Abstract
Background
Smoking is well known for its harmful effect on the respiratory system, but whether vaping is less harmful is unknown. Therefore, the aim of this study was to assess the association of smoking/vaping habits with self-reported respiratory symptoms in vapers and cigarette smokers.
Methods
An online survey was developed and shared on different vaping and smoking social media platforms and communities.
Results
Out of the 891 respondents, 788 were vapers (77 pure vapers and 711 ex-smokers) and 103 were cigarette smokers. Smokers reported more frequently respiratory symptoms such as chest pain, wheezing and whistling, sputum production, cough, dry mouth, and smokers suffered from more shortness of breath, sore throat and disturbed sleep compared to vapers. The self-reported respiratory symptoms in vapers were mainly related to the nicotine strength of the product and number of puffs per use. There were no significant differences between pure vapers and vapers who were ex-smokers.
Conclusion
Self-reported severe respiratory symptoms were less frequent in vapers than smokers, irrespective of their smoking history. This suggests that vaping is less harmful than cigarette smoking.
Keywords: Vaping, smoking, respiratory complications, self-reported respiratory, habits, wheezing
Introduction
Smoking tobacco cigarettes is well known for its harmful impact on health and particularly cardiorespiratory health [1, 2]. During smoking, chemical constituents of cigarette smoke, including but not limited to, nicotine, tar, irritants, carcinogens and carbon monoxide, are released into the lungs and may cause respiratory symptoms such as coughing, chest tightness, phlegm production, shortness of breath, sore throat and wheezing that over time may cause respiratory diseases such as chronic obstructive pulmonary disease (COPD) [3]. Nicotine may also contribute to lung injury, as it has been reported that it acts as a chemotactic for human neutrophils that through promotion of inflammation may over time lead to lung injury and ultimately airway obstruction [4].
The use of electronic cigarettes (vaping) has shown an increase where for instance the prevalence of people vaping increased in the USA from 6% in 2009 to 41% in 2013 [5], in the European Union from 7.2% in 2012 to 11.6% in 2014 [6], and in the UK 7.1% of the adult population used e-cigarettes in 2019 [7]. Of particular concern is the prevalence in the young, with up to 37% of 16–19 years olds having tried vaping in the USA and Canada, with 10% reporting to have vaped in the past week [8]. While vaping has thus become increasingly popular and is promoted as a less harmful alternative to smoking, the impact of vaping on health remains not clear yet. In fact, there are studies that report harmful effects of vaping on lung and cardiovascular tissue and function, including airway obstruction [3, 9–11].
Electronic cigarettes are battery powered devices with a heating element (atomizer) that produces an aerosol to be inhaled by the user [12]. The inhaled aerosol contains potentially harmful constituents including, but not limited to, flavourings, propylene glycol [13], heavy metals, volatile organic compounds [14–16] and nicotine [17–19]. Indeed, some studies [20–23] demonstrated that e-cigarette use resulted in respiratory symptoms such as coughing and wheezing.
It would be informative to assess the relationship of such symptoms with vaping behaviour, such as frequency of vaping, number of puffs and puff duration, volume and years of vaping, and compare this with symptoms seen in smokers [24]. To investigate this, we developed and applied a concise survey tool to assess smoking/vaping habits and assess their association with self-reported respiratory symptoms in vapers and cigarette smokers.
Methods
An online survey was produced to examine the association between smoking/vaping habits and self-reported respiratory symptoms via Google Forms. Respiratory symptoms were defined as self-reported wheezing or whistling in the chest, or a nocturnal dry cough not associated with a cold or chest infection [25]. The questions were developed and selected by four researchers (MZD, HD, CM and AA) and agreed among them, according to the recommendations of survey-development guidelines [26]. The survey comprised a total of 73 questions and took approximately 10–15 minutes to complete. The first questions concerned demographic data, followed by a question to categorise participants to a specific category: pure vapers, vapers but ex-smoker, and cigarette smokers. Respondents who both smoked and vaped were excluded from the analyses. In the next section, multiple-choice questions were used to assess vaping and smoking habits, and included questions concerning the type of vaping or cigarette product being used, type and strength of vaping juice/liquid, number and duration of puffs, history of vaping and/or smoking, duration in years, volume and intensity of cigarette smoking and the Fagerstrom Test for Nicotine Dependence [27]. These multiplechoice questions concerned self-reported respiratory symptoms according to the Likert scale.
Ethical approval was obtained from Manchester Metropolitan University Science and Engineering Research Ethics and Governance Committee reference number: 5944. All procedures adhered to the principles stated in the Declaration of Helsinki. Informed consent was obtained through a compulsory selection menu where those agreeing to the consent statement continued with the survey whilst those who did not provide consent, could not complete the survey.
Participants were men and women (age > 18 years). Data from participants were excluded from further analysis if answers to questions revealed that a participant had a diagnosed neuromuscular disease; severe musculoskeletal injury; any lower limb injury; any diagnosed mental health disorder; treatment for chronic respiratory complaints; a history of heart disease; was a smoker who currently mixed cigarette and vape; or was a water pipe (shisha) smoker. Study participants were notified that the survey was anonymous. Participants were recruited through vapers and cigarette smokers Facebook groups and pages. In addition, the survey was shared with the Consumer Advocacy Smoke Free Alternatives to Combustible Tobacco (CASAA) community and shared on the Reddit network of communities. The survey run from May – November 2020.
Data are presented as descriptive statistics including frequencies and medians/interquartile ranges, or average rank for non-parametric data and means or average ± standard deviations (SD) for parametric data. The null hypothesis was that there were no significant differences between the three groups in terms of self-reported cardio-respiratory symptoms. The non-parametric independent Kruskal-Wallis test was applied because data were not normally distributed. If a significant effect was found, a Bonferroni-corrected post-hoc test was performed to locate the differences. The level of statistical significance was set to be <0.05. To assess correlations between self-reported cardiorespiratory symptoms and smoking/vaping habits Spearman correlations were calculated. Stepwise regression was performed to assess the combined effect of habits on the presence or severity of symptoms in vapers only. The adjusted R-squared (R2adj) was shown to adjust for the predictors included in the regression model or not.
Results
Out of the 891 respondents, 788 were vapers (77 pure vapers and 711 ex-smokers) and 103 were cigarette smokers. Table 1 shows the participant characteristics for each group.
Table 1.
Descriptive statistics of pure vapers, vapers ex-smokers and cigarette smokers.
| Vapers (pure vapers) | Vapers (ex-smokers) | Cigarette smokers | ||||
|---|---|---|---|---|---|---|
| Men (n=57) | Women (n=20) | Men (n=512) | Women (n=199) | Men (n=66) | Women (n=37) | |
| Age (Years) | 25.2±7.5 | 25.1±8.2 | 35.5±9.5 | 39.3±10.1* | 27.2±10.2 | 27.8±10.8 |
| Height (m) | 1.77±0.05 | 1.61±0.08* | 1.78±0.06 | 1.65±0.06* | 1.80±0.70 | 1.61±0.06* |
| Mass (kg) | 77.9±13.1 | 67.7±10.5* | 84.4±14.5 | 73.9±15.5* | 79.1±12.8 | 65.6±12.7* |
| BMI (kg/m 2 ) | 24.8±4.2 | 26.3±4.8 | 26.4±4.4 | 27.0±5.9 | 24.3±3.6 | 25.0±4.6 |
BMI, body mass index;
significantly different from men at p<0.05.
There were no significant differences between ‘Vapers (pure vapers)’, ‘Vapers (ex-smokers) and ‘Cigarette smokers’.
Men were younger than women in vapers exsmokers (p<0.05), and men were taller and heavier than women irrespective of being vaper or cigarette smoker (p<0.05) (Table 1).
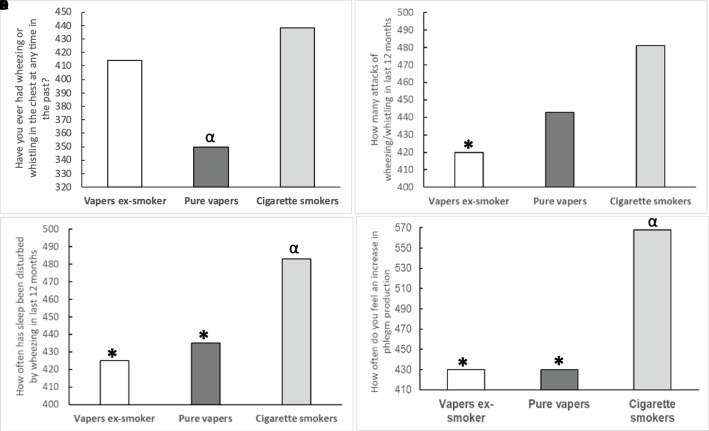
Smokers and vapers who were ex-smokers more often reported to have ever experienced wheezing or whistling in the chest in the past compared to pure vapers (p=0.002), but there was no significant difference between cigarette smokers and vapers who were exsmokers (Figure 1A). In the last 12 months, cigarette smokers suffered from more attacks of wheezing or whistling in the chest compared to vapers ex-smokers (p=0.004), but there was no significant difference between cigarette smokers and pure vapers, nor between vapers and vapers who were ex-smokers (Figure 1B). Cigarette smokers reported more often that sleep was disturbed by wheezing (Figure 1C) and phlegm (sputum) production (Figure 1D) compared to both groups of vapers (p<0.05).
Figure 1.
Prevalence of A) wheezing or whistling in the chest in the past, B) number of attacks of wheezing/whistling in the last 12 months, C) incidence of sleep disturbance due to wheezing in the last 12 months and D) incidence of phlegm production in the last 12 months in vapers who were ex-smokers, vapers and cigarette smokers. Data are presented as mean ranking. *: significantly different from cigarette smokers at p<0.05; α: significantly different from vapers ex-smokers at p<0.05. Values on the y-axis are the average ranks for each group. The rank values were obtained from the non-parametric test “ Independent-Samples Kruskal-Wallis Test’’.
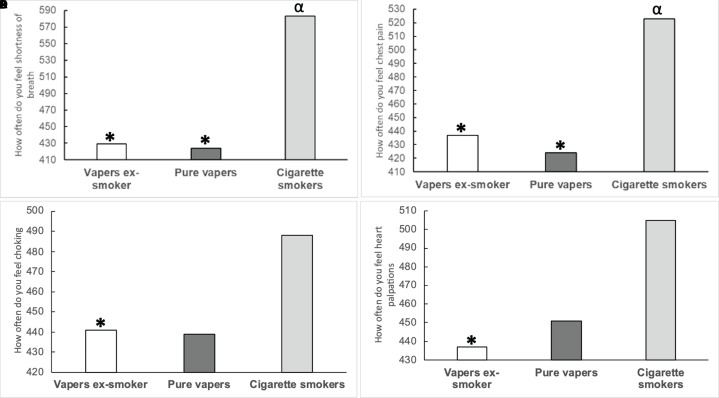
Cigarette smokers felt more shortness of breath (Figure 2A) and had more occasions of chest pain (Figure 2B) than both vaper groups (p<0.002). Choking episodes (Figure 2C) and heart palpitations (Figure 2D) were more frequent in cigarette smokers compared to vapers ex-smokers (p=0.005), whereas there was no significant difference between pure vapers and cigarette smokers (p=0.071).
Figure 2.
Frequency A) of shortness of breath, B) chest pain, C) feeling of choking and D) heart palpations in the last 12 months in vapers who were ex-smokers, vapers and cigarette smokers. Data are presented as mean ranking. *: significantly different from cigarette smokers at p<0.05; α: significantly different from vapers ex-smokers at p<0.05. Values on the y-axis are the average ranks for each group. The rank values were obtained from the non-parametric test “ Independent-Samples Kruskal-Wallis Test’’.
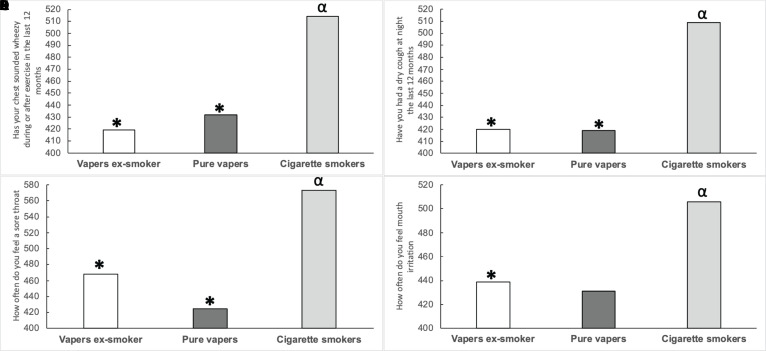
In the last 12 months, the chest of cigarette smokers sounded wheezier during or after exercise (Figure 3A), smokers suffered more frequently from dry cough at night (Figure 3B) and a sore throat (Figure 3C) compared to both vaper groups. In addition, cigarette smokers suffered from more mouth irritation than vapers ex-smokers (p=0.011), but there was no significant difference from pure vapers (p=0.068, Figure 3D).
Figure 3.
A) Chest sounding wheezy, B) dry cough, C) frequency of sore throat and D) feeling of mouth irritation in the last 12 months in vapers who were ex-smokers, vapers and cigarette smokers. Data are presented as mean ranking. *: significantly different from cigarette smokers at p<0.05; α: significantly different from vapers ex-smokers at p<0.05. Values on the y-axis are the average ranks for each group. The rank values were obtained from the non-parametric test “ Independent-Samples Kruskal-Wallis Test’’.
As we did not find any significant difference between pure vapers and vapers ex-smokers, we combined the data of all the vapers to find any correlations. In vapers, there were positive correlations of ‘nicotine strength’ in the vape juice/liquid with ‘dry cough’ (R2=0.012, p=0.006), ‘mouth irritation’ (R2=0.008, p=0.020), ‘sinus problems’ (R2=0.007, p=0.038), ‘chest pain’ (R2=0.006, p=0.046), ‘heart palpitation’ (R2=0.006, p=0.049) and ‘choking sensation’ (R2=0.007, p=0.035). Additionally, the ‘duration of puff’ was correlated with ‘wheezing’ in vapers (R2=0.010, p=0.007).
The frequency of sore throat in vapers correlated with nicotine strength (R2adj=0.012, p=0.004), and this correlation increased if the number of puffs per use was included (R2adj =0.021, p=0.015), with a further improved correlation if vaper group (pure vs. vaper ex-smokers) was included (R2adj=0.027, p=0.032). This was reflected by a higher incidence score of sore throats in vapers using >6 mg/mL nicotine (1.77 ± 0.74; n = 82) compared to those using vapes with a concentration ≤6 mg/mL (1.57 ± 0.67; n = 557) (P=0.012).
In smokers, the presence of wheezing in the chest correlated with the number of cigarettes smoked a day (R2=0.084; p=0.005). In addition, the frequency of feeling chest pain correlated with the amount of tobacco used per day used when starting with smoking (R2=0.171; p=0.001), and the frequency of feeling a sore throat correlated with the number of years smoking (R2=0.046; p=0.030).
Discussion
The main observation of the present study is that smoking was accompanied with more frequent self-reported respiratory symptoms than vaping, irrespective of smoking history in vapers. This is particularly significant when it is considered that the smokers were on average 8 years younger than the vapers who were ex-smokers in our study. Vapers, however, also suffered from respiratory symptoms that showed some relationship to the nicotine strength of the product and number of puffs per use. In addition, it was found that the frequency of respiratory symptoms was similar in pure vapers and vapers ex-smokers.
Similar to many others, in the present study we observed that cigarette smokers reported more frequently wheezing and whistling compared to vapers ex-smokers, and sleep to be disturbed, shortness of breath, chest pain, limitation during exercise, heart palpation and more sputum production and cough compared to both groups of vapers [3, 28–31]. This may well be related to the fact that cigarette smoking exposes the respiratory system to tar, nicotine and thousands of other harmful chemicals causing airway inflammation and narrowing, and damage to the alveoli that ultimately may lead to different conditions such as lung cancer, COPD and asthma [1, 2]. Consistent with this, in the present smokers, an increased volume of smoking per day and number of years smoked were associated with a higher incidence and severity of symptoms [32–35]. This is not surprising as the effects of smoking develop slowly over time, and only later in life chronic diseases may develop, a phenomenon dubbed the ‘smoking time bomb’ [36].
It is these harmful consequences of smoking that lead many smokers to search for ways to quit smoking, and take up vaping as it is considered to be a less harmful [37]. However, vaping has been shown to have harmful effects on pulmonary function that are qualitatively similar to those elicited by cigarette smoking [3, 9–11, 38]. Here we found in a comprehensive comparison of experienced respiratory symptoms between smokers and vapers that the severity and prevalence of self-reported symptoms is less in vapers than smokers, supporting the notion that vaping may be a less harmful than cigarette smoking.
It is encouraging to note that there were no significant differences between vapers who never smoked and vapers who were previous smokers. Indeed, both groups showed a lower incidence and severity of symptoms than smokers, which suggests that some of the detrimental effects of smoking may indeed be reversed by vaping. Others have seen similar symptom improvements in respiratory and cardiac symptoms when changing from smoking to vaping [39, 40]. This further encourages the use of e-cigarettes to help quit-smoking attempts, that have been shown in randomized controlled trials to be moderately effective and with similar [41] or superior effectiveness to nicotine replacement [42]. Even in smokers not intending to quit the use of e-cigarettes reduced tobacco cigarette use and resulted even in complete smoking cessation in 8.7% of smokers after 1 year [43]. Yet, in our study also vapers self-report respiratory systems and vaping cessation should also be considered. Indeed, many adolescent vapers report to have tried to quit vaping several times, and it has been suggested that strategies of vaping cessation may include less access to e-cigarettes and development of distraction techniques [44].
Nevertheless, vaping is not without its own issues, as the present vapers do report respiratory symptoms, supporting the many studies that describe adverse effects of vaping on lung function and lung tissue [3, 38, 45, 46]. The incidence and severity of symptoms appear to some extent (only 3%) to be related to the volume of vaping, nicotine strength, number of puffs per use, and being an ex-smoker or not. This indicates that while vaping is a less harmful alternative to smoking, attempts should be made to also abstain from vaping, or at least use vapes with a lower strength of nicotine, and that there are lingering effects of smoking even when one has completed stopped smoking. It is likely that such small changes may result, like continued smoking, in deleterious health effects later in life [36], but perhaps later and at a lower incidence than in smokers.
This study is not without limitations. Firstly, we had to rely on an online survey that particularly targets social media users. In addition, the survey unavoidably had to rely on self-reports of smoking and vaping habits and symptoms, and future studies may also do a clinical assessment of symptoms. It should be noted that the absence of significance between vapers and vapers ex-smokers might be related to the higher number of vapers ex-smokers (n=711) compared to pure vapers (n=77), and a larger sample size is desirable. Having said that, our study had sufficient statistical power to stratify by smoking status, and it is unlikely that a larger sample size would therefore lead to an altered conclusion. In addition, longitudinal studies are required to better understand the interaction between vaping and smoking in the sense of subjective and objective assessments and how it contributes to respiratory symptoms. Finally, it would have been interesting to assess whether the incidence and severity of self-reported symptoms in vapers were compared with those in non-vapers non-smokers.
Conclusion
Smokers had a higher incidence and severity of self-reported respiratory symptoms, even when vapers were ex-smokers. This supports the notion that vaping is less harmful than cigarette smoking.
Supplementary Information
Acknowledgement
We would like to thank Professor James Selfe for his support and advice during the development of the online survey.
Footnotes
Authors’ contributions: MZD, CM and HD contributed to the study conception. MZD, CM and HD designed and prepared the study. MZD and AA collected the data. MZD and HD analysed the data. MZD, AA and HD wrote the first draft of the manuscript. All authors commented on previous versions of the manuscript, read, and approved the final manuscript.
Ethics approval and consent to participate: Ethical approval was obtained from Manchester Metropolitan University Science and Engineering Research Ethics and Governance Committee reference number: 5944. All procedures adhered to the principles stated in the Declaration of Helsinki. Informed consent was obtained through a compulsory selection menu where those agreeing to the consent statement continued with the survey whilst those who did not provide consent, could not complete the survey.
Consent for publication: Not applicable.
Conflict of interest: Authors declare no competing interests related to this paper.
Publisher’s note: all claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Funding: No funding was received to conduct this study.
Availability of data and material
When appropriate and reasonable, anonymised data are available upon request from the corresponding author.
References
- 1.Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(26):2645–53. doi: 10.1056/NEJMoa032158. [DOI] [PubMed] [Google Scholar]
- 2.United States Public Health Service. How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the surgeon general. US Department of Health and Human Services, Public Health Service; 2010. [last accessed: 4/8/2024]. [Google Scholar]
- 3.Darabseh MZ, Selfe J, Morse CI, Degens H. Is vaping better than smoking for cardiorespiratory and muscle function? Multidiscip Respir Med. 2020;15(1) doi: 10.4081/mrm.2020.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Totti N, III, McCusker KT, Campbell EJ, Griffin GL, Senior RM. Nicotine is chemotactic for neutrophils and enhances neutrophil responsiveness to chemotactic peptides. Science. 1984;223(4632):169–71. doi: 10.1126/science.6318317. [DOI] [PubMed] [Google Scholar]
- 5.Ramo DE, Young-Wolff KC, Prochaska JJ. Prevalence and correlates of electronic-cigarette use in young adults: Findings from three studies over five years. Addict Behav. 2015;41:142–7. doi: 10.1016/j.addbeh.2014.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Filippidis FT, Laverty AA, Gerovasili V, Vardavas CI. Two-year trends and predictors of e-cigarette use in 27 european union member states. Tob Control. 2017;26(1):98–104. doi: 10.1136/tobaccocontrol-2015-052771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Action on Smoking and Health. Use of e-cigarettes (vapourisers) among adults in Great Britain. ASH fact sheet. 2019 [Google Scholar]
- 8.Hammond D, Reid JL, Rynard VL, Fong GT, Cummings KM, McNeill A, et al. Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: Repeat national cross sectional surveys. Br Med J. 2019:365. doi: 10.1136/bmj.l2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai M, Byun MK, Shin J, Crotty Alexander LE. Effects of e-cigarettes and vaping devices on cardiac and pulmonary physiology. J Physiol. 2020;598(22):5039–62. doi: 10.1113/JP279754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Echeagaray O, Savko C, Gallo A, Sussman M. Cardiovascular consequences of vaping. C Curr Opin Cardiol. 2022;37(3):227–35. doi: 10.1097/HCO.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 11.Shahandeh N, Chowdhary H, Middlekauff HR. Vaping and cardiac disease. Heart. 2021;107(19):1530–5. doi: 10.1136/heartjnl-2020-318150. [DOI] [PubMed] [Google Scholar]
- 12.Yingst J, Foulds J, Veldheer S, Du P. Device characteristics of long term electronic cigarette users: A follow-up study. Addict Behav. 2019;91:238–43. doi: 10.1016/j.addbeh.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wieslander G, Norbäck D, Lindgren T. Experimental exposure to propylene glycol mist in aviation emergency training: Acute ocular and respiratory effects. Occup Environ Med. 2001;58(10):649–55. doi: 10.1136/oem.58.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Physiol Lung Cel Mol Physiol. 2017;313(2):L193–L206. doi: 10.1152/ajplung.00071.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gotts JE, Jordt SE, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? Br Med J. 2019:366. doi: 10.1136/bmj.l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xie W, Tackett AP, Berlowitz JB, Harlow AF, Kathuria H, Galiatsatos P, et al. Association of electronic cigarette use with respiratory symptom development among us young adults. Am J Respir Crit Care Med. 2022;205(11):1320–9. doi: 10.1164/rccm.202107-1718OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korfei M. The underestimated danger of e-cigarettes-also in the absence of nicotine. Respir Res. 2018;19(1):159. doi: 10.1186/s12931-018-0870-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laugesen M. Second safety report on the ruyan® e-cigarette. Cell. 2008;27(488):4375. [Google Scholar]
- 19.Rankin GD, Wingfors H, Uski O, Hedman L, Ekstrand-Hammarström B, Bosson J, et al. The toxic potential of a fourth-generation e-cigarette on human lung cell lines and tissue explants. J Appl Toxicol. 2019;39(8):1143–54. doi: 10.1002/jat.3799. [DOI] [PubMed] [Google Scholar]
- 20.Osei AD, Mirbolouk M, Orimoloye OA, Dzaye O, Uddin SI, Benjamin EJ, et al. Association between e-cigarette use and chronic obstructive pulmonary disease by smoking status: Behavioral risk factor surveillance system. Am J Med Sci. 2020;58(3):336–42. doi: 10.1016/j.amepre.2019.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li D, Sundar IK, McIntosh S, Ossip DJ, Goniewicz ML, O’Connor RJ, et al. Association of smoking and electronic cigarette use with wheezing and related respiratory symptoms in adults: Cross-sectional results from the population assessment of tobacco and health (path) study, wave 2. Tob Control. 2020;29(2):140–7. doi: 10.1136/tobaccocontrol-2018-054694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang JB, Olgin JE, Nah G, Vittinghoff E, Cataldo JK, Pletcher MJ, et al. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the health eheart study. PloS one. 2018;13(7):e0198681. doi: 10.1371/journal.pone.0198681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho JH, Paik SY. Association between electronic cigarette use and asthma among high school students in South Korea. PloS one. 2016;11(3):e0151022. doi: 10.1371/journal.pone.0151022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Foulds J, Veldheer S, Yingst J, Hrabovsky S, Wilson SJ, Nichols TT, et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking e-cigarette users. Nicotine Tob Res. 2015;17(2):186–92. doi: 10.1093/ntr/ntu204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reddy KP, Schwamm E, Kalkhoran S, Noubary F, Walensky RP, Rigotti NA. Respiratory symptom incidence among people using electronic cigarettes, combustible tobacco, or both. Am J Respir Crit Care Med. 2021;204(2):231–4. doi: 10.1164/rccm.202012-4441LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bowling A. Research methods in health: Investigating health and health services. McGraw-hill education; (UK): 2014. [Google Scholar]
- 27.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The fagerström test for nicotine dependence: A revision of the fagerstrom tolerance questionnaire. Br J Addict. 1991;86(9):1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 28.Schneller LM, Quiñones Tavárez Z, Goniewicz ML, Xie Z, McIntosh S, Rahman I, et al. Cross-sectional association between exclusive and concurrent use of cigarettes, ends, and cigars, the three most popular tobacco products, and wheezing symptoms among us adults. Nicotine Tob Res. 2020;22(Supplement_1):S76–S84. doi: 10.1093/ntr/ntaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Courtney R. The health consequences of smoking—50 years of progress: A report of the surgeon general, 2014 us department of health and human services. Atlanta, GA: Department of health and human services, centers for disease control and prevention, national center for chronic disease prevention and health promotion, office on smoking and health; 2014. Online (grey literature): http://www.surgeongeneral.gov/library/reports/50-years-of-progressWiley Online Library; 2015. [Google Scholar]
- 30.Perez MF, Atuegwu NC, Mead EL, Oncken C, Mortensen EM. Adult e-cigarettes use associated with a self-reported diagnosis of copd. Int J Environ Res Public Health. 2019;16(20):3938. doi: 10.3390/ijerph16203938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: A longitudinal analysis. Am J Prev Med. 2020;58(2):182–90. doi: 10.1016/j.amepre.2019.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu Y, Pleasants RA, Croft JB, Wheaton AG, Heidari K, Malarcher AM, et al. Smoking duration, respiratory symptoms, and copd in adults aged≥ 45 years with a smoking history. Int J Chron Obstruct Pulmon Dis. 2015:1409–16. doi: 10.2147/COPD.S82259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhatt SP, Kim Y-i, Harrington KF, Hokanson JE, Lutz SM, Cho MH, et al. Smoking duration alone provides stronger risk estimates of chronic obstructive pulmonary disease than pack-years. Thorax. 2018;73(5):414–21. doi: 10.1136/thoraxjnl-2017-210722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pandeya N, Williams GM, Sadhegi S, Green AC, Webb PM, Whiteman DC. Associations of duration, intensity, and quantity of smoking with adenocarcinoma and squamous cell carcinoma of the esophagus. Am J Epidemiol. 2008;168(1):105–14. doi: 10.1093/aje/kwn091. [DOI] [PubMed] [Google Scholar]
- 35.Isabel U, Alberto C, María QJ, Nerea M, Xavier B, Jordi S. Smoking habit, respiratory symptoms and lung function in young adults. Eur J Public Health. 2005;15(2):160–5. doi: 10.1093/eurpub/cki113. [DOI] [PubMed] [Google Scholar]
- 36.Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tob Control. 1994;3(3):242. [Google Scholar]
- 37.Dutra LM, Grana R, Glantz SA. Philip morris research on precursors to the modern e-cigarette since 1990. Tob Control. 2017;26(e2):e97–e105. doi: 10.1136/tobaccocontrol-2016-053406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Darabseh MZ, Selfe J, Morse CI, Degens H. Impact of vaping and smoking on maximum respiratory pressures and respiratory function. Int J Adolesc. 2021;26(1):421–31. [Google Scholar]
- 39.Polosa R, Cibella F, Caponnetto P, Maglia M, Prosperini U, Russo C, et al. Health impact of e-cigarettes: A prospective 3.5-year study of regular daily users who have never smoked. Sci Rep. 2017;7(1):13825. doi: 10.1038/s41598-017-14043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flouris AD, Chorti MS, Poulianiti KP, Jamurtas AZ, Kostikas K, Tzatzarakis MN, et al. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal Toxicol. 2013;25(2):91–101. doi: 10.3109/08958378.2012.758197. [DOI] [PubMed] [Google Scholar]
- 41.Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J, et al. Electronic cigarettes for smoking cessation: A randomised controlled trial. The Lancet. 2013;382(9905):1629–37. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- 42.Brown J, Beard E, Kotz D, Michie S, West R. Real-world effectiveness of e-cigarettes when used to aid smoking cessation: A cross-sectional population study. Addiction. 2014;109(9):1531–40. doi: 10.1111/add.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Caponnetto P, Campagna D, Cibella F, Morjaria JB, Caruso M, Russo C, et al. Efficiency and safety of an electronic cigarette (eclat) as tobacco cigarettes substitute: A prospective 12-month randomized control design study. PloS one. 2013;8(6):e66317. doi: 10.1371/journal.pone.0066317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pbert L, Dubé CE, Nagawa CS, Simone DP, Wijesundara J, Sadasivam R. Vaping cessation support recommendations from adolescents who vape: A qualitative study. Res Sq. 2024 doi: 10.1186/s12889-024-19036-1. rs.3.rs-4077848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meo SA, Ansary MA, Barayan FR, Almusallam AS, Almehaid AM, Alarifi NS, et al. Electronic cigarettes: Impact on lung function and fractional exhaled nitric oxide among healthy adults. Am J Men’s Health. 2019;13(1) doi: 10.1177/1557988318806073. 1557988318806073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chaumont M, Bernard A, Pochet S, Mélot C, El Khattabi C, Reye F, et al. High-wattage e-cigarettes induce tissue hypoxia and lower airway injury: A randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):123–6. doi: 10.1164/rccm.201711-2198LE. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
When appropriate and reasonable, anonymised data are available upon request from the corresponding author.