Abstract
Discharge planning is integral to patient flow as delays can lead to hospital-wide congestion. Because a structured discharge plan can reduce hospital length of stay while enhancing patient satisfaction, this topic has caught the interest of many healthcare professionals and researchers. Predicting discharge outcomes, such as destination and time, is crucial in discharge planning by helping healthcare providers anticipate patient needs and resource requirements. This article examines the literature on the prediction of various discharge outcomes. Our review discovered papers that explore the use of prediction models to forecast the time, volume, and destination of discharged patients. Of the 101 reviewed papers, 49.5% looked at the prediction with machine learning tools, and 50.5% focused on prediction with statistical methods. The fact that knowing discharge outcomes in advance affects operational, tactical, medical, and administrative aspects is a frequent theme in the papers studied. Furthermore, conducting system-wide optimization, predicting the time and destination of patients after discharge, and addressing the primary causes of discharge delay in the process are among the recommendations for further research in this field.
Keywords: Discharge planning, Discharge prediction, Machine learning, Literature review, Regression, LOS
Introduction
Healthcare demand and expenditures are increasing, putting pressure on healthcare systems [1]. Hospital operational and financial expenditures are affected by inpatient flow management. Effective patient flow involves preparing patients for each stage of care they require [2]. One of the most critical parts of inpatient flow is the process of patient discharge, often called Discharge Planning (DP). DP connects a patient’s hospital treatment and post-discharge care [3] and ensures continuity of care for patients when they leave the hospital.
Several studies have shown that a structured discharge plan may reduce hospital Length of Stay (LOS) and readmission rates while increasing patient satisfaction. Based on several studies, standard DP can improve patient outcomes including mortality/ survival rate [4–6], readmissions [5, 7–12], LOS [8, 12–14], and health-related quality of life [5, 8]. While there is little evidence that DP can lower healthcare expenditures [3, 15, 16], several studies indicate that proper DP results in cost savings for hospitals and the whole health system [17–20].
DP is a complicated procedure in hospitals that significantly impacts the entire healthcare system. As a result, numerous researchers have attempted to analyze this process, the causes of discharge delays, and its implications on the healthcare system. Several studies help this process by applying different methods to improve outcomes for both the system and the patients. They use approaches from the process improvement field, such as standardization of DP processes [16, 21–23], re-engineering of processes [24], applying knowledge management [25, 26], lean approaches [20, 27–31], and data analysis and quality assessment [32, 33] to examine the effectiveness of DP for patients moving from the hospital.
Combining patient-level data from Electronic Health Records (EHR) with advanced predictive tools can provide visibility into patient flow and discharge to help hospitals run more efficiently. Machine learning (ML) algorithms are effective in processing large amounts of data and provide a way to forecast the patients’ discharge elements in a timely, systematic, and accurate manner. With the growth in data analysis methods, several studies utilized different ML models to predict the discharge volume [34, 35], time [36, 37], and destination [38, 39]. These and other recent studies have looked into predicting the time and destination of discharged patients. However, we could not find a literature review article on this subject. This review article examines the prediction of discharge destination, which refers to where a patient is discharged (e.g., home, long-term care facilities), discharge time, which indicates when a patient is discharged (or LOS, which stands for the duration of a patient’s stay in a hospital). Additionally, it explores volume, which refers to the number of patient discharges in a fixed time period. These findings are reported in various sources, including journal articles, conference proceedings, grey literature, and books. Our discussion encompasses the evolution and contributions of developed methodologies in this field and summarizes the literature on discharge prediction.
The search strategy and identified articles are described in Section 2. Section 3 summarizes the use of predictive models in DP, including statistical-based and ML-based predictions. Section 4 summarizes the findings and recommends ways to improve DP and DP prediction in the future.
Search strategy
Papers that met at least one of the following criteria are included in this review. (1) They investigated the prediction of DP factors from a statistical analysis. (2) They investigated prediction in DP problems utilizing ML models. The databases used are Scopus, Web of Science, Google Scholar, and Medline/Pubmed search engine. The authors discovered a group of relevant journal articles through scoping searches. These articles were then reviewed by an information specialist to generate a list of search phrases that encompassed each aspect of the review criteria, which was used to prepare the list of search terms. Search keywords in the title are Patient discharge planning; Discharge plan; Patient discharge prediction; Discharge time prediction; Patient discharge destination; Patient post-discharge; Post-discharge + long-term care; Post-discharge + home. All searches were carried out in August 2023, with a restriction on English-language publications and a period of 2002 to 2022.
Search results
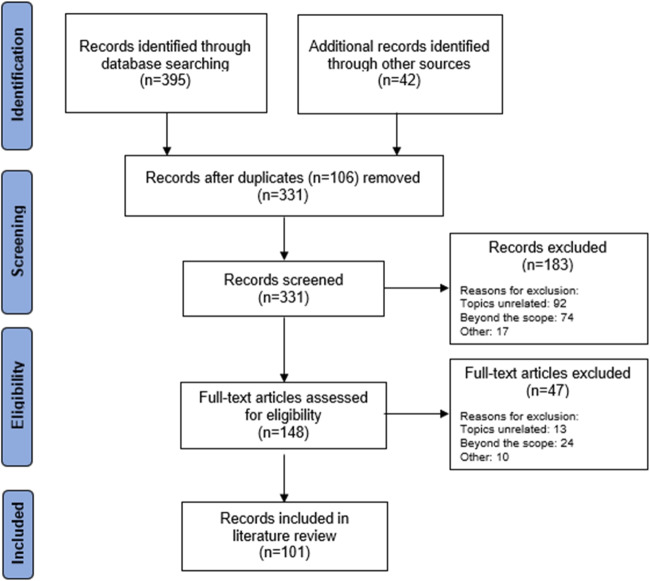
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [40, 41] were followed in reviewing the papers. The search yielded a total of 437 studies, of which 106 were identified as duplicates, ultimately leaving 331 distinct papers. Articles that did not match the criteria based on their title and abstract were disregarded. The complete texts of the remaining articles were reviewed. 101 publications met one or both evaluation criteria (see Fig. 1).
Fig. 1.
Literature search and screening flowchart
Classification of results
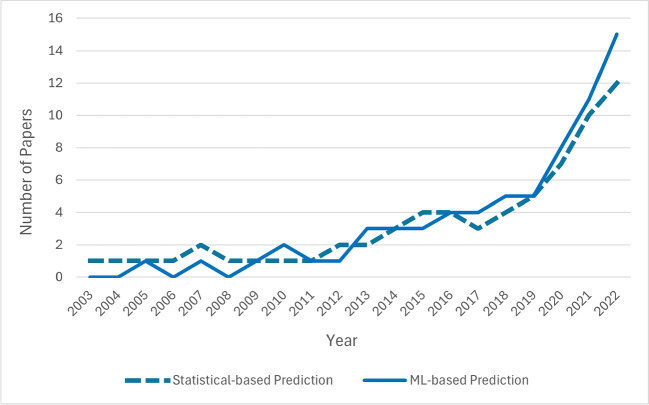
To demonstrate the breadth of this research area, we classified the articles into two categories based on their methodology. The objective of papers in both categories is the same: to predict the time or destination of patients after discharge. The first category of papers uses statistical methods (51 out of 101 papers), which is reviewed in Section 3.1. The second category of papers uses ML (50 out of 101 papers) and is reviewed in Section 3.2. The trends in these research areas are shown in Fig. 2, indicating the growing interest in understanding and improving the discharge process through prediction.
Fig. 2.
The trend of studies in discharge prediction during recent years
Predicting discharge
Prediction is a strong tool for decision-making, from inventory management to strategic management [42]. Discharge prediction aims to improve inpatient flow by giving decision-makers accurate information [43, 44]. Furthermore, forecasting different aspects of DP, such as LOS, discharge time, and discharge destination, helps healthcare providers make better decisions for the entire system [45, 46]. This section reviews articles that determine and predict discharge factors using statistical tools (Section 3.1) and studies that use ML-based methods (Section 3.2).
Statistical-based prediction
This subsection focuses on studies that analyze patient data with statistical methods to identify predictive factors related to discharge destination and discharge time. Most studies appear in clinical journals and seek the correlation between the discharge destination or time and patient factors such as demographic, socioeconomic, medical, etc. These studies use data analysis to determine the main features that can predict discharge destination and time.
Discharge destination prediction
Discharge destination is the most studied factor in this category. Knowing which characteristics impact the destination of patients is critical for physicians and hospital authorities [47, 48]. Based on their health situation, patients need to be discharged to either community-based places (e.g., home, home with support) or facility-based places (e.g., rehabilitation, long-term care).
One of the most studied groups of patients is orthopedic surgical patients. Studies help identify which patients may need additional care after surgical recovery. In several studies, different variables such as age, sex, race, socioeconomic factors, and family status are obtained as prediction factors for the next destination for patients [48–51].
Total joint arthroplasty (TJA) patients have attracted the attention of many researchers. TJA is a surgical procedure in which a damaged or diseased joint is replaced with an artificial joint or prosthesis. This procedure is commonly performed on the hip and knee. Since most of these patients need specialized care and assistance after surgery, defining their discharge destination is critical. Several studies find that demographics, clinical, and personal situations are the most important predictors of patients’ discharge destination after TJA [49, 52–58].
Mehta et al. [59] show that the level of community deprivation, representing the disadvantage or lack of resources within a community, can predict the discharge destination of patients undergoing hip arthroplasty. In a retrospective cohort study, Duque et al. [60] point to a connection between TJA performed under neuraxial anesthesia and an increased likelihood of home discharge. In a recently published study, to predict the discharge destination after total hip and knee arthroplasty, Hadad et al. [61] simultaneously investigate the performance of two tools; the preoperatively administered Predicting Location after Arthroplasty Nomogram (PLAN) and the postoperatively administered Activity Measure for Post-Acute Care (AM-PAC) “6-Clicks” basic mobility tools. They reveal that PLAN and “6-Clicks” basic mobility scores are well-performed predictors, suggesting that preoperative and postoperative variables influence discharge destination.
To investigate the impact of social support and psychological distress in the discharge plan after TJA, Zeppieri et al. [55] use the Risk Assessment and Predictive Tool (RAPT) (social support assessment) and modified STarT Back Tool (mSBT) (psychological distress assessment). Their results show that the RAPT is a proper tool to predict discharge destination. Focusing on the recent trends of community-based services, Cohen et al. [58] develop a modified RAPT score, which indicates the highest overall predictive accuracy of 92% and is capable of predicting home discharges.
Investigating spine surgery patients, Aldebeyan et al. [62] discover different demographic and clinical features that lead to facility-based discharge. They also use a multivariate logistic regression model to predict discharge destinations to other facilities rather than home. Through a retrospective cohort study focusing on the effect of age, Pennicooke et al. [63] show that patients over 70 had a higher chance of transferring to a facility-based destination. In another study, Lubelski et al. [64] create a calculator to estimate patients’ destinations after spine surgery. Their data analysis demonstrates that age, insurance type, marriage status, and surgical procedure are significantly associated with facility-based discharge destinations.
Kimmel et al. [48] develop a model to predict the facility-based destination for lower limb fracture patients. In another study, Glauser et al. [50] prove that the preoperative RAPT score is a highly predictive tool in lumbar fusion patients for discharge destinations that can predict admission to another facility or home. Using a multinomial logistic regression model, Ryder et al. [65] analyze and compare various characteristics and health outcomes of hospitalized patients with hip fractures. They also examine predictors of discharge destination to home or other facilities.
As patients have special needs after brain injury, many patients need to be discharged to a facility-based destination. To predict rehabilitation needs upon discharge after traumatic brain injury, De Guise et al. [66] consider different variables such as age, education, duration of posttraumatic amnesia, and clinical results. They find that having shorter posttraumatic amnesia lowers the chances of experiencing a disability and consequently lowers the need to be discharged to facility-based destinations. Focusing on the impact of race on the rehabilitation of traumatic brain injury patients, Oyesanya et al. [67] show that younger patients belonging to Latino or other racial/ethnic groups had a greater chance of being discharged to their homes rather than other facilities. In another study by Oyesanya et al. [68], sex and age are considered critical predictors for the discharge destination of traumatic brain injury patients. Also, using Logistic Regression (LR) on patients’ data, it is reported that younger and female patients have a lower chance of discharge to facility-based destinations.
Early prediction of post-stroke discharge destinations is found to be a way to improve patient outcomes, reduce costs, and improve the quality of care [69–72]. Also, some studies show that predicting and planning for a patient’s post-stroke discharge destination can reduce readmission rates, improve patient satisfaction, and increase the chance of successful rehabilitation [73–75]. Post-stroke discharge destination is typically predicted with clinical assessment and predictive modeling. Predictive modeling can be used to identify and analyze patient-specific predictors of post-stroke discharge destination. These predictors can determine which patients are more likely to be discharged to a facility-based or a community-based destination. Clinical assessment includes a patient’s medical history, current medical condition, and other factors such as age, sex, and comorbidities [76, 77].
Numerous studies reveal that patients’ physical situation, the family’s readiness at home, personal financial status, and marital status are significant predictive factors of discharge destination for patients after stroke [69, 71, 78–80]. A study by Nguyen et al. [81] reveals that marital status is crucial in determining discharge destination. However, immigrant and area-based socioeconomic status do not significantly impact discharge destinations. Moreover, Ouellette et al. [73] and Roberts et al. [82] propose that various functional and clinical outcome data at admission can be used to develop an accurate tool to predict discharge destinations for stroke patients. Kim et al. [83] establish a realistic assessment tool that forecasts home discharge for mild stroke patients after subacute rehabilitation therapy in tertiary institutions. This assessment tool considers a range of demographic, clinical, and functional variables as potential predictors. Cho et al. [75] investigate the link between the discharge status of post-stroke and patient characteristics using a probabilistic LR model. Based on their results, low readmission rates reflect complete care and proper discharge. Chevalley et al. [84] examine the effects of stroke patients’ socio-environmental characteristics and show that the most effective predictors of home discharge are living with others, receiving support at home, being married, and living at home before the stroke.
In another study, Gosling et al. [85] investigate the occurrence and risk factors associated with adverse discharge disposition (ADD) following cardiac surgery and present a tool to predict preoperative risks. Results show that patients with ADD are more elderly, female, have had a more extended hospital stay before surgery, and have undergone emergency surgery. Sex, race, payment type, injured region, physiologically base, and need for an Intensive Care Unit (ICU) are defined as determinant predictors of discharge destination for trauma patients by Lim et al. [86] and Strosberg et al. [87]. Hirota et al. [88] present two novel prediction models to determine where elderly patients with aspiration pneumonia will be discharged. They used various predictors, including age, sex, BMI score, and other clinical characteristics, to demonstrate that these models can aid in early-stage discharge planning. Table 1 presents an overview of the studies reviewed in this subsection, including the study name, prediction goals, patient populations, the method used, the main factors defined by studies as predictive factors, and dataset sizes.
Table 1.
Studies related to Statistical-based discharge destination prediction
| Study | Predicted parameter | Patient population | Methodology | Main factors | Dataset size |
|---|---|---|---|---|---|
| Agarwal et al. [76] | Discharge destination | Stroke patients | Logistic regressions | Age, sex, and the presence of premorbid social support | (n=104) |
| Lutz [78] | Facility-based discharges | Stroke patients | Grounded dimensional analysis | Functional Independence Measure (FIM) score, age, sex | (n=90) |
| Pablo et al. [49] | Discharge destination | Elective total hip replacement patients | Multivariate regression | walking ability, age, obesity | (n=1,276) |
| De Guise et al. [66] | Discharge destination | Traumatic brain injury patients | Logistic regressions | Age, education, Glasgow Coma Scale score | (n=339) |
| Nguyen et al. [81] | Discharge destination | Stroke patients | Multivariate logistic regression | Immigrant status, marital status | (n=326) |
| Lim et al. [86] | Discharge destination | Traumatic elderly patients | Multivariable random effect mixed model | Sex, race, payment type | (n=47,234) |
| Brauer et al. [70] | Community-based discharges | Stroke patients | Logistic regression | Admission functional status, age | (n=566) |
| Van der Zwaluw et al. [77] | Discharge destination | Stroke patients | Logistic regression | Cognitive dysfunction, age, BI score | (n=287) |
| Kimmel et al. [48] | Facility-based discharges | Lower limb fracture patients | Multivariable logistic regression | Age, proximal fracture type, fund source for the admission | (n=1,429) |
| West et al. [138] | Community-based discharges | Stroke patients | Behavioural mapping, statistical tests, multivariable median regression | Age, stroke severity, premorbid function | (n=73) |
| Stineman et al. [79] | Community-based discharges | Stroke patients | Logistic regression | Previous living circumstances, comorbidities, hospital course | (n=6,515) |
| Sharareh et al. [52] | Discharge destination | Joint arthroplasty patients | Cross-sectional analysis of different factors | Living statuses | (n=50) |
| Ouellette et al. [73] | Community-based discharges | Stroke patients | Logistic regressions and chi-square analyses | Health factors at the time of admission | (n=407) |
| Schwarzkopf et al. [139] | Discharge destination | Total hip arthroplasty patients | Multinomial regression | Race, insurance, morbidity | (n=14,326) |
| Halawi et al. [53] | Facility-based discharges | Joint arthroplasty patients | Multivariable logistic regression | Caregiver support, and patient expectation of discharge destination, age | (n=372) |
| Hansen et al. [57] | Facility-based discharges | Joint arthroplasty patients | RAPT, Binary logistic regression | Age, sex, health condition | (n=3,213) |
| Roberts et al. [82] | Discharge destination | Stroke patients | Receiver operator characteristic curve analysis, Linear regression | Functional status | (n=481) |
| Gholson et al. [54] | Community-based discharges | Joint arthroplasty patients | Multivariate logistic regression | Age, preoperative functional status, elective surgery status | (n=108,396) |
| Aldebeyan et al. [62] | Facility-based discharges | Lumbar spine fusion surgery patients | Multivariate logistic regression | Age, sex, comorbidities | (n=15,092) |
| Zeppieri et al. [55] | Discharge destination | Joint arthroplasty patients | RAPT, factorial analysis of variance | Social support, psychological distress | (n=231) |
| Dibra et al. [51] | Discharge destination | Revision joint arthroplasty patients | RAPT, Univariable logistic regression | Patient-reported discharge expectation | (n=716) |
| Sattler et al. [56] | Discharge destination | Knee arthroplasty patients | Univariable and multivariable logistic regression | Psychological, functional, and socio-demographic factors | (n=100) |
| Lubelski et al. [64] | Facility-based discharges | Spine surgery patients | Univariable and multivariable | Demographic variables, insurance status, baseline comorbidities | (n=257) |
| Ayyala et al. [39] | Facility-based discharges | Abdominal wall reconstruction patients | Multivariate logistic regression | Sex, history of diabetes, history of hypertension | (n= 4,549) |
| Glauser et al. [50] | Facility-based discharges | Posterior lumbar fusion patients | RAPT, Logistic regression | RAPT score, LOS, age | (n=432) |
| Kim et al. [30] | Community-based discharges | Moderate stroke patients | Logistic regression, weighted scoring model | Demographic, clinical, and functional factors | (n=732) |
| Mehta et al. [59] | Discharge destination | Hip arthroplasty patients | Adjusted binary logistic regression | Community area deprivation index level | (n=84,931) |
| Gosling et al. [85] | Facility-based discharges | Cardiac surgery patients | Stepwise backward logistic regression, used 5-fold and leave-one-out cross-validation | Age, sex, long LOS prior to surgery | (n=3,760) |
| Cohen et al. [58] | Discharge destination | Joint arthroplasty patients | RAPT, Multiple logistic regression | RAPT scores, demographic, and medical factors | (n=1,264) |
| Pennicooke et al. [63] | Discharge destination | Lumbar spine surgery patients | Multivariable nonlinear logistic regression | Age | (n=61,315) |
| Ryder et al. [65] | Facility-based discharges | Hip fracture patients | Multinominal logistic regression | Age, impaired cognition, reduced walking ability | (n=29,881) |
| Oyesanya et al. [67] | Discharge destination | Traumatic brain injury patients | Logistic regression | Race and ethnicity | (n=99,614) |
| Oyesanya et al. [68] | Discharge destination | Traumatic brain injury patients | Logistic regression | Age, sex | (n=221,961) |
| Hadad et al. [61] | Discharge destination | Joint arthroplasty patients | Regression models | Demographics, health factors | (n=11,672) |
| Hirota et al. [88] | Discharge destination | Aspiration pneumonia patients | Multilevel logistic regression | Age, sex, health factors | (n=34,105) |
Discharge time prediction
Although most studies focus on the destination of patients after discharge, multiple investigations consider the time of discharge or equivalently a patient’s LOS at the hospital [89]. Using the RAPT and mSBT, Zeppieri et al. [55] show that lower social support leads to longer LOS after TJA. Also, Cohen et al. [58] develop a modified RAPT score which indicates the highest overall predictive accuracy of 92% and is capable of predicting LOS. Investigating spine surgery patients, Aldebeyan et al. [62] discover different demographic and clinical features that lead to an increase in the LOS. Through a retrospective cohort study focusing on the effect of age, Pennicooke et al. [63] show that patients over 70 had a higher chance of staying more in the hospital. In another study, Lubelski et al. [64] create a calculator to estimate patients’ LOS after spine surgery.
Hintz et al. [90] use LR models with time-dependent covariate inclusion to evaluate multiple models for predicting newborns’ time to discharge. They found that the prediction of discharge time is poor if only perinatal factors are considered, but it improves considerably with knowledge of later-occurring morbidities. Shukla and Upadhyay [91] investigate the factors influencing delay in discharge time for insured patients, considering discharge Turn Around Time. Predictors of same-day discharge following benign minimally invasive hysterectomy are identified by Alashqar et al. [92]. The demographic, surgical, and surgeon characteristics connected to discharge on surgical day 0 are examined using multivariate LR. They show that higher chances of same-day discharge are connected with robotic hysterectomy, quicker surgical duration, and minimum blood loss.
Moreover, in a recent investigation conducted by Lebruan et al. [93], the efficacy of the RAPT score in predicting LOS for patients undergoing TJA is examined. Unlike previous studies that considered total knee arthroplasty (TKA) and total hip arthroplasty (THA) together when analyzing the RAPT score, this research assesses them separately. The results reveal that THA patients outperformed TKA patients with similar RAPT scores, indicating a potential difference in RAPT performance between the two procedures. Table 2 demonstrates the studies reviewed in this subsection.
Table 2.
Studies related to Statistical-based discharge time prediction
| Study | Predicted parameter | Patient population | Methodology | Main factors | Dataset size |
|---|---|---|---|---|---|
| Hintz et al. [90] | Discharge time, LOS | Newborns patients | Linear and logistic regression | Clinical characteristics | (n=2,254) |
| Carter et al. [89] | LOS | Total knee replacement patients | Statistical tests | Age, sex, consultant | (n=2,130) |
| Aldebeyan et al. [62] | LOS | Lumbar spine fusion surgery patients | Multivariate logistic regression | Age, sex, comorbidities | (n=15092) |
| Shukla and Upadhyay [91] | LOS | General patients with insurance | Correlation and linear regression | Turn Around Time for insured patients | (n=443) |
| Zeppieri et al. [55] | LOS | Joint arthroplasty patients | RAPT, factorial analysis of variance | Social support, psychological distress | (n=231) |
| Lubelski et al. [64] | LOS | Spine surgery patients | Univariable and multivariable analyses | Demographic variables, insurance status, baseline comorbidities | (n=257) |
| Cohen et al. [58] | LOS | Joint arthroplasty patients | RAPT, Multiple logistic regression | RAPT scores, demographic, and medical factors | (n=1,264) |
| Alashqar et al. [92] | Discharge time | Benign minimally invasive hysterectomy patients | Multivariate logistic regression | Operative, and surgeon factors | (n=1,084) |
| LeBrun et al. [93] | LOS | Joint arthroplasty patients | RAPT scores, Multivariable analyses | BMI, Charlson comorbidity index, age | (n=18,000) |
The studies discussed in these subsections employ statistical techniques to analyze historical data to predict the discharge destination and discharge time based on factors that are derived from the data. Many of these studies choose LR models for their analysis, depending on the specific variables, research question, and data characteristics. LR models the connection between a binary dependent variable and one or more independent variables. By examining historical data, these studies identify the primary predictors for discharge destination or discharge time, with demographic, socio-economic, and clinical factors being the main predictive elements.
RAPT is the other tool used in this area. The RAPT is a risk assessment tool that uses a set of risk factors, such as age, sex, medical status, and other patient characteristics, to calculate a risk score for each patient. The risk score is then used to categorize patients into defined classes. It should be noted that the accuracy of these prediction models is highly dependent on the quality of the data used to develop the models.
ML-based predictions
ML can refer to circumstances in which machines can simulate human minds in learning and thus be used to solve problems [94]. Researchers in the healthcare sector have been applying artificial intelligence to aid better analysis and raise the efficacy of the entire healthcare industry [95]. Prediction modeling has experienced a tremendous rise in the popularity of techniques from the ML domains [96].
Multiple studies in recent years have looked into several models to predict discharge outcomes. The main outcomes investigated are the discharge destination, LOS and discharge time, and the discharge volume. These predictions can help hospitals and healthcare providers optimize bed utilization, manage staffing levels, and coordinate patient care more effectively. This subsection investigates studies in which researchers predict discharge outcomes using various ML models. The emphasis of these papers tends to be on comparing the performance of multiple ML models and, in some of them, on reporting the most important factors affecting discharge outcomes.
Discharge destination prediction
As mentioned earlier, we consider two possible destination types for patients after discharge from the hospital: community-based (e.g., home, home with support) and facility-based (e.g., rehabilitation, long-term care). Knowing whether patients are going to their homes or other facilities directly impacts discharge planning. Lack of capacity in other facilities can lead to extended hospital stays, increased risk of complications, and poorer health outcomes overall. In addition, it is a critical component for managing resources in a healthcare system [97, 98]. Researchers use a variety of ML models to predict discharge destinations based on historical data of patients; for example, Elbattah and Molloy [99] use different ML models to aid in planning senior care with a hip fracture focused on predicting discharge destination. They found that compared to other models, Random Forest (RF) offers significantly higher accuracy.
Considering various attributes of elective inpatient lumbar degenerative disc diseases after surgery, Karhade et al. [100] show that using different ML to develop an open-access web application to predict facility-based discharges has promising results. Lu et al. [101] introduce five ML models aimed at forecasting whether patients following knee arthroplasty can be discharged to their homes or require alternative facilities. The findings indicate that the extreme gradient boosting (XGB) model outperforms the remaining models. Furthermore, they identify key factors influencing the likelihood of facility-based discharges, including total hospital LOS, preoperative hematocrit, body mass index, sex, and functional status. Bertsimas et al. [102] use a wide range of ML models to predict various elements of patient flows, including discharge destinations using a unique patient representation. The findings show that EHR data combined with interpretable ML models can be leveraged to provide visibility into patient flows.
In another study for traumatic brain injury patients, Satyadev et al. [103] develop several ML models to predict discharge destination and propose the RF model as the best-performing model. Mohammed et al. [104] develop four different ML models (Gradient boosting (GB), RF, LR, Artificial neural networks (ANN)) to predict three discharge outcomes of patients after total knee arthroplasty, including discharge destination. The findings show that these ML models can predict the desired outcomes successfully.
Imura et al. [105] demonstrate that among three classification and regression tree models, the model including basic information, functional factor, and environmental attributes has the highest accuracy for classifying the likelihood of stroke patients being discharged at home. Imura et al. [106] also use ML to discover the relevant parameters influencing stroke patients’ home discharge who require a wheelchair after discharge. Consequently, the most closely connected variables for home discharge are revealed to be physical environmental characteristics of the patient’s home which may cause accessibility challenges. In a different investigation, Bacchi et al. [107] showcase the effective validation, both prospective and external, of ML models. These models utilize six variables to predict discharge-related information, particularly concerning home discharges for stroke patients.
Utilizing the XGB model, Ikezawa et al. [108] reveal that patients with ischemic cerebral infarction had excellent rates of home discharge when early nutrition occurred within the first three days of hospital admission. Morris et al. [109] develop a novel ML model called Bayesian additive regression trees that outperforms conventional regression analysis in predicting discharge destinations after trauma in elderly patients. Investigating the data set, they also find that age and the Glasgow Coma Scale upon admission play critical roles in predicting discharge destination. Mickle and Deb [110] also find that the XGB model can classify the discharge destination for patients in acute neurological care effectively, based on demographic and medical data available within 24 hours of their hospital admission.
In another study, to predict facility-based discharge destination after total knee arthroplasty, Chen et al. [111] apply ANN, RF, histogram-based gradient boosting (HGB), and k-nearest neighbor (KNN) on a large dataset. They discover that ANN and HGB have excellent predictive performance during internal and external validations and can perform well in distinguishing facility-based discharges. In a recent study by Geng et al., it is found that patients over 65, females, those with higher American Society of Anesthesiology scores, and those requiring more extensive fusion are more likely to be discharged to community-based care after elective anterior cervical discectomy and fusion.
The studies reviewed in this subsection are summarized in Table 3. The information in the table includes the predicted parameters and the target patient population. Additionally, the table lists the ML model(s) used for prediction, the best-performing ML models in studies where various models are employed, and the database size used.
Table 3.
Studies of ML-based discharge destination prediction; the “*” denotes the best-performing model
| Study | Predicted parameter | Patient population | Methodology | Main factors | Dataset size |
|---|---|---|---|---|---|
| Elbattah and Molloy [99] | Discharge destination | Elderly patients with hip fracture care | RF*, Boosted Decision Tree (BDT), NN, Linear regression | (n=2,000) | |
| Karhade et al. [100] | Facility-based discharges | Elective lumbar degenerative disc disorders patients | NN*, BDT, SVM, Bayes Point Machine | Age, sex, BMI, fusion level, functional status | (n= 26,364) |
| Bacchi et al. [107] | Community-based discharges | Stroke patients | LR*, RF, DT, ANN | Age, sex, estimated pre-stroke mRS | (n= 2,840) |
| Lu et al. [125] | Facility-based discharges | Unicompartmental knee arthroplasty patients | Generalized linear model, RF, NN, XGB* | Total LOS, preoperative hematocrit, BMI, preoperative sodium | (n=7,275) |
| Bertsimas et al. [102] | Discharge destination | General patients | LR, CART DT*, Optimal Trees with Parallel Splits, RF, GBDT | Demographics, provider orders, diagnosis codes, medications | (n= 63,432) |
| Imura et al. [105] | Community-based discharges | Stroke patient | DT, Linear discriminant analysis, KNN*, SVM*, RF | Age, sex, stroke type | (n=481) |
| Satyadev et al. [103] | Discharge disposition | Traumatic brain injury patients | KNN, XGB, RF* | Vitals, demographics, mechanism of injury, comorbidities | (n=5,292) |
| Mohammed et al. [104] | Community-based discharges | Total knee arthroplasty patients | LR, GB*, RF*, ANN | Age, sex, race, admission month, admission on a weekend, admission type | (n=572,811) |
| Bacchi et al. [107] | Community-based discharges | Ischaemic or haemorrhagic stroke patients | LR, ANN* | Age, sex, stroke severity, health history | (n=1,158) |
| Ikezawa et al. [108] | Community-based discharges | Ischemic cerebral infarction patients | XGB | early nutritional initiation | (n=41,477) |
| Zhao et al. [133] | Facility-based discharges | Elective radical cystectomy patients | GBDT | Age, race, LOS, BMI | (n=11,881) |
| Morris et al. [109] | Discharge destination | Elderly patients with trauma | Bayesian additive regression trees | Age, comorbidities, LOS, physiologic parameters | (n=47,037) |
| Mickle and Deb [110] | Discharge destination | Acute neurological patients | LR, SVM, KNN, XGB*, RF | Age, glucose, admission weight | (n=5,245) |
| Chen et al. [111] | Facility-based discharges | Total knee arthroplasty patients | ANN*, RF, HGB*, KNN | LOS, age, BMI, sex | (n=434,550) |
| Geng et al. [137] | Facility-based discharges | Elective anterior cervical discectomy and fusion patients | RF | Age, Medicare insurance, American Society of Anesthesiology score, fusion levels | (n=2,227) |
Discharge time prediction
The LOS and discharge time significantly affect capacity, costs, and patient satisfaction. By accurately forecasting the discharge time (or, equivalently, a patient’s LOS), hospitals can proactively address patient needs and improve their overall quality of care [112, 113]. Numerous studies use ML models to forecast the discharge time. By employing tree-based supervised ML models, Barnes et al. [36] demonstrate that early discharges are less predictable than midnight discharges. Their model surpasses clinicians in predicting daily discharges with greater accuracy and can effectively rank patients in order of proximity to upcoming discharges.
A clinically interpretable feedforward Neural Network (NN) model by Safavi et al. [114] helps to foresee which patients leave the hospital within 24 hours and their obstacles. The NN model finds clinical barriers, variations in clinical practice, and non-clinical factors among the 65 hurdles to discharge. In another study, Lazar et al. [37] design an RF model to predict the clinical preparedness for discharge in the next 24 to 48 hours. They find that this model predicts surgical discharges on a 48-hour basis with greater sensitivity than clinicians. Nemati et al. [115] use six different ML and statistical analysis models to predict the discharge time of COVID-19 patients to aid health professionals in making better decisions. After comparing the results, they find that the GB survival model performs better than the others.
Some studies predict LOS rather than discharge time. In recent years, inpatient LOS prediction has been studied using various ML models. To predict LOS, Liu et al. [116] apply Decision Tree (DT), Naive Bayesian (NB) classifiers, and feature selection models to a dataset from a geriatric hospital. They discover that using NB models to deal with the sizable amount of missing data can significantly improve the classification accuracy of forecasting LOS, particularly for the long-stay group. ANN model is also utilized by Gholipour et al. [117] to predict the LOS in ICU. They find that ANN outperforms the Lagrangian regression model. Tsai et al. [118] create an ANN model to predict the LOS for inpatients in a cardiology unit. The findings show that preadmission models can predict LOS and pre-discharge models.
Muhlestein et al. [119] devise a novel strategy for constructing a model that predicts LOS after craniotomy for a brain tumor. With high internal and external validation performance, an ML ensemble model predicts LOS and generates medical insights that could enhance patient outcomes. Bacchi et al. [120] look at how well ML models could estimate the likely LOS for stroke patients using admission data. According to this study, ML models may aid in prognosticating characteristics crucial to post-stroke DP. He et al. [121] develop an ANN-based multi-task learning model for the prediction of patient LOS. This model produces better results than single-task regression and classification models. By evaluating different ML models, Zhong et al. [122] demonstrate the RF and ANN models are accurate enough to predict the LOS of ambulatory total hip arthroplasty patients. A recently published study by Zeleke et al. [123] aims to develop and compare various ML models for predicting LOS and Prolonged LOS in general patient settings for those admitted through the emergency department. The objective is to create a framework for prediction rather than favoring a specific model. Eight regression models are developed for LOS prediction, with XGB regressions displaying the lowest prediction error. The studies reviewed in this subsection are summarized in Table 4.
Table 4.
Studies related to ML-based discharge time prediction; the “*” denotes the best-performing model
| Study | Predicted parameter | Patient population | Methodology | Main factors | Dataset size |
|---|---|---|---|---|---|
| Gholipour et al. [117] | LOS | Trauma patients | ANN*, Lagrangian regression | Mechanism of trauma, the site involved, vital signs and physical examination, laboratory findings | (n=125) |
| Barnes et al. [36] | Discharge time | General patients | Tree-based supervised ML models, Regression RF* | Admission and discharge times, demographics, basic admission diagnoses | (n= 8,852) |
| Elbattah and Molloy [99] | LOS | Elderly patients with hip fracture care | RF*, BDT, NN, Linear regression | (n=2,000) | |
| Tsai et al. [118] | LOS | Cardiology patients | ANN*, Linear regression | Sex, age, location, main diagnosis | (n=2,377) |
| Turgeman et al. [112] | LOS | General patients | Regression tree | Demographics, outpatient and inpatient history, medication history, lab values and vital signs | (n=4,840) |
| Thompson et al. [135] | Prolonged LOS | Newborns | NB, Multi-layer Perceptron, Simple Logistic, SVM, DT, RF*, RT | Administrative data, minimal clinical data at the time of admission/birth | (n= 2,610) |
| Muhlestein et al. [119] | LOS | Brain tumor surgery patients | ML ensemble model | Nonelective surgery, preoperative pneumonia, sodium abnormality, race | (n= 41,222) |
| Kabir and Farrokhvar [113] | LOS | Surgical patients | ANN*, LR, SVM | surgical category | (n= 880,000) |
| Safavi et al. [114] | Discharge time | Surgical inpatients | Feedforward NN | Demographic, environmental, administrative, clinical | (n= 15,201) |
| Lazar et al. [37] | Discharge time | Surgical patients | RF | Age, sex, admission source, laboratory measurements, vitals | (n=10,904) |
| Bacchi et al. [107] | LOS | Stroke patients | LR, RF, DT, ANN* | Age, sex, estimated pre-stroke mRS | (n= 2,840) |
| Nemati et al. [115] | Discharge time | General patients | GB*, Fast SVM, Fast Kernel SVM | Age, sex | (n=1,182) |
| Bertsimas et al. [102] | Short-term discharges | General patients | Linear regression, CART DT, Optimal Trees, RF, GBT* | Demographics, provider orders, diagnosis codes, medications | (n= 63,432) |
| He et al. [121] | LOS, Flow | General patients | ANN | Age, sex, LOS, admit source department, medical features | (n=3,959) |
| Zhong et al. [122] | LOS | Ambulatory total hip arthroplasty patients | Multivariable LR, ANN*, RF* | Anesthesia type, BMI, age, ethnicity, white blood cell count | (n=63,859) |
| Gabriel et al. [136] | Discharge time | Surgical patients | Regression, RF*, balanced RF*, balanced bagging, NN, SVM | Patient’s surgical characteristics, age, sex, weight | (n=13,447) |
| Zeleke et al. [123] | LOS | General patients | Linear Regression, Ridge and Elastic-net regression, SVM, RF, KNN, XGB* | Demographic factors, mode of arrival/source of admission, risk categories, current problems | (n=12,858) |
Other discharge outcomes prediction
Utilizing ML can also be a valuable tool for hospital practitioners and staff in determining several critical discharge planning outcomes. These results aid in predicting patient needs and optimizing the DP process. Morton et al. [124] examine the performance of several supervised ML models (i.e., multiple linear regression, support vector machines (SVM), multi-task learning, and RF) for predicting long LOS vs. short LOS in hospitalized diabetes patients. The results of this study show that the SVM model is the most promising for predicting short-term LOS. The number of discharges per day in hospital or discharge volume is another outcome that can be predicted using data. Knowing daily discharge volume in advance can diminish capacity-related uncertainties, leading to more optimized decisions regarding patient admission scheduling [34]. To predict daily inpatient discharges from the nephrology department, Luo et al. [125] use three models based on time series analysis. They discover that the RF model performs best.
The performance of a novel time-series ML model for predicting hospital discharge volume is compared to more straightforward models by McCoy et al. [35]. Their results emphasize that while more highly developed models are presented, time-series-based prediction can enhance clinical planning in the short term with little effort and without using big data sets, or computational power. Moreover, VanWalraven et al. [126] validate the Tomorrow’s Expected Number of Discharges model’s accuracy in predicting the number of hospital discharges the following day. Considering gynecologic oncology surgery patients, Lambaudie et al. [127] develop a prediction model including Classification and Regression Trees to determine who can stay at the hospital for less than two days. Levin et al. [128] address the support of multidisciplinary discharge-focused rounds problem using real-time EHR data and developing an ML-based discharge prediction model. Their findings show that computerized patient discharge predictions within multidisciplinary rounds help shorten hospital stays.
To help prioritize complex individuals and reduce healthcare inefficiency, Ghazalbash et al. [129] use classification ML models to predict multimorbidity using three indices. Results show the feasibility and utility of predicting multimorbidity status utilizing ML models, allowing early detection of individuals at risk of 30-day death and readmission. Moreover, three ML models are used in a study by Gramaje et al. [130] to forecast whether a patient after surgery should remain in the hospital or not. They offer intriguing results; while ML models in the class Remain show promising results, all ML models perform poorly in class Discharge. This study recommends including non-clinical characteristics of patients such as education, availability of family, finalized DP, and final physical examinations to boost the model’s performance.
Ahn et al. [131] investigate the discharge prediction and individual features of inpatients with cardiovascular diseases using five ML models. The XGB model outperforms other models. By assessing the outcomes of prediction models and visualizing simulated bed management, they also discover risk factors in cardiovascular patients and help hospital authorities develop resource management. Also, Gao et al. [132] predict inpatient discharges by proposing a novel ensemble deep learning model based on random vector functional links (edRVFL). Numerous forecasting indicators and statistical testing show that the suggested model surpasses the benchmark by a statistically significant margin. To improve DP for patients undergoing radical cystectomy, Zhao et al. [133] develop a Gradient Boosted Decision Tree (GBDT) model that supports patients’ complex conditions and helps them receive higher care. Jaotomboa et al. [134] compare the performance of different ML models on a hospital dataset to identify patients with prolonged LOS. By evaluating AUC, they demonstrate that among LR, classification and regression trees, RF, GB, and NN, the GB classifier outperforms the other models. The studies reviewed in this subsection are summarized in Table 5.
Table 5.
Studies related to other ML-based discharge outcomes prediction; the “*” denotes the best-performing model
| Study | Predicted parameter | Patient population | Methodology | Main factors | Dataset size |
|---|---|---|---|---|---|
| Ebell et al. [140] | Survival to discharge | Cardiopulmonary patients | Classification, Regression trees | Demographics, clinical features at admission | (n = 38,092) |
| Morton et al. [124] | Prolonged LOS | Diabetic patients | MLR, SVM*, SVM+, MTL, RF | Age, Sex, Race, Expected Primary Payer, Admission Type | (n= 10,000) |
| Luo et al. [125] | Daily discharges | Nephrology patients | Time series (ARIMA, LSTM and RF* | Demographics, discharge date | (n=1,091) |
| McCoy Jr et al. [35] | Discharge volume | General patients | Time-series | (n=101,867) | |
| Van Walraven et al. [126] | Daily discharges | General patients | Survival tree approach | Age, sex, patient location throughout the admission | (n= 192,859) |
| Levin et al. [128] | Discharge rounds | General patients | Unit- specific models | Demographics, administrative, medications | (n= 12,470) |
| Ghazalbash et al. [129] | Multimorbidity status of patients | Old patients with discharge delay | Classification and regression trees, RF*, Bagging trees, XGB*, LR | Age, sex, marginalization, rural/urban residency, chronic conditions, LOS, admission type | (n=163,983) |
| Ahn et al. [131] | Discharge probability | Cardiovascular patients | XGB*, LR, RF, SVM, Multilayer perceptron | Demographics, administrative, medications | (n=572,811) |
| Gramaje et al. [130] | Discharge or Remain | Surgical patients | DT, RF, Bayesian Network* | Age, clinical conditions | (n=90) |
| Gao et al. [132] | Inpatient discharge | General patients | edRVFL | (n=417) | |
| Jaotombo et al. [134] | LOS | General patients | LR, CART, RF, GB*, NN | Discharge destination, age, emergency admission, with more comorbidities notably mental health problems and dementia | (n=73,182) |
This section explains the studies that explore the implementation of various ML models on a dataset and seek to predict discharge outcomes such as destination, time, volume, etc. However, just a few studies consider multiple discharge outcomes, such as destination, time, and volume. Another considerable gap among these studies is about the input data. Since integrating data from multiple sources can be a complex task, many studies are developed and validated using data from a single institution or a specific population, which might limit the generalizability of the results. Further research is needed to validate predictive models across diverse healthcare settings, populations, and geographic locations.
Moreover, most existing prediction models are based on historical data and may not fully use real-time data. Integrating real-time data, such as vital signs, laboratory results, and patient monitoring data, could enhance the accuracy of predictions. Limited use of advanced analytics techniques is found to be another gap in review studies. Although there are many different types of predictive modelling techniques, there has not been a lot of use of advanced analytics to predict patient discharge factors. Future studies can explore the application of advanced analytics to enhance predictions’ reliability and accuracy.
Discussion
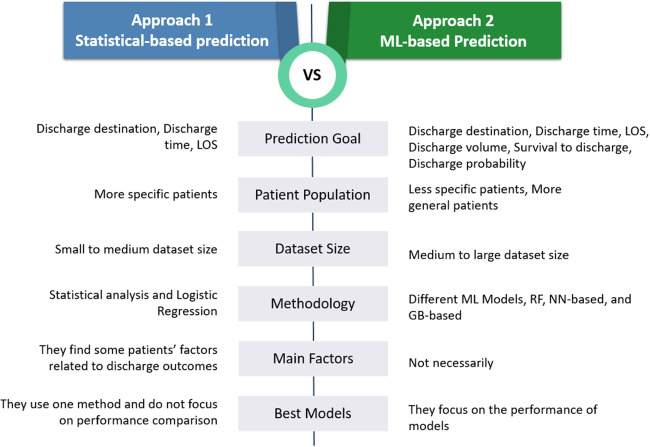
This paper presents a literature review focusing on studies that have employed prediction methods to estimate the destination, time, and volume of discharged patients. Numerous researchers have applied prediction methods to estimate different discharge factors using statistical and ML-based methods. Papers following the first approach (statistical methods in Section 3.1) aim to identify medical, demographic, and socioeconomic factors predicting patient discharge within specific cohorts. However, the second approach (ML-based models in Section 3.2) seeks to predict various discharge factors by implementing ML-based models on extensive datasets.
These two approaches share similarities but also exhibit differences. One of the significant distinctions is how they address discharge-related aspects. In the first approach, studies primarily focus on determining the destination and time of discharge. However, in the second approach, leveraging the enhanced capabilities of ML models, researchers can predict a more comprehensive array of variables such as daily discharge volume, discharge likelihood, and other related parameters.
In the first approach, discerning patient factors is para-mount, as studies endeavour to uncover influential variables for predicting discharge outcomes through statistical analyses. Conversely, ML-based studies may pinpoint significant factors, but the primary objective is not necessarily to isolate patient variables. Instead, their ultimate aim is to develop the most effective prediction model. In ML-based studies, the emphasis lies on comparing different models and identifying the one with the highest predictive accuracy.
This contrast is particularly evident when considering the methods employed. Unlike studies in the first approach, which utilize statistical methods, especially logistic regression, in the second approach, ML-based studies explore various ML models to minimize prediction errors. The statistical studies also try to customize their analyses for particular groups of patients, thereby enhancing the relevance of patient-related factors to predicted outcomes.
Figure 3 illustrates the characteristics of the two reviewed approaches. There are both similarities and differences between these approaches. However, the most noteworthy distinction lies in their methodologies, with additional notable variations. In the first approach, all the studies primarily investigate the prediction of destination and time of discharge, focusing on a specific group of patients. They aim to identify the most pertinent and critical patient factors related to discharge outcomes. Conversely, in the second approach, besides destination and time, other goals are considered. In this ML-based approach, studies are oriented toward comparing the performance of various ML models to determine the optimal model.
Fig. 3.
The characteristics of the two reviewed approaches
Most reviewed studies in Section 3.1 focus on orthopedic surgical patients, brain injury patients, and stroke. For orthopedic surgical patients, factors such as age, sex, race, socioeconomic factors, and family status are found to be significant predictors of discharge destination. Similarly, age, education, and clinical results are crucial for brain injury patients in predicting rehabilitation needs upon discharge. In stroke and cardiac surgery patients, factors such as patients’ physical condition, family readiness, financial status, and marital status play significant roles in determining discharge destinations. Also, several studies explore specific variables associated with discharge outcomes in other patient groups.
On the other hand, papers in Section 3.2 provide various ML models that utilize historical data. The chosen model is determined by the data set’s size, characteristics, and prediction type (whether a classification or a clustering model). A common application of ML-based models is in discharge destination prediction. By analyzing patient data, multiple studies utilize ML models to predict whether patients will be discharged to community-based or facility-based destinations. Another area where ML-based predictions have shown promise is in discharge time prediction. Accurately forecasting the discharge time allows hospitals to proactively address patient needs and improve patient flow and throughput. Moreover, ML-based predictions have been utilized to indicate discharge volume, enabling healthcare organizations to anticipate patient discharge outcomes. In most studies, time series models are utilized to predict discharge volumes. These approaches are effective in short-term forecasting and clinical planning without requiring extensive computational resources.
In terms of methodology, various methods are used to investigate statistical studies, such as LR and RAPT, with LR models being the most widely used. LR finds extensive application in both statistical-based and ML-based studies, although there are differences in their use and purpose. In statistical analysis, LR is primarily employed for inference, helping to understand the relationship between independent variables and binary outcomes. The emphasis here lies in comprehending the significance of each predictor. In contrast, in ML-based studies, LR is often utilized as a classification algorithm, predicting binary outcomes. The focus in this context shifts to predictive accuracy rather than inferential insights.
RF, NN-based, and GB-based models are the most commonly employed ML models in ML-based prediction studies. Among the 50 investigated studies, RF was used in 27, NN-based models in 20, and GB-based models in 17 for predictions. RF was the best-performing model in 13 studies [36, 37, 99, 103, 104, 122, 125, 126, 129, 135–137], making it the top-performing model in approximately 50% of its applications. NN models outperformed others in 11 studies [100, 106, 107, 111, 113, 114, 117, 118, 120–122], accounting for approximately 56% of their usage. GB models exhibited the best performance in 12 studies [104, 107, 108, 110, 111, 115, 123, 129, 131, 133, 134], establishing GB-based models as the best choice in 67% of their applications.
These models often outperform traditional statistical methods such as LR. It is important to note that the choice of models depends on the specific prediction task and the available data. Different ML models may suit diverse patient populations and discharge factors. Future studies can aim to validate and compare other models using more extensive and varied datasets, incorporate additional features such as non-clinical characteristics, and focus on improving the interpretability of ML models.
The researchers use various approaches to compare the performance of different ML models. One widely used performance metric is the area under the ROC curve. The ROC curve plots the true positive rate against the false positive rate for different classification thresholds. The AUC measures the overall performance of the ML model in distinguishing between positive and negative samples. Many studies use the AUC because it is easy to compute and interpret. Also, it provides a single value that summarizes the model’s overall performance, making it easier to compare the performance of different models on the same task or dataset.
Furthermore, several pieces of research focus on the destination, while others concentrate on the timing, daily discharge, or discharge volume. However, few studies examine multiple discharge patient outcomes, such as destination, LOS, volume, and clinical features. The lack of a diverse and generalized dataset is found to be another gap in this area. Incorporating input data from various healthcare institutions, populations, and locations, as well as considering real-time data, can increase the accuracy and validation of results. Another significant gap in this field is the application of prediction results as decision-making aids in hospital administration. Further effort is required to confirm the link between predictions, hospital actions, and quality of care. The incorporation of DP with other health facilities needs to be addressed for planning to be effective and precise in real-world scenarios.
Discharge is the final point of patient flow in the hospital, and for patients not discharged to home, it is linked to other healthcare facilities such as nursing homes, long-term care facilities, rehabilitation centers, etc. Accordingly, solutions to discharge concerns often lie outside the hospital and necessitate system-wide policies. Even in prediction studies, the majority of studies use a prediction tool to anticipate time or destination and assess the model’s effectiveness, and there is little discussion on the next steps. Another area of future research in this field is the practical use of the predictions to improve hospital processes and patient outcomes.
These problems need to be accurately modeled during the entire discharge process and predict system performance in a more realistic and detailed setting. While the DP problem presents itself as a difficult challenge, it also allows public health, healthcare systems, and hospitals to collaborate to develop best practices and intervention strategies. As a result, applying different tools, including data analysis, ML, operations research, and quality improvement, will benefit health administrators and patients.
Glossary
| Acronym | Description |
|---|---|
| ADD | Adverse Discharge Disposition |
| ANN | Artificial Neural Networks |
| AUC | Area Under the ROC Curve |
| BDT | Boosted Decision Tree |
| BMI | Body Mass Index |
| DP | Discharge Planning |
| DT | Decision Tree |
| EHR | Electronic Health Records |
| FIM | Functional Independence Measure |
| GBDT | Gradient Boosting Decision Trees |
| HGB | Histogram-based Gradient Boosting |
| ICU | Intensive Care Unit |
| KNN | K-nearest Neighbor |
| LOS | Length of Stay |
| LR | Logistic Regression |
| ML | Machine Learning |
| MLR | Multinomial Logistic Regression |
| mSBT | Modified STarT Back Tool |
| MTL | Multi-Task Learning |
| NB | Naive Bayesian |
| NN | Neural Networks |
| RAPT | Risk Assessment and Predictive Tool |
| RF | Random Forest |
| ROC | Receiver Operating Characteristic |
| RT | Random Trees |
| SVM | Support Vector Machine |
| TJA | Total Joint Arthroplasty |
| THA | Total Hip Arthroplasty |
| TKA | Total Knee Arthroplasty |
| XGB | Extreme Gradient Boosting |
Declarations
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Veneklaas W, Leeftink AG, Boekel P, Hans EW (2021) On the design, implementation, and feasibility of hospital admission services: The admission lounge case. Omega 100:102308 [Google Scholar]
- 2.Kriegel J, Jehle F, Dieck M, Tuttle-Weidinger L (2015) Optimizing patient flow in Austrian hospitals-improvement of patient-centered care by coordinating hospital-wide patient trails. International Journal of Healthcare Management. 8(2):89–99 [Google Scholar]
- 3.Lin C-J, Cheng S-J, Shih S-C, Chu C-H, Tjung J-J (2012) Discharge planning. Int. J Gerontol 6(4):237–240 [Google Scholar]
- 4.Yen H-Y, Chi M-J, Huang H-Y (2022) Effects of discharge planning services and unplanned readmissions on post-hospital mortality in older patients: A time-varying survival analysis. Int J Nurs Stud 128:104175. 10.1016/j.ijnurstu.2022.104175 [DOI] [PubMed] [Google Scholar]
- 5.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR (2004) Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA 291(11):1358–1367 [DOI] [PubMed] [Google Scholar]
- 6.Damiani G, Federico B, Venditti A, Sicuro L, Rinaldi S, Cirio F, Pregno C, Ricciardi W (2009) Hospital discharge planning and continuity of care for aged people in an Italian local health unit: does the care-home model reduce hospital readmission and mortality rates? BMC Health Serv Res 9(1):22. 10.1186/1472-6963-9-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vermeulen MJ, Ray JG, Bell C, Cayen B, Stukel TA, Schull MJ (2009) Disequilibrium between admitted and discharged hospitalized patients affects emergency department length of stay. Ann Emerg Med 54(6):794–804 [DOI] [PubMed] [Google Scholar]
- 8.McMartin K (2013) Discharge planning in chronic conditions: an evidence-based analysis. Ontario health technology assessment series. 13(4):1–72 [PMC free article] [PubMed] [Google Scholar]
- 9.Khaleghparast S, Ghanbari B, Kahani S, Malakouti K, SeyedAlinaghi S, Sudhinaraset M (2014) The effectiveness of discharge planning on the knowledge, clinical symptoms and hospitalisation frequency of persons with schizophrenia: a longitudinal study in two hospitals in Tehran. Iran. Journal of Clinical Nursing. 23(15–16):2215–2222. 10.1111/jocn.12499 [DOI] [PubMed] [Google Scholar]
- 10.Henke RM, Karaca Z, Jackson P, Marder WD, Wong HS (2017) Discharge planning and hospital readmissions. Med Care Res Rev 74(3):345–368 [DOI] [PubMed] [Google Scholar]
- 11.Cousin-Peterson E, Janjua HM, Barry TM, Baker MS, Kuo PC (2021) Discharge timing: Does targeting an ideal length of stay for patients undergoing colectomy impact readmissions and costs of care? The American Journal of Surgery. 221(3):570–574. 10.1016/j.amjsurg.2020.11.009 [DOI] [PubMed] [Google Scholar]
- 12.Hunt-O’Connor C, Moore Z, Patton D, Nugent L, Avsar P, O’Connor T (2021) The effect of discharge planning on length of stay and readmission rates of older adults in acute hospitals: A systematic review and meta-analysis of systematic reviews. J Nurs Manag 29(8):2697–2706 [DOI] [PubMed] [Google Scholar]
- 13.Southern WN, Berger MA, Bellin EY, Hailpern SM, Arnsten JH (2007) Hospitalist Care and Length of Stay in Patients Requiring Complex Discharge Planning and Close Clinical Monitoring. Arch Intern Med 167(17):1869–1874. 10.1001/archinte.167.17.1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakanishi M, Niimura J, Tanoue M, Yamamura M, Hirata T, Asukai N (2015) Association between length of hospital stay and implementation of discharge planning in acute psychiatric inpatients in Japan. Int J Ment Heal Syst 9(1):23. 10.1186/s13033-015-0015-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parikh PJ, Ballester N, Ramsey K, Kong N, Pook N (2017) The n-by-T target discharge strategy for inpatient units. Med Decis Making 37(5):534–543 [DOI] [PubMed] [Google Scholar]
- 16.Holland DE, Bowles KH (2012) Standardized Discharge Planning Assessments: Impact on Patient Outcomes. J Nurs Care Qual 27(3):200–208 [DOI] [PubMed] [Google Scholar]
- 17.Puschner B, Steffen S, Gaebel W, Freyberger H, Klein HE, Steinert T, Muche R, Becker T (2008) Needs-oriented discharge planning and monitoring for high utilisers of psychiatric services (NODPAM): Design and methods. BMC Health Serv Res 8(1):152. 10.1186/1472-6963-8-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aiyer M, Kukreja S, Ibrahim-Ali W, Aldag J (2009) Discharge planning curricula in internal medicine residency programs: a national survey. South Med J 102(8):795–799. 10.1097/smj.0b013e3181ad5ae8 [DOI] [PubMed] [Google Scholar]
- 19.Steffen S, Kösters M, Becker T, Puschner B (2009) Discharge planning in mental health care: a systematic review of the recent literature. Acta Psychiatr Scand 120(1):1–9. 10.1111/j.1600-0447.2009.01373.x [DOI] [PubMed] [Google Scholar]
- 20.Mathews NB, Ghrayeb L, Chintala VSN, Muthuswamy S, Mckinney C, Lindley B, Iyer R (2021) Improving Patient Discharge Process, 211–217
- 21.Ortiga B, Salazar A, Jovell A, Escarrabill J, Marca G, Corbella X (2012) Standardizing admission and discharge processes to improve patient flow: a cross sectional study. BMC Health Serv Res 12(1):1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White CM, Statile AM, White DL, Elkeeb D, Tucker K, Herzog D, Warrick SD, Warrick DM, Hausfeld J, Schondelmeyer A (2014) Using quality improvement to optimise paediatric discharge efficiency. BMJ quality & safety. 23(5):428–436 [DOI] [PubMed] [Google Scholar]
- 23.Madsen NL, Porter A, Cable R, Hanke SP, Hoerst A, Neogi S, Brower LH, White CM, Statile AM (2021) Improving Discharge Efficiency and Charge Containment on a Pediatric Acute Care Cardiology Unit. Pediatrics 148(3):2020004663. 10.1542/peds.2020-004663 [DOI] [PubMed] [Google Scholar]
- 24.Roberts S, Moore LC, Jack B (2019) Improving discharge planning using the re-engineered discharge programme. J Nurs Manag 27(3):609–615. 10.1111/jonm.12719 [DOI] [PubMed] [Google Scholar]
- 25.Kamalanathan NA, Eardley A, Chibelushi C, Collins T (2013) Improving the patient discharge planning process through knowledge management by using the Internet of Things. Advances in Internet of Things. 3(02):16–26 [Google Scholar]
- 26.Kamalanathan NA (2015) A systematic Knowledge Management model for planning the discharge of hospital patients. Staffordshire University
- 27.Fitzgerald LR, Bauer M, Koch SH, King SJ (2011) Hospital discharge: recommendations for performance improvement for family carers of people with dementia. Aust Health Rev 35(3):364–370 [DOI] [PubMed] [Google Scholar]
- 28.Allen TT, Tseng S-H, Swanson K, McClay MA (2009) Improving the hospital discharge process with Six Sigma methods. Qual Eng 22(1):13–20 [Google Scholar]
- 29.McDermott CM, Venditti FJ (2015) Implementing lean in knowledge work: Implications from a study of the hospital discharge planning process. Oper Manag Res 8(3):118–130. 10.1007/s12063-015-0103-7 [Google Scholar]
- 30.Kim SR, Laframboise S, Nelson G, McCluskey SA, Avery L, Kujbid N, Zia A, Spenard E, Bernardini MQ, Ferguson SE, May T, Hogen L, Cybulska P, Marcon E, Bouchard-Fortier G (2022) Enhanced recovery after minimally invasive gynecologic oncology surgery to improve same day discharge: a quality improvement project. International Journal of Gynecologic Cancer. 32(4):457–465. 10.1136/ijgc-2021-003065 [DOI] [PubMed] [Google Scholar]
- 31.Meo N, Cornia PB (2022) Focusing on the medically ready for discharge patient using a reliable design strategy: a quality improvement project to improve length of stay on a medicine service. Qual Manag Health Care 31(1):14–21 [DOI] [PubMed] [Google Scholar]
- 32.Shepperd S, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL (2013) Discharge planning from hospital to home. Cochrane database of systematic reviews. (1) [DOI] [PubMed]
- 33.Gonçalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S (2016) Discharge planning from hospital. Cochrane database of systematic reviews. (1) [DOI] [PMC free article] [PubMed]
- 34.Zhu T, Luo L, Zhang X, Shi Y, Shen W (2015) Time-series approaches for forecasting the number of hospital daily discharged inpatients. IEEE J Biomed Health Inform 21(2):515–526 [DOI] [PubMed] [Google Scholar]
- 35.McCoy TH, Pellegrini AM, Perlis RH (2018) Assessment of time-series machine learning methods for forecasting hospital discharge volume. JAMA Netw Open 1(7):184087–184087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barnes S, Hamrock E, Toerper M, Siddiqui S, Levin S (2016) Real-time prediction of inpatient length of stay for discharge prioritization. J Am Med Inform Assoc 23(e1):2–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lazar DJ, Kia A, Freeman R, Divino CM (2020) A Machine Learning Model Enhances Prediction of Discharge for Surgical Patients. Journal of the American College of Surgeons 231(4, Supplement 1):132. 10.1016/j.jamcollsurg.2020.07.255
- 38.Barsoum WK, Murray TG, Klika AK, Green K, Miniaci SL, Wells BJ, Kattan MW (2010) Predicting Patient Discharge Disposition After Total Joint Arthroplasty in the United States. J Arthroplasty 25(6):885–892. 10.1016/j.arth.2009.06.022 [DOI] [PubMed] [Google Scholar]
- 39.Ayyala HS, Weisberger J, Le T-M, Chow A, Lee ES (2020) Predictors of discharge destination after complex abdominal wall reconstruction. Hernia 24(2):251–256. 10.1007/s10029-019-02054-z [DOI] [PubMed] [Google Scholar]
- 40.Khan KS, Kunz R, Kleijnen J, Antes G (2003) Five steps to conducting a systematic review. J R Soc Med 96(3):118–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarkis-Onofre R, Catalá-López F, Aromataris E, Lockwood C (2021) How to properly use the prisma statement. Syst Rev 10:1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petropoulos F, Makridakis S, Assimakopoulos V, Nikolopoulos K (2014) ‘Horses for Courses’ in demand forecasting. Eur J Oper Res 237(1):152–163. 10.1016/j.ejor.2014.02.036 [Google Scholar]
- 43.Tello M, Reich ES, Puckey J, Maff R, Garcia-Arce A, Bhattacharya BS, Feijoo F (2022) Machine learning based forecast for the prediction of inpatient bed demand. BMC Med Inform Decis Mak 22(1):55. 10.1186/s12911-022-01787-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dawoodbhoy FM, Delaney J, Cecula P, Yu J, Peacock I, Tan J, Cox B (2021) Ai in patient flow: applications of artificial intelligence to improve patient flow in nhs acute mental health inpatient units. Heliyon. 7(5):06993. 10.1016/j.heliyon.2021.e06993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Socwell CP, Bucci L, Patchell S, Kotowicz E, Edbrooke L, Pope R (2018) Utility of Mayo Clinic’s early screen for discharge planning tool for predicting patient length of stay, discharge destination, and readmission risk in an inpatient oncology cohort. Support Care Cancer 26(11):3843–3849. 10.1007/s00520-018-4252-8 [DOI] [PubMed] [Google Scholar]
- 46.Loreto M, Lisboa T, Moreira VP (2020) Early prediction of icu readmissions using classification algorithms. Comput Biol Med 118:103636. 10.1016/j.compbiomed.2020.103636 [DOI] [PubMed] [Google Scholar]
- 47.Glasby J, Littlechild R, Pryce K (2006) All dressed up but nowhere to go? Delayed hospital discharges and older people. Journal of health services research & policy. 11(1):52–58 [DOI] [PubMed] [Google Scholar]
- 48.Kimmel LA, Holland AE, Edwards ER, Cameron PA, De Steiger R, Page RS, Gabbe B (2012) Discharge destination following lower limb fracture: Development of a prediction model to assist with decision making. Injury 43(6):829–834. 10.1016/j.injury.2011.09.027 [DOI] [PubMed] [Google Scholar]
- 49.Pablo P, Losina E, Phillips CB, Fossel AH, Mahomed N, Lingard EA, N. Katz J (2004) Determinants of discharge destination following elective total hip replacement. Arthritis Care Res 51(6):1009–1017. 10.1002/art.20818 [DOI] [PubMed]
- 50.Glauser G, Piazza M, Berger I, Osiemo B, McClintock SD, Winter E, Chen HI, Ali ZS, Malhotra NR (2020) The Risk Assessment and Prediction Tool (RAPT) for Discharge Planning in a Posterior Lumbar Fusion Population. Neurosurgery 86(2):140–146. 10.1093/neuros/nyz419 [DOI] [PubMed] [Google Scholar]
- 51.Dibra FF, Parvataneni HK, Gray CF, Vasilopoulos T, Prieto HA (2020) The risk assessment and prediction tool accurately predicts discharge destination after revision hip and knee arthroplasty. J Arthroplasty 35(10):2972–2976 [DOI] [PubMed] [Google Scholar]
- 52.Sharareh B, Le NB, Hoang MT, Schwarzkopf R (2014) Factors Determining Discharge Destination for Patients Undergoing Total Joint Arthroplasty. J Arthroplasty 29(7):1355–13581. 10.1016/j.arth.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 53.Halawi MJ, Vovos TJ, Green CL, Wellman SS, Attarian DE, Bolognesi MP (2015) Patient Expectation Is the Most Important Predictor of Discharge Destination After Primary Total Joint Arthroplasty. J Arthroplasty 30(4):539–542. 10.1016/j.arth.2014.10.031 [DOI] [PubMed] [Google Scholar]
- 54.Gholson JJ, Pugely AJ, Bedard NA, Duchman KR, Anthony CA, Callaghan JJ (2016) Can We Predict Discharge Status After Total Joint Arthroplasty? A Calculator to Predict Home Discharge. J Arthroplasty 31(12):2705–2709. 10.1016/j.arth.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 55.Zeppieri KE, Butera KA, Iams D, Parvataneni HK, George SZ (2019) The Role of Social Support and Psychological Distress in Predicting Discharge: A Pilot Study for Hip and Knee Arthroplasty Patients. J Arthroplasty 34(11):2555–2560. 10.1016/j.arth.2019.06.033 [DOI] [PubMed] [Google Scholar]
- 56.Sattler LN, Hing WA, Rathbone EN, Vertullo CJ (2020) Which Patient Factors Best Predict Discharge Destination After Primary Total Knee Arthroplasty? The ARISE Trial. J Arthroplasty 35(10):2852–2857. 10.1016/j.arth.2020.05.056 [DOI] [PubMed] [Google Scholar]
- 57.Hansen VJ, Gromov,K, Lebrun LM, Rubash HE, Malchau H, Freiberg AA (2015) Does the risk assessment and prediction tool predict discharge disposition after joint replacement? Clinical Orthopaedics and Related Research® 473(2):597–601 [DOI] [PMC free article] [PubMed]
- 58.Cohen E, Reid DBC, Quinn M, Walsh D, Raducha J, Hubbard L, Froehlich J (2021) Modifying the RAPT Score to Reflect Discharge Destination in Current Practice. Arthroplasty Today 7:17–21. 10.1016/j.artd.2020.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mehta B, Goodman S, Ho K, Parks M, Ibrahim SA (2021) Community Deprivation Index and Discharge Destination After Elective Hip Replacement. Arthritis Care & Research. 73(4):531–539. 10.1002/acr.24145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Duque M, Schnetz MP, Yates AJ, Monahan A, Whitehurst S, Mahajan A, Kaynar AM (2021) Impact of neuraxial versus general anesthesia on discharge destination in patients undergoing primary total hip and total knee replacement. Anesthesia & Analgesia. 133(6):1379–1386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hadad MJ, Orr MN, Emara AK, Klika AK, Johnson JK, Piuzzi NS (2022) PLAN and AM-PAC "6-Clicks" Scores to Predict Discharge Disposition After Primary Total Hip and Knee Arthroplasty. The Journal of bone and joint surgery. American Volume 104(4):326–335. 10.2106/JBJS.21.00503 [DOI] [PubMed]
- 62.Aldebeyan S, Aoude A, Fortin M, Nooh A, Jarzem P, Ouellet J, Weber M (2016) Predictors of discharge destination after lumbar spine fusion surgery. Global Spine Journal 6(1_suppl):0036 [DOI] [PubMed]
- 63.Pennicooke B, Santacatterina M, Lee J, Elowitz E, Kallus N (2021) The effect of patient age on discharge destination and complications after lumbar spinal fusion. J Clin Neurosci 91:319–326. 10.1016/j.jocn.2021.07.006 [DOI] [PubMed] [Google Scholar]
- 64.Lubelski D, Ehresman J, Feghali J, Tanenbaum J, Bydon A, Theodore N, Witham T, Sciubba DM (2020) Prediction calculator for nonroutine discharge and length of stay after spine surgery. The Spine Journal. 20(7):1154–1158. 10.1016/j.spinee.2020.02.022 [DOI] [PubMed] [Google Scholar]
- 65.Ryder, T., Close, J., Harris, I., Cameron, I.D., Seymour, H., Armstrong, E., Bell, J., Hurring, S., Mitchell, R., Group, A.S (2021) Patient and hospital factors influencing discharge destination following hip fracture. Australas J Ageing 40(3):234–243. 10.1111/ajag.12905 [DOI] [PubMed] [Google Scholar]
- 66.Guise E, LeBlanc J, Feyz M, Lamoureux J (2006) Prediction of Outcome at Discharge From Acute Care Following Traumatic Brain Injury. J Head Trauma Rehabil 21(6):527–536 [DOI] [PubMed] [Google Scholar]
- 67.Oyesanya TO, Harris G, Yang Q, Byom L, Cary MP Jr, Zhao AT, Bettger JP (2021) Inpatient rehabilitation facility discharge destination among younger adults with traumatic brain injury: differences by race and ethnicity. Brain Inj 35(6):661–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Oyesanya TO, Harris G, Cary MP, Byom L, Yang Q, Bettger JP (2021) Age- and sex-specific predictors of inpatient rehabilitation facility discharge destination for adult patients with traumatic brain injury. Brain Inj 35(12–13):1529–1541. 10.1080/02699052.2021.1972453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mees M, Klein J, Yperzeele L, Vanacker P, Cras P (2016) Predicting discharge destination after stroke: A systematic review. Clin Neurol Neurosurg 142:15–21. 10.1016/j.clineuro.2016.01.004 [DOI] [PubMed] [Google Scholar]
- 70.Brauer SG, Bew PG, Kuys SS, Lynch MR, Morrison G (2008) Prediction of Discharge Destination After Stroke Using the Motor Assessment Scale on Admission: A Prospective. Multisite Study. Arch Phys Med Rehabil 89(6):1061–1065. 10.1016/j.apmr.2007.10.042 [DOI] [PubMed] [Google Scholar]
- 71.Van der Cruyssen K, Vereeck L, Saeys W, Remmen R (2015) Prognostic factors for discharge destination after acute stroke: a comprehensive literature review. Disabil Rehabil 37(14):1214–1227. 10.3109/09638288.2014.961655 [DOI] [PubMed] [Google Scholar]
- 72.Meijer R, Limbeek J, Kriek B, Ihnenfeldt D, Vermeulen M, Haan R (2004) Prognostic social factors in the subacute phase after a stroke for the discharge destination from the hospital stroke-unit. A systematic review of the literature. Disability and Rehabilitation 26(4):191–197. 10.1080/09638280310001636437 [DOI] [PubMed]
- 73.Ouellette DS, Timple C, Kaplan SE, Rosenberg SS, Rosario ER (2015) Predicting discharge destination with admission outcome scores in stroke patients. NeuroRehabilitation 37(2):173–179 [DOI] [PubMed] [Google Scholar]
- 74.Bailey EA, Hoffman RL, Wirtalla C, Karakousis G, Kelz RR (2017) Development and validation of a prediction model for patients discharged to post-acute care after colorectal cancer surgery. Surgery. 161(4):1049–1057. 10.1016/j.surg.2016.10.015 [DOI] [PubMed] [Google Scholar]
- 75.Cho J, Place K, Salstrand R, Rahmat M, Mansouri M, Fell N, Sartipi M (2021) Developing a Predictive Tool for Hospital Discharge Disposition of Patients Poststroke with 30-Day Readmission Validation. Stroke Research and Treatment 2021:5546766. 10.1155/2021/5546766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Agarwal V, McRae MP, Bhardwaj A, Teasell RW (2003) A model to aid in the prediction of discharge location for stroke rehabilitation patients11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upo. Arch Phys Med Rehabil 84(11):1703–1709. 10.1053/S0003-9993(03)00362-9 [DOI] [PubMed] [Google Scholar]
- 77.Zwaluw CS, Valentijn SAM, Nieuwenhuis-Mark R, Rasquin SMC, Heugten CM (2011) Cognitive Functioning in the Acute Phase Poststroke: A Predictor of Discharge Destination? J Stroke Cerebrovasc Dis 20(6):549–555. 10.1016/j.jstrokecerebrovasdis.2010.03.009 [DOI] [PubMed] [Google Scholar]
- 78.Lutz BJ (2004) Determinants of Discharge Destination for Stroke Patients. Rehabil Nurs 29(5):154–163. 10.1002/j.2048-7940.2004.tb00338.x [DOI] [PubMed] [Google Scholar]
- 79.Stineman MG, Kwong PL, Bates BE, Kurichi JE, Ripley DC, Xie D (2014) Development and Validation of a Discharge Planning Index for Achieving Home Discharge After Hospitalization for Acute Stroke Among Those Who Received Rehabilitation Services. American Journal of Physical Medicine & Rehabilitation 93(3):217–230 [DOI] [PubMed] [Google Scholar]
- 80.Thorpe ER, Garrett KB, Smith AM, Reneker JC, Phillips RS (2018) Outcome measure scores predict discharge destination in patients with acute and subacute stroke: a systematic review and series of meta-analyses. J Neurol Phys Ther 42(1):2–11 [DOI] [PubMed] [Google Scholar]
- 81.Nguyen T-A, Page A, Aggarwal A, Henke P (2007) Social Determinants of Discharge Destination for Patients After Stroke With Low Admission FIM Instrument Scores. Arch Phys Med Rehabil 88(6):740–744. 10.1016/j.apmr.2007.03.011 [DOI] [PubMed] [Google Scholar]
- 82.Roberts PS, Mix J, Rupp K, Younan C, Mui W, Riggs RV, Niewczyk P (2016) Using Functional Status in the Acute Hospital to Predict Discharge Destination for Stroke Patients. American Journal of Physical Medicine & Rehabilitation 95(6):416–424 [DOI] [PubMed] [Google Scholar]
- 83.Kim M-S, Joo MC, Sohn MK, Lee J, Kim DY, Lee S-G, Shin Y-I, Kim S-Y, Oh G-J, Lee Y-S, Han EY, Han J, Ahn J, Chang WH, Kim Y-H, Choi JY, Hyun Kang S, Kim YT (2020) Development and validation of a prediction model for home discharge in patients with moderate stroke: The Korean stroke cohort for functioning and rehabilitation study. Top Stroke Rehabil 27(6):453–461. 10.1080/10749357.2019.1711338 [DOI] [PubMed] [Google Scholar]
- 84.Chevalley O, Truijen S, Saeys W, Opsommer E (2021) Socio-environmental predictive factors for discharge destination after inpatient rehabilitation in patients with stroke: a systematic review and meta-analysis. Disabil Rehabil 1–12. 10.1080/09638288.2021.1923838 [DOI] [PubMed]
- 85.Gosling AF, Hammer M, Grabitz S, Wachtendorf LJ, Katsiampoura A, Murugappan KR, Sehgal S, Khabbaz KR, Mahmood F, Eikermann M (2021) Development of an instrument for preoperative prediction of adverse discharge in patients scheduled for cardiac surgery. J Cardiothorac Vasc Anesth 35(2):482–489 [DOI] [PubMed] [Google Scholar]
- 86.Lim HJ, Hoffmann R, Brasel K (2007) Factors Influencing Discharge Location After Hospitalization Resulting From a Traumatic Fall Among Older Persons. J Trauma Acute Care Surg 63(4):902–907 [DOI] [PubMed] [Google Scholar]
- 87.Strosberg DS, Housley BC, Vazquez D, Rushing A, Steinberg S, Jones C (2017) Discharge destination and readmission rates in older trauma patients. J Surg Res 207:27–32. 10.1016/j.jss.2016.07.015 [DOI] [PubMed] [Google Scholar]
- 88.Hirota Y, Shin J-H, Sasaki N, Kunisawa S, Fushimi K, Imanaka Y (2023) Development and validation of prediction models for the discharge destination of elderly patients with aspiration pneumonia. PLoS ONE 18(2):0282272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Carter EM, Potts HW (2014) Predicting length of stay from an electronic patient record system: a primary total knee replacement example. BMC Med Inform Decis Mak 14(1):1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hintz SR, Bann CM, Ambalavanan N, Cotten CM, Das A, Higgins RD (2010) Predicting time to hospital discharge for extremely preterm infants. Pediatrics 125(1):146–154. 10.1542/peds.2009-0810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shukla K, Upadhyay S (2018) Predictive Modelling for Turn Around Time (TAT) of Discharge Process for Insured Patients in a Corporate Hospital of Pune City. J Health Manag 20(1):56–63. 10.1177/0972063417747701 [Google Scholar]
- 92.AlAshqar A, Wildey B, Yazdy G, Goktepe ME, Kilic GS, Borahay MA (2022) Predictors of same-day discharge after minimally invasive hysterectomy for benign indications. International Journal of Gynecology & Obstetrics. 158(2):308–317. 10.1002/ijgo.13992 [DOI] [PubMed] [Google Scholar]
- 93.LeBrun DG, Nguyen JT, Fisher C, Tuohy S, Lyman S, Della Valle AG, Ast MP, Carli AV (2023) The risk assessment and prediction tool (rapt) score predicts discharge destination, length of stay, and postoperative mobility after total joint arthroplasty. J Arthroplasty 38(7):121–129 [DOI] [PubMed] [Google Scholar]
- 94.Huang G, Huang G-B, Song S, You K (2015) Trends in extreme learning machines: A review. Neural Netw 61:32–48 [DOI] [PubMed] [Google Scholar]
- 95.Rong G, Mendez A, Assi EB, Zhao B, Sawan M (2020) Artificial intelligence in healthcare: review and prediction case studies. Engineering 6(3):291–301 [Google Scholar]
- 96.Hond AA, Leeuwenberg AM, Hooft L, Kant IM, Nijman SW, Os HJ, Aardoom JJ, Debray T, Schuit E, Smeden M et al (2022) Guidelines and quality criteria for artificial intelligence-based prediction models in healthcare: a scoping review. npj Digital Medicine 5(1): 1–13 [DOI] [PMC free article] [PubMed]
- 97.Bidhandi HM, Patrick J, Noghani P, Varshoei P (2019) Capacity planning for a network of community health services. Eur J Oper Res 275(1):266–279 [Google Scholar]
- 98.Bae K-H, Jones M, Evans G, Antimisiaris D (2019) Simulation modelling of patient flow and capacity planning for regional long-term care needs: a case study. Health Systems. 8(1):1–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Elbattah M, Molloy O (2016) Using machine learning to predict length of stay and discharge destination for hip-fracture patients. Proceedings of SAI Intelligent Systems Conference 207–217
- 100.Karhade AV, Ogink P, Thio Q, Broekman M, Cha T, Gormley WB, Hershman S, Peul WC, Bono CM, Schwab JH (2018) Development of machine learning algorithms for prediction of discharge disposition after elective inpatient surgery for lumbar degenerative disc disorders. Neurosurg Focus 45(5):6 [DOI] [PubMed] [Google Scholar]
- 101.Lu Y, Khazi ZM, Agarwalla A, Forsythe B, Taunton MJ (2021) Development of a Machine Learning Algorithm to Predict Nonroutine Discharge Following Unicompartmental Knee Arthroplasty. J Arthroplasty 36(5):1568–1576. 10.1016/j.arth.2020.12.003 [DOI] [PubMed] [Google Scholar]
- 102.Bertsimas D, Pauphilet J, Stevens J, Tandon M (2021) Predicting inpatient flow at a major hospital using interpretable analytics. Manufacturing & Service Operations Management (October). 10.1287/msom.2021.0971 [Google Scholar]
- 103.Satyadev N, Warman PI, Seas A, Kolls BJ, Haglund MM, Fuller AT, Dunn TW (2022) Machine Learning for Predicting Discharge Disposition After Traumatic Brain Injury. Neurosurgery 90(6):768–774 [DOI] [PubMed] [Google Scholar]
- 104.Mohammed H, Huang Y, Memtsoudis S, Parks M, Huang Y, Ma Y (2022) Utilization of machine learning methods for predicting surgical outcomes after total knee arthroplasty. PLoS ONE 17(3):0263897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Imura T, Iwamoto Y, Inagawa T, Imada N, Tanaka R, Toda H, Inoue Y, Araki H, Araki O (2021) Decision Tree Algorithm Identifies Stroke Patients Likely Discharge Home After Rehabilitation Using Functional and Environmental Predictors. J Stroke Cerebrovasc Dis 30(4):105636. 10.1016/j.jstrokecerebrovasdis.2021.105636 [DOI] [PubMed] [Google Scholar]
- 106.Imura T, Iwamoto Y, Azuma Y, Inagawa T, Imada N, Tanaka R, Araki H, Araki O (2021) Machine Learning Algorithm Identifies the Importance of Environmental Factors for Hospital Discharge to Home of Stroke Patients using Wheelchair after Discharge. J Stroke Cerebrovasc Dis 30(8):105868. 10.1016/j.jstrokecerebrovasdis.2021.105868 [DOI] [PubMed] [Google Scholar]
- 107.Bacchi S, Oakden-Rayner L, Menon DK, Moey A, Jannes J, Kleinig T, Koblar S (2022) Prospective and external validation of stroke discharge planning machine learning models. J Clin Neurosci 96:80–84. 10.1016/j.jocn.2021.12.031 [DOI] [PubMed] [Google Scholar]
- 108.Ikezawa K, Hirose M, Maruyama T, Yuji K, Yabe Y, Kanamori T, Kaide N, Tsuchiya Y, Hara S, Suzuki H (2022) Effect of early nutritional initiation on post-cerebral infarction discharge destination: A propensity-matched analysis using machine learning. Nutrition & Dietetics 79(2):247–254. 10.1111/1747-0080.12718 [DOI] [PubMed] [Google Scholar]
- 109.Morris RS, Tignanelli CJ, DeRoon-Cassini T, Laud P, Sparapani R (2022) Improved Prediction of Older Adult Discharge After Trauma Using a Novel Machine Learning Paradigm. J Surg Res 270:39–48. 10.1016/j.jss.2021.08.021 [DOI] [PubMed] [Google Scholar]
- 110.Mickle CF, Deb D (2022) Early prediction of patient discharge disposition in acute neurological care using machine learning. BMC Health Serv Res 22(1):1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen, T.L.W., Buddhiraju, A., Seo, H.H., Subih, M.A., Tuchinda, P., Kwon, Y.M.: Internal and External Validation of the Generalizability of Machine Learning Algorithms in Predicting Non-home Discharge Disposition Following Primary Total Knee Joint Arthroplasty. Journal of Arthroplasty, 1–9 (2023) 10.1016/j.arth.2023.01.065 [DOI] [PubMed]
- 112.Turgeman L, May JH, Sciulli R (2017) Insights from a machine learning model for predicting the hospital length of stay (los) at the time of admission. Expert Syst Appl 78:376–385 [Google Scholar]
- 113.Kabir S, Farrokhvar L (2019) Non-linear feature selection for prediction of hospital length of stay. In: 2019 18th IEEE International Conference On Machine Learning And Applications (ICMLA), pp. 945–950. IEEE
- 114.Safavi KC, Khaniyev T, Copenhaver M, Seelen M, Zenteno Langle AC, Zanger J, Daily B, Levi R, Dunn P (2019) Development and Validation of a Machine Learning Model to Aid Discharge Processes for Inpatient Surgical Care. JAMA Netw Open 2(12):1917221–1917221. 10.1001/jamanetworkopen.2019.17221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nemati M, Ansary J, Nemati N (2020) Covid-19 machine learning based survival analysis and discharge time likelihood prediction using clinical data. Available at SSRN 3584518 [DOI] [PMC free article] [PubMed]
- 116.Liu P, Lei L, Yin J, Zhang W, Naijun W, El-darzi E (2006) Healthcare Data Mining : Prediction Inpatient Length. (September)
- 117.Gholipour C, Rahim F, Fakhree A, Ziapour B (2015) Using an artificial neural networks (ANNs) model for prediction of intensive care unit (ICU) outcome and length of stay at hospital in traumatic patients. Journal of clinical and diagnostic research: JCDR. 9(4):19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tsai P-FJ, Chen P-C, Chen Y-Y, Song H-Y, Lin H-M, Lin F-M, Huang Q-P (2016) Length of hospital stay prediction at the admission stage for cardiology patients using artificial neural network. Journal of Healthcare Engineering 2016:7035463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Muhlestein WE, Akagi DS, Davies JM, Chambless LB (2019) Predicting inpatient length of stay after brain tumor surgery: developing machine learning ensembles to improve predictive performance. Neurosurgery 85(3):384–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Bacchi S, Oakden-Rayner L, Menon DK, Jannes J, Kleinig T, Koblar S (2020) Stroke prognostication for discharge planning with machine learning: A derivation study. J Clin Neurosci 79:100–103. 10.1016/j.jocn.2020.07.046 [DOI] [PubMed] [Google Scholar]
- 121.He L, Madathil SC, Servis G, Khasawneh MT (2021) Neural network-based multi-task learning for inpatient flow classification and length of stay prediction. Appl Soft Comput 108:107483 [Google Scholar]
- 122.Zhong H, Poeran J, Gu A, Wilson LA, Gonzalez Della Valle A, Memtsoudis SG, Liu J (2021) Machine learning approaches in predicting ambulatory same day discharge patients after total hip arthroplasty. Regional Anesthesia & Pain Medicine 46(9):779–783. 10.1136/rapm-2021-102715 [DOI] [PubMed] [Google Scholar]
- 123.Zeleke AJ, Palumbo P, Tubertini P, Miglio R, Chiari L (2023) Machine learning-based prediction of hospital prolonged length of stay admission at emergency department: a gradient boosting algorithm analysis. Frontiers in Artificial Intelligence 6:1179226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Morton A, Marzban E, Giannoulis G, Patel A, Aparasu R, Kakadiaris IA (2014) A comparison of supervised machine learning techniques for predicting short-term in-hospital length of stay among diabetic patients 428–431
- 125.Luo L, Xu X, Li J, Shen W (2017) Short-term forecasting of hospital discharge volume based on time series analysis. In: 2017 IEEE 19th International Conference on e-Health Networking, Applications and Services (Healthcom), pp. 1–6. 10.1109/HealthCom.2017.8210801
- 126.Van Walraven C, Forster AJ (2018) The TEND (Tomorrow’s Expected Number of Discharges) model accurately predicted the number of patients who were discharged from the hospital the next day. J Hosp Med 13(3):158–163 [DOI] [PubMed] [Google Scholar]
- 127.Lambaudie E, Mathis J, Zemmour C, Jauffret-Fara C, Mikhael ET, Pouliquen C, Sabatier R, Brun C, Faucher M, Mokart D, Houvenaeghel G (2020) Prediction of early discharge after gynaecological oncology surgery within ERAS. Surg Endosc 34(5):1985–1993. 10.1007/s00464-019-06974-w [DOI] [PubMed] [Google Scholar]
- 128.Levin S, Barnes S, Toerper M, Debraine A, DeAngelo A, Hamrock E, Hinson J, Hoyer E, Dungarani T, Howell E (2021) Machine-learning-based hospital discharge predictions can support multidisciplinary rounds and decrease hospital length-of-stay. BMJ Innovations. 7(2):414–421. 10.1136/bmjinnov-2020-000420 [Google Scholar]
- 129.Ghazalbash, S., Zargoush, M., Mowbray, F., Papaioannou, A.: Examining the predictability and prognostication of multimorbidity among older Delayed-Discharge Patients: A Machine learning analytics. International Journal of Medical Informatics. 156, 104597 (2021) 10.1016/j.ijmedinf.2021.104597 [DOI] [PubMed]
- 130.Gramaje A, Thabtah F, Abdelhamid N, Ray SK (2021) Patient Discharge Classification Using Machine Learning Techniques. Annals of Data Science. 8(4):755–767. 10.1007/s40745-019-00223-6 [Google Scholar]
- 131.Ahn I, Gwon H, Kang H, Kim Y, Seo H, Choi H, Cho HN, Kim M, Jun TJ, Kim Y-H (2021) Machine Learning-Based Hospital Discharge Prediction for Patients With Cardiovascular Diseases: Development and Usability Study. JMIR Med Inform 9(11):32662. 10.2196/32662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gao R, Cheng WX, Suganthan P, Yuen KF (2022) Inpatient discharges forecasting for Singapore hospitals by machine learning. IEEE J Biomed Health Inform 1. 10.1109/JBHI.2022.3172956 [DOI] [PubMed]
- 133.Zhao CC, Bjurlin MA, Wysock JS, Taneja SS, Huang WC, Fenyo D, Matulewicz RS (2022) Machine learning decision support model for radical cystectomy discharge planning. Urologic Oncology: Seminars and Original Investigations. 10.1016/j.urolonc.2022.05.026 [DOI] [PubMed]
- 134.Jaotombo F, Pauly V, Fond G, Orleans V, Auquier P, Ghattas B, Boyer L (2023) Machine-learning prediction for hospital length of stay using a french medico-administrative database. Journal of Market Access & Health Policy. 11(1):2149318 [DOI] [PMC free article] [PubMed]
- 135.Thompson B, Elish KO, Steele R (2018) Machine learning-based prediction of prolonged length of stay in newborns. 2018 17th IEEE International Conference on Machine Learning and Applications (ICMLA), 1454–1459
- 136.Gabriel RA, Harjai B, Simpson S, Goldhaber N, Curran BP, Waterman RS (2022) Machine Learning-Based Models Predicting Outpatient Surgery End Time and Recovery Room Discharge at an Ambulatory Surgery Center. Anesthesia & Analgesia 135(1):159–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Geng EA, Gal JS, Kim JS, Martini ML, Markowitz J, Neifert SN, Tang JE, Shah KC, White CA, Dominy CL et al (2023) Robust prediction of nonhome discharge following elective anterior cervical discectomy and fusion using explainable machine learning. Eur Spine J 32(6):2149–2156 [DOI] [PubMed] [Google Scholar]
- 138.West T, Churilov L, Bernhardt J (2013) Early physical activity and discharge destination after stroke: a comparison of acute and comprehensive stroke unit care. Rehabilitation Research and Practice 2013(1):498014 [DOI] [PMC free article] [PubMed]
- 139.Schwarzkopf R, Ho J, Snir N, Mukamel DD (2015) Factors influencing discharge destination after total hip arthroplasty: a California state database analysis. Geriatric orthopaedic surgery & rehabilitation 6(3):215–219 [DOI] [PMC free article] [PubMed]
- 140.Ebell MH, Afonso AM, Geocadin RG, American Heart Association (2013) Prediction of survival to discharge following cardiopulmonary resuscitation using classification and regression trees. Critical care medicine 41(12):2688–2697 [DOI] [PubMed]