Abstract
Background:
With emerging treatments for anterior cruciate ligament (ACL) injury, analysis of patient preferences is lacking to align clinical care and research with patient priorities.
Purposes:
To identify patient priorities for outcomes after surgical intervention if they were to sustain an ACL tear, analyze what outcome measures influenced preferences, and determine whether patient demographics influenced preferences.
Study Design:
Cross-sectional study.
Methods:
The authors screened patients aged 18 to 30 years who presented for upper extremity complaints to a single institution in 2023. Patients were excluded for current lower extremity injury or history of a knee injury requiring surgical consultation. The authors designed a discrete choice experiment through literature review of outcome measures for bridge-enhanced ACL restoration (BEAR) and ACL reconstruction (ACLR) with hamstring tendon autograft. Measures included return to sports, risk of arthritis, risk of reinjury, and hamstring strength. Patients chose surgery A (ACLR with hamstring tendon autograft) or surgery B (BEAR) and then rated the importance of each outcome measure on their selection.
Results:
In total, 100 participants (36 female; mean age, 25.1 ± 4.0 years) completed the discrete choice experiment. Overall, 56.0% participated in sports and 80.0% were employed. Based on surgery choice group, there were no significant differences in sex, age, Marx Activity Scale score, sports participation, or employment status between patients who selected BEAR or ACLR with hamstring tendon autograft (all P > .361). Return to sports and hamstring strength were significant priorities for patients in procedure selection (P ≤ .011). Of the patients who selected ACLR with hamstring tendon autograft, 31.6% would not elect to undergo this procedure.
Conclusion:
In this discrete choice experiment of adults without prior ACL injury, return to sports and hamstring strength were identified as patient priorities when selecting a procedure for ACL injury. Risk of reinjury, however, was not a significant factor in procedure selection. Importantly, these priorities were maintained regardless of patient characteristics, activity level, or employment status.
Keywords: football (soccer); knee ligaments, ACL; skiing/snowboarding; BEAR; discrete choice experiment; return to sports
There has been a transition in health care policy from fee-for-service models toward value-based care. The definition of value is important and should be centered around the patient, yet it requires a balance between their personal autonomy to elect to undergo surgical procedures and the outcomes deemed important by a surgeon garnered through experience. 18 Specific to anterior cruciate ligament (ACL) injury, the balance between a patient's postoperative goals for function and a surgeon's experience with short- and long-term complications impacting those goals needs to be better understood. Prior efforts have determined the Patient Acceptable Symptom State (PASS) and patient-reported outcome measures that impact the ability to achieve PASS after ACL reconstruction (ACLR).7,10,17,21,23 However, these studies did not focus on ACL repair.
ACL repair has had a resurgence in publications surrounding the topic since 2010. 5 While ACLR remains the gold standard for surgical treatment of ACL injuries, the bridge-enhanced ACL restoration (BEAR) technique has gained increasing attention since the initial results of the BEAR I and II clinical trials. 5 Despite this rise in interest, there exist little postoperative data to counsel patients on expected outcomes in comparison with established reconstruction methods.1,8,14 As with any new procedure, information available to patients in the popular press may not provide a comprehensive understanding of the potential risks and benefits of an emerging procedure. Despite this gap, patient preferences on important outcomes after this emerging procedure can be evaluated to ensure clinical care and research remain patient centered.
Whereas PASS helps to identify what postoperative factors may influence patient satisfaction, discrete choice experiments can help to identify patient priorities before injury or surgery. A recent study utilizing a discrete choice experiment to analyze patient graft selection in ACLR found that patient values influence decision-making. 22 Understanding nuances in patient preferences toward treatment options is important for counseling purposes but also to appropriately guide future research based on patient perspectives. Discrete choice experiments offer an opportunity to elicit patient preferences about surgical techniques for ACL injury and align clinical care and research with patient priorities.15,16
Therefore, the purposes of this study were to identify patient priorities for outcomes after surgical intervention if they were to sustain an ACL tear, analyze what outcome measures influenced preferences, and determine whether patient characteristics influenced preferences. We hypothesized that patients would be willing to undergo surgical intervention for an ACL injury, that all outcome measures historically used in ACL clinical research would be important to patients, and that there would be no difference in patient characteristics between groups.
Methods
Institutional review board exemption approval was obtained for this cross-sectional study at a single institution in 2023. Patients aged 18 to 30 years presenting for upper extremity complaints were screened for exclusion criteria and then prospectively enrolled. Patients were excluded if they were unable to complete a survey in English; had a prior history of a knee injury requiring surgical consultation; or had current complaints of hip, knee, leg, or ankle injury. These criteria were utilized to enroll participants similar to an age group more likely to sustain an ACL injury and undergo surgery but limit prior injuries or experiences that may skew their perspectives or preferences for ACL surgery. Demographics were collected to include age, sex, sports involvement, and employment status. Patient-reported activity level was measured by the Marx Activity Scale. 9
Discrete Choice Survey Development
The authors designed a survey to conduct a discrete choice experiment using the highest-quality comparative clinical evidence for the BEAR technique available at the time of the study. A literature review was performed and identified only level 1 studies comparing BEAR to ACLR with hamstring (HS) tendon autograft.12,13,19 Thus, the authors designed the survey to analyze patient decision-making in a choice between surgery A (ACLR with HS tendon autograft) and surgery B (BEAR). Patients were blinded to the surgery and provided only with outcome measures for each procedure derived from the literature review.
The authors selected ≤5 outcome measures in accordance with expert recommendations for designing discrete choice experiments. 16 Attributes were selected in order to measure patient preferences for stated attributes and not to reveal new ones. They were deemed to be the most important attributes for patient counseling and education by the surgeon—the effect of both procedures on HS strength, return-to-sports (RTS) rate, risk of ipsilateral reinjury, and risk of developing osteoarthritis. The highest-quality clinical evidence for BEAR or ACLR with HS tendon autograft in isolation was utilized when no direct comparison had been published between the 2 surgeries. Table 1 outlines the evidence utilized to report the surgical outcome measures provided to patients shown in Table 2 as part of the survey. The presentation of evidence-based patient education was intentionally brief and in terms familiar to respondents, in accordance with expert recommendations. 16
Table 1.
Outcome Measures From Studies Identified Through Literature Review a
| Outcome Measure | Lead Author (Year Published) | Study Design (Level of Evidence) | Sample Size | Follow-up, y | Key Findings |
|---|---|---|---|---|---|
| Ipsilateral reinjury | Murray12 (2020) | RCT (1) | 100 (65 BEAR, 35 ACLR with HS tendon autograft) | 2 | Requiring additional ACL surgery within 2 y: 14% BEAR, 6% ACLR (P = .32) |
| HS strength | Murray12 (2020) | RCT (1) | 100 (65 BEAR, 35 ACLR with HS tendon autograft) | 2 | 2-y HS strength compared with contralateral: 98% in BEAR, 63% in ACLR (P < .001) |
| RTS | Barnett1 (2021) | RCT (1) | 100 (65 BEAR, 35 ACL with HS tendon autograft) | 2 | Cleared for RTS at 1 y: 88% BEAR, 76% ACLR (P = .261) |
| Postoperative arthritis | Belk2 (2018) | Systematic review of RCTs (2) | 505 (237 ACLR with BPTB autograft, 268 with HS tendon autograft) | Mean, 11.5 (range, 3-16) | KL grade >2 in 51% of HS tendon autografts |
ACL, anterior cruciate ligament; ACLR, ACL reconstruction; BEAR, bridge-enhanced ACL restoration; BPTB, bone–patellar tendon–bone; HS, hamstring; KL, Kellgren-Lawrence; RCT, randomized controlled trial; RTS, return to sports.
Table 2.
Evidence-Based Patient Education Provided to Participants as Part of Survey
| Surgery A | Surgery B |
|---|---|
| 63% Hamstring strength compared with the nonoperated leg 2 y postsurgery | 98% Hamstring strength compared with the nonoperated leg 2 y postsurgery |
| 76% Chance of returning to sports within 1 y of surgery | 88% Chance of returning to sports within 1 y of surgery |
| 6% Chance that the repair will fail within 2 y and an additional surgery will be required to fix it | 14% Chance that the repair will fail within 2 y and an additional surgery will be required to fix it |
| 51% Chance of developing knee arthritis in 10 y | No long-term data available |
Only preclinical data on postoperative arthritis for the BEAR procedure in animal studies existed, and there had been no clinical data yet published from the BEAR trials on this outcome measure given the inadequate length of follow-up for this long-term outcome.4,11 The available clinical evidence for the risk of developing osteoarthritis after ACLR was nonetheless presented to patients in order to measure the importance of this outcome, although without the ability to compare importance based on the selected procedure.
The order of presented outcome measures was randomized for each participant. Participants were asked, based on the information provided for each surgery, “If you were to tear a stabilizing ligament of your knee and required surgery to fix it, would you prefer to get surgery A or surgery B?” Participants then rated the importance of each outcome measure in their decision-making process on a scale: not important at all, somewhat important, important, very important, or extremely important. Finally, patients were asked if they would elect to undergo the procedure they selected based on the information provided in Table 2. The full survey given to participants can be found in Supplemental Figure S1.
Statistical Analysis
Participant age and Marx Activity Scale score are reported using means and standard deviations and compared between discrete choice groups using independent-samples t tests. Participant sex, employment status, sports participation, the primary presenting complaint, and the importance (eg, important or not important) of each factor presented in Table 2 for selecting the surgery of choice are reported as frequencies and compared between discrete choice groups using chi-square tests. In addition, the odds of an individual who selected the BEAR procedure indicating that a specific factor presented in Table 2 was important in their discrete choice was characterized relative to participants who selected HS tendon autograft using odds ratios and 95% confidence intervals. An a priori alpha level was established as P < .05. Statistical analyses were performed using jamovi Version 2.2.5.0.
Results
A total of 100 participants met the inclusion criteria and completed the survey. Overall, 36% were female, the mean age was 25.1 ± 4.0 years, 56.0% participated in sports, and 80.0% were employed at the time that they completed the discrete choice experiment. Demographics for participants are summarized and compared between discrete choice groups in Table 3. A significantly greater proportion of patients (n = 81; 81.0%) indicated that they would select the BEAR procedure to treat an ACL injury given the information in Table 2 as compared with participants (n = 19; 19.0%) who selected the HS tendon autograft procedure (P < .001).
Table 3.
Summary of Demographics by Discrete Choice a
| Demographic | Discrete Choice | P | |
|---|---|---|---|
| HS Tendon Autograft (n = 19) | BEAR (n = 81) | ||
| Sex, n | .932 | ||
| Female | 7 | 29 | |
| Male | 12 | 52 | |
| Age, y | 25.3 ± 4.5 | 25.1 ± 3.9 | .830 |
| Marx Activity Scale score | 7.8 ± 5.8 | 9.2 ± 5.4 | .362 |
| Sports participation, % | 47.4 | 58.0 | .400 |
| Employment status, % | .878 | ||
| Full-time | 63.2 | 59.3 | |
| Part-time | 15.8 | 21.0 | |
| Not employed | 21.1 | 19.8 | |
| Primary complaint, % | .168 | ||
| Sports injury | 26.3 | 54.3 | |
| Work injury | 21.1 | 12.3 | |
| Chronic pain | 36.8 | 20.1 | |
| Other | 15.8 | 12.3 | |
Data are reported as mean ± SD unless otherwise indicated. BEAR, bridge-enhanced anterior cruciate ligament restoration; HS, hamstring.
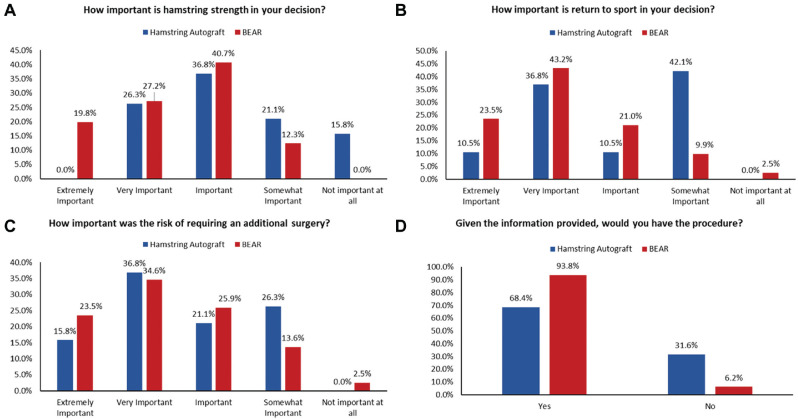
Figure 1 summarizes participant responses when asked about factors that were important in their discrete choice. Factors found to be significantly important in surgery choice selection included recovery of HS strength and the ability to RTS after surgery (Table 4). Given the lack of clinical evidence available for risk of arthritis with the BEAR procedure, a composite valuation of patient importance was determined for this factor (Figure 2). There were 7 times greater odds that participants would elect to undergo the procedure of their choice when selecting BEAR (Table 4). Sports participation was not associated with the decision to undergo either procedure when analyzing the entire cohort (P = .589) or those who chose BEAR (P = .151). Sports participation was also not associated with the rating of outcome measures as important, as shown in Table 5.
Figure 1.
Descriptive statistics and between-group comparisons for items on the survey based on selected procedure. BEAR, bridge-enhanced anterior cruciate ligament restoration.
Table 4.
Comparison of Importance of Reasons for Discrete Choice Between Groups a
| Outcome Measure | HS Tendon Autograft, n (%) | BEAR, n (%) | P | OR (95% CI) |
|---|---|---|---|---|
| HS strength | ||||
| Important | 12 (63.2) | 71 (87.7) | .011 | 4.14 (1.32-12.99) |
| Not important | 7 (36.8) | 10 (12.3) | ||
| Ability to return to sports | ||||
| Important | 11 (57.9) | 71 (87.7) | .002 | 5.16 (1.68-15.92) |
| Not important | 8 (42.1) | 10 (12.3) | ||
| Risk of additional surgery | ||||
| Important | 14 (73.7) | 68 (84.0) | .294 | 1.87 (0.57-6.09) |
| Not important | 5 (26.3) | 13 (16.0) | ||
| Potential to develop osteoarthritis | ||||
| Important | 17 (89.5) | 65 (80.2) | .346 | 0.48 (0.10-2.28) |
| Not important | 2 (10.5) | 16 (19.8) | ||
| Choice to undergo this procedure | ||||
| Yes | 13 (68.4) | 76 (93.8) | .001 | 7.02 (1.87-26.38) |
| No | 6 (31.6) | 5 (6.2) | ||
BEAR, bridge-enhanced anterior cruciate ligament restoration; HS, hamstring; OR, odds ratio.
Figure 2.
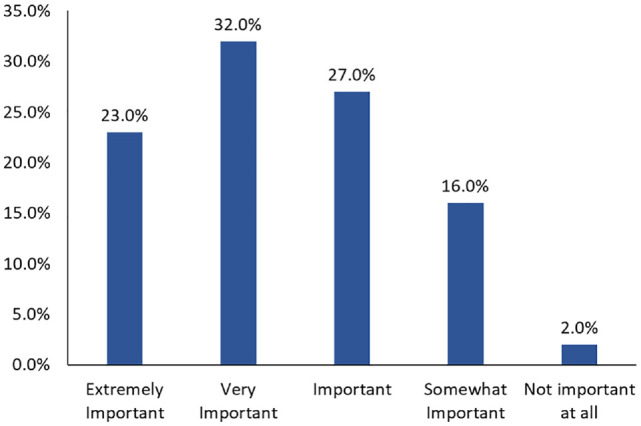
Composite rating of importance by participants for risk of osteoarthritis.
Table 5.
Association Between Sports Participation and Importance of Reasons for Procedure Selection a
| All Participants | Important, n (%) | Not Important, n (%) | P |
|---|---|---|---|
| Hamstring strength | |||
| Engaged in sports | 44 (83.0) | 9 (17.0) | .623 |
| Not engaged in sports | 30 (78.9) | 8 (21.1) | |
| Return to sports | |||
| Engaged in sports | 44 (83.0) | 9 (17.0) | .618 |
| Not engaged in sports | 33 (86.8) | 5 (13.2) | |
| Risk of additional surgery | |||
| Engaged in sports | 41 (77.4) | 12 (22.6) | .418 |
| Not engaged in sports | 32 (84.2) | 6 (15.8) | |
| Risk of osteoarthritis | |||
| Engaged in sports | 42 (79.2) | 11 (20.8) | .783 |
| Not engaged in sports | 31 (81.6) | 7 (18.4) | |
| Participants Who Selected BEAR | Important, n (%) | Not Important, n (%) | P |
| Hamstring strength | |||
| Engaged in sports | 39 (88.6) | 5 (11.4) | .475 |
| Not engaged in sports | 24 (82.8) | 5 (17.2) | |
| Return to sports | |||
| Engaged in sports | 39 (88.6) | 5 (11.4) | .526 |
| Not engaged in sports | 27 (93.1) | 2 (6.9) | |
| Risk of additional surgery | |||
| Engaged in sports | 36 (81.8) | 8 (18.2) | .918 |
| Not engaged in sports | 24 (82.8) | 5 (17.2) | |
| Risk of osteoarthritis | |||
| Engaged in sports | 35 (79.5) | 9 (20.5) | .710 |
| Not engaged in sports | 22 (75.9) | 7 (24.1) | |
BEAR, bridge-enhanced anterior cruciate ligament restoration.
Discussion
The chief findings of our discrete choice experiment were that participants rated the ability to RTS and HS strength as important outcomes in their decision when selecting an ACL procedure, but not the risk of additional surgery. Furthermore, >3 in 10 patients who selected ACLR with HS tendon autograft would not elect to undergo the procedure. We were unable to compare patient preferences for the risk of arthritis because of the unavailability of clinical evidence on risk of osteoarthritis after BEAR.
Each of the 4 selected outcome measures for our discrete choice experiment were rated as important by >80% of participants in our study, suggesting that these outcomes were acceptable for inclusion. A prior discrete choice experiment analyzing graft preference for ACLR found that aside from sports activity, patient characteristics did not affect graft selection. 22 These findings were not reflected in our discrete choice experiment, where there were no significant differences between groups who chose BEAR or ACLR with HS tendon autograft in terms of demographics, activity level, or employment status. However, patients in each group did rate the outcome measures on the discrete choice survey differently in terms of importance. Patients who selected BEAR more frequently rated HS strength and rate of returning to sports as important to their decision-making. These results demonstrate that patient selection for each surgery is determined by differing priorities and goals. Understanding and utilizing patient preferences in the surgical decision-making process may improve shared decision-making and patient satisfaction, which do not appear to be based on the aforementioned demographic variables. Providing patients with key points from the literature may better inform the decision-making process, particularly for emerging procedures, while also providing an opportunity to connect evidence-based and patient-centered care.
Rate of RTS
In the present study, participants rated the ability to RTS as a significantly important outcome in their decision-making, despite 56% of participants being engaged in sports. Notably, sports participation and Marx Activity Scale scores were not different based on the selected procedure, and sports participation was not associated with the decision to undergo either procedure or rate the factors as important. The best available evidence comparing BEAR to ACLR with HS tendon autograft demonstrated a 12% difference in clearance for RTS 1 year after surgery favoring BEAR. However, this was not a statistically significant finding and clearance for RTS was reported, which may not be indicative of RTS at the same preinjury level and was determined by the operating surgeon, potentially imparting bias for the involved procedures. 1 Further study with appropriate power to detect a difference is needed to adequately counsel patients, especially considering that participants in the present study were 5 times more likely to rate this as an important factor in selecting BEAR over ACLR, regardless of sports participation or other demographic factors. Another comparative study between BEAR and ACLR with HS tendon autograft assessed psychological readiness to RTS and found that while there was no difference at 12 and 24 months, readiness was greater at 6 months in the BEAR group and was associated with less laxity, better strength, and decreased pain. 19 Larger studies are needed to determine whether a significant difference in rate of RTS and timing exists for BEAR comparatively.
HS Strength
Patients selecting BEAR in the present study were 4 times more likely to rate HS strength as important to their decision. ACLR with autograft has associated morbidity regardless of the graft selected. HS harvesting for use as autograft has been shown to decrease HS strength; this finding was redemonstrated in initial results from the BEAR trial. 12 However, bone–patellar tendon–bone (BPTB) autograft is considered the gold standard over other graft options for reconstruction but is associated with an increased incidence of anterior knee pain. 22 BEAR has been shown to be noninferior to ACLR with HS tendon autograft in initial small studies but has not been directly compared with BPTB or quadriceps tendon autograft. HS tendon autograft ACLR may not be the ideal alternative for comparison with BEAR, but as the highest-quality clinical evidence available, it was utilized in this discrete choice experiment.
Risk of Developing Osteoarthritis
The evidence-based information in the discrete choice experiment in this study described a 51% chance of developing knee arthritis after ACLR with HS tendon autograft. While long-term outcomes related to postoperative osteoarthritis in human patients undergoing BEAR have not yet been published, this outcome has been examined in a porcine model. 11 Murray et al 11 demonstrated significantly less osteoarthritis in the porcine knee randomized to ACL repair with a bioactive scaffold compared with nonoperative healing and a strong trend toward less arthritis when compared with ACLR at 12 months. While normal kinematics was not restored with the BEAR procedure compared with the native knee, it was similar to other treatment arms. The porcine study was repeated and again demonstrated that porcine knees had significantly less arthritis than untreated knees or those undergoing ACLR. 4
The provided evidence for development of arthritis in our survey was based on level 2 evidence directly comparing ACLR with HS tendon autograft to ACLR with BPTB autograft and not to BEAR. 2 Importantly, it was decided to not include level 1 and 2 evidence of the natural history of a knee after ACL injury treated with nonoperative management based on the high levels of bias found in systematic reviews and meta-analyses.3,6 Lien-Iversen et al 6 looked at 5 studies directly comparing surgical and nonsurgical treatment of ACL rupture with at least 10 years of follow-up and found that surgery was correlated with a higher risk of radiographic knee arthritis. Cuzzolin et al 3 analyzed 12 studies directly comparing surgical with nonoperative management of ACL injuries with at least 5 years of follow-up and found that ACLR was not associated with arthritis prevention. The authors in both studies commented on the low levels of evidence and high levels of bias in the included studies, so these data may not be able to adequately inform patients further when selecting between ACL procedures.
The risk of developing osteoarthritis by procedure was not able to be compared in a meaningful way in this discrete choice experiment because of the lack of available clinical evidence. However, >80% of participants rated the risk of developing osteoarthritis as important, suggesting that high-quality clinical studies should be performed, and comparative preferences by procedure selection may warrant further study when that evidence is available.
Risk of Ipsilateral Reinjury
Neither group of study participants was more likely to rate the risk of requiring an additional surgery as important to their decision. However, participants did rate the outcome measure of reinjury to be important for selecting either procedure 82% of the time. Notably, our study did not survey patients who had a history of ACL injury who might have undergone surgery in addition to up to a year of rehabilitation and time away from a sport. That subset of patients may have different views on the importance of the risk of reinjury compared with the uninjured patients in our study.
The 2-year outcome study from BEAR II had a failure rate of 14%. 12 More recently, combining data from BEAR I through III, the failure rate remained fairly consistent at 15%. 20 While the data from BEAR III were not available at the time of literature review for this study, the small increase in failure rate likely would not have influenced the results. From BEAR II, the results did demonstrate that those patients who had conversion from BEAR to ACLR had similar outcomes to patients after their primary procedure, suggesting that lost time may be the main impact of a revision procedure after BEAR. 12 Additionally, the difference in failure rates was not found to be statistically significant in the referenced study, despite an 8% difference in rate of reinjury.
Limitations
A major limitation of our study was that patient priorities for treatment and outcomes after ACL injury were obtained from a group of patients without a prior ACL injury. While the intent was to limit bias from ongoing or past experiences or treatments related to the ACL, this sampling may limit the external validity for patients undergoing an ACL procedure. Additionally, patients were selected from a similar age group as those typically at risk for ACL injury and subsequent surgery. However, propensity matching to patients with ACL injuries was not performed specifically for those with and without sports activity in order to be able to identify distinctions in preferences based on this variable. While no differences were identified in patient preferences based on sports participation, this may still limit the external validity of our findings to a more active population.
The limitations of our study are reflective of the limited data available to appropriately counsel patients on BEAR as compared with other procedures for the treatment of ACL tears. As with any survey, the information on outcome measures and questions within may have unintentionally biased patient response or weighed in their decision-making. Surgeon selection of the evidence for the survey may have unintentionally imparted bias toward or against either procedure. However, our evidence-based survey was intended to provide information specifically from studies directly comparing BEAR with other treatment options or the best available clinical evidence if direct comparison was not available. This may have introduced bias in the information presented in the survey because 3 of the 4 outcome measures reported came from a single research group. Further long-term and comparative research is necessary to validate previous results. Patients were not offered the opportunity to discuss the presented options or other treatments with an orthopaedic surgeon, as would typically happen during an appointment. This limits our study to patient priorities for outcomes after BEAR and ACLR with HS tendon autograft and may not be generalizable to other ACLR options. In particular, we are unable to offer insights on patient preferences for ACLR with BPTB or quadriceps autograft.
Patient employment status was not different between groups, although we did not collect insurance status, income level, or education level, which may influence patient preferences. Participants also completed the survey within the office visit without the opportunity to further research either option aside from the provided evidence. This differs from access to online information that patients with ACL injuries would potentially be able to obtain and that might influence their decision. Conversely, this ensured that all patients based their preferences on the presented data and limited bias from other sources. The hypothetical nature of the injury may also have influenced patient preference either for or against certain interventions in a way that would differ from a patient presenting with the actual injury. These limitations offer areas for further study. Despite these limitations, patient responses provided a glimpse into the factors that matter to patients when deciding on a treatment for ACL injury in a population that has not sustained an ACL injury.
Conclusion
In this discrete choice experiment of adults without prior ACL injury, RTS and HS strength were identified as significantly important factors when selecting a procedure for ACL injury. Risk of reinjury, however, was not a significant priority when selecting a procedure. Importantly, these priorities were maintained regardless of patient characteristics, activity level, or employment status. There is a need for further high-quality comparative and long-term evidence to provide patients with a comprehensive understanding of the strengths and weaknesses of emerging procedures. These findings will help to appropriately counsel patients on surgical treatment options and further guide research and comparison of emerging procedures with other reconstruction techniques.
Supplemental Material
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241282657 for Evaluating the Importance of Return to Sports and Hamstring Strength in a Discrete Choice Experiment for Anterior Cruciate Ligament Injury by Scott M. Feeley, Jalen N. Broome, Rachel E. Cherelstein, Benjamin E. Neubauer, Christopher M. Kuenze and Edward S. Chang in Orthopaedic Journal of Sports Medicine
Footnotes
Final revision submitted March 20, 2024; accepted April 12, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.M.F. has received education payments from Supreme Orthopedic Systems. E.S.C. has received consulting fees from Avanos Medical and education payments from Arthrex and Supreme Orthopedic Systems. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by INOVA (U23-03-5002).
ORCID iDs: Scott M. Feeley  https://orcid.org/0000-0003-1994-9577
https://orcid.org/0000-0003-1994-9577
Benjamin E. Neubauer  https://orcid.org/0009-0005-3156-2561
https://orcid.org/0009-0005-3156-2561
Christopher M. Kuenze  https://orcid.org/0000-0001-9184-4636
https://orcid.org/0000-0001-9184-4636
Supplemental Material: Supplemental Material for this article is available at https://journals.sagepub.com/doi/full/10.1177/23259671241282657#supplementary-materials.
References
- 1. Barnett SC, Murray MM, Badger GJ, et al. Earlier resolution of symptoms and return of function after bridge-enhanced anterior cruciate ligament repair as compared with anterior cruciate ligament reconstruction. Orthop J Sports Med. 2021;9(11):23259671211052530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Belk JW, Kraeutler MJ, Carver TJ, McCarty EC. Knee osteoarthritis after anterior cruciate ligament reconstruction with bone-patellar tendon-bone versus hamstring tendon autograft: a systematic review of randomized controlled trials. Arthroscopy. 2018;34(4):1358-1365. [DOI] [PubMed] [Google Scholar]
- 3. Cuzzolin M, Previtali D, Zaffagnini S, Deabate L, Candrian C, Filardo G. Anterior cruciate ligament reconstruction versus nonoperative treatment: better function and less secondary meniscectomies but no difference in knee osteoarthritis—a meta-analysis. Cartilage. 2021;13(1)(suppl):1658S-1670S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Karamchedu NP, Murray MM, Sieker JT, et al. Bridge-enhanced ACL repair leads to greater offloading of the surgical knee and less cartilage damage in the porcine ACL transection model. Am J Sports Med. 2021;49(3):667-674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li J, Rothrauff B, Chen S, et al. Trends in anterior cruciate ligament repair: a bibliometric and visualized analysis. Orthop J Sports Med. 2022;10(10):23259671221132564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lien-Iversen T, Morgan DB, Jensen C, Risberg MA, Engebretsen L, Viberg B. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? A systematic review and meta-analysis. Br J Sports Med. 2020;54(10):592-598. [DOI] [PubMed] [Google Scholar]
- 7. Macri EM, Young JJ, Ingelsrud LH, et al. Meaningful thresholds for patient-reported outcomes following interventions for anterior cruciate ligament tear or traumatic meniscus injury: a systematic review for the OPTIKNEE consensus. Br J Sports Med. 2022;56(24):1432-1444. [DOI] [PubMed] [Google Scholar]
- 8. Mansour J, Ghanimeh J, Ghoul A, Estephan M, Khoury A, Daher M. Bridge enhanced ACL repair vs. ACL reconstruction for ACL tears: a systematic review and meta-analysis of comparative studies. SICOT J. 2023;9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213-218. [DOI] [PubMed] [Google Scholar]
- 10. Muller B, Yabroudi MA, Lynch A, et al. Defining thresholds for the Patient Acceptable Symptom State for the IKDC Subjective Knee Form and KOOS for patients who underwent ACL reconstruction. Am J Sports Med. 2016;44(11):2820-2826. [DOI] [PubMed] [Google Scholar]
- 11. Murray MM, Fleming BC. Use of a bioactive scaffold to stimulate anterior cruciate ligament healing also minimizes posttraumatic osteoarthritis after surgery. Am J Sports Med. 2013;41(8):1762-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Murray MM, Fleming BC, Badger GJ, et al. Bridge-enhanced anterior cruciate ligament repair is not inferior to autograft anterior cruciate ligament reconstruction at 2 years: results of a prospective randomized clinical trial. Am J Sports Med. 2020;48(6):1305-1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Murray MM, Flutie BM, Kalish LA, et al. The bridge-enhanced anterior cruciate ligament repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med. 2016;4(11):2325967116672176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Murray MM, Kalish LA, Fleming BC, et al. Bridge-enhanced anterior cruciate ligament repair: two-year results of a first-in-human study. Orthop J Sports Med. 2019;7(3):2325967118824356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. O’Hara NN. Eliciting health care preferences with discrete choice experiments. JAMA Netw Open. 2022;5(4):e228794. [DOI] [PubMed] [Google Scholar]
- 16. O’Hara NN, Sciadini MF. Using discrete choice experiments to quantify patient preferences. J Am Acad Orthop Surg. 2024;32(1):e9-e16. [DOI] [PubMed] [Google Scholar]
- 17. Persson K, Bergerson E, Svantesson E, et al. Greater proportion of patients report an acceptable symptom state after ACL reconstruction compared with non-surgical treatment: a 10-year follow-up from the Swedish National Knee Ligament Registry. Br J Sports Med. 2022;56(15):862-869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. [DOI] [PubMed] [Google Scholar]
- 19. Sanborn RM, Badger GJ. BEAR Trial Team, et al. Psychological readiness to return to sport at 6 months is higher after bridge-enhanced ACL restoration than autograft ACL reconstruction: results of a prospective randomized clinical trial. Orthop J Sports Med. 2022;10(2):23259671211070542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sanborn RM, Badger GJ, Fleming BC, et al. Preoperative risk factors for subsequent ipsilateral ACL revision surgery after an ACL restoration procedure. Am J Sports Med. 2023;51(1):49-57. [DOI] [PubMed] [Google Scholar]
- 21. Senorski EH, Svantesson E, Sundemo D, et al. Preoperative knee laxity measurements predict the achievement of a patient-acceptable symptom state after ACL reconstruction: a prospective multicenter study. J ISAKOS. 2018;3:26-32. [Google Scholar]
- 22. Sonnier JH, Paul RW, Sando HE, et al. Patient decision making in anterior cruciate ligament reconstruction: a discrete choice experiment examining graft preference. Orthop J Sports Med. 2023;11(2):23259671221144983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vega JF, Jacobs CA, Strnad GJ, et al. Prospective evaluation of the Patient Acceptable Symptom State to identify clinically successful anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(5):1159-1167. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241282657 for Evaluating the Importance of Return to Sports and Hamstring Strength in a Discrete Choice Experiment for Anterior Cruciate Ligament Injury by Scott M. Feeley, Jalen N. Broome, Rachel E. Cherelstein, Benjamin E. Neubauer, Christopher M. Kuenze and Edward S. Chang in Orthopaedic Journal of Sports Medicine