Abstract
BACKGROUND
E-cigarettes are promoted as less harmful than cigarettes. There has not been a direct comparison of health effects of e-cigarettes or dual use (concurrently using e-cigarettes and cigarettes) with those of cigarettes in the general population.
METHODS
Studies in PubMed, EMBASE, Web of Science, and PsychINFO published through October 1, 2023, were pooled in a random-effects meta-analysis if five or more studies were identified with a disease outcome. We assessed risk of bias with Risk Of Bias In Non-randomized Studies of Exposure and certainty with Grading of Recommendations, Assessment, Development, and Evaluations. Outcomes with fewer studies were summarized but not pooled.
RESULTS
We identified 124 odds ratios (94 cross-sectional and 30 longitudinal) from 107 studies. Pooled odds ratios for current e-cigarette versus cigarette use were not different for cardiovascular disease (odds ratio, 0.81; 95% confidence interval, 0.58 to 1.14), stroke (0.73; 0.47 to 1.13), or metabolic dysfunction (0.99; 0.91 to 1.09) but were lower for asthma (0.84; 0.74 to 0.95), chronic obstructive pulmonary disease (0.53; 0.38 to 0.74), and oral disease (0.87; 0.76 to 1.00). Pooled odds ratios for dual use versus cigarettes were increased for all outcomes (range, 1.20 to 1.41). Pooled odds ratios for e-cigarettes and dual use compared with nonuse of either product were increased (e-cigarette range, 1.24 to 1.47; dual use, 1.49 to 3.29). All studies included were assessed as having a low risk of bias. Results were generally not sensitive to study characteristics. Limited studies of other outcomes suggest that e-cigarette use is associated with additional diseases.
CONCLUSIONS
There is a need to reassess the assumption that e-cigarette use provides substantial harm reduction across all cigarette-caused diseases, particularly accounting for dual use.
Introduction
The 2018 National Academies of Science, Engineering and Medicine report Public Health Consequences of E-Cigarettes concluded that “whether e-cigarettes have an overall positive or negative impact on public health is currently unknown.”1 Public Health England’s 2015 report concluded that e-cigarettes are 95% safer than cigarettes based on the fact that e-cigarettes do not produce combustion products.2 An umbrella review using a literature search through July 2020 found the evidence for most disease outcomes “insufficient.”3 As of October 2023, however, many epidemiological studies had reported the odds of human disease associated with e-cigarettes as actually used in the general population. Meta-analyses found increased odds of asthma4–6 and chronic obstructive pulmonary disease5 (COPD) associated with e-cigarette use independent of cigarette use. There have not been meta-analyses of other disease outcomes, although three meta-analyses found that e-cigarettes adversely affected cardiovascular function7–9 and one found negative effects on dental implants.10 One qualitative summary of six studies concluded that switching completely from cigarettes to e-cigarettes was associated with lower odds of respiratory disease and no change in cardiovascular disease.11 Another study concluded that dual (concurrent) use of e-cigarettes and cigarettes was associated with odds of disease that were the same as or higher than those found with exclusive smoking.12
Some regulatory bodies continue to assume that e-cigarettes are substantially less toxic than cigarettes. In its 2022 proposed rule ending menthol as a characterizing flavor in cigarettes,13 following Levy et al.14 the U.S. Food and Drug Administration (FDA) assumed that e-cigarettes are 15% as toxic as cigarettes and dual use had risks similar to those of smoking. No specific evidence is cited to support these assumptions. FDA’s marketing granted orders for RJ Reynolds’ Vuse Solo15,16 and other e-cigarettes17,18 assuming that e-cigarettes are substantially less harmful than cigarettes based on the fact that many biomarkers of exposure or potential harm are lower in e-cigarette users than in users of cigarettes and are similar to those in smokers who are dual users.19
A 2021 review and modeling analysis of biomarker data estimated that e-cigarettes were one-third as harmful as cigarettes.20 Another review of biomarkers in clinical trials of e-cigarettes for smoking cessation in high-income countries concluded that switching from cigarettes to e-cigarettes or dual use reduced some biomarkers of potential harm.21 The number of biomarkers in these analyses was small compared with the number of toxicants in cigarettes and e-cigarettes. E-cigarettes and conventional cigarettes are different products. Research has focused on known cigarette-related toxicants (largely combustion products that are not present or present at much lower levels in e-cigarettes) even though e-cigarettes also deliver thousands of chemicals and have a toxicant profile different from that of cigarettes.22 In addition, the dose–response relationships between exposure and risk may not be linear, which means that a reduction in measures of exposure may not translate into proportionate reductions in harm. Consistent with a nonlinear dose–response, a meta-analysis of the effects of reducing cigarette consumption found no all-cause mortality benefit.23 Another study found that smoking one cigarette a day generates about 53% of the risk of coronary heart disease for men and 38% for women and 64% of the risk of stroke for men and 36% for women compared with smoking 20 cigarettes a day.24
Since e-cigarettes are often presented as a less harmful alternative to cigarettes,2,13–18 the comparison of most interest for potential harm reduction for smokers is comparison of e-cigarettes to cigarettes. In addition, many adult e-cigarette users continue to smoke cigarettes (dual use); 39.1% of U.S. e-cigarette users in 2018 to 2019,25 66.7% in Sweden in 2016,26 and 85.3% in Korea in 2013 to 201727 were dual users, making it important to compare the odds of disease associated with dual use to those found with exclusive cigarette use. In addition, the high prevalence of e-cigarette use among youth who have never smoked cigarettes28,29 makes it important to quantify the risks of e-cigarette use compared with nonuse.
This study provides a systematic review and meta-analysis of the associations between current e-cigarette use and dual use and disease outcomes in the general population compared with cigarette use and compared with not using either product.
Methods
This research was conducted following the Meta-analysis Of Observational Studies in Epidemiology reporting guidelines and registered with PROSPERO (CRD42022357914).
DATA
Study Identification
We searched PubMed, EMBASE, Web of Science, and PsychINFO for articles published from January 1, 2005 (before e-cigarettes entered the U.S. market), through October 1, 2023, for population epidemiological studies that reported the association between e-cigarette use as consumer products in the general population and diseases with no geographic or language restrictions. See Supplementary Methods in the Supplementary Appendix for specific searches, inclusion and exclusion criteria, and the data extraction protocol provided with the full text of this article at evidence.nejm.org. Diseases with at least five articles were used for quantitative meta-analysis; other outcomes were qualitatively summarized.
Exposure Definitions
Current e-cigarette users self-reported using e-cigarettes some days or every day or 1day or more during the past 30days.
Current smokers self-reported having smoked 100 cigarettes in their lifetime and smoking some days or every day or 1 day or more during the past 30 days.
Current dual users were current users of both e-cigarettes and cigarettes.
Disease Outcomes
Disease outcomes were self-reported diagnoses, using questions such as “Has a doctor, nurse, or other health professional told you that you had ___?” or identified through direct clinical observation such as NHANES (National Health and Nutrition Evaluation Survey).30 Disease was categorized as “current” (diagnosis within the last 12 months or less) or “ever.”
ASSESSMENT OF RISK OF BIAS AND CERTAINTY OF CONCLUSIONS
Two reviewers used the Risk Of Bias In Non-randomized Studies of Exposure (ROBINS-E) to assess risk of bias in individual studies31 and Grading of Recommendations, Assessment, Development, and Evaluations32 (GRADE) to assess confidence in conclusions. Differences were resolved by consensus.
ANALYSIS
We computed pooled odds ratios of each disease outcome for e-cigarettes and dual use compared with cigarettes as well as nonuse (never or noncurrent use). When articles reported relative risk, prevalence ratio, hazard ratio, or incident rate ratio, we used it as an estimate of odds ratio.33 When an article did not report odds ratios of e-cigarette use versus cigarette use (ORecig versus cig) and odds ratios of dual use versus cigarette use (ORdual versus cig), we calculated these odds ratios as detailed in Supplementary Methods.
Primary Analysis
The odds ratios and 95% confidence intervals (CIs) were pooled using random effects meta-analyses with Stata 15.1 metan. The CIs have not been adjusted for multiple comparisons. When more than one article used the same data set, we inflated the standard errors for the individual estimates using a Bonferroni correction to account for the likelihood that odds ratio estimates were correlated (details in Supplementary Methods).
Because some e-cigarette users continue to smoke, we estimated the overall odds of disease associated with e-cigarette use accounting for dual use compared with the cigarettes alone using a Monte Carlo analysis (see Supplementary Methods).
Sensitivity Analyses
We conducted sensitivity analyses to examine whether study characteristics (e.g., design, samples, control for former smoking, and last year of data collection) affected the results34,35 with meta-regression using Stata metareg of the natural logarithm of the odds ratios against study characteristics, controlling for the outcome. We tested whether treating all measures of associations (e.g., relative risk and hazard ratio) as approximations of odds ratios affected the results by repeating the meta-analyses among only studies that reported odds ratios.
Heterogeneity
The sample sizes in the individual studies were large, so I2 and the chi-squared test are not good measures of heterogeneity.34 Heterogeneity across studies for particular disease outcomes was assessed in two ways: using meta-regression with effects-coded differences in detailed outcomes within disease categories and examining whether holding one study out substantially changed the meta-analyses of the remaining studies and assessment of forest plots.35
Publication Bias
Publication bias was assessed using funnel plots and Begg, Egger, and trim-and-fill tests with Stata’s metafunnel, metabias, and metatrim.
ETHICS
Ethical approval was not required for this review of published studies. S.A.G. designed the study, did the analysis, and wrote the first draft. All authors participated in data gathering and revising the manuscript and take responsibility for the integrity of the data and the accuracy of the data analysis.
Results
STUDY SELECTION
We identified 107 studies26,27,36–140 (Tables S1–S3 in the Supplementary Appendix; PRISMA flowchart: Fig. S1). Over three-fourths (84/107) were published from 2020 to 2023. Most were based on large U.S. nationally representative surveys (PATH141 [Population Assessment of Tobacco and Health], 39; BFRSS142 [Behavioral Risk Factor Surveillance System], 28; NHANES30, 8; PRAMS143 [Pregnancy Risk Assessment Monitoring System], 5; NHIS144 [National Health Interview Survey], 9; YRBSS145 [Youth Risk Behavior Surveillance System], 3). The rest were from other U.S. surveys (15) or national surveys out-side the United States (Korea, 10; Sweden, 2; China, 1; Kuwait, 1). The sample sizes were large, ranging from 976 to 924,882 (median, 21,618; interquartile range, 9204 to 85,810). Most (88/107 [82%]) reported odds ratios. Four102,103,108,119 (4%) reported relative risks, nine46,62,63,72,76,88,101,109,112 (8%) reported hazard ratios, five36,38,53,71,107 (4%) reported prevalence ratios, and one135 (1%) reported incidence rate ratios.
There were at least 5 studies of the following disease outcomes: 12 of cardiovascular disease (coronary heart disease, erectile dysfunction, or myocardial infarction), 6 of stroke, 12 of metabolic dysfunction (metabolic syndrome and its components: obesity, hypertension, high blood sugar [prediabetes], high serum triglycerides, and low serum high-density lipoprotein), 42 of asthma, 20 of COPD, and 10 of oral disease (poor oral health, gum disease [gingivitis, periodontitis], tooth cracking or loss, and xerostomia). We found 22 studies of other conditions that were summarized without pooling odds ratios: preterm birth,75,107,127 low gestational weight gain,129 not breastfeeding,89 coronavirus disease 2019 infection,65,69,92 hospitalization or emergency department visit,72,121 sleep apnea,140 sleep disorders,60,130 arthritis,120 atopic dermatitis,113 bone fracture,36 cancer,72 difficulty concentrating,137 general health,128 fatty liver disease,74 impaired vision,93 and oral human papillomavirus.77 These studies reported a total of 124 risk estimates, all of which are considered approximations of odds ratios. Fifty of the 124 odds ratios (40%) were from studies that shared one or more data sets (Table S4).
Table S5 summarizes study characteristics for each outcome. Most odds ratios were from cross-sectional (94/124 [76%]) versus longitudinal designs, noncurrent e-cigarette (versus never) use as the reference condition (69/124 [56%]), and current (versus ever) presence of disease (90/124 [73%]). Nearly half of the odds ratios (60/124 [48%]) were from stratified models, 40% (49/124) were from multivariate models, and 12% (15/124) were from both. About half the e-cigarette versus cigarette (50/82 [61%]) and dual use versus cigarette odds ratios (55/113 = 49%) were based on stratified estimates. One third of odds ratios (39/124 [31%]) controlled for former smoking, either by including it as a covariate (17/39 [44%]), by stratifying on smoking status (16/38 [41%]), by including smoking duration as a covariate (5/39 [13%]), or by including both smoking status and duration as covariates (1/39 [3%]). All odds ratios for cardiovascular, stroke, metabolic dysfunction, and COPD studies, 52% of asthma odds ratios, and 70% of the oral disease odds ratios were estimated using adult samples.
RISK OF BIAS ASSESSMENT
As detailed in the Supplemental Results, all studies scored as having a low risk of bias (Table S3), generally because they used well-established population-based samples designed to assess overall determinants of health.
META-ANALYSIS FINDINGS
Comparisons to Cigarette Use
Comparing e-cigarette with cigarette use, the confidence intervals for the pooled odds ratios for cardiovascular disease (coronary heart disease, erectile dysfunction, and myocardial infarction; odds ratio, 0.81; 95% CI, 0.58 to 1.14), stroke (0.73; 0.47 to 1.13), and metabolic dysfunction (0.99; 0.91 to 1.09) included 1 (Fig. 1 and Table 1). The odds ratios for asthma (0.84; 0.75 to 0.95), COPD (0.53; 0.38 to 0.74), and oral disease (0.87; 0.76 to 1.00) were below 1.
Figure 1.
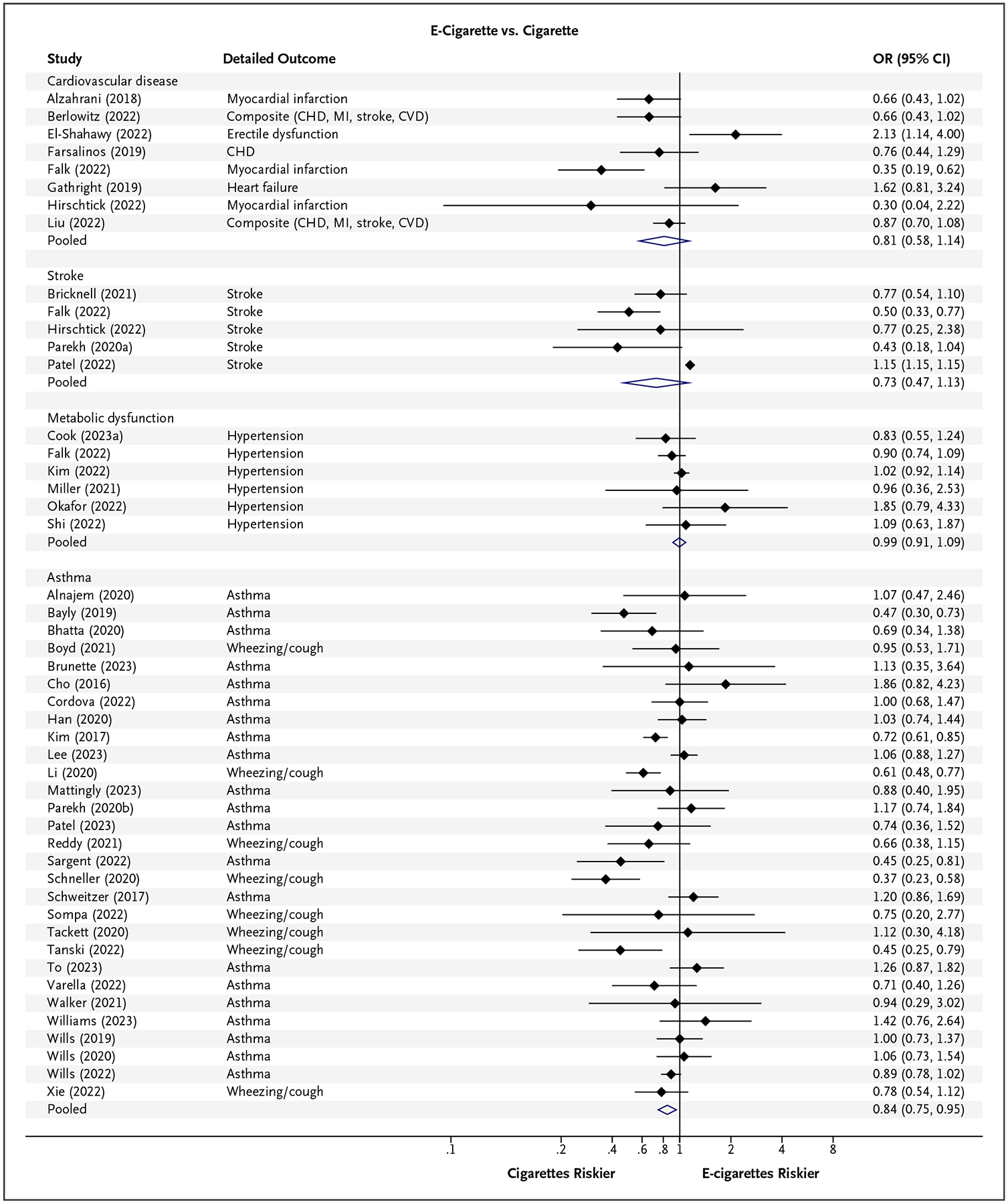
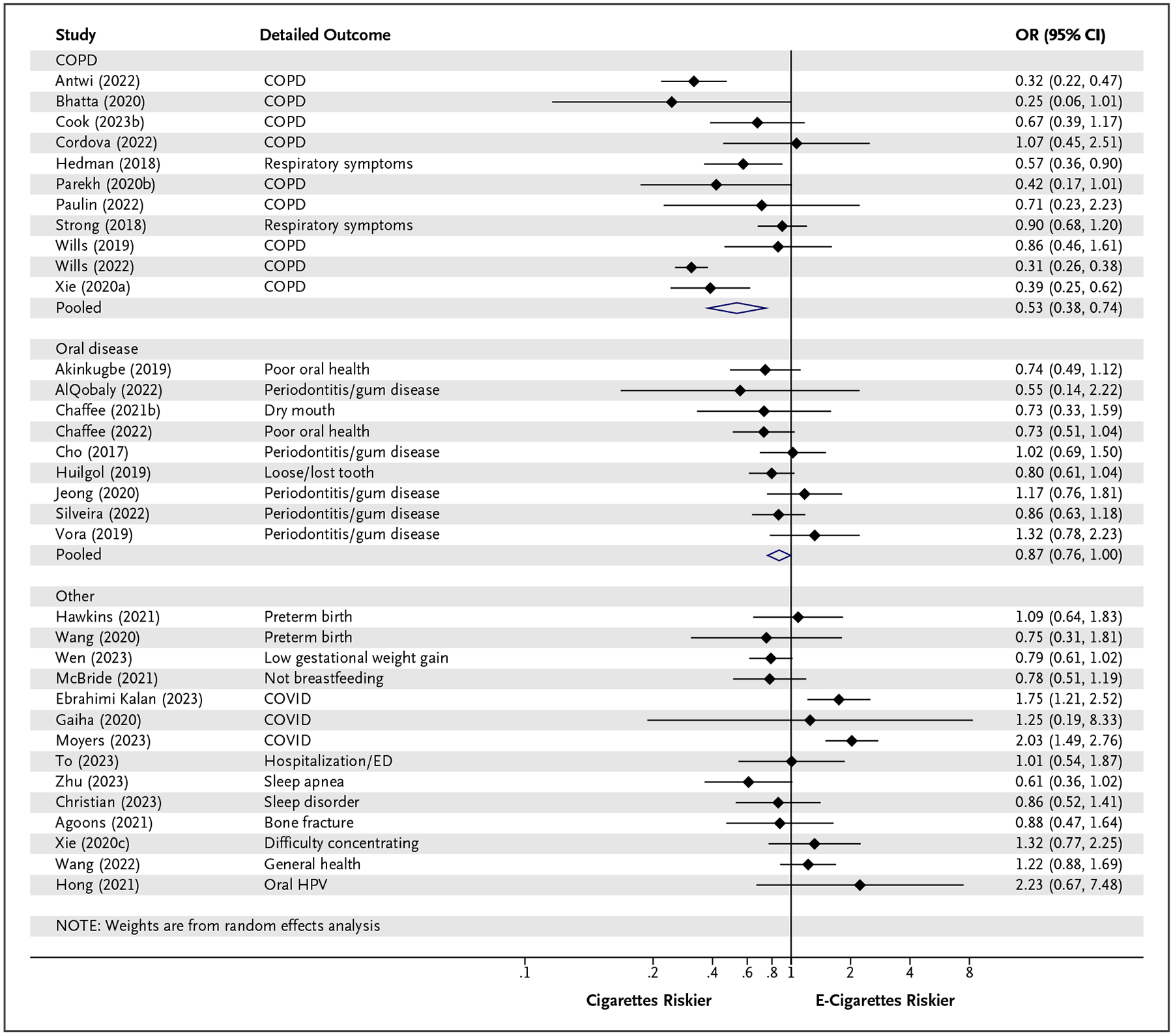
Comparative Disease Odds Ratios for E-Cigarette Use and Cigarette Smoking.
E-cigarette use and cigarette smoking have similar odds of disease for cardiovascular disease, stroke, and metabolic dysfunction and lower odds for asthma (odds ratio, 0.84), COPD (odds ratio, 0.53), and oral disease (odds ratio, 0.87). Confidence intervals include Bonferroni adjustments. Diamonds show point estimates and 95% confidence intervals for pooled odds ratios from random effects meta-analysis. Results for “other” studies were not pooled. CHD denotes coronary heart disease; CI, confidence interval; COPD, chronic obstructive pulmonary disease; COVID, coronavirus disease 2019; CVD, cardiovascular disease; ED, emergency department; HPV, human papillomavirus; MI, myocardial infarction; and OR, odds ratio.
Table 1.
Pooled Adjusted* Odds Ratios of Each Disease Outcome (95% Confidence Intervals) from the Meta-analyses.
| Comparisons | Cardiovascular | Stroke | Metabolic Dysfunction | Asthma | COPD | Oral Disease |
|---|---|---|---|---|---|---|
| Comparison to cigarette use | ||||||
| E-cigarettes vs. cigarettes | 0.81 (0.58–1.14) | 0.73 (0.47–1.13) | 0.99 (0.91–1.09) | 0.84 (0.75–0.95) | 0.53 (0.38–0.74) | 0.87 (0.76–1.00) |
| Dual use vs. cigarettes | 1.23 (0.99–1.54) | 1.26 (1.06–1.50) | 1.22 (1.15–1.31) | 1.20 (1.12–1.28) | 1.41 (1.12–1.64) | 1.27 (1.15–1.39) |
| Comparison to no use | ||||||
| E-cigarette vs. nonuse | 1.24 (1.05–1.46) | 1.32 (0.99–1.76) | 1.25 (1.18–1.33) | 1.24 (1.19–1.30) | 1.46 (1.31–1.61) | 1.47 (1.19–1.82) |
| Dual use vs. nonuse | 2.23 (1.59–3.14) | 2.39 (2.02–2.83) | 1.49 (1.17–1.91) | 1.56 (1.22–2.00) | 3.29 (1.97–5.51) | 1.78 (1.49–2.12) |
| Cigarette vs. nonuse | 1.64 (1.24–2.16) | 2.08 (1.91–2.27) | 1.27 (1.17–1.37) | 1.56 (1.34–1.80) | 2.99 (2.29–3.92) | 1.69 (1.40–2.03) |
Adjusted for covariates listed in Table S3. COPD denotes chronic obstructive pulmonary disease.
Dual use was associated with higher point estimates for odds of disease compared with cigarettes for all outcomes, ranging from 1.20 to 1.41 (Fig. 2 and Table 1).
Figure 2.
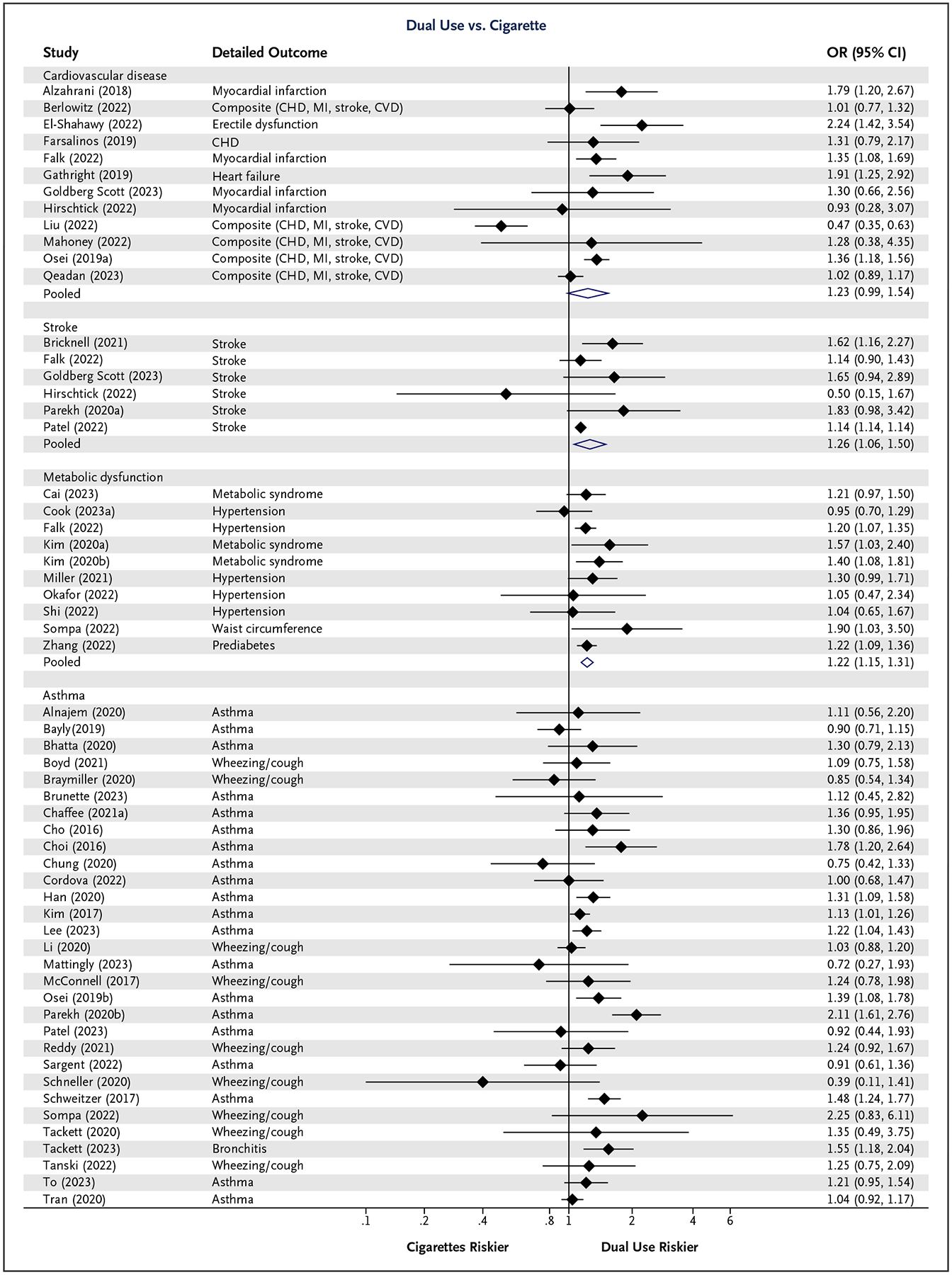
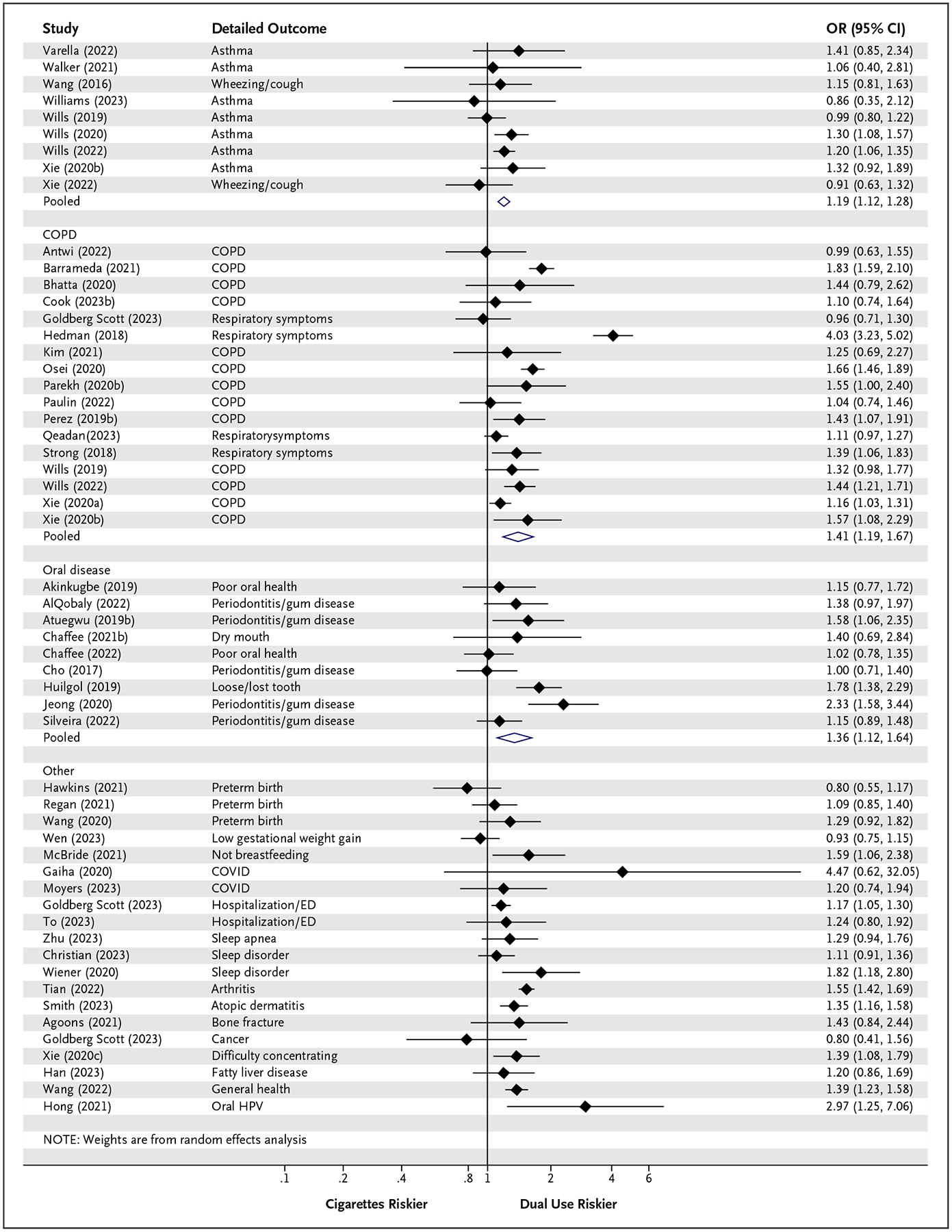
Comparative Disease Odds Ratios for Cigarette Smoking and Dual Use.
Point estimates for odds ratios of disease of all outcomes are above 1 in dual users compared to cigarette smokers (odds ratio, 1.12 to 1.41). Confidence intervals include Bonferroni adjustments. Diamonds show point estimates and 95% confidence intervals for pooled odds ratios from random effects meta-analysis. Results for “other” studies were not pooled. CHD denotes coronary heart disease; CI, confidence interval; COPD, chronic obstructive pulmonary disease; COVID, coronavirus disease 2019; CVD, cardiovascular disease; ED, emergency department; HPV, human papillomavirus; MI, myocardial infarction; and OR, odds ratio.
Comparisons to No Use
E-cigarette use compared with nonuse of e-cigarettes was associated with higher point estimates for disease for all outcomes, ranging from 1.24 to 1.47 (Fig. S2 and Table 1).
Dual use compared with nonuse of e-cigarettes or cigarettes was associated with increased odds of disease, ranging from 1.49 to 3.29 (Fig. S3 and Table 1).
Cigarette use compared with nonuse of cigarettes was also associated with increased odds of disease, ranging from 1.27 to 2.99 (Fig. S4 and Table 1).
SENSITIVITY ANALYSES AND POSSIBLE CONFOUNDING BY FORMER SMOKING
As detailed in Supplemental Results, study design characteristics, including whether the analysis controlled for former smoking (yes versus no) (Table S6), limiting the analysis to directly reported odds ratios (Table S7), youth versus adult samples (Table S8), variability in detailed outcomes within diseases categories (Table S9), variability between individual studies (Figs. S5 and S6), and the assumption that ORecig and ORcig are independent (Table S10) were unlikely to have affected the main findings. Studies of never smokers also yielded increased odds ratios for e-cigarettes.
PUBLICATION BIAS
Taken together, funnel plots (Fig. S7), Begg and Egger tests (Table S11), and trim-and-fill tests (Table S12) did not exhibit evidence of publication bias.
OVERALL ODDS RATIOS COMBINING EXCLUSIVE E-CIGARETTE USE AND DUAL USE
Accounting for the fact that some e-cigarette users use only e-cigarettes and some are dual users increases the overall odds ratio of disease associated with all e-cigarette use in the population because dual use is associated with an odds ratio greater than 1 for all outcomes (Fig. S8). Based on 39.1% U.S. dual use in 2019,25 the probabilities of odds ratios greater than 1 are 0.42 for cardiovascular disease, 0.28 for stroke, greater than 0.99 for metabolic dysfunction, 0.30 for asthma, 0.98 for COPD, and 0.77 for oral disease. These results are sensitive to prevalence of dual use. In Sweden in 2016, when dual use was 66.7%,26 these probabilities increased to 0.82 for cardiovascular disease, 0.74 for stroke, and more than 0.99 for metabolic dysfunction, asthma, COPD, and oral disease.
QUALITATIVE SUMMARY OF OTHER OUTCOMES
Among the 22 studies of other conditions (Table S13, Figs. 1 and 2, and Figs. S1–S3) where there were not enough studies to do a formal meta-analysis, individual studies of not breastfeeding, difficulty concentrating, and general health showed that ORecig versus cig was not different from 1 in all but one study. ORdual versus cig and ORecig were greater than 1 in about half the studies. These findings should be interpreted cautiously, because they are based on only one to three studies for each outcome.
GRADE EVALUATION
We have moderate confidence in the conclusions that e-cigarettes and cigarettes have comparable odds of disease for all outcomes, except COPD, for which we have high confidence (Tables S14 and S15). We have moderate confidence for the conclusion that dual use is associated with higher odds of disease than cigarettes for all outcomes (Tables S14 and S15). Confidence for comparisons of e-cigarettes, cigarettes, and dual use versus no product use was moderate to high, depending on the specific outcome.
Discussion
Observational evidence from 124 odds ratios of disease in 107 population-based epidemiological studies of real-world use of e-cigarettes revealed that the odds of disease associated with e-cigarette use were not different from those associated with cigarette smoking for cardiovascular diseases, stroke, and metabolic dysfunction but were lower for asthma, COPD, and oral disease (Table 1 and Fig. 1). Although lower than for cigarettes, the reduced odds ratios associated with e-cigarette use compared with cigarettes for asthma (odds ratio, 0.84), COPD (odds ratio, 0.53), and oral disease (odds ratio, 0.87) are 3 to 10 times the 15% risk that the FDA13 or the 5% risk that Public Health England2 have quoted. The odds of disease associated with dual use were higher than for smoking for all outcomes (odds ratio, 1.20 to 1.41; Table 1 and Fig. 2).
ORecig values for asthma and COPD are similar to those in earlier meta-analyses based on fewer studies4–6 and consistent with qualitative summaries11 that concluded that switching from cigarettes to e-cigarettes was associated with lower risk of respiratory disease but not cardiovascular diseases and that dual use was associated with higher risks than smoking.12 Although COPD takes many years to develop fully, changes begin to appear within a few years.90,146 The lower COPD ORecig for e-cigarette use may reflect the fact that e-cigarette users are, on average, younger than cigarette smokers146 and not enough time may have passed for the e-cigarette risks to be fully manifest.
The odds ratios identified in the epidemiological studies are higher than those predicted by biomarker studies.20 This direct evidence of disease diverges from conclusions based solely on biomarkers of exposure to tobacco products,19–21,147 which calls into question the FDA’s policy of authorizing tobacco companies to make modified risk claims about products based solely on the fact that some biomarkers of exposure associated with e-cigarettes are lower than those associated with cigarettes.148 Our results are consistent with pathophysiological evidence that shows a wide range of adverse cardiovascular,9,149–159 pulmonary,5,151,152,159–161 and oral health effects10,162 associated with e-cigarette use.
E-cigarettes expose users to a different toxic chemical mix than cigarettes,22 including compounds formed during heating and aerosolization that are not present in the e-liquid itself.163–165 Although there is some overlap, dual use of e-cigarettes and cigarettes together delivers a wider range of toxins than either does alone. These facts, combined with the observation that daily cigarette consumption among exclusive smokers and dual users was not different,166–168 may explain the higher odds ratios observed among dual users compared with cigarette smoking alone. It is important to account for dual use when assessing population health impacts of e-cigarette use, because the increased odds ratios associated with dual use compared with just smoking applies among smokers who use e-cigarettes who do not “switch completely,” raising the overall population impact associated with e-cigarette use (Fig. S8). Continued dual use should be listed as an adverse event in randomized controlled trials of e-cigarettes for smoking cessation, because it is a much more likely outcome than “complete switching.”169
E-cigarette findings are unlikely to be the results of confounding with current or former smoking because all the studies either controlled for smoking in the statistical model or stratified on smoking, with e-cigarette users among never smokers analyzed separately from current and, often, former smokers. Results from studies of former smokers were not different from the overall analysis of all studies, and most studies of never smokers (where there are no former smokers) found increases in the odds of disease in e-cigarette users compared with nonusers.
LIMITATIONS
E-cigarette devices and liquids differ in emissions and have changed over time. Common measures of e-cigarette use in most population studies did not capture data on specific devices or e-liquids, and thus, we could not assess these details.
Dual use includes a wide range of behaviors, with some individuals being predominantly smokers and others mostly using e-cigarettes. Another limitation is that few of the studies controlled for duration and frequency/intensity of e-cigarette and cigarette use, so we could not examine dose–response relations.
Most (76%) of the studies were cross-sectional (Table S5), which does not allow for establishing causality. For our primary comparisons of e-cigarettes versus cigarettes as well as the secondary comparisons of e-cigarettes versus nonuse and cigarettes and nonuse, there was no difference between the results of longitudinal and cross-sectional studies (Table S6). More longitudinal studies that last long enough to allow full manifestation of disease are needed to confirm the relationships reported in this meta-analysis.
Most of the disease outcomes were based on self-reported diagnoses. However, self-reported diagnosis of cardiovascular disease170,171 and COPD172,173 was validated against medical records. Population prevalence estimates in PATH are similar to results in NHANES for cardiovascular174 and oral diseases.56
E-cigarettes have been on the market for less than 20 years, which may not be long enough to observe the full manifestation of the disease impact. Even so, the available data revealed association with several diseases. To the extent that the likelihood that disease will be manifest increases with time, our estimates may underestimate the long-term associations of e-cigarette use with diseases.
CONCLUSIONS
Direct epidemiological evidence based on actual use of e-cigarettes in the general population suggests that, at least for cardiovascular disease, stroke, and metabolic dysfunction, the odds of disease between current e-cigarette and cigarette use were similar. For asthma, COPD, and oral disease, although lower than with cigarettes, the odds of disease were still substantial.
Current dual use was associated with 20 to 40% higher odds of disease than smoking, suggesting increased overall population risks for e-cigarettes even for respiratory disease. The available data are also inconsistent with the FDA’s assumption, made in its authorizations to sell Vuse Solo,16 NJOY,18 and Logic17 e-cigarettes, and the IQOS heated tobacco product,175 that dual use is less harmful or, at most, no more harmful than smoking.15,176 The dual-use findings are particularly important because dual use is a common behavior among adults who use e-cigarettes25–27,169,177 that can overcome any population benefit for those who “switch completely” even for respiratory and oral diseases.
The findings of increased odds of several diseases for e-cigarettes compared with nonuse illustrates the substantial risks for people, particularly youth and young adults, who initiate nicotine use with e-cigarettes and former smokers who restart nicotine use with e-cigarettes. Even without considering the millions of youth who initiate nicotine use with e-cigarettes,28 these results suggest a need for a careful reassessment of the assumption that e-cigarettes are a substantially less harmful alternative to cigarettes, particularly given the fact that, as consumer products, e-cigarettes are not associated with increased smoking cessation178,179 and, over the long run, are associated with less cessation and increased odds of becoming a dual user.180,181
Supplementary Material
Acknowledgments
We thank University of California, San Francisco, research and copyright librarian Peggy Tahir for advising on structuring the literature searches; Ben Chaffee, Thomas Wills, Charlotta Pisinger, Pamela Ling, Matt Springer, and Neal Benowitz for comments on the manuscript; Carolyn Calfee and Michael Matthay for advice on classification of respiratory papers; Robert Lustig for advice on metabolic dysfunction papers; and Isabel Allen for advice on how to handle related papers in the meta-analysis. We also thank the Brazilian Health Regulatory Agency (Anvisa), especially the DIRE3 and GGTAB teams, for filling in for Andre Luiz Oliveira da Silva during his UCSF postdoctoral fellowship.
Footnotes
Disclosures
Author disclosures and other supplementary materials are available at evidence.nejm.org.
References
- 1.National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. Washington, DC: National Academies Press, 2018. [PubMed] [Google Scholar]
- 2.McNeill A, Brose L, Calder R, Hitchman S, Hajek P, McRobbie H. E-cigarettes: an evidence update: a report commissioned by Public Health England. August 2015. (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/733022/Ecigarettes_an_evidence_update_A_report_commissioned_by_Public_Health_England_FINAL.pdf).
- 3.Banks E, Yazidjoglou A, Brown S, et al. Electronic cigarettes and health outcomes: umbrella and systematic review of the global evidence. Med J Aust 2023;218:267–275. DOI: 10.5694/mja2.51890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chand BR, Hosseinzadeh H. Association between e-cigarette use and asthma: a systematic review and meta-analysis. J Asthma 2022;59:1722–1731. DOI: 10.1080/02770903.2021.1971703. [DOI] [PubMed] [Google Scholar]
- 5.Wills TA, Soneji SS, Choi K, Jaspers I, Tam EK. E-cigarette use and respiratory disorders: an integrative review of converging evidence from epidemiological and laboratory studies. Eur Respir J 2021;57:1901815. DOI: 10.1183/13993003.01815-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X, Zhang Y, Zhang R, Chen F, Shao L, Zhang L. Association between e-cigarettes and asthma in adolescents: a systematic review and meta-analysis. Am J Prev Med 2022;62:953–960. DOI: 10.1016/j.amepre.2022.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Skotsimara G, Antonopoulos AS, Oikonomou E, et al. Cardiovascular effects of electronic cigarettes: a systematic review and meta-analysis. Eur J Prev Cardiol 2019;26:1219–1228. DOI: 10.1177/2047487319832975. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy CD, van Schalkwyk MCI, McKee M, Pisinger C. The cardiovascular effects of electronic cigarettes: a systematic review of experimental studies. Prev Med 2019;127:105770. DOI: 10.1016/j.ypmed.2019.105770. [DOI] [PubMed] [Google Scholar]
- 9.Siddiqi TJ, Rashid AM, Siddiqi AK, et al. Association of electronic cigarette exposure on cardiovascular health: a systematic review and meta-analysis. Curr Probl Cardiol 2023;48:101748. DOI: 10.1016/j.cpcardiol.2023.101748. [DOI] [PubMed] [Google Scholar]
- 10.Youssef M, Marzouk T, Abdelsalam H, et al. The effect of electronic cigarette use on peri-implant conditions in men: a systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2023;135:492–500. DOI: 10.1016/j.oooo.2022.08.010. [DOI] [PubMed] [Google Scholar]
- 11.Goniewicz ML, Miller CR, Sutanto E, Li D. How effective are electronic cigarettes for reducing respiratory and cardiovascular risk in smokers? A systematic review. Harm Reduct J 2020;17:91. DOI: 10.1186/s12954-020-00440-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pisinger C, Rasmussen SKB. The health effects of real-world dual use of electronic and conventional cigarettes versus the health effects of exclusive smoking of conventional cigarettes: a systematic review. Int J Environ Res Public Health 2022;19:13687. DOI: 10.3390/ijerph192013687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Food and Drug Administration. FDA proposes rules prohibiting menthol cigarettes and flavored cigars to prevent youth initiation, significantly reduce tobacco-related disease and death. April 28, 2022. (https://www.fda.gov/news-events/press-announcements/fda-proposes-rules-prohibiting-menthol-cigarettes-and-flavored-cigars-prevent-youth-initiation).
- 14.Levy DT, Meza R, Yuan Z, et al. Public health impact of a US ban on menthol in cigarettes and cigars: a simulation study. Tob Control 2023;32:e37–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glantz S, Lempert LK. Vuse Solo e-cigarettes do not provide net benefits to public health: a scientific analysis of FDA’s marketing authorisation. Tob Control 2023. February 9 (Epub ahead of print). DOI: 10.1136/tc-2022-057296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Food and Drug Administration. Technical Project Lead (TPL) review of PMTAs PM0000551, PM0000553, PM0000560. October 12, 2021. (https://www.fda.gov/media/153017/download).
- 17.U.S. Food and Drug Administration. Technical Project Lead (TPL) review of PMTAs PM0000529–PM0000541. March 23, 2022. (https://www.fda.gov/media/158754/download).
- 18.U.S. Food and Drug Administration. Technical Project Lead (TPL) review of PMTAs PM0000630–PM0000631 (unredacted). March 30, 2022. (https://www.fda.gov/media/165234/download).
- 19.Anic GM, Rostron BL, Hammad HT, et al. Changes in biomarkers of tobacco exposure among cigarette smokers transitioning to ENDS use: the Population Assessment of Tobacco and Health Study, 2013–2015. Int J Environ Res Public Health 2022;19:1462. DOI: 10.3390/ijerph19031462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson N, Summers JA, Ait Ouakrim D, Hoek J, Edwards R, Blakely T. Improving on estimates of the potential relative harm to health from using modern ENDS (vaping) compared to tobacco smoking. BMC Public Health 2021;21:2038. DOI: 10.1186/s12889-021-12103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hartmann-Boyce J, Butler AR, Theodoulou A, et al. Biomarkers of potential harm in people switching from smoking tobacco to exclusive e-cigarette use, dual use or abstinence: secondary analysis of Cochrane systematic review of trials of e-cigarettes for smoking cessation. Addiction 2023;118:539–545. DOI: 10.1111/add.16063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tehrani MW, Newmeyer MN, Rule AM, Prasse C. Characterizing the chemical landscape in commercial e-cigarette liquids and aerosols by liquid chromatography-high-resolution mass spectrometry. Chem Res Toxicol 2021;34:2216–2226. DOI: 10.1021/acs.chemrestox.1c00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang JT, Anic GM, Rostron BL, Tanwar M, Chang CM. Cigarette smoking reduction and health risks: a systematic review and meta-analysis. Nicotine Tob Res 2021;23:635–642. DOI: 10.1093/ntr/ntaa156. [DOI] [PubMed] [Google Scholar]
- 24.Hackshaw A, Morris JK, Boniface S, Tang JL, Milenković D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 2018;360:j5855. DOI: 10.1136/bmj.j5855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayer M, Reyes-Guzman C, Grana R, Choi K, Freedman ND. Demographic characteristics, cigarette smoking, and e-cigarette use among US adults. JAMA Netw Open 2020;3:e2020694–e2020694. DOI: 10.1001/jamanetworkopen.2020.20694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hedman L, Backman H, Stridsman C, et al. Association of electronic cigarette use with smoking habits, demographic factors, and respiratory symptoms. JAMA Netw Open 2018;1:e180789. DOI: 10.1001/jamanetworkopen.2018.0789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim C-Y, Paek Y-J, Seo HG, et al. Dual use of electronic and conventional cigarettes is associated with higher cardiovascular risk factors in Korean men. Sci Rep 2020;10:5612. DOI: 10.1038/s41598-020-62545-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper M, Park-Lee E, Ren C, Cornelius M, Jamal A, Cullen KA. Notes from the field: e-cigarette use among middle and high school students — United States, 2022. MMWR Morb Mortal Wkly Rep 2022;71:1283–1285. DOI: 10.15585/mmwr.mm7140a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glantz S, Jeffers A, Winickoff JP. Nicotine addiction and intensity of e-cigarette use by adolescents in the US, 2014 to 2021. JAMA Netw Open 2022;5:e2240671. DOI: 10.1001/jamanetworkopen.2022.40671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES). 2023. (https://www.cdc.gov/nchs/nhanes/).
- 31.ROBINS-E Development Group. Risk Of Bias In Non-randomized Studies — of Exposure (ROBINS-E). Launch version, June 1, 2022 (https://www.riskofbias.info/welcome/robins-e-tool).
- 32.Siemieniuk R, Guyatt G. What is GRADE? BMJ Best Practice. 2022. (https://bestpractice.bmj.com/info/toolkit/learn-ebm/what-is-grade/).
- 33.George A, Stead TS, Ganti L. What’s the risk: differentiating risk ratios, odds ratios, and hazard ratios? Cureus 2020;12:e10047. DOI: 10.7759/cureus.10047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for meta-analysis in medical research. New York: Wiley, 2000. [Google Scholar]
- 35.Rao G, Lopez-Jimenez F, Boyd J, et al. Methodological standards for meta-analyses and qualitative systematic reviews of cardiac prevention and treatment studies: a scientific statement From the American Heart Association. Circulation 2017;136:e172–e194. DOI: 10.1161/CIR.0000000000000523. [DOI] [PubMed] [Google Scholar]
- 36.Agoons DD, Agoons BB, Emmanuel KE, Matawalle FA, Cunningham JM. Association between electronic cigarette use and fragility fractures among US adults. Am J Med Open 2021;1–6:100002. DOI: 10.1016/j.ajmo.2021.100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akinkugbe AA. Cigarettes, e-cigarettes, and adolescents’ oral health: findings from the Population Assessment of Tobacco and Health (PATH) study. JDR Clin Trans Res 2019;4:276–283. DOI: 10.1177/2380084418806870. [DOI] [PubMed] [Google Scholar]
- 38.Alnajem A, Redha A, Alroumi D, et al. Use of electronic cigarettes and secondhand exposure to their aerosols are associated with asthma symptoms among adolescents: a cross-sectional study. Respir Res 2020;21:300. DOI: 10.1186/s12931-020-01569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.AlQobaly L, Abed H, Alsahafi Y, Sabbah W, Hakeem FF. Does smoking explain the association between use of e-cigarettes and self-reported periodontal disease? J Dent 2022;122:104164. DOI: 10.1016/j.jdent.2022.104164. [DOI] [PubMed] [Google Scholar]
- 40.Alzahrani T, Pena I, Temesgen N, Glantz SA. Association between electronic cigarette use and myocardial infarction. Am J Prev Med 2018;55:455–461. DOI: 10.1016/j.amepre.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Antwi GO, Rhodes DL. Association between e-cigarette use and chronic obstructive pulmonary disease in non-asthmatic adults in the USA. J Public Health (Oxf) 2022;44:158–164. DOI: 10.1093/pubmed/fdaa229. [DOI] [PubMed] [Google Scholar]
- 42.Atuegwu NC, Perez MF, Oncken C, Mead EL, Maheshwari N, Mortensen EM. E-cigarette use is associated with a self-reported diagnosis of prediabetes in never cigarette smokers: results from the behavioral risk factor surveillance system survey. Drug Alcohol Depend 2019;205:107692. DOI: 10.1016/j.drugalcdep.2019.107692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Atuegwu NC, Perez MF, Oncken C, Thacker S, Mead EL, Mortensen EM. Association between regular electronic nicotine product use and self-reported periodontal disease status: Population Assessment of Tobacco and Health Survey. Int J Environ Res Public Health 2019;16:1263. DOI: 10.3390/ijerph16071263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barrameda R, Nguyen T, Wong V, et al. Use of e-cigarettes and self-reported lung disease among US adults. Public Health Rep 2020;135:785–795. DOI: 10.1177/0033354920951140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bayly JE, Bernat D, Porter L, Choi K. Secondhand exposure to aerosols from electronic nicotine delivery systems and asthma exacerbations among youth with asthma. Chest 2019;155:88–93. DOI: 10.1016/j.chest.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berlowitz JB, Xie W, Harlow AF, et al. E-cigarette use and risk of cardiovascular disease: a longitudinal analysis of the PATH study (2013–2019). Circulation 2022;145:1557–1559. DOI: 10.1161/CIRCULATIONAHA.121.057369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med 2020;58:182–190. DOI: 10.1016/j.amepre.2019.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bircan E, Bezirhan U, Porter A, Fagan P, Orloff MS. Electronic cigarette use and its association with asthma, chronic obstructive pulmonary disease (COPD) and asthma-COPD overlap syndrome among never cigarette smokers. Tob Induc Dis 2021;19:75. DOI: 10.18332/tid/142579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boyd CJ, McCabe SE, Evans-Polce RJ, Veliz PT. Cannabis, vaping, and respiratory symptoms in a probability sample of U.S. youth. J Adolesc Health 2021;69:149–152. DOI: 10.1016/j.jadohealth.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Braymiller JL, Barrington-Trimis JL, Leventhal AM, et al. Assessment of nicotine and cannabis vaping and respiratory symptoms in young adults. JAMA Netw Open 2020;3:e2030189. DOI: 10.1001/jamanetworkopen.2020.30189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brunette MF, Halenar MJ, Edwards KC, et al. Association between tobacco product use and asthma among US adults from the Population Assessment of Tobacco and Health (PATH) study waves 2–4. BMJ Open Respir Res 2023;10:e001187. DOI: 10.1136/bmjresp-2021-001187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bricknell RAT, Ducaud C, Figueroa A, et al. An association between electronic nicotine delivery systems use and a history of stroke using the 2016 behavioral risk factor surveillance system. Medicine (Baltimore) 2021;100:e27180. DOI: 10.1097/MD.0000000000027180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cai J, Bidulescu A. Associations between e-cigarette use or dual use of e-cigarette and combustible cigarette and metabolic syndrome: results from the National Health and Nutrition Examination Survey (NHANES). Ann Epidemiol 2023;85:93–99.e2. DOI: 10.1016/j.annepidem.2023.05.009. [DOI] [PubMed] [Google Scholar]
- 54.Chaffee BW, Barrington-Trimis J, Liu F, et al. E-cigarette use and adverse respiratory symptoms among adolescents and young adults in the United States. Prev Med 2021;153:106766. DOI: 10.1016/j.ypmed.2021.106766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chaffee BW, Halpern-Felsher B, Cheng J. E-cigarette, cannabis and combustible tobacco use: associations with xerostomia among California adolescents. Community Dent Oral Epidemiol 2021;51: 180–186. DOI: 10.1111/cdoe.12721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chaffee BW, Lauten K, Sharma E, et al. Oral health in the Population Assessment of Tobacco and Health Study. J Dent Res 2022; 101:1046–1054. DOI: 10.1177/00220345221086272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cho JH, Paik SY. Association between electronic cigarette use and asthma among high school students in South Korea. PLoS One 2016;11:e0151022. DOI: 10.1371/journal.pone.0151022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cho JH. The association between electronic-cigarette use and self-reported oral symptoms including cracked or broken teeth and tongue and/or inside-cheek pain among adolescents: a cross-sectional study. PLoS One 2017;12:e0180506. DOI: 10.1371/journal.pone.0180506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Choi K, Bernat D. E-cigarette use among Florida youth with and without asthma. Am J Prev Med 2016;51:446–453. DOI: 10.1016/j.amepre.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Christian WJ, Valvi NR, Walker CJ. Investigating the relation between electronic cigarette use and sleep duration in Kentucky using the BRFSS, 2016–2017. South Med J 2023;116:326–331. DOI: 10.14423/SMJ.0000000000001529. [DOI] [PubMed] [Google Scholar]
- 61.Chung SJ, Kim BK, Oh JH, et al. Novel tobacco products including electronic cigarette and heated tobacco products increase risk of allergic rhinitis and asthma in adolescents: analysis of Korean youth survey. Allergy 2020;75:1640–1648. DOI: 10.1111/all.14212. [DOI] [PubMed] [Google Scholar]
- 62.Cook S, Hirschtick JL, Barnes G, et al. Time-varying association between cigarette and ENDS use on incident hypertension among US adults: a prospective longitudinal study. BMJ Open 2023;13: e062297. DOI: 10.1136/bmjopen-2022-062297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cook SF, Hirschtick JL, Fleischer NL, et al. Cigarettes, ENDS use, and chronic obstructive pulmonary disease incidence: a prospective longitudinal study. Am J Prev Med 2023;65:173–181. DOI: 10.1016/j.amepre.2023.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cordova J, Pfeiffer RM, Choi K, et al. Tobacco use profiles by respiratory disorder status for adults in the wave 1–wave 4 population assessment of tobacco and health (PATH) study. Prev Med Rep 2022;30:102016. DOI: 10.1016/j.pmedr.2022.102016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ebrahimi Kalan M, Jebai R, Li W, et al. COVID-19 and tobacco products use among US adults, 2021 National Health Interview Survey. Health Sci Rep 2023;6:e1542. DOI: 10.1002/hsr2.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.El-Shahawy O, Shah T, Obisesan OH, et al. Association of e-cigarettes with erectile dysfunction: the Population Assessment of Tobacco and Health study. Am J Prev Med 2022;62:26–38. DOI: 10.1016/j.amepre.2021.08.004. [DOI] [PubMed] [Google Scholar]
- 67.Falk GE, Okut H, Vindhyal MR, Ablah E. Hypertension and cardiovascular diseases among electronic and combustible cigarette users. Kans J Med 2022;15:226–230. DOI: 10.17161/kjm.vol15.16752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Farsalinos KE, Polosa R, Cibella F, Niaura R. Is e-cigarette use associated with coronary heart disease and myocardial infarction? Insights from the 2016 and 2017 National Health Interview Surveys. Ther Adv Chronic Dis 2019;10:2040622319877741. DOI: 10.1177/2040622319877741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health 2020;67:519–523. DOI: 10.1016/j.jadohealth.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gathright EC, Wu WC, Scott-Sheldon LAJ. Electronic cigarette use among heart failure patients: findings from the Population Assessment of Tobacco and Health study (Wave 1: 2013–2014). Heart Lung 2020;49:229–232. DOI: 10.1016/j.hrtlng.2019.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Giovanni SP, Keller TL, Bryant AD, Weiss NS, Littman AJ. Electronic cigarette use and chronic respiratory symptoms among U.S. adults. Am J Respir Crit Care Med 2020;201:1157–1160. DOI: 10.1164/rccm.201907-1460LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Goldberg Scott S, Feigelson HS, Powers JD, et al. Demographic, clinical, and behavioral factors associated with electronic nicotine delivery systems use in a large cohort in the United States. Tob Use Insights 2023;16:1179173x221134855. DOI: 10.1177/1179173X221134855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Han YY, Rosser F, Forno E, Celedon JC. Electronic vapor products, marijuana use, smoking, and asthma in US adolescents. J Allergy Clin Immunol 2020;145:1025–1028.e6. DOI: 10.1016/j.jaci.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Han M, Jeong S, Song J, et al. Association between the dual use of electronic and conventional cigarettes and NAFLD status in Korean men. Tob Induc Dis 2023;21:31. DOI: 10.18332/tid/159167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hawkins SS, Wylie BJ, Hacker MR. Associations between electronic nicotine delivery systems and birth outcomes. J Matern Fetal Neonatal Med 2022;35:6868–6875. DOI: 10.1080/14767058.14762021.11929156. [DOI] [PubMed] [Google Scholar]
- 76.Hirschtick JL, Cook S, Patel A, et al. Longitudinal associations between exclusive and dual use of electronic nicotine delivery systems and cigarettes and self-reported incident diagnosed cardiovascular disease among adults. Nicotine Tob Res 2023;25:386–394. DOI: 10.1093/ntr/ntac182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hong YR, Mainous AG III. Electronic cigarette use and oral human papillomavirus infection among US adult population: analysis of 2013–2016 NHANES. J Gen Intern Med 2021;36:1454–1456. DOI: 10.1007/s11606-020-05874-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Huilgol P, Bhatt SP, Biligowda N, Wright NC, Wells JM. Association of e-cigarette use with oral health: a population-based cross-sectional questionnaire study. J Public Health (Oxf) 2019;41:354–361. DOI: 10.1093/pubmed/fdy082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jeong W, Choi DW, Kim YK, et al. Associations of electronic and conventional cigarette use with periodontal disease in South Korean adults. J Periodontol 2020;91:55–64. DOI: 10.1002/JPER.19-0060. [DOI] [PubMed] [Google Scholar]
- 80.Kim SY, Sim S, Choi HG. Active, passive, and electronic cigarette smoking is associated with asthma in adolescents. Sci Rep 2017;7: 17789. DOI: 10.1038/s41598-017-17958-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim T, Choi H, Kang J, Kim J. Association between electronic cigarette use and metabolic syndrome in the Korean general population: a nationwide population-based study. PLoS One 2020;15: e0237983. DOI: 10.1371/journal.pone.0237983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim T, Kang J. Association between dual use of e-cigarette and cigarette and chronic obstructive pulmonary disease: an analysis of a nationwide representative sample from 2013 to 2018. BMC Pulm Med 2021;21:231. DOI: 10.1186/s12890-021-01590-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kim SY, Jeong SH, Joo HJ, et al. High prevalence of hypertension among smokers of conventional and e-cigarette: using the nationally representative community dwelling survey. Front Public Health 2022;10:919585. DOI: 10.3389/fpubh.2022.919585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee SY, Shin J. Association between electronic cigarettes use and asthma in the United States: data from the National Health Interview Survey 2016–2019. Yonsei Med J 2023;64:54–65. DOI: 10.3349/ymj.2022.0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li D, Sundar IK, McIntosh S, et al. Association of smoking and electronic cigarette use with wheezing and related respiratory symptoms in adults: cross-sectional results from the Population Assessment of Tobacco and Health (PATH) study, wave 2. Tob Control 2020;29:140–147. DOI: 10.1136/tobaccocontrol-2018-054694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu X, Yuan Z, Ji Y. The association between electronic cigarettes, sleep duration, and the adverse cardiovascular outcomes: findings from behavioral risk factor surveillance system, 2020. Front Cardiovasc Med 2022;9:909383. DOI: 10.3389/fcvm.2022.909383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mahoney MC, Rivard C, Kimmel HL, et al. Cardiovascular outcomes among combustible-tobacco and Electronic Nicotine Delivery System (ENDS) users in waves 1 through 5 of the Population Assessment of Tobacco and Health (PATH) study, 2013–2019. Int J Environ Res Public Health 2022;19:4137. DOI: 10.3390/ijerph19074137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mattingly DT, Cook S, Hirschtick JL, et al. Longitudinal associations between exclusive, dual, and polytobacco use and asthma among US youth. Prev Med 2023;171:107512. DOI: 10.1016/j.ypmed.2023.107512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McBride M, Haile ZT. Association between electronic nicotine delivery systems use and breastfeeding duration. Breastfeed Med 2021;16:886–893. DOI: 10.1089/bfm.2021.0132. [DOI] [PubMed] [Google Scholar]
- 90.McConnell R, Barrington-Trimis JL, Wang K, et al. Electronic cigarette use and respiratory symptoms in adolescents. Am J Respir Crit Care Med 2017;195:1043–1049. DOI: 10.1164/rccm.201604-0804OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Miller CR, Shi H, Li D, Goniewicz ML. Cross-sectional associations of smoking and e-cigarette use with self-reported diagnosed hypertension: findings from wave 3 of the Population Assessment of Tobacco and Health study. Toxics 2021;9:52. DOI: 10.3390/toxics9030052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Moyers SA, Hartwell M, Chiaf A, Greiner B, Oliver JA, Croff JM. Associations of combustible cigarette, electronic cigarette, and dual use with COVID infection and severity in the U.S.: a cross-sectional analysis of the 2021 National Health Information Survey. Tob Use Insights 2023;16:1179173x231179675. DOI: 10.1177/1179173X231179675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nguyen AX, Gaiha SM, Chung S, Halpern-Felsher B, Wu AY. Ocular symptoms in adolescents and young adults with electronic cigarette, cigarette, and dual use. JAMA Ophthalmol 2023;141: 937–946. DOI: 10.1001/jamaophthalmol.2023.3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Okafor CN, Okafor N, Kaliszewski C, Wang L. Association between electronic cigarette and combustible cigarette use with cardiometabolic risk biomarkers among U.S. adults. Ann Epidemiol 2022;71:44–50. DOI: 10.1016/j.annepidem.2022.02.002. [DOI] [PubMed] [Google Scholar]
- 95.Osei AD, Mirbolouk M, Orimoloye OA, et al. Association between e-cigarette use and cardiovascular disease among never and current combustible-cigarette smokers. Am J Med 2019;132:949–954.e2. DOI: 10.1016/j.amjmed.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 96.Osei AD, Mirbolouk M, Orimoloye OA, et al. The association between e-cigarette use and asthma among never combustible cigarette smokers: behavioral risk factor surveillance system (BRFSS) 2016 & 2017. BMC Pulm Med 2019;19:180. DOI: 10.1186/s12890-019-0950-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Osei AD, Mirbolouk M, Orimoloye OA, et al. Association between e-cigarette use and chronic obstructive pulmonary disease by smoking status: Behavioral Risk Factor Surveillance System 2016 and 2017. Am J Prev Med 2020;58:336–342. DOI: 10.1016/j.amepre.2019.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Parekh T, Pemmasani S, Desai R. Risk of stroke with e-cigarette and combustible cigarette use in young adults. Am J Prev Med 2020;58:446–452. DOI: 10.1016/j.amepre.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 99.Parekh T, Owens C, Fay K, Phillips J, Kitsantas P. Use of e-cigarettes and development of respiratory conditions in women of childbearing age. South Med J 2020;113:488–494. DOI: 10.14423/SMJ.0000000000001158. [DOI] [PubMed] [Google Scholar]
- 100.Patel U, Patel N, Khurana M, et al. Effect comparison of e-cigarette and traditional smoking and association with stroke — a cross-sectional study of NHANES. Neurol Int 2022;14:441–452. DOI: 10.3390/neurolint14020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Patel A, Cook S, Mattingly DT, et al. Longitudinal association between exclusive and dual use of cigarettes and electronic nicotine delivery systems and asthma among U.S. adolescents. J Adolesc Health 2023;73:437–444. DOI: 10.1016/j.jadohealth.2023.04.009. [DOI] [PubMed] [Google Scholar]
- 102.Paulin LM, Halenar MJ, Edwards KC, et al. Association of tobacco product use with chronic obstructive pulmonary disease (COPD) prevalence and incidence in waves 1 through 5 (2013–2019) of the Population Assessment of Tobacco and Health (PATH) study. Respir Res 2022;23:273. DOI: 10.1186/s12931-022-02197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Perez MF, Atuegwu NC, Mead EL, Oncken C, Mortensen EM. Adult e-cigarettes use associated with a self-reported diagnosis of COPD. Int J Environ Res Public Health 2019;16:3938. DOI: 10.3390/ijerph16203938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Perez MF, Atuegwu NC, Oncken C, Mead EL, Mortensen EM. Association between electronic cigarette use and asthma in never-smokers. Ann Am Thorac Soc 2019;16:1453–1456. DOI: 10.1513/AnnalsATS.201904-338RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Qeadan F, Nicolson A, Barbeau WA, Azagba S, English K. The association between dual use of electronic nicotine products and illicit drugs with adverse cardiovascular and respiratory outcomes in a longitudinal analysis using the Population Assessment of Tobacco and Health (PATH) survey. Drug Alcohol Depend Rep 2023;7:100166. DOI: 10.1016/j.dadr.2023.100166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Reddy KP, Schwamm E, Kalkhoran S, Noubary F, Walensky RP, Rigotti NA. Respiratory symptom incidence among people using electronic cigarettes, combustible tobacco, or both. Am J Respir Crit Care Med 2021;204:231–234. DOI: 10.1164/rccm.202012-4441LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Regan AK, Bombard JM, O’Hegarty MM, Smith RA, Tong VT. Adverse birth outcomes associated with prepregnancy and prenatal electronic cigarette use. Obstet Gynecol 2021;138:85–94. DOI: 10.1097/AOG.0000000000004432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sargent JD, Halenar MJ, Edwards KC, et al. Tobacco use and respiratory symptoms among adults: findings from the longitudinal Population Assessment of Tobacco and Health (PATH) study 2014–16. Nicotine Tob Res 2022;24:1607–1618. DOI: 10.1093/ntr/ntac080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Silveira ML, Everard CD, Sharma E, et al. Tobacco use and incidence of adverse oral health outcomes among US adults in the Population Assessment of Tobacco and Health study. JAMA Netw Open 2022;5:e2245909. DOI: 10.1001/jamanetworkopen.2022.45909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Schneller LM, Quiñones Tavárez Z, Goniewicz ML, et al. Cross-sectional association between exclusive and concurrent use of cigarettes, ENDS, and cigars, the three most popular tobacco products, and wheezing symptoms among U.S. adults. Nicotine Tob Res 2020;22(Suppl 1):S76–S84. DOI: 10.1093/ntr/ntaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schweitzer RJ, Wills TA, Tam E, Pagano I, Choi K. E-cigarette use and asthma in a multiethnic sample of adolescents. Prev Med 2017;105:226–231. DOI: 10.1016/j.ypmed.2017.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shi H, Leventhal AM, Wen Q, Ossip DJ, Li D. Sex differences in the association of e-cigarette and cigarette use and dual use with self-reported hypertension incidence in US adults. Nic Tob Res 2023;25:478–485. DOI: 10.1093/ntr/ntac1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Smith B, Engel P, Collier MR, et al. Association between electronic-cigarette use and atopic dermatitis among United States adults. J Am Acad Dermatol 2023;89:163–165. DOI: 10.1016/j.jaad.2023.02.027. [DOI] [PubMed] [Google Scholar]
- 114.Sompa SI, Zettergren A, Ekström S, et al. Predictors of electronic cigarette use and its association with respiratory health and obesity in young adulthood in Sweden; findings from the population-based birth cohort BAMSE. Environ Res 2022;208:112760. DOI: 10.1016/j.envres.2022.112760. [DOI] [PubMed] [Google Scholar]
- 115.Stevens ER, Xu S, Niaura R, et al. Youth e-cigarette use and functionally important respiratory symptoms: the Population Assessment of Tobacco and Health (PATH) study waves 3 and 4. Int J Environ Res Public Health 2022;19:15324. DOI: 10.3390/ijerph192215324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Strong DR, Myers MG, Pulvers K, Noble M, Brikmanis K, Doran N. Marijuana use among US tobacco users: findings from wave 1 of the population assessment of tobacco health (PATH) study. Drug Alcohol Depend 2018;186:16–22. DOI: 10.1016/j.drugalcdep.2017.12.044. [DOI] [PubMed] [Google Scholar]
- 117.Tackett AP, Keller-Hamilton B, Smith CE, et al. Evaluation of respiratory symptoms among youth e-cigarette users. JAMA Netw Open 2020;3:e2020671. DOI: 10.1001/jamanetworkopen.2020.20671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tackett AP, Urman R, Barrington-Trimis J, et al. Prospective study of e-cigarette use and respiratory symptoms in adolescents and young adults. Thorax 2023;79:163–168. DOI: 10.1136/thorax-2022-218670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tanski S, Halenar MJ, Edwards KC, et al. Tobacco product use and functionally important respiratory symptoms among US adolescents/young adults. Acad Pediatr 2022;22:1006–1016. DOI: 10.1016/j.acap.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tian Y, Jiao Z, Mao Y, Zhang Z. E-cigarette usage and arthritis in the United States, a nationwide cross-sectional survey. Front Pharmacol 2022;13:883550. DOI: 10.3389/fphar.2022.883550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.To T, Borkhoff CM, Chow C-W, et al. Vaping and health service utilization: a Canadian Health Survey and Health Administrative Data study. Ann Am Thorac Soc 2023;20:815–824. DOI: 10.1513/AnnalsATS.202207-578OC. [DOI] [PubMed] [Google Scholar]
- 122.Tran L, Tran P, Tran L. A cross-sectional analysis of electronic cigarette use in US adults by asthma status. Clin Respir J 2020;14: 991–997. DOI: 10.1111/crj.13231. [DOI] [PubMed] [Google Scholar]
- 123.Varella MH, Andrade OA, Shaffer SM, et al. E-cigarette use and respiratory symptoms in residents of the United States: A BRFSS report. PLoS One 2022;17:e0269760. DOI: 10.1371/journal.pone.0269760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Vora MV, Chaffee BW. Tobacco-use patterns and self-reported oral health outcomes: a cross-sectional assessment of the Population Assessment of Tobacco and Health study, 2013–2014. J Am Dent Assoc 2019;150:332–344.e2. DOI: 10.1016/j.adaj.2018.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Walker CJ, Christian WJ. Estimating the population attributable fraction of asthma due to electronic cigarette use and other risk factors using Kentucky Behavioral Risk Factor Survey data, 2016–2017. Subst Use Misuse 2021;56:353–358. DOI: 10.1080/10826084.2020.1868002. [DOI] [PubMed] [Google Scholar]
- 126.Wang MP, Ho SY, Leung LT, Lam TH. Electronic cigarette use and respiratory symptoms in Chinese adolescents in Hong Kong. JAMA Pediatr 2016;170:89–91. DOI: 10.1001/jamapediatrics.2015.3024. [DOI] [PubMed] [Google Scholar]
- 127.Wang X, Lee NL, Burstyn I. Smoking and use of electronic cigarettes (vaping) in relation to preterm birth and small-for-gestational-age in a 2016 U.S. national sample. Prev Med 2020;134:106041. DOI: 10.1016/j.ypmed.2020.106041. [DOI] [PubMed] [Google Scholar]
- 128.Wang Y, Sung H-Y, Lightwood J, Yao T, Max WB. Healthcare utilisation and expenditures attributable to current e-cigarette use among US adults. Tob Control 2023;32:723–728. DOI: 10.1136/tobaccocontrol-2021-057058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wen X, Thomas MA, Liu L, et al. Association between maternal e-cigarette use during pregnancy and low gestational weight gain. Int J Gynaecol Obstet 2023;162:300–308. DOI: 10.1002/ijgo.14672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wiener RC, Waters C, Bhandari R, Trickett Shockey AK, Alshaarawy O. The association of sleep duration and the use of electronic cigarettes, NHANES, 2015–2016. Sleep Disord 2020;2020:8010923. DOI: 10.1155/2020/8010923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Williams RJ, Wills TA, Choi K, Pagano I. Associations for subgroups of E-cigarette, cigarette, and cannabis use with asthma in a population sample of California adolescents. Addict Behav 2023; 145:107777. DOI: 10.1016/j.addbeh.2023.107777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wills TA, Pagano I, Williams RJ, Tam EK. E-cigarette use and respiratory disorder in an adult sample. Drug Alcohol Depend 2019;194:363–370. DOI: 10.1016/j.drugalcdep.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wills TA, Choi K, Pagano I. E-cigarette use associated with asthma independent of cigarette smoking and marijuana in a 2017 national sample of adolescents. J Adolesc Health 2020;67:524–530. DOI: 10.1016/j.jadohealth.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wills TA, Choi K, Pokhrel P, Pagano I. Tests for confounding with cigarette smoking in the association of E-cigarette use with respiratory disorder: 2020 national-sample data. Prev Med 2022;161: 107137. DOI: 10.1016/j.ypmed.2022.107137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Xie Z, Ossip DJ, Rahman I, Li D. Use of electronic cigarettes and self-reported chronic obstructive pulmonary disease diagnosis in adults. Nicotine Tob Res 2020;22:1155–1161. DOI: 10.1093/ntr/ntz234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Xie W, Kathuria H, Galiatsatos P, et al. Association of electronic cigarette use with incident respiratory conditions among US adults from 2013 to 2018. JAMA Netw Open 2020;3:e2020816. DOI: 10.1001/jamanetworkopen.2020.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Xie Z, Ossip DJ, Rahman I, O’Connor RJ, Li D. Electronic cigarette use and subjective cognitive complaints in adults. PLoS One 2020;15:e0241599. DOI: 10.1371/journal.pone.0241599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Xie W, Tackett AP, Berlowitz JB, et al. Association of electronic cigarette use with respiratory symptom development among U.S. young adults. Am J Respir Crit Care Med 2022;205:1320–1329. DOI: 10.1164/rccm.202107-1718OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhang Z, Jiao Z, Blaha MJ, et al. The association between e-cigarette use and prediabetes: results from the Behavioral Risk Factor Surveillance System, 2016–2018. Am J Prev Med 2022;62: 872–877. DOI: 10.1016/j.amepre.2021.12.009. [DOI] [PubMed] [Google Scholar]
- 140.Zhu H, Wu M. A cross-sectional study on the relationship between electronic cigarette and combustible cigarette use with obstructive sleep apnea among U.S. adults: result from NHANES 2015–2018. Arch Public Health 2023;81:54. DOI: 10.1186/s13690-023-01083-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.National Institutes of Health. PATH: Population Assessment of Tobacco and Health (PATH). 2023. (https://pathstudyinfo.nih.gov/).
- 142.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS). 2023. (https://www.cdc.gov/brfss/index.html).
- 143.Centers for Disease Control and Prevention. Pregnancy Risk Assessment Monitoring System (PRAMS). 2023. (https://www.cdc.gov/prams/index.htm).
- 144.Centers for Disease Control and Prevention. National Health Interview Survey (NHIS). 2023. (https://www.cdc.gov/nchs/nhis/).
- 145.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System (YRBSS). 2023. (https://www.cdc.gov/healthyyouth/data/yrbs/index.htm).
- 146.Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet 2022;399:2227–2242. DOI: 10.1016/S0140-6736(22)00470-6. [DOI] [PubMed] [Google Scholar]
- 147.Jacob P, St Helen G, Yu L, et al. Biomarkers of exposure for dual use of electronic cigarettes and combustible cigarettes: nicotelline, NNAL, and total nicotine equivalents. Nicotine Tob Res 2020;22: 1107–1113. DOI: 10.1093/ntr/ntz235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.U.S. Food and Drug Administration. Scientific review of Modified Risk Tobacco Product Application (MRTPA) Under Section 911(d) of the FD&C Act — Technical Project Lead. June 30, 2020. (https://www.fda.gov/media/139796/download). [Google Scholar]
- 149.Rao P, Han DD, Tan K, et al. Comparable impairment of vascular endothelial function by a wide range of electronic nicotine delivery devices. Nicotine Tob Res 2022;24:1055–1062. DOI: 10.1093/ntr/ntac019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Keith R, Bhatnagar A. Cardiorespiratory and immunologic effects of electronic cigarettes. Curr Addict Rep 2021;8:336–346. DOI: 10.1007/s40429-021-00359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Tarran R, Barr RG, Benowitz NL, et al. E-cigarettes and cardiopulmonary health. Function (Oxf) 2021;2:zqab004. DOI: 10.1093/function/zqab004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Neczypor EW, Mears MJ, Ghosh A, et al. E-cigarettes and cardiopulmonary health: review for clinicians. Circulation 2022;145:219–232. DOI: 10.1161/CIRCULATIONAHA.121.056777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Carnevale R, Sciarretta S, Violi F, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest 2016;150:606–612. DOI: 10.1016/j.chest.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 154.Caporale A, Langham MC, Guo W, Johncola A, Chatterjee S, Wehrli FW. Acute effects of electronic cigarette aerosol inhalation on vascular function detected at quantitative MRI. Radiology 2019;293:97–106. DOI: 10.1148/radiol.2019190562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Fetterman JL, Keith RJ, Palmisano JN, et al. Alterations in vascular function associated with the use of combustible and electronic cigarettes. J Am Heart Assoc 2020;9:e014570. DOI: 10.1161/JAHA.119.014570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Mohammadi L, Han DD, Xu F, et al. Chronic e-cigarette use impairs endothelial function on the physiological and cellular levels. Arterioscler Thromb Vasc Biol 2022;42:1333–1350. DOI: 10.1161/ATVBAHA.121.317749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Qiu H, Zhang H, Han DD, et al. Increased vulnerability to atrial and ventricular arrhythmias caused by different types of inhaled tobacco or marijuana products. Heart Rhythm 2023;20:76–86. DOI: 10.1016/j.hrthm.2022.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Mears MJ, Hookfin HL, Bandaru P, Vidal P, Stanford KI, Wold LE. Electronic nicotine delivery systems and cardiovascular/cardiometabolic health. Circ Res 2023;132:1168–1180. DOI: 10.1161/CIRCRESAHA.123.321565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tattersall MC, Hughey CM, Piasecki TM, et al. Cardiovascular and pulmonary responses to acute use of electronic nicotine delivery systems and combustible cigarettes in long-term users. Chest 2023;164:757–769. DOI: 10.1016/j.chest.2023.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gotts JE, Jordt SE, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ 2019;366:l5275. DOI: 10.1136/bmj.l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kelesidis T, Tran E, Nguyen R, Zhang Y, Sosa G, Middlekauff HR. Association of 1 vaping session with cellular oxidative stress in otherwise healthy young people with no history of smoking or vaping: a randomized clinical crossover trial. JAMA Pediatr 2021; 175:1174–1176. DOI: 10.1001/jamapediatrics.2021.2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Holliday R, Chaffee BW, Jakubovics NS, Kist R, Preshaw PM. Electronic cigarettes and oral health. J Dent Res 2021;100:906–913. DOI: 10.1177/00220345211002116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Herrington JS, Myers C. Electronic cigarette solutions and resultant aerosol profiles. J Chromatogr A 2015;1418:192–199. DOI: 10.1016/j.chroma.2015.09.034. [DOI] [PubMed] [Google Scholar]
- 164.Noël A, Hossain E, Perveen Z, Zaman H, Penn AL. Sub-ohm vaping increases the levels of carbonyls, is cytotoxic, and alters gene expression in human bronchial epithelial cells exposed at the air-liquid interface. Respir Res 2020;21:305. DOI: 10.1186/s12931-020-01571-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Yan B, Zagorevski D, Ilievski V, et al. Identification of newly formed toxic chemicals in E-cigarette aerosols with Orbitrap mass spectrometry and implications on E-cigarette control. Eur J Mass Spectrom (Chichester) 2021;27:141–148. DOI: 10.1177/14690667211040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Dai H, Benowitz NL, Achutan C, Farazi PA, Degarege A, Khan AS. Exposure to toxicants associated with use and transitions between cigarettes, e-cigarettes, and no tobacco. JAMA Netw Open 2022;5:e2147891–e2147891. DOI: 10.1001/jamanetworkopen.2021.47891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Goniewicz ML, Smith DM, Edwards KC, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes. JAMA Netw Open 2018;1:e185937. DOI: 10.1001/jamanetworkopen.2018.5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kim J, Lee S. Daily cigarette consumption and urine cotinine level between dual users of electronic and conventional cigarettes, and cigarette-only users. J Psychoactive Drugs 2020;52:20–26. DOI: 10.1080/02791072.2019.1706791. [DOI] [PubMed] [Google Scholar]
- 169.Carpenter MJ, Wahlquist AE, Dahne J, et al. Effect of unguided e-cigarette provision on uptake, use, and smoking cessation among adults who smoke in the USA: a naturalistic, randomised, controlled clinical trial. EClinicalMedicine 2023;63:102142. DOI: 10.1016/j.eclinm.2023.102142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tretli S, Lund-Larsen PG, Foss OP. Reliability of questionnaire information on cardiovascular disease and diabetes: cardiovascular disease study in Finnmark county. J Epidemiol Community Health 1982;36:269–273. DOI: 10.1136/jech.36.4.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 2004; 57:1096–1103. DOI: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 172.Barr RG, Herbstman J, Speizer FE, Camargo CA Jr. Validation of self-reported chronic obstructive pulmonary disease in a cohort study of nurses. Am J Epidemiol 2002;155:965–971. DOI: 10.1093/aje/155.10.965. [DOI] [PubMed] [Google Scholar]
- 173.Radeos MS, Cydulka RK, Rowe BH, Barr RG, Clark S, Camargo CA Jr. Validation of self-reported chronic obstructive pulmonary disease among patients in the ED. Am J Emerg Med 2009;27:191–196. DOI: 10.1016/j.ajem.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Mahoney MC, Rivard C, Hammad HT, et al. Cardiovascular risk factor and disease measures from the Population Assessment of Tobacco and Health (PATH) study. Int J Environ Res Public Health 2021;18:7692. DOI: 10.3390/ijerph18147692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.U.S. Food and Drug Administration. PMTA Coversheet: Technical Project Lead Review (TPL) of PMTAs PM0000424-PM0000426, PM0000479. April 29, 2019. (https://www.fda.gov/media/124247/download).
- 176.Meshnick AB, Faricy LE, Lushniak BD. Analysis of FDA’s Vuse market authorisation: limitations and opportunities. Tob Control 2023. February 9 (Epub ahead of print). DOI: 10.1136/tc-2022-057540. [DOI] [PubMed] [Google Scholar]
- 177.Hirschtick JL, Mattingly DT, Cho B, et al. Exclusive, dual, and polytobacco use among US adults by sociodemographic factors: results from 3 nationally representative surveys. Am J Health Promot 2021;35:377–387. DOI: 10.1177/0890117120964065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wang RJ, Bhadriraju S, Glantz SA. E-cigarette use and adult cigarette smoking cessation: a meta-analysis. Am J Public Health 2021;111:230–246. DOI: 10.2105/AJPH.2020.305999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Hedman L, Galanti MR, Ryk L, Gilljam H, Adermark L. Electronic cigarette use and smoking cessation in cohort studies and randomized trials: a systematic review and meta-analysis. Tob Prev Cessat 2021;7:62. DOI: 10.18332/tpc/142320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Osibogun O, Bursac Z, Maziak W. Longitudinal transition outcomes among adult dual users of e-cigarettes and cigarettes with the intention to quit in the United States: PATH study (2013–2018). Prev Med Rep 2022;26:101750. DOI: 10.1016/j.pmedr.2022.101750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Chen R, Pierce JP, Leas EC, et al. Effectiveness of e-cigarettes as aids for smoking cessation: evidence from the PATH Study cohort, 2017–2019. Tob Control 2023;32:e145–e152. DOI: 10.1136/tobaccocontrol-2021-056901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


