Cancer is a lonely illness. For many patients cancer related isolation is relieved by internet based support groups and educational resources. However in the quest to relieve the vulnerability of isolation, the source credibility of what they encounter in internet searches emerges, paradoxically, as an additional vulnerability for them. Consequently as clinicians, the article by Zenone and colleagues [1] featured in the current version of this journal resonated with us, when it was submitted for publication. The authors reviewed the Google listing and Google reviews of 47 prominent alternative cancer clinics in August 2022. They noted that Google rarely declared that these clinics were alternative, and that the clinic approval ratings were high with median scores of 4.5 on a 5 point scale. The clinics were presented as locations to improve or cure cancer in 288 reviews. While reviews also noted concerns about financial exploitation (n = 98), poorer outcomes (72), provision of poor care (n = 41) and misrepresentation of outcome (n = 23) these were counterbalanced by the positive reviews. In our practice, we see patients abandoning potentially curative cancer therapy [e.g., [2]] and forgoing evidence based therapies for these alternative cancer clinics. We have previously documented crowdfunding and other strategies to enable this alternative care to be provided [3]. An additional concern related to these findings are the lack of guard rails for vulnerable patients such as those with intellectual disability or cognitive impairment due to cancer or otherwise. Such groups assume source credibility in the results of their internet searches. Coercion from “loved ones” is a compounding dynamic that we have also encountered.
The results of the present study build on a prior evaluation by the same authors of the advertising patterns of alternative cancer treatments during December 2021 on Meta social media platforms [4]. In this analysis, 25.8% of paid advertisements included direct statements claiming that provider treatment can cure cancer or prolong life. These statements were reinforced by the use of imagery and text content that emulated evidence-based medical providers. The report noted that prior Meta advertisements had disseminated scientifically unsupported public health messages such as anti-vaccine [5] and pro-tobacco content [6]. It noted reports by patients with cancer that they had started to see advertisements for fake cancer cures after their diagnosis [7, 8]. Both studies demonstrate that analogous to the tobacco, firearm and alcoholic beverages industries there is a conflict of interest between such internet platforms and social determinants of public health [9–12].
Both reports have focused on the role of platform providers in the ecosystem of alternative medicine provision. They are published in the backdrop of rising complementary and alternative medicine use globally [13–17] with up to 87% of patients using at least one form of complementary therapy during their cancer treatment. Such use can occur even if it conflicts with medical advice [e.g., [18]] and is present in the context of a lack of engagement by health care professionals on alternative therapy use by their patients [19]. These patients are also vulnerable to the harms of lost financial resources due to in-effective treatments, negative side effects and potential drug interactions from some alternative interventions, encouragement to forego palliative care, and lost and exploited hope. The increasing use of these therapies can be viewed as reflecting the weaknesses of conventional cancer care. The side effects of conventional anti-cancer therapy, and the patriarchal structure of conventional medicine as examples of such weaknesses [20]. In this regard a wider aspect of these reports is the role of medical mistrust in facilitating patient engagement with alternative medicines. Medical mistrust centres on the belief that health care providers, the pharmaceutical industry, academic institutions, or the government as a steward of public health are acting against ones best interests or wellbeing [21].
The prevalence of medical mistrust was highlighted in vaccine hesitancy rates during the COVID-19 pandemic [22, 23]. It can range from scepticism to belief in conspiracy theories [24]. In cancer care, conspiracy theories are evident both online and off. In 2014 a survey of the American public reported that 37% believed that the Food and Drug Administration intentional suppressed natural cures for cancer at the behest of the pharmaceutical industry [25, 26]. “Big Pharma” is a constant refrain underlying much cancer information [27]. Such refrains are reinforced by the egregious behaviour of companies such as Purdue Pharma and it is associated, medically qualified Sackler family members [28, 29]. The entanglement of the medical community with the pharmaceutical industry compounds this perception [30]. The consequence of this ecosystem of conspiracy theories is significant for patients, including ones we have encountered in our clinical practice (Fig. 1).
Fig. 1.
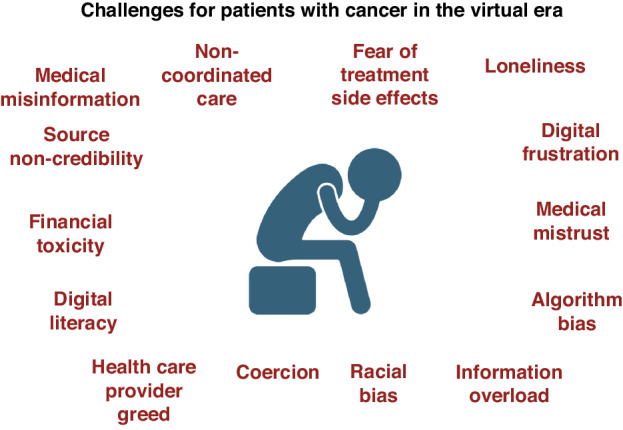
Challenges for Patients with Cancer in the Virtual Era.
Patients who subscribe to alternative therapies are twice as likely to die in the same period as those who rely on conventional therapies either due to delays in treatment or rejection of conventional therapy [31].
What are the implications of Zenone and colleagues paper to our clinical practice today? In the first instance, we need to be cognisant of the growing scale of misinformation that is present for patients and their families. Articles such as this paper can support awareness and dissemination. Moreover, increased professional engagement and discussion is required. Studies cited in this editorial demonstrate the significant prevalence of complementary and alternative therapy use in our community. A call to action is needed to scrutinise the current growth and the systems used to promote them which includes social media, podcasts in addition to organisational websites.
The issues raised by Zenone and colleagues [1, 4] and others [25] require statutory intervention to protect patients and their families, and ensure source credibility in their internet interactions. This should include consequences for service providers. We are cognisant of the fact that search engine providers can’t exclude all misinformation but integrating better signposting to reputable sources of information could be a first step in addressing this issue. Solutions could include a global agreement of information verification indicators (analogous to the X/twitter blue tick), artificial intelligence recognition of the need for caution with website claims, and expert validated Google reviews.
In our professional lifetimes we have witnessed the positive impact of the internet on cancer care. For millions of healthcare providers it is their “go to” source for treatment planning for patients. For patients and their families it is an essential repository for access to information, access to charitable support services, access to clinical research options and access to patient communities who have invaluable, shared, lived experiences. Ensuring that the internet remains a trusted resource for ALL is in everyone’s interest, including those who profit from it.
Author contributions
All authors contributed to the main manuscript text. All authors have approved the manuscript. SOR prepared Figure 1 using Biorender under export licence awarded to SOR.
Funding
Cancer Research @ UCC receives grant funding from the Health Research Board.
Competing interests
SO’R is a member of the editorial board of BJC Reports.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Artificial Intelligence Statement: Generative artificial intelligence was not used in the production of this manuscript.
Change history
10/31/2024
In this article the ORCID have been added to the authors.
References
- 1.Zenone M, Snyder J, van Schalkwyk M, Bélisle-Pipon JC, Hartwell G, Caulfield T, et al. Alternative cancer clinics’ use of Google listings and reviews to mislead potential patients. BJC Rep. 2024;2. 10.1038/s44276-024-00071-9 [DOI] [PMC free article] [PubMed]
- 2.Mc Sweeney LJ, Mc Eneaney P, O’Reilly S. Cannabis versus combination chemotherapy; n=1 trial in Hodgkin’s Lymphoma. Ir J Med Sci. 2019;188:1085–6. 10.1007/s11845-018-1914-y [DOI] [PubMed] [Google Scholar]
- 3.Iqbal S, Collins DC. Crowdfunding for anticancer therapies: an analysis of non-US GoFundMe pages. Ir J Med Sci. 2021;190:1355–61. 10.1007/s1845-020-02449-3 [DOI] [PubMed] [Google Scholar]
- 4.Zenone M, Snyder J, Belisle-Pipon JC, Caufield T, Schalkwyk M, van Maan N. Advertising alternative cancer treatments and approaches on meta social media platforms: content analysis. JMIR Infodemiol. 2023;3:e43548. 10.2196/43548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jamison AM, Broniatowski DA, Dredze M, Wood-Doughty Z, Kahn DA, Quinn SC. Vaccine-related advertisement in the Facebook Ad Archive. Vaccine. 2020;38:512–20. 10.1016/j.vaccine.2019.10.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Majmundar A, Moran M. For or against tobacco control: sponsored tobacco advocacy messages on Facebook and Instagram. Nicotine Tob Res. 2021;23:1861–8. 10.1093/ntr/ntab111 [DOI] [PubMed] [Google Scholar]
- 7.King A When hope kills: social media’s false promises to cancer patients. Healthy Debate 2021. https://healthydebate.ca/2021/08/topic/social-media-fake-cancer-treatment/
- 8.King A I have cancer. Now my Facebook feed is full of ‘alternative care’ ads. New York Times 2020. https://www.nytimes.com/20/07/10/opinion/facebook-cancer-ads.htm
- 9.De-Lacy-Vawdon C, Livingston C. Defining the commercial determinants of health: a systemic review. BMC Public Health. 2020;20:1022. 10.1186/s12889-020-09126-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zenone M, Kenworthy N, Maani N The social media industry as a commercial determinant of health. Int J Health Policy Manag 2022. 10.34172/ijhpm.2022.6840 [DOI] [PMC free article] [PubMed]
- 11.Donaldson SI, Dormanesh A, Perez C, Majmundar A, Allem J-P. Association between exposure to tobacco content on social media and tobacco use: a systemic review and meta-analysis. JAMA Pediatr. 2022;176:878–85. 10.1001/jamapediatrics.2022.2223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vertuno J Uvalde families sue Meta, Call of Duty maker on second anniversary of school massacre. May 25th 2024. www.huffpost.com (accessed 28/05/2024)
- 13.Liu L, Tang Y, Baxter GD, Yin H, Tumilty S. Complementary and alternative medicine –practice, attitudes, and knowledge among healthcare professional in New Zealand: an integrative review. BMC Complementary Med Ther. 2021;21:63 10.1086/s12906-021-03235-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Youn BY, Ch J-W, Cho S, Jeong SM, Kim HJ, Ko SG. Perception, attitudes, knowledge of using complementary and alternative medicine for cancer patients among healthcare professionals: A mixed –methods systematic review. Cancer Med. 2023;12:19149–62. 10.1002/cam4.6499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kallman M, Bergstrom S, Carlsson T, Jaras J, Holgersson G, Nordberg JH, et al. Use of CAM among patients. BMC Complementary Med Ther. 2023;23:51. 10.1186/s12906-023-03876-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones E, Nissen L, McCarthy A, Steadman K, Windsor C. Exploring the use of complementary and alternative medicine in cancer patients. Integrative Cancer Ther. 2019;18:1–9. 10.1177/1534735419846986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu A, Wu Y, Natarajan V, Singh P, Cheema W, Hossain R, et al. Complementary and alternative medicine use in patients with cancer and immigration background. JCO Global Oncol. 2023;9:e2200303. 10.1200/GO.22.00303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Donovan E, Hennessy MA, O’Reilly S Dietary supplements beliefs and use patterns among Irish patients with early stage breast cancer. Ir J Med Sci 2024 10.1007/s11845-024-0376-8 [DOI] [PMC free article] [PubMed]
- 19.Sont OM, Rombouts MD, Crul M. Attitude of healthcare professionals toward the use of complementary and alternative medication during anti-cancer therapy. J Oncol Pharm Practice. 2024;30:628–35. 10.1177/107815522311798899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Snyder J, Zenone M, Caulfield T. Crowdfunding for complementary and alternative medicine: what are cancer patients seeking? PLOS One. 2021;15:e0242048 10.1371/journal.pone.0242048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med. 2019;45:79–85. 10.1080/08964289.2019.1619511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joseph AM, Fernandez V, Kritzman S, Eaddy I, Cook OM, Lambros S, et al. COVID-19 misinformation on social media: a scoping review. Cereus. 2022;14:e24601 10.7759/cereus.24601eCollection.2022Apr [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ojikutu BO, Bogart LM, Dong L. Mistrust, empowerment, and structural change: lessons we should be learning from COVID-19. Am J Public Health. 2022;112:401–4. 10.2105/AJPH.2021.306604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Douglas KM, Uscinski JE, Sutton RM, Cichocka A, Nefes T, Ang CS, et al. Understanding conspiracy theories. Polit Psychol. 2019;40:3–35. 10.1111/pops.12568 [Google Scholar]
- 25.Grimes DR. The struggle against cancer misinformation. Cancer Discov. 2022;12:26–30. 10.1158/2159-8290.CD-21-1468 [DOI] [PubMed] [Google Scholar]
- 26.Oliver JE, Wood T. Medical conspiracy theories and health behaviours in the United States. JAMA Intern Med. 2014;174:817–8. 10.1001/jamainternmed.2014.190 [DOI] [PubMed] [Google Scholar]
- 27.Blaskiewicz R. The big Pharma conspiracy theory. Med Writing. 2013;22:259–61. 10.1179/2047480613Z.000000000142 [Google Scholar]
- 28.Kolodny A. How FDA failures contributed to the opioid crisis. AMA J Ethics. 2020;22:E743–750. 10.1001/amajethics.2020.743 [DOI] [PubMed] [Google Scholar]
- 29.Radden Keefe, P. Empire of Pain: the secret history of the Sackler Dynasty. 2021. Doubeday New York. https://lccn.loc.gov/2021931473
- 30.Moynihan R, Albarquoni L, Nangla C, Dunn AG, Lexchin J, Bero L. Financial ties between leaders of influential US professional medical associations and industry: cross sectional study. BMJ. 2020;369:m1505 10.1136/bmj.m1505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson SB, Park HS, Gross CP, James BY. Complementary medicine, refusal of conventional cancer therapy, and survival among patients with curable cancers. JAMA Oncol. 2018;4:1375–81. 10.1001/jamaoncol.2018.2487 [DOI] [PMC free article] [PubMed] [Google Scholar]


