Abstract
Background
An online mail order naloxone and harm reduction supply program was created by an interdisciplinary team at the University of Rhode Island College of Pharmacy and hosted on the university website (UNIV). The program was subsequently funded by the Rhode Island Department of Health (DOH) and added to the DOH website. This study compares demographic characteristics of the two populations submitting requests through the program’s distinct access points, UNIV and DOH, to those of populations at-risk for overdose.
Methods
This is a retrospective comparative analysis using voluntarily provided information from mail order request forms submitted through two websites from June 2020 through October 2023. The primary objective was to compare demographic characteristics of requesters through the two access points to those of individuals at-risk for experiencing or responding to an overdose. Descriptive statistics were used to characterize the two distinct populations. Chi-square tests were performed to determine if statistically significant differences in population demographics existed between access points. Odds ratios were estimated using a simple logistic regression model to assess the relationship between access point and demographic characteristic to determine if either access point had a greater likelihood of reaching individuals with at-risk demographics.
Results
A total of 5,783 (UNIV = 1662; DOH = 4121) mail order request forms were included in the analysis. Participants who completed requests through UNIV were more likely to be 44 years old or younger and/or reside in rural areas. Participants who submitted requests through DOH were more likely to reside in non-rural and/or low-income areas, and/or identify as gender minorities. Additionally, UNIV respondents were more likely to be first-time naloxone requesters while DOH respondents were more likely to have obtained and used naloxone before.
Conclusions
Results establish that different access points can reach different at-risk population subsets and support the use of multiple access points and advertising strategies to expand the reach of online mail order harm reduction programs.
Study registration
The study was retrospectively approved by the University of Rhode Island Institutional Review Board (IRB reference #2124391-2).
Keywords: Overdose, Naloxone, Mail order, Harm reduction supplies, Online program
Background
The number of lives lost to drug overdose has peaked in the United States (US) in recent years [1–3]. The majority of fatal drug overdoses in the last 10 years have been attributed to synthetic opioids other than methadone, reaching a rate of 22.7 per 100,000 in 2022 [4]. Importantly, disparities exist in the rate of fatal overdoses, with people of lower socioeconomic status (SES) comprising a significant proportion of overdose deaths [2–6]. Because of the continuously increasing rate of fatal drug overdose, it is of critical and timely importance to expand access to overdose response training and harm reduction supplies, especially for individuals at-risk for experiencing, witnessing, or responding to an overdose.
In efforts to address the ongoing opioid crisis, numerous harm reduction strategies have emerged, many of which work to expand access to naloxone. Naloxone is an opioid antagonist which can be lifesaving when administered to someone experiencing an overdose from opioids like heroin or fentanyl. The drug works by competitively binding to opioid receptors and displacing the opioid to reverse potentially fatal symptoms of an overdose. Naloxone binds with greatest affinity to mu opioid receptors, which are implicated in respiratory depression that can lead to death. The competitive antagonism of naloxone is transient, and repeat doses may be required to successfully reverse an overdose. Naloxone does not exhibit any agonistic effects and is not effective in reversing overdoses caused by drugs other than opioids [7, 8].
Naloxone received its first Food and Drug Administration (FDA) approval in 1971 as an injection; however, its use was limited to administration by medical professionals [8]. Take-home naloxone was not approved until 1996, and many community-based harm reduction organizations worked to obtain naloxone for people who use drugs (PWUD) throughout the 1990s and 2000s. Other formulations of naloxone have come to market in the last 10 years to facilitate easier administration. A naloxone auto-injector, Evzio®, was approved in April 2014 (discontinued in 2020) and a 4 milligram (mg) naloxone nasal spray formulation, Narcan®, gained approval in 2015 [9, 10].
Despite having a viable overdose reversal agent available, the prescription status of naloxone posed an ongoing barrier to access. Consequently, in the 2010s, states began passing laws requiring co-prescribing of naloxone to patients receiving opioid prescriptions, which proved to be an effective strategy for increasing naloxone awareness and distribution [11]. By the end of 2022, 18 states had passed co-prescribing laws, though requirements vary by state and range from offering patients naloxone to mandated co-prescribing [12]. Notably, the people who benefit from co-prescribed naloxone are patients receiving opioid prescriptions, and with the decline in opioid prescribing, deaths from prescription opioid overdose have likewise declined [13]. Additionally, people receiving prescription opioids and co-prescribed naloxone have established healthcare and have bypassed access barriers faced by PWUD not engaged in the healthcare system. Prescription opioids and co-prescribed naloxone processed through pharmacies are captured by insurance claims and prescription monitoring data, whereas illicitly acquired opioids and naloxone distributed outside of healthcare settings are not. Thus, there is a large gap in available information about opioid use and naloxone uptake by PWUD who are not engaged in healthcare settings [12–15].
In attempts to address the unmet needs of PWUD not seen in healthcare settings, opioid settlement money released from the federal government has led to disbursement of thousands of naloxone kits for distribution by harm reduction programs around the country, and research projecting the impact of enhanced naloxone distribution supported by these funds has emerged [16]. Furthermore, in 2023, two naloxone nasal sprays, Narcan® (4 mg) and RiVive® (3 mg), were approved as over-the-counter (OTC) products, facilitating retail access without the need for a prescription [17, 18].
Naloxone can be administered by anyone, regardless of training [19]. However, overdose response education is an important component of effective harm reduction strategies and offers benefits beyond naloxone administration information [20]. Overdose education and naloxone distribution (OEND) programs provide access to both the drug itself and training on how to identify and respond to an overdose. The benefits of OEND programs have been observed across many different demographic groups, ranging from PWUD and community bystanders to healthcare students and professionals [20–22]. People who have participated in overdose response trainings consistently report increased confidence in overdose recognition and naloxone administration [20–22]. Additionally, participants in OEND programs report changed attitudes towards naloxone, indicating that programming is also effective at increasing knowledge of barriers and combatting stigma faced by PWUD [20, 22]. A recent survey sought to gain the perspectives of PWUD and community bystanders on take-home naloxone access, experiences, and attitudes [23]. Most respondents were willing to use naloxone, would want naloxone used on them in the event of an overdose, wanted to carry naloxone, and believed it should be widely and freely available. Despite the overwhelmingly positive attitudes toward naloxone possession and use, only 24% of respondents indicated having access to harm reduction programs and only 30% currently carried naloxone.
A key characteristic of effective harm reduction programs is adaptability to changes in populations of focus, access to naloxone and other harm reduction supplies, and technological developments [24]. With PWUD and their close contacts facing many physical, social, economic, and stigma-related barriers, efforts have been made to create access points that are convenient, discreet, and free of cost. In the last decade, online mail order naloxone and harm reduction supply programs have emerged, with Needle EXchange Technology (NEXT) Distro leading the charge since its inception in 2017 [25]. The NEXT Distro program is based in New York City and works to fulfill harm reduction supply requests through their website by connecting requesters to local affiliates in all 50 states. When requesters access the NEXT Distro website (nextdistro.org), they are linked to harm reduction organizations in their state, and both access points presented in this study are linked on their website as Rhode Island resources [26].
Rhode Island has seen the increased national overdose death rate reflected on a state level [27]. To address the unmet state need for accessible harm reduction supplies, the University of Rhode Island (URI) College of Pharmacy created the Community First Responder Program (CFRP) in 2019 through an interdisciplinary collaboration with the College of Nursing and the College of the Environment and Life Sciences at URI [28]. The CFRP is an online OEND program which includes a virtual overdose response training module and a form to request naloxone and other harm reduction supplies for delivery by US mail. In 2021, the Rhode Island Department of Health (RIDOH) fully funded the CFRP initiative and expanded access to the training module and mail order request form by adding it to their harm reduction website, Prevent Overdose Rhode Island (PORI) [29]. In 2022, the program was awarded funding from a Rural Opioid Technical Assistance Regional (ROTA-R) grant and became the Northeast ROTA Regional Center [30]. Through collaboration with five partner institutions, the online OEND training modules were modified for each of the New England states and published on their university websites. To date, over 1,000 OTC naloxone kits have been mailed to New England residents outside of Rhode Island.
With greater distribution of naloxone and other harm reduction supplies, it is important to ensure that supplies are reaching individuals at increased risk for experiencing or responding to an overdose. This study is a retrospective comparative analysis of the populations completing mail order harm reduction supply requests through the program’s two unique access points, URI’s Community First Responder Program website (UNIV) and RIDOH’s Prevent Overdose Rhode Island website (DOH). The study aims to compare the demographics of the two unique populations to those of individuals at-risk for experiencing or responding to an overdose and demonstrate that different OEND access points can reach different subsets of the at-risk population.
Methods
Study aim
The aim of this study is to assess the ability of distinct access points for an online OEND program to reach individuals at-risk for experiencing or responding to an overdose. The primary objective was to compare demographic characteristics of requesters to pre-defined at-risk population demographics to determine if one access point had a greater capability to reach at-risk individuals than the other.
Design and setting
This is a retrospective comparative analysis of demographic characteristics from individuals requesting naloxone and/or other harm reduction supplies through a Rhode Island-based mail order OEND program with two unique online access points. All data were voluntarily provided and de-identified prior to inclusion in analysis. The study was retrospectively approved and registered by the University of Rhode Island Institutional Review Board [(IRB); IRB reference #2124391-2].
The CFRP and PORI are two Rhode Island internet-based harm reduction programs serving communities in the state, with CFRP hosted on the state university website (UNIV) and PORI hosted on the state Department of Health website (DOH).
Data sources and study population
Partially or fully completed mail order naloxone and harm reduction supply requests submitted through both access points from June 2020 through October 2023 were included in the study (N = 5,783). Both UNIV and DOH are publicly available websites, and therefore anyone with the ability to access UNIV or DOH can submit requests. Both UNIV and DOH request submissions contain demographic information as well as which harm reduction supplies were requested, prior naloxone requests, and outcomes associated with prior naloxone use.
The following demographic information was collected through the mail order request forms: mailing city/town, mailing zip code, gender identity, race, ethnicity, age, number of naloxone nasal spray kits requested and/or other harm reduction supplies requested. Other harm reduction supplies available for mail order include fentanyl test strips (FTS), safer smoking kits (bubble or straight pipe), and safer snorting kits. Requesters were also asked to provide the following information: main reason for ordering a naloxone kit, if it was their first time requesting a naloxone kit, and if their previous naloxone had been used to respond to an overdose.
Demographic responses were recorded as selections from a pre-determined list of options, “other” with free text response, or the option to decline to respond. Gender identity response options included male, female, genderqueer, agender/nonbinary, transgender, transmasculine, and transfeminine. Race response options included white, Black/African American, American Indian/Alaskan Native, Asian, Native Hawaiian/Pacific Islander, or “other”. Ethnicity response options were Hispanic/Latinx or Non-Hispanic/Latinx. Age responses were recorded as year ranges and categorized into 44 years of age and younger and 45 years of age or older.
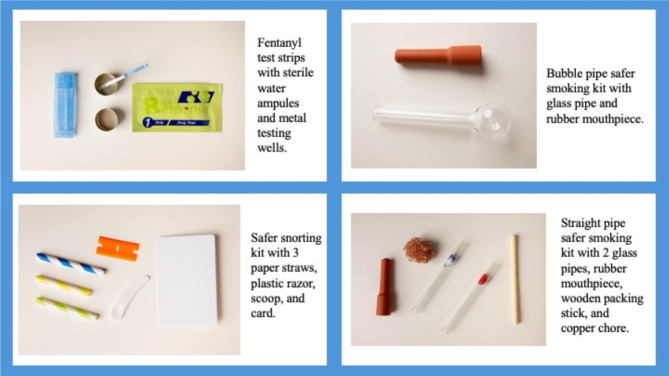
All individuals requesting naloxone received one (two-dose) intranasal naloxone kit by default, unless a reason for requesting more than one kit was noted and approved. Beyond naloxone, requesters could indicate if they needed fentanyl test strips and/or a safer snorting kit by selecting “yes” or “no” to the two questions, respectively. Requesters were also asked if they needed a safer smoking kit by selecting “yes” or “no”. If “yes”, requesters were asked to indicate which type of pipe, “straight” or “bubble”. Photographs of the kits and descriptions of their contents are presented in Fig. 1.
Fig. 1.
Contents of harm reduction supply kits available through mail order
When asked to indicate the main reason for ordering a naloxone kit, requesters were given the following response options: personal use (self or close family/friend), professional use (community health worker, healthcare professional, first responder, or educator), community responder (increased overdose activity in neighborhood or workplace”, “other” with a free text field to specify, or the option to decline to respond.
Requesters were asked if it was their first time requesting a naloxone kit. If yes, no further questions were asked. If the requester indicated previously having naloxone, they were asked if their previous naloxone kit was used to respond to an overdose, when the overdose occurred, how many naloxone doses were administered, and if the person survived.
Data organization
All responses were compiled in the University of Rhode Island’s Qualtrics website. Though names of requesters were not collected, IP addresses were, and all IP address data were removed by the data handler before being transferred to the investigators. Mailing address information, aside from city/town and zip code, were also eliminated from the analysis set to protect requesters from potential identification.
To compare population demographics from both UNIV and DOH to population demographics of those with higher rates of overdose risk in Rhode Island, “risk” first needed to be defined. Current literature assessing demographics of individuals with higher rates of overdose risk in the United States indicates that individuals of lower socioeconomic status, those living in rural areas, individuals who are White, American Indian, Alaskan Native, identify as male or gender minority, and/or those aged 30–44 are at greater risk of overdose than individuals without these characteristics [2, 5, 6]. The increased risk of overdose among people with these demographics is likewise reflected at a state level in Rhode Island [27]. To prepare the mail order data set for analysis, the following information was used to further classify responses: mailing zip codes were matched to cities/towns and coded for rurality using the definition of rurality put forth by RIDOH; mailing zip codes were matched for area income status using median household income data put forth by the Rhode Island Department of Labor and Training (DLT), then towns and cities were classified as either “low-income” (in the bottom 20th percentile of cities/towns in the state), or “other” (above the 20th percentile) [31, 32].
Statistical analysis
All requests submitted through UNIV and DOH were included in the analysis set, whether they were partially or fully completed. Blank responses were excluded from analysis on a question-by-question basis. All responses underwent initial analyses using descriptive statistics to determine the percentages of each response within each of the two data sets from their respective access points.
Tests to detect statistical significance in differences between the two data sets across access points were performed. Chi-square tests were performed to determine if greater ability to reach at-risk populations was related to which access point was used. Gender, race, ethnicity, income, rurality, FTS, smoking/snorting kits, reason for ordering, first-time naloxone, and previous naloxone used in an overdose response were compared between the two unique access points using Chi-square tests at a significance level of p ≤ 0.05. Odds ratios were used to estimate the likelihood of people with at-risk population demographics accessing either UNIV or DOH. Odds ratios were estimated using a simple logistic regression for gender minority vs. other (cisgendered); race minority vs. white; low income vs. other; rural vs. non-rural residence; ethnicity; requests for FTS, smoking (bubble pipe), smoking (straight pipe), and/or snorting kits; professional vs. personal use and community vs. personal use; first-time naloxone vs. previous naloxone possession; previous kit used or not used to respond to an overdose. Statistical analysis was completed using SAS version 9.4.
Results
During the 3-year study period, a total of 5,783 fully or partially completed mail order request forms for naloxone and other harm reduction supplies were submitted. Of all requests, 71.3% (N = 4121) were submitted through DOH and 28.7% (N = 1662) were submitted through UNIV. Of all requesters, 3.3% were gender minorities, 15.3% were racial minorities, 7% were ethnic minorities, 26.4% resided in low-income areas, and 13.5% resided in rural areas. Table 1 shows the demographic percentages of requesters by access point.
Table 1.
Percent demographics of individuals requesting mail order naloxone and harm reduction supplies by access point
| Demographics | Overall N = 5783, (%) |
UNIV N = 1662, (%) |
DOH N = 4121, (%) |
|---|---|---|---|
| Race | |||
| American Indian/Alaska Native | 20 (< 1) | 6 (< 1) | 14 (< 1) |
| Asian | 123 (2) | 42 (2.5) | 81 (2) |
| Black/African American | 214 (3.7) | 75 (4.5) | 139 (3.4) |
| Native Hawaiian/Pacific Islander | 14 (< 1) | 4 (< 1) | 10 (< 1) |
| White | 4303 (74.4) | 1226 (73.8) | 3077 (74.7) |
| Two or More Races | 163 (3.8) | 61 (3.7) | 102 (2.5) |
| Others/Unknown | 946 (16.4) | 248 (14.9) | 698 (16.9) |
| Gender | |||
| Female | 3487 (60.3) | 1105 (66.5) | 2382 (57.8) |
| Male | 1338 (23.1) | 338 (20.3) | 1000 (24.3) |
| Agender/Non-binary | 81 (1.4) | 13 (< 1) | 68 (1.7) |
| Genderqueer | 57 (< 1) | 7 (< 1) | 50 (1.2) |
| Transgender | 31 (< 1) | 10 (< 1) | 21 (< 1) |
| Transfeminine | 11 (< 1) | 4 (< 1) | 7 (< 1) |
| Transmasculine | 13 (< 1) | 4 (< 1) | 9 (< 1) |
| Unknown | 765 ((13.2) | 181 (10.9) | 584 (14.2) |
| Age | |||
| 44 and below | 3170 (54.8) | 976 (58.7) | 2194 (53.3) |
| 45 and older | 1815 (31.4) | 454 (27.3) | 1361 (33.0) |
| Unknown | 798 (13.8) | 232 (14) | 566 (13.7) |
| Ethnicity | |||
| Hispanic/Latino | 407 (7) | 123 (7.4) | 284 (6.9) |
| Non-Hispanic/Latino | 3882 (67.1) | 1055 (63.5) | 2827 (68.6) |
| Unknown/missing | 1494 (25.8) | 484 (29.1) | 1010 (24.5) |
| Income level | |||
| Low-income | 1527 (26.4) | 242 (14.6) | 1285 (31.2) |
| Other income | 2272 (39.3) | 839 (50.5) | 1433 (34.8) |
| Unknown/missing | 1984 (34.3) | 581 (35.0) | 1403 (34.0) |
| Location | |||
| Rural | 783 (13.5) | 317 (19.1) | 466 (11.3) |
| Non-rural | 4205 (72.7) | 1142 (68.7) | 3063 (74.3) |
| Unknown/missing | 795 (13.7) | 203 (12.2) | 592 (14.4) |
| Fentanyl test strips | |||
| Yes | 1511 (26.1) | 404 (24.3) | 1107 (26.9) |
| No | 1369 (23.7) | 374 (22.5) | 995 (24.1) |
| Unknown/missing | 2903 (50.2) | 884 (53.2) | 2019 (49.0) |
| Smoking kit | |||
| Yes, one straight pipe | 81 (1.4) | 21 (1.3) | 60 (1.5) |
| Yes, one bubble pipe | 230 (4) | 72 (4.3) | 158 (3.8) |
| No | 1713 (30) | 419 (25.2) | 1294 (31.4) |
| Unknown/missing | 3759 (65) | 1150 (69.2) | 2609 (63.3) |
| Snorting kit | |||
| Yes | 94 (1.6) | 30 (1.8) | 64 (1.6) |
| No | 347 (6) | 163 (9.8) | 184 (4.5) |
| Unknown/missing | 5342 (92.4) | 1469 (88.4) | 3873 (94.0) |
| Reason for ordering | |||
| Professional use | 152 (2.6) | 53 (3.0) | 99 (2.4) |
| Personal use | 86 (1.5) | 37 (2.2) | 49 (1.2) |
| Community responder | 187 (3.2) | 86 (5.2) | 101 (2.5) |
| Unknown/missing | 5358 (92.7) | 1486 (89.4) | 3872 (94.0) |
| First-time naloxone kit | |||
| Yes | 2241 (38.8) | 665 (40.0) | 1576 (38.2) |
| No | 746 (12.9) | 154 (9.3) | 592 (14.4) |
| Unsure | 70 (1.2) | 10 (0.6) | 60 (1.5) |
| Unknown/missing | 2726 (47.1) | 833 (50.1) | 1893 (45.9) |
Note the sums of some percentages exceed 100%, this is because figures were rounded up to one decimal place
Individuals completing requests through UNIV were significantly more likely to be 44 years of age or younger (χ² = 18.8, p-value < 0.0001), less likely to be gender minorities (χ² = 9.3, p-value = 0.0023), more likely to be first-time naloxone requesters (χ² = 22.9, p-value < 0.0001), less likely to reside in low-income areas (χ² = 199.3, p-value < 0.0001), more likely to reside in rural areas (χ² = 56.7, p-value < 0.0001), less likely to have previously used naloxone to respond to an overdose (χ² = 7.4, p-value = 0.0064), more likely to request a bubble pipe safer smoking kit (χ² = 5.0, p-value = 0.0249), and less likely to request a safer snorting kit (χ² = 6.8, p-value = 0.009) relative to requesters through DOH. Differences in race, ethnicity, FTS, and straight pipe safer smoking kits between the two access points were not statistically significant. Table 2 provides the demographic characteristic compared and their respective Chi-square results and odds ratio estimations.
Table 2.
Chi-square and odds ratio analyses between access points
| Demographics | Overall N = 5783, (%) |
UNIV N = 1662, (%) |
DOH N = 4121, (%) |
UNIV vs. DOH [Chi-Square, (p-value)] | UNIV vs. DOH [Odds Ratio (CI)] |
|---|---|---|---|---|---|
| Gender | Gender minority vs. other (cisgender) | ||||
| Gender Minority | 193 (3.3) | 38 (2.3) | 155 (3.8) | 9.3 (0.0023*) | 0.575 [0.401, 0.824]* |
| Other | 4825 (83.4) | 1443 (86.8) | 3382 (82.1) | ||
| Unknown/missing | 765 (13.2) | 181 (10.9) | 584 (14.2) | ||
| Race | Racial minority vs. other (white) | ||||
| Racial minority | 882 (15.3) | 267 (16.1) | 615 (14.9) | 1.1 (0.2874) | 1.090 [0.930, 1.276] |
| Other (White) | 4303 (74.4) | 1226 (73.8) | 3077 (74.7) | ||
| Unknown/missing | 598 (10.3) | 169 (10.2) | 429 (10.4) | ||
| Age | Age 44 and younger vs. 45 and older | ||||
| 44 and younger | 3170 (54.8) | 976 (58.7) | 2194 (53.2) | 18.8, (<0.0001*) | 1.334 [1.171, 1.519]* |
| 45 and older | 1815 (31.4) | 454 (27.3) | 1361 (33.0) | ||
| Unknown/missing | 798 (13.8) | 232 (14.0) | 566 (13.7) | ||
| Ethnicity | Hispanic/Latinx vs. other (non-Hispanic/Latinx) | ||||
| Hispanic/Latino | 407 (7.0) | 123 (7.4) | 284 (6.9) | 1.7 (0.1905) | 1.161 [0.929, 1.451] |
| Non-Hispanic/Latino | 3882 (67.1) | 1055 (63.5) | 2827 (68.6) | ||
| Unknown/missing | 1494 (25.8) | 484 (29.1) | 1010 (24.5) | ||
| Income level | Low income vs. other | ||||
| Low-income | 1527 (26.4) | 242 (14.6) | 1285 (31.2) | 199.3 (< 0.0001*) | 0.322 [0.274, 0.378]* |
| Other income | 2272 (39.3) | 839 (50.5) | 1433 (34.8) | ||
| Unknown/missing | 1984 (34.3) | 581 (35.0) | 1403 (34.0) | ||
| Location | Rural vs. non-rural | ||||
| Rural | 783 (13.5) | 317 (19.1) | 466 (11.3) | 56.7 (< 0.0001*) | 1.825 [1.558, 2.137]* |
| Non-rural | 4205 (72.7) | 1142 (68.7) | 3063 (74.3) | ||
| Unknown/missing | 795 (13.7) | 203 (12.2) | 592 (14.4) | ||
| Fentanyl test strips | Fentanyl test strips yes vs. no | ||||
| Yes | 1511 (26.1) | 404 (24.3) | 1107 (26.9) | 0.1 (0.7254) | 0.971 [0.824, 1.145] |
| No | 1369 (23.7) | 374 (22.5) | 995 (24.1) | ||
| Unknown/missing | 2903 (50.2) | 884 (53.2) | 2019 (49.0) | ||
| Smoking kit | Smoking kit yes vs. no | ||||
| Yes, one straight pipe | 81 (1.4) | 21 (1.3) | 60 (1.5) | 5.0 (0.0803) |
Straight Pipe 1.081 [0.650, 1.798] |
| Yes, one bubble pipe | 230 (4.0) | 72 (4.3) | 158 (3.8) | ||
| No | 1713 (29.6) | 419 (25.2) | 1294 (31.4) |
Bubble Pipe 1.407 [1.043, 1.899]* |
|
| Unknown/missing | 3759 (65.0) | 1150 (69.2) | 2609 (63.3) | ||
| Snorting kit | Snorting kit yes vs. no | ||||
| Yes | 94 (1.6) | 30 (1.8) | 64 (1.6) | 6.8 (0.0090*) | 0.529 [0.327, 0.857]* |
| No | 347 (6.0) | 163 (9.8) | 184 (4.5) | ||
| Unknown/missing | 5342 (92.4) | 1469 (88.4) | 3873 (94.0) | ||
* = Significant result; significance level p ≤ 0.05
Of the individuals who indicated their reason for ordering naloxone and/or other harm reduction supplies through both UNIV and DOH, the majority were community responders, followed by professional use, with personal use being indicated the least. For 38.8% of all requesters across both access points, it was their first-time requesting naloxone. Of the 12.9% (N = 746) who indicated having previously possessed a naloxone kit, 22% (N = 165) had used their previous kit to respond to an overdose, and 81% (N = 135) of the overdose responses had resulted in survival. Table 3 provides naloxone response information overall and analysis between sources.
Table 3.
Responses about previous naloxone kit possession and use
| Responses | Overall N, (%) |
UNIV N, (%) |
DOH N, (%) |
UNIV vs. DOH [Chi-Square, (p-value)] | UNIV vs. DOH OR[CI] |
|---|---|---|---|---|---|
| First-time naloxone kit | First-time naloxone kit yes vs. no | ||||
| Yes | 2241 (38.8) | 665 (40.0) | 1576 (38.2) | 22.9 (< 0.0001*) | 1.622 [1.329, 1.979]* |
| No | 746 (12.9) | 154 (9.3) | 592 (14.4) | ||
| Unsure | 70 (1.2) | 10 (0.6) | 60 (1.5) | ||
| Unknown/missing$ | 2726 (47.1) | 833 (50.1) | 1893 (45.9) | ||
| Previous kit used to respond to an overdose | Previous kit overdose yes vs. no | ||||
| Yes | 165 (2.9) | 22 (1.3) | 143 (3.5) | 7.4 (0.0064*) | 0.509 [0.311, 0.832]* |
| No | 521 (9.0) | 121 (7.3) | 400 (9.7) | ||
| Unsure | 56 (1.0) | 10 (0.6) | 46 (1.1) | ||
| Unknown/missing$ | 5041 (87.2) | 1509 (90.8) | 3532 (85.7) | ||
| Person survived | Person survived yes vs. no | ||||
| Yes | 135 (NA) | 20 (NA) | 115 (NA) | 0.3930# | 0.348 [0.030, 4.019] |
| No | < 5 (NA) | < 5 (NA) | < 5 (NA) | ||
| Unsure | 23 (NA) | < 5 (NA) | 21 (NA) | ||
* = Significant result; $ = Excluded from Chi-square statistics calculation; # = Fisher’s Exact test; significance level p ≤ 0.05
Discussion
The results of this study demonstrate that distinct access points can reach different subsets of populations at-risk for experiencing or responding to an overdose. Founded at the University in Rhode Island in 2019, UNIV promotes overdose response education and expands distribution of naloxone to individuals around the state. However, at the time of its inception, the reach of UNIV was limited by lack of advertising and awareness of the program outside of the university. When UNIV was expanded by RIDOH in 2021 to become part of the statewide overdose response initiative, the program was advertised in several ways, including but not limited to billboards, text message campaigns, and social media posts. Both programs and websites attract different population subsets, as seen in the results of this study.
We hypothesized that UNIV, being university-based and promoted, would reach more individuals identifying as gender minorities, those aged 44 years and younger, and those residing in rural areas. Conversely, we hypothesized that DOH, being state-run and promoted, would reach a greater proportion of individuals residing in low-income and non-rural areas, and individuals of minoritized racial and ethnic groups. In alignment with the hypotheses, DOH respondents were more likely to reside in low-income and non-rural areas and UNIV respondents were more likely to reside in rural areas and be aged 44 years or younger. In contrast to the hypotheses, UNIV respondents were less likely to be gender minorities than DOH respondents and neither access point had a greater ability to reach minoritized racial or ethnic groups. The differences between the hypotheses and results demonstrate that it is difficult to predict who will utilize OEND programs based on assumptions of the “typical” audience of access points. Therefore, a strategy for broadening the reach of OEND programs would be to create multiple access points with different advertising methods that appeal to wide swaths of people.
Of course, this program and other mail order OEND programs are not without limitations. One limitation is that online/mail order OEND programs are most likely to be accessed by individuals who have stable housing, a mailing address where they can safely receive packages, and internet access. Despite the expansion of internet service in the last two decades, a significant portion of US population still does not have reliable and consistent online access [33]. Thus, there are certainly members of the at-risk community who are unable to utilize online harm reduction resources.
Another accessibility limitation of the program is that it is currently only published in English and Spanish, and therefore not readily usable by individuals who speak different primary languages. Rhode Island has a large population of people with limited English proficiency, with Portuguese, Chinese, and French being the most spoken languages aside from English and Spanish. Thus, it is a reasonable and important goal for harm reduction programming to be published in several languages which align with those spoken in the region of focus. Additionally, current goals for readability and usability of online OEND programs is to have online materials that are written at a sixth-grade reading level [34]. The module component of the program is currently at a tenth grade reading level, and the mail order request form is at a fifth grade reading level. While the mail order request form is at a sixth-grade reading level, requesters through both UNIV and DOH encounter the training module before being able to submit their requests, and the advanced reading level of the module may pose a barrier to request submission.
As previously mentioned, an important characteristic of effective OEND programs is adaptability to changes in populations and risk factors. The program has offered mail-order naloxone since March 2020. However, to cater to the needs of PWUD as synthetic opioids are increasingly present in other unregulated substances, the program added FTS, safer smoking kits, and safer snorting kits for mail order in June 2022, December 2022, and July 2023, respectively. While offering safer use supplies for mail order is a positive development for harm reduction, the later additions of the test strips and safer use kits pose limitations to this study. Demographic data of individuals requesting supplies other than naloxone were unable to be collected for the complete duration of the study period and therefore it was not possible to detect if the additional offerings have reached more individuals at-risk for experiencing or responding to an overdose. The addition of the kits to mail order was intended to attract more PWUD and their close contacts to the program, in the future through continuing to offer safer use supplies.
For individuals who completed mail order requests through the program, self-stigma may have affected accurate reporting of the reason for requesting harm reduction supplies. The results indicated that the majority of requesters abstained from indicating their reason for requesting and the minority of requesters indicated ordering naloxone and other supplies for personal use. It is unclear if the program is not adequately reaching PWUD and their close contacts, or if self-stigma has caused requesters to answer differently or not at all. Interestingly, most respondents across both UNIV and DOH self-identified as females and/or of white race. Considering that 27.3% of DOH respondents and 33% of UNIV respondents indicated that they are age 45 or older, it is possible that the program is being accessed by people who act as caretakers.
Conclusion
This retrospective comparative analysis was designed to assess how well the online-based mail-order OEND program was reaching individuals at-risk for experiencing or responding to an overdose. The two distinct access points had differing abilities to reach certain subsets of the population at-risk, but neither had a clear advantage over the other. The program’s reach, distribution, and publishing on several other websites demonstrate that online OEND programs are usable and scalable. The results from this study stand to inform future development, web placement and advertisement strategies to further online OEND program use and reach subsets of the at-risk population.
Acknowledgements
We would like to thank Massiel Almond Frias, LMHC, and Tammy Whan, CPhT, for their work with the Community First Responder Program. We would also like to thank Jennifer Koziol and Nya Reichley for their support of our program.
Abbreviations
- CI
Confidence interval
- CFRP
Community First Responder Program
- DLT
Department of Labor and Training
- DOH
Department of Health
- FDA
Food and Drug Administration
- FTS
Fentanyl test strips
- mg
Milligram
- NEXT
Needle EXchange Technology
- OEND
Overdose education and naloxone distribution
- OR
Odds ratio
- OTC
Over-the-counter
- PORI
Prevent Overdose Rhode Island
- PWUD
People who use drugs
- RIDOH
Rhode Island Department of Health
- ROTA
Rural Opioid Technical Assistance
- ROTA
R-Rural Opioid Technical Assistance Regional
- SES
Socioeconomic status
- UNIV
University
- URI
University of Rhode Island
- US
United States
Author contributions
AJ compiled the UNIV and DOH data for analysis. AO completed the statistical analysis for the study. MP completed background research and was the main writer of the manuscript. MP prepared all tables and figures. All authors read and approved the final manuscript.
Funding
The Community First Responder Program is funded through a grant by the Rhode Island Department of Health.
Data availability
The datasets used and/or analyzed for this study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study uses previously captured, voluntarily-provided data and was approved by the University of Rhode Island Institutional Review Board (IRB reference #2124391-2).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 2018–2022 on CDC WONDER Online Database, released in 2024. Data are from the Multiple Cause of Death Files, 2018–2022, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. http://wonder.cdc.gov/ucd-icd10-expanded.html. Accessed on 2024 May 6.
- 2.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic patterns in drug and synthetic opioid overdose deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–7. 10.15585/mmwr.mm7006a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States, 1999–2020. Hyattsville, MD: National Center for Health Statistics; 2021. 10.15620/cdc:112340. NCHS Data Brief, no 428.
- 4.Spencer MR, Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2002–2022. Hyattsville, MD: National Center for Health Statistics; 2024. 10.15620/cdc:135849. NCHS Data Brief, no 491.
- 5.Altekrause SF, Cosgrove CM, Altekrause WC, Jenkins RA, Blanco C. Socioeconomic risk factors for fatal overdoses in the United States: mortality disparities in American communities study (MDAC). PLoS ONE. 2020. 10.1371/journal.pone.0227966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Britz JB, O’Loughlin KM, Henry TL, Richards A, Sabo RT, Saunders HG, et al. Rising racial disparities in opioid mortality and undertreatment of opioid use disorder and mental health comorbidities in Virginia. AJPM Focus. 2023. 10.1016/j.focus.2023.100102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Naloxone. In: Clinical Pharmacology [database on the Internet]. Tampa (FL): Elsevier; 2017 [cited 2024 Jun 26]. Available from: http://www.clinicalpharmacology.com. Subscription required to view.
- 8.Naloxone [package insert]. Richmond, VA: Kaleo, Inc; 2022.
- 9.Food and Drug Administration. FDA approves new hand-held auto-injector to reverse opioid overdose. 2014. http://wayback.archive-it.org/7993/20161022205011/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm391465.htm. Accessed 2024 Jun 25.
- 10.Food and Drug Administration. FDA moves quickly to approve easy-to-use nasal spray to treat opioid overdose. 2015. https://wayback.archive-it.org/7993/20180125101447/https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm473505.htm. Accessed 2024 Jun 25.
- 11.Green TC, Davis C, Xuan Z, Walley AY, Bratberg J. Laws mandating coprescription of naloxone and their impact on naloxone prescription in five US states, 2014–2018. Am J Public Health. 2020. 10.2105/AJPH.2020.305620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis C, Lieberman AJ, Larkin K. Naloxone prescription mandates. The Network for Public Health Law. 2023. https://www.networkforphl.org/wp-content/uploads/2023/07/Fact-Sheet-Naloxone-Prescription-Mandates-2022-update.pdf
- 13.Drug overdose death rates. NIDA. 2024. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates. Accessed 2024 Jun 27.
- 14.Holmgren AJ, Botelho A, Brandt AM. A history of Prescription Drug Monitoring Programs in the United States: political appeal and Public Health Efficacy. Am J Public Health. 2020;110(8):1191–7. 10.2105/AJPH.2020.305696. Epub 2020 Jun 18. PMID: 32552023; PMCID: PMC7349461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones CM, Compton W, Vythilingam M, Giroir B. Naloxone co-prescribing to patients receiving prescription opioids in the Medicare Part D Program, United States, 2016–2017. JAMA. 2019;322(5):462–4. 10.1001/jama.2019.7988. PMID: 31386124; PMCID: PMC6686765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zang X, Skinner A, Krieger MS, Behrends CN, Park JN, Green TC, et al. Evaluation of strategies to enhance community-based naloxone distribution supported by an opioid settlement. JAMA Netw Open. 2024. 10.1001/jamanetworkopen.2024.13861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Food and Drug Administration. FDA approves first over-the-counter naloxone nasal spray. 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-over-counter-naloxone-nasal-spray. Accessed 2024 Jun 25.
- 18.Food and Drug Administration. FDA approves second over-the-counter naloxone nasal spray product. 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-second-over-counter-naloxone-nasal-spray-product. Accessed 2024 Jun 25.
- 19.Lifesaving naloxone. CDC. 2024. https://www.cdc.gov/stop-overdose/caring/naloxone.html#cdc_generic_section_4-who-should-carry-naloxone. Accessed 2024 Jun 25.
- 20.Razaghizad A, Windle SB, Filion KB, Gore G, Kudrina I, Paraskevopoulous E, et al. The effect of overdose education and naloxone distribution: an umbrella review of systematic reviews. Am J Public Health. 2021. 10.2105/AJPH.2021.306306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dahlem CH, Patil R, Khadr L, Ploutz-Snyder RH, Boyd C, Shuman CJ. Effectiveness of take ACTION online naloxone training for law enforcement officers. Health Justice. 2023. 10.1186/s40352-023-00250-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galiher MV, Huffman M. Attitude changes following short-form opioid overdose video education: a pilot study. Harm Reduct J. 2022. 10.1186/s12954-022-00696-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwieger L, Carpenter JE, Moran TP, Erowid F, Cornelison M, Evans D, et al. Access to, experience with, and attitudes towards take home naloxone: an online survey. J Community Health. 2024. 10.1007/s10900-023-01321-6. [DOI] [PubMed] [Google Scholar]
- 24.Fairbarn N, Coffin PO, Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: challenges and innovations responding to a dynamic epidemic. Int J Drug Policy. 2017. 10.1016/j.drugpo.2017.06.005. [DOI] [PMC free article] [PubMed]
- 25.Yang C, Favaro J, Meacham MC. NEXT harm reduction: an online, mail-based naloxone distribution and harm-reduction program. Am J Public Health. 2021. 10.2105/AJPH.2020.306124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NEXT Distro.https://nextdistro.org (2024). Accessed 2024 Jun 24.
- 27.Rhode Island Department of Health. Overdose fatalities. RIDOH Drug Overdose Surveillance Data Hub. https://ridoh-drug-overdose-surveillance-fatalities-rihealth.hub.arcgis.com (2024). Accessed 2024 May 6.
- 28.Community First Responder Program. https://web.uri.edu/cfrp/ (2024). The University of Rhode Island. Accessed 2024 Apr 8.
- 29.Prevent Overdose RI. https://preventoverdoseri.org (2024). Rhode Island Department of Health. Accessed 2024 Apr 8.
- 30.URI Community First Responder Program ROTA-R. https://web.uri.edu/rota-r/ (2024). The University of Rhode Island. Accessed 2024 Apr 8.
- 31.Defining rural Rhode Island. Rhode Island Department of Health. 2022. https://health.ri.gov/publications/definitions/2022Rural-definition.pdf. Accessed 2024 Apr 8.
- 32.Rhode Island city and town income from American Community 5-year estimates 2017–2021. Rhode Island Department of Labor and Training. 2022. https://dlt.ri.gov/sites/g/files/xkgbur571/files/documents/pdf/lmi/towninc.pdf. Accessed 2024 Apr 8.
- 33.Greenberg-Worisek AJ, Kurani S, Finney Ruten LJ, Blake KD, Hesse BW. Tracking healthy people 2020 internet, broadband, and mobile device access goals: an update using data from the health information national trends survey. J Med Internet Res. 2019. 10.2196/13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dang N, Khunte M, Zhong A, Chatterjee A. Naloxone online information exceeds the recommended reading level for patient education materials. JSAD. 2023. 10.15288/jsad.22-00343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States, 1999–2020. Hyattsville, MD: National Center for Health Statistics; 2021. 10.15620/cdc:112340. NCHS Data Brief, no 428.
- Spencer MR, Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2002–2022. Hyattsville, MD: National Center for Health Statistics; 2024. 10.15620/cdc:135849. NCHS Data Brief, no 491.
Data Availability Statement
The datasets used and/or analyzed for this study are available from the corresponding author on reasonable request.