Abstract
Introduction
This study investigated the effects of automatic dual rotational Risley prisms (ADRRPs), a mobile phone application-operated device, on vergence abilities in young adults.
Methods
Fifty-six participants aged 20–24 performed vergence exercises. The test group used prisms with power changes from 30Δ base-out to 10Δ base-in, while the control group used plano lenses for 10 min. Ophthalmic examinations included lateral heterophoria, near point of convergence (NPC), vergence facility (VF), negative fusional vergence (NFV), and positive fusional vergence (PFV), all measured before and after the vergence exercises. Pre- and post-test results were analyzed using a paired sample t test. Additionally, three cases with convergence insufficiency (CI) performed similar exercises for 12 weeks.
Results
Participants were divided into the test group (n = 39; age 21.82 ± 1.10 years) and control group (n = 17; age 20.53 ± 0.51 years). In the test group, NPC improved from 6.11 ± 2.52 cm to 5.77 ± 2.30 cm (p = 0.023). VF increased from 13.75 ± 4.10 cpm to 16.50 ± 4.42 cpm (p = 0.007). PFV at 6 m and 0.4 m increased from 19.49 ± 6.77∆ to 22.19 ± 6.64∆ (p < 0.001) and 20.51 ± 7.05∆ to 22.69 ± 6.44∆ (p = 0.012), respectively. After 12 weeks, convergence insufficiency symptom survey scores for cases with CI decreased significantly, with NPC improving from 7.0 to 0 cm, 6.0 to 5.8 cm, and 6.0 to 4.7 cm. PFV increased from 10 to 25∆, 20 to 30∆, and 25 to 50∆.
Conclusion
This preliminary study showed the effect of ADRRPs on improving vergence abilities. Further studies are needed to investigate the long-term sustainability and effects in a larger population of individuals with CI of this approach.
Keywords: Automatic dual rotational Risley prisms, Convergence, Vergence abilities, Vergence exercises, Convergence insufficiency
Key Summary Points
| Why carry out this study? |
| Prolonged viewing of digital devices causes a reduction in vergence abilities. Insufficient vergence abilities might lead to visual symptoms such as eye strain, headaches, blurred vision, and diplopia. |
| The present study aims to investigate the effects of vergence exercises on enhancing vergence abilities using a novel app-operated device called automatic dual rotational Risley prisms (ADRRPs). |
| What was learned from the study? |
| The vergence parameters, including the near point of convergence, vergence facility, and positive fusional vergence were improved after 10 min of vergence exercises using the ADRRPs. |
| Using the ADRRPs for vergence exercises could also improve symptoms, breakpoint of near point of convergence, and positive fusional vergence in patients with convergence insufficiency. |
Introduction
Convergence, a crucial visual function involving the coordinated inward movement of both eyes to fuse two separate images when fixating on a nearby object, plays a pivotal role in close-up tasks [1]. In recent years, the demand for near-vision activities has rapidly increased as a result of the prevalent use of digital devices [2]. When the sustainability and strength of the convergence ability are insufficient, it may cause visual symptoms such as eyestrain, headaches, blurred vision, and diplopia [3]. Padavettan et al. [4] indicated that after healthy young adults used smartphones for 30 min, the near point of convergence (NPC) receded by 15.8%, positive fusional vergence (PFV) at near distances decreased by 3.7%, and vergence facility (VF) significantly deteriorated. People struggling to focus on nearby objects may encounter difficulties in performing work-related tasks, engaging in effective learning, and enjoying leisure activities [5, 6].
Vision therapy is an evidence-based and effective approach for enhancing vergence abilities in patients with convergence insufficiency (CI) [7–9]. Prisms are a useful tool for vision therapy for patients with CI to reduce their symptoms and improve the vergence system [8, 10]. Aletaha et al. [8] demonstrated that near exophoria, NPC, PFV, and convergence insufficiency symptom survey (CISS) scores showed significant improvement in patients with CI after they completed vision therapy with over minus lenses and a base-out prism during close work. A previous study indicated that the incidence of CI and CI-related symptoms might increase in the normal binocular vision population as a result of excessive digital device use [11]. In this era of widespread use of electronic products, it is necessary to develop an approach to prevent the potential risk of vergence dysfunctions.
Conventional vergence exercises, such as pencil push-ups and Brock string training [12, 13], are effective but often tedious and time-consuming, resulting in poor compliance. Virtual reality (VR) training methods aim to enhance engagement through gamification [14]; however, the setup costs for general VR systems are relatively high, and there are spatial requirements to consider, along with the risk of eye discomfort and dizziness due to proximity to bright light sources [15]. The automatic dual rotational Risley prisms (ADRRPs) is an app-operated device that utilizes variable prism power for visual assessment and vergence exercises. Patients can watch their preferred videos or games while doing exercise with ADRRPs, making the training course more enjoyable and thus may enhance adherence. This instrument is portable in size, making it more convenient to use and reducing spatial limitations.
The aim of this study is to examine the effects of vergence exercises on the vergence abilities of young adults with or without CI symptoms using ADRRPs.
Methods
Participants
This experimental study was approved by the Institutional Review Board of Chung Shan Medical University Hospital in Taichung, Taiwan (approval number CS2-22,104) and National Taiwan University Hospital in Taipei, Taiwan (approval number 202207058RINB). According to the tenets of the Declaration of Helsinki, the research protocol was well explained to all the participants before obtaining the written informed consent. Additionally, permission for using the participant’s photo was obtained (Fig. 2D).
Fig. 2.
Schematic diagrams of A the ADRRPs, B two pairs of counter-rotating Risley prisms, C the experimental setup of the mobile application, D a participant wearing ADRRPs while engaging in vergence exercises, and E the simulated layouts of the virtual image distance. ADRRPs automatic dual rotational Risley prisms
Inclusion criteria:
Patients between 20 and 40 years of age
Refractive error with spherical power between 0.00 and − 11.00 D
Astigmatism power ≤ − 1.25 D
Monocular best-corrected visual acuity ≤ 0.1 logMAR in both eyes
Stereoacuity < 40 s of arc
Exclusion criteria:
Patients with manifest strabismus
Amblyopia
Anisometropia > 2.0 D
History of intraocular surgery
Ophthalmic or systemic diseases
Initially, 66 optometry students were recruited for this study; however, 10 were excluded for not meeting all the recruitment criteria. We conducted a sample size estimation prior to the study’s commencement. The training group (using ADRRPs) required a larger sample size compared to the control group (using plano lenses). We aimed for a sample size ratio of approximately 2:1 between the training and control groups. Accordingly, 56 patients were randomly assigned: 39 to the training group and 17 to the control group.
In addition, we carried out 12 weeks of vergence exercises and relevant ophthalmic examinations, for three patients with CI, aged 20, 29, and 25, labelled as patients 1, 2, and 3, respectively.
Experimental Procedures
Pre- and post-test ophthalmic examinations were performed on the eligible participants before and after the 10-min vergence exercises, including refractive errors, lateral heterophoria, NPC, VF, negative fusional vergence (NFV), and PFV.
Non-cycloplegic refractive errors were obtained using an open-field autorefractor WAM-5500 (Grand Seiko Co., Ltd., Hiroshima, Japan), and spherical equivalent soft contact lenses (Ticon; St. Shine Optical Co., Ltd., New Taipei City, Taiwan) were given to the participants to achieve a corrected visual acuity of ≤ 0.1 logMAR for each eye during the experiment.
Lateral heterophoria at a distance (6 m) and near (0.4 m) was examined using a modified Thorington card. The Royal Air Force rule measured the NPC thrice. The analysis was conducted using the average breakpoint measurement obtained from three separate measurements. The distance (6 m) and near (0.4 m) NFV and PFV were measured using Risley prisms on a phoropter. Base-in and base-out prisms were continuously placed in front of the eyes of each participant until the participant reported that a single and clear 40/60 Snellen letter became unachievable to obtain the maximum base-in and base-out fusional vergence range. A prism flipper with 3∆Base-in/12∆Base-out at 0.4 m was used to evaluate the VF. Participants were instructed to report when 40/60 Snellen letters on a rock card became single once again. The total number of completed cycles in 1 min was recorded.
In this study, the test group used ADRRPs with rotating prisms, while the control group used plano lenses for the vergence exercises. The ADRRPs were head-mounted and placed in front of the eyes of each participant. The participant watched videos through the ADRRPs at a distance of 0.4 m for 10 min, in which forced divergence and convergence were induced in the participant to fuse the moving images resulting from the combination of the two rotating prisms. The participant was asked to fuse the images during the 10-min exercises. The ophthalmic examination was performed 15 min after the vergence exercise. The 10-min training duration was based on preliminary experiments, which suggested that this duration of vision therapy is sufficient to induce significant changes in vergence abilities [12]. The post-training measurements were taken 15 min after the exercises to avoid transient effects. The flowchart of the study procedures is shown in Fig. 1.
Fig. 1.
Flowchart of the study procedures. ADRRPs automatic dual rotational Risley prisms
In addition, the CISS scores, NPC, and PFV of the three patients with CI were assessed at week 0, 4, 6, and 12. Before starting vergence exercise, the patients wore the ADRRPs device and used the ADRRPs application to measure their breakpoint of PFV. If the PFV breakpoint was n prism dioptres, the Risley prisms were set to continuously and repeatedly rotate, generating horizontal prism dioptres ranging from n + 2 prism dioptres (BO) to (n + 2)/3 prism dioptres [16] during exercise. For example, if the breakpoint was 10ΔBO, the settings would rotate continuously and repeatedly between 12ΔBO and 4ΔBI. The three patients with CI underwent vergence exercise on the ADRRPs system for 15 min per day, three times a week, over 12 weeks.
Design of the ADRRPs
The ADRRPs (OrthoV Co., Ltd., Kaohsiung City, Taiwan) is a head-mounted Risley prism-based visual optical system, and the virtual image is formed at variable positions depending on the rotation angle of the prisms [17]. The system consists of two sets of counter-rotating Risley prism pairs, one set for each eye. Each component of the Risley prism pair is an 8Δ wedge glass, allowing for continuous change of the equivalent prism power between 32ΔBO and 32ΔBI during the operation (Fig. 2A, B). Additionally, the setting of the prism powers, repeat times, and duration of the vergence exercises can be configured using the ADRRPs application on a mobile phone (Fig. 2C) [17].
Vergence Exercises with the ADRRPs
Participants engaged in vergence exercises by viewing a mobile phone screen through the ADRRPs. The phone was positioned approximately 0.4 m in front of the participants, who watched videos of their choice for 10 min (Fig. 2D). While watching the videos, the Risley prisms continuously rotated, generating horizontal prism dioptres (Δ) ranging from 30ΔBO to 10ΔBI. Participants were instructed to fuse the images on the mobile phone screen throughout the exercise.
In this study, the ADRRPs were programmed to smoothly increase the prism dioptre from 0Δ to 30ΔBO over 1000 ms, followed by a 5000-ms duration at 30ΔBO. Subsequently, the 30ΔBO prism gradually shifted to 10ΔBI in 1000 ms and remained at 10ΔBI for 3000 ms. Each cycle took approximately 10 s, and the complete vergence exercise in the study was repeated 60 times within 10 min [17].
The accuracy of the rotation angle of each prism is 0.02° per step, achieved through a combination of gears and motors. The power of the prism is smoothly and continuously adjusted. The relationship between the prism dioptre and rotation angle θ is described by the following sinusoidal function:
| 1 |
A rotation angle of − 90° corresponds to − 32Δ, with the negative sign indicating a BO orientation of the double Risley prism pairs. When the rotation angle (θ) of each prism reaches 0°, the total prismatic power becomes 0, indicating no deviation between the incident and exit rays. At θ values of − 70° or 18°, the prism dioptres correspond to 30ΔBO with a virtual image distance of 130.5 mm, or 10ΔBI with a virtual image distance of 16 m, respectively (Fig. 2E).
Statistical Analysis
SPSS version 22.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis in this study. The differences between pre-test and post-test results were compared using a paired sample t test. The statistical significance was set at a p value < 0.05.
Results
This study recruited a total of 56 eligible participants aged 20–24. In the test group, there were 22 women and 17 men, with a mean age of 21.82 ± 1.10 years. In the control group, there were 8 women and 9 men, with a mean age of 20.53 ± 0.51 years.
In the test group, the mean spherical equivalent (SE) for the right eye was − 4.69 ± 3.12 D, and − 4.60 ± 3.13 D in the left eye. The distance (6 m) lateral heterophoria was 0.18 ± 2.69∆ exophoria, and at near (0.4 m), it was 1.21 ± 6.89∆ exophoria.
In the control group, the mean SE for the right eye was − 4.38 ± 3.02 D, and − 4.23 ± 3.13 D in the left eye. The distance (6 m) lateral heterophoria was 0.76 ± 2.34∆ exophoria, and at near (0.4 m), it was 3.03 ± 2.68∆ exophoria.
The parameters related to vergence abilities, including NPC, VF, and near PFV at baseline, were analyzed for differences between the two groups. The breakpoint of the NPC was 6.11 ± 2.52 cm in the test group and 3.78 ± 3.89 cm in the control group (p = 0.033). The mean VF was 13.75 ± 4.10 cpm in the test group and 14.74 ± 4.05 cpm in the control group (p = 0.552). The PFV at 0.4 m was 20.51 ± 7.05∆ in the test group and 21.07 ± 7.82∆ in the control group (p = 0.816). Although the breakpoint of the NPC at baseline showed a significant difference between the groups, this study focused on evaluating the changes before and after vergence exercises in the same group to assess the effect of training with ADRRPs.
Change in Phoria After the Vergence Exercises with the ADRRPs
The phoria differences after the vergence exercises are shown in Table 1. Although there were phoria shifts following the exercises, none of these shifts reached statistical significance. In Table 1, the average phoria of the test group at a distance (6 m) was 0.18 ± 2.69∆ exophoria, which changed to 0.15 ± 3.04∆ esophoria after the vergence exercises (p = 0.131). Similarly, the average phoria at near (0.4 m) shifted from 1.21 ± 6.89∆ exophoria to 0.65 ± 7.52∆ exophoria after the exercises (p = 0.258). In the control group, the average phoria at a distance (6 m) was 0.74 ± 2.34∆ exophoria, which became 1.79 ± 2.05∆ exophoria after the vergence exercises (p = 0.101). Likewise, the average phoria at near (0.4 m) changed from 3.03 ± 2.68∆ exophoria to 2.03 ± 4.30∆ exophoria (p = 0.258).
Table 1.
Lateral heterophoria at 6 m and 0.4 m before and after the vergence exercises with the ADRRPs
| Phoria (m [∆]) | Test group (n = 39) | p value (t test) | Control group (n = 17) | p value (t test) | ||
|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | |||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| 6 | − 0.18 ± 2.69 | + 0.15 ± 3.04 | 0.131 | − 0.74 ± 2.34 | − 1.79 ± 2.05 | 0.101 |
| 0.4 | − 1.21 ± 6.89 | − 0.65 ± 7.52 | 0.258 | − 3.03 ± 2.68 | − 2.03 ± 4.30 | 0.258 |
(−) exophoria; (+) esophoria
ADRRPs automatic dual rotational Risley prisms, SD standard deviation
Vergence Abilities After the Vergence Exercises with the ADRRPs
The average breakpoint of NPC was 6.11 ± 2.52 cm in the test group. After the vergence exercises, it was significantly reduced to 5.77 ± 2.30 cm (p = 0.023) (Table 2). However, the breakpoint of NPC in the control group was 3.78 ± 3.89 cm, and it receded to 4.19 ± 3.29 cm after the vergence exercises (p = 0.338). The VF in the test group significantly increased from 13.75 ± 4.10 cpm to 16.50 ± 4.42 cpm after the vergence exercises (p = 0.007) (Table 2). Although the VF in the control group increased from 14.74 ± 4.05 cpm to 16.15 ± 6.64 cpm, it did not reach a significant value (p = 0.213).
Table 2.
NPC and VF before and after the vergence exercises with the ADRRPs
| Test group (n = 39) |
p value (t test) |
Control group (n = 17) |
p value (t test) |
|||
|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | |||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| NPC (cm) | 6.11 ± 2.52 | 5.77 ± 2.30 | 0.023 | 3.78 ± 3.89 | 4.19 ± 3.29 | 0.338 |
| VF (cpm) | 13.75 ± 4.10 | 16.50 ± 4.42 | 0.007 | 14.74 ± 4.05 | 16.15 ± 6.64 | 0.213 |
NPC near point of convergence, VF vergence facility, ADRRPs automatic dual rotational Risley prisms, SD standard deviation
For the NFV at both 6 m and 0.4 m, neither group showed a significant difference before and after the vergence exercises (Table 3). Specifically, the NFV at 6 m changed from 7.28 ± 2.15∆ to 7.92 ± 3.24∆ in the test group (p = 0.139), and in the control group, it changed from 15.65 ± 9.36∆ to 12.47 ± 4.98∆ (p = 0.167). At 0.4 m, the NFV in the test group changed from 13.92 ± 4.37∆ to 13.18 ± 5.70∆ (p = 0.210), while in the control group, it shifted from 24.00 ± 8.94∆ to 22.94 ± 7.18∆ (p = 0.489).
Table 3.
NFV and PFV before and after the vergence exercises with the ADRRPs
| Test group (n = 39) |
p value (t test) |
Control group (n = 17) |
p value (t test) |
|||
|---|---|---|---|---|---|---|
| Pre-test | Post-test | Pre-test | Post-test | |||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| NFV (m [∆]) | ||||||
| 6 | 7.28 ± 2.15 | 7.92 ± 3.24 | 0.139 | 15.65 ± 9.36 | 12.47 ± 4.98 | 0.167 |
| 0.4 | 13.92 ± 4.37 | 13.18 ± 5.70 | 0.210 | 24.00 ± 8.94 | 22.94 ± 7.18 | 0.489 |
| PFV (m [∆]) | ||||||
| 6 | 19.49 ± 6.77 | 22.19 ± 6.64 | < 0.001 | 15.18 ± 4.94 | 14.12 ± 5.17 | 0.410 |
| 0.4 | 20.51 ± 7.05 | 22.69 ± 6.44 | 0.012 | 21.07 ± 7.82 | 21.13 ± 4.73 | 0.976 |
NFV negative fusional vergence, PFV positive fusional vergence, ADRRPs automatic dual rotational Risley prisms, SD standard deviation
The PFV in the test group at 6 m significantly increased from 19.49 ± 6.77∆ to 22.19 ± 6.64∆ after the vergence exercises (p < 0.001). In contrast, there was no significant difference in the control group (Table 3). The PFV at 0.4 m in the test group also significantly increased from 20.51 ± 7.05∆ to 22.69 ± 6.44∆ (p = 0.012). Conversely, no significant difference was observed in the control group.
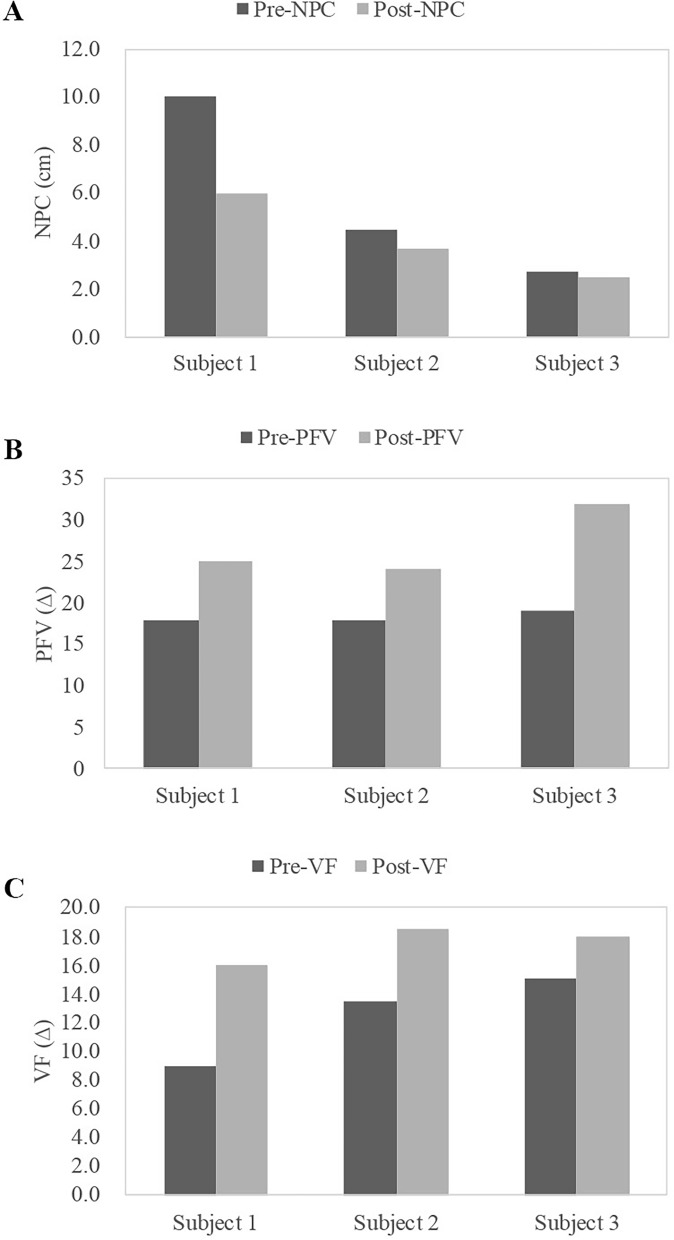
To further understand the impact of vergence exercises on the vergence abilities, we presented the results of three individual patients from the test group before and after the exercises. In Fig. 3A, the breakpoint of the NPC changed from 10 to 6 cm, 4.5 to 3.7 cm, and 2.7 to 2.5 cm. The near PFV improved from 18 to 25∆, 18 to 24∆, and 19 to 32∆ (Fig. 3B). For VF, the changes were from 9 to 16 cpm, 13.5 to 18.5 cpm, and 15 to 18 cpm (Fig. 3C) for patient 1, patient 2, and patient 3, respectively. Notably, the greatest improvement in the NPC and VF was observed in patient 1, while patient 3 showed the most significant improvement in near PFV.
Fig. 3.
Changes in A NPC, B PFV at 0.4 m, and C VF in three individual patients from the test group after vergence exercises. NPC near point of convergence, PFV positive fusional vergence, VF vergence facility
A Preliminary 12-Week ADRRPs Vergence Exercise for Three Patients with CI
The CISS scores, NPC, and near PFV were collected in three patients with CI at week 0, week 4, week 6, and week 12, as shown in Fig. 4. After 12 weeks of exercise, as illustrated in Fig. 4A, the CISS scores for patients 1, 2, and 3 decreased from 32 to 20, 38 to 17, and 28 to 10, respectively. As shown in Fig. 4B, the breakpoint of NPC for patients 1, 2, and 3 improved from 7.0 to 0 cm (to the nose, TTN), 6.0 to 5.8 cm, and 6.0 to 4.7 cm, respectively. The near PFV for patients 1, 2, and 3 increased from 10 to 25∆, 20 to 30∆, and 25 to 50∆, respectively (Fig. 4C).
Fig. 4.
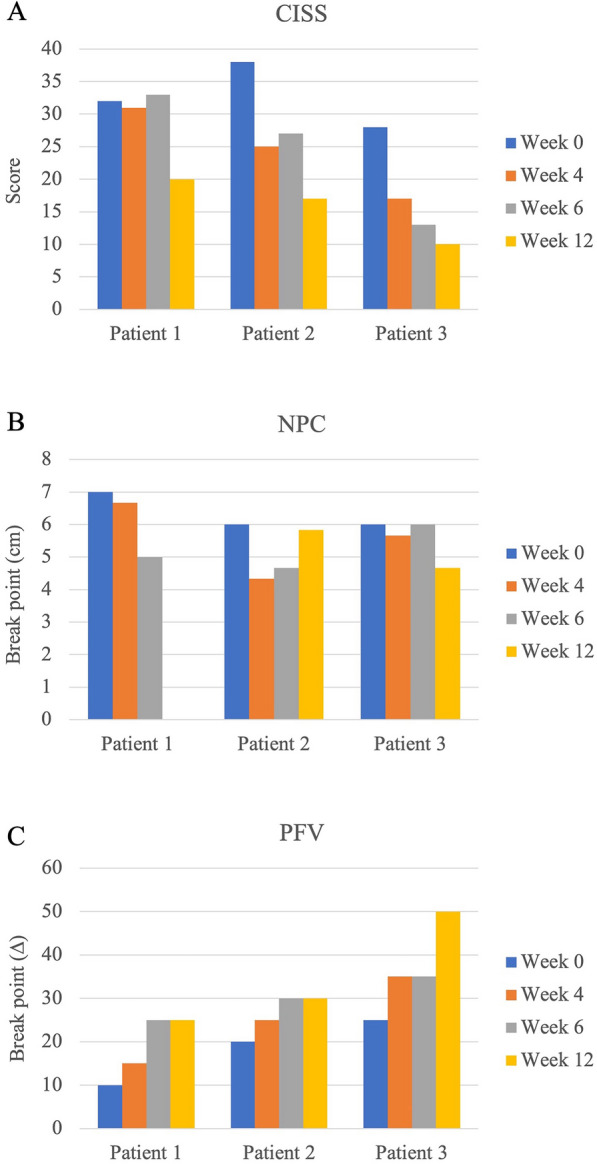
Changes in A CISS scores, B NPC, and C PFV at 0.4 m in three patients with CI at week 0, 4, 6, and 12 following vergence exercises. CISS convergence insufficiency symptom survey, NPC near point of convergence, PFV positive fusional vergence, CI convergence insufficiency
It is noteworthy that after 12 weeks of ADRRPs exercise, all three patients with CI experienced not only a significant reduction in CISS scores, reflecting a decrease in the severity of symptoms associated with CI, but also substantial improvements in convergence functions, including NPC, and PFV.
Discussion
Nowadays, digital devices are widely used in education, the healthcare industry, and leisure entertainment. With the increasingly prevalent use of digital devices, prolonged near-work time has become common in modern society [18]. However, performing excessive near work may cause visual symptoms, including headaches, eyestrain, double vision, and blur, pertinent to dry eye, abnormal eye blinking, or accommodative and vergence dysfunctions [19]. The prevalence of digital eye strain [11, 19] and symptoms related to binocular vision dysfunction [20] increased significantly during the coronavirus disease pandemic. Kang et al. [21] observed an increase in visual symptoms after 1 h of video viewing on tablets or smartphones in healthy non-presbyopic adults, with both the near point of accommodation and NPC aggravated. The near triad and binocular vision functions could be negatively affected with increased duration of using digital devices at near distances [22].
Vision therapy, a non-invasive approach for the management of accommodative and vergence dysfunctions, has been shown to successfully improve binocular vision and reduces visual symptoms [12, 13, 23–25]. In the present study, ADRRPs were used to implement vergence exercises in 39 healthy young adults, providing a convenient home-based vergence exercise regimen. The results showed a significant decrease in the breakpoint of NPC, an increase in the cycles per min of VF, and an increased PFV breakpoint at both 6 m and 0.4 m after 10 min of vergence exercises.
In the Convergence Insufficiency Treatment Trial study, normalizing the breakpoint of NPC and PFV at near distances were two goals of vision therapy for patients with CI [13]. The breakpoint of NPC in this study was measured at 6.11 ± 2.52 cm as the baseline, which significantly improved to 5.77 ± 2.30 cm after the 10-min vergence exercises. Hamed et al. [24] indicated that the mean NPC for the symptomatic group was 11.7 ± 5.0 cm and 8.4 ± 3.4 cm for the asymptomatic group. The present study results suggest that the improvement in the breakpoint of NPC to the recognized expected range after the vergence exercises (≤ 5 cm) [25] might help alleviate vergence dysfunctions. In addition to improve NPC, both the PFV breakpoint at a distance and near significantly improved to within the reasonable expected range for the distant PFV breakpoint (19.0 ± 8.0∆) and near PFV breakpoint (21.0 ± 6.0∆) after the exercises [26]. One of the criteria for diagnosing CI is the failure of Sheard’s criterion in exophoria [26]. According to Sheard’s criterion, the amplitude of fusional reserves opposing the heterophoria should be at least twice the prism dioptre of the deviation angle [27]. To meet this criterion for participants with exophoria, the breakpoint of the base-out prism should be at least two times greater than the deviation angle [28]. Scheiman and Wick indicated that asthenopic symptoms were present in individuals with exophoria having reduced PFV [26] and a failure to meet Sheard’s criterion [29, 30]. Although the average degree of phoria between the pre-tests and post-tests for all participants was not significantly different in this study, the improvement in PFV might help the participants with exophoria reduce the risk of binocular vision dysfunction.
In addition, the VF in this study significantly increased from 13.75 ± 4.10 cpm to 16.50 ± 4.42 cpm after the vergence exercises, surpassing the expected normal value of 15.0 ± 3.0 cpm [26]. Previous studies have shown that the symptomatic population exhibits poorer VF than the asymptomatic population, and there is a positive correlation between visual symptoms and deficits in VF [31, 32]. Moreover, the VF test procedure required the oculomotor system to rapidly adapt to changing fusional demands, which has been found to be associated with reading speed [33]. Dusek et al. [34] found that approximately 18.2% of school-age children with reading difficulties (n = 825) had CI, and that the prevalence of CI was significantly higher in children with reading difficulties than in those without reading problems. They also showed that vision therapy can not only increase VF but also improve reading speed and reduce reading errors [35]. The results of the present study suggest potential benefits for vergence abilities in a normal population and its application to individuals with CI. In this study, we also compared the NPC and PFV between asymptomatic and symptomatic patients. In symptomatic cases, NPC improved from 7.0 to 0 cm (patient 1), 6.0 to 5.8 cm (patient 2), and 6.0 to 4.7 cm (patient 3) after 12 weeks of vergence exercises. PFV increased from 10 to 25∆ (patient 1), 20 to 30∆ (patient 2), and 25∆ to 50∆ (patient 3). In contrast, the asymptomatic group showed a slight decrease in the average NPC breakpoint, from 6.11 ± 2.52 to 5.77 ± 2.30 cm, along with a modest improvement in PFV at near, from 20.51 ± 7.05 to 22.69 ± 6.44∆, after 10 min of exercises. These findings suggest that a 12-week vergence exercise leads to more significant improvements in NPC and PFV, emphasizing that both the duration of the exercises and the presence of symptoms may be the critical factors influencing the training effectiveness. The limitations of this study include the evaluation of the effects of vergence exercises solely on asymptomatic adults after 10 min of using ADRRPs, leaving the long-term effects uncertain.
Conclusion
ADRRPs, a novel app-operated device, has demonstrated the potential to immediately enhance vergence abilities in healthy young adults through vergence exercise. However, it is important to conduct long-term follow-up studies to evaluate the lasting effectiveness of this training. Further research is needed to investigate the long-term sustainability and effects of this approach in a larger population of individuals with CI.
Acknowledgements
We thank the participants of the study.
Medical Writing/Editorial Assistance
The authors used a large language model (ChatGPT) to assist with English editing for this article. We also thank Editage for their English language editing support. Funding for this editing assistance was provided by National Taiwan University Hospital.
Author Contributions
Conceptualization: Ya-Yu Chen and Tzu-Hsun Tsai. Investigation: Yun-Shao Hu and Shuan-Yu Huang. Resources: Shuan-Yu Huang. Data curation: Yun-Shao Hu. Formal analysis: Ya-Yu Chen and Tzu-Hsun Tsai. Software: Yun-Shao Hu. Writing—Original draft preparation: Ya-Yu Chen. Writing—Review and editing: Tzu-Hsun Tsai.
Funding
This study was partially funded by a grant from National Taiwan University Hospital (112-S0205), the National Science and Technology Council (NSTC 112-2314-B-212-001), and the Mackay Medical College (MMC-RD-113-1A-P001). The journal’s Rapid Service Fee will be covered by the grants. The funding organisations had no role in the design or conduct of this research, nor in the decision to submit the manuscript for publication.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of Interest
A Taiwan invention patent (I781072) has been registered for the automatic dual rotational Risley prisms system. Ya-Yu Chen, Yun-Shao Hu, Shuan-Yu Huang and Tzu-Hsun Tsai declare that they have no competing interests.
Ethical Approval
This experimental study was approved by the Institutional Review Board of Chung Shan Medical University Hospital in Taichung, Taiwan (approval number CS2-22104) and National Taiwan University Hospital in Taipei, Taiwan (approval number 202207058RINB). Written informed consent was obtained from all patients. The permission for use the participant’s photo in this study was also obtained (Fig. 2D).
References
- 1.Mestre C, Bedell HE, Diaz-Douton F, Pujol J, Gautier J. Characteristics of saccades during the near point of convergence test. Vision Res. 2021;187:27–40. [DOI] [PubMed] [Google Scholar]
- 2.Gur S, Ron S, Heicklen-Klein A. Objective evaluation of visual fatigue in VDU workers. Occup Med (Lond). 1994;44(4):201–4. [DOI] [PubMed] [Google Scholar]
- 3.Arnoldi K, Reynolds JD. A review of convergence insufficiency: what are we really accomplishing with exercises? Am Orthopt J. 2007;57:123–30. [DOI] [PubMed] [Google Scholar]
- 4.Padavettan C, Nishanth S, Vidhyalakshmi S, Madhivanan N, Madhivanan N. Changes in vergence and accommodation parameters after smartphone use in healthy adults. Indian J Ophthalmol. 2021;69(6):1487–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Porcar E, Montalt JC, Pons AM, Espana-Gregori E. Symptomatic accommodative and binocular dysfunctions from the use of flat-panel displays. Int J Ophthalmol. 2018;11(3):501–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer-related visual symptoms in office workers. Ophthalmic Physiol Opt. 2012;32(5):375–82. [DOI] [PubMed] [Google Scholar]
- 7.Nehad T, Salem T, Elmohamady MN. Combined office-based vergence therapy and home therapy system for convergence insufficiency in egyptian children. Open Ophthalmol J. 2018;12:12–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aletaha M, Daneshvar F, Mosallaei M, Bagheri A, Khalili MR. Comparison of three vision therapy approaches for convergence insufficiency. J Ophthalmic Vis Res. 2018;13(3):307–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheiman M, Kulp MT, Cotter SA, Lawrenson JG, Wang L, Li T. Interventions for convergence insufficiency: a network meta-analysis. Cochrane Database Syst Rev. 2020;12(12):CD006768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nabovati P, Kamali M, Mirzajani A, Jafarzadehpur E, Khabazkhoob M. The effect of base-in prism on vision-related symptoms and clinical characteristics of young adults with convergence insufficiency; a placebo-controlled randomised clinical trial. Ophthalmic Physiol Opt. 2020;40(1):8–16. [DOI] [PubMed] [Google Scholar]
- 11.Mohan A, Sen P, Shah C, Datt K, Jain E. Binocular accommodation and vergence dysfunction in children attending online classes during the COVID-19 pandemic: digital eye strain in kids (DESK) study-2. J Pediatr Ophthalmol Strabismus. 2021;58(4):224–31. [DOI] [PubMed] [Google Scholar]
- 12.Shin HS, Park SC, Maples WC. Effectiveness of vision therapy for convergence dysfunctions and long-term stability after vision therapy. Ophthalmic Physiol Opt. 2011;31(2):180–9. [DOI] [PubMed] [Google Scholar]
- 13.Scheiman M, Mitchell GL, Cotter S, et al. A randomized clinical trial of vision therapy/orthoptics versus pencil pushups for the treatment of convergence insufficiency in young adults. Optom Vis Sci. 2005;82(7):583–95. [DOI] [PubMed] [Google Scholar]
- 14.Li S, Tang A, Yang B, Wang J, Liu L. Virtual reality-based vision therapy versus OBVAT in the treatment of convergence insufficiency, accommodative dysfunction: a pilot randomized controlled trial. BMC Ophthalmol. 2022;22(1):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim HK, Park J, Choi Y, Choe M. Virtual reality sickness questionnaire (VRSQ): motion sickness measurement index in a virtual reality environment. Appl Ergon. 2018;69:66–73. [DOI] [PubMed] [Google Scholar]
- 16.Birnbaum MH, Soden R, Cohen AH. Efficacy of vision therapy for convergence insufficiency in an adult male population. J Am Optom Assoc. 1999;70(4):225–32. [PubMed] [Google Scholar]
- 17.Huang SY, Su HR, Hu YS, et al. Immediate effects of vergence exercises using automatic dual rotational Risley prisms on accommodative lag and facility. Ophthalmol Ther. 2023;12(6):3361–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3(1):e000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheedy JE, Hayes JN, Engle J. Is all asthenopia the same? Optom Vis Sci. 2003;80(11):732–9. [DOI] [PubMed] [Google Scholar]
- 20.Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clin Exp Optom. 2021;104(6):698–704. [DOI] [PubMed] [Google Scholar]
- 21.Kang JW, Chun YS, Moon NJ. A comparison of accommodation and ocular discomfort change according to display size of smart devices. BMC Ophthalmol. 2021;21(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom. 2017;100(2):133–7. [DOI] [PubMed] [Google Scholar]
- 23.Convergence Insufficiency Treatment Trial Study Group. Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Arch Ophthalmol. 2008;126(10):1336–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamed MM, David AG, Marzieh E. The relationship between binocular vision symptoms and near point of convergence. Indian J Ophthalmol. 2013;61(7):325–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scheiman M, Gallaway M, Frantz KA, et al. Nearpoint of convergence: test procedure, target selection, and normative data. Optom Vis Sci. 2003;80(3):214–25. [DOI] [PubMed] [Google Scholar]
- 26.Scheiman M, Wick B. Clinical management of binocular vision: heterophoric, accommodative, and eye movement disorders. 4th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 27.Hatt SR, Leske DA, Mohney BG, Brodsky MC, Holmes JM. Fusional convergence in childhood intermittent exotropia. Am J Ophthalmol. 2011;152(2):314–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lanca CC, Rowe FJ. Measurement of fusional vergence: a systematic review. Strabismus. 2019;27(2):88–113. [DOI] [PubMed] [Google Scholar]
- 29.Sheedy JE, Saladin JJ. Association of symptoms with measures of oculomotor deficiencies. Optom Vis Sci. 1978;55(10):670–6. [DOI] [PubMed] [Google Scholar]
- 30.Wajuihian SO. Correlations between clinical measures and symptoms: report 2: accommodative and vergence measures with symptoms. J Optom. 2021;14(2):142–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng F, Hou F, Chen R, et al. Investigation of the relationship between subjective symptoms of visual fatigue and visual functions. Front Neurosci. 2021;15:686740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Momeni-Moghaddam H, Goss DA, Dehvari A. Vergence facility with stereoscopic and nonstereoscopic targets. Optom Vis Sci. 2014;91(5):522–7. [DOI] [PubMed] [Google Scholar]
- 33.Quaid P, Simpson T. Association between reading speed, cycloplegic refractive error, and oculomotor function in reading disabled children versus controls. Graefes Arch Clin Exp Ophthalmol. 2013;251(1):169–87. [DOI] [PubMed] [Google Scholar]
- 34.Dusek W, Pierscionek BK, McClelland JF. A survey of visual function in an Austrian population of school-age children with reading and writing difficulties. BMC Ophthalmol. 2010;10:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dusek WA, Pierscionek BK, McClelland JF. An evaluation of clinical treatment of convergence insufficiency for children with reading difficulties. BMC Ophthalmol. 2011;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.