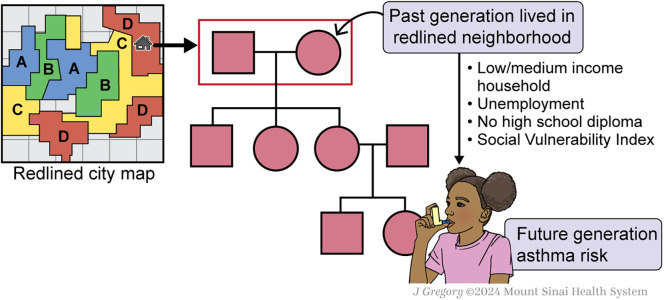
There has been an ever-expanding search for risk factors that determine a child’s risk for developing asthma. Traditional models to explain disease risk, such as gene-by-environment phenomena, have evolved to include a broader spatial landscape of environmental exposures encompassing an individual’s exposome, which individually and/or synergistically contribute to asthma development. Newer paradigms have temporally extended the search for the developmental origins of asthma to the prenatal period, illustrating how child asthma risk may originate before birth from in utero exposures. Yet, the emerging concept that a child’s asthma risk can be traced even further back in time to historical, political, and/or social events directed toward his/her/their ancestors embraces a generational perspective of disease risk apart from purely genetic inheritance (Figure 1). When adverse historical circumstances target specific groups or communities through widespread racist policies, their future children may be hurled onto a path of disadvantage and environmental trauma, contributing to a wide array of health disparities. It is an assurance that the apple will not fall far from the poisoned tree.
Figure 1.
Historical redlining and future pediatric asthma risk.
In this issue of the Journal, Ryan and colleagues (pp. 1201–1209) connect the dots specifically between historical redlining practices of the 1930s and child asthma incidence in the 21st century (1). Redlining was a federally sanctioned, race-based practice by the Home Owners’ Loan Corporation (HOLC) of discriminatory mortgage lending practices toward populations who were deemed credit unworthy, such as Black and immigrant populations (2). The practice resulted in HOLC neighborhoods graded from “A” (best) to “D” (worst or hazardous) quality, with the latter delineated by red lines on maps. This systemic racism created deep lines of residential segregation that subsequently perpetuated a diverse array of socioeconomic and environmental inequities for generations thereafter. Prior work has linked living in historically redlined neighborhoods to higher risks of disease (3), such as adverse obstetric outcomes (4), cancer (5), and asthma morbidity (6–8), compared with living in non-redlined neighborhoods. These relationships emphasize the contribution of structural racism to key health disparities. Now, using census tract data from the Children’s Respiratory and Environmental Workgroup (CREW) birth cohort consortium, Ryan and colleagues examined historical redlining as a root cause of child asthma disparities. Overall, 7 of the 10 CREW sites, representing 67% of the study population, recruited participants from cities listed in the top 10 most populous HOLC redlined areas (2, 9), highlighting the relevance of CREW in addressing these questions (although >50% of CREW participants were born in an ungraded area). Using casual mediation analyses, they found that historical redlining practices contributed to asthma disparities through the mediating effects of neighborhood-level poverty and socioeconomic position (1). Their work adds to our understanding of the pathways that carry forward the immediate impact of race-based institutional policies to asthma incidence in future generations, disproportionately burdening Black, Latinx, and other marginalized children.
Importantly, the primary focus of this study was the association of historical redlining and child asthma and assessment of potential mediating effects, adjusting for confounders such as child race. However, because over time the racial and ethnic composition of many historically redlined areas has changed, it would be interesting to also assess race and ethnicity as potential effect modifiers. This would help to gain insight into whether the historical effects of one measure of structural racism—whether direct or indirect—are manifested to a greater extent in children from racial and ethnic minoritized groups (2). Furthermore, as early childhood maternal socioeconomic exposures are associated with respiratory outcomes in their children (10), studies exploring effects of the degree of redlining of each child’s maternal birth environment, in addition to the child’s birth environment, would provide additional insights into the intergenerational effects of historical redlining and associations with incident asthma in children.
Nevertheless, the implications of this work are significant, as it provides further evidence for how racism acts as an upstream source of adverse health effects in vulnerable populations. Thus far, interpersonal racial discrimination has been one of the most studied forms of racism, acting as a psychosocial stressor and adding to allostatic load (11). However, evidence for the impact of wider structural forms of racism on individual health outcomes is growing, and understanding the mechanisms behind this are critical. Specifically, this work highlights pathways by which racial segregation shapes the entirety of a neighborhood, disproportionately subjecting racially and ethnically minoritized groups to decades of economic deprivation and entrenched inequities in environmental exposures and quality of public service (including education and health) infrastructure. We are now beginning to better understand the consequence of this cascade for present-day child asthma disparities.
Although there is no doubt that the effects of historical racist policies have endured, they are not irrevocable. The identification of mediators in these analyses emphasizes opportunities to uplift neighborhoods as a whole, leveraging the inherent strengths of communities without severing existing social networks and ties. As the authors point out, studies examining the effects of relocating children into higher-income neighborhoods as part of housing mobility programs have been associated with improved asthma morbidity (12) and long-term economic outcomes (13); however, such displacement as a global strategy is less than ideal. Rather, efforts targeted at reducing inequities and increasing investment in previously neglected areas have been shown to improve area economic conditions (11); however, the success of these place-based approaches still needs to be examined through the lens of health outcomes. Furthermore, reparative strategies need to take into consideration originally discriminated populations, who may no longer reside in those neighborhoods but who still carry an imprint of redlining’s influence (9).
Last, but not least, by no means should the term “historical redlining” suggest that racist policies are only a phenomenon of the past. Ongoing race-based exploitation is insidious and continues to manifest in many structural forms and perpetuate segregation, economic deprivation, educational deficit, and environmental injustice among Black and Brown subgroups, even in the absence of overtly racist federal policy. These influences may go unseen in real time; they are not stated in patient charts, and rarely are they acknowledged within clinical encounters. As evidence mounts on the links between neighborhood-level risk factors and determinants of respiratory health disparities, it is time to foster a collective consciousness of both past and present-day systemic factors contributing to respiratory health to ensure a better future for our children.
Footnotes
Originally Published in Press as DOI: 10.1164/rccm.202406-1225ED on July 30, 2024
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Ryan PH, Zanobetti A, Coull BA, Andrews H, Bacharier LB, Bailey D, et al. The legacy of redlining: increasing childhood asthma disparities through neighborhood poverty. Am J Respir Crit Care Med . 2024;210:1201–1209. doi: 10.1164/rccm.202309-1702OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Swope CB, Hernandez D, Cushing LJ. The relationship of historical redlining with present-day neighborhood environmental and health outcomes: a scoping review and conceptual model. J Urban Health . 2022;99:959–983. doi: 10.1007/s11524-022-00665-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kraus NT, Connor S, Shoda K, Moore SE, Irani E. Historic redlining and health outcomes: a systematic review. Public Health Nurs . 2024;41:287–296. doi: 10.1111/phn.13276. [DOI] [PubMed] [Google Scholar]
- 4. Nardone AL, Casey JA, Rudolph KE, Karasek D, Mujahid M, Morello-Frosch R. Associations between historical redlining and birth outcomes from 2006 through 2015 in California. PLoS One . 2020;15:e0237241. doi: 10.1371/journal.pone.0237241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Krieger N, Wright E, Chen JT, Waterman PD, Huntley ER, Arcaya M. Cancer stage at diagnosis, historical redlining, and current neighborhood characteristics: breast, cervical, lung, and colorectal cancers, Massachusetts, 2001-2015. Am J Epidemiol . 2020;189:1065–1075. doi: 10.1093/aje/kwaa045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schuyler A, Wenzel S. Historical redlining impacts contemporary environmental and asthma-related outcomes in black adults. Am J Respir Crit Care Med . 2022;206:824–837. doi: 10.1164/rccm.202112-2707OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nardone A, Casey JA, Morello-Frosch R, Mujahid M, Balmes JR, Thakur N. Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: an ecological study. Lancet Planet Health . 2020;4:e24–e31. doi: 10.1016/S2542-5196(19)30241-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Friedman E, Lee B, Kalman C, Wilson N. Historic racism in Kansas City affects today’s pediatric asthma burden. Health Place . 2022;78:102927. doi: 10.1016/j.healthplace.2022.102927. [DOI] [PubMed] [Google Scholar]
- 9.Perry AM, Harshbarger D. America’s formerly redlined neighborhoods have changed, and so must solutions to rectify them. The Brookings Institute; 2019. https://www.brookings.edu/articles/americas-formerly-redlines-areas-changed-so-must-solutions/ [Google Scholar]
- 10. Sternthal MJ, Coull BA, Chiu YM, Cohen S, Wright RJ. Associations among maternal childhood socioeconomic status, cord blood IgE levels, and repeated wheeze in urban children. J Allergy Clin Immunol . 2011;128:337–345.e1. doi: 10.1016/j.jaci.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet . 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 12. Pollack CE, Roberts LC, Peng RD, Cimbolic P, Judy D, Balcer-Whaley S, et al. Association of a housing mobility program with childhood asthma symptoms and exacerbations. JAMA . 2023;329:1671–1681. doi: 10.1001/jama.2023.6488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chetty R, Hendren N, Katz LF. The effects of exposure to better neighborhoods on children: new evidence from the moving to opportunity experiment. Am Econ Rev . 2016;106:855–902. doi: 10.1257/aer.20150572. [DOI] [PubMed] [Google Scholar]