Abstract
The Anterior Cruciate Ligament (ACL) is considered the most commonly injured ligament of the knee. Magnetic Resonance Imaging (MRI) has become an indispensable imaging tool and modality of choice for assessing and managing knee conditions. This article outlines an effective MRI imaging technique that improves the diagnostic accuracy of ACL injuries of the knee, covering the appropriate pulse sequences and optimal imaging planes. Furthermore, the article provides a comprehensive review of the appearance of complete and partial ACL tears on MRI in the acute and chronic phases. In addition, it identifies and illustrates the primary MRI signs (signs related to the absence or abnormal visualization of the ACL fibers) and secondary MRI signs (signs related to the mechanism of injury or associated knee injuries) of ACL injury.
Keywords: anterior cruciate ligament, magnetic resonance imaging, partial ACL tear, complete ACL tear
Introduction
The anterior cruciate ligament (ACL) is considered to be one of the most frequently injured ligaments of the knee, with ACL tears accounting for approximately half of all sport-related knee injuries in the United States.1–3 Early and accurate diagnosis of ACL tear and subsequent treatment could potentially prevent the onset of cartilage degeneration, progression of traumatic arthritis, or development of functional impairment of the knee joint.
In the case of ACL injury, knee radiographs are commonly negative or may demonstrate indirect signs of injury, such as anterior tibial translation, Segond fracture and lateral femoral sulcus sign, thus have limited value in the diagnosis of ACL tears.4,5
During physical examination, most experienced clinicians are able to accurately diagnose ACL injury using clinical tests such as the anterior drawer, Lachman, and pivot –shift tests.1,6 However, in the case of acute injury and a swollen knee, these tests may be challenging to perform because of knee pain. Furthermore, the diagnosis of ACL tear depends on the clinician’s experience and patient cooperation. In such cases, Magnetic Resonance Imaging (MRI) plays a vital role in supporting the clinical suspicion.
MRI allows for a more comprehensive imaging assessment and evaluation of the ligaments and menisci of the knee, determination of the ACL condition, and description of concurrent knee injuries.7–9 The literature has shown variation in the reported sensitivity (63–100%) and specificity (68–100%) of MRI in diagnosing ACL tears,10–12 variability that can be attributed to the slightly oblique angle at which the ACL passes the knee joint, and the challenge of displaying the entire ACL in the true sagittal plane using a single MRI scan.12 Other studies have reported that MRI can surpass the accuracy of clinical examination by detecting ACL tears that were not diagnosed during clinical examination but were confirmed arthroscopically.13
The identification of a torn ACL relies on observing abnormalities in the ligament itself, including disruption of continuity in its fibers, wavy contour of the ligament, and presence of high signal intensity within the ACL.14 Several indirect (secondary) MRI signs have been described in the literature and are recommended to improve the accuracy of reporting the ACL condition.3,14,15
In this article, our aim is to conduct a comprehensive review of ACL features on MRI, offering a helpful resource for the diagnosis of ACL injuries.
ACL Anatomy
The ACL is an intra-articular, extrasynovial ligament that moves in the oblique direction from the posteromedial aspect of the lateral condyle of the femur and inserts distally in the anterior intercondylar region of the proximal tibia.1,6 It’s function is to provide rotational stability to the knee and prevent anterior tibial translation during knee extension.16,17
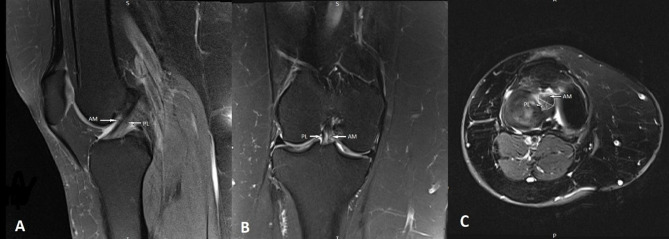
The normal ACL appears as a straight fiber band parallel to the intercondylar roof, consisting of two components named according to their tibial insertion sites: a longer anteromedial (AM) bundle and a shorter posterolateral (PL) bundle. The ACL has a wider tibial insertion than its femoral origin, fanning out, and a heterogeneous appearance between the AM and PL bundles distally through the intercondylar notch, allowing them to be distinguished from each other on axial, sagittal, and coronal cross-sectional images.18 (Figure 1 demonstrates a normal ACL appearance on an MRI scan, showing distinctively the AM and PL bundles in the A, sagittal, B, coronal, and C, axial planes). Usually, the posterolateral bundle has a higher signal intensity on MRI than the anteromedial bundle.6 Furthermore, there is a functional distinction between the two bundles. The AM bundle is maximally taut in flexion and serves to limit anterior tibial translation during flexion, whereas the PL bundle is maximally taut in extension and serves to limit the anterior tibial translation during extension and tibial rotation.18,19
Figure 1.
Normal anterior cruciate ligament anatomy in which the AM and PL bundles are clearly delineated from each other; (A) sagittal proton density (PD) weighted fat suppressed image demonstrating the normal ACL, characterized by taut, continuous, low intensity ACL fibers, (B) coronal T2 weighted fat suppressed image, and (C) axial T2 weighted fat suppressed knee MRI image that shows the AM and PL footprint.
Knee MRI Imaging Technique
MRI has been used extensively for imaging internal derangements and knee joint disorders. Knee MRI should be tailored to the specifics of each type of knee disorder to optimize the benefits of examination. However, the choice of MRI pulse sequence may be affected by the available equipment, software limitations, and clinician preference.20,21
Several magnet designs, such as closed-bore or open-bore magnets, in addition to different magnetic field strengths, can be used for imaging the knee. The accuracy of 1.5T MRI scanner or lower field strength in diagnosing partial ACL tears ranges from 25%-53%.22,23 However, a 3T MRI scanner has been demonstrated to have an accuracy of up to 95% in diagnosing partial ACL tears.24 Furthermore, a specialized extremity coil is necessary to maximize image quality. An appropriate field of view (FOV) usually tailored to the size of the knee (typically 16 cm) should be used to improve image resolution.25 A slice thickness of 4 mm or less and a small inter-slice gap (not more than 0.4 mm) are required to demonstrate the presence of subtle pathology.1,25 The patient is placed in a supine position with the knee extended inside the extremity coil. In case of an ACL injury investigation, external rotation from 5°to 10°of the knee will position the ACL orthogonal to the sagittal plane.1
The knee MRI protocol usually consists of sagittal, coronal, and axial imaging planes and starts with the acquisition of scout images in these planes. Axial slices are obtained directly from the scout images. When locating the sagittal images, an anatomical landmark, the lateral femoral epicondyle at the level of the lateral collateral ligament, is being used to ensure visualization of the ACL.26 Poor visualization of the normal ACL on sagittal images has been reported in 5–10% of patients,27 requiring additional planes to improve its identification.
Studies have shown that oblique sagittal and coronal planes may be acquired for optimal demonstration of the ACL and to improve the diagnostic accuracy of ACL injury.28–32 Oblique coronal sequences increase the sensitivity and specificity for diagnosing isolated AM or PL bundle injuries.31 By applying thin slices (2.5 mm slice thickness), the two bundles can be differentiated as separate entities.26 Moreover, the oblique coronal plane aids in visualizing the proximal insertion of bundles for hemorrhage and rupture.33 A coronal oblique sequence is obtained in the long axis of the ACL, starting at the intercondylar roof or the Blumensaat’s line.33
The knee MRI protocol uses a combination of pulse sequences such as spin echo, fast or turbo spin echo, and gradient echo sequences. However, the desired contrast weighting of the images governs the repetition time (TR), time to echo (TE), and flip angle chosen for the exam.25 The T2 weighted fat suppressed (FS) or proton density (PD)-weighted FS sequences are used to demonstrate fluid as a high-intensity signal, better outlining edema, hemorrhage, and effusion, which commonly accompany ACL injuries.34 T1 weighted images are most commonly performed without fat suppression and are suitable for delineating anatomical structures.34
Primary Signs of Acute and Chronic ACL Tears
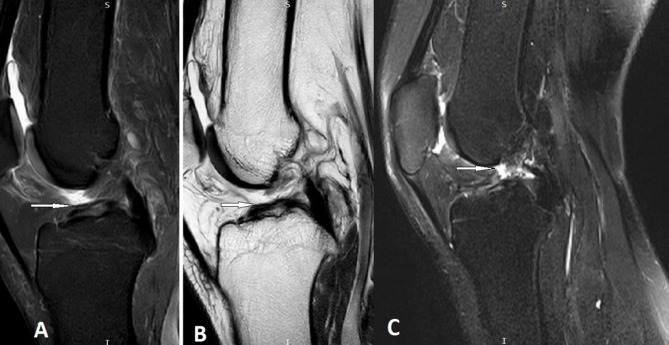
The literature supports MRI as a highly accurate diagnostic modality for complete ACL tears, with a sensitivity of 83% to 100% and a specificity of 96% to 100%.24,35–39 In the case of an acute complete ACL tear, these direct signs include failure to visualize the ACL fibers on images taken in any plane or discontinuity of the ligament (interruption of the ACL fibers seen on two different imaging planes). Another sign is the presence of an abnormal morphology characterized by an irregular or wavy contour of the ACL or an abnormal orientation of the ACL fibers. As such, ACL fibers are not parallel to the intercondylar notch roof or running more parallel to the tibial plateau7,14,15 (Figure 2). The orientation of ACL fibers can be objectively measured, as described by Gentili et al3 in two ways. First, the ACL angle is measured between a line running along the anterior surface of the ACL and a second line running parallel to the mid-lateral tibial plateau. An angle of less than 45° is considered abnormal. In the second method, the ACL-Blumensaat line angle is measured between the anterior surface of the ACL fibers and a line running at the posterior surface of the femur (Blumensaat line). In such cases, an ACL-Blumensaat line angle of greater than 9° is considered abnormal (Appendix 1).
Figure 2.
Complete ACL injury; (A) proton density weighted fat suppressed sagittal image and (B) T2 weighted fat suppressed sagittal image both demonstrate abnormal angulation of anterior cruciate ligament fibers (white arrows). (C) T2 weighted fat suppressed sagittal image showing mid-substance rupture of ACL fibers (white arrow).
Approximately 28% of all ACL tears are partial tears that may occur in the AM or PL bundles.40 The sensitivity (40–77%) and specificity (51–97%) of MRI are lower for detecting partial than complete ACL tears.22,24,41 Partial tears are suspected if the ligament appears thickened with a T2 weighted hyperintense signal (Figure 3), the ACL is of normal thickness with continuous fibers and abnormal signal intensity, or abnormal ACL morphology with intact ACL fibers or partial discontinuity.1,19,22,24 Continuous fibers being visible suggest that the tear in the ACL is not complete.
Figure 3.
Partial ACL tear; (A) T2 weighted fat suppressed sagittal image demonstrates thickened fibers with increased signal intensity within the anterior cruciate ligament (white arrow). (B) T2 SPAIR coronal image showing AM bundle tear (white arrow).
Chronic ACL tears have a more variable appearance on MRI, which occasionally makes it more difficult to detect this type of injury. This is likely attributable to the fact that some signs that were present in the acute stage of the injury, such as edema and ACL fiber thickening, may have substantially decreased at the time of examination. In chronic complete ACL tear, the ACL may appear absent, demonstrating an empty notch sign where the ACL has been replaced by fluid42 (Figure 4 shows the appearance of an empty notch sign). Occasionally, a chronic tear is replaced by fibrous scar tissue that resembles an intact ligament with a hypointense signal that connects the expected origin and insertion of the ACL.43 Sometimes, the proximal fibers of the torn ACL attach to the Posterior Cruciate Ligament PCL and display abnormal angulations.1,43 In such cases, Gentili et al reported no significant difference in the ACL-Blumensaat line angle between acute and chronic ACL tears.3
Figure 4.

In this T1 weighted coronal image, an empty lateral wall (white arrow) is observed (empty notch sign), which may indicate chronic ACL injury.
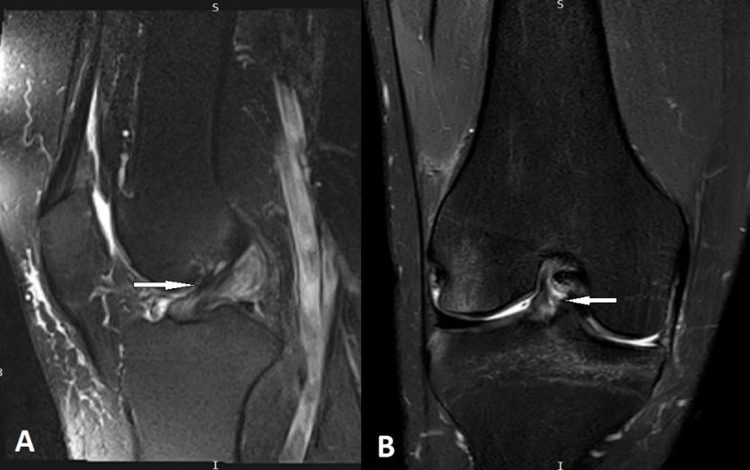
Secondary or Indirect Signs of ACL Tear
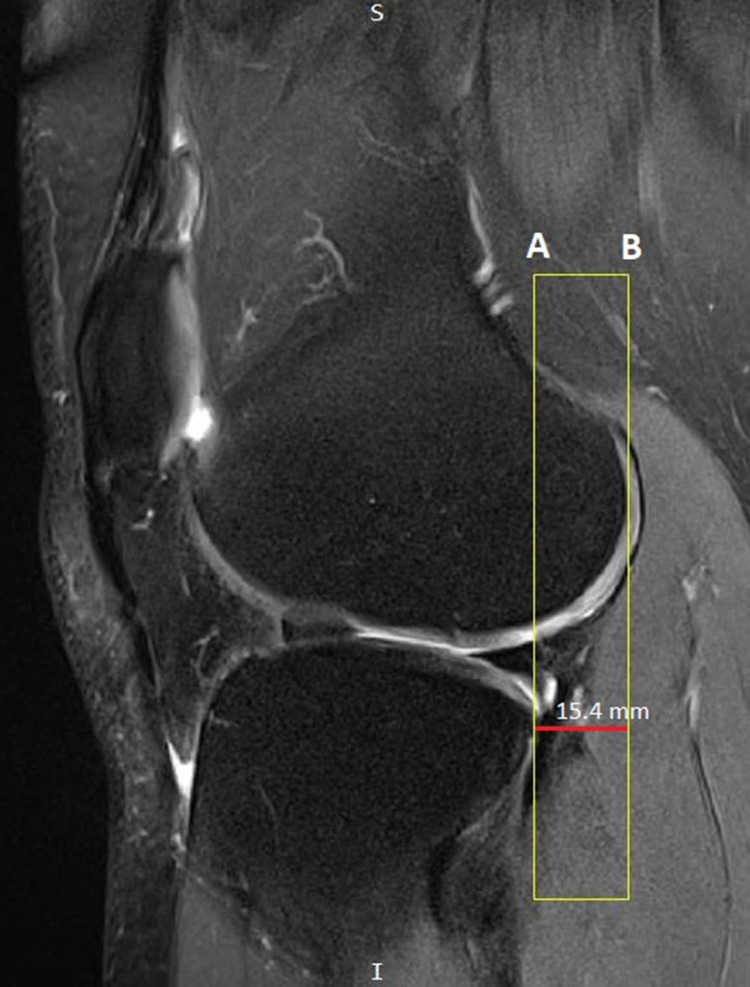
Various secondary signs associated with ACL tears have been previously described. These signs are related to the mechanism of injury or the associated knee injuries that occur because of ACL tears. Anterior tibial subluxation, also known as the anterior drawer sign, is seen in cases of complete ACL tear and is defined as the anterior translocation of the tibia relative to the femur, measured at the midsagittal plane of the lateral femoral condyle.44 Two lines parallel to the craniocaudal axis of the image are drawn (Figure 5): one that crosses the most posterior point of the posterolateral tibial plateau and the second line crossing the most posterior point of the lateral femoral condyle. The distance between the two lines is then measured. An anterior translocation equal to 3.5 mm has indicated an ACL tear with 55.2% sensitivity and 100% specificity,45 greater than 5 mm has a sensitivity ranging from 58% to 86% and a specificity of 93%–99%,44,46 while a translocation of 7 mm or more has been considered a complete diagnostic sign of an ACL tear.34 As a consequence of anterior tibial subluxation, the posterior horn of the lateral meniscus may be unveiled, in addition to complete visualization of the lateral collateral ligament (LCL) on a single coronal image.34
Figure 5.
Proton density weighted fat suppressed sagittal image demonstrates anterior tibial translation in association with ACL injury; line (A) is crossing the most posterior point of the posterolateral tibial plateau and is parallel to line (B) which is crossing the most posterior point of the lateral femoral condyle. The distance between these two lines is 15.4mm, indicating an ACL tear of the knee.
Among the secondary findings of ACL tear that occur in cases of pivot shift mechanism of injury is the deep femoral notch sign, which is also known as the sulcus sign. It is defined as a depression on the lateral femoral condyle that occurs due to bone impaction between the terminal sulcus of the lateral femoral condyle and posterolateral tibial plateau during rotational movement. It has been demonstrated that a notch depth of at least 2 mm is a reliable indirect sign of ACL tear.47 This is measured by drawing a tangent line that connects the anterior and posterior borders of the femoral notch across the sulcus on the articular surface of the femoral condyle to the deepest point of the sulcus.
Another indirect sign of an ACL tear is bone contusion, which can be detected as abnormal bone marrow signal intensity (Figure 6; reduced signal intensity on T1 weighted images and increased signal intensity on T2 and PD weighted images).34,48–51 Bone contusions can be seen in the mid-to-anterior portion of the lateral femoral condyle and posterolateral aspect of the tibial plateau. This pattern of contusion is commonly caused by a sudden forceful pivoting moment, external rotation, and a valgus impact between the posterior aspect of the tibial plateau and lateral femoral condyle.
Figure 6.
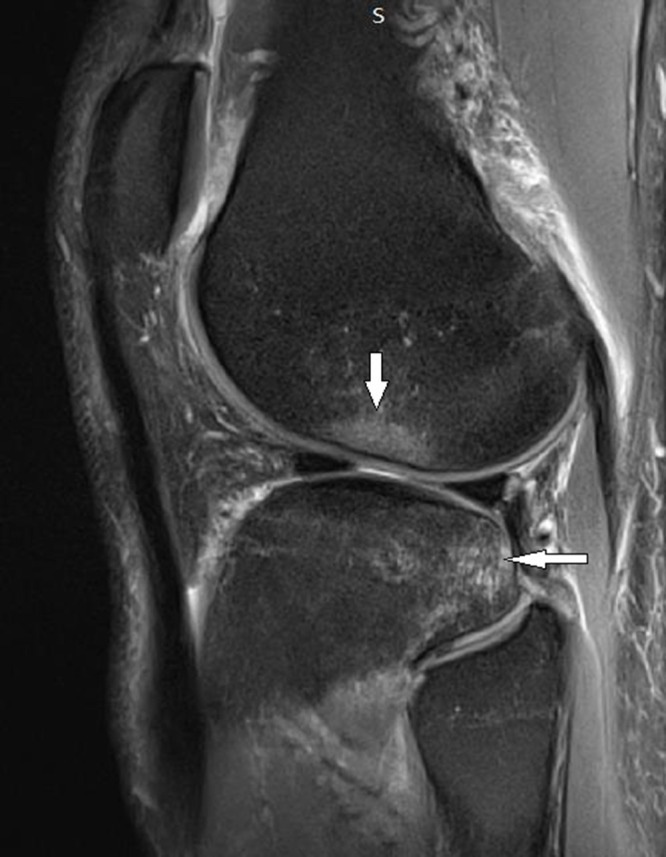
In this proton density weighted sagittal image, bone contusion pattern is observed (white arrows), associated with ACL injury.
Segond fractures, osseous avulsion fractures of the anterior lateral ligament (ALL) from the lateral tibial rim, are also associated with ACL tears.34 The incidence of Segond fracture has been reported in 2.4% of cases with ACL injuries and is usually associated with higher probability of concomitant lateral meniscal tear.52 Focal bone marrow edema adjacent to the fracture location can be observed, emitting an abnormal MRI signal.53
Secondary changes in the PCL, such as decreased posterior cruciate ligament angle or PCL buckling (Figure 7) 48,54 have also been observed in ACL tears. The PCL angle is measured by drawing lines through the central portion of the tibial insertion and the femoral insertion of the PCL. If the angle is less than 105°, it is considered a positive sign of ACL tear.55 Yang et al, found that measuring the angle of the inferior portion of PCL can enhance the diagnosis of partial ACL tears.56
Figure 7.
Proton density weighted sagittal image of the knee showing posterior cruciate ligament (PCL) buckling with decreased PCL angle in complete ACL injury.
Another sign highly suggestive of an ACL tear is an occult fracture of the posterior lateral tibial plateau with or without an associated fracture of the lateral femoral condyle.15,50 An increased femorotibial angle of 4.9° or greater57 are also secondary signs that may indicate ACL injury.
A number of factors or conditions may affect the accuracy of MRI diagnosis of partial ACL tear. First, using suboptimal imaging protocol may reduce image resolution and quality, hindering the diagnostic process.12 Second, minor partial tears which may cause only subtle changes in the appearance of the ACL can lead to false negative findings.2 Third, MRI may have limited value in accurately diagnosing ACL tear in the presence of multi ligament knee injuries.58
Conclusion
An understanding of the normal appearance of the anterior cruciate ligament on MRI and the direct and indirect signs of complete and partial ACL tears on MRI is essential for the accurate identification, diagnosis, and assessment of ACL injury.
Funding Statement
The authors would like to acknowledge the receipt of funding from Jordan University of Science and Technology, grant number 20230118.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kam C, Chee DW, Peh WC. Magnetic resonance imaging of cruciate ligament injuries of the knee. Canad Associat Radiolog Jl. 2010;61(2):80–89. doi: 10.1016/j.carj.2009.11.003 [DOI] [PubMed] [Google Scholar]
- 2.Shu HT, Wegener NR, Connors KM, et al. Accuracy of magnetic resonance imaging in predicting anterior cruciate ligament tear location and tear degree. J Orthopaed. 2021;25:129–133. doi: 10.1016/j.jor.2021.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gentili A, Seeger LL, Yao L, Do HM. Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology. 1994;193(3):835–840. doi: 10.1148/radiology.193.3.7972834 [DOI] [PubMed] [Google Scholar]
- 4.Kong AP, Robbins RM, Stensby JD, Wissman RD. The lateral knee radiograph: a detailed review. J Knee Surg. 2022;35(05):482–490. doi: 10.1055/s-0041-1741391 [DOI] [PubMed] [Google Scholar]
- 5.Gottsegen CJ, Eyer BA, White EA, Learch TJ, Forrester D. Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics. 2008;28(6):1755–1770. doi: 10.1148/rg.286085503 [DOI] [PubMed] [Google Scholar]
- 6.WHA N, Griffith JF, Hung EHY, Paunipagar B, Law BKY, Yung PSH. Imaging of the anterior cruciate ligament. World J Orthoped. 2011;2(8):75. doi: 10.5312/wjo.v2.i8.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brandser E, Riley M, Berbaum K, El-Khoury G, Bennett D. MR imaging of anterior cruciate ligament injury: independent value of primary and secondary signs. AJR. 1996;167(1):121–126. doi: 10.2214/ajr.167.1.8659355 [DOI] [PubMed] [Google Scholar]
- 8.Zhao M, Zhou Y, Chang J, et al. The accuracy of MRI in the diagnosis of anterior cruciate ligament injury. Ann Translat Med. 2020;8(24):1657. doi: 10.21037/atm-20-7391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sindhura P, Suneetha P, Venkatesh M, Bhaskarini VU. A prospective study of MRI (3 Tesla) evaluation of traumatic anterior cruciate ligament injuries with arthroscopy correlation. Int J Contemp Med Surg Radiol. 2019;4(4). doi: 10.21276/ijcmsr.2019.4.4.7 [DOI] [Google Scholar]
- 10.Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkiewicz P. The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. Knee Surg Sports Traumatol Arthrosc. 2007;15:533–536. doi: 10.1007/s00167-006-0259-7 [DOI] [PubMed] [Google Scholar]
- 11.Grubor P, Asotic A, Grubor M, Asotic M. Validity of magnetic resonance imaging in knee injuries. Acta Inform Med. 2013;21(3):200. doi: 10.5455/aim.2013.21.200-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li K, Du J, Huang L-X, Ni L, Liu T, Yang H-L. The diagnostic accuracy of magnetic resonance imaging for anterior cruciate ligament injury in comparison to arthroscopy: a meta-analysis. Sci Rep. 2017;7(1):7583. doi: 10.1038/s41598-017-08133-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kulwin RL, Schmidt GJ, Snyder DA, Klitzman RG. Clinical examination in the diagnosis of anterior cruciate ligament injury: a blinded, cross-sectional evaluation. JAAOS: Global Research and Reviews. 2023;7(2). doi: 10.5435/JAAOSGlobal-D-22-00123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prasad JR, Priyadarshini R, Davra SV. Anterior cruciate ligament tears: primary and secondary signs at MR imaging; 2021.
- 15.Tung GA, Davis LM, Wiggins ME, Fadale PD. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993;188(3):661–667. doi: 10.1148/radiology.188.3.8351329 [DOI] [PubMed] [Google Scholar]
- 16.Takai S, Woo SLY, Livesay GA, Adams DJ, Fu FH. Determination of the in situ loads on the human anterior cruciate ligament. J Orthop Res. 1993;11(5):686–695. doi: 10.1002/jor.1100110511 [DOI] [PubMed] [Google Scholar]
- 17.Gabriel MT, Wong EK, Woo SLY, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22(1):85–89. doi: 10.1016/S0736-0266(03)00133-5 [DOI] [PubMed] [Google Scholar]
- 18.Naraghi AM, White LM. Imaging of athletic injuries of knee ligaments and menisci: sports imaging series. Radiology. 2016;281(1):23–40. doi: 10.1148/radiol.2016152320 [DOI] [PubMed] [Google Scholar]
- 19.DeFranco MJ, Bach BR Jr. A comprehensive review of partial anterior cruciate ligament tears. JBJS. 2009;91(1):198–208. doi: 10.2106/JBJS.H.00819 [DOI] [PubMed] [Google Scholar]
- 20.Arnold TC, Freeman CW, Litt B, Stein JM. Low‐field MRI: clinical promise and challenges. J Magn Reson Imaging. 2023;57(1):25–44. doi: 10.1002/jmri.28408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Germann C, Marbach G, Civardi F, et al. Deep convolutional neural network–based diagnosis of anterior cruciate ligament tears: performance comparison of homogenous versus heterogeneous knee MRI cohorts with different pulse sequence protocols and 1.5-T and 3-T magnetic field strengths. Investigat Radiol. 2020;55(8):499–506. doi: 10.1097/RLI.0000000000000664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Umans H, Wimpfheimer O, Haramati N, Applbaum Y, Adler M, Bosco J. Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. AJR. 1995;165(4):893–897. doi: 10.2214/ajr.165.4.7676988 [DOI] [PubMed] [Google Scholar]
- 23.Van Dyck P, De Smet E, Veryser J, et al. Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20:256–261. doi: 10.1007/s00167-011-1617-7 [DOI] [PubMed] [Google Scholar]
- 24.Van Dyck P, Vanhoenacker FM, Gielen JL, et al. Three tesla magnetic resonance imaging of the anterior cruciate ligament of the knee: can we differentiate complete from partial tears? Skel Radiol. 2011;40:701–707. doi: 10.1007/s00256-010-1044-8 [DOI] [PubMed] [Google Scholar]
- 25.Radiology ACo. ACR–SPR–SSR practice parameter for the performance and interpretation of magnetic resonance imaging (MRI) of the knee; 2014.
- 26.Casagranda BC, Maxwell NJ, Kavanagh EC, Towers JD, Shen W, Fu FH. Normal appearance and complications of double-bundle and selective-bundle anterior cruciate ligament reconstructions using optimal MRI techniques. Am J Roentgenol. 2009;192(5):1407–1415. doi: 10.2214/AJR.08.1185 [DOI] [PubMed] [Google Scholar]
- 27.Fitzgerald SW, Remer EM, Friedman H, Rogers LF, Hendrix RW, Schafer MF. MR evaluation of the anterior cruciate ligament: value of supplementing sagittal images with coronal and axial images. AJR. 1993;160(6):1233–1237. doi: 10.2214/ajr.160.6.8498224 [DOI] [PubMed] [Google Scholar]
- 28.Buckwalter K, Pennes D. Anterior cruciate ligament: oblique sagittal MR imaging. Radiology. 1990;175(1):276–277. doi: 10.1148/radiology.175.1.2315495 [DOI] [PubMed] [Google Scholar]
- 29.Hong SH, Choi J-Y, Lee GK, Choi J-A, Chung HW, Kang HS. Grading of anterior cruciate ligament injury: diagnostic efficacy of oblique coronal magnetic resonance imaging of the knee. J Comput Assist Tomograp. 2003;27(5):814–819. doi: 10.1097/00004728-200309000-00022 [DOI] [PubMed] [Google Scholar]
- 30.Breitenseher MJ, Mayerhoefer ME. Oblique MR imaging of the anterior cruciate ligament based on three‐dimensional orientation. J Magn Reson Imaging. 2007;26(3):794–798. doi: 10.1002/jmri.20922 [DOI] [PubMed] [Google Scholar]
- 31.Duc S, Zanetti M, Kramer J, Käch K, Zollikofer C, Wentz K. Magnetic resonance imaging of anterior cruciate ligament tears: evaluation of standard orthogonal and tailored paracoronal images. Acta Radiol. 2005;46(7):729–733. doi: 10.1080/02841850500215907 [DOI] [PubMed] [Google Scholar]
- 32.Katahira K, Yamashita Y, Takahashi M, et al. MR imaging of the anterior cruciate ligament: value of thin slice direct oblique coronal technique. Radiat Med. 2001;19(1):1–7. [PubMed] [Google Scholar]
- 33.Araujo P, van Eck CF, Torabi M, Fu FH. How to optimize the use of MRI in anatomic ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1495–1501. doi: 10.1007/s00167-012-2153-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chien A, Weaver JS, Kinne E, Omar I. Magnetic resonance imaging of the knee. Polish J Radiol. 2020;85(1):509–531. doi: 10.5114/pjr.2020.99415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heron CW, Calvert PT. Three-dimensional gradient-echo MR imaging of the knee: comparison with arthroscopy in 100 patients. Radiology. 1992;183(3):839–844. doi: 10.1148/radiology.183.3.1584944 [DOI] [PubMed] [Google Scholar]
- 36.Mink JH, Levy T, Crues J. Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology. 1988;167(3):769–774. doi: 10.1148/radiology.167.3.3363138 [DOI] [PubMed] [Google Scholar]
- 37.Kijowski R, Rosas H, Samsonov A, King K, Peters R, Liu F. Knee imaging: rapid three‐dimensional fast spin‐echo using compressed sensing. J Magn Reson Imaging. 2017;45(6):1712–1722. doi: 10.1002/jmri.25507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yoon Y, Kim S, Chung H, Choe B, Ahn J. Diagnostic efficacy in knee MRI comparing conventional technique and multiplanar reconstruction with one-millimeter FSE PDW images. Acta Radiol. 2007;48(8):869–874. doi: 10.1080/02841850701459791 [DOI] [PubMed] [Google Scholar]
- 39.Ha TP, Li K, Beaulieu CF, et al. Anterior cruciate ligament injury: fast spin-echo MR imaging with arthroscopic correlation in 217 examinations. AJR. 1998;170(5):1215–1219. doi: 10.2214/ajr.170.5.9574587 [DOI] [PubMed] [Google Scholar]
- 40.Tjoumakaris FP, Donegan DJ, Sekiya JK. Partial tears of the anterior cruciate ligament: diagnosis and treatment. Am J Orthop Belle Mead NJ. 2011;40(2):92–97. [PubMed] [Google Scholar]
- 41.Yao L, Gentili A, Petrus L, Lee JK. Partial ACL rupture: an MR diagnosis? Skel Radiol. 1995;24(4):247–251. doi: 10.1007/BF00198407 [DOI] [PubMed] [Google Scholar]
- 42.Chen W-T, Shih T-F, H-Y T, Chen R-C, Shau W-Y. Partial and complete tear of the anterior cruciate ligament: direct and indirect MR signs. Acta Radiol. 2002;43(5):511–516. [PubMed] [Google Scholar]
- 43.Vahey TN, Broome D, Kayes K, Shelbourne K. Acute and chronic tears of the anterior cruciate ligament: differential features at MR imaging. Radiology. 1991;181(1):251–253. doi: 10.1148/radiology.181.1.1887042 [DOI] [PubMed] [Google Scholar]
- 44.Vahey TN, Hunt JE, Shelbourne KD. Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology. 1993;187(3):817–819. doi: 10.1148/radiology.187.3.8497637 [DOI] [PubMed] [Google Scholar]
- 45.Hardy A, Klouche S, Szarzynski P, et al. A threshold value of 3.5 mm of passive anterior tibial subluxation on MRI is highly specific for complete ACL tears. Knee Surg Sports Traumatol Arthrosc. 2019;27:885–892. doi: 10.1007/s00167-018-5159-0 [DOI] [PubMed] [Google Scholar]
- 46.Chan W, Peterfy C, Fritz R, Genant H. MR diagnosis of complete tears of the anterior cruciate ligament of the knee: importance of anterior subluxation of the tibia. AJR. 1994;162(2):355–360. doi: 10.2214/ajr.162.2.8310927 [DOI] [PubMed] [Google Scholar]
- 47.Berthold DP, Muench LN, Herbst E, et al. High prevalence of a deep lateral femoral notch sign in patients with anterior cruciate ligament (ACL) and concomitant posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2021;29:1018–1024. doi: 10.1007/s00167-020-06071-9 [DOI] [PubMed] [Google Scholar]
- 48.Chang MJ, Chang CB, Choi J-Y, Je MS, Kim TK. Can magnetic resonance imaging findings predict the degree of knee joint laxity in patients undergoing anterior cruciate ligament reconstruction? BMC Musculoskel Disord. 2014;15(1):1–12. doi: 10.1186/1471-2474-15-214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klass D, Toms AP, Greenwood R, Hopgood P. MR imaging of acute anterior cruciate ligament injuries. Knee. 2007;14(5):339–347. doi: 10.1016/j.knee.2007.04.008 [DOI] [PubMed] [Google Scholar]
- 50.Kaplan PA, Walker CW, Kilcoyne RF, Brown D, Tusek D, Dussault R. Occult fracture patterns of the knee associated with anterior cruciate ligament tears: assessment with MR imaging. Radiology. 1992;183(3):835–838. doi: 10.1148/radiology.183.3.1584943 [DOI] [PubMed] [Google Scholar]
- 51.Yoon KH, Yoo JH, Kim K-I. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. JBJS. 2011;93(16):1510–1518. doi: 10.2106/JBJS.J.01320 [DOI] [PubMed] [Google Scholar]
- 52.Yeo PY, Seah AMJ, Visvalingam V, et al. Anterior cruciate ligament rupture and associated Segond fracture: incidence and effect on associated ligamentous and meniscal injuries. Asia Pacif J Sport Med Arthros Rehabilit Technol. 2022;30:36–40. doi: 10.1016/j.asmart.2022.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weber WN, Neumann CH, Barakos JA, Petersen SA, Steinbach LS, Genant HK. Lateral tibial rim (Segond) fractures: MR imaging characteristics. Radiology. 1991;180(3):731–734. doi: 10.1148/radiology.180.3.1871286 [DOI] [PubMed] [Google Scholar]
- 54.Schweitzer ME, Cervilla V, Kursunoglu-Brahme S, Resnick D. The PCL line: an indirect sign of anterior cruciate ligament injury. Clin Imaging. 1992;16(1):43–48. doi: 10.1016/0899-7071(92)90090-V [DOI] [PubMed] [Google Scholar]
- 55.McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P. MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR. 1994;162(1):115–119. doi: 10.2214/ajr.162.1.8273648 [DOI] [PubMed] [Google Scholar]
- 56.Yang Y, Zheng B, Zhang M, et al. The angle of the lower portion of the posterior cruciate ligament assists in the diagnosis of partial anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 2024. doi: 10.1002/ksa.12346 [DOI] [PubMed] [Google Scholar]
- 57.Vassalou EE, Klontzas ME, Kouvidis GK, Matalliotaki PI, Karantanas AH. Rotational knee laxity in anterior cruciate ligament deficiency: an additional secondary sign on MRI. Am J Roentgenol. 2016;206(1):151–154. doi: 10.2214/AJR.15.14816 [DOI] [PubMed] [Google Scholar]
- 58.Li X, Hou Q, Zhan X, Chang L, Ma X, Yuan H. The accuracy of MRI in diagnosing and classifying acute traumatic multiple ligament knee injuries. BMC Musculosk Disord. 2022;23:1–7. doi: 10.1186/s12891-021-04954-7 [DOI] [PMC free article] [PubMed] [Google Scholar]