Abstract
BACKGROUND
Helicobacter pylori (H. pylori) stands as the predominant infectious agent linked to the onset of gastritis, peptic ulcer diseases, and gastric cancer (GC). Identified as the exclusive bacterial factor associated with the onset of GC, it is classified as a group 1 carcinogen by the World Health Organization. The elimination of H. pylori plays a crucial role in the primary prevention of GC. While the prevalence has declined in recent decades, H. pylori infection is still highly prevalent in China, accounting for a significant part of the disease burden of GC. Therefore, updated prevalence information for H. pylori infection, especially regional and demographic variations in China, is an important basis for the design of targeted strategies that will be effective for the prevention of GC and application of policies for H. pylori control.
AIM
To methodically evaluate the occurrence of H. pylori infection throughout China and establish a reference point for subsequent investigations.
METHODS
A systematic review and meta-analysis was conducted following established guidelines, as detailed in our methodology section.
RESULTS
Our review synthesized data from 152 studies, covering a sample of 763827 individuals, 314423 of whom were infected with H. pylori. We evaluated infection rates in mainland China and the combined prevalence of H. pylori was 42.8% (95%CI: 40.7-44.9). Subgroup analysis indicated the highest prevalence in Northwest China at 51.3% (95%CI: 45.6-56.9), and in Qinghai Province, the prevalence reached 60.2% (95%CI: 46.5-73.9). The urea breath test, which recorded the highest infection rate, showed a prevalence of 43.7% (95%CI: 41.4-46.0). No notable differences in infection rates were observed between genders. Notably, the prevalence among the elderly was significantly higher at 44.5% (95%CI: 41.9-47.1), compared to children, who showed a prevalence of 27.5% (95%CI: 19.58-34.7).
CONCLUSION
Between 2014 and 2023, the prevalence of H. pylori infection in China decreased to 42.8%, down from the previous decade. However, the infection rates vary considerably across different geographical areas, among various populations, and by detection methods employed.
Keywords: Helicobacter pylori, Meta-analysis, Prevalence, Epidemiology, China
Core Tip: Globally, Helicobacter pylori infection continues to be the most prevalent infectious disease, posing substantial public health challenges. Despite a reduction in overall prevalence to 42.8% over the past decade, high rates persist in specific areas and demographics within China, necessitating continued vigilance and targeted interventions.
INTRODUCTION
The presence of Helicobacter pylori (H. pylori) infection is linked to various gastrointestinal conditions and serves as the primary etiological agent for chronic gastritis, peptic ulcers, and gastric cancer (GC). The condition impacts approximately 4.4 billion individuals globally, representing a prevalence rate of around 48.5%, thus posing a significant public health issue on a global scale[1]. In the year 2020, global cancer statistics indicated that there were approximately 1013103 new instances of GC, which corresponded to 768793 fatalities across the globe. Notably, China accounted for 478508 of these new cases and 373706 of the deaths recorded[2]. The occurrence of GC in China is 28.68 per 100000, placing it third among cancers, following lung and colon cancers[3], and it remains a significant contributor to cancer mortality. Despite advancements in sanitation and living conditions, China continues to face a significant prevalence of H. pylori infection and GC. The elimination of H. pylori has been shown to markedly decrease immune and inflammatory responses, promote ulcer healing, and diminish the likelihood of GC development. Long-term studies from Linqu County of Shandong Province and Matsu Island of Taiwan have demonstrated reductions in GC risk by 52% and 53%, respectively, after H. pylori eradication[4,5]. A vast country, China presents a huge variation in geographic, environmental, and socioeconomic aspects of the country; hence, its prevalence rates for diseases also vary significantly amongst its regions. The National Cancer Center, the Cancer Hospital of the Chinese Academy of Medical Sciences, and Peking Union Medical College of China have all documented regional differences in cancer incidence[6]. For example, Qinghai Province exhibits the highest incidence rate of GC in the nation, while Hubei Province is positioned sixth. It is crucial to tailor prevention and treatment strategies to China's unique national circumstances, including the specific epidemiological disease profiles and the diverse needs of various regions and demographics. This is vital for decelerating disease progression and minimizing premature mortality due to end-stage events[7]. Examining the impact of H. pylori infections on disease burden is crucial for formulating national policies[8]. In this research, a meta-analysis approach will be employed, utilizing evidence-based methods with individual rental rates to examine the infection rate within the general population of China. The analysis aids in reliable evidence that is needed at clinical prevention and intervention strategies. The results are as follows.
MATERIALS AND METHODS
This meta-analysis was registered on the PROSPERO database (No. CRD42024555621) and carried out in compliance with the Preferred Items for Systematic Reviews and Meta-Analysis standards.
Search strategy
A systematic review of literature was performed using six databases: (1) PubMed; (2) EMBASE; (3) Cochrane Library; (4) China National Knowledge Infrastructure; (5) Wanfang; and (6) Cqvip, covering the period from January 1, 2014, to January 1, 2024 (Supplementary Table 1).
Inclusion criteria and exclusion criteria
The inclusion criteria were as follows: (1) Patients diagnosed with H. pylori infection via urea breath test (UBT), serological antibody test, stool antigen detection, endoscopic examination, or histopathological evaluation of gastric mucosa biopsies; (2) Studies with clearly defined time and location, involving subjects confirmed to be Chinese; (3) Studies where the infection rate was explicitly stated or could be calculated; and (4) Research findings disseminated in either Chinese or English.
The criteria for exclusion encompassed: (1) Intervention trials, reviews, conference papers, case reports, and meta-analyses; (2) Studies with questionable or incorrect data; (3) Duplicate studies; and (4) Studies with sample sizes less than 50. Literature management was facilitated using Endnote 9.1 software. Two researchers worked separately to search for and screen literature; when they disagreed, they consulted an expert third party to settle the dispute.
Data extraction and quality assessment
Two researchers worked separately to retrieve the data using an Excel spreadsheet. The first author, publication year, study site, geographical area, sample size, and gender distribution of participants were among the data points retrieved. A third researcher resolved any disagreements, and the studies were assessed according to the Loney criterion[9]. Details of these quality assessments are presented in Supplementary Table 2[10-160].
Statistical analysis
The occurrence of H. pylori infection was assessed via meta-analysis. The variation among the studies was evaluated through the application of Cochran’s Q statistic and the I-square statistics (I2). The random-effects model was utilized to calculate the pooled prevalence along with its 95%CI. Sensitivity and subgroup analyses were conducted to further investigate heterogeneity and validate the robustness of the study findings. The subgroup analyses examined the prevalence of H. pylori by province, municipality, autonomous region, geographical area, gender, age, and detection method. Meta-analyses were conducted in RStudio using the "metaprop()" function. Funnel plots were created with the "metabias()" function, and asymmetry was evaluated using the AS-Thompson test[161]. All statistical tests were two-sided, with statistical significance set at P < 0.05.
RESULTS
Literature search and screening results
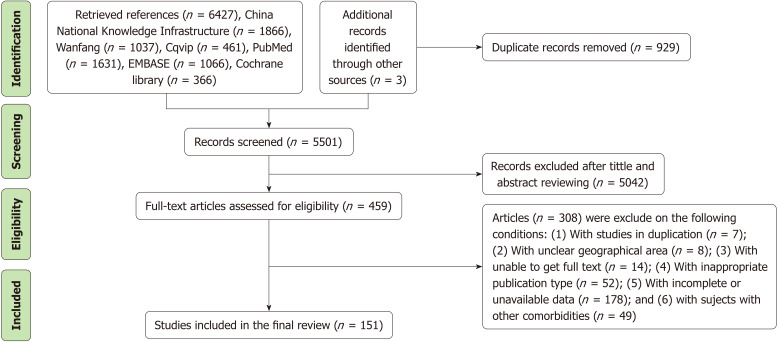
Figure 1 shows the steps involved in searching for and screening literature. The original list of books included 6430 items; 929 of those were later eliminated due to duplication. We removed 5042 results after going over their titles and abstracts. A detailed review of 459 publications was conducted, resulting in 151 studies being selected for inclusion.
Figure 1.
Literature search and screening process.
Basic characteristics of included literature
This analysis involved 152 studies, with a cumulative sample size of 763827 participants. Zou et al[10] presented two studies meeting the inclusion criteria within a single publication. As a result, the table displaying the basic characteristics of the included literature (Table 1) lists 152 studies, whereas the referenced literature totals 151 articles. The study encompassed thirty provinces, municipalities, and autonomous regions across mainland China, with Zhejiang Province (n = 12), Guangdong Province (n = 10), and Hubei Province (n = 9) recording the highest number of studies. Heilongjiang province was excluded due to the lack of studies that met the inclusion criteria during the search period. East China recorded the most studies (n = 43) among the seven geographic regions, while Northeast China had the fewest (n = 6) (Table 1)[10-160].
Table 1.
Characteristics of the included studies
|
Ref.
|
Year
|
Type of study
|
Region
|
Data collection time
|
Detection methods
|
Age (range/mean ± SD)
|
Simple size
|
Male
|
Positive (male/female)
|
Prevalence
|
95%CI
|
| North East | |||||||||||
| Zhang et al[11] | 2016 | Cross-sectional | Jilin (Jilin Province) | 2014.11-2024.12 | 2 | 21-60 | 1932 | 44.77 | 293/395 | 35.6 | 33.5-37.8 |
| Wang et al[12] | 2014 | Cross-sectional | Changchun (Jilin Province) | 2012.05-2012.12 | 1 | 22-83 | 1059 | 65.06 | 324/138 | 43.6 | 40.6-46.7 |
| Zhang et al[13] | 2014 | Cross-sectional | Shenyang (Liaoning Province) | 2012.04-2012.06 | 2 | 3-6 | 1150 | 52.00 | 79/72 | 13.1 | 11.2-15.2 |
| Zhu et al[14] | 2020 | Cross-sectional | Jinzhou (Liaoning Province) | 2019.02-2019.04 | 1 | 21-61 | 2859 | 77.86 | 792/166 | 33.5 | 31.8-35.3 |
| Jiang et al[15] | 2015 | Cross-sectional | Dalian (Liaoning Province) | 2012.12-2013.11 | 2 | 1-100 | 4127 | 53.62 | 664/591 | 30.4 | 29.0-31.8 |
| Ji and Gu[16] | 2016 | Cross-sectional | Dalian (Liaoning Province) | 2013.09-2015.09 | 2 | 18-88 | 4214 | 47.51 | 480/437 | 21.8 | 20.5-23.0 |
| North China | |||||||||||
| Zheng et al[17] | 2022 | Cross-sectional | Tangshan (Hebei Province) | 2019.07-2020.09 | 1 | 21-78 | 9944 | 67.09 | 3115/1395 | 45.4 | 44.4-46.3 |
| Yang et al[18] | 2020 | Cross-sectional | Beijing | 2013.09-2019.06 | 1 | NA | 7260 | 36.54 | 1106/1726 | 39.0 | 37.9-40.1 |
| Zhao et al[19] | 2017 | Cross-sectional | Beijing | 2009.09-2010.02 | 4 | 1 month–18 years | 1196 | 50.67 | 65/62 | 10.6 | 8.9-12.5 |
| Xi et al[20] | 2018 | Cross-sectional | Beijing | NA | 4 | 6-13 | 291 | 55.33 | 47/20 | 23.0 | 18.3-28.3 |
| Chen et al[21] | 2016 | Cross-sectional | Beijing | 2012.01-2016.12 | 1 | 14-80 | 11000 | 51.65 | 2826/2313 | 46.7 | 45.8-47.7 |
| Wu et al[22] | 2014 | Cross-sectional | Beijing | 2010.01-2013.12 | 1 | 16-88 | 10331 | 69.29 | 3236/1353 | 44.4 | 43.5-45.4 |
| Cui et al[23] | 2020 | Cross-sectional | Beijing | 2018.06-2019.05 | 1 | 18-81 | 1058 | 52.65 | 175/163 | 31.9 | 29.1-34.9 |
| Zhang et al[24] | 2014 | Cross-sectional | Beijing | 2010 | 1 | 70.9 | 2006 | 50.10 | 851/822 | 83.4 | 81.7-85.0 |
| Zhang et al[25] | 2015 | Cross-sectional | Baoding (Hebei Province) | 2015 | 2 | 20-61 | 379 | 49.34 | 86/89 | 46.2 | 41.1-51.3 |
| Chen et al[26] | 2019 | Cross-sectional | Hohhot (Inner Mongolia Autonomous Region) | 2016-2019 | 1 | 18-81 | 13568 | 56.60 | 2480/1677 | 30.6 | 29.9-31.4 |
| Wang et al[27] | 2019 | Cross-sectional | Hailar District (Inner Mongolia Autonomous Region) | 2017.01-2017.12 | 1 | 7-88 | 15293 | 56.14 | 4232/3031 | 47.5 | 46.7-48.3 |
| Kan et al[28] | 2015 | Cross-sectional | Chifeng (Inner Mongolia Autonomous Region) | 2013.1.4-2013.5.31 | 2 | 17-91 | 3282 | 60.18 | 457/230 | 20.9 | 19.6-22.4 |
| Yan et al[29] | 2020 | Cross-sectional | Chengzhi (Shanxi Province) | 2019.01-2019.12 | 2 | 16-96 | 1224 | 69.61 | 536/259 | 65.0 | 62.2-67.6 |
| Li et al[30] | 2022 | Cross-sectional | Shanxi Province | 2019.01-2021.12 | 1 | 20-86 | 3365 | 75.99 | 474/197 | 19.9 | 18.6-21.3 |
| Zhang et al[31] | 2021 | Cross-sectional | Tianjin | 2017.08-2018.08 | 1 | 16-90 | 10000 | 54.09 | 1978/1626 | 36.0 | 35.1-37.0 |
| East China | |||||||||||
| Zhang et al[32] | 2020 | Cross-sectional | She County Tongcheng (Anhui Province) | NA | 1 | 20-90 | 1536 | 39.84 | 389/581 | 63.2 | 60.7-65.6 |
| Wang et al[33] | 2022 | Cross-sectional | Suzhou (Anhui Province) | 2017.01-2020.07 | 1 | 21-85 | 33634 | 57.73 | 7603/5647 | 39.4 | 38.9-39.9 |
| Peng et al[34] | 2021 | Cross-sectional | Anqing (Anhui Province) | 2019.04-2019.08 | 2 | 18-92 | 2725 | 60.51 | 816/610 | 52.3 | 50.4-54.2 |
| Han et al[35] | 2021 | Cohort study | Anhui Province | 2017.07-2020.11 | 1 | ≥ 18 | 1094 | 67.92 | 329/153 | 44.1 | 41.1-47.1 |
| Guo et al[36] | 2019 | Cross-sectional | Jieshou (Anhui Province) | 2017.1-2018.12 | 1 | 18-97 | 9684 | 45.34 | 1356/1676 | 31.3 | 30.4-32.2 |
| Hu et al[37] | 2015 | Cross-sectional | Fujian Province | 2013.02-2013.11 | 2 | 18-76 | 2770 | NA | 1435 | 51.8 | 49.9-53.7 |
| Xie et al[38] | 2020 | Cross-sectional | Ningde (Fujian Province) | 2019.10-2020.01 | 3 | 11-83 | 417 | 55.64 | 135/112 | 59.2 | 54.3-64.0 |
| Li et al[39] | 2016 | Cross-sectional | Jinjiang (Fujian Province) | 2015.01-2015.12 | 1 | 17-86 | 8751 | 66.67 | 2640/1440 | 46.6 | 45.6-47.7 |
| Liu et al[40] | 2016 | Cross-sectional | Xiamen (Fujian Province) | 2012-2014 | 1 | 44.8 ± 12.3 | 1444 | 66.90 | 475/216 | 47.9 | 45.2-50.5 |
| Chen et al[41] | 2022 | Cross-sectional | Zhangzhou (Fujian Province) | 2019.09-2020.08 | 1 | 20-89 | 2608 | 54.79 | 655/594 | 47.9 | 46.0-49.8 |
| Mao et al[42] | 2017 | Cross-sectional | Suzhou (Jiangsu Province) | 2015.01-2015.12 | 1 | 20-80 | 963 | 77.15 | 333/92 | 44.1 | 41.0-47.3 |
| Zhang et al[43] | 2019 | Cross-sectional | Nanjing (Jiangsu Province) | 2017.05-2017.08 | 1 | 64.34 ± 8.32 | 935 | 34.33 | 126/239 | 35.9 | 32.9-39.1 |
| Xie et al[44] | 2017 | Cross-sectional | Suzhou (Jiangsu Province) | 2015.10-2016.07 | 1 | 12-93 | 2664 | 52.74 | 769/753 | 57.1 | 55.2-59.0 |
| Jiang et al[45] | 2015 | Cross-sectional | Jiangsu Province | 2013.01-2014.10 | 1 | 17-95 | 3480 | 62.44 | 949/615 | 44.9 | 43.3-46.6 |
| Li et al[46] | 2019 | Cross-sectional | Nanjing (Jiangsu Province) | 2019 | 1 | 48.75 ± 5.97 | 700 | 57.14 | 132/124 | 36.6 | 33.0-40.3 |
| Wang et al[47] | 2023 | Cross-sectional | Nanjing (Jiangsu Province) | 2022 | 1 | NA | 15160 | 54.47 | 2721/1906 | 30.5 | 29.8-31.3 |
| Meng et al[48] | 2015 | Cross-sectional | Dongtai (Jiangsu Province) | 2012.06-2013.6 | 1 | 29-75 | 1598 | 52.00 | 403/307 | 44.4 | 42.0-46.9 |
| Ji et al[49] | 2023 | Cross-sectional | Suzhou (Jiangsu Province) | 2018.1-2018.12 | 2 | 18-89 | 6588 | 64.31 | 2370/1339 | 56.3 | 55.1-57.5 |
| Zhang et al[50] | 2018 | Cross-sectional | Jiuzhou (Jiangxi Province) | 2015.07-2016.10 | 1 | 18-90 | 1200 | 54.92 | 580 | 48.3 | 45.5-51.2 |
| Ren et al[51] | 2020 | Cross-sectional | Pingxiang (Jiangxi Province) | 2016.01-2019.06 | 2 | 9-92 | 10487 | 58.81 | 3011/2010 | 47.9 | 46.9-48.8 |
| Wang et al[52] | 2017 | Cross-sectional | Jiuzhou (Jiangxi Province) | 2016.01-2017.03 | 1 | 43.89 | 6165 | 74.16 | 1689/636 | 37.7 | 36.5-38.9 |
| Fang et al[53] | 2021 | Cross-sectional | Jingdezhen (Jiangxi Province) | 2008.7-2019.12 | 1 | 6-95 | 48353 | 50.08 | 10462/10301 | 42.9 | 42.5-43.4 |
| Xu et al[54] | 2019 | Cross-sectional | Cao County (Shandong Province) | 2018.04-2018.07 | 1 | 18-90 | 1182 | 49.49 | 198/175 | 31.6 | 28.9-34.3 |
| Shi et al[55] | 2022 | Cross-sectional | Xintai (Shandong Province) | 2021.04-2022.04 | 1 | 18-84 | 400 | 52.50 | 106/46 | 38.0 | 33.2-43.0 |
| Li et al[56] | 2015 | Cross-sectional | Jining (Shandong Province) | 2012.05-2013.05 | 1, 2 | 16-72 | 580 | 56.03 | 156/106 | 45.2 | 41.1-49.3 |
| Liang et al[57] | 2014 | Cross-sectional | Jining (Shandong Province) | 2012.02-2012.12 | 1 | 16-74 | 4366 | 68.60 | 1690/750 | 55.9 | 54.4-57.4 |
| Han et al[58] | 2020 | Cross-sectional | Jining (Shandong Province) | 2017.01-2017.12 | 2 | 19-91 | 2557 | 69.42 | 782/466 | 57.4 | 55.4-59.3 |
| Kong et al[59] | 2022 | Cohort study | Shandong Province | 2021.07-2022.01 | 1 | NA | 1173 | 47.06 | 204/226 | 36.7 | 33.9-39.5 |
| Zhang et al[60] | 2019 | Cross-sectional | Shanghai | 2017.01-2018.01 | 1 | 18-90 | 5164 | 52.05 | 1008/869 | 36.3 | 35.0-37.7 |
| Sun et al[61] | 2018 | Cross-sectional | Shanghai | 2016.09-2016.12 | 2 | 40-93 | 3258 | 43.92 | 451/461 | 28.0 | 26.5-29.6 |
| Jia et al[62] | 2020 | Cross-sectional | Shanghai | 2018.10-2019.9 | 1 | 25-70 | 29986 | 59.79 | 11547/6033 | 58.6 | 58.1-59.2 |
| Qiu et al[63] | 2022 | Cross-sectional | Hanghzou (Zhejiang Province) | 2019.09-2019.11 | 1 | 21-69 | 225 | 54.67 | 31/39 | 31.1 | 25.1-37.6 |
| Yu et al[64] | 2018 | Cross-sectional | Jiaxing (Zhejiang Province) | 2016.01-2017.06 | 1, 3 | 18-80 | 4220 | 47.44 | 900/709 | 38.1 | 36.7-39.6 |
| Zhou et al[65] | 2023 | Cross-sectional | Wenzhou (Zhejiang Province) | 2020.01.1-2022.08.1 | 2 | 18-71 | 568 | 85.56 | 197/38 | 41.4 | 37.3-45.5 |
| Zheng et al[66] | 2015 | Cross-sectional | Hanghzou (Zhejiang Province) | 2013.06-2014.05 | 1 | 12-76 | 2220 | 63.96 | 658/309 | 43.6 | 41.5-45.7 |
| Yang et al[67] | 2015 | Cross-sectional | Wenzhou (Zhejiang Province) | 2013.10-2014.4 | 1 | ≥ 20 | 15817 | 60.79 | 5078/3525 | 56.9 | 56.1-57.7 |
| Lin et al[68] | 2014 | Cross-sectional | Cangnan County (Zhejiang Province) | 2007.06-2012.12 | 3 | 18-70 | 11986 | 58.06 | 3351 | 28.0 | 27.2-28.8 |
| Yang et al[69] | 2015 | Cross-sectional | Taizhou (Zhejiang Province) | 2011.01-2013.12 | 1 | 20-70 | 2072 | 53.28 | 376/336 | 34.4 | 32.3-36.5 |
| Wang et al[70] | 2015 | Cross-sectional | Wenzhou (Zhejiang Province) | 2010.04-2015.02 | 2 | 0-14 | 4520 | NA | 2118 | 46.9 | 45.4-48.3 |
| Li et al[71] | 2017 | Cross-sectional | Anji County (Zhejiang Province) | 2015.01-2016.01 | 4 | 18-80 | 943 | 51.22 | 242/259 | 53.1 | 49.9-56.4 |
| Shen et al[72] | 2014 | Cross-sectional | Hanghzou (Zhejiang Province) | 2012.1-2012.12 | 2 | 20-91 | 7911 | 54.25 | 2180/1850 | 50.9 | 49.8-52.0 |
| He et al[73] | 2016 | Cross-sectional | Jiangshan (Zhejiang Province) | 2014.05-2015.08 | 2 | 3-5 | 3143 | 50.56 | 390/358 | 23.8 | 22.3-25.3 |
| Fang et al[74] | 2022 | Cross-sectional | Jinhua (Zhejiang Province) | 2019.1-2021.12 | 2 | NA | 2060 | 50.58 | 542/523 | 51.7 | 49.5-53.9 |
| Northwest China | |||||||||||
| Yu et al[75] | 2016 | Cross-sectional | Lanzhou (Gansu Province) | 2014.05-2015.07 | 1 | 16-96 | 3239 | 70.36 | 1197/482 | 51.8 | 50.1-53.6 |
| Xie[76] | 2021 | Cross-sectional | Yuan County (Gansu Province) | 2016.01-2020.01 | 1 | 12-84 | 2369 | 43.31 | 694/927 | 68.4 | 66.5-70.3 |
| Zou et al[77] | 2018 | Cross-sectional | Gansu Province | 2015.1-2015.12 | 2 | 27-87 | 1338 | 44.84 | 99/77 | 13.2 | 11.4-15.1 |
| Qin et al[78] | 2018 | Cross-sectional | Jingtai County (Gansu Province) | 2013.05-2017.06 | 1 | ≥ 14 | 7182 | 49.71 | 1667/1890 | 49.6 | 48.5-50.8 |
| Wu et al[79] | 2016 | Cross-sectional | Lanzhou (Gansu Province) | 2013.07-2015.06 | 2 | 18-81 | 442 | 57.24 | 137/89 | 51.1 | 46.4-55.9 |
| Li[80] | 2016 | Cross-sectional | Zhangye County (Gansu Province) | 2014.01-2015.12 | 1 | 18-83 | 1000 | 52.10 | 297/263 | 56.0 | 52.9-59.1 |
| Ma et al[81] | 2018 | Cross-sectional | Baiyin (Gansu Province) | 2018 | 1 | 20-70 | 16722 | 52.76 | 4290/2802 | 42.4 | 41.7-43.2 |
| Hou et al[82] | 2020 | Cross-sectional | Qingyang (Gansu Province) | 2016.1-2019.12 | 2 | 8-92 | 8321 | 60.06 | 2894/2206 | 61.3 | 60.2-62.3 |
| Zhang et al[83] | 2020 | Cross-sectional | Yinchuan (Ningxia Hui Autonomous Region) | 2018.06-2018.09 | 1 | ≥ 18 | 800 | 50.00 | 243/211 | 56.8 | 53.2-60.2 |
| Hu et al[84] | 2019 | Cross-sectional | Ningxia Hui Autonomous Region | 2018.12-2019.12 | 1 | 14-88 | 710 | 33.10 | 146/257 | 56.8 | 53.0-60.4 |
| Li et al[85] | 2024 | Cross-sectional | Qinghai Province | 2021-2022 | 1 | 3-85 | 1131 | 42.44 | 241/356 | 52.8 | 49.8-55.7 |
| Li et al[86] | 2022 | Cross-sectional | Qinghai Province | 2021.05-2012.12 | 1 | 4-90 | 4724 | 42.65 | 1047/1484 | 53.6 | 52.1-55.0 |
| Wang et al[87] | 2019 | Cross-sectional | Qinghai Province | 2017.08-2018.11 | 1 | 14-85 | 2103 | 48.64 | 775/784 | 74.1 | 72.2-76.0 |
| Zhang et al[88] | 2014 | Cross-sectional | Xian (Shaanxi Province) | 2014.01-2014.02 | 1 | 21-82 | 548 | 74.09 | 191/72 | 48.0 | 43.7-52.3 |
| Zhang et al[89] | 2015 | Cross-sectional | Xian (Shaanxi Province) | 2009-2013 | 2 | 18-70 | 16506 | 59.95 | 2983/1671 | 27.7 | 27.0-28.3 |
| Tang et al[90] | 2017 | Cross-sectional | Xian (Shaanxi Province) | 2016 | 1 | 18-78 | 6085 | 46.05 | 1463/1585 | 50.1 | 48.8-51.4 |
| Xiao et al[91] | 2021 | Cross-sectional | Xian (Shaanxi Province) | 2019.5-2020.05 | 1 | NA | 2100 | 60.81 | 600/383 | 46.8 | 44.7-49.0 |
| Di et al[92] | 2022 | Cross-sectional | Xian (Shaanxi Province) | 2016.09-2020.12 | 1 | 5-96 | 10016 | 45.06 | 1753/1502 | 32.5 | 31.6-33.4 |
| Zhu et al[93] | 2017 | Cross-sectional | Hoboksar (Xinjiang Uygur Autonomous Region) | NA | 1, 2 | 20-78 | 1200 | 43.58 | 362/480 | 70.2 | 67.5-72.7 |
| Yao and Wang[94] | 2017 | Cross-sectional | Urumqi (Xinjiang Uygur Autonomous Region) | 2016.05.10-2016.11.24 | 1 | NA | 2301 | 43.29 | 455/585 | 45.2 | 43.1-47.3 |
| Li et al[95] | 2023 | Cross-sectional | Tarbagatay Prefecture (Xinjiang Uygur Autonomous Region) | 2019.01-2022.06 | 2 | NA | 2840 | 50.56 | 846/771 | 56.9 | 55.1-58.8 |
| Wang et al[96] | 2016 | Cross-sectional | Xinjiang Uygur Autonomous Region | 2013.06-2014.06 | 1 | 17-87 | 4780 | 56.19 | 1264/1045 | 48.3 | 46.9-49.7 |
| Fan et al[97] | 2016 | Cross-sectional | Xinjiang Uygur Autonomous Region | 2014.09-2015.09 | 1 | 16-75 | 4774 | 41.10 | 1243/1890 | 65.6 | 64.3-67.0 |
| Southwest region | |||||||||||
| Shu[98] | 2021 | Cross-sectional | Tongren County (Guizhou Province) | 2018.04-2019.04 | 1 | 20-60 | 800 | 56.38 | 252/201 | 56.6 | 53.1-60.1 |
| Yang et al[99] | 2019 | Cross-sectional | Aba Tibetan and Qiang Autonomous Prefecture (Sichuan Province) | 2015.05-2016.12 | 1 | 2-92 | 544 | 46.51 | 73/93 | 30.5 | 26.7-34.6 |
| Zhou et al[100] | 2022 | Cross-sectional | Guangyuan (Sichuan Province) | 2020.3-2021.03 | 1 | 18-81 | 4296 | 44.41 | 1140/1128 | 52.8 | 51.3-54.3 |
| Xu et al[101] | 2019 | Cross-sectional | Luzhou (Sichuan Province) | 2017.05-2018.05 | 1, 2 | 14-87 | 18684 | 63.35 | 3788/2086 | 31.4 | 30.8-32.1 |
| Xiao et al[102] | 2020 | Cross-sectional | Yibin (Sichuan Province) | 2017.01-2018.12 | 4 | 2-6 | 622 | 54.98 | 71/60 | 21.1 | 17.9-24.5 |
| Luo et al[103] | 2022 | Cross-sectional | Nanchong (Sichuan Province) | 2021.8-2022.5 | 1 | ≥ 18 | 1478 | 50.47 | 375/327 | 47.5 | 44.9-50.1 |
| Zou et al[10] | 2023 | Cross-sectional | Chengdu (Sichuan Province) | 2013-2014 | 1 | NA | 16914 | 52.49 | 3640/3341 | 41.3 | 40.5-42.0 |
| Zou et al[10] | 2023 | Cross-sectional | Chengdu (Sichuan Province) | 2019-2021 | 1 | NA | 18281 | 46.74 | 2570/3035 | 30.7 | 30.0-31.3 |
| Wu et al[104] | 2017 | Cross-sectional | The Tibet Autonomous Region | NA | 1, 3 | 2-85 | 4332 | 53.46 | 1475/1208 | 61.9 | 60.5-63.4 |
| Cai et al[105] | 2018 | Cross-sectional | Lhasa (The Tibet Autonomous Region) | 2015.11-2016.7 | 1 | 5-85 | 1000 | 44.30 | 245/331 | 57.6 | 54.5-60.7 |
| Dawa et al[106] | 2021 | Cross-sectional | The Tibet Autonomous Region | 2018-2019 | 1 | NA | 717 | 52.44 | 196/192 | 54.1 | 50.4-57.8 |
| Zhang et al[107] | 2021 | Cross-sectional | Baishe (Yunnan Province) | 2020.04-2020.08 | 4 | 3-6 | 321 | 50.47 | 159/40 | 25.9 | 21.2-31.0 |
| Xie[108] | 2017 | Cross-sectional | Qujing (Yunnang Province) | 2016.1-2016.12 | 1 | 20-79 | 8790 | 58.07 | 1712/1172 | 32.8 | 31.8-33.8 |
| Wang et al[109] | 2015 | Cross-sectional | Yunang Province | 2013.01-2014.08 | 1 | ≥ 20 | 6680 | 72.54 | 1988/688 | 40.1 | 38.9-41.2 |
| Li et al[110] | 2018 | Cross-sectional | Kunming (Yunnan Province) | 2015.01-2017.12 | 1 | 20-75 | 606 | 36.63 | 115/75 | 31.4 | 27.7-35.2 |
| Jia et al[111] | 2018 | Cross-sectional | Yunnan Province | 2013.01-2015.02 | 1 | 21-85 | 1680 | 77.74 | 433/191 | 37.1 | 34.8-39.5 |
| Fu et al[112] | 2018 | Cross-sectional | Kunming (Yunnan Province) | 2013.1-2016.12 | 1 | 3-18 | 12932 | 53.15 | 1706/1408 | 24.1 | 23.3-24.8 |
| Ding et al[113] | 2017 | Cross-sectional | Dali (Yunnan Province) | 2014.06-2016.06 | 4 | 0-14 | 1127 | 51.46 | 75/53 | 11.4 | 9.6-13.4 |
| Chen and Sun[114] | 2019 | Cross-sectional | Puer (Yunnan Province) | 2018.5.1-2019.4.30 | 1 | 18-92 | 15328 | 56.36 | 3793/2502 | 41.1 | 40.3-41.9 |
| Liu et al[115] | 2017 | Cross-sectional | Chongqing | 2014.1-2014.12 | 1 | 44.1 ± 10.8 | 10912 | 52.91 | 1949/1801 | 34.4 | 33.5-35.3 |
| Liu and Lei[116] | 2020 | Cross-sectional | Chongqing | 2017.01-2018.06 | 1 | 7-18 | 1982 | 50.15 | 109/121 | 11.6 | 10.2-13.1 |
| Zhou[117] | 2018 | Cross-sectional | Chongqing | 2012.01-2016.08 | 1, 3 | 38.7 | 1000 | 54.60 | 324/203 | 52.7 | 49.6-55.8 |
| Meng and Sun[118] | 2018 | Cross-sectional | Chongqing | 2017.1-2017.12 | 2 | 15-85 | 27662 | 59.16 | 4222/2576 | 24.6 | 24.1-25.1 |
| Liu and Fan[119] | 2016 | Cross-sectional | Chongqing | 2014.01-2014.12 | 1 | 20-90 | 5788 | 65.74 | 1074/513 | 27.4 | 26.3-28.6 |
| South China | |||||||||||
| Zhu et al[120] | 2021 | Cross-sectional | Shenzhen (Guangdong Province) | 2019.1-2019.12 | 1 | 20-69 | 985 | 55.53 | 222/164 | 39.2 | 36.1-42.3 |
| Zhang et al[121] | 2015 | Cross-sectional | Guangzhou (Guangdong Province) | 2013.07-2014.06 | 1 | 8-68 | 440 | 45.45 | 120/132 | 57.3 | 52.5-61.9 |
| Liang and Yang[122] | 2018 | Cross-sectional | Yangjiang (Guangdong Province) | 2017.09-2019.08 | 2 | NA | 6703 | 54.20 | 1741/1564 | 49.3 | 48.1-50.5 |
| Yang[123] | 2021 | Cross-sectional | Jiangmen (Guangdong Province) | 2018.01-2019.12 | 2 | 28-88 | 100 | 52.00 | 17/7 | 24.0 | 16.0-33.6 |
| Xie et al[124] | 2014 | Cross-sectional | Zhuhai (Guangdong Province) | 2013.01-2013.09 | 2 | 21-70 | 2963 | 63.75 | 1156/473 | 55.0 | 53.2-56.8 |
| Xie et al[125] | 2021 | Cross-sectional | Chaoshan (Guangdong Province) | 2018.03-2020.06 | 1 | 16-88 | 3160 | 51.27 | 892/726 | 51.2 | 49.4-53.0 |
| Tang and Zhang[126] | 2021 | Cross-sectional | Shenzhen (Guangdong Province) | 2018.06-2020.11 | 2 | NA | 3605 | 53.09 | 1154/996 | 59.6 | 58.0-61.2 |
| Guan et al[127] | 2022 | Cross-sectional | Guangzhou (Guangdong Province) | 2020.1-2020.12 | 1 | 22-88 | 6436 | 54.93 | 1110/855 | 30.5 | 29.4-31.7 |
| Dai et al[128] | 2020 | Cross-sectional | Foshan (Guangdong Province) | 2018.1-2018.12 | 1 | 28-78 | 15730 | 52.45 | 3855/3157 | 44.6 | 43.8-45.4 |
| Li et al[129] | 2022 | Cross-sectional | Shenzhen (Guangdong Province) | 2020.09-2021.09 | 1 | ≥ 20 | 5007 | 59.18 | 1052/700 | 35.0 | 33.7-36.3 |
| Xu and Yan[130] | 2018 | Cohort study | Nanning (Guangxi Zhuang Autonomous Region) | 2014.03-2017.06 | 1 | 20-65 | 2956 | 58.93 | 787/552 | 45.3 | 43.5-47.1 |
| Weng[131] | 2017 | Cross-sectional | Laibin (Guangxi Zhuang Autonomous Region) | 2014.01-2012.03 | 1 | 10-89 | 6328 | 59.07 | 2308/1054 | 53.1 | 51.9-54.4 |
| Lin and Cheng[132] | 2016 | Cross-sectional | Hechi (Guangxi Zhuang Autonomous Region) | 2016.01-2016.03 | 1 | 20-75 | 1500 | 54.47 | 486/226 | 47.5 | 44.9-50.0 |
| Wang[133] | 2021 | Cross-sectional | Nanning (Guangxi Zhuang Autonomous Region) | 2017.01-2019.12 | 1 | 21-75 | 1175 | 67.83 | 268/114 | 32.5 | 29.8-35.3 |
| Chen et al[134] | 2017 | Cross-sectional | Hezhou (Guangxi Zhuang Autonomous Region) | 2015.05-2015.12 | 1 | 18-80 | 600 | 58.67 | 162/130 | 48.7 | 44.6-52.7 |
| Chen[135] | 2022 | Cross-sectional | Nanning (Guangxi Zhuang Autonomous Region) | 2021.01-2021.12.31 | 2 | 19-89 | 1485 | 75.82 | 251/99 | 23.6 | 21.4-25.8 |
| Cao et al[136] | 2017 | Cross-sectional | Baise (Guangxi Zhuang Autonomous Region) | 2012.1-2015.12 | 2 | ≥ 7 | 3363 | 52.75 | 930/659 | 47.2 | 45.6-49.0 |
| Zhang et al[137] | 2023 | Cross-sectional | Qionghai (Hainan Province) | NA | 1 | 14-85 | 535 | 36.64 | 77/152 | 42.8 | 38.6-47.1 |
| Qiu and Xu[138] | 2017 | Cross-sectional | Chengmai County (Hainan Province) | 2015.01-2016.12 | 2 | 22-85 | 1977 | 68.03 | 483/225 | 35.8 | 33.7-38.0 |
| Ma et al[139] | 2015 | Cross-sectional | Haikou (Hainan Province) | 2013.07-2013.10 | Interdental tartar | 21-81 | 4122 | 51.55 | 550/507 | 25.6 | 24.3-27.0 |
| Zeng et al[140] | 2023 | Cross-sectional | Wuzhishan (Hainan Province) | 2023.03 | 1 | ≥ 18 | 528 | 26.70 | 61/162 | 42.2 | 38.0-46.6 |
| Liu et al[141] | 2023 | Cross-sectional | Hainan Province | 2021.07-2022.04 | 1 | NA | 1355 | 44.72 | 269/360 | 46.4 | 43.7-49.1 |
| Central China | |||||||||||
| Zhao et al[142] | 2022 | Cross-sectional | Zhengzhou (Henan Province) | 2020.01-2020.12 | 1 | 18-80 | 8312 | 61.81 | 2009/1217 | 38.8 | 37.8-39.9 |
| Chai et al[143] | 2021 | Cross-sectional | Zhengzhou (Henan Province) | 2018-2019 | 1 | 18-87 | 2589 | 55.66 | 391/303 | 26.8 | 25.1-28.6 |
| Wang et al[144] | 2018 | Cross-sectional | Henan Province | 2017.01-2017.06 | 1 | 18-67 | 2974 | 56.93 | 599/418 | 34.2 | 32.5-35.9 |
| Liu et al[145] | 2021 | Cross-sectional | Nanyang (Henan Province) | 2019.05-2021.02 | 2 | 18-78 | 856 | 59.00 | 324/206 | 61.9 | 58.6-65.2 |
| Gu et al[146] | 2014 | Cross-sectional | Luohe (Henan Province) | NA | 2 | 13-77 | 1874 | 49.73 | 559/524 | 57.8 | 55.5-60.0 |
| Fan et al[147] | 2015 | Cross-sectional | Pingdingshan (Henan Province) | 2012.04-2012.06 | 2 | 20-83 | 449 | 61.02 | 153/65 | 48.6 | 43.8-53.3 |
| Yu et al[148] | 2022 | Cross-sectional | Zhengzhou (Henan Province) | 2020.09-2021.4 | 2 | 45.36 ± 19.38 | 772 | 42.75 | 173/246 | 54.3 | 50.7-57.8 |
| Lei et al[149] | 2023 | Cross-sectional | Zhengzhou (Henan Province) | 2020.09-2021.03 | 2 | 3-90 | 731 | 54.31 | 164/233 | 54.3 | 50.6-58.0 |
| Zhang et al[150] | 2019 | Cross-sectional | Wuhan (Hubei Province) | 2017.05-2017.10 | 1 | 20-60 | 11365 | 72.59 | 3449/1242 | 41.3 | 40.4-42.2 |
| Yang[151] | 2020 | Cross-sectional | Jingmen (Hubei Province) | 2018.01-2018.12 | 1 | 15-81 | 984 | 57.62 | 243/125 | 37.4 | 34.4-40.5 |
| Li[152] | 2022 | Cross-sectional | Xianyang (Hubei Province) | 2016.10-2017.07 | 1 | 15-87 | 1756 | 56.09 | 598/445 | 59.4 | 57.1-61.7 |
| Xi[153] | 2014 | Cross-sectional | Wuhan (Hubei Province) | 2012.03-2013.02 | 1 | 16-80 | 3012 | 48.51 | 684/733 | 46.7 | 45.0-48.5 |
| Liu et al[154] | 2017 | Cross-sectional | Wuhan (Hubei Province) | 2015.07-2015.08 | 1 | 20-91 | 2366 | 55.83 | 376/315 | 29.2 | 27.4-31.1 |
| Zhou and Lin[155] | 2018 | Cross-sectional | Huangshi (Hubei Province) | 2013.10-2016.6 | 1 | 3-13 | 1240 | 51.94 | 596/284 | 46.0 | 43.2-48.9 |
| Li et al[156] | 2014 | Cross-sectional | Xiaogan (Hubei Province) | 2012.6-2013.2 | 2 | 12-81 | 2005 | 55.16 | 899/486 | 50.7 | 48.5-52.9 |
| Jia et al[157] | 2016 | Cross-sectional | Wuhan (Hubei Province) | 2015.03-2015.08 | 1 | 51.2 | 2180 | 52.02 | 549/446 | 47.0 | 44.9-49.1 |
| Deng et al[158] | 2020 | Cohort study | Wuhan (Hubei Province) | 2018.1-2019.12 | 1 | 20-70 | 2619 | 63.54 | 778/331 | 42.3 | 40.4-44.3 |
| Li et al[159] | 2015 | Cross-sectional | Chenzhou (Hunan Province) | 2013.08-2014.12 | 2 | > 20 | 7015 | 34.23 | 663/1230 | 27.0 | 25.9-28.0 |
| Peng et al[160] | 2019 | Cross-sectional | Chenzhou (Hunan Province) | 2016.01-2017.01 | 2 | 22-70 | 3123 | 63.24 | 680/382 | 34.0 | 32.3-35.7 |
NA: Not available.
The pooled prevalence of H. pylori in Mainland China
The prevalence of H. pylori infection was analyzed in 152 studies. The heterogeneity test produced an I2 = 99.7%, P < 0.001, necessitating the use of a random-effects model. The combined findings suggest that the prevalence of H. pylori infection in China from 2014 to 2023 stood at 42.8% (95%CI: 40.7-44.9). The corresponding forest plot is shown in Supplementary Figure 1[10-160].
Subgroup analysis
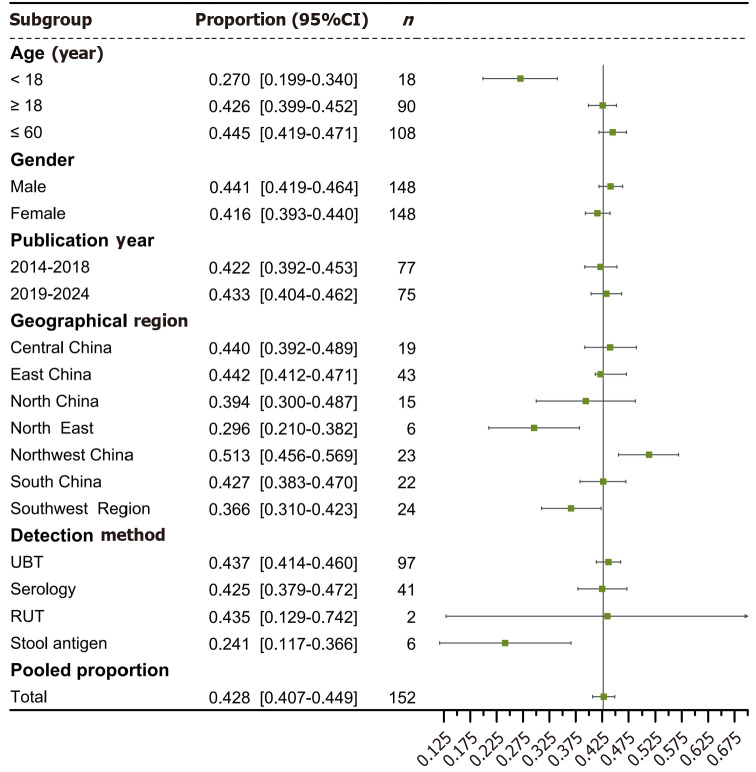
Owing to substantial heterogeneity among the studies, prevalence rates were separately analyzed based on province, municipality, autonomous region, geographic region, gender, age, detection method, and publication year (Figure 2).
Figure 2.
Subgroup analysis of Helicobacter pylori prevalence. N: Number of included studies; UBT: Urea breath test; RUT: Rapid urease test.
Among the 30 provinces, municipalities, and autonomous regions, the highest prevalence of H. pylori was observed in Qinghai Province at 60.2% (95%CI: 46.5-73.9), and the lowest in Liaoning Province at 24.7% (95%CI: 15.7-33.7). Forest plots detailing the prevalence across these areas are presented in Supplementary Figure 2. A bubble diagram illustrating the incidence of H. pylori across these administrative divisions and geographic areas is provided in Figure 3. Of the seven geographical regions, the Northwest exhibited the highest prevalence at 51.3% (95%CI: 45.6-56.9), while the Northeast had the lowest at 29.6% (95%CI: 21.0-38.2). These forest plots are available in Supplementary Figure 3.
Figure 3.
Bubble diagram of Helicobacter pylori prevalence.
Regarding gender differences, the prevalence of H. pylori was slightly higher in males at 44.1% (95%CI: 41.9-46.4) than in females at 41.6% (95%CI: 39.3-44.0); these findings are depicted in Supplementary Figure 4. The meta-analysis revealed that the prevalence of H. pylori was 27.0% (95%CI: 19.9-34.0) in minors and 42.6% (95%CI: 39.9-45.2) in adults. Among the elderly (≥ 60 years), a higher prevalence of 44.5% (95%CI: 41.9-47.1) was noted (Supplementary Figures 5 and 6).
Concerning detection methods, 97 studies used the UBT and 2 studies employed the Rapid Urease Test (RUT). The infection rates were 43.7% (95%CI: 41.4-46.0) using the UBT, 42.5% (95%CI: 37.9-47.2) with the serum antibody test, 43.5% (95%CI: 12.9-74.2) using the RUT, and 24.1% (95%CI: 11.7-36.6) with the H. pylori stool antigen method. The highest infection rate was detected by the UBT method, while the lowest was by the H. pylori stool antigen method. Forest plots for these testing modalities are included in Supplementary Figure 7. From the literature spanning 2014-2018, the prevalence of H. pylori infection was 42.2% (95%CI: 39.2-45.3), and from 2019-2024, it was 43.3% (95%CI: 40.4-46.2). The slight increase in prevalence over these periods was not statistically significant (Supplementary Figures 8 and 9).
Sensitivity analysis
Sensitivity analysis of the combined results was performed using the "leave-one-out" method. The robustness of the study results was confirmed as there were no significant changes; this analysis is shown in Supplementary Figure 10.
Publication bias assessment
Publication bias was evaluated using a funnel plot and the AS-Thompson test, with arcsine transformation used in cases of significant heterogeneity. The analysis yielded a symmetrical funnel plot (t = 1.42, P = 0.157), indicating minimal publication bias. These results are visually displayed in Supplementary Figure 11 and 12.
DISCUSSION
H. pylori, a gram-negative microaerobic bacterium, forms colonies on the epithelial surfaces of the human gastric mucosa, leading to chronic infections[162]. This bacterium has a global prevalence, affecting approximately fifty percent of the world's population, thereby constituting a significant health issue. While a significant majority of infected individuals exhibit no symptoms, the infection carries considerable health implications, as 1%-3% of those affected may progress to GC, and 0.1% may develop mucosa-associated lymphoid tissue lymphoma[163]. The optimal initial therapeutic approach involves a combination of proton pump inhibitors (PPI), amoxicillin, and clarithromycin, commonly referred to as PPI, amoxicillin, and clarithromycin. In regions with elevated primary clarithromycin resistance, bismuth-based quadruple therapies are becoming a favored alternative[164]. Additionally, traditional Chinese medicine[165,166] and microecological agents[167,168] have become crucial in boosting eradication rates and combating drug resistance to H. pylori.
Given the demographic and regional disparities in China, understanding the prevalence of H. pylori is vital for informing future research and healthcare strategies.
This study revealed that the infection rate of H. pylori in China from 2014 to 2023 was 42.8% (95%CI: 40.7-44.9), a decrease from the rates reported in earlier periods by Ren et al[3] from 1990 to 2019 (44.2%, 95%CI: 43.0-45.5) and Li et al[169] from 1983 to 2020 (49.6%, 95%CI: 46.9-52.4). Research by Li et al[170] suggests that the global estimated prevalence of H. pylori decreased from 58.2% (95%CI: 50.7-65.8) between 1980 and 1990 to 43.1% (95%CI: 40.3-45.9) between 2011 and 2022. With the continuous improvement of living environment and hygiene level, and the increasing coverage of basic medical security, the prevalence of H. pylori in China has also shown a downward trend, similar to the global trend of H. pylori prevalence.
The ingestion of raw water and the consumption of vegetables and fruits that have been washed from contaminated water sources represent risk factors for H. pylori infection[171,172]. Nevertheless, the dissemination of H. pylori infections has been constrained alongside enhancements in living standards and hygiene, including augmented access to clean water and more effective sewage treatment[173]. Public awareness of H. pylori and its modes of transmission also resulted in reducing infection rates[174,175]. Studies[176,177] have shown that the public's knowledge about H. pylori and how it is spread has increased in the last decade. The detection of H. pylori infection has been included in the health examination items. The rapid, simple and reliable detection method has been preliminarily accessible. The awareness of active medical treatment among infected people was significantly enhanced[7]. The above reasons have all contributed to the decline of H. pylori infection rate in China in the past decade.
However, the diseases associated with them remain among the great challenges to public health. This report presents updated comprehensive trends in clinically significant and relevant H. pylori infection based on a critical analysis of 152 studies that have been published over the past decade. The results of this study is of a certain credibility and timeliness, and has a certain clinical reference value.
The highest prevalence rate of H. pylori infection was found in Northwest China, which showed a percentage of 51.3% (95%CI: 45.6-56.9). In the northwest region, it is highly prevalent in Qinghai Province, showing a prevalence of 60.2% (95%CI: 46.5-73.9). On the contrary, the lowest infection rates were observed in Northeast China, where the prevalence was 29.6% (95%CI: 21.0-38.2), and the minimum rate was in Liaoning Province at 24.7% (95%CI: 15.7-33.7).
H. pylori has co-evolved with the human host ever since its origin. Local transmission and genetic isolation have facilitated the development of different bacterial populations that are characteristic for geographical areas[178]. You et al[179] conducted a comparative genomic analysis of the genomic sequence features of Chinese H. pylori, and the results of Neighbor Joining analyses of 10 Chinese H. pylori strains showed geographic clustering of H. pylori strains in China. Geographical factors play a long-term and fundamental role in regional development. The expansive northwest region of China, distinguished by its extensive deserts and delicate ecosystems, also sustains robust animal husbandry and a considerable population of nomadic herders. Inhabitants predominantly consume a meat-rich diet[180], with vegetable intake falling below the levels suggested by the Chinese Balanced Dietary Pagoda[181]. The economic development in Northwest China is relatively underdeveloped, and compared with other regions, the allocation of health resources is insufficient[182]. Oral-oral and fecal-oral pathways stand as the primary mechanisms for the transmission of H. pylori, which tends to cluster within families[183]. The region of Northeast China is characterised by fertile land, abundant water and food resources, rich mineral resources and a relatively early economic start. The long winter season and low population density serve to restrict the dissemination of H. pylori infection. Although infection rates in the Northeast are comparably low, the prevalent antibiotic resistance remains a substantial issue[184]. Two provinces in the Southwest region, Qinghai-Tibet (58.1%; 95%CI: 53.6-62.6) and Guizhou Province (56.6%; 95%CI: 53.1-60.1), have particularly high infection rates.
Zhang et al[185] has shown that the high rates of H. pylori infection and GC among Tibetan residents of the plateau are not only related to the backward level of health and economy, but also to the environmental characteristics of the plateau. The frigid, oxygen-deprived conditions of the plateau can result in gastric mucosal injury and disruption to the intestinal barrier, thereby enhancing susceptibility[186]. The Guizhou Province region has a humid climate and the locals enjoy spicy diets and pickled foods. Both were found to be independent risk factors for H. pylori infection[187,188].
Consequently, elements such as environmental conditions, economic status, and sanitation practices collectively impact the prevalence of H. pylori to varying extents.
Addressing the pronounced prevalence of H. pylori infection in Northwest China, particularly given the high incidence and mortality rates of GC in Qinghai Province and Guizhou Province[6], we should launched health education initiatives in these high-incidence and high-risk areas to improve the population's awareness of the risks associated with H. pylori, alongside the available treatment options and their benefits.
So as to fostering changes in knowledge, attitudes, and behaviors, and enable general population actively participate in the work of prevention, screening and treatment of H. pylori. This approach additionally facilitates the primary prevention of GC[177,189]. In regions characterized by heightened antibiotic resistance, the use of antibiotics should be meticulously regulated. Where conditions permit, treatment programmes can be tailored to the antibiotic susceptibility results of individual patients. Compared to these high prevalence areas, infections in other areas are not as serious. However, the prevention and treatment of the disease should not be neglected. In these areas, the compliance of infected people with prescribed treatment and re examination should be improved in order to improve the eradication rate[190]. At the same time, family based management and treatment strategies should be implemented to avoid reinfection. Promote a healthy diet and reduce the intake of ultra-processed food; develop good living habits and actively prevent the occurrence of H. pylori infection[191].
In this study, the prevalence of infection was notably higher in adults compared to minors, with significant prominence in the elderly (> 60 years) (Supplementary Figure 5 and 6). The elderly are more susceptible due to distinctive gastric features, including delayed gastric emptying[192], diminished glandular function[193,194], and a less diverse microbial environment in the stomach[195,196]. People worldwide are living longer. The worldwide demographic is experiencing a significant increase in age, with forecasts from the World Health Organization suggesting that the population aged 60 years and above will double to 2.1 billion by the year 2050[197]. H. pylori is associated with gastrointestinal disturbances as well as the development of various systemic diseases. Studies suggest that H. pylori infection could increase the likelihood of developing neurodegenerative disorders, including Alzheimer's disease[198,199] and Parkinson's syndrome[200], in addition to cardiovascular diseases[201]. In treating the elderly, medical professionals must consider factors like antibiotic resistance, potential drug interactions, and adherence to medication, while carefully balancing the risks and benefits of eradication therapy[202,203].
The incidence of H. pylori infection in pediatric populations shows considerable variation internationally, with reported rates ranging from 3.2% to 84%, influenced by factors including geographical location, environmental conditions, diagnostic techniques, host specificity, and the timing of the study[204]. Factors such as early exposure to pre-chewed food, familial history of gastric disorders, the sharing of personal hygiene items like towels and mouthwash cups[205,206], and low socioeconomic status[207] are significant contributors to the risk of H. pylori infection in children. Recent updated guidelines do not recommend the "test-and-treat" approach for asymptomatic H. pylori infections in pediatric populations, referencing a lack of substantial evidence supporting its effectiveness in reducing the risk of future GC[208].
Regarding detection methods, the highest infection rate identified by the UBT was 43.7% (95%CI: 41.4-46.0), surpassing those detected by serological tests, stool antigen tests, and RUT. Ma et al[139] reported an H. pylori positivity rate of 26.85% utilizing an immunocolloidal gold assay for interdental tartar in subjects. The UBT, preferred for its non-invasive, painless, and repeatable nature, includes two variations: 13C-UBT and 14C-UBT, with the former being more sensitive, non-radioactive, and therefore safer[209]. Recent global guidelines endorse the UBT as the preferred diagnostic tool for H. pylori, recommending it for both initial diagnosis and post-eradication evaluation[210-212], with an emphasis on maintaining stringent quality controls to improve the test's precision. The monoclonal-based stool antigen test also remains a reliable, recommended method with comparable accuracy to the UBT, particularly beneficial for children under six who are less suited for UBT[213]. Serum H. pylori antibody tests are predominantly used in clinical epidemiological studies to ascertain both past and current infections[164,214], and their diagnostic accuracy is enhanced when used in conjunction with UBT[215]. However, the value of serological screening is limited in areas with low infection rates[216]. The identification of H. pylori subtypes aids in assessing infection status and virulence, and can forecast the development of GC[217]. Although RUTs are highly sensitive, their specificity is compromised by factors like sample size and the focal distribution of H. pylori in the stomach[218]. Selecting a diagnostic approach requires consideration of regional infection rates, clinical scenarios, patient age, among other factors, to ensure the selection of suitable and reliable tests for effective treatment planning.
This study's strengths are evident in: (1) Utilizing recent literature spanning the last ten years to mirror the current situation of H. pylori infection; (2) Conducting an exhaustive examination of H. pylori's current prevalence in China, pinpointing key demographics and areas where infection rates are heightened; (3) Incorporating a significant corpus of studies with ample sample sizes, excluding any with fewer than 50 subjects to reduce potential small-sample biases; and (4) Rigorous adherence to established protocols for selecting literature and extracting data, supplemented by cross-validation to enhance the reliability of findings.
The limitations of this study include the following: (1) Some provinces and diagnostic modalities in this study had a low number of included studies, which may have had some impact on the results; and (2) Although we performed subgroup analyses for the results of the study in terms of geographic region, testing modality, age, gender, and so on, there was still a large degree of heterogeneity in the study.
CONCLUSION
In summary, the prevalence of H. pylori infection in China from 2014-2023 is 42.8% (95%CI: 40.7-44.9), marking a decrease from the preceding decade. The rates of H. pylori infection vary depending on geographic location, detection methods, and population demographics. Given the substantial disease burden associated with H. pylori infections, further studies into the mechanisms behind the disparities in H. pylori prevalence, both in China and globally, is both significant and urgent.
ACKNOWLEDGEMENTS
We are very grateful to every participant for their support and contributions to this study.
Footnotes
Conflict-of-interest statement: The authors disclose that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade C, Grade C
Novelty: Grade B, Grade B, Grade B
Creativity or Innovation: Grade B, Grade B, Grade B
Scientific Significance: Grade B, Grade B, Grade B
P-Reviewer: Zhang W; Zhang J S-Editor: Luo ML L-Editor: A P-Editor: Zheng XM
Contributor Information
Lu Xie, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; The First Clinical Medical School, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China.
Guang-Wei Liu, Department of Spleen, Stomach, Liver and Gallbladder, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China.
Ya-Nan Liu, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; The First Clinical Medical School, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China.
Peng-Yu Li, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; Henan Key Laboratory of Viral Diseases Prevention and Treatment of Chinese Medicine, Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China.
Xin-Ning Hu, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; The First Clinical Medical School, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China.
Xin-Yi He, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; The First Clinical Medical School, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China.
Rui-Bo Huan, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; The First Clinical Medical School, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China.
Tai-Long Zhao, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; The First Clinical Medical School, Henan University of Chinese Medicine, Zhengzhou 450046, Henan Province, China.
Hui-Jun Guo, Department of Acquired Immune Deficiency Syndrome Treatment and Research Center, The First Affiliated Hospital of Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China; Henan Key Laboratory of Viral Diseases Prevention and Treatment of Chinese Medicine, Henan University of Chinese Medicine, Zhengzhou 450000, Henan Province, China. guohuijun@hactcm.edu.cn.
References
- 1.Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, Malfertheiner P, Graham DY, Wong VWS, Wu JCY, Chan FKL, Sung JJY, Kaplan GG, Ng SC. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017;153:420–429. doi: 10.1053/j.gastro.2017.04.022. [DOI] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Ren S, Cai P, Liu Y, Wang T, Zhang Y, Li Q, Gu Y, Wei L, Yan C, Jin G. Prevalence of Helicobacter pylori infection in China: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2022;37:464–470. doi: 10.1111/jgh.15751. [DOI] [PubMed] [Google Scholar]
- 4.Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can. 1998;19:170–176. [PubMed] [Google Scholar]
- 5.Li WQ, Zhang JY, Ma JL, Li ZX, Zhang L, Zhang Y, Guo Y, Zhou T, Li JY, Shen L, Liu WD, Han ZX, Blot WJ, Gail MH, Pan KF, You WC. Effects of Helicobacter pylori treatment and vitamin and garlic supplementation on gastric cancer incidence and mortality: follow-up of a randomized intervention trial. BMJ. 2019;366:l5016. doi: 10.1136/bmj.l5016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng RS, Chen R, Han BF, Wang SM, Li L, Sun KX, Zeng HM, Wei WW, He J. [Cancer incidence and mortality in China, 2022] Zhonghua Zhongliu Zazhi. 2024;46:221–231. doi: 10.3760/cma.j.cn112152-20240119-00035. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention. White Paper: Helicobacter pylori Infection Prevention and Control in China. 2023. Available from: https://icdc.chinacdc.cn/zxxx/xwdt/202306/t20230603_266504.html .
- 8.Zhang JZ. [Interpretation of key points from the White Paper on Helicobacter pylori Infection Prevention and Control in China] Zhongguuo Zhongxiyi Jiehe Xiaohua Zazhi. 2024;32:279–282. [Google Scholar]
- 9.Chiang TH, Chang WJ, Chen SL, Yen AM, Fann JC, Chiu SY, Chen YR, Chuang SL, Shieh CF, Liu CY, Chiu HM, Chiang H, Shun CT, Lin MW, Wu MS, Lin JT, Chan CC, Graham DY, Chen HH, Lee YC. Mass eradication of Helicobacter pylori to reduce gastric cancer incidence and mortality: a long-term cohort study on Matsu Islands. Gut. 2021;70:243–250. doi: 10.1136/gutjnl-2020-322200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou JC, Wen MY, Huang Y, Chen XZ, Hu JK SIGES Research Group. Helicobacter pylori infection prevalence declined among an urban health check-up population in Chengdu, China: a longitudinal analysis of multiple cross-sectional studies. Front Public Health. 2023;11:1128765. doi: 10.3389/fpubh.2023.1128765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang YB, Li XO, Li Y. [Analysis of Helicobacter pylori infection in medical staff of a hospital in Jilin] Zhongguo Weisheng Chanye. 2016;13:73–75. [Google Scholar]
- 12.Wang GJ, Jin SL, Li YM. [Analysis of the positive rate of Helicobacter pylori in health examination population and health education] Zhongguo Gongcheng Zuzhi Yanjiu. 2014;z1:51–52. [Google Scholar]
- 13.Zhang XJ, Huang YH, Yang L, Li LL, Li J, Ni J, Xu LF. [Epidemiology investigation on the Helicobacter pylori infection of pre-school children in Shenyang] Zhongguo Ertong Baojian Zazhi. 2014;22:408–411. [Google Scholar]
- 14.Zhu CM, Sun ML, Xu JJ, Fang JM. [Analysis on the Detection Results of Helicobacter Pylori in Healthy People] Jinzhou Yike Daxue Xuebao. 2020;41:39–40, 46. [Google Scholar]
- 15.Jiang FQ, Hao CY, Lu XY, Zhu H, Wang XN, Gu YN, Cheng YJ. [Helicobacter pylori infection in healthy population in Dalian city] Dalian Yike Daxue Xuebao. 2015;37:182–185. [Google Scholar]
- 16.Ji N, Gu YN. [Prevalence of Helicobacter pylori Infection Among the Healthy Asymptomatic Population] Mianyi Biaoji Fenxi Yu Linchuang. 2016;23:303–305. [Google Scholar]
- 17.Zheng H, Peng YM, Zhang ZH, Li HF. [Analysis of the infection status of helicobacter pylori in healthy people under physical examination in Tangshan area] Dangdai Yixue. 2022;28:33–35. [Google Scholar]
- 18.Yang SS, Deng X, Si ZM, Ye H, Zhang XZ. [Analysis of Helicobacter pylori infection in traditional Chinese Medicine Department of general hospital] Beijing Yixue. 2020;42:782–783, 786. [Google Scholar]
- 19.Zhao S, Xu XW, Li AH. [Epidemiology of Helicobacter pylori infection in asymptomatic children in Beijing areas] Zhongguo Shiyong Erke Zazhi. 2017;32:754–758. [Google Scholar]
- 20.Xi WJ, Tan XJ, Sha CM, Wang L, Peng LH, Yang YS, Wang CB. [Prevalence and risk factors of Helicobactor pylori infection among 291 school-age children] Jiefangjun Yixueyuan Xuebao. 2018;39:753–755. [Google Scholar]
- 21.Chen L, Jia XM, Wang SX. [Analysis of 8809 cases of Helicobacter pylori in Beijing miyun area] Xiandai Xiaohua Ji Jieru Zhiliao. 2016;21:263–265. [Google Scholar]
- 22.Wu JJ, Ying MZ, Cao XT, Li F, Zeng Q. [Prevalence of helicobacter pylori infection in individuals undergoing health examination] Yinanbing Zazhi. 2014;13:1118–1122. [Google Scholar]
- 23.Cui WW, Wang K, Liang L, Guo WF. [Helicobacter pylori infection status and its influencing factors in physical examination population] Huanan Yufang Yixue. 2020;46:613–616. [Google Scholar]
- 24.Zhang M, Zhou YZ, Li XY, Tang Z, Zhu HM, Yang Y, Chhetri JK. Seroepidemiology of Helicobacter pylori infection in elderly people in the Beijing region, China. World J Gastroenterol. 2014;20:3635–3639. doi: 10.3748/wjg.v20.i13.3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang WW. [Analysis of 379 cases of Helicobacter pylori antibody detection in healthy people] Jiceng Yixue Luntan. 2015;19:3958–3959. [Google Scholar]
- 26.Chen GY, Wang XY, Na RS, Mei Y, Heng YJ, Wu RH. [Investigation and analysis of Helicobacter pylori infection among health examination population in Hohhot] Neimenggu Yixue Zazhi. 2019;51:1324–1326. [Google Scholar]
- 27.Wang GQ, Song XC, Sui X, Zhang J, Bao YH, Su NE. [Investigation of Helicobacter pylori infection in health examination population in Hailar area] Hulunbeier Daxue Xuebao. 2019;27:111–113. [Google Scholar]
- 28.Kan BH, Sun LH, Wu CH. [Analysis of results of Helicobacter pylori infection in physical examination people] Guoji Jianyan Yixue Zazhi. 2015;36:3164–3165. [Google Scholar]
- 29.Yan CW, Yan XY, Bao LX, Hu HB, Liu H, Shen LJ. [Analysis of the detection results of helicobacter pylori antibody among the physical examination population in Changzhi City] Zhongguo Linchang Shiyong Yixue. 2020;11:48–52. [Google Scholar]
- 30.Li XB, Wang H, Li JP, Guo HL, Liu LY. [Study on the influence of Helicobacter pylori infection in health examination population at Shanxi port] Shanxi Yiyao Zazhi. 2022;51:2452–2454. [Google Scholar]
- 31.Zhang YQ, Zhao CY, Sun ZJ. [Analysis of Helicobacter Pylori Infection Rate and Related Influencing Factors in 10000 Health Examination Populations in Tianjin] Jiankang Tijian Yu Guanli. 2021;2:115–118. [Google Scholar]
- 32.Zhang MW, Wang JC, Wang QZ, Ke XQ, Zheng HL, Cui YY. [Epidemiological investigation of Helicobacter pylori in central and southern area of Anhui] Zhonghua Quanke Yixue. 2020;18:1395–1398. [Google Scholar]
- 33.Wang L, Zhang YS, Ma LJ, Zhuang DM, Cao J, Xin Y, Wang XR. [Helicobacter pylori infection rate and expressions of CagA and VacA in Suzhou region of Anhui Province] Zhonghua Xiaohuabing Yu Yingxiang Zazhi. 12:41–45. [Google Scholar]
- 34.Peng J, Li XY, Wang WJ, Hu XD, Han TT, Zhu FL, Yu ZX, Liao Y, Huang XJ. [Investigation of Helicobacter Pylori Infection in Health Examination Population in Anqing Area] Xiandai Jianyan Yixue Zazhi. 2021;36:18–21. [Google Scholar]
- 35.Han Y, Yan JJ, Fang XX, Kong RD. [Correlation between current infection of Helicobacter pylori and metabolic syndrome] Shiyong Linchuang Yixue Zazhi. 2021;25:37–41. [Google Scholar]
- 36.Guo C, Xiang Y, Chen M, Hao XQ, Guo SJ. [Study on Helicobacter pylori infection in health examination subjects and outpatients in Jieshou City, Anhui Province] Xiandai Xiaohua Ji Jieru Zhenliao. 2019;24:969–971, 976. [Google Scholar]
- 37.Hu TM, Ni XQ, You HM, Zhuang LL, Huang YD, Huang SF, Zhuang YY. [Investigation and analysis of Helicobacter pylori infection and its genotype in Southern Fujian, China] Zhonghua Xiaohua Zazhi. 2015;35:262–264. [Google Scholar]
- 38.Xie JJ, Wu YL, Jiang ZJ, Huang LJ, Lin Y, Lin M, Yang T, Lin WX, Huang ZX, Xia NN. [Investigation and analysis of infection status and antibiotic resistance of Helicobacter pylori in patients with upper gastrointestinal symptoms in the border area of Fujian and Zhejiang province] Xiandai Xiaohua Ji Jieru Zhenliao. 2020;25:724–727, 734. [Google Scholar]
- 39.Li XW. [Epidemiological survey of Helicobacter pylori infection in Jinjiang area] Shijie Linchuang Yixue. 2016;10:234–235. [Google Scholar]
- 40.Liu XM, Ye ML, Wang WX, Zhou L. [Prevalence and influencing factors of Helicobacterpriori infection among heath checkup population in Xiamen area during 2012-2014] Zhonghua Jiankang Guanlixue Zazhi. 2016;10:153–158. [Google Scholar]
- 41.Chen Q, Li LH. [Analysis of the Results of Helicobacter Pylori test in 2 608 Healthy People] Zhongguo Weisheng Biaozhun Guanli. 2022;13:45–49. [Google Scholar]
- 42.Mao W. [Correlation between Helicobacter pylori infection and dyslipidemia in physical examination population] Zhongguo Xiandai Yiyao Zazhi. 2017;19:59–60. [Google Scholar]
- 43.Zhang Y, Cheng YP, Yang S, Yu SR, Wu Y, Lu JW, Zhao BC, Liu F, Kong XL, Xu SY, Sui J, Liu T, Liang GY, Shen B. [The prevalence of Helicobacter pylori and related factors among middle-aged and elderly residents in Gulou district of Nanjing] Zhongguo Yufang Yixue Zazhi. 2019;20:1–5. [Google Scholar]
- 44.Xie WC. [Statistics and analysis of the results of Helicobacter pylori infection in 2, 664 cases of health check-ups in Suzhou region] Zhongguo Baojian Yu Yingyang. 2017;27:395–396. [Google Scholar]
- 45.Jiang YH, Zhang Q, Zhou B, Wang Y, Zhu HX, Huang B. [Epidemiological investigation on Helicobacter pylori infection and serum pepsinogen in population undergoing health check-up] Jiangsu Yiyao. 2015;41:2401–2404. [Google Scholar]
- 46.Li GP. [Analysis of the results of Helicobacter pylori infection in health check-up workers] Zhongguo Xiandai Yiyao Zazhi. 2019;21:71–73. [Google Scholar]
- 47.Wang G, Zhang ZY, Mei YP, Wang YB. [An Analysis of 13 C Breath Test and Immunophenotyping Results of Helicobacter Pylori in Health Examination Population in Nanjing Area] Biaoji Mianyi Fenxi Yu Linchuang. 2023;30:57–60, 169. [Google Scholar]
- 48.Meng YP, He RM. [Analysis of the status of Helicobacter pylori infection in health check-up population] Zhonguo Xiandai Yisheng. 2015;53:70–72. [Google Scholar]
- 49.Ji LJ, Qian WY, Geng CS. [Distribution of Helicobacter Pylori Antibody Typing in Physical Examina-tion Population in Suzhou Area] Xitong Yixue. 2023;8:78–81, 85. [Google Scholar]
- 50.Zhang L, Wan ZJ, Niu GH. [Analysis of Helicobacter pylori infection in 1200 healthy people] Weiliang Yuansu Yu Jiankang Yanjiu. 2018;35:92–93. [Google Scholar]
- 51.Ren M, Huang YJ, Li FZ, Wang XM. [Epidemiological Analysis on Helicobacter Pylori Infection of 10 487 Healthy Persons in Pingxiang Area and and Its Medication Strategy] Kangganran Yaoxue. 2020;17:1189–1193. [Google Scholar]
- 52.Wang D, Luo HZ, Wang N, Sun JH. [The test results and analysis of Helicobacter pylori infection in the physical examination population in Jian-gxi Jiujiang area] Dongnan Guofang Yiyao. 2017;19:592–594. [Google Scholar]
- 53.Fang NF, Yang WS, He QX. [Analysis of 48353 cases of Helicobacter pylori infection] Zhongguo Dangdai Yiyao. 2021;28:202–205. [Google Scholar]
- 54.Xu SF, Yue SL, Xu YS. [Analysis of helicobacter pylori infection in cao county healthy people] Dangdai Yiyao Luncong. 2019;17:35–37. [Google Scholar]
- 55.Shi XL. [Analysis of Helicobacter Pylori Positive Rate and Health Education Among Healthy People] Jiankang Zhonggao. 2022;16:1–3. [Google Scholar]
- 56.Li J, Zhang DJ, Yu T. [Detection Analysis on Helicobacter Pylori Infection in a Hospital in Jining City] Jishengchongbing Yu Ganranxing Jibing. 2015;13:40–43. [Google Scholar]
- 57.Liang FR, Jia YX, Dong HX. [Analysis of Helicobacter pylori infections detected by 14C urea breath test] Zhonghua Yiyuan Ganranxue Zazhi. 2014;24:2515–2516, 2522. [Google Scholar]
- 58.Han YG, Cui YP, Li J, Tian WT, Qu HL. [Investigation of Helicobacter pylori infection situation and immunophenotype of natural population in Jinan area] Jianyan Yixue Yu Linchuang. 2020;17:630–632. [Google Scholar]
- 59.Kong Q, Li Y, Li R, Li Z, Zheng X, Wang Z, Song K, Zhang X, Liu J, Han Z, Duan M, Ding Y, Zhang W, Lin M, Wang J, Wan M, Lin B, Wang S, Zuo X, Li Y. Low compliance to post-screening recommendations in a family-based Helicobacter pylori screening and treatment program: A prospective cohort study. Helicobacter. 2022;27:e12912. doi: 10.1111/hel.12912. [DOI] [PubMed] [Google Scholar]
- 60.Zhang LL, Li NN, Zou HM, Cai YT, Wang BJ, Zhu LM. [Current Status and Influencing Factors of Helicobacter pylori Infection in Health Examination Population and Outpatients in Baoshan District, Shanghai] Weichangbingxue. 2019;24:326–330. [Google Scholar]
- 61.Sun HX, Zou Z, Huang YP, Lu DY, Cai JR, Zhang L, Shen L. [Epidemiological survey on Helicobacter pylori infection among Shanghai suburb residents] Shanghai Yufang Yixue. 2018;30:295–298. [Google Scholar]
- 62.Jia WY, Feng JN. [Analysis of the status and influencing factors of Helicobacter pylori infection of electrical power system workers in Shanghai] Gonggong Weisheng Yu Yufang Yixue. 2020;31:130–133. [Google Scholar]
- 63.Qiu XT, Ren JP, Ren LX, Wang JJ. [Analysis of the current status of Hp infection in the health check-up population in Hangzhou area] Xiandai Yiyao Weisheng. 2022;38:638–641. [Google Scholar]
- 64.Yu JY, Yin QL, Chen Y, Nan Y, Zhou MS. [Study on Helicobacter pylori Infection in Health Examination Subjects and Outpatients in Xiuzhou District, Jiaxing, Zhejiang Province] Weichengbingxue. 2018;23:363–365. [Google Scholar]
- 65.Zhou WZ, He W, Zhang Y. [Research and analysis of quantitative detection of Helicobacter pylori antibody and immunophenotyping in physical examination population] Zhongguo Weisheng Jianyan Zazhi. 2023;33:1839–1841. [Google Scholar]
- 66.Zheng DT, Zhang H, Si YP. [Analysis of Helicobacter pylori infection in 2220 physical examination people] Zhongguo Liaoyang Yixue. 2015;24:180–181. [Google Scholar]
- 67.Yang YM, Zheng ED. [Survey of Helicobacter pylori infection in 15817 physical examinees in Wenzhou] Zhejiang Zhongxiyi Jiehe Zazhi. 2015;25:801–803. [Google Scholar]
- 68.Lin CP, Lin DS, Lin L, Chen YY, Xia L, Fang L, Li YY, SHI HJ, Yang NM. [Study on the prevalence trend of Helicobacter pylori and drug resistance status in Cangnan, Zhejiang, China] Zhonghua Xiaohua Neijing Zazhi. 2014;31:340–342. [Google Scholar]
- 69.Yang ZQ, Chen LF, Yang YP, Li HX, Bao LJ. [Epidemiological study of Helicobacter pylori infection among physical examinees in Wenling] Zhongguo Weisheng Jianyan Zazhi. 2015;25:3369–3370, 3374. [Google Scholar]
- 70.Wang M, Wang LX, Tang LM, Yan CX, Pan GQ. [Epidemiological investigation of helicobacter pylori infection among children in Wenzhou] Zhongguo Gonggong Weisheng Guanli. 2015;31:688–690. [Google Scholar]
- 71.Li XF, Xu JZ, Hua DL. [Epidemiological survey of adult Helicobacter pylori infection in Anji County from 2015 to 2016] Zhongguo Xiangcun Yiyao. 2017;24:60–62. [Google Scholar]
- 72.Shen SE, Bi QH, Zhou HQ. [Investigation and analysis of helicobacter pylori infection in healthy population in Hangzhou area] Zhongguo Weisheng Jianyan Zazhi. 2014;24:1642–1643. [Google Scholar]
- 73.He S, Jiang SY. [Investigation on Helicobacter pylori infection and its influencing factors in preschool children in Jiangshan City] Yufang Yixue. 2016;28:1274–1276. [Google Scholar]
- 74.Fang LP, Feng SC, Zhu YX, Wu JQ. [Analysis of Helicobacter pylori infection and antibody typing in Jinhua area] Zhongguo Weisheng Jianyan Zazhi. 2022;32:2870–2872. [Google Scholar]
- 75.Yu XH, Zhao HZ, Li XY, Gao J, He YG, Sun YR. [Survey of Helicobacter pylori Infection in Physical Examination Population in Lanzhou, Gansu Province] Weichengbingxue. 2016;21:687–689. [Google Scholar]
- 76.Xie N. [Epidemiological analysis of 1621 cases of Helicobacter pylori positive population in Zhenyuan county] Jiankang Bidu. 2021:271–272. [Google Scholar]
- 77.Zou FM, Wei LH, Wu L, Liu G, Wei Q, Li JC, Wang X, Chen YQ, Yang YQ. [Investigation and analysis of positive results of serum Helicobacter pylori antibodies (IgG) in a population undergoing health examination] Gansu Yiyao. 2018;37:429–430. [Google Scholar]
- 78.Qin GF, Zhang JZ, Luo YM, Wang SH. [Analysis of the current situation of Helicobacter pylori infection in Jingtai County, Gansu Province and suggestions for prevention and treatment] Weisheng Zhiye Jiaoyu. 2018;36:133–135. [Google Scholar]
- 79.Wu SW, Peng LY, Wang JJ, Zou H, Shen DQ. [Analysis of Helicobacter pylori infection in the Hui people in Lanzhou] Jilin Yixue. 2016;37:1901–1903. [Google Scholar]
- 80.Li N. [Clinical analysis of 1000 cases of Helicobacter pylori test results in Zhangye City, Gansu Province, China] Yinshi Baojian. 2016;3:25. [Google Scholar]
- 81.Ma Y, Ren WD, Mi K, Liu CH. [Relationships between Hp Positive Rate and Age and Gender in Physical Examination Populations in Baiyin District] Jiefangjun Yufang Yixue Zazhi. 2018;36:1268–1270. [Google Scholar]
- 82.Hou HZ, Zhang JP, Zhu GN, Li BD, Xi WY. [Analysis on the Infection Status and Virulence Factor of Helicobacter Pylori in Healthy People Under Physical Examination in Qingyang Area] Jishengchongbing Yu Ganranxing Jibing. 2020;18:172–175, 180. [Google Scholar]
- 83.Zhang X, Zhu YP, Zhang L, Zhou Y, Yang Z, Niu M, Tian YG, Mo LR, Yang JF, Hu JP, Bai FH. [Analysis of the current situation of Helicobacter pylori infection in Yinchuan City] Zhonghua Xiaohua Zazhi. 2020;40:47–50. [Google Scholar]
- 84.Hu JP, Lu XP, Mo LR, Zhou Y, Yang JF, Niu M, Yang Z, Zhang X, You YJ, Bai FH. [Infection status and related factors of Helicobacter pylori in Shizuishan Ningxia] Zhonghua Linchuang Yixue Shijian. 2019;10:30–36. [Google Scholar]
- 85.Li CX, Wang XH, Ma ZQ, Zhan YH, Shen LJ, Wang F, Li YH. [Prevalence of Helicobacter pylori infection and risk factors among family members in Qinghai Province, China] Zhonghua Neike Zazhi. 2024;63:41–45. doi: 10.3760/cma.j.cn112138-112138-20231028-00259. [DOI] [PubMed] [Google Scholar]
- 86.Li Y, Li SH, Ma ZQ, Zhan YH, Shen LJ, Wang F, Li CX, Li YH, Zhang MJ, Wang XH. [Prevalence and risk factors of Helicobacter pylori infection in Qinghai Province] Zhonghua Xiaohua Zazhi. 2022;42:604–609. [Google Scholar]
- 87.Wang WS, Feng YM. Zhang X, Cuo M, Jin CD, Gao B, Zhang N, Zhao CP, Kang AH. [Epidemiological survey of Helicobacter pylori infection in Tibetan population in Gangcha of Qinghai, 2017-2018] Jibing Jiance. 2019;34:604–608. [Google Scholar]
- 88.Zhang WX, Pei ZH, Pan JG, Wang R. [Epidemiology of Helicobacter pylori in certain unit population in Xi'an] Zongzhuangbeibu Yixue Xuebao. 2014;16:83–85. [Google Scholar]
- 89.Zhang YP, Xiong L, He JT, Zhang L, Wang JH, Huang L. [Analysis of Helicobacter pylori infection in physical examination population in Xi’an] Guoji Jianyan Yixue Zazhi. 2015;36:117–118. [Google Scholar]
- 90.Tang HL, Zhuang K, Yan Y, Zhang X, Han K, Yang ZW. [Characteristics analysis of Helicobacter pylori infection in 6 085 cases] Zhongguo Weisheng Jianyan Zazhi. 2017;27:3620–3621. [Google Scholar]
- 91.Xiao YF, Cao W. [Epidemiological survey of 2100 cases of Helicobacter pylori infection in young and middle-aged population and study of related factors] Guizhou Yiyao. 2021;45:1256–1257. [Google Scholar]
- 92.Di J, Chang DY, Liu S, Mao SS, Li WW, Qu W, Zheng XH. [Investigation and analysis of risk factors for Helicobacter pylori infection in 10016 examined populations in Xi'an] Zhongguo Zhongxiyi Jiehe Xiaohua Zazhi. 2022;30:200–206. [Google Scholar]
- 93.Zhu JL, Zhao JX, Li HW. [Investigation on the prevalence of Helicobacter pylori infection in Hebukser County, Xinjiang] Zhongguo Baojian Yingyang. 2017;27:299–300. [Google Scholar]
- 94.Yao C, Wang Y. [Survey of Helicobacter pylori infection in 2301 healthy people at a bank of Urumqi] Xinjiang Yixue. 2017;47:1279–1280, 1287. [Google Scholar]
- 95.Li N, Liu PL, Zhao ZF. [Analysis of Helicobacter pylori Infection and Antibody Typing Status in Tacheng, Xinjiang] Zhongguo Shiyan Zhenduanxue. 2023;27:460–461. [Google Scholar]
- 96.Wang HK, Yao P. [Regression analysis of risk factors for Hp infection in Uyghur, Kazak and Han nationality people] Zhongguo Shiyong Yiyao Zazhi. 2016;11:17–18. [Google Scholar]
- 97.Fan ZY, Hu YQ, Zhou XM, Liu L, Wang DC, Chi SH, Ji ZJ. [Investigation and analysis of Helicobacter pylori infection in the Kazakh population of Ninth Division] Bingtuan Yixue. 2016;48:36–37. [Google Scholar]
- 98.Shu M. [Positive detection rate and clinical value of carbon 14 urea breath test for detecting Hp infection in gastrointestinal diseases] Yinshi Baojian. 2021:267. [Google Scholar]
- 99.Yang L, Kang LSJ, Jiang H, Luo YM, Ma XH, Kang CH, Wang K, Huang YL, Yu YY. [Epidemiological investigation and related factors analysis of Helicobacter pylori infection in Xizang population at Aba Prefecture] Shiyong Yiyuan Linchuang Zazhi. 2019;16:18–20. [Google Scholar]
- 100.Zhou Y, Li CP, Zhao P, Xie JL, Li YM. [Analysis of Current Situation and Influencing Factors of Helicobacter Pylori Infection in Sichuan Guangyuan] Shijie Zuixin Yixue Xinxi Wenzhai (Electronic Version) 2022;22:57–60. [Google Scholar]
- 101.Xu WJ, Li CP, Shi L. [Research on Helicobacter pylori infection and risk factors in physical examination population in Luzhou] Shiyong Yixue Zazhi. 2019;35:649–653. [Google Scholar]
- 102.Xiao X, Jiang QW, Chen Li, Wang XH. [Investigation and analysis of helicobacter pylori infection and drug resistance in preschool children in Yibin city] Dangdai Yiyao Luncong. 2020;18:5–7. [Google Scholar]
- 103.Luo P, Pu K, Yang GD. [Analysis of Helicobacter pylori infection and related factors in 1 478 patients undergoing physical examination in Nanchong area] Xiandai Xiaohua Ji Jieru Zhenliao. 2022;27:951–955. [Google Scholar]
- 104.Wu MH, Ci RYJ. [Correlation between Upper Gastrointestinal Diseases and Helicobacter Pylori Infection in Tibet] Xinan Junyi. 2017;19:504–506. [Google Scholar]
- 105.Cai L, Yi BRH, Zhang M, Ni M, Hu JH, Peng Z, Ba SZM. [Epidemiological investigation of Helicobacter pylori infection in Lhasa region] Zhonghua Xiaohua Zazhi. 2018;38:2–6. [Google Scholar]
- 106.Dawa ZM, Li SL, Tu DGL, Yang L, Si LCM. [Epidemiological survey of Helicobacter pylori in a population undergoing physical examination in Tibet] Gaoyuan Kexue Yanjiu. 2021;5:46–54. [Google Scholar]
- 107.Zhang WY, Du QY, Liao Y, Liang YM, Cen Z. [Risk factors of Helicobacter pylori infection in preschool children in Youj iang District of Baise] Youjiang Minzu Yike Daxue Xuebao. 2021;43:252–255, 264. [Google Scholar]
- 108.Xie PX. [Evaluation of Test Significance of Helicobacter Pylori in Physical Examination and Clinical Analysis] Zhongwai Yiliao. 2017;36:76–78. [Google Scholar]
- 109.Wang Q, Zhu NJ, Chen TT, Jiang DM. [Analysis of the current status of Helicobacter pylori infection in adults undergoing physical examination in the Yunnan Plateau region] Kunming Yike Daxue Xuebao. 2015;36:142–144. [Google Scholar]
- 110.Li YL, Li ZF, Wang LJ, He JY. [Epidemiological investigation and analysis of Helicobacter pylori infection in the population with health check-up in Chenggong District] Linchuang Heli Yongyao. 2018;11:124–125. [Google Scholar]
- 111.Jia DM, Wang Q, Zhu NJ, Chen TT, Feng Q, Gu YF. [Epidemiological survey of Helicobacter pylori infection and analysis of related factors among adult population receiving physical examination in Yunnan plateau area] Chongqing Yixue. 2018;47:950–956. [Google Scholar]
- 112.Fu TT, Wang MF, Chen T, Wang MY, Duan JT, Fang JH. [Survey on the rate of Helicobacter pylori infection in 12 932 cases of children in Kunming area] Zhongguo Yishi Jinxiu Zazhi. 2018;41:1070–1073. [Google Scholar]
- 113.Ding CG, Dai Y, Wang C, Yang PB, Liu XM, Shi YF. [Epidemiological Investigation of Helicobacter Pylori Infection in Children in Dali Area] Zhongwai Yiliao. 2017;36:60–62. [Google Scholar]
- 114.Chen HL, Sun YL. [Analysis of Helicobacter pylori infection in adults in Pu'er region] Shijie Zuixin Yixue Xinxi Wenzhai (Electronic Version) 2019;19:250, 261. [Google Scholar]
- 115.Liu J, Wang YH, Luo R, Zhao QH, Zhang MJ, Xie WB. [Prevalence and risk factors for Helicobacter pylori infection in Chongqing: a study of health examination participants based on 13C-urea breath test] Chongqing Yike Daxue Xuebao. 2017;42:1358–1362. doi: 10.3906/sag-1605-149. [DOI] [PubMed] [Google Scholar]
- 116.Liu Y, Lei Q. [Analysis of social characteristics and drug resistance of children with Helicobacter pylori infection in Chongqing] Xiandai Xiaohua Ji Jieru Zhenliao. 2020;25:1501–1504. [Google Scholar]
- 117.Zhou G. [Epidemiological Investigation and Drug Resistance of Helicobacter Pylori Chongqing Region] Zhongguo Yaoye. 2018;27:8–10. [Google Scholar]
- 118.Meng FN, Sun L. [Analysis of Helicobacter Pylori Infection in Healthy Population in Chongqing Area] Xiandai Jianyan Yixue Zazhi. 2018;33:121–122, 125. [Google Scholar]
- 119.Liu C, Fan JH. [Epidemiological survey of Helicobacter pylori infection among electric power company workers in Chongqing area] Anhui Yiyao. 2016:131–132. [Google Scholar]
- 120.Zhu P, Jiang W, Zeng QA, Li FY, Qiu JJ. [Analysis of the infection characteristics of the Helicobacter pylori for physical examination people in Pingshan district of Shenzhen] Shiyong Yiji Zazhi. 2021;28:1178–1180. [Google Scholar]
- 121.Zhang H, Yang JY, Liu XM, Liu TY, Li K. [Study of Helicobacter pylori infection and its risk factors in the residents of rural-urban continuum in Guangzhou] Xiandai Yiyuan. 2015:140–144. [Google Scholar]
- 122.Liang ZR, Yang KH. [Investigation and Analysis of Helicobacter Pylori Infection in Yangjiang Area] Guoji Ganran Zazhi (Electronic Edition) 2018;7:186–187. [Google Scholar]
- 123.Yang R. [Investigation and analysis of the positive results of serum helicobacter pylori antibody (IgG) in people undergoing health examination] Zhongguo Yiyao Kexue. 2021;11:168–170. [Google Scholar]
- 124.Xie T, Li WH, Cao SS. [Investigation and Analysis of Helicobacter Pylori Infection in Healthy Crowd] Zhongwai Yixue Yanjiu. 2014;12:75–76. [Google Scholar]
- 125.Xie B, Sun GY, Zhang JD, Hong RS, Wang JZ, Lin XH. [Infection rate and drug resistance of Helicobacterpyloriin Chaozhou area] Shantou Daxue Yixueyuan Xuebao. 2021;34:14–17, 21. [Google Scholar]
- 126.Tang D, Zhang XM. [Analysis on the Infection Status and Different Types of Helicobacter Pylori in Luohu District of Shenzhen Resident] Shijie Zuixin Yixue Xinxi Wenzhai (Electronic Version) 2021;21:163–164. [Google Scholar]
- 127.Guan RP, Dai GK, Jiang GL, Li Y, Xu Y. [Analysis of Helicobacter pylori infection and related factors among public officials in Guangzhou] Guoji Yiyao Weisheng Daobao. 2022;28:284–287. [Google Scholar]
- 128.Dai YM, Lv XH. [Analysis of Helicobacter pylori positivity rate in health check-up population and health education] Shiyong Linchuang Hulixue. 2020;5:182–183. [Google Scholar]
- 129.Li C, Yue J, Ding Z, Zhang Q, Xu Y, Wei Q, Wang J, Ning X, Zeng H, Cao J. Prevalence and predictors of Helicobacter pylori infection in asymptomatic individuals: a hospital-based cross-sectional study in Shenzhen, China. Postgrad Med. 2022;134:686–692. doi: 10.1080/00325481.2022.2085950. [DOI] [PubMed] [Google Scholar]
- 130.Xu Z, Yan B. [Analysis of correlation between the Helicobacter pylori infection and dyslipidemia of 2956 cases of healthy physical examination people] Shijie Fuhe Yixue. 2018;4:34–36, 92. [Google Scholar]
- 131.Weng FY. [Analysis of related factors and etiology of Helicobacter pylori positive rate] Yangsheng Baojian Zhinan. 2017:17–18. [Google Scholar]
- 132.Lin Y, Cheng L. [Current status of prevalence of Helicobacter pylori infection in Healthy Examination Center] Shezhi. 2016;28:304–305, 312. [Google Scholar]
- 133.Wang JB. [Analysis of the infection rate of helicobacter pylori in healthy people] Zhongguo Shequ Yishi. 2021;37:137–138. [Google Scholar]
- 134.Chen YD, Zhang HL, Zhai HZ, Kong HM. [Current situation of Helicobacter pylori infection in Hezhou] Zhongguo Baojian Yingyang. 2017;27:342–343. [Google Scholar]
- 135.Chen LH. [Analysis of Helicobacter pylori infection among physical examination population in Nanning] Yinshi Baojian. 2022:141–144. [Google Scholar]
- 136.Cao C, Zhou XH, Hu GY, Qin XS, Li GZ, Huang ZS. [Investigation of the status quos of helicobacter pylori infection in people of the area bordering Yunnan ,Guizhou and Guangxi] Shiyong Yixue Zazhi. 2017;33:1864–1867. [Google Scholar]
- 137.Zhang DY, Chen SJ, Chen RX, Zhang XD, Li D, Huang SM, Zeng F, Chen C, Chen JJ, Mo CY, Bai FH. [Survey on the current status and analysis of risk factors of Helicobacter pylori infection in Qionghai City of Hainan province] Xiandai Xiaohua Ji Jieru Zhiliao. 2023;28:818–822. [Google Scholar]
- 138.Qiu XX, Xu XY. [Analysis of Helicobacter pylori infection in 1977 physical examination population] Linchuang Yiyao Wenxian. 2017;4:8094, 8096. [Google Scholar]
- 139.Ma ZC, Ruan HQ, Huang BL, Fu SD. [Analysis on Helicobacter Pylori Detection Results of Health Examination in Haikou] Zhongguo Chuji Weisheng Baojian. 2015;29:150–151. [Google Scholar]
- 140.Zeng F, ZhangG DY, Chen SJ, Guo XY, Chen C, Huang SM, Chen RX, Zhang XD, Li D, Wang Q, Bai FH. [Investigation on the current status of Helicobacter pylori infection and analysis of related risk factors in the population of Wuzhishan City] Xiandai Xiaohua Ji Jieru Zhiliao. 2023;28:957–961. [Google Scholar]
- 141.Liu D, Pan J, Chen Z, Li S, Ma J, Xiao Y, Wang D, Mu G, Lin Y, Li J, Chen Z, Huang X. A survey on the current status of Helicobacter pylori infection in households in Hainan Province, China. BMC Gastroenterol. 2023;23:426. doi: 10.1186/s12876-023-03010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhao HZ, Chen YY, Chang J. [Analysis about the Detection Results of Helicobacter Pylori in Healthy People] XinJiang Yixue. 2022;52:814–815, 818. [Google Scholar]
- 143.Chai YZ, Wang YH, Xu HR. [Helicobacter pylori infection in hospitalized patients in gastroenterology department] Huanan Yufang Yixue. 2021;47:77–79, 83. [Google Scholar]
- 144.Wang N, Liu Y, Chen GJ. [Analysis of Helicobacter pylori infection in health examination population] Henan Yixue Yanjiu. 2018;27:2548–2549. [Google Scholar]
- 145.Liu SJ, Wang Q, Li G, Yan XQ, Du JJ. [Analysis of Helicobacter pylori infection and its immunophenotyping in 856 healthy people in Nanyang area] Jiangsu Yufang Yixue. 2021;32:719–721. [Google Scholar]
- 146.Gu CG, Li YL, Li HY, Liu GL, Wang LG. [Analysis of Helicobacter pylori infection in Luohe residents] Zhongguo Weisheng Jianyan Zazhi. 2014;24:2094–2095, 2101. [Google Scholar]
- 147.Fan MQ, Li SX, Huang ZC. [Epidemiological Survey on Helicobacter Pylori Infection in Pingdingshan Area] Zhongwai Yiliao. 2015:178–179. [Google Scholar]
- 148.Yu XC, Shao QQ, Ma J, Yu M, Zhang C, Lei L, Zhou Y, Chen WC, Zhang W, Fang XH, Zhu YZ, Wu G, Wang XM, Han SY, Sun PC, Ding SZ. Family-based Helicobacter pylori infection status and transmission pattern in central China, and its clinical implications for related disease prevention. World J Gastroenterol. 2022;28:3706–3719. doi: 10.3748/wjg.v28.i28.3706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lei L, Dang YN, Yu XC, Shao QQ, Ma J, Yu M, Zhang C, Zhao JB, Hu RB, Qi YB, Wei PR, Xiao W, Han SY, Jia BL, Wang CR, Ding SZ. [Intrafamilial infection of Helicobacter pylori in Zhengzhou area] Zhonghua Quanke Yixue Zazhi. 2023;22:697–703. [Google Scholar]
- 150.Zhang L, Zhang YH, Liu W, Yan H. [Investigation on Helicobacter pylori infection among railway workers in Wuhan] Yingyong Yufang Yixue. 2019;25:199–200, 203. [Google Scholar]
- 151.Yang LX. [Analysis of the positive rate of Helicobacter pylori in health examination population and health education] Yinshi Baojian. 2020;7:255–256. [Google Scholar]
- 152.Li X. [Statistics and analysis of Helicobacter pylori infection among residents in Xian'an District of Xianning City] Hubei Keji Xueyuan Xuebao (Medical Sciences) 2022;36:427–429. [Google Scholar]
- 153.Xi W. [Investigation of Helicobacter pylori infection in healthy people] Zhongguo Yaowu Jingjixue. 2014;9:185–186. [Google Scholar]
- 154.Liu ZJ, Yang XR, Zhang D, Wang JY. [Correlation Between Helicobacter Pylori Infection and Dyslipidemia in Populations Undergoing Healthy Examination] Huanan Guofang Yixue Zazhi. 2017;31:23–25. [Google Scholar]
- 155.Zhou XB, Lin B. [Analysis of Helicobacter pylori infection in children with upper gastrointestinal symptoms in Huangshi area] Linchuang Heli Yongyao. 2018;11:58–59. [Google Scholar]
- 156.Li Z, Yuan WJ, Chen J, Zhou X. [Serological analysis of Helicobacter pylori infection among health examination people in Xiaogan] Baotou Yixueyuan Xuebao. 2014;30:45–46. [Google Scholar]
- 157.Jia MF, Luo XH, Wang JL, Cheng XQ. [An epidemiological study of Helicobacter pylori infection and its risk factors in 2180 Wuhan residents] Huli Xuebao. 2016;23:48–52. [Google Scholar]
- 158.Deng Q, Liu LH, Zhao W. [Correlation between HP positive rate and glucose and lipid metabolism in healthy people] Hubei Keji Xueyuan Xuebao (Medical Sciences) 2020;34:425–427. [Google Scholar]
- 159.Li XL, Dai GZ, Huang CH. [Analysis of related factors of Helicobacter pylori infection in physical examination population in Chenzhou area] Guoji Jianyan Yixue Zazhi. 2015:2914–2915. [Google Scholar]
- 160.Peng YF, Zhang YN, Liao XM, Li F. [Investigation analysis of helicobacter pylori infection in physical examination population] Dangdai Yixue. 2019;25:122–125. [Google Scholar]
- 161.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH, Tetzlaff J, Deeks JJ, Peters J, Macaskill P, Schwarzer G, Duval S, Altman DG, Moher D, Higgins JP. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 162.Smith SM. Role of Toll-like receptors in Helicobacter pylori infection and immunity. World J Gastrointest Pathophysiol. 2014;5:133–146. doi: 10.4291/wjgp.v5.i3.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wang F, Meng W, Wang B, Qiao L. Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett. 2014;345:196–202. doi: 10.1016/j.canlet.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 164.Katelaris P, Hunt R, Bazzoli F, Cohen H, Fock KM, Gemilyan M, Malfertheiner P, Mégraud F, Piscoya A, Quach D, Vakil N, Vaz Coelho LG, LeMair A, Melberg J. Helicobacter pylori World Gastroenterology Organization Global Guideline. J Clin Gastroenterol. 2023;57:111–126. doi: 10.1097/MCG.0000000000001719. [DOI] [PubMed] [Google Scholar]
- 165.Lin MM, Yang SS, Huang QY, Cui GH, Jia XF, Yang Y, Shi ZM, Ye H, Zhang XZ. Effect and mechanism of Qingre Huashi decoction on drug-resistant Helicobacter pylori. World J Gastroenterol. 2024;30:3086–3105. doi: 10.3748/wjg.v30.i24.3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Jia X, Huang Q, Lin M, Chu Y, Shi Z, Zhang X, Ye H. Revealing the novel effect of Jinghua Weikang capsule against the antibiotic resistance of Helicobacter pylori. Front Microbiol. 2022;13:962354. doi: 10.3389/fmicb.2022.962354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Zhang Y, Lu B, Dong Y, Zhang Y, Du Q, Chen Y, Zhang Z. Saccharomyces boulardii combined with triple therapy alter the microbiota in the eradication of Helicobacter pylori infection. Sci Rep. 2024;14:13152. doi: 10.1038/s41598-024-63894-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ismail NI, Nawawi KNM, Hsin DCC, Hao KW, Mahmood NRKN, Chearn GLC, Wong Z, Tamil AM, Joseph H, Raja Ali RA. Probiotic containing Lactobacillus reuteri DSM 17648 as an adjunct treatment for Helicobacter pylori infection: A randomized, double-blind, placebo-controlled trial. Helicobacter. 2023;28:e13017. doi: 10.1111/hel.13017. [DOI] [PubMed] [Google Scholar]
- 169.Li M, Sun Y, Yang J, de Martel C, Charvat H, Clifford GM, Vaccarella S, Wang L. Time trends and other sources of variation in Helicobacter pylori infection in mainland China: A systematic review and meta-analysis. Helicobacter. 2020;25:e12729. doi: 10.1111/hel.12729. [DOI] [PubMed] [Google Scholar]
- 170.Li Y, Choi H, Leung K, Jiang F, Graham DY, Leung WK. Global prevalence of Helicobacter pylori infection between 1980 and 2022: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2023;8:553–564. doi: 10.1016/S2468-1253(23)00070-5. [DOI] [PubMed] [Google Scholar]
- 171.Zhou XZ, Lyu NH, Zhu HY, Cai QC, Kong XY, Xie P, Zhou LY, Ding SZ, Li ZS, Du YQ National Clinical Research Center for Digestive Diseases (Shanghai), Gastrointestinal Early Cancer Prevention and Treatment Alliance of China (GECA), Helicobacter pylori Study Group of Chinese Society of Gastroenterology and Chinese Alliance for Helicobacter pylori Study. Large-scale, national, family-based epidemiological study on Helicobacter pylori infection in China: the time to change practice for related disease prevention. Gut. 2023;72:855–869. doi: 10.1136/gutjnl-2022-328965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Vesga FJ, Venegas C, Flórez Martinez V, Sánchez-Alfonso AC, Trespalacios AA. Origin of fecal contamination in lettuce and strawberries: From microbial indicators, molecular markers, and H. pylori. Heliyon. 2024;10:e36526. doi: 10.1016/j.heliyon.2024.e36526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Farhadkhani M, Nikaeen M, Hassanzadeh A, Nikmanesh B. Potential transmission sources of Helicobacter pylori infection: detection of H. pylori in various environmental samples. J Environ Health Sci Eng. 2019;17:129–134. doi: 10.1007/s40201-018-00333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wu Y, Su T, Zhou X, Lu N, Li Z, Du Y. Awareness and attitudes regarding Helicobacter pylori infection in Chinese physicians and public population: A national cross-sectional survey. Helicobacter. 2020;25:e12705. doi: 10.1111/hel.12705. [DOI] [PubMed] [Google Scholar]
- 175.Wang YX, Zou JY, Hu LF, Liu Q, Huang RL, Tang T, Yue QQ, Sun YX, Xiao Q, Zeng X, Zeng Y. What is the general Chinese public's awareness of and attitudes towards Helicobacter pylori screening and associated health behaviours? A cross-sectional study. BMJ Open. 2022;12:e057929. doi: 10.1136/bmjopen-2021-057929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Xia P, Ma MF, Wang W. Status of Helicobacter pylori infection among migrant workers in Shijiazhuang, China. Asian Pac J Cancer Prev. 2012;13:1167–1170. doi: 10.7314/apjcp.2012.13.4.1167. [DOI] [PubMed] [Google Scholar]
- 177.Wang YX, Zou JY, Hu LF, Gong YW, Wu MZ, Fang QH, Huang RL, Zuo LJ, Zeng Y. [Investigation about Actual Situation the Awareness of Helicobacter Pylori in General Population] Zhongguo Chuji Weisheng Baojian. 2022;36:60–65. [Google Scholar]
- 178.Yamaoka Y, Saruuljavkhlan B, Alfaray RI, Linz B. Pathogenomics of Helicobacter pylori. Curr Top Microbiol Immunol. 2023;444:117–155. doi: 10.1007/978-3-031-47331-9_5. [DOI] [PubMed] [Google Scholar]
- 179.You YH, He LH, Peng XH, Sun L, Zhang JZ. [Genomic diversity and population structure of Helicobacter pylori isolates in China] Zhonghua Liuxingbingxue Zazhi. 2016;37:1397–1403. doi: 10.3760/cma.j.issn.0254-6450.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 180.Qin ED, Wang J, Qin R, Liu H, Xiong HR, Liu J, Wang HY, Zhang L. [Dietary Structure Analysis and Dietary Nutrition Recommendations in Different Regions of China] Zhongguo Shiwu Yu Yingyang. 2020;26:82–86, 59. [Google Scholar]
- 181.Su BQ, Wang YY, ShangGuang ZP. [Assessment of Food Structure and lts Security Situation in Northwest China] Shuitu Baochi Yanjiu. 2017;24:354–359. [Google Scholar]
- 182.Wang XF, Wang YS, Zhan TT, Du Y. [Analysis on resources allocation of township health center in Western China] Weisheng Ruankexue. 2020;34:48–55. [Google Scholar]
- 183.Camilo V, Sugiyama T, Touati E. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2017;22:Suppl 1. doi: 10.1111/hel.12405. [DOI] [PubMed] [Google Scholar]
- 184.Wang L, Li Z, Tay CY, Marshall BJ, Gu B Guangdong Center for Quality Control of Clinical Gene Testing and Study Group of Chinese Helicobacter pylori Infection and Antibiotic Resistance Rates Mapping Project (CHINAR-MAP) Multicentre, cross-sectional surveillance of Helicobacter pylori prevalence and antibiotic resistance to clarithromycin and levofloxacin in urban China using the string test coupled with quantitative PCR. Lancet Microbe. 2024;5:e512–e513. doi: 10.1016/S2666-5247(24)00027-2. [DOI] [PubMed] [Google Scholar]
- 185.Zhang T, Luo ZQ, Hu QZ, Cai XL. [Research progress of gastric cancer in people living at high altitudes] Zhongguo Zhongliu Linchuang. 2022;49:95–98. [Google Scholar]
- 186.Cheng J, Sun Y, Zhao Y, Guo Q, Wang Z, Wang R. Research Progress on the Mechanism of Intestinal Barrier Damage and Drug Therapy in a High Altitude Environment. Curr Drug Deliv. 2024;21:807–816. doi: 10.2174/1567201820666230309090241. [DOI] [PubMed] [Google Scholar]
- 187.Zhai HZ, Lin QM, Li LX, Deng M, Cheng YD, Liu Y, Tang C, Zhang HL. [Helicobacter pylori infection factors clinical research in Hezhou City] Manxingbingxue Zazhi. 2024;25:507–510. [Google Scholar]
- 188.Cui Y, Jin Y, Liu XL, Gong M, Wu WJ. [Hp infection rate, antibody typing and logistic regression analysis of 1111 physical examination people in plateau area] Gonggong Weisheng Yu Yufang Yixue. 2024;35:53–56. [Google Scholar]
- 189.Lin K, Du YQ, Zhu CP, Li ZS. [The Enlightenment of coping strategies against Helicobacter pylori in countries with high incidence of gastric cancer to China] Shanghai Yixue. 2019;42:695–698. [Google Scholar]
- 190.Li XT, Xu L, Zhang C, Qi YB, Hu RB, Abdun MA, Yu XC, Li K, Liu TT, Ma J, Xiao W, Lan L, Wang XM, Cao MB, Li J, Han SY, Li XL, Ding SZ. Improved Patient Adherence to Family-Based Helicobacter pylori Infection Control and Management Strategy in Central China and Its Influencing Factors. Helicobacter. 2024;29:e13114. doi: 10.1111/hel.13114. [DOI] [PubMed] [Google Scholar]
- 191.Ebrahimi Z, Shateri Z, Nouri M, Sikaroudi MK, Masoodi M, Shidfar F, Hejazi M. Ultra-Processed food intake and risk of Helicobacter pylori infection: A case-control study. Food Sci Nutr. 2024;12:5019–5026. doi: 10.1002/fsn3.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Orr WC, Chen CL. Aging and neural control of the GI tract: IV. Clinical and physiological aspects of gastrointestinal motility and aging. Am J Physiol Gastrointest Liver Physiol. 2002;283:G1226–G1231. doi: 10.1152/ajpgi.00276.2002. [DOI] [PubMed] [Google Scholar]
- 193.Tarnawski AS, Ahluwalia A, Jones MK. Increased susceptibility of aging gastric mucosa to injury: the mechanisms and clinical implications. World J Gastroenterol. 2014;20:4467–4482. doi: 10.3748/wjg.v20.i16.4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Tarnawski AS, Ahluwalia A. Increased susceptibility of aging gastric mucosa to injury and delayed healing: Clinical implications. World J Gastroenterol. 2018;24:4721–4727. doi: 10.3748/wjg.v24.i42.4721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Liatsos C, Papaefthymiou A, Kyriakos N, Galanopoulos M, Doulberis M, Giakoumis M, Petridou E, Mavrogiannis C, Rokkas T, Kountouras J. Helicobacter pylori, gastric microbiota and gastric cancer relationship: Unrolling the tangle. World J Gastrointest Oncol. 2022;14:959–972. doi: 10.4251/wjgo.v14.i5.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Shin CM, Kim N, Park JH, Lee DH. Changes in Gastric Corpus Microbiota With Age and After Helicobacter pylori Eradication: A Long-Term Follow-Up Study. Front Microbiol. 2020;11:621879. doi: 10.3389/fmicb.2020.621879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.World Health Organization. Ageing and Health. 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health .
- 198.Beydoun MA, Beydoun HA, Elbejjani M, Dore GA, Zonderman AB. Helicobacter pylori seropositivity and its association with incident all-cause and Alzheimer's disease dementia in large national surveys. Alzheimers Dement. 2018;14:1148–1158. doi: 10.1016/j.jalz.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Rezvani F, Sayadnasiri M, Rezaei O. The study of memory and executive dysfunction in patients infected with Helicobacter pylori. Neurol Res. 2017;39:953–958. doi: 10.1080/01616412.2017.1363349. [DOI] [PubMed] [Google Scholar]
- 200.Huang HK, Wang JH, Lei WY, Chen CL, Chang CY, Liou LS. Helicobacter pylori infection is associated with an increased risk of Parkinson's disease: A population-based retrospective cohort study. Parkinsonism Relat Disord. 2018;47:26–31. doi: 10.1016/j.parkreldis.2017.11.331. [DOI] [PubMed] [Google Scholar]
- 201.Mladenova I. Helicobacter pylori and cardiovascular disease: update 2019. Minerva Cardioangiol. 2019;67:425–432. doi: 10.23736/S0026-4725.19.04986-7. [DOI] [PubMed] [Google Scholar]
- 202.Cizginer S, Ordulu Z, Kadayifci A. Approach to Helicobacter pylori infection in geriatric population. World J Gastrointest Pharmacol Ther. 2014;5:139–147. doi: 10.4292/wjgpt.v5.i3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Jonaitis P, Kupcinskas J, Gisbert JP, Jonaitis L. Helicobacter pylori Eradication Treatment in Older Patients. Drugs Aging. 2024;41:141–151. doi: 10.1007/s40266-023-01090-w. [DOI] [PubMed] [Google Scholar]
- 204.Borka Balas R, Meliț LE, Mărginean CO. Worldwide Prevalence and Risk Factors of Helicobacter pylori Infection in Children. Children (Basel) 2022;9:1359. doi: 10.3390/children9091359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Ding Z, Zhao S, Gong S, Li Z, Mao M, Xu X, Zhou L. Prevalence and risk factors of Helicobacter pylori infection in asymptomatic Chinese children: a prospective, cross-sectional, population-based study. Aliment Pharmacol Ther. 2015;42:1019–1026. doi: 10.1111/apt.13364. [DOI] [PubMed] [Google Scholar]
- 206.Yuan C, Adeloye D, Luk TT, Huang L, He Y, Xu Y, Ye X, Yi Q, Song P, Rudan I Global Health Epidemiology Research Group. The global prevalence of and factors associated with Helicobacter pylori infection in children: a systematic review and meta-analysis. Lancet Child Adolesc Health. 2022;6:185–194. doi: 10.1016/S2352-4642(21)00400-4. [DOI] [PubMed] [Google Scholar]
- 207.Etukudo OM, Ikpeme EE, Ekanem EE. Seroepidemiology of Helicobacter pylori infection among children seen in a tertiary hospital in Uyo, southern Nigeria. Pan Afr Med J. 2012;12:39. [PMC free article] [PubMed] [Google Scholar]
- 208.Kato S, Shimizu T, Toyoda S, Gold BD, Ida S, Ishige T, Fujimura S, Kamiya S, Konno M, Kuwabara K, Ushijima K, Yoshimura N, Nakayama Y Japanese Society for Pediatric Gastroenterology, Hepatology and Nutrition. The updated JSPGHAN guidelines for the management of Helicobacter pylori infection in childhood. Pediatr Int. 2020;62:1315–1331. doi: 10.1111/ped.14388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Chinese Society of Health Management, Editorial Board of Chinese Journal of Health Management Chinese Society of Gastroenterology Helicobacter Pylori Group. [Consensus on technical specification of 13C urea breath test in health examination population] Zhonghua Jiankang Guanlixue Zazhi. 2021;15:14–19. [Google Scholar]
- 210.Helicobacter pylori Study Group; Chinese Society of Gastroenterology Chinese Medical Association. [Sixth Chinese national consensus report on the management of Helicobacter pylori infection (treatment excluded)] Zhonghua Xiaohua Zazhi. 2022;42:289–303. [Google Scholar]
- 211.Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, Miura S, Haruma K, Asaka M, Uemura N, Malfertheiner P faculty members of Kyoto Global Consensus Conference. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64:1353–1367. doi: 10.1136/gutjnl-2015-309252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou JM, Schulz C, Gasbarrini A, Hunt RH, Leja M, O'Morain C, Rugge M, Suerbaum S, Tilg H, Sugano K, El-Omar EM European Helicobacter and Microbiota Study group. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022 [Google Scholar]
- 213.Chinese Society of Gastroenterology Chinese Study Group on Helicobacter Pylori and Peptic Ulcer. Liu WZ, Xie Y, Lu H, Cheng H, Zeng ZR, Zhou LY, Chen Y, Wang JB, Du YQ, LV NH. [Fifth Chinese national consensus report on the management of Helicobacter pylori infection] Zhonghua Neike Zazhi. 2017;37:364–378. doi: 10.1111/hel.12475. [DOI] [PubMed] [Google Scholar]
- 214.World Organization of Gastroenterology. Zhong ZS, Xu BH. [World Gastroenterology Organisation Global Guidelines: Helicobacter pylori] Weichangbingxue. 2021;26:540–553. [Google Scholar]
- 215.Chinese Society of Health Management, National Clinical Research Center for Digestive Diseases (Shanghai) Helicobacter pylori Group of Chinese Society of Gastroenterology. [Consensus on serological test of Helicobacter pylori in health examination population(2022)] Jiankang Tijian Yu Guanli. 2022;3:329–335, 349. [Google Scholar]
- 216.Elbehiry A, Marzouk E, Aldubaib M, Abalkhail A, Anagreyyah S, Anajirih N, Almuzaini AM, Rawway M, Alfadhel A, Draz A, Abu-Okail A. Helicobacter pylori Infection: Current Status and Future Prospects on Diagnostic, Therapeutic and Control Challenges. Antibiotics (Basel) 2023;12 doi: 10.3390/antibiotics12020191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Brasil-Costa I, Souza CO, Monteiro LCR, Santos MES, Oliveira EHC, Burbano RMR. H. pylori Infection and Virulence Factors cagA and vacA (s and m Regions) in Gastric Adenocarcinoma from Pará State, Brazil. Pathogens. 2022;11:414. doi: 10.3390/pathogens11040414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Parihar V, McNamara D. Endoscopic Detection of Helicobacter pylori by the Rapid Urease Test. Methods Mol Biol. 2021;2283:37–43. doi: 10.1007/978-1-0716-1302-3_5. [DOI] [PubMed] [Google Scholar]