little research on HCPs’ beliefs about their level of capability and skilful practice (that is, self-efficacy beliefs).
Policy implications
Despite the plethora of complaint resolution guides over the years [22, 32], the majority of the included studies pointed towards failures or missed opportunities for healthcare organizations to learn lessons from complaints. While the guidance suggested a set of responses that NHS employees should follow in response to patient complaints, including expressions of sincere regret and responding to an individual on the basis of their unique circumstances, there was little focus on organizational factors influencing how complaints were viewed and utilized within the organization [99]. Whilst hospital boards use patient feedback data, the discussion of feedback does not automatically result in taking action or providing explicit quality assurance [100, 101]. As a result, there have been repeated calls for a shift in organizational culture to make NHS trusts learning organizations by using feedback in a meaningful way and translating that data into service improvements [1, 102–105]. An organizational culture which promotes the notion that complaints represent an opportunity to learn, reflect and improve clinical practice and processes creates the conditions for effective complaints management and organizational learning [95, 106, 107]. The recently published (December 2022) NHS complaints standards in collaboration with the ombudsman guidance [31] on complaints handling places organizational learning at the heart of an effective complaints handling model of best practice by recognizing complaints as valuable feedback for the organization and viewing them as opportunities to improve services. Although this is undoubtedly a major step in the right direction, the implementation of these standards is a lengthy work-in-progress and will require multiple behaviour changes, and organizational commitment and resources, while addressing various other challenges post-coronavirus disease 2019 (COVID-19) [108].
Recommendations
Our findings suggest that, while it is important to upskill HCPs and their managers in complaint management procedures for all types of complaints, as well as in interpersonal skills (for example, de-escalation), it is also necessary to allocate sufficient resources (for example, additional personnel where needed) to PALS to match the level of demand. Importantly, our recommendations emphasize the need to address role conflicts and divisions among clinical and non-clinical staff, as well as the separateness of complaints management from quality assurance and improvement within the organization. Complaints management was often treated as a separate and less significant activity compared with core clinical duties. Consistent with existing literature, our findings highlight the importance of reframing the organizational narrative about patient complaints, shifting from a policing function to an improvement function [41, 99]. The way HCPs perceive their organization to be handling and viewing patient complaints significantly influences the way they respond to complaints. When HCPs perceive their employing organizations to handle complaints ineptly or with a “tick box mentality” [109], it often results in defensive practices, trivializing patient concerns or attributing those concerns to unmodifiable traits (for example, “part of their personality”). Such responses limit HCPs’ willingness to actively listen to patients about their experience, which can lead to more helpful patterns of responding in-the-moment. Conversely, perceptions of a well-managed and fair complaints handling process may minimize unhelpful responses and increase patterns of responding that can enable greater patient satisfaction and learning from patient feedback [110].
Strengths and limitations
To our knowledge, this is the first review drawing together mixed-methods evidence on HCPs’ responses to complaints in healthcare settings in the UK. The review used a behavioural framework analysis to identify and classify the drivers of behaviours in complaints management. Results identified factors influencing response to complaints but also demonstrated gaps in the literature about immediate informal responses, thus, limiting, in turn, our findings pertaining to our original research aim. Due to variations in legal, procedural and organizational frameworks within patient complaints management systems across countries [27], our review focused solely on the UK national healthcare system. In addition, the included papers were heterogeneous, and there may also be different definitions of the term “complaint” (for example, feedback) that were not captured using our search terms. We also acknowledge that in some cases, it was not possible to clearly separate personal responses from organizational processes (informal/formal responses) in the included papers and that the two may well be interwoven.
Conclusions
This review identified a wide range of individual, social/organizational and environmental influences on complaints management in secondary and tertiary care. The behavioural analysis informed recommendations for intervention content, with particular emphasis on reframing and building on the positive aspects of complaints as an underutilized source of feedback at an individual and organizational level for patient safety and quality improvement.
Supplementary Information
Acknowledgements
We would like to thank [Dr Fiona Beyer in the Population Health Sciences Institute, Newcastle University] for her guidance on the review search strategy, as well as colleagues in [Department of Health and Social Care, UK] for critically reviewing the final version of the manuscript and for their suggestions.
Author contributions
Conceptualization and study design: P.C., V.A. and C.M. Writing – original draft: V.A. Writing review and editing: A.C., F.L., C.M., P.C., F.F.S., I.V., L.G., A.V., B.G. and A.Mc.K. Supervision and funding acquisition: A.C., P.C. and F.F.S. Final approval: all authors.
Funding
This project was funded by the National Institute for Health Research (NIHR) [Policy Research Unit in Behavioural Science (project reference PR-PRU1217-20501)]. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Availability of data and materials
Supplementary materials uploaded on Open Science Framework (OSF).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None declared.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pope R. Organizational silence in the NHS: ‘hear no, see no speak no.’ J Change Manag. 2019. 10.1080/14697017.2018.1513055. [Google Scholar]
- 2.Bismark MM, et al. Relationship between complaints and quality of care in New Zealand: a descriptive analysis of complainants and non-complainants following adverse events. Qual Saf Health Care. 2006;15(1):17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haw C, Collyer J, Sugarman P. Patients’ complaints at a large psychiatric hospital: can they lead to better patient services? Int J Health Care Qual Assur. 2010;23(4):400–9. [DOI] [PubMed] [Google Scholar]
- 4.Coulter A, et al. Collecting data on patient experience is not enough: they must be used to improve care. BMJ: Bri Med J. 2014;348:g2225. [DOI] [PubMed] [Google Scholar]
- 5.Kelsey F, Ara D, Erik M. Care pathway and organisational features driving patient experience: statistical analysis of large NHS datasets. BMJ Open. 2018;8(7):e020411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCreaddie M, Benwell B, Gritti A. Traumatic journeys; understanding the rhetoric of patients’ complaints. BMC Health Serv Res. 2018;18(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.R., F., Report of the mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary, vol. 947: the Stationery Office. 2013.
- 8.Jonsson PM, Øvretveit J. Patient claims and complaints data for improving patient safety. Int J Health Care Qual Assur. 2008;21(1):60–74. [DOI] [PubMed] [Google Scholar]
- 9.Sage WM. Putting the patient in patient safety: linking patient complaints and malpractice risk. JAMA. 2002;287(22):3003–5. [DOI] [PubMed] [Google Scholar]
- 10.Berger S, Saut AM, Berssaneti FT. Using patient feedback to drive quality improvement in hospitals: a qualitative study. BMJ Open. 2020;10(10):e037641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadjistavropoulos H, et al. Patient perceptions of hospital discharge: reliability and validity of a patient continuity of care questionnaire. Int J Qual Health Care. 2008;20(5):314–23. [DOI] [PubMed] [Google Scholar]
- 12.Jabbari A, et al. The profile of patients’ complaints in a regional hospital. Int J Health Policy Manag. 2014;2(3):131–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reader TW, Gillespie A. Patient neglect in healthcare institutions: a systematic review and conceptual model. BMC Health Serv Res. 2013;13(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bark P, et al. Clinical complaints: a means of improving quality of care. BMJ Qual Saf. 1994;3(3):123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouwman R, et al. Patients’ perspectives on the role of their complaints in the regulatory process. Health Expect. 2016;19(2):483–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Griffiths A, Leaver MP. Wisdom of patients: predicting the quality of care using aggregated patient feedback. BMJ Qual Saf. 2018;27(2):110–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsieh SY. An exploratory study of complaints handling and nature. Int J Nurs Pract. 2012;18(5):471–80. [DOI] [PubMed] [Google Scholar]
- 18.Weingart SN, et al. What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med. 2005;20(9):830–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jangland E, Gunningberg L, Carlsson M. Patients’ and relatives’ complaints about encounters and communication in health care: evidence for quality improvement. Patient Educ Couns. 2009;75(2):199–204. [DOI] [PubMed] [Google Scholar]
- 20.van Mook WNKA, et al. Poor professionalism identified through investigation of unsolicited healthcare complaints. Postgrad Med J. 2012;88(1042):443–50. [DOI] [PubMed] [Google Scholar]
- 21.Bourne T, et al. Doctors’ perception of support and the processes involved in complaints investigations and how these relate to welfare and defensive practice: a cross-sectional survey of the UK physicians. BMJ Open. 2017;7(11):e017856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.England, N., NHS England Complaints Policy, https://www.england.nhs.uk/wp-content/uploads/2016/07/nhs-england-complaints-policy-amended.pdf. 2013.
- 23.N England. Serious incident framework: supporting learning to prevent recurrence. London: NHS; 2015. [Google Scholar]
- 24.Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf. 2014;23(8):678–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gillespie A, Reader TW. The healthcare complaints analysis tool: development and reliability testing of a method for service monitoring and organisational learning. BMJ Qual Saf. 2016;25(12):937–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adams M, Maben J, Robert G. ‘It’s sometimes hard to tell what patients are playing at’: how healthcare professionals make sense of why patients and families complain about care. Health. 2018;22(6):603–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsieh SY. Healthcare complaints handling systems: a comparison between Britain, Australia and Taiwan. Health Serv Manage Res. 2011;24(2):91–5. [DOI] [PubMed] [Google Scholar]
- 28.DoH, Department of Health UK, White Paper ‘The New NHS: Modern, Dependable’ is to restructure the NHS so that it is based on ‘partnershipand driven by performance’ (Department of Health, 1997).
- 29.Dalingwater L. Right to reply: using patient complaints and testimonials to improve performance in the NHS. Revue Française de Civilisation Britannique. 2019. 10.4000/rfcb.4422. [Google Scholar]
- 30.Ombudsman PAHS. NHS complaints standards. London: Summary of Expectations; 2021. [Google Scholar]
- 31.Ombudsman, P.a.H.S., Complaints to the Parliamentary and Health Service Ombudsman, 2021–22. https://www.ombudsman.org.uk/publications/complaints-parliamentary-and-health-service-ombudsman-2021-22. 2022.
- 32.Resolution, N., Saying Sorry. https://resolution.nhs.uk/resources/saying-sorry/. 2018.
- 33.Francis R. Report of the mid-staffordshire NHS foundation trust public inquiry HC 947 house of commons. London: Stationery Office; 2013. p. 2013. [Google Scholar]
- 34.Knight M, Stanford S. Ockenden: another shocking review of maternity services. Br Med J. 2022. 10.1136/bmj.o898. [DOI] [PubMed] [Google Scholar]
- 35.NAO, National Audit Office Report. Managing the costs of clinical negligence in trusts. Department of Health. September 2017. https://www.nao.org.uk/wp-content/uploads/2017/09/Managing-the-costs-of-clinical-negligence-in-trusts-summary.pdf.
- 36.Martin GP, Chew S, Dixon-Woods M. Why do systems for responding to concerns and complaints so often fail patients, families and healthcare staff? A qualitative study. Soc Sci Med. 2021;287:114375. [DOI] [PubMed] [Google Scholar]
- 37.Gillespie A, Reader TW. Patient-centered insights: using health care complaints to reveal hot spots and blind spots in quality and safety. Milbank Q. 2018;96(3):530–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gallagher TH, Mazor KM. Taking complaints seriously: using the patient safety lens. BMJ Qual Saf. 2015;24(6):352–5. [DOI] [PubMed] [Google Scholar]
- 39.Mattarozzi K, et al. What patients’ complaints and praise tell the health practitioner: implications for health care quality. A qualitative research study. Int J Qual Health Care. 2017;29(1):83–9. [DOI] [PubMed] [Google Scholar]
- 40.Gurley KL, et al. Use of physician concerns and patient complaints as quality assurance markers in emergency medicine. West J Emerg Med. 2016;17(6):749–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Dael J, Reader TW, Gillespie A, Neves AL, Darzi A, Mayer EK. Learning from complaints in healthcare: a realist review of academic literature, policy evidence and front-line insights. BMJ Qual Saf. 2020;29(8):684–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mirzoev T, Kane S. Key strategies to improve systems for managing patient complaints within health facilities – what can we learn from the existing literature? Glob Health Action. 2018;11(1):1458938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chater A, Whittaker E, Lewis L, et al. Health psychology, behavioural science, and Covid-19 disease prevention. Health Psychol. 2020. 10.5384/bpshpu.2020.29.3.3. [Google Scholar]
- 44.P.H.E., Public Health England. Improving people’s health: Applying behavioural and social sciences to improve population health and wellbeing in England. London: Public Health England. 2018.
- 45.Hallsworth M. A manifesto for applying behavioural science. Nat Hum Behav. 2023;7(3):310–22. [DOI] [PubMed] [Google Scholar]
- 46.World Health Organisation, W., Behavioural Sciences for better health. https://www.who.int/initiatives/behavioural-sciences.
- 47.Graham-Rowe E, et al. Barriers to and enablers of diabetic retinopathy screening attendance: a systematic review of published and grey literature. Diabet Med. 2018;35(10):1308–19. [DOI] [PubMed] [Google Scholar]
- 48.Chater A, et al. Influences on antibiotic prescribing by non-medical prescribers for respiratory tract infections: a systematic review using the Theoretical Domains Framework. J Antimicrob Chemother. 2020;75(12):3458–70. [DOI] [PubMed] [Google Scholar]
- 49.Atkins L, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cane J, O’Connor D, Michie S. Validation of the Theoretical Domains Framework for use in behaviour change and implementation research. Implement Sci. 2012;7(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Atkins L, et al. Influences on NHS health check behaviours: a systematic review. BMC Public Health. 2020;20(1):1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Michie S, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]
- 54.Mann CD, et al. One-year audit of complaints made against a University Hospital Surgical Department. ANZ J Surg. 2012;82(10):671–4. [DOI] [PubMed] [Google Scholar]
- 55.Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ayiku L, et al. The medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID medline. Health Info Libr J. 2017;34(3):200–16. [DOI] [PubMed] [Google Scholar]
- 57.Hogg R, Hanley J, Smith P. Learning lessons from the analysis of patient complaints relating to staff attitudes, behaviour and communication, using the concept of emotional labour. J Clin Nurs. 2018;27(5–6):e1004–12. [DOI] [PubMed] [Google Scholar]
- 58.Hong QN, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. [Google Scholar]
- 59.Institute, T.J.B., Critical Appraisal tools for use in JBI Systematic Reviews: Checklist for Systematic Reviews and Research Syntheses. https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Systematic_Reviews2017_0.pdf. 2017.
- 60.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 61.Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. [Google Scholar]
- 62.Bingham AJ, Witkowsky P. Deductive and inductive approaches to qualitative data analysis. In: Vanover C, Mihas P, Saldaña J, editors. Analyzing and interpreting qualitative data: after the interview. Thousand Oaks: SAGE Publications; 2022. p. 133–46. [Google Scholar]
- 63.McGowan LJ, Powell R, French DP. How can use of the Theoretical Domains Framework be optimized in qualitative research? A rapid systematic review. Br J Health Psychol. 2020;25(3):677–94. [DOI] [PubMed] [Google Scholar]
- 64.Abbott S, et al. Quality criteria for patient advice and liaison services: what do patients and the public want? Health Expect. 2005;8(2):126–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abraham A. Lack of communication affects the care of patients and families. Prof Nurse. 2004;19(6):351–3. [PubMed] [Google Scholar]
- 66.Allan HT, et al. Supporting staff to respond effectively to informal complaints: findings from an action research study. J Clin Nurs. 2015;24(15–16):2106–14. [DOI] [PubMed] [Google Scholar]
- 67.Allan HT, et al. Gatekeeping access to the midwifery unit: managing complaints by bending the rules. Health. 2015;19(6):652–69. [DOI] [PubMed] [Google Scholar]
- 68.Bourne T, et al. Doctors’ experiences and their perception of the most stressful aspects of complaints processes in the UK: an analysis of qualitative survey data. BMJ Open. 2016;6(7):e011711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cooke H. “Out there, you’re on a stage”: complaints and the management of emotion work in nursing. Int J Work Organ Emot. 2007;2(2):145–60. [Google Scholar]
- 70.McCreaddie M, Benwell B, Gritti A. A qualitative study of national health service (NHS) complaint-responses. BMC Health Serv Res. 2021;21(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McGivern G, Fischer M. Medical regulation, spectacular transparency and the blame business. J Health Organ Manag. 2010. 10.1108/14777261011088683. [DOI] [PubMed] [Google Scholar]
- 72.Odelius A, et al. From transformative learning to social change? Using action research to explore and improve informal complaints management in an NHS trust. Int Pract Dev J. 2015. 10.1904/ipdj.51.006. [Google Scholar]
- 73.Scott H. The so-called" vexatious complaint": problems and solutions. Health Care Risk Rep. 2006;12(5):22. [Google Scholar]
- 74.Tingle J. Poor communication and an opaque complaints process. Br J Nurs. 2018;27(22):1338–9. [DOI] [PubMed] [Google Scholar]
- 75.Xanthos C. Conflicts and tensions in the role of NHS complaints managers. Health Care Risk Rep. 2005;11(9):14. [Google Scholar]
- 76.Xanthos, C. Conflicting obligations: role conflict among health care complaints managers. in Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2008.
- 77.Balasubramaniam MS, Mohmed Z, Purva M. How prepared are we in handling complaints from patients? Anaesthesia. 2012;67:28. [Google Scholar]
- 78.Bolton C, Goldsmith P. Complaints from patients with functional neurological disorders: a cross-sectional UK survey of why patients complain and the effect on the clinicians who look after them. BMJ Open. 2018;8(11):e021573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bourne T, et al. The impact of complaints procedures on the welfare, health and clinical practise of 7926 doctors in the UK: a cross-sectional survey. BMJ Open. 2015;5(1):e006687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Workforce, N.D., Data on written complaints in the NHS. 2017.
- 81.Robinson L, et al. A 36-month study of patient complaints at a tertiary fertility centre. Hum Fertil. 2014;17(1):45–9. [DOI] [PubMed] [Google Scholar]
- 82.Siyambalapitiya S, et al. A 22 month study of patient complaints at a national health service hospital. Int J Nurs Pract. 2007;13(2):107–10. [DOI] [PubMed] [Google Scholar]
- 83.Behavioural Insights Team (BIT), Behavioural insights into patient motivation to make a claim for clinical negligence. Final report by the Behavioural Insights Team. August 2018.
- 84.Burr, T., Feeding Back?: Learning from Complaints Handling in Health and Social Care. 2008, National Audit Office.
- 85.Hutchinson A, et al. Senior health professional’s perceptions of variations in medical practice: a qualitative and quantitative study. Med Educ. 2001;35:45–51. [DOI] [PubMed] [Google Scholar]
- 86.Treanor J. How to develop better practice in response to patients’ complaints. Nurs Manag-UK. 2014. 10.7748/nm2014.03.21.1.22.e1198. [DOI] [PubMed] [Google Scholar]
- 87.Serpa S. An overview of the concept of organisational culture. Int Bus Manag. 2016;10(1):51–61. [Google Scholar]
- 88.Barker F, Atkins L, de Lusignan S. Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. Int J Audiol. 2016;55(Suppl 3):S90–8. [DOI] [PubMed] [Google Scholar]
- 89.West, R., Michie, S., Chadwick, P., Atkins, L., Lorencatto, F., Chadborn, T., Sallis, A., Achieving behaviour change: A guide for national government. 2020: PHE publications.
- 90.Daniel AE, Burn RJ, Horarik S. Patients’ complaints about medical practice. Med J Aust. 1999;170(12):598–602. [DOI] [PubMed] [Google Scholar]
- 91.Friele RD, Reitsma PM, de Jong JD. Complaint handling in healthcare: expectation gaps between physicians and the public; results of a survey study. BMC Res Notes. 2015;8(1):529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Evans D, Powell J, Cross T. Patient advice and liaison services: results of an audit survey in England. Health Expect. 2008;11(3):304–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Keegan S, Ruta B, Charles V. How do national health service (NHS) organisations respond to patient concerns? A qualitative interview study of the patient advice and liaison service (PALS). BMJ Open. 2021;11(11):e053239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lane J, Bhome R, Somani B. National trends and cost of litigation in UK National Health Service (NHS): a specialty-specific analysis from the past decade. Scott Med J. 2021;66(4):168–74. [DOI] [PubMed] [Google Scholar]
- 95.Davies HT, Nutley SM. Developing learning organisations in the new NHS. BMJ. 2000;320(7240):998–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shipton H, et al. The impact of leadership and quality climate on hospital performance†. Int J Qual Health Care. 2008;20(6):439–45. [DOI] [PubMed] [Google Scholar]
- 97.Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021;20(1):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McCarthy I, Dawson J, Martin G. Openness in the NHS: a secondary longitudinal analysis of national staff and patient surveys. BMC Health Serv Res. 2020;20(1):900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sheard L, et al. What’s the problem with patient experience feedback? A macro and micro understanding, based on findings from a three-site UK qualitative study. Health Expect. 2019;22(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Blakemore S. Managers admit to making poor use of complaints data. Nurs Manag. 2013;20(4):5. [DOI] [PubMed] [Google Scholar]
- 101.Raleigh, V., Thompson, J., Jabbal, J., Graham, C., Sizmur, S., Coulter, A., The King’s Fund Report: Analysis of trends in NHS inpatient surveys 2005–13. December 2015. https://www.kingsfund.org.uk/publications/patients-experience-using-hospital-services/summary. 2015.
- 102.Millar R, et al. Hospital board oversight of quality and patient safety: a narrative review and synthesis of recent empirical research. Milbank Q. 2013;91(4):738–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Marsh C, et al. Patient experience feedback in UK hospitals: what types are available and what are their potential roles in quality improvement (QI)? Health Expect. 2019;22(3):317–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Alderwick H, Dixon J. The NHS long term plan. BMJ. 2019;364:l84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Britain G. Culture change in the NHS: applying the lessons of the Francis inquiries. London: Stationery Office; 2015. [Google Scholar]
- 106.Friedman C, et al. Toward a science of learning systems: a research agenda for the high-functioning learning health system. J Am Med Inform Assoc. 2015;22(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Foley, T.F., F., The Potential of Learning Healthcare Systems. The Learning Healthcare project. The Health Foundation. 2015.
- 108.McKee M, et al. The changing health needs of the UK population. Lancet. 2021;397(10288):1979–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Robert G, Cornwell J. Rethinking policy approaches to measuring and improving patient experience. J Health Serv Res Policy. 2013;18(2):67–9. [Google Scholar]
- 110.Mirzoev T. Key strategies to improve systems for managing patient complaints within health facilities – what can we learn from the existing literature? Glob Health Action. 2018. 10.1080/16549716.2018.1458938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tingle J. Trends in NHS complaint handling: The toxic cocktail still exists. Br J Nurs 2019;28(5):317–318. 10.12968/bjon.2019.28.5.317. [DOI] [PubMed]
- 112.NHS Digital. Data on written complaints in the NHS 2016-17. N. H. S. Digital Workforce Facilities Team. Leeds: NHS Digital, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Supplementary materials uploaded on Open Science Framework (OSF).