Abstract
Background
In addition to the persistence of SARS-CoV-2 infections, those with Influenza A/B and RSV have reappeared in 2022/23. To compare the development of prevalence, clinical outcomes and risk factors, we analysed data of the season 2023/24 from the same region/hospital as for 2022/23.
Methods
Patients covering the whole age range with a positive polymerase chain reaction (PCR) test for SARS-CoV-2, Influenza A/B, RSV were included from the internal, neurological and paediatric units of the RoMed hospital Rosenheim, Germany/Bavaria, from August 1st 2023 to 29th February 2024.
Results
Of 932 patients included, 912 showed single infections with SARS-CoV-2, Influenza A or RSV (47.9% female, median age 68.0 years; 52.9% SARS-CoV-2, 23.2% Influenza A, 21.8% RSV). Co-infections (2.0%) and Influenza B (0.1%) were negligible. In patients of age ≥ 18 years (n = 628, 68.5% SARS-CoV-2, 26.0% Influenza A, 5.6% RSV), patients with Influenza A were younger compared to SARS-CoV-2 (p < 0.001), with RSV similar to SARS-CoV-2. Heart failure and asthma were the most prevalent comorbidities for RSV, immunosuppression for Influenza A. Admission to Intensive Care Unit (ICU) occurred in 111 patients (17.0% of SARS-CoV-2, 17.2% Influenza A, 28.6% RSV), and 59 patients died (8.8% SARS-CoV-2, 8.6% Influenza A, 20.0% RSV). Low-flow oxygen supplementation and non-invasive ventilation (NIV) were most frequent for RSV (68.6% and 20.0%, respectively), oxygen demand upon admission for Influenza A (39.3%), without differences in high-flow oxygen supply or length of hospital stay. Among patients aged < 18 years (n = 284, 21.4% SARS-CoV-2, 18.0% Influenza A, 57.1% RSV), 15 were admitted to ICU (4.8% SARS-CoV-2, 3.8% Influenza A, 6.0% RSV); none of them died. Oxygen supply via high-flow, low-flow or upon admission was highest for RSV (23.8%, 70.2%, 21.4%, respectively), as well as the length of hospital stay.
Conclusion
Between 8/2023 to 2/2024, a large population of patients hospitalized due to respiratory tract infection, showed relative contributions of SARS-CoV-2, Influenza A or RSV similar to those in 2022/23. The findings underline that in both, adults and children, RSV posed a relatively higher clinical risk than Influenza A and SARS-CoV-2, though absolute numbers remained highest for SARS-CoV-2.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40001-024-02096-9.
Introduction
Among the causes of hospitalization, lower respiratory tract infections are common especially in young children [1–6] and the elderly [7–10]. While from 2020 to 2022 it appeared that SARS-CoV-2 strongly dominated this type of infection [11–14], in the season 2022/23 viruses such as Influenza A and Respiratory Syncytial Virus (RSV) that had been known as causes for admission previously, reappeared in appreciable numbers [15]. This provided the opportunity to compare the clinical characteristics of patients between different types of infection without the need to refer to historical data that easily might be biased. We performed such a comparison for the season 2022/23 in a large population comprising both very young and very old patients [15]; about 48% had been admitted due to SARS-CoV-2, 22% due to Influenza A and 28% due to RSV, while other types of infections and co-infections were negligible. In older patients, the rate of ICU admissions and mortality risk were similar for SARS-CoV-2 and Influenza A, but elevated for RSV. In children there was no mortality but the highest need for treatment still occurred with RSV [1, 3].
These observations raised the question, whether they represented a singular pattern that was possibly influenced by rebound effects originating from the scarcity of other infections during the dominance of SARS-CoV-2, or whether they indicated a stable situation that might continue into the future. To answer this question, we repeated the previous type of analysis [15] using data from the 2023/24 season. This approach had the advantage of guaranteeing a high degree of comparability, since data was obtained in the same large primary care hospital located in Southern Germany, with essentially the same staff and in the same population of potential patients.
Thus, the primary aim of our analysis was to determine the frequency of infections with SARS-CoV-2, Influenza A and RSV that led to hospital admission in the season 2023/24, the occurrence of co-infections, the need for admission to Intensive Care Unit (ICU) or respiratory support including oxygen supply, mortality, as well as risk factors for ICU admission and mortality. These findings could be directly compared with those obtained in the season 2022/23 in order to identify potential changes over time.
Materials and methods
Study population
This retrospective study was based on data obtained in the RoMed hospital Rosenheim, Germany, between August 1st 2023 and February 29th 2024. We included patients of all ages (n = 1065) hospitalized with positive PCR tests for SARS-CoV-2, Influenza A/B, RSV, or co-infections with these viruses. The analysis was restricted to patients from internal, neurology and pediatric units, similar to the previous study [15]. Patients from other medical units such as gynecology, surgery and urology were excluded, because we had observed that in these patients infection was often not the cause for hospitalization and not relevant for the hospital stay [16]. If there were hints for infection, a combined PCR test for SARS-CoV-2, Influenza A/B and RSV was carried out. Invalid or unclear PCR test results were confirmed by sequential testing, either with a combined test or with single specific tests. The study protocol had been approved by the Ethical Committee of the University of Regensburg, Germany (#23–3527-104).
Assessments
Presence and type of infection were confirmed by PCR testing, either directly upon admission or during the hospital stay. Among the available PCR test kits, in the season 2023/24 the following were used: Cepheid® Xpert® Xpress CoV-2 and Cepheid® Xpert® Xpress CoV-2/Flu/RSV (Cepheid GmbH, Krefeld, Germany), BD SARS-CoV-2/Flu with BD MAX™ System and BD SARS-CoV-2/Flu/RSV with BD MAX System™ (both BD Becton Dickinson GmbH, Sparks, Maryland, USA), and also the STANDARD™ M10 SARS-CoV-2 and STANDARD™ M10 FLU/RSV/SARS-CoV-2 (SD BIOSENSOR, INC., Suwon, Republic of South Korea).
The required information on the patients’ clinical state was retrieved via the software package Medico (Version 28, CGM Clinical Europe GmbH, Koblenz, Rheinland-Pfalz, Germany). Data comprised age, sex, body mass index (BMI) and the spectrum of comorbidities. As symptoms upon admission, cough, dyspnoea, fatigue, fever, diarrhoea and nausea were included. Vital parameters upon admission comprised systolic and diastolic blood pressure, respiratory rate, heart rate, body temperature and peripheral oxygen saturation (SpO2). Laboratory blood parameters upon admission were based on peripheral venous samples and included (differential) cell count, glomerular filtration rate estimated via creatine (eGFR), and the levels of C-reactive protein (CRP), procalcitonin, lactate dehydrogenase (LDH), troponin, N-terminal pro b-type natriuretic peptide (NT-proBNP), D-dimers and liver enzymes. Blood gas parameters comprised pH and arterial pressures of oxygen (pO2) and carbon dioxide (pCO2).
Outcomes
The occurrence of ICU transfer or in-hospital death were chosen as primary outcomes for comparing the types of infection with each other. Secondary outcomes comprised the occurrence of treatment with invasive ventilation, non-invasive ventilation (NIV), or high-flow or low-flow oxygen supply. For high-flow therapy (HFNC), a nasal cannula or Venturi mask was used with flow rates from 30 up to 60 L/min, while for low-flow therapy, flow rates between 2 and 4 L/min, in rare cases up to 15 L/min, were administered via Venturi mask or nasal cannula.
Data analysis
To describe the results, numbers and percentages, or median values and quartiles were computed, depending on the type of data. For comparing the types of infection, we used the exact test according to Fisher-Freeman-Halton, or the Kruskal–Wallis test, whatever was appropriate. In case of the Kruskal–Wallis test, post hoc comparisons were performed via the Mann–Whitney U-test with Bonferroni correction for the multiplicity of tests. To explore the relationship between patients’ characteristics, types of infection and the two primary outcomes, logistic regression analysis was used. Logistic regression analysis was also employed to assess whether the dependence of symptoms or comorbidities on the type of infection was related to their dependence on age and sex. The level of statistical significance was assumed at p < 0.05. All analyses were performed using the statistical software package SPSS (version 29, IBM Corporation, Armonk, NJ, USA).
Results
Anthropometric data and distribution of infections
Of 1065 patients of all departments including those with re-admission, 932 patients remained when selecting those from the internal medicine, neurology and pediatric units, who were not admitted a second time with the same virus within 4 weeks. These patients comprised 446 women (47.9%) and 486 men (52.1%). The median values (quartiles) of age and BMI were 68 (3; 81) years and 25.7 (22.6, 29.8) kg/m2, respectively. Table 1 provides additional data on the distribution of anthropometric indices across infection groups. Most patients (52.9%) showed infection with SARS-CoV-2, while Influenza A and RSV each accounted for about the half of the remaining cases (23.2% and 21.8%, respectively). Patients with Influenza B or with combined infections were rare (see Table 1), therefore the subsequent statistical comparisons comprised only the 912 patients with single infections with SARS-CoV-2, Influenza A, or RSV.
Table 1.
Baseline characteristics of all patients
| Number | n (< 18 years) | n (≥ 18 years) | Sex (m/f) | Age (years) | BMI (kg/m2)a | |
|---|---|---|---|---|---|---|
| Total | 932 | 294 | 638 | 486/446 (52.1%/47.9%) | 68 (3; 81) | 25.7 (22.6; 29.8) |
| SARS-CoV-2 | 493 (52.9%) | 63 (21.4%) | 430 (67.4%) | 267/226 (54.2%/45.8%) | 77 (61; 84)* | 25.9 (22.6; 29.5) |
| Influenza A | 216 (23.2%) | 53 (18.0%) | 163 (25.5%) | 108/108 (50.0%/50.0%) | 65 (20; 78)* | 25.5 (22.9; 31.5) |
| Influenza B | 1 (0.1%) | 0 (0.0%) | 1 (0.2%) | 1/0 (100%/0%) | n.d | n.d |
| RSV | 203 (21.8%) | 168 (57.1%) | 35 (5.5%) | 101/102 (49.8%/50.2%) | 1 (0; 3)* | 23.6 (20.7; 26.5) |
| Influenza A + SARS | 6 (0.6%) | 1 (0.3%) | 5 (0.8%) | 4/2 (66.7%/33.3%) | 82 (58; 83) | 21.4 (20.0; 30.1) |
| Influenza A + RSV | 8 (0.9%) | 5 (1.7%) | 3 (0.5%) | 2/6 (25.0%/75.0%) | 3.5 (0.8; 72) | n.d |
| Influenza B + RSV | 1 (0.1%) | 1 (0.3%) | 0 (0%) | 1/0 (100%/0%) | n.d | n.d |
| SARS + RSV | 4 (0.4%) | 3 (1.0%) | 1 (0.2%) | 2/2 (50%/50%) | 2.0 (0.3; 56) | n.d |
Numbers and percentages, or median values and quartiles (in parentheses) are given
n.d., not determined; BMI, body mass index
*significantly different from each other (p < 0.001)
aAvailable only in patients of age ≥ 18 years
In these 912 patients, sex did not show statistically significant differences between the three infection groups. BMI, which was available only in adults, also was not significantly different. Age, however, differed (p < 0.001), whereby pairwise comparisons showed that all three groups were different from each other (p < 0.001 each); it was lowest in the RSV group. Age distribution is illustrated in Fig. 1, demonstrating the two distinctive peaks at very low and at high age, as observed in 2022/23 [15].
Fig. 1.
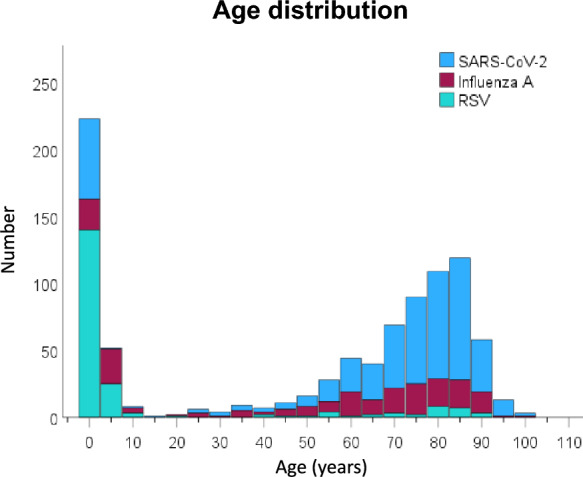
Distribution of age in hospitalized patients stratified for infection type. Absolute numbers are shown for each age category comprising 5 years. The numbers refer to the whole observation period from August 2023 to February 2024
Similarly, in patients of age ≥ 18 years, age differed between the three infection groups (p < 0.001), but in this case, only between Influenza A and SARS-CoV-2 (p < 0.001), whereas the RSV group was not significantly different from the other two groups. Median values (quartiles) were 78 (70; 84) years for SARS-CoV-2, 73 (60; 82) years for Influenza A, and 78 (57; 84) years for RSV. In patients of age < 18 years (mean age 1.43 years), age also differed between groups (p < 0.001), whereby all three groups were different from each other (p < 0.001 each), with lowest values for SARS-CoV-2 (0.54 years), highest values for Influenza A (3.28 years), and intermediate values for RSV (1.18 years). For the time course of prevalence values in the two age groups, see the Supplemental Figure S1.
Prevalence of symptoms
Self-reported symptoms were recorded only for patients aged ≥ 18 years. The prevalence of cough and dyspnoea showed significant (p < 0.001 each) differences between the three types of infection (Supplemental Table S1). Both showed the lowest values in SARS-CoV-2 and highest values in RSV. Fever also showed a difference between groups (p = 0.004) and high prevalence in patients with SARS-CoV-2. There were no significant differences regarding fatigue, diarrhoea and nausea. When using logistic regression analysis with the symptoms as dependent variable and the additional predictors age and sex, it turned out that significant differences between infections remained (p < 0.05 each) for cough and dyspnoea but not for fever, in which there was, however, a significant dependence on sex (p = 0.017).
Comorbidities
In patients aged ≥ 18 years, there were significant differences between the three groups regarding the frequencies of peripheral artery disease, heart failure, asthma, dementia and state of immunosuppression (p < 0.05 each, Table 2). Heart failure and asthma were most often found in patients with RSV infection, immunosuppression of all kind most often in Influenza A. The sum score of the comorbidities shown in Table 2 did not significantly differ between groups. In order to clarify, to which extent the differences in prevalence were due to the dependence of comorbidities on age, we again performed logistic regression analysis with the comorbidities as outcomes and the type of infection as well as age and sex as predictors. Heart failure depended on age (p < 0.001) and on RSV (p < 0.001), peripheral artery disease on sex and RSV (p < 0.05 each), asthma also on sex and RSV (p < 0.05 each), while dementia was associated with age (p < 0.001) as well as Influenza A (p = 0.016), and this was also true for immunosuppression (p < 0.001 and p = 0.033, respectively). These observations demonstrate that the association between comorbidities and the type of viral infection was not explained by their dependence on sex and age.
Table 2.
Prevalence of comorbidities in patients of age ≥ 18 years
| SARS-CoV-2 | Influenza A | RSV | P value | |
|---|---|---|---|---|
| n | 430 | 163 | 35 | |
| Hypertension | 267 (62.1%) | 96 (58.9%) | 25 (71.4%) | 0.385 |
| Peripheral artery disease (PAD) | 33 (7.7%) | 8 (4.9%) | 6 (17.1%) | 0.048 |
| Heart failure (HF) | 83 (19.3%) | 35 (21.5%) | 17 (48.6%) | < 0.001 |
| Coronary artery disease (CAD) | 103 (24.0%) | 32 (19.6%) | 7 (20.0%) | 0.529 |
| Diabetes mellitus Type 2 | 120 (27.9%) | 42 (25.8%) | 8 (22.9%) | 0.774 |
| COPD | 60 (14.0%) | 32 (19.6%) | 9 (25.7%) | 0.068 |
| Asthma | 19 (4.4%) | 14 (8.6%) | 5 (14.3%) | 0.018 |
| Other lung disease* | 134 (31.2%) | 52 (31.9%) | 14 (40.0%) | 0.565 |
| Chronic kidney disease (CKD) | 133 (30.9%) | 44 (27.0%) | 6 (17.1%) | 0.180 |
| Active malignant disease** | 97 (22.6%) | 28 (17.2%) | 7 (20.0%) | 0.354 |
| Rheumatic disease | 20 (4.7%) | 5 (3.1%) | 2 (5.7%) | 0.612 |
| Depression | 51 (11.9%) | 12 (7.4%) | 2 (5.7%) | 0.217 |
| Dementia | 71 (16.5%) | 10 (6.1%) | 5 (14.3%) | 0.002 |
| State of Immunosuppression | 21 (4.9%) | 19 (11.7%) | 3 (8.6%) | 0.012 |
| Number of Comorbidities*** | 3 (2; 4) | 2 (1; 4) | 3 (2; 4) | 0.151 |
Numbers and percentages are shown, for the sum of comorbidities median values and quartiles *except malignant lung disease, **within the last 5 years, *** sum of comorbidities from this list
Statistical comparisons between the infection groups were performed with the exact test according to Fisher-Freeman-Halton, for the sum using the Kruskal–Wallis test
Primary outcomes
The occurrence of ICU treatment and in-hospital mortality was compared between Influenza A, SARS-CoV-2 or RSV separately in patients of age ≥ 18 years and < 18 years (Table 3). In patients of age ≥ 18 years, neither regarding ICU admission nor regarding in-hospital mortality, the significant differences between the three groups were statistically, despite the fact that values were highest for RSV; however, it has to be considered that this changed in the multivariable analyses (see below). In patients of age < 18 years, case numbers were low, and there was no mortality at all in this age group. When using the exact test according Fisher-Freeman-Halton to account for the low numbers in ICU admissions, a p-value of 0.934 was obtained for comparing the three infection groups.
Table 3.
ICU admission and mortality stratified according to age group
| < 18 years | ≥ 18 years | |||||
|---|---|---|---|---|---|---|
| n | ICU admission | Mortality | n | ICU admission | Mortality | |
| Number | 284 | 15 (5.3%) | 0 (0.0%) | 628 | 111 (17.7%) | 59 (9.4%) |
| SARS-CoV-2 | 63 | 3 (4.8%) | 0 (0.0%) | 430 | 73 (17.0%) | 38 (8.8%) |
| Influenza A | 53 | 2 (3.8%) | 0 (0.0%) | 163 | 28 (17.2%) | 14 (8.6%) |
| RSV | 168 | 10 (6.0%) | 0 (0.0%) | 35 | 10 (28.6%) | 7 (20.0%) |
Numbers and percentages are shown
Mortality refers to in-hospital mortality
ICU, Intensive Care Unit
To assess whether the start of data collection in August 2023 compared to October 2022 [15] had affected the results, a similar table as Table 3 was established using only data starting in October 2023 (Supplemental Table S2). The results were very similar to those of Table 3, and identical regarding Influenza A and RSV which became prevalent only in November 2023 (see Supplemental Fig. 1).
Treatment characteristics
Table 4 shows results regarding the treatment of patients aged ≥ 18 years. The length of the hospital stay did not differ between groups, and there were also no significant differences regarding the durations of invasive or non-invasive ventilation. However, the frequencies of NIV, low-flow oxygen supply during the hospital stay, and oxygen supply upon admission differed significantly between the three groups (p < 0.05 each). While RSV showed the highest percentages for NIV and low-flow oxygen supply during the hospital stay, it showed the lowest percentage regarding oxygen supply upon admission.
Table 4.
Details of clinical treatment in patients of age ≥ 18 years
| SARS-CoV-2 | Influenza A | RSV | P value | |
|---|---|---|---|---|
| n | 430 | 163 | 35 | – |
| Length of hospital stay, days | 7.2 (3.8; 13.7) | 7.3 (4.2; 11.4) | 6.0 (3.7; 12.9) | 0.501 |
| Intensive care unit | ||||
| Frequency | 73 (17.0%) | 28 (17.2%) | 10 (28.6%) | 0.220 |
| Length of stay, days | 4.0 (2.0; 7.9) | 5.2 (2.3; 7.8) | 5.6 (2.6; 10.5) | 0.531 |
| Mechanical invasive ventilation | ||||
| Frequency | 23 (5.3%) | 6 (3.7%) | 4 (11.4%) | 0.162 |
| Duration, days | 3.8 (2.0; 7.0) | 6.2 (4.0; 18.3) | 4.6 (1.8; 7.6) | 0.229 |
| NIV | ||||
| Frequency | 26 (6.0%) | 13 (8.0%) | 7 (20.0%) | 0.017 |
| Duration, days | 2.0 (1.0; 4.0) | 3.0 (1.5; 4.5) | 5.0 (1.0; 7.0) | 0.413 |
| Oxygen supplementation | ||||
| High-flow during stay | 31 (7.2%) | 11 (6.7%) | 4 (11.4%) | 0.531 |
| Low-flow during stay | 205 (47.7%) | 93 (57.1%) | 24 (68.6%) | 0.013 |
| Upon admission | 120 (27.9%) | 64 (39.3%) | 9 (25.7%) | 0.025 |
Numbers and percentages, or median values and quartiles (in parentheses) are given
Statistical comparisons between the infection groups were performed with the exact test according to Fisher-Freeman-Halton, for the sum values (length, duration) using the Kruskal–Wallis test
NIV, non-invasive ventilation
Table 5 shows analogous data for patients of age < 18 years. The length of the hospital stay differed between the three groups (p < 0.001), with significant differences between RSV versus both SARS-CoV-2 and Influenza A (p < 0.001 each). There were no significant differences regarding ICU admission and invasive or non-invasive ventilation but marked differences regarding oxygen supply. Both high-flow and low-flow supply during the hospital stay, as well as oxygen supply upon admission were highest in the RSV group (p < 0.001 each). As the group of young children was of particular interest, we also analyzed data of patients with age < 3 years separately (Supplemental Table S3). The great majority of these children had RSV infection. Again, in RSV patients, the duration of hospital stay was longest, and this was due to a significant difference of the RSV group versus the other two groups (p < 0.001 each). Moreover, the percentages of all kind of oxygen supply were by far the highest in this group (p < 0.001 each).
Table 5.
Details of clinical treatment in patients of age < 18 years
| SARS-CoV-2 | Influenza A | RSV | P value | |
|---|---|---|---|---|
| n | 63 | 53 | 168 | – |
| Length of hospital stay, days | 1.7 (1.1; 2.1) | 1.8 (0.9; 3.6) | 3.4 (1.9; 6.1) | < 0.001 |
| Intensive care unit | ||||
| Frequency | 3 (4.8%) | 2 (3.8%) | 10 (6.0%) | 0.934 |
| Length of stay, days | 2.9 (1.0; n.d.) | 13.1 (4.3; n.d.) | 5.9 (3.0; 14.2) | 0.237 |
| Mechanical invasive ventilation | ||||
| Frequency | 0 (0.0%) | 1 (1.9%) | 2 (1.2%) | 0.561 |
| Duration, days | n.d | 11.0 (n.d.) | 4.0 (2.0; n.d.) | 0.221 |
| NIV | ||||
| Frequency | 1 (1.6%) | 0 (0.0%) | 5 (3.0%) | 0.631 |
| Duration, days | 2.0 | n.d | 4.0 (1.5; 9.0) | 0.552 |
| Oxygen supplementation | ||||
| High-flow during stay | 1 (1.6%) | 3 (5.7%) | 40 (23.8%) | < 0.001 |
| Low-flow during stay | 3 (4.8%) | 10 (18.9%) | 118 (70.2%) | < 0.001 |
| Upon admission | 3 (4.8%) | 5 (9.4%) | 36 (21.4%) | 0.002 |
Numbers and percentages, or median values and quartiles (in parentheses) are given
Statistical comparisons between the infection groups were performed with the exact test according to Fisher-Freeman-Halton, for the sum values (length, duration) using the Kruskal–Wallis test
n.d., not determined; NIV, non-invasive ventilation
Vital parameters, arterial blood gas and laboratory parameters upon admission
For patients ≥ 18 years, vital parameters upon admission are shown in Supplemental Table S4. Breathing frequency, heart frequency, body temperature, peripheral oxygen saturation and diastolic blood pressure significantly (p < 0.05 each) differed between groups, while systolic blood pressure did not. In addition, there were differences in pH and pCO2 (p < 0.05 each) but not pO2, eGFR, CRP and D-dimer levels. According to the Bonferroni-adjusted post hoc comparisons, SARS-CoV-2 differed from RSV and Influenza A regarding respiratory rate and heart rate, moreover from Influenza A oxygen saturation and diastolic blood pressure, and from RSV regarding pH (p < 0.05 each). Regarding body temperature, RSV was different from the other two groups (p < 0.05 each). For the other parameters, the adjusted pairwise comparisons did not indicate significant differences between specific groups.
Risk factors for ICU admission and in‑hospital death
The data shown in Table 3 suggested that the frequencies of ICU admission and in-hospital mortality were highest in RSV but the unadjusted analyses did not indicate a statistically significant difference. We therefore determined whether the consideration of confounding factors would indicate a higher risk for RSV, especially in patients of age ≥ 18 years. Among the relevant confounding factors could be age, sex, the need for oxygen supply, CRP as marker of inflammation, eGFR, comorbidities (Table 2) and the symptoms listed in Supplemental Table S1.
A logistic regression analysis using as predictors symptoms, age, sex and oxygen supply in addition to indicator variables of infection with Influenza A or RSV (taking SARS-CoV-2 as reference), showed a tendency for increased ICU admission with RSV infection (p = 0.065; OR = 2.4) but not Influenza A (p = 0.173). Among symptoms, only cough was relevant (p = 0.009). In addition, age (p < 0.001) and sex (p = 0.001) were statistically significant, as well as oxygen supply upon admission (p < 0.001).
To assess the reliability of these findings regarding the type of infection, we further added oxygen saturation, CRP levels upon admission and the comorbidities heart failure, peripheral arterial disease and immunosuppression (see Table 2) as predictors. Age, sex, oxygen supply upon admission and cough were confirmed as significant predictors (p < 0.05 each), and in addition fever (p = 0.047) and CRP (p = 0.004). Neither RSV (p = 0.112) nor Influenza A (p = 0.297) were specifically relevant for ICU admission in the presence of these confounders. In these analyses, comorbidities were never significant and thus omitted from the final analysis shown in Fig. 2. The results underline that the type of infection was not a significant predictor for ICU admission if adjusting for multiple patient characteristics, despite a tendency for RSV.
Fig. 2.
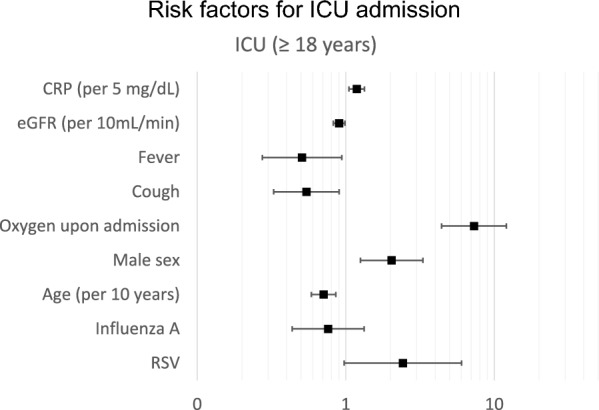
Results of multiple logistic regression analysis addressing potential risk factors for ICU admission in patients of age ≥ 18 years. Regarding the comparison of the three infections, SARS-CoV-2 was taken as the reference. Odds ratios and 95% confidence intervals are shown. CRP, C-reactive protein, eGFR, glomerular filtration rate estimated from creatinine
The analogous analysis for mortality identified RSV as highly significant risk factor (p = 0.005; OR = 4.4), besides age (p = 0.011), sex (p = 0.007), oxygen upon admission (p < 0.001), cough (p = 0.031) and eGFR (p = 0.045), while Influenza A was not (p = 0.861). Using the extended set of predictors as for ICU admission (see above), age, sex, oxygen upon admission, cough, oxygen saturation and CRP were significant predictors (p < 0.05 each), in addition to RSV (p = 0.005; OR = 4.7), while again Influenza A was not relevant (p = 0.930). Again, comorbidities did not have significant effects in the presence of the other predictors. The results are shown in Fig. 3 and demonstrate that RSV was a significant predictor for elevated mortality after adjustment for multiple patient characteristics, while SARS-CoV-2 and Influenza A were similar in this respect.
Fig. 3.
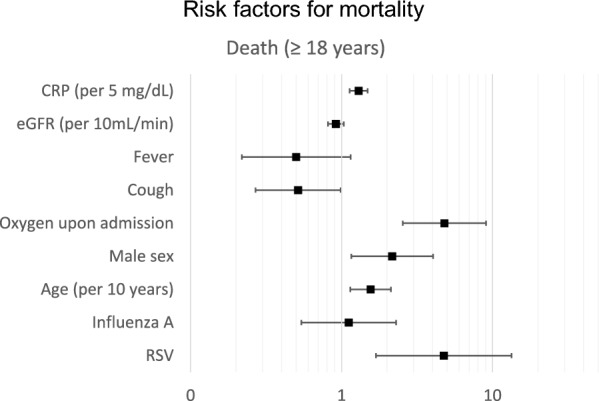
Results of multiple logistic regression analysis addressing potential risk factors for in-hospital death in patients of age ≥ 18 years. Regarding the comparison of the three infections, SARS-CoV-2 was taken as the reference. Odds ratios and 95% confidence intervals are shown. CRP, C-reactive protein, eGFR, glomerular filtration rate estimated from creatinine
Discussion
In the present study we compared the prevalence and clinical characteristics of patients hospitalized in the season 2023/24 due to infection with either SARS-CoV-2 or Influenza or RSV. This analysis comprised patients of all ages from internal, neurological and pediatric wards. The distribution of infection types across ages was similar to that observed in the same setting in 2022/23, with about 53% SARS-CoV-2, 23% Influenza A and 22% RSV as single infections, the remainder attributable to rare combined infections. Clinical characteristics of patients were also similar to those observed in 2022/23 [15], and the need for oxygen supply or NIV was again highest with RSV infection [15] in both, adults and children. However, in contrast to 2022/23, the proportion of adult patients requiring oxygen upon admission was highest with Influenza A infections not with RSV as previously.
In order to monitor the onset of the season of infections, we started data collection 2 months earlier than in the 2022/23 season [15]. This did not affect the numbers of Influenza A and RSV infections, since these occured only from November 2023 on, i.e. later than in 2022/23. Prior to November 2023, only SARS-CoV-2 was found. This was the reason why in total SARS-CoV-2 appeared slightly more prevalent than in the previous analysis [15]; when limiting the data collection to the same period of time (October to February), proportions between the numbers of infections were very similar to those of 2022/23. Conversely, when taking the longer period of data collection starting in August 2023 as a basis, the proportion of RSV in adults had slightly decreased. However, with respect to data provided by the Robert-Koch-Institute [19], the stop of recording at the end of February 2024 may have led to a slight underestimation of the prevalences of Influenza A and RSV regarding the total season 2023/24.
Nevertheless, compared to 2022/23 the relative risk for ICU admission as well as that for mortality from RSV had increased, although the absolute numbers were still markedly lower than that of SARS-CoV-2. RSV infection was associated with 4.7-fold increased risk of death compared to SARS-CoV-2 even when taking into account a number of confounders; Influenza A did not differ from SARS-CoV-2. This was confirmed in younger patients, since RSV also appeared as the most problematic and frequent infection, similar to 2022/23 [15]. These observations are in line with the findings by Ciofi et al., who monitored children with acute respiratory infections in an Italian hospital over the time period of 2018 to 2023 [2].
All analyses were performed in a similar manner as in our previous study covering the season 2022/23 [15]. The only difference was that the observation started two months earlier but a separate analysis (Supplemental Table S2) showed that with omission of these two months even increased the similarity of findings. An additional advantage was that data was retrieved from the same hospital which served the same population in the same area, had the same medical personnel and used the same criteria for diagnosis and treatment as before. This ensured a high degree of comparability between the results. When identifying risk factors, it turned out that the presence of oxygen supply upon admission was associated with a highly increased likelihood of ICU admission as well as death just as previously. The following discussion will perform comparisons with the frequencies and patterns observed in the previous season.
The distribution of infections over age was similar to that of 2022/23, with a bimodal pattern showing high numbers in patients of age much less than 18 years as well as in older patients and a peak at about 80 years. The peak in the young patients occurred at very low ages, similar to [2, 4, 15, 17], while there were only few patients between 18 and 50 years of age. Considering the time course of infection from August 2023 to February 2024, it appeared that in both younger and older patients RSV occurred later compared to 2022/23 [15], as it was present only from November 2023 onwards. Similarly, Influenza A in adults occurred later. Regarding infections with SARS-CoV-2, the contribution was about 50% and similar to that in the previous year. In the early phase of the observation period, SARS-CoV-2 was the only contributor. Regarding the relative numbers of infections, there was a slight but not statistically significant increase in SARS-CoV-2 from 48 to 53% and a slight decrease in RSV from 28 to 22%, whereas the relative frequency of Influenza A only very slightly increased from 22 to 23%. The percentages came even closer to the 2022/23 results, if August and September 2023 data was omitted from the analysis.
In adults, ICU admission was most often for RSV (28.6%), like in the season 2022/23 (19.2%). Also, mortality with SARS-CoV-2 and Influenza A was similar as in 2022/23 (9.0% and 6.8% vs. 8.8% and 8.6%) but mortality with RSV was much higher (11.1% vs. 20.0%), this is in contrast to the findings of Hamilton et al., which observed the highest mortality for SARS-CoV-2 in a large study with over 70,000 patients [17]. The overall result was that due to the same risk for ICU admission and death for SARS-CoV-2 and Influenza A, the pattern for these two infections remained stable over time. In contrast, the reduction in the relative frequency of RSV was partially compensated by the higher risk for ICU admission and death [8]. Taken together, these observations suggest that the pattern of infections leading to hospital admissions had reached a fairly stable state since 2022/23 and that at the same time RSV in adults still posed the relatively highest risk for adverse outcomes.
Although the characteristics of RSV patients were only gradually different from those of the other two infections, the importance of these differences became relevant in the multivariable analysis of mortality risk. Compared to the unadjusted data in Table 3 that showed increased mortality for RSV but without statistical significance between infections, multivariable analysis as shown in Fig. 3 demonstrated that the risk of death from RSV became statistically significant when simultaneously considering a variety of cofactors such as the presence of oxygen upon admission, age, male sex and the level of CRP. When taking itno account these confounders, the risk was elevated by a factor of more than 4 compared to SARS-CoV-2, while for Influenza A the risk remained essentially the same as for SARS-CoV-2. This suggests that the pattern of patient characteristics was relevant in order to identify specific risks from RSV infection. A stratification of mortality according to the age groups 18–59, 60–74 and 75 + years revealed that the risk was similar for SARS-CoV-2 and Influenza A in all groups, and elevated for RSV (data not shown). Although case numbers were very low, in the group 18–59 years the exact test according to Fisher-Freeman-Halton indicated even an increase of mortality from about 2% for SARS-CoV-2 and Influenza A to 22% with RSV. Whether these observations have implications for the identification of groups that may particularly benefit from RSV vaccination, remains to be studied.
Regarding ICU admission, the pattern of odds ratios was similar to that for death and RSV still showed at least a tendency for increased ICU admission, although this was not statistically significant. Considering that fact that the risk of death increased and that for ICU admission decreased with age, age might have played a role for the fact that RSV was not significant regarding ICU admissions even in multiple regression analyses. A study from Ambrosch et al. showed similar results, they observed patients with SARS-CoV-2, RSV or Influenza A/B in the period from 2017 to 2020. They found, that the risk for ICU admission and in-hospital mortality for RSV was higher than for Influenza A, but lower than the risks with SARS-CoV-2 infection [18].
Regarding the pattern of symptoms, RSV showed the highest relative frequency of dyspnoea and cough compared to the other two infections, just as in 2022/23 [15] and in the findings of Ambrosch et al. [18]. This is also in line with the results obtained by Surie and coworkers, showing that the percentage of self-reported dyspnoea was also highest in patients with RSV and reached about 80% [8]. In contrast, we found fever to be most frequent with SARS-CoV-2, and not with Influenza A as in 2022/23. Whether this reflected a difference in patient characteristics or a change in virus characteristics, cannot be decided from our data.
With respect to comorbidities, the observation that heart failure and asthma were most prevalent for RSV was similar to that of 2022/23. Regarding a state of immunosuppression, Influenza A instead of RSV showed the highest prevalence, while regarding dementia, this was least prevalent with Influenza A. Overall, there appeared to be no major changes in the pattern of comorbidities, although their number was higher in SARS-CoV-2 compared to the previous season.
We included patients of all ages, and for those under the age of 18 years there are a number of pediatric papers [1–4]. Just as in 2022/23, none of the younger patients died, but there were still ICU admissions, and these were most frequent for RSV, although numbers appeared to be lower than in 2022/23. The need for low-flow or high-flow oxygen supply was much higher in young patients with RSV compared to SARS-CoV-2 [1] and Influenza A, and in addition oxygen upon admission was most frequent in RSV. Essentially the same was true when restricting the analysis to children of age less than 3 years.
As in the previous analysis, we included laboratory parameters, blood gases and vital parameters into our analysis. There were, however, no apparent major differences compared to the season 2022/23 and no obvious clinical traits that could be linked to these parameters [18]. These parameters also turned out to be non-informative when included as additional predictors in multiple logistic regression analyses of ICU admission and death together with the set of predictors shown in Figs. 2 and 3, except for CRP.
This analysis has a number of limitations. First, this was a monocentric study, limiting its generalization, however, data of a large recently published cohort study comprising 7998 adults from 25 hospitals in 20 US states from February 1st, 2022, to May 31th, 2023, showed very similar results [8]. In this analysis rates of mechanical invasive ventilations or death were significantly higher in patients with RSV compared to SARS-CoV-2 or Influenza infection. An important aspect is that comparisons between studies can be affected by differences in the time periods analyzed. For example, our analysis may have missed cases particularly of Influenza in adults and of RSV in children in March or April 2024 (see Supplemental Fig. S1). Secondly, we had no information on vaccination status which might have been of interest, as Surie and coworkers reported that RSV infection was significantly worse when compared specifically with vaccinated COVID-19 or influenza patients [8]. Thirdly, our study was a retrospective analysis of available data, and it is possible that (electronic) patient records were not complete; this partially referred to BMI and symptoms upon admission. Symptoms were not recorded for children, as they could not reliably express them due to their young age. It was also not possible to collect this information retrospectively. Furthermore, in most cases no blood samples were taken in children, thus there were also no blood biomarkers available. Fourthly, diagnoses were taken from the discharge letter based on ICD-10 coding, and we cannot exclude the possibility that they had not been correctly coded. It also should be noted that the observed outcomes were the combined result of the hazard from each of the infections per se, the individual presence of risk factors, and the effectiveness of pharmacological and non-pharmacological treatment which differs between infections.
Conclusion
Data from a large population of patients (adults and children) admitted to a primary care hospital due to SARS-CoV-2, Influenza A or RSV infection showed, that in the season 2023/24 the relative contributions of these infections had remained similar to those of 2022/23. About 53% of patients had SARS-CoV-2, 23% Influenza A and 22% RSV, with a very low proportion of coinfections. Clinical outcomes were similar for SARS-CoV-2 and Influenza, while RSV showed higher relative rates of ICU admission and death, and these were even elevated compared to 2022/23. These findings underline that especially in adults, RSV infection poses a significant clinical risk compared to other common respiratory infections including SARS-CoV-2, despite much lower prevalence. Whether this should have implications regarding vaccination remains to be clarified.
Supplementary Information
Acknowledgements
We would like to thank the administration of the RoMed Hospital for their support in data collection from the files.
Author contributions
LW: Writing and revision of the manuscript, data collection, quality control and analysis; CF: Writing and revision of the manuscript, data analysis; RAJ: Writing and revision of the manuscript, data analysis; SE: Revision of the manuscript, support in data acquisition; PA: Revision of the manuscript, interpretation of the data; KK: Revision of the manuscript, interpretation of the data; SB: Writing and revision of the manuscript, design of the study, interpretation of the data.
Funding
None.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Approval was obtained from the ethics committee of the University Hospital of Regensburg (Number 23-3527-104).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Brigadoi G, Demarin GC, Boracchini R, Pierantoni L, Rossin S, Barbieri E, et al. Comparison between the viral illness caused by SARS-CoV-2, Influenza virus, respiratory syncytial virus and other respiratory viruses in pediatrics. Viruses. 2024;16(2):199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ciofi Degli Atti ML, Beccia F, D’Amore C, Ravà L, Bernaschi P, Russo C, et al. Impact of SARS-CoV-2 pandemic on emergency hospitalizations for acute respiratory infections: the experience of a paediatric tertiary care hospital in Italy. Influenza Other Respir Viruses. 2024;18(6):13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kandeel A, Fahim M, Deghedy O, Roshdy WH, Khalifa MK, Shesheny RE, et al. Resurgence of influenza and respiratory syncytial virus in Egypt following two years of decline during the COVID-19 pandemic: outpatient clinic survey of infants and children, October 2022. BMC Public Health. 2023;23(1):1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perez A, Lively JY, Curns A, Weinberg GA, Halasa NB, Staat MA, New Vaccine Surveillance Network Collaborators, et al. Respiratory virus surveillance among children with acute respiratory illnesses—new vaccine surveillance network, United States, 2016–2021. MMWR Morb Mortal Wkly Rep. 2022;71(40):1253–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi T, McLean K, Campbell H, Nair H. Aetiological role of common respiratory viruses in acute lower respiratory infections in children under five years: a systematic review and meta-analysis. J Glob Health. 2015;5(1): 010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Terliesner N, Unterwalder N, Edelmann A, Corman V, Knaust A, Rosenfeld L, et al. Viral infections in hospitalized children in Germany during the COVID-19 pandemic: association with non-pharmaceutical interventions. Front Pediatr. 2022;11(10): 935483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ackerson B, Tseng HF, Sy LS, Solano Z, Slezak J, Luo Y, et al. Severe morbidity and mortality associated with respiratory syncytial virus versus Influenza infection in hospitalized older adults. Clin Infect Dis. 2019;69(2):197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Surie D, Yuengling KA, DeCuir J, Zhu Y, Lauring AS, Gaglani M, et al. Severity of Respiratory syncytial virus vs COVID-19 and influenza among hospitalized US adults. JAMA Netw Open. 2024;7(40): e244954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352(17):1749–59. [DOI] [PubMed] [Google Scholar]
- 10.Wu X, Wang Q, Wang M, Su X, Xing Z, Zhang W, et al. Incidence of respiratory viral infections detected by PCR and real-time PCR in adult patients with community-acquired pneumonia: a meta-analysis. Respiration. 2015;89(4):343–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stamm P, Sagoschen I, Weise K, Plachter B, Münzel T, Gori T, et al. Influenza and RSV incidence during COVID-19 pandemic-an observational study from in-hospital point-of-care testing. Med Microbiol Immunol. 2021;210(5–6):277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Groves HE, Piché-Renaud PP, Peci A, Farrar DS, Buckrell S, Bancej C, et al. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: a population-based study. Lancet Reg Health Am. 2021;1: 100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buda S, Dürrwald R, Biere B, Buchholz U, Tolksdorf K, Schilling J et al. ARE-Wochenbericht KW 52–53/2020.
- 14.Diniz LM, Dias CS, Oliveira MCL, Simões E Silva AC, Colosimo EA, Mak RH, et al. Outcomes of SARS-CoV-2 and seasonal viruses among 2 million adults hospitalized for severe acute respiratory infection during the COVID-19 pandemic in Brazil. J Infect Dis. 2024. 10.1093/infdis/jiae295. [DOI] [PubMed] [Google Scholar]
- 15.Quarg C, Jörres RA, Engelhardt S, Alter P, Budweiser S. Characteristics and outcomes of patients hospitalized for infection with influenza, SARS-CoV-2 or respiratory syncytial virus in the season 2022/2023 in a large German primary care centre. Eur J Med Res. 2023;28(1):568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heiland LM, Jörres R, Engelhardt S, Alter P, Kahnert K, Deerberg-Wittram J, et al. Retrospective clinical-causal evaluation of a positive PCR for SARS-CoV-2 in hospitalised patients across the age spectrum in a primary care hospital. Pneumologie. 2024;78(2):100–6 (German). [DOI] [PubMed] [Google Scholar]
- 17.Hamilton MA, Liu Y, Calzavara A, Sundaram ME, Djebli M, Darvin D, et al. Predictors of all-cause mortality among patients hospitalized with influenza, respiratory syncytial virus, or SARS-CoV-2. Influenza Other Respir Viruses. 2022;16(6):1072–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ambrosch A, Luber D, Klawonn F, Kabesch M. Focusing on severe infections with the respiratory syncytial virus (RSV) in adults: risk factors, symptomatology and clinical course compared to influenza A/B and the original SARS-CoV-2 strain. J Clin Virol. 2023;161: 105399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buda S, Dürrwald R, Biere B, Reiche J, Buchholz U, Tolksdorf K et al. ARE-Wochenbericht KW 29/2024.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.


