Abstract
Suicide rates in the United States have increased over the past 15 years, with substantial geographic variation in these increases; yet there have been few attempts to cluster counties by the magnitude of suicide rate changes according to intercept and slope or to identify the economic precursors of increases. We used vital statistics data and growth mixture models to identify clusters of counties by their magnitude of suicide growth from 2008 to 2020 and examined associations with county economic and labor indices. Our models identified 5 clusters, each differentiated by intercept and slope magnitude, with the highest-rate cluster (4% of counties) being observed mainly in sparsely populated areas in the West and Alaska, starting the time series at 25.4 suicides per 100,000 population, and exhibiting the steepest increase in slope (0.69/100,000/year). There was no cluster for which the suicide rate was stable or declining. Counties in the highest-rate cluster were more likely to have agricultural and service economies and less likely to have urban professional economies. Given the increased burden of suicide, with no clusters of counties improving over time, additional policy and prevention efforts are needed, particularly targeted at rural areas in the West.
Keywords: economic factors, epidemiologic methods, growth mixture modeling, suicide
Abbreviations
- APPA
average posterior probability of assignment
- COVID-19
coronavirus disease 2019
- GMM
growth mixture model
- RR
rate ratio
Suicide poses a significant burden to population health in the United States (1). Indeed, suicide is consistently a leading cause of death in the United States overall (2) and is among the top 3 causes of death for certain demographic groups (3). After a decade of decline beginning in the 1990s, US suicide rates have increased annually, with few exceptions, since 2010, and suicide has been identified as among the most important contributors to the increase in working-age mortality and the stagnation in overall life expectancy in the United States over the past 3 decades (3). Suicide rates vary considerably across the United States, with higher rates in rural areas than in urban areas and higher rates in the West than in the rest of the country (4). Understanding where risk is concentrated and identifying the ecological factors contributing to increasing rates is critical to informing prevention and intervention efforts.
Factors that increase the risk of suicide operate across multiple levels. Individual-level risk factors include history and severity of psychiatric disorders and a history of suicide attempts (5), recent stressful life events (6, 7), family history of suicide (8), and access to lethal means (particularly firearms) (9). At the ecological level, several features of the social and built environments are associated with higher suicide rates, including mental-health provider access and firearm access (10–14) and lower prevalence of social-capital–promoting institutions (15). Macroeconomic factors also appear to play an important role. Counties with higher rates of poverty, lower median incomes, and less educated populations have higher suicide rates (16–18), and local employment shocks have been found to increase suicide rates (19–21). Further, emerging evidence indicates that economic policies such as higher minimum wages reduce suicide rates across US states (22–24).
While macroeconomic factors predict overall rates of suicide at the county level (25), it is unclear whether they predict increases in or trajectories of suicide over time and whether counties with large increases in suicide can be clustered on the basis of common economic and labor market features. Research indicates that among working-age non-Hispanic Whites, increases in suicide are steeper in counties with economies dependent on agriculture and farming (25), although the extent to which broader economic factors predict county clusters of suicide in the US population overall remains unknown. County-level economic disadvantage and declines in manufacturing labor-force participation predict increased drug overdose rates (19–21, 26–28), which may have common underlying mechanisms with suicide. Further, available evidence indicates that suicide rates have increased more in rural counties than in urban counties (11, 29–32), but little work has been done to establish economic clustering of counties according to suicide risk trajectories, especially in recent years. Findings are also inconsistent; during 2000–2015, increased economic insecurity predicted higher county-level suicide rates but did not predict increases over time (33). The extent to which these associations generalize beyond 2015 remains unknown, especially in data that cover the onset of the coronavirus disease 2019 (COVID-19) pandemic, which led to substantial economic disruption.
Understanding where suicide risk is concentrated is critical to timely dissemination of prevention and intervention efforts and to identification of etiologically important environmental causes of suicide that are seldom present in individual-level risk prediction. While previous studies have examined county-level associations with suicide rates over time, there have been no statistical attempts to cluster counties on the basis of similar suicide rates and trajectories. Furthermore, understanding how risk varies by method of suicide death is critical given that firearm access, and thus firearm suicides, cluster geographically (34) and that firearm deaths call for different prevention strategies than suicide by other methods (9). Additionally, temporal and geographic clustering of suicide, and mechanisms underlying variation, differ across age groups (35, 36); given that suicide risk is particularly high at older ages in the United States (36), consideration of differences in trajectories and correlates is warranted. Growth models provide empirical and data-driven methods for identifying clusters and patterns in longitudinal data, and they are extensively used to identify trajectories over time and their determinants, yet to our knowledge they have not been applied to suicide data to provide a statistical assessment of risk clustering across the United States.
In this study, we use cluster analysis to identify groups of US counties based on their suicide trajectories from 2008 to 2020. We test whether cluster model fit improves when clusters are identified based on the intercept and slope of the time series alone versus with the addition of annual time-varying county economic characteristics. We then identify the economic and labor market factors measured at the beginning of the time series that predict cluster membership. We also examine clusters across age groups (ages 18–64 years and ≥65 years), as well as by method of suicide death (firearm vs. nonfirearm), to assess whether trajectories of suicides are similar across these categories. This study advances the existing literature on geographic disparities in suicide by 1) statistically identifying clusters of differing trajectories across counties and 2) identifying the economic characteristics associated with different trajectory profiles.
METHODS
Data sources
We used death records for 2008–2020 from the National Vital Statistics System (37). We identified deaths resulting from suicide using International Classification of Diseases, Tenth Revision, underlying-cause-of-death codes X60–X84, Y87.0, and U03 (38). We obtained county estimates for the total population and the population stratified by age and sex from the Bridged-Race Intercensal (2008–2009) (39) and Postcensal (2011–2020) Population Estimates and used these to calculate annual crude county-level suicide mortality rates (number of suicides/100,000 population). We considered suicides overall and then separately by age group and method (firearm and nonfirearm suicides). We attempted to analyze data by sex and race/ethnicity, as well as more narrow age bands; however, these models did not converge due to sparse data in some groups. We began the time series in 2008 to match the data for economic and labor predictor indices that we correlated with suicide trajectories. Data from 3,140 counties were included in the study; 2 counties were dropped due to missing data.
Economic characteristics
For selection of the number of suicide trajectory classes, we tested model fit while including time-varying annual measures of county-level economic activity for 2008 through 2020, including: 1) proportion of the population living in poverty and median household income: annual measures of poverty prevalence and median household income, as estimated by the Census Bureau’s Small Area Income and Poverty Estimates program (40); 2) average weekly wage and annual pay: estimates of average weekly wage and annual pay across all industries, as reported to the Bureau of Labor Statistics’ Quarterly Census of Employment and Wages program (41); and 3) unemployment rate: estimates of unemployment by the Bureau of Labor Statistics (42).
After model selection, we tested associations between class membership and 5 county-level economic activity indices calculated in previous work by Monnat et al. (28), based on exploratory factor analysis of demographic, socioeconomic, occupational, and industry characteristics from the 2008–2012 administrations of the American Community Survey. Monnat et al. found that of 34 US Census variables examined, a 4-factor model best represented the correlations among 27 of the variables, with high (≥0.40) factor loadings that explained 70% of the variance across variables tested (28). The resulting factor-weighted standardized indices predicted county-level variation in overdose mortality rates (28) and reflected the economic conditions of counties at the beginning of our study period. The urban professional index includes data on population density and percentage of renter-occupied housing units, number of new residents in the previous 5 years, and numbers of workers employed in various fields—1) business/professional services; 2) finance, insurance, and real estate; 3) communication, information, and utilities industries; and 4) professional and technical, executive and managerial, retail sales, and administrative and clerical occupations. The economic disadvantage index includes the inverse of the labor force participation rate, Thiel’s L (inequality at the bottom of the income distribution), the Gini coefficient of income inequality, the ratio of federal to state median household income, and percentages of individuals living in poverty, households receiving public assistance, single-parent families, and divorced/separated persons. The blue-collar worker index includes the percentage of adults aged  25 years without a 4-year college degree and the percentages of workers employed in production, extraction, or construction; transportation or materials moving; and manufacturing. The service economy index includes the percentage of vacant housing units and the percentages of workers employed in personal service; retail, personal sales, food, and accommodations; construction; and public administration. The agricultural economy index includes the percentage of workers employed in farming, fishing, and forestry occupations and the percentage employed in the agriculture, fishing, and forestry industries. The indices are standardized (mean = 0, standard deviation = 1). This data set did not include index estimates for Alaska or Hawaii; thus, those states were excluded from regression analysis that included the indices (Alaska and Hawaii were included in other analyses). More information on the development of the indices can be found in the paper by Monnat et al. (28).
25 years without a 4-year college degree and the percentages of workers employed in production, extraction, or construction; transportation or materials moving; and manufacturing. The service economy index includes the percentage of vacant housing units and the percentages of workers employed in personal service; retail, personal sales, food, and accommodations; construction; and public administration. The agricultural economy index includes the percentage of workers employed in farming, fishing, and forestry occupations and the percentage employed in the agriculture, fishing, and forestry industries. The indices are standardized (mean = 0, standard deviation = 1). This data set did not include index estimates for Alaska or Hawaii; thus, those states were excluded from regression analysis that included the indices (Alaska and Hawaii were included in other analyses). More information on the development of the indices can be found in the paper by Monnat et al. (28).
Additional variables included in all models were metropolitan status, classified using the US Department of Agriculture Economic Research Service’s Rural-Urban Continuum Codes (43), and US Census region: Northeast, South, Midwest, or West.
Growth mixture model
The scalar form of a K-class growth mixture model (GMM) (44) with a random intercept and slope and class-specific error variance is given by
 |
where  denotes time (year),
denotes time (year),  denotes county, and
denotes county, and  denotes the suicide rate during year t in county i.
denotes the suicide rate during year t in county i.  denotes cluster or latent class (45).
denotes cluster or latent class (45).
 and
and  represent fixed effects for cluster k, the class-specific intercept (rate at the start of the study period) and slope (linear trend over the study period);
represent fixed effects for cluster k, the class-specific intercept (rate at the start of the study period) and slope (linear trend over the study period);  and
and  represent random effects that capture individual county differences in class k (intercounty variability); and
represent random effects that capture individual county differences in class k (intercounty variability); and  represents errors (intracounty variability) and is class-specific. Random effects and errors are assumed to be normally distributed with a mean of 0 and different variances—that is,
represents errors (intracounty variability) and is class-specific. Random effects and errors are assumed to be normally distributed with a mean of 0 and different variances—that is,  and
and  .
.
Note that this formulation allows each class to have a separate and distinct intercept ( ), slope (
), slope ( ), intercept variance (
), intercept variance ( ), slope variance (
), slope variance ( ), and error variance (
), and error variance ( ), as well as a different random intercept-slope covariance,
), as well as a different random intercept-slope covariance,  . In other words, each class can have a different average suicide mortality rate at the start of the study period and different slopes over the study period, counties can deviate from the class averages (both intercept and slope) by different degrees, and the magnitude of county deviation from the class average is allowed to differ across classes. These together allow for a flexible model framework. The above GMM form constitutes the base model. The alternate form with additional covariates, that is, annual time-varying county economic characteristics, is given as
. In other words, each class can have a different average suicide mortality rate at the start of the study period and different slopes over the study period, counties can deviate from the class averages (both intercept and slope) by different degrees, and the magnitude of county deviation from the class average is allowed to differ across classes. These together allow for a flexible model framework. The above GMM form constitutes the base model. The alternate form with additional covariates, that is, annual time-varying county economic characteristics, is given as
 |
where  denotes the value of covariate p in county i during year t and
denotes the value of covariate p in county i during year t and  is the class-specific coefficient to be estimated for covariate p. As described above, we identified 5 annual county-level economic measures to include in the model; hence, P = 5.
is the class-specific coefficient to be estimated for covariate p. As described above, we identified 5 annual county-level economic measures to include in the model; hence, P = 5.
The models were built using the flexmix(46–48) package in R (49). The model was initialized with different parameter priors and expectation maximized. The process was repeated 10 times with different priors (to avoid local maxima), and up to 1,000 iterations were allowed to reach convergence; the prior that maximized likelihood was retained.
Goodness of fit and assessment of model adequacy
The model’s goodness of fit was primarily assessed using the Bayesian information criterion (50, 51), the Akaike information criterion (52), and the log likelihood. We also used adequacy measures to assess the classification uncertainty of the model that are complementary to likelihood-based goodness-of-fit measures. The average posterior probability of assignment (APPA) calculates the average posterior probability of all counties assigned to class k. The APPA has clear bounds, (0, 1), with values closer to 1 indicating greater classification certainty; an APPA greater than 0.7 for all classes is considered acceptable (45, 53, 54). We also used relative entropy, which, unlike the APPA, is a global measure defined across all classes, with values close to 0 indicating low classification uncertainty, and an undefined upper bound (i.e., bounds of  ). Higher values of relative entropy indicate higher classification certainty, and values greater than 0.5 are considered acceptable (45, 53, 55, 56).
). Higher values of relative entropy indicate higher classification certainty, and values greater than 0.5 are considered acceptable (45, 53, 55, 56).
Model selection
We built models with linear trend terms (no higher-order polynomial terms were necessary), as specified above, for k = {2, …, 5}, using annual county-level (n = 3,139) suicide mortality rates from 2008–2020 (T = 15) as the response. While the Akaike information criterion and Bayesian information criterion generally improved with increasing k (see Web Figure 1, available at https://doi.org/10.1093/aje/kwad205), the changes were small at values of k greater than 5. Based on relative entropy (Web Figure 2), all models indicated acceptable fit; for the APPA (Web Figure 3), models with k > 5 had a fit that was below acceptable for at least some clusters.
We also tested the fit of models including annual time-varying economic measures to determine whether cluster identification was improved when these economic factors were included in cluster model selection. Inclusion of time-varying covariates in the model did not change the goodness of fit at smaller values of k, including at the selected value of k = 5 (Web Figure 1). Model adequacy measures met acceptable criteria and were comparable to the corresponding base model without the economic predictor variables (Web Figures 1–3). Estimates for the random effects and the proportion of counties in each cluster were similar to corresponding base model estimates. These together suggested a limited impact of inclusion of time-varying economic factors on the choice of number of latent classes, improvement of model quality, and class certainty. These observations led to our selection of a 5-class GMM without time-varying economic factors as our primary model. We built separate models with suicide rates among persons aged 18–64 years and persons aged ≥65 years, as well as suicide by firearm involvement. We varied the baseline year for robustness checks; a 5-group model was reliably recovered across baseline years.
Analysis of economic characteristics associated with cluster membership
We examined the association between county economic activity near the start of the study period and the class membership assigned by the 5-class GMM. We used a multinomial logit model to estimate the probability that county i belongs to class k, over belonging to the reference class, as
 |
where  denotes the class assigned by the GMM, q denotes one of Q time-invariant covariates as described above,
denotes the class assigned by the GMM, q denotes one of Q time-invariant covariates as described above,  is the value of covariate q in county i, and
is the value of covariate q in county i, and  is the class- and covariate-specific regression coefficient (57–61). We set the class with the smallest fixed intercept (smallest average suicide rate at the start of the study period) as the reference category, and we calculated rate ratios for other classes relative to this class.
is the class- and covariate-specific regression coefficient (57–61). We set the class with the smallest fixed intercept (smallest average suicide rate at the start of the study period) as the reference category, and we calculated rate ratios for other classes relative to this class.
Note that in transforming posterior probabilities of class membership assigned by the GMM to a categorical variable ( ), information on uncertainty of class membership is lost. To continue to account for classification uncertainty, we weighted counties in the multinomial model by GMM posterior class probabilities.
), information on uncertainty of class membership is lost. To continue to account for classification uncertainty, we weighted counties in the multinomial model by GMM posterior class probabilities.
RESULTS
Table 1 shows the model-estimated parameters for the selected 5-class model. Parameter estimates show that the two clusters with the lowest rates have considerable differences in intercept variance and error variance—that is, the intercounty heterogeneity of the suicide rate at the start of the study period and the intracounty residual during the study period, respectively—while the other parameters are more comparable (Table 1). Larger error variance was also estimated for counties in the two highest rate classes, probably influenced by low populations in these counties. The APPA was consistently high (≥0.85) and above the generally recommended threshold (0.70). Counties classified in the highest and middle-highest rate clusters had the steepest slopes (i.e., the fastest rate of increase) during the study period, at 0.69 and 0.56, respectively.
Table 1.
Estimated Parameters for a 5-Class Overall Growth Mixture Model of Suicide Mortality (Deaths/100,000a) in 3,140 Counties, United States, 2008–2020b
| Parameter c | Rate Class | ||||
|---|---|---|---|---|---|
| Lowest | Middle Lowest | Middle | Middle Highest | Highest | |
Intercept ( ) ) |
12.08 | 12.91 | 14.26 | 16.87 | 23.63 |
Slope ( ) ) |
0.41 | 0.38 | 0.44 | 0.56 | 0.69 |
Intercept variance ( ) ) |
4.17 | 2.01 | 1.28 | 1.08 | 1.03 |
Slope variance ( ) ) |
0.10 | 0.09 | 0.23 | 0.31 | 0.94 |
Intercept-slope covariance ( ) ) |
0.42 | 0.17 | 0.13 | 0.04 | 0.03 |
Error variance 
|
7.34 | 35.69 | 104.25 | 364.54 | 2,121.11 |
| Percentage of counties | 19.8 | 28.7 | 31.8 | 15.8 | 4.0 |
| APPA | 0.94 | 0.85 | 0.85 | 0.90 | 0.94 |
Abbreviation: APPA, average posterior probability of assignment.
a Average number of suicides per 100,000 population.
b Clusters are ordered by the 2008 average rate of suicide death in counties assigned to the cluster (lowest rate to highest rate).
c Estimates from the base model were not adjusted for additional covariates.
Figure 1 shows suicide rates across time in the 5-class GMM and a map depicting the location of county clusters for the overall population. Web Figures 4 and 5 show corresponding stratum-specific components (i.e., by age and firearm involvement). Class membership was largely differentiated by intercept (i.e., suicide rate in 2008), with the two highest risk clusters also exhibiting a steeper rate of change (slope) over the study period than the other clusters. The model estimated that 20% of US counties were in the lowest suicide rate group, with an average rate in 2008 of 11.4 per 100,000 population, and an increase over time to 14.0 per 100,000 in 2020. The largest cluster comprised 32% of counties, and it was a relative midpoint across clusters in terms of rate at the start of the study period. Four percent of counties were in the highest-rate cluster; these counties had a substantially higher suicide rate than any other county cluster in 2008 (25.4/100,000 population), ending with 34.2/100,000 in 2020. No clusters in which the suicide rate was stable or declined over the study period were identified.
Figure 1.
Suicide rates across time in a 5-class growth mixture model (GMM) (A) and locations of county suicide clusters for the overall population (B), United States, 2008–2020. Panel A shows the mean trajectories of posterior estimates of county suicide rates (number of suicides per 100,000 population) according to the 5-class GMM in 3,140 US counties. Numbers shown at the end of each trajectory indicate the percentage of counties assigned to that rate class. Classes are ordered by the 2008 average rate of suicide death of counties assigned to the cluster (lowest rate to highest rate). Panel B shows a map of counties’ class assignments from the 5-class GMM. (Note that the map is not to scale.)
Web Table 1 shows the average demographic characteristics of counties included in each cluster, as well as the characteristics of suicide deaths in each cluster, in the first year of the time series (2008) and the last year (2020). Counties with the highest suicide rates in 2008 and 2020 had a higher Native American/Indigenous population proportion, a lower Asian population proportion, and the lowest population density. Indeed, in 2020, the highest-rate cluster had an average population density of 2.1 people per square mile, as compared with 1,074.18 people per square mile in the lowest-rate cluster. In terms of characteristics of suicide deaths, the highest-rate clusters had a lower proportion of male suicide deaths and a higher proportion of Native American/Indigenous deaths.
The map in Figure 1B shows that the highest-rate cluster (red) runs primarily through Montana, Wyoming, the Dakotas, New Mexico, and Texas, as well as several counties in Alaska. These states also include counties in the next highest-rate cluster (orange). The West and East coasts are largely at the lower end of the rate distribution (blue, green), although there are counties in both higher and lower rate clusters throughout all states (i.e., limited intrastate homogeneity of suicide rate).
Figure 2 shows associations between county economic characteristics at the start of the study period and cluster group membership. The highest-rate cluster was distinguished from others as having higher levels of agricultural economies and lower urban professional and blue-collar labor markets. The cluster with the lowest rate had high levels of urban professionals and lower dependence on agriculture. The roles of economic disadvantage and service economy indices were roughly similar across suicide clusters.
Figure 2.
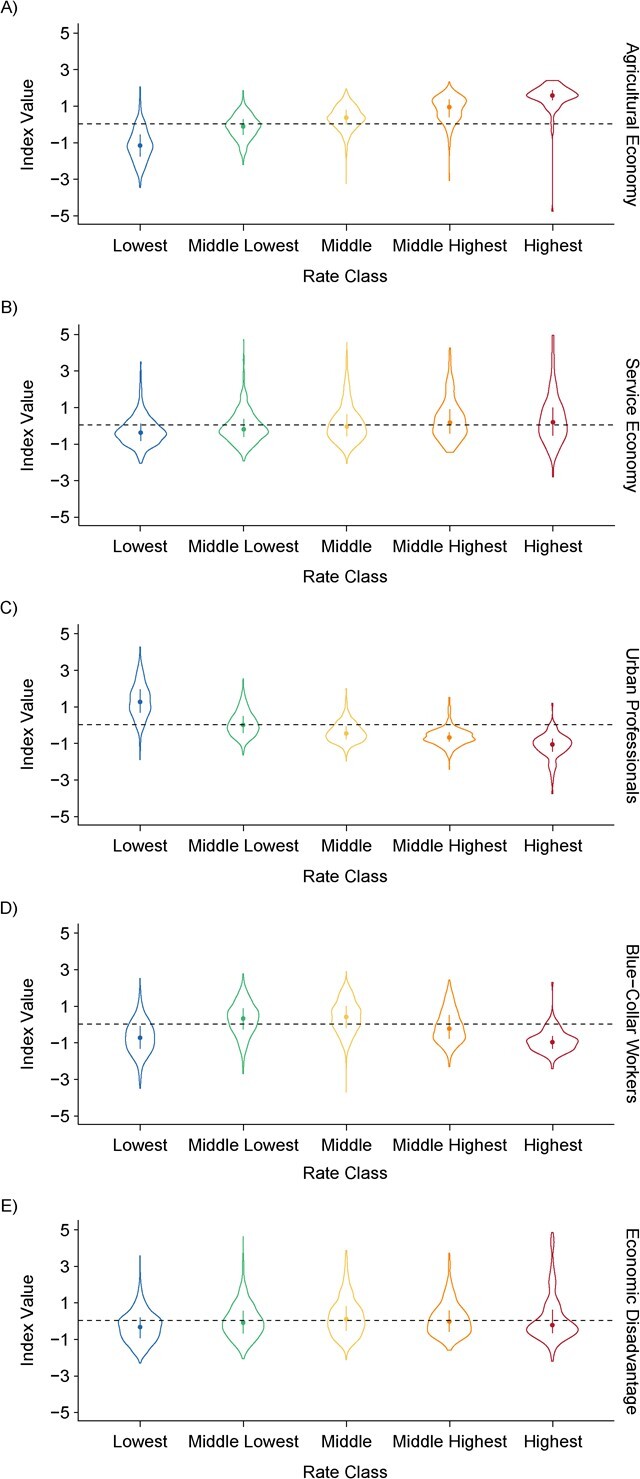
Associations between county economic characteristics at the start of the study period and cluster group membership in a study of suicide trajectories, United States, 2008–2020. The graphs show the median value (circles), interquartile range (bars), and distributions of covariate values (violin outlines) for counties assigned to each suicide rate class (x-axis) by a 5-class growth mixture model of 3,140 counties. Panels show results for areas with higher proportions of A) an agricultural economy; B) a service economy; C) urban professionals; D) blue-collar workers; and E) economic disadvantage. Rate classes: blue, lowest; green, middle lowest; yellow, middle; orange, middle highest; red, highest.
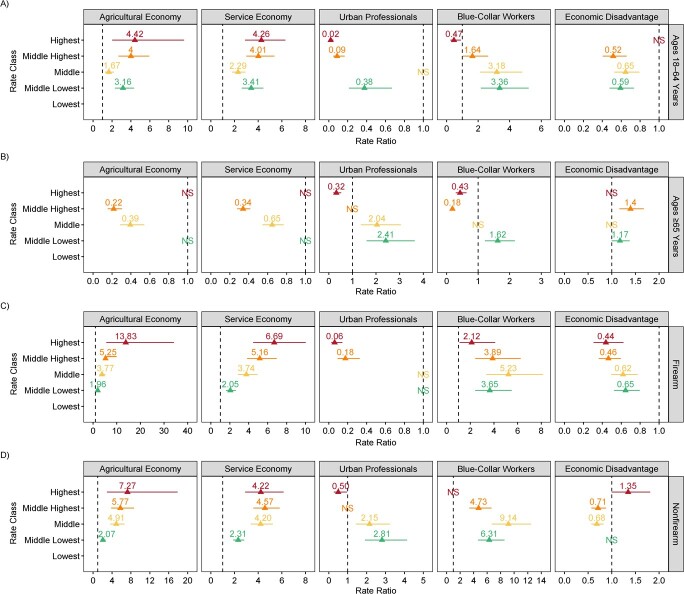
Figure 3 shows rate ratios (RRs) from multinomial regression of the association between county-level economic indices (measured in 2008–2012) and suicide trajectory class membership, with all economic indices included as covariates, as well as metropolitan status and region. Considering the highest-rate cluster, agricultural and service economies were overrepresented in every stratum except the age group ≥65 years. For example, higher agricultural (RR = 4.42) and service (RR = 4.26) economic indexes were associated with increased risk of being in the highest-rate suicide cluster among persons aged 18–64 years but not among those aged ≥65 years. Counties with a high urban professional presence were underrepresented in all strata. Counties with a higher blue-collar presence were underrepresented across both age groups (RR = 0.47 for ages 18–64 years; RR = 0.43 for ages ≥65 years) but overrepresented among firearm deaths (RR = 2.12) for the highest-rate cluster compared with the lowest-rate cluster. Counties higher on the economic disadvantage index had lower risk of being in the highest-rate cluster for firearm deaths (RR = 0.44) but higher risk of being in the highest-rate cluster for nonfirearm deaths (RR = 1.35).
Figure 3.
Rate ratios (triangles) for suicide mortality estimated by a multinomial regression model of 3,140 counties, United States, 2008–2020. A) Ages 18–64 years; B) ages ≥65 years; C) firearm deaths; D) nonfirearm deaths. Clusters are ordered on the y-axis from the lowest suicide risk at the end of the study period to the highest. The lowest suicide rate class (vertical dashed line; rate ratio = 1) was used as the reference group. “NS” (not significant) indicates a non–statistically significant estimate (e.g., the middle cluster for the blue-collar worker variable for the age ≥65 years models). Models controlled for metropolitan status and US Census region. Bars, 95% confidence intervals.
DISCUSSION
In this study, we sought to statistically identify US counties by their suicide rate trajectories from 2008 to 2020 and assess the extent to which county-level economic disadvantage and labor market characteristics predict cluster membership. First, we found 5 statistically reliable trajectories of suicide rates in the United States differentiated mainly by their suicide rates in 2008. Importantly, there was no cluster of counties where the suicide rate was stable or decreasing; suicide rates increased across all 5 clusters. Second, counties with the highest and second highest suicide rates in 2008 also had the steepest rate of increase through 2020, indicating that risk accelerated in areas for which the suicide rate was already a substantial population health burden. Third, counties with the highest rates of suicide were consistent across firearm and nonfirearm methods, as well as across both age groups (18–64 years and ≥65 years), suggesting that there may be additional underlying drivers of suicide beyond firearm access or developmental stage. Fourth, we found that county economic and labor market factors, including indices of urban professionals, blue-collar workers, and agricultural employment, measured around the start of the study period were reliably correlated with trajectory group membership, with variation in the strength and direction across age groups and methods. Counties with the highest suicide rates and steepest increases were those with more agricultural and service economies and smaller shares of urban professionals. Fifth, counties in the mountain West and along the southern border, as well as in remote areas of Alaska, consistently had the highest suicide rates, suggesting that addressing suicide will require interventions across multiple levels and dimensions. These findings are consistent with other US-based studies that documented area-level economic factors as determinants of suicide (11, 15, 17, 18). We added to this literature by examining associations through 2020 and by documenting variation across age groups and firearm use.
Given the increased burden of suicide in areas with greater concentrations of low-wage and economically precarious workforces, and given the consistent association of agricultural and service-work economies with high-rate cluster trajectories, additional efforts to support families facing financial insecurity are needed. High-rate clusters were concentrated in the mountain West and Alaska—areas with a high density of indigenous populations, among whom suicide risk is higher than in other ethnic groups due to systematic and structural oppression (62–64). Future assessment of how structural racism may mediate geographic variation in suicide, particularly in these regions, may identify mechanisms (65).
Findings are also consistent with other evidence indicating that the onset of the COVID-19 pandemic did not substantially increase suicide mortality in the United States (66). A lesson for intervention may have been learned through the COVID-19 pandemic, during which the United States implemented the largest expansion of eligibility for government-funded safety net benefits in its history (67). Despite concerns, suicide has not increased in the United States since the onset of the pandemic, and suicide deaths have decreased in many areas (66, 68). Emerging research indicates mental health benefits of antipoverty programs (69) and reduced numbers of suicides with increasing minimum wage by US state (22–24). Suicide initiatives benefit from structural interventions designed to support counties with economic precarity. Social policies may have greater impacts on suicide prevention if they consider the diverse economic and occupational profiles of places to address upstream economic determinants.
Around half of suicides in the United States are firearm-related, and national and state policies are critical to reduce access to lethal means. We find that trajectories of firearm-related suicide vary by county economic and labor market conditions, suggesting that targeting firearm suicide prevention toward counties with large shares of workers in agriculture, service, and blue-collar occupations is necessary. The need for increased firearm safety to reduce the burden of suicide is well documented, and efforts to reduce guns in the home for suicide prevention need additional support and attention (70, 71), given that current firearm policies such as background checks and other policies are not effective in preventing suicide in all states (72, 73).
While it is clear that access to firearms is an important driver of geographic disparities in US suicide (34, 74), our finding that trajectories are consistent for both firearm and nonfirearm suicides and the reality that nonfirearm suicides have also increased in recent years (75, 76) highlight the importance of suicide prevention strategies beyond controlling access to firearms. Focusing on reducing the root causes of suicidal behavior is critical, as are just-in-time interventions during a suicidal crisis (77, 78). National and state-level intervention efforts to reduce suicide death include the national 988 crisis telephone hotline, which has been live since its July 2022 rollout, is administered at the state level, and has been accompanied by increased funding by some states for mental-health crisis services (79, 80). Previous state-level analyses indicated that suicide crisis calls per capita are higher in many of the states with high suicide rates as compared with the rest of the nation (81), and increased funding and the simplicity of a 3-digit mental-health crisis phone number may thus be particularly effective in these regions, although differences in administration by state may lead to variation in support. Another area of concern that should be addressed is the increase in Internet sites with graphic content about suicide means (82), especially among youth (78), and the attendant regulatory challenges.
These results should be considered in light of their limitations. There is substantial variation across the United States in the accuracy of suicide death certification (83, 84); thus, measurement error in county-level designations of suicide should be noted. Sparsely populated counties generally have low numbers of suicides, which leads to some instability in estimates. Further, our indices of economic activity were based on data from 2008–2012 (28) and were not time-varying. While we incorporated time-varying measures of economic precarity into the model selection phase of the analysis, additional research on the role of changes in labor markets and economic precarity, as well as factors such as the minimum wage and the proportion of the population earning minimum wages, would be beneficial to move this line of research forward. Sparse data for certain subgroups precluded calculation of estimates for persons under age 18 years and by sex and racial/ethnic group, which limited our ability to draw conclusions about potential subgroup variation.
In summary, increases in suicide in the United States since 2008 have been widespread. Increases have been concentrated among counties with already comparatively high suicide rates. These places should be prioritized for allocation of suicide prevention resources. Policy-makers implementing suicide prevention programs should consider economic and labor activity as well as structural interventions that address economic and labor precarity, in addition to broader structural and social determinants of health. We encourage future research that can identify additional ecological factors (e.g., structural racism, social and health infrastructure) associated with suicide trajectories, beyond the economic factors considered here.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York, United States (Katherine Keyes, Catherine Gimbrone, Victoria Joseph, Caroline Rutherford, Mark Olfson, Madelyn Gould); Department of Environmental Health Sciences, Mailman School of Public Health, Columbia University, New York, New York, United States (Sasikiran Kandula, Jeffrey Shaman); Department of Epidemiology, Harvard T.H. Chan School of Public Health, Harvard University, Cambridge, Massachusetts, United States (Gonzalo Martinez-Ales); Department of Sociology, Center for Policy Research, and Lerner Center for Public Health Promotion and Population Health, Maxwell School of Citizenship and Public Affairs, Syracuse University, Syracuse, New York, United States (Shannon Monnat); Department of Psychiatry, Vagelos College of Physicians and Surgeons, Columbia University, New York, New York, United States (Mark Olfson, Madelyn Gould); and Columbia Climate School, Columbia University, New York, New York, United States (Jeffrey Shaman).
This work was funded by the National Institute of Mental Health (grant R01-MH121410) and the National Institute on Drug Abuse (grant U01DA055972). S.M. also acknowledges support from the National Institute on Aging–funded Center for Aging and Policy Studies at Syracuse University (grant P30AG066583) and 2 research networks funded by the National Institute on Aging (grants R24 AG065159 and 2R24 AG045061).
The data used in these analyses are not publicly available.
J.S. and Columbia University declare partial ownership of SK Analytics (New York, New York). The other authors report no potential conflicts of interest.
REFERENCES
- 1. Martínez-Alés G, Jiang T, Keyes KM, et al. The recent rise of suicide mortality in the United States. Annu Rev Public Health. 2022;43:99–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. CDC Injury Center . Leading causes of death and injury. https://www.cdc.gov/injury/wisqars/LeadingCauses.html. Reviewed November 8, 2023. Accessed April 25, 2023.
- 3. Harris KM, Majmundar MK, Becker T, eds. High and Rising Mortality Rates Among Working-Age Adults. Washington, DC: The National Academies Press; 2021. [PubMed] [Google Scholar]
- 4. National Center for Health Statistics . Suicide mortality by state. https://www.cdc.gov/nchs/pressroom/sosmap/suicide-mortality/suicide.htm. Reviewed February 15, 2023. Accessed February 28, 2023.
- 5. Olfson M, Wall M, Wang S, et al. Suicide following deliberate self-harm. Am J Psychiatry. 2017;174(8):765–774. [DOI] [PubMed] [Google Scholar]
- 6. Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187–232. [DOI] [PubMed] [Google Scholar]
- 7. Ursano RJ, Kessler RC, Heeringa SG, et al. Nonfatal suicidal behaviors in U.S. Army administrative records, 2004–2009: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Psychiatry. 2015;78(1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brent DA, Oquendo M, Birmaher B, et al. Familial pathways to early-onset suicide attempt: risk for suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry. 2002;59(9):801–807. [DOI] [PubMed] [Google Scholar]
- 9. Miller M, Hemenway D. Guns and suicide in the United States. N Engl J Med. 2008;359(10):989–991. [DOI] [PubMed] [Google Scholar]
- 10. Ha H, Tu W. An ecological study on the spatially varying relationship between county-level suicide rates and altitude in the United States. Int J Environ Res Public Health. 2018;15(4):671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Steelesmith DL, Fontanella CA, Campo J, et al. Contextual factors associated with county-level suicide rates in the United States, 1999–2016. JAMA Netw Open. 2019;2(9):e1910936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ku BS, Li J, Lally C, et al. Associations between mental health shortage areas and county-level suicide rates among adults aged 25 and older in the USA, 2010–2018. Gen Hosp Psychiatry. 70(70):44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Searles VB, Valley MA, Hedegaard H, et al. Suicides in urban and rural counties in the United States, 2006–2008. Crisis. 2014;35(1):18–26. [DOI] [PubMed] [Google Scholar]
- 14. Suk R, Hong YR, Wasserman RM, et al. Analysis of suicide after cancer diagnosis by US county-level income and rural vs urban designation, 2000–2016. JAMA Netw Open. 2021;4(10):e2129913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim D, Dev S. State- and county-level social capital as predictors of county-level suicide rates in the United States: a lagged multilevel study. Public Health Rep. 2021;136(5):538–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mobley K, Taasoobshirazi G. Predicting suicide in counties: creating a quantitative measure of suicide risk. Int J Environ Res Public Health. 2022;19(13):8173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoffmann JA, Farrell CA, Monuteaux MC, et al. Association of pediatric suicide with county-level poverty in the United States, 2007–2016. JAMA Pediatr. 2020;174(3):287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tran F, Morrison C. Income inequality and suicide in the United States: a spatial analysis of 1684 U.S. counties using geographically weighted regression. Spat Spatiotemporal Epidemiol. 2020;34:100359. [DOI] [PubMed] [Google Scholar]
- 19. Kaplan MS, Huguet N, Caetano R, et al. Economic contraction, alcohol intoxication and suicide: analysis of the National Violent Death Reporting System. Inj Prev. 2015;21(1):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kerr WC, Kaplan MS, Huguet N, et al. Economic recession, alcohol, and suicide rates: comparative effects of poverty, foreclosure, and job loss. Am J Prev Med. 2017;52(4):469–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. O’Brien R, Bair EF, Venkataramani AS. Death by robots? Automation and working-age mortality in the United States. Demography. 2022;59(2):607–628. [DOI] [PubMed] [Google Scholar]
- 22. Kaufman JA, Salas-Hernández LK, Komro KA, et al. Effects of increased minimum wages by unemployment rate on suicide in the USA. J Epidemiol Community Health. 2020;74(3):219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gertner AK, Rotter JS, Shafer PR. Association between state minimum wages and suicide rates in the U.S. Am J Prev Med. 2019;56(5):648–654. [DOI] [PubMed] [Google Scholar]
- 24. Dow WH, Godøy A, Lowenstein C, et al. Can labor market policies reduce deaths of despair? J Health Econ. 2020;74:102372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Monnat SM. Trends in U.S. working-age non-Hispanic white mortality: rural-urban and within-rural differences. Popul Res Policy Rev. 2020;39(5):805–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Monnat SM. Factors associated with county-level differences in U.S. drug-related mortality rates. Am J Prev Med. 2018;54(5):611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pierce JR, Schott PK, Caliendo L, et al. Trade liberalization and mortality: evidence from US counties. Am Econ Rev Insights. 2020;2(1):47–63. [Google Scholar]
- 28. Monnat SM, Peters DJ, Berg MT, et al. Using census data to understand county-level differences in overall drug mortality and opioid-related mortality by opioid type. Am J Public Health. 2019;109(8):1084–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rossen LM, Hedegaard H, Khan D, et al. County-level trends in suicide rates in the U.S., 2005–2015. Am J Prev Med. 2018;55(1):72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ivey-Stephenson AZ, Crosby AE, Jack SPD, et al. Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death—United States, 2001–2015. MMWR Surveill Summ. 2017;66(18):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kegler SR, Stone DM, Holland KM. Trends in suicide by level of urbanization—United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pettrone K, Curtin SC. Urban-rural differences in suicide rates, by sex and three leading methods: United States, 2000–2018. NCHS Data Brief. 2020;(373):1–8. [PubMed] [Google Scholar]
- 33. Knapp EA, Bilal U, Dean LT, et al. Economic insecurity and deaths of despair in US counties. Am J Epidemiol. 2019;188(12):2131–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Martínez-Alés G, Gimbrone C, Rutherford C, et al. Role of firearm ownership on 2001–2016 trends in U.S. firearm suicide rates. Am J Prev Med. 2021;61(6):795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Haw C, Hawton K, Niedzwiedz C, et al. Suicide clusters: a review of risk factors and mechanisms. Suicide Life Threat Behav. 2013;43(1):97–108. [DOI] [PubMed] [Google Scholar]
- 36. Martínez-Alés G, Pamplin JR, Rutherford C, et al. Age, period, and cohort effects on suicide death in the United States from 1999–2018: moderation by sex, race, and firearm involvement. Mol Psychiatry. 2021;26(7):3374–3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. National Vital Statistics System . Mortality statistics. https://www.cdc.gov/nchs/nvss/deaths.htm. Reviewed November 16, 2023. Accessed February 28, 2023.
- 38. World Health Organization . ICD-10: International Statistical Classification of Diseases and Related Health Problems. Tenth Revision. 2nd ed. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 39. National Center for Health Statistics . U.S. Census populations with bridged race categories. https://www.cdc.gov/nchs/nvss/bridged_race.htm. Reviewed October 28, 2022. Accessed February 28, 2023.
- 40. Bureau of the Census, US Department of Commerce . SAIPE state and county estimates for 2020. https://www.census.gov/data/datasets/2020/demo/saipe/2020-state-and-county.html. Published December 2021. Revised December 16, 2021. Accessed February 28, 2023.
- 41. Bureau of Labor Statistics, US Department of Labor . QCEW data files. https://www.bls.gov/cew/downloadable-data-files.htm. Modified September 6, 2023. Accessed February 28, 2023.
- 42. Bureau of Labor Statistics, US Department of Labor . Local Area Unemployment Statistics overview. https://www.bls.gov/lau/lauov.htm. Published 2023. Modified March 17, 2023. Accessed November 29, 2023.
- 43. Economic Research Service, US Department of Agriculture . Rural-urban continuum codes. Documentation. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation/. Updated December 10, 2020. Accessed February 28, 2023.
- 44. Muthén BO, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- 45. van der Nest G, Lima Passos V, Candel MJJM, et al. An overview of mixture modelling for latent evolutions in longitudinal data: modelling approaches, fit statistics and software. Adv Life Course Res. 2020;43:100323. [DOI] [PubMed] [Google Scholar]
- 46. Grün B, Leisch F. FlexMix version 2: finite mixtures with concomitant variables and varying and constant parameters. J Stat Softw. 2008;28(4):1–35.27774042 [Google Scholar]
- 47. Grün B, Leisch F. Fitting finite mixtures of generalized linear regressions in R. Comput Stat Data Anal. 2007;51(11):5247–5252. [Google Scholar]
- 48. Leisch F. FlexMix: a general framework for finite mixture models and latent class regression in R. J Stat Softw. 2004;11:1–18. [Google Scholar]
- 49. R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. https://www.r-project.org/. Accessed February 28, 2023. [Google Scholar]
- 50. Kashyap RL. Optimal choice of AR and MA parts in autoregressive moving average models. IEEE Trans Pattern Anal Mach Intell. 1982;4(2):99–104. [DOI] [PubMed] [Google Scholar]
- 51. Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–464. [Google Scholar]
- 52. Akaike H. Likelihood of a model and information criteria. J Econom. 1981;16(1):3–14. [Google Scholar]
- 53. Lennon H. LCTMtools. https://github.com/hlennon/LCTMtools/blob/master/LCTMtools.Rproj. Accessed January 30, 2023.
- 54. Nagin DS. Model selection. In: Group-Based Modeling of Development. Cambridge, MA: Harvard University Press; 2005:61–77. [Google Scholar]
- 55. Jedidi K, Ramaswamy V, Desarbo WS. A maximum likelihood method for latent class regression involving a censored dependent variable. Psychometrika. 1993;58(3):375–394. [Google Scholar]
- 56. Ramaswamy V, Desarbo WS, Reibstein DJ, et al. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science. 1993;12(1):103–124. [Google Scholar]
- 57. van de Schoot R, Sijbrandij M, Winter SD, et al. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct Equ Modeling. 2017;24(3):451–467. [Google Scholar]
- 58. Ripley B, Venables W. nnet: Feed-Forward Neural Networks and Multinomial Log-Linear Models. (Version 7.3-19). https://cran.r-project.org/web/packages/nnet/index.html. Published May 3, 2023. Accessed December 6, 2023.
- 59. Venables WN, Ripley BD. Modern Applied Statistics With S-Plus. 4th ed. New York, NY: Springer Publishing Company; 2002. [Google Scholar]
- 60. Andersen SB, Karstoft KI, Bertelsen M, et al. Latent trajectories of trauma symptoms and resilience: the 3-year longitudinal prospective USPER study of Danish veterans deployed in Afghanistan. J Clin Psychiatry. 2014;75(9):10222. [DOI] [PubMed] [Google Scholar]
- 61. Vahabi N, Salehi M, Duarte JD, et al. County-level longitudinal clustering of COVID-19 mortality to incidence ratio in the United States. Sci Rep. 2021;11(1):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Allard MD, Brundage V Jr. American Indians and Alaska Natives in the U.S. labor force. Mon Labor Rev. 2019;November:1–29. [Google Scholar]
- 63. Brave Heart MYH, Chase J, Elkins J, et al. Historical trauma among Indigenous Peoples of the Americas: concepts, research, and clinical considerations. J Psychoactive Drugs. 2011;43(4):282–290. [DOI] [PubMed] [Google Scholar]
- 64. Gone JP, Hartmann WE, Pomerville A, et al. The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: a systematic review. Am Psychol. 2019;74(1):20–35. [DOI] [PubMed] [Google Scholar]
- 65. Friedman J, Hansen H, Gone JP. Deaths of despair and indigenous data genocide. Lancet. 2023;401(10379):874–876. [DOI] [PubMed] [Google Scholar]
- 66. Pirkis J, Gunnell D, Shin S, et al. Suicide numbers during the first 9-15 months of the COVID-19 pandemic compared with pre-existing trends: an interrupted time series analysis in 33 countries. EClinicalMedicine. 2022;51(1):101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Shafer PR. Expanded unemployment benefits and their implications for health during the COVID-19 pandemic. Health Serv Res. 2022;57(1):12–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Curtin SC, Hedegaard H, Ahmad FB. Provisional Numbers and Rates of Suicide by Month and Demographic Characteristics: United States, 2020. (Vital Statistics Rapid Release, report no. 16). Atlanta, GA: Centers for Disease Control and Prevention; 2021. [Google Scholar]
- 69. Weissman DG, Hatzenbuehler ML, Cikara M, et al. Antipoverty programs mitigate socioeconomic disparities in hippocampal volume and internalizing problems among U.S. youths [preprint]. PsyArXiv. 2022. (https://psyarxiv.com/8nhej/). Accessed September 21, 2017.
- 70. Miller M, Zhang Y, Prince L, et al. Suicide deaths among women in California living with handgun owners vs those living with other adults in handgun-free homes, 2004–2016. JAMA Psychiatry. 2022;79(6):582–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Swanson JW. Preventing suicide through better firearm safety policy in the United States. Psychiatr Serv. 2021;72(2):174–179. [DOI] [PubMed] [Google Scholar]
- 72. Kagawa R, Charbonneau A, McCort C, et al. Effects of comprehensive background check policies on firearm fatalities in four states. Am J Epidemiol. 2023;192(4):539–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Smart R, Schell TL, Cefalu M, et al. Impact on nonfirearm deaths of firearm laws affecting firearm deaths: a systematic review and meta-analysis. Am J Public Health. 2020;110(10):E1–E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Miller M, Azrael D, Hepburn L, et al. The association between changes in household firearm ownership and rates of suicide in the United States, 1981–2002. Inj Prev. 2006;12(3):178–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Joseph VA, Martínez-Alés G, Olfson M, et al. Temporal trends in suicide methods among adolescents in the US. JAMA Netw Open. 2022;5(10):e2236049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zeoli AM, Goldstick J, Mauri A, et al. The association of firearm laws with firearm outcomes among children and adolescents: a scoping review. J Behav Med. 2019;42(4):741–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kessler RC, Bauer MS, Bishop TM, et al. Evaluation of a model to target high-risk psychiatric inpatients for an intensive postdischarge suicide prevention intervention. JAMA Psychiatry. 2023;80(3):230–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Coppersmith DDL, Dempsey W, Kleiman EM, et al. Just-in-time adaptive interventions for suicide prevention: promise, challenges, and future directions. Psychiatry. 2022;85(4):317–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Miller AB, Oppenheimer CW, Glenn CR, et al. Preliminary research priorities for factors influencing individual outcomes for users of the US National Suicide Prevention Lifeline. JAMA Psychiatry. 2022;79(12):1225–1231. [DOI] [PubMed] [Google Scholar]
- 80. Fix RL, Bandara S, Fallin MD, et al. Creating comprehensive crisis response systems: an opportunity to build on the promise of 988. Community Ment Health J. 2023;59(2):205–208. [DOI] [PubMed] [Google Scholar]
- 81. Keyes KM, Rutherford C, Miech R. Historical trends in the grade of onset and sequence of cigarette, alcohol, and marijuana use among adolescents from 1976–2016: implications for “gateway” patterns in adolescence. Drug Alcohol Depend. 2019;194:51–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Twohey M, Dance GJX. Where the despairing log on, and learn ways to die. New York Times.October 12, 2021. https://www.nytimes.com/interactive/2021/12/09/us/where-the-despairing-log-on.html. Published October 21, 2021. Accessed February 28, 2023.
- 83. Rockett IRH, Caine ED. Reconciling suicides with “accidental” drug-intoxication deaths: a behaviorally based definition of self-injury mortality. Am J Public Health. 2020;110(1):73–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Ali B, Rockett IRH, Miller TR, et al. Racial/ethnic differences in preceding circumstances of suicide and potential suicide misclassification among US adolescents. J Racial Ethn Health Disparities. 2022;9(1):296–304. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.