Abstract
Background:
Musculoskeletal injuries are prevalent in the NBA and are associated with a significant number of games missed. There is a lack of reference data for clinical measures in NBA players, making it difficult for sports medicine professionals to set goals and develop programs.
Hypothesis:
Values for clinical measures in NBA players will differ from those of the general population but will not differ between dominant (D) and nondominant (ND) limbs.
Study Design:
Descriptive laboratory study.
Level of Evidence:
Level 3.
Methods:
Clinical measures were taken on 325 players invited to NBA training camp (2008-2022). Measures included range of motion for great toe extension, hip rotation, weightbearing ankle dorsiflexion, flexibility, arch height (AH) indices, and tibial varum.
Results:
Clinical values for NBA players differ from reference norms of the general population. Results for NBA players include great toe extension (D, 40.4°; ND, 39.3°), 90/90 hamstring (D, 41.5°; ND, 40.9°), hip internal rotation (D, 29.0°; ND, 28.8°), hip external rotation (D, 29.7°; ND, 30.9°), total hip rotation (D, 60.2°; ND, 60.4°), Ely (D, 109.9°; ND, 108.8°), AH difference (D, 0.5 mm; ND, 0.5 mm), AH index (D, 0.310; ND, 0.307), arch stiffness (D, 0.024; ND, 0.024), arch rigidity (D, 0.924; ND, 0.925), tibial varum (D, 4.6°; ND, 4.5°), and weightbearing ankle dorsiflexion (D, 35.4°; ND, 35.6°). Descriptive statistics are presented; 2-tailed paired t tests show that, whereas most measures demonstrated differences between sides, the results were not statistically significant.
Conclusion:
Clinical measures of NBA players differ from those reported for the general population and athletes of other sports although there were no statistically significant differences between D and ND limbs.
Clinical Relevance:
Establishing a reference database may help clinicians develop more sensitive and more effective preseason and return-to-play screening processes, aiding the management of player orthopaedic care and reducing injury risk.
Keywords: basketball, clinical measures, compliance, NBA, ROM, stiffness
Over the last decade, there have been a significant number of games missed in the National Basketball Association (NBA) due to injury.28,43,63 It has been estimated that the direct cost of injuries in the NBA is US$350 million in lost revenue each season.62,63 Many of these injuries are musculoskeletal in nature28,43 and may be related to an inappropriate degree of stiffness and/or compliance in the lower extremities as they relate to tissue stress-strain dynamics.11,12 The concept of stiffness is based on Hooke’s Law, which refers to a tissue’s ability to resist deformation.11,12 Whereas lower extremity stiffness is considered to be a key factor in optimizing running, jumping, and hopping activities, too much stiffness has been associated with reduced joint motion, a decreased ability to absorb forces, and bony injury.4,15,17,72 On the other side of the continuum, too much compliance has been linked to an increased risk for soft tissue injury and muscle strain.11,12,71 Therefore, there appears to be an optimal level of muscle stiffness for athletes that allows them to maximize performance and minimize injury. However, the relationship between stiffness, compliance, and injury risk may not be linear.
Sports medicine professionals utilize a variety of assessments to help understand these factors to make informed decisions about an athlete’s rehabilitation or sports performance program. However, there is a lack of reference data for clinical measures in professional basketball players, making it difficult for sports medicine professionals to set goals, develop programs, and make interventions. In contrast, normative data exists for certain clinical measures for other professional athletes. In Major League Baseball (MLB) players, it has been well established that the degree of shoulder external rotation (ER) range of motion (ROM) (140°) - a reflection of compliance - differs from textbook values that have been reported for the general population (90°).7,10,19,23,24,29,57,58 The relationship between ROM and injury risk has been described for the lower extremity as well.3,9,25,30,31,35,36,40,44,59,64 As such, sports medicine professionals understand that not only are the ROM goals for elite overhead athletes different, but their unique degree of compliance or stiffness is vital for these athletes to perform efficiently and effectively in their sport.
For jumping athletes, it has been noted that measures such as lower extremity flexibility, ROM, and arch height (AH) and rigidity indices reflect the stiffness-compliance continuum that influences performance and functional movement. If a reference database were established and these factors were better understood, more sensitive and effective preseason and return-to-play screening could be adopted.11,12,14,18,21,22,28
The aim of this study is to retrospectively analyze preseason testing measures to establish reference values in professional NBA players.
Methods
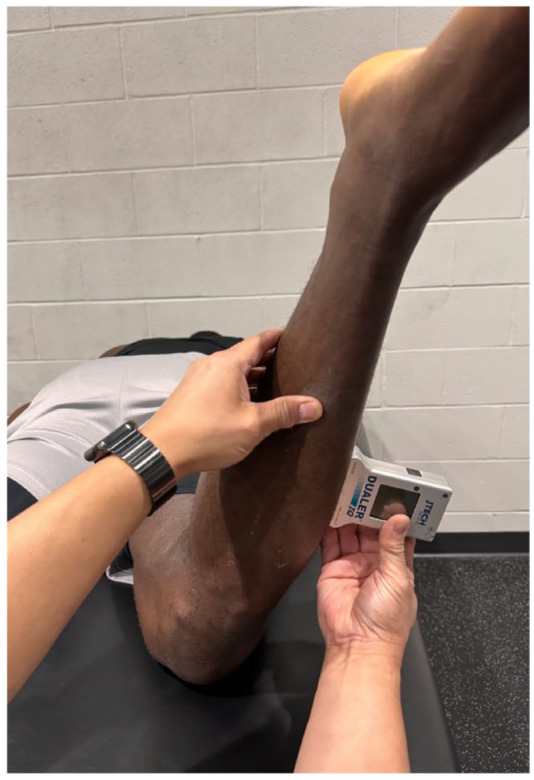
This study was approved by the university Institutional Review Board (IRB). The participants include 325 NBA players from 3 teams who were invited to NBA training camp or were on the roster for the 2008-2022 seasons (age, 25.5 ± 3.9 years; height, 2.00 ± .079 m; weight, 99.89 ± 12.38 kg; body mass index [BMI], 24.66 ± 1.89 kg/m2) In this study, 74.2% of the players were Black, 17.8% where White, 2.1% of the players were Latino of any race, and 5.9% of the players were classified as either multiracial or “other” races. Clinical measures were taken as part of the team’s typical clinical care and assessment program by a single examiner who is a board-certified clinical specialist in orthopaedic physical therapy with >20 years of experience. All research initiatives were retrospective in nature. Data were excluded for players who were injured, rehabilitating an injury, or not cleared by their team medical staffs to participate in preseason assessments. Great toe extension was measured with the subject supine and the test side knee flexed to 90° with the foot flat (Figure 1). Maintaining contact with the plantar surface of the foot on the table, the great toe was extended passively at the metatarsophalangeal joint to the first tissue stop, and ROM was measured with a digital inclinometer.33,39 The arch height index (AHI) measurement system (AHIMS) protocol was utilized to assess the arch in sitting and standing positions (Figure 2).8,16,55,65,68,71,73,74 Measurements were made in a seated position with the subject’s hips and knees flexed to 90°. Using the AHIMS protocol, foot length, truncated position, and AH were recorded. These measures were repeated with the subject standing with maximum pronation. Subsequently, AHI, AH difference, stiffness, and rigidity values were calculated. Weightbearing ankle dorsiflexion was measured with the player facing the wall with the test leg forward and the contralateral limb in-line behind the subject with the heel raised (Figure 3).5,27,40,56,70 The test foot was placed 5 inches from the wall on a taped line so that the heel and the second digit were aligned. The player was then instructed to flex the knee and bring the center of the patella as close to the wall as they could without raising the heel. The degree of ankle dorsiflexion was measured with a digital inclinometer. Hamstring (HS) length was measured with the 90/90 test (Figure 4).33,39 The athlete was positioned supine with the contralateral limb extended with neutral rotation. The test leg was flexed to 90° at the hip and knee. The knee was then extended until the first tissue stop and the ROM was measured with a digital inclinometer. Hip ROM was measured with the subject prone and the contralateral limb in a neutral position (Figure 5).1,33,39 The test leg was flexed at the knee to 90° and moved into internal rotation (IR) and ER for 3 repetitions. The hip was then moved into IR until the first tissue stop without the pelvis raising and ROM was measured with a digital inclinometer. The hip was returned to neutral and then into ER until the first tissue stop and measured with a digital inclinometer. Tibial varum was measured with the athlete standing, feet together, with a digital inclinometer aligned with a line made at the bisection of the distal third of the lower leg (Figure 6).1,33
Figure 1.

Great toe extension measured with the subject supine and knee flexed to 90° with the foot flat.
Figure 2.
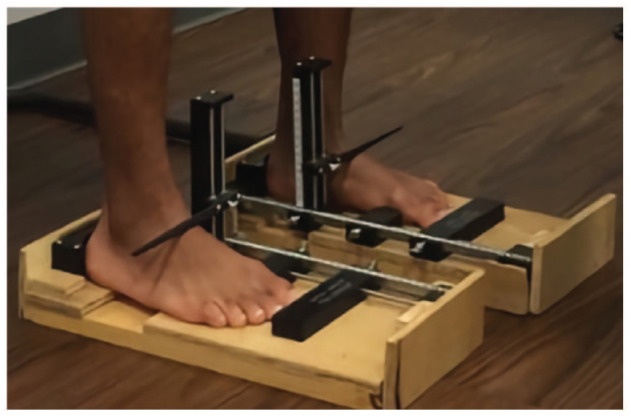
AHI measures were taken to classify arch type and to calculate arch rigidity and stiffness. AHI, arch height index.
Figure 3.
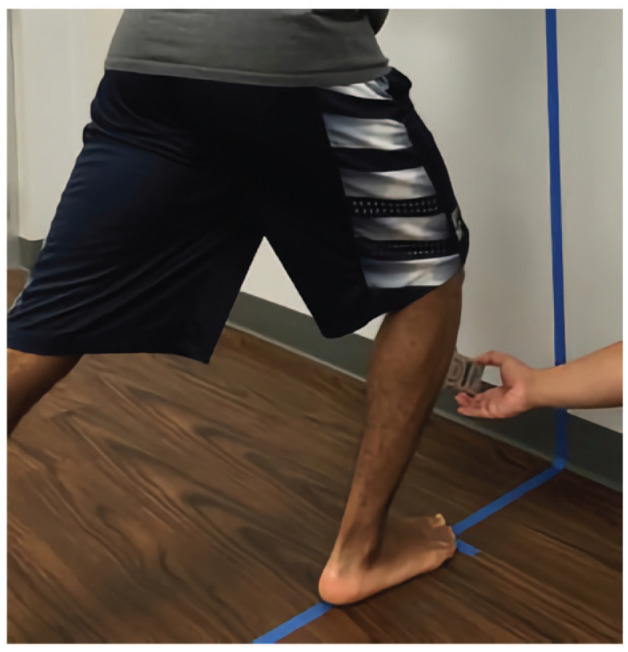
Weightbearing ankle dorsiflexion was measured with tibial advancement without raising of the heel.
Figure 4.
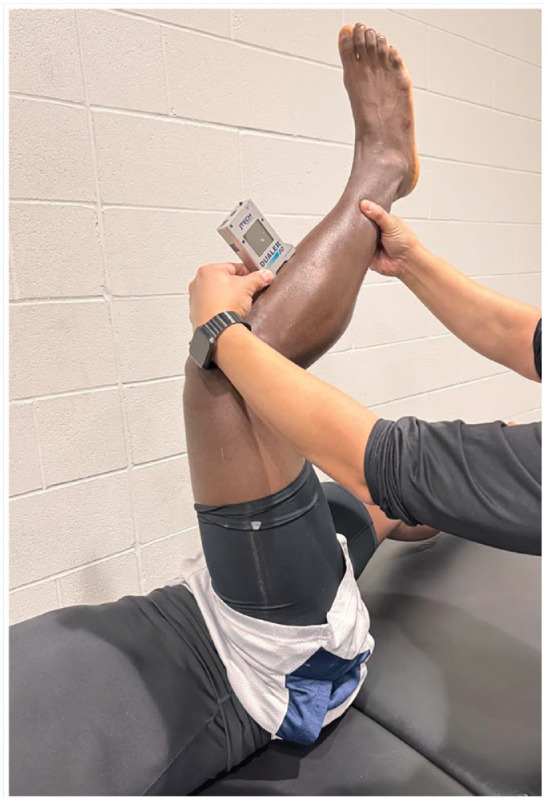
HS flexibility via the 90/90 HS test. HS, hamstring.
Figure 5.
The hip was measured for IR, ER, and total rotation ROM. ER, external rotation; IR, internal rotation; ROM, range of motion.
Figure 6.

Tibial varum.
Data Analysis
Data were retrospectively pooled, analyzed, and correlated using JMP (https://www.jmp.com). Descriptive summary statistics were calculated for all outcome measures, enabling the establishment of the reference values. Inferential statistics were also calculated and t distribution values are presented to demonstrate any significant differences between the dominant (D) and nondominant (ND) side.
Results
The results for all NBA players include great toe extension (D, 40.4°; ND, 39.3°), 90/90 HS (D, 41.5°; ND, 40.9°), hip IR (D, 29.0°; ND, 28.8°), hip ER (D, 29.7°; ND, 30.9°), total hip rotation (D, 60.2°; ND, 60.4°), Ely (D, 109.9°; ND, 108.8°), AH difference (D, 0.5 mm; ND, 0.5 mm), AHI (D, 0.310; ND, 0.307), arch stiffness (D, 0.024; ND, 0.024), arch rigidity (D, 0.924; ND, 0.925), tibial varum (D, 4.6°; ND, 4.5°), and weightbearing ankle dorsiflexion (D, 35.4°; ND, 35.6°). Descriptive statistics for D and ND limbs are tabulated in Table 1.
Table 1.
Descriptive statistics for D and ND limbs
| Significance | Mean Difference | 95% CI of the Difference | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| All | N | D | SD | ND | SD | t Value | df | Lower | Upper | ||
| Great toe extension | 326 | 40.380 | 8.9 | 39.26 | 8.3 | 1.7 | 650.0 | 0.1 | 1.1 | -0.2 | 2.4 |
| 90/90 | 325 | 41.498 | 9.8 | 40.93 | 9.5 | 0.7 | 648.0 | 0.5 | 0.6 | -0.9 | 2.1 |
| Hip IR | 326 | 28.969 | 9.4 | 28.76 | 9.9 | 0.3 | 650.0 | 0.8 | 0.2 | -1.3 | 1.7 |
| HIP ER | 326 | 29.690 | 8.9 | 30.87 | 8.8 | 1.7 | 650.0 | 0.1 | -1.2 | -2.5 | 0.2 |
| Total hip rotation ROM | 326 | 60.230 | 12.2 | 60.42 | 12.6 | 0.2 | 650.0 | 0.8 | -0.2 | -2.1 | 1.7 |
| Ely’s test | 208 | 109.856 | 16.3 | 108.82 | 14.8 | 0.7 | 414.0 | 0.5 | 1.0 | -2.0 | 4.0 |
| Arch height difference | 314 | 0.475 | 0.2 | 0.472 | 0.2 | 0.2 | 626.0 | 0.8 | 0.0 | 0.0 | 0.0 |
| AHI | 314 | 0.310 | 0.0 | 0.307 | 0.0 | 1.5 | 626.0 | 0.1 | 0.0 | 0.0 | 0.0 |
| Arch stiffness | 314 | 0.024 | 0.0 | 0.024 | 0.0 | 0.6 | 626.0 | 0.5 | 0.0 | 0.0 | 0.0 |
| Arch rigidity | 315 | 0.924 | 0.1 | 0.925 | 0.1 | 0.1 | 628.0 | 0.9 | 0.0 | 0.0 | 0.0 |
| Tibial varum | 320 | 4.578 | 3.0 | 4.52 | 3.1 | 0.2 | 638.0 | 0.8 | 0.1 | -0.4 | 0.5 |
| Weightbearing ankle dorsiflexion | 317 | 35.378 | 5.3 | 35.58 | 5.7 | 0.5 | 632.0 | 0.6 | -0.2 | -1.1 | 0.7 |
AHI, arch height index; D, dominant; ER, external rotation; IR, internal rotation; ND, nondominant; ROM, range of motion.
Two-tailed paired t tests were run comparing the D and ND clinical measures. Whereas the majority of these measures demonstrated differences between sides, the results were not statistically significant (Table 1).
Discussion
Many decisions in sports medicine and performance practice are based on clinical values, despite the fact that athletes from different sports have anatomic and physiological characteristics that lead to associated variance in their measures. Establishing a reference database of select clinical measures in specific athletic populations may be important in distinguishing the interpretation between normal variance, being advantageous to performance, or pathological versus subgroup variance. The absence of reference clinical data can lead to challenges in understanding how the interpretation of measures associated with preparticipation screening relates to risk stratification, the creation of injury prevention programs, and setting appropriate rehabilitation or performance goals.49,50,53,54,61 Of specific interest are measures that have been identified as risk factors in athletes and clinical patterns that have been identified by experienced practitioners.15,24,46,64,70
Lower extremity mobility and flexibility in basketball athletes influences performance and risk of lower quarter injury. These factors may be related to a less-than-optimal degree of stiffness and/or compliance. Stiffness has been described as the resistance of a structure to deform in response to an applied force.15,37,52 Athletic performance in tasks associated with sports, such as hopping, jumping, running, and change of direction, have been shown to be influenced by global stiffness characteristics of the lower extremity. Compliance is viewed as the inverse of stiffness and is found on the other end of the structural deformity continuum. A compliant tissue is more easily deformed under load. 13
Overall, the current study suggests that professional basketball players have less range of motion, decreased flexibility, and increased stiffness compared with the general population (Table 2). An athlete who demonstrates greater stiffness characteristics should be able to store more elastic energy when contacting the ground during the yielding phase of jumping and, thus, generate a higher level of concentric force output when pushing off. It is logical that professional basketball players present with different structural characteristics than the general population.
Table 2.
Basketball players have less range of motion, decreased flexibility, and increased stiffness compared with the general population
| All | D | ND | General Population | Sources |
|---|---|---|---|---|
| Great toe extension | 40.38° | 39.261° | 50°-65° | Kendall, 33 Magee 39 |
| 90/90 | 41.49° | 40.938° | 20°-30° | Kendall, 33 Magee 39 |
| Hip IR | 28.96° | 28.76° | 45° | American Academy of Orthopaedic Surgeons, 1 Kendall, 33 Magee 39 |
| HIP ER | 29.69° | 30.87° | 45° | |
| Total hip rotation ROM | 60.23° | 60.42° | 90° | |
| Ely test | 109.85° | 108.82° | 120°-125° | Kendell, 33 Magee 39 |
| Arch height difference | 0.475 | 0.472 | NA | |
| AHI | 0.310 | 0.307 | 0.326-0.350 | Bjelopetrovich and Barrios, 8 Butler et al, 16 Pohl et al, 55 Tipnis et al, 65 Weimar and Shroyer, 66 Williams et al, 71 Zhao et al, 73 Zifchock et al 74 |
| Arch stiffness |
0.024 | 0.024 | 0.031 | Tipnis et al, 65 Zhao et al, 73 |
| Arch rigidity | 0.924 | 0.925 | 0.903-0.913 | Tipnis et al, 65 Zhao et al, 73 |
| Tibial varum | 4.57° | 4.525° | 4°-6° | American Academy of Orthopaedic Surgeons, 1 Kendall, 33 Magee39 |
| Weightbearing ankle dorsiflexion | 35.37° | 35.58° | 50°-56.3° | Dill et al, 27 Rabin et al 56 |
AHI, arch height index; D, dominant; ER, external rotation; IR, internal rotation; ND, nondominant; ROM, range of motion.
Lower value represents greater degree of compliance.
Lower value is more stiff.
Higher value is more stiff.
The American Academy of Orthopaedic Surgeons 1 reports a mean hip internal and external ROM of 45°, but athletes from various sports have been shown to have hip IR values between 26° and 36° and ER values ranging from 39° to 44°.3,35,36,44,64 The current study found the mean degree of hip IR and ER for NBA players to be about 29° and 30°, respectively. It has been reported that decreased ROM is a risk factor for groin pain if the combined hip rotation ROM is <85°. 64 Cam morphology and dysfunction such as femoral acetabular impingement has been linked with limitations in hip ROM.36,44 It has been reported that male athletes participating in specific high-level impact sports such as basketball are at increased risk of physeal abnormalities of the anterosuperior head-neck junction, and are 1.9 to 8.0 times more likely to develop a cam deformity than male controls. 47 However, the exact relationship between hip structure and pain is unclear. 31 In fact, increased stiffness at the hip joint may be an advantage in sport performance, and athletes have been identified as having mean rotational and combined motion <85°.3,36,44 Hockey players have demonstrated a mean total hip rotational ROM of 70°, 44 and soccer players have shown a mean of 75°. 36 The mean degree of total hip rotation ROM in our study was 60°. This may suggest that professional basketball players have a stiffer hip joint, which may be advantageous with regard to their ability to pivot quickly and change direction during basketball play or, alternatively, this motion loss could be an acquired characteristic similar to the loss of IR of the throwing shoulder in baseball pitchers. 10
The 90/90 test has been described as a measure of HS flexibility with the general population presenting with a mean popliteal angle of 20°.33,39 The NBA players in the current study demonstrated less flexibility, with a mean of 41.5° and 40.9° on D and ND limbs, respectively. Similarly, the Ely test is commonly used as a measure of rectus femoris flexibility with a positive sign being the inability to bring the heel of the test leg to the ipsilateral buttock.33,39 The mean value of knee flexion in the current study during Ely tests was about 109°, with the inability to meet the criteria for the test as noted. These measures are in alignment with the overall presentation of elite NBA players such that their lower extremity musculature appears to be less compliant and more stiff compared with the general population. It is well recognized that HS and quadriceps work synergistically to dynamically stabilize the knee joint during athletic activities, especially acceleration and deceleration.25,27,42,65
Tibial varum values in the general population have been reported at between 4° and 6°.1,33,39 The athletes in this study demonstrated a mean of 4.5° bilaterally. An optimal degree of tibial varum may be important to elite basketball players because there may be an increased risk for injury at each extreme. A low degree of tibial varum is associated with genu valgus and can lead to excessive frontal plane motion at the knee, which is commonly associated with patellofemoral dysfunction and medial collateral ligament or anterior cruciate ligament (ACL) injuries. 66 Likewise, an extreme degree of tibial varum is associated with a decreased ability to absorb ground reaction forces and has been linked to stress fractures, lateral ankle sprains, and degenerative joint disease. 6 The current study also demonstrated that the vast majority (>97%) of NBA players assessed presented with genu varus.
Dominant limb weightbearing ankle dorsiflexion in the general population has been shown to mean 50° with an ND side mean as high as 56.3°.27,56 Limitations in ankle motion have been associated with injury risk such as ACL rupture, patellofemoral pain syndrome, or ankle sprains.9,30,51
In female volleyball athletes, <45° ankle motion had a strong correlation with patellar tendinopathy. 40 However, the optimal degree of stiffness does appear to vary for athletes of different sports. 5 The current study found that professional basketball players have a mean 35.4° on the D limb and 35.6° on the ND side. Increased stiffness in the gastroc-soleus complex can be considered an advantage for jumping athletes because this tissue modulus offers a higher level of elastic energy and spring required to propel off the ground.11-12,15,37,72
Foot type may be associated with both performance and injury risk. A change in foot type may occur as an adaptation to physical demands. A large and planus foot may be associated with the athletic population. 73 Foot type may be predictive of function during athletic tasks such as running. 2 The AHIMS has been utilized to classify foot type and describe arch rigidity and stiffness.8,16,55,65,68,71,73,74 The mean AHI measures in this study were 0.310 (D) and 0.307 (ND). These values are much lower than what has been reported in the general population (0.338-0.343) and suggest that the mean NBA player foot type is pes planus.55,68,74 The mean arch rigidity index (ARI) values and arch stiffness (AS) values for our subjects were found to be 0.925 (ARI) and 0.024 (AS), respectively, suggesting that the typical NBA player has an arch that is more stiff and rigid compared with the general population.16,65,74 A predominant foot type for performance by way of improved force production may come at the expense of other physical attributes such as balance, and may predispose players to certain pathologies due to its unbalanced position on the stiffness-compliance spectrum. 16
The kinetic chain relationship of stiffness and compliance throughout the lower extremity should be considered when reviewing clinical measures. Athletes may develop functional adaptations or biomechanically self-select toward a specific sport. We hypothesize that a stiff and planus foot with limited weightbearing ankle dorsiflexion may provide an athlete a stiffer spring to generate force and create a competitive advantage. Similarly, reduced mobility in the hips may be a driver of multiplanar force generation. The joint measures have been shown to influence movement at a fundamental and functional level. 20 Specifically, local mobility limitations at the ankle and hip have been shown to be associated with changes in multijoint movements such as squatting and lunging.20,21,32,34,38 Further, morphological and mobility limitations may impact balance and multiplanar single leg control. 48 The multifactorial relationship of various clinical measures on the movement system may be combined to assess the risk or association with future injury. 42 Further analysis in different athletic populations may determine whether the relationships between various clinical measures have direct implications on specific sporting populations as they relate to performance, injury risk, and return to performance after injury.
Our analyses did not demonstrate any statistically significant differences between D and ND side. This finding is of note because side-to-side ROM differences have been documented in other sports. Asymmetrical glenohumeral ROM in professional baseball pitchers is well established,7,10,19,23,24,29,57,58 whereas American college football players show no lower extremity ROM differences in D versus ND limb or across positions. 25 Male field hockey players were found to have no clinically relevant differences in hip ROM between D or ND leg or different playing positions. 3 In elite soccer academy players, higher ROM values were found in D versus ND hip ROM, whereas playing position yielded no differences. Interestingly, in professional soccer players, leg dominance did not yield side-to-side ROM differences. 44
Although there may be a perception that basketball players prefer to jump and pivot off 1 leg, our findings suggest that this preference does not impact D versus ND side-to-side ROM values but may be better explained by positional demands and body type. In today’s NBA, certain positions demand more frequent sprints at full speed, more frequent and abrupt changes of direction, and more repetitive jumping and intense deceleration, all of which can impact body stresses and subsequent ROM. Our results suggest that leg dominance may not need to be accounted for when examining injury risk. We would suggest that positional demands and subsequent movement strategies specific to those demands account for ROM differences between professional basketball players.
In elite sport, overdiagnosis is always a risk given the ready access to diagnostic capabilities via imaging, movement assessments, and a seemingly endless choice of technologies promising to reduce injuries. 26 These data, often not clinically meaningful or fully understood, should lead clinicians to be cautious that it does not lend itself to overdiagnosis of the athlete. Overdiagnosis occurs when an abnormality is diagnosed correctly (ie, limited dorsiflexion) but the abnormality or diagnosis is irrelevant.45,67
Our hope is that proper understanding of these reference values, combined with an athlete’s history and physical exam, will better inform clinicians as they develop an evidence-based plan of care. Incorrectly labeling an athlete as high risk is unfair to the athlete and may lead clinicians down an incorrect and inefficient plan of care. This reference database decreases instances of overdiagnosis and frees clinicians up from unnecessary treatment strategies. 41
Limitations
In line with clinical practice patterns, we used a digital inclinometer to measure ROM without any stabilization equipment (ie, belts). Additional stabilization would improve the validity and/or reliability of these measurements. Although all measures were taken by a single examiner, due to time constraints we did not determine intrarater reliability measures. The findings of this study are also specific to NBA players and should be applied accordingly. The measures are not generalizable to other populations including women, or high school or collegiate players, etc. Unfortunately, we were unable to identify a database that contained these measures of persons from the general population that were of a similar height, weight, and body composition as the NBA players in this study. A limitation of this investigation is that the reference database was the more heterogeneous “general population.” In addition, although we attempted to represent a wide spectrum of NBA players from 3 teams over many seasons, it is likely that selection bias occurred regarding the type of player each team prefers (athletic vs strong vs long, etc).
Conclusion
The findings of this study support the hypothesis that NBA players present with clinical measures that are different from textbook values reported for the general population and athletes of other sports. Establishing a reference database for elite basketball players is relevant clinically and regarding performance because values that most accurately represent the physical characteristics of the player can give insight into their anatomic, biomechanical, and physiological make-up.
Lower extremity injury in elite basketball players is a significant problem for athletes, coaches, medical and performance staff members, and their teams. 28 The identification of modifiable risk factors is essential for injury prevention and management of player health. 60 Establishing a reference database for elite basketball players may play an important role in the management of the player’s orthopaedic care and in reducing subsequent risk. By understanding these reference values, clinicians can better assess risk (or lack thereof) and mitigate unnecessary anxiety for both the athlete and clinician on clinical findings that may be abnormal for a normal population but are very well the norm in elite basketball players.
Requisite mobility norms for professional basketball players are not well quantified, nor is the effect, or lack thereof, of limb dominance on these reference values. Understanding these values, in addition to the impact of sport-specific joint kinematics and strength, may play a role in identifying athletes that carry higher susceptibility to acute or chronic orthopedic conditions. 69 This information may lead the clinician to a more detailed and efficient plan of care.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
ORCID iD: Philip A. Anloague  https://orcid.org/0000-0003-0054-3702
https://orcid.org/0000-0003-0054-3702
References
- 1. American Academy of Orthopaedic Surgeons. Joint Motion: Method of Measuring and Recording. Chicago, IL: American Academy of Orthopaedic Surgeons; 1965. [Google Scholar]
- 2. Bade MB, Aaron K, McPoil TG. Accuracy of self-reported foot strike pattern in intercollegiate and recreational runners during shod running. Int J Sports Phys Ther. 2016;11(3):350-355. [PMC free article] [PubMed] [Google Scholar]
- 3. Beddows TPA, van Klij P, Agricola R, et al. Normal values for hip muscle strength and range of motion in elite, sub-elite and amateur male field hockey players. Phys Ther Sport. 2020;46:169-176. doi: 10.1016/j.ptsp.2020.08.014 [DOI] [PubMed] [Google Scholar]
- 4. Bell DR, Smith MD, Pennuto AP, Stiffler MR, Olson ME. Jump-landing mechanics after anterior cruciate ligament reconstruction: a landing error scoring system study. J Athl Train. 2014;49(4):435-441. doi: 10.4085/1062-6050-49.3.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bennell K, Talbot R, Wajswelner H, Techovanich W, Kelly D, Hall A. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aus J Physiother. 1998;44(3):175-180. [DOI] [PubMed] [Google Scholar]
- 6. Beynnon B, Renström P, Alosa D, Baumhauer J, Vacek P. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19(2):213-220. [DOI] [PubMed] [Google Scholar]
- 7. Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25(5):609-613. [DOI] [PubMed] [Google Scholar]
- 8. Bjelopetrovich A, Barrios JA. Effects of incremental ambulatory-range loading on arch height index parameters. J Biomech. 2016;49(14):3555-3558. doi: 10.1016/j.jbiomech.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 9. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome the joint undertaking to monitor and prevent ACL injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Borsa PA, Dover GC, Wilk KE, Reinold MM. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38:21-26. [DOI] [PubMed] [Google Scholar]
- 11. Brazier J, Bishop C, Simons C, Antrobus M, Read PJ, Turner AN. Lower extremity stiffness: effects on performance and injury and implications for training. Strength Condit J. 2014;36(5):103-112. [Google Scholar]
- 12. Brazier J, Maloney S, Bishop C, Read PJ, Turner AN. Lower extremity stiffness: considerations for testing, performance enhancement, and injury risk. J Strength Condit Res. 2019;33(4):1156-1166. [DOI] [PubMed] [Google Scholar]
- 13. Brughelli M, Cronin J. Influence of running velocity on vertical, leg and joint stiffness: modelling and recommendations for future research. Sports Med. 2008;38(8):647-657. [DOI] [PubMed] [Google Scholar]
- 14. Butler RJ, Contreras M, Burton LC, Plisky PJ, Goode A, Kiesel K. Modifiable risk factors predict injuries in firefighters during training academies. Work. 2013;46(1):11-17. [DOI] [PubMed] [Google Scholar]
- 15. Butler R, Crowell H, III, Davis I. Lower extremity stiffness: implications for performance and injury. Clin Biomech (Bristol, Avon). 2003;18(6):511-517. [DOI] [PubMed] [Google Scholar]
- 16. Butler RJ, Hillstrom H, Song J, Richards CJ, Davis IS. Arch height index measurement system - establishment of reliability and normative values. J Am Podiatr Med Assoc. 2008;98(2):102-106. [DOI] [PubMed] [Google Scholar]
- 17. Cameron KL, Peck KY, Davi SM, et al. Association between landing error scoring system (less) items and the incidence rate of lower extremity stress fracture. Orthop J Sports Med. 2022;10(6):23259671221100790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chapman RF, Laymon AS, Arnold T. Functional movement scores and longitudinal performance outcomes in elite track and field athletes. Int J Sports Physiol Perf. 2014;9(2):203-211. [DOI] [PubMed] [Google Scholar]
- 19. Chant CB, Litchfield R, Griffin S, Thain LMF. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. J Orthop Sports Phys Ther. 2007;37(9):514-520. [DOI] [PubMed] [Google Scholar]
- 20. Chimera NJ, Knoeller S, Cooper R, Kothe N, Smith C, Warren M. Prediction of functional movement screen™ performance from lower extremity range of motion and core tests. Int J Sports Phys Ther. 2017;12(2):173-181. [PMC free article] [PubMed] [Google Scholar]
- 21. Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. North Am J Sports Phys Ther. 2010;5(2):47-54. [PMC free article] [PubMed] [Google Scholar]
- 22. Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function - part 1. Int J Sports Phys Ther. 2014;9(3):396-409. [PMC free article] [PubMed] [Google Scholar]
- 23. Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20-26. [DOI] [PubMed] [Google Scholar]
- 24. Deal MJ, Richey BP, Pumilia CA, et al. Regional interdependence and the role of the lower body in elbow injury in baseball players: a systematic review. Am J Sports Med. 2020;48(14):3652-3660. [DOI] [PubMed] [Google Scholar]
- 25. Deneweth JM, Pomeroy SM, Russell JR, et al. Position-specific hip and knee kinematics in NCAA football athletes. Orthop J Sports Med. 2014;2(6):2325967114534591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. de Vos RJ. Overdiagnosis in sports medicine. Aspetar Sports Med J. 2017;6:28-32. [Google Scholar]
- 27. Dill KE, Begalle RL, Frank BS, Zinder SM, Padua DA. Altered knee and ankle kinematics during squatting in those with limited weight-bearing-lunge ankle-dorsiflexion range of motion. J Athl Train. 2014;49(6):723-732. doi: 10.4085/1062-6050-49.3.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Drakos MC, Domb B, Starkey C, Callahan L, Allen AA. Injury in the National Basketball Association: a 17-year overview. Sports Health. 2010;2(4):284-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ellenbecker TS, Roetert EP, Piorkowski PA, Schulz DA. Glenohumeral joint internal and external rotation range of motion in elite junior tennis players. J Orthop Sports Phys Ther. 1996;24(6):336-341. [DOI] [PubMed] [Google Scholar]
- 30. Fong DTP, Leung W-C, Mok K-M, Yung PSH. Delayed ankle muscle reaction time in female amateur footballers after the first 15 min of a simulated prolonged football protocol. J Exper Orthop. 2020;7(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Heerey J, Risberg MA, Magnus J, et al. Impairment-based rehabilitation following hip arthroscopy: postoperative protocol for the HIP ARThroscopy International Randomized Controlled Trial. J Orthop Sports Phys Ther. 2018;48(4):336-342. [DOI] [PubMed] [Google Scholar]
- 32. James J, Ambegaonkar JP, Caswell SV, Onate J, Cortes N. Analyses of landing mechanics in Division I athletes using the landing error scoring system. Sports Health. 2016;8(2):182-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kendall FP. Muscles: Testing and Function with Posture and Pain. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 34. Kiesel K, Plisky P, Butler R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sport. 2011;21(2):287-292. [DOI] [PubMed] [Google Scholar]
- 35. Kouyoumdjian P, Coulomb R, Sanchez T, Asencio G. Clinical evaluation of hip joint rotation range of motion in adults. Orthop Traumatol Surg Res. 2012;98(1):17-23. [DOI] [PubMed] [Google Scholar]
- 36. Larson CM, Ross JR, Kuhn AW, et al. Radiographic hip anatomy correlates with range of motion and symptoms in National Hockey League players. Am J Sports Med. 2017;45(7):1633-1639. [DOI] [PubMed] [Google Scholar]
- 37. Latash ML, Zatsiorsky VM. Joint stiffness: myth or reality? Hum Mov Sci. 1993;12:653-692. [Google Scholar]
- 38. Lisman P, O’Connor FG, Deuster PA, Knapik JJ. Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc. 2013;45(4):636-643. [DOI] [PubMed] [Google Scholar]
- 39. Magee DJ. Orthopedic Physical Assessment. 5th ed. Toronto: Saunders Elsevier, 2008. [Google Scholar]
- 40. Malliaras P, Cook JL, Kent P. Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players. J Sci Med Sport. 2006;9(4):304-309. [DOI] [PubMed] [Google Scholar]
- 41. McLean BD, Strack DS, Martin DT. “Avoidance preening”, displacement behavior and co-dependency in professional team sport: when wants become more important than needs. Int J Sports Phys Ther. 2022;17(5):945-949. [PMC free article] [PubMed] [Google Scholar]
- 42. Mendonca LD, Ocarino JM, Bittencourt NFN, Macedo LG, Fonseca ST. Association of hip and foot factors with patellar tendinopathy (jumper’s knee) in athletes. J Orthop Sports Phys Ther. 2018;48(9):676-684. [DOI] [PubMed] [Google Scholar]
- 43. Minhas SV, Kester BS, Larkin KE, Hsu WK. The effect of an orthopaedic surgical procedure in the National Basketball Association. Am J Sports Med. 2016;44(4):1056-1061. [DOI] [PubMed] [Google Scholar]
- 44. Mosler AB, Crossley KM, Thorborg K, et al. Hip strength and range of motion: normal values from a professional football league. J Sci Med Sport. 2017;20(4):339-343. [DOI] [PubMed] [Google Scholar]
- 45. Moynihan R, Glasziou P, Woloshin S, Schwartz L, Santa J, Godlee F. Winding back the harms of too much medicine: registration is opening and abstracts closing soon for our “Preventing Overdiagnosis” conference. Br Med J. 2013;346(7897):10. [DOI] [PubMed] [Google Scholar]
- 46. Neal BS, Griffiths IB, Dowling GJ, et al. Foot posture as a risk factor for lower limb overuse injury: a systematic review and meta-analysis. J Foot Ankle Res. 2014;7(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nepple JJ, Vigdorchik JM, Clohisy JC. What is the association between sports participation and the development of proximal femoral cam deformity?: A systematic review and meta-analysis. Am J Sports Med. 2015;43(11):2833-2840. [DOI] [PubMed] [Google Scholar]
- 48. Overmoyer GV, Reiser RF, II. Relationships between lower-extremity flexibility, asymmetries, and the Y balance test. J Strength Condit Res. 2015;29(5):1240-1247. [DOI] [PubMed] [Google Scholar]
- 49. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Jr, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics. The JUMP-ACL study. Am J Sports Med. 2009;37(10):1996-2002. [DOI] [PubMed] [Google Scholar]
- 50. Padua DA, DiStefano LJ, Beutler AI, de la Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50(6):589-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Payne KA, Berg K, Latin RW. Ankle injuries and ankle strength, flexibility, and proprioception in college basketball players. J Athl Train. 1997;32(3):221-225. [PMC free article] [PubMed] [Google Scholar]
- 52. Pearson SJ, McMahon J. Lower limb mechanical properties: determining factors and implications for performance. Sports Med. 2012;42(11):929-940. [DOI] [PubMed] [Google Scholar]
- 53. Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. North Am J Sports Phys Ther. 2009;4(2):92-99. [PMC free article] [PubMed] [Google Scholar]
- 54. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911-919. [DOI] [PubMed] [Google Scholar]
- 55. Pohl MB, Farr L. A comparison of foot arch measurement reliability using both digital photography and calliper methods. J Foot Ankle Res. 2010;3(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rabin A, Kozol Z, Spitzer E, Finestone A. Ankle dorsiflexion among healthy men with different qualities of lower extremity movement. J Athl Train. 2014;49(5):617-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Reinold MM, Wilk KE, Reed J, Crenshaw K, Andrews JR. Change in shoulder and elbow range of motion of professional baseball pitchers before and after pitching. (Abstract). J Orthop Sports Phys Ther. 2003;33(2):A-50. [Google Scholar]
- 58. Ruotolo C, Price E, Panchal A. Loss of total arc of motion in collegiate baseball players. J Shoulder Elbow Surg. 2006;15(1):67-71. [DOI] [PubMed] [Google Scholar]
- 59. Sanz A, Pablos C, Ballester R, Sánchez-Alarcos JV, Huertas F. Range of motion and injury occurrence in elite Spanish soccer academies. Not only a hamstring shortening-related problem. J Strength Cond Res. 2020;34(7):1924-1932. [DOI] [PubMed] [Google Scholar]
- 60. Saragiotto BT, Di Pierro C, Lopes AD. Risk factors and injury prevention in elite athletes: a descriptive study of the opinions of physical therapists, doctors and trainers [Article in English, Portuguese]. Braz J Phys Ther. 2014;18(2):137-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Phys. 2012;40(3):521-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Smith S. What is the real cost of injuries in professional sport? https://medium.com/@stephensmith_ie/what-is-the-real-cost-of-injuries-in-professional-sport-fee1d66a7502. Accessed July 6, 2020.
- 63. Stotts J. NBA injury analysis. http://instreetclothes.com/nba-injury-analysis/. Accessed September 1, 2016.
- 64. Tak I, Engelaar L, Gouttebarge V, et al. Is lower hip range of motion a risk factor for groin pain in athletes? A systematic review with clinical applications. Br J Sports Med. 2017;51(22):1611-1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Tipnis RA, Anloague PA, Laubach LL, Barrios JA. The dose-response relationship between lateral foot wedging and the reduction of knee adduction moment. Clin Biomech (Bristol, Avon). 2014;29(9):984-989. [DOI] [PubMed] [Google Scholar]
- 66. Tomaro J. Measurement of tibiofibular varum in subjects with unilateral overuse symptoms. J Orthop Sports Phys Ther. 1995;21(2):86-89. [DOI] [PubMed] [Google Scholar]
- 67. Treadwell J, McCartney M. Overdiagnosis and overtreatment: generalists - it’s time for a grassroots revolution. Br J Gen Pract. 2016;66(644):116-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Weimar WH, Shroyer JF. Arch height index normative values of college-aged women using the arch height index measurement system. J Am Podiatr Med Assoc. 2013;103(3):213-217. [DOI] [PubMed] [Google Scholar]
- 69. Whittaker JL, Small C, Maffey L, Emery CA. Risk factors for groin injury in sport: an updated systematic review. Br J Sports Med. 2015;49(12):803-809. [DOI] [PubMed] [Google Scholar]
- 70. Whitting JW, Steele JR, Mcghee DE, Munro BJ. Dorsiflexion capacity affects Achilles tendon loading during drop landings. Med Sci Sports Exerc. 2011;43(4):706-713. [DOI] [PubMed] [Google Scholar]
- 71. Williams D, III, Davis I, Scholz J, Hamill J, Buchanan T. High-arched runners exhibit increased leg stiffness compared to low-arched runners. Gait Posture. 2004;19(3):263-269. [DOI] [PubMed] [Google Scholar]
- 72. Williams D, McClay I, Scholz J, Buchanan T, Hamill J. Lower extremity stiffness in runners with different foot types. In Proceedings of the 24th Annual Meeting of the American Society of Biomechanics. July 19-22, 2000. American Society of Biomechanics: Chicago, IL; 2000:57-58. [Google Scholar]
- 73. Zhao X, Tsujimoto T, Kim B, Tanaka K. Association of arch height with ankle muscle strength and physical performance in adult men. Biol Sport. 2017;34(2):119-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Zifchock R, Davis I, Hillstrom H, Song J. The effect of gender, age, and lateral dominance on arch height and arch stiffness. Foot Ankle Int. 2006;27(5):367-372. [DOI] [PubMed] [Google Scholar]


