Abstract
Purpose
There is a high possibility of trauma patients being referred to an unsuitable medical institution for their rehabilitation treatment since the decision is made by them. This study sought to develop a standardized scale to evaluate the need for specialized rehabilitation in patients with multiple traumas and evaluate the effectiveness of the developed scale.
Methods
This study employed a systematic review of existing literature to inform the development of a specialized rehabilitation evaluation scale. An expert panel consisting of trauma surgeons, orthopedic surgeons, and rehabilitation medicine physicians collaborated to create a discharge-planning checklist by assessing the need for specialized rehabilitation. The checklist was validated using retrospective data from trauma patients treated at Seoul National University Hospital.
Results
We identified 12 studies, providing factors influencing the discharge location and rehabilitation needs of trauma patients. The checklist was developed through expert consensus and comprised 3 criteria: discharge feasibility to specialized rehabilitation facilities, diagnostic eligibility for specialized rehabilitation, and functional assessment. Validation of the checklist demonstrated that the percentage agreement, likelihood ratio of a positive test, and Cohen’s kappa value were 82.1%, 5.21, and 0.375, respectively when comparing whether the checklist was met and the actual discharge location, indicating its effectiveness.
Conclusion
This study established standardized criteria for assessing the need for specialized rehabilitation in trauma patients, offering a practical tool for clinical use. Implementation of this assessment scale has the potential to improve the trajectory of trauma survivors by facilitating access to appropriate rehabilitation services.
Keywords: Wounds and injuries, Patient discharge, Patient selection, Rehabilitation
INTRODUCTION
Care of injured patients is based on appropriate, timely, and accurate interventions through each link in the trauma chain of survival [1]. The trauma chain of survival consists of early first aid to prevent immediate deterioration, early basic/advanced life support to secure vital functions, early advanced therapy to limit or repair injury, and early rehabilitation to restore the quality of life [1].
To date, optimizing resuscitative strategies and training in surgical techniques have been emphasized in the trauma chain of survival, and this is something domestic trauma centers have been working on. Due to these efforts, the trauma survival rate has improved [2]. However, as the number of trauma survivors is increasing in Korea, attention has been paid to appropriate rehabilitation to restore quality of life, which is the last chain of trauma survival.
Until recently, surgeons did not pay much attention to the process of patients recovering their function and returning to society after surgery. Typically, the responsibility of the patient and their family is to determine the appropriate hospital for post-acute treatment upon discharge, with support often provided by referral centers.
Patients with diseases that do not require rehabilitation may decide whether to go home or to another nursing facility, based on their perceived needs. However, for trauma patients, there is a high possibility that they may be referred to an unsuitable medical institution for rehabilitation treatment if they decide where to go on their own because rehabilitation needs cannot be decided subjectively by the patient. Insufficient or delayed rehabilitation can affect the final functional outcomes of patients [3,4]. Therefore, it is reasonable to assert that the role of trauma surgeons includes connecting trauma survivors to the appropriate rehabilitation facilities.
The functional assessment tools for establishing discharge plans after acute treatment are limited to specific diseases. Examples include the National Institutes of Health Stroke Scale [5], Activity Measure for Post-Acute Care (AM-PAC) [6], and Predicting Location after Arthroplasty Nomogram [7]. To the best of our knowledge, there is no standardized evaluation tool for determining the discharge location of patients with polytrauma after acute treatment. It is presumed that in Korea, many patients with multiple traumas are transferred to hospitals that are not appropriate for their rehabilitation needs in the post-acute treatment stage. Moreover, the absence of an objective standard to determine whether a patient has been linked to an appropriate rehabilitation institution makes it difficult to determine their current domestic status. To prevent insufficient rehabilitation treatment, there is an urgent need to develop a scale to evaluate trauma patients who require specialized rehabilitation. Therefore, this study sought to develop a standardized scale to evaluate the need for specialized rehabilitation in patients with trauma and to evaluate the effectiveness of the developed scale.
METHODS
First, a systematic review of the literature was conducted to develop a scale to evaluate the rehabilitation needs of patients with trauma. A scale to evaluate the need for specialized rehabilitation was developed with reference to the selected literature, and a retrospective medical record survey was conducted to evaluate the effectiveness of the developed scale. This study was approved by the Institutional Review Board of Seoul National University Hospital (No. 2210-008-1364).
Systematic review
Inclusion and exclusion criteria
Among studies targeting adults (≥18 years old) hospitalized for multiple traumas, those that analyzed factors predicting discharge location, assessed the need for specialized rehabilitation, or described methods for establishing discharge plans were included. All study types were considered eligible for inclusion. Studies were excluded if they focused on isolated injuries or if the design did not match. Articles that were not written in English or Korean were also excluded.
Search strategy
A literature search was performed using PubMed, Embase, and Cochrane Library. Further search strategies included manual searching of the reference lists of potential articles in Google Scholar and KoreaMed. The search was conducted in May 2022 using a combination of 4 themes: multiple trauma/injury, rehabilitation, discharge/disposition, and prediction/planning. A full description of the key search terms used to identify the potential studies is provided in Supplementary Tables 1, 2, 3.
Study selection
After removing duplicates, 2 reviewers (YJJ and YRC) independently screened all titles and abstracts using the inclusion and exclusion criteria. The inclusion criteria and study design of the articles for which the full text was available were reviewed. The reviewers recorded the reasons for the exclusion. The screening was conducted in 2 rounds, and disagreements were discussed with a third reviewer (SAL). The reviewers shortlisted articles that were deemed eligible after reviewing the full text.
Data extraction
Data were extracted by 2 authors (YJJ and YRC) using the standard pro forma. The information obtained from all included studies included authors, publication year, trauma type, sample size, data source, discharge location, and predictive factors for discharge location.
Discharge checklist development
To develop the scale, an expert group consisting of 3 trauma surgeons, 3 orthopedic surgeons, and 3 rehabilitation medicine physicians was formed (Supplementary Table 4). A group of experts systematically reviewed the content extracted from the selected studies. A discussion was held regarding the classification of discharge locations, timing, methods, and criteria for assessing rehabilitation needs. A consensus was reached to create new standards suitable for Korea using the nominal group technique [8].
Validation of the checklist
The study subjects were patients who visited Seoul National University Hospital between September 2021 and August 2022. Patients who died after acute treatment, were discharged from the emergency room without being hospitalized, or were under 18 years of age were excluded from data collection. Data on the study subjects’ demographics, injury severity score (ISS), diagnosis and operation, admission to the intensive care unit (ICU), length of hospitalization, discharge location, reason for disposition, and all items in the checklist were collected.
Discharge locations were classified into 5 categories: specialized rehabilitation facilities (SRF); rehabilitation facilities other than SRF; tertiary referral hospitals; secondary, primary, and nursing hospitals; and homes. An SRF was defined as a hospital designated by the Ministry of Health and Welfare that meets specific standards for facilities, equipment, and medical personnel.
To evaluate the effectiveness of the checklist, the sensitivity, specificity, negative predictive value, positive predictive value, percent agreement, likelihood ratio of the positive test, and Cohen’s kappa value were evaluated by comparing whether the checklist met the actual discharge location. If the checklist results and the actual location after discharge did not match, the reason was collected. IBM SPSS Statistics ver. 24.0 (IBM Corp.) was used for the statistical analysis.
RESULTS
Systematic review
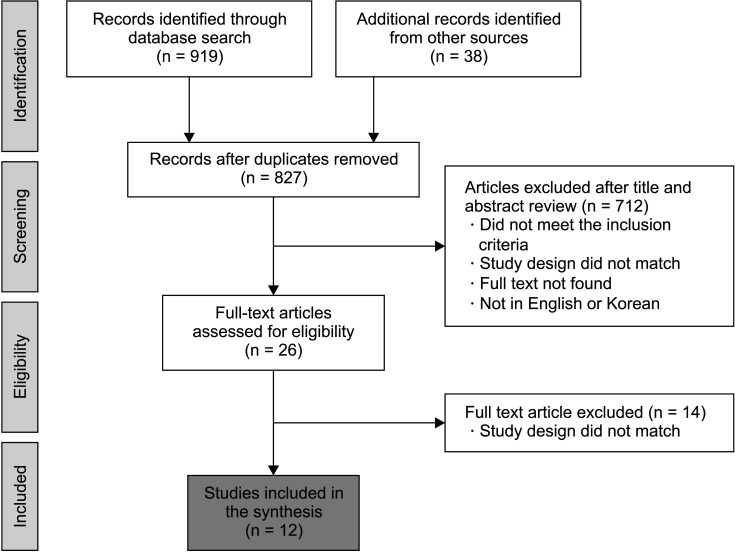
The search identified 957 titles: 333 from PubMed, 572 from Embase, 14 from Cochrane Library, 28 from Google Scholar, and 10 from KoreaMed. After removing duplicates, 827 articles were screened for assessment. Reviewers excluded 712 abstracts after 2 rounds of screening. Through a full-text review, 12 studies fulfilled the inclusion criteria for a total of 26 articles. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram is shown in Fig. 1.
Fig. 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram showing the selection of articles for review.
Characteristics of included studies
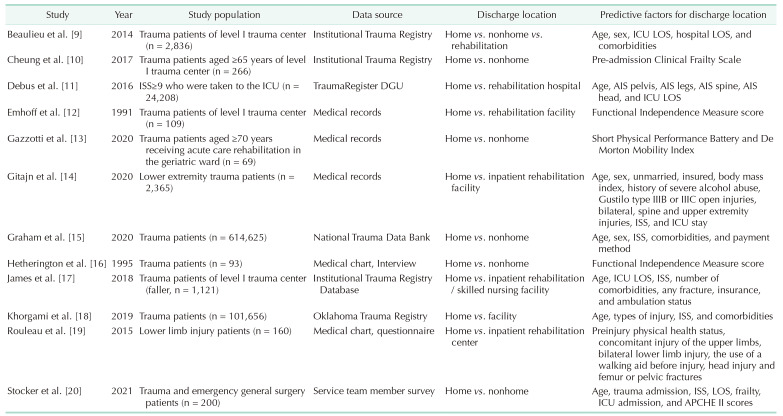
Previous studies (Table 1 [9–20]) have mainly used existing trauma registries or medical records as data sources. Discharge location was often divided into home and nonhome, and nonhome was often subdivided into nursing and advanced rehabilitation facilities. Of the 12 references, 7 studies [9,10,13,15,17,18,19] developed a scale to predict discharge location by analyzing registries or databases using statistical techniques.
Table 1. Characteristics of included studies.
ICU, intensive care unit; LOS, length of stay; DGU, Deutsche Gesellschaft für Unfallchirurgie; AIS, abbreviated injury score; ISS, injury severity score; APACHE, Acute Physiology and Chronic Health Evaluation.
Checklist regarding the need for specialized rehabilitation for trauma patients
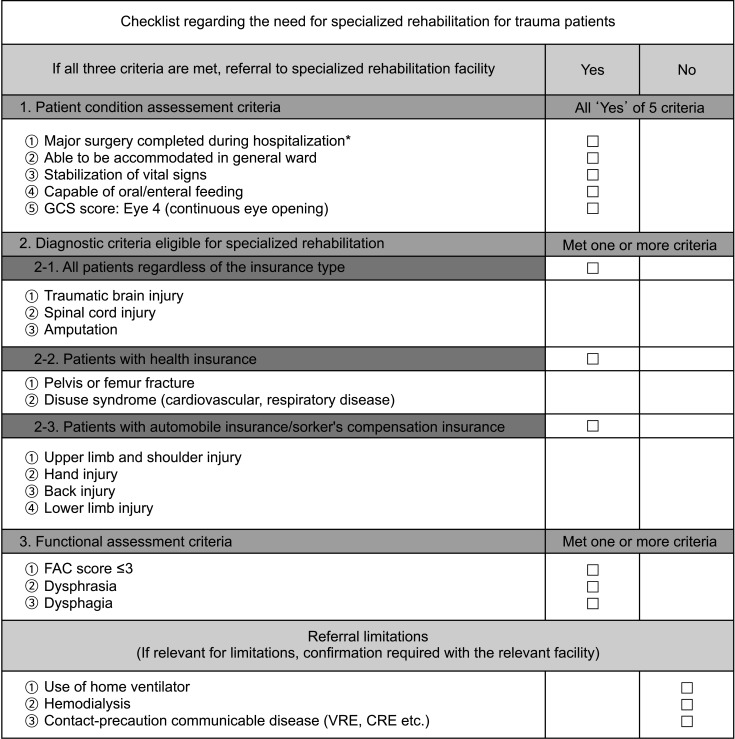
If the output of the scale, specifically the location after discharge from a trauma treatment facility (TTF), is overly detailed, there is a risk that the accuracy of the scale may decrease. Therefore, the intended purpose of using this scale was to screen for the need for specialized rehabilitation. Therefore, the scale was developed in the form of a checklist that could derive the yes/no need for specialized rehabilitation (Fig. 2). “Yes” was defined as transfer to an SRF certified by the Korean Ministry of Health and Welfare.
Fig. 2. Checklist regarding the need for specialized rehabilitation for trauma patients. GCS, Glasgow Coma Scale; FAC, functional assessment criteria; VRE, vancomycin-resistant Enterococcus; CRE, carbapenem-resistant Enterobacteriaceae.
The checklist consists of the following 3 items: evaluation of whether discharge from the TTF for SRF is possible, whether there is a diagnosis that can be treated with rehabilitation, and post-trauma functional assessment. If all 3 criteria are met, specialized rehabilitation is required, resulting in the need for transfer to an SRF. However, even if the checklist is satisfied, the actual transfer may not be possible if there is a clinical condition that limits transfer. Therefore, a referral limitation section was added at the bottom of the checklist.
Patient condition assessment criteria
The first scale is a criterion for evaluating whether a patient can be transferred from TTF to SRF. The first scale is met if all 5 of the following are satisfied: whether all major operations have been completed; whether the patient is hospitalized in a general ward (not in the ICU); whether vital signs such as blood pressure and heart rate are stable; whether oral or enteral feeding is possible; and whether continuous eye opening is possible. Wound problems not requiring major operations and interval operations planned after readmission were excluded from the definition of “major operations.” The evaluation process was simplified by using only the Glasgow Coma Scale eye score to determine the functional mental status eligible for rehabilitation treatment.
Diagnostic criteria eligible for specialized rehabilitation
To be admitted to an SRF, the medical need for specialized rehabilitation and the cost of treatment for professional rehabilitation must be reimbursed by insurance. The second criterion of the checklist is the list of diagnoses that can be reimbursed for the treatment of the checklist. As the list of diagnoses that can be reimbursed by national health insurance, car insurance, and industrial accident insurance is slightly different, ‘Article 14 of the Notice on Designation and Operation of Rehabilitation Medical Institutions’ and ‘Industrial Accident Compensation Insurance Nursing Care Benefit Calculation Standards’ was adopted as a reference.
In addition to the list of diagnoses that can be reimbursed, disuse syndrome was included in the criteria to prevent patients whose functional status was significantly reduced due to prolonged ICU care or a post-trauma immobilized state from being omitted from rehabilitation treatment. To be reimbursed for disuse syndrome, 2 prerequisites must be met: (1) within 60 days after surgery or disease occurrence; and (2) a Manual Muscle Testing score of less than 48 and a Korean Modified Barthel Index of 80 points or less, or Berg Balance Scale of 40 points or less. If one or more of the diagnostic criteria were met, the second criterion was met.
Functional assessment criteria
Among the functional evaluation tools collected through systemic review, the expert group decided to use the Functional Ambulation Category (FAC) [21], which is simple and can be easily evaluated even by non-rehabilitation specialists to determine whether specialized rehabilitation is necessary. The FAC scores ranged from 0 to 5, depending on ambulatory function. To select subjects for specialized rehabilitation, the cutoff was set at ‘3 points or less,’ which indicated difficulty in independent walking. Therefore, a score of 3 (ambulator, dependent on supervision), 1–2 points (ambulator, dependent on physical assistance), or 0 points (nonfunctional ambulator) was defined as the target for specialized rehabilitation.
Dysphrasia and dysphagia were included in consideration of neurological deficits that required specialized rehabilitation. Isolated upper extremity injuries were not included as a criterion because outpatient rehabilitation is usually performed without hospitalization at the SRF. If one or more items were met, the functional assessment criterion was met.
Referral limitations
Depending on the patient, clinical conditions may exist that make discharge to the SRF impossible. Therefore, we checked whether the following conditions existed: use of a home ventilator, hemodialysis, or diagnosis of a contact precautionary communicable disease. Confirmation from a relevant institution was required if a referral limitation existed.
Validation of the checklist
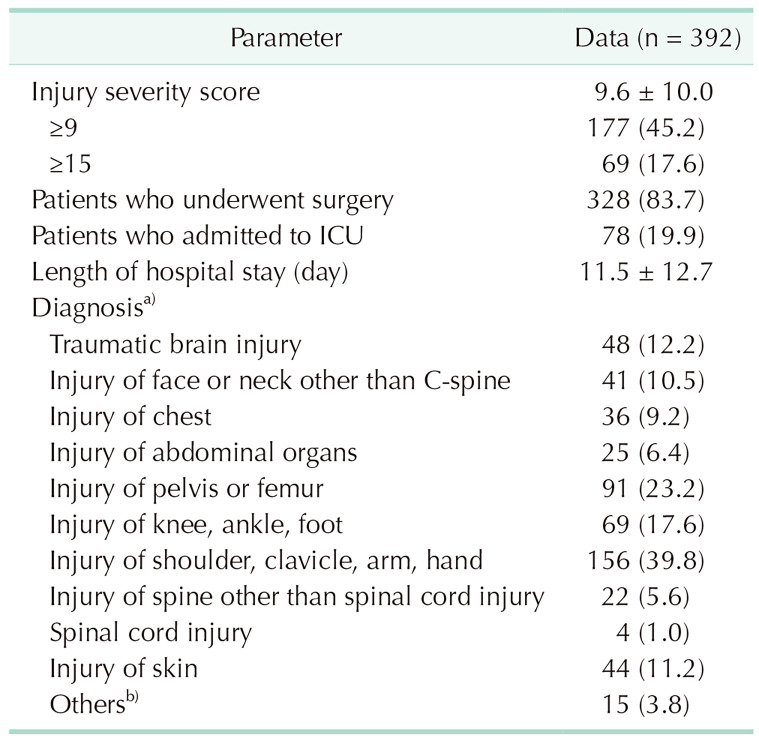
After excluding 46 of the 438 patients with missing clinical information, the checklist was validated on 392 subjects. The mean ISS was 9.6, and 17.6% scored higher than 15 points, which is the criterion for severe trauma. Of all patients, 83.7% received surgical treatment and 19.9% received ICU care. The mean length of the hospital stay was 11.5 days (Table 2).
Table 2. Demographics of the research participants used for validation.
Values are presented as mean ± standard deviation or number (%).
ICU, intensive care unit.
a)Duplicates allowed. b)Asphyxia, cerebral concussion, traumatic shock.
Checklist results versus actual location after discharge
As a result of the medical chart review of the checklist items, 95.1% of the 392 subjects met item #1, 36.7% met item #2, and 40.8% met item #3. A total of 98 patients (25.0%) who met all 3 criteria of the checklist were judged to be in need of hospitalization at the SRF.
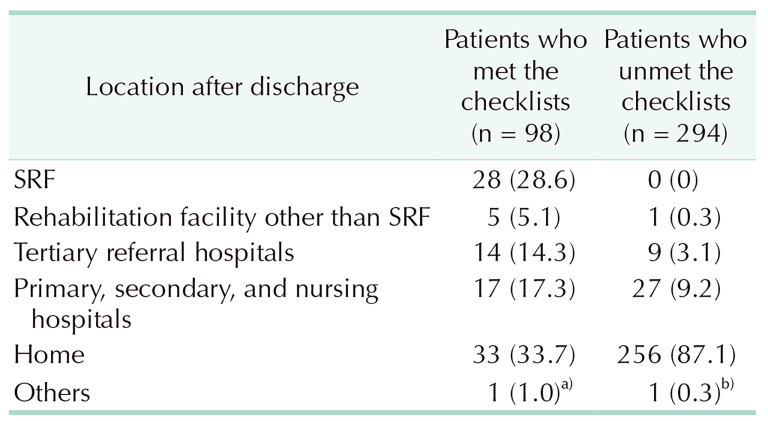
Among patients’ discharge locations, most (73.7%) underwent outpatient rehabilitation after discharge. Among the 98 patients who required hospitalization at SRF, 28.6% went to SRF, and 33.7% were discharged. Among the 294 patients who did not meet the checklist criteria, none were transferred to the SRF (Table 3).
Table 3. Actual location after discharge depending on whether the checklist is met.
Values are presented as number (%).
SRF, specialized rehabilitation facility.
a)Oriental hospital. b)Flight to home country for foreign nationals.
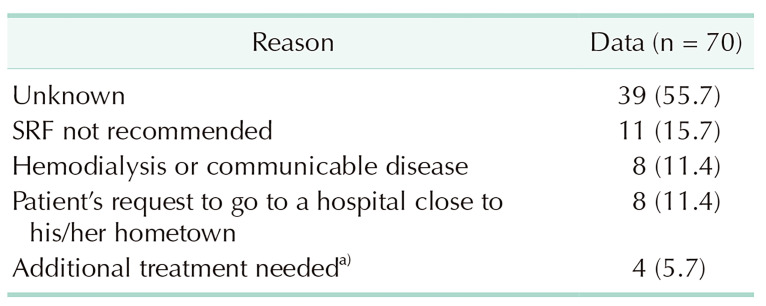
The reasons for discrepancies among the 70 patients who satisfied the checklist but were not transferred to the SRF were often difficult to identify owing to the retrospective nature of the study (55.7%). The reasons identified included medical staff not recommending SRF to the patient or family (15.7%), referral limitations preventing admission to SRF (11.4%), or the patient or family preferring to go to a hospital near their hometown (11.4%) (Table 4).
Table 4. Reasons for discrepancies between checklist results and actual location after discharge.
SRF, specialized rehabilitation facility.
a)Wound care, chemotherapy, coronary intervention.
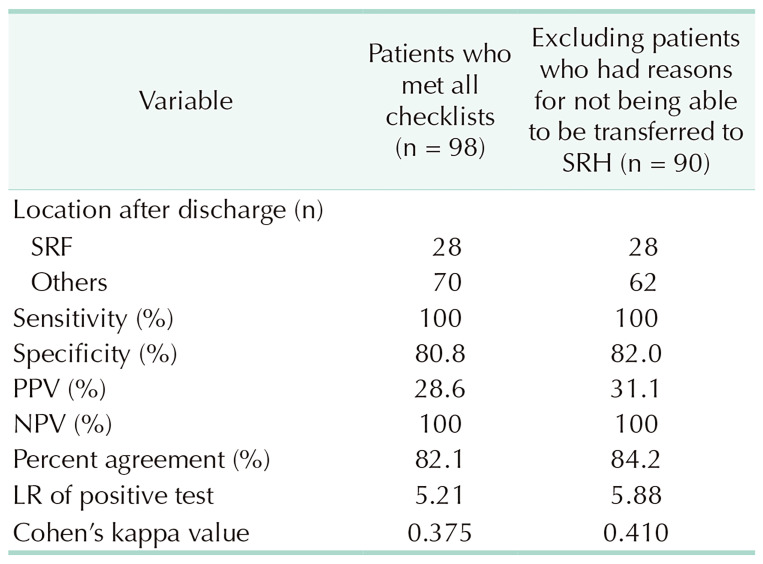
Validation results of the checklist
When comparing whether the checklist was met and the actual discharge location, the percentage agreement was 82.1%, the likelihood ratio of a positive test was 5.21, and Cohen’s kappa value was 0.375. Nineteen patients (4.8%) had SRF referral limitations, 9 of whom met the checklist and were eligible for specialized rehabilitation treatment. Of these 9 patients, only one was transferred to SRF. When the 8 patients who did not undergo SRF were excluded, all values, including percent agreement, improved (Table 5).
Table 5. Validation results of the checklist.
SRF, specialized rehabilitation facility; PPV, positive predictive value; NPV, negative predictive value; LR, likelihood ratio.
DISCUSSION
According to the injury fact book published by the Korea Disease Control and Prevention Agency, the number of patients hospitalized for injuries in 2021 was 960,000 [22]. The number of severe trauma patients by International Classification of Diseases 9th Edition Injury Severity Score [23] criteria in 2022 was 86,159 [24] and the number of patients treated at regional trauma centers was reported to be 35,019 [25]. The socioeconomic cost of injury is estimated to be 5.3 trillion Korean won in 2021 [22].
The treatment of trauma patients does not end when they are discharged from a trauma center, and many require ongoing rehabilitation even after discharge. Timely multidisciplinary rehabilitation improves patient outcomes [3,4]. In a survey conducted in 2021, Korean trauma specialists recognized that multidisciplinary treatment for patients with trauma was necessary. However, the number of regional trauma centers capable of in-hospital transfer to the Department of Rehabilitation Medicine was reported to be very limited [26].
The Korean Ministry of Health and Welfare began a rehabilitation medical institution certification project in 2020, and nationally designated rehabilitation facilities are currently in operation. However, there is still no standard for determining which patients should undergo SRF; therefore, the domestic trauma-rehabilitation linkage system still needs much improvement.
In the United Kingdom, the National Clinical Audit Specialist Rehabilitation following Major Injury (NCASRI) [27] includes the identification of patients’ rehabilitation needs while in the major trauma centers. To enable timely assessment and transfer to level 1 and 2 specialist rehabilitation units, a national standard requires that all trauma patients have an ISS score of 9 or higher within 10 days and be transferred within 6 weeks. In addition, standards for evaluating the patients’ measurable gains or goal achievement were set to ensure that the patients reached their goals. These standards require that all patients achieve some measurable gain or goal upon discharge, and discharge destinations are mandatorily recorded. In Australia, the time to rehabilitation from referral and discharge destinations is included as a quality indicator of trauma care [28]. The Korean Trauma Data Bank contains inaccurate information on discharge locations and does not collect information that can be used to determine the rehabilitation linkage process or post-injury functional status.
Most previous studies on disposition planning have used statistical methods to determine the risk factors and predictors of discharge locations. Statistical methods can be applied only under the assumption that the discharge disposition has been made ideally and that the data of the registry are collected correctly. However, in Korea, patients and their families often decide the discharge location independently; therefore, statistical methods were not used. Instead, a group of experts reached a consensus on the criteria for determining the need for specialized rehabilitation by referring to factors investigated in a systematic review and then selected a checklist in a format that was easy to understand at a glance.
In this study, the FAC was selected as an evaluation tool for the necessity of specialized rehabilitation in patients with multiple traumas. Among the existing indicators used to determine discharge location, the AM-PAC [9] was developed as a tool to determine the discharge location after acute treatment by evaluating the patient’s condition, functional mobility, and ability to perform daily activities. Existing studies using the abbreviated form of ‘AM-PAC 6-Clicks’ either targeted all patients who received acute hospital care regardless of the cause [29] or targeted too specific disease groups [30], and only classified the discharge location as home or institution [29,30]. Predicting Location after Arthroplasty Nomogram [7], developed in 2010, is a tool used to predict patient discharge disposition after total joint arthroplasty and can be evaluated preoperatively to make appropriate arrangements and avoid potential delays in patient discharge who require an extended care facility. However, it cannot be applied to patients with multiple traumas. In this study, the FAC was selected because it is sufficiently simple to be used by non-rehabilitation medical staff without the help of rehabilitation physicians.
This study had limitations in that the number of expert groups was small, and there may be issues that require supplementation in clinical practice. In addition, although the term “validation” was used to assess the effectiveness of the checklist, it is more accurate to say that the checklist developed in this study was used to evaluate how an institution’s trauma-rehabilitation linkage is being carried out. A domestic multicenter follow-up study is being conducted.
Nevertheless, the significance of this study is that it was the first in Korea to establish standards for evaluating the need for specialized rehabilitation and present standards as a starting point for identifying the unmet need for rehabilitation, identifying its causes, and suggesting solutions. As of 2023, interhospital transfer departments of several domestic institutions began using the checklist developed in this study. The scale developed in this study has the advantage of preventing patients in need of specialized rehabilitation from being excluded. In addition, it is expected to contribute to improving the domestic trauma-rehabilitation linkage system for the last chain of trauma survival by making it possible to prospectively collect the proportion and reasons for not being transferred to a specialized rehabilitation medical institution among those eligible for specialized rehabilitation.
In conclusion, this study established standards for assessing the need for specialized rehabilitation in patients with polytrauma and validated that this simple scale is effective for clinical use. This scale is expected to contribute to early rehabilitation to restore the quality of life and the last chain of the trauma chain of survival. In the next stage of research, the authors will be conducting a domestic multicenter study using this checklist.
ACKNOWLEDGEMENTS
The authors would like to express their deep gratitude to Ga-In Shin (Research professor at National Traffic Injury Rehabilitation Hospital, Yangpyeong, Korea) for conducting the systematic literature search.
Footnotes
Fund/Grant Support: This study was supported by the National Traffic Injury Rehabilitation research fund (No. NTRH RF-2024001).
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: SAL, Goo Joo Lee, YRC.
- Formal Analysis, Investigation: SAL, YJJ, YRC.
- Methodology: SYC, JWC, SWC, JG, HHK, KHL, Gil Jae Lee, Goo Joo Lee, YRC.
- Data curation: SAL, YJJ.
- Project Administration: Goo Joo Lee, YRC.
- Writing – Original Draft: SAL, YJJ, YRC.
- Writing – Review & Editing: All authors.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1-4 can be found via https://doi.org/10.4174/astr.2024.107.5.274.
Search strategy on PubMed
Search strategy on Embase
Search strategy on Cochrane Library
Expert group
References
- 1.Søreide K. Strengthening the trauma chain of survival. Br J Surg. 2012;99(Suppl 1):1–3. doi: 10.1002/bjs.7795. [DOI] [PubMed] [Google Scholar]
- 2.Im J, Seo EW, Jung K, Kwon J. Understanding Regional Trauma Centers and managing a trauma care system in South Korea: a systematic review. Ann Surg Treat Res. 2023;104:61–70. doi: 10.4174/astr.2023.104.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Hanna R, Amatya B, Lizama LE, Galea MP, Khan F. Multidisciplinary rehabilitation in persons with multiple trauma: a systematic review. J Rehabil Med. 2020;52:jrm00108. doi: 10.2340/16501977-2737. [DOI] [PubMed] [Google Scholar]
- 4.Khan F, Amatya B, Hoffman K. Systematic review of multidisciplinary rehabilitation in patients with multiple trauma. Br J Surg. 2012;99(Suppl 1):88–96. doi: 10.1002/bjs.7776. [DOI] [PubMed] [Google Scholar]
- 5.Brott T, Adams HP, Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–870. doi: 10.1161/01.str.20.7.864. [DOI] [PubMed] [Google Scholar]
- 6.Haley SM, Andres PL, Coster WJ, Kosinski M, Ni P, Jette AM. Short-form activity measure for post-acute care. Arch Phys Med Rehabil. 2004;85:649–660. doi: 10.1016/j.apmr.2003.08.098. [DOI] [PubMed] [Google Scholar]
- 7.Barsoum WK, Murray TG, Klika AK, Green K, Miniaci SL, Wells BJ, et al. Predicting patient discharge disposition after total joint arthroplasty in the United States. J Arthroplasty. 2010;25:885–892. doi: 10.1016/j.arth.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 8.Van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health. 1972;62:337–342. doi: 10.2105/ajph.62.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaulieu RA, McCarthy MC, Markert RJ, Parikh PJ, Ekeh AP, Parikh PP. Predictive factors and models for trauma patient disposition. J Surg Res. 2014;190:264–269. doi: 10.1016/j.jss.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 10.Cheung A, Haas B, Ringer TJ, McFarlan A, Wong CL. Canadian study of health and aging clinical frailty scale: does it predict adverse outcomes among geriatric trauma patients? J Am Coll Surg. 2017;225:658–665. doi: 10.1016/j.jamcollsurg.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Debus F, Lefering R, Lang N, Oberkircher L, Bockmann B, Ruchholtz S, et al. Which factors influence the need for inpatient rehabilitation after severe trauma? Injury. 2016;47:2683–2687. doi: 10.1016/j.injury.2016.06.035. [DOI] [PubMed] [Google Scholar]
- 12.Emhoff TA, McCarthy M, Cushman M, Garb JL, Valenziano C. Functional scoring of multi-trauma patients: who ends up where? J Trauma. 1991;31:1227–1232. doi: 10.1097/00005373-199109000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Gazzotti A, Meyer U, Freystaetter G, Palzer M, Theiler R, Abderhalden L, et al. Physical performance among patients aged 70 + in acute care: a preliminar comparison between the Short Physical Performance Battery and the De Morton Mobility Index with regard to sensitivity to change and prediction of discharge destination. Aging Clin Exp Res. 2020;32:579–586. doi: 10.1007/s40520-019-01249-9. [DOI] [PubMed] [Google Scholar]
- 14.Gitajn IL, Reider L, Scharfstein DO, O’Toole RV, Bosse MJ, Castillo RC, et al. Variability in discharge disposition across US trauma centers after treatment for high-energy lower extremity injuries. J Orthop Trauma. 2020;34:e78–e85. doi: 10.1097/BOT.0000000000001657. [DOI] [PubMed] [Google Scholar]
- 15.Graham M, Parikh P, Hirpara S, McCarthy MC, Haut ER, Parikh PP. Predicting discharge disposit ion in trauma patients: development, validation, and generalization of a model using the national trauma data bank. Am Surg. 2020;86:1703–1709. doi: 10.1177/0003134820949523. [DOI] [PubMed] [Google Scholar]
- 16.Hetherington H, Earlam RJ, Kirk CJ. The disability status of injured patients measured by the functional independence measure (FIM) and their use of rehabilitation services. Injury. 1995;26:97–101. doi: 10.1016/0020-1383(95)92185-d. [DOI] [PubMed] [Google Scholar]
- 17.James MK, Robitsek RJ, Saghir SM, Gentile PA, Ramos M, Perez F. Clinical and non-clinical factors that predict discharge disposition after a fall. Injury. 2018;49:975–982. doi: 10.1016/j.injury.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Khorgami Z, Ewing KL, Mushtaq N, Chow GS, Howard CA. Predictors of discharge destination in patients with major traumatic injury: analysis of Oklahoma Trauma Registry. Am J Surg. 2019;218:496–500. doi: 10.1016/j.amjsurg.2018.11.045. [DOI] [PubMed] [Google Scholar]
- 19.Rouleau DM, Place A, Bérubé M, Laflamme YG, Feldman D. Rehabilitation after lower limb injury: development of a predictive score (RALLI score) Can J Surg. 2015;58:278–283. doi: 10.1503/cjs.015014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stocker B, Weiss HK, Weingarten N, Engelhardt KE, Engoren M, Posluszny J. Challenges in predicting discharge disposition for trauma and emergency general surgery patients. J Surg Res. 2021;265:278–288. doi: 10.1016/j.jss.2021.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L. Clinical gait assessment in the neurologically impaired: reliability and meaningfulness. Phys Ther. 1984;64:35–40. doi: 10.1093/ptj/64.1.35. [DOI] [PubMed] [Google Scholar]
- 22.Choi JK, Jeong YH, Bae WC, Lee JE, Lee JS, Park SH, Lee MJ, editors. Injury Factbook 2023. Seoul: Korea Disease Control and Prevention Agency; 2023. [Google Scholar]
- 23.Osler T, Rutledge R, Deis J, Bedrick E. ICISS: an international classification of disease-9 based injury severity score. J Trauma. 1996;41:380–388. doi: 10.1097/00005373-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 24.National Emergency Medical Center. Emergency medical statistics annual report, 2022. National Emergency Medical Center. 2023 [Google Scholar]
- 25.National Emergency Medical Center. Korean Trauma Data Bank statistics annual report, 2022. National Emergency Medical Center. 2023 [Google Scholar]
- 26.Lee SA, Joo YJ, Chang YR. Perceptions regarding the multidisciplinary treatment of patients with severe trauma in Korea: a survey of trauma specialists. J Trauma Inj. 2023;36:322–328. doi: 10.20408/jti.2023.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turner-Stokes L NCASRI Project team. Final report of the National Clinical Audit of Specialist Rehabilitation following major Injury. Northwick Park Hospital. 2019 [Google Scholar]
- 28.Kovoor JG, Jacobsen JH, Balogh ZJ Trauma Care Verification and Quality Improvement Writing Group. Quality improvement strategies in trauma care: review and proposal of 31 novel quality indicators. Med J Aust. 2022;217:331–335. doi: 10.5694/mja2.51699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94:1252–1261. doi: 10.2522/ptj.20130359. [DOI] [PubMed] [Google Scholar]
- 30.Hadad MJ, Orr MN, Emara AK, Klika AK, Johnson JK, Piuzzi NS. PLAN and AM-PAC “6-Clicks” scores to predict discharge disposition after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2022;104:326–335. doi: 10.2106/JBJS.21.00503. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy on PubMed
Search strategy on Embase
Search strategy on Cochrane Library
Expert group