Abstract
Study Design
Retrospective Matched Cohort Study.
Objectives
Low median household income (MHI) has been correlated with worsened surgical outcomes, but few studies have rigorously controlled for demographic and medical factors at the patient level. This study isolates the relationship between MHI and surgical outcomes in a lumbar fusion cohort using coarsened exact matching.
Methods
Patients undergoing single-level, posterior lumbar fusion at a single institution were consecutively enrolled and retrospectively analyzed (n = 4263). Zip code was cross-referenced to census data to derive MHI. Univariate regression correlated MHI to outcomes. Patients with low MHI were matched to those with high MHI based on demographic and medical factors. Outcomes evaluated included complications, length of stay, discharge disposition, 30- and 90 day readmissions, emergency department (ED) visits, reoperations, and mortality.
Results
By univariate analysis, MHI was significantly associated with 30- and 90 day readmission, ED visits, reoperation, and non-home discharge, but not mortality. After exact matching (n = 270), low-income patients had higher odds of non-home discharge (OR = 2.5, P = .016) and higher length of stay (mean 100.2 vs 92.6, P = .02). There were no differences in surgical complications, ED visits, readmissions, or reoperations between matched groups.
Conclusions
Low MHI was significantly associated with adverse short-term outcomes from lumbar fusion. A matched analysis controlling for confounding variables uncovered longer lengths of stay and higher rates of discharge to post-acute care (vs home) in lower MHI patients. Socioeconomic disparities affect health beyond access to care, worsen surgical outcomes, and impose costs on healthcare systems. Targeted interventions must be implemented to mitigate these disparities.
Keywords: household income, length of stay, discharge disposition, lumbar fusion
Introduction
Social determinants of health (SDOH) such as income, wealth, education, employment, and food security have been widely studied and are known to influence health outcomes broadly on both individual and population scales.1-6 Literature on the effects of SDOH such as race, gender, and economics in neurosurgery is emerging, yet gaps remain in identifying how these factors specifically influence surgical outcomes and how they can be mitigated. 7
Median household income is known to be associated with mortality and has been associated with multiple medical and surgical outcomes.3,8-10 In neurosurgical studies, lower median household income has been correlated to increased 30- and 90 day mortality for posterior fossa brain tumor cases,11,12 increased mortality in glioblastoma, 13 and increased 90 day ED visits for supratentorial meningioma resections. 14 Salwi et al 15 demonstrated a higher composite socioeconomic score correlated to improved outcomes and decreased mortality in stroke.
In spine surgery specifically, Lambrecths et al implicated a correlation between household income and radiographic severity of cervical degenerative disc disease. 16 Barrie et al 17 found that SES was significantly correlated to increased length of stay, as well as 90 day opioid prescriptions and ER visits for all spine surgery patients in their cohort. Chan et al 18 recently found that socioeconomic status augmented the predictive value of the Centers for Medicare and Medicaid Services Hierarchical Condition risk adjustment model for adverse outcomes such as mortality, length of stay, and non-home discharge in a large cohort undergoing lumbar fusion.
Lumbar fusion is a common spine procedure worldwide that has been increasing in frequency and utilization. 19 Previous research has demonstrated that appropriately selected patients experience an increase in healthcare-related quality of life after spine surgery, and optimizing postoperative outcomes though risk-mitigation strategies is important for long-term improvements in these patients.20,21 Although household income has been shown to correlate with negative outcomes for many types of surgery, there are complex interactions with other socioeconomic and medical factors such as age, race, body mass index, and comorbidity. Prior research in spine surgery has not controlled for such factors to establish the direct impact of household income. In a widely performed surgery with good outcomes and limited complications at baseline, 22 the correlation between household income and surgical outcomes may be due to complex interactions between 1 or more of these factors.
Building upon prior studies, this study aims to isolate any effect that Median Household Income (MHI) may have on short-term outcomes among patients undergoing single-level, posterior-only lumbar fusion at a single academic medical center. We implement a coarsened exact matching (CEM) protocol to control for patient-level factors independently related to surgical outcomes and isolate the influence of MHI. By this method, high and low-income patients are paired 1:1 by finding those who exactly match across all controlled variables, allowing the isolation of the effect of income. 23
Methods
Sample Selection
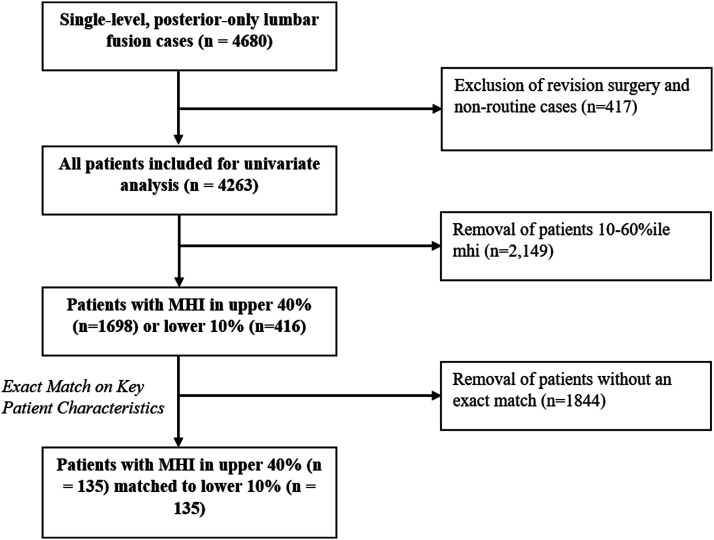
Consecutive adult patients undergoing non-revision, single-level posterior-only lumbar fusion surgery between 2013-2021 were enrolled in our study (Figure 1), yielding 4679 observations. This study was approved by the Institutional Review Board at the Hospital of the University of Pennsylvania (IRB 832794). Informed consent was waived as this study was considered minimal risk to patients. Our cohort was limited to include only clean wounds, general anesthesia, routine (non-urgent) inpatient admissions, and body mass index (BMI) between 10 and 70, thus equating to a total of 4263 observations.
Figure 1.
Study selection and sample size.
Data Extraction
Patient and outcome data were obtained using Epilog – a non-proprietary data acquisition system integrated with the electronic health record (EHR) to facilitate quality improvement initiatives without disrupting workflow. 24 Patient zip-code was cross-referenced to the 2012-2016 U.S. Census Bureau 5 Year American Community report to derive MHI adjusted for inflation to US$2016. Other obtained patient characteristics included BMI, age, gender, race, American Society of Anesthesiologists (ASA) score, smoking status, prior back surgery history, CCI score, and insurance type (public vs private). Outcomes measured included surgical complication, length of stay, discharge home vs non-home, and 30- and 90- day readmissions, emergency department (ED) evaluation, reoperation, and all-cause mortality.
Statistical Methods
Univariate logistic regression was performed to compare MHI with patient outcomes. Patients were then split into deciles of observed median household income values. Patients from the lowest decile of MHI (0-10) in our sample were paired with counterparts at the opposite end of the MHI spectrum in the highest 4 deciles (60-100) who matched exactly by gender, ASA grade, age (by decade), smoking, insurance type (private vs public), any prior surgery, prior surgery in 30 days, CCI (<4, 5-6, >7), BMI (<18.5, normal, and obese >30), and race (white/non-white). Income percentiles were intentionally selected to assess outcomes in the lowest 10th percentile of MHI to define a feasible target population for long-term risk mitigation strategies, similar to income-based risk stratification strategies seen in other medical specialties and value-based payment models.25-27 McNemar’s test was used to compare surgical outcomes between these 2 coarsened exact matched groups. Nonparametric testing was used to compare length of stay.
Results
Patient Characteristics
In our cohort comprising n = 4263 initially analyzed with univariate analysis, the median length of stay was 80 h. There were 1698 patients in the upper 40% of MHI and 416 in the lowest 10%. A total of 270 patients were matched exactly between these groups. Prior to matching, significant differences were found between patients in the highest 40% and lowest 10%ile of MHI with respect to age, gender, race, BMI, smoking status, CCI, ASA, and prior surgical history. After matching, no differences in these social, medical, and surgical factors remained between these groups (Table 1).
Table 1.
Patient Demographic and Medical Information Before (n = 2114) and After (n = 270) Exact Matching, Grouped by Patients in the Top 40% and Bottom 10% by MHI. *Continuous Variables Were Compared via Nonparametric Tests, While Discrete Variables Were Compared by Chi-Squared or Fisher’s Exact Tests.
| Before Exact Matching | After Exact Matching | |||||
|---|---|---|---|---|---|---|
| Total | Top 40% (n = 1698) | Lowest 10% (n = 416) | P-value* | Top 40% (n = 135) | Lowest 10% (n = 135) | P-value* |
| Gender, n (%) | ||||||
| Male | 768 (45.2) | 149 (35.8) | .001 | 50 (37) | 50 (37) | 1.0 |
| Female | 930 (54.8) | 267 (64.2) | 85 (63) | 85 (63) | ||
| Age, n (%) | ||||||
| <50 | 229 (13.5) | 83 (10) | <.001 | 25 (19) | 25 (19) | 1.0 |
| 50-60 | 361 (21.3) | 132 (31.7) | 31 (23) | 31 (23) | ||
| 60-70 | 519 (30.6) | 129 (31) | 49 (36) | 49 (36) | ||
| 70-80 | 491 (28.9) | 55 (13.2) | 26 (19) | 26 (19) | ||
| >80 | 98 (5.8) | 17 (4.1) | 4 (3) | 4 (3) | ||
| Insurance type, n (%) | ||||||
| Private | 837 (49.3) | 136 (32.7) | <.001 | 65 (48.1) | 65 (48.1) | 1.0 |
| Government | 861 (50.7) | 280 (67.3) | 70 (51.9) | 70 (51.9) | ||
| Any lifetime surgical intervention prior to the index operation, n (%) | ||||||
| No | 1106 (65.1) | 192 (46.2) | <.001 | 95 (70.4) | 95 (70.4) | 1.0 |
| Yes | 592 (34.9) | 224 (53.9) | 40 (29.6) | 40 (29.6) | ||
| Any surgical intervention 30 days prior to the index operation, n (%) | ||||||
| No | 1649 (97.1) | 400 (96.2) | .31 | 134 (99) | 134 (99) | 1.0 |
| Yes | 49 (2.9) | 16 (3.9) | 1 (1) | 1 (1) | ||
| CCI score, n (%) | ||||||
| Low (≤4) | 1369 (80.6) | 308 (74) | .002 | 115 (85.2) | 115 (85.2) | 1.0 |
| Medium (5,6) | 222 (13.1) | 63 (15.1) | 17 (12.6) | 17 (12.6) | ||
| High (≥7) | 107 (6.3) | 45 (10.8) | 3 (2.2) | 3 (2.2) | ||
| Body mass index (kg/m2), mean | ||||||
| <18.5 | 12 (.71) | 4 (1) | <.001 | - | - | |
| 18.5 – 29.9 | 1021 (60.1) | 182 (43.7) | 71 (52.6) | 71 (52.6) | 1.0 | |
| >30.0 | 665 (39.1) | 230 (55.3) | 64 (47.4) | 64 (47.4) | ||
| Smoking status, n (%) | ||||||
| Smoker | 147 (8.7) | 96 (23.1) | <.001 | 13 (9.6) | 13 (9.6) | 1.0 |
| Non-smoker | 1544 (90.9) | 318 (76.4) | 122 (90.4) | 122 (90.4) | ||
| Unknown | 7 (.4) | 2 (.5) | - | - | ||
| Race | ||||||
| White | 1516 (89.28) | 105 (25.2) | <.001 | 76 (56.3) | 76 (56.3) | 1.0 |
| Non-white | 182 (10.72) | 311 (74.8) | 59 (43.7) | 59 (43.7) | ||
| American society of anesthesiologists grade, mean (range) | ||||||
| 2.40 (1-4) | 2.50 (1-4) | <.001 | 2.33 (2-3) | 2.33 (2-3) | 1.0 | |
Statistical Results
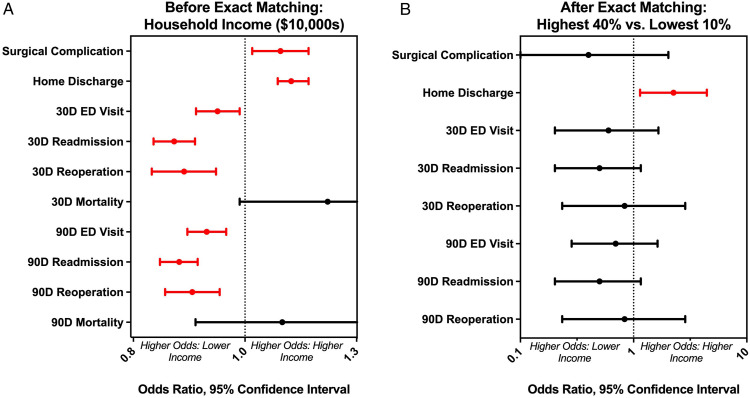
Univariate regression analysis found that lower MHI was significantly correlated to non-home discharge and 30- and 90 day ER visits, admissions, and reoperations (Figure 2(a), Table 2). Higher MHI was significantly correlated to increased surgical complications. No significant relationship was observed between MHI and mortality at both 30- and 90 days. After coarsened exact matching, a statistically significant relationship was observed between MHI and discharge to home (OR = 2.5, P = .0163), indicating higher odds of non-home discharge for low-income patients (Figure 2(b), Table 2). Length of stay was higher in the low-income compared to the matched high-income group (mean 100.24 vs 92.60, p-.02). No significant relationship was found between MHI and ER visits, admissions, reoperations, or surgical complications between the matched groups.
Figure 2.
Panel A– Results of Univariate Regression. Lower MHI corresponded to significantly higher odds of non-home discharge, ED visits, readmissions, and reoperations. Higher MHI corresponded to higher odds of surgical complications. Panel B– Results of Coarsened Exact Matching. Odds ratios shown for high MHI relative to low MHI. Patients with low MHI had significantly higher odds of non-home discharge relative to otherwise exactly matched patients with high MHI.
Table 2.
Results of Analyses Before (Left) and After (Right) Coarsened Exact Matching. Odds Ratios and P-values for Logistic Regression Reported Using MHI in US$10,000 Units. Coarsened Exact Matching Odds Ratios Comparing the Highest 40% to the Lowest 10% in MHI.
| Before Exact Matching | After Exact Matching | |||
|---|---|---|---|---|
| Univariate MHI (US$10,000s) | Top 40% vs Bottom 10% | |||
| Outcome | OR (95% CI) | P-Value | Or (95% CI) | P-Value |
| Intraoperative complication | 1.08 (1.02-1.14) | .014 | .40 (.05 - 2.03) | .29 |
| Home discharge | 1.10 (1.07-1.14) | <.001 | 2.25 (1.14 - 4.44) | .02 |
| 30D ED visit | .95 (.90-.99) | .015 | .60 (.20 - 1.66) | .33 |
| 30D readmission | .86 (.83-.90) | <.001 | .50 (.20 - 1.16) | .11 |
| 30D reoperation | .88 (.83-.94) | <.001 | .83 (.23 - 2.86) | .77 |
| 30D mortality | 1.19 (.99-1.42) | .07 | N/A | N/A |
| 90D ED visit | .92 (.89-.96) | <.001 | .69 (.28 - 1.63) | .40 |
| 90D readmission | .87 (.84-.91) | <.001 | .50 (.20 - 1.16) | .11 |
| 90D reoperation | .90 (.85-.95) | <.001 | .83 (.23 - 2.86) | .77 |
| 90D mortality | 1.08 (.90-1.29) | .40 | N/A | N/A |
Discussion
Our study extends prior work examining SES as a predictor of outcomes to lumbar spinal fusion, one of the most common procedures in neurosurgery. By univariate regression, we found a significant increase in 30-day and 90-day ED visits, readmissions, and reoperations, as well as decreased surgical complications and decreased home discharge for lower median household income for patients undergoing lumbar fusion. This is congruent with prior literature exploring the relationship between SES and surgical outcomes and with prior observations in lumbar fusion.11,15,16,28,29 The correlation between household income and outcomes from lumbar fusion is particularly notable given the low baseline morbidity and mortality of this procedure. 22 As seen in Table 1, however, low MHI patients in our cohort tended more often to be female, younger, publicly insured, non-white, smokers, and have a prior history of any surgery and greater comorbidity and surgical risk measured by CCI and ASA. While higher medical risk may account for the increase in short-term resource utilization, younger age in the low MHI cohort may account for the inverse correlation seen with intraoperative complications such as unintended durotomy. Private insurance in the U.S. is often employer-based and may offer options for more extensive coverage than public insurance; that is, employment status, insurance access and coverage, and income are all correlated but may be separately driving health outcomes. These highlight the complex interactions within social determinants of health and motivate our matching analysis to isolate more direct effects of MHI on short-term lumbar fusion outcomes.
After isolating MHI from covariates by CEM, we observed that patients within the lowest ten percent of observed median household income values had over double the odds of non-home discharge compared to their higher-income counterparts and had an average hospital stay 8 hours longer. This relationship that SES relates to worsened discharge disposition has been observed in prior studies such as post-thrombectomy for stroke and arthroplasty.30,31 Inverse relationships between household income and length of stay have also been found in neurosurgery.17,18 Notably, these prior observations were gathered using multivariate regression models. By exactly matching patients one-to-one, our finding furthers this evidence to support a direct correlation between income and discharge to home. Our findings suggest that MHI may serve as a social risk adjustment tool to identify high-risk patients who may benefit from targeted interventions to reduce health inequities.
In comparison to our findings, a prior study of discharge location after joint replacement surgery generally found that lower SES was associated with lower levels of post-surgical rehabilitation care and 32 suggested that medical or surgical complicating factors associated with lower SES may be confounding factors. 32 In our study, the tendency for non-home discharge in lower-income patients contrasts with the lack of any other observable difference between the matched patients in surgical complications, readmissions, or reoperations. This may suggest a lack of socioeconomic support at home necessary for post-surgical rehabilitation may be responsible for our findings rather than inherent medical or surgical differences between the groups. Despite similar demographics, medical risk, and insurance coverage, low MHI may nonetheless influence the preparedness of patients for discharge after lumbar fusion and may hinder opportunities for at-home rehabilitation. Patients with lower MHI may face challenges accessing necessary equipment and resources, lack social support, and have limited transportation access for follow-up care, which may warrant consideration and longer planning of discharge to rehabilitation facilities.
While the role of household income as a determinant of health outcomes is evident in the U.S., similar patterns are observed globally, where lower income levels often correlate with reduced access to healthcare services and poorer health outcomes.33,34 This similarity across countries highlights how income universally impacts health, regardless of the specific healthcare system. Improving access to rehabilitation is recognized as a key factor in improving surgical outcomes globally. Ongoing research is highlighting the barriers to rehabilitation in low and middle-income countries and identifying areas needed for further study.34-38 While our study is conducted at a single medical center in the United States, it provides important insight into socioeconomic determinants of rehabilitation in a single model of healthcare and may guide further cost-value analyses of these dynamics globally.
Importantly, these findings come from a cohort of patients for whom care has already been established. While lack of income poses significant barriers to access to care, our findings come from patients who had already received spinal surgery at our medical center, providing further evidence of SDOH that exist beyond the initial barrier of access to care. By increasing discharge rates to rehabilitation and nursing facilities, poverty at the individual level may contribute to overall increased healthcare utilization and costs at the system level.39,40 Interventions providing patients the means and support to be discharged home safely for rehabilitation may prove cost-effective in the long run and improve patient satisfaction. Further study would be needed to determine if increasing coverage for at-home health care or access to transportation would save systemic costs of longer stays and rehabilitation facilities. Pre-surgical initiation of discharge coordination may identify potential barriers and inform immediate perioperative care to optimize rehabilitation.
Limitations
While our study is novel in the isolation of a homogenous population and controlled evaluation of socioeconomic determinants of short-term surgical outcomes, our findings come with limitations. Our cohort comes from a retrospective analysis of patients at a single large academic center which limits our generalizability. In our CEM protocol, we limit our sample size by design in order to exactly match patients and isolate MHI as an independent variable. A limitation of CEM is the limited resolution of the control categories; for instance, by categorizing insurance into public and private, we may not capture variances within each group. Lower-income patients with private insurance may still have limited coverage for certain services, such as home health care, which may confound our results. Further, our study intentionally isolates MHI as the studied variable, though intricately related components of socioeconomic status such as education level, employment status, transportation barriers, and social support may also partially explain our results. This highlights the need for further research into composite measures of socioeconomic status and identifying which components are most sensitive to identify vulnerable patient populations who can benefit from risk-mitigation strategies.
The primary outcomes evaluated in this study are short-term surgical outcomes and do not provide information about long-term disease trajectories. These outcomes were deliberately chosen as they are easily interpreted, reproducible, and commonly used for quality assessment and improvement initiatives. These efforts should inform future study to capture longer-term dynamics of the social determinants of lumbar fusion outcomes. While MHI has historically been widely studied as a SDOH and is a broadly intuitive metric, income is only a single measurement to evaluate socioeconomic opportunity, and further study is warranted with other, more holistic metrics.
Conclusion
This study isolated median household income as it relates to outcomes following lumbar fusion. Congruent with prior literature, we found significant univariate correlations when looking at MHI across all patients in our cohort. Between otherwise exactly matched patients, low-income individuals were significantly less likely to be discharged home than high-income counterparts and stayed in the hospital longer, yet no differences remained between surgical complications, ED visits, readmissions, or reoperations. Further studies must evaluate the mechanisms of these processes and target interventions to improve both patient satisfaction and healthcare costs.
Acknowledgments
The EpiLog Project and The Bernadette and Kevin McKenna Family Research Fund.
Appendix.
- MHI
Median Household Income
- ED
Emergency Department
- OR
Odds Ratio
- SDOH
Social Determinants of Health
- CEM
Coarsened exact matching
- EHR
Electronic Health Record
- BMI
Body mass index
- ASA
American Society of Anesthesiologists
- CCI
Charlson Comorbidity Index
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Bernadette and Kevin McKenna Family Research Fund.
Contributorship: RSG and NRM were involved in the design and conception of this manuscript. RSG, RK, AJB, EGM, and NRM performed the literature review and compiled the primary manuscript. RSG, AJB, JN, and NRM collected and analyzed data. RSG and RK compiled the figures and tables. RSG, RK, AJB, EGM, MAP, JN, SDM, and NRM critically revised the manuscript. All authors approved the manuscript as it is written.
Ethical Statement
Ethics Committee Approval
This study was approved by the IRB at the Hospital of the University of Pennsylvania. The IRB number for this study is 832 794. All ethical guidelines and rules were followed to protect patient privacy.
ORCID iDs
Ryan S. Gallagher https://orcid.org/0000-0002-1789-9142
Ritesh Karsalia https://orcid.org/0000-0001-6002-3296
Neil R. Malhotra https://orcid.org/0000-0002-0754-6423
References
- 1.Institute of Medicine . Unequal treatment: confronting racial and ethnic disparities in health care; 2002. https://nap.nationalacademies.org/catalog/12875/unequal-treatment-confronting-racial-and-ethnic-disparities-in-health-care [PMC free article] [PubMed] [Google Scholar]
- 2.Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S, Health Commission on Social Determinants of . Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661-1669. doi: 10.1016/s0140-6736(08)61690-6 [DOI] [PubMed] [Google Scholar]
- 3.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the United States, 2001-2014. JAMA. 2016;315(16):1750-1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Catalyst N. Social Determinants of Health (SDOH) . NEJM Catalyst. 2017;3(6). Published online December 1. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0312 [Google Scholar]
- 5.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annual Review of Public Health. 2011;32:381-398. https://www.annualreviews.org/doi/pdf/10.1146/annurev-publhealth-031210-101218 [DOI] [PubMed] [Google Scholar]
- 6.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(1_suppl2):19-31. doi: 10.1177/00333549141291s206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glauser G, O’Connor A, Brintzenhoff J, Roth SC, Malhotra NR, Cabey WV. A scoping review of the literature on the relationship between social and structural determinants of health and neurosurgical outcomes. World Neurosurg. 2021;158:24-33. doi: 10.1016/j.wneu.2021.10.109 [DOI] [PubMed] [Google Scholar]
- 8.Rubinger L, Chan C, Andrade D, et al. Socioeconomic status influences time to surgery and surgical outcome in pediatric epilepsy surgery. Epilepsy and Behavior. 2016;55:133-138. [DOI] [PubMed] [Google Scholar]
- 9.Anderson BR, Fieldston ES, Newburger JW, Bacha EA, Glied SA. Disparities in outcomes and resource use after hospitalization for cardiac surgery by neighborhood income. Pediatrics. 2018;141(3):e20172432. doi: 10.1542/peds.2017-2432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herrera-Escobar JP, Seshadri AJ, Rivero R, et al. Lower education and income predict worse long-term outcomes after injury. J Trauma Acute Care. 2019;87(1):104-110. doi: 10.1097/ta.0000000000002329 [DOI] [PubMed] [Google Scholar]
- 11.Blue R, Dimentberg R, Detchou DK, et al. The impact of household economics on short-term outcomes in a posterior fossa tumor population. Cureus. 2020;12(7):e8968. doi: 10.7759/cureus.8968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blue R, Yang AI, Zhou C, et al. Telemedicine in the era of coronavirus disease 2019 (COVID-19): a neurosurgical perspective. World Neurosurgery. 2020;139:549-557. doi: 10.1016/j.wneu.2020.05.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu EK, Yu S, Sulman EP, Kurz SC. Racial and socioeconomic disparities differentially affect overall and cause-specific survival in glioblastoma. J Neurooncol. 2020;149(1):55-64. doi: 10.1007/s11060-020-03572-y [DOI] [PubMed] [Google Scholar]
- 14.Spadola M, Farooqi A, Dimentberg R, et al. The effect of household income on outcomes following supratentorial meningioma resection. Clinical Neurology and Neurosurgery. 2020;195:106031. doi: 10.1016/j.clineuro.2020.106031 [DOI] [PubMed] [Google Scholar]
- 15.Salwi S, Kelly KA, Patel PD, et al. Neighborhood socioeconomic status and mechanical thrombectomy outcomes. Journal of Stroke and Cerebrovascular Diseases. 2021;30(2):105488. doi: 10.1016/j.jstrokecerebrovasdis.2020.105488 [DOI] [PubMed] [Google Scholar]
- 16.Lambrechts MJ, Maryan K, Whitman W, et al. Comorbidities associated with cervical spine degenerative disc disease. J Orthop. 2021;26:98-102. doi: 10.1016/j.jor.2021.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barrie U, Montgomery EY, Ogwumike E, et al. Household income as a predictor for surgical outcomes and opioid use after spine surgery in the United States. Global Spine J. Published online January. 2022;10:21925682211070824. doi: 10.1177/21925682211070823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan AK, Shahrestani S, Ballatori AM, et al. Is the centers for medicare and medicaid services hierarchical condition category risk adjustment model satisfactory for quantifying risk after spine surgery? Neurosurgery. 2022;91(1):123-131. doi: 10.1227/neu.0000000000001980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP. Trends in lumbar spinal fusion-a literature review. J Spine Surg. 2020;6(4):752-761. doi: 10.21037/jss-20-492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chotai S, Parker SL, Sivaganesan A, et al. Effect of complications within 90 days on patient-reported outcomes 3 months and 12 months following elective surgery for lumbar degenerative disease. Neurosurg Focus. 2015;39(6):E8. doi: 10.3171/2015.8.focus15302 [DOI] [PubMed] [Google Scholar]
- 21.Nayak NR, Stephen JH, Piazza MA, Obayemi AA, Stein SC, Malhotra NR. Quality of life in patients undergoing spine surgery: systematic review and meta-analysis. Glob Spine J. 2019;9(1):67-76. doi: 10.1177/2192568217701104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lambrechts MJ, Siegel N, Heard JC, et al. Trends in single-level lumbar fusions over the past decade using a national database. World Neurosurg; 2022. doi: 10.1016/j.wneu.2022.07.092. Published online 2022. [DOI] [PubMed] [Google Scholar]
- 23.Iacus SM, King G, Porro G. Causal inference without balance checking: coarsened exact matching. Political Anal. 2012;20(1):1-24. doi: 10.1093/pan/mpr013. [DOI] [Google Scholar]
- 24.Gawande A. Why doctors hate their computers. The New Yorker. 12. Advance Magazine Publishers. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers (2018). [Google Scholar]
- 25.Martikainen P, Mäkelä P, Koskinen S, Valkonen T. Income differences in mortality: a register-based follow-up study of three million men and women. Int J Epidemiology. 2001;30(6):1397-1405. doi: 10.1093/ije/30.6.1397 [DOI] [PubMed] [Google Scholar]
- 26.Avanceña ALV, DeLuca EK, Iott B, et al. Income and income inequality are a matter of life and death. what can policymakers do about it? Am J Public Heal. 2021;111(8):1404-1408. doi: 10.2105/ajph.2021.306301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mackillop WJ, Zhang Salomons J, Boyd CJ, Groome PA. Associations between community income and cancer incidence in Canada and the United States. Cancer. 2000;89(4):901-912. doi: [DOI] [PubMed] [Google Scholar]
- 28.Blue R, Detchou DK, Dimentberg R, et al. The influence of household income on survival following posterior fossa tumor resection at a large academic medical center. J Neurol Surg B Skull Base. 2021;82(6):631-637. doi: 10.1055/s-0040-1715590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foy AB, Sawin KJ, Derflinger T, et al. Sociodemographic disparities in fetal surgery for myelomeningocele: a single-center retrospective review. Journal of Neurosurgery: Pediatrics. 2021;1(aop):1-5. doi: 10.3171/2021.7.peds20836 [DOI] [PubMed] [Google Scholar]
- 30.Inneh IA, Clair AJ, Slover JD, Iorio R. Disparities in discharge destination after lower extremity joint arthroplasty: analysis of 7924 patients in an urban setting. J Arthroplast. 2016;31(12):2700-2704. doi: 10.1016/j.arth.2016.05.027 [DOI] [PubMed] [Google Scholar]
- 31.Mehta AM, Fifi JT, Shoirah H, et al. Racial and socioeconomic disparities in the use and outcomes of endovascular thrombectomy for acute ischemic stroke. Am J Neuroradiol. 2021;42(9):1576-1583. doi: 10.3174/ajnr.a7217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freburger JK, Holmes GM, Ku LJE, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in post-acute rehabilitation care for joint replacement. Arthritis Care Res (Hoboken). 2011;63(7):1020-1030. doi: 10.1002/acr.20477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-624. doi: 10.1016/s0140-6736(15)60160-x [DOI] [PubMed] [Google Scholar]
- 34.Barth CA, Wladis A, Roy N, Blake C, Kolo SM, O’Sullivan C. Ways to improve surgical outcomes in low- and middle-income countries. Bull World Heal Organ. 2022;100(11):726-732. doi: 10.2471/blt.22.287950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pritwani S, Pandey S, Shrivastava P, et al. Challenges in rehabilitation and continuum of care provision after knee replacement: a mixed-methods study from a low- and middle-income country. Disabil Rehabilitation 2023;11-1111. doi: 10.1080/09638288.2023.2236012 [DOI] [PubMed] [Google Scholar]
- 36.Ibbotson JL, Luitel B, Adhikari B, et al. Overcoming barriers to accessing surgery and rehabilitation in low and middle income countries: An innovative model of patient navigation in Nepal. World J Surg. 2021;45(8):2347-2356. doi: 10.1007/s00268-021-06035-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bernhardt J, Urimubenshi G, Gandhi DBC, Eng JJ. Stroke rehabilitation in low-income and middle-income countries: a call to action. Lancet. 2020;396(10260):1452-1462. doi: 10.1016/s0140-6736(20)31313-1 [DOI] [PubMed] [Google Scholar]
- 38.Velez M, Lugo-Agudelo LH, Lugo DFP, et al. Factors that influence the provision of home‐based rehabilitation services for people needing rehabilitation: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2023;2023(2):CD014823. doi: 10.1002/14651858.cd014823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Theologis AA, Lau D, Dalle-Ore C, Tsu A, Deviren V, Ames CP. Costs and utility of post-discharge acute inpatient rehabilitation following adult spinal deformity surgery. Spine Deformity. 2021;9(3):817-822. doi: 10.1007/s43390-020-00251-w [DOI] [PubMed] [Google Scholar]
- 40.Passias PG, Poorman GW, Bortz CA, et al. Predictors of adverse discharge disposition in adult spinal deformity and associated costs. Spine J. 2018;18(10):1845-1852. doi: 10.1016/j.spinee.2018.03.022 [DOI] [PubMed] [Google Scholar]