Abstract
Spinal cord injury (SCI) results in significant neural damage and inhibition of axonal regeneration due to an imbalanced microenvironment. Extensive evidence supports the efficacy of mesenchymal stem cell (MSC) transplantation as a therapeutic approach for SCI. This review aims to present an overview of MSC regulation on the imbalanced microenvironment following SCI, specifically focusing on inflammation, neurotrophy and axonal regeneration. The application, limitations and future prospects of MSC transplantation are discussed as well. Generally, a comprehensive perspective is provided for the clinical translation of MSC transplantation for SCI.
Keywords: Spinal cord injury, Mesenchymal stem cells, Microenvironment imbalance, Paracrine
Introduction
SCI is a catastrophic event that results in extensive cellular death and significant damage to the central nervous system (CNS), due to primary injury and subsequent secondary cascades [1–3]. Given its low cure rate and high mortality rate, SCI imposes a substantial burden on a global scale [4]. The initial mechanical trauma directly harms the tissue and triggers an inflammatory amplification. Additionally, the deficiency of neurotrophic factors and disruption of vascular integrity compromise the nutrient microenvironment. The formation of inhibitory scar tissue, coupled with the insufficient intrinsic mechanisms, ultimately hinders axonal regeneration, leading to failure in the recovery process [5, 6].
MSCs are pluripotent stem cells derived from multiple tissues with self-renew and multiple differentiation ability, serving promising candidates for cell transplantation therapy in many diseases, particularly in the treatment of SCI [7]. (i) The powerful paracrine ability comprehensively improves the imbalanced microenvironment [8, 9]. (ii) MSCs can be separated and cultured easily while maintain active after multiple passages [10]. (iii) Numerous chemokine receptors (CXCR1, CXCR2 and CCR2 etc.) expressed on the surface of MSCs allow them to target the lesion site precisely without additional modification [11]. (iv) The low immunogenicity and tumorigenicity due to un-prominent surface antigen, makes it a safe choice for clinical therapy [12, 13]. Nevertheless, due to variations in different experimental focus, the existing literature on MSC regulation for the imbalanced microenvironment following SCI lacks a comprehensive understanding.
This review mainly elucidates the comprehensive mechanism by which MSCs regulate the imbalanced microenvironment following SCI, especially in inflammation, neurotrophy and axonal regeneration. A summary of the application of MSCs is also discussed, highlighting its limitations and future directions.
Microenvironment imbalance after SCI
Following SCI, the destruction of neurons, glial cells and other cells, as well as the disruption of the surrounding environment, have been observed [1, 14]. Previous studies extensively examined the phases (acute, subacute, intermediate and chronic) following SCI and established an international consensus [1, 5, 15]. Therefore, a novel perspective on the imbalance of the microenvironment after SCI is aimed to be offered (Fig. 1).
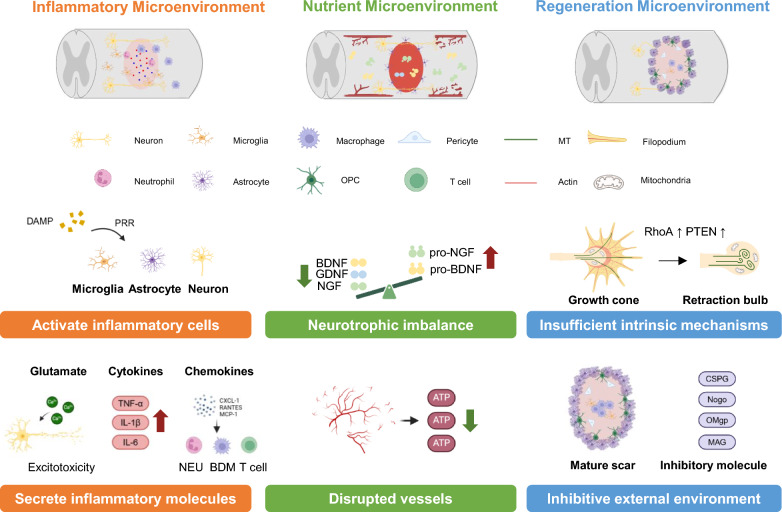
Fig. 1.
The imbalanced microenvironment after SCI. In inflammatory microenvironment, DAMP released by dead cells binds to PRRs on microglia, astrocytes and neurons to activate the initial inflammatory response. Glutamate released due to massive neuronal death leads to excitotoxicity. Cytokines such as TNF-α, IL-1β and IL-6 secreted by microglia and astrocytes are upregulated rapidly. Chemokines attract immune cells to the lesion site leading to cascade amplification. In neurotrophic microenvironment. The upregulation of NF and downregulation of pro-NF lead to a neurotrophic imbalance. Disrupted vessels result in an insufficient energy supply, culminating in cytotoxic edema and demyelination. In regeneration microenvironment, the silence of intrinsic regenerative mechanism (upregulation of RhoA and PTEN) transforms the growth cone into a retraction bulb. The inhibitive external microenvironment, including mature scar and inhibitory molecules further impedes axonal regeneration
Activation and cascade amplification of inflammation
In the context of SCI, inflammation assumes a pivotal role as the initial stress response. It functions as a dual-edged sword, wherein appropriate inflammation safeguards the tissue and hampers the propagation of damage. Conversely, excessive inflammation and the subsequent cascade of injuries contribute to additional neuronal demise and impede the regeneration of axons [5, 6].
The pattern recognition receptor (PRR) is recognized as the primary responder [16]. Following SCI, deceased cells discharge their contents, including the damage-associated molecular pattern (DAMP), which binds to PRR (Toll-like receptors (TLRs), Nod-like receptors (NLRs) etc.) expressed on microglial cells, astrocytes and neurons, thereby initiating the initial inflammatory response [16]. In the early stage, pro-inflammatory cytokines such as tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) and IL-1β, primarily secreted by astrocytes and microglia cells, experience a significant surge, resulting in heightened cellular demise [17–22]. Extensive neuronal apoptosis triggers massive release of glutamate, which induces excessive influx of calcium on neurons and glial cells called excitotoxicity, leading to mitochondrial dysfunction and cellular demise [23–26].
Chemokines such as CXCL-1, RANTES and MCP-1 are increasingly expressed after SCI to attract immune cells from blood to the lesion site, infiltrating the broken blood spinal cord barrier (BSCB) [27–30]. In mice models, neutrophils reach their peak at 24 h after SCI and subsequently release reactive oxygen species (ROS) and reactive nitrogen species (RNS), which induces lipid peroxidation to clear cellular debris. [31, 32]. Blood-derived macrophage (BDM) and microglial cells reach their peak at 7 days [33, 34]. The pro-inflammatory cytokines and chemokines secreted by them not only clear debris but also induce axon retraction and dieback, which exacerbates inflammatory response [35]. T cells reach their peak at 14 days [36]. After SCI, the balance between pro- and anti-inflammatory phenotype disrupts, for cytotoxic T-cells (Th1 and Th17) more than 90% while regulatory T-cells (Th2 and Treg) less than 10% [37], leading to an increased release of IFN-γ, TNF-β and IL-17 [38, 39]. The perforin produced by CD8 T cells exacerbates secondary injury by disrupting the BSCB [40].
Regardless of the initial cause of inflammation or the subsequent cascade resulting from various aforementioned factors, it will give rise to a positive feedback loop, ultimately leading to an overexpression of inflammation and excessive tissue damage.
Damaged neurotrophic environment
The neurotrophic factor (NF) is comprised of nerve growth factor (NGF), brain derived neurotrophic factor (BDNF), neurotrophin-3 (NT-3) and neurotrophin-4/5 (NT-4/5), binding to tropomyosin-related kinase (Trk) receptors and non-specific receptor p75 [41] to promote neuronal survival, modify glia phenotype and enhance axonal plasticity [42]. NF is initially synthesized as a precursor, some of which can function as distinct ligands by binding to the p75 receptor and sortilin to induce cell death [41, 42]. Following SCI, neurotrophic factor precursor (pro-NF) increases. It leads to a relative deficiency of NF, which disrupts the balance of the neurotrophic microenvironment. This disruption in the balance between NF and pro-NF serves as the pathological foundation for the neurotrophic microenvironment. Pro-BDNF increases within 1 to 3 days after SCI, which acts as a suppressor for macrophage migration and infiltration [43]. Pro-NGF induces apoptosis at nanomolar concentrations. It can mediate oligodendrocyte death after SCI and break the integrity of myelin sheath [44–46]. Several studies have demonstrated the efficiency of reducing pro-NF in treatment of SCI, which provides evidence of the detrimental impact of pro-NF [47–49].
Another manifestation of the imbalanced neurotrophic microenvironment is the damaged vasculature. The initial injury directly impairs the blood vessels, and the ensuing cascade damage further injures the vascular endothelial cells. This results in a lack of energy supply, impairing ATP-dependent ion pumps on the cell membrane. Consequently, the permeability of the membrane increases, causing an imbalance of ions across it [14]. Excessive intracellular sodium leads to cytotoxic edema and exacerbates acidosis [50], while the potassium imbalance hinders the transmission of active potentials and leads to demyelination [51].
Inhibition of axonal regeneration
The achievement of favorable axonal regeneration continues to be of utmost importance, serving as the structural basis for functional recovery. Nevertheless, the inadequate activation of intrinsic mechanisms and the presence of inhibitory external factors pose significant challenges in attaining the desired regenerative outcomes.
Insufficient intrinsic regeneration mechanisms
The cytoskeleton regulates the extension of the axon. It is mainly composed of actin and microtubules (MT). During the elongation, actin extends to form filopodia, along which MT extends outward to form the cytoskeleton of axon. However, the orderly structure is disrupted after SCI, forming a malnourished structure called retraction bulb, in which MT and actin highly overlap. This is considered as the intrinsic structure basis for the failure of axonal regeneration [52].
The RhoA/ROCK pathway has been extensively investigated for regulating the cytoskeleton and is commonly regarded detrimental for axonal regeneration [52]. After SCI, Rock activates LIMK1, which phosphorylates cofilin at Ser-3, inhibiting its depolymerization function for actin [53]. Rock also phosphorylates collapsin response mediator protein-2 (CRMP-2), thereby impeding the interaction between CRMP-2 and MTs [54]. These result in the inhibition of MT extension and axon growth.
The PI3K-mTOR pathway plays a crucial role in regulating cell growth and its inhibition after SCI leads to unsuccessful axonal regeneration. PTEN is an upstream component, which can diminish mTOR activity and reduce its mRNA translation. Inhibiting PTEN while activating mTOR show great axonal regeneration after SCI [55–57].
The inadequate understanding of the intrinsic regeneration mechanism necessitates further investigation. It is emphasized for the significance of comprehending the intrinsic pathway accurately, rather than relying on imprecise adjustments. A precise understanding of the upstream and downstream components is essential to identify the pivotal element which can stimulate intrinsic regeneration effectively.
Inhibitive external microenvironment
Traditionally, the glial scar has been viewed as an inhibitory barrier impeding axonal regeneration. However, it also plays a crucial role in limiting inflammation extension and preventing additional tissue damage. Given its dual nature and indispensable function, a comprehensive analysis will be presented on cellular and molecular levels.
Cellular behavior
After SCI, peripheral-derived macrophage (PDM) and microglia near the lesion site rapidly infiltrate the core through the mediation of Plexin-B2 (PB-2) [58, 59]. PDM occupies a central position while microglial cells surround it. They clear debris, limit inflammation and compact extracellular matrix [59]. However, it is important to note that they also secrete pro-inflammatory cytokines and chemokines, which can contribute to further tissue damage.
Astrocytes transform into a reactive state characterized by hypertrophy and elongated processes in the first week after SCI, activated by neuroinflammation and ischemia probably through TNF-STAT3-a1ACT signaling axis [60]. They are divided into A1 and A2 phenotype. A1 exhibits neurotoxic properties and promotes inflammation while A2 possess neuroprotective qualities and facilitates axonal regeneration [61]. YAP pathway (bFGF-RhoA-YAP-p27Kip1) and PI3K/AKT pathway mediate astrocyte proliferation [62, 63] and Type I collagen triggers its maturation into a scar-forming morphology with thicker processes through the integrin-N-cadherin pathway, which creates an impermeable barrier to inhibit axonal regeneration [64].
It is worth noting, though, that the binary divisions of reactive astrocytes into A1/A2 is easily comprehensible and memorable, it is vague and cannot represent the complex reality [65]. Multidimensional methods should be used to indicate different characteristics of subtypes of astrocytes [66]. A comprehensive working model to define diverse astrocyte responses to CNS disorders has been proposed, including morphology, proliferation, molecular expression pattern through transcriptome and proteome, cellular functions and interactions [67]. Based on a comprehensive review in SCI, the reactive astrocytes are non-proliferative with variable degrees of cellular hypertrophy, marked by CD44, C3, Hsbp1, Vim and GFAP to seclude inflammatory cells at early phase. While scar-forming astrocytes are proliferative with thicker processes, marked by Cdh2, Sox9, Xylt1 and Chst11 to form astrocytic scar [61, 68, 69]. A more accurate and detailed definition is needed for different subtypes of astrocytes to characterize their subtle and diverse functions.
NG2 cells, also referred to oligodendrocyte precursor cell (OPC) has lineage plasticity to differentiate into oligodendrocytes, astrocytes, and Schwann cells. Nevertheless, a significant proportion of NG2 cells remain undifferentiated and secrete chondroitin sulfate proteoglycan (CSPG) to form glial scar to impede axonal regeneration [70].
Pericytes can differentiate into fibroblasts to secrete collagen and fibronectin in the lesion site, constituting connective tissue of the scar [36, 71]. Additionally, they show exert vasoconstrictive effects and regulate blood flow [72].
In summary, a comprehensive analysis of the cellular composition of the glial scar is presented. The pericenter of the scar is occupied by PDM with microglia surrounding it. Pericytes are dispersed around the microglia and secrete stromal components. Astrocytes form a barrier and encapsulate the scar along with NG2 cells. The initial formation of the glial scar is believed to have beneficial effects by limiting neuroinflammation and preventing further tissue damage. However, the mature scar sets an insurmountable obstacle for axonal regeneration. It is imperative to gain a deeper understanding of this complex phenomenon and implement appropriate adjustments at different stages, such as improving tissue contraction and containment of damaged tissue during the acute phase, while inhibiting its maturation during the chronic phase.
Inhibitive molecule
After SCI, reactive astrocytes are primarily responsible for secreting CSPG, the primary inhibitory matrix in CNS, mainly comprising a glycosaminoglycan (GAG) [73, 74]. CSPG has two important protein tyrosine phosphatases receptors (RPTPs), protein tyrosine phosphatase σ (PTPσ) and leukocyte antigen-related (LAR) subfamily in adult mammals [75–77], through which it inhibits axonal regeneration by RhoA/ROCK and PKC pathway [78]. CSPG can inhibit lysosome and autophagosome fusion during autophagy process, thereby impacting autophagy regulation for the growth cone [79]. Besides, CSPG hinders transformation of immune cells from a pro-inflammatory to a pro-repair state via the TLR4-dependent pathway, which offers a novel perspective [80].
Another inhibitory molecule is myelin-associated inhibitors (MAI), which is a consequence of demyelination. Accumulating myelin debris after SCI, due to destroyed oligodendrocytes, are referred to as Nogo, oligodendrocyte myelin glycoprotein (OMgp) and myelin-associated glycoprotein (MAG). Nogo-A is the main inhibitor and has a synergistic effect on MAG and OMgp [1, 81]. The clearance of MAI becomes challenging due to the significant reduction in macrophage phagocytic ability after SCI. This is attributed to the excessive consumption of lipids, which transforms macrophages into a ‘foamy’ phenotype [82]. MAI share common receptors, NgR1 (Nogo receptor 1) and paired immunoglobulin-like receptor B (PirB) [83], while NgR2 (Nogo receptor 2) is specific for MAG signaling pathway [84], which can inhibit neuron regeneration and upregulate NG2/CSPG4 in macrophages, diminishing its phagocytic capacity [85].
The dual effects of imbalanced microenvironment on MSC transplantation after SCI
The unfavorable microenvironment poses challenges for the viability of transplanted MSCs, making it imperative to enhance its survival and target rate to reduce costs. Simultaneously, the powerful adaptive capacity of MSCs makes adjustments to the microenvironment to facilitate tissue repair. Therefore, it is reasonable to investigate the objective effects of the microenvironment on MSCs.
Inflammatory microenvironment threatens the survival of MSCs in acute phase
Inflammation persists throughout the entire process, yet it is most pronounced during the initial phase. The primary inflammatory response, along with subsequent cascades, undoubtedly impairs the survival and function of MSCs upon transplantation. Pro-inflammatory cytokines potentially induce cellular apoptosis. Additionally, the secretion of ROS and RNS by infiltrated neutrophils may lead to lipid peroxidation and cellular membrane damage. The subsequent cascade amplifies this adverse effect.
Inflammatory microenvironment activates the immunomodulatory effects of MSCs in acute phase
MSCs interact with immune system actively, through which they adopt both anti-inflammatory and pro-inflammatory capacity [86–88]. MSCs sensor inflammatory signals to make corresponding phenotype changes to modulate immune cells for better tissue repair [89–91]. MSCs pretreated with inflammatory cytokines in vitro, mimicking injury environment, show enhanced immunomodulatory effect to treat CNS injury, partly due to the metabolic reprogramming by inflammatory cytokines to increase glycolysis of MSCs [92, 93].
Therefore, the double-edged role of the immune system is also reflected in its impact on MSCs. To mitigate the adverse consequences of the microenvironment while improve the adaptability of MSCs, employing modified MSCs capable of secreting anti-inflammatory factors could potentially serve as a viable remedy. This approach may confer MSCs resistance to inflammation, thereby enabling them to survive and assume diverse advantageous functions in acute phase.
Mature scar formation and declined axonal plasticity limit the effectiveness of MSCs in chronic phase
The presence of a mature scar hinders the therapeutic efficacy of MSCs in promoting axonal regeneration, as it creates an impassable barrier and diminishes axonal plasticity. The body naturally attempts to minimize the size of the scar, aiming to limit tissue destruction at the lowest possible expense. However, it becomes pathological basis to inhibit axonal regeneration.
Would scar formation help MSCs to achieve a better regeneration in chronic phase?
The common sense is to inhibit scar formation for its harmful effect discussed above. However, it is interesting to find an unfavorable outcome when scar formation is prevented [94]. The scar-forming astrocytes support robust axonal regeneration through upregulating growth supportive molecules. It is worth exploring whether it plays a synergistic role with MSC in promoting nerve regeneration. Another advantage is the significantly reduced inflammation accompanied by massive neovascularization in chronic phase, making a stable environment for therapeutic effect of MSCs.
In conclusion, a precise regulation is sought to achieve that neither hampers the restriction for further tissue damage in early stage nor impedes future axonal regeneration. This inquiry may offer a novel perspective for MSC-based treatments. Further investigation is required to fully elucidate the underlying mechanism.
Transplanted MSCs regulate the imbalanced microenvironment after SCI
The therapeutic effects of MSCs on SCI can be mainly attributed to the paracrine capacity. MSCs secrete cytokines and extracellular vesicles (EVs) including micro-vesicles and exosomes [8, 9]. These EVs contain numerous proteins, mRNA and micro-RNA, thereby influencing cell metabolism. Direct cell-to-cell communication also plays a role in the regulation. However, the differentiation potential of MSCs exhibits limited efficiency, as the majority remain undifferentiated [95].
Consequently, the impact and mechanism of microenvironment regulation by MSCs, due to their paracrine ability and direct cell-to-cell communication, are aimed to be comprehensively examined to enhance the understanding of MSC treatment for SCI (Fig. 2).
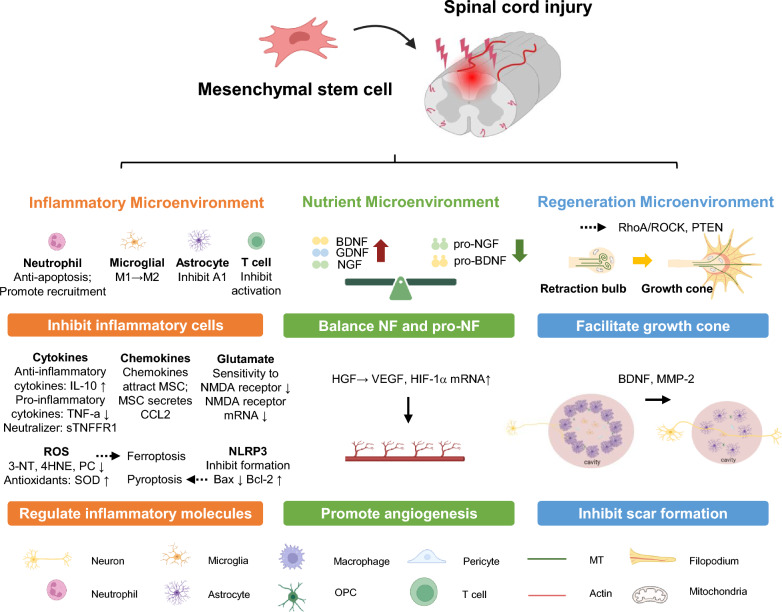
Fig. 2.
Regulation of MSCs on different imbalanced microenvironment. In inflammatory microenvironment, there is a significant infiltration of inflammatory cells accompanied by an increase of cytokines, chemokines, and other factors. MSCs have the ability to inhibit the activation of inflammatory cells, transform them into the anti-inflammatory phenotype and decrease the levels of inflammatory molecules. In nutrient microenvironment, the balance between NF and pro-NF is disrupted with damaged blood vessels. MSCs can secrete NF and counteract pro-NF to restore the balance. Additionally, MSCs can regulate key genes such as VEGF and HIF-1a to promote angiogenesis. In regeneration microenvironment, the intrinsic mechanism operates silently and insufficiently, leading to the formation of retraction bulb. The reactive astrocytes form a dense glial scar thereby impeding axonal regeneration. MSCs possess the ability to activate the intrinsic mechanism and secrete MMP-2 and BDNF, which effectively reduces the expression of GFAP and inhibits the formation of the glial scar, consequently resulting in a decrease of the cavity size
Inflammation microenvironment
As one of the main targets, Inflammation emerges promptly following injury and persists over the whole process. The immunomodulatory function of MSCs has been comprehensively characterized through intricate interactions with immune cells, mediated either by the soluble secretions or direct cell communication [96]. The impact of MSCs on various inflammatory components at the molecular and cellular levels after SCI is aimed to be elucidated.
MSCs inhibit inflammatory cell activation
Numerous cells actively engage in the initial inflammatory response and subsequent cascade after SCI, as discussed above. MSCs modulate the metabolic activities of diverse inflammatory cells either via secretome or direct cellular communication, thereby influence their function within the inflammatory microenvironment.
Neutrophils
MSCs reduce infiltration of neutrophils to modulate inflammatory response through downregulating CXCL2 in traumatic brain injury [97]. However, there is a lack of specific mechanistic studies related in SCI and CNS injury currently. Based on experiments in vitro and other disease models, it can be generalized for the dual regulation of MSCs on neutrophils. MSCs inhibit apoptosis of neutrophils through IL-6, IFN-β and granulocyte–macrophage colony-stimulating factor (GM-CSF) [87, 98, 99], which preserves its cellular pool, thereby facilitating the clearance of debris in early inflammation. Conversely, MSCs inhibit the infiltration of neutrophils and impedes the formation of neutrophil extracellular through superoxide dismutase-3 [100, 101], thereby inhibiting the amplification of inflammation.
Hence, it is of academic interest to investigate the precise regulation mechanism of MSCs on neutrophil in SCI. Given the observed surge of neutrophils at 1 day after SCI, this endeavor will provide a novel perspective in understanding the early inflammatory response.
Microglia and macrophages
MSCs regulate the phenotype transform of microglia and macrophages from M1 to M2 in order to reduce inflammation after SCI [102, 103]. M1 (classically activated macrophage) and M2 (alternatively activated macrophage) represent two terminals of the full spectrum of macrophage activation [104]. M1 is a pro-inflammation phenotype, marked by iNOS, CD80 and CD86, with enhanced expression of TNF-α, IL-1 and IL-6 while M2 is characterized by anti-inflammation ability, marked by Arg1, CD206 and CD163, with increased secretion of IL-10 and transforming growth factor-β (TGF-β) [104–109].
For macrophages, IL-4 and IL-13 are critical medium secreted by MSCs to regulate the polarization, through activating JNK, JAK/STAT6 and PI3K pathway to promote M2 related genes expression after SCI [108, 110–113]. MSCs secrete CCL5, which induces enhanced production of IL-4, accelerating M2 polarization [108, 114]. In microglial cells, MSCs can activate A2bR/cAMP/PKA pathway and counteract the downregulation of Zbtb16, Per3, and Hif3a genes after SCI, thereby facilitating M2 polarization [115, 116].
Astrocytes
Astrocytes induce inflammation and form glial scar after SCI. In this section, the MSC regulation of inflammation in astrocytes will be reviewed. The scar formation content will be discussed in the subsequent section. A1 astrocytes (reactive astrocytes) primarily contribute to inflammation, known to be neurotoxic [117]. MSCs secrete tumor necrosis factor-stimulated gene-6 (TSG-6) to decrease cyclooxygenase-2 (COX-2) and IL-6 levels [118, 119], which downregulates NF-κB pathway to inhibit the formation of A1 astrocytes [120–122]. Extracellular vesicles secreted by MSCs promote A2 phenotype transformation for SCI recovery [123]. The Jagged1/Notch pathway in astrocytes is inhibited by MSCs which induces a reduction in JAK/STAT3 phosphorylation, thereby exhibiting a therapeutic impact [124]. The activation of astrocytes is known to be dependent on microglial activity. It remains to be investigated whether the regulation of astrocytes is directly on itself or MSCs affect the crosstalk between microglia and astrocytes.
As discussed above, it is inappropriate and imprecise to define astrocytes in terms of binary divisions (A1, A2). Phenotype switch and function changes of astrocytes regulated by MSCs can similarly be characterized by multidimensional methods. More comprehensive studies are needed to elucidate the intricate interactions between MSCs and astrocytes in the future.
T cells
MSCs can inhibit and escape from T cell mediated inflammation. (i) Lack of CD40, CD80, and CD86 on the surface of MSCs makes it hard to activate T cells [125]. (ii) MSCs can secrete nitric oxide (NO), indoleamine 2,3-dioxygenase (IDO) and TGF-β to inhibit T cell proliferation and activation [126, 127]. (iii) MSCs can escape from T cell recognition, due to the absence of major histocompatibility complex II (MHC-II) and the limited expression of major histocompatibility complex I (MHC-I) on the surface [125].
MSCs reduce inflammatory molecule levels
Inflammatory cytokines
Inflammatory cytokines can be categorized as pro-inflammatory (such as TNF-α, IL-1β, IFN-γ) and anti-inflammatory (such as IL-10, TNF-β). MSCs can increase IL-4, IL-10, IL13 and TGF-β levels [128–130] and decrease IL-6 and TNF-α expression [102, 129] after transplantation. Besides, many studies also report the improvement of inflammatory microenvironment after MSC administration, leading to functional recovery of SCI [124, 131].
The potential mechanism can be summarized as two points. MSCs can directly secrete anti-inflammatory cytokines and neutralizers for pro-inflammatory molecules [132]. Furthermore, MSCs can modulate the metabolism and polarization of inflammatory cells as discussed above, thereby transforming them into an anti-inflammatory phenotype.
In conclusion, the phenomenon that inflammatory cytokines undergo a shift towards an anti-inflammatory orientation after MSCs transplantation serves as the basis for the treatment of SCI. It is essential to pay attention to the intricate interplay between inflammatory cells and molecules to achieve a comprehensive understanding.
Chemokines
Chemokines recruit inflammatory cells and induce amplification of subsequent cascade. Chemokines interact with MSCs. Stromal cell-derived factor 1 (SDF-1) and MCP-1 are up-regulated after SCI [133–135], which attracts MSCs to the lesion site through CXCR4 and CCR2 expressed on the surface [136, 137]. MSCs secrete C–C motif ligand 2 (CCL2) to attract macrophages and induce their transformation into M2 phenotype, thereby protecting neurons and myelin sheaths [138].
It is interesting to identify an optimal timing for inhibiting the recruitment function of chemokines. This timing should neither impede the early clearance of debris after inflammation, nor exacerbate the tissue damage caused by the cascade.
ROS
The peroxide background after SCI leads to cellular death and hinders the regeneration of axons, with ROS serving as the primary mediator of oxidative harm. MSCs secrete superoxide dismutase to decrease oxidative metabolites (3-NT, 4HNE and PC) in SCI and other neurodegenerative diseases [139].
Ferroptosis is a distinct form of programmed cell death, which differs from apoptosis, autophagy and pyroptosis. It is closely associated with the peroxidation microenvironment, specifically involving lipid peroxidation of the cell membrane and impairment of the intracellular antioxidant system [140]. The important role of ferroptosis in the serious consequences of secondary injury following SCI is reviewed [141]. Neurons mainly suffer from ferroptosis after SCI and MSCs mediate mitochondria transfer to inhibit mitochondrial quality control and ferroptosis, which promotes neuronal survival after SCI [142]. Besides, the antioxidative capacity of MSCs can inhibit neuronal ferroptosis after SCI to attenuate neuronal dysfunction through miR-5627-5p/FSP1 axis [143].
NLRP3 inflammasome
Nucleotide-binding oligomerization domain-like receptor protein 3 (NLRP3) inflammasome involves in the secondary inflammatory cascade after SCI. MSCs can impede the formation of NLRP3 inflammasome, which decreases the pro-apoptotic protein Bax and increases the anti-apoptotic protein Bcl-2, showing a neurological functional recovery after SCI [144]. MSCs inhibit activity of caspase-1 and decrease levels of IL-1β, IL-18 and TNF-α, resulting in a notable improvement in motor function [145, 146].
Furthermore, the NLRP3 inflammasome is significant in pyroptosis, a form of cell death closely linked to proinflammatory responses, which primarily occurs in myeloid lineage cells, specifically professional phagocytes such as macrophages and neutrophils. After SCI, DAMP recruit pro-caspase-1 through activating apoptosis-associated speck-like protein containing a CARD (ASC), leading to formation of NLRP3 inflmmasome [147–149]. It mediates pyroptosis, which triggers downstream neuroinflammation [150]. MSCs inhibit pyroptosis by increasing autophagy through PELI1 axis, which reduces inflammation after SCI [151]. Besides, this inhibition also mitigates tissue damage and maintains integrity of BSCB, resulting in functional recovery [152, 153].
Glutamate and excitotoxicity
Inflammation-induced neuronal cell death results in the release of glutamate (Glu) and subsequent excitotoxicity. MSCs reduce the mRNA expression of glutamate N-methyl-D-aspartate (NMDA) receptor subunits and down-regulates neuronal sensitivity to the ligand of the NMDA receptor [154]. This modulation impedes the calcium influx triggered by glutamate, ultimately inhibiting excitotoxicity.
Nutrient microenvironment
A stable and advantageous nutrient microenvironment serves a neuroprotective function by inhibiting neuron apoptosis and increasing neuron counts. It facilitates axon regrowth and extensive sprouting, resulting in improved functional recovery. The regulation of MSCs in the nutrient microenvironment can be attributed to the impact on the balance between NF and pro-NF and pro-angiogenesis function.
MSCs regulate the balance between NF and pro-NF
MSCs can secrete NF to ameliorate the imbalance. An increase of BDNF, NGF and glial cell-derived neurotrophic factor (GDNF) has been observed after transplantation, which results in an increase in the area of grey matter and white matter and functional improvement [155–157]. A reduction of pro-NGF and pro-BDNF after administration of MSCs also accounts for neuroprotection effect [158, 159]. These results demonstrate the equilibrium capacity of MSCs for NF and pro-NF. However, their findings are limited to a descriptive analysis and lack a comprehensive investigation of the underlying mechanisms. Except for direct secretion, it is imperative to further explore whether MSCs influence the synthesis process of NF in other cells, secretes neutralizing antagonists or employs other mechanisms.
The conventional mechanism demonstrates NF binds to respective receptors and exerts a neuroprotective effect. However, it is reported that MSCs secrete BDNF to enhance the balance between excitation and inhibition, which is achieved through the upregulation of g-aminobutyric acid type A receptor (GABAAR) subunits β3 & γ2 and K+/Cl− cotransporter 2 (KCC2) in injured neurons [160]. These findings present a novel angle for MSC-mediated recovery in SCI and contribute to our understanding of the role of NF.
The present investigation into the secretion of NF by MSCs is overly broad. It should be asserted that a more precise and specific regulatory mechanism pertaining to a particular lineage of neurons is important. For instance, IGF-1 facilitates axonal growth in cortical spinal tract (CST) neurons [161], NT-3 induces sprouting of CST neurons [162] and BDNF enhances their branching and arborization [163], as well as promoting connections with spared descending interneurons [164]. Different NFs exhibit distinct neuroprotective priorities for CST. Instead of making generalizations, it is advisable to identify the most appropriate NF for specific stages and subsequently enhance its expression through MSC transplantation to achieve the optimal regulation.
Pro-angiogenesis effect of MSCs
Angiogenesis plays a crucial role in tissue regeneration after SCI, offering benefits of enhanced blood supply, metabolic regulation and cell transportation. MSCs show pro-angiogenic effect after transplantation for treating SCI. This phenomenon is primarily attributed to the MSC regulation of key genes in endothelial cell vasculature. MSCs secrete hepatocyte growth factor (HGF), leading to increased expression of vascular endothelial growth factor (VEGF) and hypoxia-inducible factor-1α (HIF-1α) mRNA, thereby promoting angiogenesis [165].
Regeneration microenvironment
Axonal regeneration serves as the fundamental mechanism for achieving functional recovery after SCI, making it a crucial focus for therapeutic interventions. MSCs possess the ability to modulate the intrinsic regenerative microenvironment at the molecular level, while also regulate the extrinsic inhibitory microenvironment at the cellular and tissue levels.
MSCs activate intrinsic regeneration mechanism
MSCs have the ability to restore the disrupted cytoskeleton and modulate the development of growth cone. Following transplantation of MSCs, a significant presence of growth cone-like structures occurs [166], which can be partially attributed to the regulation of RhoA/ROCK and PTEN/mTOR pathway discussed above.
There is a decrease of RhoA level after MSC transplantation, with the most pronounced effect one week after SCI [167], which suggests that MSCs have the potential to alleviate the inhibitory effects of the RhoA/ROCK pathway on MT extension, thereby promoting a more organized MT structure that facilitates growth cone formation. MSCs secrete EVs containing miR-29b-3p targeting PTEN gene to suppress its expression [168]. Consequently, the inhibition exerted by PTEN on the mTOR pathway is relieved, resulting in the activation of the mTOR pathway and subsequent promotion of axonal growth.
In summary, MSCs inhibit retraction bulb formation and make an orderly growth cone by modulating RhoA/ROCK and PTEN/mTOR pathways, thereby influencing MT assembly and extension. However, the current research on the interaction between MSCs and the intrinsic pathway is insufficient and further investigation is necessary to gain a comprehensive understanding on the regulation of the intrinsic regeneration microenvironment.
MSCs improve inhibitive external microenvironment
The glial scar has been extensively investigated and serves as a significant evaluation of the effectiveness of MSC therapy. After MSC transplantation, it demonstrates a reduction in cavity size and tissue loss from the epicenter to rostral and caudal levels, accompanied by a decrease in GFAP [169], which suggests that MSCs inhibit the formation of glial scar. Several factors contribute to this phenomenon. MSCs inhibit reactive astrocytes, secretes BDNF and enhances Matrix metalloproteinases-2 (MMP-2) expression, resulting in a reduction in the expression and immunoreactivity of CSPG to prevent scar formation, which effectively mitigates cavity size [166, 170, 171].
The inhibitory effects of MSCs on glial scar formation on different levels are concluded. On the molecular level, MSCs secrete BDNF and upregulates MMP-2 expression. On the cellular level, MSCs exert inhibitory regulation on reactive astrocytes. On the tissue level, MSCs contribute to a reduction in cavity size and tissue loss. It is highlighted for the importance of investigating the impact of MSCs on other cellular components of the glial scar, such as macrophages, microglia and pericytes. Currently, research primarily focuses on the inflammatory aspects of these cells, as discussed above, rather than their role in scar formation and regeneration inhibition.
It is worth mentioning that even though the scar has already formed, MSCs have the ability to facilitate axonal regeneration through mechanisms known as 'cell bridge' and 'cell towing'. MSCs can migrate on inhibitory molecules such as CSPG or MAG/Nogo-A, acting as a cell bridge to facilitate the growth of dorsal root ganglion (DRG) across these inhibitory environments [172]. Additionally, MSCs can also tow the growth of co-located DRG. The elucidation of the mechanism behind MSC migration on inhibitory molecules and its role in promoting DRG growth presents an intriguing area of investigation. Several research have demonstrated that the secretome by MSCs including BDNF, NGF, VEGF and SDF-1 can effectively enhance the outgrowth of motor neurites in the presence of glial scar inhibitors. It is plausible to hypothesize that MSCs not only serve as a physical substrate but also actively releases cytokines to facilitate neuronal growth in the inhibitory environment.
In summary, MSCs have demonstrated the ability to not only impede scar formation at different levels, but also facilitate axonal regeneration on a formed glial scar through paracrine effects and ‘cell bridge’. Consequently, MSCs hold significant potential for the treatment of SCI, particularly in the chronic phase.
The regulation of the imbalanced microenvironment after SCI by MSCs covers the entire period, including inflammatory, nutrient and regeneration microenvironments. A brief overview has been provided to facilitate a more comprehensive understanding of the regulatory mechanisms of MSCs (Table 1).
Table 1.
Imbalanced microenvironment regulation of different sources of MSCs
| Source of MSCs | Mechanism of MSCs | Effect | Refs. |
|---|---|---|---|
| Inflammatory microenvironment | |||
| UCMSCs | Zbtb16, Per3, and Hif3a genes↑ | Promote M1 to M2 of microglial | [115, 116] |
| TSG-6↑ | Inhibit A1 astrocyte formation | [118–122] | |
| sTNFR1 ↑ | Counteract TNF-α | [132] | |
| Inhibit NLRP3 formation | IL-1β, IL-18 ↓ | [145] | |
| BMSCs | Secrete EVs (NO, IDO, TGF-β) | Inhibit T cell proliferation and activation | [126, 127] |
| IL-6, IFN-1β, GM-CSF ↑ | Inhibit neutrophil apoptosis | [87, 98, 99] | |
| Secrete EVs (miR-21) | Transform the phenotype of astrocytes to A2 | [123] | |
| Increase autophagy through PELI1 axis | Inhibit pyroptosis | [151] | |
| NMDA receptor subunit mRNA↓ | Inhibit excitotoxicity of neurons | [154] | |
| BMSCs, ADMSCs |
Anti-inflammatory cytokines↑ Pro-inflammatory cytokines↓ |
IL-4, IL-10, IL13 and TGF-β ↑ IL-6 and TNF-α ↓ |
[102, 129] |
| ADMSCs | Inhibiting the Jagged1/Notch pathway | Reduce JAK/STAT3 phosphorylation in astrocytes | [124] |
| 3-NT, 4HNE, and PC↓ | Anti-oxidation | [139] | |
| CBMSCs | CCL2↑ | attract macrophages, induce into M2 | [138] |
| EFMSCs | Inhibit NLRP3 formation | Bax↓ Bcl-2↑ | [144] |
| Nutrient microenvironment | |||
| UCMSCs | GDNF↑ | Promote tissue repair | [156] |
| BDNF↑, upregulate β3 & γ2 and KCC2 | balance excitation and inhibition in injured neurons | [159] | |
| BMSCs | BDNF, NGF↑ | Stimulate recovery of SCI | [155] |
| NGF↑ | increase the area of grey matter and white matter | [157] | |
| pro-NGF↓ | Improve nutrient microenvironment | [158] | |
| AFMSCs | HGF↑ | VEGF and HIF-1α↑, promote angiogenesis | [165] |
| Regeneration microenvironment | |||
| UCMSCs | Secrete miR-29b-3p | PTEN↓, promote axon growth | [168] |
| Inhibit reactive astrocytes | Inhibit scar formation | [166] | |
| MMP-2↑ | CSPG↓, inhibit scar formation | [170] | |
| UCMSCs, ADMSCs | GFAP↓ | Decrease cavity size and tissue loss | [169] |
| BMSCs | ‘Cell bridge' and 'cell towing' | Facilitate neuronal growth | [172] |
| CMSCs | RhoA↓ | Promote growth cone formation | [167] |
| UCBMSCs | BDNF↑ | CSPG↓, mitigate cavity formation | [171] |
Application of MSCs in SCI
Clinical trials demonstrate the effectiveness of MSCs in treating SCI
In addition to the numerous basic studies and animal experiments which proved the recovery of SCI after MSC administration, many clinical trials also show promising improvement. Most MSCs used clinically are derived from bone marrow or umbilical cord. The patients enrolled are complete or incomplete injury grade, with American Spinal Injury Association (ASIA) Impairment Scale scoring from A-C. After treatment for different periods, there are varying degrees of improvement in sensation function, motor function, electrophysiology, imaging and urodynamics [173–180]. Table 2 summarizes some clinical trials of MSC therapy for SCI, including cell type, dose, transplantation route, therapeutic phase and treatment effect. Taken together, MSCs bring functional recovery, which show promising prospect (Table 2).
Table 2.
Clinical trials of MSC treatment for SCI
| # | Registration number | Status | Country | Participants | Cell type | Dose | Implantation route | Immunogenicity | Phase | ASIA Scoring | Electrophysiology | Imaging | Urodynamics | Refs. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensation | Motor | ||||||||||||||
| 1 | NCT02510365 | Finished | China | 40 | UCMSCs | 4 × 107 | in situ transplantation | allogeneic | acute | ↑ | ↑ | ↑ | ↑ | ↑ | [175] |
| 2 | NCT03003364 | Finished | Spain | 10 | UCMSCs | 10 × 106 | Intrathecal transplantation | allogeneic | chronic | ↑ | ↑ | [173] | |||
| 3 | NCT01393977 | Finished | China | 34 | UCMSCs | 4 × 107 | in situ transplantation | allogeneic | chronic | ↑ | ↑ | [174] | |||
| 4 | NCT02352077 | Finished | China | 8 | UCMSCs | 4 × 107 | in situ transplantation | allogeneic | chronic | ↑ | ↑ | [188] | |||
| 5 | NCT01909154 | Finished | Spain | 8 | BMSCs | 1.2 × 106/kg | in situ + intra spinal canal + intravenous | autologous | acute, chronic | ↑ | ↑ | ↑ | ↑ | [176] | |
| 6 | NCT01325103 | Finished | Brazil | 14 | BMSCs | 5 × 106/cm3 | in situ transplantation | autologous | chronic | ↑ | ↑ | [178] | |||
| 7 | NCT01676441 | Finished | Korea | 10 | BMSCs | 9 × 107 | in situ + intradural injection + lumbar tapping | autologous | chronic | ↑ | ↑ | ↑ | [179] | ||
| 8 | NCT05018793 | On going | Greece | 14 | ADMSCs | 9 × 107 | Intrathecal transplantation | autologous | subacute, chronic | ↑ | ↑ | [177] | |||
| 9 | NCT03308565 | Finished | America | 10 | ADMSCs | 1 × 108 | Intrathecal transplantation | autologous | subacute, chronic | ↑ | ↑ | ↑ | [180] | ||
However, the recovery in clinical trials is far less significant and effective than that in preclinical experiments. This can be attributed to different designs between preclinical and clinical trials. A good paradigm for discussing this issue is proposed [181]. Based on this, a brief overview is provided to illustrate the design differences (Table 3). For the disease model, species differences should be prioritized, emphasizing the need to select more representative animals, such as non-human primates. Animal models are typically young and healthy, exhibiting homogeneity degrees of injury, whereas actual patients often present with comorbidities and varying injury severities. Individual differences should also be considered. For transplanted MSCs, immunogenicity and source should be considered substantially. Besides, the preservation, dose and time of transplantation are also critical. For evaluation metrics, preclinical experiments typically observe effects over a short period. Conversely, clinical trials require long-term follow-up to comprehensively evaluate efficacy and safety. Differences in evaluation methods and ethical considerations further limit clinical translation.
Table 3.
Design differences between preclinical experiments and clinical trials
| Preclinical experiments | Clinical trials | |
|---|---|---|
| Disease model | ||
| Species | Rodents | Human |
| Degree of injury | Relative homogeneity | Varying degree of severity |
| Comorbidity | Healthy | Different degree |
| Individual differences (age, gender…) | Relative homogeneity | Considerable variability |
| MSCs | ||
| Immunogenicity | Allogeneic & xenogeneic | Autologous & allogeneic |
| Source | Various sources | BM, UC, AT |
| Preservation | Cryopreserved | Fresh |
| Transplantation dose | Relatively small quantity | Large quantity |
| Time window | Mainly subacute | Mainly chronic |
| Evaluation Metrics | ||
| Fllow-up duration | Short-term | Long-term |
| Evaluation method | BMS, BBB | ASIA, Imaging |
| Ethics | Less consideration | Thorough consideration |
The optimal transplantation strategy of MSCs
Timing
The effectiveness of different transplantation time points of MSCs has been assessed through experimental models and clinical trials. In experimental models, the subacute phase (2 weeks after SCI) is often considered the optimal choice [182, 183]. Because the intense inflammation and a detrimental environment in the acute phase hinders MSC survival and the formation of a mature scar in the chronic phase limits the efficacy [184–187]. Meta-analysis related proves subacute phase as the most effective time window in preclinical experiments [183, 188]. However, clinical trials have not yet determined an optimal time point. Due to practical considerations, most patients included in the trials are in the subacute or chronic phase as discussed above. Therefore, more comprehensive research should be conducted in the future to determine the optimal time window for transplantation.
Dose
The therapeutic effect of MSC transplantation for SCI is dose-dependent. In rodent animals, high dose (> 1 × 106) reports better functional recovery than low dose (< 1 × 106) in umbilical cord derived mesenchymal stem cells (UCMSCs) and adipose derived mesenchymal stem cells (ADMSCs) [182, 183]. However, an over-dose transplantation may trigger inflammation, which harms repair effect [189]. Consequently, 106 is utilized as an effective dose in most rodent models [190]. In large animal models, canines and pigs are administrated a dose of 107 [139, 191, 192]. There is currently no research on MSC transplantation for SCI therapy in non-human primates. However, one study involving the transplantation of MSC-derived neurons into rhesus monkeys, with a dosage of 2.5 × 106, can be referenced for further research [193]. In humans, there are no systematic clinical trials comparing the optimal transplantation dose. Currently, the dose range is 107–108 [174, 175, 177, 179, 180, 188]. A more precise criterion is 1.2 × 106/kg or 5 × 106/cm3 (per lesion volume which was performed by MRI analysis) [176, 178] The allometric dose translation approach should be investigated in the future to advance clinical translation.
Route
Despite being a non-invasive method, intravenous injection lacks specificity, with the majority of the cells predominantly accumulating in the lungs, spleen and kidneys [194], showing inferior efficacy compared to local transplantation [182, 183]. in situ injection has been documented as a direct means to target the lesion site. However, it may potentially cause secondary damage. Given the practical circumstances in clinical settings, intrathecal injection is considered as a relatively safe and valid method because it makes MSCs circulate in CSF to target lesion site [195].
Notably, the powerful homing and migration capabilities of MSCs have been systematically documented. After entering into blood flow, MSCs extravasate at the injury site crossing endothelial barrier through ‘leukocyte-like process’, finally targeting lesion site precisely [196]. SDF-1/CXCR4 plays a crucial role in recruiting MSCs in SCI [197]. However, due to massive capture of MSCs by lungs, spleen and kidneys when administrated through intravenous injection, strategies to improve homing capacity require urgent development. For instance, Integrin α4 overexpression enhances trans-endothelial migration of MSCs [198]. This is highly promising. It may promote intravenous injection as a superior administration route in the future, which is a non-invasive transplantation method to completely eliminate the risk of secondary injury to the spinal cord.
Source
Bone marrow (BM), umbilical cord (UC) and adipose tissue (AT) are three main sources utilized in experiments and clinical trials [199]. In spite of different characters, they all show effective therapy in different phases of SCI. As pluripotent stem cells, bone marrow derived mesenchymal stem cells (BMSCs) can differentiate into neurons and glial cells [200, 201]. However, the therapeutic effect mainly relies on the paracrine and transdifferentiation capacity, which can reduce inflammation, recover BSCB integrity, secrete neurotrophic factor and promote axonal regeneration [201–204]. UCMSCs can be easily obtained in a non-invasive manner. Besides, the low immunogenicity and rapid proliferation capacity make it a safer and more economical candidate [205]. They can inhibit reactive astrocytes activity, neuron apoptosis and scar formation [166, 171, 206]. ADMSCs contain more somatic stem cells with higher proliferation activity [207, 208]. They may activate angiogenesis more significantly due to enhanced expression of IGF-1, IL-8 and VEGF-D [209].
Immunogenicity
The low immunogenicity of MSCs minimizes the risk of immune rejection. However, it is still a nonnegligible issue to be discussed in the future clinical transformation. Autologous MSCs are isolated from self-body, expanded in vitro and then administrated back to self. It is considered the safest without the risk of immune rejection, which is widely used in clinical trials [176–180]. Although allogeneic MSC are not derived from the patients themselves, they achieve immune escape due to lack of CD40, CD80, CD86 and low expression of MHC complex as well as ability to inhibit T cell activation [125–127, 205]. UCMSCs are classical examples utilized clinically, which show effective restoration [173–175]. Xenogeneic MSC transplantation is limited to animal experiments with effective functional recovery while it is rare clinically because of species difference [210, 211]. It is promising if applied clinically because it holds the potential to solve the problem of insufficient clinical donors, provided it is ethical.
Survival
The adverse environment following SCI reduces the survival rate of transplanted MSCs, thereby limiting the effectiveness. Despite the presence of MSCs being detectable 6–8 weeks post-transplantation, their survival rate is less than 1% after 8 weeks [212, 213]. There are two methods to improve the survival rate and quantity of transplanted MSCs, including preconditioning of MSCs to enhance survival capacity (such as chemical factors or hypoxia) and administering multiple injections at different time points [214–217].
In conclusion, developing the optimal transplantation strategy to construct a comprehensive transplantation system is a complex yet essential task, particularly for future clinical translation. Critical factors including timing, dose, route, sources, immunogenicity and cell survival have been summarized, aiming to provide insightful directions for subsequent research.
Exosomes derived from MSCs show promising effects
Due to certain constraints associated with MSCs, exosomes have emerged as an alternative therapeutic option, which is attributed to their distinct advantages, such as the absence of ethical concerns, the ability to evade capture by the liver and lungs and smaller size that facilitates easier infiltration of the BSCB [218].
Exosomes demonstrate similar effects to MSCs by means of their secretory activity, which can be summarized as anti-inflammatory, regulation of macrophage polarization, reduction of A1 astrocytes and protection of BSCB integrity [219]. Exosomes derived from hUCMSCs can induce a phenotype switch toward anti-inflammation of macrophage and decrease the levels of TNF-α, MIP-1α, IL-6 and IFN-γ [119].
Moreover, exosomes have the ability to modulate signal pathways via miRNA. Currently, miRNA-21, miRNA-133 and miRNA-126 have been identified as potential targets. These miRNAs specifically target crucial genes which are involved in the process of injury repair. Exosome-derived miRNA-21 targets PTEN, thereby facilitating functional recovery [220]. miRNA-133b suppresses RhoA, leading to the activation of PI3K/AKT and MEK/ERK pathways, ultimately promoting regeneration [221]. In addition to inhibitory function, miRNA-133b promotes the phosphorylation of CREB and STAT3, which is associated with axonal regeneration [221].
However, there remain certain limitations that require resolution. It is imperative to attain the standardization in the isolation method, purification technology and source of MSCs for exosomes. Additionally, further investigation is necessary to discern harmful components in exosomes.
Modification of MSCs to enhance effectiveness
Different imbalanced microenvironments emphasize different therapeutic priorities. The modification of MSCs in vitro can potentially alter the properties. Therefore, it is advantageous to enhance the performance of MSCs through modification to adapt to various environment. In general, there are two approaches called preconditioning and genetic modifications [222].
Preconditioning
Preconditioning can be achieved through hypoxia, cytokines and physical factors. Hypoxia preconditioning has been shown to enhance the proliferation and migration of MSCs [223]. Additionally, the expression of pro-survival signals and trophic factors is increased after hypoxia/reoxygenation [224]. Cytokine preconditioning has also demonstrated beneficial effects, as evidenced by the upregulation of VEGF and activation of the pro-growth pathways AKT and ERK in MSCs treated with SDF-1 [225]. Additionally, physical factors and materials also show favorable effect. Pretreatment with pulsed electromagnetic fields (PEMF) can effectively enhance the AKT and RAS signaling pathways, thereby inhibiting the apoptosis of MSCs [226].
Different primed conditions show various effect. The optimal and suitable preconditioning method should be identified for different microenvironments. Particularly, whether preconditioning is harmful remains to be explored.
Genetic modification
MSCs can undergo genetic modification through trophic factors, cytokines and anti-apoptosis factors. MSCs genetically modified by NT-3 develop larger spare myelin sheaths and reduce the capsular area, which leads to significant improvement in motor function after SCI [227]. Similarly, BDNF, GDNF and NGF have also been employed, yielding notable effects [228].
Genetic modification presents a promising approach for regulating the properties of MSCs at different stages following injury. The selection of an appropriate gene for specific modifications of MSCs is crucial to enable their adaptation to diverse microenvironments. Additionally, understanding the intricate interplay between genes and achieving multi-gene modifications is of utmost importance.
Biomaterials and scaffold combination with MSCs
The direct administration of MSCs yields a diminished rate of cell survival and the migration of MSCs results in a reduced targeting efficiency. The utilization of degradable biomaterials can facilitate the retention of MSCs at the site of injury, ensure a sustained supply of nutrients and offer a structural substrate for axonal regeneration.
Currently, four primary materials, including collagen, fibrin, chitosan and poly lactic-co-glycolic acid (PLGA), are predominantly utilized. Each material possesses distinct characteristics [229]. After transplantation of MSC-scaffold, there is an increase in neurofilaments 200 (NF-200) and CD31 as well as a decrease in CD11b, indicating a reduction in inflammation, ultimately promoting angiogenesis, axonal regeneration and motor ability restoration of SCI [229, 230].
In addition to experimental evidence, clinical trials have also demonstrated potential value. In the clinical trial NCT02352077, Zhao et al. conducted a transplantation of hUCMSC-biodegradable collagen scaffolds to patients with SCI in the chronic phase, which improves the level of sensation, increases MEP reactive area and enhances trunk stability [188]. In the clinical trial NCT02510365, Xiao et al. observed a gradual recovery of electrical conduction and walking ability after transplantation in the acute phase [175].
Immunotherapy benefits MSC transplantation
Immunotherapy on SCI modulates innate and adaptive immune responses, which improves the intense inflammation after SCI [231]. Methylprednisolone (MP) is considered as a significant innate immune suppressant with anti-inflammatory and neuroprotective effects [232]. It exerts neuroprotective function by mitigating oligodendrocyte apoptosis induced neuron death through the inhibition of lipid peroxidation. It is also demonstrated of the enhancement of motor scores after administration of MP in clinical trials [233]. Human immunoglobulin G (hIgG) serves as a regulator of the adaptive immune response, which promotes the integrity of the BSCB by downregulating inflammatory enzymes and upregulating the expression of tight junction proteins, thereby reducing the infiltration of immune cells. It induces neutrophils to migrate into the spleen by increasing chemoattractant there, leading to a reduction in the inflammatory cascade in the spinal cord [234, 235].
There is little research on the combination of MSCs and immunotherapy. The inflammatory response following SCI poses a significant threat to the survival of MSCs, particularly during the early stages. Employing immunotherapy to suppress the inflammatory response at the lesion site can create a conducive environment for MSCs. Nevertheless, prior to implementation, it is imperative to assess the influence of MP on MSCs and the safety of immunotherapy to avert potential systemic complications.
Technologies for tracking transplanted MSC
In preclinical experiments, MSCs labeled with human nuclear antigen or green fluorescent protein (GFP) can be tracked through immunofluorescence imaging at cellular level [124, 236],while transfection with luciferase followed by in vivo imaging system (IVIS) allows imaging MSCs at the macroscopic level [237]. However, they are not suitable for clinical transformation for inaccuracy, lack of real-time capability as well as safety concern. Some research has already been conducted to identify suitable imaging tools to facilitate the clinical translation of MSC transplantation. Magnetic resonance imaging (MRI) is a non-invasive imaging modality with precise surveillance of MSCs labeled by exogenous contrast agents such as iron-oxide nanoparticles and gadolinium diethylenetriamine pentaacetic acid (Gd-DTPA), which shows safe and effective outcomes [238–240]. Besides, a combined ultrasound (US) and photoacoustic (PA) imaging technology is developed with capability for accurate guidance and quantitative imaging, which enables real-time tracking of MSCs and provides precise navigation for the safety of clinical MSC transplantation [241, 242].
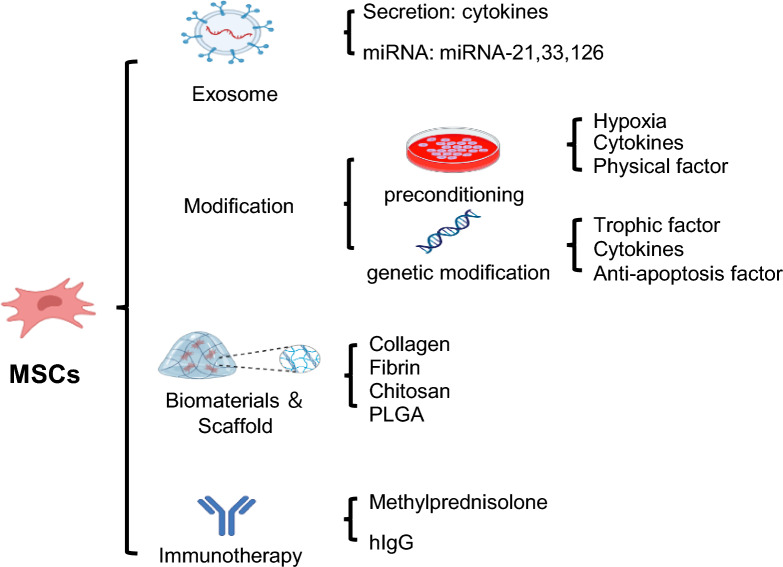
A schematic diagram of MSC applications is provided to summarize the current common approaches (Fig. 3). In addition to the aforementioned methods, functional electrical stimulation (FES) holds promise as a rehabilitation training technique due to its effectiveness. The intricate pathological process of microenvironment imbalance following SCI involves multiple phases, targets and pathways. Merely focusing on a singular aspect is inadequate for comprehensive clinical rehabilitation. Consequently, a multiple-target and multiple-disciplinary treatment (MDT), such as combining MSC transplantation with other approaches is suggested.
Fig. 3.
Different applications for MSCs. Exosomes show promising effect, which do not raise ethical concerns and possess the ability to evade capture by the liver and lungs as well as easily cross through the BSCB. The modification of MSCs, through methods such as preconditioning and genetic modification, can enhance the regulatory and adaptive capabilities of MSCs in different microenvironments. Co-transplantation with biomaterials and scaffolds can improve the survival and targeting rate of MSCs. Immunotherapy can be employed as a preliminary treatment to create a more conducive environment for MSCs
Limitation and future direction
Although MSC transplantation therapy has a relatively robust experimental foundation and some clinical evidence, there exist several limitations. The majority of current animal models employed in studies are rodents, which may not precisely reflect the pathological progression following SCI in humans. Consequently, the direct application of these findings to humans lacks accuracy, necessitating the inclusion of large animal models, especially non-human primate for further investigation, like in stroke research [243]. In terms of anatomical structure, their spinal cord closely resembles that of humans. Regarding effectiveness of SCI modeling, the post-injury periods and microenvironment changes they undergo are more analogous to those observed in humans. For evaluation metrics, evaluation criteria and identical imaging techniques in clinical trials can be employed. Additionally, inadequate translational studies and clinical trials impede the advancement and widespread implementation of this therapy. Furthermore, the ethical boundaries and risk assessment pertaining to this matter remain unresolved, especially for antigenicity and tumorigenicity.
In future research, it is imperative to conduct further investigation into the paracrine function and accurate underlying mechanism of MSCs. The specific and precise regulation will be the most efficient and economical approach. In order to facilitate the clinical application of MSCs, it is necessary to link preclinical experiment with clinical trials. More clinical trials are also warranted for risk assessment and to determine the optimal transplantation strategy. Additionally, the standardization and commercialization of MSCs are crucial for achieving large-scale production and widespread availability.
Conclusions
SCI results in significant neural impairment, imposing a substantial burden on both the patient and society. The initial mechanical trauma directly causes tissue destruction and triggers subsequent inflammatory cascades. The disrupted balance between NF and pro-NF, along with damaged vasculature contributes to an unfavorable nutrient microenvironment. The inhibitory glial scar formation and insufficient intrinsic mechanisms hinder axonal regeneration. As a promising therapeutic approach, MSCs modulate the imbalanced microenvironment through its paracrine abilities and direct cellular communication. The administration of MSCs has been shown to mitigate inflammation, restore the nutrient balance and improve the inhibitory microenvironment, ultimately resulting in the regeneration of axons and the recovery of neurological function. Clinical trials and the optimal transplantation strategy are discussed. Various forms of MSC application, such as exosomes, modification and combination with biomaterials, have been explored. At present, it is crucial to acquire a comprehensive and thorough comprehension of MSC regulation on the imbalanced microenvironment following SCI. Further research that is more specific is warranted to propel us towards an era of enhanced precision and targeted regulation.
Acknowledgements
Illustrations were created with BioRender.com.
Abbreviations
- ADMSCs
Adipose derived mesenchymal stem cells
- AFMSCs
Amniotic fluid derived mesenchymal stem cells
- ASC
Apoptosis-associated speck-like protein containing a CARD
- ASIA
American Spinal Injury Association
- AT
Adipose tissue
- BBB
Basso, Beattie, and Bresnahan Scale
- BDMs
Blood-derived macrophages
- BDNF
Brain-derived neurotrophic factor
- BMS
Basso Mouse Scale
- BSCB
Blood spinal cord barrier
- BM
Bone marrow
- BMSCs
Bone marrow derived mesenchymal stem cells
- CBMSCs
Cord blood mesenchymal stem cells
- CCL2
C-C motif ligand 2
- ChABC
Chondroitin ABC
- CMSCs
Canine mesenchymal stem cells
- CNS
Central nervous system
- COX-2
Cyclooxygenase-2
- CRMP-2
Collapsin response mediator protein-2
- CSF
Cerebrospinal fluid
- CSPG
Chondroitin sulfate proteoglycan
- CST
Cortical spinal tract
- DAMP
Damage-associated molecular pattern
- DLK
Dual leucine-zipper kinase
- DRG
Dorsal root ganglion
- EFMSCs
Epidural fat derived mesenchymal stem cells
- EV
Extracellular vesicle
- FES
Functional electrical stimulation
- GABAAR
G-aminobutyric acid type A receptor
- GAG
Glycosaminoglycan
- Gd-DTPA
Gadolinium diethylenetriamine pentaacetic acid
- GDNF
Glial cell-derived neurotrophic factor
- GFP
Green fluorescent protein
- Glu
Glutamate
- GM-CSF
Granulocyte–macrophage colony-stimulating factor
- HGF
Hepatocyte growth factor
- Hif-1a
Hypoxia-inducible factor-1α
- hIgG
Human immunoglobulin G
- HUCMSCs
Human umbilical cord-derived mesenchymal stem cells
- IDO
Indoleamine 2,3-dioxygenase
- IL
Interleukin
- IVIS
In Vivo Imaging System
- KCC2
K+/Cl− cotransporter 2
- LAR
Leukocyte antigen-related
- LZK
Leucine zipper kinase
- MAG
Myelin-associated glycoprotein
- MAI
Myelin-associated inhibitors
- MDT
Multiple-disciplinary treatment
- MHC-I
Major histocompatibility complex I
- MHC-II
Major histocompatibility complex II
- MIF
Macrophage migration inhibitory factor
- MMP-2
Matrix metalloproteinases-2
- MP
Methylprednisolone
- MRI
Magnetic resonance imaging
- MSCs
Mesenchymal stem cells
- MT
Microtubules
- NF
Neurotrophic factor
- NF200
Neurofilaments 200
- NGF
Nerve growth factor
- NgR1
Nogo receptor 1
- NgR2
Nogo receptor 2
- NLR
Nod-like receptor
- NLRP3
Nucleotide-binding oligomerization domain-like receptor protein 3
- NMDA
N-methyl-D-aspartate
- NO
Nitric oxide
- NT-3
Neurotrophin-3
- NT-4
Neurotrophin-4
- NT-5
Neurotrophin-5
- OMgp
Oligodendrocyte myelin glycoprotein
- OPC
Oligodendrocyte precursor cells
- PA
Photoacoustic
- PAMP
Pathogen-associated molecular pattern
- PB-2
Plexin-B2
- PDM
Peripheral-derived macrophages
- PEMF
Pulsed electromagnetic fields
- PGE2
Prostaglandin E2
- PirB
Paired immunoglobulin-like receptor B
- PKC
Protein kinase C
- PLGA
Poly lactic-co-glycolic acid
- PNN
Perineuronal nets
- Pro-NF
Neurotrophic factor precursor
- PRR
Pattern recognition receptor
- PTPσ
Protein tyrosine phosphatase σ
- RNS
Reactive nitrogen species
- ROCK
RhoA-associated protein kinase
- ROS
Reactive oxygen species
- RPTPs
Protein tyrosine phosphatases receptors
- RNS
Reactive nitrogen species
- ROCK
RhoA-associated protein kinase
- ROS
Reactive oxygen species
- RPTPs
Protein tyrosine phosphatases receptors
- SCI
Spinal cord injury
- SDF-1
Stromal cell-derived factor 1
- TGF-β
Transforming growth factor β
- TLR
Toll-like receptor
- TNF-α
Tumor necrosis factor-α
- Trk
Tropomyosin-related kinase
- TSG-6
Tumor necrosis factor-stimulated gene-6
- UC
Umbilical cord
- UCBMSCs
Umbilical cord blood mesenchymal stem cells
- UCMSCs
Umbilical cord derived mesenchymal stem cells
- US
Ultrasound
- VEGF
Vascular endothelial growth factor
- WISCI
Walk Index for SCI
- YAP
Yes-associated protein
Author contributions
YFL, CXZ and SQF select the topic and determine the review structure. YFL and LQL searched the literature. YFL wrote the manuscript and drafted the figures and tables. CXZ, RZ, YLP and SQF critically revised and edited the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Key Research and Development Program (2019YFA0112100) and the Natural Science Foundation of Shandong Province Youth Program (ZR2023QH114).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yifan Liu and Chenxi Zhao have contributed equally to this work.
References
- 1.Fan B, Wei Z, Feng S. Progression in translational research on spinal cord injury based on microenvironment imbalance. Bone Res. 2022;10(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mothe AJ, Coelho M, Huang L, Monnier PP, Cui YF, Mueller BK, Jacobson PB, Tator CH. Delayed administration of the human anti-RGMa monoclonal antibody elezanumab promotes functional recovery including spontaneous voiding after spinal cord injury in rats. Neurobiol Dis. 2020;143:104995. [DOI] [PubMed] [Google Scholar]
- 3.Ray SK. Modulation of autophagy for neuroprotection and functional recovery in traumatic spinal cord injury. Neural Regen Res. 2020;15(9):1601–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu Y, Li L, Hong B, Xie Y, Li T, Feng C, Yang F, Wang Y, Zhang J, Yu Y, et al. Epidemiological features of traumatic spinal cord injury in China: a systematic review and meta-analysis. Front Neurol. 2023;14:1131791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, Fehlings MG. Traumatic spinal cord injury. Nat Rev Dis Primers. 2017;3:17018. [DOI] [PubMed] [Google Scholar]
- 6.Orr MB, Gensel JC. Spinal cord injury scarring and inflammation: therapies targeting glial and inflammatory responses. Neurotherapeutics. 2018;15(3):541–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samsonraj RM, Raghunath M, Nurcombe V, Hui JH, van Wijnen AJ, Cool SM. Concise review: multifaceted characterization of human mesenchymal stem cells for use in regenerative medicine. Stem Cells Transl Med. 2017;6(12):2173–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phinney DG, Di Giuseppe M, Njah J, Sala E, Shiva S, St Croix CM, Stolz DB, Watkins SC, Di YP, Leikauf GD, et al. Mesenchymal stem cells use extracellular vesicles to outsource mitophagy and shuttle microRNAs. Nat Commun. 2015;6:8472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wen D, Peng Y, Liu D, Weizmann Y, Mahato RI. Mesenchymal stem cell and derived exosome as small RNA carrier and Immunomodulator to improve islet transplantation. J Control Release. 2016;238:166–75. [DOI] [PubMed] [Google Scholar]
- 10.Mushahary D, Spittler A, Kasper C, Weber V, Charwat V. Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A. 2018;93(1):19–31. [DOI] [PubMed] [Google Scholar]
- 11.Ringe J, Strassburg S, Neumann K, Endres M, Notter M, Burmester GR, Kaps C, Sittinger M. Towards in situ tissue repair: human mesenchymal stem cells express chemokine receptors CXCR1, CXCR2 and CCR2, and migrate upon stimulation with CXCL8 but not CCL2. J Cell Biochem. 2007;101(1):135–46. [DOI] [PubMed] [Google Scholar]
- 12.Guan YT, Xie Y, Li DS, Zhu YY, Zhang XL, Feng YL, Chen YP, Xu LJ, Liao PF, Wang G. Comparison of biological characteristics of mesenchymal stem cells derived from the human umbilical cord and decidua parietalis. Mol Med Rep. 2019;20(1):633–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xie Q, Liu R, Jiang J, Peng J, Yang C, Zhang W, Wang S, Song J. What is the impact of human umbilical cord mesenchymal stem cell transplantation on clinical treatment? Stem Cell Res Ther. 2020;11(1):519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan B, Wei Z, Yao X, Shi G, Cheng X, Zhou X, Zhou H, Ning G, Kong X, Feng S. Microenvironment imbalance of spinal cord injury. Cell Transplant. 2018;27(6):853–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tran AP, Warren PM, Silver J. The biology of regeneration failure and success after spinal cord injury. Physiol Rev. 2018;98(2):881–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kigerl KA, de Rivero Vaccari JP, Dietrich WD, Popovich PG, Keane RW. Pattern recognition receptors and central nervous system repair. Exp Neurol. 2014;258:5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pineau I, Lacroix S. Proinflammatory cytokine synthesis in the injured mouse spinal cord: multiphasic expression pattern and identification of the cell types involved. J Comp Neurol. 2007;500(2):267–85. [DOI] [PubMed] [Google Scholar]
- 18.Stammers AT, Liu J, Kwon BK. Expression of inflammatory cytokines following acute spinal cord injury in a rodent model. J Neurosci Res. 2012;90(4):782–90. [DOI] [PubMed] [Google Scholar]
- 19.Bethea JR, Nagashima H, Acosta MC, Briceno C, Gomez F, Marcillo AE, Loor K, Green J, Dietrich WD. Systemically administered interleukin-10 reduces tumor necrosis factor-alpha production and significantly improves functional recovery following traumatic spinal cord injury in rats. J Neurotrauma. 1999;16(10):851–63. [DOI] [PubMed] [Google Scholar]
- 20.Pan JZ, Ni L, Sodhi A, Aguanno A, Young W, Hart RP. Cytokine activity contributes to induction of inflammatory cytokine mRNAs in spinal cord following contusion. J Neurosci Res. 2002;68(3):315–22. [DOI] [PubMed] [Google Scholar]
- 21.Streit WJ, Semple-Rowland SL, Hurley SD, Miller RC, Popovich PG, Stokes BT. Cytokine mRNA profiles in contused spinal cord and axotomized facial nucleus suggest a beneficial role for inflammation and gliosis. Exp Neurol. 1998;152(1):74–87. [DOI] [PubMed] [Google Scholar]
- 22.Wang J, Chen J, Jin H, Lin D, Chen Y, Chen X, Wang B, Hu S, Wu Y, Wu Y, et al. BRD4 inhibition attenuates inflammatory response in microglia and facilitates recovery after spinal cord injury in rats. J Cell Mol Med. 2019;23(5):3214–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sloan SA, Darmanis S, Huber N, Khan TA, Birey F, Caneda C, Reimer R, Quake SR, Barres BA, Paşca SP. Human astrocyte maturation captured in 3D cerebral cortical spheroids derived from pluripotent stem cells. Neuron. 2017;95(4):779–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alizadeh A, Dyck SM, Karimi-Abdolrezaee S. Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Front Neurol. 2019;10:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oyinbo CA. Secondary injury mechanisms in traumatic spinal cord injury: a nugget of this multiply cascade. Acta Neurobiol Exp (Wars). 2011;71(2):281–99. [DOI] [PubMed] [Google Scholar]
- 26.Xu GY, Hughes MG, Zhang L, Cain L, McAdoo DJ. Administration of glutamate into the spinal cord at extracellular concentrations reached post-injury causes functional impairments. Neurosci Lett. 2005;384(3):271–6. [DOI] [PubMed] [Google Scholar]
- 27.Ellman DG, Degn M, Lund MC, Clausen BH, Novrup HG, Flæng SB, Jørgensen LH, Suntharalingam L, Svenningsen ÅF, Brambilla R, et al. Genetic ablation of soluble TNF does not affect lesion size and functional recovery after moderate spinal cord injury in mice. Mediators Inflamm. 2016;2016:2684098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ellman DG, Lund MC, Nissen M, Nielsen PS, Sørensen C, Lester EB, Thougaard E, Jørgensen LH, Nedospasov SA, Andersen DC et al. Conditional ablation of myeloid TNF improves functional outcome and decreases lesion size after spinal cord injury in mice. Cells. 2020; 9(11). [DOI] [PMC free article] [PubMed]
- 29.Mukhamedshina YO, Akhmetzyanova ER, Martynova EV, Khaiboullina SF, Galieva LR, Rizvanov AA. Systemic and local cytokine profile following spinal cord injury in rats: a multiplex analysis. Front Neurol. 2017;8:581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu WR, Fehlings MG. Fas/FasL-mediated apoptosis and inflammation are key features of acute human spinal cord injury: implications for translational, clinical application. Acta Neuropathol. 2011;122(6):747–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carlson SL, Parrish ME, Springer JE, Doty K, Dossett L. Acute inflammatory response in spinal cord following impact injury. Exp Neurol. 1998;151(1):77–88. [DOI] [PubMed] [Google Scholar]
- 32.Taoka Y, Okajima K, Uchiba M, Murakami K, Kushimoto S, Johno M, Naruo M, Okabe H, Takatsuki K. Role of neutrophils in spinal cord injury in the rat. Neuroscience. 1997;79(4):1177–82. [DOI] [PubMed] [Google Scholar]
- 33.Bellver-Landete V, Bretheau F, Mailhot B, Vallières N, Lessard M, Janelle ME, Vernoux N, Tremblay M, Fuehrmann T, Shoichet MS, et al. Microglia are an essential component of the neuroprotective scar that forms after spinal cord injury. Nat Commun. 2019;10(1):518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Popovich PG, Wei P, Stokes BT. Cellular inflammatory response after spinal cord injury in Sprague-Dawley and Lewis rats. J Comp Neurol. 1997;377(3):443–64. [DOI] [PubMed] [Google Scholar]
- 35.O’Shea TM, Burda JE, Sofroniew MV. Cell biology of spinal cord injury and repair. J Clin Invest. 2017;127(9):3259–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hellenbrand DJ, Quinn CM, Piper ZJ, Morehouse CN, Fixel JA, Hanna AS. Inflammation after spinal cord injury: a review of the critical timeline of signaling cues and cellular infiltration. J Neuroinflammation. 2021;18(1):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu Y, Lin YH, Shi LL, Yao ZF, Xie XM, Jiang ZS, Tang J, Hu JG, Lü HZ. Temporal kinetics of CD8(+) CD28(+) and CD8(+) CD28(−) T lymphocytes in the injured rat spinal cord. J Neurosci Res. 2017;95(8):1666–76. [DOI] [PubMed] [Google Scholar]
- 38.Anjum A, Yazid MD, Fauzi Daud M, Idris J, Ng AMH, Selvi Naicker A, Ismail OHR, Athi Kumar RK, Lokanathan Y. Spinal cord injury: pathophysiology, multimolecular interactions, and underlying recovery mechanisms. Int J Mol Sci. 2020; 21(20) [DOI] [PMC free article] [PubMed]
- 39.Garcia E, Aguilar-Cevallos J, Silva-Garcia R, Ibarra A. Cytokine and growth factor activation in vivo and in vitro after spinal cord injury. Mediators Inflamm. 2016;2016:9476020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu Z, Zhang H, Xia H, Wang B, Zhang R, Zeng Q, Guo L, Shen K, Wang B, Zhong Y, et al. CD8 T cell-derived perforin aggravates secondary spinal cord injury through destroying the blood-spinal cord barrier. Biochem Biophys Res Commun. 2019;512(2):367–72. [DOI] [PubMed] [Google Scholar]
- 41.Boyce VS, Mendell LM. Neurotrophic factors in spinal cord injury. Handb Exp Pharmacol. 2014;220:443–60. [DOI] [PubMed] [Google Scholar]
- 42.Harvey AR, Lovett SJ, Majda BT, Yoon JH, Wheeler LP, Hodgetts SI. Neurotrophic factors for spinal cord repair: which, where, how and when to apply, and for what period of time? Brain Res. 2015;1619:36–71. [DOI] [PubMed] [Google Scholar]
- 43.Wong I, Liao H, Bai X, Zaknic A, Zhong J, Guan Y, Li HY, Wang YJ, Zhou XF. ProBDNF inhibits infiltration of ED1+ macrophages after spinal cord injury. Brain Behav Immun. 2010;24(4):585–97. [DOI] [PubMed] [Google Scholar]
- 44.Lee JY, Kang SR, Yune TY. Fluoxetine prevents oligodendrocyte cell death by inhibiting microglia activation after spinal cord injury. J Neurotrauma. 2015;32(9):633–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yune TY, Lee JY, Jung GY, Kim SJ, Jiang MH, Kim YC, Oh YJ, Markelonis GJ, Oh TH. Minocycline alleviates death of oligodendrocytes by inhibiting pro-nerve growth factor production in microglia after spinal cord injury. J Neurosci. 2007;27(29):7751–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ryu JC, Tooke K, Malley SE, Soulas A, Weiss T, Ganesh N, Saidi N, Daugherty S, Saragovi U, Ikeda Y, et al. Role of proNGF/p75 signaling in bladder dysfunction after spinal cord injury. J Clin Invest. 2018;128(5):1772–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bi J, Chen C, Sun P, Tan H, Feng F, Shen J. Neuroprotective effect of omega-3 fatty acids on spinal cord injury induced rats. Brain Behav. 2019;9(8):e01339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen C, Yang Q, Ma X. Synergistic effect of ascorbic acid and taurine in the treatment of a spinal cord injury-induced model in rats. 3 Biotech. 2020;10(2):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang H, Xiang Z, Duan X, Jiang JL, Xing YM, Zhu C, Song Q, Yu QR. Antitumor and anti-inflammatory effects of oligosaccharides from Cistanche deserticola extract on spinal cord injury. Int J Biol Macromol. 2019;124:360–7. [DOI] [PubMed] [Google Scholar]
- 50.Liu WM, Wu JY, Li FC, Chen QX. Ion channel blockers and spinal cord injury. J Neurosci Res. 2011;89(6):791–801. [DOI] [PubMed] [Google Scholar]
- 51.Bacia A, Wollmann R, Soliven B. K+ channel blockade impairs remyelination in the cuprizone model. Glia. 2004;48(2):156–65. [DOI] [PubMed] [Google Scholar]
- 52.Kulkarni R, Thakur A, Kumar H. Microtubule dynamics following central and peripheral nervous system axotomy. ACS Chem Neurosci. 2022;13(9):1358–69. [DOI] [PubMed] [Google Scholar]
- 53.Maekawa M, Ishizaki T, Boku S, Watanabe N, Fujita A, Iwamatsu A, Obinata T, Ohashi K, Mizuno K, Narumiya S. Signaling from Rho to the actin cytoskeleton through protein kinases ROCK and LIM-kinase. Science. 1999;285(5429):895–8. [DOI] [PubMed] [Google Scholar]
- 54.Mulherkar S, Tolias KF. RhoA-ROCK signaling as a therapeutic target in traumatic brain injury. Cells. 2020; 9(1). [DOI] [PMC free article] [PubMed]
- 55.Kar AN, Lee SJ, Sahoo PK, Thames E, Yoo S, Houle JD, Twiss JL. MicroRNAs 21 and 199a-3p regulate axon growth potential through modulation of Pten and mTor mRNAs. eNeuro. 2021; 8(4). [DOI] [PMC free article] [PubMed]
- 56.Liu G, Detloff MR, Miller KN, Santi L, Houlé JD. Exercise modulates microRNAs that affect the PTEN/mTOR pathway in rats after spinal cord injury. Exp Neurol. 2012;233(1):447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saikia JM, Chavez-Martinez CL, Kim ND, Allibhoy S, Kim HJ, Simonyan L, Smadi S, Tsai KM, Romaus-Sanjurjo D, Jin Y, et al. A critical role for DLK and LZK in axonal repair in the mammalian spinal cord. J Neurosci. 2022;42(18):3716–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li Y, Kang S, Halawani D, Wang Y, Junqueira Alves C, Ramakrishnan A, Estill M, Shen L, Li F, He X, et al. Macrophages facilitate peripheral nerve regeneration by organizing regeneration tracks through Plexin-B2. Genes Dev. 2022;36(3–4):133–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou X, Wahane S, Friedl MS, Kluge M, Friedel CC, Avrampou K, Zachariou V, Guo L, Zhang B, He X, et al. Microglia and macrophages promote corralling, wound compaction and recovery after spinal cord injury via Plexin-B2. Nat Neurosci. 2020;23(3):337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim H, Leng K, Park J, Sorets AG, Kim S, Shostak A, Embalabala RJ, Mlouk K, Katdare KA, Rose IVL, et al. Reactive astrocytes transduce inflammation in a blood-brain barrier model through a TNF-STAT3 signaling axis and secretion of alpha 1-antichymotrypsin. Nat Commun. 2022;13(1):6581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li X, Li M, Tian L, Chen J, Liu R, Ning B. Reactive astrogliosis: implications in spinal cord injury progression and therapy. Oxid Med Cell Longev. 2020;2020:9494352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xie C, Shen X, Xu X, Liu H, Li F, Lu S, Gao Z, Zhang J, Wu Q, Yang D, et al. Astrocytic YAP promotes the formation of glia scars and neural regeneration after spinal cord injury. J Neurosci. 2020;40(13):2644–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.He X, Li Y, Deng B, Lin A, Zhang G, Ma M, Wang Y, Yang Y, Kang X. The PI3K/AKT signalling pathway in inflammation, cell death and glial scar formation after traumatic spinal cord injury: mechanisms and therapeutic opportunities. Cell Prolif. 2022;55(9):e13275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hara M, Kobayakawa K, Ohkawa Y, Kumamaru H, Yokota K, Saito T, Kijima K, Yoshizaki S, Harimaya K, Nakashima Y, et al. Interaction of reactive astrocytes with type I collagen induces astrocytic scar formation through the integrin-N-cadherin pathway after spinal cord injury. Nat Med. 2017;23(7):818–28. [DOI] [PubMed] [Google Scholar]
- 65.Verkhratsky A, Butt A, Li B, Illes P, Zorec R, Semyanov A, Tang Y, Sofroniew MV. Astrocytes in human central nervous system diseases: a frontier for new therapies. Signal Transduct Target Ther. 2023;8(1):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Escartin C, Galea E, Lakatos A, O’Callaghan JP, Petzold GC, Serrano-Pozo A, Steinhäuser C, Volterra A, Carmignoto G, Agarwal A, et al. Reactive astrocyte nomenclature, definitions, and future directions. Nat Neurosci. 2021;24(3):312–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sofroniew MV. Astrocyte reactivity: subtypes, states, and functions in CNS innate immunity. Trends Immunol. 2020;41(9):758–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liddelow SA, Olsen ML, Sofroniew MV. Reactive astrocytes and emerging roles in central nervous system (CNS) disorders. Cold Spring Harb Perspect Biol. 2024; 16(7). [DOI] [PMC free article] [PubMed]
- 69.O'Shea TM, Ao Y, Wang S, Ren Y, Cheng AL, Kawaguchi R, Shi Z, Swarup V, Sofroniew MV. Derivation and transcriptional reprogramming of border-forming wound repair astrocytes after spinal cord injury or stroke in mice. Nat Neurosci. 2024. [DOI] [PMC free article] [PubMed]
- 70.Bigler R, Stamm O. Long-term chemotherapy of ovarian carcinomas with reference to the enzyme pattern. Arch Gynakol. 1971;211(1):345–6. [DOI] [PubMed] [Google Scholar]
- 71.Göritz C, Dias DO, Tomilin N, Barbacid M, Shupliakov O, Frisén J. A pericyte origin of spinal cord scar tissue. Science. 2011;333(6039):238–42. [DOI] [PubMed] [Google Scholar]
- 72.Picoli CC, Coimbra-Campos LMC, Guerra DAP, Silva WN, Prazeres P, Costa AC, Magno LAV, Romano-Silva MA, Mintz A, Birbrair A. Pericytes act as key players in spinal cord injury. Am J Pathol. 2019;189(7):1327–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aragonès Benaiges E. Evaluation of the Accutrend GC for cholesterol determination. Aten Primaria. 1996;18(9):528. [PubMed] [Google Scholar]
- 74.Costa G, Ribeiro FF, Sebastião AM, Muir EM, Vaz SH. Bridging the gap of axonal regeneration in the central nervous system: a state of the art review on central axonal regeneration. Front Neurosci. 2022;16:1003145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fisher D, Xing B, Dill J, Li H, Hoang HH, Zhao Z, Yang XL, Bachoo R, Cannon S, Longo FM, et al. Leukocyte common antigen-related phosphatase is a functional receptor for chondroitin sulfate proteoglycan axon growth inhibitors. J Neurosci. 2011;31(40):14051–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rodemer W, Zhang G, Sinitsa I, Hu J, Jin LQ, Li S, Selzer ME. PTPσ knockdown in lampreys impairs reticulospinal axon regeneration and neuronal survival after spinal cord injury. Front Cell Neurosci. 2020;14:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shen Y, Tenney AP, Busch SA, Horn KP, Cuascut FX, Liu K, He Z, Silver J, Flanagan JG. PTPsigma is a receptor for chondroitin sulfate proteoglycan, an inhibitor of neural regeneration. Science. 2009;326(5952):592–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sivasankaran R, Pei J, Wang KC, Zhang YP, Shields CB, Xu XM, He Z. PKC mediates inhibitory effects of myelin and chondroitin sulfate proteoglycans on axonal regeneration. Nat Neurosci. 2004;7(3):261–8. [DOI] [PubMed] [Google Scholar]
- 79.Tran AP, Warren PM, Silver J. Regulation of autophagy by inhibitory CSPG interactions with receptor PTPσ and its impact on plasticity and regeneration after spinal cord injury. Exp Neurol. 2020;328:113276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Francos-Quijorna I, Sánchez-Petidier M, Burnside ER, Badea SR, Torres-Espin A, Marshall L, de Winter F, Verhaagen J, Moreno-Manzano V, Bradbury EJ. Chondroitin sulfate proteoglycans prevent immune cell phenotypic conversion and inflammation resolution via TLR4 in rodent models of spinal cord injury. Nat Commun. 2022;13(1):2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bradbury EJ, Burnside ER. Moving beyond the glial scar for spinal cord repair. Nat Commun. 2019;10(1):3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang X, Cao K, Sun X, Chen Y, Duan Z, Sun L, Guo L, Bai P, Sun D, Fan J, et al. Macrophages in spinal cord injury: phenotypic and functional change from exposure to myelin debris. Glia. 2015;63(4):635–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Llorens F, Gil V, del Río JA. Emerging functions of myelin-associated proteins during development, neuronal plasticity, and neurodegeneration. FASEB J. 2011;25(2):463–75. [DOI] [PubMed] [Google Scholar]
- 84.Cafferty WB, Duffy P, Huebner E, Strittmatter SM. MAG and OMgp synergize with Nogo-A to restrict axonal growth and neurological recovery after spinal cord trauma. J Neurosci. 2010;30(20):6825–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu Y, Hammel G, Shi M, Cheng Z, Zivkovic S, Wang X, Xu P, He X, Guo B, Ren Y, et al. Myelin debris stimulates NG2/CSPG4 expression in bone marrow-derived macrophages in the injured spinal cord. Front Cell Neurosci. 2021;15:651827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Keating A. Mesenchymal stromal cells: new directions. Cell Stem Cell. 2012;10(6):709–16. [DOI] [PubMed] [Google Scholar]
- 87.Le Blanc K, Mougiakakos D. Multipotent mesenchymal stromal cells and the innate immune system. Nat Rev Immunol. 2012;12(5):383–96. [DOI] [PubMed] [Google Scholar]
- 88.Lee RH, Yoon N, Reneau JC, Prockop DJ. Preactivation of human MSCs with TNF-α enhances tumor-suppressive activity. Cell Stem Cell. 2012;11(6):825–35. [DOI] [PubMed] [Google Scholar]
- 89.Chiossone L, Conte R, Spaggiari GM, Serra M, Romei C, Bellora F, Becchetti F, Andaloro A, Moretta L, Bottino C. Mesenchymal stromal cells induce peculiar alternatively activated macrophages capable of dampening both innate and adaptive immune responses. Stem Cells. 2016;34(7):1909–21. [DOI] [PubMed] [Google Scholar]
- 90.Petri RM, Hackel A, Hahnel K, Dumitru CA, Bruderek K, Flohe SB, Paschen A, Lang S, Brandau S. Activated tissue-resident mesenchymal stromal cells regulate natural killer cell immune and tissue-regenerative function. Stem Cell Rep. 2017;9(3):985–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rashedi I, Gómez-Aristizábal A, Wang XH, Viswanathan S, Keating A. TLR3 or TLR4 activation enhances mesenchymal stromal cell-mediated treg induction via notch signaling. Stem Cells. 2017;35(1):265–75. [DOI] [PubMed] [Google Scholar]
- 92.Fang J, Hou P, Liu S, Zuo M, Liu Z, Chen W, Han Y, Li Y, Wang T, Feng C, et al. NAD(+) salvage governs the immunosuppressive capacity of mesenchymal stem cells. Cell Mol Immunol. 2023;20(10):1171–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Serrenho I, Ferreira SA, Baltazar G. Preconditioning of MSCs for acute neurological conditions: from cellular to functional impact-a systematic review. Cells. 2024; 13(10). [DOI] [PMC free article] [PubMed]
- 94.Anderson MA, Burda JE, Ren Y, Ao Y, O’Shea TM, Kawaguchi R, Coppola G, Khakh BS, Deming TJ, Sofroniew MV. Astrocyte scar formation aids central nervous system axon regeneration. Nature. 2016;532(7598):195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yang C, Wang G, Ma F, Yu B, Chen F, Yang J, Feng J, Wang Q. Repeated injections of human umbilical cord blood-derived mesenchymal stem cells significantly promotes functional recovery in rabbits with spinal cord injury of two noncontinuous segments. Stem Cell Res Ther. 2018;9(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Diehl R, Ferrara F, Müller C, Dreyer AY, McLeod DD, Fricke S, Boltze J. Immunosuppression for in vivo research: state-of-the-art protocols and experimental approaches. Cell Mol Immunol. 2017;14(2):146–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang R, Liu Y, Yan K, Chen L, Chen XR, Li P, Chen FF, Jiang XD. Anti-inflammatory and immunomodulatory mechanisms of mesenchymal stem cell transplantation in experimental traumatic brain injury. J Neuroinflammation. 2013;10:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Brandau S, Jakob M, Hemeda H, Bruderek K, Janeschik S, Bootz F, Lang S. Tissue-resident mesenchymal stem cells attract peripheral blood neutrophils and enhance their inflammatory activity in response to microbial challenge. J Leukoc Biol. 2010;88(5):1005–15. [DOI] [PubMed] [Google Scholar]
- 99.Cassatella MA, Mosna F, Micheletti A, Lisi V, Tamassia N, Cont C, Calzetti F, Pelletier M, Pizzolo G, Krampera M. Toll-like receptor-3-activated human mesenchymal stromal cells significantly prolong the survival and function of neutrophils. Stem Cells. 2011;29(6):1001–11. [DOI] [PubMed] [Google Scholar]
- 100.Valiukevičius P, Mačiulaitis J, Pangonytė D, Siratavičiūtė V, Kluszczyńska K, Kuzaitytė U, Insodaitė R, Čiapienė I, Grigalevičiūtė R, Zigmantaitė V et al. Human placental mesenchymal stem cells and derived extracellular vesicles ameliorate lung injury in acute respiratory distress syndrome murine model. Cells. 2023; 12(23). [DOI] [PMC free article] [PubMed]
- 101.Jiang D, Muschhammer J, Qi Y, Kügler A, de Vries JC, Saffarzadeh M, Sindrilaru A, Beken SV, Wlaschek M, Kluth MA, et al. Suppression of neutrophil-mediated tissue damage: a novel skill of mesenchymal stem cells. Stem Cells. 2016;34(9):2393–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nakajima H, Uchida K, Guerrero AR, Watanabe S, Sugita D, Takeura N, Yoshida A, Long G, Wright KT, Johnson WE, et al. Transplantation of mesenchymal stem cells promotes an alternative pathway of macrophage activation and functional recovery after spinal cord injury. J Neurotrauma. 2012;29(8):1614–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhou HL, Zhang XJ, Zhang MY, Yan ZJ, Xu ZM, Xu RX. Transplantation of human amniotic mesenchymal stem cells promotes functional recovery in a rat model of traumatic spinal cord injury. Neurochem Res. 2016;41(10):2708–18. [DOI] [PubMed] [Google Scholar]
- 104.Liu YC, Zou XB, Chai YF, Yao YM. Macrophage polarization in inflammatory diseases. Int J Biol Sci. 2014;10(5):520–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Li B, Hu Y, Zhao Y, Cheng M, Qin H, Cheng T, Wang Q, Peng X, Zhang X. Curcumin attenuates titanium particle-induced inflammation by regulating macrophage polarization in vitro and in vivo. Front Immunol. 2017;8:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8(12):958–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pérez S, Rius-Pérez S. Macrophage polarization and reprogramming in acute inflammation: a redox perspective. Antioxidants (Basel). 2022; 11(7). [DOI] [PMC free article] [PubMed]
- 108.Van Dyken SJ, Locksley RM. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu Rev Immunol. 2013;31:317–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yunna C, Mengru H, Lei W, Weidong C. Macrophage M1/M2 polarization. Eur J Pharmacol. 2020;877:173090. [DOI] [PubMed] [Google Scholar]
- 110.An N, Yang J, Wang H, Sun S, Wu H, Li L, Li M. Mechanism of mesenchymal stem cells in spinal cord injury repair through macrophage polarization. Cell Biosci. 2021;11(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Czimmerer Z, Varga T, Kiss M, Vázquez CO, Doan-Xuan QM, Rückerl D, Tattikota SG, Yan X, Nagy ZS, Daniel B, et al. The IL-4/STAT6 signaling axis establishes a conserved microRNA signature in human and mouse macrophages regulating cell survival via miR-342-3p. Genome Med. 2016;8(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hao J, Hu Y, Li Y, Zhou Q, Lv X. Involvement of JNK signaling in IL4-induced M2 macrophage polarization. Exp Cell Res. 2017;357(2):155–62. [DOI] [PubMed] [Google Scholar]
- 113.Junttila IS. Tuning the cytokine responses: an update on interleukin (IL)-4 and IL-13 receptor complexes. Front Immunol. 2018;9:888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Dooley D, Lemmens E, Vangansewinkel T, Le Blon D, Hoornaert C, Ponsaerts P, Hendrix S. Cell-based delivery of interleukin-13 directs alternative activation of macrophages resulting in improved functional outcome after spinal cord injury. Stem Cell Rep. 2016;7(6):1099–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhu X, Wang Z, Sun YE, Liu Y, Wu Z, Ma B, Cheng L. Neuroprotective effects of human umbilical cord-derived mesenchymal stem cells from different donors on spinal cord injury in mice. Front Cell Neurosci. 2021;15:768711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhai X, Chen K, Yang H, Li B, Zhou T, Wang H, Zhou H, Chen S, Zhou X, Wei X, et al. Extracellular vesicles derived from CD73 modified human umbilical cord mesenchymal stem cells ameliorate inflammation after spinal cord injury. J Nanobiotechnology. 2021;19(1):274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yang T, Dai Y, Chen G, Cui S. Dissecting the dual role of the glial scar and scar-forming astrocytes in spinal cord injury. Front Cell Neurosci. 2020;14:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chaubey S, Thueson S, Ponnalagu D, Alam MA, Gheorghe CP, Aghai Z, Singh H, Bhandari V. Early gestational mesenchymal stem cell secretome attenuates experimental bronchopulmonary dysplasia in part via exosome-associated factor TSG-6. Stem Cell Res Ther. 2018;9(1):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sun G, Li G, Li D, Huang W, Zhang R, Zhang H, Duan Y, Wang B. hucMSC derived exosomes promote functional recovery in spinal cord injury mice via attenuating inflammation. Mater Sci Eng C Mater Biol Appl. 2018;89:194–204. [DOI] [PubMed] [Google Scholar]
- 120.Lian H, Yang L, Cole A, Sun L, Chiang AC, Fowler SW, Shim DJ, Rodriguez-Rivera J, Taglialatela G, Jankowsky JL, et al. NFκB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer’s disease. Neuron. 2015;85(1):101–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, Bennett ML, Münch AE, Chung WS, Peterson TC, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541(7638):481–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mukhamedshina Y, Shulman I, Ogurcov S, Kostennikov A, Zakirova E, Akhmetzyanova E, Rogozhin A, Masgutova G, James V, Masgutov R et al. Mesenchymal stem cell therapy for spinal cord contusion: a comparative study on small and large animal models. Biomolecules. 2019;9(12). [DOI] [PMC free article] [PubMed]
- 123.Yang Z, Liang Z, Rao J, Xie H, Zhou M, Xu X, Lin Y, Lin F, Wang C, Chen C. Hypoxic-preconditioned mesenchymal stem cell-derived small extracellular vesicles promote the recovery of spinal cord injury by affecting the phenotype of astrocytes through the miR-21/JAK2/STAT3 pathway. CNS Neurosci Ther. 2024;30(3):e14428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhou Z, Tian X, Mo B, Xu H, Zhang L, Huang L, Yao S, Huang Z, Wang Y, Xie H, et al. Adipose mesenchymal stem cell transplantation alleviates spinal cord injury-induced neuroinflammation partly by suppressing the Jagged1/Notch pathway. Stem Cell Res Ther. 2020;11(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhao L, Hu C, Han F, Cai F, Wang J, Chen J. Preconditioning is an effective strategy for improving the efficiency of mesenchymal stem cells in kidney transplantation. Stem Cell Res Ther. 2020;11(1):197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.He C, Yang Y, Zheng K, Chen Y, Liu S, Li Y, Han Q, Zhao RC, Wang L, Zhang F. Mesenchymal stem cell-based treatment in autoimmune liver diseases: underlying roles, advantages and challenges. Ther Adv Chronic Dis. 2021;12:2040622321993442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pachler K, Ketterl N, Desgeorges A, Dunai ZA, Laner-Plamberger S, Streif D, Strunk D, Rohde E, Gimona M. An in vitro potency assay for monitoring the immunomodulatory potential of stromal cell-derived extracellular vesicles. Int J Mol Sci. 2017;18(7). [DOI] [PMC free article] [PubMed]
- 128.Deng J, Li M, Meng F, Liu Z, Wang S, Zhang Y, Li M, Li Z, Zhang L, Tang P. 3D spheroids of human placenta-derived mesenchymal stem cells attenuate spinal cord injury in mice. Cell Death Dis. 2021;12(12):1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Xu C, Diao YF, Wang J, Liang J, Xu HH, Zhao ML, Zheng B, Luan Z, Wang JJ, Yang XP, et al. Intravenously infusing the secretome of adipose-derived mesenchymal stem cells ameliorates neuroinflammation and neurological functioning after traumatic brain injury. Stem Cells Dev. 2020;29(4):222–34. [DOI] [PubMed] [Google Scholar]
- 130.Yang L, Cao J, Du Y, Zhang X, Hong W, Peng B, Wu J, Weng Q, Wang J, Gao J. Initial IL-10 production dominates the therapy of mesenchymal stem cell scaffold in spinal cord injury. Theranostics. 2024;14(2):879–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Urdzíková LM, Růžička J, LaBagnara M, Kárová K, Kubinová Š, Jiráková K, Murali R, Syková E, Jhanwar-Uniyal M, Jendelová P. Human mesenchymal stem cells modulate inflammatory cytokines after spinal cord injury in rat. Int J Mol Sci. 2014;15(7):11275–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wang B, Chang M, Zhang R, Wo J, Wu B, Zhang H, Zhou Z, Li Z, Zhang F, Zhong C, et al. Spinal cord injury target-immunotherapy with TNF-α autoregulated and feedback-controlled human umbilical cord mesenchymal stem cell derived exosomes remodelled by CRISPR/Cas9 plasmid. Biomater Adv. 2022;133:112624. [DOI] [PubMed] [Google Scholar]
- 133.Knerlich-Lukoschus F, von der Ropp-Brenner B, Lucius R, Mehdorn HM, Held-Feindt J. Spatiotemporal CCR1, CCL3(MIP-1α), CXCR4, CXCL12(SDF-1α) expression patterns in a rat spinal cord injury model of posttraumatic neuropathic pain. J Neurosurg Spine. 2011;14(5):583–97. [DOI] [PubMed] [Google Scholar]
- 134.Liu SQ, Ma YG, Peng H, Fan L. Monocyte chemoattractant protein-1 level in serum of patients with acute spinal cord injury. Chin J Traumatol. 2005;8(4):216–9. [PubMed] [Google Scholar]
- 135.Pineau I, Sun L, Bastien D, Lacroix S. Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain Behav Immun. 2010;24(4):540–53. [DOI] [PubMed] [Google Scholar]
- 136.Wynn RF, Hart CA, Corradi-Perini C, O’Neill L, Evans CA, Wraith JE, Fairbairn LJ, Bellantuono I. A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood. 2004;104(9):2643–5. [DOI] [PubMed] [Google Scholar]
- 137.Li L, Yang M, Wang C, Zhao Q, Liu J, Zhan C, Liu Z, Li X, Wang W, Yang X. Effects of cytokines and chemokines on migration of mesenchymal stem cells following spinal cord injury. Neural Regen Res. 2012;7(14):1106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Papa S, Vismara I, Mariani A, Barilani M, Rimondo S, De Paola M, Panini N, Erba E, Mauri E, Rossi F, et al. Mesenchymal stem cells encapsulated into biomimetic hydrogel scaffold gradually release CCL2 chemokine in situ preserving cytoarchitecture and promoting functional recovery in spinal cord injury. J Control Release. 2018;278:49–56. [DOI] [PubMed] [Google Scholar]
- 139.Kim Y, Jo SH, Kim WH, Kweon OK. Antioxidant and anti-inflammatory effects of intravenously injected adipose derived mesenchymal stem cells in dogs with acute spinal cord injury. Stem Cell Res Ther. 2015;6:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, Patel DN, Bauer AJ, Cantley AM, Yang WS, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Shi Z, Yuan S, Shi L, Li J, Ning G, Kong X, Feng S. Programmed cell death in spinal cord injury pathogenesis and therapy. Cell Prolif. 2021;54(3):e12992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yao S, Pang M, Wang Y, Wang X, Lin Y, Lv Y, Xie Z, Hou J, Du C, Qiu Y, et al. Mesenchymal stem cell attenuates spinal cord injury by inhibiting mitochondrial quality control-associated neuronal ferroptosis. Redox Biol. 2023;67:102871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Shao C, Chen Y, Yang T, Zhao H, Li D. Mesenchymal stem cell derived exosomes suppress neuronal cell ferroptosis via lncGm36569/miR-5627-5p/FSP1 axis in acute spinal cord injury. Stem Cell Rev Rep. 2022;18(3):1127–42. [DOI] [PubMed] [Google Scholar]
- 144.Huang JH, Fu CH, Xu Y, Yin XM, Cao Y, Lin FY. Extracellular vesicles derived from epidural fat-mesenchymal stem cells attenuate NLRP3 inflammasome activation and improve functional recovery after spinal cord injury. Neurochem Res. 2020;45(4):760–71. [DOI] [PubMed] [Google Scholar]
- 145.Nazari S, Pourmand SM, Motevaseli E, Hassanzadeh G. Mesenchymal stem cells (MSCs) and MSC-derived exosomes in animal models of central nervous system diseases: targeting the NLRP3 inflammasome. IUBMB Life. 2023;75(10):794–810. [DOI] [PubMed] [Google Scholar]
- 146.Mohamadi Y, Noori Moghahi SMH, Mousavi M, Borhani-Haghighi M, Abolhassani F, Kashani IR, Hassanzadeh G. Intrathecal transplantation of Wharton’s jelly mesenchymal stem cells suppresses the NLRP1 inflammasome in the rat model of spinal cord injury. J Chem Neuroanat. 2019;97:1–8. [DOI] [PubMed] [Google Scholar]
- 147.Kelley N, Jeltema D, Duan Y, He Y. The nlrp3 inflammasome: an overview of mechanisms of activation and regulation. Int J Mol Sci. 2019; 20(13). [DOI] [PMC free article] [PubMed]
- 148.Bauernfeind FG, Horvath G, Stutz A, Alnemri ES, MacDonald K, Speert D, Fernandes-Alnemri T, Wu J, Monks BG, Fitzgerald KA, et al. Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J Immunol. 2009;183(2):787–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gao S, Xu T, Guo H, Deng Q, Xun C, Liang W, Sheng W. Ameliorative effects of echinacoside against spinal cord injury via inhibiting NLRP3 inflammasome signaling pathway. Life Sci. 2019;237:116978. [DOI] [PubMed] [Google Scholar]
- 150.Xu S, Wang J, Zhong J, Shao M, Jiang J, Song J, Zhu W, Zhang F, Xu H, Xu G, et al. CD73 alleviates GSDMD-mediated microglia pyroptosis in spinal cord injury through PI3K/AKT/Foxo1 signaling. Clin Transl Med. 2021;11(1):e269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gu J, Wu J, Wang C, Xu Z, Jin Z, Yan D, Chen S. BMSCs-derived exosomes inhibit macrophage/microglia pyroptosis by increasing autophagy through the miR-21a-5p/PELI1 axis in spinal cord injury. Aging (Albany NY). 2024;16(6):5184–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhou Y, Wen LL, Li YF, Wu KM, Duan RR, Yao YB, Jing LJ, Gong Z, Teng JF, Jia YJ. Exosomes derived from bone marrow mesenchymal stem cells protect the injured spinal cord by inhibiting pericyte pyroptosis. Neural Regen Res. 2022;17(1):194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhao Y, Chen Y, Wang Z, Xu C, Qiao S, Liu T, Qi K, Tong D, Li C. Bone marrow mesenchymal stem cell exosome attenuates inflammasome-related pyroptosis via delivering circ_003564 to improve the recovery of spinal cord injury. Mol Neurobiol. 2022;59(11):6771–89. [DOI] [PubMed] [Google Scholar]
- 154.Voulgari-Kokota A, Fairless R, Karamita M, Kyrargyri V, Tseveleki V, Evangelidou M, Delorme B, Charbord P, Diem R, Probert L. Mesenchymal stem cells protect CNS neurons against glutamate excitotoxicity by inhibiting glutamate receptor expression and function. Exp Neurol. 2012;236(1):161–70. [DOI] [PubMed] [Google Scholar]
- 155.Duan DP, Su Q, Hu W, You WL, Dang XQ, Wang KZ. Analysis of chronergy for treatment of spinal cord injury with the allogeneic bone mesenchymal stem cells (BMscs) transplantation in rats. Zhongguo Gu Shang. 2013;26(10):845–9. [PubMed] [Google Scholar]
- 156.Wu LL, Pan XM, Chen HH, Fu XY, Jiang J, Ding MX. Repairing and analgesic effects of umbilical cord mesenchymal stem cell transplantation in mice with spinal cord injury. Biomed Res Int. 2020;2020:7650354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Quertainmont R, Cantinieaux D, Botman O, Sid S, Schoenen J, Franzen R. Mesenchymal stem cell graft improves recovery after spinal cord injury in adult rats through neurotrophic and pro-angiogenic actions. PLoS ONE. 2012;7(6):e39500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chen D, Zeng W, Fu Y, Gao M, Lv G. Bone marrow mesenchymal stem cells combined with minocycline improve spinal cord injury in a rat model. Int J Clin Exp Pathol. 2015;8(10):11957–69. [PMC free article] [PubMed] [Google Scholar]
- 159.Wei P, Jia M, Kong X, Lyu W, Feng H, Sun X, Li J, Yang JJ. Human umbilical cord-derived mesenchymal stem cells ameliorate perioperative neurocognitive disorder by inhibiting inflammatory responses and activating BDNF/TrkB/CREB signaling pathway in aged mice. Stem Cell Res Ther. 2023;14(1):263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Cao T, Chen H, Huang W, Xu S, Liu P, Zou W, Pang M, Xu Y, Bai X, Liu B, et al. hUC-MSC-mediated recovery of subacute spinal cord injury through enhancing the pivotal subunits β3 and γ2 of the GABA(A) receptor. Theranostics. 2022;12(7):3057–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ozdinler PH, Macklis JD. IGF-I specifically enhances axon outgrowth of corticospinal motor neurons. Nat Neurosci. 2006;9(11):1371–81. [DOI] [PubMed] [Google Scholar]
- 162.Schnell L, Schneider R, Kolbeck R, Barde YA, Schwab ME. Neurotrophin-3 enhances sprouting of corticospinal tract during development and after adult spinal cord lesion. Nature. 1994;367(6459):170–3. [DOI] [PubMed] [Google Scholar]
- 163.Bilimoria PM, Bonni A. Molecular control of axon branching. Neuroscientist. 2013;19(1):16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Vavrek R, Girgis J, Tetzlaff W, Hiebert GW, Fouad K. BDNF promotes connections of corticospinal neurons onto spared descending interneurons in spinal cord injured rats. Brain. 2006;129(Pt 6):1534–45. [DOI] [PubMed] [Google Scholar]
- 165.Bottai D, Scesa G, Cigognini D, Adami R, Nicora E, Abrignani S, Di Giulio AM, Gorio A. Third trimester NG2-positive amniotic fluid cells are effective in improving repair in spinal cord injury. Exp Neurol. 2014;254:121–33. [DOI] [PubMed] [Google Scholar]
- 166.Hu SL, Luo HS, Li JT, Xia YZ, Li L, Zhang LJ, Meng H, Cui GY, Chen Z, Wu N, et al. Functional recovery in acute traumatic spinal cord injury after transplantation of human umbilical cord mesenchymal stem cells. Crit Care Med. 2010;38(11):2181–9. [DOI] [PubMed] [Google Scholar]
- 167.Park SS, Byeon YE, Ryu HH, Kang BJ, Kim Y, Kim WH, Kang KS, Han HJ, Kweon OK. Comparison of canine umbilical cord blood-derived mesenchymal stem cell transplantation times: involvement of astrogliosis, inflammation, intracellular actin cytoskeleton pathways, and neurotrophin-3. Cell Transplant. 2011;20(11–12):1867–80. [DOI] [PubMed] [Google Scholar]
- 168.Xiao X, Li W, Rong D, Xu Z, Zhang Z, Ye H, Xie L, Wu Y, Zhang Y, Wang X. Human umbilical cord mesenchymal stem cells-derived extracellular vesicles facilitate the repair of spinal cord injury via the miR-29b-3p/PTEN/Akt/mTOR axis. Cell Death Discov. 2021;7(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Liu AM, Chen BL, Yu LT, Liu T, Shi LL, Yu PP, Qu YB, So KF, Zhou LB. Human adipose tissue- and umbilical cord-derived stem cells: which is a better alternative to treat spinal cord injury? Neural Regen Res. 2020;15(12):2306–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wu Q, Wang Q, Li Z, Li X, Zang J, Wang Z, Xu C, Gong Y, Cheng J, Li H, et al. Human menstrual blood-derived stem cells promote functional recovery in a rat spinal cord hemisection model. Cell Death Dis. 2018;9(9):882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Veeravalli KK, Dasari VR, Tsung AJ, Dinh DH, Gujrati M, Fassett D, Rao JS. Human umbilical cord blood stem cells upregulate matrix metalloproteinase-2 in rats after spinal cord injury. Neurobiol Dis. 2009;36(1):200–12. [DOI] [PubMed] [Google Scholar]
- 172.Wright KT, El Masri W, Osman A, Roberts S, Chamberlain G, Ashton BA, Johnson WE. Bone marrow stromal cells stimulate neurite outgrowth over neural proteoglycans (CSPG), myelin associated glycoprotein and Nogo-A. Biochem Biophys Res Commun. 2007;354(2):559–66. [DOI] [PubMed] [Google Scholar]
- 173.Albu S, Kumru H, Coll R, Vives J, Vallés M, Benito-Penalva J, Rodríguez L, Codinach M, Hernández J, Navarro X, et al. Clinical effects of intrathecal administration of expanded Wharton jelly mesenchymal stromal cells in patients with chronic complete spinal cord injury: a randomized controlled study. Cytotherapy. 2021;23(2):146–56. [DOI] [PubMed] [Google Scholar]
- 174.Cheng H, Liu X, Hua R, Dai G, Wang X, Gao J, An Y. Clinical observation of umbilical cord mesenchymal stem cell transplantation in treatment for sequelae of thoracolumbar spinal cord injury. J Transl Med. 2014;12:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Deng WS, Ma K, Liang B, Liu XY, Xu HY, Zhang J, Shi HY, Sun HT, Chen XY, Zhang S. Collagen scaffold combined with human umbilical cord-mesenchymal stem cells transplantation for acute complete spinal cord injury. Neural Regen Res. 2020;15(9):1686–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Geffner LF, Santacruz P, Izurieta M, Flor L, Maldonado B, Auad AH, Montenegro X, Gonzalez R, Silva F. Administration of autologous bone marrow stem cells into spinal cord injury patients via multiple routes is safe and improves their quality of life: comprehensive case studies. Cell Transplant. 2008;17(12):1277–93. [DOI] [PubMed] [Google Scholar]
- 177.Hur JW, Cho TH, Park DH, Lee JB, Park JY, Chung YG. Intrathecal transplantation of autologous adipose-derived mesenchymal stem cells for treating spinal cord injury: a human trial. J Spinal Cord Med. 2016;39(6):655–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mendonça MV, Larocca TF, de Freitas Souza BS, Villarreal CF, Silva LF, Matos AC, Novaes MA, Bahia CM, de Oliveira Melo Martinez AC, Kaneto CM et al. Safety and neurological assessments after autologous transplantation of bone marrow mesenchymal stem cells in subjects with chronic spinal cord injury. Stem Cell Res Ther. 2014;5(6):126. [DOI] [PMC free article] [PubMed]
- 179.Park JH, Kim DY, Sung IY, Choi GH, Jeon MH, Kim KK, Jeon SR. Long-term results of spinal cord injury therapy using mesenchymal stem cells derived from bone marrow in humans. Neurosurgery. 2012; 70(5):1238–1247; discussion 1247. [DOI] [PubMed]
- 180.Bydon M, Qu W, Moinuddin FM, Hunt CL, Garlanger KL, Reeves RK, Windebank AJ, Zhao KD, Jarrah R, Trammell BC, et al. Intrathecal delivery of adipose-derived mesenchymal stem cells in traumatic spinal cord injury: Phase I trial. Nat Commun. 2024;15(1):2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Cui LL, Golubczyk D, Tolppanen AM, Boltze J, Jolkkonen J. Cell therapy for ischemic stroke: Are differences in preclinical and clinical study design responsible for the translational loss of efficacy? Ann Neurol. 2019;86(1):5–16. [DOI] [PubMed] [Google Scholar]
- 182.Lu Y, Zhang W, Tian Z, Liang Q, Liu C, Wu Y, Zhang L, Rong L. The optimal transplantation strategy of umbilical cord mesenchymal stem cells in spinal cord injury: a systematic review and network meta-analysis based on animal studies. Stem Cell Res Ther. 2022;13(1):441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Shang Z, Wang R, Li D, Chen J, Zhang B, Wang M, Wang X, Wanyan P. Spinal cord injury: a systematic review and network meta-analysis of therapeutic strategies based on 15 types of stem cells in animal models. Front Pharmacol. 2022;13:819861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cizkova D, Novotna I, Slovinska L, Vanicky I, Jergova S, Rosocha J, Radonak J. Repetitive intrathecal catheter delivery of bone marrow mesenchymal stromal cells improves functional recovery in a rat model of contusive spinal cord injury. J Neurotrauma. 2011;28(9):1951–61. [DOI] [PubMed] [Google Scholar]
- 185.Krupa P, Vackova I, Ruzicka J, Zaviskova K, Dubisova J, Koci Z, Turnovcova K, Urdzikova LM, Kubinova S, Rehak S et al. The Effect of Human Mesenchymal Stem Cells Derived from Wharton's Jelly in Spinal Cord Injury Treatment Is Dose-Dependent and Can Be Facilitated by Repeated Application. Int J Mol Sci. 2018; 19(5). [DOI] [PMC free article] [PubMed]
- 186.Okada S, Ishii K, Yamane J, Iwanami A, Ikegami T, Katoh H, Iwamoto Y, Nakamura M, Miyoshi H, Okano HJ, et al. In vivo imaging of engrafted neural stem cells: its application in evaluating the optimal timing of transplantation for spinal cord injury. FASEB J. 2005;19(13):1839–41. [DOI] [PubMed] [Google Scholar]
- 187.Parr AM, Kulbatski I, Tator CH. Transplantation of adult rat spinal cord stem/progenitor cells for spinal cord injury. J Neurotrauma. 2007;24(5):835–45. [DOI] [PubMed] [Google Scholar]
- 188.Zhao Y, Tang F, Xiao Z, Han G, Wang N, Yin N, Chen B, Jiang X, Yun C, Han W, et al. Clinical study of neuroregen scaffold combined with human mesenchymal stem cells for the repair of chronic complete spinal cord injury. Cell Transplant. 2017;26(5):891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kumamaru H, Ohkawa Y, Saiwai H, Yamada H, Kubota K, Kobayakawa K, Akashi K, Okano H, Iwamoto Y, Okada S. Direct isolation and RNA-seq reveal environment-dependent properties of engrafted neural stem/progenitor cells. Nat Commun. 2012;3:1140. [DOI] [PubMed] [Google Scholar]
- 190.Zhang C, Morozova AY, Abakumov MA, Mel’nikov PA, Gabashvili AN, Chekhonin VP. Evaluation of the optimal number of implanted mesenchymal stem cells for the treatment of post-traumatic syrinx and recovery of motor activity after chronic spinal cord injury. Bull Exp Biol Med. 2023;175(4):557–68. [DOI] [PubMed] [Google Scholar]
- 191.Jung DI, Ha J, Kang BT, Kim JW, Quan FS, Lee JH, Woo EJ, Park HM. A comparison of autologous and allogenic bone marrow-derived mesenchymal stem cell transplantation in canine spinal cord injury. J Neurol Sci. 2009;285(1–2):67–77. [DOI] [PubMed] [Google Scholar]
- 192.Zurita M, Vaquero J, Bonilla C, Santos M, De Haro J, Oya S, Aguayo C. Functional recovery of chronic paraplegic pigs after autologous transplantation of bone marrow stromal cells. Transplantation. 2008;86(6):845–53. [DOI] [PubMed] [Google Scholar]
- 193.Deng YB, Yuan QT, Liu XG, Liu XL, Liu Y, Liu ZG, Zhang C. Functional recovery after rhesus monkey spinal cord injury by transplantation of bone marrow mesenchymal-stem cell-derived neurons. Chin Med J (Engl). 2005;118(18):1533–41. [PubMed] [Google Scholar]
- 194.Lamanna JJ, Miller JH, Riley JP, Hurtig CV, Boulis NM. Cellular therapeutics delivery to the spinal cord: technical considerations for clinical application. Ther Deliv. 2013;4(11):1397–410. [DOI] [PubMed] [Google Scholar]
- 195.Liu G, Zhao Z, Wang H, Hao C, Wang W, Zhang C, Wang T, Li X, Xi J, Li S, et al. Therapeutic efficacy of human mesenchymal stem cells with different delivery route and dosages in rat models of spinal cord injury. Cell Transplant. 2022;31:9636897221139734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Nitzsche F, Müller C, Lukomska B, Jolkkonen J, Deten A, Boltze J. Concise review: MSC adhesion Cascade-insights into homing and transendothelial migration. Stem Cells. 2017;35(6):1446–60. [DOI] [PubMed] [Google Scholar]
- 197.Zhao A, Chung M, Yang Y, Pan X, Pan Y, Cai S. The SDF-1/CXCR4 signaling pathway directs the migration of systemically transplanted bone marrow mesenchymal stem cells towards the lesion site in a rat model of spinal cord injury. Curr Stem Cell Res Ther. 2023;18(2):216–30. [DOI] [PubMed] [Google Scholar]
- 198.Cui LL, Nitzsche F, Pryazhnikov E, Tibeykina M, Tolppanen L, Rytkönen J, Huhtala T, Mu JW, Khiroug L, Boltze J, et al. Integrin α4 overexpression on rat mesenchymal stem cells enhances transmigration and reduces cerebral embolism after intracarotid injection. Stroke. 2017;48(10):2895–900. [DOI] [PubMed] [Google Scholar]
- 199.Kim GU, Sung SE, Kang KK, Choi JH, Lee S, Sung M, Yang SY, Kim SK, Kim YI, Lim JH et al. Therapeutic Potential of Mesenchymal Stem Cells (MSCs) and MSC-Derived Extracellular Vesicles for the Treatment of Spinal Cord Injury. Int J Mol Sci. 2021; 22(24). [DOI] [PMC free article] [PubMed]
- 200.Charbord P. Bone marrow mesenchymal stem cells: historical overview and concepts. Hum Gene Ther. 2010;21(9):1045–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hofstetter CP, Schwarz EJ, Hess D, Widenfalk J, El Manira A, Prockop DJ, Olson L. Marrow stromal cells form guiding strands in the injured spinal cord and promote recovery. Proc Natl Acad Sci USA. 2002;99(4):2199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cízková D, Rosocha J, Vanický I, Jergová S, Cízek M. Transplants of human mesenchymal stem cells improve functional recovery after spinal cord injury in the rat. Cell Mol Neurobiol. 2006;26(7–8):1167–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Han D, Wu C, Xiong Q, Zhou L, Tian Y. Anti-inflammatory mechanism of bone marrow mesenchymal stem cell transplantation in rat model of spinal cord injury. Cell Biochem Biophys. 2015;71(3):1341–7. [DOI] [PubMed] [Google Scholar]
- 204.Matsushita T, Lankford KL, Arroyo EJ, Sasaki M, Neyazi M, Radtke C, Kocsis JD. Diffuse and persistent blood-spinal cord barrier disruption after contusive spinal cord injury rapidly recovers following intravenous infusion of bone marrow mesenchymal stem cells. Exp Neurol. 2015;267:152–64. [DOI] [PubMed] [Google Scholar]
- 205.Weiss ML, Anderson C, Medicetty S, Seshareddy KB, Weiss RJ, VanderWerff I, Troyer D, McIntosh KR. Immune properties of human umbilical cord Wharton’s jelly-derived cells. Stem Cells. 2008;26(11):2865–74. [DOI] [PubMed] [Google Scholar]
- 206.Dasari VR, Veeravalli KK, Tsung AJ, Gondi CS, Gujrati M, Dinh DH, Rao JS. Neuronal apoptosis is inhibited by cord blood stem cells after spinal cord injury. J Neurotrauma. 2009;26(11):2057–69. [DOI] [PubMed] [Google Scholar]
- 207.De Ugarte DA, Morizono K, Elbarbary A, Alfonso Z, Zuk PA, Zhu M, Dragoo JL, Ashjian P, Thomas B, Benhaim P, et al. Comparison of multi-lineage cells from human adipose tissue and bone marrow. Cells Tissues Organs. 2003;174(3):101–9. [DOI] [PubMed] [Google Scholar]
- 208.Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, Benhaim P, Lorenz HP, Hedrick MH. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7(2):211–28. [DOI] [PubMed] [Google Scholar]
- 209.Hsiao ST, Asgari A, Lokmic Z, Sinclair R, Dusting GJ, Lim SY, Dilley RJ. Comparative analysis of paracrine factor expression in human adult mesenchymal stem cells derived from bone marrow, adipose, and dermal tissue. Stem Cells Dev. 2012;21(12):2189–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Luzzi S, Crovace AM, Lacitignola L, Valentini V, Francioso E, Rossi G, Invernici G, Galzio RJ, Crovace A. Engraftment, neuroglial transdifferentiation and behavioral recovery after complete spinal cord transection in rats. Surg Neurol Int. 2018;9:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Suvarna A, Hoque M, Saxena AC, Kumar V, Singh R, Bag S. The effect of different routes of xenogeneic mesenchymal stem cell transplantation on the regenerative potential of spinal cord injury. Regener Eng Transl Med. 2023;9(3):407–15. [Google Scholar]
- 212.Kim JW, Ha KY, Molon JN, Kim YH. Bone marrow-derived mesenchymal stem cell transplantation for chronic spinal cord injury in rats: comparative study between intralesional and intravenous transplantation. Spine (Phila Pa 1976). 2013; 38(17):E1065–1074. [DOI] [PubMed]
- 213.Yousefifard M, Nasirinezhad F, Shardi Manaheji H, Janzadeh A, Hosseini M, Keshavarz M. Human bone marrow-derived and umbilical cord-derived mesenchymal stem cells for alleviating neuropathic pain in a spinal cord injury model. Stem Cell Res Ther. 2016;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Hu J, Chen L, Huang X, Wu K, Ding S, Wang W, Wang B, Smith C, Ren C, Ni H, et al. Calpain inhibitor MDL28170 improves the transplantation-mediated therapeutic effect of bone marrow-derived mesenchymal stem cells following traumatic brain injury. Stem Cell Res Ther. 2019;10(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Luo Z, Wu F, Xue E, Huang L, Yan P, Pan X, Zhou Y. Hypoxia preconditioning promotes bone marrow mesenchymal stem cells survival by inducing HIF-1α in injured neuronal cells derived exosomes culture system. Cell Death Dis. 2019;10(2):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Pourjafar M, Saidijam M, Mansouri K, Ghasemibasir H, Karimi Dermani F, Najafi R. All-trans retinoic acid preconditioning enhances proliferation, angiogenesis and migration of mesenchymal stem cell in vitro and enhances wound repair in vivo. Cell Prolif. 2017; 50(1). [DOI] [PMC free article] [PubMed]
- 217.Wang C, Shi D, Song X, Chen Y, Wang L, Zhang X. Calpain inhibitor attenuates ER stress-induced apoptosis in injured spinal cord after bone mesenchymal stem cells transplantation. Neurochem Int. 2016;97:15–25. [DOI] [PubMed] [Google Scholar]
- 218.Zhang X, Jiang W, Lu Y, Mao T, Gu Y, Ju D, Dong C. Exosomes combined with biomaterials in the treatment of spinal cord injury. Front Bioeng Biotechnol. 2023;11:1077825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Liu WZ, Ma ZJ, Li JR, Kang XW. Mesenchymal stem cell-derived exosomes: therapeutic opportunities and challenges for spinal cord injury. Stem Cell Res Ther. 2021;12(1):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kang J, Li Z, Zhi Z, Wang S, Xu G. MiR-21 derived from the exosomes of MSCs regulates the death and differentiation of neurons in patients with spinal cord injury. Gene Ther. 2019;26(12):491–503. [DOI] [PubMed] [Google Scholar]
- 221.Li D, Zhang P, Yao X, Li H, Shen H, Li X, Wu J, Lu X. Exosomes derived from miR-133b-modified mesenchymal stem cells promote recovery after spinal cord injury. Front Neurosci. 2018;12:845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Hu C, Li L. Preconditioning influences mesenchymal stem cell properties in vitro and in vivo. J Cell Mol Med. 2018;22(3):1428–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kheirandish M, Gavgani SP, Samiee S. The effect of hypoxia preconditioning on the neural and stemness genes expression profiling in human umbilical cord blood mesenchymal stem cells. Transfus Apher Sci. 2017;56(3):392–9. [DOI] [PubMed] [Google Scholar]
- 224.Kim YS, Noh MY, Cho KA, Kim H, Kwon MS, Kim KS, Kim J, Koh SH, Kim SH. Hypoxia/reoxygenation-preconditioned human bone marrow-derived mesenchymal stromal cells rescue ischemic rat cortical neurons by enhancing trophic factor release. Mol Neurobiol. 2015;52(1):792–803. [DOI] [PubMed] [Google Scholar]
- 225.Liu X, Duan B, Cheng Z, Jia X, Mao L, Fu H, Che Y, Ou L, Liu L, Kong D. SDF-1/CXCR4 axis modulates bone marrow mesenchymal stem cell apoptosis, migration and cytokine secretion. Protein Cell. 2011;2(10):845–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Urnukhsaikhan E, Cho H, Mishig-Ochir T, Seo YK, Park JK. Pulsed electromagnetic fields promote survival and neuronal differentiation of human BM-MSCs. Life Sci. 2016;151:130–8. [DOI] [PubMed] [Google Scholar]
- 227.Shang AJ, Hong SQ, Xu Q, Wang HY, Yang Y, Wang ZF, Xu BN, Jiang XD, Xu RX. NT-3-secreting human umbilical cord mesenchymal stromal cell transplantation for the treatment of acute spinal cord injury in rats. Brain Res. 2011;1391:102–13. [DOI] [PubMed] [Google Scholar]
- 228.Cui X, Chen L, Ren Y, Ji Y, Liu W, Liu J, Yan Q, Cheng L, Sun YE. Genetic modification of mesenchymal stem cells in spinal cord injury repair strategies. Biosci Trends. 2013;7(5):202–8. [PubMed] [Google Scholar]
- 229.Blando S, Anchesi I, Mazzon E, Gugliandolo A. Can a Scaffold Enriched with Mesenchymal Stem Cells Be a Good Treatment for Spinal Cord Injury? Int J Mol Sci. 2022; 23(14). [DOI] [PMC free article] [PubMed]
- 230.Li M, Mei X, Lv S, Zhang Z, Xu J, Sun D, Xu J, He X, Chi G, Li Y. Rat vibrissa dermal papilla cells promote healing of spinal cord injury following transplantation. Exp Ther Med. 2018;15(4):3929–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Al Mamun A, Monalisa I, Tul Kubra K, Akter A, Akter J, Sarker T, Munir F, Wu Y, Jia C, Afrin Taniya M, et al. Advances in immunotherapy for the treatment of spinal cord injury. Immunobiology. 2021;226(1):152033. [DOI] [PubMed] [Google Scholar]
- 232.Donovan J, Kirshblum S. Clinical trials in traumatic spinal cord injury. Neurotherapeutics. 2018;15(3):654–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Cheung V, Hoshide R, Bansal V, Kasper E, Chen CC. Methylprednisolone in the management of spinal cord injuries: lessons from randomized, controlled trials. Surg Neurol Int. 2015;6:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Chio JCT, Wang J, Badner A, Hong J, Surendran V, Fehlings MG. The effects of human immunoglobulin G on enhancing tissue protection and neurobehavioral recovery after traumatic cervical spinal cord injury are mediated through the neurovascular unit. J Neuroinflammation. 2019;16(1):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Chio JCT, Wang J, Surendran V, Li L, Zavvarian MM, Pieczonka K, Fehlings MG. Delayed administration of high dose human immunoglobulin G enhances recovery after traumatic cervical spinal cord injury by modulation of neuroinflammation and protection of the blood spinal cord barrier. Neurobiol Dis. 2021;148:105187. [DOI] [PubMed] [Google Scholar]
- 236.Hodgetts SI, Simmons PJ, Plant GW. A comparison of the behavioral and anatomical outcomes in sub-acute and chronic spinal cord injury models following treatment with human mesenchymal precursor cell transplantation and recombinant decorin. Exp Neurol. 2013;248:343–59. [DOI] [PubMed] [Google Scholar]
- 237.Yang Y, Cao TT, Tian ZM, Gao H, Wen HQ, Pang M, He WJ, Wang NX, Chen YY, Wang Y, et al. Subarachnoid transplantation of human umbilical cord mesenchymal stem cell in rodent model with subacute incomplete spinal cord injury: preclinical safety and efficacy study. Exp Cell Res. 2020;395(2):112184. [DOI] [PubMed] [Google Scholar]
- 238.Liu Y, He ZJ, Xu B, Wu QZ, Liu G, Zhu H, Zhong Q, Deng DY, Ai H, Yue Q, et al. Evaluation of cell tracking effects for transplanted mesenchymal stem cells with jetPEI/Gd-DTPA complexes in animal models of hemorrhagic spinal cord injury. Brain Res. 2011;1391:24–35. [DOI] [PubMed] [Google Scholar]
- 239.Sykova E, Cizkova D, Kubinova S. Mesenchymal stem cells in treatment of spinal cord injury and amyotrophic lateral sclerosis. Front Cell Dev Biol. 2021;9:695900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Syková E, Jendelová P. Magnetic resonance tracking of implanted adult and embryonic stem cells in injured brain and spinal cord. Ann N Y Acad Sci. 2005;1049:146–60. [DOI] [PubMed] [Google Scholar]
- 241.Donnelly EM, Kubelick KP, Dumani DS, Emelianov SY. Photoacoustic image-guided delivery of plasmonic-nanoparticle-labeled mesenchymal stem cells to the spinal cord. Nano Lett. 2018;18(10):6625–32. [DOI] [PubMed] [Google Scholar]
- 242.Kubelick KP, Emelianov SY. Prussian blue nanocubes as a multimodal contrast agent for image-guided stem cell therapy of the spinal cord. Photoacoustics. 2020;18:100166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Taha A, Bobi J, Dammers R, Dijkhuizen RM, Dreyer AY, van Es A, Ferrara F, Gounis MJ, Nitzsche B, Platt S, et al. Comparison of large animal models for acute ischemic stroke: which model to use? Stroke. 2022;53(4):1411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.