Abstract
Background
Access to care is a major challenge for patients with musculoskeletal disorders (MSKDs). Telemedicine is one of the solutions to improve access to care. However, initial remote diagnosis of MSKDs involves some challenges, such as the impossibility of touching the patient during the physical examination, which makes it more complex to obtain a valid diagnosis. No meta-analysis has been performed to date to synthesize evidence regarding the initial assessment including a physical evaluation using telemedicine to diagnose patients with MSKDs.
Objective
This study aims to appraise the evidence on diagnostic and treatment plan concordance between remote assessment using synchronous or asynchronous forms of telemedicine and usual in-person assessment for the initial evaluation of various MSKDs.
Methods
An electronic search was conducted up to August 2023 using terms related to telemedicine and assessment of MSKDs. Methodological quality of studies was assessed with the Quality Assessment of Diagnostic Accuracy Studies 2 tool. Random-effect model meta-analyses were performed. The Grading of Recommendations, Assessment, Development, and Evaluations framework was used to synthesize the quality and certainty of the evidence.
Results
A total of 23 concordance studies were eligible and included adult participants (N=1493) with various MSKDs. On the basis of high certainty, pooled κ and prevalence-adjusted and bias-adjusted κ for the diagnostic concordance between remote and in-person assessments of MSKDs were 0.80 (95% CI 0.72-0.89; 7 studies, 353 patients) and 0.83 (95% CI 0.76-0.89; 6 studies, 306 patients). On the basis of moderate certainty, pooled Gwet AC1 for treatment plan concordance between remote and in-person assessments of MSKDs was 0.90 (95% CI 0.80-0.99; 2 studies, 142 patients).
Conclusions
The diagnostic concordance for MSKDs is good to very good. Treatment plan concordance is probably good to excellent. Studies evaluating the accuracy to detect red and yellow flags as well as the potential increase in associated health care resources use, such as imaging tests, are needed.
Keywords: telemedicine, musculoskeletal diseases, physical examination, diagnosis, treatment, health care, telecare, meta-analysis, systematic review, telehealth, orthopedic, test, musculoskeletal disorder, MSKD, older adult, older adults, older person, older people, aging, musculoskeletal, mobile phone
Introduction
Background
Almost 1.7 billion people have a musculoskeletal disorder (MSKD) in the world [1]. MSKDs refer to disorders affecting muscles, bones, and joints, such as low back pain, osteoarthritis, or tendinopathy [2]. MSKDs can lead to pain, disability, and poor health-related quality of life, resulting in a significant burden to health care systems as well as to society [2-6]. Evidence shows that a valid diagnosis through a careful initial evaluation and prompt treatment are essential for MSKDs [2,7]. Recommendations for various MSKDs emphasize the importance of screening for signs and symptoms of underlying serious pathologies (red flags) and for psychological factors associated with a poorer prognosis (yellow flags) during the initial evaluation as well as conducting a physical examination that includes measurements of mobility, strength, and use of orthopedic tests [2,8].
Significant health inequalities exist between urban and low-density population areas in several countries, with rural populations having a higher rate of injury and a higher risk of chronic MSKDs [9-11]. These inequalities can partially be explained by difficulties in accessing primary and secondary care [12-14]. The COVID-19 pandemic exacerbated these difficulties, with nearly 1 in 5 individuals unable to access health care during the first year of the COVID-19 pandemic, and patients with MSKDs were more affected by these delays than other patient populations [6,15-17]. Access to care is a major challenge for patients with MSKDs as delays can negatively impact clinical outcomes, such as pain, disability, or quality of life, while also potentially exacerbating psychological distress [18].
Telemedicine has been shown to have many benefits for patients, health care systems, and society [19]. It is an interesting option for optimizing health care access by removing unnecessary hurdles, such as geographical location or for patients with impaired mobility [19-21]. Telemedicine first appeared under asynchronous forms where communication between parties was not happening in real time [22]. Asynchronous forms are still used today for communication between patients and health care providers via messaging systems (emails and instant SMS text messaging) or smartphone apps for follow-up or counselling [23]. Synchronous forms of telemedicine with phone calls and videoconferencing allow real-time interaction between parties [22]. The use of videoconferencing in telemedicine has been a major progress by allowing visual evaluation of movement, edema, or scars, for example, or to observe patient physical performance and function [24]. The use of telemedicine in high-income countries now mainly focuses on patient remote management or follow-ups of patients who have already been assessed in person [25]. Telemedicine is well implanted in medical specialties, such as radiology, dermatology, or psychiatry, but is not widely used in the MSKDs care pathways, particularly for the initial assessment of new patients where a diagnosis is required [25,26]. The use of telemedicine for MSKDs brings many challenges related to the geographical distancing of the patient and the health care provider [27-31]. The loss of physical contact during the physical examination and treatments raises questions among patients and clinicians about the relevance, safety, and effectiveness of remote care [27,30,31]. Patients and health care providers also express concerns about the quality of the therapeutic relationship when consultations are not conducted in person [27,28]. However, telemedicine offers advantages to patients and health care providers, such as better accessibility, greater flexibility, and the possibility to offer interventions that are adapted to a patient’s environment as the remote consultation will likely be in a person’s home [27].
Previous systematic reviews and meta-analyses have reported that remote patient follow-up management after an in-person initial evaluation is a valid alternative to usual in-person management and leads to similar benefits in clinical outcomes for various MSKDs, such as low back pain, neck pain, shoulder pain, or neurological conditions [32-35]. Previous systematic reviews focusing on synchronous remote initial assessment highlighted that most clinical measures remotely evaluated have a good concurrent validity and an excellent reliability [24,36]. Remote diagnoses were highly concordant with in-person diagnoses, but no meta-analysis was performed on these results, and these systematic reviews only included studies with physiotherapists as evaluators, excluding other health care providers who usually assess patients with MSKDs, such as orthopedic surgeons or primary care physicians [36]. As the diagnosis as well as the treatment plan are key elements of an initial assessment, it is crucial to undertake a comprehensive appraisal, including a meta-analysis of the concordance between remote and in-person assessment for new patients with MSKDs.
Objective
This systematic review with meta-analysis aimed to appraise the available evidence on diagnosis and care concordance after an initial assessment between a remote evaluation and an in-person evaluation for the evaluation of various MSKDs.
Therefore, the research question for this systematic review was as follows: Can a complete, valid, and safe assessment be carried out using asynchronous, synchronous or both forms of telehealth to diagnose various MSKDs?
Methods
Protocol, Registration, and Deviation
The protocol of this systematic review has been registered on PROSPERO (CRD42022335606) [37]. A total of 2 deviations from the protocol have occurred and are as follows: (1) We now only present results for the first specific objective (concordance of diagnosis and management) in this publication, as there were too much data concerning the second objective (concordance of clinical measures) to be presented in 1 publication (data concerning the second objective will be presented in a second publication); (2) We have now added the calculation of prediction intervals to further assess the heterogeneity of the pooled estimates in addition to the I2 and τ² statistics.
Literature Search
An electronic search was conducted in 4 databases (MEDLINE, Embase, Cochrane Central, and CINAHL) from January 2000 to August 2023 using terms related to telemedicine by any type of health care providers (physicians, orthopedic surgeons, physiotherapists, or other providers), MSKDs, and the assessment or the clinical examination of these conditions. A trained librarian was consulted during the development of our research strategy. We chose to limit our search to the last 2 decades to identify technologies still in use and readily available to clinicians. The full search strategy is available in the Multimedia Appendix 1. Reference lists of identified published studies and previous systematic reviews were checked for any additional studies.
Study Selection
A pair of reviewers (RV and MC or AAC) independently reviewed titles and abstracts to identify studies of interest. Consensus from reviewers was required to include studies. A third reviewer (SL) was available if a consensus was not achieved by the 2 initial reviewers. Textbox 1 shows the inclusion criteria for articles.
Inclusion criteria for eligible studies.
Inclusion criteria
Participants with symptoms related to suspected musculoskeletal disorders.
Participants assessed during a remote evaluation (synchronous or asynchronous) and compared with an in-person evaluation by any health care provider.
Any type of diagnostic, care or treatment plan concordance outcomes (such as raw agreement, κ, prevalence-adjusted and bias-adjusted κ, or other concordance coefficients).
Technologies used for the remote assessment had to be accessible for routine clinical use (no experimental setup and no use of sensors to be placed on the participants).
Full-article or conference abstracts written in French or English.
Data Extraction
Data of included studies were extracted using a predefined standardized form documenting the following: authors’ names, year of publication, study design, country, care settings, characteristics of the remote assessment (modality and technology used as well as the presence of a third party to help with patient evaluation), body region or regions affected, number of participants, participant characteristics, health care provider characteristics, and outcome measures. Data extraction was performed by 1 evaluator (RV), and the extracted data were reviewed and verified by a second evaluator (MC or AAC). When data were missing or incomplete, attempts to contact original authors were made to obtain complete data and results.
Methodological Quality Assessment
Methodological quality of included studies was assessed with the valid and reliable Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool [38]. This tool appraises patient selection, index tests, reference standard, flow, and timing. QUADAS-2 also assesses the presence of applicability concerns that would decrease the external validity of the study results. Assessment of methodological quality and applicability concerns was performed by a pair of independent evaluators (RV and MC or SL or AAC or Claudia Cosculluela); the final score was obtained through consensus. In case of disagreement, a third evaluator was available to facilitate consensus (MC or SL). Studies were considered at risk of bias if at least 1 item of the QUADAS-2 was evaluated at high risk of bias.
Data Synthesis
κ, prevalence-adjusted and bias-adjusted κ (PABAK), and Gwet AC1 coefficients were pooled into separate meta-analyses. Weighted means were calculated for raw agreement. Random-effect model meta-analyses were performed using the metafor package in RStudio Team (2020, Rstudio: Integrated Development for R. Rstudio) [39,40]. Secondary analyses for different modalities of delivery (asynchronous or synchronous) and for affected body regions were performed. Sensitivity analyses were also performed, including only studies with a low risk of bias (with no item ranked as high risk of bias on the QUADAS-2). Pooled concordance estimates were interpreted as follows: 0.00-0.20=weak, 0.21-0.40=slight, 0.41-0.60=moderate, 0.61-0.80=good, 0.81-0.90=very good, and 0.91-1.00=excellent agreement [41,42]. Coding scripts are available in Multimedia Appendix 2. For all meta-analyses, α levels were set at .05, and 95% CIs were calculated. Statistical heterogeneity was quantified and reported using the I2 and τ² statistics and interpreted according to the Cochrane methodology [43]. Prediction intervals were also calculated using the Comprehensive Meta-Analysis software (version 4.0; H.Biostat) to further assess the heterogeneity of the pooled estimates [44,45]. A narrative synthesis was performed for studies and outcomes not pooled in meta-analyses or for conference abstracts included in this review.
The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) framework was used for grading the quality and certainty of evidence and for formulating recommendations [46]. Level of evidence was interpreted as follows: very low certainty: the true effect is probably markedly different from the pooled estimated effect, low certainty: the true effect might be markedly different from the pooled estimated effect, moderate certainty: we believe that the true effect is probably close to the pooled estimated effect, and high certainty: we are very confident that the true effect is similar to the pooled estimated effect.
Results
Overview
After full-text review, 11 studies on in-person remote diagnostic concordance [42,47-56], 7 studies on in-person remote diagnostic and treatment plan concordance [41,57-62], and 3 studies on in-person remote treatment plan concordance [63-65] were included (Figure 1). No studies presented results on triage concordance of surgical candidates. A total of 2 conference abstracts were also included on in-person remote diagnostic concordance [66,67]. Reasons for exclusions are available in Multimedia Appendix 3. Full characteristics of the included studies are presented in Tables 1 and 2 and Table S1 in Multimedia Appendix 4.
Figure 1.
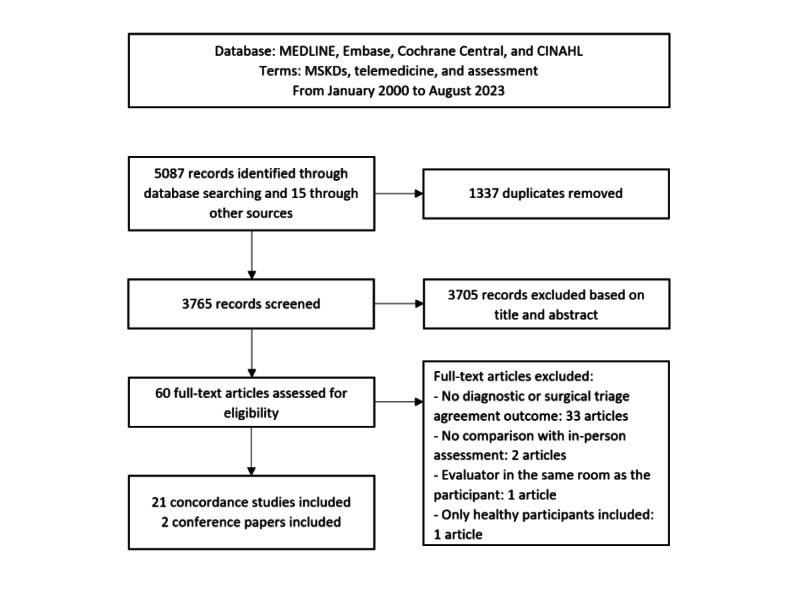
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for concordance studies selection.
Table 1.
Characteristics of the included studies (study settings).
| Author and year | Design | Country | Care setting | Modality of assessment | Technology |
| Abboud et al [57], 2005 | Prospective cohort | United States | Orthopedic | Asynchronous | Recorded photographs and data |
| Bovonratwet et al [58], 2022 | Retrospective cohort | United States | Orthopedic | Synchronous | Videoconferencing |
| Bradley et al [47], 2021 | Case control | United States | Orthopedic | Synchronous | Videoconferencing |
| Demaerschalk et al [48], 2022 | Retrospective cohort | United States | Clinic | Synchronous | Videoconferencing |
| Dias et al [56], 2023 | Prospective cohort | Brazil | Orthopedic | Synchronous | Videoconferencing |
| Exposto et al [42], 2022 | Prospective cohort | Denmark | Dentistry | Synchronous | Videoconferencing |
| Melnick et al [65], 2023 | Retrospective cohort | United States | Orthopedic | Synchronous | Videoconferencing |
| Michaelson et al [62], 2023 | Retrospective cohort | United States | Orthopedic | Synchronous | Videoconferencing with the presence of the patient’s caregiver |
| Rabin et al [61], 2022 | Prospective cohort | Israel | Orthopedic | Synchronous | Videoconferencing with presence of a research assistant or the patient’s caregiver |
| Tachakra et al [54], 2000 | Prospective cohort | United Kingdom | Emergency Department | Synchronous | Videoconferencing with presence of a nurse |
| Wang et al [55], 2022 | Prospective cohort | United States | Orthopedic | Asynchronous | Recorded video of a standardized clinical examination with presence of a research assistant |
| Cottrell et al [59], 2018 | Prospective cohort | Australia | Physiotherapy | Synchronous | Videoconferencing |
| Lade et al [49], 2012 | Prospective cohort | Australia | Physiotherapy | Synchronous | Videoconferencing |
| Lovo et al [41], 2022 | Prospective cohort | Canada | Rural clinic | Synchronous | Videoconferencing with presence of a nurse |
| Peterson et al [63], 2019 | Prospective cohort | United States | Physiotherapy | Synchronous | Videoconferencing |
| Richardson et al [50], 2017 | Prospective cohort | Australia | Physiotherapy | Synchronous | Videoconferencing |
| Russell et al [52], 2010 | Prospective cohort | Australia | Physiotherapy | Synchronous | Videoconferencing |
| Russell et al [51], 2010 | Prospective cohort | Australia | Physiotherapy | Synchronous | Videoconferencing |
| Steele et al [53], 2012 | Prospective cohort | Australia | Physiotherapy | Synchronous | Videoconferencing |
| Turner et al [60], 2019 | Prospective cohort | United Kingdom | Physiotherapy | Synchronous | Telephone |
| Worboys et al [64], 2018 | Prospective cohort | Australia | Occupational therapy | Synchronous | Videoconferencing with presence of an assistant |
Table 2.
Characteristics of the included studies (patient and evaluator characteristics).
| Author and year | Patients | Evaluators | Access to imaging tests to make diagnosis | ||||||
|
|
Musculoskeletal disorders (MSKDsa) | Values, n | Age (y), mean (SD) | Female (%) | Profession (number of evaluators) | Training |
|
||
| Abboud et al [57], 2005 | Upper extremity MSKDs | 100 | 43 (NRb) | 50 | Orthopedic surgeons (n=3) | NR | Yes | ||
| Bovonratwet et al [58], 2022 | Spine MSKDs | 65 | 57.5 (14.8) | 46 | Orthopedic surgeons (n=5) | NR | Yes | ||
| Bradley et al [47], 2021 | Shoulder MSKDs | 50 | 58.2 | 53 | Orthopedic surgeons (n=9) | NR | No | ||
| Demaerschalk et al [48], 2022 | MSKDs | 300 | NR | NR | Physicians, nurses, and physician assistants | NR | NR | ||
| Dias et al [56], 2023 | Low back pain | 122 | 47.8 (13.1) | 66 | Orthopedic surgeons (n=17) | NR | NR | ||
| Exposto et al [42], 2022 | Temporomandibular joint disorders | 15 | 31 (12) | 75 | Dentists (n=5) | 10 hours of training | NR | ||
| Melnick et al [65], 2023 | Spine MSKDs | 152 | 61.4 (15.4) | 43 | Orthopedic surgeons (n=7) | NR | NR | ||
| Michaelson et al [62], 2023 | Shoulder MSKDs | 82 | 52.6 (NR) | NR | Orthopedic surgeons (n=5) | NR | Yes | ||
| Rabin et al [61], 2022 | Shoulder MSKDs | 47 | 44.6 (22) | 36 | Orthopedic surgeons (n=2) | 4 hours of meeting and training with 5 pilot test participants | Yes | ||
| Tachakra et al [54], 2000 | Minor trauma injuries | 200 | NR | 31 | Emergency physician | NR | Yes | ||
| Wang et al [55], 2022 | Shoulder MSKDs | 32 | 50.2 (16.2) | 47 | Orthopedic surgeon (n=1) | NR | Yes | ||
| Cottrell et al [59], 2018 | Chronic MSKDs | 42 | 52.7 (14.5) | 57 | Advanced practice physiotherapists (n=6) | Training with 4 pilot test participants | Yes | ||
| Lade et al [49], 2012 | Elbow MSKDs | 10 | 38 (13) | 10 | Physiotherapy students (n=3) | Support by an experienced physiotherapist | NR | ||
| Lovo et al [41], 2022 | Chronic back pain | 27 | 53.7 (18.1) | 70 | Physiotherapists (n=2) and nurses (n=2) | Interprofessional training before the study | NR | ||
| Peterson et al [63], 2019 | Low back pain | 47 | 48.6 (15) | 70 | Physiotherapists (n=2) | NR | NR | ||
| Richardson et al [50], 2017 | Knee MSKDs | 18 | 23 (7) | 55 | Physiotherapists (n=3) | Training with 2 pilot test participants | NR | ||
| Russell et al [52], 2010 | Ankle MSKDs | 15 | 24.5 (10.8) | 67 | Physiotherapy students (n=3) | Training with 2 pilot test participants | NR | ||
| Russell et al [51], 2010 | Lower limb MSKDs (nonarticular) | 19 | 26 (13) | 74 | Physiotherapists (n=3) | Training with 2 pilot test participants | NR | ||
| Steele et al [53], 2012 | Shoulder MSKDs | 22 | 30.7 (14.2) | 27 | Physiotherapy students (n=3) | Support by an experienced physiotherapist | NR | ||
| Turner et al [60], 2019 | MSKDs | 55 | NR | NR | Physiotherapists (n=22) | NR | NR | ||
| Worboys et al [64], 2018 | Hand injuries | 18 | NR | 45 | Occupational therapists (n=4) | NR | NR | ||
aMSKD: musculoskeletal disorder.
bNR: not reported.
Countries and Clinical Settings
Studies were conducted in Australia (7/23, 30%), the United States (8/23, 35%), the United Kingdom (4/23, 17%), Denmark (1/23, 4%), Canada (1/23, 4%), Brazil (1/23, 4%), and Israel (1/23, 4%). In terms of care settings, studies were conducted in physiotherapy primary care clinics (8/23, 35%) [49-53,59,60,63], in orthopedic specialized care (8/23, 35%) [47,55-58,61,62,65], and in primary medical care (4/23, 17%) [41,48,66,67]; one study was conducted in an emergency department [54]. One study was concerning temporomandibular disorders in dentistry [42], and 1 study was conducted in an occupational therapy clinic [64]. Synchronous modalities were the most frequent way of contacting patients (21/23, 91%), with 18 (78%) of the 23 studies using a videoconferencing interface [41,42,47-56,58,59,61-63,65] and 3 (13%) using telephone calls [60,66,67]. Support staff was present to help with patient assessment and mobilization during the remote evaluation in 5 (22%) of the 23 studies [41,54,55,61,65]. Asynchronous modalities were used in 2 (8%) of the 23 studies, 1 using photographs of the patients [57] and 1 using video recordings of a self-performed clinical examination under the supervision of an assistant [55].
Participants
A total of 1849 participants were included. Mean age of participants was 49.6 (SD 14.9) years. Female gender accounted for 48% (887/1849) of the participants. Included participants had spinal disorders (703/1849, 38.02%), upper limb disorders (375/1849, 20.3%), lower limb disorders (201/1849, 10.9%), temporomandibular disorders (15/1849, 0.8%), and unspecified various MSKDs (555/1849, 30%). Of the 23 studies, 5 (22%) were conducted in university physiotherapy and dentistry clinics, which included a younger sample of patients and more acute or traumatic pathologies [42,50-53]. Other studies were conducted essentially in usual orthopedic and physiotherapy clinics and included broader samples with various MSKDs clinical representations.
Evaluators and Training
Evaluators were physiotherapists in 35% (8/23) of the studies, physiotherapy students in 13% (3/23) of the studies, or orthopedic surgeons in 35% (8/23) of the studies. Other health care providers involved were nurses, dentists, occupational therapists, and emergency and primary care physicians. In 7 (30%) of the 23 studies, evaluators received specific training on how to perform and adapt their remote assessment [41,42,50-52,59,61]. No information regarding specific training was available for the remaining studies [47,48,54-58,60,62-67]. Of the 23 studies, 3 (13%) involving physiotherapy students allowed them to be advised by a senior physiotherapist if they felt the need [49,52,53]. In 7 (30%) of the 23 studies, evaluators had access to participants’ imaging test results [54,55,57-59,61,62] while in 3 (13%) studies they did not [47,66,67]. No information regarding access to imaging results was available for the remaining studies.
Methodological Quality of Included Studies
Of the 21 studies, 3 (14%) had a perfect QUADAS-2 score [55-57]. A total Of the 21 studies, 11 (52%) had at least 1 item of the QUADAS-2 scored as a high a risk of bias [42,47,49,52-54,58,59,62,63,65] and 9 (43%) had at least 1 item of the QUADAS-2 score scored with an unclear risk of bias [41,48,49,51-54,58,61]. The main shortcomings concerned recruitment method or patient selection [50-52,58,59,61,63,64], the use of case-control study design [42,47], and the lack of blinding or validity of the evaluators’ diagnosis (diagnoses made by physiotherapy students with inconsistent supervision) [49,52-54,62,65]. Of the 9 (43%) had an applicability concern related to the representativeness of the sample of patients recruited [50-53,58,60,61,63,64]. A study had applicability concerns due to the choice of the index test and of the reference standard for the remote and in-person assessments because the remote and in-person assessments were conducted simultaneously [64]. Details are presented in Table 3.
Table 3.
Quality of the included concordance studies based on the Quality Assessment of Diagnostic Accuracy Studies 2 Tool.
| Author and year | Risk of bias | Applicability concerns | ||||||
|
|
Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard | |
| Abboud et al [57], 2005 | Low | Low | Low | Low | Low | Low | Low | |
| Dias et al [56], 2023 | Low | Low | Low | Low | Low | Low | Low | |
| Wang et al [55], 2022 | Low | Low | Low | Low | Low | Low | Low | |
| Bovonratwet et al [58], 2022 | Higha | Low | Unclear | Low | Higha | Low | Low | |
| Bradley et al [47], 2021 | Highb | Low | Low | Low | Low | Low | Low | |
| Cottrell et al [59], 2018 | Highc | Low | Low | Low | Low | Low | Low | |
| Demaerschalk et al [48], 2022 | Low | Low | Unclear | Low | Low | Low | Low | |
| Exposto et al [42], 2022 | Highb | Low | Low | Low | Low | Low | Low | |
| Lade et al [49], 2012 | Unclear | Low | Highd | Low | Low | Low | Low | |
| Lovo et al [41], 2022 | Unclear | Low | Low | Low | Low | Low | Low | |
| Melnick et al [65], 2023 | Low | Low | Highe | Low | Low | Low | Low | |
| Michaelson et al [62], 2023 | Low | Low | Highe | Unclear | Low | Unclear | Low | |
| Peterson et al [63], 2019 | Highf,g | Low | Low | Low | Highg | Low | Low | |
| Rabin et al [61], 2022 | Low | Unclear | Unclear | Low | Highh | Low | Low | |
| Richardson et al [50], 2017 | Low | Low | Low | Low | Highi | Low | Low | |
| Russell et al [52], 2010 | Unclear | Low | Highd | Low | Highi | Low | Low | |
| Russell et al [51], 2010 | Unclear | Low | Low | Low | Highi | Low | Low | |
| Steele et al [53], 2012 | Unclear | Low | Highd | Low | Highi | Low | Low | |
| Tachakra et al [54], 2022 | Unclear | Low | Highj | Low | Low | Low | Low | |
| Turner et al [60], 2019 | Low | Low | Low | Low | Unclear | Low | Low | |
| Worboys et al [64], 2018 | Low | Low | Low | Low | Highk | Highk | Highk | |
aPatients who did not have a specific diagnosis and treatment plan during the remote assessment were excluded, which could increase agreement by including only patients who could be easily assessed remotely.
bCase-control design was used in the study.
cOnly a convenience sampling was used for recruitment.
dAssessments were conducted by physiotherapy students, which could reduce the validity of the diagnoses made by evaluators.
eDuring the in-person assessment, evaluators had access to the treatment plan proposed after the remote assessment.
fOnly a convenience sampling was used for recruitment.
gPatients with surgical history of the lumbosacral spine, visible deformity, or no reproduction of symptoms with certain orthopedic tests were excluded.
hAlmost half of the patients (22/47, 47%) were evaluated during a postoperative or nonoperative follow-up consultation, which could increase agreement on diagnosis and treatment plan.
iThis cohort was composed of younger patients recruited in the university clinic with only acute or subacute injuries, without degenerative pathologies.
jThe same evaluator conducted the remote and in-person assessments.
kInitial assessments were excluded, and a third party was present with the patient to assist with data collection, which could have increased the agreement.
Diagnostic Concordance Between Remote and In-Person Assessments
Of the 23 studies, 17 (74%) reported diagnostic concordance results between in-person and remote assessments, and a study [62] reported diagnostic changes between in-person and remote assessments; the overall raw agreement was 85.9% (1352/1574 patients). Of the 23 studies, diagnostic concordance between in-person and remote assessments pooled estimations were possible for 7 (30%) studies for κ and 6 (26%) for PABAK estimates. The pooled estimates are presented in Figure 2. The pooled κ was 0.80 (95% CI 0.72-0.89; 7 studies, 353 patients), and the pooled PABAK was 0.83 (95% CI 0.76-0.89; 6 studies, 306 patients), corresponding to very good agreement between both types of assessments. Statistical heterogeneity measured with the I2 statistic were 65% and 38%, respectively, and considered potentially moderate for these meta-analyses. Prediction intervals for the pooled κ and PABAK were (0.52-0.92) and (0.68-0.91), which were very similar to the calculated CIs for the PABAK but not for the κ, and that difference could be attributed to the κ estimate in the study by Dias et al [56].
Figure 2.
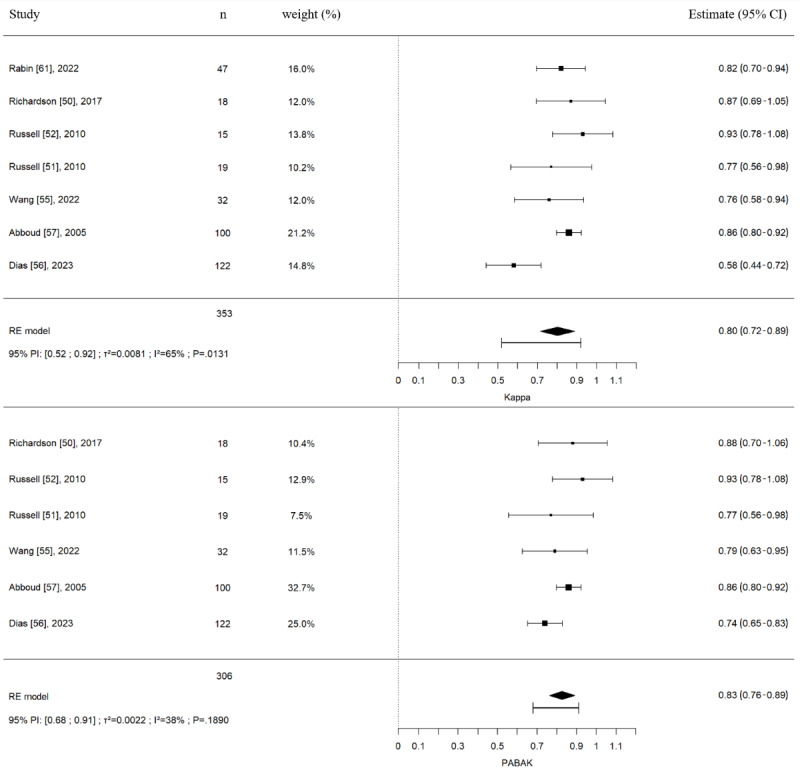
Diagnostic concordance (Cohen κs and prevalence-adjusted and bias-adjusted κs [PABAK]) between in-person and remote assessment in patients with musculoskeletal disorders. Meta-analysis with pooled Cohen κs included studies with physiotherapists (6/32, 19%), orthopedic surgeons (23/32, 72%), and physiotherapy students (3/32, 9%) as evaluators. Meta-analysis with pooled PABAKs included studies with physiotherapists (6/30, 33%), orthopedic surgeons (21/30, 50%) and physiotherapy students (3/30, 17%) as evaluators. 95% PI: 95% prediction interval; RE: random-effect model; τ2/I2/P: test for heterogeneity [50-52,55-57,61].
Another study could not be pooled in previous analyses as Fleiss κs were used to evaluate the agreement between in-person and remote assessments [42]. Diagnostic concordance between in-person and remote assessments for the study by Exposto et al [42] for patients with temporomandibular disorders reported Fleiss κs between 0.52 and 1.0, depending on the specific temporomandibular disorders (myalgia of the masseter or the temporalis muscles, temporomandibular arthralgia, or disk displacement with reduction).
Subgroup analyses were performed according to the presence or not of a third party to evaluate the participant during the remote evaluation (Figure S1 in Multimedia Appendix 4), profession of the health care providers (Figures S2 and S3 in Multimedia Appendix 4), body regions (Figures S2 and S4 in Multimedia Appendix 4), and asynchronous or synchronous evaluation forms of telemedicine used (Figures S5 and S6 in Multimedia Appendix 4). Similar results for diagnostic concordance were reported for all these subgroup analyses. For body regions, subgroup analyses were performed specific to upper and lower limb MSKDs. Analyses excluding high risk-of-bias studies (studies with a QUADAS-2 without items evaluated at high risk of bias) reported similar results for diagnostic concordance (Figure S7 in Multimedia Appendix 4).
Treatment Plan Concordance Between Remote and In-Person Assessments
Of the 23 studies, 8 (35%) reported treatment plan concordance outcomes between in-person and remote assessments and 2 (9%) [62,65] reported treatment plan changes between in-person and remote assessments. Overall raw agreement was 84% (406/483 patients). Treatment plan concordance between in-person and remote assessments pooled estimations were only possible for 2 (9%) of the 23 studies for Gwet AC1 coefficient estimates. The pooled estimates are presented in Figure 3. The pooled Gwet AC1 coefficient was 0.90 (95% CI 0.80-0.99; 2 studies, 142 patients), corresponding to a good to excellent agreement between both types of assessments. Statistical heterogeneity (I2=50%) was potentially moderate for this meta-analysis. Prediction intervals could not be calculated as this meta-analysis is based on only 2 studies.
Figure 3.
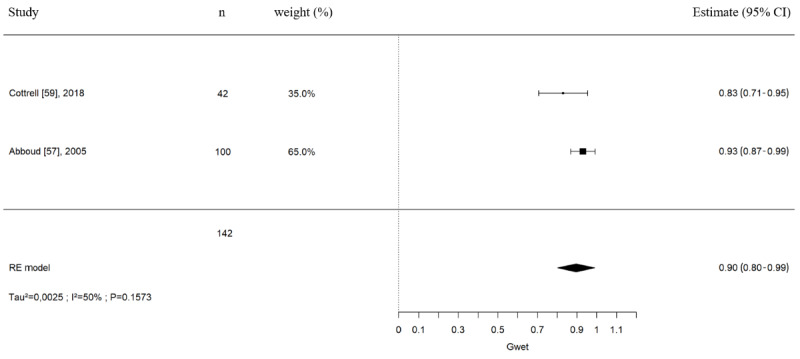
Treatment plan concordance (Gwet AC1 coefficients) between in-person and remote assessment in patients with musculoskeletal disorders. Meta-analysis with pooled Gwet AC1 coefficients included studies with advanced practice physiotherapists (6/9, 67%) and orthopedic surgeons (3/9, 33%). Gwet: Gwet AC1 coefficient; RE: random-effect model; τ2/I2/P: test for heterogeneity [57,59].
Of the 23 studies, 2 (9%) reporting κ estimates (2 studies, n=147) were not pooled together because of statistical heterogeneity (I2=94.79%). The first study by Abboud et al [57] compared the treatment plan concordance among 3 orthopedic surgeons for patients with upper limb MSKDs and reported an excellent agreement with a κ of 0.91 (95% CI 0.85-0.97; 100 patients). The other study by Rabin et al [61] compared the treatment plan concordance between 2 orthopedic surgeons for patients with shoulder pathologies. The authors reported only moderate agreement between remote and in-person proposed treatment plans with a κ of 0.43 (95% CI 0.22-0.64; 47 patients).
Another study was not pooled in these analyses as the evaluators were physiotherapists and had to choose among 3 physiotherapy treatments for low back pain patients (manipulation, specific exercises, or stabilization exercises). In the study by Peterson et al [63], the treatment plan concordance between in-person and remote assessments evaluated was only moderate with a κ of 0.52 (95% CI 0.32-0.72) and a PABAK of 0.52 (95% CI 0.31-0.72).
GRADE Analysis
Pooled results for diagnostic concordance were of high certainty, highlighting a good to very good concordance between remote and in-person assessments (Figure 4).
Figure 4.
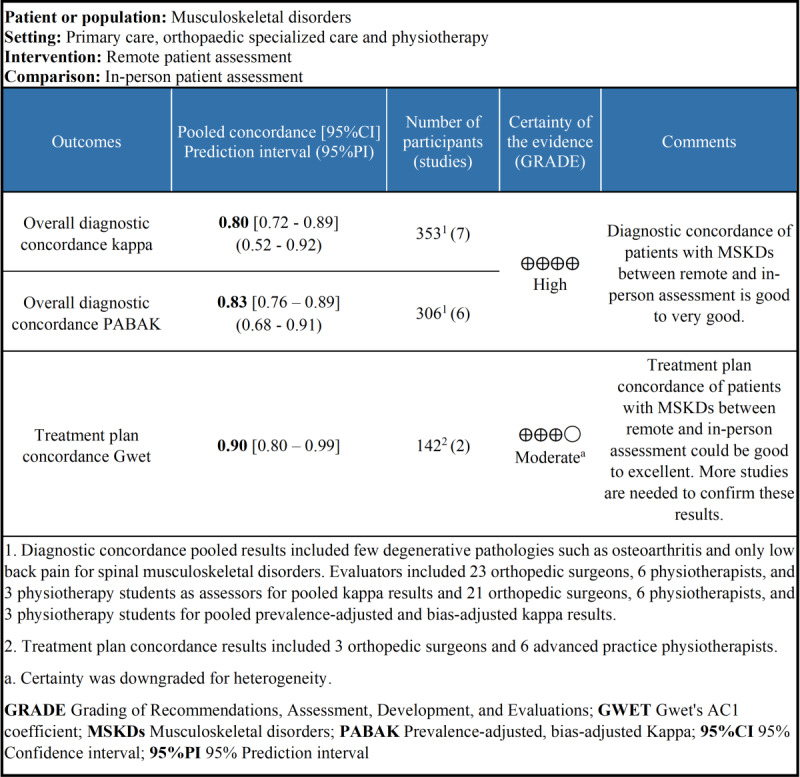
Summary of the findings and Grading of Recommendations, Assessment, Development, and Evaluations analysis for diagnostic and treatment plan concordance.
Pooled results for treatment plan concordance were of moderate certainty, highlighting a good to excellent concordance between remote and in-person assessments (Figure 4). The I2 was at 50%, and prediction intervals could not be calculated; therefore, certainty of the results was downgraded.
Discussion
Principal Findings
The aim of this systematic review and meta-analysis was to appraise the available evidence on diagnosis and care concordance after an initial assessment between a remote evaluation and an in-person evaluation for the initial evaluation of various MSKDs. On the basis of our results, health care providers can remotely make a diagnosis that is concordant with a usual in-person assessment. These results are robust and among various populations with acute or chronic MSKDs; we conducted several secondary analyses to assess the impact of various factors that may affect the validity and the feasibility of a remote assessment. Presence of assistance with the patient, body region being assessed, technologies used, and different health care providers’ profession did not appear to influence the accuracy of the remote assessment, but these findings need to be confirmed due to the limited number of studies in certain analyses. Sensitivity analyses, including only studies without high risk of bias and results from the study by Exposto et al [42], not pooled in the meta-analysis, yielded similar results. The study by Dias et al [56] reported a lower κ than the rest of the pooled studies but a similar raw agreement and PABAK (not calculated in the original paper but extracted and calculated by our team). The distribution of diagnoses in the study by Dias et al [56] shows a very high prevalence of some diagnostic categories and a very low prevalence of others. This imbalance may have biased and lowered the κ statistical value [68,69]. Overall concordance was found to be high in our review, but it may still vary across certain MSKDs, and our secondary analyses with fewer study and participants may not have been able to capture this issue. Moreover, studies on various spinal disorders, such as neck pain, or on degenerative pathologies, such as osteoarthritis, which were only marginally represented in the included studies, but very prevalent, are also needed.
Treatment plans proposed remotely had a good to excellent concordance with the treatment plans proposed in person. It may seem logical that if the remote diagnosis is correct, the treatment plan would be similar. However, there is uncertainty about these results because overall less data were available on the treatment plan in the literature; only 2 studies could be pooled and showed potentially moderate heterogeneity. Raw agreement between remote and in-person treatment plan was 84% (406/483 patients; 9 studies), which can be considered high. Again, these results are promising but need to be confirmed by more studies using statistical estimates to conclude on treatment plan concordance.
However, it should be kept in mind that an initial assessment is not only a diagnosis and a treatment plan. Some other key elements were not or could not have been properly evaluated with a remote assessment in several of the included studies. No data are available on the detection of serious pathologies (red flags) or the evaluation psychosocial risk factors (yellow flags) using a remote assessment [24]. Most red or yellow flags are identified during the subjective examination by elements of the patient’s history, specific questions, or questionnaires [8,70]. They may also be identifiable during a remote assessment by using the same screening procedure as during an in-person assessment. However, some tests used to rule out the presence of serious pathologies cannot be performed remotely, such as certain tests of the neurological examination, and patients may be less likely to talk about the psychosocial problems they are experiencing during a remote video or phone encounter. Among the studies we included, none reported having identified serious pathologies. However, given the small sample sizes of the studies and the low prevalence of serious conditions, it is unlikely that several patients with a serious condition were in the included samples [8]. Caution is therefore warranted when concluding that a remote assessment is as safe as traditional in-person assessment and that patients with important psychosocial risk factors are accurately identified. This is the first systematic review with meta-analyses addressing the agreement between remote and in-person diagnoses and treatment plan for MSKDs. Our results are consistent with previous reviews investigating the validity and reliability of different parts of a remote physical examination for MSKDs. Previous reviews have highlighted that most clinical measures assessed by videoconferencing applications, such as pain (visual analog scale) or range of motion assessment in patients with MSKDs, have good concurrent validity and excellent reliability [24,36]. Nevertheless, some measures, such as orthopedic tests, which are usually hands on, have lower concurrent validity and reliability when assessed remotely or simply cannot be performed [47]. Adaptations to the usual in-person physical examination in the musculoskeletal field still need to be developed to achieve validity and reliability comparable to in-person physical examination or to establish that the accuracy of a remote assessment is not as high [24,36,71]. Our results are complementary to other reviews with meta-analyses conducted on remote management of patients with MSKDs that show that remote care after an in-person assessment leads to similar improvements in clinical outcomes as the usual fully in-person approach [32-35]. Guidelines for MSKDs management now emphasize the importance of patient education and self-management as well as physical activity and exercise prescription [2]; all these interventions can be performed remotely [72,73]. In conjunction with our conclusions, the actual body of evidence on remote patient follow-up and clinical measures as well as recommended interventions for MSKDs potentially support the benefits of full remote care pathways for patients with MSKDs.
As stated earlier, more evidence is still needed on the impact of remote assessment for MSKDs. Future studies should also focus on the potential impacts of an initial remote evaluation on health care resources use, such as the use of imaging and other paraclinical investigations, as telemedicine could increase their use. Clinicians and patients express doubts on the validity and safety of a complete remote evaluation because of the impossibility of a hands-on assessment [29,74-76]. This uncertainty induced by the use of telemedicine could increase their use to confirm their diagnosis. There could also be an impact on follow-up visits and referrals to other health care providers and on modification of the relationship between the health care provider and the patient (therapeutic alliance) due to a first video or phone encounter. Telemedicine being an evolution in professional practices, quality standards and proper training of health care providers as well as the integration into the curriculum for trainees must also be anticipated to ensure the quality of remote care and promote the integration of telehealth [28,77,78]. Moreover, digital innovations, such as tools for clinical decision-making aids and improvements in information communication technologies, could compensate for the loss of hands-on assessment and could promote the acceptability of telemedicine by providing additional tools to help clinicians with evaluations and treatments [79-81].
Particular attention should as well be focused on the implementation of telemedicine that does not exclude populations, particularly in rural areas and low-income populations that may be affected by inequalities in access to information and communication technologies, such as access to reliable high-speed internet connections [82]. It is important to develop remote assessment methods using devices available to the public (smartphone and tablet) in contexts similar to clinical reality and not to neglect research of alternatives for populations without access to a high-speed internet connection, such as assessment by phone [60,66,67].
Strengths and Limitations
Strengths of this review include the use of 4 major bibliographical databases, a comprehensive search strategy, the use of the validated QUADAS-2 score to assess methodological quality of included studies, and the use of the Grading of Recommendations, Assessment, Development and Evaluations approach to rate the certainty of the evidence. Prediction intervals were used to assess the impact of the heterogeneity on the results [45]. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were followed to ensure a robust review methodology [83]. Furthermore, this study is one of the first meta-analyses to pool concordance outcomes using novel validated statistical approaches [40,84].
However, some limitations should be highlighted. The presence of publication bias could not be assessed because there were <10 studies to conduct a funnel plot [85]. Our results highlighted that the accuracy of remote diagnoses was not influenced by the type of health care provider or the body region involved. However, the studies pooled in the meta-analyses included only orthopedic surgeons or physiotherapists to evaluate mostly adults with peripheral MSKDs. The accuracy of remote diagnoses made by other health care providers or in different clinical settings, such as rheumatology, or for spinal disorders, such as neck pain, could be different. Moreover, the included studies were carried out in experimental settings, which could overestimate the accuracy of the diagnoses compared to real-life conditions when participants are at home and not in a medical environment. Most of the studies (3/6, 50%) included in the meta-analyses used technologies developed specifically for telemedicine, ensuring an optimal quality of exchange between the evaluator and the participant. The limited number of studies included for treatment plans should also be highlighted. Therefore, more methodologically sound studies with larger sample size are needed.
Conclusions
Health care providers can remotely make a diagnosis that is concordant with a usual in-person assessment for various MSKDs. Diagnostic concordance between remote and in-person assessments is good to very good, and future studies are unlikely to modify this conclusion. Type of health care provider, body region, technology used, and the presence of assistance with the patient do not seem to influence the accuracy of remote diagnoses, but more studies are needed to confirm the impact of such factors. Health care providers offer treatment plans that are consistent with those usually proposed in person. Treatment plan concordance between remote and in-person assessments is probably good to excellent, but future studies may modify these conclusions. There are still some considerations, such as the economic impact, modification of therapeutic alliance between health care provider and patient, or detection of serious pathologies and psychosocial risk factors, to investigate to fully appraise the challenges and benefits of the initial remote evaluation for patients with MSKDs. This systematic review with meta-analysis adds support for further development of hybrid or fully remote care pathways for patients with MSKDs to facilitate access to musculoskeletal care.
Acknowledgments
The authors would like to express their gratitude to James M Gregory, Yuri Martins Costa, and Seth Peterson for sharing their data to perform the required analyses and to Claudia Cosculluela for her participation in the risk-of-bias analysis. FD is an Fonds de Recherche du Québéc-Santé FRQ-S Senior Scholar, DK is an Fonds de Recherche du Québéc-Santé Junior-2 Scholar and RV is supported by PhD scholarships from the Faculté de médecine de l’Université de Montréal, the École de réadaptation de l’Université de Montréal, and the Réseau provincial de recherche en adaptation-réadaptation.
Abbreviations
- GRADE
Grading of Recommendations, Assessment, Development, and Evaluations
- MSKD
musculoskeletal disorder
- PABAK
prevalence-adjusted and bias-adjusted κ
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QUADAS-2
Quality Assessment of Diagnostic Accuracy Studies 2
Search strategy.
Codes used in RStudio.
Manuscripts excluded with reasons.
Supplementary materials (characteristics of conference abstracts and subgroup analyses).
PRISMA 2020 checklist.
Data Availability
All analyses are available in Multimedia Appendix 4. The data sets generated during and analyzed during this study are available from the corresponding author on reasonable request.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2021 Dec 19;396(10267):2006–17. doi: 10.1016/S0140-6736(20)32340-0. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(20)32340-0 .S0140-6736(20)32340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, Straker L, Maher CG, O'Sullivan PP. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020 Jan 02;54(2):79–86. doi: 10.1136/bjsports-2018-099878.bjsports-2018-099878 [DOI] [PubMed] [Google Scholar]
- 3.Safiri S, Kolahi AA, Cross M, Hill C, Smith E, Carson-Chahhoud K, Mansournia MA, Almasi-Hashiani A, Ashrafi-Asgarabad A, Kaufman J, Sepidarkish M, Shakouri SK, Hoy D, Woolf AD, March L, Collins G, Buchbinder R. Prevalence, deaths, and disability-adjusted life years due to musculoskeletal disorders for 195 countries and territories 1990-2017. Arthritis Rheumatol. 2021 Apr;73(4):702–14. doi: 10.1002/art.41571. doi: 10.1002/art.41571. [DOI] [PubMed] [Google Scholar]
- 4.Briggs AM, Cross MJ, Hoy DG, Sànchez-Riera L, Blyth FM, Woolf AD, March L. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization world report on ageing and health. Gerontologist. 2016 Apr 18;56 Suppl 2(Suppl 2):S243–55. doi: 10.1093/geront/gnw002.gnw002 [DOI] [PubMed] [Google Scholar]
- 5.Bevan S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract Res Clin Rheumatol. 2015 Jun;29(3):356–73. doi: 10.1016/j.berh.2015.08.002.S1521-6942(15)00094-7 [DOI] [PubMed] [Google Scholar]
- 6.Moir M, Barua b. Waiting your turn: wait times for health care in Canada, 2021 report. Fraser Institute. 2021. Dec 15, [2023-08-23]. https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2021 .
- 7.Ojha HA, Wyrsta NJ, Davenport TE, Egan WE, Gellhorn AC. Timing of physical therapy initiation for nonsurgical management of musculoskeletal disorders and effects on patient outcomes: a systematic review. J Orthop Sports Phys Ther. 2016 Feb;46(2):56–70. doi: 10.2519/jospt.2016.6138. [DOI] [PubMed] [Google Scholar]
- 8.Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL, Beneciuk JM, Leech RL, Selfe J. International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Ther. 2020 Jul;50(7):350–72. doi: 10.2519/jospt.2020.9971. [DOI] [PubMed] [Google Scholar]
- 9.Grimmer K, Bowman P. Differences between metropolitan and country public hospital allied health services. Aust J Rural Health. 1998 Nov;6(4):181–8. doi: 10.1111/j.1440-1584.1998.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 10.Bath B, Trask C, McCrosky J, Lawson J. A biopsychosocial profile of adult Canadians with and without chronic back disorders: a population-based analysis of the 2009-2010 Canadian Community Health Surveys. Biomed Res Int. 2014;2014:919621. doi: 10.1155/2014/919621. doi: 10.1155/2014/919621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.How healthy are rural Canadians? : an assessment of their health status and health determinants. Canadian Institute for Health Information. 2006. [2023-08-23]. https://secure.cihi.ca/free_products/rural_canadians_2006_report_e.pdf .
- 12.Ono T, Schoenstein M, Buchan J. Geographic imbalances in doctor supply and policy responses. Organisation for Economic Cooperation and Development. 2014. Apr 3, [2023-08-23]. https://www.oecd-ilibrary.org/social-issues-migration-health/geographic-imbalances-in-doctor-supply-and-policy-responses_5jz5sq5ls1wl-en .
- 13.Huguet M. Centralization of care in high volume hospitals and inequalities in access to care. Soc Sci Med. 2020 Sep;260:113177. doi: 10.1016/j.socscimed.2020.113177. doi: 10.1016/j.socscimed.2020.113177.S0277-9536(20)30396-8 [DOI] [PubMed] [Google Scholar]
- 14.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004 Oct;94(10):1682–6. doi: 10.2105/ajph.94.10.1682.94/10/1682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health at a glance: Europe 2022. Organisation for Economic Co-operation and Development. 2022. Dec 5, [2023-08-23]. https://www.oecd.org/en/publications/health-at-a-glance-europe-2022_507433b0-en.html .
- 16.Enquête sur l'accès aux soins de santé et aux produits pharmaceutiques pendant la pandémie (EASSPPP) Statistics Canada. 2021. Jun 2, [2023-08-23]. https://www.statcan.gc.ca/fr/enquete/menages/5346 .
- 17.Pujolar G, Oliver-Anglès A, Vargas I, Vázquez ML. Changes in access to health services during the COVID-19 pandemic: a scoping review. Int J Environ Res Public Health. 2022 Feb 03;19(3):1749. doi: 10.3390/ijerph19031749. https://www.mdpi.com/resolver?pii=ijerph19031749 .ijerph19031749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deslauriers S, Déry J, Proulx K, Laliberté M, Desmeules F, Feldman DE, Perreault K. Effects of waiting for outpatient physiotherapy services in persons with musculoskeletal disorders: a systematic review. Disabil Rehabil. 2021 Mar 14;43(5):611–20. doi: 10.1080/09638288.2019.1639222. [DOI] [PubMed] [Google Scholar]
- 19.Report of the WCPT/INPTRA digital physical therapy practice task force. International Network of Physiotherapy Regulatory Authorities. 2019. May 15, [2023-08-23]. https://www.med.unc.edu/healthsciences/physical/schoolbasedpt/wp-content/uploads/sites/662/2020/04/WCPTINPTRA_DigitalPTPractice.pdf .
- 20.Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016 Jan 14;79(1-2):169–76. doi: 10.1038/pr.2015.192. http://paperpile.com/b/vyHST5/VFvju .pr2015192 [DOI] [PubMed] [Google Scholar]
- 21.Moffatt JD, Eley DS. The reported benefits of telehealth for rural Australians. Aust Health Rev. 2010 Aug 25;34(3):276–81. doi: 10.1071/AH09794. doi: 10.1071/AH09794. [DOI] [PubMed] [Google Scholar]
- 22.Jagarapu JR, Savani RC. A brief history of telemedicine and the evolution of teleneonatology. Semin Perinatol. 2021 Aug;45(5):151416. doi: 10.1016/j.semperi.2021.151416. doi: 10.1016/j.semperi.2021.151416.S0146-0005(21)00029-X [DOI] [PubMed] [Google Scholar]
- 23.Ganjali R, Jajroudi M, Kheirdoust A, Darroudi A, Alnattah A. Telemedicine solutions for clinical care delivery during COVID-19 pandemic: a scoping review. Front Public Health. 2022 Jul 22;10:937207. doi: 10.3389/fpubh.2022.937207. https://europepmc.org/abstract/MED/35937265 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mani S, Sharma S, Omar B, Paungmali A, Joseph L. Validity and reliability of internet-based physiotherapy assessment for musculoskeletal disorders: a systematic review. J Telemed Telecare. 2016 Mar 31;23(3):379–91. doi: 10.1177/1357633x16642369. [DOI] [PubMed] [Google Scholar]
- 25.WHO Global Observatory for eHealth Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. World Health Organization. 2010. [2023-08-23]. https://iris.who.int/handle/10665/44497 .
- 26.El Aoufy K, Melis MR, Bellando Randone S, Blagojevic J, Bartoli F, Fiori G, Nacci F, Conforti ML, Cometi L, Bruni C, Orlandi M, Moggi-Pignone A, Rasero L, Guiducci S, Matucci-Cerinic M. The positive side of the coin: Sars-Cov-2 pandemic has taught us how much telemedicine is useful as standard of care procedure in real life. Clin Rheumatol. 2022 Feb 05;41(2):573–9. doi: 10.1007/s10067-021-05975-2. https://europepmc.org/abstract/MED/34739619 .10.1007/s10067-021-05975-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farzad M, MacDermid J, Ferreira L, Szekeres M, Cuypers S, Shafiee E. A description of the barriers, facilitators, and experiences of hand therapists in providing remote (tele) rehabilitation: an interpretive description approach. J Hand Ther. 2023 Oct;36(4):805–16. doi: 10.1016/j.jht.2023.06.004.S0894-1130(23)00083-2 [DOI] [PubMed] [Google Scholar]
- 28.Rethorn ZD, Lee AC, Rethorn TJ. Connecting at the webside: rapid telehealth implementation for musculoskeletal clinicians. J Orthop Sports Phys Ther. 2021 Jan;51(1):8–11. doi: 10.2519/jospt.2021.9902. [DOI] [PubMed] [Google Scholar]
- 29.Renard M, Gaboury I, Michaud F, Tousignant M. The acceptability of two remote monitoring modalities for patients waiting for services in a physiotherapy outpatient clinic. Musculoskeletal Care. 2022 Sep;20(3):616–24. doi: 10.1002/msc.1622. doi: 10.1002/msc.1622. [DOI] [PubMed] [Google Scholar]
- 30.Malliaras P, Merolli M, Williams CM, Caneiro JP, Haines T, Barton C. 'It's not hands-on therapy, so it's very limited': telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021 Apr;52:102340. doi: 10.1016/j.msksp.2021.102340. https://europepmc.org/abstract/MED/33571900 .S2468-7812(21)00024-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rabanifar N, Hoseini MA, Abdi K. Exploring barriers to implementing telerehabilitation from experiences of managers, policymakers, and providers of rehabilitation services in Iran: a qualitative study. Med J Islam Repub Iran. 2022 Dec 22;36:157. doi: 10.47176/mjiri.36.157. https://europepmc.org/abstract/MED/36660003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cottrell MA, Galea OA, O'Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017 May 02;31(5):625–38. doi: 10.1177/0269215516645148.0269215516645148 [DOI] [PubMed] [Google Scholar]
- 33.Suso-Martí L, La Touche R, Herranz-Gómez A, Angulo-Díaz-Parreño S, Paris-Alemany A, Cuenca-Martínez F. Effectiveness of telerehabilitation in physical therapist practice: an umbrella and mapping review with meta-meta-analysis. Phys Ther. 2021 May 04;101(5):101. doi: 10.1093/ptj/pzab075. https://europepmc.org/abstract/MED/33611598 .6145901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gava V, Ribeiro LP, Barreto RP, Camargo PR. Effectiveness of physical therapy given by telerehabilitation on pain and disability of individuals with shoulder pain: a systematic review. Clin Rehabil. 2022 Jun 01;36(6):715–25. doi: 10.1177/02692155221083496. [DOI] [PubMed] [Google Scholar]
- 35.Krzyzaniak N, Cardona M, Peiris R, Michaleff ZA, Greenwood H, Clark J, Scott AM, Glasziou P. Telerehabilitation versus face-to-face rehabilitation in the management of musculoskeletal conditions: a systematic review and meta-analysis. Phys Ther Rev. 2023 Apr 12;28(2):71–87. doi: 10.1080/10833196.2023.2195214. [DOI] [Google Scholar]
- 36.Zischke C, Simas V, Hing W, Milne N, Spittle A, Pope R. The utility of physiotherapy assessments delivered by telehealth: a systematic review. J Glob Health. 2021 Dec 18;11:04072. doi: 10.7189/jogh.11.04072. https://europepmc.org/abstract/MED/34956637 .jogh-11-04072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vincent C, Lafrance S, Charron M, Kairy D, Desmeules F. Remote assessment and management of patients with musculoskeletal disorders: a systematic review with meta-analyses. PROSPERO. 2022. [2024-09-08]. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=335606 .
- 38.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011 Oct 18;155(8):529–36. doi: 10.7326/0003-4819-155-8-201110180-00009. https://www.acpjournals.org/doi/abs/10.7326/0003-4819-155-8-201110180-00009?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .155/8/529 [DOI] [PubMed] [Google Scholar]
- 39.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 40.Sun S. Meta-analysis of Cohen’s kappa. Health Serv Outcomes Res Method. 2011;11:145–63. doi: 10.1007/s10742-011-0077-3. [DOI] [Google Scholar]
- 41.Lovo S, Harrison L, O’Connell ME, Rotter T, Bath B. A physical therapist and nurse practitioner model of care for chronic back pain using telehealth: diagnostic and management concordance. J Telemed Telecare. 2022 May 12;30(5):842–50. doi: 10.1177/1357633x221098904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Exposto FG, Castrillon EE, Exposto CR, Costa DM, Gøkhan MA, Svensson P, Costa YM. Remote physical examination for temporomandibular disorders. Pain. 2022 May 01;163(5):936–42. doi: 10.1097/j.pain.0000000000002455.00006396-202205000-00019 [DOI] [PubMed] [Google Scholar]
- 43.Higgins JP, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions version 6.4. The Cochrane Collaboration. [2023-08-23]. https://training.cochrane.org/handbook .
- 44.Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I² is not an absolute measure of heterogeneity. Res Synth Methods. 2017 Mar;8(1):5–18. doi: 10.1002/jrsm.1230. [DOI] [PubMed] [Google Scholar]
- 45.IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016 Jul 12;6(7):e010247. doi: 10.1136/bmjopen-2015-010247. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=27406637 .bmjopen-2015-010247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 26;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. https://europepmc.org/abstract/MED/18436948 .336/7650/924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bradley KE, Cook C, Reinke EK, Vinson EN, Mather RC 3rd, Riboh J, Lassiter T, Wittstein JR. Comparison of the accuracy of telehealth examination versus clinical examination in the detection of shoulder pathology. J Shoulder Elbow Surg. 2021 May;30(5):1042–52. doi: 10.1016/j.jse.2020.08.016. https://europepmc.org/abstract/MED/32871264 .S1058-2746(20)30689-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demaerschalk BM, Pines A, Butterfield R, Haglin JM, Haddad TC, Yiannias J, Colby CE, TerKonda SP, Ommen SR, Bushman MS, Lokken TG, Blegen RN, Hoff MD, Coffey JD, Anthony GS, Zhang N. Assessment of clinician diagnostic concordance with video telemedicine in the integrated multispecialty practice at mayo clinic during the beginning of COVID-19 pandemic from March to June 2020. JAMA Netw Open. 2022 Sep 01;5(9):e2229958. doi: 10.1001/jamanetworkopen.2022.29958. https://europepmc.org/abstract/MED/36053531 .2795871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lade H, McKenzie S, Steele L, Russell TG. Validity and reliability of the assessment and diagnosis of musculoskeletal elbow disorders using telerehabilitation. J Telemed Telecare. 2012 Oct 19;18(7):413–8. doi: 10.1258/jtt.2012.120501.jtt.2012.120501 [DOI] [PubMed] [Google Scholar]
- 50.Richardson BR, Truter P, Blumke R, Russell TG. Physiotherapy assessment and diagnosis of musculoskeletal disorders of the knee via telerehabilitation. J Telemed Telecare. 2016 Jul 08;23(1):88–95. doi: 10.1177/1357633x15627237. [DOI] [PubMed] [Google Scholar]
- 51.Russell T, Truter P, Blumke R, Richardson B. The diagnostic accuracy of telerehabilitation for nonarticular lower-limb musculoskeletal disorders. Telemed J E Health. 2010 Jun;16(5):585–94. doi: 10.1089/tmj.2009.0163. [DOI] [PubMed] [Google Scholar]
- 52.Russell TG, Blumke R, Richardson B, Truter P. Telerehabilitation mediated physiotherapy assessment of ankle disorders. Physiother Res Int. 2010 Sep 17;15(3):167–75. doi: 10.1002/pri.471. [DOI] [PubMed] [Google Scholar]
- 53.Steele L, Lade H, McKenzie S, Russell TG. Assessment and diagnosis of musculoskeletal shoulder disorders over the internet. Int J Telemed Appl. 2012;2012:945745. doi: 10.1155/2012/945745. doi: 10.1155/2012/945745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tachakra S, Lynch M, Newson R, Stinson A, Sivakumar A, Hayes J, Bak J. A comparison of telemedicine with face-to-face consultations for trauma management. J Telemed Telecare. 2000 Dec 02;6 Suppl 1(1_suppl):S178–81. doi: 10.1258/1357633001934591. [DOI] [PubMed] [Google Scholar]
- 55.Wang G, Fiedler AK, Warth RJ, Bailey L, Shupe PG, Gregory JM. Reliability and accuracy of telemedicine-based shoulder examinations. J Shoulder Elbow Surg. 2022 Aug;31(8):e369–75. doi: 10.1016/j.jse.2022.04.005.S1058-2746(22)00432-3 [DOI] [PubMed] [Google Scholar]
- 56.Dias JM Jr, Mendes AF Jr, Pestana de Aguiar E, Silveira LC, Noel Dias MF, Barbosa Raposo NR. Interobserver agreement and satisfaction with the use of telemedicine for evaluating low back pain: a primary, observational, cross-sectional, analytical study. Global Spine J. 2023 Aug 16;:21925682231194453. doi: 10.1177/21925682231194453. (forthcoming) https://journals.sagepub.com/doi/10.1177/21925682231194453?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed. [DOI] [PubMed] [Google Scholar]
- 57.Abboud JA, Bozentka DJ, Beredjiklian PK. Telemedicine consultation for patients with upper extremity disorders is reliable. Clin Orthop Relat Res. 2005 Jun;435(435):250–7. doi: 10.1097/01.blo.0000155009.77961.5c.00003086-200506000-00036 [DOI] [PubMed] [Google Scholar]
- 58.Bovonratwet P, Song J, Kim YE, Shinn D, Morse KW, Dowdell JE, Huang RC, Albert TJ, Sandhu HS, Qureshi SA, Iyer S. Telemedicine visits can generate highly accurate diagnoses and surgical plans for spine patients. Spine (Phila Pa 1976) 2022 Sep 01;47(17):1194–202. doi: 10.1097/BRS.0000000000004387.00007632-202209010-00002 [DOI] [PubMed] [Google Scholar]
- 59.Cottrell MA, O'Leary SP, Swete-Kelly P, Elwell B, Hess S, Litchfield MA, McLoughlin I, Tweedy R, Raymer M, Hill AJ, Russell TG. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract. 2018 Dec;38:99–105. doi: 10.1016/j.msksp.2018.09.014.S2468-7812(18)30096-1 [DOI] [PubMed] [Google Scholar]
- 60.Turner D. An exploratory study of physiotherapy telephone assessment. Int J Therapy Rehab. 2009 Feb;16(2):97–105. doi: 10.12968/ijtr.2009.16.2.38897. [DOI] [Google Scholar]
- 61.Rabin A, Dolkart O, Kazum E, Wengier R, Goldstein Y, Maman E, Chechik O. Shoulder assessment by smartphone: a valid alternative for times of social distancing. Arch Orthop Trauma Surg. 2022 Jun 13;142(6):979–85. doi: 10.1007/s00402-021-03762-x. https://europepmc.org/abstract/MED/33439302 .10.1007/s00402-021-03762-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Michaelson EM, Wiesel BB, Siedlarz B, Murthi AM, Sethi PM, Lutton DM, Nagda SH. Accuracy of telemedicine for the diagnosis and treatment of patients with shoulder complaints. Curr Orthop Pract. 2023;34(3):112–6. doi: 10.1097/BCO.0000000000001199. [DOI] [Google Scholar]
- 63.Peterson S, Kuntz C, Roush J. Use of a modified treatment-based classification system for subgrouping patients with low back pain: agreement between telerehabilitation and face-to-face assessments. Physiother Theory Pract. 2019 Nov 03;35(11):1078–86. doi: 10.1080/09593985.2018.1470210. [DOI] [PubMed] [Google Scholar]
- 64.Worboys T, Brassington M, Ward EC, Cornwell PL. Delivering occupational therapy hand assessment and treatment sessions via telehealth. J Telemed Telecare. 2017 Feb 13;24(3):185–92. doi: 10.1177/1357633x17691861. [DOI] [PubMed] [Google Scholar]
- 65.Melnick K, Porche K, Sriram S, Goutnik M, Cuneo M, Murad G, Chalouhi N, Polifka A, Hoh DJ, Decker M. Evaluation of patients referred to the spine clinic via telemedicine and the impact on diagnosis and surgical decision-making. J Neurosurg Spine. 2023 Oct 01;39(4):600–6. doi: 10.3171/2023.5.SPINE23182. [DOI] [PubMed] [Google Scholar]
- 66.Higginson R, Hutchinson C. Diagnostic accuracy of knee pathologies by a telephone based Advanced Level Physiotherapy service. Physiotherapy. 2017 Dec;103(Supplement 1):e104. doi: 10.1016/j.physio.2017.11.080. [DOI] [Google Scholar]
- 67.Hutchinson C, Higginson R. The diagnostic accuracy of spinal pathologies referred for by a telephone based advanced level physiotherapy triage service. Physiotherapy. 2017 Dec;103(Supplement 1):e99. doi: 10.1016/j.physio.2017.11.072. [DOI] [Google Scholar]
- 68.Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol. 1993 May;46(5):423–9. doi: 10.1016/0895-4356(93)90018-V. doi: 10.1016/0895-4356(93)90018-V.0895-4356(93)90018-V [DOI] [PubMed] [Google Scholar]
- 69.Flight L, Julious SA. The disagreeable behaviour of the kappa statistic. Pharm Stat. 2015;14(1):74–8. doi: 10.1002/pst.1659. doi: 10.1002/pst.1659. [DOI] [PubMed] [Google Scholar]
- 70.Stearns ZR, Carvalho ML, Beneciuk JM, Lentz TA. Screening for yellow flags in orthopaedic physical therapy: a clinical framework. J Orthop Sports Phys Ther. 2021 Sep;51(9):459–69. doi: 10.2519/jospt.2021.10570. [DOI] [PubMed] [Google Scholar]
- 71.Lu AD, Veet CA, Aljundi O, Whitaker E, Smith WB 2nd, Smith JE. A systematic review of physical examination components adapted for telemedicine. Telemed J E Health. 2022 Dec 01;28(12):1764–85. doi: 10.1089/tmj.2021.0602. [DOI] [PubMed] [Google Scholar]
- 72.Kennedy CA, Warmington K, Flewelling C, Shupak R, Papachristos A, Jones C, Linton D, Beaton DE, Lineker S, Hogg-Johnson S. A prospective comparison of telemedicine versus in-person delivery of an interprofessional education program for adults with inflammatory arthritis. J Telemed Telecare. 2016 Jul 09;23(2):197–206. doi: 10.1177/1357633x16635342. [DOI] [PubMed] [Google Scholar]
- 73.van der Kolk NM, de Vries NM, Kessels RP, Joosten H, Zwinderman AH, Post B, Bloem BR. Effectiveness of home-based and remotely supervised aerobic exercise in Parkinson's disease: a double-blind, randomised controlled trial. Lancet Neurol. 2019 Nov;18(11):998–1008. doi: 10.1016/S1474-4422(19)30285-6.S1474-4422(19)30285-6 [DOI] [PubMed] [Google Scholar]
- 74.Cottrell MA, Hill AJ, O'Leary SP, Raymer ME, Russell TG. Patients are willing to use telehealth for the multidisciplinary management of chronic musculoskeletal conditions: a cross-sectional survey. J Telemed Telecare. 2018 Aug;24(7):445–52. doi: 10.1177/1357633X17706605. [DOI] [PubMed] [Google Scholar]
- 75.Kairy D, Tousignant M, Leclerc N, Côté AM, Levasseur M, The Telage Researchers The patient's perspective of in-home telerehabilitation physiotherapy services following total knee arthroplasty. Int J Environ Res Public Health. 2013 Aug 30;10(9):3998–4011. doi: 10.3390/ijerph10093998. https://www.mdpi.com/resolver?pii=ijerph10093998 .ijerph10093998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lawford BJ, Bennell KL, Kasza J, Hinman RS. Physical therapists' perceptions of telephone- and internet video-mediated service models for exercise management of people with osteoarthritis. Arthritis Care Res (Hoboken) 2018 Mar 29;70(3):398–408. doi: 10.1002/acr.23260. [DOI] [PubMed] [Google Scholar]
- 77.Davies L, Hinman RS, Russell T, Lawford B, Bennell K, International Videoconferencing Steering Group An international core capability framework for physiotherapists to deliver quality care via videoconferencing: a Delphi study. J Physiother. 2021 Oct;67(4):291–7. doi: 10.1016/j.jphys.2021.09.001. https://linkinghub.elsevier.com/retrieve/pii/S1836-9553(21)00099-0 .S1836-9553(21)00099-0 [DOI] [PubMed] [Google Scholar]
- 78.Munce S, Andreoli A, Bayley M, Guo M, Inness EL, Kua A, McIntyre M. Clinicians' experiences of implementing a telerehabilitation toolkit during the COVID-19 pandemic: qualitative descriptive study. JMIR Rehabil Assist Technol. 2023 Mar 10;10:e44591. doi: 10.2196/44591. https://rehab.jmir.org/2023//e44591/ v10i1e44591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lowe C, Browne M, Marsh W, Morrissey D. Usability testing of a digital assessment routing tool for musculoskeletal disorders: iterative, convergent mixed methods study. J Med Internet Res. 2022 Aug 30;24(8):e38352. doi: 10.2196/38352. https://www.jmir.org/2022/8/e38352/ v24i8e38352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lervik LC, Vasseljen O, Austad B, Bach K, Bones AF, Granviken F, Hill JC, Jørgensen P, Øien T, Veites PM, Van der Windt DA, Meisingset I. SupportPrim-a computerized clinical decision support system for stratified care for patients with musculoskeletal pain complaints in general practice: study protocol for a randomized controlled trial. Trials. 2023 Apr 11;24(1):267. doi: 10.1186/s13063-023-07272-6. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-023-07272-6 .10.1186/s13063-023-07272-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Létourneau D, Brière S, Maheux MA, Godin C, Warren P, Lauzier G, Joly IM, Bourque J, Arsenault P, Vilanova C, Tousignant M, Michaud F. OpenTera: a framework for telehealth applications. J Open Source Softw. 2023 Nov;8(91):5497. doi: 10.21105/joss.05497. [DOI] [Google Scholar]
- 82.The state of broadband 2020: tackling digital inequalities. International Telecommunication Union and United Nations Educational, Scientific and Cultural Organization. 2020. Sep, [2023-08-23]. https://www.itu.int/dms_pub/itu-s/opb/pol/S-POL-BROADBAND.21-2020-PDF-E.pdf .
- 83.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lafrance S, Vincent R, Demont A, Charron M, Desmeules F. Advanced practice physiotherapists can diagnose and triage patients with musculoskeletal disorders while providing effective care: a systematic review. J Physiother. 2023 Oct;69(4):220–31. doi: 10.1016/j.jphys.2023.08.005. https://linkinghub.elsevier.com/retrieve/pii/S1836-9553(23)00081-4 .S1836-9553(23)00081-4 [DOI] [PubMed] [Google Scholar]
- 85.Page MJ, Higgins JP, Sterne JA. Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. London, UK: The Cochrane Collaboration; 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy.
Codes used in RStudio.
Manuscripts excluded with reasons.
Supplementary materials (characteristics of conference abstracts and subgroup analyses).
PRISMA 2020 checklist.
Data Availability Statement
All analyses are available in Multimedia Appendix 4. The data sets generated during and analyzed during this study are available from the corresponding author on reasonable request.


