Abstract
Background
Emotional eating (EE) is particularly prevalent in overweight or obese women, who may turn to food as a way to cope with stress, sadness, or anxiety. Limited research has been conducted on the association between EE and nutritional intake. Therefore, present study was designed to explore this association in adult women with overweight and obesity.
Methods
In this cross-sectional study, the relationship between EE and nutritional intake in 303 overweight and obese women (aged 18–50 years) was examined. The researchers used the validated semi-quantitative Food Frequency Questionnaire (FFQ) to assess participants’ nutritional intake and the Dutch Eating Behavior Questionnaire (DEBQ) to evaluate their eating behavior. To determine the association between EE and nutritional intake, we employed the multiple linear regression analysis.
Results
The frequency of high intensity EE was 64.4% among the study participants and the mean total score of EE subscale of DBEQ was 2.32 ± 0.81. The total score of EE was positively associated with the energy intake (β = 0.396, P = 0.007), even after adjusting for age and BMI. In addition, a significant inverse association was found between the score of EE and the daily intake of calcium (β= -0.219, P = 0.026), riboflavin (β= -0.166, P = 0.043), and vitamin B12 (β= -0.271, P = 0.035), independent from energy and age. Also the results showed a significant positive association between the score of EE and the frequency of daily intake of cracker, muffin, cake, cream cake, pastry, candy, ice cream, pickles, melon, hydrogenated vegetable oil, peanut, salted and roasted seeds, and corn-cheese puff snack.
Conclusion
This study found that overweight or obese women with higher intensity of EE might have a higher intake of energy and a lower intake of dietary calcium, riboflavin and vitamin B12. Integrating a balanced diet with psychotherapy is suggested to help individuals with EE reducing the urge to eat in response to emotions.
Keywords: Emotional eating, Nutritional intake, Overweight, Obesity
Introduction
The prevalence of obesity has increased dramatically over the last decades, making it a major public health concern worldwide [1, 2]. This increase in the prevalence of obesity is more concerning among women [3]. According to the latest report by the World Health Organization (WHO), approximately 15% of women around the world are suffering from obesity [4]. Obesity often coexists with eating disorders [5]. Eating disorders have different types, such as anorexia nervosa, bulimia nervosa, binge eating and stress-induced restrained appetite [5]. Of note, other eating behaviors might be co-occurred with overweight and obesity such as emotional eating (EE) [6]. EE is defined as overeating after experiencing negative emotions and feelings [7], which is the tendency to eat unhealthy foods to cope with negative emotions such as depression [8] and anxiety [9]. Also, EE occurs due to the inability to express emotions and lack of emotion regulation [10]. Other factors include genetics [11] and stress [12]. Stress and negative emotions can make a person lose control and cause an increase in appetite, leading to overeating [13]. Appetite regulation is done through two mechanisms. First, in the hedonic phase, by stimulating the reward system, the production of dopamine and serotonin after eating delicious foods is increased. Second, through homeostatic regulation, which is regulated by biological needs and via regulating hormones , such as leptin, it affects appetite and the eating process [14]. Overeating with negative emotions is associated with an increase in the number of dopamine D2 receptors in lean and obese individuals [15]. Response to pleasure stimulates opioid receptors and dopamine is released by stimulating opioid receptors [16].
It is noteworthy that the prevalence of EE in women is reported to be higher than in men [17]and that the response of men to stress is more in the form of decreased appetite [18, 19]. EE has been suggested to be one of the major barriers to weight-loss diet adherence [20]. Consequently, the increased desire for high-calorie foods such as fatty foods and sweet carbohydrates [21] leads to excessive energy consumption and weight gain during the negative emotional conditions [22]. This increase in weight can raise the risk of obesity, diabetes [23], elevated levels of low-density lipoprotein-cholesterol (LDL-C) and total serum cholesterol [24], hypertension [25], the occurrence and persistence of metabolic syndrome [26], and failure of the diet [27]. Additionally, it can lead to decreased self-esteem [28].The treatment methods that have been considered for this disorder include psychotherapy [29], nutrition therapy, and exercise [30]. EE with increasing intake of high-calorie foods causes poor quality of the diet received [21]. The quality of the diet depends on the intake of fiber, protein, fruits, and vegetables [31]. Generally, it depends on enhancing the intake of micronutrients and protein [32]. Dietary quality is considered a modifiable risk factor for mental disorders via many biological mechanisms, such as inflammation, oxidative stress, and the intestinal microbiome. Additionally, previous studies have confirmed that fatty acids and micronutrients such as vitamin D, vitamin C, and zinc play a positive role in improving mental disorders and diseases [33–38].
Nutrients are known to play a role in the development of EE. On the other hand, the dietary pattern of individuals with this disorder includes high-calorie intake and poor intake of nutrients. This leads to a vicious cycle between nutrient deficiencies and the occurrence and persistence of EE. Hence, this study was carried out to investigate the associations between EE and nutritional intake in women with overweight and obesity.
Methods
Study design
The present study is a cross-sectional observation performed using the Dutch Eating Behavior Questionnaire (DEBQ) and the validated semi-quantitative Food Frequency Questionnaire (FFQ) [39] to explore the relationship between emotional eating and nutritional intake in adult women with overweight and obesity. This study was conducted between February 10, 2020, and April 21, 2022.
Participants
The study population included women who had been referred to the comprehensive health service centers of Kashan City affiliated with Kashan University of Medical Sciences, which had the following criteria: (1) Iranian women aged 18–50 years, (2) Women with a body mass index (BMI) above 25 kg/m2.
The exclusion criteria for this study were as follows: (1) Individuals with chronic diseases such as diabetes and hypothyroidism, (2) Individuals with certain and diagnosed syndromic, monogenic, and polygenic causes of obesity [40], (3) Individuals with any type of cancer, (4) Individuals with major mental disorders such as bulimia, bipolar disorder, schizophrenia, and major depressive disorder, (5) Pregnant women, (6) Breastfeeding mothers, (7) Women in menopause, (8) Professional athletes, (9) Individuals who used alcohol, (10) Individuals who smoked cigarettes, 11) Individuals who used antidepressants and sedatives, and 12) Individuals who used herbal supplements to reduce or increase appetite/body metabolism.
Since no previous study had examined the prevalence of emotional eating in Iran, 30 women completed the DEBQ as a pilot study. Based on the results obtained, 30% of the women reported EE. Consequently, the sample size was calculated according to the following formula: n = Z2pq/d2= (1.96)2 × 0.3 × 0.7/ (0.06)2=225. Therefore, it was determined that 225 samples were necessary for this study. Taking into account the possibility of 20% dropouts and non-responses, the number of samples increased to 270 women.
Procedures
This study was performed in line with the principles of the Declaration of Helsinki, and all the participants signed the written informed consent form. Approval was granted by the Ethics Committee of Kashan University of Medical Sciences, Kashan, Iran (IR.KAUMS.MEDNT.REC.1399.209). Due to the pandemic conditions of COVID-19, it was impossible to complete the questionnaire face-to-face. For this reason, the questionnaires were made available to the participants online (the address of the website: www.porsall.com). The exception was in the case of illiterate people who were a limited number in the present study. All the questionnaires in the present study were completed in the form of face-to-face online interviews with these participants. A trained person was responsible for conducting interviews with illiterate participants. This study had three questionnaires: The general questionnaire, the DEBQ, and the validated semi-quantitative FFQ. Their details have been explained as follows.
Questionnaires
The initial questionnaire used in this study was a general one that aimed to gather demographic information such as age, marital status, level of education, and employment status. It also included questions on current medications, physical activity levels, and anthropometric variables such as weight, height, and BMI. This questionnaire was designed specifically for the present study.
The second questionnaire used in this study was the DEBQ. The diagnosis of emotional eating in the present study was based on DEBQ, which consists of 33 items divided into three scales: restrained eating (10 items), emotional eating (13 items), and external eating (10 items) [41]. This questionnaire utilized a five-point Likert scale ranging from ‘never’ (1) to ‘most of the time’ (5). Summing the scores of the items in each subscale and dividing it by the number of items gives the total score of each subscale. Higher scores indicate a higher rate of eating behavior related to that subscale. In present study, we used the obtained total score of “emotional eating” subscale as a surrogate of EE status in our participants. In addition, to find the frequency of EE among the study sample we applied the cut-off-points for total score of “emotional eating” subscale that was used by van Strien et al. [42]. According to this cut-off-point, participants whose total score for emotional eating subscale was equal to and above 2.6 had high intensity of EE, and subjects whose mean total score in this subscale was less than 1.8 do not have this disorder. The DEBQ has the validity of retesting, internal consistency (Cronbach’s alpha coefficients between 0.8 and 0.95), and appropriate factor validity. The validity of this questionnaire in Iran has been reported as favorable, and its validity has been announced using the Kuder-Richardson method, which was equal to 0.74 [41]. The Cronbach’s alpha was 0.91 for restrained eating and 0.95 for emotional eating across the three subscales.
The validated semi-quantitative FFQ was the third questionnaire used in this study to inquire about the intake of 168 food items during the last year. The validity and reliability of this FFQ have been confirmed by Mirmiran et al. [39]. The questionnaire also provides a standard portion size for each food item, which is more commonly understood by the general population.
The daily intake of each food item was calculated by multiplying the portion of each food item consumed into grams. Next, it was analyzed using Nutritionist IV software to calculate the average daily food intake, including energy intake, macronutrients, and micronutrients for each individual. In addition, the frequency of daily consumption of each food item in the FFQ was calculated in order to evaluate the relationship between EE and the consumption of each food item.
Statistical analysis
Descriptive statistics such as mean, standard deviation, frequency, etc., were used to show the basic characteristics of participants. Data distribution was examined for normality by the Kolmogorov–Smirnov test. Multiple linear regression analysis was used to determine the association between the score of EE and daily intake of dietary nutrients, while adjusting for confounding variables such as energy intake, age and BMI. In addition, participants in whom their nutrient intake was estimated to be outlier were excluded from the analysis. Also, the relationship between the score of EE and the daily frequency intake of each food items in FFQ was evaluated by the multiple linear regression. The score of EE, age, BMI, and the energy intake were selected as independent variables while the value of daily dietary nutrients as well as the frequency intake of each food item were entered in the model as dependent variables. Regression coefficients are given as standardized β values, referring to the number of standard deviations (SDs) the dependent variable changes, per SD increase of independent variables. Data was analyzed using SPSS statistical software, version 16 (SPSS Inc, Chicago, Ill). Two-sided P values < 0.05 were considered statistically significant.
Results
General characteristics of the participants
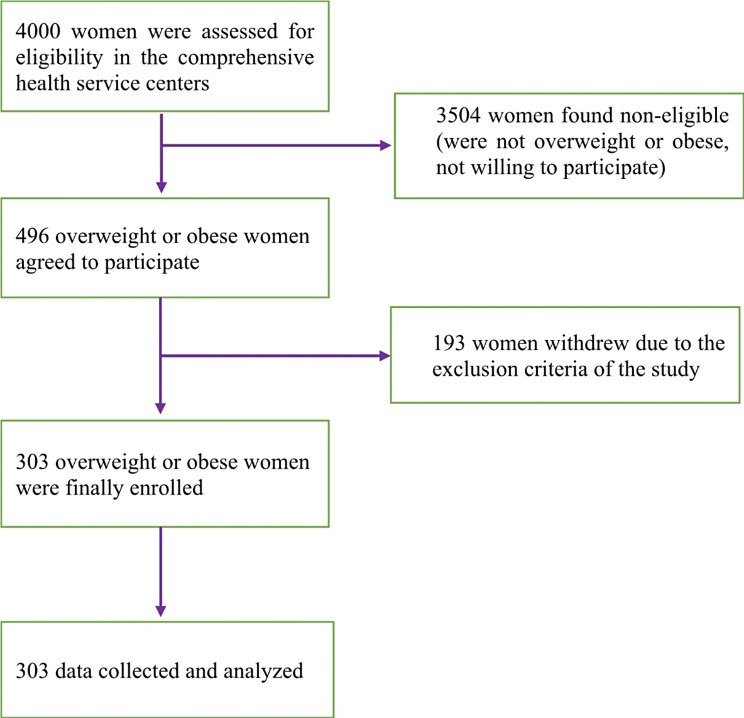
In this study, 4000 women were contacted, of which 496 overweight or obese women agreed to participate. Of the 496 women, 193 were excluded from the study due to exclusion criteria, and 303 were examined. The flow diagram for participant selection is illustrated in Fig. 1.
Fig. 1.
Flow diagram for the selection of participants
The age range of the participants was 18–50 years, and their mean age was 35.56 years with a standard deviation of 8.44. The participants had an average weight of 80.36 ± 12.5 kg, an average height of 160.49 ± 15.5 cm, and an average BMI of 30.66 ± 4.5 kg/m2.
The demographic characteristics of the participants of this study are summarized in Table 1. Most of the participants were married (92.4%). In total, 66% of participants were housewives. Regarding education level, 50% had undergraduate and postgraduate education, and 25.4% had university education.
Table 1.
General characteristics of the participants
| Variable | Classification | Number | Percent |
|---|---|---|---|
| Marital status | Married | 280 | 92.4% |
| Single | 23 | 7.6% | |
| Employment status | Unemployed | 46 | 15.2% |
| University student | 16 | 5.3% | |
| Housewife | 202 | 66.7% | |
| Freelance job | 22 | 7.3% | |
| Worker or farmer | 2 | 0.7% | |
| Private sector employee | 3 | 1.0% | |
| government employee | 11 | 3.6% | |
| Senior employee or University staff | 1 | 0.3% | |
| Education status | Illiterate | 17 | 5.6% |
| Literacy for reading and writing | 8 | 2.6% | |
| Primary | 49 | 16.2% | |
| Guidance school | 45 | 14.9% | |
| Diploma degree | 107 | 35.3% | |
| Associate degree | 20 | 6.6% | |
| Bachelor degree and higher | 57 | 18.8% | |
|
Taking any medications (except for the drugs mentioned in the exclusion criteria) |
No | 213 | 70.3% |
| Yes | 90 | 29.7% | |
| Physical activity | No physical activity | 213 | 70.3% |
| 1 to 2 times a week | 48 | 15.8% | |
| 3 to 4 times a week | 27 | 8.9% | |
| 5 to 6 times a week | 11 | 3.6% | |
| More than 6 times a week | 4 | 1.3% | |
| Duration of physical activity each time ( n = 88) | Less than 30 min | 29 | 32.9% |
| 30 min | 21 | 23.9% | |
| 30 to 60 min | 31 | 35.2% | |
| More than 60 min | 7 | 8.0% |
The frequency of high intensity EE was 64.4% among the study participants (the mean score of EE ≥ 2.6). In addition, the mean score of EE subscale of DBEQ was 2.32 ± 0.81.
The relationship between EE and nutrient intake
Table 2 presents the results of the multiple linear regression analysis. In this analysis, the independent association between the score of EE and the daily intake of energy was assessed, while adjusting for confounding variables such as age and BMI. Based on the obtained results, there was a significant positive association between EE and the daily intake of energy. Also, the relationship between the score of EE and the daily intake of macro- and micro- nutrients was evaluated while adjusting for the energy intake and age. The results showed a significant inverse association between the score of EE and the daily intake of calcium, riboflavin (vitamin B2) and vitamin B12 (cobalamin)(Table 2).
Table 2.
The results of the multiple linear regression analysis investigating the association between emotional eating and the daily intake of nutrients*
| Nutrients | β | t | P-value |
|---|---|---|---|
| Energy | 0.396 | 2.809 | 0.007 a |
| Protein | -0.076 | -0.753 | 0.458 b |
| Carbohydrate | -0.029 | -0.514 | 0.610 b |
| Fat | 0.067 | 1.111 | 0.273 b |
| Cholesterol | -0.118 | -0.877 | 0.385 b |
| Saturated fatty acids | -0.085 | -1.100 | 0.277 b |
| Monounsaturated fatty acids | 0.076 | 1.041 | 0.317 b |
| Polyunsaturated fatty acids | 0.203 | 1.909 | 0.063 b |
| Sodium | 0.007 | 0.052 | 0.959 b |
| Potassium | -0.114 | -1.303 | 0.200 b |
| Iron | 0.082 | 0.492 | 0.625 b |
| Calcium | -0.219 | -2.305 | 0.026 b |
| Magnesium | -0.063 | -0.940 | 0.353 b |
| Phosphorus | -0.111 | -1.518 | 0.137 b |
| Zinc | -0.067 | -0.478 | 0.635 b |
| Copper | 0.123 | 1.735 | 0.090 b |
| Manganese | 0.199 | 1.956 | 0.057 b |
| Selenium | -0.112 | -0.786 | 0.436 b |
| Chromium | 0.081 | 1.092 | 0.277 b |
| Vitamin A | -0.143 | -0.930 | 0.358 b |
| Vitamin E | -0.006 | -0.050 | 0.960 b |
| Vitamin B1 | 0.034 | 0.397 | 0.693 b |
| Vitamin B2 (Riboflavin) | -0.166 | -2.091 | 0.043 b |
| Vitamin B3 | 0.024 | 0.314 | 0.755 b |
| Vitamin B6 | 0.031 | 0.336 | 0.738 b |
| Folic acid | -0.055 | -0.533 | 0.597 b |
| Vitamin B12 | -0.271 | -2.185 | 0.035 b |
| Pantothenic acid | -0.084 | -1.091 | 0.282 b |
| Biotin | -0.158 | -1.350 | 0.184 b |
| Vitamin C | -0.167 | -1.050 | 0.300 b |
| Vitamin D | -0.142 | -0.887 | 0.380 b |
| Vitamin K | -0.131 | -0.851 | 0.399 b |
| Fiber | -0.003 | -0.027 | 0.979 b |
| Sugar | -0.122 | -1.254 | 0.217 b |
* Variables such as the score of emotional eating, energy, age and body mass index (BMI)were selected as independent variables while each of the nutrient was entered in the model as a dependent variable
a Adjusted for age and BMI
b Adjusted for the energy intake and age
The relationship between EE and the frequency of Daily Consumption of Food items
The association between the score of EE and the frequency of daily consumption of food items was assessed by the multiple linear regression analysis while adjusting for the age of the participants as a confounding variable. Because the number of food items in the used FFQ was large (168 items), in order to clarify and better understand the relationship, only the results that were statistically significant are presented in Table 3. The analysis revealed a significant positive association between the score of EE and the frequency of daily intake of cracker, muffin, cake, cream cake, pastry, candy, ice cream, pickles, melon, hydrogenated vegetable oil, peanut, salted and roasted seeds and corn-cheese puff snack.
Table 3.
The results of the multiple linear regression analysis investigating the association between emotional eating and the frequency of daily consumption of food items*
| Food items | β | t | P-value |
|---|---|---|---|
| Cracker | 0.324 | 2.971 | 0.004 |
| Muffin | 0.295 | 2.683 | 0.009 |
| Cake | 0.245 | 2.151 | 0.035 |
| Cream cake | 0.233 | 2.113 | 0.038 |
| Pastry | 0.300 | 2.721 | 0.008 |
| Candy | 0.260 | 2.362 | 0.021 |
| Ice cream | 0.263 | 2.351 | 0.021 |
| Hamburger | 0.227 | 1.957 | 0.054 |
| Pickled cucumber | 0.383 | 3.593 | 0.001 |
| Melon | 0.364 | 3.273 | 0.002 |
| Grape | 0.219 | 1.899 | 0.062 |
| Hydrogenated vegetable oil | 0.297 | 2.590 | 0.012 |
| Peanut | 0.228 | 1.948 | 0.055 |
| Salted and roasted seeds of sunflower | 0.218 | 2.188 | 0.032 |
| Corn-cheese puff snack | 0.274 | 2.541 | 0.013 |
* Variables such as the score of emotional eating, and age were selected as independent variables while the frequency of daily consumption of each food item was entered in the model as a dependent variable
Discussion
The findings of the present study showed a high rate of EE in the study participants, which was equal to 64.4%. This rate was near to the prevalence of EE that was reported among overweight or obese participants in previous studies [43, 44]. Madali et al. evaluated EE predisposition of Turkish individuals [44]. They found that 74.1% of obese participants were emotional eaters [44]. Similar to our study, they conducted their research during the COVID-19 pandemic [44]. However, unlike present study, their participants were both men and women, and the method used for assessing EE was Emotional Eating Scale [44]. They concluded that sudden lifestyle changes and the increase in stress levels during COVID-19 pandemic may affect emotional eating behavior [44].
According to the surveys conducted, there are very few studies about the role of emotional eating in nutritional intake and vice versa [21, 45, 46]. The present study is one of the first studies that examined the relationship between EE and nutritional intake in Iranian overweight and obese women. We found a positive association between EE and daily intake of energy, independent from age and BMI. This higher energy intake in individuals with EE is consistent with the results of the previous studies [47, 48]. Consuming high amounts of hyper-tasty energy-dense foods that contain high fat and sugar levels can be a reason for higher energy intake in emotional eaters [49]. The results of the study by Alejandra Betancourt-Núñez et al. showed that individuals with EE who had abdominal obesity followed a dietary pattern with many snacking and fast food [46]. However, in a study conducted by Madali et al. in Turkey during the COVID-19 pandemic, a rise in the intake of fresh fruits and vegetables, eggs, red meat and milk was reported by emotional eaters while they reported a decrease in the intake of junk foods such as chips, biscuits, chocolates, bread, syrupy desserts, and pastries [44]. To explain these unexpected findings, they stated that during the quarantine period of the COVID-19 pandemic, Turkish people had more access to vegetables and fruits, and since they had more time at home to cook, they decreased the intake of ready-to-eat foods. As a result, it seems that some factors and conditions such as availability of certain foods, changes in mood such as stress, depression and anxiety, as well as culture might affect the types of foods consumed by emotional eaters. In the present study the positive association was found between total score of EE and the consumption of energy-dense, high-sugary, high-fat and salty foods such as cracker, muffin, cake, cream cake, pastry, candy, ice cream, pickles, melon, peanut, salted and roasted seeds and corn-cheese puff snack. In fact, emotional eaters increase the consumption of high-sugary, high fat foods to cope with the negative emotions such as depression, stress and anxiety. Food is a powerful natural reward that triggers the release of dopamine and consequently activates pleasure and reward centers in the brain. A person repeatedly eats certain foods to experience this positive feeling of satisfaction. Thus, overeating and morbid obesity result from satisfying habits [50]. Some foods, especially those high in sugar and fat, are substantial rewards that reinforce eating (even without an energy requirement) and cause a learned association between stimulus and reward [51].
In current study, the increase in the intensity of EE was associated with the intake of more hydrogenated vegetable oil that is a source of saturated fatty acids and trans fatty acids (TFA). One of the interesting findings in the present study was the increase in the intake of some salty food items, such as pickled cucumber, salty roasted seeds, and corn-cheese puff snack following the increase in the intensity of EE. Most of Iranians consume pickles with meals specially with fast foods. They also use salty nuts and seeds as a snack between meals. It seems that negative emotions increase the craving for salty foods. Researchers suggested that dopaminergic and opioidergic neurotransmission within ventral striatal brain regions associated with reward may be important for salt craving [52, 53]. Of note, the increased intake of sugar, saturated fatty acids, TFA and salt can predispose the emotional eaters to insulin resistance, cardiovascular diseases and hypertension, as well as nutrient deficiency, especially in those who suffered from overweight and obesity.
From one point of view, the relationship between EE and micronutrient deficiencies can be considered as a vicious cycle. As it has been discussed, negative emotional conditions such as depression, anxiety and stress trigger some individuals to eat unhealthy energy-dense foods to alleviate the unwanted emotions. This can lead to an unbalanced diet with some nutrient deficiency. Then, a nutrient deficiency may alter the neurotransmitters synthesis or function that consequently affects mental health and increase the risk of depression and mood disorders; and the cycle continues. In the present study, the increased total score of EE was associated with the lower intake of calcium, riboflavin and vitamin B12. This result may be due to a lower intake of dairy products (the good sources of calcium and riboflavin) by emotional eaters in the present study. In fact, we found an inverse relationship between the EE score and each of the food items in the dairy group, although this relationship was not statistically significant for each dairy items (data not shown). A low intake of dietary calcium not only increases the risk of osteoporosis in emotional eaters, but also can impair mood and mental states, which are part of the triggers of EE. The results of the study on 14,971 participants from the US National Health and Nutrition Examination Survey (NHANES) showed a significant negative association between calcium intake and the risk of depressive symptoms [54]. Evidence from research has shown that extracellular calcium influx has an important role in a variety of neural functions [55]. The modulation of extracellular calcium concentration may have a role in regulating emotions, maybe through the direct impact of calcium on stabilizing the plasma membrane [56]. In addition, calcium stimulates tryptophan hydroxylase in the biosynthetic pathways that lead to the manufacture of serotonin [57]. Therefore, any disruptions in the control of calcium levels can have a significant impact on cellular function, potentially affecting mood. Similar to dietary calcium, B vitamins, including riboflavin and vitamin B12, which had an inverse relationship with EE in the present study, also have an effect on mood and mental states [58]. As a result, reducing their intake can intensify EE in whom suffered from this eating behavior disorder. Some previous studies have reported an inverse association between riboflavin and psychological disorders [59, 60]. The involvement of riboflavin coenzymes in the processes of re-methylation of homocysteine may provide an explanation for the possible effects of riboflavin on mental health [61]. Also, It has been reported that vitamin B12 deficiency causes mental disorders in many persons [62]. Vitamin B12 is a vital substance that plays a crucial role in the synthesis of monoamine neurotransmitters in the brain [63]. Specifically, the methylcobalamin form of this vitamin helps convert homocysteine to methionine, which is essential for the formation of S-adenosyl methionine (SAMe). SAMe acts as a methyl donor for the production of monoamine neurotransmitters. Monoamine neurotransmitters, including norepinephrine, dopamine, and serotonin, play an important role in maintaining a normal mood [64, 65].
Based on the findings of the present study, it seems that it is very important to pay attention to the dietary pattern of overweight and obese women who suffer from EE. By modifying the food pattern and following a balanced diet that prevents nutritional deficiencies, it is possible to break the vicious cycle of emotional eating-nutrient deficiency and prevent weight gain and chronic diseases associated with obesity such as glucose intolerance, cardiovascular diseases and some cancers.
For individuals struggling with EE, integrating dietary recommendations with psychotherapy can be profoundly beneficial. A balanced diet rich in whole foods, including fruits, vegetables, lean proteins, low fat dairy and whole grains, can help stabilize blood sugar levels and mood, potentially reducing the urge to eat in response to emotions. Pairing these dietary changes with psychotherapy allows for a holistic approach: while a nutritionist can provide strategies for healthier eating patterns, a therapist can help address the underlying emotional triggers and develop healthier coping mechanisms. Together, these approaches support both the physiological and psychological aspects of EE, fostering sustainable changes in behavior and improving overall well-being.
There were some strong points in our study. To the best of our knowledge, it is the first study to examine the association between EE and nutritional intake in Iranian women who were overweight or obese. Additionally, FFQ was utilized to assess food intake in our study. This method offers a comprehensive overview of an individual’s dietary habits, taking into account a more extended period of typically one year, which gives it an advantage over other methods. However, the present study has some limitations. Firstly, studies investigating food intake are often affected by selection and recall bias, which may also influence this research. Furthermore, the method used in this study to evaluate nutrient intake may have some limitations in terms of underestimating or overestimating the actual intake. However, we controlled for this by excluding those who were outlier regarding the energy intake. Lastly, due to the COVID-19 pandemic, it was not feasible to conduct face-to-face interviews to collect questionnaire data and the participants’ body weight and height information were acquired based on their statements.
Designing a future study that includes a larger and diverse population of Iranian women will provide findings that can be generalized to a wider community. Additionally, it is suggested to conduct clinical trials to determine the beneficial effects of following a special dietary pattern or taking the necessary supplements for women suffering from EE.
Conclusion
The present study aimed to evaluate the relationship between EE and nutritional intake in women with overweight and obesity. The findings of this study indicated that the increased intensity of EE was associated to the increased intake of energy in overweight or obese women, even after adjusting for age and BMI. This increase in daily energy intake among emotional eaters in the current study might be due to their increased intake of cracker, muffin, cake, cream cake, pastry, candy, ice cream, pickles, melon, peanut, salted and roasted seeds and corn-cheese puff snack. In addition, the higher intensity of EE was significantly related to a lower intake of calcium, riboflavin and vitamin B12 after adjusting for energy and age. It seems that for individuals struggling with EE, integrating a balanced diet with psychotherapy can help stabilize blood sugar levels and mood and potentially reducing the urge to eat in response to emotions.
Acknowledgements
We thank the Vice-Chancellor for Research and Technology of Kashan University of Medical Sciences and the Research Center for Biochemistry and Nutrition in Metabolic Diseases, Kashan University of Medical Sciences, Kashan, Iran.
Abbreviations
- EE
Emotional Eating
- FFQ
Food Frequency Questionnaire
- DEBQ
Dutch Eating Behavior Questionnaire
- WHO
World Health Organization
- LDL-C
Low-Density Lipoprotein-Cholesterol
- HDL-C
High-Density Lipoprotein Cholesterol
- BMI
Body Mass Index
- SAMe
S-Adenosyl Methionine
Author contributions
N.S. and H.Z. designed, supervised and drafted the research. H.Z. and A.O. involved in study design, data collection and drafting the manuscript. H.R. contributed to the study design and the statistical analysis of the data. F.N. contributed in conception, study design and data collection. All authors reviewed the final manuscript and approved it.
Funding
This work was supported by the Vice-Chancellor for Research and Technology of Kashan University of Medical Sciences, Kashan, Iran (grant number: 99210).
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the rules and regulations of the Research Center for Biochemistry and Nutrition in Metabolic Diseases at the Kashan University of Medical Science, but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki and the written informed consent form was signed by all the participants. Approval was granted by the Ethics Committee of Kashan University of Medical Sciences, Kashan, Iran (IR.KAUMS.MEDNT.REC.1399.209).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9· 1 million participants. Lancet. 2011;377(9765):557–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the long-term future in 18 European countries and in the USA. Obes Facts. 2020;13(5):514–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koliaki C, Dalamaga M, Liatis S. Update on the Obesity Epidemic: After the Sudden Rise, Is the Upward Trajectory Beginning to Flatten? Curr Obes Rep. 2023 Dec;12(4):514-527. [DOI] [PMC free article] [PubMed]
- 5.Camacho-Barcia L, Giel KE, Jiménez-Murcia S, Álvarez Pitti J, Micali N, Lucas I, et al. Eating disorders and obesity: bridging clinical, neurobiological, and therapeutic perspectives. Trends Mol Med. 2024;30(4):361–79. [DOI] [PubMed] [Google Scholar]
- 6.Vasileiou V, Abbott S. Emotional eating among adults with healthy weight, overweight and obesity: a systematic review and meta-analysis. J Hum Nutr Diet. 2023;36(5):1922–30. [DOI] [PubMed] [Google Scholar]
- 7.Schnepper R, Blechert J, Arend AK, Yanagida T, Reichenberger J. Emotional eating: elusive or evident? Integrating laboratory, psychometric and daily life measures. Eat Weight Disord. 2023;28(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lazarevich I, Camacho MEI, del Consuelo Velázquez-Alva M, Zepeda MZ. Relationship among obesity, depression, and emotional eating in young adults. Appetite. 2016;107:639–44. [DOI] [PubMed] [Google Scholar]
- 9.Zysberg L. Emotional intelligence, anxiety, and emotional eating: a deeper insight into a recently reported association? Eat Behav. 2018;29:128–31. [DOI] [PubMed] [Google Scholar]
- 10.Van Strien T. Causes of emotional eating and matched treatment of obesity. Curr Diab Rep. 2018;18:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Lauzon-Guillain B, Clifton EA, Day FR, Clément K, Brage S, Forouhi NG, et al. Mediation and modification of genetic susceptibility to obesity by eating behaviors. Am J Clin Nutr. 2017;106(4):996–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Denke G, Rawls E, Lamm C. Attentional conflict moderates the association between anxiety and emotional eating behavior: an ERP Study. Front Hum Neurosci. 2018;12:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldsmith R, Joanisse DR, Gallagher D, Pavlovich K, Shamoon E, Leibel RL, et al. Effects of experimental weight perturbation on skeletal muscle work efficiency, fuel utilization, and biochemistry in human subjects. Am J Physiology-Regulatory Integr Comp Physiol. 2010;298(1):R79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freitas A, Albuquerque G, Silva C, Oliveira A. Appetite-related eating behaviours: an overview of Assessment methods, determinants and effects on children’s weight. Ann Nutr Metab. 2018;73(1):19–29. [DOI] [PubMed] [Google Scholar]
- 15.Eisenstein SA, Bischoff AN, Gredysa DM, Antenor-Dorsey JAV, Koller JM, Al-Lozi A, et al. Emotional eating phenotype is associated with central dopamine D2 receptor binding independent of body mass index. Sci Rep. 2015;5(1):11283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Worley J. The role of pleasure neurobiology and dopamine in mental health disorders. J PsychoSoc Nurs Ment Health Serv. 2017;55(9):17–21. [DOI] [PubMed] [Google Scholar]
- 17.Péneau S, Ménard E, Méjean C, Bellisle F, Hercberg S. Sex and dieting modify the association between emotional eating and weight status. Am J Clin Nutr. 2013;97(6):1307–13. [DOI] [PubMed] [Google Scholar]
- 18.Alexandrino-Silva C, Wang Y-P, Viana MC, Bulhões RS, Martins SS, Andrade LH. Gender differences in symptomatic profiles of depression: results from the Sao Paulo Megacity Mental Health Survey. J Affect Disord. 2013;147(1–3):355–64. [DOI] [PubMed] [Google Scholar]
- 19.Marcus SM, Young EA, Kerber KB, Kornstein S, Farabaugh AH, Mitchell J, et al. Gender differences in depression: findings from the STAR* D study. J Affect Disord. 2005;87(2–3):141–50. [DOI] [PubMed] [Google Scholar]
- 20.De Leon A, Roemmich JN, Casperson SL. Identification of barriers to adherence to a weight loss Diet in Women using the nominal group technique. Nutrients. 2020;12(12). [DOI] [PMC free article] [PubMed]
- 21.Whitaker KM, Sharpe PA, Wilcox S, Hutto BE. Depressive symptoms are associated with dietary intake but not physical activity among overweight and obese women from disadvantaged neighborhoods. Nutr Res. 2014;34(4):294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Janke EA, Jones E, Hopkins CM, Ruggieri M, Hruska A. Catastrophizing and anxiety sensitivity mediate the relationship between persistent pain and emotional eating. Appetite. 2016;103:64–71. [DOI] [PubMed] [Google Scholar]
- 23.Kilkus JM, Booth JN, Bromley LE, Darukhanavala AP, Imperial JG, Penev PD. Sleep and eating behavior in adults at risk for type 2 diabetes. Obesity. 2012;20(1):112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mensorio MS, Cebolla A, Lisón JF, Rodilla E, Palomar G, Miragall M, et al. Emotional eating as a mediator between anxiety and cholesterol in population with overweight and hypertension. Psychol Health Med. 2017;22(8):911–8. [DOI] [PubMed] [Google Scholar]
- 25.Bellisle F. Assessing various aspects of the motivation to eat that can affect food intake and body weight control. L’encephale. 2008;35(2):182–5. [DOI] [PubMed] [Google Scholar]
- 26.Song Y-M, Lee K. Eating behavior and metabolic syndrome over time. Eating and Weight disorders-studies on Anorexia. Bulimia Obes. 2020;25:545–52. [DOI] [PubMed] [Google Scholar]
- 27.Sharifi N, Mahdavi R, Ebrahimi-Mameghani M. Perceived barriers to weight loss programs for overweight or obese women. Health Promotion Perspect. 2013;3(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jáuregui-Lobera I, García-Cruz P, Carbonero-Carreño R, Magallares A, Ruiz-Prieto I. Psychometric properties of Spanish version of the three-factor eating Questionnaire-R18 (Tfeq-Sp) and its relationship with some eating-and body image-related variables. Nutrients. 2014;6(12):5619–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Annesi JJ, Mareno N, McEwen K. Psychosocial predictors of emotional eating and their weight-loss treatment-induced changes in women with obesity. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2016;21:289 – 95. [DOI] [PubMed]
- 30.Annesi JJ. Exercise predicts long-term weight loss in women with class 1 and class 2 obesity through effects on emotional eating and its correlates. J Phys Activity Health. 2018;15(1):57–63. [DOI] [PubMed] [Google Scholar]
- 31.Finn K, Jacquier E, Kineman B, Storm H, Carvalho R. Nutrient intakes and sources of fiber among children with low and high dietary fiber intake: the 2016 feeding infants and toddlers study (FITS), a cross-sectional survey. BMC Pediatr. 2019;19:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gwin JA, Karl JP, Lutz LJ, Gaffney-Stomberg E, McClung JP, Pasiakos SM. Higher protein density diets are associated with greater diet quality and micronutrient intake in healthy young adults. Front Nutr. 2019;6:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marx W, Moseley G, Berk M, Jacka F. Nutritional psychiatry: the present state of the evidence. Proceedings of the Nutrition Society. 2017;76(4):427 – 36. [DOI] [PubMed]
- 34.Pertile RA, Cui X, Eyles DW. Vitamin D signaling and the differentiation of developing dopamine systems. Neuroscience. 2016;333:193–203. [DOI] [PubMed] [Google Scholar]
- 35.Eid A, Khoja S, AlGhamdi S, Alsufiani H, Alzeben F, Alhejaili N, et al. Vitamin D supplementation ameliorates severity of generalized anxiety disorder (GAD). Metab Brain Dis. 2019;34(6):1781–6. [DOI] [PubMed] [Google Scholar]
- 36.Chambial S, Dwivedi S, Shukla KK, John PJ, Sharma P. Vitamin C in disease prevention and cure: an overview. Indian J Clin Biochem. 2013;28(4):314–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gromova O, Torshin IY, Pronin A, Kilchevsky M. Synergistic application of zinc and vitamin C to support memory, attention and the reduction of the risk of the neurological diseases. Zhurnal Nevrologii i psikhiatrii imeni. SS Korsakova. 2017;117(7):112–9. [DOI] [PubMed] [Google Scholar]
- 38.Fuentes-Albero M, Martínez-Martínez MI, Cauli O. Omega-3 long-chain polyunsaturated fatty acids intake in children with attention deficit and hyperactivity disorder. Brain Sci. 2019;9(5). [DOI] [PMC free article] [PubMed]
- 39.Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62. [DOI] [PubMed] [Google Scholar]
- 40.Tirthani E, Said MS, Rehman A, Genetics. and Obesity: StatPearls Publishing, Treasure Island (FL); 2023 2023. [PubMed]
- 41.Ashrafi E, Kachooei M, Ghazaghi M. Investigating the reliability and validity of the power of food scale (PFS). Knowl Res Appl Psychol. 2017;16(3):113–25. [Google Scholar]
- 42.van Strien T, Cebolla A, Etchemendy E, Gutiérrez-Maldonado J, Ferrer-García M, Botella C, et al. Emotional eating and food intake after sadness and joy. Appetite. 2013;66:20–5. [DOI] [PubMed] [Google Scholar]
- 43.Calderón-Asenjo RE, Jalk-Muñoz MC, Calizaya-Milla YE, Calizaya-Milla SE, Ramos-Vera C, Saintila J. Association between Emotional Eating, Sociodemographic Characteristics, physical activity, Sleep Duration, and Mental and Physical Health in Young adults. J Multidiscip Healthc. 2022;15:2845–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Madalı B, Alkan ŞB, Örs ED, Ayrancı M, Taşkın H, Kara HH. Emotional eating behaviors during the COVID-19 pandemic: a cross-sectional study. Clin Nutr ESPEN. 2021;46:264–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paans NPG, Gibson-Smith D, Bot M, van Strien T, Brouwer IA, Visser M, et al. Depression and eating styles are independently associated with dietary intake. Appetite. 2019;134:103–10. [DOI] [PubMed] [Google Scholar]
- 46.Betancourt-Núñez A, Torres-Castillo N, Martínez-López E, De Loera-Rodríguez CO, Durán-Barajas E, Márquez-Sandoval F et al. Emotional eating and dietary patterns: reflecting Food choices in people with and without abdominal obesity. Nutrients. 2022;14(7). [DOI] [PMC free article] [PubMed]
- 47.Lu Q, Tao F, Hou F, Zhang Z, Ren LL. Emotion regulation, emotional eating and the energy-rich dietary pattern. A population-based study in Chinese adolescents. Appetite. 2016;99:149–56. [DOI] [PubMed] [Google Scholar]
- 48.Camilleri GM, Méjean C, Kesse-Guyot E, Andreeva VA, Bellisle F, Hercberg S, et al. The associations between emotional eating and consumption of energy-dense snack foods are modified by sex and depressive symptomatology. J Nutr. 2014;144(8):1264–73. [DOI] [PubMed] [Google Scholar]
- 49.Dakanalis A, Mentzelou M, Papadopoulou SK, Papandreou D, Spanoudaki M, Vasios GK et al. The Association of Emotional Eating with Overweight/Obesity, Depression, Anxiety/Stress, and dietary patterns: a review of the current clinical evidence. Nutrients. 2023;15(5). [DOI] [PMC free article] [PubMed]
- 50.Singh M. Mood, food, and obesity. Front Psychol. 2014;5:925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15(1):37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morris MJ, Na ES, Johnson AK. Salt craving: the psychobiology of pathogenic sodium intake. Physiol Behav. 2008;94(5):709–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lucas LR, Grillo CA, McEwen BS. Involvement of mesolimbic structures in short-term sodium depletion: in situ hybridization and ligand-binding analyses. Neuroendocrinology. 2003;77(6):406–15. [DOI] [PubMed] [Google Scholar]
- 54.Shen X, Gu X, Liu YY, Yang L, Zheng M, Jiang L. Association between dietary calcium and depression among American adults: National health and nutrition examination survey. Front Nutr. 2023;10:1042522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xu L, Zhang S, Chen W, Yan L, Chen Y, Wen H, et al. Trace elements differences in the depression sensitive and resilient rat models. Biochem Biophys Res Commun. 2020;529(2):204–9. [DOI] [PubMed] [Google Scholar]
- 56.Mockett BG, Guévremont D, Wutte M, Hulme SR, Williams JM, Abraham WC. Calcium/calmodulin-dependent protein kinase II mediates group I metabotropic glutamate receptor-dependent protein synthesis and long-term depression in rat hippocampus. J Neurosci. 2011;31(20):7380–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Knapp S, Mandell AJ, Bullard WP. Calcium activation of brain tryptophan hydroxylase. Life Sci. 1975;16(10):1583–93. [DOI] [PubMed] [Google Scholar]
- 58.Jahan-Mihan A, Stevens P, Medero-Alfonso S, Brace G, Overby LK, Berg K et al. The role of Water-Soluble vitamins and Vitamin D in Prevention and Treatment of Depression and Seasonal Affective disorder in adults. Nutrients. 2024;16(12). [DOI] [PMC free article] [PubMed]
- 59.Wu Y, Zhang L, Li S, Zhang D. Associations of dietary vitamin B1, vitamin B2, vitamin B6, and vitamin B12 with the risk of depression: a systematic review and meta-analysis. Nutr Rev. 2022;80(3):351–66. [DOI] [PubMed] [Google Scholar]
- 60.Rouhani P, Amoushahi M, Keshteli AH, Saneei P, Afshar H, Esmaillzadeh A, et al. Dietary riboflavin intake in relation to psychological disorders in Iranian adults: an observational study. Sci Rep. 2023;13(1):5152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCormick DB. Two interconnected B vitamins: riboflavin and pyridoxine. Physiol Rev. 1989;69(4):1170–98. [DOI] [PubMed] [Google Scholar]
- 62.Kaner G, Soylu M, Yüksel N, Inanç N, Ongan D, Başmısırlı E. Evaluation of nutritional status of patients with depression. Biomed Res Int. 2015;2015. [DOI] [PMC free article] [PubMed]
- 63.Bar-Shai M, Gott D, Marmor S. Acute psychotic depression as a sole manifestation of vitamin B12 deficiency. Psychosomatics. 2011;52(4):384–6. [DOI] [PubMed] [Google Scholar]
- 64.Moore K, Hughes CF, Hoey L, Ward M, Cunningham C, Molloy AM, et al. B-vitamins in relation to depression in older adults over 60 years of age: the Trinity Ulster Department of Agriculture (TUDA) Cohort Study. J Am Med Dir Assoc. 2019;20(5):551–7. e1. [DOI] [PubMed] [Google Scholar]
- 65.Froese DS, Fowler B, Baumgartner MR. Vitamin B12, folate, and the methionine remethylation cycle—biochemistry, pathways, and regulation. J Inherit Metab Dis. 2019;42(4):673–85. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available due to the rules and regulations of the Research Center for Biochemistry and Nutrition in Metabolic Diseases at the Kashan University of Medical Science, but are available from the corresponding author on reasonable request.