Abstract
Aim:
Determine the frequency with which computed tomography (CT) after out-of-hospital cardiac arrest (OHCA) identifies clinically important findings.
Methods:
We included non-traumatic OHCA patients treated at a single center from February 2019 to February 2021. Clinical practice was to obtain CT head in comatose patients. Additionally, CT of the cervical spine, chest, abdomen, and pelvis were obtained if clinically indicated. We identified CT imaging obtained within 24 hours of emergency department (ED) arrival and summarized radiology findings. We used descriptive statistics to summarize population characteristics and imaging results, report their frequencies and, post hoc, compared time from ED arrival to catheterization between patients who did and did not undergo CT.
Results:
We included 597 subjects, of which 491 (82.2%) had a CT obtained. Time to CT was 4.1 hours [2.8–5.7]. Most (n = 480, 80.4%) underwent CT head, of which 36 (7.5%) had intracranial hemorrhage and 161 (33.5%) had cerebral edema. Fewer subjects (230, 38.5%) underwent a cervical spine CT, and 4 (1.7%) had acute vertebral fractures. Most subjects (410, 68.7%) underwent a chest CT, and abdomen and pelvis CT (363, 60.8%). Chest CT abnormalities included rib or sternal fractures (227, 55.4%), pneumothorax (27, 6.6%), aspiration or pneumonia (309, 75.4%), mediastinal hematoma (18, 4.4%) and pulmonary embolism (6, 3.7%). Significant abdomen and pelvis findings were bowel ischemia (24, 6.6%) and solid organ laceration (7, 1.9%). Most subjects that had CT imaging deferred were awake and had shorter time to catheterization.
Conclusions:
CT identifies clinically important pathology after OHCA.
Keywords: Cardiac arrest, Heart arrest, Computed tomography, Injuries
Introduction
Emergency medical services respond to more than 347,000 adult out-of-hospital cardiac arrests (OHCA) annually.1 For patients who survive to Emergency Department admission, diagnostic testing can identify the etiology of arrest, trauma from chest compressions such as rib fractures or pneumothorax, and consequences of pulselessness including cerebral edema and bowel ischemia.2–6 Both etiology and sequelae of arrest can inform early management and predict overall prognosis for recovery.5,7–10 European Resuscitation Council guidelines for post-resuscitation care support obtaining a brain CT in comatose post-arrest patients,11 but no recommendations are made regarding other cross-sectional imaging.
A prospective, single-center cohort of patients resuscitated from OHCA found head-to-pelvis CT identified injuries associated with resuscitation in 81% of cases, with nearly 1 in 7 being time-critical findings requiring intervention.2 Other observational studies found that early CT after OHCA can expedite the diagnosis of potential causes of arrest and can affect clinical management.12,13 A limitation of prior work has been small sample sizes, limiting ability to estimate prevalence and clinical significance of less common radiographic findings. The aim of the current study is to describe the frequency of radiographic findings on post-resuscitation imaging for a large population of OHCA patients. We hypothesized that early cross-sectional imaging identifies clinically important pathology. As a post hoc comparison, we evaluated time to cardiac catheterization in patients that underwent cross-section imaging prior to catheterization or had imaging deferred.
Methods
Study population
The University of Pittsburgh Human Research Protection Office approved this retrospective, observational case-series (STUDY19020205). We identified consecutive patients with return of spontaneous circulation after OHCA or in emergency department (ED) arrest treated at our academic medical center from February 2019 to February 2021. We excluded patients <18 years of age, those who presented >24 hours after arrest, patients with a traumatic etiology of arrest, and patients who did not suffer a true cardiac arrest upon subsequent review of prehospital records. To describe our cohort, we abstracted patient demographics including age, sex, race, and ethnicity, arrest characteristics, etiology of arrest categorized as cardiac, respiratory, neurological, or other,7 Pittsburgh Cardiac Arrest Category, cardiac catheterization results when performed, survival to hospital discharge, and Cerebral Performance Category at hospital discharge from our prospective registry.14–16
CT acquisition and review
Our Post Cardiac Arrest Service (PCAS) evaluated patients on arrival to the ED and directed ongoing resuscitation and diagnostic workup. During the study period, our practice was to obtain non-contrast head CT in all patients with coma, and consider CT of the cervical spine, chest with pulmonary angiogram, and abdomen and pelvis based on clinical situation. We did not acquire coronary or intra-arrest CT in this patient population. We used a GE lightspeed VCT 64 channel scanner (128 KVP and 225 mA) during the study period.
Four co-investigators reviewed radiology interpretations of both contrasted and unenhanced CT imaging for each patient. We extracted acute findings from reports of images obtained within the first 24 hours of arrival after OHCA. When multiple images of the same region were obtained within 24 hours, we only considered the images obtained most proximate to arrest. We defined time to CT as date and time listed on the first image Digital Imaging and Communications in Medicine subtracted by date and time of cardiac arrest. Given our center receives a high volume of interfacility transfers and potential for transfer delay or distance influencing time from arrest to catheterization, we defined time to catheterization as time the patient was received by the catheterization laboratory subtracted by time of arrival to our facility or, in case of arrest in our ED rather than transfers, time of arrest. We did not abstract reports from facilities outside our health system. We defined radiographic findings a priori based upon group consensus for this study listed in Supplemental Table 1. To determine if there were common features associated with cervical spine injury, we separately reviewed all medical records, arrest characteristics, and circumstances around collapse for cases where acute cervical fractures were identified.
Table 1 -.
Cohort Characteristics.
| Characteristic (n%) | All (n = 597) |
|---|---|
|
| |
| Mean age in years (SD) | 60.0 (15.5) |
| Female sex | 232 (38.9%) |
| Race | |
| - American Indian/Alaskan Native | 5 (0.8%) |
| - Asian | 5. (0.8%) |
| - Black/African American | 75 (12.5%) |
| - White | 431 (72.2%) |
| - Unknown | 80 (13.4%) |
| - Other | 1 (0.1%) |
| Ethnicity | |
| - Hispanic/Latino | 2 (0.3%) |
| - Non-Hispanic/Latino | 493 (82.6%) |
| - Unknown | 102 (17.1%) |
| Witnessed status | |
| - EMS | 96 (16.1%) |
| - Bystander | 255 (42.7%) |
| - Unwitnessed | 139 (23.3%) |
| - ED arrest | 107 (17.9%) |
| Initial rhythm | |
| - VF/pVT | 185 (31.0%) |
| - PEA | 188 (31.5%) |
| - Asystole | 179 (30.0%) |
| - Unknown | 45 (7.5%) |
| Median CPR duration in min [IQR] | 20 [11 – 35] |
| Median defibrillator shocks [IQR] | 0 [0 – 2] |
| Median epinephrine doses [IQR] | 3 [1–5] |
| Pittsburgh Cardiac Arrest Category | |
| - I | 97 (16.3%) |
| - II | 112 (18.8%) |
| - III | 49 (8.2%) |
| - IV | 291 (48.7%) |
| - Unknown | 48 (8.0%) |
| Arrest etiology | |
| - Cardiac | 193 (32.3%) |
| - Respiratory | 110 (18.4%) |
| - Neurologic | 23 (3.9%) |
| - Other | 271 (45.4%) |
| Interfacility transfer | 372 (62.3%) |
| Any cross-sectional imaging obtained | 491 (82.2%) |
| Median hours from arrest to CT [IQR] | 4.1 [2.8 – 5.7] |
| Cardiac catheterization | 112 (18.8) |
| Survived to hospital admission | 570 (95.5%) |
| Survival to hospital discharge | 193 (32.3%) |
| Cerebral performance category | |
| - 1 | 43 (7.2%) |
| - 2 | 49 (8.5%) |
| - 3 | 86 (14.4%) |
| - 4 | 13 (2.2%) |
| - 5 | 404 (67.7%) |
CT- computed tomography; PEA- pulseless electrical activity; VF/pVT- ventricular fibrillation/pulseless ventricular tachycardia.
Statistical analysis
We report mean with standard deviation (SD) and median with interquartile range [IQR] for continuous variables as appropriate. We report number, with corresponding percentages, and calculated 95% confidence intervals (CI) for each radiographic finding. The frequency of findings was defined by the number of patients with a finding among patients who had imaging of that body region. For diagnoses that require contrast, we report frequency among patients that had contrasted imaging. We report survival rate for each radiographic finding encountered. Finally, post hoc, we compared time to cardiac catheterization between subjects that underwent CT imaging prior to catheterization and those who did not using Wilcoxon rank sum test. We performed all analyses in STATA Version 17 (College Station, Texas, USA).
Results
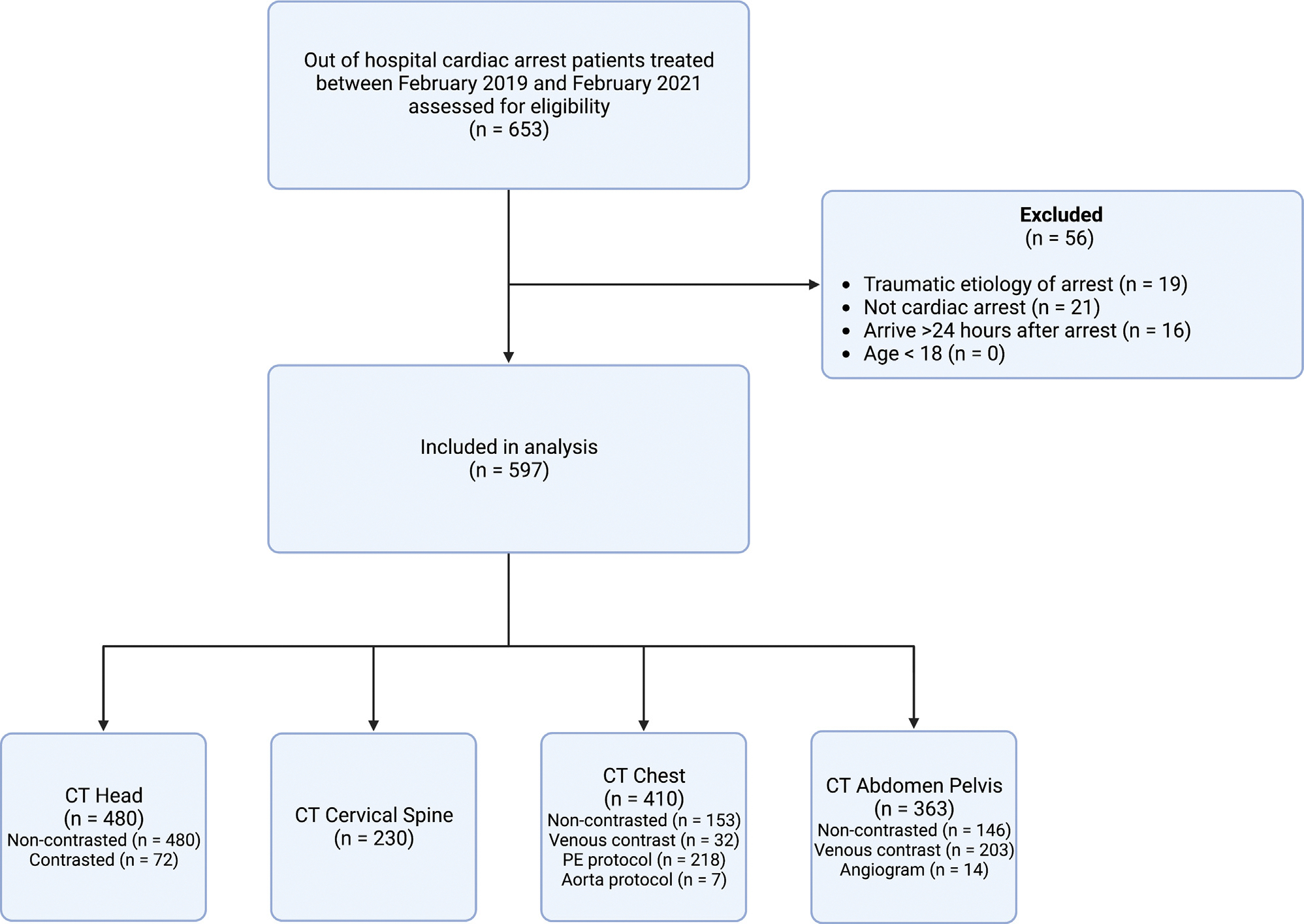
A total of 653 OHCA patients were treated at our facility during the study period, of whom 56 met exclusion criteria (Fig. 1), leaving 597 for analysis. Mean age was 60 years (SD 15.5) and 185 (31.0%) had an initial shockable rhythm (Table 1). Median CPR duration was 20 [IQR 11–35] minutes and 500 (83.8%) subjects were comatose on presentation. A minority of patients (PCAC I n = 97, 16.6%) were awake on arrival. Most subjects (n = 570, 95.5%) survived to hospital admission and had at least one CT obtained (n = 497, 82.2%). Median time to CT imaging was 4.1 hours [2.7 – 5.7] after cardiac arrest.
Fig. 1 – Study inclusion.
Intracranial hemorrhage (36, 7.5% [95%CI 5.3–10.2%]) and cerebral edema (161, 33.5% [95%CI 29.3–37.9%]) were common findings among subjects who underwent brain imaging (n = 480, 80.4%) (Table 2). Six of the identified intracranial hemorrhages were thought to be due to trauma (i.e., collapse) unrelated to etiology of arrest. Of those who had intracranial hemorrhage, 4 (11.1%) survived to hospital discharge and of those for whom a radiologist interpreted there to be cerebral edema, 6 (3.7%) survived to hospital discharge.
Table 2 -.
Computed tomography findings.
| Pathology | Number, denominator and % of imaged subjects with findings | 95% Confidence Interval | Number and % with finding that survived hospital discharge | 95% Confidence Interval |
|---|---|---|---|---|
|
| ||||
| CT Head | ||||
| Intracranial hemorrhage | 36/480 (7.5%) | (5.3 – 10.2%) | 4 (11.1%) | (3.1 – 26.1%) |
| Cerebral edema | 161/480 (33.5%) | (29.3 – 37.9%) | 6 (3.7%) | (1.4 – 7.9%) |
| Arterial thrombosis^ | 3/72 (4.2%) | (0.8 – 11.7%) | 1 (33.3%) | (0.8 – 90.5%) |
| Decreased intracranial contrast flow^ | 15/72 (20.8%) | (12.2 – 32.0%) | 0 (0.0%) | (0.0 – 21.8%) |
| CT Cervical Spine | ||||
| Vertebral fracture | 4/230 (1.7%) | (0.4 – 4.3%) | 0 (0.0%) | (0.0 – 60.2%) |
| CT Chest | ||||
| Rib/sternal fracture | 227/410 (55.3%) | (50.4 – 60.2%) | 59 (25.9%) | (20.4 – 32.2%) |
| Pneumothorax | 27/410 (6.6%) | (4.4% – 9.4%) | 6 (22.2%) | (8.6 – 42.2%) |
| Hemothorax | 9/410 (2.2%) | (1.0 – 4.1%) | 2 (22.2%) | (2.8 – 60.0%) |
| Pneumonia/aspiration | 309/410 (75.3%) | (70.9 – 79.5%) | 91 (29.4%) | (24.4 – 34.9%) |
| Pulmonary edema | 76/410 (18.5%) | (14.9 – 22.6%) | 17 (22.3%) | (13.6 – 33.3%) |
| Hemopericardium | 4/410 (0.9%) | (0.2 – 2.5%) | 1 (25.0%) | (0.6 – 80.6%) |
| Pericardial effusion | 13/410 (3.2%) | (1.7 – 5.4%) | 3 (23.1%) | (5.0 – 53.8%) |
| Mediastinal hematoma | 18/410 (4.4%) | (2.6 – 6.8%) | 3 (16.7%) | (3.6 – 41.4%) |
| Pulmonary infarct | 4/410 (0.9%) | (0.2 – 2.5%) | 1 (25.0%) | (0.6 – 80.9%) |
| Endotracheal tube displacement | 23/410 (5.6%) | (3.6 – 8.3%) | 3 (13.0%) | (2.8 – 33.6%) |
| Pulmonary Embolism* | 6/218 (3.7%) | (1.0 – 5.9%)* | 0 (0.0%) | (0.0 – 45.9%) |
| Aortic dissection& | 1/221 (0.5%) | (0.1 – 2.5%) | 0 (0.0%) | (0.0 – 97.5%) |
| CT Abdomen and Pelvis | ||||
| Hemoperitoneum | 4/363 (1.1%) | (0.3 – 2.8%) | 1 (25.0%) | (0.6 – 80.6%) |
| Pneumoperitoneum | 1/363 (0.2%) | (0.0 – 1.5%) | 1 (100%) | (2.5 – 100%) |
| Retroperitoneal hematoma | 5/363 (1.4%) | (0.4 – 3.2%) | 1 (20.0%) | (0.5 – 71.6%) |
| Solid organ injury (liver, spleen) | 7/363 (1.9%) | (0.8 – 3.9%) | 3 (42.9%) | (0.9 – 81.6%) |
| Bowel ischemia | 24/363 (6.6%) | (4.3 – 9.7%) | 0 (0.0%) | (0.0 – 14.2%) |
| Bowel obstruction | 6/363 (1.7%) | (0.7 – 3.5%) | 3 (50.0%) | (11.8 – 88.1%) |
| Pancreatitis | 9/363 (2.5%) | (1.1 – 4.7%) | 2 (22.2%) | (2.8 – 60.0%) |
| UTI (Pyleonephritis/cystitis) | 12/363 (3.3%) | (1.7 – 5.7%) | 5 (41.7%) | (15.1 – 72.3%) |
% of CTA head studies obtained;
% of CTA Chest PE protocol studies obtained;
% of contrasted CT chest studies obtained.
Among subjects who had cervical spine CT imaging (n = 230, 38.5%), 4 (1.7% [95%CI 0.4–4.3%]) had vertebral fractures. None of the 4 patients with cervical fractures survived to hospital discharge. Details of these patients are in Table 3.
Table 3 -.
Clinical scenario and arrest characteristics of subjects found to have cervical spine injuries.
| Clinical Scenario | Arrest Details | CT Cervical Spine Findings |
|---|---|---|
|
| ||
| 73-year-old male found unresponsive in home bathroom after subject’s roommate heard a “thud.” Found in cardiac arrest by EMS. | Unwitnessed collapse, no bystander CPR, PEA initial rhythm, 4 milligrams epinephrine, no defibrillation, 37 minutes of CPR. | C4 superior endplate pathologic fracture with evidence of neoplasm/multiple myeloma. |
| 83-year-old male found unresponsive at his nursing facility noted by EMS to be in cardiac arrest. | Unwitnessed collapse, PEA initial rhythm, 13 milligrams epinephrine, no defibrillation, 67 minutes of CPR. | Questionable acute C3 and C4 vertebral body fractures. |
| 73-year-old female unwitnessed fall off of toilet. Transferred by EMS to ED. Has cardiac arrest in CT scanner. | ED arrest, PEA initial rhythm, 3 milligrams epinephrine, no defibrillation, 11 minutes of CPR. | Acute fractures of C1 right posterior arch and C5 left posterior lamina. |
| 78-year-old male found unresponsive with inhaler in his hand. Found in cardiac arrest by EMS. | Unwitnessed collapse, no bystander CPR, asystole initial rhythm. Epinephrine dose, defibrillations, and CPR duration not reported. | Acute fracture C2 anterior inferior vertebral body. |
Thoracic pathologies identified on CTs of the chest (n = 410, 68.7% of subjects) included aspiration or possible pneumonia (309, 75.3% [95%CI 70.9–79.5%]), rib or sternal fractures (227, 55.3% [95%CI 50.4–60.2%]), and pulmonary edema (76, 18.5% [95%CI 14.9–22.6%]). Less frequent findings included pneumothorax (27, 6.6% [95%CI 4.4–9.4%), endotracheal tube malposition (23, 5.6% [95%CI 3.6–8.3%]), mediastinal hematoma (18, 4.4% [95%CI 2.6–6.8%]), pericardial effusion (13, 3.2% [95%CI 1.7–5.4%]), pulmonary embolism (6, 3.7% [95%CI 1–5.9%]), hemothorax (9, 2.2% [1.0–4.1%]), hemopericardium (4, 0.9% [95%CI 0.2–2.5%]), and aortic dissection (1, 0.5% [95%CI 0.1–2.5%]). Clinical outcomes varied with each pathology (Table 2).
For subjects who had a CT abdomen and pelvis performed (n = 363, 60.8%), identified pathologies included bowel ischemia (24, 6.6% [95%CI 4.3–9.7%]), possible urinary tract infection (12, 3.3% [95CI 1.7–5.7%]), pancreatitis (9, 2.5% [95%CI 1.1–4.7%]), and splenic or liver laceration (7, 1.9% [95%CI 0.8–3.9%]). Less frequent findings included retroperitoneal hematoma (5, 1.4% [95%CI 0.4–3.2%]), hemoperitoneum (4, 1.1% [95%CI 0.3–2.8%]), and pneumoperitoneum (1, 0.2% [95%CI 0.0–1.5%]). No patients with bowel ischemia survived to hospital discharge (Table 2).
A total of 112 subjects (18.8%) underwent a cardiac catheterization during the index hospitalization of which 29 (25.9%) had no imaging in the first 24 hours, 13 (11.6%) had imaging obtained after catheterization, and 70 (62.5%) had imaging prior to catheterization. Median time to catheterization from arrival to our facility overall was 2.9 hours [1.6 – 14.5]. Subjects with imaging obtained prior to catheterization were less often awake (imaged subjects PCAC I n = 11, 28.9%; not imaged subjects PCAC I n = 27, 71.1%) and had longer times to intervention (imaged subjects median 4.6 hours [1.9 – 18.2]; not imaged subjects median 1.9 hours [1.1 – 3.7], p value < 0.001).
Discussion
Clinically important pathology related to cardiac arrest and resuscitation are frequently present on cross-sectional CT imaging. Cerebral edema based on qualitative radiology interpretation was present in 1 in 3 patients in whom head CT was obtained. Prior studies report rates of cerebral edema between 16% and 30%,17,18 differences that may be due to timing of imaging and subjectivity on interpretation.19 Similar to our findings, intracranial hemorrhage is identified in 5% of patients resuscitated from OHCA.4 Thoracoabdominal findings included pathology such as rib fracture, pneumothorax, pulmonary embolism, liver/spleen injury, and bowel ischemia, all which inform post-arrest management. Subjects that had imaging obtained prior to cardiac catheterization had longer times to catheterization, though relatively few subjects underwent catheterization in our cohort. Moreover, most subjects that went direct to catheterization were awake. Decision making regarding catheterization in resuscitated cardiac arrest patients is complex and dependent on history, hemodynamic and electrical stability, and neurological considerations not fully captured in our data. Head to pelvis cross-sectional CT imaging may be considered not only to assess underlying etiology of arrest but also sequela of cardiopulmonary resuscitation. However, non-trivial risks of imaging such as delays to time critical interventions such as catheterization as well as radiation exposure are not addressed by this analysis but should be considered.20
Cervical spine injuries were identified on dedicated cervical imaging in patients who were found on the ground or who had a history suggesting a fall from a standing position. There are case reports describing similar encounters, but they have not been described in larger cohorts.21 Patients are often found on the ground in arrest, unknown if they fell from standing. Clinicians should have a high index of suspicion for possible cervical injury when history is clear that the patient fell from standing or circumstances pertaining to the arrest are unknown.
Chest wall injuries are common after resuscitation, require pain control, aggressive pulmonary hygiene, and are an important consideration for ventilator weaning and liberation. Rib fractures are a risk factor for pneumonia in the post-resuscitation period.22 Respiratory failure is a common etiology of OHCA, and providers note aspiration of gastric contents in over 30% of out of hospital resuscitation.7,6 Chest compressions alone can cause pulmonary consolidation and edema.23 Over 70% of chest images were interpreted as having aspiration and/or pneumonia. Chest imaging abnormalities are common, but agreement regarding underlying cause as aspiration, pneumonia, or contusion is poor.24 Chest x-ray or ultrasound can identify rib fractures and consolidations, though excluding diagnoses such as pulmonary embolism prior to intensive care unit admission may add value in patients with hemodynamic instability or deterioration.
Intra-abdominal findings such as solid organ injuries may require surgical control and affect decisions about anticoagulation or antiplatelet drugs. It is common for patients in the immediate post-arrest period to be comatose, pharmacologically sedated or paralyzed, making abdominal examination unreliable. Consistent with our data, a previous retrospective study found clinically unexpected intraabdominal injuries in many resuscitated OHCA patients.25 All patients with bowel ischemia in our cohort died. Radiographically apparent intestinal ischemia likely reflected prolonged arrest in these patients.
This study has several limitations. This is an analysis of observational data from a single high volume cardiac arrest center which limits generalizability of our results. While many subjects had CT imaging, there was variability of anatomical regions imaged and use of contrast. Pertinent history or physical exam findings that influence choice of imaging were not available in our data. Thus, our current analysis may overestimate the actual incidence of findings in OHCA patients. For example, the prevalence of cerebral edema in our cohort reflects our local imaging practice which overestimates edema when considering all resuscitated cardiac arrest patients but approximates prevalence in those with coma. Moreover, it is unclear if diagnoses such as ruptured intracranial aneurysm were clinically suspected by history that then prompted imaging. Cervical spine imaging was obtained in a minority of patients and prevalence of acute cervical spine fractures reflects prevalence in those with coma and collapsed during arrest or where circumstances surrounding arrest are unclear. Prospective studies of CT imaging protocols are needed to address these limitations.
Conclusions
Early cross-sectional imaging identifies clinically important findings in patients resuscitated from non-traumatic OHCA.
Supplementary Material
Acknowledgements
We acknowledge Valerie Arias MD, Joanna Fong-Isariyawongse MD, Mark Schmidhofer MD, and Amy K Wagner MD who provided care to patients during this study.
Figures were created using Biorender software.
Appendix A
The University of Pittsburgh Post-Cardiac Arrest Service Investigators are:
Niravkumar Barot MD, MPH
Clifton W Callaway MD, PhD
Joseph P Condle MIS
Patrick J Coppler PA-C
Joseph M Darby MD
Ankur A Doshi MD
Byron C Drumheller MD
Jonathan Elmer MD, MS
Katharyn L Flickinger PhD, MS
Adam N Frisch MD
Francis X Guyette MD, MS, MPH
Barinder S Hansra MD
A Murat Kaynar MD, MPH
Joseph Mettenburg MD, PhD
Masashi Okubo MD, MS
Cecelia Ratay DNP, CRNP
Zachary J Rhinehart MD
Kelly N Sawyer MD, MS
Kim Schatz DNP, CRNP
Sara Sprouse MSL
Alexis Steinberg MD, MS
Alexandra Weissman MD, MS, MPH
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
CRediT authorship contribution statement
Jonathan Tam: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Christopher Soufleris: Conceptualization, Data curation, Writing – review & editing. Cecelia Ratay: Writing – review & editing. Adam Frisch: Conceptualization, Methodology, Writing – review & editing. Jonathan Elmer: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Nicholas Case: Data curation, Writing – review & editing. Katharyn L Flickinger: Data curation, Writing – review & editing. Clifton Callaway: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. Patrick J Coppler: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing.
Appendix B. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resuscitation.2023.109898.
The members of the University of Pittsburgh Post-Cardiac Arrest Service Investigators are listed in Appendix A at the end of the article.
REFERENCES
- 1.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation 2023. [DOI] [PubMed] [Google Scholar]
- 2.Karatasakis A, Sarikaya B, Liu L, et al. Prevalence and Patterns of Resuscitation-Associated Injury Detected by Head-to-Pelvis Computed Tomography After Successful Out-of-Hospital Cardiac Arrest Resuscitation. J Am Heart Assoc 2022;11 e023949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esdaille CJ, Coppler PJ, Faro JW, et al. Duration and clinical features of cardiac arrest predict early severe cerebral edema. Resuscitation 2020;153:111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee KY, So WZ, Ho JSY, et al. Prevalence of intracranial hemorrhage amongst patients presenting with out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation 2022;176:136–49. [DOI] [PubMed] [Google Scholar]
- 5.Paul M, Bougouin W, Legriel S, et al. Frequency, risk factors, and outcomes of non-occlusive mesenteric ischaemia after cardiac arrest. Resuscitation 2020;157:211–8. [DOI] [PubMed] [Google Scholar]
- 6.Simons RW, Rea TD, Becker LJ, Eisenberg MS. The incidence and significance of emesis associated with out-of-hospital cardiac arrest. Resuscitation 2007;74:427–31. [DOI] [PubMed] [Google Scholar]
- 7.Chen N, Callaway CW, Guyette FX, et al. Arrest etiology among patients resuscitated from cardiac arrest. Resuscitation 2018;130:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Na MK, Kim W, Lim TH, et al. Gray matter to white matter ratio for predicting neurological outcomes in patients treated with target temperature management after cardiac arrest: a systematic review and meta-analysis. Resuscitation 2018;132:21–8. [DOI] [PubMed] [Google Scholar]
- 9.Prins JTH, Van Lieshout EMM, Van Wijck SFM, et al. Chest wall injuries due to cardiopulmonary resuscitation and the effect on inhospital outcomes in survivors of out-of-hospital cardiac arrest. J Trauma Acute Care Surg 2021;91:966–75. [DOI] [PubMed] [Google Scholar]
- 10.Hubner P, Meron G, Kürkciyan I, et al. Neurologic causes of cardiac arrest and outcomes. J Emerg Med 2014;47:660–7. [DOI] [PubMed] [Google Scholar]
- 11.Nolan JP, Sandroni C, Böttiger BW, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med 2021;47:369–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viniol S, Thomas RP, König AM, Betz S, Mahnken AH. Early whole-body CT for treatment guidance in patients with return of spontaneous circulation after cardiac arrest. Emerg Radiol 2020;27:23–9. [DOI] [PubMed] [Google Scholar]
- 13.Branch KRH, Strote J, Gunn M, et al. Early head-to-pelvis computed tomography in out-of-hospital circulatory arrest without obvious etiology. Acad Emerg Med 2021;28:394–403. [DOI] [PubMed] [Google Scholar]
- 14.Rittenberger JC, Guyette FX, Tisherman SA, DeVita MA, Alvarez RJ, Callaway CW. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation 2008;79:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coppler PJ, Elmer J, Calderon L, et al. Validation of the Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation 2015;89:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nassal MMJ, Nichols D, Demasi S, Rittenberger JC, Panchal AR, Kurz MC. External validation of Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation 2022;172:32–7. [DOI] [PubMed] [Google Scholar]
- 17.Adriaansens KO, Jewbali LSD, Lemkes JS, et al. Routine reporting of grey-white matter differentiation in early brain computed tomography in comatose patients after cardiac arrest: a substudy of the COACT trial. Resuscitation 2022;175:13–8. [DOI] [PubMed] [Google Scholar]
- 18.Fisher R, Bernett MJ, Paternoster R, Karabon P, Devlin W, Swor R. Utility of Abnormal Head Computed Tomography in Predicting Outcome in Out-of-Hospital Cardiac Arrest Victims. Ther Hypothermia Temp Manag 2021;11:164–9. [DOI] [PubMed] [Google Scholar]
- 19.Caraganis A, Mulder M, Kempainen RR, et al. Interobserver Variability in the Recognition of Hypoxic-Ischemic Brain Injury on Computed Tomography Soon After Out-of-Hospital Cardiac Arrest. Neurocrit Care 2020;33:414–21. [DOI] [PubMed] [Google Scholar]
- 20.Hui CM, MacGregor JH, Tien HC, Kortbeek JB. Radiation dose from initial trauma assessment and resuscitation: review of the literature. Can J Surg 2009;52:147–52. [PMC free article] [PubMed] [Google Scholar]
- 21.Mayà-Casalprim G, Ortiz J, Tercero A, et al. Cervical spinal cord injury by a low-impact trauma as an unnoticed cause of cardiorespiratory arrest. Eur Heart J Case Rep 2020;4:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawai Y, Takano K, Miyazaki K, et al. Association of multiple rib fractures with the frequency of pneumonia in the post-resuscitation period. Resusc Plus 2022;11 100267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magliocca A, Rezoagli E, Zani D, et al. Cardiopulmonary Resuscitation-associated Lung Edema (CRALE). A Translational Study. Am J Respir Crit Care Med 2021;203:447–57. [DOI] [PubMed] [Google Scholar]
- 24.Weissman A, Gozansky E, Andrews G, Rittenberger J, Callaway C. 143EMF Chest Radiograph Findings Suggestive of Pneumonia Following Cardiac Arrest. Ann Emerg Med 2018;72:S59–60. [Google Scholar]
- 25.Dunham GM, Perez-Girbes A, Bolster F, Sheehan K, Linnau KF. Use of whole body CT to detect patterns of CPR-related injuries after sudden cardiac arrest. Eur Radiol 2018;28:4122–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


