Abstract
Acute kidney injury (AKI) describes a condition associated with elevated serum creatinine levels and decreased glomerular filtration rate. AKI can develop as a result of sepsis, the nephrotoxic properties of several drugs, and ischemia/reperfusion injury. Renal damage can be associated with metabolic acidosis, fluid overload, and ionic disorders. As the molecular background of the pathogenesis of AKI is insufficiently understood, more studies are needed to identify the key signaling pathways and molecules involved in the progression of AKI. Consequently, future treatment methods may be able to restore organ function more rapidly and prevent progression to chronic kidney disease. MicroRNAs (miRNAs) are small molecules that belong to the non-coding RNA family. Recently, numerous studies have demonstrated the altered expression profile of miRNAs in various diseases, including inflammatory and neoplastic conditions. As miRNAs are major regulators of gene expression, their dysregulation is associated with impaired homeostasis and cellular behavior. The aim of this article is to discuss current evidence on the involvement of miRNAs in the pathogenesis of AKI.
Keywords: acute kidney injury, non-coding RNA, microRNA
1. Introduction
Acute kidney injury (AKI) is a term that represents several disorders that are associated with increased serum levels of creatinine and decreased glomerular filtration rates (GFR) [1]. The prevalence of AKI is estimated at approximately 20%, but it can be higher in critically ill patients hospitalized in intensive care units (ICUs) [2,3]. Renal impairment in AKI may lead to fluid overload, ionic disorders, and metabolic acidosis. Depending on the extent of these disorders, patients may need to undergo a renal replacement therapy (RRT) such as hemofiltration and hemodialysis, among other methods [4]. As in every pathological condition, understanding the pathogenetic mechanisms and pathophysiology is important to improve the prevention, diagnosis, and treatment of the disease. Furthermore, the identification of novel therapeutic targets and signaling pathways implicated in the pathogenesis of particular diseases could prevent the development of subsequent complications. In recent years, non-coding RNAs (ncRNAs) have been widely investigated as molecules that are frequently dysregulated in numerous conditions [5,6], including renal diseases [7]. ncRNAs are important regulators of gene expression, and thus they significantly affect cellular behavior. For instance, miR-19 mediates aldosterone responsiveness and controls sodium transport [8]. Several classes of RNA molecules belong to the ncRNA family, including microRNA (miRNA), long non-coding RNA (lncRNA), and circular RNA (circRNA), among others. The aim of this review is to summarize the current evidence relating to the involvement of miRNAs in the pathogenesis of AKI.
2. The Role of MicroRNA in the Pathogenesis of Acute Kidney Injury—In Vitro and Animal Models
2.1. Brief Overview of miRNA Biogenesis and Functionality
miRNAs were discovered in Caenorhabditis elegans in 1993; to this day, 2654 human miRNAs have been described [9,10]. The molecules are responsible for cell homeostasis by controlling gene expression. Their biogenesis begins when chromosomal DNA undergoes transcription from RNA polymerase II into primary miRNA transcripts (pri-miRNA) which later become stem-loop like structures which are precursor miRNAs (pre-miRNAs) with approximately 70 nucleotides by RNase III Drosha [11,12]. Subsequently, pre-miRNA is transported with specific carrier exportin-5 from the nucleus to the cytoplasm [13,14]. In the cytoplasm, pre-miRNAs are separated by Dicer/TRBP enzyme complexes into single-stranded RNA miRNA duplexes, while one strand is degraded [15]. miRNAs duplexes are 21–24 nucleotides in size [16,17]. Subsequently, the guide strand interacts with the Argonaute (AGO) protein of an RNA-induced silencing complex (RISC). The complex interferes with complimentary mRNA to induce its destabilization or translational repression [18]. Thus, the classical mechanism of action of miRNA molecules involves negative post-transcriptional regulation [19,20]. These molecules are located both intra- and extra-cellularly, making it possible to monitor their expression in blood samples [21]. Moreover, they have been isolated from urine, follicular fluid, cerebrospinal fluid (CSF), and saliva [22].
2.2. miRNA in Sepsis-Induced AKI
The classical function of miRNAs in regulating gene expression is to suppress translation after binding to their target mRNA. Some studies have also demonstrated that miRNAs can enhance gene expression [23]. Under pathological conditions, the expression of miRNAs changes in the affected tissue, as well as in biological fluids. Diseased tissues contribute to the altered expression profile of circulating molecules by secreting extracellular vesicles that contain miRNAs. In addition, as a result of tissue damage and cellular death, miRNAs are released into the extracellular space. In the case of renal tissue, different patterns of expression of RNA molecules can be detected in urine.
Several studies have demonstrated that the state of AKI significantly alters the expression of miRNAs. In a mouse model of hypoxia-induced renal damage, 18 miRNAs were found to be differentially expressed [24]. Moreover, poisoning induced alterations in urinary expression of miRNA molecules [25]. Such studies demonstrate that pathological conditions are associated with altered expression of miRNAs. Importantly, since these agents are significant gene expression regulators, their dysregulated presence can mediate the progression of AKI.
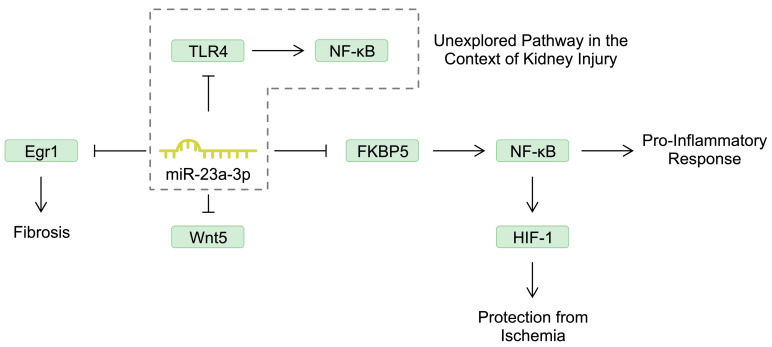
Renal damage during AKI development is associated with inflammatory responses and the increased expression and release of pro-inflammatory cytokines, chemokines, and adhesion molecules, as well as with the infiltration of immune cells [26]. miRNAs are known to regulate the expression of genes encoding inflammatory molecules. Nuclear factor kappa beta (NF-κB) is a major regulator of inflammatory responses that is implicated in the pathogenesis of several diseases [27,28]. Reducing the activity of NF-κB has also been suggested to induce positive effects in septic AKI [29]. miR-23a-3p is one of the molecules that is downregulated in patients with septic AKI [30]. An in vitro study demonstrated that stimulating HK-2 cells (proximal tubule epithelial cells) with lipopolysaccharide (LPS) reduced the expression of miR-23a-3p. Mechanistically, this miRNA negatively regulated FKBP prolyl isomerase 5 (FKBP5), which was associated with suppressed apoptosis and the release of inflammatory mediators (IL-8, IL-6). By targeting FKBP5, miR-23a-3p inactivates NF-κB, thus suppressing inflammatory responses [31]. Interestingly, NF-κB not only enhances inflammation, but can also induce protective mechanisms for the kidney. Specifically, it can stimulate the expression of hypoxia-inducible factor-1 (HIF-1), which can protect against ischemic conditions [32]. It is widely known that miRNAs are involved in a broad network of interactions and frequently target numerous genes. In the case of miR-23a-3p, Ye et al. [33] found that the molecule also negatively regulates Wnt5a, an element of the Wnt/β-catenin signaling pathway. The Wnt/β-catenin pathway plays an important role in kidney development and is considered to be protective in kidney injury. However, some evidence also suggests that this pathway could mediate the progression of AKI towards chronic kidney disease (CKD), possibly by modulating fibrosis [34]. In the previously mentioned study, Ye and colleagues [33] demonstrated that miR-23a-3p could mitigate kidney damage by downregulating Wnt5. In another study, miR-23a-3p suppressed the expression of pro-inflammatory mediators in HK-2 cells by targeting early growth response 1 (Egr1), a molecule suggested to be involved in the process of fibrosis [35]. miR-23a-3p might also play a role in the progression of AKI to CKD. Moreover, miR-23a-3p can also target toll-like receptor 4 (TLR4), as demonstrated in other cellular models [36,37]. Stimulating TLR4 can induce an intracellular signaling pathway that is myeloid differentiation primary response gene 88 (MyD88)-dependent and subsequently activates NF-κB, contributing to the pro-inflammatory response [38]. Stimulation of this pathway aggravates kidney cell injury [39]. A detailed review of the associations between TLR4 and AKI was conducted by Vázquez-Carballo et al. [40]. These studies demonstrate the broad interactions of miR-23a-3p that could take part in various mechanisms associated with AKI or with progression to CKD (Figure 1). Future studies should examine the miR-23a-3p/TLR4 axis in the model of AKI.
Figure 1.
The involvement of miR-23a-3p in several pathways that could regulate the progression of acute kidney injury.
miR-106a is another miRNA involved in the pathogenesis of renal diseases [41]. In contrast to miR-23a-3p, miR-106a is upregulated in septic patients. Stimulation of mouse kidney epithelial cells with LPS decreases their viability, which could be restored by transfection of miR-106 inhibitor. Similarly, inhibiting the molecule could reduce LPS-induced expression of pro-inflammatory mediators, such as IL-6, TNF-α, and IL-1β. Mechanistically, miR-106a could target and negatively regulate the expression of thrombospondin 2, a protein with antiangiogenic effects [42]. However, in HK-2 cells, miR-106a-5p was found to target high-mobility group 1 (HMGB1), an alarmin that stimulates inflammatory responses. In AKI mouse models, the expression of HMGB1 is elevated and associated with podocyte injury [43,44]. The signaling of HMGB1 involves stimulation of the TLR4/NF-κB pathway. miR-22 suppresses septic AKI by targeting the HMGB1/TLR4/NF-κB signaling pathway [45].
IL-6 is a pleiotropic cytokine that is classically associated with activation of the JAK/STAT signaling pathway. It is considered to exert both pro- and anti-inflammatory effects, but in inflammatory and malignant diseases it usually induces inflammatory reactions. Conflicting results have been published regarding the role of IL-6 in the pathogenesis of AKI. The expression of IL-6 increases in animal AKI models, and cytokine deficiency could prevent the development of renal injury. Furthermore, knockdown of IL-6 suppressed infiltration with neutrophils, an important cellular population that plays a role in AKI progression [46]. Furthermore, in pediatric patients undergoing cardiac surgery, elevated levels of IL-6 were observed in patients that developed post-operative AKI [47]. In patients admitted to the ICU, higher concentrations of IL-6 were associated with lower urine outputs within 72 h and a greater risk of persistent anuria. In contrast, this cohort demonstrated a lower risk of persistent AKI development [48]. However, in mice injected with cisplatin, knockout of IL-6 was associated with increased acute renal injury [49]. Moreover, IL-6 trans-signaling has been suggested to induce beneficial effects by stimulating anti-oxidating and repair mechanisms [50]. Thus, the role of IL-6 seems to be complex and might depend on the cellular context and the type of underlying injury. The IL-6 pathway is also regulated by miRNAs. Specifically, in a septic mouse model of AKI, the expression of miR-26a-5p is induced. This molecule has been suggested to stimulate protective mechanisms by targeting and downregulating IL-6 expression. Interestingly, the induction of miR-26a-5p expression was found to depend on NF-κB, further confirming the involvement of this transcription factor in protective mechanisms in the kidney [51]. Similarly to other RNA molecules, miR-26a-5p is implicated in a wider interaction network. Li et al. demonstrated that HK-2 cells can secrete this miRNA in exosomes. Blocking the release of exosomes could increase the expression of mir-26a-5p in proximal tubule cells. Consequently, increased expression of the molecule could inhibit the inflammatory response induced by bovine serum albumin. Specifically, miR-26a-5p could reduce protein expression of IL-6. Mechanistically, miR-26a-5p was found to target CHAC1, a molecule that enhances the activity of NF-κB and the expression of pro-inflammatory mediators. Therefore, these studies might demonstrate how different pro-inflammatory environments might change the mechanisms induced by NF-κB signaling [52]. In unilateral ureteral occlusion (UUO) mouse models, miR-26a-5p was also found to suppress fibrotic mechanisms [53]. Modulating the expression of miR-26a-5p could be an interesting approach for future studies, as its anti-inflammatory properties have been confirmed in other disease models as well [54,55,56].
Under septic conditions that occur in the development of AKI, other signaling pathways play an important role as well. Specifically, phosphatase and tensin homolog (PTEN) has been suggested to regulate renal function. This molecule is a member of several pathways, but one of the most frequently investigated signaling pathways associated with PTEN is the PI3K/AKT/mTOR pathway, which regulates major cellular functions. In a sepsis rat model, elevated expression of PTEN was accompanied by the decreased expression of miR-22-3p. Importantly, the induction of miR-22-3p in an in vivo experiment resulted in suppressed apoptosis of kidney tissue, inflammatory response, and markers of renal injury. Similarly, miR-22-3p reduced septic damage in HK-2 cells by targeting PTEN [57]. Another miRNA that regulates the expression of PTEN and the progression of AKI is miR-93. Zhan and colleagues demonstrated that its expression was reduced in kidney tissue obtained from septic AKI mouse models. In an in vitro experiment, miR-93 enhanced the viability of LPS-pretreated renal cells and reduced the expression of inflammatory mediators (IL-6, TNF-α, and IL-1β). By targeting PTEN, miR-93 stimulated the activity of the AKT/mTOR signaling pathway [58]. Similar results were observed regarding the miR-214 molecule [59]. However, one of the most investigated miRNAs targeting PTEN is miR-21, which has been investigated in numerous inflammatory diseases and malignancies [60,61,62]. In sepsis-related renal injury, the introduction of miR-21 significantly reduced the renal injury score [63]. Interestingly, miR-21 also contributes to sepsis protection induced by short periods of ischemia/reperfusion in femoral arteries. Specifically, sepsis-induced kidney damage was not prevented in miR-21 knockout animals [64]. In contrast to these studies, Wei et al. found that miR-21 can contribute to sepsis-related kidney damage by targeting cyclin-dependent kinase 6 (CDK6) [65]. Therefore, these studies demonstrate different mechanisms induced by a particular miRNA due to its involvement in different signaling pathways. Furthermore, different disease models can also alter miRNA functionality. In UUO mouse models, miR-21 encapsulated in the exosomes enhanced the fibrotic processes occurring in the kidneys [66].
Apart from the molecules described above, there is a growing number of investigated molecules regulating inflammation in sepsis-associated AKI. For instance, the expression of miR-128-3p is elevated in in vitro and in vivo sepsis models. By targeting neuropilin 1 (NRP1), miR-128-3p was found to stimulate the expression of pro-inflammatory mediators such as IL-6, TNF-α, IL-1β, and NF-κB. Importantly, introducing the inhibitor of miR-128-3p suppressed renal damage by reducing inflammation and improving kidney histology [67]. According to the literature, miR-128-3p can exert both pro- and anti-inflammatory features depending on the investigated cells and disease models [68,69,70]. However, in another study examining the involvement of miR-128-3p in sepsis, the authors observed that treatment of HK-2 cells with LPS downregulated the expression of miR-128-3p. Overexpression of this miRNA could suppress the pro-inflammatory response induced by LPS. Mechanistically, miR-128-3p regulated the expression of transforming growth factor beta receptor II (TGFBR2) [71]. Thus, the cellular context needs to be investigated to understand which molecule is being preferentially targeted by a particular miRNA.
Another group of miRNAs that regulate renal function under septic conditions are molecules regulating the expression of B-cell lymphoma-2 (BCL-2). BCL-2 is a group of proteins that regulate cell death and survival, named after the first member to be discovered, which has anti-apoptotic features [72]. miR-16-5p exacerbates the LPS-induced inflammatory responses in HK-2 cells. By targeting BCL-2, it could regulate apoptosis [73]. Similar results have been obtained regarding miR543 [74]. Other miRNA molecules that regulate inflammatory pathways in the development of AKI include miR-34b-5p [75], miR-181a-2-3p [76], miR-150-5p [77], and miR-20a-3p [78], among others. The abundance of such studies highlights the impressive number of regulatory mechanisms regulating apoptosis and inflammatory processes in AKI (Table 1).
Table 1.
Summary of microRNA molecules that regulate mechanisms associated with acute kidney injury under septic conditions.
| MicroRNA | Mechanism Associated with Acute Kidney Injury | References |
|---|---|---|
| miR-23a-3p | miR-23a-3p negatively regulates FKBP5, thus suppressing the activity of the NF-κB and reducing pro-inflammatory response. | [31] |
| miR-23a-3p | miR-23a-3p suppresses kidney injury by targeting Wnt5, a member of the Wnt/β-catenin signaling pathway. | [33] |
| miR-106a | miR-106a further stimulates kidney cell injury by targeting the anti-angiogenic thrombospondin 2. | [42] |
| miR-106a-5p | miR-106a-5p targets HMGB1, which is associated with podocyte injury and the expression of which is elevated in mouse models of AKI. | [43,44] |
| miR-22 | miR-22 suppresses septic AKI due to inhibiting the HMGB1/TLR4/NF-κB signaling pathway. | [45] |
| miR-26a-5p | miR-26a-5p induced protective mechanisms in septic models of AKI by targeting IL-6. | [51] |
| miR-22-3p | miR-22-3p suppresses inflammatory responses in animal sepsis AKI models and LPS-stimulated HK-2 cells by targeting PTEN. | [57] |
| miR-93 | miR-93 targets PTEN and activates the signaling of the AKT/mTOR pathway, which is associated with improved viability in LPS-pretreated renal cells. | [58] |
| miR-214 | By targeting PTEN, miR-214 improved renal parameters, suppressed inflammation, and improves renal histopathology in septic mice. | [59] |
| miR-21 | miR-21 can suppress renal injury induced by sepsis by targeting PTEN. | [63] |
| miR-21 | miR-21 contributes to the kidney damage induced by LPS by targeting CDK6. | [65] |
| miR-128-3p | miR-128-3p contributes to sepsis-associated kidney damage by targeting NRP1 and enhancing inflammatory response. | [67] |
| miR-16-5p | By targeting BCL-2, miR-16-5p regulates apoptosis and further stimulates LPS-induced inflammation. | [73] |
| miR-543 | Downregulating miR-543, which targets BCL-2, reduces inflammatory response and apoptosis. | [74] |
2.3. miRNAs in AKI Induced by Nephrotoxic Agents
In the previous section, we focused on AKI that develops under septic conditions. However, kidney damage due to nephrotoxic agents is another significant challenge with complex mechanisms involved in its pathophysiology. For example, anticancer cytostatic drugs are known for their nephrotoxicity. Cisplatin is a frequently used chemotherapeutic agent used in the treatment of various neoplasms. Recent studies have demonstrated that alterations in the miRNA profile are involved in the pathogenesis of cisplatin-induced AKI.
In an analysis by Wu and colleagues, treatment of HK-2 cells with cisplatin significantly altered the expression of 47 miRNAs [79]. Induction of cisplatin-related AKI (cis-AKI) is associated with increased expression of miR-483-5p, overexpression of which further deteriorates kidney function. Mechanistically, the molecule dysregulates apoptosis and autophagy of tubular epithelial cells by targeting GPX3, a member of the glutathione peroxidase family [80]. GPX3 was confirmed to be important in renal health in another study by Wu et al., who demonstrated that overexpression of GPX3 reduced the damage induced by ischemia-reperfusion [81]. Intriguingly, another member of the family, GPX4, was also found to mediate cisplatin-dependent AKI. Specifically, in in vitro and in vivo experiments, cis-AKI was associated with the elevated expression of miR-214-3p, a molecule that targeted GPX4. Suppression of miR-214-3p inhibited ferroptosis, a type of programmed cell death implicated in the pathogenesis of AKI [82,83]. In addition, cisplatin enhances another type of programmed cell death that is associated with inflammation: pyroptosis. Zhu and collaborators showed that cisplatin could enhance the pyroptosis of renal cells and stimulated these cells to secrete exosomes that prompted surrounding cells to initiate the programmed cell death process. Cellular death was suppressed by miR-122, which indicates the need for further research involving this molecule and renal damage [84].
DNA damage is also involved in the pathogenesis of cisplatin-induced renal damage. The metabolism of cisplatin involves modifications that allow it to bind to DNA, which then activates the DNA damage response signaling (DDR) pathway. Chronic activation of this pathway eventually leads to cell dysfunction or death [85]. A recent study demonstrated that cisplatin-induced DDR signaling could involve IL-22 signaling [86]. Intriguingly, repeated injections of cisplatin in mice causes DNA damage that leads to the state of CKD [87]. miRNAs were also suggested to mediate DNA damage processes. Yin and colleagues found that miR-155 knockout was associated with reduced accumulation of the DNA damage marker γH2AX. Moreover, the inhibition of miR-155 expression protected against apoptosis stimulated by the chemotherapeutic agent [88].
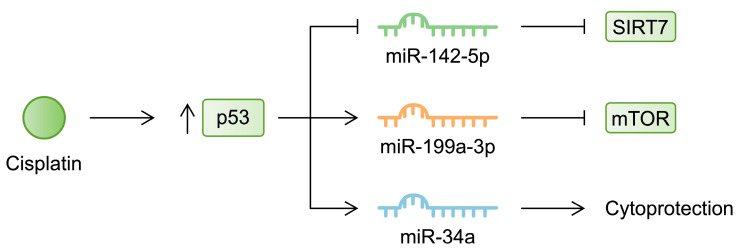
Similarly to sepsis-induced AKI, the nephrotoxic activity of cisplatin alters signaling pathways, and as previously mentioned, miRNAs are major regulators of signaling cascades. For instance, cisplatin was found to induce apoptosis and fibrosis in proximal tubular cells, and inhibition of p53 reduced these responses [89]. According to the previously mentioned study by Wu et al., the p53 pathway was among the most upregulated pathways in HK-2 cells treated with cisplatin [79]. P53 is a tumor suppressor that regulates the cell cycle and apoptosis by stimulating pro-apoptotic molecules such as PUMA. Cisplatin stimulates the expression of PUMA in renal cells, thus demonstrating its pro-apoptotic effects [90]. The p53 pathway is affected by miRNA activity, which ultimately modulates cisplatin-induced alterations. Specifically, overexpression of miR-142-5p suppressed the apoptosis of HK-2 cells that was enhanced by cisplatin. Inhibition of p53, which was activated by cisplatin, increased the expression of miR-142-5p. Mechanistically, miR-142-5p targets sirtuin 7 (SIRT7), a member of the SIRT family that has previously been suggested to be a therapeutic target in cis-AKI [91,92]. In another study, the expression of miR-199a-3p was found to be p53-dependent. Treatment of HK-2 cells with cisplatin was associated with increased expression of this miRNA, which was diminished in the presence of a p53 inhibitor. In turn, miR-199a-3p targeted and inhibited mTOR, a major regulator of cell survival, apoptosis, and autophagy [93]. In a recent review by Wang and collaborators, the authors discussed the involvement of mTOR in the pathogenesis of cis-AKI. The authors highlighted the complex role of mTOR in regulating the progression of the disease, but suggested that it plays a protective role [94]. Studies investigating the role of particular signaling cascades frequently demonstrate conflicting results, which shows the complex regulatory mechanisms that may depend on the cellular context. In the case of p53, Bhatt et al. found that cisplatin enhanced the expression of miR-34a via a p53-dependent mechanism. However, in contrast to miR-199a-3p, this molecule was suggested to play a protective role, as its inhibition further increased cell damage [95] (Figure 2). In addition, miRNAs can indirectly affect p53. According to Qin et al., treatment with cisplatin upregulated miR-449 in rat proximal tubular cells. Inhibiting the expression of this molecule stimulated the viability of renal cells. The molecule mediated the expression of SIRT1, which was associated with altered p53 acetylation status [96]. Consequently, the transcriptional properties of p53 changed, as described in more detail in a comprehensive review by Nagasaka and colleagues [97]. Moreover, other studies described the involvement of miRNAs in regulating other signaling cascades. For instance, cisplatin downregulates miR-30e-5p in mouse models. In an in vitro experiment, transfection of miR-30e-5p improved the viability of cisplatin-treated renal cells. Mechanistically, the molecule regulated the activity of the adenosine 5‘-monophosphate-activated protein kinase (AMPK) pathway [98]. Table 2 summarizes the expression profile and mechanisms linking miRNAs with cis-AKI. The studies discussed highlight the importance of miRNAs in renal injuries induced by nephrotoxic agents. Importantly, regeneration from cisplatin also involves miRNA modification. In a study by Candido de Almeida, the authors proved that administration of mesenchymal stem cells (MSCs) and MSC-derived microvesicles to cisplatin-pretreated mice stimulates the regeneration of damaged kidneys. Mechanistically, the authors showed that treatment with MSCs upregulated and downregulated 50 and 11 miRNAs, respectively. Furthermore, this treatment strategy restored physiological levels of proteins involved in the biogenesis of miRNAs [99]. Thus, this study proves the powerful impact of miRNAs in kidney functionality. Specifically, both damaging molecules, as well as regenerative therapies, alter miRNA expression profiles, which changes the renal parameters.
Figure 2.
Cisplatin stimulates p53 activity, which then affects the expression of several miRNA molecules.
Table 2.
Summary of expression profile of selected microRNAs and mechanisms associated with cisplatin-induced AKI.
| MicroRNA | Expression in Cisplatin-Induced AKI (In Vitro or In Vivo) | Mechanism | References |
|---|---|---|---|
| miR-483-5p | Increased | miR-483-5p disrupted apoptosis and autophagy in renal cells through targeting GPX3, a member of the glutathione peroxidase family. | [80] |
| miR-214-3p | Increased | miR-214-3p regulates ferroptosis by targeting GPX4. | [82] |
| miR-155 | Increased | Targeting miR-155 suppresses cisplatin-induced DNA damage. | [88] |
| miR-142-5p | Decreased | Suppression of p53 enhances the expression of miR-142-5p, which inhibits apoptosis induced by cisplatin. | [91] |
| miR-199a-3p | Increased | Cisplatin-induced expression of miR-199a-3p was p53-dependent, and the molecule regulated the mTOR gene. | [93] |
| miR-34a | Increased | miR-34a has cytoprotective features as its inhibition further enhanced cisplatin-induced cell damage. | [95] |
| miR-449 | Increased | Suppression of miR-449 enhances renal cell viability. | [96] |
| miR-30e-5p | Decreased | Overexpression of miR-30e-5p improves cell viability in cisplatin-treated renal cells. The molecule regulates the AMPK pathway. | [98] |
2.4. Ischemia-Reperfusion AKI
It is estimated that up to 25% of cardiac output is delivered to the kidneys. However, as the oxygen tension is low, alterations in blood delivery may create an imbalance between nutrient and oxygen availability, resulting in organ injury. In the case of mild injuries, repair processes can restore organ function. In severe damage, patients may develop CKD, which leads to progressive organ dysfunction. Ischemia-reperfusion injury (IRI) is associated with the activation of the HIF and NF-κB pathways, as well as inflammatory responses [100]. Recent studies have demonstrated that the expression of miRNAs is also dysregulated following IRI, which could contribute to the progression of AKI.
The expression of miR-182 is upregulated in the renal tissue of rats exposed to IRI. This molecule was found to enhance apoptosis in renal tubular epithelial cells and to target the forkhead box O3 (FoxO3) transcription factor [101], which plays a protective role in hypoxic renal injury by regulating autophagy and oxidative stress responses [102]. FoxO3 is a transcription factor involved in major cellular processes, such as proliferation and metabolism. However, it is difficult to precisely demonstrate its effects on the pathogenesis of AKI, as its activity depends on cellular location and modification. In the context of hypoxia, FoxO3 has also been suggested to induce pro-apoptotic effects, which can be compensated for by the activity of deacetylase SIRT1 [103], thus suggesting the beneficial effects induced by SIRT1. In line with these findings, renal IRI enhances the expression of miR-132-3p, which targets and downregulates SIRT1 [104].
In the paragraph discussing sepsis-associated AKI, we mentioned the involvement of miR-21 in the pathogenesis of renal damage. Intriguingly, studies have also examined the role of this molecule in renal IRI. Specifically, the molecule is negatively associated with the maturation of dendritic cells (DCs). In contrast to immature DCs, mature cells stimulate inflammatory responses. Suppressing the expression of miR-21 in kidneys exposed to IRI was found to exacerbate the inflammatory response by increasing the expression of NF-κB and pro-inflammatory cytokines [105]. Moreover, miR-21 mimics inhibit DC maturation and thus reduce the expression of TNF-α and IL-6. Interestingly, injection of miR-21-overexpressing DCs into mice after IRI suppressed pro-inflammatory cytokines, along with the expression of NF-κB. Importantly, the transfer significantly reduced the serum creatinine level after 24 h of IRI [106]. Additionally, miR-21 was found to mediate the renoprotective properties of ghrelin [107], enhance proliferation, and suppress the apoptosis of renal cells in gentamicin-induced kidney injury in fish models [108]. In addition, miR-211 [109], miR-192-5p [110], miR-187 [111], and miR-194 [112] were also investigated in the context of IRI/hypoxia and reoxygenation (Table 3). Recently, Chen et al. demonstrated that miR-155-3p contributes to the previously mentioned cell death, pyroptosis. Intriguingly, the authors found that miR-155-3p is transferred into adjacent cells through gap junctions formed by connexin 32, inhibition of which could suppress pyroptosis [113]. Additionally, researchers suggest the important involvement of PTEN in regulating IRI-based kidney injury. miR-486-5p, a molecule that targets PTEN, induced protective mechanisms in IRI mice [114]. However, as with other miRNAs, miR-486-5p has several targets and its influence on kidney functionality may depend on other pathways. Vinas and collaborators showed that apart from downregulating PTEN, miR-486-5p suppresses the expression of TNF and apoptotic genes [115]. The activity of miR-17-5p was also found to induce protective effects on kidney function in the IRI mice model. This molecule also targets the expression of PTEN [116]. However, as pharmacological inhibition of PTEN was associated with more pronounced kidney damage in the IRI context [117], the protective role of miRNAs could depend on their broad regulatory network, which also involves PTEN. Regarding miR-17, the molecule belongs to the cluster known as miR-17~92, which contains several miRNAs that regulate major cellular processes and are frequently dysregulated in a number of pathological conditions [118]. The cluster has important proangiogenic properties which are suggested to induce positive effects under ischemic conditions. Accordingly, the loss of function of the cluster in renal endothelial cells was associated with enhanced renal damage after IRI. By contrast, administration of miR-18a and miR-18b mimics (members of the miR-17~92 cluster) stimulated renal recovery [119].
Table 3.
Summary of selected microRNAs with known altered expression profiles in IRI-associated AKI, which contributes to the pathogenesis of renal injury.
| MicroRNA | Impact of Ischemia-Reperfusion Injury on Expression in Renal Tissue/Cells | Mechanism Linking to Acute Kidney Injury | References |
|---|---|---|---|
| miR-182 | Increased | miR-182 enhances apoptosis of tubular epithelial cells through targeting FoxO3. | [101] |
| miR-132-3p | Increased | miR-132-3p targets SIRT1 and further deteriorates oxidative balance in ischemia. | [104] |
| miR-21 | Increased | miR-21 plays a protective role in IRI-associated AKI by suppressing dendritic cell maturation, thus limiting the inflammatory responses. | [105] |
| miR-211 | Decreased | Through inhibiting TGF-β/SMAD signaling, miR-211 improves cell viability. | [109] |
| miR-192-5p | Increased | Suppression of miR-192-5p improved viability of renal cells under hypoxia/reoxygenation conditions. The molecule targets FTO. | [110] |
| miR-187 | Decreased | Increasing the expression of miR-187 reduces podocyte damage. | [111] |
| miR-194 | Decreased | By targeting Rheb, miR-194 reduces inflammation and oxidative stress in renal cells stimulated by hypoxia and reoxygenation. | [112] |
As previously mentioned, ischemic conditions enhance the expression of HIF-1, which regulates the important processes of angiogenesis, survival, and metabolic adaptation [120]. Researchers demonstrated that HIF-1 induces protective effects by regulating the expression of miRNAs. According to Wei et al., HIF-1 upregulates miR-668, a molecule that has antiapoptotic properties. Mechanistically, this miRNA prevented mitochondrial fragmentation by binding to the mitochondrial protein 18 kDa (MTP18) [121]. Similarly, HIF-1 enhances the expression of miR-489, which targets PARP1 and suppresses apoptosis [122].
3. microRNA in Clinical Studies and Their Role as Diagnostic Biomarkers
In previous sections, we have discussed the involvement of miRNA molecules in various pathways associated with the pathogenesis of AKI. It is considered that abnormal expression of these molecules dysregulates signaling pathways, which eventually stimulates pathological mechanisms in the kidney. From the clinical perspective, altered levels of miRNAs could be monitored to detect the developing AKI. Under septic conditions, 27 down- and 13 upregulated molecules were detected in patients who developed AKI [30].
Indeed, the potential role of miRNAs as diagnostic biomarkers has been investigated. For instance, a recent study by Aomatsu et al. suggested that monitoring the serum expression of miR-5100 could distinguish patients with AKI from healthy volunteers. The authors observed a reduced expression of this miRNA in the serum of patients. The receiver operating curve (ROC) analysis highlighted high diagnostic potential with the area under curve (AUC) set at 0.96 [123]. Another approach to the use of miRNAs in the diagnosis of AKI could involve the identification of hub genes significantly associated with the disease. Subsequently, a regulatory set of miRNA molecules could be investigated to create a diagnostic panel. Sun and colleagues performed a similar study and identified 15 hub genes for critically ill patients with AKI. The authors found that miR-6884-5p, miR-532-5p, miR-218-5p, miR-485-5p, and miR-181c-5p represent enriched molecules associated with the identified hub genes [124]. Importantly, these novel molecular biomarkers could be used to detect AKI in patients with different background conditions, thus creating an opportunity for personalized diagnosis panels. Recently, a relationship between the altered expression of miR-22-3p and the occurrence of AKI was observed. We have previously mentioned that downregulated miR-22-3p has been associated with worse kidney functionality in AKI in preclinical models. In septic patients, the occurrence of AKI and the increased severity of the condition reduced the expression of miR-22-3p in serum and urinary samples. The diagnostic potential of using the AUC was 0.851 for serum and 0.911 for urinary miRNA expression, suggesting its promising diagnostic accuracy. Interestingly, Zhang et al. showed that lower expression of miR-22-3p is also associated with worse survival rates [125]. In contrast-induced AKI, the AUC value of circulating miR-188-5p was 0.725 [126]. Furthermore, another condition associated with impaired renal function is acute decompensated heart failure (ADHF) [127]. miR-652-3p and miR-423-5p represent miRNAs recently suggested to have a promising diagnostic potential in diagnosing AKI in patients with ADHF [128,129]. Additionally, miRNAs could potentially serve as diagnostic biomarkers of AKI in transplant recipients, as they are suggested to be involved in the expression and regulation of hub genes associated with renal impairment [130]. Furthermore, miR-21 has been investigated in the diagnostic context. Gaede et al. demonstrated that monitoring of serum miR-21 could predict the occurrence of AKI in patients after major cardiac surgery [131]. Thus, current evidence demonstrates the broad and promising uses of miRNAs as clinical biomarkers in patients with AKI.
4. miRNA-Based Therapeutics
This review, together with numerous other papers, discusses the involvement of the dysregulated expression of miRNAs in the pathogenesis of disease. These pieces of knowledge suggest novel therapeutic targets that could be used in treatments. However, knowledge about the use of miRNA-based therapeutics is still limited; it mainly comes from in vivo animal experiments, and there are very few examples of clinical research articles. For instance, in a study by Deng et al., the use of miR-206 agomir delayed preterm births in mice [132]. In cases of miRNAs contributing to the progression of disorders, these molecules can be targeted by oligonucleotides to reduce their expression. Miravirsen is an miR-122-targeting oligonucleotide that is being investigated in patients with chronic HCV infection, a condition in which miR-122 plays a role in pathogenesis [133].
Unfortunately, systemic administration of miRNA-based therapeutics is associated with certain limitations. These molecules can undergo degradation by RNases or cellular endocytic compartments [134]. To prevent degradation, therapeutics can be modified or encapsulated. This approach has been examined in oncological treatments implementing miRNAs. For example, MRX34 is a liposomal miR-34a mimic, which has been investigated as a potential therapeutic in solid tumors. However, a phase 1 clinical trial was terminated due to adverse events [135], which demonstrates another limitation of miRNA-based drugs that needs to be eliminated. Currently, a significant number of studies are needed to try to form an effective and safe delivery method for miRNA therapeutics [136,137].
5. Conclusions
To conclude, numerous miRNAs have been found to contribute to the pathogenesis of AKI. Various renal injury models, such as sepsis and drug-induced nephrotoxicity, as well as IRI, alter the expression of miRNA, thus changing the gene expression profile. The dysregulated profile of miRNAs is associated with abnormal inflammatory responses, fibrosis, and renal cell apoptosis, as well as abnormal signaling pathways, leading to abnormalities in cell viability and autophagy. Understanding these regulatory mechanisms could lead to the introduction of novel treatment methods that perhaps will induce renal regeneration more rapidly and prevent progression to CKD. Moreover, by accumulating knowledge regarding the expression of miRNAs in patients with AKI, recent studies have started evaluating their diagnostic potential. As conditions associated with renal impairment are frequently severe and involve multi-organ damage, such as sepsis, the use of miRNA biomarkers could help to precisely identify damaged organs or pathological conditions requiring interventions.
Author Contributions
Conceptualization, A.P.; writing—original draft preparation, E.B., K.K. and A.P.; writing—review and editing, E.B., K.K. and A.P.; and supervision, A.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Levey A.S., James M.T. Acute Kidney Injury. Ann. Intern. Med. 2017;167:ITC66–ITC80. doi: 10.7326/AITC201711070. [DOI] [PubMed] [Google Scholar]
- 2.Hoste E.A.J., Kellum J.A., Selby N.M., Zarbock A., Palevsky P.M., Bagshaw S.M., Goldstein S.L., Cerdá J., Chawla L.S. Global epidemiology and outcomes of acute kidney injury. Nat. Rev. Nephrol. 2018;14:607–625. doi: 10.1038/s41581-018-0052-0. [DOI] [PubMed] [Google Scholar]
- 3.Ounci E., Boukabous S., Bkiyar H., Abda N., Bentata Y., Housni B. Acute kidney injury in critically ill patients with COVID-19: Prevalence, risk factors and mortality in eastern Morocco. J. Nephrol. 2022;35:2383–2386. doi: 10.1007/s40620-022-01401-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaudry S., Palevsky P.M., Dreyfuss D. Extracorporeal Kidney-Replacement Therapy for Acute Kidney Injury. N. Engl. J. Med. 2022;386:964–975. doi: 10.1056/NEJMra2104090. [DOI] [PubMed] [Google Scholar]
- 5.Kiełbowski K., Ptaszyński K., Wójcik J., Wojtyś M.E. The role of selected non-coding RNAs in the biology of non-small cell lung cancer. Adv. Med. Sci. 2023;68:121–137. doi: 10.1016/j.advms.2023.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Yuan Y., Xu L., Geng Z., Liu J., Zhang L., Wu Y., He D., Qu P. The role of non-coding RNA network in atherosclerosis. Life Sci. 2021;265:118756. doi: 10.1016/j.lfs.2020.118756. [DOI] [PubMed] [Google Scholar]
- 7.Baker M.A., Davis S.J., Liu P., Pan X., Williams A.M., Iczkowski K.A., Gallagher S.T., Bishop K., Regner K.R., Liu Y., et al. Tissue-Specific MicroRNA Expression Patterns in Four Types of Kidney Disease. J. Am. Soc. Nephrol. 2017;28:2985–2992. doi: 10.1681/ASN.2016121280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farrell C.E., Liu X., Yagan N.O., Suda A.C., Cerqueira D.M., Bodnar A.J., Kashlan O.B., Subramanya A.R., Ho J., Butterworth M.B. MicroRNA-19 is regulated by aldosterone in a sex-specific manner to alter kidney sodium transport. Am. J. Physiol. Cell Physiol. 2024;326:C282–C293. doi: 10.1152/ajpcell.00385.2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kozomara A., Birgaoanu M., Griffiths-Jones S. miRBase: From microRNA sequences to function. Nucleic Acids Res. 2019;47:D155–D162. doi: 10.1093/nar/gky1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee R.C., Feinbaum R.L., Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-Y. [DOI] [PubMed] [Google Scholar]
- 11.Lee Y., Kim M., Han J., Yeom K.H., Lee S., Baek S.H., Kim V.N. MicroRNA genes are transcribed by RNA polymerase II. EMBO J. 2004;23:4051–4060. doi: 10.1038/sj.emboj.7600385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee Y., Ahn C., Han J., Choi H., Kim J., Yim J., Lee J., Provost P., Rådmark O., Kim S., et al. The nuclear RNase III Drosha initiates microRNA processing. Nature. 2003;425:415–419. doi: 10.1038/nature01957. [DOI] [PubMed] [Google Scholar]
- 13.Yi R., Qin Y., Macara I.G., Cullen B.R. Exportin-5 mediates the nuclear export of pre-microRNAs and short hairpin RNAs. Genes. Dev. 2003;17:3011–3016. doi: 10.1101/gad.1158803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bohnsack M.T., Czaplinski K., Gorlich D. Exportin 5 is a RanGTP-dependent dsRNA-binding protein that mediates nuclear export of pre-miRNAs. RNA. 2004;10:185–191. doi: 10.1261/rna.5167604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang H., Kolb F.A., Brondani V., Billy E., Filipowicz W. Human Dicer preferentially cleaves dsRNAs at their termini without a requirement for ATP. EMBO J. 2002;21:5875–5885. doi: 10.1093/emboj/cdf582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu T.X., Rothenberg M.E. MicroRNA. J. Allergy Clin. Immunol. 2018;141:1202–1207. doi: 10.1016/j.jaci.2017.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reichholf B., Herzog V.A., Fasching N., Manzenreither R.A., Sowemimo I., Ameres S.L. Time-Resolved Small RNA Sequencing Unravels the Molecular Principles of MicroRNA Homeostasis. Mol. Cell. 2019;75:756–768.e757. doi: 10.1016/j.molcel.2019.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ender C., Meister G. Argonaute proteins at a glance. J. Cell Sci. 2010;123:1819–1823. doi: 10.1242/jcs.055210. [DOI] [PubMed] [Google Scholar]
- 19.Swolin-Eide D., Forsander G., Pundziute Lyckå A., Novak D., Grillari J., Diendorfer A.B., Hackl M., Magnusson P. Circulating microRNAs in young individuals with long-duration type 1 diabetes in comparison with healthy controls. Sci. Rep. 2023;13:11634. doi: 10.1038/s41598-023-38615-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bartel D.P. MicroRNAs: Target recognition and regulatory functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitchell P.S., Parkin R.K., Kroh E.M., Fritz B.R., Wyman S.K., Pogosova-Agadjanyan E.L., Peterson A., Noteboom J., O’Briant K.C., Allen A., et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA. 2008;105:10513–10518. doi: 10.1073/pnas.0804549105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Godoy P.M., Bhakta N.R., Barczak A.J., Cakmak H., Fisher S., MacKenzie T.C., Patel T., Price R.W., Smith J.F., Woodruff P.G., et al. Large Differences in Small RNA Composition Between Human Biofluids. Cell Rep. 2018;25:1346–1358. doi: 10.1016/j.celrep.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Place R.F., Li L.C., Pookot D., Noonan E.J., Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc. Natl. Acad. Sci. USA. 2008;105:1608–1613. doi: 10.1073/pnas.0707594105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Su Y., Li C., Liu W., Liu Y., Li L., Chen Q. Comprehensive analysis of differentially expressed miRNAs in mice with kidney injury induced by chronic intermittent hypoxia. Front. Genet. 2022;13:918728. doi: 10.3389/fgene.2022.918728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shihana F., Wong W.K.M., Joglekar M.V., Mohamed F., Gawarammana I.B., Isbister G.K., Hardikar A.A., Seth D., Buckley N.A. Urinary microRNAs as non-invasive biomarkers for toxic acute kidney injury in humans. Sci. Rep. 2021;11:9165. doi: 10.1038/s41598-021-87918-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akcay A., Nguyen Q., Edelstein C.L. Mediators of inflammation in acute kidney injury. Mediat. Inflamm. 2009;2009:137072. doi: 10.1155/2009/137072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li J., Tang R.S., Shi Z., Li J.Q. Nuclear factor-κB in rheumatoid arthritis. Int. J. Rheum. Dis. 2020;23:1627–1635. doi: 10.1111/1756-185X.13958. [DOI] [PubMed] [Google Scholar]
- 28.Wu S., Zhou Y., Liang J., Ying P., Situ Q., Tan X., Zhu J. Upregulation of NF-κB by USP24 aggravates ferroptosis in diabetic cardiomyopathy. Free. Radic. Biol. Med. 2024;210:352–366. doi: 10.1016/j.freeradbiomed.2023.11.032. [DOI] [PubMed] [Google Scholar]
- 29.Ren Q., Guo F., Tao S., Huang R., Ma L., Fu P. Flavonoid fisetin alleviates kidney inflammation and apoptosis via inhibiting Src-mediated NF-κB p65 and MAPK signaling pathways in septic AKI mice. Biomed. Pharmacother. 2020;122:109772. doi: 10.1016/j.biopha.2019.109772. [DOI] [PubMed] [Google Scholar]
- 30.Ge Q.M., Huang C.M., Zhu X.Y., Bian F., Pan S.M. Differentially expressed miRNAs in sepsis-induced acute kidney injury target oxidative stress and mitochondrial dysfunction pathways. PLoS ONE. 2017;12:e0173292. doi: 10.1371/journal.pone.0173292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu H., Wang Z. MicroRNA-23a-3p ameliorates acute kidney injury by targeting FKBP5 and NF-κB signaling in sepsis. Cytokine. 2022;155:155898. doi: 10.1016/j.cyto.2022.155898. [DOI] [PubMed] [Google Scholar]
- 32.Li Z.L., Ji J.L., Wen Y., Cao J.Y., Kharbuja N., Ni W.J., Yin D., Feng S.T., Liu H., Lv L.L., et al. HIF-1α is transcriptionally regulated by NF-κB in acute kidney injury. Am. J. Physiol. Renal Physiol. 2021;321:F225–F235. doi: 10.1152/ajprenal.00119.2021. [DOI] [PubMed] [Google Scholar]
- 33.Ye J., Feng H., Peng Z. miR-23a-3p inhibits sepsis-induced kidney epithelial cell injury by suppressing Wnt/β-catenin signaling by targeting wnt5a. Braz. J. Med. Biol. Res. 2022;55:e11571. doi: 10.1590/1414-431x2021e11571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huffstater T., Merryman W.D., Gewin L.S. Wnt/β-Catenin in Acute Kidney Injury and Progression to Chronic Kidney Disease. Semin. Nephrol. 2020;40:126–137. doi: 10.1016/j.semnephrol.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheng S., Zou M., Yang Y., Guan M., Ren S., Wang X., Wang L., Xue Y. miR-23a-3p regulates the inflammatory response and fibrosis in diabetic kidney disease by targeting early growth response 1. Vitr. Cell. Dev. Biol. Anim. 2021;57:763–774. doi: 10.1007/s11626-021-00606-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gao Z., Huang D. lncRNA GAS5-mediated miR-23a-3p promotes inflammation and cell apoptosis by targeting TLR4 in a cell model of sepsis. Mol. Med. Rep. 2021;24:510. doi: 10.3892/mmr.2021.12149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang X., Lu L., Wu C., Zhang F. ATP2B1-AS1 exacerbates sepsis-induced cell apoptosis and inflammation by regulating miR-23a-3p/TLR4 axis. Allergol. Immunopathol. (Madr) 2023;51:17–26. doi: 10.15586/aei.v51i2.782. [DOI] [PubMed] [Google Scholar]
- 38.Kuzmich N.N., Sivak K.V., Chubarev V.N., Porozov Y.B., Savateeva-Lyubimova T.N., Peri F. TLR4 Signaling Pathway Modulators as Potential Therapeutics in Inflammation and Sepsis. Vaccines. 2017;5:34. doi: 10.3390/vaccines5040034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhong Y., Wu S., Yang Y., Li G.Q., Meng L., Zheng Q.Y., Li Y., Xu G.L., Zhang K.Q., Peng K.F. LIGHT aggravates sepsis-associated acute kidney injury via TLR4-MyD88-NF-κB pathway. J. Cell. Mol. Med. 2020;24:11936–11948. doi: 10.1111/jcmm.15815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vázquez-Carballo C., Guerrero-Hue M., García-Caballero C., Rayego-Mateos S., Opazo-Ríos L., Morgado-Pascual J.L., Herencia-Bellido C., Vallejo-Mudarra M., Cortegano I., Gaspar M.L., et al. Toll-Like Receptors in Acute Kidney Injury. Int. J. Mol. Sci. 2021;22:816. doi: 10.3390/ijms22020816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang L., Lin J., Yu T., Zuo Q., Shen B., Zhang H., Liu B., Cai D., Mao H., Zhao H., et al. Identification of plasma miR-106a-5p and miR-30a-5p as potential biomarkers for mesangial proliferative glomerulonephritis. Clin. Biochem. 2020;84:79–86. doi: 10.1016/j.clinbiochem.2020.07.001. [DOI] [PubMed] [Google Scholar]
- 42.Shen Y., Yu J., Jing Y., Zhang J. MiR-106a aggravates sepsis-induced acute kidney injury by targeting THBS2 in mice model. Acta Cir. Bras. 2019;34:e201900602. doi: 10.1590/s0102-865020190060000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu H.P., Ma X.Y., Yang C. Circular RNA TLK1 Promotes Sepsis-Associated Acute Kidney Injury by Regulating Inflammation and Oxidative Stress Through miR-106a-5p/HMGB1 Axis. Front. Mol. Biosci. 2021;8:660269. doi: 10.3389/fmolb.2021.660269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gao Z., Lu L., Chen X. Release of HMGB1 in Podocytes Exacerbates Lipopolysaccharide-Induced Acute Kidney Injury. Mediat. Inflamm. 2021;2021:5220226. doi: 10.1155/2021/5220226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J., Chen Q., Dai Z., Pan H. miR-22 alleviates sepsis-induced acute kidney injury via targeting the HMGB1/TLR4/NF-κB signaling pathway. Int. Urol. Nephrol. 2023;55:409–421. doi: 10.1007/s11255-022-03321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nechemia-Arbely Y., Barkan D., Pizov G., Shriki A., Rose-John S., Galun E., Axelrod J.H. IL-6/IL-6R axis plays a critical role in acute kidney injury. J. Am. Soc. Nephrol. 2008;19:1106–1115. doi: 10.1681/ASN.2007070744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu K.D., Altmann C., Smits G., Krawczeski C.D., Edelstein C.L., Devarajan P., Faubel S. Serum interleukin-6 and interleukin-8 are early biomarkers of acute kidney injury and predict prolonged mechanical ventilation in children undergoing cardiac surgery: A case-control study. Crit. Care. 2009;13:R104. doi: 10.1186/cc7940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shimazui T., Nakada T.A., Tateishi Y., Oshima T., Aizimu T., Oda S. Association between serum levels of interleukin-6 on ICU admission and subsequent outcomes in critically ill patients with acute kidney injury. BMC Nephrol. 2019;20:74. doi: 10.1186/s12882-019-1265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mitazaki S., Kato N., Suto M., Hiraiwa K., Abe S. Interleukin-6 deficiency accelerates cisplatin-induced acute renal failure but not systemic injury. Toxicology. 2009;265:115–121. doi: 10.1016/j.tox.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 50.Su H., Lei C.T., Zhang C. Interleukin-6 Signaling Pathway and Its Role in Kidney Disease: An Update. Front. Immunol. 2017;8:405. doi: 10.3389/fimmu.2017.00405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Y., Zhou X., Wu Y. The miR-26a-5p/IL-6 axis alleviates sepsis-induced acute kidney injury by inhibiting renal inflammation. Ren. Fail. 2022;44:551–561. doi: 10.1080/0886022X.2022.2056486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li S., Jia Y., Xue M., Hu F., Zheng Z., Zhang S., Ren S., Yang Y., Si Z., Wang L., et al. Inhibiting Rab27a in renal tubular epithelial cells attenuates the inflammation of diabetic kidney disease through the miR-26a-5p/CHAC1/NF-kB pathway. Life Sci. 2020;261:118347. doi: 10.1016/j.lfs.2020.118347. [DOI] [PubMed] [Google Scholar]
- 53.Chung Y.H., Huang G.K., Kang C.H., Cheng Y.T., Kao Y.H., Chien Y.S. MicroRNA-26a-5p Restoration Ameliorates Unilateral Ureteral Obstruction-Induced Renal Fibrosis in Mice Through Modulating TGF-β Signaling. Lab. Investig. 2023;103:100131. doi: 10.1016/j.labinv.2023.100131. [DOI] [PubMed] [Google Scholar]
- 54.Lu Y., Liu M., Guo X., Wang P., Zeng F., Wang H., Tang J., Qin Z., Tao T. miR-26a-5p alleviates CFA-induced chronic inflammatory hyperalgesia through Wnt5a/CaMKII/NFAT signaling in mice. CNS Neurosci. Ther. 2023;29:1254–1271. doi: 10.1111/cns.14099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bian J., Ge W., Jiang Z. miR-26a-5p Attenuates Oxidative Stress and Inflammation in Diabetic Retinopathy through the USP14/NF- J. Ophthalmol. 2024;2024:1470898. doi: 10.1155/2024/1470898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li H., Yang T., Fei Z. miR-26a-5p alleviates lipopolysaccharide-induced acute lung injury by targeting the connective tissue growth factor. Mol. Med. Rep. 2021;23:5. doi: 10.3892/mmr.2020.11643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang X., Wang Y., Kong M., Yang J. MiR-22-3p suppresses sepsis-induced acute kidney injury by targeting PTEN. Biosci. Rep. 2020;40:BSR20200527. doi: 10.1042/BSR20200527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhan Y., Zhu M., Liu S., Lu J., Ni Z., Cai H., Zhang W. MicroRNA-93 inhibits the apoptosis and inflammatory response of tubular epithelial cells via the PTEN/AKT/mTOR pathway in acute kidney injury. Mol. Med. Rep. 2021;24:666. doi: 10.3892/mmr.2021.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sang Z., Dong S., Zhang P., Wei Y. miR-214 ameliorates sepsis-induced acute kidney injury via PTEN/AKT/mTOR-regulated autophagy. Mol. Med. Rep. 2021;24:683. doi: 10.3892/mmr.2021.12322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xie X., Qu P., Wu H., Liu P., Luo J., Chi J., Liu X., Chen X., Xu C. Circulating exosomal miR-21 mediates HUVEC proliferation and migration through PTEN/PI3K/AKT in Crohn’s disease. Ann. Transl. Med. 2022;10:258. doi: 10.21037/atm-22-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu H.Y., Zhang Y.Y., Zhu B.L., Feng F.Z., Yan H., Zhang H.Y., Zhou B. miR-21 regulates the proliferation and apoptosis of ovarian cancer cells through PTEN/PI3K/AKT. Eur. Rev. Med. Pharmacol. Sci. 2019;23:4149–4155. doi: 10.26355/eurrev_201905_17917. [DOI] [PubMed] [Google Scholar]
- 62.Zhu J., Liu B., Wang Z., Wang D., Ni H., Zhang L., Wang Y. Exosomes from nicotine-stimulated macrophages accelerate atherosclerosis through miR-21-3p/PTEN-mediated VSMC migration and proliferation. Theranostics. 2019;9:6901–6919. doi: 10.7150/thno.37357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fu D., Dong J., Li P., Tang C., Cheng W., Xu Z., Zhou W., Ge J., Xia C., Zhang Z. MiRNA-21 has effects to protect kidney injury induced by sepsis. Biomed. Pharmacother. 2017;94:1138–1144. doi: 10.1016/j.biopha.2017.07.098. [DOI] [PubMed] [Google Scholar]
- 64.Pan T., Jia P., Chen N., Fang Y., Liang Y., Guo M., Ding X. Delayed Remote Ischemic Preconditioning ConfersRenoprotection against Septic Acute Kidney Injury via Exosomal miR-21. Theranostics. 2019;9:405–423. doi: 10.7150/thno.29832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wei W., Yao Y.Y., Bi H.Y., Zhai Z., Gao Y. miR-21 protects against lipopolysaccharide-stimulated acute kidney injury and apoptosis by targeting CDK6. Ann. Transl. Med. 2020;8:303. doi: 10.21037/atm.2020.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhao S., Li W., Yu W., Rao T., Li H., Ruan Y., Yuan R., Li C., Ning J., Li S., et al. Exosomal miR-21 from tubular cells contributes to renal fibrosis by activating fibroblasts via targeting PTEN in obstructed kidneys. Theranostics. 2021;11:8660–8673. doi: 10.7150/thno.62820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang L., Wang K., Tian Z. miR-128-3p Inhibits NRP1 Expression and Promotes Inflammatory Response to Acute Kidney Injury in Sepsis. Inflammation. 2020;43:1772–1779. doi: 10.1007/s10753-020-01251-8. [DOI] [PubMed] [Google Scholar]
- 68.Wu L., Zhang G., Guo C., Zhao X., Shen D., Yang N. MiR-128-3p mediates TNF-α-induced inflammatory responses by regulating Sirt1 expression in bone marrow mesenchymal stem cells. Biochem. Biophys. Res. Commun. 2020;521:98–105. doi: 10.1016/j.bbrc.2019.10.083. [DOI] [PubMed] [Google Scholar]
- 69.Pang Y., Luo D., Wang S. miR-128-3p inhibits the inflammation by targeting MAPK6 in penicillin-induced astrocytes. Neuroreport. 2022;33:742–749. doi: 10.1097/WNR.0000000000001840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu X., Cui H., Bai Q., Piao H., Song Y., Yan G. miR-128-3p alleviates airway inflammation in asthma by targeting SIX1 to regulate mitochondrial fission and fusion. Int. Immunopharmacol. 2024;130:111703. doi: 10.1016/j.intimp.2024.111703. [DOI] [PubMed] [Google Scholar]
- 71.Yang P., Han J., Li S., Luo S., Tu X., Ye Z. miR-128-3p inhibits apoptosis and inflammation in LPS-induced sepsis by targeting TGFBR2. Open Med. 2021;16:274–283. doi: 10.1515/med-2021-0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Borkan S.C. The Role of BCL-2 Family Members in Acute Kidney Injury. Semin. Nephrol. 2016;36:237–250. doi: 10.1016/j.semnephrol.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 73.Li H., Duan J., Zhang T., Fu Y., Xu Y., Miao H., Ge X. miR-16-5p aggravates sepsis-associated acute kidney injury by inducing apoptosis. Ren. Fail. 2024;46:2322688. doi: 10.1080/0886022X.2024.2322688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang W.Q., Wang H.J., Li Y.Z., Du X.F., Hao X.L., Jiang H.M., Yang L.H. Inhibition of microRNA-543 alleviates sepsis-induced acute kidney injury via targeting Bcl-2. Eur. Rev. Med. Pharmacol. Sci. 2022;26:2305–2312. doi: 10.26355/eurrev_202204_28460. [DOI] [PubMed] [Google Scholar]
- 75.Zheng C., Wu D., Shi S., Wang L. miR-34b-5p promotes renal cell inflammation and apoptosis by inhibiting aquaporin-2 in sepsis-induced acute kidney injury. Ren. Fail. 2021;43:291–301. doi: 10.1080/0886022X.2021.1871922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Yi H.X., Jiang S.Y., Yu L.H., Chen K., Yang Z.X., Wu Q. MicroRNA 181a-2-3p Alleviates the Apoptosis of Renal Tubular Epithelial Cells via Targeting GJB2 in Sepsis-Induced Acute Kidney Injury. Mol. Cell. Biol. 2021;41:e0001621. doi: 10.1128/MCB.00016-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shi L., Zhang Y., Xia Y., Li C., Song Z., Zhu J. MiR-150-5p protects against septic acute kidney injury via repressing the MEKK3/JNK pathway. Cell. Signal. 2021;86:110101. doi: 10.1016/j.cellsig.2021.110101. [DOI] [PubMed] [Google Scholar]
- 78.Mao W., Wang X., Zhang Y., Zhu H., Dai L., Chen J. Nuclear factor-kappa B p50-induced microRNA-20a-3p plays a detrimental role in sepsis-induced acute kidney injury. Cell. Mol. Biol. 2023;69:198–202. doi: 10.14715/cmb/2023.69.8.30. [DOI] [PubMed] [Google Scholar]
- 79.Wu J., Li D.D., Li J.Y., Yin Y.C., Li P.C., Qiu L., Chen L.M. Identification of microRNA-mRNA networks involved in cisplatin-induced renal tubular epithelial cells injury. Eur. J. Pharmacol. 2019;851:1–12. doi: 10.1016/j.ejphar.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 80.Xia Y., Pan W., Xiao X., Zhou X., Gu W., Liu Y., Zhao Y., Li L., Zheng C., Liu J., et al. MicroRNA-483-5p accentuates cisplatin-induced acute kidney injury by targeting GPX3. Lab. Investig. 2022;102:589–601. doi: 10.1038/s41374-022-00737-3. [DOI] [PubMed] [Google Scholar]
- 81.Wu Y., Shi H., Xu Y., Shu G., Xiao Y., Hong G., Xu S. Targeted Restoration of GPX3 Attenuates Renal Ischemia/Reperfusion Injury by Balancing Selenoprotein Expression and Inhibiting ROS-mediated Mitochondrial Apoptosis. Transplantation. 2024 doi: 10.1097/TP.0000000000005068. [DOI] [PubMed] [Google Scholar]
- 82.Zhou J., Xiao C., Zheng S., Wang Q., Zhu H., Zhang Y., Wang R. MicroRNA-214-3p aggravates ferroptosis by targeting GPX4 in cisplatin-induced acute kidney injury. Cell Stress. Chaperones. 2022;27:325–336. doi: 10.1007/s12192-022-01271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang Y., Quan F., Cao Q., Lin Y., Yue C., Bi R., Cui X., Yang H., Yang Y., Birnbaumer L., et al. Quercetin alleviates acute kidney injury by inhibiting ferroptosis. J. Adv. Res. 2021;28:231–243. doi: 10.1016/j.jare.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhu B., He J., Ye X., Pei X., Bai Y., Gao F., Guo L., Yong H., Zhao W. Role of Cisplatin in Inducing Acute Kidney Injury and Pyroptosis in Mice via the Exosome miR-122/ELAVL1 Regulatory Axis. Physiol. Res. 2023;72:753–765. doi: 10.33549/physiolres.935129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yan M., Tang C., Ma Z., Huang S., Dong Z. DNA damage response in nephrotoxic and ischemic kidney injury. Toxicol. Appl. Pharmacol. 2016;313:104–108. doi: 10.1016/j.taap.2016.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Taguchi K., Sugahara S., Elias B.C., Pabla N.S., Canaud G., Brooks C.R. IL-22 is secreted by proximal tubule cells and regulates DNA damage response and cell death in acute kidney injury. Kidney Int. 2024;105:99–114. doi: 10.1016/j.kint.2023.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yamashita N., Nakai K., Nakata T., Nakamura I., Kirita Y., Matoba S., Humphreys B.D., Tamagaki K., Kusaba T. Cumulative DNA damage by repeated low-dose cisplatin injection promotes the transition of acute to chronic kidney injury in mice. Sci. Rep. 2021;11:20920. doi: 10.1038/s41598-021-00392-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yin Q., Zhao Y.J., Ni W.J., Tang T.T., Wang Y., Cao J.Y., Yin D., Wen Y., Li Z.L., Zhang Y.L., et al. MiR-155 deficiency protects renal tubular epithelial cells from telomeric and genomic DNA damage in cisplatin-induced acute kidney injury. Theranostics. 2022;12:4753–4766. doi: 10.7150/thno.72456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fu S., Hu X., Ma Z., Wei Q., Xiang X., Li S., Wen L., Liang Y., Dong Z. p53 in Proximal Tubules Mediates Chronic Kidney Problems after Cisplatin Treatment. Cells. 2022;11:712. doi: 10.3390/cells11040712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jiang M., Wei Q., Wang J., Du Q., Yu J., Zhang L., Dong Z. Regulation of PUMA-alpha by p53 in cisplatin-induced renal cell apoptosis. Oncogene. 2006;25:4056–4066. doi: 10.1038/sj.onc.1209440. [DOI] [PubMed] [Google Scholar]
- 91.Chen G., Xue H., Zhang X., Ding D., Zhang S. p53 inhibition attenuates cisplatin-induced acute kidney injury through microRNA-142-5p regulating SIRT7/NF-κB. Ren. Fail. 2022;44:368–380. doi: 10.1080/0886022X.2022.2039195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miyasato Y., Yoshizawa T., Sato Y., Nakagawa T., Kakizoe Y., Kuwabara T., Adachi M., Ianni A., Braun T., Komohara Y., et al. Sirtuin 7 Deficiency Ameliorates Cisplatin-induced Acute Kidney Injury through Regulation of the Inflammatory Response. Sci. Rep. 2018;8:5927. doi: 10.1038/s41598-018-24257-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yang A., Liu F., Guan B., Luo Z., Lin J., Fang W., Liu L., Zuo W. p53 induces miR-199a-3p to suppress mechanistic target of rapamycin activation in cisplatin-induced acute kidney injury. J. Cell. Biochem. 2019;120:17625–17634. doi: 10.1002/jcb.29030. [DOI] [PubMed] [Google Scholar]
- 94.Wang Y., Liu Z., Shu S., Cai J., Tang C., Dong Z. AMPK/mTOR Signaling in Autophagy Regulation During Cisplatin-Induced Acute Kidney Injury. Front. Physiol. 2020;11:619730. doi: 10.3389/fphys.2020.619730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bhatt K., Zhou L., Mi Q.S., Huang S., She J.X., Dong Z. MicroRNA-34a is induced via p53 during cisplatin nephrotoxicity and contributes to cell survival. Mol. Med. 2010;16:409–416. doi: 10.2119/molmed.2010.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Qin W., Xie W., Yang X., Xia N., Yang K. Inhibiting microRNA-449 Attenuates Cisplatin-Induced Injury in NRK-52E Cells Possibly via Regulating the SIRT1/P53/BAX Pathway. Med. Sci. Monit. 2016;22:818–823. doi: 10.12659/MSM.897187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nagasaka M., Miyajima C., Aoki H., Aoyama M., Morishita D., Inoue Y., Hayashi H. Insights into Regulators of p53 Acetylation. Cells. 2022;11:3825. doi: 10.3390/cells11233825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mao W., Zhang L., Wang Y., Sun S., Wu J., Sun J., Zou X., Chen M., Zhang G. Cisplatin induces acute kidney injury by downregulating miR-30e-5p that targets Galnt3 to activate the AMPK signaling pathway. Environ. Toxicol. 2024;39:1567–1580. doi: 10.1002/tox.24054. [DOI] [PubMed] [Google Scholar]
- 99.de Almeida D.C., Bassi E.J., Azevedo H., Anderson L., Origassa C.S., Cenedeze M.A., de Andrade-Oliveira V., Felizardo R.J., da Silva R.C., Hiyane M.I., et al. A Regulatory miRNA-mRNA Network Is Associated with Tissue Repair Induced by Mesenchymal Stromal Cells in Acute Kidney Injury. Front. Immunol. 2016;7:645. doi: 10.3389/fimmu.2016.00645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nørgård M., Svenningsen P. Acute Kidney Injury by Ischemia/Reperfusion and Extracellular Vesicles. Int. J. Mol. Sci. 2023;24:15312. doi: 10.3390/ijms242015312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Du Y., Ning J.Z. MiR-182 Promotes Ischemia/Reperfusion-Induced Acute Kidney Injury in Rat by Targeting FoxO3. Urol. Int. 2021;105:687–696. doi: 10.1159/000515649. [DOI] [PubMed] [Google Scholar]
- 102.Li L., Kang H., Zhang Q., D’Agati V.D., Al-Awqati Q., Lin F. FoxO3 activation in hypoxic tubules prevents chronic kidney disease. J. Clin. Investig. 2019;129:2374–2389. doi: 10.1172/JCI122256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Meng F., Zhang Z., Chen C., Liu Y., Yuan D., Hei Z., Luo G. PI3K/AKT activation attenuates acute kidney injury following liver transplantation by inducing FoxO3a nuclear export and deacetylation. Life Sci. 2021;272:119119. doi: 10.1016/j.lfs.2021.119119. [DOI] [PubMed] [Google Scholar]
- 104.Li C., Han S., Zhu J., Cheng F. MiR-132-3p activation aggravates renal ischemia-reperfusion injury by targeting Sirt1/PGC1alpha axis. Cell. Signal. 2023;110:110801. doi: 10.1016/j.cellsig.2023.110801. [DOI] [PubMed] [Google Scholar]
- 105.Song N., Zhang T., Xu X., Lu Z., Yu X., Fang Y., Hu J., Jia P., Teng J., Ding X. miR-21 Protects against Ischemia/Reperfusion-Induced Acute Kidney Injury by Preventing Epithelial Cell Apoptosis and Inhibiting Dendritic Cell Maturation. Front. Physiol. 2018;9:790. doi: 10.3389/fphys.2018.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jia P., Pan T., Xu S., Fang Y., Song N., Guo M., Liang Y., Xu X., Ding X. Depletion of miR-21 in dendritic cells aggravates renal ischemia-reperfusion injury. FASEB J. 2020;34:11729–11740. doi: 10.1096/fj.201903222RR. [DOI] [PubMed] [Google Scholar]
- 107.Zhang W., Shu L. Upregulation of miR-21 by Ghrelin Ameliorates Ischemia/Reperfusion-Induced Acute Kidney Injury by Inhibiting Inflammation and Cell Apoptosis. DNA Cell Biol. 2016;35:417–425. doi: 10.1089/dna.2016.3231. [DOI] [PubMed] [Google Scholar]
- 108.Hoppe B., Pietsch S., Franke M., Engel S., Groth M., Platzer M., Englert C. MiR-21 is required for efficient kidney regeneration in fish. BMC Dev. Biol. 2015;15:43. doi: 10.1186/s12861-015-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shang J., Sun S., Zhang L., Hao F., Zhang D. miR-211 alleviates ischaemia/reperfusion-induced kidney injury by targeting TGFβR2/TGF-β/SMAD3 pathway. Bioengineered. 2020;11:547–557. doi: 10.1080/21655979.2020.1765501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang C., Guan G., Wang J., Wei H., Cai J. MicroRNA-192-5p downregulates Fat Mass and Obesity-associated Protein to aggravate renal ischemia/reperfusion injury. Ren. Fail. 2023;45:2285869. doi: 10.1080/0886022X.2023.2285869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yue J., Si Y., Zhu T., Yang J., Xu X., Fang Y., Fu W. MicroRNA-187 Reduces Acute Ischemic Renal Podocyte Injury via Targeting Acetylcholinesterase. J. Surg. Res. 2019;244:302–311. doi: 10.1016/j.jss.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 112.Shen Y., Zhao Y., Wang L., Zhang W., Liu C., Yin A. MicroRNA-194 overexpression protects against hypoxia/reperfusion-induced HK-2 cell injury through direct targeting Rheb. J. Cell. Biochem. 2019;120:8311–8318. doi: 10.1002/jcb.28114. [DOI] [PubMed] [Google Scholar]
- 113.Chen L., Fang H., Li X., Yu P., Guan Y., Xiao C., Deng Z., Hei Z., Chen C., Luo C. Connexin32 gap junction channels deliver miR155-3p to mediate pyroptosis in renal ischemia-reperfusion injury. Cell Commun. Signal. 2024;22:121. doi: 10.1186/s12964-023-01443-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Vinas J.L., Burger D., Zimpelmann J., Haneef R., Knoll W., Campbell P., Gutsol A., Carter A., Allan D.S., Burns K.D. Transfer of microRNA-486-5p from human endothelial colony forming cell-derived exosomes reduces ischemic kidney injury. Kidney Int. 2016;90:1238–1250. doi: 10.1016/j.kint.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 115.Vinas J.L., Spence M., Porter C.J., Douvris A., Gutsol A., Zimpelmann J.A., Campbell P.A., Burns K.D. micro-RNA-486-5p protects against kidney ischemic injury and modifies the apoptotic transcriptome in proximal tubules. Kidney Int. 2021;100:597–612. doi: 10.1016/j.kint.2021.05.034. [DOI] [PubMed] [Google Scholar]
- 116.Ma M., Fu L., Jia Z., Zhong Q., Huang Z., Wang X., Fan Y., Lin T., Song T. miR-17-5p attenuates kidney ischemia-reperfusion injury by inhibiting the PTEN and BIM pathways. Ann. Transl. Med. 2021;9:1545. doi: 10.21037/atm-21-4678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhou J., Jia L., Hu Z., Wang Y. Pharmacological Inhibition of PTEN Aggravates Acute Kidney Injury. Sci. Rep. 2017;7:9503. doi: 10.1038/s41598-017-10336-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mogilyansky E., Rigoutsos I. The miR-17/92 cluster: A comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ. 2013;20:1603–1614. doi: 10.1038/cdd.2013.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chiba T., Cerqueira D.M., Li Y., Bodnar A.J., Mukherjee E., Pfister K., Phua Y.L., Shaikh K., Sanders B.T., Hemker S.L., et al. Endothelial-Derived miR-17 approximately 92 Promotes Angiogenesis to Protect against Renal Ischemia-Reperfusion Injury. J. Am. Soc. Nephrol. 2021;32:553–562. doi: 10.1681/ASN.2020050717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sethi K., Rao K., Bolton D., Patel O., Ischia J. Targeting HIF-1alpha to Prevent Renal Ischemia-Reperfusion Injury: Does It Work? Int. J. Cell Biol. 2018;2018:9852791. doi: 10.1155/2018/9852791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wei Q., Sun H., Song S., Liu Y., Liu P., Livingston M.J., Wang J., Liang M., Mi Q.S., Huo Y., et al. MicroRNA-668 represses MTP18 to preserve mitochondrial dynamics in ischemic acute kidney injury. J. Clin. Investig. 2018;128:5448–5464. doi: 10.1172/JCI121859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wei Q., Liu Y., Liu P., Hao J., Liang M., Mi Q.S., Chen J.K., Dong Z. MicroRNA-489 Induction by Hypoxia-Inducible Factor-1 Protects against Ischemic Kidney Injury. J. Am. Soc. Nephrol. 2016;27:2784–2796. doi: 10.1681/ASN.2015080870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Aomatsu A., Kaneko S., Yanai K., Ishii H., Ito K., Hirai K., Ookawara S., Kobayashi Y., Sanui M., Morishita Y. MicroRNA expression profiling in acute kidney injury. Transl. Res. 2022;244:1–31. doi: 10.1016/j.trsl.2021.11.010. [DOI] [PubMed] [Google Scholar]
- 124.Sun T., Cao Y., Huang T., Sang Y., Dai Y., Tao Z. Comprehensive analysis of fifteen hub genes to identify a promising diagnostic model, regulated networks, and immune cell infiltration in acute kidney injury. J. Clin. Lab. Anal. 2022;36:e24709. doi: 10.1002/jcla.24709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhang H., Che L., Wang Y., Zhou H., Gong H., Man X., Zhao Q. Deregulated microRNA-22-3p in patients with sepsis-induced acute kidney injury serves as a new biomarker to predict disease occurrence and 28-day survival outcomes. Int. Urol. Nephrol. 2021;53:2107–2116. doi: 10.1007/s11255-021-02784-z. [DOI] [PubMed] [Google Scholar]
- 126.Yu R., Wu C., Xiao Y., Li Q., Chen J., Song J., Chen H., Wang Z., Wang W. The clinical predictive value and regulation mechanism of microRNA-188-5p in contrast-induced acute kidney injury. Biochem. Biophys. Res. Commun. 2023;679:215–223. doi: 10.1016/j.bbrc.2023.09.019. [DOI] [PubMed] [Google Scholar]
- 127.Schulze P.C., Bogoviku J., Westphal J., Aftanski P., Haertel F., Grund S., von Haehling S., Schumacher U., Mobius-Winkler S., Busch M. Effects of Early Empagliflozin Initiation on Diuresis and Kidney Function in Patients With Acute Decompensated Heart Failure (EMPAG-HF) Circulation. 2022;146:289–298. doi: 10.1161/CIRCULATIONAHA.122.059038. [DOI] [PubMed] [Google Scholar]
- 128.Liu J., Zhang H., Li X., Wang L., Yu H., Huang J., Liu Q., Wang C., Jiang A. Diagnostic and prognostic significance of aberrant miR-652-3p levels in patients with acute decompensated heart failure and acute kidney injury. J. Int. Med. Res. 2020;48:300060520967829. doi: 10.1177/0300060520967829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhang H., Liu J., Li X., Wang L., Yu H., Huang J., Liu Q., Wang C., Jiang A. MicroRNA-423-5p as a biomarker for early diagnosis and outcome prediction of acute kidney injury in patients with acute decompensated heart failure. Int. J. Urol. 2021;28:25–32. doi: 10.1111/iju.14380. [DOI] [PubMed] [Google Scholar]
- 130.Pei J., Zhang J., Yu C., Luo J., Wen S., Hua Y., Wei G. Transcriptomics-based exploration of shared M1-type macrophage-related biomarker in acute kidney injury after kidney transplantation and acute rejection after kidney transplantation. Transpl. Immunol. 2024;85:102066. doi: 10.1016/j.trim.2024.102066. [DOI] [PubMed] [Google Scholar]
- 131.Gaede L., Liebetrau C., Blumenstein J., Troidl C., Dörr O., Kim W.K., Gottfried K., Voss S., Berkowitsch A., Walther T., et al. Plasma microRNA-21 for the early prediction of acute kidney injury in patients undergoing major cardiac surgery. Nephrol. Dial. Transplant. 2016;31:760–766. doi: 10.1093/ndt/gfw007. [DOI] [PubMed] [Google Scholar]
- 132.Deng W., Chen L., Wen B., Wang X., Wang L., Yang F., Chen Y., Bao J., Zhang G., Ji K., et al. MicroRNA-206 functions as a potential oligonucleotide therapeutics in preterm birth. Chin. Med. J. 2024;137:1000–1002. doi: 10.1097/CM9.0000000000002876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.van der Ree M.H., van der Meer A.J., van Nuenen A.C., de Bruijne J., Ottosen S., Janssen H.L., Kootstra N.A., Reesink H.W. Miravirsen dosing in chronic hepatitis C patients results in decreased microRNA-122 levels without affecting other microRNAs in plasma. Aliment. Pharmacol. Ther. 2016;43:102–113. doi: 10.1111/apt.13432. [DOI] [PubMed] [Google Scholar]
- 134.De Santi C., Greene C.M. Challenges facing microRNA therapeutics for cystic fibrosis lung disease. Epigenomics. 2020;12:179–181. doi: 10.2217/epi-2019-0395. [DOI] [PubMed] [Google Scholar]
- 135.Hong D.S., Kang Y.K., Borad M., Sachdev J., Ejadi S., Lim H.Y., Brenner A.J., Park K., Lee J.L., Kim T.Y., et al. Phase 1 study of MRX34, a liposomal miR-34a mimic, in patients with advanced solid tumours. Br. J. Cancer. 2020;122:1630–1637. doi: 10.1038/s41416-020-0802-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Alswailem R., Alqahtani F.Y., Aleanizy F.S., Alrfaei B.M., Badran M., Alqahtani Q.H., Abdelhady H.G., Alsarra I. MicroRNA-219 loaded chitosan nanoparticles for treatment of glioblastoma. Artif. Cells Nanomed. Biotechnol. 2022;50:198–207. doi: 10.1080/21691401.2022.2092123. [DOI] [PubMed] [Google Scholar]
- 137.Thibonnier M., Ghosh S. Strategy for Pre-Clinical Development of Active Targeting MicroRNA Oligonucleotide Therapeutics for Unmet Medical Needs. Int. J. Mol. Sci. 2023;24:7126. doi: 10.3390/ijms24087126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.