Summary:
After burn injury, patients may have abdominal pain due to several causes and etiologies, some of which could be life-threatening, including pancreatitis, stress ulcers, Clostridium difficile infection, and so forth. This pain sometimes poses a major diagnostic challenge. This scoping review is the first reported review to address and discuss this entity of patients after burn injury in abdominal pain of gastrointestinal origin. A scoping review of PubMed, Google Scholar, and other electronic research sites was performed. All relevant articles of any study design were included in this review. Variables included in this study were sex distribution, age, related total burn surface area, incidence rate, characteristics of pain, diagnosis, management, outcomes, and mortality rate. The medical literature identified 114 articles. According to our inclusion criteria, 91 articles were reviewed in this article. Through these articles, we reviewed in detail the characteristics of postburn abdominal pain, the relevant diseases responsible for this complaint, the epidemiologic features of these diseases, and potential management approaches aiming to help burn specialists in making earlier diagnosis and, thus, timely treatment. Early recognition of postburn abdominal pain, as well as timely diagnosis and treatment, play a significant role in prognosis and mortality. Thus, it is extremely important for burn specialists and plastic surgeons to thoroughly investigate postburn abdominal pain. Also, one of the aims of this review was to shed light on the important role of the multidisciplinary team in burn patient management to improve the prognosis.
Takeaways
Question: In burn patients, does early recognition of postburn abdominal pain as well as the timely diagnosis and treatment play a significant role in prognosis and mortality?
Findings: It is extremely important for burn specialists and plastic surgeons to thoroughly investigate postburn abdominal pain.
Meaning: Abdominal pain represents 1 of the most important features of postburn gastrointestinal complications.
INTRODUCTION
Abdominal pain represents 1 of the most important features of postburn gastrointestinal complications.1 So far, a review of medical literature revealed that no articles discuss clearly the relationship between abdominal pain and burn injury. Abdominal pain may represent a leading symptom to a serious underlying disease.2 Herein, we discuss the relevant diseases of gastrointestinal origin responsible for this symptom in patients after burn injury, which include pancreatitis, stress ulcers, Clostridium difficile infection, and other diseases, which will be later discussed separately.1–12 Furthermore, abdominal pain can be a complication of electrical burns.9–11 The management of these entities differs greatly, as it can be conservative or surgical depending on the causative mechanism of this pain.12
METHODS
Literature Search
A scoping review of PubMed, Google Scholar, Scopus, Embase, Cochrane, and other electronic research sites was performed using the search terms with strategy burn AND (abdominal pain OR abdominal pain OR pain, abdominal OR pain, abdominal). All relevant articles of any study design (published till April 15, 2023) were included and narratively discussed in this review. In this review, we followed the checklist of The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 statement: an updated guideline for reporting systematic reviews.13 Variables included in this study were sex distribution, age, related total body surface area (TBSA), incidence rate, characteristics of pain, diagnosis, management, outcomes, and mortality rate.
Scopes and Criteria
The primary objective of this review is to describe the characteristics of postburn abdominal pain of gastrointestinal origin and its possible causative diseases depending on these characteristics, and to review the epidemiologic features of these diseases, narrate potential treatment methods and approaches, and lay down a differential diagnosis for postburn abdominal pain. The inclusion criteria comprised any study design, English language, and studies discussing postburn abdominal pain on human subjects. All the included papers were discussed narratively.
RESULTS
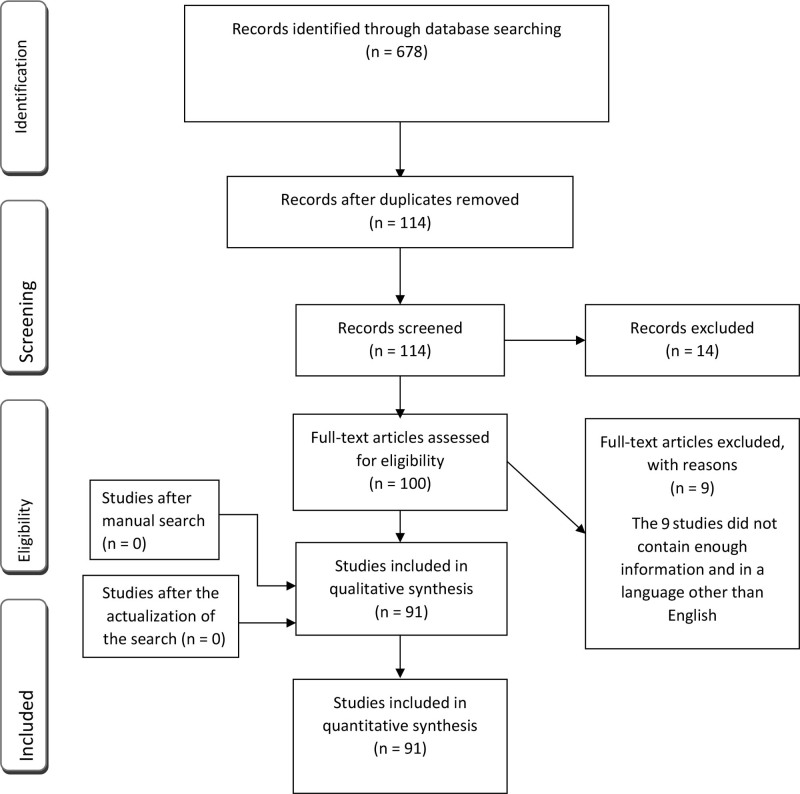
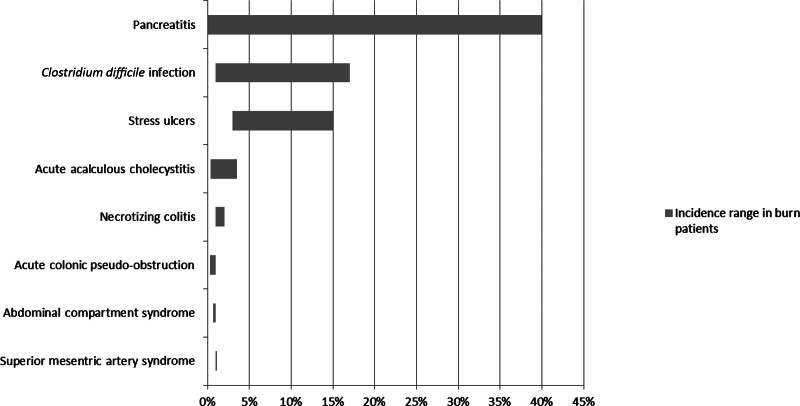
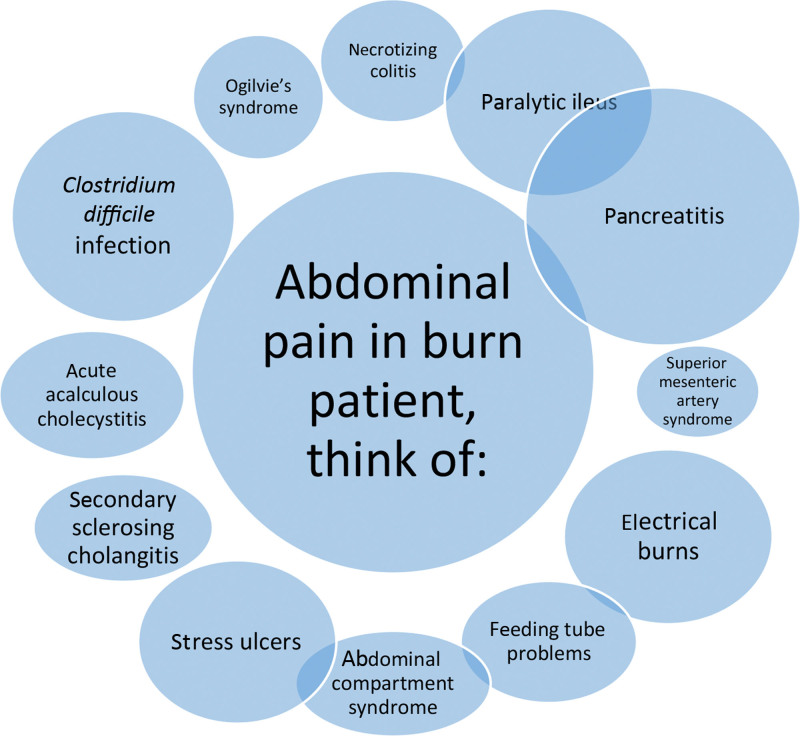
The selection process is explained by the PRISMA flow diagram (Fig. 1). The primary screening according to the suggested strategy identified 678 articles. After removing the similar or exact copies, there were 114 articles. According to our inclusion criteria, of them, 91 articles and reports were eligible for inclusion in this scoping review. We found that patients after burn injury may have abdominal pain due to several causes and etiologies such as (Fig. 2) pancreatitis (0.05%–40), superior mesenteric artery syndrome (SMAS) (1.1%), paralytic ileus, necrotizing colitis (1%–2%), acute colonic pseudo-obstruction (ACPO) (Ogilvie syndrome) (0.29%–1), C. difficile infection (1%–17%), acute acalculous cholecystitis (0.4%–3.5%), secondary sclerosing cholangitis complications, stress ulcers (1.5%–15), and abdominal compartment syndrome (ACS) (0.7%–1). In addition, it can also be due to feeding tube problems. Furthermore, abdominal pain can be a complication of electrical burns (5%–17.25%) and is also considered a common presenting symptom of nonocclusive mesenteric ischemia (NOMI) in patients with burn injury. Also, a few reports in the medical literature showed that sigmoid diverticulitis perforation and emphysema gastritis (EG) may be the cause of abdominal pain in patients with burn injuries. We will discuss in each entity the onset time, incidence rate, characteristics, etiology, and management. The most common possible options are presented in Figure 3.
Fig. 1.
PRISMA 2020 flow diagram explaining the selection process.
Fig. 2.
Incidence ranges of gastrointestinal complications in patients with burn injury.
Fig. 3.
Abdominal pain causes in patients with burn injury; a higher proportion gets a larger circle size.
DISCUSSION
Abdominal pain of gastrointestinal origin should not be overlooked in patients after burn injury, as it can be the leading symptom of a serious underlying disease. Herein, we are discussing the possible causes that can give rise to this symptom.
First, abdominal pain radiating to the back can be seen in postburn pancreatitis, as this complication occurs in 0.05%–40% of patients with burn injury (Fig. 2).1 Abdominal pain in acute pancreatitis in patients with burn injury may be associated with feeding intolerance, and a 3-fold increase of amylase and/or lipase, with radiologic signs of pancreatic edema.14 However, abdominal pain may be absent.15,16 Management varies from conservative measurements to surgery if complications occur.1,13 Mortality may occur in about 30% of cases.1
Abdominal pain can also be seen in stress ulcers secondary to systemic burns, known as Curling ulcers,5 with burn area of more than 20% TBSA.1,17,18 In typical cases, abdominal pain may be presented with coffee ground vomitus, hematemesis, melena, nausea, and orthostasis in severe cases. In general, the most common presentation is upper gastrointestinal bleeding, which ranges from 1.5% to 15%,5 depending on whether or not patients received prophylaxis such as proton pump inhibitors, early enteral nutrition, and fluid replacement, which decreased the occurrence of these ulcers from 15% to 3% (Fig. 2), besides a reduction in the mortality rate after it was up to 70%.1,19 Management for Curling ulcers is similar to the management of peptic ulcer disease in general, including the treatments just described, endoscopic control of bleeding, or even surgery.1,5
Moreover, abdominal pain is the most common presenting symptom of acute acalculous cholecystitis in patients with burn injuries.3 The incidence rate is between 0.4% and 3.5% (Fig. 2), with a male predominance.3 Mean burn surface area was 45% (22%–80%) according to Walsh et al3 and 37.4% ± 5% (6%–92%) according to Arnoldo et al.20 Mean age varied across multiple studies, the average of the reported mean ages is 40.3 years.3,21–25 The pathophysiology involves biliary stasis, systemic infection, ischemic injury, and the activation of the XII-factor-dependent pathways.3,25 Slight epigastric pain accompanied by reflex nausea, vomiting, and radiating to the upper quadrant should make burn specialists suspect acute acalculous cholecystitis.25 A palpable gallbladder and localized tenderness could also be present.26 According to Walsh et al3 only 14% of patients with burn injuries were reporting pain in the right upper quadrant. This disease can be complicated with perforation of the gallbladder, gangrenous cholecystitis, abscess, and empyema.26 Length of burn intensive care unit stay ranged from 63.4 to 97 days.21,26 Mortality varied from 14% to 53.3%.22,26 As might be expected, mortality following complications such as gangrene or perforation is as high as 65%.1 Ultrasound is the first choice of imaging modality.21 Treatment consists of initiation of antibiotics, and either cholecystectomy or placement of a cholecystostomy tube. Cholecystectomy is the conclusive treatment of acute acalculous cholecystitis in patients with burn injuries.1,21,27
In addition, right upper quadrant pain can be a prominent feature in patients after burn injury with secondary sclerosing cholangitis in critically ill patients (SSC-CIP).4 SSC-CIP is another newly described biliary complication caused by severe burns. Age and TBSA ranged from 18 to 56 years and from 35% to 95%, respectively.28 In the case series conducted by Ben-Ari et al28 on 4 patients, all patients were male and 2 patients (50%) died. The mean length of intensive care unit stay was 129.2 ± 53 days. SSC-CIP is likely caused by ischemic injury to the bile ducts followed by bacterial colonization.28 Diagnosis is based on magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography.28,29
Another disease with abdominal pain and postburn injuries is paralytic ileus, which is a decreased gastrointestinal motility due to Auerbach and Meissner plexuses failure, mainly caused by severe illness or surgery.1 Male gender and advanced age are considered risk factors.30 Davies et al31 revealed that its incidence increases when TBSA exceeds 20%. Usually, the onset of the disease starts 5 days after burn injury.32 Invasive treatment is not substantial, and conservative treatments such as nil per os and electrolyte balance are the gold standard.32 Unfortunately, the mortality rate could be more than 45%.33
Moreover, mild abdominal pain can also be encountered in ACPO in patients after burn injury.1 This medical condition is reported in only about 0.29% of burn cases, according to a study of 2703 patients with burn injury with ACPO34; 0.47%, according to a 5-year study of 422 patients with burn injury35; and 1%, according to Lescher et al36 (Fig. 2). TBSA has differed greatly among studies, with a minimum percentage of 7% in Kadesky et al34 and a maximum percentage of 83% in Estela et al.37 Also, according to John et al,38 TBSA percentages were lower in patients with obesity. The mean age is 63.5 ± 17.9 years (ranging from 27 to 82).34 This condition appears to be equal in incidence between men and women,38,39 although some data indicates that men can be more prone to this kind of injury.40–42 In all cases, the abdominal distention is always present. Abdominal pain is usually mild but when colonic dilation increases, it gets worse.36 The most serious complications are ischemia and colonic perforation. Also, in some cases, peritonitis can develop as a consequence of this perforation.43 The initial diagnosis is made by an x-ray that shows dilation in all colonic segments. On the other hand, barium enema can be useful in both confirming the diagnosis and treatment.41 Computed tomography (CT) is also effective in confirming the diagnosis, which shows dilation in colonic segments with no evidence of mechanical obstruction.44,45 Management is based initially on conservative treatments in noncomplicated ACPO.1 Some exceptions such as colonic perforation, peritonitis, and ischemia need urgent intervention, for that, surgical colostomy is recommended in such complications.1,38 According to Ross et al46 the overall mortality rate is 7.7%. According to Davies et al,31 it was 25%–35% in the absence of complications, and it increases to 50% when the perforation occurs. These mortality rates will rise in patients with burn injury.
Furthermore, in the case of SMAS in patients with burn injury, abdominal pain is postprandial and epigastric, and is characterized by its intermittent appearance.46 This symptom can be diminished by lying on the left side, in a prone or a knee–chest position.47,48 The supine position, structural abnormalities, and acute weight loss due to hypermetabolic states can all trigger SMAS by reducing the angle between the aorta and superior mesenteric artery. This acute angle, which ranges between 6 and 25 degrees, leads to a compressed duodenum in its third portion and to a chronic duodenal ileus.46,49 According to Elizabeth et al,47 in a normal state, the angle varies from 38 to 56 degrees. SMAS, which is more common in thin, young female patients, was seen in the age group of 33–43 years.46 SMAS is diagnosed by radiologic studies such as ultrasound, CT, fluoroscopic examination, and barium swallow.1 When diagnosed early, mortality rate becomes ignored.46 However, mortality increases in patients with burn injuries and could reach 30%.50 Herein, 2 studies revealed how many patients with burn injuries were admitted to the US Army Institute of Surgical Research during a specific time. In the first study, Lescher et al50 concluded that 37 of 3536 (1%) patients with burn injury developed SMAS in 12 years. In the second study, Kirksey et al51 reported that 19 of 1687 (1.1%) patients with burn injuries developed SMAS in 5 years (Fig. 2). The management of SMAS is usually conservative.51
Abdominal pain with diarrhea and fever can be associated with C. difficile infection in patients after burn injury.52 The incidence and the mean TBSA were, respectively, 1%–17% (Fig. 2) and 1%–77.5%.53,54 The mean age of the patients was 33.5 years old, with male predominance.54 The mortality rate was 28.5%.54 Prolonged hospital admission, proton pump inhibitors, immunosuppressants, the indicated surgery, nasogastric tubes, and broad coverage antibiotics can change bacterial flora of the gut, which predisposes the disease.52,54,55 The most causative medications for this disease are ampicillin, cephalosporine, and clindamycin.55 Silver sulfadiazine may be the cause in rare cases.56 Enzyme-linked immunosorbent assay and stool samples can detect the pathogenic agent of the disease.1,55 Colonoscopy can be diagnostic and therapeutic by colonic decompression.55 Metronidazole is the drug of choice for the treatment.52
Abdominal pain may also be a consequence of necrotizing colitis in patients with burn injury.57 Postburn necrotizing colitis is not common (1%–2%) (Fig. 2), but it is a fatal complication with severe burns with a 75% mortality rate.58,59 Most patients with postburn necrotizing colitis are middle-aged with male predominance and TBSA of 20%–98%.60,61 In addition to abdominal pain, patients can have rectal bleeding.58 Necrotizing colitis can present at any time of the postburn period.59,62 The duration of hospitalization was 55 ± 15 days.60 Increased TBSA, systemic sepsis, vasoconstriction, ileus, vasopressor agents, resuscitation fluids, and postburn pancreatitis are all associated with an increased risk of necrotizing colitis.57–59,61–64 Colonoscopy and computerized tomography are the most important diagnostic procedures.59,64 Bowel rest and nasogastric tube are the initial steps of treatment.64 Patients with no symptoms should undergo conservative management such as oxygen and antibiotics.64 Surgery should be done when patients present with serious symptoms.64
In addition, abdominal pain can also be a prominent feature of ACS in patients after burn injury. This pain may precede the evolution of ACS, which is defined as an intra-abdominal pressure (IAP) more than 20 mmHg and recent organ failure.65 This complaint results from the rising of IAP, which interrupts gut perfusion.6,65,66 The incidence of ACS is unclear yet, whereas Steven showed that it increases proportionally with the depth and the size of the burned area (TBSA).67 Aron reveals that it was 0.7%–1% in adult patients with burn injury (Fig. 2) and may be higher in children.68 Moreover, it was found that children were predisposed to develop ACS at a lower IAP.69 ACS often occurs within the first 12 hours of presentation.68 According to Hobson, almost all ACS patients were males, and the mean age was 48, ranging between 29 and 79 years.70 The TBSA ranged from 22% to 80%.71–73 Ivy et al71 recommended bladder pressure measurement when peak inspiratory pressure is more than 40 cm H2O and fluid resuscitation is more than 0.25 L/kg. When diagnosed, sedation, chemical paralysis, and escharotomy should be performed.71 Decompressive laparotomy is the most frequent procedure, and percutaneous drainage is also recommended; despite that, mortality ranges from 70% to 100%.74,75
Furthermore, abdominal pain can also be associated with the usage of feeding tubes in patients after burn injury. The most common findings are diarrhea and vomiting.76–81 In addition, these feeding tubes can also increase the risk of C. difficile infection, which can lead to pseudomembranous colitis.7
According to Shih et al,82 abdominal pain can also be a feature of electrical burn injury, with an incidence of less than 5% of burn injuries. Another study of 182 patients with electrical burn injury reveals an incidence of 17.25%.83,84 High-voltage injuries can cause abdominal pain in several etiologies, including visceral perforation, which is not a common complication,9 paralytic ileus, Curling ulcer, pancreatic injury,10 and Henoch-Schönlein purpura, which is reported to be an extremely rare condition.11 Abdominal pain from visceral perforation due to low-voltage injury is rarely described in the literature.85 It is unusual for abdominal complications to be a presentation of electrical injuries, but it should be considered if digestive symptoms develop.85
Also, patients with burn injuries are at risk of developing serious intestinal complications due to reduced blood flow to the abdominal organs.86,87 NOMI is the most frequent cause of gastrointestinal infarction.86 Abdominal pain is a common presenting symptom of NOMI in patients with burn injury and should prompt immediate evaluation and intervention. Treatment involves aggressive resuscitation with intravenous fluids and correction of any electrolyte abnormalities. In some cases, surgical intervention may be necessary to revascularize the affected bowel or remove necrotic tissue.86
In addition, others described cases of abdominal pain in patients with burn injury with sigmoid diverticulitis perforation, which developed later during their hospital stay.87 Finally, some authors have also reported a case of EG in a patient with burn injury who presented with severe abdominal pain.88 Diagnosis of EG, a rare, life-threatening condition in patients with burn injury, can be challenging due to the overlap of symptoms with other gastrointestinal complications commonly seen in patients with burn injury. Imaging studies such as CT scans can help confirm the diagnosis.88
Consequently, the abdominal pain in patients with burn injury may be a reflection of a serious medical condition, so the diagnosis is accurate and made on time, and the patients with burn injuries have the best opportunity for positive outcomes. Moreover, we see that the abdominal pain in patients with burn injury represents an overlapping entity in many specialties, and this emphasizes the important role of a multidisciplinary team in burn management.89–91
CONCLUSIONS
Early recognition of postburn abdominal pain as well as the timely diagnosis and treatment play a significant role in prognosis and mortality. Thus, it is extremely important for burn specialists and plastic surgeons to thoroughly investigate postburn abdominal pain. In addition, one of the aims of this review was to shed light on the important role of the multidisciplinary team in burn patient management to improve the prognosis, as this abdominal pain in patients with burn injury represents an overlapping entity in many specialties.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 13 November 2024.
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Lopez ON, Bohanon FJ, Radhakrishnan RS, et al. Surgical management of complications of burn injury. In Herndon DN. (ed.): Total Burn Care (5th ed.). Elsevier; 2018:386–395.e3. [Google Scholar]
- 2.Flasar MH, Cross R, Goldberg E. Acute abdominal pain. Prim Care. 2006;33:659–684. [DOI] [PubMed] [Google Scholar]
- 3.Walsh K, Goutos I, Dheansa B. Acute acalculous cholecystitis in burns: a review. J Burn Care Res. 2018;39:724–728. [DOI] [PubMed] [Google Scholar]
- 4.Leonhardt S, Veltzke-Schlieker W, Adler A, et al. Secondary sclerosing cholangitis in critically Ill patients: clinical presentation, cholangiographic features, natural history, and outcome: a series of 16 cases. Medicine (Baltim). 2015;94:e2188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siddiqui AH, Farooq U, Siddiqui F. Curling Ulcer. Treasure Island, FL: StatPearls Publishing; 2024. [Updated April 16, 2023]. Available at https://www.ncbi.nlm.nih.gov/books/NBK482347/. Accessed October 19, 2024. [PubMed] [Google Scholar]
- 6.Hershberger RC, Hunt JL, Arnoldo BD, et al. Abdominal compartment syndrome in the severely burned patient. J Burn Care Res. 2007;28:708–714. [DOI] [PubMed] [Google Scholar]
- 7.Wang D, Dong D, Wang C, et al. Risk factors and intestinal microbiota: Clostridioides difficile infection in patients receiving enteral nutrition at intensive care units. Crit Care. 2020;24:426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014;20:8505–8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller FE, Peterson D, Miller J. Abdominal visceral perforation secondary to electrical injury: case report and review of the literature. Burns Incl Therm Inj. 1986;12:505–507. [DOI] [PubMed] [Google Scholar]
- 10.Vande Ven H. Electrical burn injuries. Medscape.com. 2021. Available at: https://emedicine.medscape.com/article/1277496-overview. Accessed October 23, 2023. [Google Scholar]
- 11.Duan X, Yu D, Yu C, et al. Henoch-Schönlein purpura following high-voltage electric burn injury: a case report and review of the literature. Exp Ther Med. 2016;11:540–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams FN, Lee JO. Chemical burns. In Herndon DN. (ed.): Total Burn Care (5th ed.). Elsevier; 2018:408-413.e1. [Google Scholar]
- 13.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin Res Ed.). 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rivero HG, Lee JO, Herndon DN, et al. The role of acute pancreatitis in pediatric burn patients. Burns. 2011;37:82–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson MD, Sugden P, Durrani A, et al. Acute pancreatitis complicating 50% full-thickness burns in a 5-year-old child. Burns. 2003;29:619–621. [DOI] [PubMed] [Google Scholar]
- 16.Drewes AM, Bouwense SAW, Campbell CM, et al. ; Working Group for the International (IAP–APA–JPS–EPC) Consensus Guidelines for Chronic Pancreatitis. Guidelines for the understanding and management of pain in chronic pancreatitis. Pancreatology. 2017;17:720–731. [DOI] [PubMed] [Google Scholar]
- 17.Choi YH, Lee JH, Shin JJ, et al. A revised risk analysis of stress ulcers in burn patients receiving ulcer prophylaxis. Clin Exp Emerg Med. 2015;2:250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Battal MN, Hata Y, Matsuka K, et al. Effect of a prostaglandin I2 analogue, beraprost sodium, on burn-induced gastric mucosal injury in rats. Burns. 1997;23:232–237. [DOI] [PubMed] [Google Scholar]
- 19.Raff T, Germann G, Hartmann B. The value of early enteral nutrition in the prophylaxis of stress ulceration in the severely burned patient. Burns. 1997;23:313–318. [DOI] [PubMed] [Google Scholar]
- 20.Arnoldo BD, Hunt JL, Purdue GF. Acute cholecystitis in burn patients. J Burn Care Res. 2006;27:170–173. [DOI] [PubMed] [Google Scholar]
- 21.Hermiz SJ, Diegidio P, Garimella R, et al. Acalculous cholecystitis in burn patients: is there a role for percutaneous cholecystostomy? Clin Plast Surg. 2017;44:567–571. [DOI] [PubMed] [Google Scholar]
- 22.McClain T, Gilmore BT, Peetz M. Laparoscopic cholecystectomy in the treatment of acalculus cholecystitis in patients after thermal injury. J Burn Care Rehabil. 1997;18:141–146. [DOI] [PubMed] [Google Scholar]
- 23.Munster AM, Goodwin MN, Pruitt BA, Jr. Acalculous cholecystitis in burned patients. Am J Surg. 1971;122:591–593. [DOI] [PubMed] [Google Scholar]
- 24.Alawneh I. Acute non-calculous cholecystitis in burns. Br J Surg. 1978;65:243–245. [DOI] [PubMed] [Google Scholar]
- 25.Castana O, Rempelos G, Anagiotos G, et al. Acute acalculous cholecystitis: a rare complication of burn injury. Ann Burns Fire Disasters. 2009;22:48–50. [PMC free article] [PubMed] [Google Scholar]
- 26.Theodorou P, Maurer CA, Spanholtz TA, et al. Acalculous cholecystitis in severely burned patients: incidence and predisposing factors. Burns. 2009;35:405–411. [DOI] [PubMed] [Google Scholar]
- 27.Chen X, Wang Q, Li F. Incomplete duodenal obstruction caused by cholecystitis in an extensive burn patient. Chin Med J (Engl). 2019;132:1241–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ben-Ari Z, Levingston D, Weitzman E, et al. Secondary sclerosing cholangitis following major burn. Ann Hepatol. 2015;14:695–701. [PubMed] [Google Scholar]
- 29.Ruemmele P, Hofstaedter F, Gelbmann CM. Secondary sclerosing cholangitis. Nat Rev Gastroenterol Hepatol. 2009;6:287–295. [DOI] [PubMed] [Google Scholar]
- 30.Venara A, Neunlist M, Slim K, et al. Postoperative ileus: pathophysiology, incidence, and prevention. J Visc Surg. 2016;153:439–446. [DOI] [PubMed] [Google Scholar]
- 31.Davies MP, Ward DJ. Long-term gastrointestinal problems in burns patients. Burns. 1993;19:423–425. [DOI] [PubMed] [Google Scholar]
- 32.Weledji EP. Perspectives on paralytic ileus. Acute Med Surg. 2020;7:e573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pishgar M, Razo M, Theis J, et al. Process mining model to predict mortality in paralytic ileus patients. ArXiv [Cs.LG]. 2021. [Google Scholar]
- 34.Kadesky K, Purdue GF, Hunt JL. Acute pseudo-obstruction in critically ill patients with burns. J Burn Care Rehabil. 1995;16:132–135. [DOI] [PubMed] [Google Scholar]
- 35.Tsoutsos D, Tsakou EG, Lykoudis E, et al. Acute colonic pseudo-obstruction (Ogilvie’s syndrome): a rare complication of severe thermal injury. Report on two cases. Medbc.com. 1999;XII. Published June 1999. Available at http://www.medbc.com/annals/review/vol_12/num_2/text/vol12n2p88.htm. Accessed July 29, 2022. [Google Scholar]
- 36.Lescher TJ, Teegarden DK, Pruitt BA, Jr. Acute pseudo-obstruction of the colon in thermally injured patients. Dis Colon Rectum. 1978;21:618–622. [DOI] [PubMed] [Google Scholar]
- 37.Estela CM, Burd DA. Conservative management of acute pseudo-obstruction in a major burn. Burns. 1999;25:523–525. [DOI] [PubMed] [Google Scholar]
- 38.John AA, Anand R, Frost J, et al. Acute colonic pseudo-obstruction: a critical complication in burn patients. Burns Open. 2022;6:37–41. [Google Scholar]
- 39.Cagir B. Intestinal pseudo-obstruction. Medscape.com; 2022. Available at: https://emedicine.medscape.com/article/2162306-overview. Updated July 23, 2018. Accessed October 23, 2023. [Google Scholar]
- 40.Tsirline VB, Zemlyak AY, Avery MJ, et al. Colonoscopy is superior to neostigmine in the treatment of Ogilvie’s syndrome. Am J Surg. 2012;204:849–855; discussion 855. [DOI] [PubMed] [Google Scholar]
- 41.Ives A, Muller M, Pegg S. Colonic pseudo-obstruction in burns patients. Burns. 1996;22:598–601. [DOI] [PubMed] [Google Scholar]
- 42.Vanek VW, Al-Salti M. Acute pseudo-obstruction of the colon (Ogilvie’s syndrome): an analysis of 400 cases. Dis Colon Rectum. 1986;29:203–210. [DOI] [PubMed] [Google Scholar]
- 43.Valero Gasalla J, Vazquez-Barro A, Pousa Real F, et al. Acute colonic pseudo-obstruction in a burn patient. Burns. 1993;19:538–540. [DOI] [PubMed] [Google Scholar]
- 44.Choi JS, Lim JS, Kim H, et al. Colonic pseudoobstruction: CT findings. AJR Am J Roentgenol. 2008;190:1521–1526. [DOI] [PubMed] [Google Scholar]
- 45.Gebre-Giorgis AA, Roderique EJD, Stewart D, et al. Neostigmine to relieve a suspected colonic pseudo-obstruction in a burn patient: a case-based review of the literature. Eplasty. 2013;13:e1. [PMC free article] [PubMed] [Google Scholar]
- 46.Ross DC, Lee KC, Peters WJ, et al. Acalculous cholecystitis in association with major burns. Burns Incl Therm Inj. 1987;13:488–491. [DOI] [PubMed] [Google Scholar]
- 47.Clinical case. Superior mesenteric artery (SMA) syndrome. Medscape.com; 2021. Available at https://emedicine.medscape.com/article/932220-overview. Updated October 10, 2024. Accessed October 29, 2024. [Google Scholar]
- 48.Milner EA, Cioffi WG, McManus WF, et al. Superior mesenteric artery syndrome in a burn patient. Nutr Clin Pract. 1993;8:264–266. [DOI] [PubMed] [Google Scholar]
- 49.Neri S, Signorelli SS, Mondati E, et al. Ultrasound imaging in diagnosis of superior mesenteric artery syndrome: diagnosis of SMA syndrome. J Intern Med. 2005;257:346–351. [DOI] [PubMed] [Google Scholar]
- 50.Lescher TJ, Sirinek KR, Pruitt BA, Jr. Superior mesenteric artery syndrome in thermally injured patients. J Trauma. 1979;19:567–571. [DOI] [PubMed] [Google Scholar]
- 51.Kirksey TD, Moncrief JA, Pruitt BA, Jr, et al. Gastrointestinal complications in burns. Am J Surg. 1968;116:627–633. [DOI] [PubMed] [Google Scholar]
- 52.Reckler JM, Bruck HM, Munster AM, et al. Superior mesenteric artery syndrome as a consequence of burn injury. J Trauma. 1972;12:979–985. [DOI] [PubMed] [Google Scholar]
- 53.Finnerty CC, Herndon DN, Lee JO, et al. Morbidity and mortality in severely burned children with Clostridium difficile-associated diarrhea. Surgery. 2016;159:1631–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alinejad F, Barati M, Tabrisi MS, et al. Hospital acquired diarrhea in a burn center of Tehran. Iran J Microbiol. 2015;7:310. [PMC free article] [PubMed] [Google Scholar]
- 55.Crabtree SJ, Robertson JL, Chung KK, et al. Clostridium difficile infections in patients with severe burns. Burns. 2011;37:42–48. [DOI] [PubMed] [Google Scholar]
- 56.Jennings LJ, Hanumadass M. Silver sulfadiazine induced Clostridium difficile toxic megacolon in a burn patient: a case report. Burns. 1998;24:676–679. [DOI] [PubMed] [Google Scholar]
- 57.Osuka A, Sugenoya S, Onishi S, et al. Acute pancreatitis and necrotizing colitis following extensive burn injury. Acute Med Surg. 2016;3:283–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Soussi S, Taccori M, De Tymowski C, et al. ; PRONOBURN Group. Risk factors for acute mesenteric ischemia in critically ill burns patients: a matched case-control study. Shock. 2019;51:153–160. [DOI] [PubMed] [Google Scholar]
- 59.Meares C, Liang D, Wijewardena A, et al. Massive bowel infarction in a severe burn patient: a case report. Australian and New Zealand Burn Association, Annual Scientific Meeting; October2019. Available at https://anzbaasm.com/wp-content/uploads/2019/10/Charles-Meares-ANZBA2019_Meares_Charles-Infarction.pdf. Accessed October 19, 2024. [Google Scholar]
- 60.Kowal-Vern A, McGill V, Gamelli RL. Ischemic necrotic bowel disease in thermal injury. Arch Surg. 1997;132:440–443. [DOI] [PubMed] [Google Scholar]
- 61.Fadel MG, Iskandarani M, Cuddihy J, et al. Colonic perforation following major burns: experience from a burns center and a systematic review. Burns. 2021;47:1241–1251. [DOI] [PubMed] [Google Scholar]
- 62.Markell KW, Renz EM, White CE, et al. Abdominal complications after severe burns. J Am Coll Surg. 2009;208:940–947; discussion 947. [DOI] [PubMed] [Google Scholar]
- 63.Andres LA, Ford RD, Wilcox RM. Necrotizing colitis caused by systemic aspergillosis in a burn patient. J Burn Care Res. 2007;28:918–921. [DOI] [PubMed] [Google Scholar]
- 64.Balledux J, McCurry T, Zieger M, et al. Pneumatosis intestinalis in a burn patient: case report and literature review. J Burn Care Res. 2006;27:399–403. [DOI] [PubMed] [Google Scholar]
- 65.Kirkpatrick AW, Ball CG, Nickerson D, et al. Intraabdominal hypertension and the abdominal compartment syndrome in burn patients. World J Surg. 2009;33:1142–1149. [DOI] [PubMed] [Google Scholar]
- 66.Burke BA, Latenser BA. Defining intra-abdominal hypertension and abdominal compartment syndrome in acute thermal injury: a multicenter survey. J Burn Care Res. 2008;29:580–584. [DOI] [PubMed] [Google Scholar]
- 67.Breederveld RS, Van Waes OJF. A systematic review on intra-abdominal pressure in severely burned patients. Burns. 2014a;40:9–16. [DOI] [PubMed] [Google Scholar]
- 68.Jensen AR, Hughes WB, Grewal H. Secondary abdominal compartment syndrome in children with burns and trauma: a potentially lethal complication. J Burn Care Res. 2006;27:242–246. [DOI] [PubMed] [Google Scholar]
- 69.Newcombe J, Mathur M, Ejike JC. Abdominal compartment syndrome in children. Crit Care Nurse. 2012;32:51–61. [DOI] [PubMed] [Google Scholar]
- 70.Hobson KG, Young KM, Ciraulo A, et al. Release of abdominal compartment syndrome improves survival in patients with burn injury. J Trauma. 2002;53:1129–1133; discussion 1133. [DOI] [PubMed] [Google Scholar]
- 71.Ivy ME, Atweh NA, Palmer J, et al. Intra-abdominal hypertension and abdominal compartment syndrome in burn patients. J Trauma. 2000;49:387–391. [DOI] [PubMed] [Google Scholar]
- 72.Kollias S, Stampolidis N, Kourakos P, et al. Abdominal compartment syndrome (ACS) in a severely burned patient. Ann Burns Fire Disasters. 2015;28:5–8. [PMC free article] [PubMed] [Google Scholar]
- 73.Tanaka H, Matsuda T, Miyagantani Y, et al. Reduction of resuscitation fluid volumes in severely burned patients using ascorbic acid administration: a randomized, prospective study. Arch Surg. 2000;135:326–331. [DOI] [PubMed] [Google Scholar]
- 74.Oda J, Ueyama M, Yamashita K, et al. Hypertonic lactated saline resuscitation reduces the risk of abdominal compartment syndrome in severely burned patients. J Trauma. 2006;60:64–71. [DOI] [PubMed] [Google Scholar]
- 75.Tuggle D, Skinner S, Garza J, et al. The abdominal compartment syndrome in patients with burn injury. Acta Clin Belg. 2007;62:136–140. [PubMed] [Google Scholar]
- 76.McWey RE, Curry NS, Schabel SI, et al. Complications of nasoenteric feeding tubes. Am J Surg. 1988;155:253–257. [DOI] [PubMed] [Google Scholar]
- 77.McDonald WS, Sharp CW, Jr, Deitch EA. Immediate enteral feeding in burn patients is safe and effective. Ann Surg. 1991;213:177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hiebert JM, Brown A, Anderson RG, et al. Comparison of continuous vs intermittent tube feedings in adult burn patients. JPEN J Parenter Enteral Nutr. 1981;5:73–75. [DOI] [PubMed] [Google Scholar]
- 79.Numata Y, Ishii K, Seki H, et al. Perforation of abdominal esophagus following nasogastric feeding tube intubation: a case report. Int J Surg Case Rep. 2018;45:67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shah R, Shah M, Aleem A. Gastrostomy Tube Replacement. Treasure Island, FL: StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK482422/. Updated April 17, 2023. Accessed October 19, 2024. [PubMed] [Google Scholar]
- 81.Shahbani DK, Goldberg R. Peritonitis after gastrostomy tube replacement in the emergency department. J Emerg Med. 2000;18:45–46. [DOI] [PubMed] [Google Scholar]
- 82.Shih JG, Shahrokhi S, Jeschke MG. Review of adult electrical burn injury outcomes worldwide: an analysis of low-voltage vs high-voltage electrical injury. J Burn Care Res. 2017;38:e293–e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Buja Z, Arifi H, Hoxha E. Electrical burn injuries. An eight-year review. Ann Burns Fire Disasters. 2010;23:4–7. [PMC free article] [PubMed] [Google Scholar]
- 84.Ding H, Huang M, Li D, et al. Epidemiology of electrical burns: a 10-year retrospective analysis of 376 cases at a burn centre in South China. J Int Med Res. 2020;48:300060519891325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Singh AP, Mathur V, Tanger R, et al. Low voltage electric current causing ileal perforation: a rare injury. APSP J Case Rep. 2016;7:17. [PMC free article] [PubMed] [Google Scholar]
- 86.Muschitz GK, Alexandra F, Maike K, et al. Non-occlusive mesenteric ischaemia: the prevalent cause of gastrointestinal infarction in patients with severe burn injuries. Injury. 2015;46:124–130. [DOI] [PubMed] [Google Scholar]
- 87.Cirodde A, Jault P, Leclerc T, et al. Sigmoid diverticulitis perforation in burns: case reports and review of the literature. Ann Burns Fire Disasters. 2012;25:22–25. [PMC free article] [PubMed] [Google Scholar]
- 88.Carlson AP, Jennifer WHC, Ketai LH, et al. Emphysematous gastritis in a severely burned patient: case report and literature review. J Trauma. 2007;62:765–767. [DOI] [PubMed] [Google Scholar]
- 89.Herndon DN. Introduction: the multidisciplinary team approach to burn care. Surg Clin North Am. 2023;103:369–376. [DOI] [PubMed] [Google Scholar]
- 90.Al Khalfan AA, Al Ghamdi AA, De Simone S, et al. The impact of multidisciplinary team care on decreasing intensive care unit mortality. Saudi Crit Care J. 2021;5:13–18. [Google Scholar]
- 91.Win TS, Nizamoglu M, Maharaj R, et al. Relationship between multidisciplinary critical care and burn patients survival: A propensity-matched national cohort analysis. Burns. 2018;44:57–64. [DOI] [PubMed] [Google Scholar]