Abstract
This review explores the multifaceted exposures in the workplace that contribute to cardiovascular diseases (CVD), including physical, ergonomics, chemical, biological, psychosocial, and emerging occupational hazards. These well-documented occupational hazards have long been linked to heart disease. Exposures arising from these hazards present significant concerns for worker health and safety. Moreover, heat stress is an emerging and increasingly pervasive threat, exacerbated by climate change, particularly in outdoor, high-exposure industries like agriculture and construction. While the epidemiological links between heat and CVD are well established, there is a critical gap in research on the physiological impacts of heat on workers’ cardiovascular health. In particular, migrant workers are especially vulnerable to these occupational hazards, particularly in the absence of targeted, equitable interventions. As global temperatures rise, addressing these occupational exposures is important for protecting the cardiovascular health of the workforce and the expanding field of occupational cardiology.
Keywords: occupational cardiology, heat workers, climate change, occupational health and safety, migrant workers
Background
Cardiovascular disease (CVD) remains the leading cause of death globally, responsible for 1 in every 3 deaths.1 In 2022, approximately 1 in 5 deaths from CVD occurred in adults under the age of 65.2 CVD is the leading cause of death and permanent disability among workers.3 Heart disease is also responsible for the most costs in the healthcare system than any other disease or injury.4 While well-known risk factors such as preexisting health conditions, tobacco use, diet, and exercise are significant determinants of heart disease, work-related factors often play a predominant yet overlooked role in the development of heart disease.
Exposure to substandard social, organizational, and environmental conditions can all lead to heart disease.5 Certain occupations are classified as higher risk or “high hazard” due to the potential dangers associated with cardiovascular emergencies that workers might face.6 Findings suggest that in the United States, 5% to 8% of healthcare costs and 120,000 deaths are directly linked to 10 work-related factors. For the working-age population, this number is even higher, with 10% to 20% of all CVD deaths caused by working conditions.7 It has been well established in the medical literature that certain occupational exposures worsen or even cause CVD. While some of these instances of risk are still commonplace within many industries, some have been regulated out and are now quite rare while others are emerging in the 21st century. This review summarizes these work-related challenges to heart disease from a contemporary perspective, highlighting the ongoing and emerging occupational risk factors that contribute to the global burden of CVD in today’s workforce.
Common Workplace Exposures
1. Physical Hazards
Physical hazards include exposure to burns, noise and vibration, illumination, radiation, and heat. Burns can occur from contact with hot surfaces and flames such as furnaces and kitchens. While skin burns do not have a direct link to heart disease, severe burns can trigger systemic responses such as inflammation, fluid imbalance, increased metabolic demand, and risk of infection, all of which may strain the cardiovascular system. Prolonged exposure to noise pollution exceeding 80 decibels in the workplace can cause a vascular dysfunction (endothelial dysfunction) and an elevation in blood pressure that increases the relative risk for cardiovascular disease.8 A recent meta-analysis commissioned by the World Health Organization found that road traffic noise increases the incidence of coronary heart disease by 8% for every 10-decibel rise in noise levels.9 Evidence suggests that workers who are frequently exposed to traffic noise or employed near major roads or highways are at higher risk of stroke and increased mortality in individuals with coronary artery disease.10 Vibration, which may affect the entire body or specific parts (hand-arm vibration vs whole-body vibration) depending on the equipment used, has strong evidence linking it to cardiovascular system impacts, particularly by affecting the arterial intima and heart-rate variability.11 Exposure to different colors of fluorescent light is associated with heart rate variability and autonomic regulation.12 One study shows that for the elderly in Hong Kong, those who were exposed to outdoor light at night were more likely to be associated with a higher risk of coronary heart disease (CHD) and CHD-related mortality. Conducted over an 11-year observation period, the study shows that higher nighttime light levels were linked to a greater likelihood of CHD hospitalizations and deaths and were significantly worse among patients exposed to higher levels of PM2.5 and road traffic noise pollution.13 Long-term shift work and circadian disruption that come with irregular shift work can negatively impact cardiovascular health by altering short-term heart rate and blood pressure oscillations.14 Light regulates the body’s circadian rhythm, which affects numerous physiological processes, including cardiovascular function. Disruptions to the circadian rhythm, such as those caused by irregular light exposure (eg, working an overnight shift), can lead to misalignment between the body’s internal clock and the external environment. This has been linked to increased cardiovascular risks such as increased blood pressure and heart rate.15
2. Ergonomics Hazards
Ergonomic hazards include lack of physical activity associated with sedentary positions or irregular heavy physical excretion. Lack of physical activity within a sedentary position contributes to an inactive lifestyle, which is closely linked to the cardiovascular system, thus increasing the risk of heart disease.16 Irregular physical activity and heavy physical exertion characterized by 6 metabolic equivalents (METS) or more have been associated with an increased risk of acute myocardial infarction for the first hour after exertion.17 One study with 13,960 participants shows that replacing 30 minutes of sedentary time per day with light-intensity physical activity is associated with a 16% lower risk of cardiovascular mortality.18
3. Chemical Hazards
Multiple chemical hazards are found in different occupations that are linked with specific cardiovascular conditions. These chemical hazards include lead, arsenic, carbon monoxide, carbon disulfide, nitrate esters, cobalt, and solvents such as bromofluorocarbons, methyl chloroform, methylene chloride, and trichloroethylene.19
Lead exposure is one of the most well-documented occupational hazards linked to CVD.20 Chronic lead exposure has been associated with increased blood pressure, hypertension, and an elevated risk of coronary heart disease. Lead interferes with the body’s ability to regulate blood pressure by impairing renal function, promoting oxidative stress, and disturbing calcium signaling in vascular smooth muscle cells, which can lead to arterial stiffness and hypertension.21 The recognition of these risks has led to significant regulatory efforts. The Occupational Safety and Health Administration (OSHA) and the Environmental Protection Agency (EPA) have implemented stringent regulations to limit occupational exposure to lead. These measures have resulted in a significant reduction in blood lead levels among workers and the general public.
Arsenic exposure, particularly in industries such as mining, smelting, and pesticide manufacturing, is another serious concern. Chronic exposure to inorganic arsenic has been linked to an increased risk of CVD, including ischemic heart disease, hypertension, and peripheral arterial disease. Arsenic induces oxidative stress, inflammation, and endothelial dysfunction, all of which contribute to cardiovascular pathology.22 Regulatory efforts to reduce arsenic exposure, such as the EPA’s reduction of the maximum contaminant level for arsenic in drinking water from 50 parts per billion (ppb) to 10 ppb, have been effective in lowering the incidence of arsenic-related cardiovascular conditions. However, occupational exposure to arsenic fumes remains a significant risk in certain industries.23
Carbon monoxide (CO) is a ubiquitous chemical asphyxiant gas in many occupations, especially in industries where combustion processes are common, such as manufacturing, mining, and firefighting.24 CO binds with hemoglobin with an affinity of 200 times that of oxygen to form carboxyhemoglobin, which reduces the oxygen-carrying capacity of blood, leading to tissue hypoxia. CO is one of the leading causes of death by poisoning worldwide and is associated with approximately 4.6 deaths per million individuals.25 Chronic exposure to low levels of CO has been linked to an increased risk of CVD, particularly among workers with preexisting cardiovascular conditions. CO exposure can exacerbate angina, increase the risk of arrhythmias, and lead to long-term damage to the heart muscle.26 Despite regulatory measures to limit CO exposure, such as OSHA’s permissible exposure limit of 50 parts per million over an 8-hour workday, CO remains a significant health threat in many occupational settings.
4. Biological Hazards
Many occupations continue to face biological hazards, including exposure to animals, humans, or their byproducts, particularly in industries such as food and agriculture. Workers with preexisting cardiovascular disease are at greater risk from the infective agents present within these biological hazards, as the combination of infectious stressors and preexisting conditions can exacerbate cardiovascular outcomes. Bacteria play a significant role in multiple cardiovascular diseases. Infections can lead to or exacerbate conditions such as infective endocarditis, myocarditis, and pericarditis.27 Infectious myocarditis is typically a result of an acute viral infection, leading to inflammation of the heart muscle.28 If left untreated, myocarditis brought on by viral or bacterial infection can progress to dilated cardiomyopathy, a condition where the heart becomes enlarged and weakened, leading to long-term impairment of heart function and reduced lifespan.29 COVID-19 brought on by the SARS-CoV-2 virus can cause a range of cardiovascular complications, including myocarditis, acute coronary syndrome, heart failure, and arrhythmias. These complicated outcomes can occur directly because of viral effects or inflammatory responses and secondary effects from the illness.19
5. Psychosocial Hazards
Psychosocial hazards are common in the workplace and result from exposure to occupational stress and strain.30 As early as 1977, there was evidence indicating that coronary heart disease patients experienced significantly higher levels of occupational stress compared with healthy controls.31 Recent studies indicate that bullying, effort-reward balance, and job insecurity in the workplace are all associated with heart disease.30 The literature suggests that such job stressors are correlated with ambulatory systolic blood pressure. The rise in blood pressure has been shown to extend past the work environment and into off-hours time.32 Lowering the level of exposure to job strain that these workers experience has been shown to reduce the likelihood of morbidity. Common exposures associated with occupational stress include working long hours, highly demanding occupations, irregular working shifts, and financial pressures that constrain workers and limit them from attaining the health care they need.33
Shift work is linked with weight gain and changes within the body composition, causing workers to deposit more adipose tissue when compared with non-shift workers. Shift work is one of the most common psychosocial work environment risk factors for cardiovascular disease and is linked via three pathways.34 The nature of shift work can lead to the mismatch of circadian rhythms, social disruption, and behavioral changes. Certain shift hours cause workers to have irregular eating habits and are linked with higher cholesterol values, increased intake of calories at night, and mismatched circadian rhythms. The time commitments that shift work demands impact the availability of social support the workers can access, which is a risk factor in heart disease. Shift work has also been shown to lead to behavioral changes—such as higher smoking rates, altering eating habits by missing meals, or choosing to snack more—that increase the rate of cardiovascular disease. Both acute-psychological and chronic stress lead to the long-term development of coronary heart disease and have been linked with transient myocardial ischemia, increased risk of recurrent CHD events, and increased mortality rates.35 Research shows that repeated exposure to heat-stress-inducing environments is directly correlated with increased concentrations of the stress hormone cortisol.36 Elevated levels of cortisol are associated with hypertension, a significant predictor of heart disease.
An Emerging Exposure: Heat in the Workplace
A Warming World
The rise in global surface temperature has risen dramatically since the preindustrial era between the years 1850 and 1900. The 10 warmest years on historical record occurred in the past decade between 2014 and 2023, with 2023 being the warmest year on record since the global temperatures began in 1850. The average temperature in 2023 was 1.18°C above the 20th-century average and 1.35°C above the preindustrial average. Since 1850, the global surface temperature has risen by 0.06°C each decade. Since 1982, the rate of temperature increase has more than tripled, reaching 0.20°C per decade.37 Although the change in rate of increase in global temperature is significant in itself, it does not tell the whole story. The global average considers all regions of the world in both the southern and northern hemispheres. Some areas are much colder, while others are extremely hot. While the trend in global temperatures cannot specify which regions are most impacted, the Earth’s energy budget is certainly shifting, with more sunlight being retained than radiated into space as heat. The impact of rising global temperatures is evident in the effect it has had over recent monthly records.37
Occupational Heat
The number of workers impacted by excessive heat is alarming, and occupational safety and health protections have struggled to keep pace. According to an International Labor Organization report in 2024, at least 2.41 billion workers (representing 71% of the global workforce) are exposed to excessive heat, leading to 22.85 million injuries and 18,970 deaths each year.38 Acute and chronic exposure to heat in working environments has been linked to acute kidney injury and chronic kidney disease.39 Around the globe, 26.2 million individuals are living with chronic kidney disease caused by heat stress at work. These cases make up about 3% of all chronic kidney disease cases, with the proportion varying from 3.34% in Africa to 1.8% in the Americas. However, despite the pervasiveness of heat in the workplace, little is known about the effects of heat on worker’s cardiovascular health.
As temperatures continue to rise each year, the risk of heat stress and cardiovascular disease among exposed workers increases. The impact of workplace heat stress extends beyond individual health, affecting both the well-being of workers and the operations of businesses (Figure 1). Health issues resulting from heat stress not only diminish the quality of life for workers but also contribute to loss in productivity.40 For employers, the consequences are profound, including higher turnover rates in specialized roles, reduced work quality, and the potential burden of medical costs, all of which underscore the growing concern about heat in the workplace.
Figure 1.
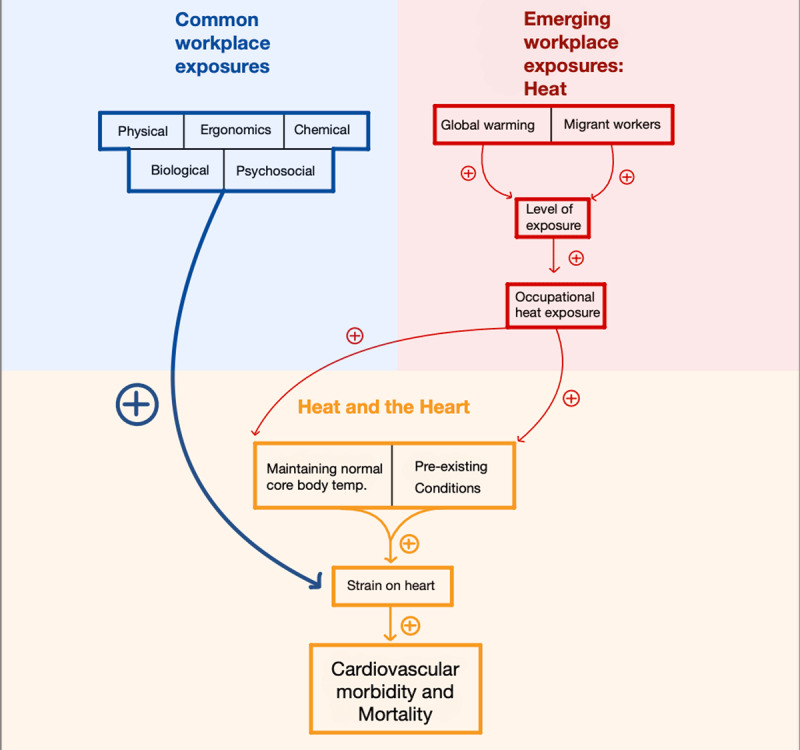
The connection between common workplace exposures and emerging occupational heat exposure. Heat stress, particularly in workers with preexisting conditions, leads to cardiovascular strain and increases the risk of cardiovascular morbidity and mortality, particularly under extreme heat conditions.
Epidemiology of Heat and CVD
Population health studies show that high and low ambient temperatures are linked to higher rates of mortality and morbidity from CVD.41 A meta-analysis revealed that the risk of cardiovascular mortality rises with each 1°C increase in heat exposure.42 Another meta-analysis found a 15% increase in CVD mortality during heatwaves.43 A more recent meta-analysis from 2022 showed that heatwaves elevated the risk of CVD-related mortality by 11.7%, with an even greater risk for the elderly (aged over 65).44 Additionally, a recent global study spanning 27 countries estimated that, for every 1,000 cardiovascular deaths, two excess deaths were attributed to extreme heat.45 This negative impact is exacerbated in regions that experience higher temperatures.
Heat and the Heart
For body function to be normal, one must maintain a core body temperature of 37.0°C (98.6°F). Anything above 38.0°C (100.4°F) impairs both physical and cognitive function, and anything above 40.6°C (105.0°F) can lead to organ damage and loss of consciousness, and the rate of death increases dramatically. Humans compensate for extreme temperatures through four different methods: conduction, convection, radiation, and evaporative cooling through sweat. As the ambient air temperatures rise above internal core body temperature, the body relies more heavily on evaporative cooling through sweat. Working conditions that force workers to be in inadequate conditions for cooling, such as high humidity conditions and spaces confined from air movement, cause evaporative cooling from sweat to be less effective, thus requiring more energy from the body and putting more strain on our internal organs. The cardiovascular system holds a crucial role in thermoregulation and the body’s response to heat stress.46 In heat stress and strain conditions, the heart has to compensate by doing extra work to maintain the body’s core temperature at normal levels.
The individual health status of a person is a contributing factor in how their body and cardiovascular system reacts under conditions of heat stress.47 Patients with preexisting conditions such as diabetes and CVD are more prone to heat-related illness.48 The increased strain that patients with CVD experience under conditions of heat stress leads to decreased cardiovascular function and a decreased capacity to properly thermoregulate and, as a result, increases the risk of illnesses related to heat stress.47 A clinical example of the link between preexisting health conditions and heat-related illness are patients diagnosed with hypertension. Hypertension affects the peripheral blood to the skin, which impairs the body’s ability to dissipate heat and puts more strain on the heart.49 The hypertensive medications and beta blockers that patients take may also reduce thermoregulatory functions through mechanisms such as reduced peripheral blood flow to the skin.50
Studies show that a large percentage of the working population have preexisting chronic conditions such as CVD, which would affect their body’s response to conditions of heat stress.51 A study conducted by surveying 46,781 employed adults between the ages of 18 and 34 showed that 26.1% were obese, 11% had high blood pressure, and 9.7% had high cholesterol.52 Obesity is directly correlated with cardiovascular risk factors such as dyslipidemia, type 2 diabetes, hypertension, and sleep disorders. Obesity also directly linked with the development of CVD and CVD mortality independently of other cardiovascular risk factors.53 Increased ambient temperatures are also associated with lower high-density lipoprotein, higher low-density lipoprotein, and reduced physical activity levels, which all increase long-term CVD risk.54
Another factor contributing to the link between CVD and heat stress is the release of heat shock proteins (HSP). About 17 genes in the human genome encode multiple HSP70 proteins.55 These proteins are activated to help the body maintain normal function in heat stress and strain conditions when there are changes in the environment. Evidence in the literature suggests that the HSP60 and HSP70 heat shock proteins are linked to cardiovascular disease because of the role they play in immune system activation and inflammation. HSPs can further promote the development of heart disease because they can stimulate the immune response by presenting antigens and enhancing inflammation.56
In patients who already have CVD, the effects of heat stress and strain on the body can further worsen their condition. One study that explored the effect of heat stress on the thermoregulatory responses of patients with class II–III congestive heart failure versus healthy control subjects showed more pronounced negative effects on the subjects with congestive heart failure. Both groups had similar sweating responses to an increased internal temperature. Where the patients differed was their cutaneous vasodilation response. Subjects with class II–III congestive heart failure had a lowered elevation in forearm cutaneous vascular conductance when compared with the healthy control subjects.57 The subjects with congestive heart failure were shown to have a significantly lower vasodilator capacity to direct local heating when compared to the healthy control subjects.
Heat-vulnerable Workers
Workers in occupations exposed to high ambient air temperatures, such as those in farming and construction, are particularly vulnerable to the effects of heat stress. These workers often experience temperatures higher than the recorded ambient air temperature due to direct exposure to sunlight and other environmental factors. Among these vulnerable groups, migrant workers are particularly at risk, yet their health is often overlooked because they are generally considered “young and healthy.” However, migrants face numerous risk factors in host countries that profoundly affect their physical and mental well-being as well as their overall right to health. The cumulative impact of stressors across four key areas—their individual circumstances, workplace conditions, environmental factors, and community settings—further exacerbates the health challenges faced by migrant workers, making them even more susceptible to the hazardous exposure of heat.58 Migrant workers often take lower-paying jobs with longer working hours, typically lacking protection from public policies, working in unsafe conditions with minimal occupational safety and health training, and facing a high risk of occupational injuries.59
The literature suggests that in high-income countries such as the United States, there are significant differences in the CVD morbidity and mortality between migrant populations and host populations.60 The disparities in morbidity and mortality rates varies greatly depending on the country of residence, length of stay, and on the individual migrant’s background. Migration negatively impacts multiple aspects of health, including CVD, and is more evidently documented in migrants who move to high-income countries. An example of this is in Spain, where rates of CVD are higher in workers from the Caribbean, sub-Saharan Africa, and Asia, whereas rates of CVD are lower in workers from North Africa and South America.61 There are similar findings for the variations in CVD outcomes in the Netherlands, where CVD mortality differs greatly between migrants from Suriname and Morocco.61
Migrant populations in high-income countries often exhibit higher rates of CVD risk factors such as obesity, diabetes, and hypertension compared with host populations. The prevalence of these risk factors varies significantly depending on the migrant’s country of origin. Factors contributing to the increased CVD risk among migrants include psychosocial stress, limited socioeconomic resources, inadequate access to health care, and greater exposure to environmental and occupational hazards. In hot regions, migrant workers take on more demanding and physically strenuous outdoor work and therefore higher exposure and vulnerability to extreme heat. For instance, a study in Kuwait demonstrated that certain subpopulations, such as non-Kuwaiti migrant workers and the elderly, are more vulnerable to mortality due to extreme temperatures, with males and individuals aged 15 to 64 years facing a significantly higher risk of death.62 The study found that male migrant workers had a significantly higher relative risk (RR 3.15; 95% CI, 1.44–6.91) of dying from cardiovascular disease during extreme hot temperatures compared with the minimum mortality temperature. Similarly, others highlighted that labor migrants, particularly those from South Asia, face a higher burden of CVD risk factors, such as obesity and diabetes, which are exacerbated by lifestyle changes in the host country.63
Future Directions
The field of occupational cardiology stands at the forefront of addressing the complex interplay between work-related exposures and CVD.64 As this emerging field gains traction, it becomes increasingly important to develop more sophisticated strategies for accurate cardiovascular risk stratification, particularly given the significant number of individuals who develop CVD during their working lives. In high-hazard occupational settings, the implications of such diseases are profound.
While some workplace exposures to CVD are well documented, new and emerging threats, particularly those associated with climate change, demand urgent attention. The pervasive nature of heat due to global warming presents a ubiquitous challenge to the cardiovascular health of workers, especially those in outdoor, high-exposure industries like agriculture and construction. Although there is a substantial body of epidemiological literature on the effects of heat on CVD, there remains a significant gap in the physiological quantification of these effects. Research focused on heart biomarkers and heart imaging before and after intensive heat exposure is sparse, highlighting an area ripe for further exploration.
As regulatory bodies such as OSHA and international agencies work to develop effective, real-world standards and guidelines for mitigating the adverse health effects of extreme heat on workers, it is imperative that we also address the disparities faced by vulnerable working populations, particularly migrant workers. Despite findings that indicate these workers are disproportionately affected by heat-related cardiovascular issues, there is a noticeable lack of research into actionable measures and strategies that employers can take to ensure equitable health outcomes.
Looking ahead, it is evident that as global temperatures continue to rise, so too will the rates of morbidity and mortality among workers in high-exposure industries. The urgent need to protect the cardiovascular health of our most vulnerable workers will not only improve their quality of life but also alleviate the financial burden on healthcare systems and employers alike. The path forward requires innovative approaches, grounded in solid research, to ensure that occupational cardiology can meet the challenges posed by a warming world.
Key Points
Workplace exposures significantly contribute to cardiovascular diseases through physical, chemical, biological, ergonomic, and psychosocial hazards.
New and emerging workplace threats, particularly those linked to climate change, show the urgent need for updated research and regulatory measures to protect worker health.
Heat stress exacerbates cardiovascular strain, particularly in outdoor workers.
Migrant workers are particularly vulnerable to cardiovascular risks from extreme heat exposure.
Occupational cardiology is an emerging field that focuses on the intersection of work-related exposures and cardiovascular disease.
Funding Statement
This investigation was made possible by Grant No. T42 OH008416 from the National Institute for Occupational Safety and Health (NIOSH) through Harvard-NIOSH Education and Research Center (ERC) pilot grant awarded to Barrak Alahmad.
Funding Information
Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIOSH.
Competing Interests
The authors have no competing interests to declare.
References
- 1.WHO [Internet]. Geneva, Switzerland: World Health Organization; c2021. Cardiovascular diseases (CVDs); 2021. Jun [cited 2024 Oct 7]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) [Google Scholar]
- 2.CDC [Internet]. Atlanta, GA: US Centers for Disease Control and Prevention; c2024. Heart Disease Facts; 2024. [cited 2024 Oct 7]. Available from: https://www.cdc.gov/heart-disease/data-research/facts-stats/index.html [Google Scholar]
- 3.Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020. Dec 22;76(25):2982-3021. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015. Jan 27;131(4):e29-322. doi: [DOI] [PubMed] [Google Scholar]
- 5.Price AE. (2004). Heart disease and work. Heart. 2004 Sep;90(9):1077-84. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parsons IT, Nicol ED, Holdsworth D, et al. Cardiovascular risk in high-hazard occupations: the role of occupational cardiology. Eur J Prev Cardiol. 2022. Mar 30;29(4):702-713. doi: [DOI] [PubMed] [Google Scholar]
- 7.CDC [Internet]. Atlanta, GA: US Centers for Disease Control and Prevention; c2024. About work-related heart disease. Centers for Disease Control and Prevention; 2024. Jan [cited 2024 Oct 7]. Available from: https://www.cdc.gov/niosh/heartdisease/about/index.html [Google Scholar]
- 8.Dzhambov A, Dimitrova D. Heart disease attributed to occupational noise, vibration and other co-exposure: Self-reported population-based survey among Bulgarian workers. Med Pr. 2016;67(4):435-45. doi: [DOI] [PubMed] [Google Scholar]
- 9.Hahad O, Kröller-Schön S, Daiber A, Münzel T. The Cardiovascular Effects of Noise. Dtsch Arztebl Int. 2019. Apr 5;116(14):245-250. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jemielita P, Lip GY, Kurasz A, et al. 2024. Noise and light exposure and cardiovascular outcomes: A review of evidence, potential mechanisms and implications. Trends Cardiovasc Med. 2024. Jul 6:S1050-1738(24)00059-8. doi: [DOI] [PubMed] [Google Scholar]
- 11.Tamaian, L, Cocarla A. Na3Pt10Si5: A Non-Centrosymmetric Superconductor Having Rattling Na Atoms in the Tunnel Framework Structure. Inorg Chem. 2019. Oct 7;58(19):12911-12917. doi: [DOI] [PubMed] [Google Scholar]
- 12.Schäfer A, Kratky KW. The effect of colored illumination on heart rate variability. Forsch Komplementmed. 2006. Jun;13(3):167-73. doi: [DOI] [PubMed] [Google Scholar]
- 13.Münzel T, aHahad O, Daiber A. The dark side of nocturnal light pollution. Outdoor light at night increases risk of coronary heart disease. Eur Heart J. 2021. Feb 21;42(8):831-834. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molcan L, Zeman M. Shifts in the light-dark cycle increase unpredictability of the cardiovascular system. Auton Neurosci. 2017. Sep:206:51-59. doi: [DOI] [PubMed] [Google Scholar]
- 15.Chellappa SL, Lasauskaite R, Cajochen C. 2017. In a Heartbeat: Light and Cardiovascular Physiology. Front Neurol. 2017. Oct 20:8:541. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holtermann A, Marott JL, Gyntelberg F, et al. Self-reported occupational physical activity and cardiorespiratory fitness: Importance for cardiovascular disease and all-cause mortality. Scand J Work Environ Health. 2016. Jul 1;42(4):291-8. doi: [DOI] [PubMed] [Google Scholar]
- 17.Koskinen HL, Kauppinen T, Tenkanen L. Dual role of physical workload and occupational noise in the association of the metabolic syndrome with risk of coronary heart disease: findings from the Helsinki Heart Study. Occup Environ Med. 2011. Sep;68(9):666-73. doi: [DOI] [PubMed] [Google Scholar]
- 18.Qiu S, Cai X, Jia L, et al. Does objectively measured light-intensity physical activity reduce the risk of cardiovascular mortality? A meta-analysis. Eur Heart J Qual Care Clin Outcomes. 2021. Sep 16;7(5):496-504. doi: [DOI] [PubMed] [Google Scholar]
- 19.Alexander T, Thomson VS, Malviya A, et al. Guidance for health care providers on management of cardiovascular complications in patients suspected or confirmed with COVID 19 virus infection. J Assoc Physicians India. 2020. May;68(5):46-49. PMID: 32610866 [PubMed] [Google Scholar]
- 20.Navas-Acien A, Guallar E, Silbergeld EK, Rothenberg SJ. Lead exposure and cardiovascular disease—a systematic review. Environ Health Perspect. 2007. Mar;115(3):472-82. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaziri ND. Mechanisms of lead-induced hypertension and cardiovascular disease. Am J Physiol Heart Circ Physiol. 2008. Aug;295(2):H454-65. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wāng Y, Ma L, Wang C, Gao T, Han Y, Xu DX. Cardiovascular adverse effects and mechanistic insights of arsenic exposure: A Review. Environ Chem Lett. 2024. Jan 9;22(3):1437-1472. doi: [Google Scholar]
- 23.Moon K, Guallar E, Navas-Acien A. Arsenic exposure and cardiovascular disease: an updated systematic review. Curr Atheroscler Rep. 2012. Dec;14(6):542-55. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Atkins EH, Baker EL. Exacerbation of coronary artery disease by occupational carbon monoxide exposure: a report to two fatalities and a review of the literature. Am J Ind Med. 1985;7(1):73-9. doi: [DOI] [PubMed] [Google Scholar]
- 25.Al-Matrouk A, Al-Hemoud A, Al-Hasan M, Alabouh Y, Dashti A, Bojbarah H. Carbon Monoxide Poisoning in Kuwait: A Five-year, Retrospective, Epidemiological Study. Int J Environ Res Public Health. 2021. Aug 22;18(16):8854. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Armstrong TJ, Burdorf A, Descatha A, et al. Authors’ response: Letter to the Editor concerning OCRA as preferred method in ISO standards on biomechanical risk factors. Scand J Work Environ Health. 2018. Jul 1;44(4):439-440. doi: [DOI] [PubMed] [Google Scholar]
- 27.Arora, A, Suri P, Arora V. Bacteria and the human heart: the occurrence, etiopathogenesis, treatment, and challenges. J Cardiovasc Med. 2021. Jan 1;1(4):256-278. doi: [Google Scholar]
- 28.Kuffner M, Pawlak A, Przybylski M. Viral infection of the heart: pathogenesis and diagnosis. Polish J Microbiol. 2017;65(4):391-398. doi: [DOI] [PubMed] [Google Scholar]
- 29.Badrinath A, Bhatta S, Kloc A. Persistent viral infections and their role in heart disease. Front Microbiol. 2022. Nov 24:13:1030440. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sara D, Prasad M, Eleid MF, Zhang M, Widmer RJ, Lerman A. Association Between Work-Related Stress and Coronary Heart Disease: A Review of Prospective Studies Through the Job Strain, Effort-Reward Balance, and Organizational Justice Models. J Am Heart Assoc. 2018. Apr 27;7(9):e008073. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med. 1977. Mar;31(1):42-8. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schnall PL, Schwartz JE, Landsbergis PA, Warren K, Pickering TG. (1992). Relation between job strain, alcohol, and ambulatory blood pressure. Hypertension. 1992 May;19(5):488-94. doi: [DOI] [PubMed] [Google Scholar]
- 33.Kivimäki M, Kawachi I. Work Stress as a Risk Factor for Cardiovascular Disease. Curr Cardiol Rep. 2015. Sep;17(9):630. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schettini MA, Passos RF, Koike BD. Shift Work and Metabolic Syndrome Updates: A Systematic Review. Sleep Sci. 2023. Jul 6;16(2):237-247. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012. Apr 3;9(6):360-70. doi: [DOI] [PubMed] [Google Scholar]
- 36.McMorris T, Swain J, Smith M, et al. Heat stress, plasma concentrations of adrenaline, noradrenaline, 5-hydroxytryptamine and cortisol, mood state and cognitive performance. Int J Psychophysiol. 2006. Aug;61(2):204-15. doi: [DOI] [PubMed] [Google Scholar]
- 37.NCEINOAA [Internet]. Ashville, NC: National Centers for Environmental Information; National Oceanic and Atmospheric Administration; c2024. Annual 2023 Global Climate Report; 2023. [cited 2024 Sep 27]. Available from: https://www.ncei.noaa.gov/access/monitoring/monthly-report/global/202313 [Google Scholar]
- 38.International Labour Organization [Internet]. Geneva, Switzerland: International Labour Organization; c2024; [cited 2024 Oct 7]. Available from: https://www.ilo.org [Google Scholar]
- 39.Flouris AD, Dinas PC, Ioannou LG, et al. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. 2018. Dec;2(12):e521-e531. doi: [DOI] [PubMed] [Google Scholar]
- 40.Morrissey MC, Brewer GJ, Williams WJ, Quinn T, Casa DJ. Impact of occupational heat stress on worker productivity and economic cost. Am J Ind Med. 2021. Dec;64(12):981-988. doi: [DOI] [PubMed] [Google Scholar]
- 41.Desai Y, Khraishah H, Alahmad B. Heat and the Heart. Yale J Biol Med. 2023. Jun 30;96(2):197-203. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moghadamnia MT, Ardalan A, Mesdaghinia A, Keshtkar A, Naddafi K, Yekaninejad MS. Ambient temperature and cardiovascular mortality: a systematic review and meta-analysis. Peer J. 2017. Aug 4:5:e3574. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cheng J, Xu Z, Bambrick H, et al. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ Res. 2019. Oct:177:108610. doi: [DOI] [PubMed] [Google Scholar]
- 44.Liu J, Varghese BM, Hansen A, et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis. Lancet Planet Health. 2022. Jun;6(6):e484-e495. doi: [DOI] [PubMed] [Google Scholar]
- 45.Alahmad B, Khraishah H, Royé D, et al. Associations Between Extreme Temperatures and Cardiovascular Cause-Specific Mortality: Results From 27 Countries. Circulation. 2023. Jan 3;147(1):35-46. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.González-Alonso J. Human thermoregulation and the cardiovascular system. Exp Physiol. 2012. Mar;97(3):340-6. doi: [DOI] [PubMed] [Google Scholar]
- 47.Semenza J, McCullough JE, Flanders WD, McGeehin MA, Lumpkin JR. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999. May;16(4):269-77. doi: [DOI] [PubMed] [Google Scholar]
- 48.Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O. Heat stress in older individuals and patients with common chronic diseases. CMAJ. 2010. Jul 13;182(10):1053-60. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wong BJ, Hollowed CG. Current concepts of active vasodilation in human skin. Temperature (Austin). 2016. Jun 21;4(1):41-59. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Epstein Y, Yanovich R. (2019). Heatstroke. N Engl J Med. 2019 Jun 20;380(25):2449-2459. doi: [DOI] [PubMed] [Google Scholar]
- 51.Boersma P, Black LI, Ward BW. Prevalence of Multiple Chronic Conditions Among US Adults, 2018. Prev Chronic Dis. 2020. Sep 17:17:E106. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.CDC [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; c2024. Watson KB. Chronic conditions among adults aged 18–34 years - United States, 2019; 2022. Jul 29 [cited 2024 Oct 7]. Available from: https://www.cdc.gov/mmwr/volumes/71/wr/mm7130a3.htm [Google Scholar]
- 53.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021. May 25;143(21):e984-e1010. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khraishah H, Alahmad B, Ostergard RL Jr., et al. Climate change and cardiovascular disease: implications for global health. Nat Rev Cardiol. 2022. Dec;19(12):798-812. doi: [DOI] [PubMed] [Google Scholar]
- 55.Hu C, Yang J, Qi Z, et al. Heat shock proteins: Biological functions, pathological roles, and therapeutic opportunities. MedComm (2020). 2022. Aug 2;3(3):e161. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rodríguez-Iturbe B, Johnson R. Heat shock proteins and cardiovascular disease. Physiol Int. 2018. Mar 1;105(1):19-37. doi: [DOI] [PubMed] [Google Scholar]
- 57.Cui J, Arbab-Zadeh A, Prasad A, Durand S, Levine BD, Crandall CG. Effects of heat stress on thermoregulatory responses in congestive heart failure patients. Circulation. 2005. Oct 11;112(15):2286-92. doi: [DOI] [PubMed] [Google Scholar]
- 58.Alahmad B, Kurdi H, Colonna K, Gasana J, Agnew J, Fox MA. COVID-19 stressors on migrant workers in Kuwait: cumulative risk considerations. BMJ Glob Health. 2020. Jul;5(7):e002995. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moyce SC, Schenker M. Migrant Workers and Their Occupational Health and Safety. Annu Rev Public Health. 2018. Apr 1:39:351-365. doi: [DOI] [PubMed] [Google Scholar]
- 60.Singh G, Siahpush M, Azuine RE, Williams SD. Increasing Area Deprivation and Socioeconomic Inequalities in Heart Disease, Stroke, and Cardiovascular Disease Mortality Among Working Age Populations, United States, 1969-2011. Int J MCH AIDS. 2015;3(2):119-33. [PMC free article] [PubMed] [Google Scholar]
- 61.Agyemang C, Van Den Born BJ. Cardiovascular health and disease in migrant populations: a call to action. Nat Rev Cardiol. 2022. Jan;19(1):1-2. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alahmad B, Shakarchi AF, Khraishah H, et al. Extreme temperatures and mortality in Kuwait: Who is vulnerable? Sci Total Environ. 2020. Aug 25:732:139289. doi: [DOI] [PubMed] [Google Scholar]
- 63.Mishra SR, Ghimire S, Joshi C, et al. Cardio-metabolic disease risk factors among South Asian labour migrants to the Middle East: a scoping review and policy analysis. Global Health. 2019. May 2;15(1):33. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chamley RR, Holdsworth DA, D’arcy JL, Nicol ED. An Introduction to Occupational Cardiology. Eur Heart J. 2019. Aug 1;40(29):2389-2392. doi: [DOI] [PubMed] [Google Scholar]


