Abstract
Background:
High volumes and competing priorities delay care initiation for neonatal hyperbilirubinemia within the pediatric emergency department (ED). Our freestanding children’s hospital developed a quality improvement project to implement a nurse-initiated neonatal hyperbilirubinemia clinical pathway (CP) intended to decrease treatment initiation and intravenous fluid (IVF) rates.
Methods:
A multidisciplinary team used the model for improvement to delineate and address key drivers of treatment delays. The team established a nurse-driven CP and enhanced the electronic health record to support and enforce new workflows, which included capillary specimen collection and phototherapy initiation before the first provider assessment. IVF criteria and laboratory evaluation were standardized. The primary aim was to decrease the time to initiation of phototherapy from a mean of 136 to 60 minutes after ED arrival for 6 months. The secondary aim was to decrease the proportion of patients obtaining IVF from 31% to 15% for the same time frame.
Results:
ED arrival to phototherapy initiation decreased from 136 to 49 minutes. The IVF rate decreased from 31% to 12%. ED length of stay decreased from 185 to 122 minutes. Hospital length of stay remained unchanged.
Conclusions:
A nurse-initiated CP for neonates with hyperbilirubinemia improved time-to-care initiation and ED throughput while decreasing unnecessary IVF administration.
INTRODUCTION
Neonatal hyperbilirubinemia occurs in 8%–11% of neonates.1 Jaundice has been reported to account for 21%–25% of neonatal emergency department (ED) visits,2,3 with similar local rates and accounts for three-quarters of readmissions.4 ED care is variable, especially regarding laboratory studies and intravenous fluids (IVFs).5 In 2022, the American Academy of Pediatrics updated management guidelines for infants born ≥35 weeks gestation to improve and decrease variation in care.6
Hyperbilirubinemia is an abnormal accumulation of bilirubin in the blood, causing yellow discoloration of the eyes and skin resulting from elevated levels of conjugated or unconjugated bilirubin. Turnover of fetal red blood cells, the inability of the newborn liver to conjugate bilirubin, and increased enterohepatic circulation cause benign neonatal hyperbilirubinemia. More than 80% of newborns will have some degree of hyperbilirubinemia,7,8 and most cases are benign and self-limited. However, very high levels of unconjugated bilirubin are neurotoxic. If left untreated, a portion of the unconjugated bilirubin can freely cross the blood–brain barrier and lead to acute bilirubin encephalopathy with acute and chronic neurologic impairment.9 Some risk factors for developing significant hyperbilirubinemia include prematurity, hemolysis, exclusive breastfeeding with poor intake, scalp hematoma, macrosomia, Down syndrome, and a family history of inherited blood disorders. Acute bilirubin encephalopathy occurs in approximately 1 in 10,000 live births, resulting in potentially permanent neurological disabilities, including developmental delay, cerebral palsy, and hearing loss. Thus, it is important to diagnose and treat hyperbilirubinemia promptly using a streamlined approach.5,6 Timely intervention in the ED has the additional benefit of improving throughput.10
Clinical pathways (CPs) have been shown to reduce variation and directly impact patient outcomes, hospital length of stay (HLOS), and cost.11–13 CPs are developed using evidence, published clinical practice guidelines, and data from quality or continuous improvement protocols.11 Nurse-initiated care in the ED has been shown to expedite management initiation and decrease admission rates.14 Neonatal hyperbilirubinemia CPs have decreased time to phototherapy, time in the ED, and IVF rates.15,16 The American Academy of Pediatrics’s clinical practice guideline for managing neonatal hyperbilirubinemia highlighted the importance of timely treatment of infants with this diagnosis and the continued oral feeding of patients on phototherapy.6
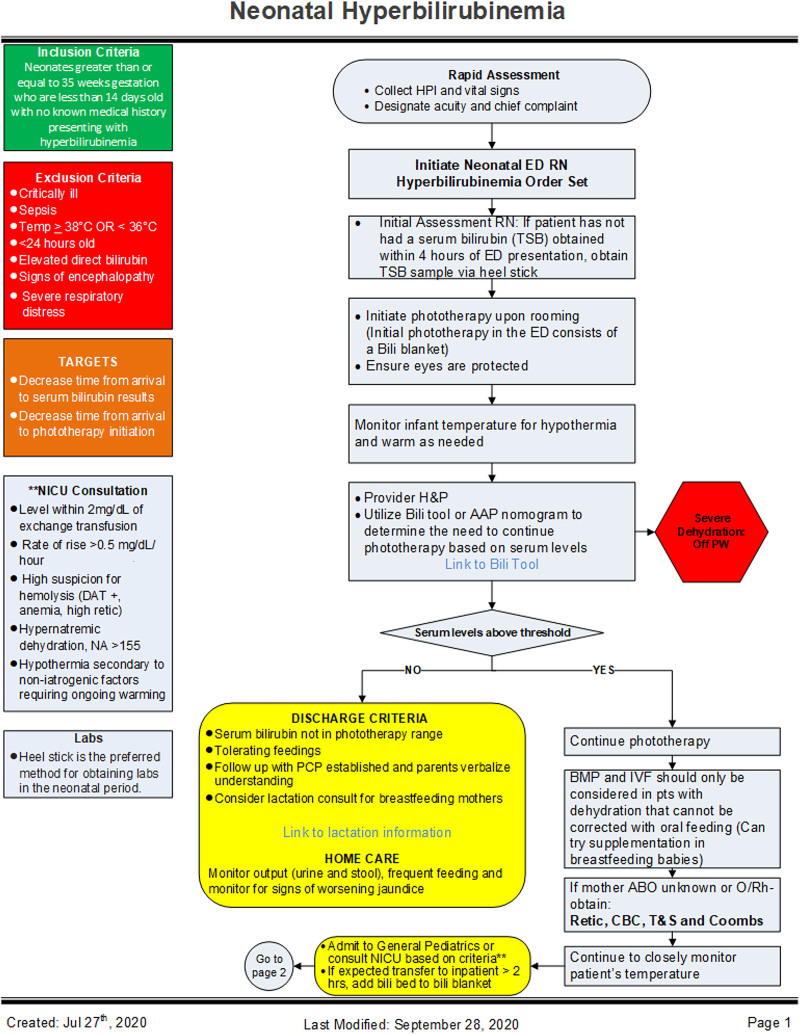
Within our pediatric ED, no standard protocol existed for the care of neonatal hyperbilirubinemia. Therefore, the provider-based timing of specimen collection and phototherapy resulted in prolonged time-to-care initiation and ED time. Additionally, ancillary laboratory evaluation and IVF therapy varied between providers. Both Wolff et al15 and Long et al17 reported improved standardization of care, timeliness of care, and ED LOS secondary to a nurse-initiated jaundice protocol. Using the Institute for Healthcare Improvement model for improvement, our team designed a quality improvement (QI) project to standardize and optimize the care of patients seen in our ED by creating a CP (Fig. 1) with nurse-initiated orders. The primary aim of this QI project was to decrease the time to initiation of phototherapy after ED arrival from a mean of 136 to 60 minutes for 6 months. The secondary aim was to decrease the proportion of patients obtaining IVF from 31% to 15%.
Fig. 1.
Hyperbilirubinemia CP. The CP shows the medical management in the emergency department and inpatient units for infants with hyperbilirubinemia. RN, registered nurse; AAP, American Academy of Pediatrics; ABO, blood type group; BMP, basic metabolic panel; CBC, complete blood count; DDX, differential diagnosis; IVF, intravenous fluids; H&P, history and physical; HPI, history of present illness; IVIG, intravenous immunoglobulin; mIVF, maintenance intravenous fluids; NA, sodium; O/Rh−, Rhesus factor negative; T&S, type and screen.
METHODS
The institutional review board reviewed this project and deemed it exempt because it was determined to be QI, not human subject research.
Context
This prospective, interrupted time series QI initiative occurred at a tertiary-care, suburban, pediatric, Level I trauma center ED with a volume of 60,000 annual visits. The ED is part of a 208-inpatient freestanding children’s hospital staffed by board-certified pediatric emergency medicine attending physicians, general pediatricians, nurse practitioners, physician assistants, and residents from various training programs. Triage nurses evaluate patient acuity and facilitate ED throughput.
Patient Population
Neonates greater ≥35 weeks gestation between 1 and 14 days old who presented to the ED with a chief complaint of hyperbilirubinemia or jaundice were included in this study. Patients who were febrile, hypothermic, had indications of dehydration, or had other concurrent known illnesses were excluded.
Interventions
The QI team included representatives from nursing administration, clinical informatics, emergency medicine, neonatology, hospital medicine and primary care. It was essential to partner with all care teams interacting with patients to understand challenges and develop effective countermeasures. The team created a current state process map to highlight barriers to early initiation of phototherapy. (See Figure 1, Supplemental Digital Content 1, http://links.lww.com/PQ9/A608.) Then, it altered the sequence of care to move essential steps earlier in the visit. Interventions included nursing-driven protocol orders created with a nursing order set. These orders allow care to begin during the triage process immediately upon patient arrival rather than waiting for evaluation by a provider. This order set included obtaining a neonatal bilirubin panel blood specimen when 4 hours had lapsed from outpatient laboratory draw and then initiating phototherapy. Phototherapy began on all infants presenting with a chief complaint of hyperbilirubinemia instead of waiting for the laboratory results. This intervention ensured rapid phototherapy initiation for all patients, preventing bilirubin levels from rising in the ED.
ED, inpatient, and neonatal intensive care unit (NICU) representatives identified ancillary laboratory results required for hospital admission. Capillary blood collection laboratory evaluation prevented unnecessary venipuncture. Providers encouraged oral hydration in all patients, including formula supplementation in breastfed infants before IV hydration. NICU versus inpatient pediatric unit admission criteria were clarified.
Plan-do-study-act (PDSA) cycles drove and sustained improvement, including data sharing with staff and emphasizing key points with re-education. PDSA cycles identified multiple key drivers and process gaps. Important components included are as follows:
Proper documentation of phototherapy start time.
ED technicians’ ability to document within the electronic health record (EHR).
Early initiation of phototherapy following blood collection.
Standardization on proper technique of capillary blood collection.
Criteria for IVF initiation and laboratory evaluation.
Enhanced EHR functionality allowed nurses to document birth history and implement a standardized provider note template to assess key historical information accurately. A best practice alert was triggered when phototherapy initiation was outside the appropriate time window. When ED volumes increased, clinical decision support embedded within the order set reminded triage nurses to initiate phototherapy in any available room.
Implementation Strategies
Multipronged implementation strategies ensured the success of the pathway’s structures, processes, and outcomes. First, ED triage nurses were granted access to necessary equipment. Nurses received training at staff meetings, followed by more detailed individual sessions. Training included improvement opportunities, pathophysiology of hyperbilirubinemia, patient inclusion criteria, preference of capillary blood specimens, process changes, protocol order set, and EHR enhancements. To gain buy-in, we allowed all providers to give feedback. Once finalized, provider education occurred at a staff meeting, followed by one-to-one education for those unable to attend the staff meeting. Educational content included smart aims, creation of nursing protocol, preference of oral intake over IVF, recommended laboratory evaluation, ability to send labs via capillary sample, and NICU admission criteria. The triage desk, workstations, and staff huddle boards displayed copies of the CP as a visual reminder of the new workflow. To increase engagement, a group of interested attending physicians joined the QI team and received maintenance of certification credit for their participation.
During the initial implementation period, clinical staff received in-the-moment coaching and feedback when caring for a child with hyperbilirubinemia, focusing primarily on the early initiation of phototherapy and capillary blood specimen collection. Outcome data shared with clinical teams during huddles and staff meetings focused on success and areas for improvement.
Staff Surveys
Staff completed anonymous Likert scale surveys electronically before and 60 days after the CP’s introduction. (See Figure 2, Supplemental Digital Content 2, http://links.lww.com/PQ9/A609.) Responses included self-report of ED role, length of time working in the ED, and knowledge of hyperbilirubinemia, including risk factors, complications, the likelihood of placing an IV, and satisfaction regarding the management of hyperbilirubinemia.
Measures
The primary outcome measure was the time from ED arrival to phototherapy initiation. The secondary outcome measure was the percentage of patients who received IVF. The process measure was nursing order utilization rates. The balancing measures were time from rooming to disposition decision and HLOS. Time from ED rooming-to-disposition was measured rather than the entire ED LOS because LOS is dependent on ED volumes and discharge processes outside the scope of this work. With newly established IV placement and laboratory assessment standards, keeping track of these balancing measures was important to ensure timely care decisions.
Data Collection
All patients with a chief complaint of jaundice or hyperbilirubinemia ≤14 days of age were included in the data analysis unless they had a concurrent chief complaint of weight loss, lethargy, abdominal mass, reduced appetite, decreased urination, dehydration, fever, or low body temperature. We monitored pathway adherence and outcomes in a dashboard. Because phototherapy initiation was not documented in a standardized location in the baseline period, the time of initiation was extracted manually in the baseline and verified for all patients in the postimplementation phase. De-identified data were maintained in an ongoing spreadsheet. Identified outliers and manual chart audits assessed process barriers at the project’s outset. Data collection included staff surgery responses.
Data Analysis
Descriptive statistics compared demographic differences between pre- and postimplementation groups (Table 1). We analyzed demographic data using “R” software (R version 4.2.2; The R Foundation, r-project.org). An independent t test compared patients’ ages, and chi-square goodness of fit tests identified whether the 2 groups were disproportionately characterized by sex or race/ethnicity.
Table 1.
Patient Demographics of the Entire Neonatal Population and before and after CP Implementation
| Total Population (N = 387) | Pre-CP (N = 83) | Post-CP (N = 304) | P | |
|---|---|---|---|---|
| Age | 4.48 (1.78) | 4.55 (1.70) | 4.47 (1.80) | 0.70 |
| Race/ethnicity | 0.92 | |||
| Black/African American | 98 (25%) | 20 (24%) | 78 (26%) | — |
| White/Caucasian | 209 (54%) | 48 (58%) | 161 (53%) | — |
| Asian | 30 (8%) | 6 (7%) | 24 (8%) | — |
| American Indian | 1 (<1%) | 0 (0%) | 1 (<1%) | — |
| Other | 49 (13%) | 9 (11%) | 40 (13%) | — |
| Sex | 0.45 | |||
| Male | 205 (53%) | 47 (57%) | 158 (52%) | — |
| Female | 182 (47%) | 36 (43%) | 146 (48%) | — |
We tracked and graphed time measures monthly using X-BAR S statistical process control charts, whereas proportion measures were tracked with P-charts. Standard rules determine if changes result from common or special cause variation. Control charts were created using QI-charts V.2.0.23 software (Scoville Associates, 2009) for Microsoft Excel (Microsoft, 2016). Fisher’s chi-square test calculated whether a statistically significant difference was present in demographics pre- and postimplementation using IBM SPSS Statistics (IBM) and Social Science Statistics’ Easy Fisher’s Exact Test Calculator (Socscistatistics.com, 2023). Staff survey data analysis was completed using “R” software. Based on statistical analysis indicating the pre- and postsurvey responses were not normally distributed, Mann–Whitney U tests compared response differences.
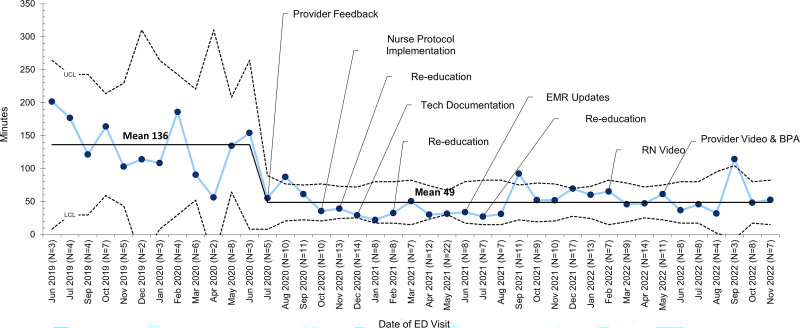
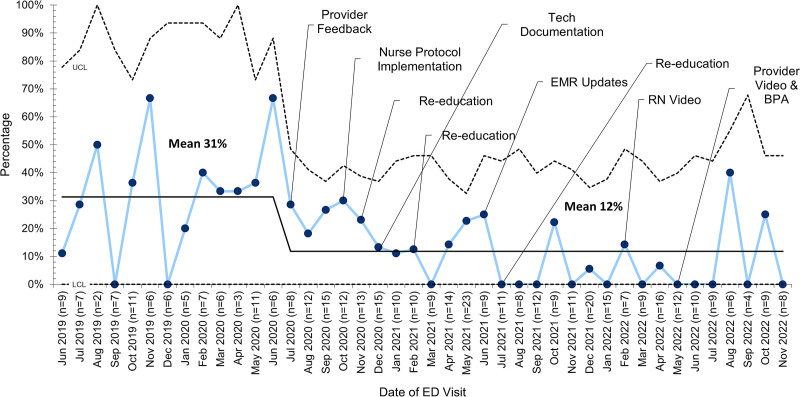
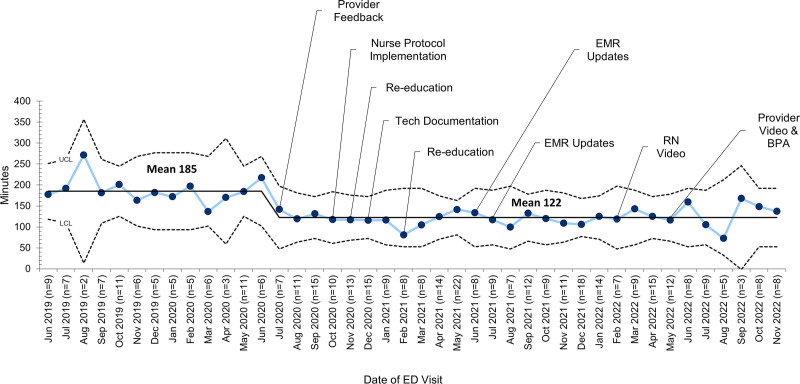
RESULTS
In the baseline phase from July 2019 to June 2020, the cohort included 83 infants; in the implementation phase from July 2020 to November 2022, the cohort included 304 infants, with 26 excluded. Demographic characteristics were similar in the pre- and postimplementation groups (Table 1). The time to initiate phototherapy decreased from an average of 136–49 minutes in July 2020 after provider feedback and was sustained throughout the report (Fig. 2; see Figure 3, Supplemental Digital Content 3, http://links.lww.com/PQ9/A610). The proportion of patients who received IVF decreased from a mean of 31%–12% in July 2020, which reflected the initial provider acknowledgment of pathway recommendations. This improvement continued throughout the project (Fig. 3). The time from patient rooming-to-disposition decision decreased by 63 minutes from an average of 185–122 minutes (Fig. 4; see Figure 4, Supplemental Digital Content 4, http://links.lww.com/PQ9/A611). Nurses activated protocol orders for 63% of patients between July 2022 and November 2022.
Fig. 2.
Time to phototherapy initiation. X-bar chart showing the time from emergency department arrival to phototherapy before and after CP implementation. August 2019 was ghosted since it was a baseline outlier above the upper control limit. BPA, Epic Best Practice Advisory; EMR, electronic medical record; LCL, lower control limit; RN, registered nurse; UCL, upper control limit.
Fig. 3.
The proportion of patients who received intravenous fluids. P-chart for the proportion of patients who received intravenous fluids before and after implementation of the CP. EMR, electronic medical record; LCL, lower control limit; RN, registered nurse; UCL, upper control limit.
Fig. 4.
Time from ED room placement to disposition. X-bar chart for the time from emergency department rooming to disposition before and after CP implementation. EMR, electronic medical record; LCL, lower control limit; RN, registered nurse; UCL, upper control limit.
Forty staff members completed the survey preimplementation, and 25 staff members completed the survey post-CP implementation. Staff surveys identified the demographics of respondents, who were nurses and technicians (Table 2). Responses regarding 3 questions in the survey addressing participant knowledge of hyperbilirubinemia management, knowledge of complications, and risk factors indicated no differences before and after the CP introduction (P > 0.05). Satisfaction with the management of hyperbilirubinemia increased significantly following pathway initiation (pre: M = 2.25) and (post: M = 1.6), where lower scores are associated with greater satisfaction. Report of IV utilization decreased significantly before and after implementation (pre: M = 2.7; post: M = 3.54). Lower scores indicate more frequent IV use (Table 2).
Table 2.
Staff Survey Demographic and Response Analyses
| Pretest (N = 40) | Posttest (N = 25) | Test-Statistic | P | |
|---|---|---|---|---|
| Role | ||||
| Registered Nurse | 33 (83%) | 20 (80%) | — | — |
| Technician | 7 (17%) | 5 (20%) | — | — |
| Years on unit | ||||
| Less than 1 | 9 (23%) | 5 (20%) | — | — |
| 1–5 | 23 (57%) | 13 (52%) | — | — |
| 5–10 | 4 (10%) | 6 (24%) | — | — |
| 10–20 | 2 (5%) | 1 (4%) | — | — |
| 20+ | 2 (5%) | 0 (0%) | — | — |
| Hyperbilirubinemia knowledge | ||||
| Neonatal | 2.23 (0.83) | 1.96 (0.46) | 586 | 0.19 |
| Complications | 2.33 (0.80) | 2.28 (0.68) | 527 | 0.69 |
| Risk factors | 2.30 (0.82) | 2.04 (0.46) | 581 | 0.20 |
| Satisfaction management | 2.25 (0.78) | 1.60 (0.58) | 727 | <0.001 |
| Comfortable | 1.58 (0.84) | 1.63 (0.92) | 462 | 0.78 |
| Delayed treatment | 2.63 (0.90) | 3.04 (0.94) | 367 | 0.06 |
| PIV placement | 2.70 (1.81) | 3.54 (1.10) | 289 | 0.006 |
| CP | ||||
| Satisfaction | — | 1.28 (0.46) | — | — |
| Use (% yes) | — | 22 (88%) | — | — |
| Satisfaction education | — | 9.40 (0.96) | — | — |
*Hypothesis testing includes the Mann–Whitney U test.
PIV, peripheral intravenous.
DISCUSSION
An ED neonatal hyperbilirubinemia CP improved time to phototherapy initiation by 65% (136 to 49 min). The improvements began with provider knowledge of goals and were augmented with the nurse-driven protocol implementation. Additionally, IVF rates decreased by 60%. Standardization decreased venipuncture, and resequencing of care all improved ED throughput by 63 minutes without increasing HLOS. The success could be due to the preexisting culture of accepting care standardization using pathways and protocol orders for other disease processes.
Others have also shown that hyperbilirubinemia pathways can standardize care, reduce time in the ED, limit unnecessary diagnostic studies, and decrease the time from arrival to phototherapy initiation.16–18 Romero et al16 implemented ED and inpatient CPs to improve quality of care and included data from 186 patients. Time from ED arrival to phototherapy decreased from 101 to 54 minutes. Similar to our work, 2 institutions utilized nurse-driven care to improve time to phototherapy and ED throughput.15,17 Only one of these institutions used standing nursing orders in a large pediatric ED to facilitate early diagnosis and decreased time to phototherapy.17 Our initiative showed the reproducibility of their work conducted in a Canadian pediatric ED. Additionally, our methodology utilized the Institute for Healthcare Improvement model for improvement, including PDSA cycles of learning, which was a different design than both Wolff et al and Long et al.15,17
Education to optimize feeding with lactation specialists during business hours and collaborative agreement with hospital pediatrics decreased the use of IVF. HLOS did not increase, and intermittent review of patient charts showed no inpatient IV placements and further labs were not drawn during the admission. Reducing the number of peripheral intravenous catheters placed in the ED likely contributed to improved throughput. Although this study did not assess patient satisfaction, IV placement, which can cause patient pain, parental anxiety, prolonged ED time, and place patients at increased risk for infiltrates, was decreased.
Nurse order set activation was the proxy for initiating the pathway and process adherence. Some patients arrived with outpatient laboratory results within 4 hours of ED presentation and did not require a repeat blood draw. For these patients, nurses could initiate phototherapy without entering an order, and therefore, a lack of order set utilization does not necessarily indicate a lack of early phototherapy initiation. Additionally, in some cases, providers activated the order set before evaluating the patients because they were aware of pathway goals. These contributing factors likely allowed for overall improvement in phototherapy initiation times even though nurses only applied protocol orders 63% of the time. Staff satisfaction with patient management improved after pathway implementation, likely related to earlier care initiation and improved ED throughput. On the other hand, knowledge of hyperbilirubinemia management, risk factors, and complications did not change as a result of interventions, likely because staff had a solid foundational understanding of disease pathophysiology.18,19
ED room-to-disposition was initially a balancing measure because several variables impact ED time. Further laboratory evaluations or decisions regarding IV hydration could occur later in the ED course and prolong ED time. However, room-to-disposition time improved soon after implementation. ED overcrowding increases wait times, ambulance diversions, medical errors, mortality, safe patient care, and financial losses.19,20 This initiative improved ED throughput significantly. Therefore, the benefit of starting all patients on phototherapy and ceasing phototherapy for patients who did not meet treatment thresholds outweighed the risks. Risks associated with phototherapy include skin rash, loose stool, overheating, dehydration, and retinal injury, which are unlikely if exposed to phototherapy for short periods wearing eye protection. This protocol exposed approximately 40% of patients unnecessarily to phototherapy; however, this was a brief exposure, and phototherapy ceased when laboratory results were less than the phototherapy threshold. As such, the benefit of early phototherapy initiation for the individual patient and ED flow outweighed the potential risk to the patient. In addition to low risk, the cost of disposable supplies associated with phototherapy was low, and families were not charged for phototherapy unless they were admitted because ED billing is by service bundles.
Limitations
This study had several limitations. First, we initiated phototherapy on all infants presenting with jaundice to prevent further rise in serum bilirubin levels, but some infants unnecessarily received phototherapy. The benefits of this strategy outweigh the risks. Second, infants at higher risk with other illnesses or underlying diagnoses were excluded from the pathway and thus could not benefit from the pathway. Third, this study did not measure family experience as an indication of increasing quality of care. Fourth, this initiative may not be generalizable to all settings. Finally, the success of this pathway depended on continuous education, which can be a challenge in a busy ED with limited implementation resources.
A data collection limitation is that phototherapy initiation time measurement depends on appropriate EHR documentation. This documentation needed to be more consistent in the baseline and early implementation phases, so charts had to be manually reviewed to determine start times. Order time was used when the EHR did not contain phototherapy start times, possibly leading to underestimated start times. This effect would have been greater in the baseline than in the postimplementation population.
CONCLUDING SUMMARY
Implementing a neonatal hyperbilirubinemia CP was associated with decreased phototherapy, IVF utilization, and ED time. Utilization of a nursing protocol to initiate evaluation and treatment is effective. A modified CP implemented in children’s hospitals and community EDs can standardize the care of neonates with hyperbilirubinemia. We plan to scale this work by finding other opportunities for nurse-initiated protocols within our ED.
Supplementary Material
Footnotes
Published online November 20, 2024.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
To cite: Miller CR, Haut C, Zomorrodi A, Chara K, Wilson J. Implementation of a Neonatal Hyperbilirubinemia Clinical Pathway in a Pediatric Emergency Department. Pediatr Qual Saf 2024;9:e774.
REFERENCES
- 1.Ullah S, Rahman K, Hedayati M. Hyperbilirubinemia in neonates: types, causes, clinical examinations, preventive measures and treatments: a narrative review article. Iran J Public Health. 2016;45:558–568. [PMC free article] [PubMed] [Google Scholar]
- 2.Millar KR, Gloor JE, Wellington N, et al. Early neonatal presentations to the pediatric emergency department. Pediatr Emerg Care. 2000;16:145–150. 10.1097/00006565-200006000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Lee HC, Bardach NS, Maselli JH, et al. Emergency department visits in the neonatal period in the United States. Pediatr Emerg Care. 2014;30:315–318. 10.1097/PEC.0000000000000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Britton JR, Britton HL, Beebe SA. Early discharge of the term newborn: a continued dilemma. Pediatrics. 1994;94:291–295. [PubMed] [Google Scholar]
- 5.DePorre AG, Hall M, Puls HT, et al. Variation in care and clinical outcomes among infants hospitalized with hyperbilirubinemia. Hosp Pediatr. 2020;10:844–850. 10.1542/hpeds.2020-0161. [DOI] [PubMed] [Google Scholar]
- 6.Kemper AR, Newman TB, Slaughter JL, et al. Clinical practice guideline revision: Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2022;150:e2022058859. 10.1542/peds.2022-058859. [DOI] [PubMed] [Google Scholar]
- 7.Keren R, Tremont K, Luan X, et al. Visual assessment of jaundice in term and late preterm infants. Arch Dis Child Fetal Neonatal Ed. 2009;94:F317–F322. 10.1136/adc.2008.150714. [DOI] [PubMed] [Google Scholar]
- 8.Bhutani VK, Stark AR, Lazzeroni LC, et al. ; Initial Clinical Testing Evaluation and Risk Assessment for Universal Screening for Hyperbilirubinemia Study Group. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. J Pediatr. 2013;162:477–482.e1. 10.1016/j.jpeds.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 9.Watchko JF. TcB, FFR, phototherapy and the persistent occurrence of kernicterus spectrum disorder. J Perinatol. 2020;40:177–179. 10.1038/s41372-019-0583-7. [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto LG, Killeen J, French GM. Transcutaneous bilirubin measurement methods in neonates and its utility for emergency department use. Pediatr Emerg Care. 2012;28:380–384. 10.1097/PEC.0b013e31824dcb43. [DOI] [PubMed] [Google Scholar]
- 11.Buchert AR, Butler GA. Clinical pathways: driving high-reliability and high-value care. Pediatr Clin North Am. 2016;63:317–328. 10.1016/j.pcl.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Flaherty MR, Whalen K, Lee J, et al. Implementation of a nurse-driven asthma pathway in the pediatric intensive care unit. Pediatr Qual Saf. 2021;6:e503. 10.1097/pq9.0000000000000503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schiessler MM, Darwin LM, Phipps AR, et al. Don’t have a doubt, get the catheter out: a nurse-driven CAUTI prevention protocol. Pediatr Qual Saf. 2019;4:e183. 10.1097/pq9.0000000000000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burgess L, Kynoch K, Theobald K, et al. The effectiveness of nurse-initiated interventions in the emergency department: a systematic review. Australas Emerg Care. 2021;24:248–254. 10.1016/j.auec.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Wolff M, Schinasi DA, Lavelle J, et al. Management of neonates with hyperbilirubinemia: improving timeliness of care using a clinical pathway. Pediatrics. 2012;130:e1688–e1694. 10.1542/peds.2012-1156. [DOI] [PubMed] [Google Scholar]
- 16.Romero HM, Ringer C, Leu MG, et al. Neonatal jaundice: Improved quality and cost savings after implementation of a standard pathway. Pediatrics. 2018;141:e20161472. 10.1542/peds.2016-1472. [DOI] [PubMed] [Google Scholar]
- 17.Long M, Farion KJ, Zemek R, et al. A nurse-initiated jaundice management protocol improves quality of care in the paediatric emergency department. Paediatr Child Health. 2017;22:259–263. 10.1093/pch/pxx056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Preloger E, Wedoff M, Lemke JT, et al. Decreasing laboratory testing for neonatal jaundice through revision of a clinical practice pathway. Hosp Pediatr. 2022;12:e67–e72. 10.1542/hpeds.2021-006019. [DOI] [PubMed] [Google Scholar]
- 19.Salway RJ, Valenzuela R, Shoenberger JM, et al. Emergency department (ED) overcrowding: evidence-based answers to frequently asked questions. Rev Méd Clín Las Condes. 2017;28:213–219. 10.1016/j.rmclc.2017.04.008. [Google Scholar]
- 20.Kane A, Tackett S, Ngo T, et al. Impact of an emergency department saturation tool on a pediatric hospital’s capacity management policy. Pediatr Emerg Care. 2023;39:457–461. 10.1097/PEC.0000000000002964. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.