Abstract
Background and Purpose
Neurohospitalists specialize in the care of hospitalized patients with neurological conditions. As the neurohospitalist model of patient care has grown rapidly and in diverse ways, there has been increasing demand for a formal definition of the field, particularly to support curriculum development for learners at multiple levels.
Methods
The Neurohospitalist Society (NHS) formed a Core Competencies Committee in 2021. This committee defined the scope of the Neurohospitalist Core Competencies and organized the competency topics into chapters. This chapter list was approved by the members of the NHS. An open invitation was made to the general membership of the NHS to write chapters on a first-come, first-served basis, using a standardized chapter template developed by the Committee. A three-step editing process was completed, with members of the Committee serving as editors. A dissemination strategy was designed, including drafting of 2 manuscripts (the Core Competencies themselves, and this accompanying manuscript) and outreach to the general membership of the NHS.
Results
The Neurohospitalist Core Competencies include 27 chapters divided into 3 sections: neurological conditions; clinical interventions and interpretations of ancillary studies; and neurohospitalist role in the health care system. The complete version of the Neurohospitalist Core Competencies is published as a separate manuscript in this issue of The Neurohospitalist.
Conclusions
The creation of the Neurohospitalist Core Competencies was a multi-year initiative intended to support practicing neurohospitalists, trainees interested in pursuing careers in the field, medical education leaders, and administrative leaders of hospitals and departments.
Keywords: neurohospitalist clinical specialty, education techniques, quality techniques
Introduction
Neurohospitalists are neurologists who subspecialize in the care of hospitalized patients with neurological disorders. The term “neurohospitalist” first appeared in the medical literature in 2005, a decade after the term “hospitalist” was coined to describe internal medicine physicians who focus on the care of hospitalized patients.1,2 The neurohospitalist field has grown rapidly in the ensuing years, marked by the formation of the Neurohospitalist Section of the American Academy of Neurology (AAN) in 2009, the creation of the Neurohospitalist Society (NHS) in 2010, the launch of the subspecialty journal The Neurohospitalist in 2011, and the development of neurohospitalist fellowship training programs across the United States.3,4 Neurohospitalist practice has been associated with improvements in clinical quality metrics such as documentation of acuity of patient diagnosis, length of stay, and cost.5-7 In addition, implementation of neurohospitalist models of practice have been associated with improvements in the educational experience of medical students and neurology residents.6,8
With fewer than 15 neurohospitalist fellowship training positions available annually as of 2024 and with many practicing neurohospitalists having completed vascular neurology or neurocritical care fellowships, the field has long been defined more by what we do than by a particular training experience.4,9-11 Therefore, while individuals who consider themselves neurohospitalists share an emphasis on the care of hospitalized patients, their specific practices can vary significantly depending on the local needs and infrastructure of a given hospital or health care system. As evidenced by national surveys, examples of practice variabilities include: academic vs community setting; the presence of a primary neurology service vs consultation only; most common patient diagnoses; participation in teleneurology; participation in acute stroke coverage; and participation in non-clinical roles such as education, research, and administration.9-11
Historically, it has been typical for rapidly growing site-based medical specialties to develop core competencies with the goals of defining and characterizing the field and offering a structure for curriculum development. Relevant examples include hospital medicine, pediatric hospital medicine, and neurocritical care.12-15 As a central unifying organization of neurohospitalists, the NHS has recognized repeated calls for both defining the scope of the field and offering a framework for curriculum development for neurology residency and neurohospitalist fellowship programs. 16
In this manuscript, we describe the steps taken to develop and disseminate the Neurohospitalist Core Competencies. We also discuss how the Neurohospitalist Core Competencies may be utilized by multiple stakeholder groups. The full text of the Neurohospitalist Core Competencies is published as a separate manuscript in this issue of The Neurohospitalist.
Methods
Structure and Functions of the NHS
The NHS was formed in 2010 by a small group of neurologists practicing in the inpatient setting with the goal of creating a central unifying organization of neurohospitalists. As of 2024, the NHS has 1042 members representing 48 of the 50 United States plus Washington, DC and 12 other countries (Australia, Brazil, Canada, Georgia, Italy, Japan, Malaysia, Mexico, Morocco, Pakistan, Portugal, United Kingdom). The NHS is led by a President and a Vice President, each of whom serves a 2-year term, with the option of 1 additional 2-year term. These leaders are supported by a 5 to 16-member Board of Directors, each of whom is elected by a vote of the general membership of the NHS. The Board of Directors meet quarterly. Among the authors of this paper, 2 served as President (J.W, 2017-2021; M.B.R, 2021-2023) and 1 served as Vice President (J.G.M, 2021-2023) of the NHS during the period of development of the Neurohospitalist Core Competencies. The remaining authors served on the Board of Directors of the NHS (C.A.G, 2021-present; J.P.K, 2014-present).
The NHS has organized an Annual Meeting since 2013 that provides scientific updates and formal and informal opportunities for the general membership to share their requests for future initiatives of the Society. Subsequently, the President, Vice President, and Board of Directors prioritize these suggestions and form Committees when appropriate. Current Committees include the Fellowship Accreditation Committee (formed in 2021), the Advanced Practice Provider Education Committee (formed in 2023), and the Neurohospitalist Consultant Committee (formed in 2024). The Committees report out on their progress quarterly to the Board of Directors and yearly to the general membership at the Annual Meeting.
Formation of the Core Competencies Committee
Formally characterizing the breadth of the neurohospitalist field had been a long-term goal since the early years of the NHS. For example, Dr S. Andrew Josephson, the inaugural Vice President of the NHS, predicted in 2011, “I’m sure that, just like hospital medicine, there will be a point at which time our subspecialty becomes defined more formally and systematically.” 17 Multiple events crystallized defining the field as a top priority. First, NHS leaders received multiple inquiries regarding the scope of practice for neurohospitalists by institutions looking to start a program, and by neurohospitalists needing to delineate their skill set as requested by their potential employers. Second, a presentation by Dr Rebecca Tenney-Soiero at the April 2019 meeting of the Neurohospitalist Section of the AAN about the history of pediatric hospital medicine and that field’s approach to developing core competencies energized many in the audience. The establishment of an NHS neurohospitalist fellowship program accreditation process in 2021 further demonstrated the need for competencies upon which to build training curricula. That year, the NHS Board of Directors set the creation of Core Competencies as a strategic goal for the organization to improve the quality of fellowship programs and clinical practice.
The Core Competencies Committee formed in the winter of 2021 by volunteer members from the NHS Board of Directors (Table 1). The goals of the competencies were to help identify the unique skill set of the neurohospitalist. The committee met via teleconference on an ad hoc basis with frequent email communications between meetings.
Table 1.
Members of the Core Competencies Committee.
| Name | Affiliation |
|---|---|
| Carolin I. Dohle, MD | New York Medical College |
| Vanja C. Douglas, MD | University of California, San Francisco |
| Carl A. Gold, MD, MS | Stanford University |
| Joshua P. Klein, MD, PhD | Brigham and Women’s Hospital |
| David Likosky, MD | Evergreen Health, University of Washington |
| Matthew W. Luedke, MD | Duke University |
| Jane G. Morris, MD | Maine Medical Center, Tufts University School of Medicine |
| Karen D. Orjuela, MD, MSCR, MBA | University of Colorado |
| Jamie Palaganas, MD | University of North Carolina, Weill Cornell Medical College |
| Megan B. Richie, MD | University of California, San Francisco |
| Jennifer R. Simpson, MD | University of Colorado |
| Brian J. Scott, MD | Stanford University |
| Maulik P. Shah, MD, MHS | University of California, San Francisco |
| Jana J. Wold, MD (Chair) | University of Utah |
Selection of the Chapter List
The first task for the Core Competencies Committee was to generate the chapter list for the Neurohospitalist Core Competencies. The Core Competencies Committee actively decided to draft the chapter list as a definition of the field, rather than a definition of competencies to be demonstrated by any individual practicing neurohospitalist or neurohospitalist fellow. This process involved each member reviewing their local residency curricula, neurology textbooks, as well as their own clinical experience to create an initial draft list that was discussed amongst the group, edited, and refined several times. Disagreements were adjudicated via discussion and consensus. Chapter lists were presented to the Board of Directors for approval, then circulated to the NHS members for feedback and further revision. The chapter list was finalized in 2022.
Writing and Editing the Chapters
The formatting of the Neurohospitalist Core Competencies chapters was based upon the formatting of the chapters in the core competencies in hospital medicine. 12 Each chapter topic consisted of bulleted points outlining key concepts divided into sections of Knowledge, Skills, Attitudes, and Systems Organization and Improvement, flanked by a brief Introduction and key References.
In August 2022, the Core Competencies Committee sent an email inviting members of the NHS to sign up to author 1 or more specific chapters of the Neurohospitalist Core Competencies on a first-come, first-served basis. One completed chapter, “Vascular Disease of the Nervous System,” was attached to this email as an example and template. The first drafts of all chapters were completed over the period of October 2022-June 2024, with iterative reassignment of authors as needed when original authorship commitments could not be honored.
All members of the Core Competencies Committee were invited to participate in the editing process. Each chapter underwent a three-step editing process. First, a primary editor suggested changes in content, style, and language. Next, a secondary editor reviewed the suggestions of the primary editor, accepting or rejecting each 1, and making additional changes if indicated. Finally, a tertiary editor—often assigned all or many chapters within a given section—reviewed the secondary edits, typically with an emphasis on avoiding redundancy in content among chapters. Of note, the author(s) of each chapter were not provided feedback or an opportunity to comment on changes made during the editorial process.
After tertiary editing, standardized formatting was performed by the association managers of the NHS.
Dissemination Strategy
The Core Competencies Committee Designed a Seven-part Dissemination Strategy:
1. Publication of the Neurohospitalist Core Competencies in The Neurohospitalist.
2. Simultaneous publication of this manuscript describing the process and methodology of the development of the Neurohospitalist Core Competencies in The Neurohospitalist.
3. Press release and social medial posts by the NHS upon publication of the Neurohospitalist Core Competencies in The Neurohospitalist.
4. Open access availability of the Neurohospitalist Core Competencies on the website of the NHS.
5. Email to general membership of the NHS announcing the publication of the Neurohospitalist Core Competencies.
6. Presentation and discussion of the Neurohospitalist Core Competencies at the NHS Annual Meeting.
Data Analysis
There is no relevant data analysis to report.
Results
The section and chapter titles of the Neurohospitalist Core Competencies are listed in Table 2. In total, 31 individuals served as authors of chapters, including 10 members of the Core Competencies Committee (Table 3). Nine chapters had 2 authors and no chapter had 3 or more authors. Nine individuals participated in the authorship of more than 1 chapter (6 individuals: 2 chapters; 2 individuals: 3 chapters; 1 individual: 5 chapters). Among the 14 members of the Neurohospitalist Core Competencies Committee, 12 participated in the editing process.
Table 2.
Sections and Chapter Titles of the Neurohospitalist Core Competencies.
| Section 1: Neurological Conditions |
| 1. Vascular disease of the nervous system |
| 2. Seizures and status epilepticus |
| 3. Acute disorders of consciousness and cognition |
| 4. Infectious disorders of the nervous system |
| 5. Acute toxic and metabolic conditions of the nervous system |
| 6. Acute headache |
| 7. Acute disorders of the peripheral nervous system |
| 8. Neoplastic disorders of the nervous system |
| 9. Autoimmune and paraneoplastic conditions of the nervous system |
| 10. Acute disorders of the vestibular system |
| 11. Traumatic injuries of the nervous system |
| 12. Neurological conditions specific to reproduction, sex, and gender |
| 13. Perioperative and transplant neurology |
| 14. Functional neurological disorders |
| Section 2: Clinical Interventions and Interpretations of Ancillary Studies |
| 1. Determine death by neurologic criteria |
| 2. Intravenous thrombolysis |
| 3. Lumbar puncture |
| 4. Indications and clinical correlation of nervous system diagnostic imaging |
| 5. Indications and clinical correlation of neurophysiology studies |
| Section 3: Neurohospitalist Role in the Health care System |
| 1. Equitable and inclusive care |
| 2. Inpatient perioperative consultation for neurologic patients |
| 3. Neuroprognostication |
| 4. Teleneurology |
| 5. Neurological risk reduction for the hospitalized patient |
| 6. Medical risk reduction for the hospitalized patient |
| 7. Neurohospitalist as educator |
| 8. Hospitalist skills for the neurohospitalist |
| a. Transitions of care |
| b. Patient safety |
| c. Quality improvement |
| d. Process optimization |
| e. Co-management in the hospital setting |
| f. Resource stewardship |
| g. Professionalism and medical ethics |
| h. Care of the caregiver |
| i. Practice management |
| j. Information management |
Table 3.
Authors of the Neurohospitalist Core Competencies in Alphabetical Order.
| Name | Affiliation a |
|---|---|
| Roshni S. Dhoot, MD | Duke University |
| Carolin I. Dohle, MD | New York Medical College |
| Jonathan P. Donnelly, MD | Rochester Regional Health |
| Rachelle Dugue, MD, PhD | Stanford University |
| Shefali Dujari, MD | Stanford University |
| Matthew E. Ehrlich, MD, MPH | Duke University |
| Kristin Galetta, MD | Stanford University |
| Carl A. Gold, MD, MS | Stanford University |
| Tarini Goyal, MD | Columbia University |
| Jerome A. Jeevarajan, MD | University of Texas McGovern Medical School |
| Joshua P. Klein, MD, PhD | Brigham and Women’s Hospital |
| Molly G. Knox, MD | Mayo Clinic Arizona |
| Kathryn A. Kvam, MD | Stanford University |
| Matthew W. Luedke, MD | Duke University |
| Matthew B. Maas, MD, MS | Northwestern University |
| Vishal A. Mandge, MD, MPH | Duke University |
| Elizabeth Marriott, MD | Duke University |
| Ethan Meltzer, MD | University of Texas at Austin Dell Medical School |
| Jane G. Morris, MD | Maine Medical Center, Tufts University School of Medicine |
| Rafid Mustafa, MD | Mayo Clinic Rochester |
| Jamie Palaganas, MD | University of North Carolina, Weill Cornell Medical College |
| Megan B. Richie, MD | University of California, San Francisco |
| Jetter Robertson, DO | University of Minnesota |
| Jennifer R. Simpson, MD | University of Colorado |
| Brian J. Scott, MD | Stanford University |
| Guillermo E. Solorzano, MD | University of Virginia |
| Prateek Thatikunta, MD | Kaiser Permanente, Oakland |
| Michel Toledano, MD | Mayo Clinic Rochester |
| Lahoud Touma, MD | University of Montreal |
| Jana J. Wold, MD | University of Utah |
| Margaret Y. Yu, MD | University of Illinois at Chicago |
aCurrent affiliation(s) at time of submission of this manuscript; some authors had different affiliations at the time they drafted the chapters.
In terms of dissemination, the full version of the Neurohospitalist Core Competencies is published as a separate manuscript in this issue of The Neurohospitalist. The press release and social media posts, permanent posting on the NHS website, and email to the general membership all coincide with the timing of this publication. One of the authors (J.W.) provided an update to the general membership at the NHS Annual Meeting in Baltimore, Maryland in October 2024. An additional presentation will be made at the NHS Annual Meeting in October 2025.
Discussion
Two decades after the neurohospitalist specialty was first named in the medical literature, the NHS has developed core competencies to more formally define the scope of the field and to support related curriculum development. 1 Divided into 3 sections comprised of 27 chapters, the Neurohospitalist Core Competencies reflect the input of the membership of the NHS, the leadership of the Board of Directors and the Core Competencies Committee, and the contributions of individual authors. The Neurohospitalist Core Competencies are published as a separate manuscript in this issue of The Neurohospitalist and are being disseminated through multiple channels by the NHS. Below we discuss the contents of the 3 sections and the potential uses of the Neurohospitalist Core Competencies for multiple stakeholder groups.
Section 1 includes 14 chapters on different classes of neurological disorders. This section reflects the diversity of clinical practice among neurohospitalists and the breadth of conditions that neurohospitalists may be responsible for diagnosing and treating. For example, detailed knowledge of the evidence-based hospital management of patients with common conditions such as acute ischemic stroke (Section 1, Chapter 1), seizure (Section 1, Chapter 2), and toxic-metabolic encephalopathy (Section 1, Chapter 5) is fundamental for neurohospitalists. 11 At the same time, neurohospitalists—and especially those in academic settings—may serve as institutional experts in the diagnosis and initial treatment of uncommon or rare conditions such as rapidly progressive dementia (Section 1, Chapter 3), autoimmune encephalitis (Section 1, Chapter 9), and neurological complications of solid organ transplantation (Section 1, Chapter 12). This balance of the common and the rare is reflected in the agendas of the NHS Annual Meetings and in the pages of The Neurohospitalist, and may be a contributor to professional fulfillment among practicing neurohospitalists. 11
Section 2 is composed of 5 chapters focused on clinical interventions and interpretations of ancillary studies. Throughout the medical literature, there are many examples of neurohospitalists being called upon to determine the need for testing such as neuroimaging and electroencephalography, or to clinically interpret the results of these studies after they have been completed.18-24 Effective resource utilization and thoughtful interpretation of test results promote appropriate care and patient progression.
Section 3 includes 8 chapters describing the role of neurohospitalists in the health care system. The chapters reflect the many identities of the neurohospitalist, such as: skilled communicators of uncertain prognoses (Section 3, Chapter 3); dedicated educators with a special emphasis on systems-based practice (Section 3, Chapter 7); administrative leaders in patient safety (Section 3, Chapter 8, sub-chapter b) and quality improvement (Section 3, Chapter 8, sub-chapter c); collaborative innovators in teleneurology (Section 3, Chapter 4), co-management of hospitalized patients (Section 3, Chapter 8, sub-chapter e), and transitions of care (Section 3, Chapter 8, sub-chapter a).8,11,25-29 To a significant degree, it is these identities that have driven the rapid growth of the neurohospitalist model of care. 30
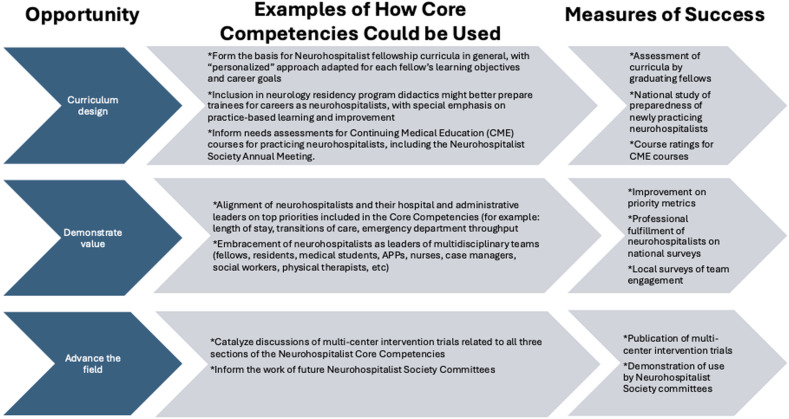
Much has been written about the value and potential uses of core competencies in general and in related fields such as hospital medicine.12,31 Within the medical education literature there has been significant emphasis on competency systems, such as the 1 developed by the Accreditation Council for Graduate Medical Education (ACGME), in which each individual learner is intended to demonstrate proficiency in every defined competency. 32 It should be emphasized that the Neurohospitalist Core Competencies were intentionally designed to define the field, and not to define individual proficiency. Figure 1 demonstrates possible uses of the Neurohospitalist Core Competencies by key stakeholder groups, including practicing neurohospitalists, medical education leaders and trainees, and hospital and departmental administrative leaders. The uses are divided into 3 main areas: curriculum design, demonstration of value, and advancing the field. We do not anticipate that the Neurohospitalist Core Competencies will be the start of a path towards board certification, especially given the diversity of training paths among practicing neurohospitalists. 30
Figure 1.
Model of how the Neurohospitalist Core Competencies may be utilized.
There are several limitations to note in the process of developing the Neurohospitalist Core Competencies. First, since the practice of neurohospitalists can be so varied, the contents of the 27 chapters may not fully encompass the scope of the field. Second, academic neurohospitalists and those practicing on the West Coast of the United States may have been overrepresented on the Core Competencies Committee, while community neurohospitalists and individuals practicing in the Midwest, in any of the 10 largest most populous cities in the United States, or internationally may have been underrepresented. 33 Third, many members of the Core Competencies Committee simultaneously served on the NHS Board of Directors, which provided oversight of the Core Competencies Committee, potentially limiting the Board’s ability to provide meaningful feedback to the Committee.
In summary, the Neurohospitalist Core Competencies mark a milestone in the maturation of the field. We anticipate that key stakeholders, including practicing neurohospitalists, trainees interested in the field, education leaders, and hospital administrators, will find value in the existence of the Neurohospitalist Core Competencies. The NHS plans for its current and future committees to seamlessly incorporate the Neurohospitalist Core Competencies. Given the breadth of the field and its continual evolution, the NHS Board of Directors plans to review the Neurohospitalist Core Competencies every 5 years to determine the need for preparing and releasing an update. The approach to such a revision will build on best practices from other related societies, including the experience of the pediatric hospital medicine field, which released revisions in 2020 after the original publication of its core competencies in 2010.13,14
Acknowledgements
The authors wish to thank: the members of the Core Competencies Committee, and the authors of the chapters, and the Board of Directors of the NHS for their dedication to this endeavor; and NHS association managers Amanda Pacia and Faye Silag for their administrative support.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Carl A. Gold https://orcid.org/0000-0002-4868-4152
Joshua P. Klein https://orcid.org/0000-0001-6139-8081
Jana J. Wold https://orcid.org/0000-0003-3689-6024
References
- 1.Avitzur O. Neurohospitalists: a new term for a new breed of neurologist. Neurol Today. 2005;5(10):44-45. [Google Scholar]
- 2.Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514-517. doi: 10.1056/NEJM199608153350713 [DOI] [PubMed] [Google Scholar]
- 3.Douglas VC. A message from the editor in chief. Neurohospitalist. 2011;1(1):4. doi: 10.1177/1941875210392322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The neurohospitalist society - neurohospitalist prospective fellows. https://neurohospitalistsociety.org/Accreditation/prospective-fellows.php. Accessed September 6, 2024.
- 5.Freeman WD, Dawson SB, Raper C, Thiemann K, Josephson SA, Barrett KM. Neurohospitalists reduce length of stay for patients with ischemic stroke. Neurohospitalist. 2011;1(2):67-70. doi: 10.1177/1941875210394202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douglas VC, Scott BJ, Berg G, Freeman WD, Josephson SA. Effect of a neurohospitalist service on outcomes at an academic medical center. Neurology. 2012;79(10):988-994. doi: 10.1212/WNL.0b013e31826846cb [DOI] [PubMed] [Google Scholar]
- 7.Gold CA, Scott BJ, Weng Y, Bernier E, Kvam KA. Outcomes of a neurohospitalist program at an academic medical center. Neurohospitalist. 2022;12(3):453-462. doi: 10.1177/19418744221083182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dujari S, Scott BJ, Gold CA, Weng Y, Kvam KA. Education research: educational outcomes associated with the introduction of a neurohospitalist program. Neurol Educ. 2024;3(2):e200131. doi: 10.1212/NE9.0000000000200131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Likosky D, Shulman S, Restrepo L, Freeman WD. Survey of neurohospitalists: subspecialty definition and practice characteristics. Front Neurol. 2010;1:9. doi: 10.3389/fneur.2010.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Likosky DJ, Josephson SA, Coleman M, Freeman WD, Biller J. Survey of current neurohospitalist practice. Neurol Clin Pract. 2012;2(4):319-327. doi: 10.1212/CPJ.0b013e318278be3e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Probasco JC, Greene J, Harrison A, et al. Neurohospitalist practice, perspectives, and burnout. Neurohospitalist. 2019;9(2):85-92. doi: 10.1177/1941874418813029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dressler DD, Pistoria MJ, Budnitz TL, McKean SCW, Amin AN. Core competencies in hospital medicine: development and methodology. J Hosp Med. 2006;1(1):48-56. doi: 10.1002/jhm.6 [DOI] [PubMed] [Google Scholar]
- 13.Stucky ER, Ottolini MC, Maniscalco J. Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5(6):339-343. doi: 10.1002/jhm.843 [DOI] [PubMed] [Google Scholar]
- 14.Maniscalco J, Gage S, Teferi S, Fisher ES. The pediatric hospital medicine core competencies: 2020 revision. J Hosp Med. 2020;15(7):389-394. doi: 10.12788/jhm.3391 [DOI] [PubMed] [Google Scholar]
- 15.Mayer SA, Coplin WM, Chang C, et al. Core curriculum and competencies for advanced training in neurological intensive care: United Council for Neurologic Subspecialties guidelines. Neurocrit Care. 2006;5(2):159-165. doi: 10.1385/ncc:5:2:159 [DOI] [PubMed] [Google Scholar]
- 16.Probasco JC, George BP, Dorsey ER, Venkatesan A. Neurohospitalists: perceived need and training requirements in academic neurology. Neurohospitalist. 2014;4(1):9-17. doi: 10.1177/1941874413495880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butcher L. Career tracks: neurohospitalist movement growing rapidly—more fellowships, A new journal, and an AAN section. Neurol Today. 2011;11(7):56-57. [Google Scholar]
- 18.Kvam KA, Douglas VC, Whetstone WD, Josephson SA, Betjemann JP. Yield of emergent CT in patients with epilepsy presenting with a seizure. Neurohospitalist. 2019;9(2):71-78. doi: 10.1177/1941874418808676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson MR, O’Donovan BD, Gelfand JM, et al. Chronic meningitis investigated via metagenomic next-generation sequencing. JAMA Neurol. 2018;75(8):947-955. doi: 10.1001/jamaneurol.2018.0463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Betjemann JP, Nguyen I, Santos-Sanchez C, Douglas VC, Josephson SA. Diagnostic yield of electroencephalography in a general inpatient population. Mayo Clin Proc. 2013;88(4):326-331. doi: 10.1016/j.mayocp.2012.12.013 [DOI] [PubMed] [Google Scholar]
- 21.Satyanarayan S, Spiegel J, Hovsepian D, et al. Continuous EEG monitoring detects nonconvulsive seizure and Ictal-Interictal Continuum abnormalities in moderate to severe ICANS following systemic CAR-T therapy. Neurohospitalist. 2023;13(1):53-60. doi: 10.1177/19418744221128852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Broadhurst MJ, Dujari S, Budvytiene I, Pinsky BA, Gold CA, Banaei N. Utilization, yield, and accuracy of the FilmArray meningitis/encephalitis panel with diagnostic stewardship and testing algorithm. J Clin Microbiol. 2020;58(9):e00311. doi: 10.1128/JCM.00311-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Galetta K, Gheihman G, Rosen A, Klein JP, Bhattacharyya S. Influence of autoimmune antibody testing on the use of immunotherapy on an inpatient neurology service. Neurohospitalist. 2021;11(3):214-220. doi: 10.1177/1941874420977761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lyman KA, Madill E, Thatikunta P, Threlkeld ZD, Banaei N, Gold CA. An electronic health record intervention to limit viral testing of cerebrospinal fluid. Neurohospitalist. 2023;13(2):173-177. doi: 10.1177/19418744231152103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goyal T, Bereknyei Merrell S, Weimer-Elder B, Kline M, Rassbach CE, Gold CA. A novel serious illness communication curriculum improves neurology residents’ confidence and skills. J Palliat Med. 2023;26(9):1180-1187. doi: 10.1089/jpm.2022.0371 [DOI] [PubMed] [Google Scholar]
- 26.Kvam KA, Bernier E, Gold CA. Quality improvement metrics and methods for neurohospitalists. Neurol Clin. 2022;40(1):211-230. doi: 10.1016/j.ncl.2021.08.011 [DOI] [PubMed] [Google Scholar]
- 27.McCormick R, Estrada J, Whitney C, et al. Teleneurology comprehensive inpatient consultations expedite access to care and decreases hospital length of stay. Neurohospitalist. 2021;11(3):229-234. doi: 10.1177/19418744211000951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greene JG. Collaborative comanagement between neurohospitalists and internal medicine hospitalists decreases provider costs and enhances satisfaction with neurology care at an academic medical center. Neurohospitalist. 2018;8(2):74-81. doi: 10.1177/1941874417735173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah M, Douglas V, Scott B, Josephson SA. A neurohospitalist discharge clinic shortens the transition from inpatient to outpatient care. Neurohospitalist. 2016;6(2):64-69. doi: 10.1177/1941874415618707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Josephson SA. Inpatient neurologic care: continued challenges of a neurohospitalist model. JAMA Neurol. 2013;70(7):825-826. doi: 10.1001/jamaneurol.2013.2968 [DOI] [PubMed] [Google Scholar]
- 31.Enginoğlu D, Arikan CL. A literature review on core competencies. Int J Manag. 2016;7(3):120-127. [Google Scholar]
- 32.Lewis SL, Józefowicz RF, Kilgore S, Dhand A, Edgar L. Introducing the neurology milestones. J Grad Med Educ. 2014;6(1s1):102-104. doi: 10.4300/JGME-06-01s1-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Census Population Clock . Census.gov. https://www.census.gov/popclock/embed.php?component=populous. Accessed September 6, 2024.