Abstract
INTRODUCTION
We used clinical assessment records to provide pan‐Canadian estimates of the prevalence and risks associated with recent (within the last 3 days) critical wandering among home care clients, with and without dementia.
METHODS
The data source is interRAI Home Care (interRAI HC) assessments. The population was all long‐stay home care clients assessed between 2004 and 2021 in seven Canadian provinces and territories (N = 1,598,191). We tested associations between wandering and cognition and dementia diagnoses using chi‐square tests and logistic regression.
RESULTS
Approximately 84% of the sample was over the age of 65. The overall rate of recent wandering was 3.0%. Dementia diagnosis was strongly associated with two to four times higher rates in the prevalence of recent critical wandering.
DISCUSSION
InterRAI HC offers insights into the wandering risk of home care clients. This information should be used to manage risks in the community and could be shared with first responders.
Highlights
In all the study regions combined, the rate of recent wandering is 3.0%.
Dementia was associated with 18 times greater prevalence of recent critical wandering.
Home care clients at risk of wandering have complex clinical profiles that pose important risks for their health and well‐being.
Collaboration and information sharing between search and rescue and health professions is essential for managing risks related to critical wandering.
Keywords: Alzheimer's disease, critical wandering, dementia, lost person, interRAI, missing person, prevalence
1. BACKGROUND
As the world's population ages, the number of older adults living with dementia increases. Currently, the global prevalence of dementia is ≈ 55 million. 1 With ≈ 10 million new diagnoses each year, 1 the total number of cases is expected to rise to 78 million by 2030. 1 In Canada, ≈ 546,000 have been diagnosed with dementia and the prevalence is steadily increasing. 2 It is expected that by 2030 the number of Canadians with dementia will be 912,000.
Wandering is a behavior common in people living with dementia. Wandering is a locomotive behavior that may or may not be purposeful and an individual who wanders may or may not be aware of this behavior. 3 Not all wandering behaviors are problematic, 3 but the most concerning type is critical wandering. According to Algase et al. 4 critical wandering occurs when a person leaves home or a facility unaccompanied and is unaware of place or time. If unattended, an exit event can occur in which an individual with dementia gets lost and goes missing. 5 Persons living with dementia who experience a wandering‐related missing incident are at risk of serious injury or death, especially if the person is not found within the first 24 hours. 6
With an increase in the prevalence of dementia, one would expect a higher number of critical wandering incidents. However, the evidence is inconclusive. Research on prevalence estimation of wandering and critical wandering incidents has been overlooked or has yielded mixed statistics, at best. The literature on prevalence estimation of wandering and critical wandering incidents reveals significant limitations. First, there is a lack of consistency in reports of prevalence, 3 leading to disparate statistics. For example, McShane et al. 7 report that 40% of people with dementia get lost, and 5% get lost repeatedly. The Alzheimer's Association estimates 60% of people with Alzheimer's disease (AD) will wander, 8 and a considerably larger set of studies show that the prevalence of wandering varies from 11% to 50%. Second, previous studies included low sample sizes from limited secondary data sources (e.g., high percentage of missing data, from social media, and data such as police data not retained for > 5 years, 9 leading to a limited scope of the statistical analyses. Third, studies have focused on conducting cross‐sectional or correlational studies examining the risk factors associated with getting lost, leaving unclear the temporal precedence of risk factors and how the wandering prevalence changes over time. 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 Finally, most studies were located outside of the Canadian context, mainly conducted in the United States, Japan, and Korea, 12 , 13 , 14 , 19 , 20 , 21 , 23 , 24 , 25 , 27 , 28 , 30 , 31 , 32 leaving the prevalence of critical wandering in Canada unknown.
The consequence of these methodological and conceptual inconsistencies is that the prevalence of critical wandering for people living with dementia remains an open question. Thus, studies that examine the prevalence of critical wandering among Canadians living with dementia would fill a gap in the literature and inform practice. 3 Although critical wandering can occur from one's home in a community or a facility, 3 the majority of cases occur in the community. 3 If missing persons are not found within 24 hours, up to half of these individuals will experience serious injury or death. 33 Thus, accurate prevalence data from home care could be used to advocate for appropriate resources to manage risks associated with dementia‐related wandering.
In this study, we used 17 years of cross‐sectional clinical assessment records at intake from home care services based on interRAI Home Care (interRAI HC) assessments, 34 , 35 , 36 to provide pan‐Canadian estimates of the prevalence and clinical risks associated with recent critical wandering among community‐based individuals. In addition, we used longitudinal follow‐up assessments to provide an estimate of transition rates in wandering behavior to inform a synthetic estimation of longer term wandering rates.
RESEARCH IN CONTEXT
Systematic review: The authors reviewed the literature using electronic databases (e.g., PubMed). Previous publications about estimation of the prevalence of critical wandering among home care clients in Canada showed important limitations. Retrospective studies are limited by small sample sizes, poor data quality, and missing data, leading to a limited scope of the statistical analyses.
Interpretation: Research on prevalence estimation of critical wandering incidents has been overlooked or has yielded mixed statistics. Knowledge about the rates of critical wandering among home care clients in the Canadian context would inform programs and policies.
Future directions: The 5‐year estimate of ≈ 42% indicates the size of the population that might have wandering behavior at any point in the foreseeable future. This estimate identifies the need for preventive initiatives to reduce the probability of a critical wandering event to occur in the future.
2. METHODS
2.1. Sample
The population for this study included all long‐stay community‐based clients receiving publicly funded home care services between 2004 and 2021 in six provinces and one territory. These individuals typically remained on service for ≥ 60 days and received mainly personal support and nursing services to live in the community and avoid nursing home placement. In the participating regions, all eligible clients were included in the study sample except for those who died, were hospitalized, or were discharged to nursing homes in the 14 days before their initial intake assessment. The total sample was 1,598,191 unique individuals.
There are two main settings in which interRAI HC assessments were used in Canada: community settings for ongoing home care, and hospitals where persons were awaiting placement in long‐term care facilities. Our study focused on the initial intake assessment of the population of home care clients aged ≥ 18 and excluded hospital‐based assessments. We also excluded clients who were assessed to have no locomotion abilities as the focus of this study was on wandering.
2.2. Ethics
Ethics clearance was obtained through the University of Waterloo Office of Research Ethics (study code protocol: 43164). The need for informed consent was waived by the University of Waterloo ethics review board, because of the retrospective nature of the study involving secondary analyses of deidentified data.
2.3. Measures
The data source for this study was interRAI HC assessments completed as part of routine clinical practice in home care settings in Canada. interRAI is an international not‐for‐profit network of health researchers, clinicians, and policy experts focused on the development and application of comprehensive standardized assessment systems that span the continuum of health‐care settings. 37 The interRAI HC assessments are usually done at intake by regulated health professionals (e.g., nurses and social workers) to support care planning, service allocation, risk management, and outcome measurement at the personal level. 38 The data can be aggregated at the population level for need analysis, performance measurement, and case‐mix–based funding. 39 , 40 , 41 , 42 , 43
To maximize the study sample size, we combined datasets based on two generations of HC assessments. The older version, Resident Assessment Instrument–Home Care (RAI‐HC), was first implemented in Canada in 2002 and it includes the largest number of observations to date. The newer interRAI HC was first implemented in Ontario in 2018 and is now considered the pan‐Canadian standard for home care supported by the Canadian Institute for Health Information (CIHI). Both generations of assessments operationalize critical wandering and the covariates of interest in the same way. That is, the clinician completing the assessment uses all sources of information available, including direct observations, interviews of the client and caregivers, medical records, and reports from other health professionals, to obtain evidence regarding current or recent wandering behavior. The clinician exercises best judgment about what is the most appropriate response regarding wandering frequency in the last 3 days. Recent wandering that was not evident in the last 3 days but remains an important consideration was also captured. The definition of wandering excludes purposeful movement within the home and also excludes pacing behaviors. For our study, the data based on the RAI‐HC included: the Yukon Territory, British Columbia, Alberta, Manitoba (Winnipeg Regional Health Authority only), Ontario, Nova Scotia, Newfoundland, and Labrador, between January 2004 and March 31, 2018. The newer version (interRAI HC assessment) was implemented in Ontario in April 2018 and we used data collected up to the end of January 2022.
interRAI assessments are completed using all sources of information available to a clinician, including direct observation and interviews with the person being assessed, discussions with family caregivers, clinical records, and communication between staff members. The assessor uses standardized definitions provided with the interRAI HC assessment that delineates the time frames, inclusion and exclusion criteria, assessment processes, intent, and illustrative examples for each item. The assessor exercises clinical judgment as to which available source of information best reflects the person's status at the time of assessment. interRAI HC data are recorded in a person's electronic health records and are subject to data quality checks as specified by CIHI's national reporting systems. 44 The reliability and validity of interRAI assessments have been verified through extensive studies between care settings and cross‐nationally. 43 , 45 , 46 , 47 , 48 , 49
The main clinical variable of interest is the recent occurrence of critical wandering. The interRAI HC includes critical wandering incidents that occurred in the last 3 days, as well as recent episodes of wandering that suggest it is a current clinical concern. The definition of critical wandering includes moving about without discernable or rational purpose where the person may be unaware of risks to physical health or safety. It excludes purposeful movement (e.g., retrieval of food/drink, use of toilet) and it also excludes pacing back and forth. Locomotion by walking or wheelchair are included. This definition differs from others used in the literature that rely on cumulative estimates over prolonged periods of time or lifetime risk; however, such risk profiles could be evaluated using repeated interRAI assessments completed over time. Our approach was to focus on the first known assessment for the individual to estimate prevalence at the start of home care episodes. Given that these data draw from 17 years of assessment records, we also compared annual rates of wandering to determine whether there were notable historical differences in these rates.
The remaining variables of interest include demographic and clinical variables used to identify the prevalence of critical wandering within subgroups of interest and to delineate the clinical risks present among persons who do or do not have recent wandering behaviors.
There are three major clinical variables that could be used to create risk‐adjusted estimates of the prevalence of critical wandering: dementia diagnosis, cognitive impairment, and Activities of Daily Living (ADL) functioning. Diagnosis of dementia includes AD and other types of dementia as determined by a physician. Validity of the diagnostic data in interRAI assessments has been reported elsewhere. 47 The Cognitive Performance Scale (CPS) 35 is a summary measure of cognitive impairment with scores ranging from 0 (no impairment) to 6 (severe cognitive impairment). The CPS has been validated against the Mini‐Mental State Examination and Montreal Cognitive Assessment in numerous care settings. 50 , 51 The ADL Hierarchy 52 is a scale that uses four early‐, mid‐, and late‐loss ADL items to provide a score of 0 (no impairment) to 6 (total dependence). ADL impairment is relevant because it can provide a physical hindrance to wandering even when the propensity for wandering is present.
Aside from understanding the rates of wandering behavior within demographic and clinical subgroups, we estimated the rates of three types of clinical problems among those with and without critical wandering: mental health issues, physical health concerns, and medication use. We chose the following clinical factors because they could pose imminent risks to the health and safety of a person with wandering behavior (and in some cases to the well‐being of others). The specific issues of interest regarding health risks for persons who go missing included:
Any presence of aggressive behaviors including physical abuse, verbal abuse, socially inappropriate behavior, and physical resistance to care;
Scores of ≥ 3 on the Depression Rating Scale (DRS), 53 which indicates potential depression;
Any presence of hallucinations or delusions;
Daily bladder incontinence;
Health instability based on scores of ≥ 3 on the Changes in Health, End‐Stage Disease and Signs and Symptoms (CHESS) scale, 49 which has been shown to be highly predictive of mortality in various settings, including home care;
Multiple falls in the last 90 days;
Severe or complete hearing impairment;
Daily bowel incontinence;
Severe or complete vision impairment;
Polypharmacy based on nine or more medications;
Use of four types of psychoactive medications: antipsychotics, antidepressants, anxiolytics, and sedatives.
2.4. Analyses
We used the first assessment for each person to estimate the rate of critical wandering at the start of the long‐stay episode of home care. The RAI‐HC and interRAI HC datasets were merged using the items that were consistent between the two generations of instruments. Items with different response sets were harmonized to ensure that common measures were used over time. All cross‐tabulations were completed using chi‐square tests of significance. Except where noted, all subgroup differences reported in this paper were significant at the p < 0.05 levels. Also, we tested associations between wandering and dementia and cognitive impairment using cross‐tabulations and chi‐square tests of significance. In addition, we used observed 6‐month rates of new wandering behavior for synthetic estimates of the longitudinal prevalence of ever wandering over time. To quantify the strength of the association among dementia diagnosis, cognition, and wandering, we fitted a logistic regression model to obtain the c statistic.
We estimated the prevalence of wandering among newly admitted home care clients using the full sample of 1,598,191 individuals as the denominator. The numerator was based on persons with any wandering behavior in the last 3 days or for whom wandering was not exhibited in the last 3 days but concerns about wandering are currently present from the perspective of the clinician. In addition, we stratified the estimates of the prevalence of wandering at intake by year to examine temporal trends.
We also created a cohort of 603,218 individuals who had an initial assessment at intake with a follow‐up reassessment in the next 6 months to estimate the rates of new wandering behavior over time. We then applied these transition rates to provide a synthetic estimate of the prevalence of ever wandering over a 5‐year time period. All analyses were done with SAS version 9.4.
3. RESULTS
Table 1 shows the distribution of key demographic and clinical stratification variables in the study sample as well as the rates of recent wandering within subgroups of those variables. The bulk of the data came from Ontario home care clients with the smallest numbers from the Yukon Territory. That said, even though the percentages for regions were skewed toward Ontario, the relative sizes of the samples match the order of differences in sizes of the full populations in these regions.
TABLE 1.
Sample characteristics and rates of recent wandering among community‐assessed home care clients, Canada.
| Percentage (n) in sample | Percentage (n) with wandering | |||
|---|---|---|---|---|
| Variable | % | N | % | N |
| Province/territory a | ||||
| Alberta | 8.0 | 128,290 | 4.3 | 5551 |
| British Columbia | 12.6 | 202,010 | 3.6 | 7241 |
| Manitoba | 2.8 | 43,974 | 1.4 | 616 |
| Newfoundland and Labrador | 1.3 | 20,795 | 4.5 | 927 |
| Nova Scotia | 2.9 | 46,813 | 3.2 | 1484 |
| Ontario | 72.3 | 1,154,901 | 2.8 | 32,781 |
| Yukon Territory | 0.09 | 1408 | 2.9 | 41 |
| All regions | 100.0 | 1,598,191 | 3.0 | 48,641 |
| Age group | ||||
| < 65 | 15.7 | 251,476 | 1.5 | 3841 |
| 65–74 | 16.4 | 261,520 | 2.7 | 7093 |
| 75–84 | 33.7 | 538,689 | 3.7 | 19,706 |
| 85+ | 34.2 | 546,505 | 3.3 | 18,001 |
| Sex | ||||
| Female | 60.9 | 973,007 | 2.8 | 27,523 |
| Male | 39.1 | 625,184 | 3.4 | 21,118 |
| Dementia diagnosis | ||||
| Not present | 76.4 | 1,220,623 | 0.6 | 7790 |
| Present | 23.6 | 377,568 | 10.8 | 40,851 |
| Cognitive Performance Scale | ||||
| 0 | 35.3 | 563,697 | 0.1 | 310 |
| 1 | 16.9 | 270,100 | 0.3 | 901 |
| 2 | 34.9 | 558,311 | 2.2 | 12,463 |
| 3 | 7.9 | 126,021 | 14.4 | 18,120 |
| 4 | 1.1 | 18,185 | 21.9 | 3975 |
| 5 | 3.4 | 54,077 | 23.2 | 12,555 |
| 6 | 0.5 | 7799 | 4.1 | 317 |
| Activities of Daily Living Hierarchy Scale | ||||
| 0 | 57.8 | 923,649 | 1.1 | 10,439 |
| 1 | 12.2 | 194,758 | 6.3 | 12,196 |
| 2 | 14.9 | 237,550 | 4.9 | 11,619 |
| 3 | 8.4 | 134,856 | 8.3 | 11,094 |
| 4 | 3.9 | 62,615 | 4.3 | 2522 |
| 5 | 2.3 | 36,162 | 2.2 | 731 |
| 6 | 0.5 | 8593 | 0.5 | 40 |
Based on raw population counts for the included regions, Ontario is over‐represented and Alberta, British Columbia, and Manitoba are somewhat under‐represented. In part this is due to Ontario being one of the first provinces to implement the interRAI home care assessment, so those data span a longer time period than provinces that are more recent adopters.
In all study regions combined, the overall rate of recent wandering was 3.0%, representing 48,641 unique individuals in the study period. The prevalence rates of recent wandering were similar in most regions except for Alberta and Newfoundland and Labrador where the relative rates were ≈ 50% higher (4.3% and 4.5%, respectively) and Manitoba where the relative rates were half the overall average (1.4%).
The sample comprised mainly older adults, with 84.3% over the age of 65. As expected, the rates of wandering were higher among older age groups, with the peak rates between ages 75 and 84, declining somewhat in the oldest old. The sample was also predominately female (60.9%). Although the sex differences were statistically significant, the absolute differences in recent wandering for males and females were relatively modest (3.4% and 2.8%, respectively).
A dementia diagnosis including AD or other dementias was present in 23.6% of the sample, and dementia was strongly associated with the prevalence of recent wandering χ 2 [(1, N = 1,598,191) = 101,298.866, p < 0.0001]. Among those without a dementia diagnosis, the rate of wandering was only 0.6% but the rate was 18 times higher for those with a dementia diagnosis (10.8%). Of the 48,461 individuals with recent wandering, 40,851 had a dementia diagnosis.
It is important to recall that the severity of symptoms is rarely the same within diagnostic groups. Hence, while it is informative to consider dementia diagnosis, it is perhaps more revealing to examine the relationship between clinical signs of cognitive impairment and wandering. Table 1 shows that ≈ one third of home care clients are cognitively intact and they have a rate of wandering of 0.1%. Approximately half of the clients have mild cognitive impairment (CPS of 1–2), and rates of wandering increased immediately with the presence of cognitive impairment. However, with a CPS score of 3, indicating moderate cognitive impairment (≈ 8% of the sample) the rates of wandering already exceeded the estimates based on dementia diagnosis alone. In the CPS categories of 4 and 5 (representing ≈ 5% of clients), the rates of recent wandering exceeded 20% with the CPS 5 group having rates > 230 times higher in relative terms compared to the cognitively intact group. We found that cognitive impairment was strongly associated with the prevalence of recent wandering (in bivariate crosstabulations χ 2 = 176322.0, df = 7, p < 0.0001). Note, however, that the rate of wandering in the most severely cognitively impaired group drops to ≈ 4%. In other words, there is a strong non‐linear relationship between cognitive impairment and wandering that is not evident when one considers diagnosis alone. That is, the rate of wandering increases exponentially until the second highest level of cognitive impairment, but it drops off dramatically among persons with the most severe level of impairment.
Table 1 also shows the relationship between ADL impairment and wandering. ADL performance is known to be strongly associated with cognition, so one might expect to see parallel findings as noted for the CPS above. However, the relationship of ADL function with wandering is notably different. Rates of recent wandering are higher in moderately higher ADL groups (peaking in ADL Hierarchy level 3), but they drop off notably with more severe impairment with rates of ≈ 0.5% in the most severely impaired group.
Figure 1 shows the estimates of wandering for the pan‐Canadian sample by year. There were statistically significant (χ 2 = 3560.2, df = 19, p < 0.0001) annual fluctuations in these rates with the lowest levels occurring in 2007 (1.9%) and the highest values observed in 2021 (4.8%). These differences could be a result of a number of factors, including changes in the case mix of home care clients over time as well as the inclusion of more provinces/territories that adopted the interRAI assessment system in later years.
FIGURE 1.
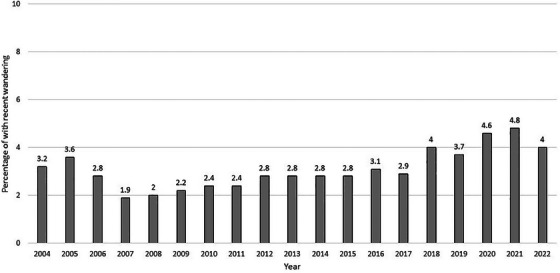
Prevalence of recent wandering among new home care clients by year, Canada.
Table 2 shows synthetic estimates of the transitions in rates of ever wandering over a 5‐year time period based on the observed rates in the baseline cohort of 79,230 individuals who remained in home care and were reassessed in the next 6 months on average. For the initial longitudinal cohort, 4.8% had a new incident of wandering when they had no prior wandering. This means that by the first follow‐up assessment, the percentage who had any wandering behavior at any time in the observation period was observed to be 9.1%. If one were to extend these baseline rates with the assumption that the rates are fixed over time, there was no loss to follow‐up, and the composition of risk factors was unchanged in the cohort (i.e., no increase in the prevalence of dementia or cognitive impairment), we estimate that 41.7% of the baseline cohort would have had at least one wandering episode in the 5‐year window.
TABLE 2.
Synthetic estimate of prevalence of ever wandering over 5‐year period based on incidence of new wandering in baseline cohort from initial assessment to next reassessment.
| 6‐month reassessment | No wandering (n) | New wandering (n) | Ever wandered (n) | Total (N) | Ever wandered (%) |
|---|---|---|---|---|---|
| 1 | 566,135 | 21,408 | 37,083 | 603,218 | 6.1 |
| 2 | 544,727 | 20,092 | 37,083 | 581,810 | 9.7 |
| 3 | 524,635 | 19,332 | 56,415 | 581,050 | 13.0 |
| 4 | 505,303 | 18,619 | 75,034 | 580,337 | 16.2 |
| 5 | 486,684 | 17,933 | 92,967 | 579,651 | 19.3 |
| 6 | 468,751 | 17,272 | 110,240 | 578,990 | 22.3 |
| 7 | 451,479 | 16,636 | 126,875 | 578,354 | 25.2 |
| 8 | 434,843 | 16,023 | 142,898 | 577,741 | 27.9 |
| 9 | 418,820 | 15,432 | 158,331 | 577,150 | 30.6 |
| 10 | 403,387 | 14,864 | 173,194 | 576,582 | 33.1 |
Figure 2 demonstrates the importance of considering both diagnosis and cognitive performance when estimating the prevalence of recent wandering. For both persons with and without a dementia diagnosis, the rate of wandering is exponentially higher among groups with more cognitive impairment with peak values for CPS levels 4 and 5. In both groups, the rates of wandering are dramatically lower in the most severely impaired CPS levels. However, within the same CPS groups, the rates of recent wandering are higher in those with a dementia diagnosis. Conversely, if one considered only those with a dementia diagnosis a large portion of persons with high risks of wandering would be missed. A logistic regression model that includes only the dementia diagnosis variable provided a c statistic of 0.81 (see Table S1 in supporting information); however, when the CPS was added to the model as a class variable to allow for non‐linear effects the c statistic rose to 0.91. The patterns for the odds ratios in the model with both dementia diagnosis and CPS scores in Table S1 are consistent with the percentage distributions shown in Figure 2.
FIGURE 2.
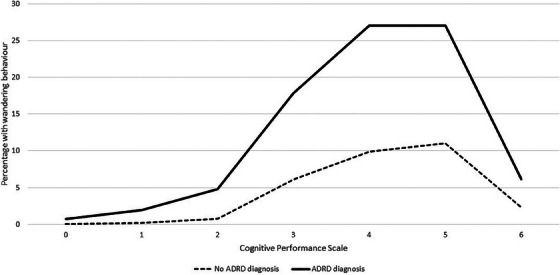
Percentage of home care clients with recent wandering by cognitive performance and dementia diagnosis, Canada. ADRD, Alzheimer's disease and related dementias.
Among home care clients with recent wandering, 84.0% have a diagnosis of AD or other dementias, but for 16.0% this diagnosis was not present. Critical wandering among persons with cognitive impairments poses serious concerns because of risks related to environmental exposure, injury in hazardous environments, and difficulty in locating persons who may be confused or disoriented. However, in addition to the risks associated with impairments in cognitive skills for decision making and memory there are other important clinical problems that elevate health risks if unaddressed, or that may make interactions with first responders (or the general public) challenging. Figure 3 shows the percentage of home care clients with and without recent wandering who present with different types of clinical concerns, including issues related to mental health, physical health, and medication use. In all cases, except for polypharmacy, the rates of the highlighted clinical problems are greater among those with recent wandering than those without the behavior. This means that while each of the shown health concerns are important for all home care clients, they are even more important for those with recent wandering.
FIGURE 3.
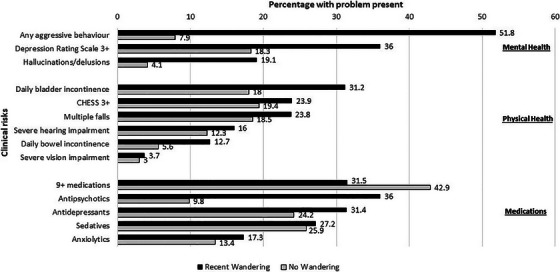
Percentage of home care clients with clinical risks present by recent wandering, Canada. Aggressive behavior includes any verbal or physical abuse, socially inappropriate behavior, or resisting care in the last 3 days. DRS scores of ≥ 3 are a conventional threshold for potential depression. CHESS is a measure of health instability and a score of ≥ 3 is associated with a substantial increase in risk of mortality. Medication items deal with use in the last 7 days. CHESS, Changes in Health, End‐Stage Disease and Signs and Symptoms; DRS, Depression Rating Scale.
In terms of mental health concerns, Figure 3 shows marked differences in the two study groups with respect to presence of any aggressive behavior. Home care clients without recent wandering have rates of aggressive behaviors < 10% but the rates exceed 50% among those with recent wandering. In addition, rates of depressive symptoms suggestive of potential depression (DRS of ≥ 3) are about twice as high among those with recent wandering. Also, the rates of hallucinations and delusions are almost five times higher in the wandering group compared to those without recent wandering.
The differences in health concerns are also evident with respect to physical health but the relative differences are not of the same magnitude as seen with mental health indicators. Approximately one third of clients with wandering behavior have daily bladder incontinence and ≈ one quarter have substantially increased risk of mortality based on a CHESS score of ≥ 3. In addition, ≈ one quarter of those who have recently wandered also had ≥ 2 falls in the last 90 days. Hearing impairments and daily bowel incontinence are less common, but still more likely to be present among those who wander. Only severe or total vision impairments are similar between the two groups affecting ≈ 4% of those with recent wandering.
Polypharmacy is present at a higher rate among those who do not have recent wandering; however, it occurs for ≈ one third of those with recent wandering. Not surprisingly the rates of use of all four types of psychoactive medications are higher among those with recent wandering; however, the starkest difference is with respect to antipsychotic use. Among those with recent wandering, 36% received antipsychotic medications compared to ≈ 10% of those without recent wandering.
4. DISCUSSION
Our analyses indicate that the prevalence of wandering behavior among home care clients is ≈ 3% among new intakes to that care setting; however, these rates vary over time and among regions. Although this rate may appear low, the longer term estimate of forever wandering could include up to one third of clients over a 5‐year period. There is a strong association between wandering and dementia diagnoses; however, measures of the severity of cognitive impairment provide much more precise information about risk levels than diagnosis does on its own. Our analyses also show that persons with wandering behavior experience many different additional clinical problems that can pose important risks to their health and would require the attention of first responders and health professionals.
This research addressed four major shortcomings in the literature. First, the small sample size is a problem in the literature put forth by Lai and Arthur. 54 The sample of 1,598,191 unique individuals examined here is notably larger than is typical of this literature. Second, sampling bias is a major threat to the validity of most prevalence studies 54 ; however, the present estimates were from population‐level data for all eligible home care recipients in six provinces and one territory of Canada. Therefore, our estimates can be assumed to be representative of home care clients in these regions. Third, many studies dealt with wandering in nursing home settings, but this is one of the first to examine wandering in home care. In a four‐country comparison of home care and nursing home settings, Guthrie et al. showed that Canadian nursing home residents have more severe cognitive impairment, lower rates of mobility, more severe ADL impairment, higher rates of impairment in expressive and receptive communication, and higher rates of daily incontinence than Canadian home care clients. 55 In addition to these important differences in clinical characteristics, these populations have different risk profiles and there are different control and oversight resources available to manage wandering in the two settings. Fourth, our study extends the examination of risk factors beyond dementia alone to include cognitive impairment and other clinical conditions. Dementia diagnoses are often under‐reported in electronic medical records. 56 Moreover, reliance on diagnosis alone provides no insight into the severity of dementia, which is strongly associated with wandering. Therefore, to have a true estimate of the magnitude of risk of wandering related to dementia, it is essential to also have a direct measure of the severity of cognitive impairment.
It is also important to specify an observation period when reporting prevalence rates of wandering. Our study provided empirical estimates of the short‐term risks of wandering and synthetic estimates of the long‐term risk of it occurring. Lifetime estimates will always be greater than point estimates. Our results showed that at a given point in time, ≈ 3% of home care clients have had recent wandering behavior in the last 3 days. However, if one were to estimate that rate over a 5‐year period one could expect rates of any occurrence in the last 5 years to be as high as 42%. Differences in observational time periods will be an important explanation for inconsistencies in prevalence estimates in the literature. Nonetheless, it is important to consider both the immediate measures that must be taken to manage imminent risks of critical wandering (e.g., 2–4 weeks), while also considering the longer term implications such as ongoing stress and concern for family caregivers. 57
The practical implications of these differences in prevalence estimates are highly relevant for families, health professionals, and first responders. The point estimate of 3% highlights the need for immediate actions to protect safety of clients and support family caregivers. The 5‐year estimate of 42% identifies the need for preventive initiatives to reduce the probability of a critical wandering event occurring in the future. 15
Our results also demonstrate the complexity of the health needs of persons with wandering behaviors. While dementia and severity of cognitive impairment are important factors to consider, there are many additional health concerns that must be addressed in this population. 58 Like other home care clients, persons with wandering behavior have diverse physical and mental health concerns in addition to impaired cognition and memory. There are several implications for caregivers and first responders when these individuals are lost. First, search and rescue professionals must be trained to understand factors affecting how this population will respond, which includes the effects of dementia on memory and decision making. 59 Second, indicators of aggressive behaviors, depression, and psychosis are prevalent in the population with wandering behaviors. This means that first responders should have broad training in mental health considerations when dealing with persons who are lost. 60 Third, problems with continence (e.g., bladder and bowel) could affect a person's level of distress when lost and may also result in stigma, which makes help from others in the community less likely to occur. 61 Fourth, the high rates of high CHESS scores in this population suggest that they are very frail with complex medical problems posing elevated risks of mortality even in controlled environments. Fifth, several other health concerns pose risks if not attended to rapidly. For example, the high rates of multiple falls among those with wandering behavior means that they have a higher propensity to fall again without appropriate supports. 62 Sixth, cognitive impairment and sensory impairments could affect a person's judgment and elevate safety risks in hazardous environments (e.g., crossing streets in heavy traffic). Finally, polypharmacy and use of psychoactive medications could result in adverse medical events due to non‐adherence of medication regimens when lost.
There is some discussion in the literature about establishment of registries to support management of risks related to wandering. 59 , 63 In jurisdictions that do not yet have interRAI systems implemented, new registries could consider the use of the interRAI HC for the assessment of risks related to wandering. In jurisdictions that have already implemented interRAI HC assessments, this system should provide the first line of information for this population. The assessments are updated routinely, have been tested for psychometric rigor, are completed by health professionals as part of routine practice, and are supported by sophisticated data management systems. Any additional registry for that population would represent an unnecessary, redundant cost. For sectors not covered by the interRAI HC assessments, it would be most cost effective to establish risk assessments that are compatible with the interRAI standard like the interRAI Check‐Up for primary care. 63
To maximize the opportunity to manage risks related to getting lost, it is important for stakeholders to work together to ensure that interRAI assessment data can be used in all stages of the strategy to manage these risks. In other words, clinicians should use and interpret interRAI assessments to inform their judgment about levels of risk to the person and to engage the person and support system in a shared decision‐making process about how to manage risk. In addition, home care professionals should work with first responders to ensure that there is timely sharing of information about clinical risks identified in the HC (or other sources) when incidents of getting lost occur. It would be technically feasible to include health information from clinical assessments like the interRAI HC on tracking devices; however, privacy, ethical, and safety concerns might preclude this approach. Instead, protocols should be established that respect privacy considerations while also allowing for timely sharing of important health information that pertains directly to the search and rescue situation (e.g., ability to communicate, behavior patterns, fall risk). Such communication protocols for health data sharing between health professionals and first responders should be established pre‐emptively rather than in a moment of crisis.
There are several next steps to pursue in this research. First, interRAI should develop a specific algorithm that flags risks of critical wandering incidents. This can be used for care planning at the person level and can be combined with geospatial information to allow first responders to understand risk patterns at the community level. Second, the synthetic analyses done here to estimate wandering incidents over a longer time period should be done using actual longitudinal records that account for censoring and changes in risk factors over time. Finally, cross‐sector comparisons using interRAI data in nursing homes and mental health environments would also be of interest to understand risks in other contexts and to identify risks of becoming lost with transitions from home care to other care settings.
In conclusion, our evidence shows that wandering behavior is a common problem in home care settings that poses considerable risk to the person and involves person‐level and environmental risk factors if they become lost. The factors leading to wandering behavior and the factors exacerbating health risks when lost are diverse, serious, and complex.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare. Author disclosures are available in the supporting information.
CONSENT STATEMENT
The University of Waterloo Ethics Review Board approved this study (study code protocol: 43164). As this was a secondary data analysis study, no consent to participate was applicable. The need for informed consent was waived by the University of Waterloo Ethics Review Board, because of the retrospective nature of the study.
Supporting information
Supporting Information
Supporting Information
ACKNOWLEDGMENTS
This work was supported by the Search and Rescue New Initiative Fund (SAR NIF) program, Public Safety Canada (grant number 22005).
Cruz AM, Perez H, Jantzi M, Liu L, Hirdes JP. Pan‐Canadian estimates of the prevalence and risks associated with critical wandering among home care clients. Alzheimer's Dement. 2024;20:7079–7089. 10.1002/alz.14195
REFERENCES
- 1. World Health Organization [WHO] . Dementia. WHO; 2021. Accessed August 23, 2022. https://www.who.int/news‐room/fact‐sheets/detail/dementia [Google Scholar]
- 2. Alzheimer Society of Canada . Prevalence and Monetary Costs of Dementia in Canada: Population Health Expert Panel. Alzheimer Society of Canada; 2016. [Google Scholar]
- 3. Petonito G, Muschert GW, Carr DC, Kinney JM, Robbins EJ, Brown JS. Programs to locate missing and critically wandering elders: a critical review and a call for multiphasic evaluation. Gerontologist. 2013;53:17‐25. doi: 10.1093/geront/gns060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Algase DL, Moore DH, Vandeweerd C, Gavin‐Dreschnack DJ. Mapping the maze of terms and definitions in dementia‐related wandering. Aging Ment Health. 2007;11:686‐698. doi: 10.1080/13607860701366434 [DOI] [PubMed] [Google Scholar]
- 5. Houston AM, Brown LM, Rowe MA, Barnett SD. The informal caregivers’ perception of wandering. Am J Alzheimers Dis Other Demen. 2011;26:616‐622. doi: 10.1177/1533317511432731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alzheimer's Association . Alzheimer's Disease Facts and Figures. Alzheimers Dis Dement n.d. Accessed August 23, 2022. https://www.alz.org/alzheimers‐dementia/facts‐figures
- 7. McShane R, Gedling K, Kenward B, Kenward R, Hope T, Jacoby R. The feasibility of electronic tracking devices in dementia: a telephone survey and case series. Int J Geriatr Psychiatry. 1998;13:556‐563. doi: 10.1002/(SICI)1099-1166(199808)13:83C;556::AID-GPS8343Et;3.0.CO;2-6 [DOI] [PubMed] [Google Scholar]
- 8. Alzheimer's Association . Wandering. Alzheimers Dis Dement n.d. Accessed August 23, 2022. https://alz.org/help‐support/caregiving/stages‐behaviors/wandering
- 9. Ferguson L. Risk factors and missing persons: advancing an understanding of ‘risk.’ Humanit Soc Sci Commun. 2022;9:1‐10. doi: 10.1057/s41599-022-01113-8 [DOI] [Google Scholar]
- 10. McShane R, Gedling K, Keene J, Fairburn C, Jacoby R, Hope T. Getting lost in dementia: a longitudinal study of a behavioral symptom. Int Psychogeriatr. 1998;10:253‐260. doi: 10.1017/S1041610298005365 [DOI] [PubMed] [Google Scholar]
- 11. MacAndrew M, Fielding E, Kolanowski A, O'Reilly M, Beattie E. Observing wandering‐related boundary transgression in people with severe dementia. Aging Ment Health. 2017;21:1197‐1205. doi: 10.1080/13607863.2016.1211620 [DOI] [PubMed] [Google Scholar]
- 12. Edgerly ES, Donovick PJ. Neuropsychological correlates of wandering in persons with Alzheimer's disease. Am J Alzheimers Dis. 1998;13:317‐329. doi: 10.1177/153331759801300607 [DOI] [Google Scholar]
- 13. Algase DL, Antonakos C, Beattie ERA, Beel‐Bates CA, Yao L. Empirical derivation and validation of a wandering typology. J Am Geriatr Soc. 2009;57:2037‐2045. doi: 10.1111/j.1532-5415.2009.02491.x [DOI] [PubMed] [Google Scholar]
- 14. Algase DL, Beattie ERA, Antonakos C, Beel‐Bates CA, Yao L. Wandering and the physical environment. Am J Alzheimers Dis Dementias®. 2010;25:340‐346. doi: 10.1177/1533317510365342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ali N, Luther SL, Volicer L, et al. Risk assessment of wandering behavior in mild dementia. Int J Geriatr Psychiatry. 2016;31:367‐374. doi: 10.1002/gps.4336 [DOI] [PubMed] [Google Scholar]
- 16. Ballard CG, Mohan RNC, Bannister C, Handy S, Patel A. Wandering in dementia sufferers. Int J Geriatr Psychiatry. 1991;6:611‐614. doi: 10.1002/gps.930060811 [DOI] [Google Scholar]
- 17. Dawson P, Reid DW. Behavioral dimensions of patients at risk of wandering. Gerontologist. 1987;27:104‐107. doi: 10.1093/geront/27.1.104 [DOI] [PubMed] [Google Scholar]
- 18. Beattie ERA, Song J, LaGore S. A comparison of wandering behavior in nursing homes and assisted living facilities. Res Theory Nurs Pract. 2005;19:181‐196. [PubMed] [Google Scholar]
- 19. Jeong JG, Song JA, Park KW. A relationship between depression and wandering in community‐dwelling elders with dementia. Dement Neurocognitive Disord. 2016;15:1‐6. doi: 10.12779/dnd.2016.15.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schonfeld L, King‐Kallimanis B, Brown LM, et al. Wanderers with cognitive impairment in department of veterans affairs nursing home care units. J Am Geriatr Soc. 2007;55:692‐699. doi: 10.1111/j.1532-5415.2007.01135.x [DOI] [PubMed] [Google Scholar]
- 21. de Leon MJ, Potegal M, Gurland B. Wandering and parietal signs in senile dementia of Alzheimer's type. Neuropsychobiology. 2008;11:155‐157. doi: 10.1159/000118069 [DOI] [PubMed] [Google Scholar]
- 22. Kwok TCY, Yuen KSL, Ho FKY, Chan WM. Getting lost in the community: a phone survey on the community‐dwelling demented people in Hong Kong. Int J Geriatr Psychiatry. 2010;25:427‐432. doi: 10.1002/gps.2361 [DOI] [PubMed] [Google Scholar]
- 23. Hong G‐RS, Song J‐A. Relationship between familiar environment and wandering behaviour among Korean elders with dementia. J Clin Nurs. 2009;18:1365‐1373. doi: 10.1111/j.1365-2702.2008.02566.x [DOI] [PubMed] [Google Scholar]
- 24. Volicer L, van der Steen JT, Frijters DHM. Involvement in activities and wandering in nursing home residents with cognitive impairment. Alzheimer Dis Assoc Disord. 2013;27:272‐277. doi: 10.1097/WAD.0b013e31826d012e [DOI] [PubMed] [Google Scholar]
- 25. Detweiler MB, Murphy PF, Myers LC, Kim KY. Does a wander garden influence inappropriate behaviors in dementia residents? Am J Alzheimers Dis Other Demen. 2008;23:31‐45. doi: 10.1177/1533317507309799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Okita M, Hanyu H, Hirao K, Shimizu S, Umahara T, Sakurai H. Missing incidents in individuals with dementia attending a memory clinic. J Am Geriatr Soc. 2016;64:1365‐1366. doi: 10.1111/jgs.14151 [DOI] [PubMed] [Google Scholar]
- 27. Song J‐A, Algase D. Premorbid characteristics and wandering behavior in persons with dementia. Arch Psychiatr Nurs. 2008;22:318‐327. doi: 10.1016/j.apnu.2007.10.008 [DOI] [PubMed] [Google Scholar]
- 28. Song J‐A, Lim YM, Hong G‐RS. Wandering behaviour of persons with dementia in Korea: investigation of related factors. Aging Ment Health. 2008;12:366‐373. doi: 10.1080/13607860802120821 [DOI] [PubMed] [Google Scholar]
- 29. Chung JCC, Lai CKY. Elopement among community‐dwelling older adults with dementia. Int Psychogeriatr. 2011;23:65‐72. doi: 10.1017/S1041610210000657 [DOI] [PubMed] [Google Scholar]
- 30. Klein DA, Steinberg M, Galik E, et al. Wandering behaviour in community‐residing persons with dementia. Int J Geriatr Psychiatry. 1999;14:272‐279. doi: 10.1002/(SICI)1099-1166(199904)14:43C;272::AID-GPS8963E;3.0.CO;2-P [DOI] [PubMed] [Google Scholar]
- 31. Marcus JF, Cellar JS, Ansari FP, Bliwise DL. Utility of the Algase Wandering Scale in an outpatient Alzheimer's disease sample. Int J Geriatr Psychiatry. 2007;22:801‐805. doi: 10.1002/gps.1745 [DOI] [PubMed] [Google Scholar]
- 32. Thomas DW, Glogoski C, Johnson J. The effect of a supervised walking program on wandering among residents with dementia. Act Adapt Aging. 2006;30:1‐13. doi: 10.1300/J016v30n04_01 [DOI] [Google Scholar]
- 33. Neubauer NA, Lapierre N, Ríos‐Rincón A, Miguel‐Cruz A, Rousseau J, Liu L. What do we know about technologies for dementia‐related wandering? A scoping review: examen de la portée : que savons‐nous à propos des technologies de gestion de l'errance liée à la démence? Can J Occup Ther. 2018;85:196‐208. doi: 10.1177/0008417418777530 [DOI] [PubMed] [Google Scholar]
- 34. Gray LC, Berg K, Fries BE, et al. Sharing clinical information across care settings: the birth of an integrated assessment system. BMC Health Serv Res. 2009;9:71. doi: 10.1186/1472-6963-9-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Morris JN, Fries BE, Steel K, et al. Comprehensive clinical assessment in community setting: applicability of the MDS‐HC. J Am Geriatr Soc. 1997;45:1017‐1024. doi: 10.1111/j.1532-5415.1997.tb02975.x [DOI] [PubMed] [Google Scholar]
- 36. Carpenter I, Hirdes JP. Using interRAI assessment systems to measure and maintain quality of long‐term care. Good Life Old Age. OECD Publishing; 2013:93‐139. doi: 10.1787/9789264194564-7-en [DOI] [Google Scholar]
- 37. Hirdes JP, van Everdingen C, Ferris J, et al. The interRAI suite of mental health assessment instruments: an integrated system for the continuum of care. Front Psychiatry. 2020;10:926. doi: 10.3389/fpsyt.2019.00926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Heckman G, Gray LC, Hirdes J. Addressing health care needs for frail seniors in Canada: the role of interRAI instruments. Can Geriatr Soc J CME. 2013;3:8‐16. [Google Scholar]
- 39. Hirdes JP, Poss JW, Curtin‐Telegdi N. The Method for Assigning Priority Levels (MAPLe): a new decision‐support system for allocating home care resources. BMC Med. 2008;6:9. doi: 10.1186/1741-7015-6-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Morris JN, Fries BE, Frijters D, Hirdes JP, Steel RK. interRAI home care quality indicators. BMC Geriatr. 2013;13:127. doi: 10.1186/1471-2318-13-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Poss JW, Hirdes JP, Fries BE, McKillop I, Chase M. Validation of Resource Utilization Groups Version III for Home Care (RUG‐III/HC): evidence from a Canadian home care jurisdiction. Med Care. 2008;46:380‐387. doi: 10.1097/MLR.0b013e31815c3b6c [DOI] [PubMed] [Google Scholar]
- 42. Mitchell LA, Hirdes J, Poss JW, Slegers‐Boyd C, Caldarelli H, Martin L. Informal caregivers of clients with neurological conditions: profiles, patterns and risk factors for distress from a home care prevalence study. BMC Health Serv Res. 2015;15:350. doi: 10.1186/s12913-015-1010-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Morris JN, Carpenter I, Berg K, Jones RN. Outcome measures for use with home care clients. Can J Aging Rev Can Vieil. 2000;19:87‐105. doi: 10.1017/S071498080001391X [DOI] [Google Scholar]
- 44. Canadian Institute for Health Information . Integrated interRAI Reporting System (IRRS) metadata. Canadian Institute for Health Information. n.d. Accessed September 19, 2023. https://www.cihi.ca/en/integrated‐interrai‐reporting‐system‐irrs‐metadata [Google Scholar]
- 45. Morris JN, Berg K, Fries BE, Steel K, Howard EP. Scaling functional status within the interRAI suite of assessment instruments. BMC Geriatr. 2013;13:128. doi: 10.1186/1471-2318-13-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hirdes JP, Ljunggren G, Morris JN, et al. Reliability of the interRAI suite of assessment instruments: a 12‐country study of an integrated health information system. BMC Health Serv Res. 2008;8:277. doi: 10.1186/1472-6963-8-277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Foebel AD, Hirdes JP, Heckman GA, Kergoat M‐J, Patten S, Marrie RA. Diagnostic data for neurological conditions in interRAI assessments in home care, nursing home and mental health care settings: a validity study. BMC Health Serv Res. 2013;13:457. doi: 10.1186/1472-6963-13-457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hogeveen SE, Chen J, Hirdes JP. Evaluation of data quality of interRAI assessments in home and community care. BMC Med Inform Decis Mak. 2017;17:150. doi: 10.1186/s12911-017-0547-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hirdes JP, Poss JW, Mitchell L, Korngut L, Heckman G. Use of the interRAI CHESS Scale to predict mortality among persons with neurological conditions in three care settings. PLoS ONE. 2014;9:e99066. doi: 10.1371/journal.pone.0099066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Jones K, Perlman CM, Hirdes JP, Scott T. Screening cognitive performance with the resident assessment instrument for mental health Cognitive Performance Scale. Can J Psychiatry. 2010;55:736‐740. doi: 10.1177/070674371005501108 [DOI] [PubMed] [Google Scholar]
- 51. Morris JN, Howard EP, Steel K, et al. Updating the Cognitive Performance Scale. J Geriatr Psychiatry Neurol. 2016;29:47‐55. doi: 10.1177/0891988715598231 [DOI] [PubMed] [Google Scholar]
- 52. Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol Ser A. 1999;54:M546‐M553. doi: 10.1093/gerona/54.11.M546 [DOI] [PubMed] [Google Scholar]
- 53. Burrows AB, Morris JN, Simon SE, Hirdes JP, Phillips C. Development of a minimum data set‐based Depression Rating Scale for use in nursing homes. Age Ageing. 2000;29:165‐172. doi: 10.1093/ageing/29.2.165 [DOI] [PubMed] [Google Scholar]
- 54. Lai CKY, Arthur DG. Wandering behaviour in people with dementia. J Adv Nurs. 2003;44:173‐182. doi: 10.1046/j.1365-2648.2003.02781.x [DOI] [PubMed] [Google Scholar]
- 55. Guthrie DM, Declercq A, Finne‐Soveri H, Fries BE, Hirdes JP. The health and well‐being of older adults with Dual Sensory Impairment (DSI) in four countries. PLoS ONE. 2016;11. doi: 10.1371/journal.pone.0155073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Danila O, Hirdes JP, Maxwell CJ, et al. Prevalence of neurological conditions across the continuum of care based on interRAI assessments. BMC Health Serv Res. 2014;14:29. doi: 10.1186/1472-6963-14-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Neubauer NA, Liu L. Evaluation of antecedent behaviors of dementia‐related wandering in community and facility settings. Neurodegener Dis Manag. 2020;10:125‐135. doi: 10.2217/nmt-2019-0030 [DOI] [PubMed] [Google Scholar]
- 58. Leng M, Sun Y, Chang H, Wang Z. Clustering analysis of the care problems of people with dementia based on the minimum spanning tree algorithm: a cross‐sectional study. J Alzheimers Dis. 2022;87:1637‐1646. doi: 10.3233/JAD-215682 [DOI] [PubMed] [Google Scholar]
- 59. Miguel Cruz A, Marshall S, Daum C, Perez H, Hirdes J, Liu L. Data silos undermine efforts to characterize, predict, and mitigate dementia‐related missing person incidents. Healthc Manage Forum. 2022;35:333‐338. doi: 10.1177/08404704221106156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ (Clinical research ed.). 2015;350:h369. 10.1136/bmj.h369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Murphy C, De Laine C, Macaulay M, Hislop Lennie K, Fader M. Problems faced by people living at home with dementia and incontinence: causes, consequences and potential solutions. Age Ageing. 2021;50:944‐954. doi: 10.1093/ageing/afaa262 [DOI] [PubMed] [Google Scholar]
- 62. Hoe J, Profyri E, Kemp C, et al. Risk assessment for people living with dementia: a systematic review. Int Psychogeriatr. 2023;36(4):263‐288. doi: 10.1017/S1041610223004398 [DOI] [PubMed] [Google Scholar]
- 63. Moore DH, Algase DL, Powell‐Cope G, Applegarth S, Beattie ERA. A framework for managing wandering and preventing elopement. Am J Alzheimers Dis Other Demen. 2009;24:208‐219. doi: 10.1177/1533317509332625 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information


