Abstract
Steatotic liver diseases (SLD) are the principal worldwide cause of cirrhosis and end-stage liver cancer, affecting nearly a quarter of the global population. SLD includes metabolic dysfunction-associated alcoholic liver disease (MetALD) and metabolic dysfunction-associated steatotic liver disease (MASLD), resulting in asymptomatic liver steatosis, fibrosis, cirrhosis and associated complications. The immune processes include gut dysbiosis, adiposeliver organ crosstalk, hepatocyte death and immune cell-mediated inflammatory processes. Notably, various immune cells such as B cells, plasma cells, dendritic cells, conventional CD4+ and CD8+ T cells, innate-like T cells, platelets, neutrophils and macrophages play vital roles in the development of MetALD and MASLD. Immunological modulations targeting hepatocyte death, inflammatory reactions and gut microbiome include N-acetylcysteine, selonsertib, F-652, prednisone, pentoxifylline, anakinra, JKB-121, HA35, obeticholic acid, probiotics, prebiotics, antibiotics and fecal microbiota transplantation. Understanding the immunological mechanisms underlying SLD is crucial for advancing clinical therapeutic strategies.
Keywords: Liver diseases, Immunity, Dysbiosis, Adipose tissue
INTRODUCTION
Excessive alcohol consumption and a high-calorie diet are two major etiologic factors for chronic steatotic liver disease (SLD), including metabolic dysfunction-associated alcoholic liver disease (MetALD) [1] and metabolic dysfunctionassociated steatotic liver disease (MASLD) [2]. Meanwhile, the development of MetALD and MASLD increases the burden of cirrhosis and liver cancer [3] and becomes leading causes of death worldwide [4]. It is imperative to thoroughly dissect the pathoph-ysiology of MetALD and MASLD in detail, which promotes the development of new therapeutic modalities and alleviates the socioeconomic burden associated with liver diseases [5].
The role of immunity in promoting inflammation and the progression of MetALD and MASLD has been demonstrated through continuous accumulation of clinical and experimental research [6]. In the development of MetALD and MASLD, the liver is not an isolated organ but rather undergoes complex interactions with other organs, such as adipose tissue and intestines, through blood circulation and immune cells. For example, alcohol, metabolites of ethanol, microbes and microbial metabolites damage the gastrointestinal tract and adipocytes, subsequently disrupting the immune system in MetALD [7]. Furthermore, the dysfunction of the immune system contributes to the formation of MASLD [2].
Importantly, abnormal aggregation of hepatic immune cells leads to uncontrolled inflammatory reactions and liver injury in MetALD and MASLD. The complex interplay between multiple immune cells and hepatocytes, such as hepatic stellate cells (HSCs) and hepatic sinusoidal endothelial cells, plays a crucial role in disease progression [8]. For example, dysregulated metabolism in MetALD and MASLD affects the activation and proliferation of immune cells such as T cells, B cells, macrophages, neutrophils, dendritic cells (DCs), natural killer (NK) cells, and natural killer T (NKT) cells [9,10].
In this review, we focus on the impact of immunity in Met-ALD and MASLD, along with the possible clinical mechanisms involved in affecting intestinal disorders, the adipose-liver axis, accelerating hepatocyte death and affecting immune cell-mediated inflammatory processes. In particular, we also discuss recent advances in pathways regulating multiple immune cells and corresponding immunological modulations in MetALD and MASLD. In conclusion, the liver is an immune organ that undoubtedly plays a key role in the pathology of SLD.
IMMUNOLOGICAL MECHANISMS IN SLD
The mechanisms underlying the pathogenesis of Met-ALD and MASLD differ in some ways, but the immune system plays an indelible role in both diseases [11]. The immunity in MetALD and MASLD is complex and multifactorial, involving the gut-liver axis [12,13], adipocyte-liver axis [14,15], adaptive and innate immune cells [15,16], and increased inflammatory cytokines released by hepatocytes, adipocytes and mucosal immune cells (Fig. 1) [17].
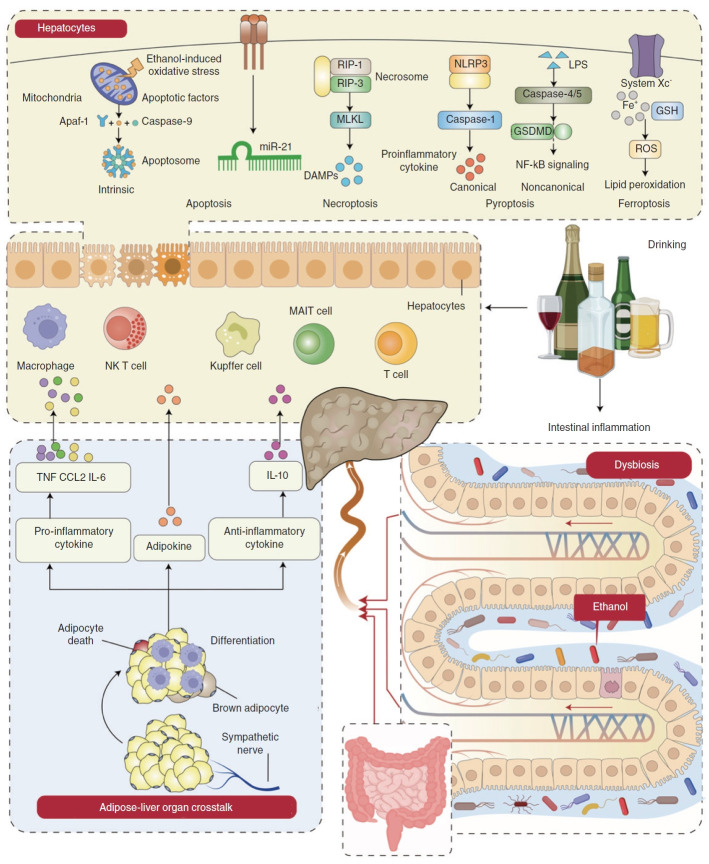
Figure 1.
Immune dysregulation in MetALD through the interaction of the gut, liver, and adipose organs. The immune dysregulation in MetALD involves hepatocyte death, the adipocyte-liver axis and gut dysbiosis. (1) Chronic alcohol damages the intestinal barrier, increases intestinal permeability, and triggers an immune response. The dysfunctional gut barrier and products released by gut microbiota lead to the transfer of components and metabolites to the liver and initiate an immune reaction through the biliary system and portal vein communicating with the liver via the gut-liver axis [27]. (2) The crosstalk between adipose and liver organs is mediated by various factors, including neurotransmitters, pro-inflammatory cytokines (e.g., TNF, CCL2, IL-6), anti-inflammatory cytokines (e.g., IL-10), miRNAs, extracellular vesicles (EVs), metabolites, and adipocytokines. This crosstalk promotes hepatocyte damage and inflammation in MetALD [38]. (3) Excessive alcohol consumption can lead to various types of hepatocyte death, such as apoptosis, necroptosis, pyroptosis, and ferroptosis. Hepatocyte apoptosis involves the secretion of apoptosis factors that combine with apaf-1 and caspase-9 to form the apoptosome (intrinsic) and cell apoptosis through miR-21 (extrinsic) [50, 51]. Hepatocyte necroptosis involves RIP1 and RIP3 activation and subsequent MLKL phosphorylation, leading to DAMPs [54, 55]. Canonical pyroptosis depends on caspase-1 and is mediated by the NLRP3 inflammasome, inducing the release of proinflammatory cytokines [57]. Noncanonical pyroptosis is activated by LPS and then activates caspase-4/5 and GSDMD, which regulates NF-ĸB signaling [61]. Ferroptosis is an iron-dependent cell death mechanism characterized by glutathione (GSH) depletion and damage to system Xc-, leading to cell death through ROS accumulation and lipid peroxidation [63]. These factors activate mucosal immune cells such as macrophages, NK T cells, KCs, MAIT cells and T cells releasing proinflammatory cytokines and chemokines, ultimately leading to hepatocyte death. MetALD, metabolic dysfunction-associated alcoholic liver disease; CCL2, Chemokine (CC-motif) ligand 2; IL, interleukin; RIP-1/3, receptor interacting protein-1/3; MLKL, mixed lineage kinase domain like; DAMPs, danger associated molecular patterns; NLRP3, NACHT, LRR, and PYD domains-containing protein 3; LPS, lipopolysaccharide; GSDMD, gasdermin D; NFĸB, nuclear factor kappa B; ROS, reactive oxygen species; KCs, Kupffer cells; MAIT, Mucosal Associated Invariant T cells.
Immunological mechanisms in MetALD
In terms of MetALD, hepatotoxicity induced by alcohol and oxidative stress are the major factors leading to immune responses [18]. However, studies suggest that immune responses may also play a key role in the development of MetALD [19], especially in its inflammatory condition, alcoholic steatohepatitis (ASH) [20]. Immune involvement in the pathogenesis of MetALD involves multiple organs and pathways, mainly including gut microbiota and microbiota products, adipose tissue, and hepatocytes [21].
The main mechanism is as follows: (1) Alcohol intake damages the intestinal barrier, allowing gut-derived metabolites or gut microbiota itself to reach hepatocytes. This triggers an immune response by disrupting communication between the gut and liver through effects on the gut-liver axis, biliary system and portal vein system [19,22]. (2) Alcohol consumption alters adipose tissue secretion of adipokines, pro-inflammatory, anti-inflammatory cytokines and adipokines to activate immune cells, leading to liver inflammation and deterioration of fibrosis [23]. (3) The immune response leads to various types of hepatocyte death, such as apoptosis, necroptosis, pyroptosis, and ferroptosis, affecting the severity of liver inflammation and the progression of Met-ALD [24].
Gut dysbiosis in MetALD
The gut microbiota maintains the integrity of the intestinal barrier, regulating intestinal homeostasis and stimulating host immune responses [25]. Intestinal barrier integrity and gut microbiota and their metabolites are necessary for regulating MetALD progression [26]. The intestine communicates with the liver through the biliary system and portal vein via the gut-liver axis, transferring intestinal-derived metabolic substances or intestinal microbiota itself to the liver and stimulating immune reactions in MetALD progression [27]. For example, antibiotics alleviate alcohol-induced intestinal tight junction damage and inflammatory activation [28]. Probiotic compounds reverse the gut dysbiosis induced by Met-ALD and maintain the integrity of the intestinal barrier, thus reducing liver injury, mainly by upregulating the production of mucus and the expression of tight junction proteins [29]. Additionally, intestinal bacterial metabolites such as shortchain fatty acids can penetrate into the blood and then modulate immune cells such as DCs precursors in the bone marrow [30]. Commensals regulate both innate and adaptive immune systems to establish sustained tolerance to innocuous antigens. Innate lymphocytes are often located in peripheral tissues and are regulated by microbiota [31]. Adaptive lymphocytes are also influenced by gut microbes, such as B cells generating IgA controlled by microbes, TH17 cells regulated by segmented filamentous bacteria, regulatory T (Treg) cells modulated by Clostridia, and T follicular helper cells influenced by Akkermansia muciniphila [32].
Adipose-liver organ crosstalk in MetALD
Ethanol is likely unique among toxins in that it perturbs almost all aspects of hepatic adipose tissue, partly due to the enormous metabolic demand of alcohol metabolism on the liver [33,34]. Alcohol-induced adipose injury is regulated by the release of mediators containing pro-inflammatory and anti-inflammatory cytokines and adipokines. For instance, after consuming ethanol, the differentiation of preadipocytes and the production of adipokines by adipocytes are impaired [35], leading to adipose tissue inflammation and adipocyte death [36,37]. These factors result in insulin resistance in adipose tissue, increased lipolysis and the production of pro-inflammatory cytokines [38], especially TNF, IL-1β, CCL2, IL-10 and IL-18 production. These factors are positively correlated with the severity of MetALD [38-40]. In addition, multiple immune cells are present in adipose tissue, including macrophages, DCs, neutrophils, T cells and B cells, which are affected by excessive alcohol intake and toll-like receptors (TLR)4 expression [41]. Moreover, excessive alcohol intake alters the adipokine secretion of leptin, visfatin, resistin, and adiponectin to activate both Kupffer cells (KCs) and HSCs, leading to liver inflammation and fibrosis formation [42,43]. A recent study found that excessive drinking increases the expression and activity of uncoupling protein 1 (UCP1) in brown adipose tissue [44]. Brown adipose tissue and beige fat oxidize fatty acids to provide fuel for UCP1-mediated thermogenesis, thus inhibiting lipid transport to the liver. The deletion of the UCP1 gene exacerbates alcohol-induced liver steatosis, injury, inflammation, and fibrosis [45,46]. Acute adipocyte death causes liver injury and activates inflammation in a chemokine (C-C motif) receptor 2-positive (CCR2+) macrophage-dependent manner, further increasing the sensitivity of hepatocytes to lipotoxicity [47]. Therefore, adipose-liver crosstalk plays a role in increasing liver inflammation and injury in MetALD. However, for future clinical considerations, it is necessary to continuously explore more potential mechanisms.
Hepatocyte death crosstalk in MetALD
Excessive alcohol consumption can result in various types of hepatocyte death, such as apoptosis, necroptosis, pyroptosis, and ferroptosis, which are closely linked to the severity of inflammation in MetALD [48]. Ethanol is metabolized by alcohol dehydrogenase, cytochrome P450 family 2, subfamily E, polypeptide 1 (CYP2E1) and catalase, leading to the production of reactive oxygen species (ROS) [49]. Ethanol-induced oxidative stress activates the mitochondrial (intrinsic) apoptosis pathway, involving the release of apoptosis factors like cytochrome c and apoptosis-inducing factors into the cytosol. These factors combine with apoptotic protease activating factor 1 (apaf-1) and caspase-9 to form the “apoptosome”, finally activating the internal apoptotic pathway [50,51]. Therefore, apoptotic cells are efficiently engulfed by surrounding macrophages, contributing to the non-inflammatory nature of the MetALD pathway. Prolonged alcohol exposure triggers death receptor-mediated (extrinsic) cell apoptosis pathways, including Fas ligands and TNF-α, and induces cell apoptosis through miR-21 [52]. Hepatocyte stress is a result of ethanol metabolism and increased exposure to gut-derived pathogen-associated molecular patterns (PAMPs) and endogenous danger-associated molecular patterns (DAMPs), establishing a close link to necroptosis.
The characteristics of necroptosis include damage to the structure of the cell membrane, nucleus, and cytoplasm to varying degrees, increased permeability of the cell membrane, deformation and dissolution of the nucleus, and loss of activity in enzymes and proteins in the cytoplasm during the progression of MetALD. Necroptotic cells release various damage-associated molecular patterns (DAMPs) that trigger inflammatory responses [53]. The process is regulated by the activation of receptor-interacting protein (RIP) 1 and RIP3, which is partially induced by the necrosome complex and subsequent phosphorylation of mixed lineage kinase domain like (MLKL) [54,55]. As a result, necrotic liver cell death is immunogenic, leading to excessive inflammation and hepatocyte death by activating innate immune cells or inducing other forms of hepatocyte death, such as pyroptosis [56].
Pyroptosis also plays a crucial role in the progression of MetALD. Canonical pyroptosis relies on caspase-1 and is facilitated by inflammatory bodies, such as the NLR family pyrin domain-containing 3 (NLRP3) [57], resulting in LPS-induced ER stress in hepatocytes [58]. Similarly, the absence of NLRP3 can ameliorate liver steatosis and chronic ethanol damage [59]. Moreover, pyroptosis triggered by intestinal PAMP and metabolic DAMP, such as uric acid and adenosine triphosphate, leads to the secretion of inflammasomedependent cytokines by immune cells damaged by ethanol [60]. Additionally, LPS can directly trigger noncanonical pyroptosis signaling independently of TLR4. Mechanistically, activated caspase-11 or caspase-4/5 in the liver detects intracellular LPS, cleaves gasdermin D (GSDMD) within its linker ring, binds to phosphoinositol on the plasma membrane, cleaves it, and ultimately induces cell death. Furthermore, GSDMD regulates adipogenesis, inflammatory response, and nuclear factor kappa B (NF-ĸB) signaling, all of which are critical in the progression of MetALD [61].
Ferroptosis is induced in hepatocytes treated with ethanol [62]. Excessive alcohol consumption promotes an increase in serum ferritin concentration and transferrin saturation, leading to an increase in liver iron reserves [63]. Ferroptosis is an iron-dependent oxidative programmed cell death mechanism characterized by glutathione (GSH) depletion, damage to the glutamate antiporter (system Xc-), and overexpression of lipid hydroperoxides [64]. This process produces oxygen and causes local inflammation in the liver [65]. Subsequently, the inactivation of glutathione peroxidase 4, which can reduce lipid peroxides in the plasma membrane, leads to cell death through the accumulation of ROS caused by excessive iron-induced lipid peroxidation or the Fenton reaction [66]. These reactive hydroxyl radicals destroy the lipid membrane, induce lipid peroxidation and membrane instability, and eventually lead to the leakage of cell substances and cell death [67].
All in all, the immunological mechanisms in MetALD are complex and multifactorial, involving hepatocyte death, adipose-liver organ crosstalk disorder, and intestinal disturbance caused by excessive alcohol intake. However, the mechanisms between MetALD and MASLD are quite different.
Immunological mechanisms in MASLD
The spectrum of MASLD includes steatosis, metabolic dysfunction associated steatohepatitis (MASH), fibrosis, cirrhosis, and MASH associated hepatocellular carcinoma (HCC) [68,69]. Recent research suggests the “multiple hit” hypothesis for the development of MASLD, indicating that immunological mechanisms in the liver, intestines, and adipose tissue influence the progression of MASLD [5].
The main mechanisms include: (1) Damage to the intestinal barrier results in the transfer of bacteria or bacterial components into the bloodstream, which is necessary for liver inflammation and the progression of MASLD [70]. (2) Adipose tissue plays a key role in regulating MASLD progression by releasing adiponectin, leptin, lipid moieties and lipid substances like tumor necrosis factor-α (TNF-α), interleukin (IL)-6 and calprotectin such as S100A8 and S100A9 [71]. (3) Different immune cells produce various cytokines and chemokines, such as TNF-α, IL-1 and IL-18 (Fig. 2) [16].
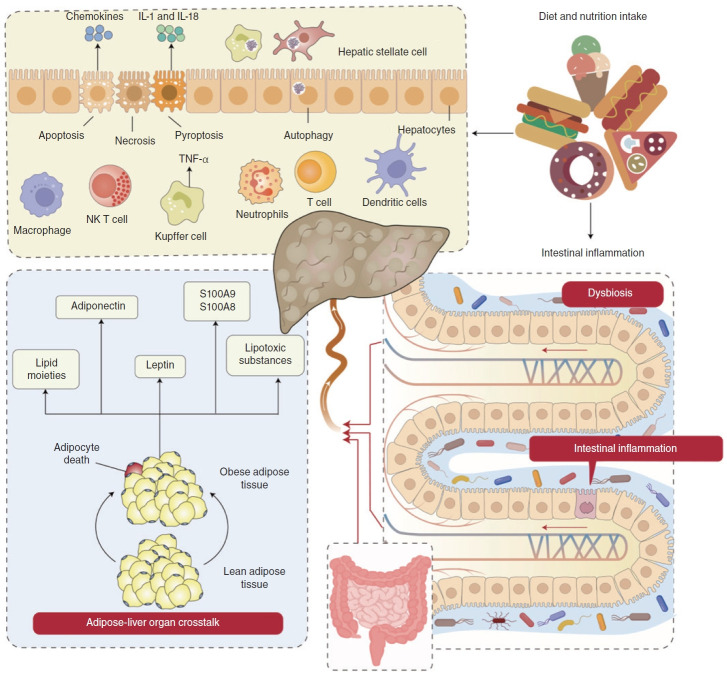
Figure 2.
Immune dysregulation in MASLD through the interaction of the gut, liver, and adipose organs. The immune dysregulation in MASLD involves hepatocyte death, the adipocyte-liver axis and gut dysbiosis. (1) High fat diets (HFD) consumption leads to gut barrier dysfunction, escalating intestinal inflammation and triggering an ectopic immune response. Damage to the intestinal barrier facilitates the passage of bacteria or bacterial components into the bloodstream, essential for hepatocyte death and MASLD progression [12]. (2) HFD consumption transforms lean adipose tissue into obese adipose tissue. Obese adipose tissue releases adiponectin, leptin and lipid moieties like palmitic acids, ceramide, IL-6 and TNF, inducing cell stress and hepatocyte death in MASLD.83,84 (3) Both gut dysbiosis and obese adipose tissue lead to hepatocyte death, which mainly encompasses apoptosis, necroptosis and pyroptosis. These factors activate KCs, producing TNF, TRAIL and FAS ligands by engulfing apoptotic bodies, thereby stimulating the secretion of chemokines and triggering hepatocyte apoptosis [96]. These factors further damage hepatocytes, leading to necroptosis and pyroptosis. This process involves the release of IL-1 and IL-18 into the bloodstream, influencing autophagy alterations in hepatocytes and nonparenchymal cells like KCs and HSCs [103]. All these factors then activate the mucosal immune cells such as macrophages, NK T cells, Kupffer cells, neutrophils, T cells and DCs to release inflammatory cytokines and chemokines, further leading to hepatocyte death. MASLD, metabolic dysfunctionassociated steatotic liver disease; IL, interleukin; KCs, Kupffer cells; TRAIL, tumour necrosis factor-related apoptosis-inducing ligand; HSCs, hepatic stellate cells; DCs, dendritic cells.
Gut dysbiosis in MASLD
Gut microbiota is also essential for the progression of MASLD [12]. The intestines and liver communicate through tight junction interactions via the biliary tract, portal vein and systemic circulation. This communication allows gutderived products to be directly transported to the liver, while the liver provides feedback on bile and antibody secretion to the intestine [8]. An unhealthy state of gut microbiota in MASLD patients is characterized by a high abundance of pathogens such as Escherichia coli, Campylobacter jejuni, Salmonella enterica, Vibrio cholerae, and Bacteroides fragilis and a low abundance of key genera including Bacteroides, Prevotella and Ruminococcus, which represents an unhealthy state for gut microbiota in MASLD patients [72,73]. Furthermore, MASLD is associated with intestinal inflammation, where the number of immune cells in the intestinal mucosa, such as CD4+ and CD8+ T lymphocytes, is reduced. This reduction is linked to increased cytokine secretion, leading to the breakdown of the tight junctions in the intestinal barrier [74].
Bile acid metabolism is completed under the influence of gut microbiota, and the enzymes produced by gut microbiota play a crucial role in the enterohepatic circulation of bile acids [75]. Additionally, bile acids regulate the size and composition of gut microbiota [76]. These interactions between bile acids and intestinal microbiota significantly impact lipid metabolism and the progression of MASLD [77], consequently influencing the immune response. Bile acids also influence the differentiation of T cells and the polarization of macrophages. The metabolism of bile acids and a distinct lymphocyte population collectively maintain the integrity of the intestinal barrier system, with Treg cells expressing forkhead box protein P3 (FOXP3) contributing to the homeostasis of the intestinal immune system. Furthermore, bile acids promote the polarization of macrophages towards the M1 phenotype, partly through the transactivation of TLR2 by M2 muscarinic acetylcholine receptor, leading to an increased production of pro-inflammatory cytokines.
In addition, the development of damage-associated molecular patterns (DAMPs) and pathogen-associated molecular patterns (PAMPs) is encouraged by immunity, which is linked to changes in the gut microbiota, particularly the activity of LPS [78]. These factors then cause the production of cytokines, chemokines, and growth factors by stimulating and activating TLRs and inflammasomes. These occurrences promote the recruitment, activation, and differentiation of monocytes into tumor-associated macrophages, which leads to angiogenesis and fibrosis and works in concert with cancer-associated fibroblasts [79]. Furthermore, HSCs activation and differentiation into myofibroblast-like cells exacerbate fibrogenesis. Moreover, active HSCs promote T-reg activation while impairing the capacity of Natural Killer cells (NKs) to induce HSC death, hence impairing immuno-tolerance [80]. The aforementioned macrophages, which can stimulate a TH2 immune response and result in an immuno-tolerance status, also aid in these last steps. All the processes mentioned above exacerbate and advance MASLD development [81].
Adipose-liver organ crosstalk in MASLD
Adipose tissue is the largest endocrine organ in the body, involved in various physiological and pathological processes such as energy metabolism, endocrine homeostasis, and inflammatory reactions. Adipose-liver crosstalk influences systemic metabolism and insulin resistance [82]. Recent studies have revealed that adipose tissue not only serves as the primary source of fatty acids in the liver but also plays a crucial role in regulating MASLD progression by releasing adiponectin, leptin, lipid moieties, lipotoxic substances and calprotectin [83,84]. Adiponectin inhibits the proliferation of HSCs [85], while leptin triggers inflammation by activating KCs and enhancing their release of TNF-α [86]. Additionally, lipid moieties like palmitic acids and ceramide released by adipocytes inhibit the functions of the endoplasmic reticulum (ER) and mitochondria, causing cell stress and eventual hepatocyte death [87]. Furthermore, lipotoxic substances and calprotectin (S100A8 and S100A9) from adipose tissue stimulate infiltrating macrophages [88] and KCs [89] through TLR4 and NLRP3 signaling [90,91]. These processes result in the release of inflammatory factors from adipose tissue, such as TNF-α, leading to hepatocyte death and activation of KCs through JNK pathways [92,93]. A recent study demonstrated that acute adipocyte death triggers lipolysis by activating chemokine receptor 2-positive CCR2+ macrophages and increasing epinephrine and norepinephrine levels [94]. Therefore, adipose-liver crosstalk contributes to the escalation of liver inflammation and injury in MASLD [33]. However, for future clinical considerations, a comprehensive understanding of adipose-liver crosstalk is essential to continually explore additional potential mechanisms.
Hepatocyte death in MASLD
Hepatocyte death is a major factor contributing to the progression of MASLD [95]. Various mechanisms of hepatocyte death, such as apoptosis, necroptosis, and pyroptosis, play a crucial role in the development of MASLD [96]. Hepatocyte apoptosis leads to the release of DNA fragments from apoptotic bodies, activates HSCs, and contributes to fibrosis formation, making it a significant contributor to MASLD [97]. Furthermore, hepatocyte death induced by death receptors like TRAIL stimulates the release of extracellular vesicles (EVs) and certain chemokines, which in turn enhance the recruitment and activation of the immune system [98,99]. Additionally, by engulfing apoptotic particles, KCs release TNF, TRAIL, and FAS ligands, thereby accelerating hepatocyte death and leading to hepatitis and fibrosis [96]. Necrosis, a regulated form of programmed cell death, is mediated by a combination of RIP1 and RIP3. In MASLD, increased RIP3 expression is associated with JNK activity and inflammation [100,101], and hepatic inflammation and liver fibrosis are significantly reduced with RIP3 deficiency [102]. Pyroptosis, a recently identified form of caspase 1-dependent cell death, activates the inflammasome, leading to the release of IL-1 and IL-18, and continuous release of cytoplasmic contents [103]. The circulation of IL-1 and IL-18 activates the immune system [104]. Several studies suggest that altered autophagy in hepatocytes and nonparenchymal cells like KCs and HSCs contributes to the pathophysiology of MASLD [105]. For example, dysregulated unfolded protein response (UPR) in hepatocytes led to apoptosis and inflammation in mice [106]. Moreover, reduced liver autophagy results in inadequate clearance of damaged mitochondria, leading to MASLD-related oxidative stress, release of mitochondrial factors, hepatocyte death and liver inflammation [107]. In animal models of MASLD, inhibiting IL-1 signaling reduced liver fibrosis, inflammation, steatosis and hepatocyte death [108].
In summary, the immunological mechanisms in MASLD are complex and multifactorial, involving hepatocyte death, adipose-liver organ crosstalk disorder, and intestinal disorder induced by metabolic dysfunction. These factors subsequently impact the accumulation of immune cells in the liver.
IMMUNE CELLS-INDUCED IMMUNE DYSREGULATION IN SLD
The liver, the largest immune organ, houses a variety of innate and adaptive immune cells, such as macrophages, KCs and lymphocytes [109]. These cells possess immunological functions and can eliminate viruses, bacteria, and specific antigens from the body. Moreover, the liver’s high level of vascularization, combined with reduced blood flow in its fenestrated capillary-like sinusoids, creates a unique environment that promotes immune cell exposure to bloodborne and intestinal infections [16,110]. The liver contains a wide range of immune cells, including lymphoid and myeloid cell lineages, primarily situated in the sinusoids, intravascular spaces and subcapsular compartments (Fig. 3) [111].
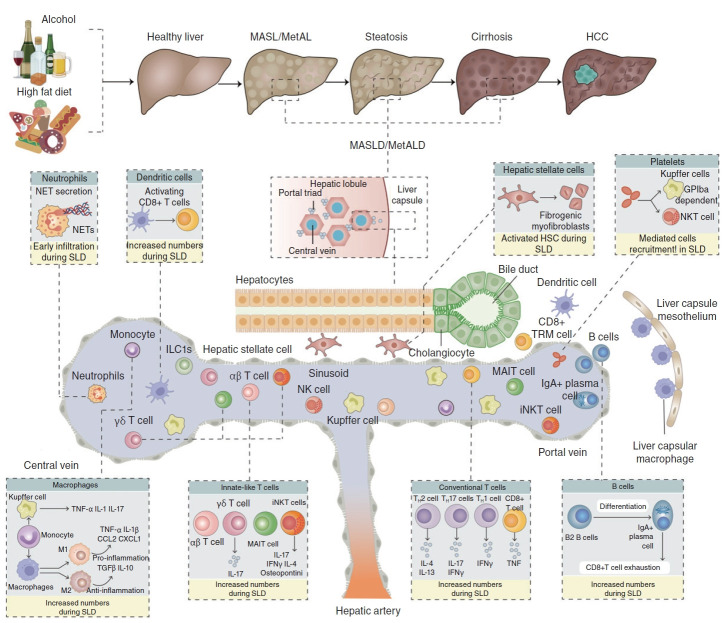
Figure 3.
Immune modulations of SLD pathogenesis. The hepatic immune cell repertoire is altered and participates in the uncontrolled inflammatory environment that promotes hepatocyte death and liver fibrosis. These immune cells include innate-like T cells, such as iNKT cells, MAIT cells and γδ T cells, as well as conventional CD8+ T cells and CD4+ T cell subsets, including IFNγ-producing TH1 cells [156], IL-4- and/or IL-13-producing TH2 cells [169], and IL-17-producing TH17 cells [157]. NETs are secreted or released during NETosis. Neutrophil accumulation is a precursor to SLD that causes inflammation and liver damage [189, 190]. The population of DCs and type 1 conventional DCs (cDC1s in particular) increases, promoting hepatic damage and liver inflammation by activating CD8+ T cells [131, 132]. Monocytes are also quickly recruited to the liver, where they can develop into pro-inflammatory macrophages or differentiate into KCs, which are derived from monocytes [194, 195]. Platelets are more numerous and more active, which promotes liver steatosis, inflammation, and damage. This suggests that platelets may activate and directly bind to KCs in a glycoprotein GPIb-dependent manner. B lymphocytes, particularly IgA+ plasma cells, accelerate the development of SLD by exhausting CD8+ T lymphocytes, which is one of their immunosuppressive actions [185, 186]. Additionally, the cytotoxic actions of fatty acids reduce the anti-injury potential of CD4+ T cells, promoting SLD progression to HCC [142, 143]. Moreover, CD8+ T cells and, particularly, the auto-aggressive CXCR6+ subset promote liver damage and the SLD-HCC transition by secreting pro-inflammatory cytokines like TNF and directly killing hepatocytes in a FASL-dependent and TNF-dependent manner [159, 160]. SLD, steatotic liver diseases; NKT cell, natural killer T cells; MAIT, Mucosal Associated Invariant T cells; IFNγ, interferon γ; NETs, neutrophil extracellular traps; SLD, steatotic liver diseases; DCs, dendritic cells; KCs, Kupffer cells; HCC, hepatocellular carcinoma.
Recent developments have improved our understanding of how the immune cell repertoire is altered during MetALD and MASLD in mice, as well as in the cirrhotic liver of humans [112]. For example, significant changes in the myeloid compartment were observed in both mice and humans, accompanied by a notable influx of monocytes and cells originating from monocytes [113]. These alterations in the hepatic immune cell composition likely contribute to the uncontrolled inflammatory environment that exacerbates liver damage and progresses MetALD and MASLD [114]. Throughout these diseases, there is undoubtedly a complex interplay among various immune cell types, hepatocytes, HSCs, and liver sinusoidal endothelial cells [115]. However, the complexity of this interaction is still not fully understood, and our current knowledge is primarily based on the study of specific immune cell types in the pathogenesis of Met-ALD and MASLD, as shown in the following (Table 1) [116].
Table 1.
Immune cell populations in SLD pathogenesis
| Cell type | Relative increase/Decrease | Function | Reference |
|---|---|---|---|
| B cells | + | Promoting the differentiation of B2 B cells into IgA+ plasma cells and exhausting CD8+ T lymphocytes | [117, 120] |
| DCs | + | Stimulating CD4+ T cells | [131, 132] |
| CD4+ T cells | + | Differentiating TH1, TH2 and TH17 cells and releasing cytokines | [142, 143] |
| CD8+ T cells | + | Producing IFN, TNF and cytotoxic chemicals | [159, 160] |
| iNKT cells | + | Producing IFN, IL-4, osteopontin and IL-17 | [172, 173] |
| γδ T cells | + | Releasing IL-17 and cause hepatic damage | [178] |
| MAIT cells | + | Regulating anti-inflammatory macrophages | [180, 181] |
| TH1 cells | + | Producing IFNγ | [156] |
| TH17 cells | + | Producing IFNγ and IL-17 | [157] |
| TH2 cells | + | Producing IL-4 and IL-13 | [169] |
| Platelets | + | Releasing GPIbα and boosting NKT cell recruitment leading to cell aggregates | [185, 186] |
| Neutrophils | + | Producing ROS, cytokines, proteases, and NETs | [189, 190] |
| Macrophages | + | Developing into pro-inflammatory macrophages or differentiate into KCs | [194, 195] |
SLD, steatotic liver diseases; IFNγ, interferon γ; IL, interleukin; NKT cell, natural killer T cells; ROS, reactive oxygen species; NETs, neutrophil extracellular traps; KCs, Kupffer cells; DCs, dendritic cells; MAIT, Mucosal Associated Invariant T cells.
B cells and plasma cells in SLD
B cells generate immunoglobulins [117], present antigens [118] and release cytokines [119] after activating pathogen-related molecular patterns mediated by TLR, impacting immunemediated inflammatory responses in numerous ways [120]. In mice, B cells have pro-inflammatory properties in the SLD, which involves the adaptive immune mechanism mediated by B cell receptors and the myeloid differentiation primary response 88 (MyD88)-dependent innate immune mechanism [121]. In humans, B cells were activated concurrently with the beginning of steatohepatitis, developed into plasmablasts and plasma cells, and then accumulated in SLD with lobular inflammation and fibrosis [122]. Furthermore, B cells may be influenced by the increase in intestinal permeability and inflammatory mediators produced by the microbiota. Finally, decreased inflammation and fibrosis in B-cell defective animals resulted in a reduction in SLD severity [121,123].
B cells can be categorized into two main lineages based on their heterogeneity [124]. In secondary lymphoid organs, B2 cells are activated and supported by CD4+ T helper (TH) cells to generate high-affinity antibodies that target specific antigens. As part of an innate-like immune response, B1 cells produce “natural” antibodies such as immunoglobulins encoded by the germline and present even without external antigen stimulation [125]. Depletion of B2 cells has been associated with a decrease in SLD-related hepatic fibrosis [122], although the exact role of B1 cells in SLD remains unknown. Serum levels of B cell-activating factor (BAFF), a cytokine that regulates B2 cell development and survival but not B1 cell survival [126], are elevated in SLD patients and further increased in those with fibrosis. In mice, neutralizing BAFF reduced liver damage in SLD [127].
B2 cells undergo differentiation after activation to become plasma cells or long-lived B cells that produce antibodies [128]. The liver is particularly abundant in plasma cells that produce IgA, IgG, or IgE, the number of these cells increases during SLD [129]. Moreover, patients with SLD had increased numbers of activated intestinal B-cells and showed a positive correlation between IgA levels and activated Fc receptor gamma-chain in hepatic myeloid cells as well as the degree of liver fibrosis [130]. However, although there is ample evidence linking B cells and IgA to SLD pathophysiology, more research on the underlying mechanisms is necessary. More research is needed to determine the antigen specificity of the B cells that are produced in SLD patients and are involved in the development of the disease.
Dendritic cells in SLD
DCs play a significant role in directing hepatic immunity. The plasmacytoid and myeloid subsets of DCs, which constitute less than 1% of all hepatic myeloid cells, are further categorized into type 1 and type 2 DCs [131]. The onset of SLD is associated with the expansion of myeloid DCs and their ability to specifically stimulate CD4+ T cells, triggering an adaptive immune response [132]. DCs contribute to local inflammation by recognizing various PAMP, including TLR and other pattern-recognition receptors [133,134]. While both CD103+ cDC1s and CD11b+ cDC2s subsets of conventional DCs are present in the liver and increase during SLD in mice, their specific roles in the disease’s pathophysiology remain unclear [135]. In humans, individuals with SLD exhibit higher levels of cDC1s in their livers, and an increase in cDC1s was associated with more SLD-specific symptoms. Activation of SLD in ATF-Like-3-deficient animals lacking cDC1s leads to elevated liver triglyceride levels but comparable levels of liver damage [136,137]. Similarly, SLD induction in ATF-Like-3-deficient mice lacking cDC1s leads to increased liver triglyceride levels but similar liver injury levels [138,139]. However, this whole-body deletion of ATF-Like-3 may have influenced SLD independently of cDC1 loss. Using a more precise cDC1 depletion model, cDC1s induce liver damage in mice, although the mechanisms are still not fully understood [140]. On the other hand, the role of cDC2s in SLD has not been explored yet. In conclusion, further research is needed to comprehensively comprehend the role of cDCs in SLD pathogenesis and the associated mechanisms.
Conventional CD4+ and CD8+ T cells in SLD
Conventional CD4+ TH cells play a crucial role in immune surveillance and adopt various specialized cell fates through interactions with specific DC subpopulations and cytokine environments [141]. TH1, TH2 and TH17 cell fates are distinguished by the production of interferon-γ (IFNγ), IL-4 and/or IL-13 and IL-17, respectively [142]. The roles of these cytokines and their signaling pathways have been studied in SLD [143]. As these cytokines are also secreted by cell types other than CD4+ T cells, it is challenging to definitively attribute the observed phenotype to alterations in the TH cell population. Therefore, further research is necessary to enhance our comprehension of this aspect.
Mice lacking IFN, the prototype TH1 cell cytokine, had a substantial inhibition of macrophage inflammatory response and further suppressed HSCs activation and liver fibrosis [144]. Reduced fibrosis in these animals is related to much lower production of osteopontin, a recognized inducer of liver fibrogenesis, although its mechanisms are still mostly unclear [144]. Other cell types that produce IFN, such as CD8+ T cells, contribute to the phenotype [145]. Additionally, CXCL10, an IFN-inducible chemokine, is also implicated in SLD etiology [146]. CXCL10 causes CXCR3-expressing cells, including T lymphocytes, to chemotaxis [147]. CXCL10 levels in the blood are elevated in SLD patients, and CXCL10 deletion or antibody-mediated CXCL10 neutralization reduces steatosis, liver damage, and fibrosis in rats [148]. CXCR3 deficiency decreased the development of SLD. Thus, reduced CXCL10-CXCR3 signaling may help to explain the impact of IFN insufficiency on SLD.
It has also been discussed how several cytokines linked to TH2 cells affect SLD [149]. Higher serum levels of IL-13, and their livers have higher levels of IL-13RA2 expression in SLD. HSCs express IL-13RA2, and the clinical characteristics of SLD are ameliorated by cytotoxin-mediated death of IL-13RA2+ cells. Patients with SLD have higher serum levels of IL-13 and higher liver expression levels of its receptor, IL-13RA2 [150]. IL-33 induces the secretion of type 2 cytokines IL-4, IL-5, and IL-13, which is consistent with the recognized involvement of type 2 cytokines in extracellular matrix synthesis [151]. IL-33 therapy also contributes to tissue regeneration and fibrosis after injury in mice [152]. However, treatment with IL-33 restricts the buildup of hepatic triglycerides and results in a minor decrease in liver damage in a mouse model of SLD [153]. In general, it is uncertain how TH2 cell-mediated immunity is involved in SLD.
TH17 cells cells perform various functions, including maintaining the gut barrier in response to commensals and contributing to inflammatory disorders in response to pathogens [154]. Patients with SLD show an increase in TH17 cells and the expression of TH17 cell-related genes [155]. In SLD mouse models, there is an elevation of TH17 cells, particularly a subset of pro-inflammatory CXCR3+ TH17 cells that contribute to SLD [148]. SLD worsens in animals lacking the unconventional prefoldin RPB5 interactor (Uri1) in hepatocytes (HepΔUri1 mice) due to DNA damage, which is linked to TH17 cell differentiation and increased hepatic IL-17A production [156,157]. In HepΔUri1 mice, blocking IL-17A with a monoclonal antibody or reducing TH17 cells production with the RORγt inhibitor digoxin reduces the hallmarks of SLD. Lack of IL-17A provides protection, while administering recombinant IL-17A exacerbates hepatic DNA damage, steatosis, liver injury, and fibrosis in wild-type mice fed an SLD-inducing diet. Disrupted IL-17-induced signaling in myeloid cells shields HepΔUri1 animals from SLD, suggesting significant communication IL-17-producing cells, especially TH17 cells and phagocytes [158]. Depleting all CD4+ T cells reduce hepatic fibrosis, aligning with the fibrosis-promoting effects of cytokines produced by TH1, TH2 and TH17 cells as mentioned earlier [143].
CD8+ T cells are primarily responsible for the production of IFN, TNF and cytotoxic chemicals such as perforins [159,160]. In both mice and humans, the number of hepatic CD8+ T cells increases during SLD, particularly CD8+ T cells expressing CXCR6 [161]. CXCR6+ CD8+ T lymphocytes stimulate hepatocyte death in a perforin-independent, FasL (CD95L)-dependent way. CD8+ T cell depletion reduced liver damage in a diet-induced animal model of SLD. SLD symptoms were enhanced in perforin 1-deficient animals, which have a larger amount and activating state of hepatic CD8+ T cells [162]. Perforin deficiency has been shown to promote CD8+ T cell activation [163,164]. This action is cell-extrinsic and includes the survival of immunostimulatory DCs in the absence of antigen-loaded DCs being killed by perforin [165,166]. Furthermore, CXCR6+ CD8+ T cells that concentrate in SLD express the exhaustion marker PD1, block PD1 and increase the activation CD8+ T cells, leading to faster SLD pathogenesis in mice [167]. As a result, CD8+ T lymphocytes are expected to contribute to hepatic damage during SLD.
Overall, there is a lack of an integrated mechanism explaining how T cell subsets are activated and contribute to increased hepatic inflammation in SLD [168]. The majority of current research focuses on cytokines released by T cell subsets rather than on T cells themselves [169]. Furthermore, while CD8+ T cell-mediated hepatocyte death develops in an antigen-independent manner during SLD, it is uncertain if adaptive, antigen-specific T cell responses are also involved [170,171]. More studies will be needed to fill these information gaps and discover how these pathways might be addressed therapeutically without compromising immune defenses.
Innate-like T cells in SLD
iNKT cells are generally concentrated in the liver relative to other organs and are significantly elevated in SLD disease progression [172]. CD1D-deficient or TRAJ18-deficient mice, in which iNKT cells do not mature, were used to study their function in SLD etiology [173]. iNKT cells enhance liver fibrosis by increasing osteopontin expression in the liver, which promotes fibrogenesis in SLD [174,175]. Recent research found that iNKT cells promote hepatic steatosis and, together with CD8+ T cells, cause hepatic injury, leading to SLD progression [176]. T-bet+ iNKT1 cells, GATA3+ iNKT2 cells and RORγt+ iNKT17 cells are all types of iNKT cells that generate IFN, IL-4 and IL-17, respectively [177]. Type 2 cytokines like IL-4 promote collagen formation and extracellular matrix deposition, which is intriguing to investigate the involvement of iNKT2 cells in SLD-induced fibrosis [151].
γδ T cells are another type of innate-like T cell that exists in the steady-state liver and develops and is sustained in a microbiota-dependent way [178]. During SLD, the number of γδ T cells in the mouse liver rises, promoting hepatic damage. Importantly, the formation of hepatic γδ T cells is hindered in Cd1d–/– mice, which may contribute to the dampened SLD phenotype [179].
MAIT cells proliferate during SLD development, and their absence exacerbates hepatic inflammation and damage [180,181]. However, it remains unclear how MAIT cells protect against diet-induced SLD, despite possessing pro-inflammatory characteristics similar to monocyte-derived macrophages and enhancing the mitogenic and pro-inflammatory functions of fibrogenic cells [182]. Additionally, this study did not investigate the involvement of MAIT cells in fibrosis, although previous studies have suggested a pro-fibrogenic impact of MAIT cells in acute liver injury models [183]. Therefore, further research is warranted to elucidate the role of MAIT cells in SLD, particularly in hepatic damage.
Platelets in SLD
In addition to their primary roles in coagulation and hemostasis, platelets also play a role in regulating inflammatory processes [184]. For example, platelets coming into contact with blood-borne pathogens enhance Kupffer cellmediated bacterial clearance in the liver. Moreover, platelets collaborate with monocytes to promote atherosclerotic plaque formation, boost arterial inflammation and facilitate additional leukocyte recruitment [185,186]. Platelets are implicated in the development of SLD. Anti-platelet medication has been shown to reduce SLD development in mice [187]. However, the underlying processes remain unknown. Recent research has revealed platelet activation, adhesion, and platelet-derived granules are crucial in SLD development. Platelets interact with KCs during both the early and late phases of SLD, promoting steatosis, inflammation, and damage in mice. Additionally, platelets enhance the accumulation of inflammatory cells in the liver during SLD through a glycoprotein GPIbα-dependent mechanism [188]. Therefore, based on the aforementioned findings, platelets may play a significant role in SLD development.
Neutrophils in SLD
Compared to their positive effects in fighting infection, neutrophils exhibit a negative impact on chronic inflammatory diseases by producing ROS, cytokines, proteases, and neutrophil extracellular traps (NETs) [189,190]. Both animal models and human biopsies demonstrate hepatic neutrophil infiltration in SLD [191]. Neutrophil accumulation occurs early in SLD mouse models [192]. Depleting neutrophils slows the progression of SLD in rats by reducing inflammation and liver damage, but these benefits diminish as the disease progresses. Inhibiting the serine protease neutrophil elastase has a similar effect in the early stages of SLD. Neutrophil elastase is produced as a component of NETs [190], which are detected very early in the liver during SLD pathogenesis in mice and at high levels in the blood of SLD patients [193]. Dismantling NETs using deoxyribonuclease I reduces hepatic inflammation, liver damage and liver fibrosis in rats, suggesting that these structures are harmful to SLD development [193]. Overall, neutrophils seem to play a crucial role in the initial stages of SLD through NETs formation, but their significance in later stages of SLD remains unknown.
Macrophages in SLD
Inflammatory signals during SLD promote the recruitment of blood monocytes to the liver, where they differentiate locally into monocyte-derived macrophages, expanding the liver’s macrophage pool [194]. Recent research has given information on the variety of hepatic macrophages in SLD [195].
A significant finding is that the self-maintenance of embryonically generated KCs is reduced in SLD mice due to the presence of KCs with low TIMD4 cell surface expression levels [194]. These TIMD4low KCs resemble the monocytederived KCs that are produced in mice following the nonphysiological reduction of embryonically derived KCs, indicating the generation of monocyte-derived KCs during SLD [196]. Monocytes contribute to the pool of KCs during SLD, and immunostaining studies have shown that these monocyte-derived KCs localize to hepatic sinusoids, similar to embryonically formed KCs. Monocyte-derived KCs are generated in response to the increased mortality of embryonically derived KCs during SLD, with the goal of maintaining KCs levels. During SLD, a gene signature related to lipotoxicity is enriched in both embryonically generated and monocyte-derived KCs, as indicated by a transcriptomic study.
This type of cellular stress signature most likely explains why embryonically derived KCs die during SLD and why they are unable to effectively self-renew. Although the generation of KCs from monocytes helps maintain the KCs population in the liver, their gene expression profile differs from that of embryonically derived KCs. Specifically, monocyte-derived Kupffer cells do not exhibit the full spectrum of gene expression associated with auxiliary functions of embryonically derived KCs, such as erythrophagocytosis. As a result, monocyte-derived KCs have a more pronounced inflammatory profile compared to their embryonically derived counterparts.
Finally, monocyte-derived KCs and embryonically generated KCs have differing functional effects on SLD. Although monocyte-derived KCs reduce hepatic triglyceride accumulation, they cause more liver damage than embryonically produced KCs. Thus, during SLD, Kupffer cell homeostasis is significantly disrupted, which influences liver pathophysiology [197].
Monocytes, in addition to contributing to the pool of KCs, follow a typical differentiation route during SLD, resulting in the formation of monocyte-derived inflammatory macrophages. It is worth noting that the SLD environment has a systemic influence on monocytes, as they already exhibit SLD-associated transcriptional changes in mouse bone marrow [198]. Monocyte-derived macrophages in the liver produce significant quantities of secreted phosphoprotein 1, integrin subunit alpha X, glycoprotein nonmetastatic B, CD9, and triggering receptor expressed on myeloid cells 2, all of which are also expressed in monocyte-derived KCs [199]. The monocyte-derived macrophages that accumulate in the liver during SLD resemble the lipid-associated macrophages found in obese white adipose tissue, suggesting that metabolic inflammation induces a common gene signature in monocyte-derived macrophages in different tissues and metabolic contexts [200]. In terms of function, monocyte-derived macrophages in the mouse liver localize to regions of tissue fibrosis near desmin+ HSCs, indicating their potential involvement in hepatic fibrosis [201]. Similar findings were reported in cirrhotic human liver [202]. During human liver fibrosis, a TREM2+CD9+ monocyte-derived macrophage population with profibrotic characteristics increases [202].
As previously stated, various immune cell populations are involved in SLD pathogenesis, and the roles of additional immune cell subsets, such as NK cells and ILCs, are still unknown. The hepatic inflammatory environment seen during SLD might result from coordinated immune cell interactions. Nevertheless, the detailed pathogenesis of SLD with this comprehensive immune response has not been extensively investigated.
In summary, various immune cells, including B cells, plasma cells, dendritic cells, conventional CD4+ and CD8+ T cells, innate-like T cells, platelets, neutrophils and macrophages play crucial roles in the development of MetALD and MASLD. Targeting the immune mechanisms of Met-ALD and MASLD holds significant therapeutic potential, and numerous clinical studies are required to investigate potential targeted therapies.
Immune cells in HCC
SLD is the primary risk factor for the development of HCC, due to alterations in the immune cell environment caused by liver inflammation as mentioned earlier [203,204]. In a mouse model of HFD-induced SLD and HCC, CD8+ T cells and NKT cells contribute to hepatic steatosis and damage, ultimately resulting in the progression of SLD to HCC. Notably, the depletion of CD8+ T cells and NKT cells does not worsen the advancement of SLD, which could serve as a foundation for preventing HCC development [162].
In addition, CD8+ T cells protect IgA-deficient MUP-uPA mice fed an HFD from SLD-induced HCC. CD8+ T cells have a limited ability to promote the progression of SLD, as HCC resistance is associated with a decrease in depleted CD8+ T cells. Subsequently, PDL1 blockade improved T cell dysfunction in MUP-uPA mice fed an HFD, resulting in enhanced anti-tumor immune function and reduced tumor incidence. Therefore, CD8+ T cells play a crucial role in anti-tumor effects in HFD-fed MUP-uPA mice. Additionally, Cd8a-deficient mice exhibit a higher tumor burden in other SLD-induced HCC models. This study suggests that despite the high tumor burden, the improvement of SLD severity by CD8+ T cells is limited, which may also contribute significantly to their anti-tumor effect. In summary, in other models, the role of CD8+ T cells in promoting SLD pathogenesis may mask their superior anti-tumor ability [205].
In the SLD-enhanced HCC mice model, CD4+ T cells have been proven to inhibit the development of HCC. In this model, fatty acids induce CD4+ T cell apoptosis through mitochondrial ROS production, while ROS clearance limits CD4+ T cell loss and reduces tumor burden [206]. The impact of CD4+ T cells on tumor growth is attributed to their ability to initiate tumor-specific immune responses, rather than their ability to contribute to the progression of MASH. Furthermore, in another SLD-enhanced HCC model, the opposite effect of CD4+ T cells has been demonstrated. Additionally, TH17 cells that produce IL-17A promote the development of SLD towards HCC through IL-17A-induced signaling in myeloid cells. In this study, TH17 cells accelerate the progression of SLD disease rather than playing a role in anti-tumor immune responses, resulting in a faster transition from SLD to HCC [158,207]. Therefore, depending on the model used for the transition from SLD to HCC, CD4+ T cells can regulate the transition from SLD to HCC through different mechanisms.
Innate immune cells can also affect SLD induced HCC. Neutrophils accelerate the development of SLD by releasing NETs. Restricting the production of NETs reduces inflammatory factors related to SLD and inhibits SLD-induced HCC, where the reason is the limited development of SLD [193]. The mechanism of other myeloid cells such as KCs in SLD induced HCC has not been studied and still requires a lot of research to explore.
Innate immune cells can also influence SLD-induced HCC. Neutrophils accelerate the development of SLD by releasing NETs. Limiting the production of NETs decreases inflammatory factors associated with SLD and hinders SLD-induced HCC, as the restricted SLD development is the cause [193]. The role of other myeloid cells, such as KCs, in SLD-induced HCC has not been investigated and necessitates further research.
POTENTIAL THERAPEUTIC MODULATIONS
Targeting inflammatory responses
Chronic inflammation is a key factor in the development of MetALD and MASLD, indicating that regulating inflammatory response is a promising therapeutic strategy for improving disease progression in MetALD and MASLD (Table 2). Since many immune cells, including NK cells, neutrophils, and KCs, as well as inflammatory mediators, including TNF-α, TLR4 and IL-1β, play multiple functions in liver damage and regeneration, comprehensive treatment strategies are required rather than just promoting or inhibiting inflammatory responses [208]. Corticosteroids, such as prednisone, are now frequently utilized as first-line anti-inflammatory medications in patients with severe ASH. Prednisone, however, raises the risk of bacterial and fungal infections and is ineffective in the majority of patients [209].
Table 2.
Immunological modulation in SLD pathogenesis
| Modulation | Targeting/ Formula | Candidate | Diseases | Reference |
|---|---|---|---|---|
| Targeting hepatocyte death | Oxidative stress | N-acetylcysteine | MetALD | [222] |
| Metoprolol | MetALD | [223] | ||
| S-adenosylmethionine | MetALD | [224, 225] | ||
| Selonsertib | MASLD | [226] | ||
| Vitamin E | MASLD | [227, 228] | ||
| Betaine | MASLD | [230] | ||
| Ursodeoxycholic acid | MASLD | [231] | ||
| Liver regeneration | G-CSF | MetALD | [232, 233] | |
| F-652 | MetALD | [234] | ||
| Bavachinin | MASLD | [235] | ||
| Targeting inflammatory responses | Inflammatory factor | Prednisone | MetALD | [209] |
| TNF | Infliximab | MetALD | [210] | |
| Enalapril | MetALD | [211] | ||
| PTX | MASLD | [213] | ||
| [212] | ||||
| TLR | JKB-121 | MASLD | [217] | |
| Vitamin D | MASLD | [217] | ||
| HA35 | MetALD | [214, 215] | ||
| IL-1 | Anakinra | MetALD | [209] | |
| FXR | Obeticholic acid | MetALD | NA | |
| Obeticholic acid | MASLD | [218] | ||
| EDP-305 | MASLD | [220] | ||
| LPS | HA35 | MetALD | [214] | |
| IMM-124E | MASLD | [221] | ||
| Targeting gut microbiota | Lactobacillus rhamnosus GG | Probiotics | MetALD | [238] |
| Lactobacillus rhamnosus R0011 and Lactobacillus acidophilus R0052 | Probiotics | MetALD | [239, 240] | |
| Streptococcus thermophilus, Bifidobacterium and Lactobacillus | Probiotics | MASLD | [244] | |
| Inulin-type fructans | Prebiotic | MASLD | [246] | |
| Oligofructose | Prebiotic | MASLD | [245] | |
| Vancomycin, gentamicin and meropenem | Antibiotics | MetALD | [241] | |
| Cidomycin | Antibiotics | MASLD | [247] | |
| Rifaximin | Antibiotics | MASLD | [248] | |
| Amoxicillin | Antibiotics | MetALD | [242] | |
| Lachnospiraceae and Ruminococcaceae | FMT | MetALD | [250] | |
| Healthy donor microbiome | FMT | MetALD | [251] | |
| FMT | MASLD | [252] |
SLD, steatotic liver diseases; MetALD, metabolic dysfunction-associated alcoholic liver disease; TLR, toll-like receptors; IL, interleukin; FXR, farnesoid X receptor; LPS, lipopolysaccharide; FMT, fecal microbiota transplantation.
In MetALD, two randomized controlled trials with anti-TNF medications, such as enalapril and infliximab, display unsatisfactory results, and the anti-TNF group has a higher number of deaths in patients with severe ASH [210,211]. In MASLD, pentoxifylline (PTX) as a methylxanthine derivative inhibits several pro-inflammatory cytokines like TNF-α, which exhibits lipid peroxidation inhibition, oxidative stress reduction, and peroxyl and hydroxyl radical scavenging properties [212,213].
The effects of anti-IL-1 on individuals with ASH are being studied in two current randomized clinical trials. In the first trial, patients with severe ASH are being treated with kanamycin monoclonal antibodies from the IL-1β antibody family to see if they are safe and effective. After 28 days of therapy, the primary outcome was histological improvement in liver biopsy ASH (NCT03775109). The other research (NCT04072822) primarily assesses the impact of anakinra as an IL-1 receptor antagonist on the 90-day death rate in individuals suffering from alcohol-associated hepatitis [209].
TLR receptors are expressed on the surface of macrophages, dendritic cells and epithelial cells. The inflammation of MetALD may originate from initiating TLR response. In animal models, HA35, a tiny and specific-sized hyaluronic acid molecule, suppresses the ethanol-induced TLR4 signaling pathway in KCs [214,215]. A randomized controlled trial on the effects of HA35 on the change of skeletal muscle mass in patients with ASH is registered, but patient recruitment has not started (NCT05018481). TLR receptors is crucial for MASLD as well [216]. Long-acting JKB-121 is a tiny chemical that works well as a weak antagonist at the TLR4. It has recently been established that vitamin D is a hormone that has anti-inflammatory, antifibrotic, and immunomodulatory effects [217]. Well-designed studies have investigated the possibility that vitamin D alleviates MASH (NCT01623024).
Targeting bile acid dysregulation provides hepatoprotective effects by exerting anti-inflammatory and antioxidant effects and by regulating lipid metabolism. Drugs including farnesoid X receptor (FXR) agonists, peroxisome proliferator-activated receptor alpha (PPARα) agonists, ursodeoxycholic acid, and its derivatives have entered different phases of clinical trials, and some of them have shown promising therapeutic effects. For example, a phase II randomized clinical trial using obeticholic acid, an FXR agonist, in patients with ASH was conducted. However, the clinical trial is terminated because of hepatotoxicity associated with obeticholic acid (NCT02039219). Obeticholic acid as a steroidal FXR agonist improves fibrosis and key characteristics of MASLD in a phase III trial (NCT02548351) [218]. However, it induces mild to moderate pruritus, HDL-C lowering, LDL-C increasing, and a potential for drug-induced liver toxicity [219]. EDP-305, another potent steroidal FXR agonist, is being developed. A phase IIa trial (NCT03421431) indicates that EDP-305 reduced ALT levels and liver fat content. Its adverse events are the same as those of obeticholic acid, like pruritus, nausea, vomiting, diarrhea, headache and dizziness [220].
Reducing LPS inhibits the activation of inflammatory cells and releases inflammatory mediators, which has a positive effect on improving MetALD. The ability of the antioxidant HA35 to reduce liver damage by preventing LPS from flowing out of the intestine has been demonstrated in animal models [214]. Oral administration of IMM-124E, an anti-LPSenriched bovine colostrum, is suggested to alleviate chronic inflammation, liver damage, and insulin resistance associated with MASLD in mice models and a small cohort of patients with biopsy-proven MASLD [221].
Targeting hepatocyte death
Hepatocyte injury plays an important role in the progression of MetALD and MASLD, and treatment for hepatocyte injury is considered promising therapies (Table 2). Longterm exposure to ethanol can lead to depletion of glutathione, making hepatocytes more susceptible to oxidative stress. Oxidative stress is one of the key mechanisms leading to hepatocyte damage in MetALD. Nevertheless, individual classic antioxidant molecules such as N-acetylcysteine or metoprolol are not effective against severe forms of ASH [222,223]. One of the reasons for the failure of these antioxidant therapies in ASH might be the absence of particular mitochondrial antioxidant effects. S-adenosylmethionine may be a viable treatment option for MetALD, since this molecule can restore glutathione in mitochondria and ameliorate steatosis in animals [224,225]. More clinical trials are needed to determine the efficacy of mitochondrialtargeted antioxidants in treating ASH. However, there is currently a scarcity of therapeutic modulations that target these hepatocyte death patterns. Because of the link between several types of cell death and MetALD, blocking a single cell death mechanism may not be enough to ameliorate ASH. In a phase II clinical trial, selonsertib (GS-4997), an oral inhibitor of apoptosis signal regulated kinase-1 enzyme, has no advantages over prednisone alone in the treatment of severe ASH (NCT02854631) [226]. Some clinical studies targeting apoptosis are increasing in MASLD. GS-4997 reduces liver fibrosis in the phase II trial. However, a phase III trial suggests that selonsertib had no anti-fibrotic effect in patients with bridging fibrosis or compensated cirrhosis due to MASLD [227,228]. Therefore, the anti-MASLD clinical research of GS-4997 is terminated. Antioxidants such as vitamin E, betaine and ursodeoxycholic acid show a better clinical perspective in MASLD [229-231]. For example, vitamin E alleviates MASLD progression as well as improved hepatic steatosis and lobular inflammation, but without effect on the development of fibrosis [229].
It is difficult to inhibit hepatocyte mortality, thus encouraging liver regeneration is seen as a complementary therapeutic strategy. Granulocyte colony-stimulating factor (GCSF) is a potent growth factor that accelerates liver cell regeneration in severe ASH. The meta-analysis results show that G-CSF is associated with a reduction of over 70% in mortality rate in ASH patients at 90 days [232,233]. In addition, IL-22 is a key anti-inflammatory cytokine that protects the liver and promotes regeneration. Currently, a phase II open-label clinical trial is now being conducted to investigate the impact of IL-22 agonists (F-652) on individuals with ASH. F-652 is a recombinant fusion protein containing human IL-22 and human IgG2 fragments, and its mechanism of action is identical to that of natural IL-22. Based on MELD and Lille scores, F-652 is associated with high improvement rates, increased liver regeneration markers and decreased inflammatory markers [234]. In MASLD, bavachinin is proven to possess liver-protecting effect against MAFLD, which binds to the pocket of PCNA facilitating its interaction with DNA polymerase delta and proregeneration effect [235].
Targeting gut microbiota
In recent years, with the continuous improvement of understanding in the impact of intestinal pathophysiology, the gut microbiota has become the main target for studying the modulations of MetALD and MASLD (Table 2) [236,237].
Probiotics and antibiotics from early clinical studies have shown promising results in MetALD. For example, two ongoing randomized clinical trials are investigating the impact of probiotics on ASH patients. The first trial is currently being conducted to test the efficacy and safety of probiotics mainly Lactobacillus rhamnosus GG in patients with moderate ASH. The main endpoint is the change in MELD score after 30 days (NCT01922895) [238]. Another study is evaluating the effects of probiotics mainly Lactobacillus rhamnosus R0011 and Lactobacillus acidophilus R0052 on liver enzyme, endotoxin, and cytokine levels in ASH patients after 7 days (NCT02335632) [239,240]. Antibiotics also alter the gut microbiota. However, using a mixture of antibiotics such as vancomycin, gentamicin and meropenem, there was no improvement in hepatitis and systemic inflammation [241]. A multicenter, double-blind randomized controlled trial evaluated the efficacy of a combination of corticosteroids and antibiotic amoxicillin in the treatment of severe ASH (NCT02281929), and the results are yet to be confirmed [242]. At present, the role of conventional antibiotics in ASH management has not been determined.
Probiotics, prebiotics and antibiotic affect the gut microbiota in MASLD. VSL#3 as probiotic mixture is used for MASLD in clinical studies, which is a mixture of eight different bacteria such as Bifidobacterium longum, Bifidobacterium infantis, Bifidobacterium breve, Lactobacillus acidophilus, Lactobacillus bulgaricus, Lactobacillus plantarum, Lactobacillus casei and Streptococcus thermophilus [243]. In a randomized controlled trial, the 4-month supplement of VSL#3 activated GLP-1, and improved fatty liver and body mass index in obese children with MASH (NCT01650025) [244]. Prebiotics contain no living microorganisms and nondigestible food ingredients that selectively promote the proliferation of gut microbes. Oligofructose and inulin-type fructans as common prebiotics, increased the abundance of Bifidobacterium spp, and significantly improved hepatic steatosis and NAS (NCT03184376 and NCT03042494) [245,246]. The treatment with cidomycin, as a non-absorbable antibiotic, indicates its potential to alleviating the severity of MASLD by intestinal microbiota modulations [247]. Besides, rifaximin as a non-absorbable, broadspectrum and gastrointestinal-specific antibiotic displayed effective and safe in biopsy-proven MASH (NCT02884037 and EudraCT 2010-021515-17) [248].
Fecal microbiota transplantation (FMT) might be an option for rebuilding a healthy gut microbiota. In preliminary research and an open-label experiment, FMT in patients with severe ASH from healthy donors increased survival and liver function by reducing gut microbiota, which contributes to the development of ASH. These studies demonstrate that the donor microbiota can change the recipient microbiota and improve MetALD without complications, even in individuals with severe ASH [249]. Cytolysin-secreting E. faecalis strains are an important factor contributing significantly to hepatocyte damage and mortality in individuals with severe alcoholism. Individuals with alcoholism had much higher numbers of E. faecalis in their feces than nonalcoholics or individuals with alcohol-related illnesses. Interestingly, the overall quantity of E. faecalis, not just the presence of cytolysin-positive strains, may be important in the severity of liver disease and subsequent mortality [250]. In severe ASH, FMT improves 90-day survival and reduces infections by positively regulating microbial communities such as pathogenic taxa and anaerobes, making it a viable option to prednisolone treatment. Importantly, this approach provides a way to precisely edit the gut microbiota [251].
Clinical investigations have revealed that FMT may have a therapeutic impact on MASLD. In a randomized clinical study, FMT successfully improved the therapeutic benefits on MASLD patients, and its clinical efficacy was greater in lean MASLD patients than in obese MASLD patients [252]. The changes in gut microbiota composition caused by FMT further lead to plasma metabolites such as phenylacetylcarnitine in MASLD patients’ extensive changes in phenylacetylcarnitine, phenylacetylglutamine and choline-derived metabolites and liver DNA methylation profiles [253]. Notably, other clinical trials evaluating the treatment of MASLD patients with FMT are presently underway (NCT02469272).
PERSPECTIVES
SLD are important chronic liver disorders that affect people worldwide, and their pathogens involve multiple mechanisms. Immunity plays a crucial role in promoting the progression from SLD to more severe forms of liver injury, such as steatohepatitis, cirrhosis and HCC. Immunity involves multiple mechanisms in the progression of SLD, mainly affecting intestinal disorders, the adipose-liver axis, accelerating hepatocyte death and affecting immune cellmediated inflammatory processes. Additionally, multiple immune cells are involved, including B cells, plasma cells, dendritic cells, conventional CD4+ and CD8+ T cells, innatelike T cells, platelets, neutrophils and macrophages. Some immunological modulations targeting hepatocyte death, inflammatory responses and gut microbiome are constantly increasing. The immunological modulations mainly include N-acetylcysteine, selonsertib, F-652, prednisone, pentoxifylline, anakinra, JKB-121, HA35, obeticholic acid, probiotics, prebiotics, antibiotics and FMT. However, our understanding of the immunological signals that drive SLD is incomplete, and further research is needed to better understand the involvement of specific immune cell subsets in these diseases. Future research to identify these key immunity drivers will not only enhance our understanding of the etiology of SLD but also discover new effective therapeutic interventions for treating MetALD and MASLD. We look forward to more clinical trials targeting immunological mechanisms for SLD in the future.
Acknowledgments
The National Natural Science Foundation of China (82074069) funded this work.
Abbreviations
- Apaf-1
apoptotic protease activating factor 1
- ASH
alcoholic steatohepatitis
- BAFF
B cell-activating factor
- CCL2
Chemokine (CC-motif) ligand 2
- CCR2+
chemokine (C-C motif) receptor 2-positive
- cDC1s
conventional DCs
- CXCL
chemokine (C-X-C motif) ligand
- CYP2E1
cytochrome P450 family 2
- DAMPs
danger associated molecular patterns
- DCs
dendritic cells
- ER
endoplasmic reticulum
- EVs
extracellular vesicles
- FMT
fecal microbiota transplantation
- FXR
farnesoid X receptor
- G-CSF
Granulocyte colony-stimulating factor
- GSDMD
gasdermin D
- GSH
glutathione
- HA35
Hyaluronic acid 35
- HCC
hepatocellular carcinoma
- HSCs
hepatic stellate cells
- IFNγ
interferon γ
- IL
interleukin
- ILCs
lymphoid cells
- KCs
Kupffer cells
- LPS
lipopolysaccharide
- MAIT
Mucosal Associated Invariant T cells
- MASH
metabolic dysfunction-associated steatohepatitis
- MASLD
metabolic dysfunction-associated steatotic liver disease
- MetALD
metabolic dysfunction-associated alcoholic liver disease
- MLKL
mixed lineage kinase domain like
- MyD88
myeloid differentiation primary response 88
- NETs
neutrophil extracellular traps
- NF-ĸB
nuclear factor kappa B
- NK cells
natural killer cells
- NKT cell
natural killer T cells
- NLRP3
NACHT
- PAMPs
pathogen associated molecular patterns
- PPARα
peroxisome proliferator-activated receptor alpha
- PTX
pentoxifylline
- RIP-1/3
receptor interacting protein-1/3
- RORγt
retinoid-related orphan receptorgammat
- ROS
reactive oxygen species
- SLD
steatotic liver diseases
- TGF-β
transforming growth factor-β
- TH
T helper
- TLR
toll-like receptors
- TNF-α
tumor necrosis factor-α
- TRAIL
tumour necrosis factor-related apoptosis-inducing ligand
- UCP1
uncoupling protein 1
- UPR
unfolded protein response
- Uri1
unconventional prefoldin RPB5 interactor
Footnotes
Authors’ contribution
Mengyao Yan: Investigation, writing original draft, review & editing, figure drawing. Shuli Man: Conceptualization, design, writing-review & editing, figure drawing, funding acquisition. Long Ma: Supervision, review & editing. Lanping Guo and Luqi Huang: Review & editing. Wenyuan Gao: Conceptualization, review & editing. The final version of the work has been read and approved by all of the authors.
Conflicts of Interest
The authors declare that there are no conflicts of interest
REFERENCES
- 1.Mackowiak B, Fu Y, Maccioni L, Gao B. Alcohol-associated liver disease. J Clin Invest. 2024;134:e176345. doi: 10.1172/JCI176345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parola M, Pinzani M. Liver fibrosis in NAFLD/NASH: from pathophysiology towards diagnostic and therapeutic strategies. Mol Aspects Med. 2024;95:101231. doi: 10.1016/j.mam.2023.101231. [DOI] [PubMed] [Google Scholar]
- 3.Singal AK, Shah VH, Malhi H. Emerging targets for therapy in ALD: Lessons from NASH. Hepatology. 2024;80:223–237. doi: 10.1097/HEP.0000000000000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ajmera V, Cepin S, Tesfai K, Hofflich H, Cadman K, Lopez S, et al. A prospective study on the prevalence of NAFLD, advanced fibrosis, cirrhosis and hepatocellular carcinoma in people with type 2 diabetes. J Hepatol. 2023;78:471–478. doi: 10.1016/j.jhep.2022.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rong L, Zou J, Ran W, Qi X, Chen Y, Cui H, et al. Advancements in the treatment of non-alcoholic fatty liver disease (NAFLD) Front Endocrinol (Lausanne) 2023;13:1087260. doi: 10.3389/fendo.2022.1087260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang R, Tang R, Li B, Ma X, Schnabl B, Tilg H. Gut microbiome, liver immunology, and liver diseases. Cell Mol Immunol. 2021;18:4–17. doi: 10.1038/s41423-020-00592-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albillos A, de Gottardi A, Rescigno M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J Hepatol. 2020;72:558–577. doi: 10.1016/j.jhep.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Tilg H, Adolph TE, Dudek M, Knolle P. Non-alcoholic fatty liver disease: the interplay between metabolism, microbes and immunity. Nat Metab. 2021;3:1596–1607. doi: 10.1038/s42255-021-00501-9. [DOI] [PubMed] [Google Scholar]
- 9.Moayedfard Z, Sani F, Alizadeh A, Bagheri Lankarani K, Zarei M, Azarpira N. The role of the immune system in the pathogenesis of NAFLD and potential therapeutic impacts of mesenchymal stem cell-derived extracellular vesicles. Stem Cell Res Ther. 2022;13:242. doi: 10.1186/s13287-022-02929-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao B, Ahmad MF, Nagy LE, Tsukamoto H. Inflammatory pathways in alcoholic steatohepatitis. J Hepatol. 2019;70:249–259. doi: 10.1016/j.jhep.2018.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sutti S, Albano E. Adaptive immunity: an emerging player in the progression of NAFLD. Nat Rev Gastroenterol Hepatol. 2020;17:81–92. doi: 10.1038/s41575-019-0210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tilg H, Adolph TE, Trauner M. Gut-liver axis: Pathophysiological concepts and clinical implications. Cell Metab. 2022;34:1700–1718. doi: 10.1016/j.cmet.2022.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Bauer KC, Littlejohn PT, Ayala V, Creus-Cuadros A, Finlay BB. Nonalcoholic fatty liver disease and the gut-liver axis: Exploring an undernutrition perspective. Gastroenterology. 2022;162:1858–1875.e2. doi: 10.1053/j.gastro.2022.01.058. [DOI] [PubMed] [Google Scholar]
- 14.Park SH, Seo W, Xu MJ, Mackowiak B, Lin Y, He Y, et al. Ethanol and its nonoxidative metabolites promote acute liver injury by inducing ER stress, adipocyte death, and lipolysis. Cell Mol Gastroenterol Hepatol. 2023;15:281–306. doi: 10.1016/j.jcmgh.2022.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheja L, Heeren J. Metabolic interplay between white, beige, brown adipocytes and the liver. J Hepatol. 2016;64:1176–1186. doi: 10.1016/j.jhep.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 16.Nati M, Chung KJ, Chavakis T. The role of innate immune cells in nonalcoholic fatty liver disease. J Innate Immun. 2022;14:31–41. doi: 10.1159/000518407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gramignoli R, Ranade AR, Venkataramanan R, Strom SC. Effects of pro-inflammatory cytokines on hepatic metabolism in primary human hepatocytes. Int J Mol Sci. 2022;23:14880. doi: 10.3390/ijms232314880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seitz HK, Bataller R, Cortez-Pinto H, Gao B, Gual A, Lackner C, et al. Alcoholic liver disease. Nat Rev Dis Primers. 2018;4:16. doi: 10.1038/s41572-018-0014-7. [DOI] [PubMed] [Google Scholar]
- 19.Avila MA, Dufour JF, Gerbes AL, Zoulim F, Bataller R, Burra P, et al. Recent advances in alcohol-related liver disease (ALD): summary of a Gut round table meeting. Gut. 2020;69:764–780. doi: 10.1136/gutjnl-2019-319720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011;141:1572–1585. doi: 10.1053/j.gastro.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mandrekar P, Ambade A. Immunity and inflammatory signaling in alcoholic liver disease. Hepatol Int. 2014;8 Suppl 2:439–446. doi: 10.1007/s12072-014-9518-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Szabo G. Gut-liver axis in alcoholic liver disease. Gastroenterology. 2015;148:30–36. doi: 10.1053/j.gastro.2014.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shim YR, Jeong WI. Recent advances of sterile inflammation and inter-organ cross-talk in alcoholic liver disease. Exp Mol Med. 2020;52:772–780. doi: 10.1038/s12276-020-0438-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miyata T, Nagy LE. Programmed cell death in alcohol-associated liver disease. Clin Mol Hepatol. 2020;26:618–625. doi: 10.3350/cmh.2020.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zafari N, Velayati M, Fahim M, Maftouh M, Pourali G, Khazaei M, et al. Role of gut bacterial and non-bacterial microbiota in alcohol-associated liver disease: Molecular mechanisms, biomarkers, and therapeutic prospective. Life Sci. 2022;305:120760. doi: 10.1016/j.lfs.2022.120760. [DOI] [PubMed] [Google Scholar]
- 26.Malaguarnera G, Giordano M, Nunnari G, Bertino G, Malaguarnera M. Gut microbiota in alcoholic liver disease: pathogenetic role and therapeutic perspectives. World J Gastroenterol. 2014;20:16639–16648. doi: 10.3748/wjg.v20.i44.16639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang W, Kong D. The intestinal microbiota as a therapeutic target in the treatment of NAFLD and ALD. Biomed Pharmacother. 2021;135:111235. doi: 10.1016/j.biopha.2021.111235. [DOI] [PubMed] [Google Scholar]
- 28.Gyongyosi B, Cho Y, Lowe P, Calenda CD, Iracheta-Vellve A, Satishchandran A, et al. Alcohol-induced IL-17A production in Paneth cells amplifies endoplasmic reticulum stress, apoptosis, and inflammasome-IL-18 activation in the proximal small intestine in mice. Mucosal Immunol. 2019;12:930–944. doi: 10.1038/s41385-019-0170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu H, Kang X, Yang X, Yang H, Kuang X, Ren P, et al. Compound probiotic ameliorates acute alcoholic liver disease in mice by modulating gut microbiota and maintaining intestinal barrier. Probiotics Antimicrob Proteins. 2023;15:185–201. doi: 10.1007/s12602-022-10005-x. [DOI] [PubMed] [Google Scholar]
- 30.Hosseinkhani F, Heinken A, Thiele I, Lindenburg PW, Harms AC, Hankemeier T. The contribution of gut bacterial metabolites in the human immune signaling pathway of non-communicable diseases. Gut Microbes. 2021;13:1–22. doi: 10.1080/19490976.2021.1882927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hammerich L, Tacke F. Hepatic inflammatory responses in liver fibrosis. Nat Rev Gastroenterol Hepatol. 2023;20:633–646. doi: 10.1038/s41575-023-00807-x. [DOI] [PubMed] [Google Scholar]
- 32.Pal A, Sun S, Armstrong M, Manke J, Reisdorph N, Adams VR, et al. Beneficial effects of eicosapentaenoic acid on the metabolic profile of obese female mice entails upregulation of HEPEs and increased abundance of enteric Akkermansia muciniphila. Biochim Biophys Acta Mol Cell Biol Lipids. 2022;1867:159059. doi: 10.1016/j.bbalip.2021.159059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parker R, Kim SJ, Gao B. Alcohol, adipose tissue and liver disease: mechanistic links and clinical considerations. Nat Rev Gastroenterol Hepatol. 2018;15:50–59. doi: 10.1038/nrgastro.2017.116. [DOI] [PubMed] [Google Scholar]
- 34.Joshi-Barve S, Kirpich I, Cave MC, Marsano LS, McClain CJ. Alcoholic, nonalcoholic, and toxicant-associated steatohepatitis: Mechanistic similarities and differences. Cell Mol Gastroenterol Hepatol. 2015;1:356–367. doi: 10.1016/j.jcmgh.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haghgoo SM, Sharafi H, Alavian SM. Serum cytokines, adipokines and ferritin for non-invasive assessment of liver fibrosis in chronic liver disease: a systematic review. Clin Chem Lab Med. 2019;57:577–610. doi: 10.1515/cclm-2018-0357. [DOI] [PubMed] [Google Scholar]
- 36.Mathur M, Yeh YT, Arya RK, Jiang L, Pornour M, Chen W, et al. Adipose lipolysis is important for ethanol to induce fatty liver in the National Institute on Alcohol Abuse and Alcoholism murine model of chronic and binge ethanol feeding. Hepatology. 2023;77:1688–1701. doi: 10.1002/hep.32675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Keshavarzian A, Farhadi A, Forsyth CB, Rangan J, Jakate S, Shaikh M, et al. Evidence that chronic alcohol exposure promotes intestinal oxidative stress, intestinal hyperpermeability and endotoxemia prior to development of alcoholic steatohepatitis in rats. J Hepatol. 2009;50:538–547. doi: 10.1016/j.jhep.2008.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Voican CS, Njiké-Nakseu M, Boujedidi H, Barri-Ova N, Bouchet-Delbos L, Agostini H, et al. Alcohol withdrawal alleviates adipose tissue inflammation in patients with alcoholic liver disease. Liver Int. 2015;35:967–978. doi: 10.1111/liv.12575. [DOI] [PubMed] [Google Scholar]
- 39.Fantuzzi G. Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 2005;115:911–919. doi: 10.1016/j.jaci.2005.02.023. quiz 920. [DOI] [PubMed] [Google Scholar]
- 40.Li W, Amet T, Xing Y, Yang D, Liangpunsakul S, Puri P, et al. Alcohol abstinence ameliorates the dysregulated immune profiles in patients with alcoholic hepatitis: A prospective observational study. Hepatology. 2017;66:575–590. doi: 10.1002/hep.29242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hyun J, Han J, Lee C, Yoon M, Jung Y. Pathophysiological aspects of alcohol metabolism in the liver. Int J Mol Sci. 2021;22:5717. doi: 10.3390/ijms22115717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim JE, Kim JS, Jo MJ, Cho E, Ahn SY, Kwon YJ, et al. The roles and associated mechanisms of adipokines in development of metabolic syndrome. Molecules. 2022;27:334. doi: 10.3390/molecules27020334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Correale J, Marrodan M. Multiple sclerosis and obesity: The role of adipokines. Front Immunol. 2022;13:1038393. doi: 10.3389/fimmu.2022.1038393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shen H, Jiang L, Lin JD, Omary MB, Rui L. Brown fat activation mitigates alcohol-induced liver steatosis and injury in mice. J Clin Invest. 2019;129:2305–2317. doi: 10.1172/JCI124376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Beek SMM, Kalinovich A, Schaart G, Bengtsson T, Hoeks J. Prolonged β2-adrenergic agonist treatment improves glucose homeostasis in diet-induced obese UCP1-/-mice. Am J Physiol Endocrinol Metab. 2021;320:E619–E628. doi: 10.1152/ajpendo.00324.2020. [DOI] [PubMed] [Google Scholar]
- 46.Crombie IK, Cunningham KB, Irvine L, Williams B, Sniehotta FF, Norrie J, et al. Modifying Alcohol Consumption to Reduce Obesity (MACRO): development and feasibility trial of a complex community-based intervention for men. Health Technol Assess. 2017;21:1–150. doi: 10.3310/hta21190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117:175–184. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou Y, Wu R, Wang X, Bao X, Lu C. Roles of necroptosis in alcoholic liver disease and hepatic pathogenesis. Cell Prolif. 2022;55:e13193. doi: 10.1111/cpr.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaczmarek A, Vandenabeele P, Krysko DV. Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity. 2013;38:209–223. doi: 10.1016/j.immuni.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 50.Hao L, Zhong W, Dong H, Guo W, Sun X, Zhang W, et al. ATF4 activation promotes hepatic mitochondrial dysfunction by repressing NRF1-TFAM signalling in alcoholic steatohepatitis. Gut. 2021;70:1933–1945. doi: 10.1136/gutjnl-2020-321548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.King AL, Swain TM, Mao Z, Udoh US, Oliva CR, Betancourt AM, et al. Involvement of the mitochondrial permeability transition pore in chronic ethanol-mediated liver injury in mice. Am J Physiol Gastrointest Liver Physiol. 2014;306:G265–G277. doi: 10.1152/ajpgi.00278.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McDaniel K, Herrera L, Zhou T, Francis H, Han Y, Levine P, et al. The functional role of microRNAs in alcoholic liver injury. J Cell Mol Med. 2014;18:197–207. doi: 10.1111/jcmm.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Frank D, Vince JE. Pyroptosis versus necroptosis: similarities, differences, and crosstalk. Cell Death Differ. 2019;26:99–114. doi: 10.1038/s41418-018-0212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kondylis V, Pasparakis M. RIP Kinases in liver cell death, inflammation and cancer. Trends Mol Med. 2019;25:47–63. doi: 10.1016/j.molmed.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 55.Yuan J, Amin P, Ofengeim D. Necroptosis and RIPK1-mediated neuroinflammation in CNS diseases. Nat Rev Neurosci. 2019;20:19–33. doi: 10.1038/s41583-018-0093-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shi J, Gao W, Shao F. Pyroptosis: Gasdermin-mediated programmed necrotic cell death. Trends Biochem Sci. 2017;42:245–254. doi: 10.1016/j.tibs.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 57.Coll RC, Schroder K, Pelegrín P. NLRP3 and pyroptosis blockers for treating inflammatory diseases. Trends Pharmacol Sci. 2022;43:653–668. doi: 10.1016/j.tips.2022.04.003. [DOI] [PubMed] [Google Scholar]
- 58.Arioz BI, Tastan B, Tarakcioglu E, Tufekci KU, Olcum M, Ersoy N, et al. Melatonin attenuates LPS-induced acute depressive-like behaviors and microglial NLRP3 inflammasome activation through the SIRT1/Nrf2 Pathway. Front Immunol. 2019;10:1511. doi: 10.3389/fimmu.2019.01511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yao H, Zhang D, Yu H, Yuan H, Shen H, Lan X, et al. Gut microbiota regulates chronic ethanol exposure-induced depressive-like behavior through hippocampal NLRP3-mediated neuroinflammation. Mol Psychiatry. 2023;28:919–930. doi: 10.1038/s41380-022-01841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhong W, Wei X, Hao L, Lin TD, Yue R, Sun X, et al. Paneth cell dysfunction mediates alcohol-related steatohepatitis through promoting bacterial translocation in mice: Role of zinc deficiency. Hepatology. 2020;71:1575–1591. doi: 10.1002/hep.30945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen X, Lin S, Dai S, Han J, Shan P, Wang W, et al. Trimetazidine affects pyroptosis by targeting GSDMD in myocardial ischemia/reperfusion injury. Inflamm Res. 2022;71:227–241. doi: 10.1007/s00011-021-01530-6. [DOI] [PubMed] [Google Scholar]
- 62.Li LX, Guo FF, Liu H, Zeng T. Iron overload in alcoholic liver disease: underlying mechanisms, detrimental effects, and potential therapeutic targets. Cell Mol Life Sci. 2022;79:201. doi: 10.1007/s00018-022-04239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ferrao K, Ali N, Mehta KJ. Iron and iron-related proteins in alcohol consumers: cellular and clinical aspects. J Mol Med (Berl) 2022;100:1673–1689. doi: 10.1007/s00109-022-02254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang L, Liu Y, Du T, Yang H, Lei L, Guo M, et al. ATF3 promotes erastin-induced ferroptosis by suppressing system Xc. Cell Death Differ. 2020;27:662–675. doi: 10.1038/s41418-019-0380-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ali N, Ferrao K, Mehta KJ. Liver iron loading in alcohol-associated liver disease. Am J Pathol. 2023;193:1427–1439. doi: 10.1016/j.ajpath.2022.08.010. [DOI] [PubMed] [Google Scholar]
- 66.Hu CL, Nydes M, Shanley KL, Morales Pantoja IE, Howard TA, Bizzozero OA. Reduced expression of the ferroptosis inhibitor glutathione peroxidase-4 in multiple sclerosis and experimental autoimmune encephalomyelitis. J Neurochem. 2019;148:426–439. doi: 10.1111/jnc.14604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jia M, Zhang H, Qin Q, Hou Y, Zhang X, Chen D, et al. Ferroptosis as a new therapeutic opportunity for nonviral liver disease. Eur J Pharmacol. 2021;908:174319. doi: 10.1016/j.ejphar.2021.174319. [DOI] [PubMed] [Google Scholar]
- 68.Targher G, Byrne CD, Tilg H. MASLD: a systemic metabolic disorder with cardiovascular and malignant complications. Gut. 2024;73:691–702. doi: 10.1136/gutjnl-2023-330595. [DOI] [PubMed] [Google Scholar]
- 69.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASDEASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD) J Hepatol. 2024;81:492–542. doi: 10.1016/j.jhep.2024.04.031. [DOI] [PubMed] [Google Scholar]
- 70.Aron-Wisnewsky J, Vigliotti C, Witjes J, Le P, Holleboom AG, Verheij J, et al. Gut microbiota and human NAFLD: disentangling microbial signatures from metabolic disorders. Nat Rev Gastroenterol Hepatol. 2020;17:279–297. doi: 10.1038/s41575-020-0269-9. [DOI] [PubMed] [Google Scholar]
- 71.Azzu V, Vacca M, Virtue S, Allison M, Vidal-Puig A. adipose tissue-liver cross talk in the control of whole-body metabolism: Implications in nonalcoholic fatty liver disease. Gastroenterology. 2020;158:1899–1912. doi: 10.1053/j.gastro.2019.12.054. [DOI] [PubMed] [Google Scholar]
- 72.Zhang X, Coker OO, Chu ES, Fu K, Lau HCH, Wang YX, et al. Dietary cholesterol drives fatty liver-associated liver cancer by modulating gut microbiota and metabolites. Gut. 2021;70:761–774. doi: 10.1136/gutjnl-2019-319664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aron-Wisnewsky J, Warmbrunn MV, Nieuwdorp M, Clément K. Nonalcoholic fatty liver disease: Modulating gut microbiota to improve severity? Gastroenterology. 2020;158:1881–1898. doi: 10.1053/j.gastro.2020.01.049. [DOI] [PubMed] [Google Scholar]
- 74.Mohamad Nor MH, Ayob N, Mokhtar NM, Raja Ali RA, Tan GC, Wong Z, et al. The effect of probiotics (MCP® BCMC® Strains) on hepatic steatosis, small intestinal mucosal immune function, and intestinal barrier in patients with nonalcoholic fatty liver disease. Nutrients. 2021;13:3192. doi: 10.3390/nu13093192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schoeler M, Caesar R. Dietary lipids, gut microbiota and lipid metabolism. Rev Endocr Metab Disord. 2019;20:461–472. doi: 10.1007/s11154-019-09512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jiao N, Baker SS, Chapa-Rodriguez A, Liu W, Nugent CA, Tsompana M, et al. Suppressed hepatic bile acid signalling despite elevated production of primary and secondary bile acids in NAFLD. Gut. 2018;67:1881–1891. doi: 10.1136/gutjnl-2017-314307. [DOI] [PubMed] [Google Scholar]
- 77.Ji Y, Yin Y, Li Z, Zhang W. Gut microbiota-derived components and metabolites in the progression of non-alcoholic fatty liver disease (NAFLD) Nutrients. 2019;11:1712. doi: 10.3390/nu11081712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jin M, Fang J, Wang JJ, Shao X, Xu SW, Liu PQ, et al. Regulation of toll-like receptor (TLR) signaling pathways in atherosclerosis: from mechanisms to targeted therapeutics. Acta Pharmacol Sin. 2023;44:2358–2375. doi: 10.1038/s41401-023-01123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ochando J, Mulder WJM, Madsen JC, Netea MG, Duivenvoorden R. Trained immunity - basic concepts and contributions to immunopathology. Nat Rev Nephrol. 2023;19:23–37. doi: 10.1038/s41581-022-00633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang S, Xia P, Chen Y, Huang G, Xiong Z, Liu J, et al. Natural Killer-like B cells prime innate lymphocytes against microbial infection. Immunity. 2016;45:131–144. doi: 10.1016/j.immuni.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 81.He Y, Hwang S, Ahmed YA, Feng D, Li N, Ribeiro M, et al. Immunopathobiology and therapeutic targets related to cytokines in liver diseases. Cell Mol Immunol. 2021;18:18–37. doi: 10.1038/s41423-020-00580-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Koenen M, Hill MA, Cohen P, Sowers JR. Obesity, adipose tissue and vascular dysfunction. Circ Res. 2021;128:951–968. doi: 10.1161/CIRCRESAHA.121.318093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rajesh Y, Sarkar D. Association of adipose tissue and adipokines with development of obesity-induced liver cancer. Int J Mol Sci. 2021;22:2163. doi: 10.3390/ijms22042163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Saponaro C, Sabatini S, Gaggini M, Carli F, Rosso C, Positano V, et al. Adipose tissue dysfunction and visceral fat are associated with hepatic insulin resistance and severity of NASH even in lean individuals. Liver Int. 2022;42:2418–2427. doi: 10.1111/liv.15377. [DOI] [PubMed] [Google Scholar]
- 85.Adachi M, Brenner DA. High molecular weight adiponectin inhibits proliferation of hepatic stellate cells via activation of adenosine monophosphate-activated protein kinase. Hepatology. 2008;47:677–685. doi: 10.1002/hep.21991. [DOI] [PubMed] [Google Scholar]
- 86.Chatterjee S, Ganini D, Tokar EJ, Kumar A, Das S, Corbett J, et al. Leptin is key to peroxynitrite-mediated oxidative stress and Kupffer cell activation in experimental non-alcoholic steatohepatitis. J Hepatol. 2013;58:778–784. doi: 10.1016/j.jhep.2012.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Marra F, Svegliati-Baroni G. Lipotoxicity and the gut-liver axis in NASH pathogenesis. J Hepatol. 2018;68:280–295. doi: 10.1016/j.jhep.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 88.Mouton AJ, Li X, Hall ME, Hall JE. Obesity, hypertension, and cardiac dysfunction: Novel roles of immunometabolism in macrophage activation and inflammation. Circ Res. 2020;126:789–806. doi: 10.1161/CIRCRESAHA.119.312321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ni Y, Nagashimada M, Zhan L, Nagata N, Kobori M, Sugiura M, et al. Prevention and reversal of lipotoxicity-induced hepatic insulin resistance and steatohepatitis in mice by an antioxidant carotenoid, β-cryptoxanthin. Endocrinology. 2015;156:987–999. doi: 10.1210/en.2014-1776. [DOI] [PubMed] [Google Scholar]
- 90.Zhao B, Lu R, Chen J, Xie M, Zhao X, Kong L. S100A9 blockade prevents lipopolysaccharide-induced lung injury via suppressing the NLRP3 pathway. Respir Res. 2021;22:45. doi: 10.1186/s12931-021-01641-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pruenster M, Vogl T, Roth J, Sperandio M. S100A8/A9: From basic science to clinical application. Pharmacol Ther. 2016;167:120–131. doi: 10.1016/j.pharmthera.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 92.Cao Y, Liu M, Wu S, Xu J, Wang W, Qi X, et al. Kupffer cells play a crucial role in monocrotaline-induced liver injury by producing TNF-α. Toxicology. 2022;468:153101. doi: 10.1016/j.tox.2022.153101. [DOI] [PubMed] [Google Scholar]
- 93.Choe SS, Huh JY, Hwang IJ, Kim JI, Kim JB. Adipose tissue remodeling: Its role in energy metabolism and metabolic disorders. Front Endocrinol (Lausanne) 2016;7:30. doi: 10.3389/fendo.2016.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kim SJ, Feng D, Guillot A, Dai S, Liu F, Hwang S, et al. Adipocyte death preferentially induces liver injury and inflammation through the activation of chemokine (C-C Motif) receptor 2-positive macrophages and lipolysis. Hepatology. 2019;69:1965–1982. doi: 10.1002/hep.30525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shojaie L, Iorga A, Dara L. Cell death in liver diseases: A review. Int J Mol Sci. 2020;21:9682. doi: 10.3390/ijms21249682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brenner C, Galluzzi L, Kepp O, Kroemer G. Decoding cell death signals in liver inflammation. J Hepatol. 2013;59:583–594. doi: 10.1016/j.jhep.2013.03.033. [DOI] [PubMed] [Google Scholar]
- 97.Schwabe RF, Luedde T. Apoptosis and necroptosis in the liver: a matter of life and death. Nat Rev Gastroenterol Hepatol. 2018;15:738–752. doi: 10.1038/s41575-018-0065-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bernardi S, Toffoli B, Tisato V, Bossi F, Biffi S, Lorenzon A, et al. TRAIL reduces impaired glucose tolerance and NAFLD in the high-fat diet fed mouse. Clin Sci (Lond) 2018;132:69–83. doi: 10.1042/CS20171221. [DOI] [PubMed] [Google Scholar]
- 99.Xu X, Poulsen KL, Wu L, Liu S, Miyata T, Song Q, et al. Targeted therapeutics and novel signaling pathways in nonalcohol-associated fatty liver/steatohepatitis (NAFL/NASH) Signal Transduct Target Ther. 2022;7:287. doi: 10.1038/s41392-022-01119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cho YS, Challa S, Moquin D, Genga R, Ray TD, Guildford M, et al. Phosphorylation-driven assembly of the RIP1-RIP3 complex regulates programmed necrosis and virus-induced inflammation. Cell. 2009;137:1112–1123. doi: 10.1016/j.cell.2009.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Luedde T, Kaplowitz N, Schwabe RF. Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology. 2014;147:765–783. doi: 10.1053/j.gastro.2014.07.018. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Roychowdhury S, McCullough RL, Sanz-Garcia C, Saikia P, Alkhouri N, Matloob A, et al. Receptor interacting protein 3 protects mice from high-fat diet-induced liver injury. Hepatology. 2016;64:1518–1533. doi: 10.1002/hep.28676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yu P, Zhang X, Liu N, Tang L, Peng C, Chen X. Pyroptosis: mechanisms and diseases. Signal Transduct Target Ther. 2021;6:128. doi: 10.1038/s41392-021-00507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Arend WP, Palmer G, Gabay C. IL-1, IL-18, and IL-33 families of cytokines. Immunol Rev. 2008;223:20–38. doi: 10.1111/j.1600-065X.2008.00624.x. [DOI] [PubMed] [Google Scholar]
- 105.Filali-Mouncef Y, Hunter C, Roccio F, Zagkou S, Dupont N, Primard C, et al. The ménage à trois of autophagy, lipid droplets and liver disease. Autophagy. 2022;18:50–72. doi: 10.1080/15548627.2021.1895658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Senft D, Ronai ZA. UPR, autophagy, and mitochondria crosstalk underlies the ER stress response. Trends Biochem Sci. 2015;40:141–148. doi: 10.1016/j.tibs.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lyamzaev KG, Tokarchuk AV, Panteleeva AA, Mulkidjanian AY, Skulachev VP, Chernyak BV. Induction of autophagy by depolarization of mitochondria. Autophagy. 2018;14:921–924. doi: 10.1080/15548627.2018.1436937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mridha AR, Wree A, Robertson AAB, Yeh MM, Johnson CD, Van Rooyen DM, et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol. 2017;66:1037–1046. doi: 10.1016/j.jhep.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Racanelli V, Rehermann B. The liver as an immunological organ. Hepatology. 2006;43(2 Suppl 1):S54–62. doi: 10.1002/hep.21060. [DOI] [PubMed] [Google Scholar]
- 110.Cheng ML, Nakib D, Perciani CT, MacParland SA. The immune niche of the liver. Clin Sci (Lond) 2021;135:2445–2466. doi: 10.1042/CS20190654. [DOI] [PubMed] [Google Scholar]
- 111.Pikarsky E, Heikenwalder M. Focal and local: Ectopic lymphoid structures and aggregates of myeloid and other immune cells in liver. Gastroenterology. 2016;151:780–783. doi: 10.1053/j.gastro.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 112.Saviano A, Henderson NC, Baumert TF. Single-cell genomics and spatial transcriptomics: Discovery of novel cell states and cellular interactions in liver physiology and disease biology. J Hepatol. 2020;73:1219–1230. doi: 10.1016/j.jhep.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kalucka J, de Rooij LPMH, Goveia J, Rohlenova K, Dumas SJ, Meta E, et al. Single-cell transcriptome atlas of murine endothelial cells. Cell. 2020;180:764–779.e20. doi: 10.1016/j.cell.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 114.Zheng C, Zheng L, Yoo JK, Guo H, Zhang Y, Guo X, et al. Landscape of infiltrating T cells in liver cancer revealed by single-cell sequencing. Cell. 2017;169:1342–1356.e16. doi: 10.1016/j.cell.2017.05.035. [DOI] [PubMed] [Google Scholar]
- 115.Zhao J, Zhang S, Liu Y, He X, Qu M, Xu G, et al. Single-cell RNA sequencing reveals the heterogeneity of liver-resident immune cells in human. Cell Discov. 2020;6:22. doi: 10.1038/s41421-020-0157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bogdanos DP, Gao B, Gershwin ME. Liver immunology. Compr Physiol. 2013;3:567–598. doi: 10.1002/cphy.c120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Botía-Sánchez M, Alarcón-Riquelme ME, Galicia G. B Cells and microbiota in autoimmunity. Int J Mol Sci. 2021;22:4846. doi: 10.3390/ijms22094846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gaudin E, Rosado M, Agenes F, McLean A, Freitas AA. Bcell homeostasis, competition, resources, and positive selection by self-antigens. Immunol Rev. 2004;197:102–115. doi: 10.1111/j.0105-2896.2004.0095.x. [DOI] [PubMed] [Google Scholar]
- 119.Catalán D, Mansilla MA, Ferrier A, Soto L, Oleinika K, Aguillón JC, et al. Immunosuppressive mechanisms of regulatory B cells. Front Immunol. 2021;12:611795. doi: 10.3389/fimmu.2021.611795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cargill T, Culver EL. The role of B cells and B cell therapies in immune-mediated liver diseases. Front Immunol. 2021;12:661196. doi: 10.3389/fimmu.2021.661196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Barrow F, Khan S, Fredrickson G, Wang H, Dietsche K, Parthiban P, et al. Microbiota-driven activation of intrahepatic B cells aggravates NASH through innate and adaptive signaling. Hepatology. 2021;74:704–722. doi: 10.1002/hep.31755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bruzzì S, Sutti S, Giudici G, Burlone ME, Ramavath NN, Toscani A, et al. B2-Lymphocyte responses to oxidative stress-derived antigens contribute to the evolution of nonalcoholic fatty liver disease (NAFLD) Free Radic Biol Med. 2018;124:249–259. doi: 10.1016/j.freeradbiomed.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 123.Khan S, Luck H, Winer S, Winer DA. Emerging concepts in intestinal immune control of obesity-related metabolic disease. Nat Commun. 2021;12:2598. doi: 10.1038/s41467-021-22727-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Courey-Ghaouzi AD, Kleberg L, Sundling C. Alternative B cell differentiation during infection and inflammation. Front Immunol. 2022;13:908034. doi: 10.3389/fimmu.2022.908034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sanz I, Wei C, Jenks SA, Cashman KS, Tipton C, Woodruff MC, et al. Challenges and opportunities for consistent classification of human B cell and plasma cell populations. Front Immunol. 2019;10:2458. doi: 10.3389/fimmu.2019.02458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kanemitsu-Okada K, Abe M, Nakamura Y, Miyake T, Watanabe T, Yoshida O, et al. Role of B cell-activating factor in fibrosis progression in a murine model of non-alcoholic steatohepatitis. Int J Mol Sci. 2023;24:2509. doi: 10.3390/ijms24032509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Miyake T, Abe M, Tokumoto Y, Hirooka M, Furukawa S, Kumagi T, et al. B cell-activating factor is associated with the histological severity of nonalcoholic fatty liver disease. Hepatol Int. 2013;7:539–547. doi: 10.1007/s12072-012-9345-8. [DOI] [PubMed] [Google Scholar]
- 128.Nutt SL, Hodgkin PD, Tarlinton DM, Corcoran LM. The generation of antibody-secreting plasma cells. Nat Rev Immunol. 2015;15:160–171. doi: 10.1038/nri3795. [DOI] [PubMed] [Google Scholar]
- 129.Moro-Sibilot L, Blanc P, Taillardet M, Bardel E, Couillault C, Boschetti G, et al. Mouse and human liver contain immunoglobulin A-secreting cells originating from Peyer’s patches and directed against intestinal antigens. Gastroenterology. 2016;151:311–323. doi: 10.1053/j.gastro.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 130.Kotsiliti E, Leone V, Schuehle S, Govaere O, Li H, Wolf MJ, et al. Intestinal B cells license metabolic T-cell activation in NASH microbiota/antigen-independently and contribute to fibrosis by IgA-FcR signalling. J Hepatol. 2023;79:296–313. doi: 10.1016/j.jhep.2023.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Miyake T, Akbar SM, Yoshida O, Chen S, Hiasa Y, Matsuura B, et al. Impaired dendritic cell functions disrupt antigen-specific adaptive immune responses in mice with nonalcoholic fatty liver disease. J Gastroenterol. 2010;45:859–867. doi: 10.1007/s00535-010-0218-4. [DOI] [PubMed] [Google Scholar]
- 132.Morante-Palacios O, Fondelli F, Ballestar E, Martínez-Cáceres EM. Tolerogenic dendritic cells in autoimmunity and inflammatory diseases. Trends Immunol. 2021;42:59–75. doi: 10.1016/j.it.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 133.Sun L, Zhang W, Zhao Y, Wang F, Liu S, Liu L, et al. Dendritic cells and T cells, partners in atherogenesis and the translating road ahead. Front Immunol. 2020;11:1456. doi: 10.3389/fimmu.2020.01456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Huang C, Zhou Y, Cheng J, Guo X, Shou D, Quan Y, et al. Pattern recognition receptors in the development of nonalcoholic fatty liver disease and progression to hepatocellular carcinoma: An emerging therapeutic strategy. Front Endocrinol (Lausanne) 2023;14:1145392. doi: 10.3389/fendo.2023.1145392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lee JS, Jeong SJ, Kim S, Chalifour L, Yun TJ, Miah MA, et al. Conventional dendritic cells impair recovery after myocardial infarction. J Immunol. 2018;201:1784–1798. doi: 10.4049/jimmunol.1800322. [DOI] [PubMed] [Google Scholar]
- 136.Deczkowska A, David E, Ramadori P, Pfister D, Safran M, Li B, et al. XCR1+ type 1 conventional dendritic cells drive liver pathology in non-alcoholic steatohepatitis. Nat Med. 2021;27:1043–1054. doi: 10.1038/s41591-021-01344-3. [DOI] [PubMed] [Google Scholar]
- 137.Deczkowska A, David E, Ramadori P, Pfister D, Safran M, Li B, et al. Publisher correction: XCR1+ type 1 conventional dendritic cells drive liver pathology in non-alcoholic steatohepatitis. Nat Med. 2022;28:214. doi: 10.1038/s41591-021-01668-0. [DOI] [PubMed] [Google Scholar]
- 138.Heier EC, Meier A, Julich-Haertel H, Djudjaj S, Rau M, Tschernig T, et al. Murine CD103+ dendritic cells protect against steatosis progression towards steatohepatitis. J Hepatol. 2017;66:1241–1250. doi: 10.1016/j.jhep.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 139.Hao L, Zhong W, Woo J, Wei X, Ma H, Dong H, et al. Conventional type 1 dendritic cells protect against gut barrier disruption via maintaining Akkermansia muciniphila in alcoholic steatohepatitis. Hepatology. 2023;78:896–910. doi: 10.1097/HEP.0000000000000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chauhan KS, Das A, Jaiswal H, Saha I, Kaushik M, Patel VK, et al. IRF8 and BATF3 interaction enhances the cDC1 specific Pfkfb3 gene expression. Cell Immunol. 2022;371:104468. doi: 10.1016/j.cellimm.2021.104468. [DOI] [PubMed] [Google Scholar]
- 141.Goold HD, Escors D, Conlan TJ, Chakraverty R, Bennett CL. Conventional dendritic cells are required for the activation of helper-dependent CD8 T cell responses to a model antigen after cutaneous vaccination with lentiviral vectors. J Immunol. 2011;186:4565–4572. doi: 10.4049/jimmunol.1002529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Murphy KM, Stockinger B. Effector T cell plasticity: flexibility in the face of changing circumstances. Nat Immunol. 2010;11:674–680. doi: 10.1038/ni.1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Her Z, Tan JHL, Lim YS, Tan SY, Chan XY, Tan WWS, et al. CD4+ T cells mediate the development of liver fibrosis in high fat diet-induced NAFLD in humanized mice. Front Immunol. 2020;11:580968. doi: 10.3389/fimmu.2020.580968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Luo XY, Takahara T, Kawai K, Fujino M, Sugiyama T, Tsuneyama K, et al. IFN-γ deficiency attenuates hepatic inflammation and fibrosis in a steatohepatitis model induced by a methionine- and choline-deficient high-fat diet. Am J Physiol Gastrointest Liver Physiol. 2013;305:G891–G899. doi: 10.1152/ajpgi.00193.2013. [DOI] [PubMed] [Google Scholar]
- 145.Jonsson AH, Zhang F, Dunlap G, Gomez-Rivas E, Watts GFM, Faust HJ, et al. Granzyme K+ CD8 T cells form a core population in inflamed human tissue. Sci Transl Med. 2022;14:eabo0686. doi: 10.1126/scitranslmed.abo0686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wen W, Wu P, Zhang Y, Chen Z, Sun J, Chen H. Comprehensive analysis of NAFLD and the therapeutic target identified. Front Cell Dev Biol. 2021;9:704704. doi: 10.3389/fcell.2021.704704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhang X, Shen J, Man K, Chu ES, Yau TO, Sung JC, et al. CXCL10 plays a key role as an inflammatory mediator and a non-invasive biomarker of non-alcoholic steatohepatitis. J Hepatol. 2014;61:1365–1375. doi: 10.1016/j.jhep.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 148.Zhang X, Han J, Man K, Li X, Du J, Chu ES, et al. CXC chemokine receptor 3 promotes steatohepatitis in mice through mediating inflammatory cytokines, macrophages and autophagy. J Hepatol. 2016;64:160–170. doi: 10.1016/j.jhep.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 149.Van Herck MA, Weyler J, Kwanten WJ, Dirinck EL, De Winter BY, Francque SM, et al. The differential roles of T cells in non-alcoholic fatty liver disease and obesity. Front Immunol. 2019;10:82. doi: 10.3389/fimmu.2019.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Shimamura T, Fujisawa T, Husain SR, Kioi M, Nakajima A, Puri RK. Novel role of IL-13 in fibrosis induced by nonalcoholic steatohepatitis and its amelioration by IL-13R-directed cytotoxin in a rat model. J Immunol. 2008;181:4656–4665. doi: 10.4049/jimmunol.181.7.4656. [DOI] [PubMed] [Google Scholar]
- 151.Gieseck RL 3rd, Wilson MS, Wynn TA. Type 2 immunity in tissue repair and fibrosis. Nat Rev Immunol. 2018;18:62–76. doi: 10.1038/nri.2017.90. [DOI] [PubMed] [Google Scholar]
- 152.Kotsiou OS, Gourgoulianis KI, Zarogiannis SG. IL-33/ST2 axis in organ fibrosis. Front Immunol. 2018;9:2432. doi: 10.3389/fimmu.2018.02432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Tan Z, Liu Q, Jiang R, Lv L, Shoto SS, Maillet I, et al. Interleukin-33 drives hepatic fibrosis through activation of hepatic stellate cells. Cell Mol Immunol. 2018;15:388–398. doi: 10.1038/cmi.2016.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Miossec P, Kolls JK. Targeting IL-17 and TH17 cells in chronic inflammation. Nat Rev Drug Discov. 2012;11:763–776. doi: 10.1038/nrd3794. [DOI] [PubMed] [Google Scholar]
- 155.Moreno-Fernandez ME, Giles DA, Oates JR, Chan CC, Damen MSMA, Doll JR, et al. PKM2-dependent metabolic skewing of hepatic Th17 cells regulates pathogenesis of nonalcoholic fatty liver disease. Cell Metab. 2021;33:1187–1204.e9. doi: 10.1016/j.cmet.2021.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.West EE, Kolev M, Kemper C. Complement and the regulation of T cell responses. Annu Rev Immunol. 2018;36:309–338. doi: 10.1146/annurev-immunol-042617-053245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Taniki N, Nakamoto N, Chu PS, Ichikawa M, Teratani T, Kanai T. Th17 cells in the liver: balancing autoimmunity and pathogen defense. Semin Immunopathol. 2022;44:509–526. doi: 10.1007/s00281-022-00917-9. [DOI] [PubMed] [Google Scholar]
- 158.Gomes AL, Teijeiro A, Burén S, Tummala KS, Yilmaz M, Waisman A, et al. Metabolic inflammation-associated IL-17A causes non-alcoholic steatohepatitis and hepatocellular carcinoma. Cancer Cell. 2016;30:161–175. doi: 10.1016/j.ccell.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 159.Kaech SM, Cui W. Transcriptional control of effector and memory CD8+ T cell differentiation. Nat Rev Immunol. 2012;12:749–761. doi: 10.1038/nri3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Montacchiesi G, Pace L. Epigenetics and CD8+ T cell memory. Immunol Rev. 2022;305:77–89. doi: 10.1111/imr.13057. [DOI] [PubMed] [Google Scholar]
- 161.Wang B, Wang Y, Sun X, Deng G, Huang W, Wu X, et al. CXCR6 is required for antitumor efficacy of intratumoral CD8+ T cell. J Immunother Cancer. 2021;9:e003100. doi: 10.1136/jitc-2021-003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wolf MJ, Adili A, Piotrowitz K, Abdullah Z, Boege Y, Stemmer K, et al. Metabolic activation of intrahepatic CD8+ T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell. 2014;26:549–564. doi: 10.1016/j.ccell.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 163.Badovinac VP, Hamilton SE, Harty JT. Viral infection results in massive CD8+ T cell expansion and mortality in vaccinated perforin-deficient mice. Immunity. 2003;18:463–474. doi: 10.1016/s1074-7613(03)00079-7. [DOI] [PubMed] [Google Scholar]
- 164.Gulzar N, Copeland KF. CD8+ T-cells: function and response to HIV infection. Curr HIV Res. 2004;2:23–37. doi: 10.2174/1570162043485077. [DOI] [PubMed] [Google Scholar]
- 165.Terrell CE, Jordan MB. Perforin deficiency impairs a critical immunoregulatory loop involving murine CD8(+) T cells and dendritic cells. Blood. 2013;121:5184–5191. doi: 10.1182/blood-2013-04-495309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Boissonnas A, Scholer-Dahirel A, Simon-Blancal V, Pace L, Valet F, Kissenpfennig A, et al. Foxp3+ T cells induce perforin-dependent dendritic cell death in tumor-draining lymph nodes. Immunity. 2010;32:266–278. doi: 10.1016/j.immuni.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 167.Pfister D, Núñez NG, Pinyol R, Govaere O, Pinter M, Szydlowska M, et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature. 2021;592:450–456. doi: 10.1038/s41586-021-03362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Wang H, Zhang H, Wang Y, Brown ZJ, Xia Y, Huang Z, et al. Regulatory T-cell and neutrophil extracellular trap interaction contributes to carcinogenesis in non-alcoholic steatohepatitis. J Hepatol. 2021;75:1271–1283. doi: 10.1016/j.jhep.2021.07.032. [DOI] [PubMed] [Google Scholar]
- 169.Zhou Y, Zhang H, Yao Y, Zhang X, Guan Y, Zheng F. CD4+ T cell activation and inflammation in NASH-related fibrosis. Front Immunol. 2022;13:967410. doi: 10.3389/fimmu.2022.967410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.O’Leary K. T cell drivers in NASH-HCC. Nat Rev Cancer. 2021;21:341. doi: 10.1038/s41568-021-00362-0. [DOI] [PubMed] [Google Scholar]
- 171.Maccioni L, Loriot A, Dewulf J, Bommer G, Horsmans Y, Lanthier N, et al. Duodenal CD8+ T resident memory cell apoptosis contributes to gut barrier dysfunction and microbial translocation in early alcohol-associated liver disease in humans. Aliment Pharmacol Ther. 2022;56:1055–1070. doi: 10.1111/apt.17177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Gu X, Chu Q, Ma X, Wang J, Chen C, Guan J, et al. New insights into iNKT cells and their roles in liver diseases. Front Immunol. 2022;13:1035950. doi: 10.3389/fimmu.2022.1035950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Syn WK, Agboola KM, Swiderska M, Michelotti GA, Liaskou E, Pang H, et al. NKT-associated hedgehog and osteopontin drive fibrogenesis in non-alcoholic fatty liver disease. Gut. 2012;61:1323–1329. doi: 10.1136/gutjnl-2011-301857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Diao H, Kon S, Iwabuchi K, Kimura C, Morimoto J, Ito D, et al. Osteopontin as a mediator of NKT cell function in T cellmediated liver diseases. Immunity. 2004;21:539–550. doi: 10.1016/j.immuni.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 175.Kumar V. NKT-cell subsets: promoters and protectors in inflammatory liver disease. J Hepatol. 2013;59:618–620. doi: 10.1016/j.jhep.2013.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Konduri V, Oyewole-Said D, Vazquez-Perez J, Weldon SA, Halpert MM, Levitt JM, et al. CD8+CD161+ T-cells: Cytotoxic memory cells with high therapeutic potential. Front Immunol. 2021;11:613204. doi: 10.3389/fimmu.2020.613204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lee YJ, Holzapfel KL, Zhu J, Jameson SC, Hogquist KA. Steady-state production of IL-4 modulates immunity in mouse strains and is determined by lineage diversity of iNKT cells. Nat Immunol. 2013;14:1146–1154. doi: 10.1038/ni.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Li F, Hao X, Chen Y, Bai L, Gao X, Lian Z, et al. Erratum: The microbiota maintain homeostasis of liver-resident γδT-17 cells in a lipid antigen/CD1d-dependent manner. Nat Commun. 2017;8:15265. doi: 10.1038/ncomms15265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Li F, Hao X, Chen Y, Bai L, Gao X, Lian Z, et al. The microbiota maintain homeostasis of liver-resident γδT-17 cells in a lipid antigen/CD1d-dependent manner. Nat Commun. 2017;7:13839. doi: 10.1038/ncomms13839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Naimimohasses S, O’Gorman P, Wright C, Ni Fhloinn D, Holden D, Conlon N, et al. Differential effects of dietary versus exercise intervention on intrahepatic MAIT cells and histological features of NAFLD. Nutrients. 2022;14:2198. doi: 10.3390/nu14112198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Mabire M, Hegde P, Hammoutene A, Wan J, Caër C, Sayegh RA, et al. MAIT cell inhibition promotes liver fibrosis regression via macrophage phenotype reprogramming. Nat Commun. 2023;14:1830. doi: 10.1038/s41467-023-37453-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Wallace SJ, Tacke F, Schwabe RF, Henderson NC. Understanding the cellular interactome of non-alcoholic fatty liver disease. JHEP Rep. 2022;4:100524. doi: 10.1016/j.jhepr.2022.100524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hegde P, Weiss E, Paradis V, Wan J, Mabire M, Sukriti S, et al. Mucosal-associated invariant T cells are a profibrogenic immune cell population in the liver. Nat Commun. 2018;9:2146. doi: 10.1038/s41467-018-04450-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Semple JW, Italiano JE, Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11:264–274. doi: 10.1038/nri2956. [DOI] [PubMed] [Google Scholar]
- 185.Wong CH, Jenne CN, Petri B, Chrobok NL, Kubes P. Nucleation of platelets with blood-borne pathogens on Kupffer cells precedes other innate immunity and contributes to bacterial clearance. Nat Immunol. 2013;14:785–792. doi: 10.1038/ni.2631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Huo Y, Schober A, Forlow SB, Smith DF, Hyman MC, Jung S, et al. Circulating activated platelets exacerbate atherosclerosis in mice deficient in apolipoprotein E. Nat Med. 2003;9:61–67. doi: 10.1038/nm810. [DOI] [PubMed] [Google Scholar]
- 187.Fujita K, Nozaki Y, Wada K, Yoneda M, Endo H, Takahashi H, et al. Effectiveness of antiplatelet drugs against experimental non-alcoholic fatty liver disease. Gut. 2008;57:1583–1591. doi: 10.1136/gut.2007.144550. [DOI] [PubMed] [Google Scholar]
- 188.Malehmir M, Pfister D, Gallage S, Szydlowska M, Inverso D, Kotsiliti E, et al. Platelet GPIbα is a mediator and potential interventional target for NASH and subsequent liver cancer. Nat Med. 2019;25:641–655. doi: 10.1038/s41591-019-0379-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Jorch SK, Kubes P. An emerging role for neutrophil extracellular traps in noninfectious disease. Nat Med. 2017;23:279–287. doi: 10.1038/nm.4294. [DOI] [PubMed] [Google Scholar]
- 190.Papayannopoulos V. Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol. 2018;18:134–147. doi: 10.1038/nri.2017.105. [DOI] [PubMed] [Google Scholar]
- 191.Gadd VL, Skoien R, Powell EE, Fagan KJ, Winterford C, Horsfall L, et al. The portal inflammatory infiltrate and ductular reaction in human nonalcoholic fatty liver disease. Hepatology. 2014;59:1393–1405. doi: 10.1002/hep.26937. [DOI] [PubMed] [Google Scholar]
- 192.Zang S, Wang L, Ma X, Zhu G, Zhuang Z, Xun Y, et al. Neutrophils play a crucial role in the early stage of nonalcoholic steatohepatitis via neutrophil elastase in mice. Cell Biochem Biophys. 2015;73:479–487. doi: 10.1007/s12013-015-0682-9. [DOI] [PubMed] [Google Scholar]
- 193.van der Windt DJ, Sud V, Zhang H, Varley PR, Goswami J, Yazdani HO, et al. Neutrophil extracellular traps promote inflammation and development of hepatocellular carcinoma in nonalcoholic steatohepatitis. Hepatology. 2018;68:1347–1360. doi: 10.1002/hep.29914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Guilliams M, Scott CL. Liver macrophages in health and disease. Immunity. 2022;55:1515–1529. doi: 10.1016/j.immuni.2022.08.002. [DOI] [PubMed] [Google Scholar]
- 195.Heymann F, Tacke F. Immunology in the liver--from homeostasis to disease. Nat Rev Gastroenterol Hepatol. 2016;13:88–110. doi: 10.1038/nrgastro.2015.200. [DOI] [PubMed] [Google Scholar]
- 196.Scott CL, Zheng F, De Baetselier P, Martens L, Saeys Y, De Prijck S, et al. Bone marrow-derived monocytes give rise to self-renewing and fully differentiated Kupffer cells. Nat Commun. 2016;7:10321. doi: 10.1038/ncomms10321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Krenkel O, Tacke F. Liver macrophages in tissue homeostasis and disease. Nat Rev Immunol. 2017;17:306–321. doi: 10.1038/nri.2017.11. [DOI] [PubMed] [Google Scholar]
- 198.Krenkel O, Hundertmark J, Abdallah AT, Kohlhepp M, Puengel T, Roth T, et al. Myeloid cells in liver and bone marrow acquire a functionally distinct inflammatory phenotype during obesity-related steatohepatitis. Gut. 2020;69:551–563. doi: 10.1136/gutjnl-2019-318382. [DOI] [PubMed] [Google Scholar]
- 199.Seidman JS, Troutman TD, Sakai M, Gola A, Spann NJ, Bennett H, et al. Niche-specific reprogramming of epigenetic landscapes drives myeloid cell diversity in nonalcoholic steatohepatitis. Immunity. 2020;52:1057–1074.e7. doi: 10.1016/j.immuni.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Jaitin DA, Adlung L, Thaiss CA, Weiner A, Li B, Descamps H, et al. Lipid-associated macrophages control metabolic homeostasis in a Trem2-dependent manner. Cell. 2019;178:686–698.e14. doi: 10.1016/j.cell.2019.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Remmerie A, Martens L, Thoné T, Castoldi A, Seurinck R, Pavie B, et al. Osteopontin expression identifies a subset of recruited macrophages distinct from kupffer cells in the fatty liver. Immunity. 2020;53:641–657.e14. doi: 10.1016/j.immuni.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ramachandran P, Dobie R, Wilson-Kanamori JR, Dora EF, Henderson BEP, Luu NT, et al. Resolving the fibrotic niche of human liver cirrhosis at single-cell level. Nature. 2019;575:512–518. doi: 10.1038/s41586-019-1631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Friedman SL, Neuschwander-Tetri BA, Rinella M, Sanyal AJ. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24:908–922. doi: 10.1038/s41591-018-0104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Anstee QM, Reeves HL, Kotsiliti E, Govaere O, Heikenwalder M. From NASH to HCC: current concepts and future challenges. Nat Rev Gastroenterol Hepatol. 2019;16:411–428. doi: 10.1038/s41575-019-0145-7. [DOI] [PubMed] [Google Scholar]
- 205.Shalapour S, Lin XJ, Bastian IN, Brain J, Burt AD, Aksenov AA, et al. Inflammation-induced IgA+ cells dismantle anti-liver cancer immunity. Nature. 2017;551:340–345. doi: 10.1038/nature24302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ma C, Kesarwala AH, Eggert T, Medina-Echeverz J, Kleiner DE, Jin P, et al. NAFLD causes selective CD4(+) T lymphocyte loss and promotes hepatocarcinogenesis. Nature. 2016;531:253–257. doi: 10.1038/nature16969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ma HY, Yamamoto G, Xu J, Liu X, Karin D, Kim JY, et al. IL-17 signaling in steatotic hepatocytes and macrophages promotes hepatocellular carcinoma in alcohol-related liver disease. J Hepatol. 2020;72:946–959. doi: 10.1016/j.jhep.2019.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Peiseler M, Schwabe R, Hampe J, Kubes P, Heikenwälder M, Tacke F. Immune mechanisms linking metabolic injury to inflammation and fibrosis in fatty liver disease - novel insights into cellular communication circuits. J Hepatol. 2022;77:1136–1160. doi: 10.1016/j.jhep.2022.06.012. [DOI] [PubMed] [Google Scholar]
- 209.Gawrieh S, Dasarathy S, Tu W, Kamath PS, Chalasani NP, McClain CJ, et al. Randomized trial of anakinra plus zinc vs. prednisone for severe alcohol-associated hepatitis. J Hepatol. 2024;80:684–693. doi: 10.1016/j.jhep.2024.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Sharma P, Kumar A, Sharma BC, Sarin SK. Infliximab monotherapy for severe alcoholic hepatitis and predictors of survival: an open label trial. J Hepatol. 2009;50:584–591. doi: 10.1016/j.jhep.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 211.Naranjo CA, Kadlec KE, Sanhueza P, Woodley-Remus D, Sellers EM. Enalapril effects on alcohol intake and other consummatory behaviors in alcoholics. Clin Pharmacol Ther. 1991;50:96–106. doi: 10.1038/clpt.1991.108. [DOI] [PubMed] [Google Scholar]
- 212.Zein CO, Lopez R, Fu X, Kirwan JP, Yerian LM, McCullough AJ, et al. Pentoxifylline decreases oxidized lipid products in nonalcoholic steatohepatitis: new evidence on the potential therapeutic mechanism. Hepatology. 2012;56:1291–1299. doi: 10.1002/hep.25778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Baniasadi N, Salajegheh F, Pardakhty A, Seyedmirzaee SM, Hayatbakhsh MM, Nikpoor AR, et al. Effects of pentoxifylline on non-alcoholic steatohepatitis: A randomized, double-blind, placebo-controlled trial in Iran. Hepat Mon. 2015;15:e32418. doi: 10.5812/hepatmon.32418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ray S, Huang E, West GA, Mrdjen M, McMullen MR, de la Motte C, et al. 35kDa hyaluronan ameliorates ethanol driven loss of anti-microbial defense and intestinal barrier integrity in a TLR4-dependent manner. Matrix Biol. 2023;115:71–80. doi: 10.1016/j.matbio.2022.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Saikia P, Roychowdhury S, Bellos D, Pollard KA, McMullen MR, McCullough RL, et al. Hyaluronic acid 35 normalizes TLR4 signaling in Kupffer cells from ethanol-fed rats via regulation of microRNA291b and its target Tollip. Sci Rep. 2017;7:15671. doi: 10.1038/s41598-017-15760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Farrell GC, van Rooyen D, Gan L, Chitturi S. NASH is an inflammatory disorder: Pathogenic, Prognostic and therapeutic implications. Gut Liver. 2012;6:149–171. doi: 10.5009/gnl.2012.6.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Nelson JE, Roth CL, Wilson LA, Yates KP, Aouizerat B, Morgan-Stevenson V, et al. Vitamin D deficiency is associated with increased risk of non-alcoholic steatohepatitis in adults with non-alcoholic fatty liver disease: Possible role for MAPK and NF-κB? Am J Gastroenterol. 2016;111:852–863. doi: 10.1038/ajg.2016.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Younossi ZM, Ratziu V, Loomba R, Rinella M, Anstee QM, Goodman Z, et al. Obeticholic acid for the treatment of nonalcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2019;394:2184–2196. doi: 10.1016/S0140-6736(19)33041-7. [DOI] [PubMed] [Google Scholar]
- 219.Neuschwander-Tetri BA, Loomba R, Sanyal AJ, Lavine JE, Van Natta ML, Abdelmalek MF, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebocontrolled trial. Lancet. 2015;385:956–965. doi: 10.1016/S0140-6736(14)61933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Ratziu V, Rinella ME, Neuschwander-Tetri BA, Lawitz E, Denham D, Kayali Z, et al. EDP-305 in patients with NASH: A phase II double-blind placebo-controlled dose-ranging study. J Hepatol. 2022;76:506–517. doi: 10.1016/j.jhep.2021.10.018. [DOI] [PubMed] [Google Scholar]
- 221.Rotman Y, Sanyal AJ. Current and upcoming pharmacotherapy for non-alcoholic fatty liver disease. Gut. 2017;66:180–190. doi: 10.1136/gutjnl-2016-312431. [DOI] [PubMed] [Google Scholar]
- 222.Thursz M, Morgan TR. Treatment of severe alcoholic hepatitis. Gastroenterology. 2016;150:1823–1834. doi: 10.1053/j.gastro.2016.02.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Lake-Bakaar G. Glucocorticoids plus N-acetylcysteine in alcoholic hepatitis. N Engl J Med. 2012;366:476–477. doi: 10.1056/NEJMc1114239. author reply 477. [DOI] [PubMed] [Google Scholar]
- 224.Tkachenko P, Maevskaya M, Pavlov A, Komkova I, Pavlov C, Ivashkin V. Prednisolone plus S-adenosil-L-methionine in severe alcoholic hepatitis. Hepatol Int. 2016;10:983–987. doi: 10.1007/s12072-016-9751-4. [DOI] [PubMed] [Google Scholar]
- 225.Lieber CS. Alcoholic liver disease: new insights in pathogenesis lead to new treatments. J Hepatol. 2000;32(1 Suppl):113–128. doi: 10.1016/s0168-8278(00)80420-1. [DOI] [PubMed] [Google Scholar]
- 226.Xia SW, Wang ZM, Sun SM, Su Y, Li ZH, Shao JJ, et al. Endoplasmic reticulum stress and protein degradation in chronic liver disease. Pharmacol Res. 2020;161:105218. doi: 10.1016/j.phrs.2020.105218. [DOI] [PubMed] [Google Scholar]
- 227.Harrison SA, Wong VW, Okanoue T, Bzowej N, Vuppalanchi R, Younes Z, et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: Results from randomized phase III STELLAR trials. J Hepatol. 2020;73:26–39. doi: 10.1016/j.jhep.2020.02.027. [DOI] [PubMed] [Google Scholar]
- 228.Loomba R, Lawitz E, Mantry PS, Jayakumar S, Caldwell SH, Arnold H, et al. The ASK1 inhibitor selonsertib in patients with nonalcoholic steatohepatitis: A randomized, phase 2 trial. Hepatology. 2018;67:549–559. doi: 10.1002/hep.29514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Vogli S, Naska A, Marinos G, Kasdagli MI, Orfanos P. The effect of vitamin E supplementation on serum aminotransferases in non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis. Nutrients. 2023;15:3733. doi: 10.3390/nu15173733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Seo J, Kwon D, Kim SH, Byun MR, Lee YH, Jung YS. Role of autophagy in betaine-promoted hepatoprotection against non-alcoholic fatty liver disease in mice. Curr Res Food Sci. 2023;8:100663. doi: 10.1016/j.crfs.2023.100663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Mueller M, Castro RE, Thorell A, Marschall HU, Auer N, Herac M, et al. Ursodeoxycholic acid: Effects on hepatic unfolded protein response, apoptosis and oxidative stress in morbidly obese patients. Liver Int. 2018;38:523–531. doi: 10.1111/liv.13562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Moreau R, Rautou PE. G-CSF therapy for severe alcoholic hepatitis: targeting liver regeneration or neutrophil function? Am J Gastroenterol. 2014;109:1424–1426. doi: 10.1038/ajg.2014.250. [DOI] [PubMed] [Google Scholar]
- 233.Morgan TR. Is granulocyte colony stimulating factor a new treatment for alcoholic hepatitis? Clin Gastroenterol Hepatol. 2018;16:1564–1565. doi: 10.1016/j.cgh.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 234.Arab JP, Sehrawat TS, Simonetto DA, Verma VK, Feng D, Tang T, et al. An open-label, dose-escalation study to assess the safety and efficacy of IL-22 agonist F-652 in patients with alcohol-associated hepatitis. Hepatology. 2020;72:441–453. doi: 10.1002/hep.31046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Dong X, Lu S, Tian Y, Ma H, Wang Y, Zhang X, et al. Bavachinin protects the liver in NAFLD by promoting regeneration via targeting PCNA. J Adv Res. 2024;55:131–144. doi: 10.1016/j.jare.2023.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Benedé-Ubieto R, Cubero FJ, Nevzorova YA. Breaking the barriers: the role of gut homeostasis in Metabolic-Associated Steatotic Liver Disease (MASLD) Gut Microbes. 2024;16:2331460. doi: 10.1080/19490976.2024.2331460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Dubinkina VB, Tyakht AV, Odintsova VY, Yarygin KS, Kovarsky BA, Pavlenko AV, et al. Links of gut microbiota composition with alcohol dependence syndrome and alcoholic liver disease. Microbiome. 2017;5:141. doi: 10.1186/s40168-017-0359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Vatsalya V, Feng W, Kong M, Hu H, Szabo G, McCullough A, et al. The beneficial effects of lactobacillus GG therapy on liver and drinking assessments in patients with moderate alcohol-associated hepatitis. Am J Gastroenterol. 2023;118:1457–1460. doi: 10.14309/ajg.0000000000002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Hong M, Kim SW, Han SH, Kim DJ, Suk KT, Kim YS, et al. Probiotics (Lactobacillus rhamnosus R0011 and acidophilus R0052) reduce the expression of toll-like receptor 4 in mice with alcoholic liver disease. PLoS One. 2015;10:e0117451. doi: 10.1371/journal.pone.0117451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Bang CS, Hong SH, Suk KT, Kim JB, Han SH, Sung H, et al. Effects of Korean Red Ginseng (Panax ginseng), urushiol (Rhus vernicifera Stokes), and probiotics (Lactobacillus rhamnosus R0011 and Lactobacillus acidophilus R0052) on the gut-liver axis of alcoholic liver disease. J Ginseng Res. 2014;38:167–172. doi: 10.1016/j.jgr.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Forrest E, Bernal W. The role of prophylactic antibiotics for patients with severe alcohol-related hepatitis. JAMA. 2023;329:1552–1553. doi: 10.1001/jama.2023.1729. [DOI] [PubMed] [Google Scholar]
- 242.Louvet A, Labreuche J, Dao T, Thévenot T, Oberti F, Bureau C, et al. Effect of prophylactic antibiotics on mortality in severe alcohol-related hepatitis: A randomized clinical trial. JAMA. 2023;329:1558–1566. doi: 10.1001/jama.2023.4902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Jena PK, Sheng L, Li Y, Wan YY. Probiotics VSL#3 are effective in reversing non-alcoholic steatohepatitis in a mouse model. Hepatobiliary Surg Nutr. 2020;9:170–182. doi: 10.21037/hbsn.2019.09.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Alisi A, Bedogni G, Baviera G, Giorgio V, Porro E, Paris C, et al. Randomised clinical trial: The beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2014;39:1276–1285. doi: 10.1111/apt.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Bomhof MR, Parnell JA, Ramay HR, Crotty P, Rioux KP, Probert CS, et al. Histological improvement of non-alcoholic steatohepatitis with a prebiotic: a pilot clinical trial. Eur J Nutr. 2019;58:1735–1745. doi: 10.1007/s00394-018-1721-2. [DOI] [PubMed] [Google Scholar]
- 246.Reimer RA, Soto-Vaca A, Nicolucci AC, Mayengbam S, Park H, Madsen KL, et al. Effect of chicory inulin-type fructancontaining snack bars on the human gut microbiota in low dietary fiber consumers in a randomized crossover trial. Am J Clin Nutr. 2020;111:1286–1296. doi: 10.1093/ajcn/nqaa074. [DOI] [PubMed] [Google Scholar]
- 247.Wu WC, Zhao W, Li S. Small intestinal bacteria overgrowth decreases small intestinal motility in the NASH rats. World J Gastroenterol. 2008;14:313–317. doi: 10.3748/wjg.14.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Cobbold JFL, Atkinson S, Marchesi JR, Smith A, Wai SN, Stove J, et al. Rifaximin in non-alcoholic steatohepatitis: An open-label pilot study. Hepatol Res. 2018;48:69–77. doi: 10.1111/hepr.12904. [DOI] [PubMed] [Google Scholar]
- 249.Shasthry SM. Fecal microbiota transplantation in alcohol related liver diseases. Clin Mol Hepatol. 2020;26:294–301. doi: 10.3350/cmh.2020.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Bajaj JS, Gavis EA, Fagan A, Wade JB, Thacker LR, Fuchs M, Pet al. A randomized clinical trial of fecal microbiota transplant for alcohol use disorder. Hepatology. 2021;73:1688–1700. doi: 10.1002/hep.31496. [DOI] [PubMed] [Google Scholar]
- 251.Pande A, Sharma S, Khillan V, Rastogi A, Arora V, Shasthry SM, et al. Fecal microbiota transplantation compared with prednisolone in severe alcoholic hepatitis patients: a randomized trial. Hepatol Int. 2023;17:249–261. doi: 10.1007/s12072-022-10438-0. [DOI] [PubMed] [Google Scholar]
- 252.Xue L, Deng Z, Luo W, He X, Chen Y. Effect of fecal microbiota transplantation on non-alcoholic fatty liver disease: A randomized clinical trial. Front Cell Infect Microbiol. 2022;12:759306. doi: 10.3389/fcimb.2022.759306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Stols-Gonçalves D, Mak AL, Madsen MS, van der Vossen EWJ, Bruinstroop E, Henneman P, et al. Faecal Microbiota transplantation affects liver DNA methylation in Non-alcoholic fatty liver disease: a multi-omics approach. Gut Microbes. 2023;15:2223330. doi: 10.1080/19490976.2023.2223330. [DOI] [PMC free article] [PubMed] [Google Scholar]