Abstract
Objective: To investigate the epidemiological patterns of respiratory infectious diseases in Jinan from 2021 to 2023 and to elucidate the relationship among these diseases, meteorological factors, and air pollution. Methods: We conducted a retrospective analysis of outpatient and inpatient data related to respiratory infectious diseases recorded by the Jinan Health Care Development Center from 2021 to 2023. Additionally, we gathered data on outdoor air pollution indicators and meteorological variables from 14 environmental monitoring stations in Jinan. A generalized Poisson regression model for time series analysis was employed to examine the correlation between meteorological factors, air pollution levels, and hospitalization rates for respiratory infectious diseases. Results: From 2021 to 2023, the daily average concentrations of atmospheric pollutants sulfur dioxide (SO2), nitrogen dioxide (NO2), and carbon monoxide (CO) adhered to the national air quality standards, while the daily average concentrations of inhalable particulate matter (PM10) and fine particulate matter (PM2.5) exceeded the national first-class limits. The daily average concentration of ozone (O3) surpassed the national secondary standard, indicating severe O3 pollution. Regarding respiratory disease patients, the relative risk (RR) values of PM10, PM2.5, SO2, NO2, and CO were highest at a lag of 07 d. Compared to other age groups, PM2.5, SO2, NO2, and CO had a more significant impact on respiratory disease treatment on children aged 0-12, while PM10 significantly affected individuals aged 60 and above. In the single pollution model, RR values corresponding to PM10, PM2.5, SO2, CO, and NO2 were 1.008, 1.058, 1.224, 1.405, and 1.102 respectively on lag07d. The multi-pollutant model maintained the positive relationship between the total hospitalization frequency of respiratory diseases and CO, NO2, SO2, PM10, and PM2.5. Conclusion: Our study found a strong, positive correlation with a lag effect between total number of hospitalizations for common respiratory diseases and pollutants CO, NO2, SO2, PM10, and PM2.5 in the examined sample.
Keywords: Outdoor air pollution, meteorological factors, respiratory infectious diseases, number of hospital visits, correlation
Introduction
Environmental risk factors play a pivotal role for human health. Among these, outdoor air pollution stands as a prominent threat. According to the 2019 Global Burden of Disease (GBD) study, outdoor air pollution ranks as the fourth leading cause of mortality worldwide, accounting for approximately 6.67 million deaths annually, thereby eliciting unprecedented societal concern regarding its detrimental health effects [1]. Extensive research by international scholars has highlighted the adverse impact of air pollution on numerous non-communicable diseases, such as lung cancer, stroke, ischemic heart disease, respiratory infections, and chronic obstructive pulmonary disease [2-7].
China, in recent years, has undergone rapid industrialization, which has unfortunately been accompanied by a marked deterioration in air quality. Among the various outdoor air pollutants, haze poses the most significant challenge, primarily comprising particulate matter (PM10 and PM2.5) [8]. Specifically, inhalable particulate matter (PM10) predominantly accumulates in the upper respiratory tract, whereas fine particulate matter (PM), with its smaller size, can penetrate deeper into the body, reaching the trachea, alveoli, and even circulating in the bloodstream, thereby predisposing individuals to cardiovascular and respiratory diseases [9-11].
For many years, numerous studies have documented air quality findings across various cities and regions in China. Given the disparity in meteorological conditions and air pollution levels across these areas, their health impacts may vary significantly [12]. Jinan, as the provincial capital of Shandong Province, functions as a political, cultural, transportation, and economic hub, and is also emblematic of severe air pollution challenges in North China. Since the inception of China’s Clean Air Action in 2013, Jinan has made notable strides in mitigating key air quality pollutants [13].
Nevertheless, prior research on Jinan’s air pollution overlooked the intricate interplay between air quality, meteorological factors, and respiratory infectious diseases [14]. Furthermore, during the COVID-19 pandemic, cities experienced enforced lockdowns, creating a relatively “simplified” living environment for urban dwellers.
Hence, this study endeavored to elucidate the temporal variations of outdoor air pollutants in Jinan from 2021 to 2023 and the influence of meteorological factors on respiratory infectious disease incidence. Our findings aimed to inform future assessment of the disease burden associated with outdoor air pollution and assist relevant authorities in devising effective management strategies.
Materials and methods
Data source
Data on respiratory infectious diseases
Retrospective data on outpatient and inpatient cases of respiratory infectious diseases in Jinan Health Care Development Center, spanning from January 1, 2021 to December 31, 2023, were electronically extracted from the medical record system. These cases were categorized according to the 10th revision of the International Classification of Diseases (ICD-10). The study protocol was endorsed by the Ethics Committee of Jinan Health Care Development Center, adhering to the principles outlined in the Helsinki Declaration. Given the retrospective nature of the study, the ethics committee granted an exemption from informed consent.
Patients with ICD-10 codes falling within the range J00-J99 were included, encompassing conditions such as acute upper respiratory tract infections, acute and chronic tracheobronchitis, pneumonia, influenza, tuberculosis, acute tonsillitis, pharyngitis, laryngitis, asthma, and related disorders. Cases attributed to surgical procedures, accidents, or other non-natural causes were excluded. In total, 20,148 patients were included in this study, with a gender distribution of 9,772 females and 10,376 males.
Air pollution monitoring data
Air pollution data for Jinan City during the same period frame were systematically compiled. The data came from the daily data of 14 environmental monitoring sites of Jinan Bureau of Ecological Environment. In this study, the average value of 14 monitoring sites was taken as the representative of the air quality level of Jinan City. Air pollution indicators included: inhalable PM10, fine PM2.5, carbon monoxide (CO), ozone (O3), nitrogen dioxide (NO2) and sulfur dioxide (SO2).
Meteorological data
Concomitant meteorological data for Jinan City were also gathered and organized. The source of these meteorological indicators was the Jinan Meteorological Bureau. The variables included in the study were relative humidity, average daily temperature, minimum temperature, and maximum temperature, all of which were deemed relevant to the analysis.
Generalized additive model (GAM) analysis
To investigate the associations between PM pollution and daily outpatient visits for various respiratory diseases, we integrated daily outpatient counts, air pollution indices, and meteorological parameters by date. This time series approach is widely employed in assessing the acute health impacts of air pollution, offering the advantage of repeatedly observing health effects among a consistent study population under varying exposure conditions. Consequently, factors that remain relatively stable over the study period, such as age, gender, smoking habits, hypertension status, and socioeconomic factors, are inherently controlled for, minimizing confounding effects.
Given that daily outpatient events are independent, low-probability occurrences that approximate a Poisson distribution, and the nonlinear nature of the relationship between outpatient counts and explanatory variables, we employed the GAM as our primary analytical tool. Additionally, to address the common issue of “over-dispersion” in outpatient counts, we integrated the quasi-Poisson distribution within the GAM framework. This Poisson regression-based GAM was designed to explore the intricate relationships between outdoor air pollutants, meteorological factors, and outpatient visits for respiratory diseases. The model constructed in this article was:
The GAM model is as follows:
Among them, the expected number of outpatient visits on day (t) is denoted by {E}(Y_t) in person-times, with (α) representing the intercept. The pollutant concentration on day (t) is represented by (Zt), measured in units of (µg/m^3). The cubic spline function is denoted by (S), with degrees of freedom represented by (df). Time (T) is a temporal variable in years, used to control for long-term and seasonal trends in the time series data. Other meteorological factors include temperature (T), relative humidity (RH). The categorical indicator variable for “which day of the week” is denoted by (DOW), the indicator variable for “holiday effect” by (Holiday), and the indicator independent variable for “influenza outbreak week” by (Influenza).
To refine the model, we adjusted it using the natural cubic spline function (ns) and incorporated the influence of meteorological factors and day-of-week (DOW) effects as categorical variables. The fundamental modeling strategy employed is:
(1) Incorporate a cubic spline smoothing function of time into the model to account for both the long-term trend and seasonal variation in daily outpatient visits. (2) In constructing the model for this study, the selection of the degrees of freedom (df) for the time smoothing function is paramount. This process was facilitated by utilizing the partial autocorrelation function (PACF). A range of 4-12 df/year was explored to fit the time trend, sequentially testing the models and plotting PACF graphs with a 30-day lag. When the absolute values of the first two lags in these plots fell below 0.1, we deemed the model to have effectively controlled for autocorrelation. If this criterion was not met, an autoregressive term with a maximum lag of 7 days was introduced to refine the model [15]. Ultimately, we opted for 7 df/year to effectively manage seasonal and long-term temporal trends. (3) To control for temporal patterns within the time series, we introduced the dummy variable DOW into the model. This allowed us to account for the “day of the week effect”, wherein outpatient visits may exhibit periodic fluctuations due to factors such as weekends. (4) Furthermore, the “holiday” indicator variable was incorporated into the baseline model to mitigate the potential “holiday effect”, where changes in outpatient visits may occur due to various reasons associated with holidays. (5) In the fundamental model, we incorporated a dummy variable indicating “flu outbreak week” to regulate the interplay between hospital visits and influenza epidemics. This variable is defined by comparing weekly influenza visits to the annual average; if the weekly count exceeds 75% of this average, it is classified as an outbreak week, otherwise, a non-outbreak week. (6) To delve into the associations among PM pollution, outpatient visits, and seven other factors, we augmented the model with two crucial variables: RH and T. Notably, the relationship between outpatient volumes and meteorological parameters is nonlinear, necessitating the application of a cubic spline smoothing function. Here, we set the degrees of freedom for humidity and temperature at 3. Existing research underscores the health impacts of temperature, with a lag effect spanning at least 10 days [16], whereas no such delayed effect has been observed for relative humidity [17]. Consequently, our analysis considers RH and the average T over the 14-day outpatient period.
Statistical analysis
The Excel software was employed to construct a comprehensive database, incorporating all gathered outdoor air pollution indices, meteorological parameters, and hospital patient records. The dataset underwent rigorous pre-processing, including sorting, detection of logical inconsistencies, and verification of missing values.
Statistical analyses were performed utilizing SPSS 22.0 software. The distribution of all indicators approximated normality and were thus presented as mean ± standard deviation (±s), complemented by descriptive statistics including P25, P50, and P75 percentiles, and the minimum and maximum values.
To investigate the correlations between hospitalization rates for respiratory infectious diseases, meteorological factors, and the significance level was set at α = 0.05 (two-tailed). Spearman’s correlation analysis was selected for this purpose, with statistical significance denoted by P<0.05.
Furthermore, a GAM based on Poisson distribution was utilized to quantify the relationships between outdoor air pollutants, meteorological variables, and the number of patients diagnosed with respiratory infectious diseases.
Results
Descriptive analysis of basic data
Between January 1, 2021 and December 31, 2023, Jinan’s annual daily mean temperature was 16.12°C, ranging from -4.50°C to 34.00°C. The daily average relative humidity stood at 58.40%, with a wide variation from 26.07% to 397.41%. For our country, 150 g/m3 was the second level.
Regarding air quality, the daily average concentration of PM10 was 109.06 μg/m3, falling between the national first (50 μg/m3) and second (150 μg/m3) air quality standards. Similarly, PM2.5 concentrations averaged 53.29 μg/m3, positioned between the primary (35 μg/m3) and secondary (75 μg/m3) standards. Concentrations of SO2 and NO2 complied with national first-class standards. However, O3 levels, with a daily average of 174.88 μg/m3, significantly exceeded the national secondary standard of 160 μg/m3, indicating a relatively high level of pollution from this pollutant.
In terms of air quality rankings among 168 key cities nationwide, Jinan ranked 157th in 2021 and 158th in 2023, with 182 and 227 days of good air quality, respectively.
During the study period, a total of 170,014 outpatient and inpatient visits for respiratory infectious diseases were recorded, averaging 465.82 visits per day (ranging from 73 to 951 visits/day). Among these patients, 50.56% (85,957) were male, and 49.44% (84,057) were female. Age-wise, 21.09% (35,852) were ≤12 years old, 53.69% (91,288) were between 13 and 60 years old, and 25.22% (42,874) were ≥60 years old. These findings are summarized in Table 1.
Table 1.
Descriptive statistical results of outdoor air pollution indicators, meteorological indicators and daily number of hospital visits for respiratory infectious diseases in Jinan from 2021 to 2023
| Indicator | ±s | P25 | P50 | P75 | Min | Max | |
|---|---|---|---|---|---|---|---|
| Air pollution | PM10 (µg/m3) | 109.06±94.51 | 53.26 | 102.81 | 148.98 | 9.89 | 333.05 |
| PM2.5 (µg/m3) | 53.29±36.77 | 21.56 | 44.43 | 73.91 | 7.68 | 183.84 | |
| SO2 (µg/m3) | 15.01±9.88 | 7.67 | 13.93 | 20.59 | 4.05 | 51.02 | |
| NO2 (µg/m3) | 45.02±31.28 | 21.48 | 42.80 | 62.33 | 8.12 | 139.66 | |
| O3 (µg/m3) | 174.88±129.56 | 76.73 | 160.95 | 248.31 | 9.80 | 542.63 | |
| CO (mg/m3) | 1.41±0.96 | 0.66 | 1.35 | 2.03 | 0.38 | 4.28 | |
| Meteorological factor | Daily minimum temperature (°C) | 22.45±11.37 | 11.50 | 22.00 | 31.00 | -1.00 | 38.00 |
| Daily minimum temperature (°C) | 11.46±10.40 | 1.00 | 12.00 | 21.00 | -9.00 | 31.00 | |
| Daily average temperature (°C) | 16.17±10.52 | 5.75 | 17.00 | 25.00 | -4.50 | 34.00 | |
| Daily average relative humidity (%) | 58.45±35.68 | 30.17 | 55.39 | 84.77 | 26.07 | 97.41 | |
| Number of hospital visits | Total number of hospital visits | 462.84±393.00 | 197.00 | 393.00 | 627.00 | 73.00 | 951.00 |
| Male | 233.48±181.65 | 102.00 | 189.00 | 325.00 | 57.00 | 629.00 | |
| Female | 231.33±184.73 | 100.00 | 194.00 | 312.00 | 64.00 | 644.00 | |
| ≤12 years | 98.23±89.22 | 38.00 | 75.00 | 130.00 | 43.00 | 394.00 | |
| 12-60 years | 250.10±208.84 | 98.00 | 200.00 | 340.00 | 53.00 | 741.00 | |
| ≥60 years | 117.48±99.67 | 46.00 | 89.00 | 156.00 | 46.00 | 419.00 | |
Note: PM10: inhalable particulate matter; PM2.5: fine particulate matter; SO2: sulfur dioxide; NO2: nitrogen dioxide; O3: ozone; CO: carbon monoxide.
Spearman correlation analysis
Our analysis elucidates a strong interdependence among various air pollutants and meteorological factors. Specifically, PM10 and PM2.5 exhibit a significant negative correlation (P<0.01), indicating a mutual influence in their concentrations. Likewise, O3 displays a positive correlation with temperature (P<0.01), suggesting that warmer conditions favor O3 formation. In contrast, O3 negatively correlates with PM10 and PM2.5 (P<0.01), likely due to their competing chemical pathways.
Furthermore, PM10 is positively correlated with NO2 and CO (P<0.05), emphasizing the interconnectedness of pollutant sources and their atmospheric behavior. Notably, the daily maximum temperature significantly influences this relationship. Additionally, SO2 and PM2.5 are positively correlated (P<0.05), with the daily average temperature having a marked impact on this association.
Temperature and daily average relative humidity also demonstrate a positive correlation (P<0.05), with temperature exhibiting the strongest link among the analyzed variables. The comprehensive results of this Spearman correlation analysis are presented in Table 2.
Table 2.
Correlation analysis between outdoor air pollution and meteorological factors in Jinan City from 2021 to 2023
| Variable | PM10 | PM2.5 | SO2 | NO2 | O3 | CO | Daily maximum temperature | Daily minimum temperature | Daily average temperature |
|---|---|---|---|---|---|---|---|---|---|
| PM2.5 | 0.183* | ||||||||
| SO2 | 0.139* | 0.135* | |||||||
| NO2 | 0.129* | 0.025 | 0.017 | ||||||
| O3 | -0.188** | -0.223* | -0.183* | -0.151* | |||||
| CO | 0.112* | 0.068 | 0.113 | 0.054* | -0.155* | ||||
| Daily maximum temperature | -0.265** | -0.277** | -0.254** | -0.242** | 0.334** | -0.246** | |||
| Daily minimum temperature | -0.242** | -0.257** | -0.261** | -0.257** | 0.361** | -2.262** | 0.981** | ||
| Daily average temperature | -0.253** | -0.265** | -0.257** | -0.2354** | 0.372** | -0.271** | 0.981** | 0.989** | |
| Daily average relative humidity | -0.025 | -0.021 | 0.029 | -0.038 | 0.085 | 0.022 | 0.119* | 0.113* | 0.109* |
indicated P<0.01;
indicated P<0.05;
PM10: inhalable particulate matter; PM2.5: fine particulate matter; SO2: sulfur dioxide; NO2: nitrogen dioxide; O3: ozone; CO: carbon monoxide.
Time trend of PM2.5 and respiratory infectious disease hospital visits
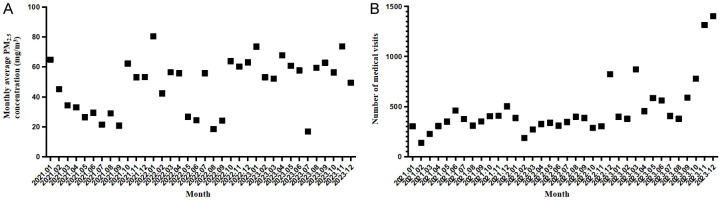
Figure 1 depicts a notable seasonal pattern in PM2.5 concentrations in Jinan during 2021 and 2023, with peak levels observed in winter (December to January) and troughs in summer (May to August). However, the seasonal trend in PM2.5 concentrations did not mirror a significant corresponding trend in the frequency of hospital visits for respiratory infectious diseases. Both metrics exhibited a similar seasonal variation, with the lowest incidence occurring from May to August and peaking from December to February.
Figure 1.
Time trend of PM2.5 and number of hospital visits for respiratory infectious diseases in Jinan from 2021 to 2023. A: Time trend of PM2.5 in Jinan from 2021 to 2023. B: Time trend of number of hospital visits for respiratory infectious diseases in Jinan from 2021 to 2023.
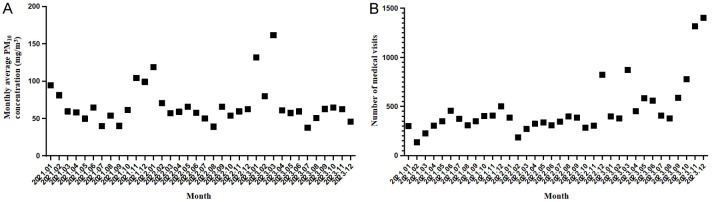
Time trend of PM10 and respiratory infectious disease hospital visits
Analogously, Figure 2 illustrates a distinct seasonal trend in PM10 concentrations in Jinan over the same time frame, with the highest concentrations in winter (December to January) and the lowest in summer (May to August). Despite this clear seasonal variation in PM10 levels, no significant correlation was observed between its trend and the frequency of hospital visits for respiratory infectious diseases. Similar to PM2.5, the incidence of respiratory infectious diseases was lowest during May to August and peaked during December to February.
Figure 2.
Time trend of PM10 and number of hospital visits for respiratory infectious diseases in Jinan from 2021 to 2023. A: Time trend of PM10 in Jinan from 2021 to 2023. B: Time trend of number of hospital visits for respiratory infectious diseases in Jinan from 2021 to 2023.
Analysis results of GAM
In order to test the impact of co-pollutants in the atmosphere (SO2, NO2, CO and O3) on the estimated health effects of PM pollution, we employed a series of single-pollutant models, each augmented with an additional pollutant. Subsequently, a multi-pollutant model was fitted to determine the robustness of the individual PM effects on hospital visits for respiratory diseases. We conducted a comprehensive analysis of the lagging effects between health outcomes and particulate pollutants, considering lags from lag0 (pollution day) to lagN (N days after exposure), as well as cumulative lags (e.g., lag01, lag02, lag03) representing the average impact over 1 to N days. Setting the reference concentration for air pollution, we consistently 0 μg/m3, acknowledging its theoretical minimum and facilitating interpretation. Based on the constructed GAMs, we estimated the relative risk (RR) and 95% confidence interval (CI) for respiratory disease visits, associated with a 10 μg/m3 increase in PM10 and PM2.5 concentrations.
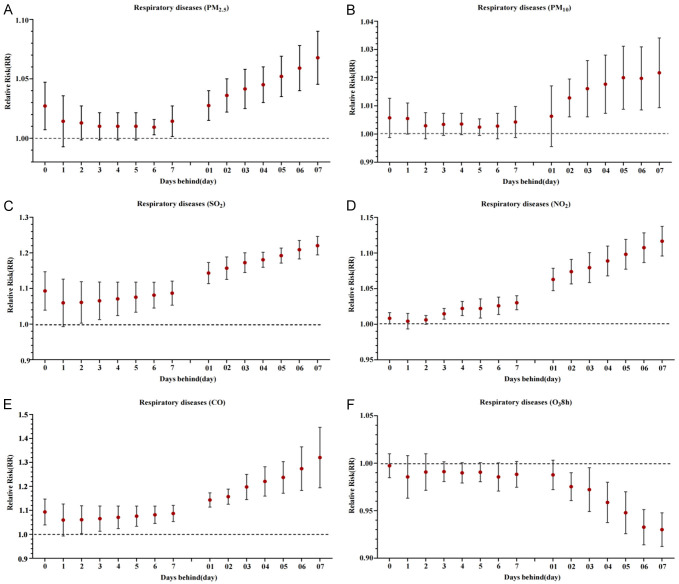
Single pollutant model
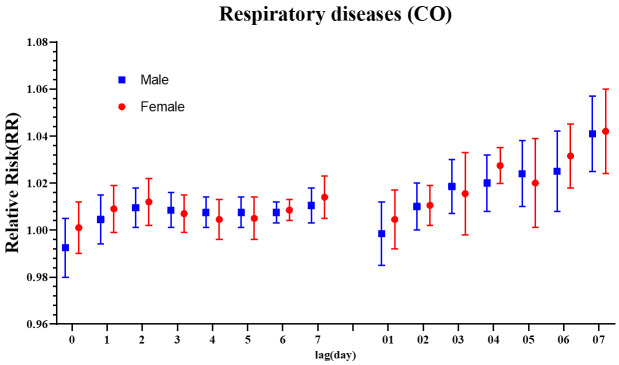
Figure 3 presents the estimated impact of a 10 μg/m3 increase (or 1 mg/m3 for CO) in various air pollutants on the total number of hospitalizations for respiratory diseases in Jinan City from 2021 to 2023. Significant adverse effects were observed for PM2.5, SO2, and CO on lags ranging from lag0 to lag7 (inclusive), with cumulative lags (lag01 to lag07) also exhibiting significant impacts. Notably, the strongest effect for PM2.5, SO2, and CO was observed at lag7, with corresponding RR values were of 1.058, 1.224, and 1.405, respectively. For PM10, significant effects were seen on lag2 and cumulative lags from lag02 to lag07, with the highest RR at lag7. Similarly, NO2 had a notable effect across lags 0, 3 to 7, and cumulative lags 01 to 07, peaking at lag7 with an RR of 1.102 (95% CI: 1.082-1.121). Conversely, no significant association was found between O3 (8-hour average) and respiratory hospitalizations across various lag periods.
Figure 3.
Influence of air pollution on total number of hospital visits for respiratory diseases. A: Influence of PM2.5 on total number of hospital visits for respiratory diseases. B: Influence of PM10 on total number of hospital visits for respiratory diseases. C: Influence of SO2 on total number of hospital visits for respiratory diseases. D: Influence of NO2 on total number of hospital visits for respiratory diseases. E: Influence of CO on total number of hospital visits for respiratory diseases. F: Influence of O3 on total number of hospital visits for respiratory diseases. Note: RR: relative risk; PM10: inhalable particulate matter; PM2.5: fine particulate matter; SO2: sulfur dioxide; NO2: nitrogen dioxide; O3: ozone; CO: carbon monoxide.
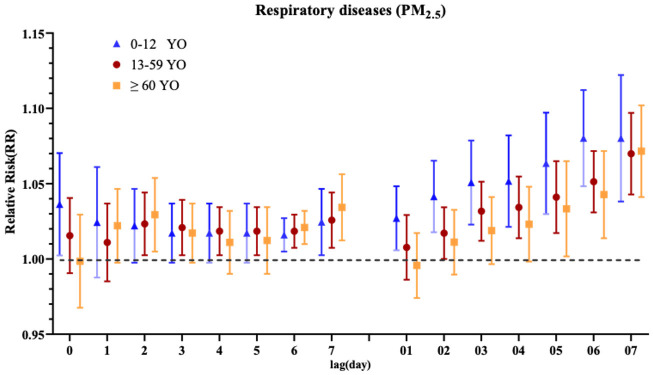
Further examination of age-specific impacts of PM2.5 on respiratory hospitalizations, as depicted in Figure 4, reveals that children aged 0-12 years were particularly vulnerable, with significant effects observed on lags 0, 5 to 7, and cumulative lags 1 to 7. In the 13-59 age group, significant effects were noted on lags 2-3, 5-7, and cumulative lags 02 to 07. Among the elderly (≥60 years), significant effects were observed on lags 2-3, 6-7, and cumulative lags 05 to 07, indicating age-dependent susceptibilities to PM2.5 exposure.
Figure 4.
Influence of PM2.5 on total number of hospital visits for respiratory diseases in different age groups. Note: RR: relative risk; PM2.5: fine particulate matter; YO: years old.
Figure 5 illustrates the differential impact of PM2.5 on respiratory disease hospitalizations by gender. A clear pattern emerges, indicating that women are more adversely affected by PM2.5 exposure than men. For women, PM2.5 exhibits a significant cumulative lag effect on respiratory emergency visits, with the strongest influence observed at lag07. In contrast, for men, the detrimental effects of PM2.5 on respiratory emergency visits are evident on days 0-lag1, lag2-lag5, and cumulative lags 02-lag07, peaking at lag07. Notably, the cumulative lag effect surpasses the single-day lag effect for both genders.
Figure 5.
Influence of PM2.5 on total number of hospital visits for respiratory diseases in different age groups. Note: RR: relative risk; CO: carbon monoxide.
Multi-pollutant model
To discern the individual and combined effects of multiple pollutants, we selected the pollutant with the most pronounced effect at lag07 to fit a dual-pollutant model. This approach allowed us to assess the stability of our model results, as detailed in Table 3. Given the high correlation between PM2.5 and PM10 (r = 0.86), they were not simultaneously included in the dual-pollutant model to avoid multicollinearity. Our findings reveal that the inclusion of additional pollutants did not significantly alter the effect estimates of SO2 and NO2 on the total number of respiratory disease hospitalizations.
Table 3.
Dual pollutant model analysis of the influence of air pollution on the total number of hospital visits for respiratory diseases in Jinan City from 2021 to 2023
| Model | PM2.5 | SO2 | NO2 | O3 | CO |
|---|---|---|---|---|---|
| Single pollutant model | 1.066 (1.055, 1.083) | 1.239 (1.195, 1.243) | 1.102 (1.082, 1.121) | 0.951 (0.942, 0.960) | 1.417 (1.341, 1.492) |
| PM2.5 | // | 1.205 (1.162, 1.248) | 1.098 (1.067, 1.128) | 0.953 (0.933, 0.973) | 1.404 (1.314, 1.493) |
| SO2 | 1.062 (1.046, 1.078) | // | 1.102 (1.072, 1.131) | 0.956 (0.942, 0.969) | 1.403 (1.324, 1.481) |
| NO2 | 1.051 (1.035, 1.066) | 1.227 (1.176, 1.277) | // | 0.961 (0.939, 0.982) | 1.401 (1.332, 1.469) |
| O3 | 1.054 (1.042, 1.066) | 1.226 (1.181, 1.271) | 1.096 (1.059, 1.133) | // | 1.387 (1.299, 1.475) |
| CO | 1.034 (1.037, 1.030) | 1.226 (1.183, 1.269) | 1.099 (1.055, 1.142) | 0.951 (0.934, 0.968) | // |
Note: PM10: inhalable particulate matter; PM2.5: fine particulate matter; SO2: sulfur dioxide; NO2: nitrogen dioxide; O3: ozone; CO: carbon monoxide.
Discussion
Jinan, a representative city in northern China utilizing central heating, experienced air quality issues from 2021 to 2023. During this period, daily average concentrations of CO and SO2 surpassed national first-level standards, while PM2.5 and PM10 fell between the first and second levels, and O3 exceeded the second-level standard. Notably, O3 and PM emerged as the primary pollutants of concern, with PM10 pollution exceeding that of PM2.5.
Using medical records from respiratory infectious disease patients treated in a local hospital over the same timeframe, this study employed a GAM model based on Poisson regression to explore the association between respiratory disease hospitalizations and air pollution exposure. Our findings underscore that not only O3 but also particulate pollutants like PM2.5 and PM10 significantly impact the total number of respiratory disease visits, exhibiting an approximately linear non-threshold relationship and a lag effect.
Specifically, the strongest effects of PM2.5, PM10, SO2, NO2, and CO were observed at a lag of 7 days (lag07). At this point, a 10 μg/m3 increase in PM2.5, PM10, SO2, and NO2, and a 1 mg/m3 increase in CO, were associated with respective RRs of 1.058, 1.008, 1.224, 1.102, and 1.405 for total respiratory disease hospitalizations. The multi-pollutant model maintained the positive correlation between respiratory disease hospitalizations and pollutants like PM2.5 and PM10, without altering their relationship. Notably, this model mitigated the significant health effects attributed solely to PM, aligning with previous findings by Wang et al. [18] and Wang et al. [19].
Our study highlights that children aged 0-12 are particularly vulnerable to PM2.5 exposure, experiencing more pronounced impacts than other age groups. This heightened sensitivity can be attributed to their growth and developmental stage, where they are more susceptible to environmental factors compared to adults. Epidemiological evidence supports this, indicating that PM2.5 adversely affects children’s immune status [20-22], significantly elevating their risk of respiratory diseases.
Conversely, PM10 exerts a greater influence on the elderly aged 60 and above. This may stem from the elderly’s reduced physical resilience and prevalent underlying health conditions. PM10 primarily deposits in the upper respiratory tract, where its accompanying bacteria, viruses, and harmful substances can easily trigger respiratory irritation and lung infections [23,24]. Domestic and international research consistently demonstrates a strong correlation between inhalable PM in the air and the number of respiratory outpatient visits [25,26]. Gu et al. [27] observed a notable increase in respiratory disease mortality with rising PM2.5 concentrations. Similarly, Duan et al.’s [28] study in Chengdu revealed that elevated PM2.5 levels augment the risk of respiratory illnesses, subsequently boosting outpatient clinic visits. Yin et al. [29], in their Shanghai-based research, concurred, reporting an increase in respiratory clinic visits with daily average PM2.5 concentrations.
Cui et al. [30], investigating Jinan City’s air pollution from 2014 to 2016, found that PM2.5 concentration hikes led to a 0.40% rise in circulatory system outpatient visits and a 0.28% increase in internal medicine clinic visits. Additionally, PM10 concentration increments were associated with a 0.25% increase in circulatory system outpatient cases, though the final sentence concerning outpatient numbers appears incomplete, likely an oversight. Our study aligns with these findings while acknowledging the variability in natural environments, air pollutant compositions, and population demographics across study areas.
It is noteworthy that our analysis did not account for potential confounding variables such as smoking habits, occupation, outdoor activity patterns, lifestyle choices, education levels, and other individual behavioral factors. The exclusion of these factors may introduce bias into our results. Future studies should endeavor to incorporate these variables to provide a more comprehensive understanding of the complex interplay between air pollution and human health. This study is subject to several limitations. Firstly, the data was solely sourced from a single hospital in Jinan City over a three-year period, inherently introducing potential selection bias and limiting the generalizability of findings. The brevity of the observation period and narrow data scope fail to comprehensively mirror the respiratory disease treatment landscape in Jinan. Secondly, while the GAM accounts for long-term trends, weekday effects, temperature, humidity, and age, it overlooks the influence of individual lifestyle factors and physical health status on respiratory morbidity. The study’s relatively short duration may also constrain the applicability of conclusions. To address these limitations, future endeavors should encompass longer-term data collection and more nuanced investigations, encompassing a broader array of possible confounding variables.
In conclusion, in line with prior research, our findings underscore the positive correlation between elevated concentrations of atmospheric pollutants, notably PM2.5 and PM10, and the heightened risk of respiratory diseases. Consequently, the government of Jinan should devise tailored measures to mitigate environmental pollution and enhance ecological health, taking into account the sources and seasonal variations of air pollution. Additionally, residents are advised to minimize exposure during dusty or hazy weather, utilizing protective gear such as masks, to decrease the inhalation of harmful airborne particles and thereby prevent respiratory illnesses.
Disclosure of conflict of interest
None.
References
- 1.GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: World Health Organization; 2021. [PubMed] [Google Scholar]
- 3.Verhoeven JI, Allach Y, Vaartjes ICH, Klijn CJM, de Leeuw FE. Ambient air pollution and the risk of ischaemic and haemorrhagic stroke. Lancet Planet Health. 2021;5:e542–e552. doi: 10.1016/S2542-5196(21)00145-5. [DOI] [PubMed] [Google Scholar]
- 4.Montone RA, Rinaldi R, Bonanni A, Severino A, Pedicino D, Crea F, Liuzzo G. Impact of air pollution on ischemic heart disease: evidence, mechanisms, clinical perspectives. Atherosclerosis. 2023;366:22–31. doi: 10.1016/j.atherosclerosis.2023.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Coleman NC, Burnett RT, Ezzati M, Marshall JD, Robinson AL, Pope CA 3rd. Fine particulate matter exposure and cancer incidence: analysis of SEER cancer registry data from 1992-2016. Environ Health Perspect. 2020;128:107004. doi: 10.1289/EHP7246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian Y, Liu H, Wu Y, Si Y, Song J, Cao Y, Li M, Wu Y, Wang X, Chen L, Wei C, Gao P, Hu Y. Association between ambient fine particulate pollution and hospital admissions for cause specific cardiovascular disease: time series study in 184 major Chinese cities. BMJ. 2019;367:l6572. doi: 10.1136/bmj.l6572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen JS, Wang Q, Shen HP. Does industrial air pollution increase health care expenditure? Evidence from China. Front Public Health. 2021;9:695664. doi: 10.3389/fpubh.2021.695664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Yang Y, Deng G, Jiang X, Zhang Y, Che H, Sun T, Niu T, Li D. Global view on China’s foggy-haze associated with air-pollutant conveyor belts. Sci Total Environ. 2019;693:133448. doi: 10.1016/j.scitotenv.2019.07.254. [DOI] [PubMed] [Google Scholar]
- 9.Ratajczak A, Badyda A, Czechowski PO, Czarnecki A, Dubrawski M, Feleszko W. Air pollution increases the incidence of upper respiratory tract symptoms among Polish children. J Clin Med. 2021;10:2150. doi: 10.3390/jcm10102150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xie W, You J, Zhi C, Li L. The toxicity of ambient fine particulate matter (PM2.5) to vascular endothelial cells. J Appl Toxicol. 2021;41:713–723. doi: 10.1002/jat.4138. [DOI] [PubMed] [Google Scholar]
- 11.Krittanawong C, Qadeer YK, Hayes RB, Wang Z, Virani S, Thurston GD, Lavie CJ. PM2.5 and cardiovascular health risks. Curr Probl Cardiol. 2023;48:101670. doi: 10.1016/j.cpcardiol.2023.101670. [DOI] [PubMed] [Google Scholar]
- 12.Li X, Hussain SA, Sobri S, Md Said MS. Overviewing the air quality models on air pollution in Sichuan Basin, China. Chemosphere. 2021;271:129502. doi: 10.1016/j.chemosphere.2020.129502. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y, Wang ZJ, Sun KZ, Dai XJ, Zhu M, Ma SS, Zhang LH. Evaluation of environmental air quality and its changing trends in Jinan City from 2013 to 2020. Chinese Society of Environmental Sciences: 2021 Annual Science and Technology Conference; 2021. pp. 247–254. [Google Scholar]
- 14.Cui L, Zhou J, Peng X, Ruan S, Zhang Y. Analyses of air pollution control measures and co-benefits in the heavily air-polluted Jinan city of China, 2013-2017. Sci Rep. 2020;10:5423. doi: 10.1038/s41598-020-62475-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fan L, Gu Q, Zeng Q. Progress in the application of generalized additive model in the epidemiological study of air pollution. Environmental and Occupational Medicine. 2019;36:676–681. [Google Scholar]
- 16.Zhang XJ, Ma WP, Zhao NQ, Wang XL. Time series analysis of the association between ambient temperature and cerebrovascular morbidity in the elderly in Shanghai, China. Sci Rep. 2016;6:19052. doi: 10.1038/srep19052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–53. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Zhang YS, Li XP. The impact of air pollution in Jinan urban area on the outpatient volume of respiratory diseases. China Environmental Science. 2008;28:571–576. [Google Scholar]
- 19.Wang S, Li Y, Niu A, Liu Y, Su L, Song W, Liu J, Liu Y, Li H. The impact of outdoor air pollutants on outpatient visits for respiratory diseases during 2012-2016 in Jinan, China. Respir Res. 2018;19:246. doi: 10.1186/s12931-018-0958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y, Li S, Liu B, Zhang J, Wang C, Feng L. Maternal urban particulate matter (SRM 1648a) exposure disrupted the cellular immune homeostasis during early life: the potential attribution of altered placental transcriptome profile. Sci Total Environ. 2024;912:169432. doi: 10.1016/j.scitotenv.2023.169432. [DOI] [PubMed] [Google Scholar]
- 21.Liu Bei, Zheng JY, Wang SL, Wang J, Gao P, Wu B, Lv LJ. Systematic evaluation of the impact of environmental air pollution on autoimmune diseases. Chinese Journal of Rheumatology. 2022;26:615–621. [Google Scholar]
- 22.Balasubramani K, Prasad KA, Kodali NK, Abdul Rasheed NK, Chellappan S, Sarma DK, Kumar M, Dixit R, James MM, Behera SK, Shekhar S, Balabaskaran Nina P. Spatial epidemiology of acute respiratory infections in children under 5 years and associated risk factors in India: district-level analysis of health, household, and environmental datasets. Front Public Health. 2022;10:906248. doi: 10.3389/fpubh.2022.906248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz J. PM10, ozone, and hospital admissions for the elderly in Minneapolis-St. Paul, Minnesota. Arch Environ Health. 1994;49:366–74. doi: 10.1080/00039896.1994.9954989. [DOI] [PubMed] [Google Scholar]
- 24.Xing LY, Chen X, Sun J. The effect of short-term exposure to fine particles in Tianjin on the readmission of patients with chronic heart failure aggravated by heart failure and the exploration of susceptible population. Adv Cardiol. 2022;43:846–851. [Google Scholar]
- 25.Lu Y, Jie X, Zou F, Wang D, Da H, Li H, Zhao H, He J, Liu J, Fan X, Liu Y. Investigation analysis of the acute asthma risk factor and phenotype based on relational analysis with outdoor air pollutants in Xi’an, China. Environ Geochem Health. 2024;46:75. doi: 10.1007/s10653-023-01816-0. [DOI] [PubMed] [Google Scholar]
- 26.Ravindra K, Bahadur SS, Katoch V, Bhardwaj S, Kaur-Sidhu M, Gupta M, Mor S. Application of machine learning approaches to predict the impact of ambient air pollution on outpatient visits for acute respiratory infections. Sci Total Environ. 2023;858:159509. doi: 10.1016/j.scitotenv.2022.159509. [DOI] [PubMed] [Google Scholar]
- 27.Gu WW, Yang LX, Cheng QL. Meta-analysis of the effect of atmospheric PM2.5 on mortality of respiratory diseases. Prev Med. 2018;30:1100–1105. 1111. [Google Scholar]
- 28.Duan ZH, Gao XF, Du HL, Qin FK, Chen J, Ju Y, Wu X, Hu Y. A time series study of PM2.5 concentration in the air and the number of outpatients with respiratory diseases in Chengdu. Xian Dai Yu Fang Yi Xue. 2015;42:611–614. [Google Scholar]
- 29.Yin YW, Cheng JP, Duan YS, Wei HP, Ji RX, Yu JL, Yu HR. Correlation analysis between PM2.5 and PM10 pollution and the number of outpatient clinics in respiratory and pediatric respiratory departments during haze in Shanghai. Environ Sci. 2011;32:1894–1898. [PubMed] [Google Scholar]
- 30.Cui LL, Man JY, Han LY, Yu KK, Wu XB, Yue KS, Zhou JW. Analysis of the acute effect of atmospheric particulates on the number of outpatient visits of community population in areas with serious air pollution in Jinan from 2014 to 2016. Proceedings of the First China Conference on Environment and Health; 2017. pp. 319–325. [Google Scholar]