Abstract
Background:
Asthma, a chronic respiratory disease, is associated with high economic burden. This study estimates per-worker medical and incremental medical costs associated with treated asthma by socioeconomic and demographic characteristics, industries, medical events, and sources of payments for workers aged ≥18 years.
Methods:
We analyzed Medical Expenditure Panel Survey data from 2018 to 2020 to assess medical costs for treated asthma among workers using the International Classification of Diseases, Tenth Revision, Clinical Modification code for asthma (J45). We used two-part regression models to estimate medical and incremental medical costs controlling for covariates. All results are adjusted for inflation and presented in 2022 US dollar values.
Results:
An estimated annual average of 8.2 million workers out of 176 million had at least one medical event associated with treated asthma. The annualized estimated per-worker incremental medical costs for those with treated asthma was $457 and was highest among: those in the age group of 35–44 years ($534), in the western region ($768), of Hispanic ethnicity ($693), employed in the utility and transportation industries ($898), males ($650), and for inpatient admissions ($754). The total annualized medical costs of treated asthma was $21 billion and total of incremental medical costs was $3.8 billion.
Conclusion:
Findings of higher incremental medical costs for treated asthma among workers in certain socioeconomic, demographic, and industry groups highlight the economic benefit of prevention and early intervention to reduce morbidity of asthma in working adults. Our results suggest that the per-person incremental medical costs of treated asthma among workers are lower than that for all US adults.
Keywords: asthma, incremental medical costs, industries, medical costs, working adults
1 |. INTRODUCTION
Asthma, a chronic airway disease characterized by inflammation and variable airflow limitation, is associated with a significant economic burden among US adults.1 An estimated 16% of asthma cases among adults are related to workplace exposures.2 Asthma prevalence increased from 7.3% in 2006 to 7.7% in 2018 among US adults.3 In 2019, an estimated 20 million US adults had asthma and, of those, an estimated 8 million had asthma attacks in the past 12 months.4,5 Asthma is associated with poor quality of life, decreased productivity at work, increased healthcare utilization, and significant economic burden both globally and in the United States.1,6,7
According to the cost-of-illness approach that broadly considers medical costs and productivity losses, the economic burden of a disease comprises medical costs for treating the disease and other non-medical costs, including costs of transportation, caregiver fees, costs incurred by productivity losses, school days lost, and costs associated with premature mortality.1,7–11 Researchers have been estimating these costs using data on healthcare utilization and aggregating related estimates of average per-person costs.12–17 A pioneering study on the economic burden of asthma used this approach and data from 1983 to 1987 to estimate the costs of asthma at $6.2 billion (1990 US. dollars) which included medical costs, value of time lost from school, and productivity losses.8 Kamble and Bharmal18 reported the total estimated medical costs at $37.2 billion for the year 2004 for treated asthma for adults and children together (2007 US dollars). Since the 1990s, novel methods for cost-of-illness studies have been used, including estimating the excess cost of having a disease, including incremental medical costs.18–25 The incremental medical cost isolates the effect of a specific disease on medical cost while controlling for other factors. Recent studies that used these new methods estimated that per-person annual incremental medical costs for asthma were $1907 for 2003 and 2005 (2008 US dollars),26 $2077 for the year 2004 (2007 US dollars),18 and $3761 for the years 2008–2013 (2015 US dollars)1 among adults.
A previously healthy worker can have asthma caused from workplace exposures, which can also trigger asthma in workers with pre-existing asthma.27 An estimated 16% of new onset of asthma2 and 22% of exacerbation of pre-existing adult asthma28 are attributable to occupational exposures. Asthma caused or made worse by workplace exposures has been found to be more severe and associated with greater healthcare utilization than asthma not caused by or made worse by, occupational exposures.27–29 Research estimating the costs associated with asthma is limited, and no study has examined incremental medical costs for asthma among workers. Syamlal et al.30 estimated that during 2011–2015 the US annualized per-person average medical costs of workers associated with treated asthma was $901 for a total nationwide cost of $7 billion in 2017 US dollars. Expressing the disease burden of asthma in monetary terms can aid in comprehending the impact of the disease to help mitigate its economic burden.31–35 Therefore the objectives of the current study are: and (1) to estimate per-person medical costs and per-person incremental medical costs associated with treated asthma among workers aged ≥18 years; and (2) to assess incremental medical costs among workers with treated asthma by selected socioeconomic and demographic characteristics, industries, medical events, and sources of payments.
2 |. DATA AND METHODOLOGY
We analyzed Medical Expenditure Panel Survey (MEPS) data (AHRQ, https://meps.ahrq.gov/mepsweb/) for the years 2018–2020 to assess the total and incremental medical costs associated with treated asthma among workers (≥18 years). MEPS is a nationally representative survey of the US civilian noninstitutionalized population that collects detailed information on self-reported health conditions and associated medical events, expenditures, payment sources, and health insurance coverage.36 The MEPS data used in this study is obtained through multiple rounds of in-person interviews of the individuals. The MEPS data collection was approved by the Research Ethics Review Board and approved by the Westat IRB, established under a multi-project assurance (MPA M-1531) granted by the U.S. Office of Management and Budget. For this study, a secondary data analysis of the publicly available data were used, and National Institute for Occupational Safety and Health Internal Review Board approval was not required. In this study we examined medical events and estimated the medical and incremental medical costs associated with treated asthma among workers. All medical events for treated asthma incorporated in this study are non-fatal cases. A worker was considered to have treated asthma in the year if she or he reported at least one medical event (i.e., office-based provider visits, hospital-based outpatient visits, inpatient hospitalizations, emergency room (ER) visits, and prescription medications) with an International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code for asthma (J45) in that particular year. Incremental medical costs associated with treated asthma were estimated controlling for sex, age group, region, race/ethnicity, education, annual household income, health insurance coverage, smoking habits, and Charlson comorbidity index.37 We classified age into four groups,—(i) 18–34 years, (ii) 35–44 years, (iii) 45–64 years, and (iv) 65 years and over; region into four groups,—(i) Northeast, (ii) Midwest, (iii) Southeast, and (iv) West; race/ethnicity into four groups,—(i) Hispanic, (ii) White, non-Hispanic, (iii) Black, non-Hispanic, and (iv) Other, non-Hispanic; education status into two groups,—(i) did not complete high school, and (ii) completed high school and beyond; annual household income into three groups,—(i) less than $35,000, (ii) $35,000–$74,999, and (iii) greater than $75,000. The industries are classified into 15 groups following MEPS classification, (i) natural resources, (ii) mining, (iii) construction, (iv) manufacturing, (v) wholesale and retail trade, (vi) transportation and utilities, (vii) information, (viii) financial activities, (ix) professional and business services, (x) education, health, and social services, (xi) leisure and hospitality, (xii) other services, (xiii) public administration, (xiv) military, and (xv) unclassifiable industry.38 We used the D’Hoore adaptation of the Charlson Comorbidity Index as another independent variable and calculated it following the D’Hoore methodology.37 The Charlson Comorbidity Index is a weighted index of comorbid conditions which can alter the risk of mortality within 1 year of hospitalization for patients. The comorbidities included in this version are myocardial infarct, congestive heart failure, peripheral vascular disease, dementia, cerebrovascular disease, chronic pulmonary disease, connective tissue disease, ulcer disease, mild liver disease, hemiplegia, moderate or severe renal disease, diabetes, any tumor, leukemia, lymphoma, moderate or severe liver disease, and metastatic solid tumor.37
We combined MEPS data for the years 2018–2020 and used survey weights provided by MEPS to obtain national estimates. The survey response rates are 27.6% for 2020, 39.5% for 2019, and 42.7% for 2018.39
2.1 |. Statistical analysis
We used two-part regression models to estimate per-worker medical and incremental medical costs for treated asthma among workers, following the Manning and Mullahy40 methodology. We used Stata 17 software to conduct the analysis. In the first part, we used a logistic regression model to estimate the probability of a worker having treated asthma using the entire working population. In the second part we used a linear regression model to estimate the medical costs of the workers and it included workers who reported greater than zero dollars in medical costs associated with any medical event. We defined incremental medical cost per-worker as the difference between the predicted medical costs for workers considering a hypothetical situation, where all workers were associated with treated asthma and the predicted medical costs of the workers without treated asthma. We controlled for the same set of covariates in the analyses for both groups of workers. The incremental medical costs were also estimated by type of medical events (i.e., office-based provider visits, hospital-based outpatient visits, inpatient hospitalizations, ER visits, and prescription medications), and sources of payment (i.e., out-of-pocket, Medicare, Medicaid, and private health insurance). We controlled for sex, age group, region, race/ethnicity, education, annual household income, health insurance coverage, smoking habits, and the Charlson Comorbidity Index in all the regression models. The reference groups used were males, workers aged 18–25 years, those residing in the Northeast region, those with Hispanic ethnicity, those who have not completed high school, with an annual household income below $35,000, not covered by health insurance, nonsmokers, and a Charlson Comorbidity Index equal to zero. Using the Medical Consumer Price Index, we adjusted all costs for inflation and presented them in 2022 US dollar values.41
3 |. RESULTS
During 2018–2020, the US adult population ranged from 252.5 million in 2018 to 265.4 million persons in 2020. Of those, an estimated 175.3 million (in 2018) to 176.1 million (in 2020) were working in the 12 months before the survey interview.
Table 1 presents the estimated number and percentage distribution of workers with treated asthma during 2018–2020 by year, socioeconomic and demographic characteristics, and industries and the associated 95% confidence intervals. The number of workers with treated asthma varied from 8.1 million in 2019 to 8.3 million in 2020 and an estimated annual average of 8.2 million (4.7% of all workers). The highest annualized proportion of workers with treated asthma were female (62.7%), aged 45–64 years (43.3%), workers in the South region (33.1), non-Hispanic Whites (66.6%), those with a high school education and beyond (50.9%), workers with an annual household income of greater than or equal to $75,000 (53.6%), with a health insurance (97.4%), smokers (77.8%), and workers in the education, health, and social services (32.1%) industry.
TABLE 1.
Percentages of selected demographic characteristics of employed adults with treated asthma, 2018–2020.
| Variables | 2018 [N = 8,213,380] (95% CIs) % | 2019 [N = 8,126,462] (95% CIs) % | 2020 [N = 8,325,721] (95% CIs) % | Estimated annual average [N = 8,221,854] (95% CIs) % |
|---|---|---|---|---|
| Sex | ||||
| Female | 62.2 (57.6–66.8) | 62.7 (58.3–67) | 63.4 (59–67.9) | 62.7 (58.3–67.2) |
| Male | 37.8 (33.2–42.4) | 37.3 (33–41.7) | 36.6 (32.1–41) | 37.2 (32.8–41.7) |
| Age categories (years) | ||||
| 18–34 | 9.3 (6.5–12) | 12.5 (9.4–15.6) | 7.4 (4.9–9.9) | 9.2 (7.31–211.0) |
| 35–44 | 38 (33.1–42.9) | 35.3 (31.5–39.2) | 39.8 (35.7–43.9) | 37.7 (33.4–42) |
| 45–64 | 42.7 (37.8–47.6) | 44.4 (40.3–48.5) | 43.1 (39.4–46.9) | 43.3 (39.1–47.7) |
| ≥65 | 10 (7.2–12.7) | 7.8 (5.6–10) | 9.7 (7.2–12.2) | 9.1 (6.7–11.6) |
| Region | ||||
| Northeast | 20.4 (16.4–24.4) | 20.2 (16.1–24.2) | 21.6 (18–25.3) | 20.7 (16.8–24) |
| Midwest | 25.5 (21.4–29.5) | 22 (18.6–25.4) | 19.8 (16.8–22.8) | 22.4 (18.9–25) |
| South | 32.5 (27.8–37.2) | 32.2 (28–36.3) | 34.9 (30.8–39) | 33.1 (28.9–37.5) |
| West | 21.7 (17.2–26.2) | 25.7 (22.4–29) | 23.6 (20.5–26.7) | 23.6 (20–27) |
| Race/ethnicity | ||||
| Hispanic | 10.5 (8.6–12.5) | 13 (10.5–15.4) | 13.9 (11.6–16.2) | 12.4 (10.2–14) |
| White, non-Hispanic | 68.4 (63.9–72.8) | 65.9 (62.2–69.7) | 65.5 (61–70) | 66.6 (62.4–70.8) |
| Black, non-Hispanic | 12.7 (9.1–16.3) | 11.7 (9.3–14.2) | 13.5 (10.2–16.8) | 12.6 (9.5–15.8) |
| Other, non-Hispanic | 8.4 (6–10.8) | 9.4 (6.6–12.1) | 7.1 (4.3–9.9) | 8.3 (5.7–10.9) |
| Education | ||||
| Did not complete high school | 47.8 (43–52.7) | 48.5 (43.3–53.6) | 50.8 (45.7–55.9) | 49 (44–54) |
| High school and beyond | 52.2 (47.3–57) | 51.6 (46.4–56.7) | 49.2 (44.1–54.3) | 50.9 (46–56) |
| Annual household income | ||||
| <$35,000 | 21.9 (18.8–25.1) | 20.6 (17.2–24.1) | 18.5 (15.5–21.6) | 20.3 (17.2–23.6) |
| $35,000–74,999 | 25.2 (21.5–28.9) | 24.8 (21.1–28.6) | 27.8 (23.4–32.2) | 25.9 (22–29.9) |
| ≥$75,000 | 52.9 (48.3–57.4) | 54.5 (49.8–59.3) | 53.7 (49.5–57.8) | 53.6 (49.2–58.2) |
| Health insurance | ||||
| Health insurance | 97.4 (96.1–98.7) | 96.9 (95.5–98.3) | 98.1 (97.1–99.1) | 97.4 (96.2–98.7) |
| No health insurance | 2.6 (1.3–3.9) | 3.1 (1.7–4.6) | 2 (1–3) | 2.6 (1.3–3.8) |
| Smoking status | ||||
| Smoker | 72.9 (68.6–77.1) | 77.4 (73.3–81.5) | 83.3 (79.3–87.2) | 77.8 (73.7–81.9) |
| Non-smoker | 27.1 (22.9–31.4) | 22.6 (18.6–26.7) | 16.7 (12.8–20.7) | 22.1 (18.1–26.3) |
| Industry | ||||
| Natural resources | 0.9 (0–1.8) | 1.4 (0.5–2.3) | 1.4 (0.6–2.1) | 1.2 (0.4–2.1) |
| Mining | 0.4 (0–1) | 0.1 (0–0.4) | 0.5 (0–1) | 0.3 (0–0.8) |
| Construction | 5.2 (3–7.3) | 4 (2.4–5.5) | 3.5 (1.9–5.1) | 4.2 (2.4–6) |
| Manufacturing | 7.1 (5.2–9.1) | 6.7 (4.6–8.7) | 7.3 (5–9.5) | 7 (4.9–9.1) |
| Wholesale and retail trade | 12.5 (9.5–15.4) | 11.2 (7.8–14.6) | 12.4 (9.3–15.5) | 12 (8.9–15.2) |
| Transportation and utilities | 3.4 (2–4.9) | 4.3 (2.6–6.1) | 4.5 (2.4–6.7) | 4.1 (2.3–5.9) |
| Information | 1.9 (0.8–2.9) | 2.8 (1.4–4.2) | 2 (0.9–3.2) | 2.2 (1–3.5) |
| Financial activities | 6.2 (4.1–8.3) | 4.9 (3.1–6.8) | 7.6 (5.2–10) | 6.2 (4.1–8.4) |
| Professional and business services | 9.5 (6.8–12.2) | 10.6 (7.9–13.3) | 7.5 (5.3–9.8) | 9.2 (6.6–11.7) |
| Education, health, and social services | 32.6 (28–37.2) | 32.3 (28.4–36.2) | 31.6 (27.8–35.4) | 32.1 (28.1–36.3) |
| Leisure and hospitality | 7.2 (5.2–9.3) | 9.1 (6.3–11.8) | 7.8 (5.6–10) | 8 (5.7–10.3) |
| Other services | 6.8 (4.3–9.3) | 4.6 (2.7–6.6) | 5.6 (3.2–7.9) | 5.7 (3.4–7.9) |
| Public administration | 5.9 (3.8–8.1) | 7 (4.6–9.4) | 7.7 (5–10.3) | 6.9 (4.5–9.3) |
| Military | 0.1 (0–0.2) | - | 0.3 (0–0.8) | 0.2 (0–0.5) |
| Unclassifiable industry | 0.3 (0–0.7) | 1.1 (0–2) | 0.4 (0–0.9) | 0.6 (0–1.2) |
Note: “-” Implies that there was no data available for that category.
Abbreviation: CI, confidence interval.
The annualized per-worker and total estimated medical costs and estimated incremental medical costs with treated asthma are presented in Table 2. The 95% confidence intervals are also added for per-worker medical costs and incremental medical costs. During 2018–2020, the annualized per-worker incremental medical costs of asthma was $457. By sex, males ($650) had higher incremental medical costs than females ($225). By age group, workers aged 35–44 years had the highest incremental medical costs ($534). By region, workers in the West had the highest incremental medical costs ($768). By race/ethnicity, Hispanic workers had the highest incremental medical costs ($693). Workers who did not complete high school had higher incremental medical costs ($480), those with an annual household income of ≥$75,000 ($571), those who were covered by health insurance ($499), nonsmokers ($500), and those employed in the transportation and utilities industry sector ($898), followed by the manufacturing industry sector ($730) also had higher incremental medical costs associated with treated asthma. An estimated annual average of 8.2 million workers reported at least one medical event associated with asthma during the period of 2018–2020. The total annualized medical costs associated with treated asthma was $21 billion and the total annualized incremental medical costs was $3.8 billion. Total incremental medical costs varied across socioeconomic and demographic characteristics, and industries. It was highest among males ($2 billion), those in the age group of 35–44 years ($1.7 billion), residing in the west ($1.5 billion), white non-Hispanic ($1.8 billion), those who did not complete high school ($1.9 billion), those earning $75,000 or more annually ($2.5 billion), those covered by health insurance ($4 billion), smokers ($2.6 billion), and workers employed in education, health, and social services industry ($865 million).
TABLE 2.
Estimated annualized per-worker and total medical costs and incremental medical costs of treated asthma from the two-part model, 2018–2020, 2022 US dollar values.
| Healthcare utilization | Medical costs of workers without asthma (95% CIs) ($) | Medical costs of workers with asthma (95% CIs) ($) | Incremental medical costs of asthma (95% CIs) ($) | Total medical costs of asthma (mil. $)a | Total incremental medical costs (mil. $)b |
|---|---|---|---|---|---|
| Per-worker medical costs | 2140 (1985–2294) | 2597 (2301–2892) | 457 (209–705) | 21,349 | 3755 |
| Sex | |||||
| Female | 2067 (1847–2287) | 2291 (1956–2627) | 225 (7–443) | 11,818 | 1160 |
| Male | 2201 (2050–2351) | 2850 (2530–3171) | 650 (392–908) | 8711 | 1985 |
| Age categories | |||||
| 18–34 | 1595 (1347–1843) | 2102 (1631–2573) | 507 (209–806) | 1677 | 405 |
| 35–44 | 1981 (1781–2181) | 2515 (2144–2886) | 534 (269–799) | 7790 | 1654 |
| 45–64 | 2628 (2414–2842) | 3058 (2736–3380) | 430 (193–667) | 10,894 | 1531 |
| ≥65 | 1688 (1439–1938) | 1514 (1162–1867) | - | 1137 | - |
| Region | |||||
| Northeast | 1923 (1678–2167) | 2281 (1903–2659) | 359 (110–608) | 3882 | 610 |
| Midwest | 2552 (2312–2792) | 3045 (2658–3432) | 493 (236–750) | 5608 | 908 |
| South | 1669 (1490–1847) | 1939 (1598–2281) | 270 (12–529) | 5282 | 737 |
| West | 2621 (2289–2953) | 3389 (2869–3909) | 768 (485–1051) | 6575 | 1490 |
| Race/ethnicity | |||||
| Hispanic | 1858 (1528–2188) | 2551 (1961–3142) | 693 (366–1021) | 2601 | 707 |
| White, non-Hispanic | 2241 (2076–2406) | 2563 (2282–2843) | 322 (81–562) | 14,026 | 1761 |
| Black, non-Hispanic | 2023 (1740–2307) | 2608 (2101–3114) | 584 (283–886) | 2695 | 604 |
| Other, non-Hispanic | 2287 (1930–2643) | 2920 (2354–3485) | 633 (339–927) | 1985 | 430 |
| Education | |||||
| Did not complete high school | 1905 (1752–2059) | 2385 (2053–2717) | 480 (218–741) | 9602 | 1931 |
| High school and beyond | 2366 (2163–2569) | 2800 (2483–3118) | 435 (193–677) | 11,726 | 1820 |
| Annual household income | |||||
| Less than $35,000 | 1491 (1308–1674) | 1752 (1418–2086) | 261 (8–513) | 2928 | 436 |
| $35,000–74,999 | 1886 (1642–2130) | 2295 (1906–2685) | 409 (152–667) | 4887 | 872 |
| ≥$75,000 | 2579 (2389–2769) | 3150 (2798–3501) | 571 (311–831) | 13,889 | 2516 |
| Health insurance | |||||
| Covered by health insurance | 2337 (2165–2508) | 2836 (2530–3142) | 499 (253–746) | 22,712 | 3998 |
| No health insurance | 524 (415–633) | 631 (249–1013) | 108 (46–169) | 132 | 23 |
| Smoking status | |||||
| Smoker | 2502 (2299–2705) | 2909 (2593–3225) | 406 (164–648) | 18,599 | 2599 |
| Non-smoker | 1828 (1671–1984) | 2328 (1999–2657) | 500 (241–759) | 4236 | 910 |
| Industry | |||||
| Natural resources | 2067 (1312–2822) | 2670 (1453–3887) | 603 (93–1114) | 270 | 61 |
| Mining | 1182 (175–2189) | 1381 (103–2658) | 199 (40–358) | 39 | 6 |
| Construction | 1625 (1370–1881) | 2143 (1639–2648) | 518 (203–833) | 740 | 179 |
| Manufacturing | 2720 (2389–3050) | 3450 (2939–3961) | 730 (453–1008) | 1988 | 421 |
| Wholesale and retail Trade | 1831 (1576–2086) | 2209 (1725–2693) | 379 (77–680) | 2174 | 373 |
| Transportation and utilities | 2594 (2194–2993) | 3491 (2832–4150) | 898 (572–1224) | 1174 | 302 |
| Information | 1912 (1507–2316) | 2205 (1599–2812) | 294 (8–580) | 404 | 54 |
| Financial activities | 2354 (2033–2674) | 2793 (2318–3268) | 440 (175–704) | 1433 | 226 |
| Professional and business services | 2091 (1747–2435) | 2452 (1964–2940) | 361 (102–619) | 1859 | 273 |
| Education, health, and social services | 2213 (1884–2543) | 2541 (2049–3032) | 328 (59–596) | 6712 | 865 |
| Leisure and hospitality | 1571 (1322–1821) | 1895 (1422–2367) | 323 (26–621) | 1251 | 213 |
| Other services | 2788 (2189–3387) | 3462 (2581–4342) | 674 (317–1030) | 1614 | 314 |
| Public administration | 2620 (2200–3041) | 3070 (2524–3616) | 449 (198–701) | 1731 | 253 |
| Military | 296 (33–558) | 152 (51–251) | 250 (50–450) | 2 | 3 |
| Unclassifiable industry | 786 (7–1565) | 853 (124–1582) | 67 (803–937) | 41 | 3 |
Total medical costs are estimated as a product of the number of workers who had an event of treated asthma (from Table 1) in a particular group and the associated medical costs of asthma ($) of that group.
Total incremental medical costs are estimated as a product of the number of workers who had an event of treated asthma (from Table 1) in a particular group and the associated incremental medical costs of asthma ($) of that group.
Figure 1 represents the trends of estimated medical costs associated with treated asthma and those with no treated asthma and the incremental medical costs of asthma from 2018 to 2020. The annual per-worker estimated medical costs and estimated incremental medical costs increased from 2018 (incremental medical costs, $395) to 2020 (incremental medical costs, $567). The rate of increase was 12% from 2018 to 2019 and 28% from 2019 to 2020, with an overall increase of 43% from 2018 to 2020.
FIGURE 1.
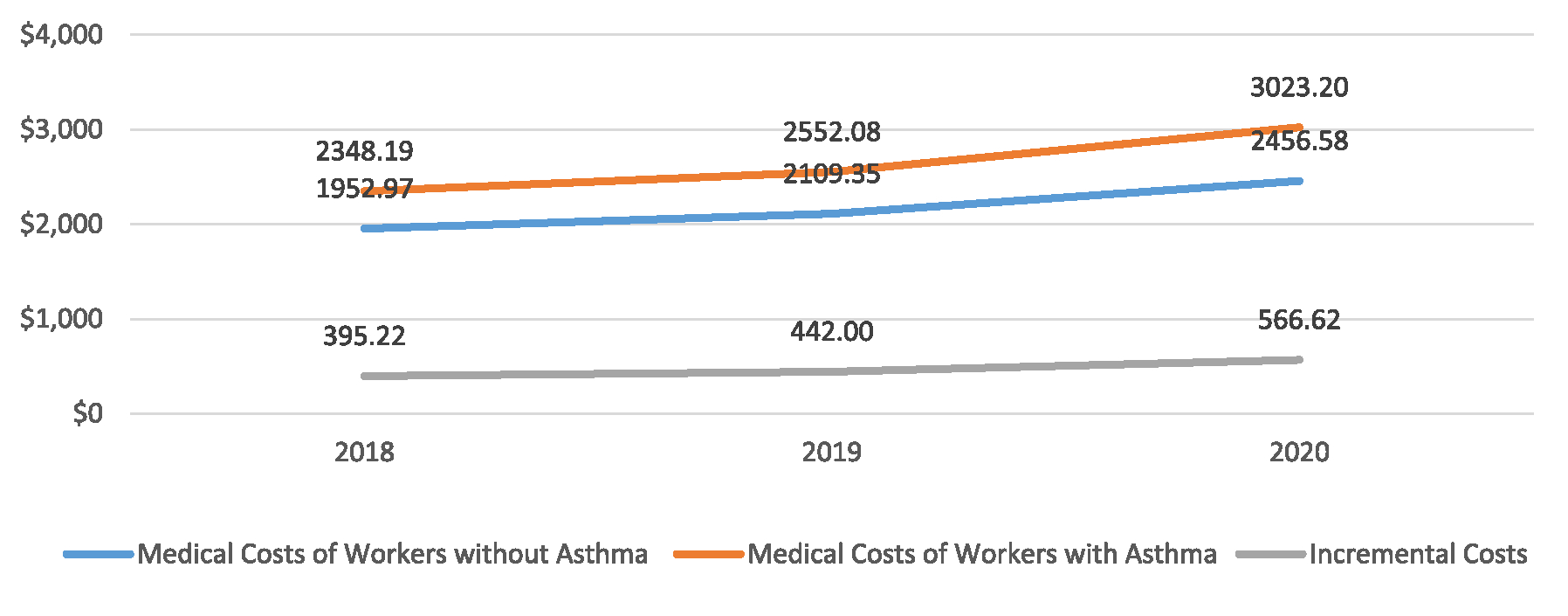
Trends of per-worker estimated medical costs and incremental medical costs of treated asthma, 2018–2020, 2022 US dollar values.
Table 3 shows the annual per-worker incremental medical costs of treated asthma with confidence intervals, by the different types of medical events for 2018–2020. These costs were similar for the different types of medical events across the years. Incremental medical costs of inpatient admissions were the highest for all the years (annualized incremental medical costs, $754) and incremental medical costs of ER visits were the lowest for all these years (annualized incremental medical costs, $20).
TABLE 3.
Estimated per-worker incremental medical costs of treated asthma by medical event by year, 2018–2020, 2022 US dollar values.
| Medical events | 2018 (95% CIs) ($) | 2019 (95% CIs) ($) | 2020 (95% CIs) ($) | Annualized (95% CIs) ($) |
|---|---|---|---|---|
| Overall | 395 (255–535) | 443 (291–594) | 567 (407–726) | 457 (316–598) |
| Prescription medications | 274 (103–446) | 227 (70–384) | 277 (80–473) | 249 (87–412) |
| Office based visits | 56 (12–100) | 59 (14–104) | 61 (9–112) | 58 (12–105) |
| Hospital-based outpatient visit | 113 (77–148) | 129 (99–159) | 115 (93–136) | 120 (104–136) |
| Inpatient admissions | 746 (165–1327) | 785 (135–1436) | 748 (168–1328) | 754 (123–1385) |
| Emergency room visits | 17 (5–29) | 16 (−4–36) | 23 (3–43) | 20 (10–30) |
| Home health | 142 (30–255) | 203 (43–364) | 80 (28–132) | 140 (96–184) |
Abbreviation: CI, confidence interval.
Table 4 presents the per-worker incremental medical costs of treated asthma with confidence intervals by the different sources of payments for the years 2018–2020 in 2022 US dollar values. Similar to the outputs in Table 3, the trends of these costs were similar across the years for the types of sources of payments, with private health insurance being the highest (annualized incremental medical costs, $750), followed by Medicaid (annualized incremental medical costs, $492), and out-of-pocket is the lowest (annualized incremental medical costs, $132). Incremental costs associated with Medicare only decreased significantly between the years, 2018 ($204) and 2020 ($132).
TABLE 4.
Per-worker incremental medical costs of treated asthma by sources of payments, 2018–2020, 2022 US dollar values.
| 2018 (95% CIs) ($) | 2019 (95% CIs) ($) | 2020 (95% CIs) ($) | Annualized (95% CIs) ($) | |
|---|---|---|---|---|
| Overall | 395 (255–535) | 443 (291–594) | 567 (407–726) | 457 (316–598) |
| Out-of-pocket | 135 (29–241) | 122 (2–243) | 140 (36–245) | 132 (22–242) |
| Medicare | 205 (42–367) | 199 (28–369) | 132 (22–242) | 205 (35–375) |
| Medicaid | 513 (290–735) | 458 (264–652) | 509 (283–736) | 492 (282–702) |
| Private health insurance | 749 (444–1054) | 741 (429–1053) | 762 (450–75) | 750 (441–1058) |
Abbreviation: CI, confidence interval.
4 |. DISCUSSION
This study estimated the burden of medical costs and incremental medical costs for treated asthma among workers. The disease burden estimated in monetary terms can help policy makers understand the impact of the disease and inform discussions on how to reduce the economic burden of asthma. During 2018–2020, an estimated 8.2 million US workers reported at least one medical event associated with asthma. The total annualized medical costs associated with treated asthma was $21 billion, and the total annualized incremental medical costs was $3.8 billion. The disease burden estimated in monetary terms can help policy makers understand the impact of the disease and inform discussions on how to reduce the economic burden of asthma.
Our results are consistent with previous studies on per-person medical costs and incremental medical costs associated with treated asthma among US adults.1,26,42,43 We found that among US workers the overall incremental medical costs of treated asthma were high ($457) but lower than that among all US adults ($1785 for the years 2003–2006 in 2006 US dollars44 to $3760 for the years 2008–2013 in 2015 US dollar values1) reported by previous studies. Lower medical costs among workers may be associated with factors that includes the healthy worker effect, as the working population is relatively healthy compared to non-workers, which include individuals with critical health conditions, higher comorbidities, or other disabilities that may prevent them from working.45,46 Our sample did not include adults out of work for more than 12 months before the survey, which may have resulted in lower incremental medical costs. Moreover, the majority of the working population is covered by health insurance (from their employer) while the unemployed population has lower coverage of health insurance, which helps the workers to utilize preventive healthcare measures, thus reducing the probabilities of certain health conditions that can trigger costly asthma-related events.47 Studies that included the entire population (both working and non-working), have a higher percentage of population not covered by health insurance and it is likely that a proportion of the non-working population is not healthy enough to work as explained by the healthy worker effect and, therefore, have higher health related medical costs compared to the working population.1,43,45
Previous studies have reported on the burden of asthma associated with work and found that the average medical costs were high ($901 in 2017 US dollars reported by Syamlal et al.30). However, the incremental medical costs of workers with asthma have not been estimated in earlier studies.30 Because incremental medical cost provides the additional medical cost that a health system incurs due to excess utilization of healthcare services to treat asthma, it provides a more comprehensive estimate of the cost of treating this medical condition.
We found that workers with no health insurance coverage had lower incremental medical costs for treated asthma compared to those who had health insurance, similar to previous studies.1 These individuals may have chosen not to seek care due to financial barriers. Previous research has indicated that adults with asthma caused or made worse by exposures in their workplace were more likely to be unable to see their primary care physician or an asthma specialist, or unable to buy medications because of the cost.47 Similar to earlier findings, our results also show that Black non-Hispanic and Hispanic workers had higher incremental medical costs compared to workers of other race/ethnicity groups.1,48 Workers who did not complete high school had higher incremental medical costs ($480) compared to those who had an education level of high school and beyond ($435), which is also supported by previous findings.1
Our results suggest that males ($650) had higher incremental medical costs compared to females ($225), and higher incremental medical costs were also observed among workers aged 35–44 years ($534) compared to the workers in all other age groups, and those in the higher income (≥$75,000) group ($571) compared to the workers in all the annual household income groups. These outcomes varied from previous findings from Nurmagambetov (2018) that estimated for the entire population,1 but similar to Syamlal et al.,30 that estimated average medical costs and total medical costs for the working population which could be partially due to the population studied here. We did not come across studies that compared the incremental medical costs of treated asthma across industries. We found that workers employed in the transportation and utilities industry sector ($898) followed by manufacturing ($730) had the highest incremental medical costs with treated asthma. Syamlal et al.30 reported the average medical costs associated with treated asthma among workers and found that workers in public administration had the highest average medical costs ($1279 in 2017 US dollars) followed by transportation and utilities ($1222 in 2017 US dollars).
Among the five medical events studied, inpatient admissions (annualized incremental medical costs, $754) for asthma were associated with the highest incremental medical costs followed by prescription medicine ($250). Previous findings on treated asthma by medical events, indicated that prescription medication costs were highest among all US adults.1,49 Working adults may have exposures in the workplace that cause new onset of asthma or worsening of pre-existing asthma.27 Adults with asthma caused or worsened by exposures in their workplace have been shown to have more severe symptoms than those without,50 which may explain the higher incremental medical costs among inpatient admissions in the current study.
5 |. LIMITATIONS
The data used in this study were self-reported and may be subject to misclassification. Asthma could not be classified as work-related, because a discrete diagnosis code for work-related asthma does not currently exist in ICD-10-CM and information on workplace exposure is not collected in the MEPS survey. In addition, workers might have changed their place of work (industry) and when they reported asthma- related medical events; therefore, medical expenditures by industry group might represent the industry where they were employed when the expenditures incurred. Finally, overall burden for treated asthma could not be assessed, due to lack of data on non-medical costs, productivity losses, losses due to presenteeism, costs of pain and suffering, transportation costs, or medical appointment wait time.
6 |. CONCLUSION
This is the first study to our knowledge focusing on the overall incremental medical costs of treated asthma among workers by socioeconomic and demographic characteristics, industry, medical events, and sources of payments. Our results showed that medical costs associated with treated asthma among workers are higher than those associated with workers without treated asthma. Incremental medical costs of asthma varied by socioeconomic and demographic characteristics, industry, and medical event. Workers in the utility and transportation industries had the highest incremental medical cost. Our results suggest that the per person incremental medical costs of treated asthma among workers are lower than that of all US adults (including working and non-working adults) as reported by previous studies.1,44 Our findings of higher incremental medical costs for treated asthma among workers highlight the economic benefit of prevention and early intervention to reduce morbidity of asthma in working adults.51 Programs to manage and control asthma and treatments to prevent and reduce asthma symptoms may have a positive effect on controlling medical costs related to treated asthma and improving worker health and wellbeing.
Abbreviations:
- ER
emergency room visits
- ICD-10-CM
International Classification of Diseases, Tenth Revision, Clinical Modification
- MEPS
Medical Expenditure Panel Survey
- US
United States
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
ETHICS STATEMENT
No human subjects were involved in this study, all data used here are publicly available and secondary data collected by Agency for Healthcare Research and Quality. Therefore institutional review approval was not required to conduct this study.
An alphabetical list of ideas or topics central to the study: age, asthma, demographic variables, education, healthcare utilization, income, incremental medical costs, industries, medical costs, medical events, race/ethnicity, region, sex, sources of payments for medical treatments, total incremental medical costs, total medical costs, treated asthma, workers associated with asthma.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in Medical Expenditure Panel Survey at https://meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp. These data were derived from the following resources available in the public domain—2020 data, https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=2020&cboDataTypeY=101%2CConsolidated+Data&cboDataTypeY=103%2CMedical+Conditions&cboDataTypeY=110%2CEmployment+Variables&cboDataTypeY=104%2CJobs+File&cboDataTypeY=204%2CHo—2019 data, https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=2019&cboDataTypeY=101%2CConsolidated+Data&cboDataTypeY=103%2CMedical+Conditions&cboDataTypeY=110%2CEmployment+Variables&cboDataTypeY=104%2CJobs+File&cboDataTypeY=204%2CHo—2018 data, https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=2018&cboDataTypeY=101%2CConsolidated+Data&cboDataTypeY=103%2CMedical+Conditions&cboDataTypeY=110%2CEmployment+Variables&cboDataTypeY=104%2CJobs+File&cboDataTypeY=204%2CHo.
REFERENCES
- 1.Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008–2013. Ann Am Thorac Soc. 2018;15:348–356. [DOI] [PubMed] [Google Scholar]
- 2.Blanc PD, Annesi-Maesano I, Balmes JR, et al. The occupational burden of nonmalignant respiratory diseases. An official American Thoracic Society and European Respiratory Society Statement. Am J Respir Crit Care Med. 2019;199:1312–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pate CA, Zahran HS, Qin X, Johnson C, Hummelman E, Malilay J. Asthma surveillance - United States, 2006–2018. MMWR. Surveillance Summaries. 2021;70(5):1–32. doi: 10.15585/mmwr.ss7005a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Current Asthma Population Estimates — in thousands by Age, United States: National Health Interview Survey, 2019. Accessed December 10, 2023. (https://www.cdc.gov/asthma/nhis/2019/table3-1.htm).
- 5.Asthma Attack Population Estimates among those with Current Asthma — in thousands by Age, United States: National Health Interview Survey, 2019. (2019. National Health Interview Survey (NHIS) Data | CDC; ), Accessed December 10, 2023. [Google Scholar]
- 6.Lee LK, Ramakrishnan K, Safioti G, Ariely R, Schatz M. Asthma control is associated with economic outcomes, work productivity and health-related quality of life in patients with asthma. BMJ Open Respir Res. 2020;7(1):e000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Global Asthma Report, 2014.
- 8.Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med. 1992;326(13):862–866. [DOI] [PubMed] [Google Scholar]
- 9.Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985–1994. J Allergy Clin Immunol. 2000;106(3):493–499. [DOI] [PubMed] [Google Scholar]
- 10.Lozano P, Sullivan SD, Smith DH, Weiss KB. The economic burden of asthma in US children: estimates from the National Medical Expenditure Survey. J Allergy Clin Immunol. 1999;104:957–963. [DOI] [PubMed] [Google Scholar]
- 11.Lee YR, Cho B, Jo MW, et al. Measuring the economic burden of disease and injury in Korea, 2015. J Korean Med Sci. 2019;34(suppl 1):e80. doi: 10.3346/jkms.2019.34.e80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lefrant JY, Garrigues B, Pribil C, et al. The daily cost of ICU patients: a micro-costing study in 23 French intensive care units. Anaesth Crit Care Pain Med. 2015;34(3):151–157. [DOI] [PubMed] [Google Scholar]
- 13.Brennan A, Jackson A, Horgan M, Bergin CJ, Browne JP. Resource utilisation and cost of ambulatory HIV care in a regional HIV centre in Ireland: a micro–costing study. BMC Health Serv Res. 2015;15:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hendriks ME, Bolarinwa OA, Nelissen HE, et al. Costs of cardiovascular disease prevention care and scenarios for cost saving: a micro–costing study from rural Nigeria. J Hypertens. 2015;33:376–684. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien C, Fogarty E, Walsh C, et al. The cost of the inpatient management of febrile neutropenia in cancer patients--a micro-costing study in the Irish healthcare setting. Eur J Cancer Care. 2015;24:125–132. [DOI] [PubMed] [Google Scholar]
- 16.Parkinson F, Kent SJW, Aldous C, Oosthuizen G, Clarke D. The hospital cost of road traffic accidents at a South African regional trauma centre: a micro-costing study. Injury. 2014;45:342–345. [DOI] [PubMed] [Google Scholar]
- 17.McLaughlin AM, Hardt J, Canavan JB, Donnelly MB. Determining the economic cost of ICU treatment: a prospective “micro-costing” study. Intensive Care Med. 2009;35:2135–2140. [DOI] [PubMed] [Google Scholar]
- 18.Kamble S, Bharmal M. Incremental direct expenditure of treating asthma in the United States. J Asthma. 2009;46(1):73–80. doi: 10.1080/02770900802503107 [DOI] [PubMed] [Google Scholar]
- 19.Yelin E, Trupin L, Cisternas M, Eisner M, Katz P, Blanc P. A national study of medical care expenditures for respiratory conditions. Eur Respir J. 2002;19:414–421. [DOI] [PubMed] [Google Scholar]
- 20.Ward MM, Javitz HS, Smith WM, Bakst A. A comparison of three approaches for attributing hospitalizations to specific diseases in cost analyses. Int J Technol Assess Health Care. 2000;16:125–136. [DOI] [PubMed] [Google Scholar]
- 21.Martin BC, Ricci JF, Kotzan JA, Lang K, Menzin J. The net cost of Alzheimer disease and related dementia: a population-based study of Georgia Medicaid recipients. Alzheimer Dis Assoc Disord. 2000;14:151–159. [DOI] [PubMed] [Google Scholar]
- 22.Gabriel SE, Gabriel SE, Tosteson ANA, et al. Direct medical costs attributable to osteoporotic fractures. Osteoporos Int. 2002;13:323–330. [DOI] [PubMed] [Google Scholar]
- 23.Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis. Pharmacoeconomics. 2004;22:95–105. [DOI] [PubMed] [Google Scholar]
- 24.Lee DW, Meyer JW, Clouse J. Implications of controlling for comorbid conditions in cost-of-illness estimates: a case study of osteoarthritis from a managed care system perspective. Value Health. 2001;4:329–334. [DOI] [PubMed] [Google Scholar]
- 25.Martin BC, Ganguly R, Pannicker S, Frech F, Barghout V. Utilization patterns and net direct medical cost to Medicaid of irritable bowel syndrome. Curr Med Res Opin. 2003;19:771–780. [DOI] [PubMed] [Google Scholar]
- 26.Sullivan PW, Ghushchyan VH, Slejko JF, Belozeroff V, Globe DR, Lin SL. The burden of adult asthma in the United States: evidence from the medical expenditure panel survey. J Allergy Clin Immunol. 2011;127:363–369.e3. [DOI] [PubMed] [Google Scholar]
- 27.Tarlo SM, Balmes J, Balkissoon R, et al. Diagnosis and management of work-related asthma. Chest. 2008;134(suppl):1S–41S. doi: 10.1378/chest.08-0201 [DOI] [PubMed] [Google Scholar]
- 28.Henneberger PK, Redlich CA, Callahan DB, et al. An Official American Thoracic Society Statement: work-exacerbated asthma. Am J Respir Crit Care Med. 2011;184(3):368–378. [DOI] [PubMed] [Google Scholar]
- 29.Knoeller GE, Mazurek JM, Moorman JE. Characteristics associated with health care professional diagnosis of work-related asthma among individuals who describe their asthma as being caused or made worse by workplace exposures. J Occup Environ Med. 2012;54:485–490. [DOI] [PubMed] [Google Scholar]
- 30.Syamlal G, Bhattacharya A, Dodd KE. Medical expenditures attributed to asthma and chronic obstructive pulmonary disease among workers — United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2020;69:809–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gold M Panel on cost-effectiveness in health and medicine. Med Care. 1996;34:197–199. [PubMed] [Google Scholar]
- 32.Weinstein MC. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1253–1258. [PubMed] [Google Scholar]
- 33.Russell LB. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996;276:1172–1177. [PubMed] [Google Scholar]
- 34.Haddix AC, Teutsch SM, Corso PS. Prevention Effectiveness: a guide to decision analysis and economic evaluation. Second ed. Oxford University Press; 2003:2003. [Google Scholar]
- 35.Gold MR, Siegel JE, Russel LB, Weinstein MC. Cost-effectiveness in Health and Medicine. Oxford University Press; 1996. [Google Scholar]
- 36.Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support healthcare cost research and inform policy and practice. Med Care. 2009;47 (7 suppl 1):S44–S50. [DOI] [PubMed] [Google Scholar]
- 37.D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol. 1996;49:1429–1433. [DOI] [PubMed] [Google Scholar]
- 38.MEPS Industry Codes Condensing Rules Beginning with FY2010, Accessed January 19th, 2024. https://meps.ahrq.gov/data_stats/download_data/pufs/ind_occ/ind3.pdf
- 39.MEPS-HC Response Rates by Panel, Accessed May 19th, 2024. https://meps.ahrq.gov/survey_comp/hc_response_rate.jsp
- 40.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. [DOI] [PubMed] [Google Scholar]
- 41.US Bureau of labor statistics, Measuring price change in the CPI: Medical care, Accessed November 21st, 2023. https://www.bls.gov/cpi/factsheets/medical-care.htm
- 42.Barnett SBL, Nurmagambetov TA. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol. 2011;127(1):145–152. [DOI] [PubMed] [Google Scholar]
- 43.Song HJ, Blake KV, Wilson DL, et al. Medical costs and productivity loss due to mild, moderate, and severe asthma in the United States. J Asthma Allergy. 2020;13:545–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shenolikar R, Song X, Anderson JA, Chu BC, Cantrell CR. Costs of asthma among U.S. working adults. Am J Manag Care. 2011;17:409–416. [PubMed] [Google Scholar]
- 45.Pearce N, Checkoway H, Kriebel D. Bias in occupational epidemiology studies. Occup Environ Med. 2007;64(8):562–568. doi: 10.1136/oem.2006.026690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le Moual N, Kauffmann F, Eisen EA, Kennedy SM. The healthy worker effect in asthma: work may cause asthma, but asthma may also influence work. Am J Respir Crit Care Med. 2008;177(1):4–10. doi: 10.1164/rccm.200703-415PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Driscoll AK, Bernstein AB. Health and access to care among employed and unemployed adults: United States, 2009–2010. NCHS Data Brief. 2012;83:1–8. [PubMed] [Google Scholar]
- 48.Pearlman DN, Zierler S, Meersman S, Kim HK, Viner-Brown SI, Caron C. Race disparities in childhood asthma: does where you live matter? J Natl Med Assoc. 2006;98:239–247. [PMC free article] [PubMed] [Google Scholar]
- 49.Jang J, Gary Chan KC, Huang H, Sullivan SD. Trends in cost and outcomes among adult and pediatric patients with asthma: 2000–2009. Ann Allergy Asthma Immunol. 2013;111(Issue 6):516–522. doi: 10.1016/j.anai.2013.09.007 [DOI] [PubMed] [Google Scholar]
- 50.Knoeller GE, Mazurek JM, Moorman JE. Asthma symptoms among adults with work-related asthma. J Asthma. 2013;50(2):166–173. doi: 10.3109/02770903.2012.754029 [DOI] [PubMed] [Google Scholar]
- 51.Lau A, Tarlo SM. Update on the management of occupational asthma and work-exacerbated asthma. Allergy, Asthma Immunol Res. 2019;11(2):188–200. doi: 10.4168/aair.2019.11.2.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available in Medical Expenditure Panel Survey at https://meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp. These data were derived from the following resources available in the public domain—2020 data, https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=2020&cboDataTypeY=101%2CConsolidated+Data&cboDataTypeY=103%2CMedical+Conditions&cboDataTypeY=110%2CEmployment+Variables&cboDataTypeY=104%2CJobs+File&cboDataTypeY=204%2CHo—2019 data, https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=2019&cboDataTypeY=101%2CConsolidated+Data&cboDataTypeY=103%2CMedical+Conditions&cboDataTypeY=110%2CEmployment+Variables&cboDataTypeY=104%2CJobs+File&cboDataTypeY=204%2CHo—2018 data, https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=2018&cboDataTypeY=101%2CConsolidated+Data&cboDataTypeY=103%2CMedical+Conditions&cboDataTypeY=110%2CEmployment+Variables&cboDataTypeY=104%2CJobs+File&cboDataTypeY=204%2CHo.


