Abstract
Background
The occupational stress that contributes to the development of burnout syndrome remains one of the greatest scientific challenges. Despite years of research into burnout and its determinants, burnout continues to attract the attention of researchers, and healthcare workers (HCWs) continue to experience burnout in large numbers. Burnout has a significant impact on both the mental and physical well-being of HCWs and reduces patient-centered healthcare. This review aims to identify the factors affecting healthcare workers’ burnout (FAHCWB) and their conceptual models.
Methods
The review was conducted according to Arksey and O'Malley's framework using Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). Searches were conducted in PubMed, Scopus, Wiley, ProQuest, Sage, Science Direct, and EBSCO using the following keywords: healthcare professionals, burnout, and internal/external factors. Empirical, qualitative, quantitative, and mixed-design research articles published in English with full-text access in peer-reviewed journals that investigated the FAHCWB were included. For an in-depth analysis of the included articles, the authors developed a data synthesis table, and thematic analysis was applied to the analysis.
Results
According to the inclusion criteria, 38 articles were selected for further data analysis. Six main themes were identified: (1) FAHCWB; (2) conceptual models of FAHCWB; (3) research tools for studying FAHCWB; (4) findings on FAHCWB in the context of different models; (5) differences between findings from different models; (6) what is known and not known about FAHCWB. The results of the review show that most researchers conduct research on factors affecting burnout (FAB) based on factors related to the work environment, with fewer studies based on individual factors, including personality factors. Most of the research is based on the model developed by Maslach et al. The Maslach Burnout Inventory (MBI) has been used in most studies.
Conclusions
Despite years of research, burnout continues to evolve rapidly, indicating that scientific research needs to be re-focused. Research should be conducted using different conceptual models and new research tools that allow the syndrome to be studied from a multidimensional perspective, including both the work environment and individual factors.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40359-024-02130-9.
Keywords: Professional stress, Burnout Factors, Conceptual models, Healthcare Workers
Background
Occupational stress is one of the greatest challenges to well-being and safety, and the number of incidents is rising rapidly. If not properly managed, it leads to burnout, which has significant implications for the individual, the organization and society as a whole [1, 2]. Identifying the factors that contribute to burnout is a complex and intricate process, starting with the need to consolidate clear causes for an unclear pathology that is subject to a complex differential diagnosis.
Compared with the general population, health professionals are at higher risk of experiencing burnout in their work. Burnout among health care workers (HCWs) has become one of the most serious threats to the health care sector, as evidenced by the results of several studies [1–8]. Shaher Al-Otaibi et al. reported that 40% of trauma-orthopedic surgeons in Saudi Arabia suffer from emotional exhaustion and depersonalization [9]. A recent study among orthopedic surgeons reported burnout rates of up to 70% of respondents [10, 11]. In 2023, results from a Latvian study also showed high levels of emotional exhaustion, moderate levels of depersonalization and low levels of personal accomplishment in a sample of HCWs [2]. In addition, the linguistic factor has recently been found to be an important psychological marker in the development of burnout [12]. For example, employees who are more likely to use negative words or words that convey personal responsibility, such as "I" and "my", are more likely to experience an increased risk of burnout. In addition, excessive self-reflection and a focus on negative events in language may contribute to the development of long-term burnout. This suggests that linguistic factors may be an early predictor of the development of burnout, as specific linguistic manifestations, such as emotional expression and cognitive processing, may reveal an individual's psychological exhaustion and inability to deal effectively with professional challenges [12].
In the healthcare sector, stress tolerance and the development of burnout are mainly linked to the factors that influence it. Stress reactions are manifested not only in behavioral changes but also in the physical and mental health of staff. This causes significant damage to the well-being of HCWs and organizations and reduces patient-centered healthcare [13–15], leading to the development of burnout syndrome. FAB can be both work-related and personal [16], and there is some controversy in the research community about approaches to studying FAB Some researchers believe that FAB should be studied from the perspective of work stressors, where the development of burnout is explained as a response to work stress, influenced by factors such as work overload, lack of control, inadequate pay, lack of a sense of community, lack of fairness and conflicting values [17]. As research on FAB developed, Demerouti et al. also defined burnout as an increasing negative response to ongoing work stressors [18]. Furthermore, Portoghese et al. linked FAB to disproportionate workload that is accompanied by low mood, reduced sense of competence, low productivity, increased absenteeism, and turnover. The study of work-related factors considers occupational diversity and complex interactions [19].
About personal factors, the scientific literature refers to both socio-demographic variables and personality traits of the employee. These factors have been identified as predisposing or contributing to the development of burnout, resulting in the development of both physical and mental health problems [20]. Studies of socio-demographic factors [21, 22] have shown a significant relationship between age and burnout. Employees experience lower levels of burnout as they get older. However, the results are not always as consistent. A systematic review of the determinants of burnout [23, 24] found a significant association between increasing age and an increased risk of depersonalization, though also a higher sense of personal achievement. In terms of gender, most studies show that emotional exhaustion and low professional accomplishment are more common in women, while depersonalization is more common in men [25]. In terms of personal factors, it has been shown that the development of burnout depends on how an individual respond to stressors in the work environment. An individual's personality type influences how they perceive their work environment and how they cope with the demands of their work environment [26–28]. Employee exhaustion is not caused by the stressors themselves, but the individual perceives and copes with them [29]. The personality of the individual plays a very important role in this and has a significant impact on professional effectiveness [30, 31], which is why people who are prone to anxiety are more vulnerable to work-related stress [32, 33]. The published scientific literature on FAB and personality traits confirms that certain personality traits could potentially act as both contributing and protective factors for burnout [34].
Considering the above empirical evidence, health care organizations, HCW unions and HCW training institutions are increasingly focusing on HCW well-being, justifying it as a strategic priority and a moral and ethical imperative not only for HCWs but also for the patients they treat [35]. Several conceptual models have been developed in the scientific literature to identify the factors contributing to HCW burnout, based on the scientific literature and empirical research on the high prevalence of HCW burnout, its triggers, and the tragic consequences for HCWs' physical and mental health. The purpose of a conceptual model is to provide a simplified representation of a complex system to facilitate understanding and communication and to inform future research [35]. The process of developing a conceptual model involves deciding what to include or exclude from a given model. For this reason, it is possible to explain the same phenomenon using multiple conceptual model approaches [35]. In the case of burnout among HCWs, the factors that influence burnout are explained within the framework of more than one conceptual model. This advantage and the diversity of conceptual models provides a broader understanding of the factors contributing to burnout. For example, in his article, De Hert combined several models of the factors affecting burnout: The work demand-control model, which focuses on job responsibilities (work demand vs. control) [36], the effort-reward imbalance model, which focuses on the employment contract (effort vs. reward) [37] and the organizational injustice model, which focuses on organizational justice (unfair procedures) [38], resulting in the division of the aetiological factors affecting burnout into two groups: external (work environment) and internal (personality-related) [1]. In addition, scientific literature contains many different conceptual models of burnout contributing factors, such as the person-environment fit model [39], the job characteristics model [40], the diathesis stress model [41], the job demands resource model [42], the NAM model [43], and the multidimensional model [17]. For many years, science has been trying to conceptualize FAB to develop a multidimensional approach to the study of this syndrome.
The most used conceptual model in FAHCWB research that considers factors related to the work environment is the Job Demand-Resource (JD-R) model by Bakker & Demerouti [44]. This model suggests that although each job may have its specific risk factors associated with the development of stress and burnout, these factors can be divided into two main categories: job demands and job resources. Job demands are the organizational psychosocial aspects of work that require cognitive and emotional effort. On the other hand, job resources are the physical, psychosocial, and organizational aspects of work that contribute to the achievement of work goals, professional development, personal development and reduce job demands and their associated psychological or physiological costs [44]. On the other hand, one of the most common conceptual models in FAHCWB research that considers employees' personal burnout factors [45] is the Big Five model [46]. The advantage of this model over other personality research models lies in the broad spectrum of personality research in which everyone is examined based on five core personality dimensions, namely openness (to experience), conscientiousness, extraversion, agreeableness and neuroticism (emotional instability) [46]. Openness includes traits such as broad interests and imagination. Conscientiousness includes organization and the ability to plan. Extraversion includes more specific traits such as talkativeness, energy, and self-confidence. Agreeableness includes compassion, kindness, and affection. Neuroticism includes tension, moodiness, and anxiety [46].
Given that it is detrimental for HCWs, organizations and patient-centered care [13–15], and that there is a positive correlation between it and quitting [47], work-related illness [48] and suicide [49] in the scientific literature, as well as depression, anxiety [50], moral distress [51–55], medical errors [56–58], reduced job satisfaction [59, 60], reduced quality of work life [61], and increased alcohol and drug use [62, 63], it is important to assess the risks of burnout. To do this, it is necessary to identify the most common factors influencing the development of burnout, both at the professional level and at the individual personality level. Scientific evidence on burnout risk factors will help to identify root causes and develop targeted interventions and prevention strategies. Through an understanding of the risk factors, HCWs will be able to change their behavior strategies and adaptation mechanisms. Furthermore, awareness of risk factors will help employers to design their business models to maximize work efficiency and minimize stress within the work environment. This review aims to examine the factors influencing HCW burnout and how they are conceptualized.
Methods
A scoping review strategy was chosen to explore the existing literature relevant to the topic of the study. A scoping review aims to identify the relevant literature on a particular topic, without focusing on assessing the quality of the studies or scrutinizing the selected studies, as is usually done in systematic reviews. A scoping review is a form of knowledge synthesis that identifies existing trends and highlights gaps in the existing knowledge base [64–66]. This review was conducted according to the PRISMA extension for scoping reviews (PRISMA—Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2021 guidelines [67], based on the methodological tool developed by Arksey and O'Malley [64]. Arksey and O'Malley were the first to provide methodological guidance for conducting scoping reviews. To help scientists conduct a qualitative scoping review, the authors suggested that the review should be organized based on six steps (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies for inclusion; (4) extracting and organizing the data;(5) collating, summarizing, and reporting the findings and (6) inclusion of expert advice [64].
Identifying the research question
Based on Arksey & O' Malley's first stage, before launching a scoping review, the research questions should be clearly defined in line with the stated research objective [64].
To clarify the factors affecting burnout and their conceptual models, the following research questions were posed:
What are the factors affecting healthcare worker burnout (FAHCWB)?
Which conceptual models of FAHCWB are the identified studies based on?
What research tools have been used in the empirical studies on FAHCWB?
What are the findings on FAHCWB within the different models?
What differences exist between the results obtained from different models of FAHCWB?
What is known and not known about FAHCWB?
Identifying relevant studies
The second stage of Arksey and O'Malley's framework focuses on the identification of relevant literature based on the stated research aim and questions [64].
At the start of the phase, the three authors collaboratively developed a research search strategy. A three-stage approach was used: (1) searching for existing literature in at least two appropriate databases; (2) identifying relevant keywords and index terms to conduct secondary searches in all selected databases; and (3) manually reviewing references of included articles to identify additional relevant studies. To identify keywords from abstracts and publication titles, this stage of the Arksey and O'Malley framework, the first round of the search was conducted to assess the extent of the relevant literature and identify search terms. An initial limited search was conducted on the PubMed platform: (("professional burnout" OR "occupational burnout" OR "career burnout" OR "burnout syndrome")) AND (("healthcare professionals" OR "health professionals" OR "healthcare worker" OR "health personnel")) AND (("internal factors" OR "external factors" OR "individual factors" OR "work factors" OR "organization factors" OR "national factors" OR "risk factors")). The following keywords were selected for further research: healthcare professionals, burnout, and internal/external factors.
Selecting studies for inclusion
The third stage of Arksey and O'Malley's framework concerns the process of study selection [64].
In this stage, a second and third round of literature searches were conducted. Consequently, the research team jointly developed inclusion and exclusion criteria before the scoping review was initiated (Table 1).
Table 1.
Inclusion and exclusion criteria
| No | Inclusion criteria | Exclusion criteria |
|---|---|---|
| 1 | Empirical studies | Secondary studies |
| 2 | Qualitative, quantitative, and mixed-methods research design. Longitudinal studies | Scoping reports, meta-analyses, systematic reviews |
| 3 | Studies investigating factors affecting burnout in practising health care professionals | Studies investigating factors affecting burnout in samples of health care professionals who are no longer practising |
| 4 | Studies investigating factors affecting burnout in samples of HCWs | Studies investigating factors affecting burnout in non-HCW samples |
| 5 | Studies investigate the factors affecting burnout in doctors, residents, general nurses, and physician assistants | Studies investigating the factors affecting burnout in nurse assistants |
| 6 | Publications which include a conceptual model of the factors affecting burnout | Publications which do not include a conceptual model of the factors affecting burnout |
| 7 | Publications with full-text access | Publications for which the full text was not available |
| 8 | Articles in the English language | Articles in languages other than English |
| 9 | Publications in peer-reviewed journals | Introductory notes, discussions, commentaries, methodological articles, book chapters, conference abstracts, proceedings, reviews, laboratory studies are not included in this scoping report |
| 10 | Publications for the period 2013—2023 | Publications that do not fall within the specified period |
| 11 | Publication duplicates |
According to the keywords identified, from 1 November 2023 to 1 January 2024, two librarians, independent of each other, conducted a comprehensive research search in the following database systems to identify the studies on factors affecting burnout in healthcare professionals:
PubMed – using the filters: 10 years, human, English.
Scopus – using the filters: 10 years, English, article/abstract/ keywords.
Wiley – using the filters: Journals; 2013/2023.
ProQuest – using the filters: peer reviewed; 10 years, English.
Sage – using the filters: Research article; 10 years.
Science Direct – using the filters: research article; 10 years; English.
EBSCO – using the filters: Peer reviewed; 10 years; English.
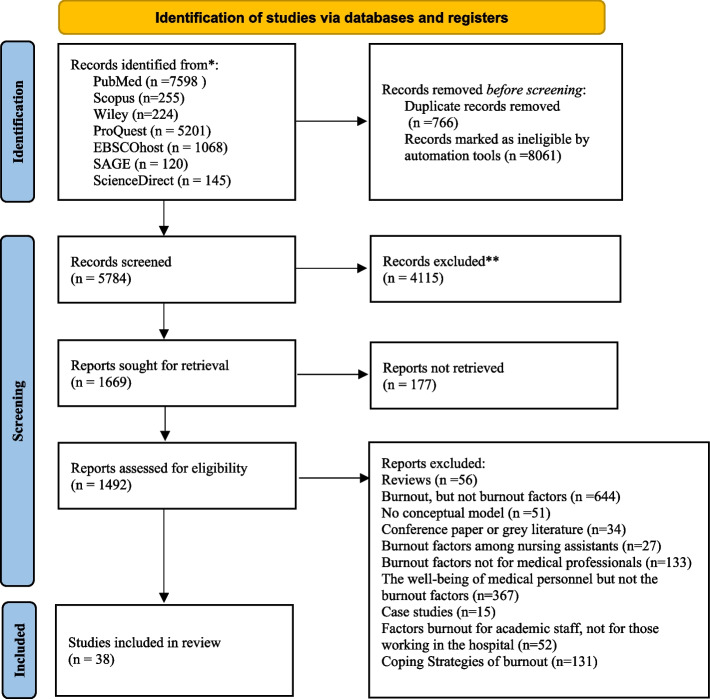
The second search round used search items that had been defined by the researchers and tailored to each database: MEDLINE (PubMed), Scopus, Wiley online library, Sage journals, ProQuest platform, EBSCO platform – namely, the databases MEDLINE Complete; Academic Search Complete; Health Source: Consumer Edition; Health Source: Nursing/Academic Edition; MEDLINE and Science direct. The third-round strategy involved searching within the list of all studies that met the inclusion criteria. MeSH subheadings, Text word, subjects were merged into each set by concatenating with "OR", while distinct sets were concatenated with “AND". We included English-language articles and reviews that provided information on factors affecting burnout among health care workers published in the period 2013–2023. The search strategies for this scoping review are available as an appendix (see S1). Selected studies were exported into the reference management tool EndNote, which helped to improve the screening process of the selected studies. First, duplicate publications were excluded. Next, two independent researchers screened the exported articles by title and abstract against the inclusion/exclusion criteria and the purpose of the scoping review study. In cases where it was not possible to acquire objective information about the relevance of a particular study to the purpose of the scoping review from the publication summary, the full text of the publication was obtained and re-analyzed. In cases where there was disagreement about an article, a third researcher was consulted to decide whether the article met the inclusion/exclusion criteria. All disagreements were resolved in the research group meetings. The PRISMA diagram of the included studies is shown in Fig. 1.
Fig. 1.
Flow diagram of selected studies. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
Extracting and organizing the data
The fourth stage of Arksey and O'Malley's framework refers to the use of descriptive-analytical methods to produce diagrams or a mapping of the data [64].
In this stage of the scoping review, Arksey and O'Malley propose data diagramming/mapping as one of the most effective techniques for synthesizing and interpreting the qualitative data obtained [64]. Therefore, in this scoping review, the three researchers jointly developed a data synthesis matrix based on inclusion and exclusion criteria according to the purpose of the scoping review. Using a standardized template, the following information was extracted: year of publication, author, study title, country, aim, study design, sample size, sample participants, study instruments, theoretical background, outcomes, and burnout factors. A pilot study was conducted in which five publications were independently reviewed by two researchers to determine whether the data synthesis matrix developed clarified the necessary information for the research questions. The two researchers then compared the data to ensure consistency. After analyzing the results, the researchers agreed that the existing data synthesis table identified the research questions raised by the scoping review according to the inclusion and exclusion criteria and was valid for extracting the necessary information.
Collating, summarizing, and reporting the findings
The fifth stage of Arksey and O'Malley's framework refers to the process of developing an analytical system that describes the breadth of literature and prioritizes areas within that literature [64].
Search results
Figure 1 presents a flowchart of the PRISMA-ScR search strategy for the scoping report. The search identified a total of 14,611 titles in seven databases. PubMed (n = 7598), Scopus (n = 255), Wiley (n = 224), ProQuest (n = 5201), EBSCOhost (n = 1068), SAGE (n = 120) and ScienceDirect (n = 145). Of the articles identified, 766 were duplicates and were therefore excluded from further data analysis. In addition, the automated tool excluded 8061 articles that were found to be invalid. Thus, 8827 articles were excluded in the first stage of article identification. In the second stage of screening, the screening of article titles and abstracts, 1669 articles remained for full-text review. However, 177 were excluded because the full text was not available (abstract only) or the full text was not available at all. The full texts of the remaining 1492 publications were assessed against the inclusion/exclusion criteria. As a result, the following articles were also excluded: reviews (n = 56), burnout, but not burnout factors (n = 645), no conceptual models (n = 51), conference paper or grey literature (n = 34), burnout factors among nursing assistants (n = 27), burnout factors not for medical professionals (n = 133), well-being of medical personal but not the burnout factors (n = 367), case studies (n = 15), factors burnout for academic staff, not for those working in the hospital (n = 52), coping strategies of burnout (n = 131). In total, 38 studies were included in the review that were eligible for further analysis.
Characteristics and descriptive analysis of the included studies (n = 38)
A careful, repeated reading of the title, abstract, and full text of each article was the first step in data analysis. After repeated independent reviews of the articles by two researchers, the necessary information was summarized in a data synthesis table developed by the researchers. A third researcher, as an independent expert, reviewed all the publications included in the data synthesis table and checked that they met the inclusion/exclusion criteria.
Most studies were conducted in the United States (n = 5), Australia (n = 2), France (n = 2), Italy (n = 2), Jordania (n = 2), followed by Norway, Romania, Tanzania, North East of Iran, Turkey, Middle East and North Africa, Eastern Ethiopia, Jordan, Singapore, China, Pakistan, Ethiopia, Spain, China, Netherlands, Greece, Marocco, California, South Khorasan, Brazil, Korea, Namibia, Germany, Belgium, and the United Kingdom. Included studies comprised quantitative research designs (n = 26) [25, 26, 68–91], qualitative research designs (n = 9) [92–100] and mixed research designs (n = 2) [101, 102]. A total of 18,518 healthcare practitioners were included. Based on the inclusion criteria, the following HCWs were studied in all reviewed studies: midwives, residents, general nurses, anesthetists, occupational therapists, oncologists, radiologists, neurosurgeons, intensive care physicians, dental hygienists, physiotherapists, general practitioners, pharmacists.
Factors affecting healthcare workers' burnout (FAHCWB)
The development of burnout in HCWs is influenced by many factors at different levels, which can be categorized into socio-demographic [25, 72, 75], individual [87, 88, 103], and work environment [72, 73, 84] factors. The following FAHCWB were identified in this scoping review: socio-demographic, including age (younger respondents) (n = 10), marital status (n = 5) (single respondents), education (n = 3), dependents, gender (n = 2), gender identity, living conditions (n = 1). Individual: personality type (n = 5), moral distress (n = 3), stress resilience (n = 2). Less frequently identified were commitment, values, self-esteem, ability to say no, altruism, perfectionism, lack of confidence, quality of life, sacrifice of personal time, lack of leisure time, lack of regular meals, lack of physical activity, income, psychological distress (n = 1). Work environment related: work experience (n = 7), amount of work, number of hours worked (n = 6), pay (n = 5), specialty, recognition from supervisor, work stress (n = 3), number of patients per day, number of on-call hours per week, amount of work responsibility, lack of training, interpersonal communication problems, work-life balance (n = 2). Less frequently mentioned were the location of the workplace, desire to quit, regret about career choice, type of institution (public or private), number of jobs, type of on-call duty, number of hours of sleep at night, conflicts with superiors, professional demands, conflicts with colleagues, staff rotation, difficulty in taking leave, time between on-calls, professional quality of life, patient location, hospital budget, uncertainty, professional ethics, team, overtime, identification with team or organization, fear of infection, lack of personal protective equipment, lack of professional support, growth opportunities, generational change, passive management style (n = 1).
The above factors are associated with the development of burnout syndrome in HCW, highlighting the need for a holistic approach to the study of burnout syndrome, considering the interplay of the above factors.
Conceptual models
Multidimensional model of Burnout (MMB) [17]. MMB was the most frequently used conceptual model (n = 24) in the studies explaining the development of FAHCWB in terms of work environment factors, mostly in combination with socio-demographic factors [25, 68–70, 72–75, 77, 78, 80–86, 88, 91, 92, 94, 99, 101, 104]. FAHCWB is viewed as chronic stress syndrome (CSS). CSS is characterized by exhaustion, cynicism, and lack of professional effectiveness.
Job demands resource model (JD-R) [42]. The JD-R was the next most common model used in (n = 5) studies [71, 79, 97, 100, 102], which, similarly to the MMB model, explains the development of FAHCWB in terms of work environment factors. In this model, the development of AEFI is explained by analyzing the ratio between work demands and resources [44].
Social Exchange model (SEM) [105]. SEM addresses FAHCWB from the perspective of work environment factors, focusing on the imbalance between individual effort and professional performance. The model was used in (n = 2) studies [74, 90].
Burnout and resilience model (B-RM) [106]. The B-RM model explains FTEF in terms of work environment factors, based on the analysis of two groups of factors: the factors that contribute to burnout and the factors that contribute to resistance to burnout. The model was used in (n = 2) studies [95, 96].
Big Five personality model (BFFM) [46]. The personality theory model, which explores FAHCWB from a personality perspective, focusing on personality openness to experience, conscientiousness, extraversion, agreeableness, and neuroticism, was applied in (n = 4) studies [75, 81, 82, 107].
Three Factor personality model (TFPM) [108]. Compared to the BFFM, the TFPM provides an alternative perspective on the impact of personality on the development of FAHCWB. The personality model focuses on personality dimensions such as extraversion/introversion, emotional stability/instability, and psychoticism/psychasthenia. The model was applied in a (n = 1) study [83].
The conservation of resources theory (COR) [109]. The COR, in the context of the JD-R model, explains the development of FAHCWB from the perspective of Individual personal factors, focusing on the individual factors and how resource losses can contribute to the development of FAHCWB The model was used in (n = 2) studies [97, 110].
Compassion Satisfaction & Compassion Fatigue model (CS-CF) [111]. The development of FAHCWB is explained in terms of individual factors and distinguishes two main components: compassion satisfaction and compassion fatigue, where compassion satisfaction refers to positive feelings while compassion fatigue refers to negative emotions contributing to the development of burnout. The CS-CF model was used (n = 1) in a study [89].
The vulnerability–stress model (VSM) [112]. The development of FAHCWB is explained in terms of individual factors, as the result of an interaction between one's predisposition to vulnerability and the degree of stressors and was used (n = 1) in a study [98].
Burnout subtypes model (BSM) [113]. The model explains the development of FAHCWB in terms of individual factors, based on the individual's three clinical subtypes of burnout: frenetic, under-challenged, and worn-out, and was used (n = 1) in a study [114].
Moral distress model (MDM) [53]. The development of FAHCWB is explained in terms of individual factors, where moral distress arises when an individual is aware of the right actions to take, but institutional constraints make it almost impossible to take the ethically right actions. The MDM model was used in (n = 2) studies [88, 104].
The development of burnout syndrome in HCWs has been explained in scientific literature based on different conceptual models, considering the multidimensional nature of burnout syndrome. As well as the factors influencing burnout, conceptual models also explain the development of burnout in terms of individual and work environment aspects. Conceptual models that focus on the individual study of FAHCWB provide an important perspective on how different personality factors influence the development of burnout in BP. In turn, conceptual models that focus on work environment factors help to explain what work environment factors may contribute to the development of burnout and how this can be prevented by providing the necessary resources and support.
Approaching the development of burnout from the perspective of conceptual models of individual and work environment factors provides a holistic approach to the prevention and control of FAHCWB that can be effective at both individual and organizational levels.
Tools for the empirical research of healthcare workers' burnout (FAHCWB) factors
The following research instruments were identified from a review of the available literature on FAHCWB:
Socio-demographic surveys, which collected: age [69, 71, 72, 80], sex [71–73], place of residence (city or region) [68], education [73, 74, 90], marital status [69, 72–74], dependents [68, 72, 74], hobbies [68, 72], sexual orientation [25], health status [78], living conditions [93], presence of harmful habits [84], chronic illnesses [84]. The following variables were considered for the analysis of occupational factors: work experience [71, 73, 75, 76, 90], specialization [68, 72, 73, 76], number of jobs [70, 78, 90], number of working hours per week [73], number of patients per week [72, 93], documentation burden [72, 92], sector of provision (public or private practice) [72], number of workloads [78, 92], hours of sleep per night [80], number of on-call hours per week [69], opportunities for promotion [70], job commitment [70], job satisfaction [70], relationships between colleagues [72, 80], work-life balance [68, 71], availability of supervision [73], mentoring [25], remuneration [73, 74], communication with management [76], number of calls at night [69], continuing training courses [25, 84, 93], working environment [25, 74, 77], intention to leave [78], number of days of leave taken in the past year [80], number of overtime hours per week [80], number of night shifts per week [80], number of duties [93], rotational working [84], type of on-call (scheduled/called) [84], regret of career choice [84], difficulty in taking leave [84], insufficient time between on-calls to rest [84], duration of on-calls [84].
Maslach Burnout Inventory—Human Services Survey (MBI-HSS) [115]. The instrument was used in (n = 19) studies. It consists of 22 questions exploring factors related to the working environment. Responses are rated on a 7-point Likert scale ranging from never to daily [115]. The instrument measures 3 dimensions of burnout: emotional exhaustion (EE), depersonalization (DP), and personal achievement (PA). The MBI-HSS measures burnout development within the MMB theoretical model.
NEO Five-Factor Inventory (NEO-FFI) [116]. The instrument was used in (n = 5) studies. It consists of 60 questions. Responses are rated on a 5-point Likert scale ranging from strongly disagree to strongly agree. The instrument measures 5 personality dimensions: neuroticism, extraversion, openness, agreeableness, and conscientiousness. The NEO-FFI measures personality factors related to burnout within the theoretical model of the FFM.
Copenhagen burnout inventory(CBI) [117]. The instrument was used in (n = 2) studies. It consists of 19 questions. Responses are rated on a 5-point Likert scale ranging from never to often. The CBI examines burnout in different domains: personal burnout, work-related burnout, and client-related burnout [118]. The CBI measures burnout related to the work environment within the framework of the MMB and SEM theoretical models.
Measure of Moral Distress – Healthcare Professionals (MMD-HP) [119]. The instrument was used in (n = 2) studies. It consists of 27 questions followed by 2 additional questions. Responses are rated on a 5-point Likert scale from 0 to 4. The MMD-HP measures the frequency and level of moral distress. The instrument measures the development of burnout from the perspective of individual factors and was used within the MMD theoretical model.
Professional Quality of Life (ProQOL) [111]. The instrument was used in the (n = 1) study. It consists of 30 questions. Responses are rated on a 6-point Likert scale ranging from never to very often. ProQQL measures an individual's compassion, satisfaction, burnout, and secondary traumatic stress. The instrument measures the development of burnout in terms of individual factors and was used within the CS-CF model.
Job satisfaction survey (JSS) [120]. The instrument was used in the (n = 1) study. It consists of 36 questions. Responses are rated on a 6-point Likert scale ranging from strongly disagree to strongly agree. The JSS measures burnout factors related to the work environment: pay, promotion, supervision, fringe benefits, possible rewards (performance-based rewards), operating procedures (mandatory rules and procedures), colleagues, work type, and communication. The tool was used within the framework of the MMB model.
Eysenck personality inventory (EPI) [121]. The instrument was used in the (n = 1) study. It consists of 57 questions. Responses are rated on a 6-point Likert scale ranging from completely appropriate to completely inappropriate. The instrument examines 3 dimensions of an individual's personality: extraversion, emotional stability, and psychoticism. The EPI measures burnout-related personality factors within the TEMP model.
Oldenburg Burnout Inventory (OLBI) [18]. The instrument was used in the (n = 1) study. It consists of 16 questions. Responses were rated on a 4-point Likert scale ranging from strongly agree to strongly disagree. The instrument assesses two aspects of burnout, emotional exhaustion (OLBI-E) and disengagement (OLBI-D), including the cognitive and somatic aspects. The OLBI measures the work environment-related factors of burnout within the framework of the JD-R model.
Burnout Clinical Subtypes Questionnaire (BCSQ-36) [122]. The instrument was used in the (n = 1) study. The BCSQ-36 consists of 36 questions. Responses are rated on a 7-point Likert scale ranging from strongly disagree to strongly agree. The instrument assesses 3 subtypes of burnout: frenetic, under-challenged, and worn-out. The BCSQ-36 measures burnout in terms of individual factors and was used in the BSM model.
Burnout Assessment Tool (BAT-23) [123]. The instrument was used in the (n = 1) study. It consists of 23 questions. Responses are rated on a 5-point Likert scale ranging from never to always. The instrument measures the development of burnout based on two dimensions: primary symptoms (exhaustion, psychological distance, cognitive and emotional disturbances) and secondary symptoms (psychological distress, psychosomatic complaints). The BAT-23 measures the development of burnout in terms of work environmental factors and was used in the framework of the SEM model.
Semi-Structured Interview. This approach was used in (n = 6) studies. The instrument was used to explore burnout and the factors leading to it, as well as what individual and professional factors influence the development of burnout, and coping strategies.
Focus group interviews. This instrument was used in (n = 2) studies. It was used to identify FAHCWB, the strategies to promote burnout resilience, and possible solutions to reduce burnout that is related to workplace culture and effectiveness, work-life balance, and resilience.
Findings on FAHCWB under different models
Multidimensional model of Burnout (MMB) [17]. Within this model, it was found that AEIF is associated with work environment factors such as job satisfaction [68], lack of support at work, long working hours, lack of employees [25], and thoughts of resigning [78]. This model was mostly used in combination with socio-demographic factors: work-life balance [68], marital status [90], and age [75]. From the above, it can be concluded that employees who experienced lower job satisfaction, lack of support at work, and long working hours experienced emotional burnout. Thoughts of resignation are fostered by insufficient professional support and lack of resources, which characterize the depersonalization of the individual. As a result, the employee ends up with a reduction in professional achievements. Furthermore, socio-demographic factors were associated with the development of the burnout syndrome. Work environment factors in interplay with socio-demographic factors influence the development of burnout syndrome in HCWs.
Job demands resource model (JD-R) [42]. Within this model, FAHCWB was found to be associated with work environment factors such as work environment, overall job satisfaction, and employee dedication [71]. Meanwhile, personal resources such as the opportunity to develop professional skills and patient-centered healthcare act as protective factors [79]. From the above, it can be concluded that burnout develops in situations where there is an imbalance between professional demands and employee resources.
The conservation of resources theory (COR) [109]. Within this model, the passive management style and the number of work conflicts were identified as significant work environment related FAHCWB. These are positively associated with burnout and poorer physical health, as well as increased work-family conflict [110]. It can therefore be concluded that the passive management style has a certain impact on both the organization and the employee and their private life. This in turn contributes to employee dissatisfaction and the development of burnout syndrome.
Social Exchange model [105]. Within this model, work environment related FAHCWB was found to be the work in the outpatient department and the reorganization of the hospital [90]. In addition, when looking at the association of work environment factors with socio-demographic factors, a positive association was found with age (younger) and marital status (single) [90]. It can be concluded from the above that the specific characteristics of the work environment and changes in the organization create a more stressful and high-pressure situation for employees, which in turn contributes to the development of burnout syndrome. In addition, younger workers and those without a partner are more susceptible to stress and pressure in the work environment, which increases the risk of developing burnout.
The diathesis-stress model/the vulnerability–stress model [112]. Within this model, individual vulnerability was identified as one of the FAHCWB. This aspect is explained as the employee's desire to do the job well. In addition, the work environment-related FAHCWB were identified, which were the immediate supervisor, the work-life balance, and the teamwork [98]. From the above, it can be concluded that employees with high standards and those who are demanding of themselves are at a higher risk of stress as well as of developing burnout syndrome. In addition, work-life imbalances and conflicts with the work team or the manager contribute to the development of burnout.
Burnout and resilience model [106]. Within this model, the work environment related FAHCWB were identified as systemic factors: the impact of problems in local, regional, and national systems that make it difficult to care for patients during hospitalization and after discharge, and long queues of patients. Administrative factors: the focus on acute conditions and ignoring the causes of readmissions, the intense pressure to discharge patients, and the lack of resources [96]. In addition, individual FAHCWB were identified as contributing to persistency: engagement in meaningful work, patient-centered care, and positive interactions with the patient [96]. From the above, it can be concluded that systemic and administrative factors lead to increased stress and psychological pressure. The limited availability of resources led to feelings of powerlessness and meaninglessness among the HCWs, contributing to the development of burnout syndrome. On the other hand, individual factors that promote resilience act as protective factors against burnout. These factors contribute to employee motivation and positive attitudes, which help to reduce the risk of burnout.
Big Five personality model [46]. Within this model, one of the individual FAHCWB was found to be personality, a relatively stable trait that influences behavior and how PHCWs deal with everyday situations. Certain personality factors, such as neuroticism, show a strong association with the development of burnout. At the same time, burnout is negatively associated with extraversion, agreeableness, conscientiousness, and openness to experience [107]. From the above, it can be concluded that an individual's personality plays a role as one of the individual FAHCWB. Neurotic people are prone to emotional instability and stress reactions that contribute to the development of burnout syndrome.
Moral Distress (MD) [53]. Within this model, the MD was found to serve as one of the individual FAHCWB [87, 88]. The MD may vary depending on the HCW's specialization [87], with physicians having higher levels of MD than general nurses. This suggests that in situations where HCWs experience MD, a burnout syndrome develops. The development of burnout about MD in different professional fields may in turn reflect the different values, beliefs, and approaches across professional fields in how individuals experience and respond to ethical dilemmas and moral situations.
Stamm’s Compassion Satisfaction & Compassion Fatigue model (CS-CF) [111]. Within this model, such individual FAHCWB as compassion satisfaction and compassion fatigue were identified. Compassion satisfaction is fostered by altruistic behaviors that help to alleviate patients' suffering. Compassion fatigue, on the other hand, develops in situations where the individual is faced with high emotional burdens and negative stressors [89]. Thus, it can be concluded from the above that when compassion fatigue becomes too pronounced and prolonged, it leads to burnout syndrome, especially in situations where the individual cannot effectively restore their emotional resources and feel satisfaction from their professional performance.
Eysenck’s Personality, a 3-factor model [108]. Within this model, an individual personality factor such as neuroticism was identified as one of the FAHCWB positively associated with the development of burnout. In contrast, extraversion shows a negative association with the development of burnout [83]. From the above, it can be inferred that people with high levels of neuroticism may react more strongly to environmental stimuli and find it more difficult to recover from each emotionally arousing experience, which contributes to the development of burnout syndrome.
Differences between the results derived from different FAHCWB models
Most conceptual models of FAHCWB focus specifically on the development of burnout because of work-related environmental factors, but research is based on different aspects of the work environment. This scoping review identified several conceptual models related to work environment factors that explore the development of burnout from different aspects of the work environment. For example, the multidimensional model of burnout [17] explains the development of burnout in terms of these three dimensions: emotional burnout, depersonalization, and reduction in personal achievement. The Job demands resource model [42] examines the development of burnout based on the professional demands and resources of the employee. The social exchange model [105] focuses on the imbalance between the individual's effort and professional performance. The burnout and resilience model [106] explains the development of burnout by exploring two types of factors: the factors that contribute to burnout and the factors that contribute to the resistance to burnout [105]. Some of the main work environment-related factors that contribute to burnout were work experience (n = 7), working hours, work volume (n = 6), remuneration (n = 5), work stress (n = 3), etc.
A deeper analysis of the conceptual models of FAHCWB in the studies included in this scoping review revealed a shift in research focus, with researchers emphasizing the role of individual factors in the development of burnout, in addition to the work environment-related factors. One of these models is the Big Five personality model [46]. It examines the development of burnout from the perspective of personality factors, namely openness to experience, conscientiousness, extraversion, agreeableness, and neuroticism, and explores the predisposition to burnout syndrome. Neuroticism has been shown in several studies to be a factor in FAHCWB [75, 81, 82, 107]. Neuroticism as a burnout predisposing factor is also supported by Eysenck's personality, i.e. a 3-factor model [108]. Another important FAHCWB is the moral distress (MD) experienced by HCWs in situations of moral and ethical dilemmas in their professional activities [53].
Differences within the frameworks are observed depending on the research paradigm chosen for the study of the burnout FAHCWB. Different conceptual models focus on different factors contributing to burnout to explain the multidimensional phenomenon of burnout.
What is known and what is not known about the factors that influence the development of burnout
The analysis of the scientific literature revealed that:
Current research on the concept, development, and study of burnout is closely related to the Maslach Burnout Inventory [115] and its variants, which is supported by this scoping review which found that of the 38 included studies, 19 studies used the MBI and its variants (see S2). Accordingly, burnout is categorized and measured by most studies as a work-related syndrome characterized by emotional exhaustion, cynicism, and reduced professional efficacy (feelings of incompetence) that individuals experience about their work [115]. MBI is considered the gold standard for measuring burnout [124]. However, there is a growing scientific debate that the MBI dimensions do not include information on other characteristics of burnout. To date, it has been established that one of the characteristics of burnout is a negative change in one's cognitive abilities. Changes in concentration, attention, and working memory have been noted [125]. Given this, it can be argued that Maslach's multidimensional conceptual framework is insufficient to capture the multidimensional nature of burnout syndrome. There is concern in the scientific community as to whether one of the dimensions of MBI, i.e. personal achievement reduction, serves as a constituent of burnout [124]. In addition, the MBI was designed as a research tool, not as an instrument to gauge the level of burnout in organizations. More importantly, over the years, several conceptual as well as technical challenges have been raised against the use of the MBI. For example, it has been argued that reduced professional effectiveness should be seen because of burnout rather than as a component [124]. Conversely, impaired cognitive functioning is erroneously not considered as an indicator of burnout in the MBI [125]. From a psychometric perspective, the MBI has been criticized for (1) biased response patterns that may affect its reliability; (2) reversing positively worded items to assess negative psychological states; and (3) scoring three different subscales instead of a single, composite burnout score [123]. Therefore, an alternative self-assessment questionnaire has recently been developed which effectively addresses these conceptual and technical issues; namely the Burnout Assessment Tool (BAT) [123]. The questionnaire includes four subscales: exhaustion (extreme fatigue); mental distancing (psychological withdrawal); cognitive and emotional impairment (reduced ability to regulate one's cognitive and emotional processes properly) [123].
This close link between the 'gold standard' theory and the research instrument has led to the neglect of other conceptual approaches to studying the burnout syndrome. As a result of this neglect, the development of burnout is viewed from a narrow perspective, which defines the development of burnout as being exclusively related to work environmental factors. The syndrome continues to develop on a massive scale, causing disproportionate losses. This demonstrates the need to complement the current standards with both new conceptual research models and new instruments. A deeper understanding of why, despite years of study into this syndrome, it remains an issue, and HCWs continue to burn out, and it causes great losses to organizations, to the well-being of HCWs, and the healthcare sector.
Socio-demographic factors of the worker are known to contribute to the development of burnout [75–77, 90], but it is still unclear which socio-demographic factors play a key role in the development of burnout. Which socio-demographic factors are protective for burnout in HCWs? How does the place of residence of an individual influence the development of burnout, e.g. if they live in a city or if they live in a country outside a city?
Personality traits influence burnout [75, 81–83], but it remains unclear how an individual's personality influences and exacerbates the development of burnout. How does an individual's emotional intelligence influence the development of burnout? How does an individual's self-esteem influence the development of burnout? What is the role of empathy and altruism in burnout?
The development of burnout is influenced by HCWs' satisfaction with the quality of their working life [89], but it remains unclear which aspects of the quality of working life contribute to the development of burnout.
There is a positive association between job satisfaction and the development of burnout [74], but which aspects of job satisfaction play a key role in the development of burnout is still not explored in scientific literature. Which employee personality traits influence job satisfaction and what is the impact of these two variables on the development of burnout? What is the mechanism of the onset of burnout: does the burnout syndrome develop from job dissatisfaction or does job dissatisfaction result from burnout? Which aspects of professional satisfaction serve as protective factors for burnout?
Inadequate work-life balance is a contributing factor to physical and emotional burnout [68], but the determinants of this imbalance that play a critical role in the development of burnout are still not identified. What aspects of work-life balance serve as mitigating factors for burnout?
The development of burnout varies depending on individual characteristics (e.g. personality or socio-demographic factors) [75] and the work environment (e.g. job requirements or management styles) [79], but it remains unclear which personal factors, in combination with work environment factors, pose a greater or lesser risk of the development of the burnout syndrome. For example, do all personality types experience the same manifestations and consequences when exposed to the same occupational stressor? Which personality subtypes are more vulnerable to burnout when exposed to triggers? Which are potentially more dangerous combinations of individual characteristics and work environment triggers? And which are less dangerous?
Most studies of FAHCWB are based either on the work environment [69, 90, 91] or an individual employee's factors [26, 75]. Very few studies consider the development of this syndrome as a multidimensional phenomenon, which should be studied considering the interaction of the two aforementioned factor domains. How does the interaction of these factors affect the quality of patient care? How does the interaction of these factors affect patient safety?
There is a positive association between MD and burnout [126–129], but it is still unclear to what extent MD is a factor contributing to burnout. MD and burnout are similar phenomena, so it may be argued that their determinants are also similar, for example, the association of burnout with patient death and ethical decision-making [130, 131].
Most recent studies on FAHCWB have used a quantitative research approach [68, 69, 71, 72, 74, 75, 80, 90, 91]. However, the results obtained in the scientific literature confirmed that burnout syndrome should be considered a multidimensional phenomenon [71]. Accordingly, the syndrome should be studied using different research methods that complement each other. For a holistic study of the factors influencing burnout, the results obtained from quantitative research methods should be complemented with an in-depth exploration of individual experiences of burnout using qualitative research methods or a mixed-methods approach.
Most FAHCWB studies confirm that work environment-related factors are highly prevalent (see S3). And one of the determining factors is the professional cooperation with one's superiors [85]. It is still not studied how exactly the hyperfunctional or dysfunctional role of superiors contributes to the development of burnout. How does an active or passive management style affect the employees' stress levels, productivity, fatigue, overwork, mental and physical health, patient-centered healthcare, and increased risk of conflict within the family?
Inclusion of expert advice
The integration of expert consultants in the scoping review process is emphasized in academic literature [64, 66, 132, 133]. Many scholars agree that the involvement of experts in the process provides the key feedback for determining the breadth of the scoping review and integrating the knowledge gained. However, there is debate in the scientific literature on the timing and extent of expert involvement throughout the scoping review process [64, 65]. Furthermore, the original conceptual framework by Arksey and O'Malley referred to expert advice as an optional component of the scoping review [64]. Consequently, we have also not included expert advice in this scoping review.
Discussion
This review aims to explore FAHCWB and its conceptual models and to provide a comprehensive overview of the available scientific evidence. All studies included in this review focused on the identification of FAHCWB. In addition, it was important to clarify which conceptual models in scientific literature explain the development of burnout. To address the prevalence of burnout syndrome among HCWs, it is first necessary to identify potential risk factors and the interactions between these risk factors. In assessing FAHCWB, several factors were considered, the most important of which were occupational environmental factors and individual factors: socio-demographic factors as well as personality traits. Evidence-based scientific research will serve as a basis for the development of interventions aimed at reducing the development of burnout in HCWs.
Factors affecting healthcare workers' burnout (FAHCWB)
When addressing the factors that predispose healthcare workers to burnout, several FAHCWB were identified, which were classified based on previous research as socio-demographic, individual, and work environment-related.
Socio-demographic factors
This review identified age as one of the socio demographic FAHCWB factors, with a tendency towards younger age HCW. These results were confirmed in the studies by other researchers [134–136], education being consistent with [137], marital status being consistent with [138]. Researchers are divided into genders as a contributing factor. Studies that have examined men and women were unable to establish a clear correlation, so gender should not be seen as one of the critical contributing factors in the development of burnout. Within the context of this scoping review, only 2 studies [73, 102] mentioned gender as a contributing factor to burnout. If this factor is considered from the perspective of an entrenched gender stereotype, men may feel much more pressure in the breadwinner role, which makes it more difficult to leave a career that they do not enjoy. Male respondents are more interested in remuneration and career progression [139]. On the other hand, women are considered to have different priorities and manage to balance family life and work roles, which may explain some of the gender differences in the development of burnout [139, 140]. Work experience was another socio-demographic factor mentioned [73, 84, 91], which is in line with the results of other studies. It is important to consider the contradictory results presented in the literature. Some studies suggested that lower work experience was associated with the development of burnout [141, 142]. In contrast, other studies found that it was the respondents' duration of work experience that served as a contributing factor to burnout [139, 143]. Marital status was confirmed as one of the FABs in some studies, which is also supported by other studies where, for example, being married was found to be associated with the development of burnout [144, 145]. Another study identified that unmarried or divorced people are at risk of developing burnout [90]. However, not all studies support the importance of marital status, and more specifically the fact of being unmarried, as a predisposing factor for burnout [146]. Studies are showing higher levels of stress in physicians who are married or widowed compared to unmarried or divorced physicians, which in turn may contribute to the development of burnout [147].
Thus, socio-demographic factors such as age (with a tendency towards younger ages), gender, education, work experience, and marital status were found to play a significant role in the development of burnout in HCW. A holistic study of FAHCWB requires socio-demographic factors to be studied in interaction to form a complex syndrome.
Individual factors
MD has been cited as an individual risk factor [87, 88]. The positive association of burnout with MD has also been demonstrated in many other scientific studies [126, 127, 148]. This influencing factor has been widely recognized in HCWs who carry out their professional activities in intensive care units and are exposed to various ethical problems and stressors related to the clinical situations of patients and their families (e.g. critically ill or dying patients; dealing with families' perception of certain treatments as being futile), as well as the dynamics of the relationship within their work group/interdisciplinary healthcare teams (e.g. poor communication), and the organizational context (e.g. lack of resources), which can play pivotal roles in both MD and burnout development [149]. In addition to individual factors, human personality traits were mentioned. The influence of this factor on the development of burnout has also been demonstrated in other studies, in which individuals with high levels of neuroticism and extraversion were also found to report high levels of stress and show high levels of burnout [103].
Individual factors such as MD, and personality traits (neuroticism, extraversion) are positively associated with the development of burnout, supporting the fact that the study of individual and personality factors plays an important role in the understanding of burnout syndrome.
Factors related to the work environment
Communication with colleagues, immediate supervisors, heavy workload, lack of resources, and lack of support were some of the most frequently mentioned risk factors related to the work environment [74, 78, 84]. The salary factor was a frequent factor, which is consistent with the results of other authors [150]. This could be explained by the investment of time needed for financial security, with less time available for leisure, family, or hobbies. Time shortages/constraints, workload, and the impossibility of career development. The relationship between these factors to burnout is likely to depend on the specialization of the HCW concerned, their level of preparedness, the degree of autonomy, and interpersonal relationships, both within the team and with the management and patients. These results are supported by other studies that demonstrated a positive association with longer working hours and an inverse association with occupational satisfaction [145, 151–153]. Additionally, employees' thoughts about leaving their jobs were mentioned [78], which is consistent with [154]. The lack of support from supervisors (managers who encourage and advise when necessary) [94] was identified as one of the work environment-related factors contributing to burnout. Support for HCWs can serve as an opportunity to develop new skills and improve the efficiency and quality of their care delivery. Work experience that is consistent with studies in Ethiopia [138, 154]. In addition, the HCWs also mentioned administrative burden and digitalization as factors contributing to burnout, depriving caregivers of time that otherwise could be spent on care, which is in line with the results obtained by West and colleagues [155]. All the above factors have an impact on employees' satisfaction with their professional activity, which serves as one of the determinants of the development of burnout [71, 76]. Correlational studies on job satisfaction by other researchers have shown a significant inverse relationship between the determinants of job satisfaction and emotional exhaustion and depersonalization (excluding promotions and fringe benefits) [74], which was confirmed in the results obtained in this scoping study. Job dissatisfaction can lead to higher levels of burnout, which is consistent with the results of other studies [156]. According to the theory of the organizational health approach, a lack of incentives and rewards leads to lower employee morale and higher anxiety [157], which in turn is supported by a study in Croatia that confirmed a highly significant correlation between emotional exhaustion and reward and reward satisfaction [157].
Research instruments
Several assessment tools have been used to study burnout, with different approaches and focuses. The Maslach Burnout Inventory-Human Services Survey (MBI-HSS) [115] focuses on three main dimensions: emotional exhaustion, depersonalization, and personal accomplishment, but does not fully capture factors related to interaction with patients and staff. The Copenhagen Burnout Inventory (CBI) [117] extends this approach by including questions about customer relationships, which are particularly relevant in the healthcare sector. Personality instruments such as the Eysenck Personality Inventory (EPI) [121] and the NEO-FFI [116] focus on individual causes of burnout by examining personality traits, but they underestimate the impact of the work environment. The Moral Distress for Healthcare Professionals (MMD-HP) [119] examines moral distress caused by ethical dilemmas and conflicts and its impact on burnout. The Job Satisfaction Survey (JSS) [120] analyses job satisfaction and its relationship to burnout, focusing on pay and management aspects. The Professional Quality of Life (ProQOL) [111] assesses compassion fatigue and emotional satisfaction, with a focus on emotional distress in health and social care. The Burnout Assessment Tool (BAT-23) [123] covers burnout symptoms in the context of both emotional exhaustion and psychosomatic complaints, with a particular focus on work environmental factors. In addition, the Oldenburg Burnout Inventory (OLBI) [18] assesses emotional exhaustion and detachment from work, while the Burnout Clinical Subtypes Questionnaire (BCSQ-36) [122] identifies three subtypes of burnout: fanatical, detached, and resigned.
These instruments offer different perspectives and can be divided into two categories: personality instruments, which explore individual factors of burnout, and work environment instruments, which highlight the importance of the interaction between working conditions and clients. The type of instrument chosen has a significant impact on the findings of the study and their practical application in the development of burnout prevention and management strategies.
Conceptual models
In this scoping review, the majority of the studies were performed based on the multidimensional Maslach burnout model [17]. This model describes burnout as a syndrome of depersonalization, reduced personal achievement, and emotional exhaustion as related to 'people work' [115]. However, this model has been increasingly criticized and, as an alternative, it has been proposed to study burnout through the Social Exchange model [105]. This model suggests that burnout is an interaction between inability and unwillingness. An individual no longer expends the efforts required to do the job properly. According to the author, 'inability' is manifested as a lack of energy, while 'unwillingness' is manifested as increased resistance, decreased commitment, lack of interest, and disengagement. Inability and unwillingness are two inseparable components of the phenomenon of burnout, reflecting its energetic and motivational dimensions respectively [123]. This model is complemented by the job demand-resource model (JD-R) [158], where the main components of the burnout process are a lack of energy leading to exhaustion and increased fatigue, while at the same time, mental disengagement is manifested in a lack of professional interest and dislike of work. De Beer [159] and Sakakibara and colleagues [160] also based their research on the Social Exchange Model, where they looked at burnout as work-related exhaustion, extreme fatigue with a reduced ability to regulate cognitive and emotional processes, and mental distancing. As a result, depressed mood and non-specific psychological and psychosomatic complaints can develop. These basic conceptual models of burnout are combined with different models of individual burnout factors, such as [46], which is consistent with conceptual models selected by others in burnout research [161], and Moral Distress (MD) [53], which is consistent with [162].
The diversity of conceptual models supports the need for a multidimensional and integrated approach to research on burnout, incorporating both work environment factors and individual and personal characteristics.
Research methodology
Despite the breadth and diversity of the literature, most of the included studies (n = 26) used quantitative research methods, most commonly cross-sectional research designs. While this methodological model is certainly important in comparing findings across groups and between countries, it fails to answer the 'why' or 'how' questions that might shed light on the experiences of HCWs struggling with burnout. Without undermining the value and importance of existing research in expanding the understanding of burnout among HCWs, a qualitative research methodology would additionally provide the depth of insight needed into how HCWs experience burnout and in identifying possible solutions. This may be particularly important when researching sensitive topics such as burnout and mental health. Cross-sectional models, which allow researchers to explore the relationship between variables, do not allow us to identify causal and temporal effects between burnout and other factors. Longitudinal research designs would allow researchers to identify which factors cause burnout or what solutions or strategies mitigate it. Only one review used a longitudinal study design [94].
The burnout syndrome is a global challenge for healthcare systems worldwide, affecting from 25 to 75% of healthcare professionals. Prevalence rates vary by specialization in some countries [163]. The results highlight the need for a holistic approach to the well-being of HCWs. Furthermore, the results confirm the need for preventive support programs, which should include a mix of individual and organizational strategies. The implementation of strategies to help reduce work-related stress may contribute to reducing burnout syndrome in the healthcare sector. Strategies should be targeted at the employee individually as well as collectively from an organizational perspective. Reorganizing the work process, selecting staff according to demand, allocating responsibilities by existing resources, recognizing the early signs of the burnout syndrome, modifying stress factors, and developing and implementing organizational policies that improve both the quality of work and the individual and professional life of the employee, in addition to offering emotional support and incorporating integrative and complementary practices [164]. The above strategies can have a positive impact on the physical and mental health and well-being of HCWs. Moreover, they may also improve the quality of patient care and the patient-centered holistic healthcare approach.
Conclusions
The burnout syndrome is a multidimensional phenomenon that depends on many factors differing in their nature. The scientific literature attempts to explain the complex nature of burnout syndrome through several conceptual models. This demonstrates that there is still no clear consensus on how to understand, study, and identify the factors influencing this syndrome. Furthermore, it is necessary to use both inductive and deductive methods of knowledge building.
MBI served as one of the first research tools that have led to a wealth of important knowledge on the way to understanding the complexities of this syndrome. Over time and owing to the great interest of scientists in the study of this syndrome, knowledge has been substantially increased. The burnout syndrome has been studied from different aspects that we, as researchers, were previously unaware of. Consequently, many new aspects have now emerged that were not considered when the Maslach Multidimensional Conceptual Model was developed. Consequently, conducting burnout research solely based on the MBI, which is an outdated tool, is incorrect, misleading, and may lead to incorrect conclusions.
It is crucial to distinguish between the manifestations of burnout syndrome. These can be at the level of an individual's complaints, where the person is experiencing short-term stress but is still engaged in professional activity. Or chronic disorders, whereby the person is no longer able and no longer perform his or her professional activity. Van Dam defines this condition under the term 'clinical burnout' for chronic stress disorders [165]. Consequently, most of the research and knowledge is based on questionnaire studies, i.e. investigations of the complaints of burnout in relatively healthy, occupationally active individuals.
It is important to recognize that burnout should not simply be denied or defined as a complaint but understood as a real and medically recognized diagnosis that may require professional assessment and appropriate treatment. Burnout syndrome involves a variety of manifestations and implications for an individual's well-being, occupational sphere, and overall quality of life. Treatment strategies may include therapy, psychological support, Balint groups, supervision, changes in working practices and lifestyle, and, where necessary, pharmacological treatment.
Limitations
Given the specific epidemiology and evolving nature of professional burnout, which differs from other psychosocial constructs, the search constructs used in this scoping review were not exhaustive of all burnout terminology that is currently and historically used. Therefore, some of the studies that identified influencing factors of burnout syndrome may have been missing. A further limitation was that the publications are limited to the English language, which could potentially introduce bias, however, the lack of expertise in language skills prevented us from comprehensively analyzing publications in other languages. The Scoping Review contained no assessment of the quality of publications. The publications included in the review do not cover all studies carried out in the past, as a specific time range for the search was specified. Burnout syndrome was studied in HCWs in general, but the factors influencing this syndrome may vary by specialization and the demographics of the respondents. Despite these limitations, the review examines in detail the factors influencing burnout in HCWs and their conceptual models, which have important implications for HCWs' well-being and patient-centered healthcare. The evidence presented in the review will contribute to a broader understanding of the FAHCWB, which should be considered when conducting research in larger samples of HCWs and when designing interventions to reduce burnout.
Further research
Based on the FAHCWB identified in the scoping review, it would be worthwhile to complement and develop the knowledge gained in the following future research areas:
New research tools: there is a need to develop new and improved tools that capture the multidimensional nature of burnout syndrome, including both subjective levels of complaints and objective indicators of chronic disorders and clinical burnout.
Broadening the common understanding: focusing research on new perspectives and factors that could influence the development of burnout, such as the use of digital technologies at the workplace, the impact of globalization on work organization and professional practices, and the impact of climate change on the health care system.
Clarifying clinical manifestations and diagnostics: more research is needed on the clinical manifestations and diagnostic criteria of burnout syndrome to ensure correct detection and treatment. This includes assessing individual factors as well as evaluating organizational and social impacts.
Research on the effectiveness of interventions: there is a need to investigate the effectiveness of different interventions and treatment strategies, including therapy, psychological support, organizational changes, and preventive measures. This will help to identify the most effective approaches to preventing and coping with the burnout syndrome.
Longitudinal analysis: long-term studies are needed to understand the continuing impact of burnout on individuals and organizations, and to track the long-term effectiveness of treatments and interventions.
These future research directions provide an opportunity to improve our understanding of burnout syndrome, the factors influencing it, and the relevant solutions that could improve the well-being and effectiveness of both individuals and organizations.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- FAHCWB
Factors affecting healthcare workers' burnout
- FAB
Factors affecting burnout
- HCW
Healthcare worker
- MBI
Maslach Burnout Inventory
- MBI-HSS
Maslach Burnout Inventory-Human Services Survey
- MBI-GS
Maslach Burnout Inventory-General Survey
- JSS
Job Satisfaction Survey
- CBI
Copenhagen burnout inventory
- OLBI
Oldenburg Burnout InventoryBurnout
- BCSQ-36
Clinical Subtypes Questionnaire
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
- MMB
Multidimensional model of Burnout
- JD – R
The job demands a resource model
- COR
The conservation of resources theory
- SEM
Social Exchange model
- B-RM
Burnout and resilience model
- FFM
Five personality model
- TEPM
Three Factor personality model
- CS – CF
Compassion Satisfaction & Compassion Fatigue mode
Authors’ contributions
EN performed the initial literature search, organized the obtained results, summarized, and interpreted them, and wrote the first version of the manuscript. IG, SM developed the research questions, and revised the written manuscript. OR, AI, IS performed the selection of studies, and examined the full articles of the obtained studies according to the inclusion and exclusion criteria. OR performed the translation work of the manuscript.
Funding
Not applicable.
Data availability
All data obtained or analyzed during this study are included in the Supplementary [S1, S2, S3].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. 2020;13:171–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagle E, Cerela-Boltunova O, Blumberga S, Mihailova S, Griskevica I. The burnout and professional deformation of latvian healthcare workers during the COVID-19 pandemic at the traumatology and orthopaedics hospital. Social Sci. 2023;12(3): 175. [Google Scholar]
- 3.Novilla MLB, Moxley VBA, Hanson CL, Redelfs AH, Glenn J, Donoso Naranjo PG, et al. COVID-19 and psychosocial well-being: did COVID-19 worsen US frontline healthcare workers’ burnout, anxiety, and depression? Int J Environ Res Public Health. 2023;20(5):4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le RT, Sifrig B, Chesire D, Hernandez M, Kee-Sampson J, Matteo J, et al. Comparative analysis of radiology trainee burnout using the Maslach burnout inventory and Oldenburg burnout inventory. Acad Radiol. 2023;30(5):991–7. [DOI] [PubMed] [Google Scholar]
- 5.Delgado N, Delgado J, Betancort M, Bonache H, Harris LT. What is the Link Between Different Components of Empathy and Burnout in Healthcare Professionals? A Systematic Review and Meta-Analysis. Psychol Res Behav Manag. 2023;16:447–63. [DOI] [PMC free article] [PubMed]
- 6.Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Wang H, Carlasare LE, Dyrbye LN. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2020. In: Mayo Clinic Proceedings, Vol. 97, No. 3. Elsevier; 2022. p. 491–506. [DOI] [PubMed]
- 7.Kane L. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape; 2020. Available from: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460.
- 8.Lyubarova R, Salman L, Rittenberg E. Gender differences in physician burnout: driving factors and potential solutions. Permanente J. 2023;27(2):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Otaibi MLS, Alyali SA, Alshehri TK, Alshehri AK, Alshahrani AA, Banah AG, et al. Burnout syndrome among southern region orthopedic surgeons, Saudi Arabia. J Fam Med Prim Care. 2020;9(5):2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu J, Zou F, Sun Y. Job satisfaction, engagement, and burnout in the population of orthopedic surgeon and neurosurgeon trainees in mainland China. Neurosurg Focus. 2020;48(3):E3. [DOI] [PubMed] [Google Scholar]
- 11.Liang S, Zhou W, Zhao Q, Li L. Prevalence and risk factors of burnout among Chinese pediatric orthopedic surgeons. J Pediatr Orthop. 2021;41(1):e80–4. [DOI] [PubMed] [Google Scholar]
- 12.Castiglioni M, et al. Linguistic predictors of psychological adjustment in healthcare workers during the COVID-19 pandemic. Int J Environ Res Public Health. 2023;20(5):4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(10):1317–31. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ open. 2017;7(6):e015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boo YL, Liam CCK, Lim SY, Look ML, Tan MH, Ching SM, et al. Stress and burnout syndrome in health-care providers treating dengue infection: a cross-sectional study. Med J Malaysia. 2018;73(6):371–5. [PubMed] [Google Scholar]
- 17.Maslach C. A multidimensional theory of burnout. Theories Organ Stress. 1998;68(85):16. [Google Scholar]
- 18.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499. [PubMed] [Google Scholar]
- 19.Portoghese I, Galletta M, Coppola RC, Finco G, Campagna M. Burnout and workload among health care workers: the moderating role of job control. Saf Health Work. 2014;5(3):152–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montero-Marin J, Zubiaga F, Cereceda M, Marcelo Marcos Piva D, Trenc P, Garcia-Campayo J. Burnout subtypes and absence of self-compassion in primary healthcare professionals: a cross-sectional study. PLoS One. 2016;11(6):e0157499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. 2015;52(2):649–61. [DOI] [PubMed] [Google Scholar]
- 22.Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach. 2017;39(2):160–3. [DOI] [PubMed] [Google Scholar]
- 23.O’Connor AW, Helfrich CD, Nelson KM, Sears JM. Changes in electronic notification volume and primary care provider burnout. Am J Manag Care. 2023;29(1):57–63. [DOI] [PubMed] [Google Scholar]
- 24.O’Connor K, Neff DM, Pitman S. Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur Psychiatry. 2018;53:74–99. [DOI] [PubMed] [Google Scholar]
- 25.Afonso AM, Cadwell JB, Staffa SJ, Zurakowski D, Vinson AE. Burnout rate and risk factors among anesthesiologists in the United States. Anesthesiology. 2021;134(5):683–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pérez-Fuentes MdC, Molero-Jurado MdM, Gázquez-Linares JJ, Simón-Márquez MdM. Analysis of burnout predictors in nursing: risk and protective psychological factors. Eur J Psychol Appl Legal Context. 2019;11(1):33–40. [Google Scholar]
- 27.Galaiya R, Kinross J, Arulampalam T. Factors associated with burnout syndrome in surgeons: a systematic review. Ann R Coll Surg Engl. 2020;102(6):401–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim MH, Mazenga AC, Yu X, Simon K, Nyasulu P, Kazembe PN, et al. Factors associated with burnout amongst healthcare workers providing HIV care in Malawi. PLoS One. 2019;14(9):e0222638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009;26(12):1118–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deniz ME, Satici SA. The relationships between big five personality traits and subjective vitality. Anales de Psicología/Ann Psychol. 2017;33(2):218–24. [Google Scholar]
- 31.Mirbaha S, Kashani P, Arhami Dolatabadi A, Amini A, Meschi F, Baratloo A. The prevalence of personality disorders in nurses: role of the workplace environment. J Emerg Pract Trauma. 2017;3(2):59–63. [Google Scholar]
- 32.Duan-Porter W, Hatch D, Pendergast JF, Freude G, Rose U, Burr H, et al. 12-month trajectories of depressive symptoms among nurses—Contribution of personality, job characteristics, coping, and burnout. J Affect Disord. 2018;234:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wersebe H, Lieb R, Meyer AH, Hofer P, Gloster AT. The link between stress, well-being, and psychological flexibility during an Acceptance and Commitment Therapy self-help intervention. Int J Clin Health Psychol. 2018;18(1):60–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bakker AB, Van Der Zee KI, Lewig KA, Dollard MF. The relationship between the big five personality factors and burnout: A study among volunteer counselors. J Soc Psychol. 2006;146(1):31–50. [DOI] [PubMed] [Google Scholar]
- 35.Stewart MT, Reed S, Reese J, Galligan MM, Mahan JD. Conceptual models for understanding physician burnout, professional fulfillment, and well-being. Curr Probl Pediatr Adolesc Health Care. 2019;49(11):100658. [DOI] [PubMed] [Google Scholar]
- 36.Karasek RA Jr. Job demands, job decision latitude, and mental strain: Implications for job redesign. Admin Sci Quart. 1979;24:285–308. [Google Scholar]
- 37.Siegrist J. Applying occupational health theories to educational stress and health: Evidence from the effort-reward imbalance model. Educator stress: An occupational health perspective. 2017. p. 223–35.
- 38.Greenberg J. Organizational justice: Yesterday, today, and tomorrow. J Manag. 1990;16(2):399–432. [Google Scholar]
- 39.Ganster DC, Schaubroeck J. Work stress and employee health. J Manag. 1991;17(2):235–71. [Google Scholar]
- 40.Mark GM, Smith AP. Stress models: a review and suggested new direction. sl: In: Houdmont J, Leka S, editors. Occup heal psychol, eur perspect res, vol. 3. Nottingham: Nottingham University Press; 2008.
- 41.Colligan TW, Higgins EM. Workplace stress: Etiology and consequences. J Work Behav Health. 2006;21(2):89–97. [Google Scholar]
- 42.Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512. [PubMed] [Google Scholar]
- 43.Brigham T, Barden C, Dopp AL, Hengerer A, Kaplan J, Malone B, et al. A journey to construct an all-encompassing conceptual model of factors affecting clinician well-being and resilience. NAM perspectives. 2018;8(1):201801b. [Google Scholar]
- 44.Bakker AB, Demerouti E. Towards a model of work engagement. Career Dev Int. 2008;13(3):209–23. [Google Scholar]
- 45.Chang H-T, Chou Y-J, Liou J-W, Tu Y-T. The effects of perfectionism on innovative behavior and job burnout: Team workplace friendship as a moderator. Personality Individ Differ. 2016;96:260–5. [Google Scholar]
- 46.McAdams DP. The person: An introduction to the science of personality psychology. Hoboken, NJ: John Wiley & Sons; 2008.
- 47.Ran L, Chen X, Peng S, Zheng F, Tan X, Duan R. Job burnout and turnover intention among Chinese primary healthcare staff: the mediating effect of satisfaction. BMJ Open. 2020;10(10): e036702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pei P, Lin G, Li G, Zhu Y, Xi X. The association between doctors’ presenteeism and job burnout: a cross-sectional survey study in China. BMC Health Serv Res. 2020;20(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Menon NK, Shanafelt TD, Sinsky CA, Linzer M, Carlasare L, Brady KJ, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA network open. 2020;3(12):e2028780-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Du J, Dong LU, Wang T, Yuan C, Fu R, Zhang L, Bouey J. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;67:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hally SM, Settle M, Nelson BD, Dowling D, Schierholz E, Parker L. Relationship between moral distress and intent to leave a position among neonatal intensive care nurses. Adv Neonatal Care. 2021;21(6):E191–8. [DOI] [PubMed] [Google Scholar]
- 52.Barr P. Moral distress and considering leaving in NICU nurses: direct effects and indirect effects mediated by burnout and the hospital ethical climate. Neonatology. 2021;117(5):646–9. [DOI] [PubMed] [Google Scholar]
- 53.Jameton A. Nursing Practice: The Ethical Issues. Englewood Cliffs, NJ: Prentice-Hall; 1984.
- 54.Donkers MA, Gilissen VJHS, Candel MJJM, van Dijk NM, Kling H, Heijnen-Panis R, et al. Moral distress and ethical climate in intensive care medicine during COVID-19: a nationwide study. BMC Med Ethics. 2021;22(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagle E, Šuriņa S, Griškēviča I. Healthcare workers’ moral distress during the COVID-19 pandemic: a scoping review. Social Sciences. 2023;12(7): 371. [Google Scholar]
- 56.Menon NK, Shanafelt TD, Sinsky CA, Linzer M, Carlasare L, Brady KJS, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA network open. 2020;3(12):e2028780-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Al-Ghunaim TA, Johnson J, Biyani CS, Alshahrani KM, Dunning A, O’Connor DB. Surgeon burnout, impact on patient safety and professionalism: A systematic review and meta-analysis. The American Journal of Surgery. 2022;224(1):228–38. [DOI] [PubMed] [Google Scholar]
- 58.Yung M, Du B, Gruber J, Yazdani A. Developing a Canadian fatigue risk management standard for first responders: defining the scope. Saf Sci. 2021;134:105044.. [Google Scholar]
- 59.West CP, Dyrbye LN, Satele DV, Shanafelt TD. Colleagues Meeting to Promote and Sustain Satisfaction (COMPASS) Groups for Physician Well-Being: A Randomized Clinical Trial. Mayo Clin Proc. 2021;96(10):2606–14. [DOI] [PubMed]
- 60.Nguyen J, Liu A, McKenney M, Liu H, Ang D, Elkbuli A. Impacts and challenges of the COVID-19 pandemic on emergency medicine physicians in the United States. Am J Emerg Med. 2021;48:38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lazarides AL, Belay ES, Anastasio AT, Cook CE, Anakwenze OA. Physician burnout and professional satisfaction in orthopedic surgeons during the COVID-19 Pandemic. Work. 2021;69(1):15–22. [DOI] [PubMed] [Google Scholar]
- 62.Rath KS, Huffman LB, Phillips GS, Carpenter KM, Fowler JM. Burnout and associated factors among members of the Society of Gynecologic Oncology. Am J Obstet Gynecol. 2015;213(6):824-e821. [DOI] [PubMed] [Google Scholar]
- 63.Oreskovich MR, Shanafelt T, Dyrbye LN, Tan L, Sotile W, Satele D, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24(1):30–8. [DOI] [PubMed] [Google Scholar]
- 64.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 65.Levac D, Colquhoun H, O’Brien K. Scoping studies: Advancing the methodology. Implemention Science. 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tricco AC, Lillie E, Zarin W, O’brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O’Dea RE, Lagisz M, Jennions MD, Koricheva J, Noble DWA, Parker TH, et al. Preferred reporting items for systematic reviews and meta-analyses in ecology and evolutionary biology: a PRISMA extension. Biol Rev. 2021;96(5):1695–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fenwick J, Lubomski A, Creedy DK, Sidebotham M. Personal, professional and workplace factors that contribute to burnout in Australian midwives. J Adv Nurs. 2018;74(4):852–63. [DOI] [PubMed] [Google Scholar]
- 69.Lwiza AF, Lugazia ER. Burnout and associated factors among healthcare workers in acute care settings at a tertiary teaching hospital in Tanzania: an analytical cross-sectional study. Health Sci Rep. 2023;6(5):e1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Amiri M, Khosravi A, Eghtesadi AR, Sadeghi Z, Abedi G, Ranjbar M, et al. Burnout and its influencing factors among primary health care providers in the North East of Iran. PLoS One. 2016;11(12):e0167648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abaoğlu H, Demirok T, Kayıhan H. Burnout and its relationship with work-related factors among occupational therapists working in public sector in Turkey. Scand J Occup Ther. 2021;28(4):294–303. [DOI] [PubMed] [Google Scholar]
- 72.Abusanad A, Bensalem A, Shash E, Mula-Hussain L, Benbrahim Z, Khatib S, et al. Burnout in oncology: magnitude, risk factors and screening among professionals from Middle East and North Africa (BOMENA study). Psychooncology. 2021;30(5):736–46. [DOI] [PubMed] [Google Scholar]
- 73.Ahmed F, Hawulte B, Yuya M, Birhanu S, Oljira L. Prevalence of burnout and associated factors among health professionals working in public health facilities of Dire Dawa city administration, Eastern Ethiopia. Front Public Health. 2022;10:836654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alakhras M, Al-Mousa DS, Lewis S. Assessment and correlation between job satisfaction and burnout among radiographers. Radiography. 2022;28(2):283–7. [DOI] [PubMed] [Google Scholar]
- 75.Ang SY, Dhaliwal SS, Ayre TC, Uthaman T, Fong KY, Tien CE, et al. Demographics and personality factors associated with burnout among nurses in a Singapore tertiary hospital. BioMed Res Int. 2016;2016:6960184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Asante JO, Li MJ, Liao J, Huang YX, Hao YT. The relationship between psychosocial risk factors, burnout and quality of life among primary healthcare workers in rural Guangdong province: a cross-sectional study. BMC Health Serv Res. 2019;19(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ashraf F, Ahmad H, Aftab S. Interactive role of personal and work related factors in psychological burnout: a study of Pakistani doctors. JPMA J Pak Med Assoc. 2020;70(8):1413–7. [PubMed] [Google Scholar]
- 78.Amede AF, Bilchut AH, Teferi BB. Prevalence and associated factors of burnout among midwives in governmental hospitals, Eastern Amhara, Ethiopia, 2022. Health. 2023;8(3):40. [Google Scholar]
- 79.Barello S, Caruso R, Palamenghi L, Nania T, Dellafiore F, Bonetti L, et al. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: an application of the job demands-resources model. Int Arch Occup Environ Health. 2021;94(8):1751–61. [DOI] [PMC free article] [PubMed]
- 80.Tang L, Pang Y, He Y, Chen Z, Leng J. Burnout among early-career oncology professionals and the risk factors. Psychooncology. 2018;27(10):2436–41. [DOI] [PubMed] [Google Scholar]
- 81.Baumgarten C, Michinov E, Rouxel G, Bonneterre V, Gay E, Roche P-H. Personal and psychosocial factors of burnout: a survey within the French neurosurgical community. PLoS ONE. 2020;15(5):e0233137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.van der Wal RAB, Bucx MJL, Hendriks JCM, Scheffer G-J, Prins JB. Psychological distress, burnout and personality traits in Dutch anaesthesiologists: a survey. Eur J Anaesthesiol | EJA. 2016;33(3):179–86. [DOI] [PubMed] [Google Scholar]
- 83.Ntantana A, Matamis D, Savvidou S, Giannakou M, Gouva M, Nakos G, et al. Burnout and job satisfaction of intensive care personnel and the relationship with personality and religious traits: An observational, multicenter, cross-sectional study. Intensive Crit Care Nurs. 2017;41:11–7. [DOI] [PubMed] [Google Scholar]
- 84.Benhamza S, Khalayla M, Lahlou L, Amine Z, Lazraq M, Youssef M, et al. The Prevalence and Contributing Factors of Burnout Among Anesthesiologists and Intensive Care Unit Staff in Morocco: A Cross-Sectional Analysis. Cureus. 2023;15(9). [DOI] [PMC free article] [PubMed]
- 85.Bercasio LV, Rowe DJ, Yansane A-I. Factors associated with burnout among dental hygienists in California. Am Dent Hygienists’ Assoc. 2020;94(6):40–8. [PubMed] [Google Scholar]
- 86.Bijari B, Abassi A. Prevalence of burnout syndrome and associated factors among rural healthworkers (Behvarzes) in South Khorasan. Iran Red Crescent Med J. 2016;18(10):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Carletto S, Ariotti MC, Garelli G, Di Noto L, Berchialla P, Malandrone F, et al. Moral distress and burnout in neonatal intensive care unit healthcare providers: a cross-sectional study in Italy. Int J Environ Res Public Health. 2022;19(14):8526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fumis RRL, Junqueira Amarante GA, de Fátima NA, Vieira Junior JM. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann Intensive Care. 2017;7(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen J, Liu X, Wang D, Jin Y, He M, Ma Y, et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc Psychiatry Psychiatr Epidemiol. 2021;56(1):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Henriksen L, Lukasse M. Burnout among Norwegian midwives and the contribution of personal and work-related factors: a cross-sectional study. Sex Reprod Healthc. 2016;9:42–7. [DOI] [PubMed] [Google Scholar]
- 91.Taranu SM, Ilie AC, Turcu A-M, Stefaniu R, Sandu IA, Pislaru AI, et al. Factors associated with burnout in healthcare professionals. Int J Environ Res Public Health. 2022;19(22):14701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Agarwal SD, Pabo E, Rozenblum R, Sherritt KM. Professional dissonance and burnout in primary care: a qualitative study. JAMA Intern Med. 2020;180(3):395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ashipala DO, Nghole TM. Factors contributing to burnout among nurses at a district hospital in Namibia: A qualitative perspective of nurses. J Nurs Manag. 2022;30(7):2982–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Baillat L, Vayre E, Préau M, Guérin C. Burnout and brownout in intensive care physicians in the era of COVID-19: a qualitative study. Int J Environ Res Public Health. 2023;20(11):6029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Barreto T, Eden A, Brock A. The impact of practicing obstetrics on burnout among early-career family physicians. Fam Med. 2020;52(6):408–13. [DOI] [PubMed] [Google Scholar]
- 96.Bredenberg E, Tietbohl C, Dafoe A, Thurman L, Calcaterra S. Identifying factors that contribute to burnout and resilience among hospital-based addiction medicine providers: a qualitative study. J Subst Abuse Treat. 2023;144:108924. [DOI] [PubMed] [Google Scholar]
- 97.Eder LL, Meyer B. Self-endangering: a qualitative study on psychological mechanisms underlying nurses’ burnout in long-term care. Int J Nurs Sci. 2022;9(1):36–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Geuens N, Franck E, Verheyen H, De Schepper S, Roes L, Vandevijvere H, et al. Vulnerability and stressors for burnout within a population of hospital nurses: a qualitative descriptive study. Can J Nurs Res. 2021;53(1):16–26. [DOI] [PubMed] [Google Scholar]
- 99.Hoffman R, Bonney A. Junior doctors, burnout and wellbeing: understanding the experience of burnout in general practice registrars and hospital equivalents. Aus J Gen Pract. 2018;47(8):571–5. [DOI] [PubMed] [Google Scholar]
- 100.Algunmeeyn A, El-Dahiyat F, Altakhineh MM, Azab M, Babar Z-U-D. Understanding the factors influencing healthcare providers’ burnout during the outbreak of COVID-19 in Jordanian hospitals. J Pharmaceut Policy Pract. 2020;13:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dominic C, Gopal DP, Sidhu A. ‘It’s like juggling fire daily’: Well-being, workload and burnout in the British NHS-A survey of 721 physicians. Work. 2021;70(2):395–403. [DOI] [PubMed] [Google Scholar]
- 102.Alrawashdeh HM, AaB Al-Tammemi, Alzawahreh MK, Al-Tamimi A, Elkholy M, Al Sarireh F, et al. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: a convergent parallel mixed-method study. BMC Public Health. 2021;21:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Divinakumar KJ, Bhat PS, Prakash J, Srivastava K. Personality traits and its correlation to burnout in female nurses. Ind Psychiatry J. 2019;28(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Carletto S, Ariotti MC, Garelli G, Di Ludovica N, Berchialla P, Malandrone F, et al. Moral distress and burnout in neonatal intensive care unit healthcare providers: a cross-sectional study in Italy. Int J Environ Res Public Health. 2022;19(14):8526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schaufeli WB, Maassen GH, Bakker AB, Sixma HJ. Stability and change in burnout: A 10-year follow-up study among primary care physicians. J Occup Organ Psychol. 2011;84(2):248–67. [Google Scholar]
- 106.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826–32. [DOI] [PubMed] [Google Scholar]
- 107.Pérez-Fuentes MdC, Molero Jurado MdM, Martos Martínez Á, Gázquez Linares JJ. Burnout and engagement: personality profiles in nursing professionals. J Clin Med. 2019;8(3):286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Eysenck HJ. Personality and extra-sensory perception. J Soc Psych Res. 1967;44(729):55–71.
- 109.Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol. 1989;44(3):513. [DOI] [PubMed] [Google Scholar]
- 110.Che XX, Zhou ZE, Kessler SR, Spector PE. Stressors beget stressors: The effect of passive leadership on employee health through workload and work–family conflict. Work Stress. 2017;31(4):338–54. [Google Scholar]
- 111.Stamm B. The Concise Manual for the Professional Quality of Life Scale. 2nd ed. Pocatello, ID: ProQOL.org; 2010.
- 112.Zubin J, Spring B. Vulnerability: a new view of schizophrenia. J Abnorm Psychol. 1977;86(2):103. [DOI] [PubMed] [Google Scholar]
- 113.Farber BA. Subtypes of burnout: theory, research and practice. In: Annual Conference, American Psychological Association. San Francisco. 2001.
- 114.Montero-Marin J, Tops M, Manzanera R, Piva Demarzo MM, Alvarez de Mon M, García-Campayo J. Mindfulness, resilience, and burnout subtypes in primary care physicians: The possible mediating role of positive and negative affect. Front Psychol. 2015;6:148357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. Lanham, MD: Scarecrow Education; 1997.
- 116.McCrae RR, Costa PT Jr. The NEO Personality Inventory: Using the five-factor modeI in counseling. J Couns Dev. 1991;69(4):367–72. [Google Scholar]
- 117.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(3):192–207. [Google Scholar]
- 118.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & stress. 2005 Jul 1;19(3):192-207.
- 119.Epstein EG, Whitehead PB, Prompahakul C, Thacker LR, Hamric AB. Enhancing understanding of moral distress: the measure of moral distress for health care professionals. AJOB Empirical Bioethics. 2019;10(2):113–24. [DOI] [PubMed] [Google Scholar]
- 120.Spector PE. Measurement of human service staff satisfaction: development of the job satisfaction survey. Am J Community Psychol. 1985;13(6):693. [DOI] [PubMed] [Google Scholar]
- 121.Eysenck HJ, Eysenck SBG. Eysenck Personality Questionnaire (Junior & Adult). San Diego, CA: EdITS/Educational and Industrial Testing Service; 1975.
- 122.Montero-Marín J, García-Campayo J. A newer and broader definition of burnout: Validation of the" Burnout Clinical Subtype Questionnaire (BCSQ-36)". BMC Public Health. 2010;10:1–9. [DOI] [PMC free article] [PubMed]
- 123.Schaufeli WB, Desart S, De Witte H. Burnout Assessment Tool (BAT)—development, validity, and reliability. Int J Environ Res Public Health. 2020;17(24):9495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Schaufeli WB, Taris TW. The conceptualization and measurement of burnout: common ground and worlds apart. Work Stress. 2005;19(3):256–62. [Google Scholar]
- 125.Deligkaris P, Panagopoulou E, Montgomery AJ, Masoura E. Job burnout and cognitive functioning: a systematic review. Work Stress. 2014;28(2):107–23. [Google Scholar]
- 126.Dryden-Palmer K, Moore G, McNeil C, Larson CP, Tomlinson G, Roumeliotis N, et al. Moral distress of clinicians in Canadian pediatric and neonatal ICUs. Pediatr Crit Care Med. 2020;21(4):314–23. [DOI] [PubMed] [Google Scholar]
- 127.Larson CP, Dryden-Palmer KD, Gibbons C, Parshuram CS. Moral distress in PICU and neonatal ICU practitioners: a cross-sectional evaluation. Pediatr Crit Care Med. 2017;18(8):e318–26. [DOI] [PubMed] [Google Scholar]
- 128.Prentice TM, Gillam L, Davis PG, Janvier A. Always a burden? Healthcare providers’ perspectives on moral distress. Arch Dis Child Fetal Neonatal Ed. 2018;103(5)–F445. [DOI] [PubMed]
- 129.Johnson-Coyle L, Opgenorth D, Bellows M, Dhaliwal J, Richardson-Carr S, Bagshaw SM. Moral distress and burnout among cardiovascular surgery intensive care unit healthcare professionals: a prospective cross-sectional survey. Can J Crit Care Nurs. 2016;27(4):27. [PubMed] [Google Scholar]
- 130.Shoorideh FA, Ashktorab T, Yaghmaei F, Alavi MH. Relationship between ICU nurses’ moral distress with burnout and anticipated turnover. Nurs Ethics. 2015;22(1):64–76. [DOI] [PubMed] [Google Scholar]
- 131.Martins Pereira S, Teixeira CM, Carvalho AS, Hernández-Marrero P, InPalIn. Compared to palliative care, working in intensive care more than doubles the chances of burnout: results from a nationwide comparative study. PloS one. 2016;11(9):e0162340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4. [DOI] [PubMed] [Google Scholar]
- 133.Daudt HM, Van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Evanoff BA, Strickland JR, Dale AM, Hayibor L, Page E, Duncan JG, et al. Work-related and personal factors associated with mental well-being during the COVID-19 response: survey of health care and other workers. J Med Internet Res. 2020;22(8):e21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tiete J, Guatteri M, Lachaux A, Matossian A, Hougardy J-M, Loas G, et al. Mental health outcomes in healthcare workers in COVID-19 and non-COVID-19 care units: a cross-sectional survey in Belgium. Front Psychol. 2021;11:612241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Selamu M, Hanlon C, Medhin G, Thornicroft G, Fekadu A. Burnout among primary healthcare workers during implementation of integrated mental healthcare in rural Ethiopia: a cohort study. Hum Resour Health. 2019;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kupcewicz E, Jóźwik M. Association of burnout syndrome and global self-esteem among Polish nurses. Arch Med Sci. 2020;16(1):135–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zewdu T, Abera H, Abebe N, Mulugeta H, Dessie G. Level of burnout and associated factors among nurses working in public health institutions north shoa zone, Amhara. Ethiopia Int J Soc Relev Concern. 2017;5(8):17–26. [Google Scholar]
- 139.Pustulka-Piwnik U, Ryn ZJ, Krzywoszanski L, Stozek J. Burnout syndrome in physical therapists - demographic and organizational factors/zespól wypalenia zawodowego u fizjoterapeutów a zmienne demograficzne i organizacyjne. Med Pr. 2014;65(4):453–62. [DOI] [PubMed] [Google Scholar]
- 140.Alkassabi OY, Al-Sobayel H, Al-Eisa ES, Buragadda S, Alghadir AH, Iqbal A. Job satisfaction among physiotherapists in Saudi Arabia: does the leadership style matter? BMC Health Serv Res. 2018;18:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Bae Y-H, Min KS. Associations between work-related musculoskeletal disorders, quality of life, and workplace stress in physical therapists. Ind Health. 2016;54(4):347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Starr JA, Holmes MB, Riley E, McDonnell B, Driscoll L, Camarinos J, et al. A quantitative measurement of physical therapists’ empathy and exploration of the relationship with practice setting and work engagement. Eval Health Prof. 2020;43(4):255–63. [DOI] [PubMed] [Google Scholar]
- 143.Bejer A, Domka-Jopek E, Probachta M, Lenart-Domka E, Wojnar J. Burnout syndrome in physiotherapists working in the Podkarpackie province in Poland. Work. 2019;64(4):809–15. [DOI] [PubMed] [Google Scholar]
- 144.Oe M, Ishida T, Favrod C, Martin-Soelch C, Horsch A. Burnout, psychological symptoms, and secondary traumatic stress among midwives working on perinatal wards: a cross-cultural study between Japan and Switzerland. Front Psych. 2018;9:387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Muliira RS, Ssendikadiwa VB. Professional quality of life and associated factors among Ugandan midwives working in Mubende and Mityana rural districts. Matern Child Health J. 2016;20:567–76. [DOI] [PubMed] [Google Scholar]
- 146.Simons BS, Foltz PA, Chalupa RL, Hylden CM, Dowd TC, Johnson AE. Burnout in US military orthopaedic residents and staff physicians. Mil Med. 2016;181(8):835–9. [DOI] [PubMed] [Google Scholar]
- 147.Zhang LM, Cheung EO, Eng JS, Ma M, Etkin CD, Agarwal G, et al. Development of a conceptual model for understanding the learning environment and surgical resident well-being. Am J Surg. 2021;221(2):323–30. [DOI] [PubMed] [Google Scholar]
- 148.Barr P. Burnout in neonatal intensive care unit nurses: relationships with moral distress, adult attachment insecurities, and proneness to guilt and shame. J Perinat Med. 2020;48(4):416–22. [DOI] [PubMed] [Google Scholar]
- 149.Badolamenti S, Fida R, Biagioli V, Caruso R, Zaghini F, Sili A. Modified Moral Distress Scale (MDS-11): Validation Study Among Italian Nurses. Professioni Infermieristiche. 2017;70(4):238–48. [DOI] [PubMed]
- 150.Śliwiński Z, Starczyńska M, Kotela I, Kowalski T, Kryś-Noszczyk K, Lietz-Kijak D, et al. Burnout among physiotherapists and length of service. Int J Occup Med Environ Health. 2014;27:224–35. [DOI] [PubMed] [Google Scholar]
- 151.Silva SCPS, Nunes MAP, Santana VR, Reis FP, Machado Neto J, Lima SO. Burnout syndrome in professionals of the primary healthcare network in Aracaju, Brazil. Cien Saude Colet. 2015;20:3011–20. [DOI] [PubMed] [Google Scholar]
- 152.Hu H-X, Liu L-T, Zhao F-J, Yao Y-Y, Gao Y-X, Wang G-R. Factors related to job burnout among community nurses in Changchun. Chin J Nurs Res. 2015;23(3):172–80. [DOI] [PubMed] [Google Scholar]
- 153.Pandey J, Singh M. Donning the mask: effects of emotional labour strategies on burnout and job satisfaction in community healthcare. Health Policy Plan. 2016;31(5):551–62. [DOI] [PubMed] [Google Scholar]
- 154.Adbaru D, Assen Z, Demelew T, Teshome GS. Magnitude of burnout and its associated factors among nurses working in public hospitals of Amhara regional state. Ethiop MOJ Womens Health. 2019;8(2):133–41. [Google Scholar]
- 155.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–29. [DOI] [PubMed] [Google Scholar]
- 156.Akyurt N. Job satisfaction and perceived stress among radiology technicians: a questionnaire survey in relation to sociodemographic and occupational risk factors. Int Arch Occup Environ Health. 2021;94:1617–26. [DOI] [PubMed] [Google Scholar]
- 157.Charles MA. Motivation Strategies Healthcare Leaders Use With High Performing Employees. Northcentral University; 2021.
- 158.Bakker AB, Costa PL. Chronic job burnout and daily functioning: a theoretical analysis. Burn Res. 2014;1(3):112–9. [Google Scholar]
- 159.De Beer LT, Schaufeli WB, De Witte H, Hakanen JJ, Shimazu A, Glaser J, et al. Measurement invariance of the Burnout Assessment Tool (BAT) across seven cross-national representative samples. Int J Environ Res Public Health. 2020;17(15):5604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sakakibara K, Shimazu A, Toyama H, Schaufeli WB. Validation of the Japanese version of the burnout assessment tool. Front Psychol. 2020;11:1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ramaci T, Barattucci M, Vella F, Senia P, Cannizzaro E, Scorciapino A, et al. Straining at work and its relationship with personality profiles and individual consequences in healthcare workers (HCWs). Int J Environ Res Public Health. 2020;17(2):610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Finlayson F, Dobson H, Digby R, Bucknall T, Malpas C, Winton-Brown T. P396 Moral distress and burnout in healthcare workers during the COVID-19 pandemic: quantitative results from a large Australian public hospital survey. J Cyst Fibros. 2023;22:S185. [Google Scholar]
- 163.Güler Y, Şengül S, Çaliş H, Karabulut Z. Burnout syndrome should not be underestimated. Rev Assoc Med Bras. 2019;65:1356–60. [DOI] [PubMed] [Google Scholar]
- 164.Soares JP, Lopes RH, de Souza Mendonça PB, Silva CRDV, Rodrigues CCFM, de Castro JL. Use of the Maslach Burnout inventory among public health care professionals: scoping review. JMIR Mental Health. 2023;10(1):e44195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Van Dam A. A clinical perspective on burnout: diagnosis, classification, and treatment of clinical burnout. Eur J Work Organ Psy. 2021;30(5):732–41. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data obtained or analyzed during this study are included in the Supplementary [S1, S2, S3].