Abstract
Background
In the United States, Black and Latino children with asthma are more likely than White children with asthma to require emergency department visits or hospitalizations because of an asthma exacerbation. Although many cite patient-level socioeconomic status and access to health care as primary drivers of disparities, there is an emerging focus on a major root cause of disparities—systemic racism. Current conceptual models of asthma disparities depict the historical and current effects of systemic racism as the foundation for unequal exposures to social determinants of health, environmental exposures, epigenetic factors, and differential healthcare access and quality. These ultimately lead to biologic changes over the life course resulting in asthma morbidity and mortality.
Methods
At the 2022 American Thoracic Society International Conference, a diverse panel of experts was assembled to identify gaps and opportunities to address systemic racism in childhood asthma research. Panelists found that to examine and address the impacts of systemic racism on children with asthma, researchers and medical systems that support biomedical research will need to 1) address the current gaps in our understanding of how to conceptualize and characterize the impacts of systemic racism on child health, 2) design research studies that leverage diverse disciplines and engage the communities affected by systemic racism in identifying and designing studies to evaluate interventions that address the racialized system that contributes to disparities in asthma health outcomes, and 3) address funding mechanisms and institutional research practices that will be needed to promote antiracism practices in research and its dissemination.
Results
A thorough literature review and expert opinion discussion demonstrated that there are few studies in childhood asthma that identify systemic racism as a root cause of many of the disparities seen in children with asthma. Community engagement and participation in research studies is essential to design interventions to address the racialized system in which patients and families live. Dissemination and implementation studies with an equity lens will provide the multilevel evaluations required to understand the impacts of interventions to address systemic racism and the downstream impacts. To address the impacts of systemic racism and childhood asthma, there needs to be increased training for research teams, funding for studies addressing research that evaluates the impacts of racism, funding for diverse and multidisciplinary research teams including community members, and institutional and financial support of advocating for policy changes based on study findings.
Conclusions
Innovative study design, new tools to identify the impacts of systemic racism, community engagement, and improved infrastructure and funding are all needed to support research that will address impacts of systemic racism on childhood asthma outcomes.
Keywords: asthma, racism, health disparities, minority and disadvantaged populations, social determinants of health
Contents
Introduction
- Methods
- Formation of the Steering Committee
- American Thoracic Society Systemic Racism in Pediatric Asthma Workshop
- ATS Workshop Report Preparation
- Results
- Conceptualizing Systemic Racism and the Impacts on Pediatric Asthma
- Considerations for Ethical Study Design in Research to Address Systemic Racism and Pediatric Asthma
- Using Dissemination and Implementation Science to Apply an Antiracism Lens to Addressing Pediatric Asthma Disparities
- Funding and Institutional Priorities for Research to Address the Impacts of Systemic Racism on Pediatric Asthma
Conclusions
Introduction
Disparities in pediatric asthma prevalence and outcomes across racial and ethnic groups in the United States persist without a precise determination of their cause. Underlying biology cannot explain these differences, because racial categories used in the U.S. census and in research are social definitions of race that lack a biologic, genetic, or anthropologic basis (1, 2). The social concept of race based on perceived differences in individuals’ skin color led to the creation of a racialized system that perpetuates inequities in social caste, socioeconomic position, environmental exposures, access to quality health care, and other contextual factors that contribute to health inequities; thus, racism is a root cause of many health disparities, including those in asthma. One example of the racialized system in the United States is redlining, a discriminatory practice created by the federal government’s Home Owner’s Loan Corporation in the late 1930s to color code maps and identify “high-risk” areas for mortgages and home loans, overwhelming and systematically identified minoritized people and neighborhoods as “high risk” or grade “D,” thus discouraging any loans. This practice continued until the Fair Housing Act was passed in 1968 (3). Studies now show that many historically redlined neighborhoods have low homeownership, poor housing, poor air quality, increased violence, decreased access to health care, poor neighborhood opportunity, and poor respiratory and other pediatric health outcomes, including asthma (4–8). The current residents of those redlined areas are more likely to be from minoritized backgrounds and to have lower incomes. Although this is not true of every urban area, because populations shift, the long-term impacts are clear. As a result of policies such as redlining in societies influenced by a racial caste system, race often approximates social position and contributes to differential access to social determinants of health, including clean environments, quality education, housing, employment, and health care. These tenets of social and environmental justice substantially affect pediatric asthma outcomes (4, 9–14).
Behavioral and social sciences have explored racism and health for decades. In the last decade, there has been a concentration of studies demonstrating clear associations between racism—both interpersonal and structural—and asthma (15–18). Furthermore, interventions specifically designed to counter the effects of racism show benefits, providing additional evidence for systemic racism as a root cause of pediatric asthma (19). Studies indicate that interpersonal racism leads to biologic changes in inflammatory response, telomere length, and poor mental health (20, 21). Coogan and colleagues showed that everyday and lifetime racism were associated with an increased incidence of adult-onset asthma in Black women and that the association was stronger in Black women who reported persistent racism over a 10-year study period (22). Thakur and colleagues demonstrated that interpersonal discrimination contributes to worse asthma outcomes in children (23–25). Other studies have shown the impacts of racial inequities in the care of children with asthma and the impact on specialist care, medications, and asthma control. Nevertheless , very few studies that examine the effect of racialized policies and the impact on child health outcomes identify systemic racism as the root cause; therefore, the direct impacts of systemic racism on health outcomes for Black, Latino, and other historically marginalized populations have not been well delineated.
There are several barriers to understanding the role of systemic racism in pediatric asthma outcomes. 1) There is a lack of consensus on how to quantify systemic racism. 2) There is not a clear methodology for developing and assessing interventions targeting systemic racism. 3) Research teams lack diversity in composition and do not have expertise in the lived experience of children and families experiencing interpersonal or systemic racism. 4) Current research funding together with entrenched institutional research frameworks do not support products that will change the status quo. 5) To understand, identify, and quantify targets to reduce downstream health effects of systemic racism, one needs to include data from several sources and interpret data with multidisciplinary teams. Data from multiple sectors (e.g., education, housing, employment) and community levels (e.g., census tract, block group, state) (26, 27) are required to evaluate unintended impacts. 6) Without the consultation or inclusion of affected populations in interpreting the results, contextualizing multilevel data may lead to inappropriate conclusions (28). Community-based participatory researchers have long advocated for the inclusion of diverse research partners and increased participation of minoritized patient populations. However, a recent systematic review of all published clinical trials reporting patient engagement in research from 2011 to 2016 found heterogeneity in the type and extent of patient engagement. Moreover, in the context of all concurrent clinical trials, less than 1% reported any type of community engagement (29, 30). 7) Current funding models perpetuate this problem by limiting funding for multisector interventions targeting systemic racism and by not enforcing or supporting their own requirements for rigorous community engagement for all health equity research.
This workshop report outlines priorities for research addressing the direct impacts of systemic racism on pediatric patients with asthma, by discussing 1) a conceptualization of systemic racism in pediatric asthma; 2) ethical considerations in designing studies to address disparities in pediatric asthma outcomes; 3) how to design and implement studies to identify inequities due to systemic racism and how to evaluate interventions targeting systemic racism in pediatric patients with asthma; and 4) how funders and institutions can promote racial equity in pediatric asthma research and advocacy to improve health outcomes.
Methods
Formation of the Steering Committee
In 2022, the cochairs convened a diverse group of researchers, clinical scholars, social scientists, and community health workers with expertise in pediatric asthma, asthma research, health disparities, environmental health, epidemiology, population health, social sciences, psychology, and systemic racism to participate in a series of virtual workshop discussions. The goals of the workshop were to 1) evaluate the current evidence for the impacts of systemic racism on children with asthma, 2) identify gaps in understanding of the impacts of racism and a racialized system, and 3) create a framework for researchers to address those gaps in the future.
American Thoracic Society Systemic Racism in Pediatric Asthma Workshop
Meetings were conducted virtually. Prerecorded sessions that addressed fundamental concepts related to the content of the workshop were made available to all participants before the workshop sessions to ensure that all participants were familiar with concepts that may have been outside of their respective disciplines. The initial large committee meeting with all workshop participants was 2 hours long. Follow-up cochair meetings led to the creation of four workgroups, assignment of workgroup leaders, and a draft of a manuscript outline. Each workgroup met at least once virtually, and workgroup leaders met virtually after those meetings to review the content discussed in the meeting and to create a writing plan. The large committee meeting and small workgroup meetings were recorded, and the transcripts were reviewed in preparation for writing the manuscript. A detailed description of workshop participants (see Table E1 in the data supplement) and workshop activities, including background reading, presentations, and description of session activities (Table E2), is provided in the appendix. Potential conflicts of interest were disclosed and managed in accordance with the policies and procedures of the American Thoracic Society (ATS).
ATS Workshop Report Preparation
A comprehensive review of the literature included PubMed and Google Scholar searches for the following in both the healthcare and social sciences literature: race, racism, ethnicity, disparity, inequity, environmental justice, community-based research, dissemination and implementation (D&I), and asthma. The literature search helped delineate the barriers noted in the introduction and defined the overall workshop goal to create a guide for the design and implementation of studies to investigate systemic racism and pediatric asthma. Please see an abbreviated example of one search in the appendix (Table E3) for studies evaluated for the research design section. Further discussion with subject matter experts, including the cochairs and others, delineated the importance of the other three workshop goals: 1) defining and conceptualizing systemic racism; 2) addressing the complicated ethical issues that are part of working with minoritized and marginalized populations, including building trust, understanding their lived experience, and respecting their goals for health and research; and 3) identifying barriers within institutions and funders to conduct these studies. After the first large committee meeting, the initial outline of the workshop report was authored by the cochairs and workgroup leaders. After each of the four smaller workgroup meetings, workgroup leaders and cochairs worked together to prepare an initial draft of the manuscript. All workshop participants reviewed and edited the complete workshop report, and it was finalized by the cochairs. The final workshop report underwent several cycles of external peer review and revisions, followed by review and approval by the ATS Board of Directors.
Results
Conceptualizing Systemic Racism and the Impacts on Pediatric Asthma
A critical first step in understanding the role of racism in pediatric asthma is to define terms. “Race” is a social construct, the social interpretation of how one looks in a given place and time (31). That is, one’s racial and ethnic classification is dynamic and informed by geography, culture, social and political climate, and time in history. The conflation of race and ethnicity, genetic ancestry, and biologic differences is a common misconception. Although there have always been labels to distinguish inhabitants of different countries, tribes, and ethnicities, the current racialized system of identification was developed to facilitate and justify oppression, slavery, and conquest (32–34).
Camara Phyllis Jones defines “racism” as the “system of structuring opportunity and assigning value based on the social interpretation of how one looks (which is what we call ‘race’), that unfairly disadvantages some individuals and communities, unfairly advantages other individuals and communities, and saps the strength of the whole society through the waste of human resources” (31, 35). Braveman and colleagues stated, “Racism is the relegation of people of color to inferior status and treatment based on unfounded beliefs about innate inferiority, as well as unjust treatment and oppression of people of color, whether intended or not. Racism is not always conscious, intentional, or explicit—often it is systemic and structural” (36, 37). There are several types of racism. “Interpersonal racism” refers to race-based bias or prejudice between individuals. “Institutional racism” refers to differential access to goods, services, and opportunities by race within a singular institution, such as differential access to quality education in a public school system. Institutional racism is often written into laws or bylaws (e.g., redlining) but could also be behavioral norms (e.g., people with “Black”-sounding names receiving fewer interviews for the same résumé). Systemic and structural racism connects multiple institutions to reinforce racial hierarchy. Structural racism “emphasizes the role of structures (e.g., laws, policies, institutional practices, and entrenched norms)” that are the backbone of our sociopolitical systems and is a subset of systemic racism (36). The term “systemic racism” represents the whole system, including the structures that uphold the systems. It is generally understood to refer to “forms of racism that are pervasively and deeply embedded in and throughout systems, laws, written or unwritten policies, entrenched practices, and established beliefs and attitudes that produce, condone, and perpetuate widespread unfair treatment of people of color” (38). Systemic racism reinforces discriminatory beliefs, values, and distribution of resources and perpetuates historical injustices (36). For example, slavery and Jim Crow laws were designed to disenfranchise Black adults and restrict their right to work and get a quality education (39). Unfortunately, although civil rights legislation made it illegal to discriminate against Black adults in education and employment institutions, systems unintentionally perpetuate historical injustices and fail to correct inequities (36). For example, voter suppression and gerrymandering are still used to disenfranchise Black adults (36, 40, 41), and banks continue to grant minoritized persons fewer home mortgages and often offer them mortgages with higher rates and fees (3, 42, 43).
The concept that many systems have a racialized foundation is critical to our understanding of differences in pediatric asthma outcomes, because it focuses on the complex historical and current interactions between social systems (e.g., political, legal, educational, economic, health care, media) and their impacts on resources and other social determinants of health shown to have long-term effects on health and health outcomes. Martinez and colleagues provide one conceptual model to explain the pathways by which systemic racism leads to the development and worsening of asthma through modifying biologic processes that lead to altered airway microenvironments and T-helper type 1–type 2 imbalance that contributes to the pathogenesis of atopic diseases (33). The authors show how determinants of health (e.g., culture, societal institutions, health behaviors, biology, ancestry) influence how structural racism is perpetrated and ultimately affects biologic embedding and leads to racial disparities in allergy and immunologic conditions. The authors further break down structural racism into upstream factors (e.g., current and historical racist policies such as redlining) and proximal factors (e.g., physical and social environment) to show how racism affects several important domains known to contribute to asthma disparities.
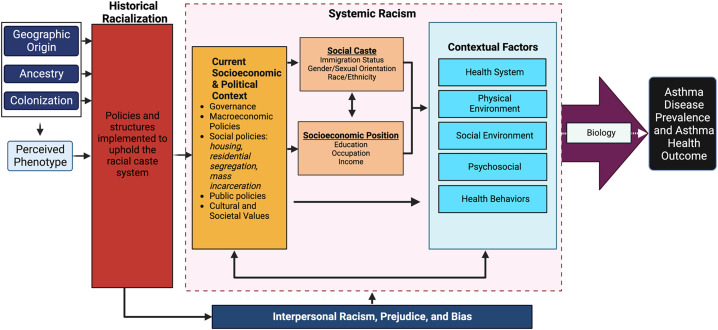
Building from the conceptual model published by Martinez and colleagues (33), and drawing from other conceptual models showing how racism affects health (44), we propose a revised conceptual model (Figure 1) that 1) incorporates the historical process of racialization by which human biological variation, ancestry, and geographic origin were reduced to perceived phenotypic differences and then mapped to discrete, socially defined “races”; 2) includes colonization as a driving force of historic racialization; and 3) emphasizes the compounding influence of historical racialized policies (e.g., redlining) on current manifestations of systemic racism (e.g., physiologic response to environment) that contribute to asthma outcomes.
Figure 1.
Conceptual model of the impacts of historical racialization and systemic racism on asthma disease prevalence and outcomes. Conceptual model describing how perceived phenotypes led to historical racialization, which led to a system that perpetuates social caste and socioeconomic status positions that exist within a social and political context. The model demonstrates the impacts of systemic racism and interpersonal racism on biology and disease manifestation.
Considerations for Ethical Study Design in Research to Address Systemic Racism in Pediatric Asthma
The workshop identified several core ethical considerations in the design of research to address systemic racism and pediatric asthma, including 1) steps to engage communities disproportionately burdened by asthma morbidity in the design of research; 2) how to create diverse research teams, adequately compensating participants for their time; 3) ensuring appropriate representation through flexible recruitment and retention practices; 4) careful collection and analysis of personal data; and 5) thoughtful evaluation in selecting reference populations (see Table 1 for workshop recommendations on ethical conduct of research to address systemic racism and pediatric asthma).
Table 1.
Recommendations and considerations for conducting ethical research to address systemic racism and pediatric asthma
| Considerations | Descriptions |
|---|---|
| Evaluate use of race as a variable (119) |
|
| Use a restorative justice approach to systemic inequities |
|
| Establish multidisciplinary teams and diverse research teams |
|
| Collect accurate and inclusive data |
|
| Decenter Whiteness in the evaluation |
|
Engaging communities in design of asthma research
Community engagement ensures that research is relevant to the population being studied, aligns the goals of the researchers and the community, addresses community priorities, and results in interventions that are likely to be sustained beyond the project period (30). When research team members who are working with communities and recruiting participants reflect the populations involved, community engagement and recruitment will be more successful (45). Effective engagement encompasses involving, codesigning, cocreating, and cultivating relationships with key partners, particularly those historically underrepresented in research, who are invested in the field of study. Engaging all parties with an interest in the outcome of the research as members of the research team requires building trust, establishing alignment, and recognizing and respecting the knowledge that each party brings. If done well, these partnerships allow “bidirectional learning, mutual benefit and trust, and equitable distribution of power and resources” (46). Building partnerships and mutual trust also limits the risk that racist approaches leading to mistreatment and mistrust are embedded in the research (47). In pediatric asthma research, the lived experience of families and children with asthma and the community partners that support them are required for the iterative process of hypothesis testing and evaluating data in the context of personal experiences needed to identify meaningful metrics of success and solutions to disparities in childhood asthma (48, 49).
Community engagement can be challenging. Research groups may find that power dynamics within groups (50) and the lingering effects of “historical trauma” stand in the way of meaningful collaboration (51, 52). Mistrust or distrust in medical research and ongoing experiences of racism in the health system are critically important barriers to successful recruitment and retention of exploited communities (45), especially in studies of racism. Although the community members may not have the same academic training, their contribution as experts in the lived experience of the population offers a unique and impactful contribution to the approach and interpretation of outcomes. Employing community members as equal members on asthma research teams, with titles that are commensurate with other members of the research team, is a particularly effective mechanism for building trust and forging connections between researchers and participants (45, 53, 54). Thus, community members’ expertise is valued equally to that of principal investigators, and resources can be fairly and adequately shared. Finally, community members should be compensated at levels similar to those of traditional coinvestigators for their participation in research design, conduct, and dissemination and should be included in author bylines (51, 55).
Building diverse, multidisciplinary research teams
Much of the groundbreaking work for the examination of race and racism has been laid by social and behavioral scientists. Anderson showed that multilevel research collaborations that combine the expertise of several disciplines to address complex health concerns is a key component of addressing sociobehavioral effects of disease at the organ system, cellular, and molecular levels (56). Thus, to meaningfully address the impacts of systemic racism on pediatric asthma, we must engage colleagues from diverse disciplines with varied levels of expertise.
Study populations: recruitment and retention of diverse participants
To maximize scientific validity, it is important that researchers appropriately identify and collaborate with the populations most deeply and adversely impacted when designing studies to address systemic racism (57). Recruitment strategies that include outreach in the community (e.g., religious centers, community events) are more likely to be successful at identifying a wide range of individuals who may experience racism. Individuals from racially and ethnically marginalized populations may experience barriers to participating in research because of time and resource constraints (45). Thus, investigators who cannot provide flexible times, visit lengths, and locations for visits should be cognizant of potential sampling bias. For example, some parents may not be able to take time off from work or secure transportation, resulting in unintentionally disproportionate recruitment from unemployed or underemployed households. Study visits that take place at participants’ homes, local community centers, or schools may be more convenient and comfortable for the participants and their families and more representative of the community of interest (58–62). These steps to ensure diversity in the study population will optimize the scientific output of the research findings.
Data collection: allowing participants to self-identify and communities to define the problems
To address systemic racism in research, it is essential to have accurate data that reflect the impacts of policies and other aspects of systemic racism that led to inequities in health and health care. At the foundation is collecting accurate self-identified race, ethnicity, ethnic background, and language data for the populations being studied and served. It is also notable that although there is correlation between self-identified race and genetic ancestry, individuals frequently are unaware of their true origins (63). It is important to understand how these data, together with other demographic factors, are collected in the electronic health records before using them to identify inequities and disparities in health. For example, using the question, “How do OTHER people usually classify you in this country? Would you say White, Black or African American, Hispanic of Latino, Asian, American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, or some other group?” allows more direct measurement of the substrate on which racism operates day to day (31). In addition, it is important to recognize the importance of intersectionality, or the complex and cumulative ways that multiple different identities experienced by an individual (e.g., multiple races, ethnicities, gender identities) may amplify the impacts of racism. Once race and ethnicity data have been collected, investigators should thoughtfully consider the best approaches to including these variables in analysis. Several approaches exist, including the hierarchical model that combines all Hispanic participants, regardless of race, versus the additive model that sets multiple categories for Hispanic participants, depending on identified race (64).
Communities at the center of a research project or intervention should be consulted to understand additional data elements, including markers of success, desired short- and long-term outcomes, how the data/results should be disseminated, and what data are needed for sustained change, including policy goals. Quantitative studies are helpful in identifying where racism may be contributing to disparities. However, qualitative research is critical to understanding how racism is operating and being experienced by community members (65, 66). Indeed, Jones has introduced the question, “How is racism operating here?” as a tool for identifying the mechanisms of systemic racism in our structures, policies, practices, norms, and values. These mechanisms are actually the elements of decision making: Structures are the “who,” “what,” “when,” and “where” of decision making; policies are the written “how” of decision making; practices and norms are the unwritten “how” of decision making; and values are the “why.” By engaging with communities in asking “How is racism operating here?” with regard to differential pediatric asthma morbidity in various settings, we can identify promising levers for intervention and early targets for action (67).
Thoughtful evaluation in selecting reference populations: decentering Whiteness in research
White normativity, the notion that Whiteness is the standard racial identity, pervades medical research, where participants identified as White have historically been designated as the reference group with which other racial and ethnic groups are compared (68, 69). The use of White race as the norm reinforces and perpetuates the notion that Whiteness is the standard for optimal health. Pediatric asthma disparities research traditionally identifies differences in access, treatment, and outcomes among children from minoritized groups and compares these data with data for children in a White reference group for the purpose of quantifying and closing gaps in disparities to achieve health equity. Centering on White race as the standard for optimal health focuses attention on racial deficits rather than focusing on root causes, such as racism and its effects on health as the source of disparate asthma outcomes (70). In addition, when trying to understand how an exposure or risk factor operates in a single community, including other groups can be a distractor and may not allow appropriate understanding of how the exposure influences that specific population. A recent systematic review of pediatric clinical practice guidelines concluded that race was frequently used in ways that could have a negative impact on healthcare inequities (71). Many scholars note that current reporting of health disparities places the burden and responsibility of the outcomes on marginalized, minoritized populations rather than focusing the analytic lens on institutional policies and practices that have propped up a system where disparities thrive (72).
To decenter Whiteness, researchers will need to pivot away from White de facto reference groups and adopt other comparators, such as the whole population, multiple reference groups, or nondominant race groups, depending on the outcome of interest. When the inclusion of a reference group is appropriate, there should be explicit justification for using a privileged versus historically marginalized population. These approaches will require adequate representation with diverse study populations based on relative advantage and disadvantage experienced between different groups in the community of interest (70). Also, reviewers of grants and manuscripts should be discouraged from reflexively asking for White “control” or comparator groups, and, if they do, they should be required to provide justification for doing so. In addition, race-neutral reference ranges should be adopted to ensure that measures are not artificially scaled to normalize disparities, as was recently recommended by the American Thoracic Society Statement on Race and Ethnicity in Pulmonary Function Test Interpretation (73).
Using Dissemination and Implementation Science to Apply an Antiracism Lens to Addressing Pediatric Asthma Disparities
D&I science evaluates how evidence-based practices and policies are effectively communicated and/or adapted to real-world settings, including clinical practice and residential communities. The workshop participants agreed that D&I science provides an ideal study design for interventions targeting systemic racism in childhood asthma (19, 74). Research to address the impacts of systemic racism in children with asthma should be grounded in frameworks that allow a multilevel evaluation of the impacts of racism on asthma outcomes as well as the barriers to the adoption, acceptance, sustainability, or implementation of evidence-based interventions (see Table 2). Moreover, interventions targeting racial disparities in childhood asthma should contain upstream implementation targets such as historical policies or embedded social norms that contribute to the social, physical, economic, or political environments influencing health (74). Shelton and colleagues describe five core elements of implementation science through which researchers should apply an antiracism lens: 1) community and partner engagement; 2) conceptual frameworks/models; 3) development, selection, and/or adaptation of evidence-based interventions; 4) evaluation approaches; and 5) implementation strategies (46). Another approach is a “natural experiment” design that can be a common and powerful way of studying the impact of a policy implementation (19). Here we describe several strategies that adopt an antiracism lens toward D&I research strategies in the study of pediatric asthma.
Table 2.
Recommendations for design and evaluation of research to address systemic racism and pediatric asthma
| Considerations | Descriptions |
|---|---|
| Engage community members and partners from other sectors |
|
| Study design/framework |
|
| Choose effective intervention methodology |
|
| Evaluation: data |
|
| Evaluation: methods |
|
Community-based participatory research and community engagement as a basis for social justice research
Including those who directly experience the unfair disadvantages created and perpetuated by racism as part of the research process results in research questions and study outcomes that are better tailored to impact those outcomes most important to the participants themselves (51, 55). Community-based participatory research and participatory action research approaches are well poised to help define and address research questions surrounding social justice (75–77). Appropriately sustained engagement of members of the community requires involvement at each stage of research, including formulation of the research questions, data collection, analysis, interpretation, and reporting of results broadly, including to the affected communities (78). The foundational work to build trust and the involvement in research needs to occur before pursuing traditional grant funding mechanisms, which calls for a new national funding model that includes funded planning phases for community work as discussed above (55). Community-engaged studies should be a colearning experience: The academic team learns from and about the community (community strengths, problem definitions, approaches to solving those problems), and the community team learns from and about academia (scientific methods, grant applications, publication) (79). Study teams should consider the time it may take for community members to complete any required training on the responsible conduct of research that they might not otherwise do except to be able to meaningfully participate on the research team. Community team members will need to be compensated for that time and might benefit from research team support in the completion of any required training. Research teams also need to pursue additional funding that supports patient and community engagement as a fundamental aspect of the research process; The Patient-Centered Outcomes Research Institute engagement award program is an example of a federal grant for community-engaged research (80).
A final tenet that has historically been difficult for many research teams is to ensure that findings are sensitively communicated back to the participating communities so that outcomes can be addressed. Ensuring that study results are shared with community members also illustrates the degree to which research studies are not only coproduced but also co-owned. However, mistrust in data sharing may be founded on concerns about confidentiality and sensitive information sharing. At the beginning and end of the study, community partners should participate in any discussion of data safety and how best to sensitively share results with participants and key partners.
Dissemination and implementation science and frameworks
D&I science evaluates the gap between research and real-world application or practice using tools including frameworks, theories, and models. There are several conceptual frameworks used to plan and execute D&I research studies. These conceptual frameworks and models highlight multilevel context with respect to disseminating and implementing research; however, none underscore the importance of the extraorganizational or social context, including racism, that shapes our institutions, communities, and provision of care (e.g., racism). We recommend a select group of frameworks that effectively allow researchers to use an antiracism lens (Table 3). In particular, the National Institute on Minority Health and Health Disparities framework presents a structure for researchers to use as they consider the impacts of multiple interacting layers of factors on different domains of minority health and health disparities at the levels of the patient, family/organization, community, and population. Implementation of these frameworks can be bolstered by using tools such as the action-oriented community diagnosis tool that is centered on understanding communities and context to implement meaningful solutions (81).
Table 3.
Research methods and dissemination and implementation frameworks with antiracism lens
| Considerations | Descriptions |
|---|---|
| Nationally available framework | National Institutes on Minority Health and Health Disparities (NIMHD) research framework (102). This framework provides an invaluable visual depiction of the numerous and complex levels and domains that influence the health of historically minoritized populations. We recommend that researchers use the NIMHD framework to thoroughly reflect on the necessary components that should be included in their intervention and evaluation approaches. |
| Research frameworks that embed critical race theory | Public Health Critical Race Framework (120, 121) and Healing ARC (122, 123). These frameworks are vital for research interventions at the institution level because they center on medical restitution and guide researchers to move beyond typical, indirect interventions such as bias training. The Healing ARC—acknowledgment, redress, and closure—is a pragmatic framework for addressing institutional racial inequities in health care delivery and treatment. |
| Research frameworks that consider context | Health Equity Implementation Framework and race(ism) Consolidated Framework for Implementation Research (CFIR) (124). This framework uses the Public Health Critical Race Praxis to adapt CFIR to delineate how health equity may be concomitantly assessed and addressed in planning the implementation of an evidence-based intervention. Exploration Preparation, Implementation, and Sustainment (EPIS) framework (125–127). This framework describes the phases of and factors that lead to implementation intervention. It can be expanded to examine the intersectional lens of racism and sexism. |
| Qualitative design | Qualitative research and study designs used by other disciplines (e.g., public health and sociology) provide foundational work, including qualitative and focus group work, that helps identify problems with the intervention that can be disseminated and implemented. |
Development, selection, and/or adaptation of evidence-based interventions
To reduce disparities in pediatric asthma morbidity, research questions and study objectives must focus on interventions that address aspects of systemic racism, such as institutional racism, structural racism, and discrimination (82). Study teams will need to consider how intervention studies can be designed not only to understand the impacts of a racialized system on asthma outcomes but also how best to maximize the impacts of the findings on policy. For example, a growing body of research demonstrates that institutional racist policies such as historical redlining contributed to differences in environmental exposures and asthma outcomes (4, 7, 8). These data have been used in California to drive air pollution legislation such as the creation of the California Air Resources Board (https://ww2.arb.ca.gov/capp).
Research questions that address systems and policy change have the potential for meaningful long-term impacts. One example is the Allies Against Asthma Program that was funded by the Robert Wood Johnson Foundation and included seven coalitions of community organizations in low-income communities of color across the United States (83, 84). This 5-year program was created to support communities in targeting effective asthma management and led to 45 policy changes and 44 system changes related to childhood asthma across their communities, including changes in institutional policies and statewide legislation. Examples of institutional policy and system changes included establishing community health worker programs, legislation to prevent diesel truck idling, and expansion of asthma education. Children who lived in communities that were part of the coalition reported improvement in asthma symptoms (83), thus demonstrating that upstream interventions designed to address policies and systems can have significant impacts on personal clinical outcomes. For studies that do not directly attempt to address the impacts of racism on the outcome, investigators need to consider how racism contributes to the observed findings.
Tools for evaluating the impacts of systemic racism in clinical research
The evaluation of studies that identify racism as a root cause for inequities in care and/or disparities in outcomes will vary on the basis of the study. Any assessment of systemic or structural racism and asthma will need to include the multiple layers of factors that may impact the outcomes. For example, analyzing current and historical data across sectors may further the researchers’ understanding of the interacting exposures that lead to the downstream impacts of systemic racism (85). Coupling publicly available current data (e.g., claims data) with deprivation indices allows researchers to understand the intersection of multiple factors with race and ethnicity. The Index of Concentrations at Extremes can be used to evaluate the extremes of deprivation and how income is disparately distributed across race in a neighborhood (86). The Child Opportunity Index integrates multiple neighborhood-level factors to evaluate opportunity within a neighborhood for children and can be coupled with race and ethnicity data to understand those opportunities for children unfairly disadvantaged by systemic and structural racism (87). The Structural Racism Effect Index is a promising new indicator designed to capture the totality of the downstream impacts of systemic racism across society and associated with life expectancy (88). Qualitative data can help the research team understand the context and barriers of the problem to be considered in data collection and analysis (e.g., using a mixed-methods model that includes the qualitative data gathered). Working with experts outside of health care, such as epidemiologists, social and behavioral scientists, public health researchers, and others, may also be important to design and complete the analysis of the data.
The growing body of research dedicated to measuring racism has provided tools that can be applied to pediatric asthma research. In a recent review, Groos and colleagues outlined over a dozen unique measures of structural racism that have been used in recent research related to residential neighborhood and housing, social institutions, socioeconomic status, and other domains (26). Most of the studies focused on Black versus White racial comparisons; however, measures of racism related to immigration and border enforcement have also been described (26). Validated tools such as the Everyday Discrimination Scale can be used to measure racial discrimination and have been used in pediatric research (25, 89, 90).
Unfortunately, although many pediatric asthma studies identify and address disparities in exposure to negative risk factors, few evaluate systemic racism as the root cause of those disparities or of the inequities in exposures and resources that lead to them. This important knowledge gap persists.
Funding and Institutional Priorities for Research to Address the Impacts of Systemic Racism on Pediatric Asthma
The agencies and foundations that fund asthma research and the institutions that provide physical and intellectual research infrastructure have a unique platform to promote antiracism change in research. Systemic racism is, by definition, a set of structural problems built into society. Resolving such fundamental inequities will require deliberate and coordinated efforts at the institutional and societal levels. Federal and other funding agencies have the power to insist that research priorities align with dismantling racism. Funders can frame specific research initiatives to better understand and, most important, address systemic racism and its effect on childhood asthma. In addition, they can forge and foster changes in the scientific community that address the pervasiveness of structural inequities and impacts on patient experiences (see Table 4 for workshop recommendations).
Table 4.
Recommendations for funding and institutional practices for research to address impacts of systemic racism on pediatric asthma
| Considerations | Descriptions |
|---|---|
| Investigative team |
|
| Study design |
|
| Responsible conduct of research |
|
| Review |
|
Fomenting specific research initiatives
The research funding process can be biased at many levels, and systemic racism and discrimination have contributed to disparities in who is awarded grants (91–94). Racially and ethnically minoritized investigators tend to be underfunded even when their score is above the pay line, regardless of the investigator’s degree. In a National Science Foundation study, racial disparities (racism) were found to be widespread; non-Hispanic White principal investigators were consistently funded at higher rates than most principal investigators of color across all disciplinary directorates (95). Similarly, Ginther and colleagues studied National Institutes of Health (NIH) funding from 2001 to 2006 and found that Black applicants were 1.7 times less likely than White applicants to be funded (96), a racial funding gap that was unchanged on subsequent evaluation of funding from 2011 to 2015 (97) and persisted even after accounting for other applicant and application factors (92).
Funders need to be intentional in dismantling racist practices and policies by incorporating specific mandates for funding proposals (98, 99). Implicit biases that are not intentionally dismantled can lead to studies that do not include the patients who are most impacted by the diseases studied and therefore in most need of improved treatments. For instance, monoclonal antibodies (“biologics”) for asthma have advanced treatment for severe asthma; yet, many studies do not even list race in their results. For grant applications, investigators should explicitly discuss how they will ensure that the population studied is representative of the population served; it should no longer suffice to state that “no racial/ethnic groups will be excluded.”
In response to the substantial health inequities for patients with asthma, federal agencies have developed several programs to improve racial and ethnic disparities in asthma outcomes and improve workforce diversity. The Coordinated Federal Action Plan to Reduce Racial and Ethnic Asthma Disparities (100) resulted in the 2012 President’s Task Force on Environmental Health Risks and Safety Risks to Children, which led to additional funding to assess community needs for children with asthma (RFA HL 15-028) and encourage clinical trials to reduce childhood asthma disparities (RFA HL 17-001). The NIH UNITE initiative was established to identify and address structural racism within the NIH-supported community and the greater scientific community. It aims to establish an equitable and civil culture within the biomedical research enterprise and reduce barriers to racial equity in the biomedical research workforce (101). The NIH has a site dedicated to diversity-related funding opportunity announcements (https://extramural-diversity.nih.gov/guidedata/data), and the National Institute on Minority Health and Health Disparities has several programs that directly or indirectly support asthma research in minority populations (102). ComPASS (Community Partnerships to Advance Science for Society), an NIH Common Fund initiative, specifically funds a consortium of “Community-led, Health Equity Structural Intervention (CHESI) projects that intervene on structural factors that create and perpetuate health inequities and Health Equity Research Hubs to provide localized technical assistance to the community-led health equity structural interventions” (103).
Additional efforts by the NIH continue to address some of the barriers to equitable research (104), but more is needed to address systemic racism. For example, the DECIPHeR (Disparities Elimination through Coordinated Interventions to Prevent and Control Heart and Lung Disease Risk) Alliance promotes late-stage implementation research, specifically calls out “the persistent, significant health inequities” that exist for patients from underrepresented racial and ethnic backgrounds, and requires participation of community organizations (105). This announcement could make a stronger impact on racism in research by calling for and empowering community investigators to collaborate with the academic researchers and have equal standing instead of simply calling for a community advisory board. A recent NIH funding opportunity, “Addressing the Impact of Structural Racism and Discrimination on Minority Health and Health Disparities” (106), specifically focuses on intervention research that addresses structural racism and discrimination to improve minority health or reduce health disparities. Unfortunately, this announcement calls for collaboration but does not specifically require that a community and/or patient participate as a leader in the project. Until individuals from minoritized populations are treated as an essential part of the research team and their efforts are appropriately supported with research funds, it will be difficult to address racist practices that lead to incomplete science and poor health outcomes.
In addition to including individuals from minoritized populations in the research team, funders should also modify their scientific review mechanisms by 1) requiring a framework for evaluating investigators’ treatment of and approach to systemic racism in asthma research proposals and 2) developing a review system that has adequate and diverse expertise to evaluate multidisciplinary (e.g., social and biomedical sciences) research proposals. Finally, dismantling the effects of systemic racism on asthma (and other multifactorial diseases) will require long-term investment and should be reflected in appropriate timelines and metrics. Historical racism over the past 400 years has impacted the health outcomes of Black, Brown, and Indigenous patients for many generations. Therefore, funders must be intentional in establishing metrics that can be tracked over time and not hold unrealistic expectations for solutions that can be studied or implemented in 4- or 5-year project periods. Federal funding and regulatory agencies such as the NIH and Food and Drug Administration should also consider ways to ensure that pharmaceutical and biotechnology companies have structured long-term initiatives to ensure equitable access to new medications and treatments and then hold those companies accountable. A systematic approach to evaluating the treatment of race, ethnicity, disparities, and contextual factors in proposals should be developed and used to inform funding decisions. This includes issues such as the role of racism in measurement (e.g., survey tools, physiologic and biologic measurements) and the interpretation of study results focused on genetics and ancestry.
Forging general awareness
Addressing racism in research is integral to all aspects of training. Beyond providing incentives for specific research on systemic racism in asthma, calls for federal funding at any level should include requirements for best practices to address racism in research. The NIH and Agency for Healthcare Research and Quality current recommended topics are shown in Box 1 (107). We suggest adding required modules on understanding the effects of systemic racism on health equity and on proven approaches to incorporating antiracism methodologies into all aspects of human research (whether or not a research project is specifically focused on racism or health inequities). These could either stand alone as independent training modules or be incorporated into the existing suite of modules. For example, institutional review boards and ethics committees mandate Collaborative Institutional Training Initiative training and periodic recertification for researchers participating in human research. Additional Collaborative Institutional Training Initiative modules should be required on structural health disparities, systemic racism, and the importance of incorporating antiracism approaches in ethical clinical research. Trainings on health equity, racism awareness, and antiracism approaches should not be suggested, recommended, or preferred; it should be mandatory and expected before investigators at all career levels can participate in federally funded human research. Required trainings will help trainees and early career investigators become more aware of the problem and better equipped to address it, and the hope is that these younger generations will internalize and propagate these lessons.
Box 1. Current topics recommended for responsible conduct of research training, together with potential new topic suggestions (denoted by bold font) as standalone modules or integrated into current modules
-
•
Conflict of interest
-
•
Policies on research with human subjects and vertebrate animals
-
•
Mentor/mentee responsibilities
-
•
Safe and inclusive research environments
-
•
Collaborative research
-
•
Peer review
-
•
Data acquisition and analysis
-
•
Secure and ethical data use and confidentiality
-
•
Research misconduct
-
•
Responsible authorship
-
•
Scientist as responsible members of society
-
•
The effects of systemic racism on health disparities and inequities
-
•
Incorporating antiracism methodologies into research on human subjects
Academic institutions and clinical research organizations have similar oversight and responsibility for the conduct of research. Organizations must ensure that their research offices include the necessary expertise to advise investigators. Institutions provide resources for biostatistics and study design; they should also facilitate consultation with experts on antiracism methodologies during the development phase of a study or proposal. Institutional review board committees should include representatives with adequate expertise as well. Importantly, the advice and support provided by these experts should be properly recognized with protected time, recognition for promotion and tenure, and adequate compensation. Institutions should offer continuous training on social determinants of health, history of systemic racism and its impacts on health outcomes, how to recruit and train community investigators, and research-to-policy implications.
Racially and ethnically marginalized researchers face structural barriers to successful funding, and funding agencies should take initiatives to reverse such disparities. Several mechanisms have begun to foster the career development of underrepresented minorities in biomedical research. Funders may consider supporting institutions that share the same priorities, such as historically Black colleges and universities and Hispanic-serving institutions. Moreover, racially and ethnically marginalized investigators and scholars should be sufficiently supported by their institutions rather than being taxed with fighting structural inequities within and outside of the organization (108–113). Examples of institutional supports include investing in financial support for professional development activities, providing opportunities and support for multiple levels of mentoring (e.g., affinity groups, peer and near-peer mentoring teams), supporting and facilitating cross-disciplinary mentoring and collaboration, attaching value to health equity work and research that is commensurate with “traditional” scholarship activities, attaching value to the additional mentoring and advising responsibilities that many investigators from marginalized groups engage in, providing financial support to alleviate additional burdens, and providing competitive startup packages and bridge funding supports. Institutions can also be intentional about mentoring investigators from backgrounds underrepresented in health care by encouraging applications to internal pilot award programs, multiyear internal institutional grants, T32 training grants, NIH Stimulating Access to Research in Residency R38, internal and national K12 programs, the NIH Programs for Inclusion and Diversity Among Individuals Engaged in Health-related Research Program (114), NIH loan repayment programs, and foundation award programs such as the Amos Medical Faculty Development Award Program (115). In addition, institutions should be actively engaged in promoting pathways to health care for individuals from marginalized groups starting as early as elementary and middle school through science training programs and observerships (108, 116–118). Regulatory agencies should systematically require that pharmaceutical industries, foundations, and other funders include underrepresented investigators in their funding calls, research programs, and clinical trials.
Finally, academic institutions and healthcare systems need to begin to collaborate in bringing research outcomes to policy recommendations. Researchers’ and clinicians’ voices can strengthen calls for policy change to address inequities in health care at multiple levels. Further training in best practices for sharing results and advocacy with institutional, local, or federal policy makers will increase the impact of the research on system-level change.
Conclusions
Systemic racism is the most pervasive cause of the differential distribution of the social determinants of health in the United States. Childhood asthma is a prominent example of a host-by-environment condition that disproportionately affects urban, minoritized children. Progress in dismantling the structures, policies, practices, norms, values, systems, beliefs, and attitudes that created and perpetuate societal inequity and disparities in health outcomes is challenging. Medical research develops new knowledge and establishes factual relationships in human health and disease and therefore must ensure equitable, unbiased practices in the planning and execution of scientific discoveries. All research and research funding that aims to understand and mitigate the impact of systemic racism on children with asthma should include a plan to dismantle the policies that perpetuate the inequities created by systemic racism. The ATS workshop identified key gaps and recommendations to advance identification, study, and mitigation of systemic racism in pediatric asthma research that can be broadly applied.
Acknowledgments
Acknowledgment
Michelle Freemer (National Heart, Lung, and Blood Institute Program Director) and Elsy Peoples (family perspective) participated in one of the workshop discussions.
This workshop report was prepared by an ad hoc subcommittee of the ATS Assembly on Pediatrics.
Members of the subcommittee are as follows:
Stephanie Lovinsky-Desir, M.D., M.S. (Co-Chair)1*
Isaretta L. Riley, M.D., M.P.H. (Co-Chair)2‡
Jonathan M. Gaffin, M.D., M.S.Sc. (Co-Chair)4§
Monica J. Federico, M.D. (Co-Chair)6§
Andrea J. Apter, M.D., M.Sc.7‖
Andrew F. Beck, M.D., M.P.H.8¶
Keisha L. Bentley-Edwards, Ph.D., M.A.3**
Carol Berkowitz, M.D.9¶
Charmane Braxton, B.S.-R.T.11‡‡
Tyra Bryant-Stephens, M.D.12¶,§§
Heather De Keyser, M.D., M.S.C.S.6§,§§
Jasmine Dean, B.A.11‡‡
Erick Forno, M.D., M.P.H.13§,§§
Camara Phyllis Jones, M.D., Ph.D., M.P.H.14‖‖
Daphne Koinis-Mitchell, Ph.D.15¶¶
Ariangela J. Kozik, Ph.D.16§§,***
Margee Louisias, M.D., M.P.H.5‖,§§,‡‡‡
Elizabeth C. Matsui, M.D., M.H.S.17§§,‡‡‡
Sande O. Okelo, M.D., Ph.D.10§
Beverley J. Sheares, M.D., M.S.18§§,§§§
Jennifer L. Taylor-Cousar, M.D., M.S.C.S.19,20‡,§
Stephen J. Teach, M.D., M.P.H.21‖‖‖
Neeta Thakur, M.D.22,23‡,§§
Michael E. Wechsler, M.D., M.M.Sc.19‡
*Pediatric Pulmonary and Environmental Health Sciences
‡Adult Pulmonary
§Pediatric Pulmonary
‖Adult Allergy
¶Pediatrics
**General Internal Medicine
‡‡Pediatric Community Health Worker and Asthma Research Assistant
§§Group Leader
‖‖Family Medicine and Epidemiology
¶¶Psychology
***Microbiology
‡‡‡Pediatric Allergy
§§§Pediatric Pulmonary and Medical Education
‖‖‖Pediatric Emergency Medicine
1Division of Pediatric Pulmonology, Columbia University Vagelos College of Physicians and Surgeons, New York, New York; 2Division of Pulmonary, Allergy and Critical Care and 3Division of General Internal Medicine, Department of Medicine, Duke University School of Medicine, Durham, North Carolina; 4Division of Pulmonary Medicine, Boston Children’s Hospital, Department of Pediatrics, and 5Division of Allergy and Clinical Immunology, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts; 6Breathing Institute, University of Colorado School of Medicine and Children’s Hospital Colorado, Aurora, Colorado; 7Pulmonary Allergy Critical Care Division, University of Pennsylvania, Philadelphia, Pennsylvania; 8Cincinnati Children’s, Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, Ohio; 9Department of Pediatrics and 10Division of Pediatric Pulmonology and Sleep Medicine, The David Geffen School of Medicine, University of California, Los Angeles, Los Angeles, California; 11The Community Asthma Prevention Program and 12General Pediatrics, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; 13Pulmonology, Allergy/Immunology, and Sleep Medicine, Department of Pediatrics, Indiana University School of Medicine, Indianapolis, Indiana; 14O’Neill Institute for National and Global Health Law, Georgetown University Law Center, Washington, District of Columbia; 15Department of Pediatrics, Department of Child Psychiatry, Rhode Island Hospital and Alpert Medical School of Brown University, Providence, Rhode Island; 16Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine and Department of Molecular, Cellular, and Developmental Biology, University of Michigan, Ann Arbor, Michigan; 17Department of Population Health, Department of Pediatrics, University of Texas Austin Dell Medical School, Austin, Texas; 18Section of Pulmonary Allergy/Immunology & Sleep Medicine, Yale School of Medicine, New Haven, Connecticut; 19Divisions of Pulmonary, Critical Care and Sleep Medicine and Pediatric Pulmonary Medicine, National Jewish Health, Denver, Colorado; 20Divisions of Pulmonary Sciences and Critical Care Medicine and Pediatric Pulmonology, University of Colorado Anschutz Medical Campus, Aurora, Colorado; 21Children’s National Hospital, Washington, District of Columbia; 22Division of Pulmonary and Critical Care Medicine, Zuckerberg San Francisco General Hospital, San Francisco, California; and 23Department of Medicine, University of California, San Francisco, San Francisco, California
Footnotes
This official workshop report of the American Thoracic Society was approved May 2024
This document was funded by the American Thoracic Society.
This document has a data supplement, which is accessible at the Supplements tab.
Subcommittee Disclosures: H.D.K. received research support from Propeller Health/ResMed and NHLBI. M.L. served as a consultant for RubiconMD and received research support from Brigham and Women's Hospital Minority Faculty Career Development Award, and the Bristol Myers Squibb Foundation Robert A. Winn Award. H.D.K. is an employee of Sanofi. E.C.M. served on an advisory committee for AAAAI, American Academy of Pediatrics, National Academy of Sciences, Engineering, and Medicine and received research support from NIH. J.L.T.-C. served on an advisory committee for 4DMT, Cystic Fibrosis Foundation, Emily's Entourage, Insmed, Lancet Respiratory Medicine, Polarean, Proteostasis, and Vertex. J.L.T.-C served on a data safety and monitoring board for AbbVie and as a speaker for Vertex. Additionally, J.L.T.-C served on the editorial board for the Journal of Cystic Fibrosis, and received research support from 4DMT, Cystic Fibrosis Foundation, Eloxx, NIH, Proteostasis, and Vertex. S.J.T. received research support from NIH/NIAID, NIH/NHLBI, Novartis, and royalties from UpToDate. M.E.W. served as a consultant for Allakos, Amgen, Areteia, Arrowhead, AstraZeneca, Avala, Boehringer Ingelheim, Celldex, Cerecor, Cohero, Cytoreason, Eli Lilly, Equillium, GlaxoSmithKline, Incyte, Kinaset, Merck, Novartis, Phylaxis, Pulmatrix, Rapt Therapeutics, Recludix, Regeneron, Roche/Genentech, Sanofi Genzyme, Sound Biologics, Tetherex, Teva, Uniquity Bio, Upstream Bio, Verona Pharma, and Zurabio. Additionally, M.E.W. served on a data safety and monitoring board for Sentien and received research support from AstraZeneca, Avala, GlaxoSmithKline, Pulmatrix, Rapt Therapeutics, Regeneron, and Upstream Bio. Finally, M.E.W holds equity in Upstream Bio. S.L.-D., I.L.R., T.B.-S., E.F., A.J.K., B.J.S., N.T., A.J.A., A.F.B., K.L.B.-E., C.Berkowitz, C.Braxton, J.D., C.P.J., D.K.-M., S.O.O., J.M.G., and M.J.F. reported no commercial or relevant non-commercial interests from ineligible companies.
References
- 1.U.S. Census Bureau. United States census definition of race. https://www.census.gov/quickfacts/fact/note/US/RHI625222#:~:text=OMB%20requires%20five%20minimum%20categories,report%20more%20than%20one%20race
- 2.Roberts D. Fatal invention: how science, politics, and big business re-create race in the twenty-first century. New York: New Press; 2011. [Google Scholar]
- 3.Rothstein R. The color of law. New York: Liveright Publishing; 2017. [Google Scholar]
- 4. Schuyler AJ, Wenzel SE. Historical redlining impacts contemporary environmental and asthma-related outcomes in Black adults. Am J Respir Crit Care Med . 2022;206:824–837. doi: 10.1164/rccm.202112-2707OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Blatt LR, Sadler RC, Jones EJ, Miller P, Hunter-Rue DS, Votruba-Drzal E. Historical structural racism in the built environment and contemporary children’s opportunities. Pediatrics . 2024;153:e2023063230. doi: 10.1542/peds.2023-063230. [DOI] [PubMed] [Google Scholar]
- 6. Lee EK, Donley G, Ciesielski TH, Gill I, Yamoah O, Roche A, et al. Health outcomes in redlined versus non-redlined neighborhoods: a systematic review and meta-analysis. Soc Sci Med . 2022;294:114696. doi: 10.1016/j.socscimed.2021.114696. [DOI] [PubMed] [Google Scholar]
- 7. Nardone A, Casey JA, Morello-Frosch R, Mujahid M, Balmes JR, Thakur N. Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study. Lancet Planet Health . 2020;4:e24–e31. doi: 10.1016/S2542-5196(19)30241-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hwa Jung K, Pitkowsky Z, Argenio K, Quinn JW, Bruzzese JM, Miller RL, et al. The effects of the historical practice of residential redlining in the United States on recent temporal trends of air pollution near New York City schools. Environ Int . 2022;169:107551. doi: 10.1016/j.envint.2022.107551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gao C, Sanchez KM, Lovinsky-Desir S. Structural and social determinants of inequitable environmental exposures in the United States. Clin Chest Med . 2023;44:451–467. doi: 10.1016/j.ccm.2023.03.002. [DOI] [PubMed] [Google Scholar]
- 10. Bailey ZD, Feldman JM, Bassett MT. How structural racism works—racist policies as a root cause of US racial health inequities. N Engl J Med . 2020;384:768–773. doi: 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Canino G, Koinis-Mitchell D, Ortega AN, McQuaid EL, Fritz GK, Alegría M. Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Soc Sci Med . 2006;63:2926–2937. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 12. Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol . 2009;123:1209–1217. doi: 10.1016/j.jaci.2009.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Correa-Agudelo E, Ding L, Beck AF, Brokamp C, Altaye M, Kahn RS, et al. Understanding racial disparities in childhood asthma using individual- and neighborhood-level risk factors. J Allergy Clin Immunol . 2022;150:1427–1436.e5. doi: 10.1016/j.jaci.2022.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kopel LS, Phipatanakul W, Gaffin JM. Social disadvantage and asthma control in children. Paediatr Respir Rev . 2014;15:256–262. doi: 10.1016/j.prrv.2014.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez A, Thakur N. In: Precision approaches to heterogeneity in asthma. Brasier AR, Jarjour NN, editors. Cham, Switzerland: Springer; 2023. Structural racism and the social determinants of health in asthma; pp. 101–115. [DOI] [PubMed] [Google Scholar]
- 16. Baugh A, Thakur N. Race, racism, and respiratory health. Clin Chest Med . 2023;44:469–478. doi: 10.1016/j.ccm.2023.03.003. [DOI] [PubMed] [Google Scholar]
- 17. Okelo SO. Structural inequities in medicine that contribute to racial inequities in asthma care. Semin Respir Crit Care Med . 2022;43:752–762. doi: 10.1055/s-0042-1756491. [DOI] [PubMed] [Google Scholar]
- 18. Okelo SO. Racial inequities in asthma care. Semin Respir Crit Care Med . 2022;43:684–708. doi: 10.1055/s-0042-1756492. [DOI] [PubMed] [Google Scholar]
- 19. Pollack CE, Roberts LC, Peng RD, Cimbolic P, Judy D, Balcer-Whaley S, et al. Association of a housing mobility program with childhood asthma symptoms and exacerbations. JAMA . 2023;329:1671–1681. doi: 10.1001/jama.2023.6488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Phillippe M. Telomeres, oxidative stress, and timing for spontaneous term and preterm labor. Am J Obstet Gynecol . 2022;227:148–162. doi: 10.1016/j.ajog.2022.04.024. [DOI] [PubMed] [Google Scholar]
- 21. Martz CD, Allen AM, Fuller-Rowell TE, Spears EC, Lim SS, Drenkard C, et al. Vicarious racism stress and disease activity: the Black Women’s Experiences Living with Lupus (BeWELL) study. J Racial Ethn Health Disparities . 2019;6:1044–1051. doi: 10.1007/s40615-019-00606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Coogan PF, Yu J, O’Connor GT, Brown TA, Cozier YC, Palmer JR, et al. Experiences of racism and the incidence of adult-onset asthma in the Black Women’s Health Study. Chest . 2014;145:480–485. doi: 10.1378/chest.13-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carlson S, Borrell LN, Eng C, Nguyen M, Thyne S, LeNoir MA, et al. Self-reported racial/ethnic discrimination and bronchodilator response in African American youth with asthma. PLoS One . 2017;12:e0179091. doi: 10.1371/journal.pone.0179091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jones BL, Staggs V, Woods-Jaeger B. Chronic stress exposure among young African American children with asthma: racism is a factor. Ann Allergy Asthma Immunol . 2019;123:507–508. doi: 10.1016/j.anai.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 25. Thakur N, Barcelo NE, Borrell LN, Singh S, Eng C, Davis A, et al. Perceived discrimination associated with asthma and related outcomes in minority youth: the GALA II and SAGE II studies. Chest . 2017;151:804–812. doi: 10.1016/j.chest.2016.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Groos M, Wallace M, Hardeman R. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Dispar Res Pract . 2018;11:13. [Google Scholar]
- 27. Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping neighborhood health geomarkers to clinical care decisions to promote equity in child health. Health Aff (Millwood) . 2017;36:999–1005. doi: 10.1377/hlthaff.2016.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parsons A, Unaka NI, Stewart C, Foster J, Perez V, Jones NY, et al. Seven practices for pursuing equity through learning health systems: notes from the field. Learn Health Syst . 2021;5:e10279. doi: 10.1002/lrh2.10279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fergusson D, Monfaredi Z, Pussegoda K, Garritty C, Lyddiatt A, Shea B, et al. The prevalence of patient engagement in published trials: a systematic review. Res Involv Engagem . 2018;4:17. doi: 10.1186/s40900-018-0099-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Han HR, Xu A, Mendez KJW, Okoye S, Cudjoe J, Bahouth M, et al. Exploring community engaged research experiences and preferences: a multi-level qualitative investigation. Res Involv Engagem . 2021;7:19. doi: 10.1186/s40900-021-00261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jones CP, Truman BI, Elam-Evans LD, Jones CA, Jones CY, Jiles R, et al. Using “socially assigned race” to probe white advantages in health status. Ethn Dis . 2008;18:496–504. [PubMed] [Google Scholar]
- 32. Borrell LN, Elhawary JR, Fuentes-Afflick E, Witonsky J, Bhakta N, Wu AHB, et al. Race and genetic ancestry in medicine—a time for reckoning with racism. N Engl J Med . 2021;384:474–480. doi: 10.1056/NEJMms2029562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Martinez A, de la Rosa R, Mujahid M, Thakur N. Structural racism and its pathways to asthma and atopic dermatitis. J Allergy Clin Immunol . 2021;148:1112–1120. doi: 10.1016/j.jaci.2021.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilkerson I. Caste: the origins of our discontent. New York: Penguin Random House; 2020. [Google Scholar]
- 35. Camara PJ. Confronting institutionalized racism. Phylon (1960-) . 2002;50:7–22. [Google Scholar]
- 36. Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic and structural racism: definitions, examples, health damages, and approaches to dismantling. Health Aff (Millwood) . 2022;41:171–178. doi: 10.1377/hlthaff.2021.01394. [DOI] [PubMed] [Google Scholar]
- 37.Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health 2000; 90:1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bonilla-Silva E. Rethinking racism: toward a structural interpretation. Am Sociol Rev . 1997;62:465–480. [Google Scholar]
- 39.National Research Council. Measuring racial discrimination. Washington, DC: National Academies Press; 2004. [Google Scholar]
- 40.Brennan Center for Justice. Voting laws roundup: October 2021. 2021. https://www.brennancenter.org/our-work/research-reports/voting-laws-roundup-october-2021
- 41.Keyssar A. The right to vote: the contested history of democracy in the United States. New York, NY: Basic Books; 2009. [Google Scholar]
- 42.Office of the New York State Attorney General Letitia James. Racial disparities in homeownership: how lending practices have prevented New Yorkers of color from purchasing homes and deepened wealth inequality. Albany, NY: Author; 2023. [Google Scholar]
- 43.Amalie Z, Liam R.How local differences in race and place affect mortgage lending. 2022. https://www.urban.org/urban-wire/how-local-differences-race-and-place-affect-mortgage-lending
- 44.Asthma and Allergy Foundation of America. Arlington, VA: Author; 2020. . Asthma disparities in America: a roadmap to reducing burden on racial and ethnic minorities. [Google Scholar]
- 45. Thakur N, Lovinsky-Desir S, Appell D, Bime C, Castro L, Celedon JC, et al. Enhancing recruitment and retention of minority populations for clinical research in pulmonary, critical care, and sleep medicine: an Official American Thoracic Society research statement. Am J Respir Crit Care Med . 2021;204:e26–e50. doi: 10.1164/rccm.202105-1210ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shelton RC, Adsul P, Oh A, Moise N, Griffith DM. Application of an antiracism lens in the field of implementation science (IS): recommendations for reframing implementation research with a focus on justice and racial equity. Implement Res Pract . 2021;2:26334895211049482. doi: 10.1177/26334895211049482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ojikutu BO, Stephenson KE, Mayer KH, Emmons KM. Building trust in COVID-19 vaccines and beyond through authentic community investment. Am J Public Health . 2021;111:366–368. doi: 10.2105/AJPH.2020.306087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mainardi AS, Harris D, Rosenthal A, Redlich CA, Hu B, Fenick AM. Reducing asthma exacerbations in vulnerable children through a medical–legal partnership. J Asthma . 2023;60:262–269. doi: 10.1080/02770903.2022.2045307. [DOI] [PubMed] [Google Scholar]
- 49. Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health . 2010;100((Suppl 1)):S30–S35. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Andress L, Hall T, Davis S, Levine J, Cripps K, Guinn D. Addressing power dynamics in community-engaged research partnerships. J Patient Rep Outcomes . 2020;4:24. doi: 10.1186/s41687-020-00191-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Minkler M. Ethical challenges for the “outside” researcher in community-based participatory research. Health Educ Behav . 2004;31:684–697. doi: 10.1177/1090198104269566. [DOI] [PubMed] [Google Scholar]
- 52. Prakash S. Power, privilege and participation: meeting the challenge of equal research alliances. Race Poverty Environ . 2004;11:16–19. [Google Scholar]
- 53. Campbell JD, Brooks M, Hosokawa P, Robinson J, Song L, Krieger J. Community health worker home visits for Medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health . 2015;105:2366–2372. doi: 10.2105/AJPH.2015.302685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health . 2009;99((Suppl 3)):S657–S665. doi: 10.2105/AJPH.2009.165423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Fleming PJ, Stone LC, Creary MS, Greene-Moton E, Israel BA, Key KD, et al. Antiracism and community-based participatory research: synergies, challenges, and opportunities. Am J Public Health . 2023;113:70–78. doi: 10.2105/AJPH.2022.307114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Anderson NB. Levels of analysis in health science: a framework for integrating sociobehavioral and biomedical research. Ann N Y Acad Sci . 1998;840:563–576. doi: 10.1111/j.1749-6632.1998.tb09595.x. [DOI] [PubMed] [Google Scholar]
- 57. Warren CM, Brown E, Wang J, Matsui EC. Increasing representation of historically marginalized populations in allergy, asthma, and immunologic research studies: challenges and opportunities. J Allergy Clin Immunol Pract . 2022;10:929–935. doi: 10.1016/j.jaip.2022.01.014. [DOI] [PubMed] [Google Scholar]
- 58. Mansour ME, Rose B, Toole K, Luzader CP, Atherton HD. Pursuing perfection: an asthma quality improvement initiative in school-based health centers with community partners. Public Health Rep . 2008;123:717–730. doi: 10.1177/003335490812300608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Halterman JS, Szilagyi PG, Fisher SG, Fagnano M, Tremblay P, Conn KM, et al. Randomized controlled trial to improve care for urban children with asthma: results of the School-Based Asthma Therapy trial. Arch Pediatr Adolesc Med . 2011;165:262–268. doi: 10.1001/archpediatrics.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Eakin MN, Zaeh S, Eckmann T, Ruvalcaba E, Rand CS, Hilliard ME, et al. Effectiveness of a home- and school-based asthma educational program for Head Start children with asthma: a randomized clinical trial. JAMA Pediatr . 2020;174:1191–1198. doi: 10.1001/jamapediatrics.2020.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Knopf JA, Finnie RKC, Peng Y, Hahn RA, Truman BI, Vernon-Smiley M, et al. Community Preventive Services Task Force School-based health centers to advance health equity: a community guide systematic review. Am J Prev Med . 2016;51:114–126. doi: 10.1016/j.amepre.2016.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Krieger JW, Philby ML, Brooks MZ. Better home visits for asthma: lessons learned from the Seattle–King County asthma program. Am J Prev Med . 2011;41:S48–S51. doi: 10.1016/j.amepre.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 63. Banda Y, Kvale MN, Hoffmann TJ, Hesselson SE, Ranatunga D, Tang H, et al. Characterizing race/ethnicity and genetic ancestry for 100,000 subjects in the Genetic Epidemiology Research on Adult Health and Aging (GERA) cohort. Genetics . 2015;200:1285–1295. doi: 10.1534/genetics.115.178616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Klein DJ, Elliott MN, Haviland AM, Morrison PA, Orr N, Gaillot S, et al. A comparison of methods for classifying and modeling respondents who endorse multiple racial/ethnic categories: a health care experience application. Med Care . 2019;57:e34–e41. doi: 10.1097/MLR.0000000000001012. [DOI] [PubMed] [Google Scholar]
- 65. Kerkhoff AD, Farrand E, Marquez C, Cattamanchi A, Handley MA. Addressing health disparities through implementation science—a need to integrate an equity lens from the outset. Implement Sci . 2022;17:13. doi: 10.1186/s13012-022-01189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sewell A. The racism-race reification process: a mesolevel political economic framework for understanding racial health disparities. Sociol Race Ethn (Thousand Oaks) . 2016;2:402–432. [Google Scholar]
- 67. Jones CP. Toward the science and practice of anti-racism: launching a national campaign against racism. Ethn Dis . 2018;28:231–234. doi: 10.18865/ed.28.S1.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ramírez M, Ford ME, Stewart AL, Teresi JA. Measurement issues in health disparities research. Health Serv Res . 2005;40:1640–1657. doi: 10.1111/j.1475-6773.2005.00450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wolff LS, Acevedo-Garcia D, Subramanian SV, Weber D, Kawachi I. Subjective social status, a new measure in health disparities research: do race/ethnicity and choice of referent group matter? J Health Psychol . 2010;15:560–574. doi: 10.1177/1359105309354345. [DOI] [PubMed] [Google Scholar]
- 70. Elliott T, Floyd James K, Coleman KJ, Skrine Jeffers K, Nau CL, Choi K. Cross-sectional comparison of disparities by race using White vs Hispanic as reference among children and youths with developmental disabilities referred for speech therapy. JAMA Netw Open . 2022;5:e2234453. doi: 10.1001/jamanetworkopen.2022.34453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Gilliam CA, Lindo EG, Cannon S, Kennedy L, Jewell TE, Tieder JS. Use of race in pediatric clinical practice guidelines: a systematic review. JAMA Pediatr . 2022;176:804–810. doi: 10.1001/jamapediatrics.2022.1641. [DOI] [PubMed] [Google Scholar]
- 72. Newman AM. Moving beyond mistrust: centering institutional change by decentering the White analytical lens. Bioethics . 2022;36:267–273. doi: 10.1111/bioe.12992. [DOI] [PubMed] [Google Scholar]
- 73. Bhakta NR, Bime C, Kaminsky DA, McCormack MC, Thakur N, Stanojevic S, et al. Race and ethnicity in pulmonary function test interpretation: an official American Thoracic Society statement. Am J Respir Crit Care Med . 2023;207:978–995. doi: 10.1164/rccm.202302-0310ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Thakur N, Martinez A. Housing reparations as an avenue to counter the impact of structural racism on asthma. JAMA . 2023;329:1645–1647. doi: 10.1001/jama.2023.7242. [DOI] [PubMed] [Google Scholar]
- 75. Oetzel JG, Wallerstein N, Duran B, Sanchez-Youngman S, Nguyen T, Woo K, et al. Impact of participatory health research: a test of the community-based participatory research conceptual model. Biomed Res Int . 2018;2018:7281405. doi: 10.1155/2018/7281405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Wallerstein N, Oetzel JG, Sanchez-Youngman S, Boursaw B, Dickson E, Kastelic S, et al. Engage for equity: a long-term study of community-based participatory research and community-engaged research practices and outcomes. Health Educ Behav . 2020;47:380–390. doi: 10.1177/1090198119897075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Devia C, Baker EA, Sanchez-Youngman S, Barnidge E, Golub M, Motton F, et al. Advancing system and policy changes for social and racial justice: comparing a rural and urban community-based participatory research partnership in the US. Int J Equity Health . 2017;16:17. doi: 10.1186/s12939-016-0509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guptill M.Engaging communities as experts throughout the assessment process—health resources in action. 2021. https://hria.org/2021/11/01/communityassessment/
- 79. Emmons KM, Curry M, Lee RM, Pless A, Ramanadhan S, Trujillo C. Enabling community input to improve equity in and access to translational research: the Community Coalition for Equity in Research. J Clin Transl Sci . 2022;6:e60. doi: 10.1017/cts.2022.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patient-Centered Outcomes Research Institute (PCORI) Eugene Washington PCORI Engagement Award Program. https://www.pcori.org/engagement/eugene-washington-pcori-engagement-award-program
- 81. Eng E, Blanchard L. Action-oriented community diagnosis: a health education tool. Int Q Community Health Educ . 1990;11:93–110. doi: 10.2190/W8MU-5H9X-PQW1-LV38. [DOI] [PubMed] [Google Scholar]
- 82. Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health . 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Clark NM, Lachance L, Doctor LJ, Gilmore L, Kelly C, Krieger J, et al. Policy and system change and community coalitions: outcomes from allies against asthma. Am J Public Health . 2010;100:904–912. doi: 10.2105/AJPH.2009.180869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Butterfoss FD, Gilmore LA, Krieger JW, Lachance LL, Lara M, Meurer JR, et al. From formation to action: how allies against asthma coalitions are getting the job done. Health Promot Pract . 2006;7:34S–43S. doi: 10.1177/1524839906287063. [DOI] [PubMed] [Google Scholar]
- 85. Brown AF, Ma GX, Miranda J, Eng E, Castille D, Brockie T, et al. Structural interventions to reduce and eliminate health disparities. Am J Public Health . 2019;109:S72–S78. doi: 10.2105/AJPH.2018.304844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Krieger N. Living and dying at the crossroads: racism, embodiment, and why theory is essential for a public health of consequence. Am J Public Health . 2016;106:832–833. doi: 10.2105/AJPH.2016.303100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Acevedo-Garcia D, McArdle N, Hardy EF, Crisan UI, Romano B, Norris D, et al. The Child Opportunity Index: improving collaboration between community development and public health. Health Aff (Millwood) . 2014;33:1948–1957. doi: 10.1377/hlthaff.2014.0679. [DOI] [PubMed] [Google Scholar]
- 88. Dyer Z, Alcusky MJ, Galea S, Ash A. Measuring the enduring imprint of structural racism on American neighborhoods. Health Aff (Millwood) . 2023;42:1374–1382. doi: 10.1377/hlthaff.2023.00659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med . 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 90. Taylor TR, Kamarck TW, Shiffman S. Validation of the Detroit Area Study Discrimination Scale in a community sample of older African American adults: the Pittsburgh Healthy Heart Project. Int J Behav Med . 2004;11:88–94. doi: 10.1207/s15327558ijbm1102_4. [DOI] [PubMed] [Google Scholar]
- 91. Ginther DK, Schaffer WT, Schnell J, Masimore B, Liu F, Haak LL, et al. Race, ethnicity, and NIH research awards. Science . 2011;333:1015–1019. doi: 10.1126/science.1196783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Taffe MA, Gilpin NW. Racial inequity in grant funding from the US National Institutes of Health. Elife . 2021;10:e65697. doi: 10.7554/eLife.65697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Shavers VL, Fagan P, Lawrence D, McCaskill-Stevens W, McDonald P, Browne D, et al. Barriers to racial/ethnic minority application and competition for NIH research funding. J Natl Med Assoc . 2005;97:1063–1077. [PMC free article] [PubMed] [Google Scholar]
- 94. Zimmermann A, Klavans R, Offhaus HM, Grieb TA, Smith C. Award rate inequities in biomedical research. PLoS One . 2022;17:e0270612. doi: 10.1371/journal.pone.0270612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Chen CY, Kahanamoku SS, Tripati A, Alegado RA, Morris VR, Andrade K, et al. Systemic racial disparities in funding rates at the National Science Foundation. Elife . 2022;11:e83071. doi: 10.7554/eLife.83071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Ginther DK, Haak LL, Schaffer WT, Kington R. Are race, ethnicity, and medical school affiliation associated with NIH R01 type 1 award probability for physician investigators? Acad Med . 2012;87:1516–1524. doi: 10.1097/ACM.0b013e31826d726b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Hoppe TA, Litovitz A, Willis KA, Meseroll RA, Perkins MJ, Hutchins BI, et al. Topic choice contributes to the lower rate of NIH awards to African-American/black scientists. Sci Adv . 2019;5:eaaw7238. doi: 10.1126/sciadv.aaw7238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Haeny AM, Holmes SC, Williams MT. Applying anti-racism to clinical care and research. JAMA Psychiatry . 2021;78:1187–1188. doi: 10.1001/jamapsychiatry.2021.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Matsui EC, Perry TT, Adamson AS. An antiracist framework for racial and ethnic health disparities research. Pediatrics . 2020;146:e2020018572. doi: 10.1542/peds.2020-018572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.U.S. Environmental Protection Agency. Coordinated federal action plan to reduce racial and ethnic asthma disparities. 2023. https://www.epa.gov/asthma/coordinated-federal-action-plan-reduce-racial-and-ethnic-asthma-disparities
- 101.National Institutes of Health. Ending structural racism. https://www.nih.gov/ending-structural-racism/unite
- 102.National Institute on Minority Health and Health Disparities. NIMHD minority health and health disparities research framework. 2017. https://www.nimhd.nih.gov/about/overview/research-framework/ [DOI] [PMC free article] [PubMed]
- 103.National Institutes of Health. Community Partnerships to Advance Science for Society (ComPASS) https://commonfund.nih.gov/compass
- 104.National Institutes of Health. Ending structural racism. https://www.nih.gov/ending-structural-racism
- 105. Kho A, Daumit GL, Truesdale KP, Brown A, Kilbourne AM, Ladapo J, et al. The National Heart Lung and Blood Institute Disparities Elimination through Coordinated Interventions to Prevent and Control Heart and Lung Disease Alliance. Health Serv Res . 2022;57((Suppl 1)):20–31. doi: 10.1111/1475-6773.13983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.U.S. Department of Health and Human Services. Overview information. https://grants.nih.gov/grants/guide/pa-files/PAR-23-112.html
- 107.National Institutes of Health. FY 2022 updated guidance: requirement for instruction in the responsible conduct of research. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-22-055.html
- 108. Stephenson N, Forno E, Laguna TA, Lovinsky-Desir S, Moore PE, Sheares BJ, et al. Diversity, equity, and inclusion in the pediatric pulmonary workforce: an official American Thoracic Society workshop report. Ann Am Thorac Soc . 2023;20:1373–1388. doi: 10.1513/AnnalsATS.202306-583ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Okelo SO, Chesley CF, Riley I, Diaz AA, Collishaw K, Schnapp LM, et al. Accelerating action: roadmap for the American Thoracic Society to address oppression and health inequity in pulmonary and critical care medicine. Ann Am Thorac Soc . 2024;21:17–26. doi: 10.1513/AnnalsATS.202305-412PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ransdell LB, Lane TS, Schwartz AL, Wayment HA, Baldwin JA. Mentoring new and early-stage investigators and underrepresented minority faculty for research success in health-related fields: an integrative literature review (2010-2020) Int J Environ Res Public Health . 2021;18:432. doi: 10.3390/ijerph18020432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med . 2013;88:541–549. doi: 10.1097/ACM.0b013e31828589e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Settles IH, Linderman JJ, Rivas-Drake D, Saville J, Conner S. Three strategies for engaging campus leaders in transformative initiatives to retain faculty of color. J Divers High Educ . 2023 doi: 10.1037/dhe0000511. [DOI] [Google Scholar]
- 113. Martinez M, Arora V, Gonzalez CM, Dzeng E, Williams JS. Doubling down on diversity: enhancing the recruitment and retention of underrepresented academic physicians in a post-affirmative action era. J Gen Intern Med . 2024;39:1541–1543. doi: 10.1007/s11606-024-08741-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.National Heart, Lung, and Blood Institute. Programs for inclusion and diversity among individuals engaged in health-related research (PRIDE) https://www.nhlbi.nih.gov/grants-and-training/training-and-career-development/diversity/pride
- 115.Harold Amos Medical Faculty Development Program. https://www.amfdp.org/
- 116. Macedo B, Christophers B, Barrere-Cain R, Albrecht YS, Granovetter MC, Kumar R, et al. The virtual summer research program: supporting future physician-scientists from underrepresented backgrounds. J Clin Transl Sci . 2022;6:e120. doi: 10.1017/cts.2022.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Escalante E, Smiley Y, Agrawal D, Teach SJ, Cora-Bramble D, Barber A. Increasing pediatric residency class diversity to improve patient outcomes and address structural racism. Acad Med . 2022;97:850–854. doi: 10.1097/ACM.0000000000004468. [DOI] [PubMed] [Google Scholar]
- 118. Schultz PW, Hernandez PR, Woodcock A, Estrada M, Chance RC, Aguilar M, et al. Patching the pipeline: reducing educational disparities in the sciences through minority training programs. Educ Eval Policy Anal . 2011;33:10.3102/0162373710392371. doi: 10.3102/0162373710392371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Jones CP. Invited commentary: “race,” racism, and the practice of epidemiology. Am J Epidemiol . 2001;154:299–304. doi: 10.1093/aje/154.4.299. [Discussion, 305–306.] [DOI] [PubMed] [Google Scholar]
- 120. Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med . 2010;71:1390–1398. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 121.Public Health Critical Race Praxis. https://www.publichealthcriticalrace.org/?page_id=8
- 122. Wispelwey Bram P, Marsh Regan H, Wilson M, Mazimba S, Heysell Scott K, Aisiku Imoigele P, et al. Leveraging clinical decision support for racial equity: a sociotechnical innovation. NEJM Catalyst . 2022 https://catalyst.nejm.org/doi/full/10.1056/CAT.22.0076 [Google Scholar]
- 123.Healing ARC Framework. https://healingarccampaign.com/
- 124. Allen M, Wilhelm A, Ortega LE, Pergament S, Bates N, Cunningham B. Applying a race(ism)-conscious adaptation of the CFIR framework to understand implementation of a school-based equity-oriented intervention. Ethn Dis . 2021;31:375–388. doi: 10.18865/ed.31.S1.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Aarons GA, Green AE, Palinkas LA, Self-Brown S, Whitaker DJ, Lutzker JR, et al. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implement Sci . 2012;7:32. doi: 10.1186/1748-5908-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the Exploration, Preparation, Implementation, Sustainment (EPIS) framework. Implement Sci . 2019;14:1. doi: 10.1186/s13012-018-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Stanton MC, Ali SB, The Sustain Center Team A typology of power in implementation: building on the Exploration, Preparation, Implementation, Sustainment (EPIS) framework to advance mental health and HIV health equity. Implement Res Pract . 2022;3:26334895211064250. doi: 10.1177/26334895211064250. [DOI] [PMC free article] [PubMed] [Google Scholar]