Abstract
Background
After an increase of central line–associated bloodstream infections (CLABSIs) at our community hospital in 2021, a case-control study suggested that patients with CLABSIs were 3.0 times more likely to have missed daily chlorhexidine gluconate (CHG) bathing than patients without CLABSIs.
Objective
To increase the rate of daily CHG bathing in hospitalized patients with central lines and subsequently reduce the number of CLABSIs.
Methods
Our pre-post intervention was launched on September 2022 and consisted of enhancements to the electronic health record (EHR) to simplify the identification of overdue CHG bathing instances to increase compliance, and therefore decrease the CLABSI rate at our hospital. A workflow was implemented Monday–Friday utilizing these EHR enhancements for active surveillance to engage frontline nursing staff and address gaps in care in real time.
Results
After the initiative was implemented, adherence to daily CHG bathing increased from 94.9% to 95.3%, with a considerable disparity between weekdays (97.6%) and weekends (89.3%). After weekend data were excluded, the post-intervention increase in the adherence rate was statistically significant (p = .003).
Discussion
This initiative underscored the importance of involving health care informatics partners and showed how technology can bridge gaps in health care quality. Outreach and reminders effectively improved CHG bathing adherence by emphasizing the importance of consistent communication and follow-up.
Keywords: Bloodstream infection, central venous catheters, infection control, infection prevention, quality improvement
Introduction
Central line–associated bloodstream infections (CLABSIs) are a common type of hospital-acquired infections (HAIs). A meta-analysis performed by the Agency for Healthcare Research and Quality, (2018) estimated an additional 150 excess deaths for every 1000 in-hospital CLABSI cases, as well as an estimated additional cost of $48,108 for every case. Garcia (2023) also reported CLABSIs are associated with increased mortality, as well as increased in length of stay, and at a substantial cost to healthcare facilities as costs associated with CLABSIs are not reimbursed. CLABSIs are largely preventable with appropriate management and insertion of the central line according to the Guidelines for the Prevention of Intravascular Catheter Related Infections (O’Grady et al., 2011) and more recently the Society for Healthcare Epidemiology of America/Infectious Diseases Society of America Strategies to Prevent Central Line–Associated Bloodstream Infections in Acute Care Hospitals (Buetti et al., 2022). One of these strategies is daily skin cleansing with a 2% chlorhexidine gluconate (CHG) topical solution.
Numerous studies, including those done by Chapman et al. (2021), Destine et al. (2023), Knobloch et al. (2021), Livingston (2021), and Reagan et al. (2019), have shown that daily CHG bathing is an effective method to reduce CLABSIs, prevent the emergence of antimicrobial-resistant organisms, and decrease HAIs. CHG bathing has also been shown to reduce CLABSIs when implemented as part of a multifaceted approach (Clarkson, 2020; Ghonim and Ennin-Evelyn, 2020). Studies have shown that using the Define, Measure, Analyze, Improve, and Control process from Six Sigma is an effective strategy to reduce both CLABSIs and HAIs overall (Kuwaiti and Subbarayalu, 2017; Loftus et al., 2015).
The studies referenced above collectively underscore the importance of evidence-based practices, multidisciplinary collaboration, and focused methodologies for the successful prevention and reduction of HAIs, particularly CLABSIs.
In 2021, an increase in the CLABSI standard infection ratio at our hospital led the Infection Prevention and Control (IPAC) department to conduct an internal case-control study to identify potential risk factors for CLABSIs. After we controlled for age, sex, central line type, and central line duration, our findings showed that patients with CLABSIs were 3.0 times more likely to have missed daily CHG bathing than were patients without CLABSIs (unpublished data). Because review of daily CHG bathing was performed retrospective to the previous day at our hospital, IPAC was not able to intervene for these cases in real time.
The project team, consisting of IPAC and nursing informatics, as well as nursing and physician leadership, aimed to increase the rate of daily CHG bathing adherence for patients to subsequently decrease the number of CLABSIs at our hospital through a quality improvement project (QIP). For this project, consultation and collaboration with a nurse informaticist led to enhancements of our electronic health record (EHR) that improved identification of patients requiring care. An active outreach workflow was also initiated to intervene in real time for patients with missing CHG bathing documentation. The primary objective of our QIP was an increase in the daily CHG bathing rate for patients with central lines by 3.3%, from a pre-intervention rate of 94.9% to a post-intervention rate of 97.0%.
Methods
Our QIP was conducted at a licensed, 166-bed acute care community hospital, which serves as a hub hospital in a large health system comprising five regional hospitals in the US Midwest. The initial project spanned from September 2022 to December 2022, but interventions were maintained following the success of the project. We focused on patients hospitalized in the intensive care unit, progressive care unit, and medical/surgical units that had a central line in situ. The primary outcome measure for the project was the CHG bathing adherence rate. The procedure on CHG daily treatment requires staff to apply CHG from jaw to toes daily on all non-contraindicated adult patients with central lines using either a 4% CHG solution or 2% CHG impregnated cloth. Staff must demonstrate competency and understanding of the workflow, which includes the documentation process. Chlorhexidine gluconate bathing was determined as adherent if EHR documentation of CHG bathing had been completed during the previous calendar day. This measure served as a leading indicator for the overall goal of CLABSI reduction. Analysis of CHG bathing compliance was completed by an IPAC member within the EHR during weekdays and was focused on the previous calendar day.
Quality improvement tools including a Fishbone Diagram and an Impact Effort Matrix were used to identify barriers. One key barrier identified was the difficulty in easily identifying CHG bathing documentation, as well as patients that are due for bathing. Based on this the project team hypothesized that the development of a Time Since CHG Bathing column and a subsequent overall report created in the EHR would make the identification of missing CHG bathing opportunities more apparent. Informatics created the column, and our IPAC team used the new column to identify admitted patients with central lines who were overdue for CHG bathing. The IPAC team then contacted frontline nursing staff to provide real-time feedback that CHG bathing was overdue for a specific patient. By using a consistent message and messaging platform within the EHR, we standardized both the content of the message and the method of delivery. If nursing staff had questions about how to approach patients who declined CHG bathing just-in-time education was provided to help improve knowledge. The education was based on an established refusal procedure that included escalation to the attending provider, and up to physician leadership if needed.
To ensure that the implemented interventions and achieved improvements lasted longer than the time frame of the project, we enacted a sustainability plan. The plan included using the tools and dashboards we created to develop individualized plans focusing on ownership and empowerment of the frontline staff to ensure CHG bathing. The plan was created by a multidisciplinary group using shared decision making to develop personalized action plans for frontline units. Data on CHG bathing adherence was sent to the units on a weekly basis, and nursing leadership provided oversight and accountability utilizing the data.
Our internal Institutional Review Board (IRB) acknowledged that based on the responses submitted for this activity through the internal electronic IRBe Human Subjects Research Wizard tool, and in accordance with the Code of Federal Regulations, 45 CFR 46.102, the above noted activity does not require IRB review.
Statistical analysis
A 2-proportion t test was performed to compare pre-intervention and post-intervention data. During the pre-intervention period, the overall CHG bathing adherence rate included both weekday and weekend cases, and these data were not segmented to analyze weekday and weekend adherence rates separately. Therefore, the data were summarized according to CHG bathing adherence rate during weekdays, weekends, and both weekdays and weekends combined (i.e., overall) during the post-intervention period and according to the overall rate during the pre-intervention period. The National Healthcare Safety Network Statistics Calculator developed by the Center for Disease and Prevention (2021) was used to analyze the data that were abstracted from our EHR. p values <.05 were considered statistically significant.
Results
As the project was initiated, baseline data from August 1, 2021, through July 31, 2022, were reviewed. Of 3840 cases reviewed, 195 patients had missed CHG bathing the previous calendar day. Therefore, the pre-intervention CHG bathing adherence rate was 94.9%. The rate of central line use was 10.3%, and eight CLABSIs occurred during the 12-month pre-intervention period, which resulted in a CLABSI rate of 1.89.
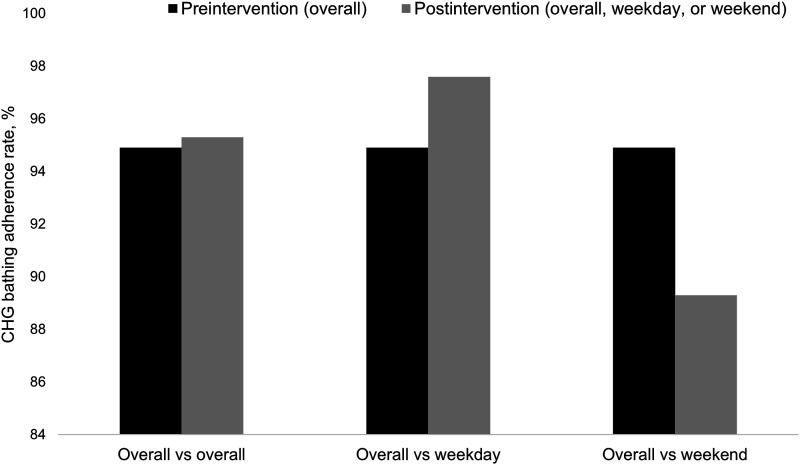
After the interventions were implemented on September 7, 2022, the overall adherence rate increased to 95.3% by November 30, 2022. Although overall CHG bathing adherence increased by 0.42% from the pre-intervention period, this increase was not statistically significant (p = .71). Because the pre-intervention CHG bathing adherence rate included both weekday and weekend data and the interventions were implemented only on weekdays, the overall pre-intervention data were compared with overall, weekday, and weekend post-intervention data. The CHG bathing adherence rate increased from an overall pre-intervention rate of 94.9% to a weekday post-intervention rate of 97.6%, which represents a 2.8% increase (p = .003). Notably, the post-intervention weekend CHG bathing adherence rate was significantly lower (89.3%) than the weekday rate (97.6%) (p < .001) (Figure 1). The project team used these data to validate and confirm that the QIP interventions instituted only during the weekdays were effective for increasing overall CHG bathing adherence.
Figure 1.
Pre-intervention versus post-intervention CHG bathing adherence rates. Weekday, weekend, and overall CHG bathing adherence rates are shown. CHG indicates chlorhexidine gluconate.
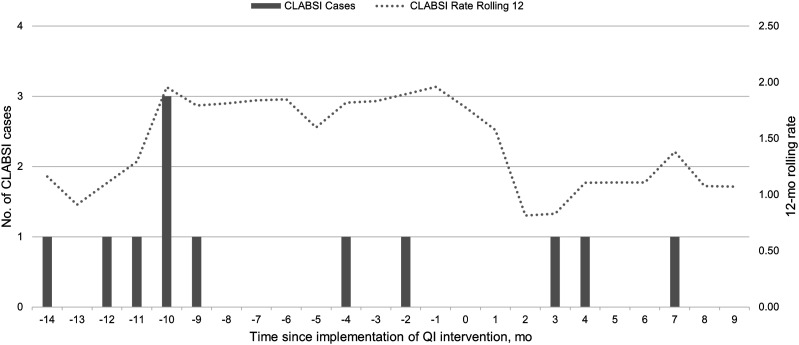
The rate of CLABSIs in our hospital was difficult to assess before and after the QIP interventions because the total number of reported CLABSIs were small. Although we did not identify any CLABSIs during our 3-month project window, the 12-month CLABSI rolling rate decreased from 1.78 in September 2022 to 1.07 in June 2023. However, the sample size was too small to perform statistical analyses of these data (Figure 2).
Figure 2.
Reported CLABSI cases by month. Bars represent the number of CLABSIs reported for each month at our hospital. The solid line represents the rolling 12-month rolling rate of CLABSIs calculated for each month. CLABSI indicates central line–associated bloodstream infection. QI, quality improvement.
Discussion
Our initiative focused on reducing the burden of CLABSI while providing data-driven solutions that were sustainable and engaged frontline staff. By measuring, analyzing, and sharing information, we enhanced our hospital’s overall compliance of CHG bathing and increased positive outcomes for patients. Although evidence from previous infection prevention studies supports daily CHG bathing as an effective method of CLABSI reduction, our internal review of current practices exposed barriers to providing this care for patients consistently. These barriers included difficulty in easily identifying patients who required CHG bathing, as well as the time-consuming process to review clinical notes and nursing documentation in the EHR manually.
A limitation to our QIP was that our pre-intervention CHG bathing adherence rate included both weekday and weekend cases. Before the initiative, the data were not segmented to show weekday and weekend CHG bathing adherence rates separately. However, this limitation provided an opportunity for improvement that led us to develop a method to distinguish between weekday and weekend CHG bathing adherence, which thereby allowed us to report and review these data separately. The importance of this was evidenced by the various nuanced differences between weekday and weekend operations and staffing.
The stark difference we observed in CHG bathing adherence between weekdays and weekends stresses the importance of active surveillance performed by the infection preventionist. Because of limited IPAC resources, coverage was not sustainable during weekends, and our findings indicated the need to transfer responsibility to the frontline nurses who provide continuous care to the patient.
To this end, another workgroup was formed to address concerns regarding the lower weekend CHG bathing adherence rate after the conclusion of our project. This included incorporating the Time Since CHG Bathing EHR column into the frontline nursing team’s standard practice. Our QIP allowed our hospital to improve adherence during weekends by using the columns and reports created in our EHR intervention.
Our initial improvements, which increased visibility of CHG bathing adherence in the reporting tools, were evident especially during weekdays. We then extended these improvements to weekends, with similar process improvement tactics and engagement of frontline staff. This was accomplished by real-time feedback to our nursing staff via input and direction from our IPAC project team. Clinical leadership support and having multidisciplinary team engagement with clinicians and other team members was also an important success factor.
One of the key accomplishments of this QIP initiative was to highlight the benefits of a collaborative partnership among IPAC, nursing informatics, and the frontline staff providing direct patient care. This partnership was more effective at disseminating the interventions than an individual department would have been. The results of this QIP endorse previous evidence showing that CHG bathing can reduce risk of infection. In addition, our findings show that nursing informatics, real-time surveillance, and outreach can be leveraged to increase CHG bathing adherence. Although further studies are needed to validate our findings, a multidisciplinary approach empowering frontline caregivers with proactive, data-driven leading indicators of infection prevention may effectively decrease the high morbidity and mortality rates associated with HAIs such as CLABSIs.
Acknowledgments
The authors express their sincere gratitude to our institute’s Scientific Publications group for their invaluable contributions, which include a thorough review and meticulous editorial assistance.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Brad A Krier https://orcid.org/0009-0001-3898-6114
Pawan Bhandari https://orcid.org/0000-0002-4235-3029
Ashley M Brooks https://orcid.org/0009-0006-1236-7792
Kristin J Schultz https://orcid.org/0009-0006-6946-0517
Jonna J Zarbano https://orcid.org/0009-0006-9120-5360
Gokhan Anil https://orcid.org/0000-0002-0247-7211
References
- Agency for Healthcare Research and Quality (2018) Eliminating CLABSI, a National Patient Safety Imperative. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Buetti N, Marschall J, Drees M, et al. (2022) Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 Update. Infection Control and Hospital Epidemiology 43(5): 553–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (2021) National Healthcare Safety Network Statistics Calculator. Center for Disease Control and Prevention: Atlanta, GA, USA. Available at: https://nhsn2.cdc.gov/ (accessed 17 October). [Google Scholar]
- Chapman L, Hargett L, Anderson T, et al. (2021) Chlorhexidine gluconate bathing program to reduce health care-associated infections in both critically ill and non-critically ill patients. Critical Care Nurse 41(5): e1–e8. [DOI] [PubMed] [Google Scholar]
- Clarkson RR. (2020) Zero CLABSI is achievable. American Journal of Infection Control 48(8, Supplement): S35. [Google Scholar]
- Destine Y, Capes K, Reynolds SS. (2023) Reduction in patient refusal of CHG bathing. American Journal of Infection Control 51(9): 1034–1037. [DOI] [PubMed] [Google Scholar]
- Garcia R. (2023) Moving beyond central line-associated bloodstream infections: enhancement of the prevention process. Journal of Infusion Nursing 46(4): 217–222. [DOI] [PubMed] [Google Scholar]
- Ghonim ER, Ennin-Evelyn J. (2020) Reducing central line associated blood stream infections in a major academic facility using a novel comprehensive tool. American Journal of Infection Control 48(8): S56. [Google Scholar]
- Knobloch MJ, Musuuza JS, McKinley L, et al. (2021) Implementing daily chlorhexidine gluconate (CHG) bathing in VA settings: the human factors engineering to prevent resistant organisms (HERO) project. American Journal of Infection Control 49(6): 775–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwaiti AA, Subbarayalu AV. (2017) Reducing hospital-acquired infection rate using the Six Sigma DMAIC approach. Saudi J Med Med Sci 5(3): 260–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston M. (2021) CLABSI prevention - using a 90 Day sprint. American Journal of Infection Control 49(6, Supplement): S18–S19. [Google Scholar]
- Loftus K, Tilley T, Hoffman J, et al. (2015) Use of Six Sigma strategies to pull the line on central line-associated bloodstream infections in a neurotrauma intensive care unit. Journal of Trauma Nursing 22(2): 78–86. [DOI] [PubMed] [Google Scholar]
- O'Grady NP, Alexander M, Burns LA, et al. (2011) Guidelines for the prevention of intravascular catheter-related infections. Clinical Infectious Diseases 52(9): e162–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reagan KA, Chan DM, Vanhoozer G, et al. (2019) You get back what you give: decreased hospital infections with improvement in CHG bathing, a mathematical modeling and cost analysis. American Journal of Infection Control 47(12): 1471–1473. [DOI] [PubMed] [Google Scholar]