Abstract
Aim
The aim of this study was to investigate the association between unhealthy lifestyle factors and the development of depressive symptoms with adjustment for sociodemographic characteristics in university students using health checkup data.
Methods
Among information obtained from university student health checkups conducted in 2017 and 2019, we analyzed both the clinical data and responses to questionnaires. The subjects used for analysis were 3190 individuals (2382 men and 808 women, mean age 19.0 years) who had been free of depressive symptoms in the 2017 survey and were available for a 2‐year follow‐up. The Patient Health Questionnaire (PHQ‐2) was used as a self‐rating scale for depressive symptoms. Multivariable logistic regression analysis was conducted to investigate the association between lifestyle factors (such as body mass index, self‐rated health, whether breakfast was taken, degree of exercise, satisfaction with sleep, smoking, and alcohol drinking) in the 2017 survey and any development of depressive symptoms revealed in the 2019 survey, adjusting for sociodemographic variables and other lifestyle factors.
Results
Multivariable logistic analysis showed that poor satisfaction with sleep (odds ratio [OR), 4.09; 95% confidence interval [CI), 1.96–8.53; p < 0.01) and female gender (OR, 2.16; 95% CI, 1.01–4.60; p = 0.05) were significantly associated with the development of depressive symptoms 2 years later.
Conclusion
This study has revealed an association between poor satisfaction with sleep and the development of depressive symptoms. We believe that these findings may be useful for the prevention and treatment of depressive symptoms in university students.
Keywords: depressive symptoms, lifestyle factors, satisfaction with sleep, university students, women
We examined the relationship between unhealthy lifestyle factors and the development of depressive symptoms. We analyzed data from an annual health checkup of students at a Japanese university 2 years later. Poor satisfaction with sleep and female gender were associated with the development of depressive symptoms.
INTRODUCTION
Most mental disorders begin during adolescence/young adulthood (ages 12–24 years), with three‐quarters of lifetime mental disorders occurring by age 25. 1 Depression is a common mental disorder, and highly prevalent among university students; a meta‐analysis of previous studies reported a prevalence of depressive symptoms of about one‐third in this population. 2 Depression is an important problem in adolescence because it reduces the quality of life and is associated with suicide risk. 3
It is widely known that genetic and temperament‐related factors and stressful life events, such as academic stress, traumatic experiences, poor economic status, and low self‐confidence, are associated with depression. 4 In addition, previous studies have indicated that healthy lifestyle habits are undoubtedly essential for maintenance of good mental health. 5 Several lifestyle‐related factors are known to be associated with depression or anxiety among university students, such as smoking, frequent alcohol use, poor sleep quality, irregular eating habits, and perceived health status. 2 , 6 These modifiable risk factors are considered to be useful targets for the treatment and prevention of depression. 7
However, previous studies of the association between unhealthy lifestyle factors and depression among university students have had some limitations. Although adolescence is a time of much stress due to physical and mental growth and environmental changes, only a limited number of studies have prospectively examined the relationship between unhealthy lifestyle factors and the development of depression, 2 while also considering the temporal relationship. Furthermore, although unhealthy lifestyle factors influence each other, few studies have adjusted for the confounding effects of various unhealthy lifestyle factors. 8 , 9
In the present study, we analyzed data from an annual health checkup of students at a large Japanese university to investigate the association between unhealthy lifestyle factors and the development of depressive symptoms. Our aim was to examine this association in a longitudinal survey. We hypothesized that individual unhealthy lifestyle factors would have different associations with the development of depressive symptoms.
METHODS
Study participants and data collection
Kyoto University Occupational Welfare Division carries out an annual health checkup for all students every April, as we have reported previously in detail. 6 , 10 This checkup consists of anthropometric measures, including height and weight, as well as blood pressure, urinalysis, and a self‐administrated web‐based questionnaire that addresses lifestyle, physical and mental health status, medical history, and current health status. The questionnaire includes the first two items of the nine‐item Patient Health Questionnaire (PHQ‐9), 11 known as the PHQ‐2, 12 as well as items about sleep satisfaction and self‐rated health (SRH). Data for this longitudinal study were obtained in 2017 and 2019.
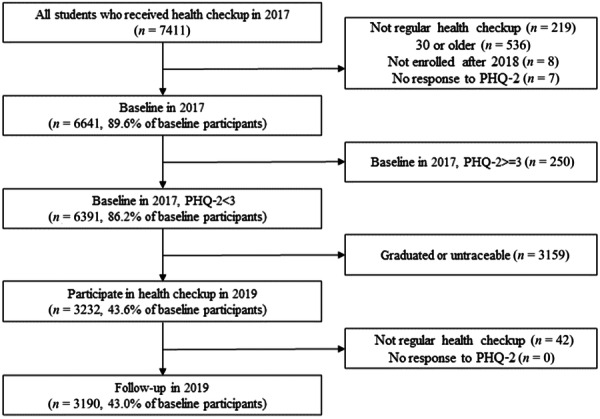
We used the data from the 2017 health checkup for a baseline survey, and those from the 2019 health checkup for a follow‐up survey. A total of 7411 students received health checkups in the baseline year. We excluded participants who had not received regular health checkups (n = 219), who were 30 years of age or older (n = 536), who had not enrolled after 2018 (n = 8), and who did not respond to the PHQ‐2 (n = 7). For the baseline survey, we selected data from 6641 subjects. Next, subjects with PHQ‐2 scores of 3 or more (n = 250) were excluded, leaving 6391 students with PHQ‐2 scores of less than 3. Among them, we excluded those who had graduated or were untraceable (n = 3159), and 3232 samples were included in the longitudinal analysis. Among them, we excluded individuals who had not undergone regular health checkups (n = 42) and had not responded to the PHQ‐2 (n = 0) during the follow‐up survey. Finally, for the longitudinal analysis, we included data from a total of 3190 subjects (Figure 1).
Figure 1.
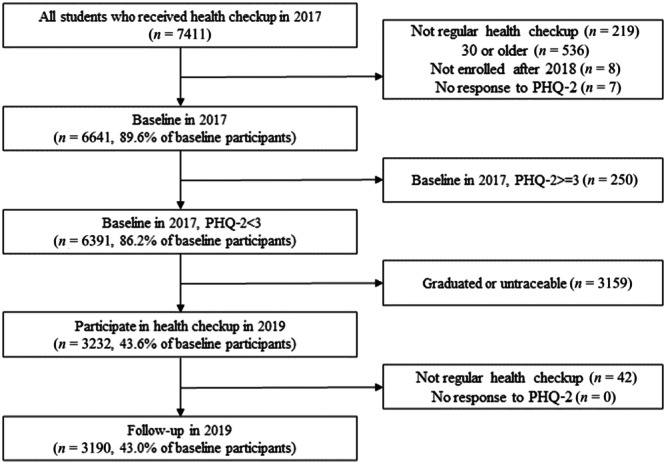
Flowchart of participants selection.
Outcome, exposure, and confounding variables
Depressive symptoms
Depressive symptoms were assessed using the first two items of the PHQ‐9, 11 known as the PHQ‐2. 12 These two items query the frequency of symptoms of depressed mood (feeling down, melancholy, or hopelessness) and loss of pleasure (little interest or enjoyment in things) and are scored on a scale comprising 0 (not at all), 1 (a few days), 2 (more than half of all days), and 3 (almost daily). Thus, the total PHQ‐2 score ranges from 0 to 6. We set a cutoff score of 3 by dichotomizing this variable into two categories, as recommended previously. 13 The PHQ‐2 has shown good reliability and validity for assessment of major depression in primary care patients. 12 Depressive symptoms were considered to have developed when participants with PHQ‐2 scores of less than 3 in the baseline survey were found to have PHQ‐2 scores of 3 or more in the follow‐up survey. Cronbach's α coefficient for the PHQ‐2 in the follow‐up survey was 0.830, which indicated good internal consistency.
Unhealthy lifestyle factors
Self‐rated health was assessed by asking the question “How would you rate your health in general?” Possible answers were very good, good, fair, bad or very bad. 14 This variable was further dichotomized into two categories: poor (including bad and very bad) and good (including fair, good and very good) self‐rated health, with reference to the previous study. 6
Sleep satisfaction was categorized as very satisfied, satisfied, dissatisfied, or very dissatisfied. Responses of somewhat dissatisfied/very dissatisfied were defined as poor satisfaction with sleep, with reference to the previous study. 6
Breakfast was categorized as daily, sometimes, or never. The answer never was treated as skipping breakfast.
Exercise was categorized as daily, sometimes, or seldom. Seldom was defined as no exercise, with reference to the previous study. 6
Alcohol drinking was categorized as never, sometimes—averaging 1 or less a day (7 or less a week), averaging 1 or more a day (7 or more a week), and have had repeated problems caused by alcohol at home, school, work, etc. All categories except for never were defined as drinking.
Smoking was categorized as no, about 10 cigarettes/day, about 20 cigarettes/day, about 30 or more cigarettes/day, and more than 30 cigarettes/day. All categories except for no were defined as smoking.
Height and weight were measured as part of the health checkup. We calculated body mass index (BMI) as weight in kilograms divided by height in meters squared (kg/m2) and categorized it into three groups: underweight (<18.5), normal weight (18.5–24.9), and obese (≥25), with reference to the previous study. 6
Sociodemographic characteristics
We collected data for the following variables: sex (male, female), age (quantitative variable), nationality (Japanese or foreign), faculty (arts, science, medicine), and admission year (2017, 2016, 2015, before 2014).
Statistical analyses
Descriptive statistics were calculated for all variables.
Associations between unhealthy lifestyle factors and the development of depressive symptoms were analyzed using crude and multivariable logistic regression. We conducted a series of logistic regression analyses to examine the association between unhealthy lifestyle factors at the baseline and the development of depressive symptoms at follow‐up, adjusting for sociodemographic variables and other lifestyle factors. Baseline covariates included sex, age, nationality, faculty, admission year, BMI, SRH, breakfast, exercise, satisfaction with sleep, smoking, and alcohol drinking. Results were expressed as OR and 95% CI. All analyses were performed using SPSS 27.0 for Windows.
RESULTS
The baseline characteristics of the participants are shown in Table 1. The subjects used for statistical analysis were 3190 individuals (2382 men and 808 women, mean age 19.0 years) who had been free of depressive symptoms in the 2017 survey and were available for the 2‐year follow‐up.
Table 1.
Baseline characteristics of the study participants.
| Population characteristics | All participants | |
|---|---|---|
| n | % | |
| Total number of participants | 3190 | |
| Age mean (SD) | 19.0 | 1.2 |
| Sex | ||
| Women | 808 | 25.3 |
| Men | 2382 | 74.7 |
| Nationality | ||
| Foreign | 42 | 1.3 |
| Japanese | 3148 | 98.7 |
| Faculty | ||
| Arts | 1220 | 38.2 |
| Science | 1334 | 41.8 |
| Medicine | 636 | 19.9 |
| Admission year | ||
| 2017 | 1978 | 62.0 |
| 2016 | 810 | 25.4 |
| 2015 | 199 | 6.2 |
| Before 2014 | 203 | 6.4 |
| BMI | ||
| <18.5 | 520 | 16.3 |
| 18.5–24.9 | 2373 | 74.4 |
| ≥25 | 249 | 7.8 |
| SRH | ||
| Poor | 91 | 2.9 |
| Fair | 3099 | 97.1 |
| Skipping breakfast | ||
| Yes | 769 | 24.1 |
| No | 2421 | 75.9 |
| Lack of exercise | ||
| Yes | 985 | 30.9 |
| No | 2205 | 69.1 |
| Satisfaction with sleep | ||
| Poor | 560 | 17.6 |
| Fair | 2630 | 82.4 |
| Smoking | ||
| Yes | 19 | 0.6 |
| No | 3171 | 99.4 |
| Alcohol drinking | ||
| Yes | 575 | 18.0 |
| No | 2615 | 82.0 |
Abbreviations: BMI, body mass index; SD, standard deviation; SRH, self‐rated health.
The results of multivariable logistic regression analyses for the development of depressive symptoms in subjects who had shown no depressive symptoms in 2017 are shown in Table 2. The prevalence of development of depressive symptoms was 1.2% among the subjects as a whole (n = 3190): 1.0% in men and 1.9% in women. The final logistic regression model (Nagelkerke R Square 0.087) showed that poor satisfaction with sleep (OR, 4.09; 95% CI, 1.96–8.53; p < 0.01) and female gender (OR, 2.16; 95% CI, 1.01–4.60; p = 0.05) were significantly associated with the development of depressive symptoms 2 years later.
Table 2.
Results of multivariable logistic regression analysis of the development of depressive symptoms in subjects without depressive symptoms in 2017 (n = 3190).
| Percentage of subjects who developed depressive symptoms | Crude | Adjusted | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | OR | 95% CI | p‐value | AOR | 95% CI | p‐value | |||
| Sex | ||||||||||
| Women | 15 | 1.9 | 1.94 | 1.01 | 3.74 | 0.05 | 2.16 | 1.01 | 4.60 | 0.05 |
| Men | 23 | 1.0 | 1.00 | 1.00 | ||||||
| Age | 1.10 | 0.86 | 1.40 | 0.46 | 0.94 | 0.56 | 1.58 | 0.81 | ||
| Nationality | ||||||||||
| Foreign | 0 | 0.0 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 1.00 | ||
| Japanese | 38 | 1.2 | 1.00 | 1.00 | ||||||
| Faculty | 0.36 | 0.53 | ||||||||
| Arts | 12 | 1.0 | 0.56 | 0.25 | 1.29 | 0.66 | 0.27 | 1.63 | ||
| Science | 15 | 1.1 | 0.65 | 0.30 | 1.41 | 1.00 | 0.40 | 2.50 | ||
| Medicine | 11 | 1.7 | 1.00 | 1.00 | ||||||
| Admission year | 0.23 | 0.59 | ||||||||
| 2017 | 18 | 0.9 | 1.00 | 1.00 | ||||||
| 2016 | 14 | 1.7 | 1.92 | 0.95 | 3.87 | 1.53 | 0.58 | 4.03 | ||
| 2015 | 2 | 1.0 | 1.11 | 0.25 | 4.80 | 0.71 | 0.07 | 7.66 | ||
| Before 2014 | 4 | 2.0 | 2.19 | 0.73 | 6.53 | 2.98 | 0.33 | 26.97 | ||
| BMI | 0.41 | 0.39 | ||||||||
| <18.5 | 5 | 1.0 | 0.88 | 0.33 | 2.29 | 0.81 | 0.31 | 2.16 | ||
| 18.5–24.9 | 26 | 1.1 | 1.00 | 1.00 | ||||||
| ≥25 | 5 | 2.0 | 1.85 | 0.70 | 4.86 | 1.89 | 0.68 | 5.21 | ||
| SRH | ||||||||||
| Poor | 4 | 4.4 | 4.14 | 1.44 | 11.94 | 0.01 | 2.60 | 0.77 | 8.74 | 0.12 |
| Fair | 34 | 1.1 | 1.00 | 1.00 | ||||||
| Skipping breakfast | ||||||||||
| Yes | 12 | 1.6 | 1.46 | 0.73 | 2.91 | 0.28 | 1.02 | 0.45 | 2.35 | 0.96 |
| No | 26 | 1.1 | 1.00 | 1.00 | ||||||
| Lack of exercise | ||||||||||
| Yes | 13 | 1.3 | 1.17 | 0.59 | 2.29 | 0.65 | 0.76 | 0.36 | 1.60 | 0.47 |
| No | 25 | 1.1 | 1.00 | 1.00 | ||||||
| Poor satisfaction with sleep | ||||||||||
| Yes | 17 | 3.0 | 3.89 | 2.04 | 7.42 | 0.00 | 4.09 | 1.96 | 8.53 | <0.01 |
| No | 21 | 0.8 | 1.00 | 1.00 | ||||||
| Smoking | ||||||||||
| Yes | 0 | 0.0 | 0.00 | 0.00 | 1.00 | 0.00 | 0.00 | 1.00 | ||
| No | 38 | 1.2 | 1.00 | 1.00 | ||||||
| Alcohol drinking | ||||||||||
| Yes | 5 | 0.9 | 0.69 | 0.27 | 1.77 | 0.43 | 0.37 | 0.11 | 1.24 | 0.11 |
| No | 33 | 1.3% | 1.00 | 1.00 | ||||||
Note: A series of logistic regression analyses to examine the association between unhealthy lifestyle factors at the baseline and the development of depressive symptoms at follow‐up. Adjusted for sex, age group, nationality, faculty, admission year, BMI, SRH, skipping breakfast, lack of exercise, poor satisfaction with sleep, smoking, and alcohol drinking.
Abbreviations: AOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; OR, odds ratio; SRH, self‐rated health.
Additional analyses
Characteristics at the baseline in 2017 for the PHQ‐2 < 3 group (n = 6391) who received a health checkup in 2019 and for those who were not followed up are shown in Table S1. The Student's unpaired t‐test was employed for the analysis of continuous variables, while the chi‐square test was utilized for categorical variables. The mean age was significantly lower for subjects who participated in 2019 than for those who did not. The percentages of subjects who developed depressive symptoms according to faculty, admission year, BMI, skipping breakfast, satisfaction with sleep, smoking, and alcohol drinking differed significantly between the two groups.
DISCUSSION
In the present study, we investigated the association between unhealthy lifestyle factors and the development of depressive symptoms 2 years later among Japanese university students. The results showed that poor satisfaction with sleep and female gender were significantly associated with the development of depressive symptoms. As sleep habits can be modifiable, they are a potentially valuable target for the treatment and prevention of depression.
In the present study, poor satisfaction with sleep was significantly associated with the development of depressive symptoms after 2 years. Significant associations between poor satisfaction with sleep and the onset of depression have also been reported in several prospective studies across different countries. In a French cohort study, poor sleep quality was significantly associated with incident depressive symptoms over a 4‐year follow‐up period. 15 In a cohort study of older US women, poor satisfaction with sleep was a risk factor for the development of depressive symptoms 6 years later. 16 In another cohort study of US women, subjective poor sleep quality was associated with a higher likelihood of worsening depressive symptoms. 17 The present results are consistent with these previous studies. However, the measures of sleep satisfaction used in those studies differed. To establish the validity of sleep assessment during regular health checkups, further research should be conducted on the association between poor sleep satisfaction and the development of depressive symptoms using validated and reliable rating scales, such as the Pittsburgh Sleep Quality Index 18 or RU‐SATED, 19 , 20 or by conducting objective sleep assessment studies using wearable devices. 21 In addition, previous studies have employed various methods for improvement of adolescent sleep health, including individual psychotherapy, 21 school‐based programs, 22 and digital interventions, 23 , 24 which have demonstrated positive effects. Continued innovation in these areas is warranted.
In the present study, female gender was significantly associated with the development of depressive symptoms 2 years later. Depression has been consistently reported to be more common in women, with a lifetime prevalence about twice as high as that in men, and three times as high in early teens. 25 The causes of this gender difference in the prevalence of depression need to be examined from multiple perspectives, including sociological factors (poverty, vulnerability to violence, inequality, etc.), psychological factors, and biological factors (hormones, etc.), in addition to the unhealthy lifestyle factors investigated in this survey.
In this study, crude analyses showed that poor SRH was significantly associated with the development of depressive symptoms 2 years later. However, these associations lost significance in the adjusted model, indicating that other covariates may impact the relationship between SRH and the development of depressive symptoms. The association between SRH and depressive symptoms has been investigated in several cross‐sectional and prospective studies. In a cross‐sectional study of university students in France and Japan, poor SRH was associated with higher PHQ‐2 scores (more depressive symptoms). 6 In a longitudinal study of Finnish subjects aged 18–79 years, the association between poor SRH and depression was significant at 2 years. A study examining the association between poor SRH and depressive symptoms assessed using the Hospital Anxiety and Depression Scale found that SRH was associated with a two‐ to threefold increase in the likelihood of developing depressive symptoms 3 years later. 26 An Australian study of older adults reported that SRH, assessed on a scale of 0–100, was a risk factor for the development of depressive symptoms 2 years later. 27 Though the results of the present study differed from those of previous ones, it appears that the association between SRH and depressive symptoms among university students may be partly a direct one.
Some of the lifestyle habits suggested to be associated with depressive symptoms in previous studies, such as alcohol drinking, smoking, skipping breakfast, obesity, and lack of exercise, 2 , 5 , 6 , 28 did not show significant associations in the crude or multivariate models employed in the present study. This may have been due to the characteristics of the subjects. Although it has been pointed out that alcohol drinking, smoking, obesity, and lack of exercise are associated with depressive symptoms, 2 , 5 , 6 , 28 the young age of the present study's subjects and the small number of drinkers and smokers may have had an influence. In addition, because many of the subjects were young, healthy, and in good physical condition, any effects of obesity and lack of exercise may have been difficult to detect. Further studies are warranted to examine the complex interactions between unhealthy lifestyle habits, which showed no significant relationships in the present study, and the development of depressive symptoms.
The present study had several limitations. First, it used two main diagnostic symptoms to define depressive symptoms. As any previous history of depressive symptoms and other mental disorders was not evaluated, a further study using clinically diagnosed symptoms of depression would be required. Second, the validity and reliability of the questionnaire used for assessing lifestyle factors had not been evaluated. Therefore, to confirm the present findings, a different questionnaire or a more objective method will be necessary. Third, the study was conducted at a single university, albeit a large one, which may have introduced sampling bias in the attributes of the participants. To increase generalizability, further multicenter studies will be required. Fourth, in the present study, some participants were not included in the 2‐year follow‐up, and differed in background factors, such as age, and frequency of drinking and smoking, compared with those included in the follow‐up. This may have caused additional sampling bias. Fifth, participants with a history of previous depressive symptoms, or who experienced depressive symptoms between the two surveys but had recovered by the time of the follow‐up survey, may not have been recognized in this study. Sixth, questions on sociodemographic factors, such as separation from friends, staying in school, and the death of a parent, were not included in the questionnaire. These factors may have an influence on depressive symptoms. Questionnaires used in future studies of unhealthy lifestyle factors and depression will need to include items on the above points for improvement of validity.
CONCLUSION
In conclusion, the present study of Japanese university students has demonstrated that poor satisfaction with sleep is associated with the development of depressive symptoms 2 years later. Our results suggest that promotion of a healthy lifestyle focusing on improved sleep may be important for the treatment and prevention of depressive symptoms among university students.
AUTHOR CONTRIBUTIONS
All authors contributed to and have approved the final manuscript. Ryuji Furihata, Mami Ishida, Yukako Nakagami, Maya Yanase, Teruhisa Uwatoko, Satoe Okabayashi, Kosuke Kiyohara and Takashi Kawamura contributed to study design, data collection, data interpretation, and preparation of the manuscript. Ryuji Furihata performed the statistical data analyses.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS APPROVAL STATEMENT
The study was approved by the Institutional Review Board of the Kyoto University Ethics Committee (R1732‐1).
PATIENT CONSENT STATEMENT
All analyses and procedures were anonymized. As de‐identified clinical data were employed in accordance with Japanese ethical guidelines, the need for individual informed consent was waived.
CLINICAL TRIAL REGISTRATION
N/A.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
We would like to thank Douglas Scientific Editing Services for English‐language editing. R.F. was supported by JSPS KAKENHI Grant Numbers 20K07967 and 22H03412.
Furihata R, Ishida M, Nakagami Y, Yanase M, Uwatoko T, Okabayashi S, et al. A 2‐year longitudinal study of the association between unhealthy lifestyle factors and the development of depressive symptoms in university students. Psychiatry Clin Neurosci Rep. 2024;3:e70020. 10.1002/pcn5.70020
DATA AVAILABILITY STATEMENT
N/A.
REFERENCES
- 1. Tabor E, Patalay P, Bann D. Mental health in higher education students and non‐students: evidence from a nationally representative panel study. Soc Psychiatry Psychiatr Epidemiol. 2021;56:879–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Li W, Zhao Z, Chen D, Peng Y, Lu Z. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta‐analysis. J Child Psychol Psychiatry. 2022;63:1222–1230. [DOI] [PubMed] [Google Scholar]
- 3. Ebert DD, Buntrock C, Mortier P, Auerbach R, Weisel KK, Kessler RC, et al. Prediction of major depressive disorder onset in college students. Depress Anxiety. 2019;36:294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM‐5‐TR. Washington, DC: American Psychiatric Association; 2022. [Google Scholar]
- 5. Furihata R, Konno C, Suzuki M, Takahashi S, Kaneita Y, Ohida T, et al. Unhealthy lifestyle factors and depressive symptoms: a Japanese general adult population survey. J Affect Disord. 2018;234:156–161. [DOI] [PubMed] [Google Scholar]
- 6. Ishida M, Montagni I, Matsuzaki K, Shimamoto T, Cariou T, Kawamura T, et al. The association between depressive symptoms and self‐rated health among university students: a cross‐sectional study in France and Japan. BMC Psychiatry. 2020;20:549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wong VW‐H, Ho FY‐Y, Shi N‐K, Sarris J, Chung K‐F, Yeung W‐F. Lifestyle medicine for depression: a meta‐analysis of randomized controlled trials. J Affect Disord. 2021;284:203–216. [DOI] [PubMed] [Google Scholar]
- 8. Saha S, Okafor H, Biediger‐Friedman L, Behnke A. Association between diet and symptoms of anxiety and depression in college students: a systematic review. J Am Coll Health. 2023;71:1270–1280. [DOI] [PubMed] [Google Scholar]
- 9. Yan S, Jin Y, Oh Y, Choi Y. Effect of exercise on depression in university students: a meta‐analysis of randomized controlled trials. J Sports Med Phys Fitness. 2016;56:811–816. [PubMed] [Google Scholar]
- 10. Kiyohara K, Kawamura T, Kitamura T, Takahashi Y. The start of smoking and prior lifestyles among Japanese college students: a retrospective cohort study. Nicotine Tob Res. 2010;12:1043–1049. [DOI] [PubMed] [Google Scholar]
- 11. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self‐report version of PRIME‐MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. [DOI] [PubMed] [Google Scholar]
- 12. Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire‐2: validity of a two‐item depression screener. Med Care. 2003;41:1284–1292. [DOI] [PubMed] [Google Scholar]
- 13. Sheeran T, Reilly CF, Raue PJ, Weinberger MI, Pomerantz J, Bruce ML. The PHQ‐2 on OASIS‐C: a new resource for identifying geriatric depression among home health patients. Home Healthc Nurse. 2010;28:92–102 [DOI] [PMC free article] [PubMed] [Google Scholar]; quiz 102–104.
- 14. Idler EL, Benyamini Y. Self‐rated health and mortality: a review of twenty‐seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 15. Jaussent I, Bouyer J, Ancelin M‐L, Akbaraly T, Peres K, Ritchie K, et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep. 2011;34:1103–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Furihata R, Hall MH, Stone KL, Ancoli‐Israel S, Smagula SF, Cauley JA, et al. An Aggregate measure of sleep health is associated with prevalent and incident clinically significant depression symptoms among community‐dwelling older women. Sleep. 2017;40:zsw075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Maglione JE, Ancoli‐Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, et al. Subjective and objective sleep disturbance and longitudinal risk of depression in a cohort of older women. Sleep. 2014;37:1179–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 19. Buysse DJ. Sleep health: can we define it? Does it matter. Sleep. 2014;37:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Furihata R, Tateyama Y, Nakagami Y, Akahoshi T, Itani O, Kaneita Y, et al. The validity and reliability of the Japanese version of RU‐SATED. Sleep Med. 2022;91:109–114. [DOI] [PubMed] [Google Scholar]
- 21. Gadam S, Pattinson CL, Rossa KR, Soleimanloo SS, Moore J, Begum T, et al. Interventions to increase sleep duration in young people: a systematic review. Sleep Med Rev. 2023;70:101807. [DOI] [PubMed] [Google Scholar]
- 22. Gaskin CJ, Venegas Hargous C, Stephens LD, Nyam G, Brown V, Lander N, et al. Sleep behavioral outcomes of school‐based interventions for promoting sleep health in children and adolescents aged 5 to 18 years: a systematic review. Sleep Adv. 2024;5:zpae019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Furihata R, Shimamoto T, Makino Y, Kimata S, Tateyama Y, Okabayashi S, et al. Efficacy of sleep extension therapy using a remote support system in university students with increased social jetlag: a parallel, single‐blind, randomized controlled trial. Sleep Biol Rhythms. 2023;21:359–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Furihata R, Shimamoto T, Ikeda Y, Makino Y, Nakagami Y, Tateyama Y, et al. Efficacy of digital brief behavioral treatment for insomnia using a smartphone application in conjunction with light therapy in university students with insomnia symptoms with late chronotypes: a pilot randomized controlled trial. J Sleep Res. 2024:e14361. [DOI] [PubMed] [Google Scholar]
- 25. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta‐analyses of diagnoses and symptoms. Psychol Bull. 2017;143:783–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Östberg D, Nordin S. Three‐year prediction of depression and anxiety with a single self‐rated health item. J Ment Health. 2022;31:402–409. [DOI] [PubMed] [Google Scholar]
- 27. Chan LLY, van Schooten KS, Lord SR, Delbaere K, Brodie M. Short daily‐life walking bouts and poor self‐reported health predict the onset of depression in community‐dwelling older people: a 2‐year longitudinal cohort study. J Am Med Dir Assoc. 2022;23:1242–1247.e3. [DOI] [PubMed] [Google Scholar]
- 28. Fan Y, Wang D, Wang W, Chen H, Lin J, Lin W, et al. Depression, anxiety, and development of obesity from childhood to young adulthood in China. J Psychosom Res. 2024;185:111867. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
N/A.


