Abstract
Objectives:
We examine recent trends in pain prevalence among adults aged 50+ across Europe.
Methods:
Data for 15 countries from the Survey of Health, Ageing, and Retirement in Europe are examined for two periods: 2004–2011 and 2013–2015. Trends are shown descriptively, using a multilevel modeling strategy controlling for covariates, and modeled on a country-specific basis.
Results:
Population-level pain prevalence ranges from about 30% to about 60% depending on the country and year. Pain is more prevalent in women and generally increases with age. There is an increase in prevalence over time, net of age, and other predictors. Prevalence increased with an annual average of 2.2% between 2004 and 2011 and 5.8% between 2013 and 2015, in fully adjusted models.
Discussion:
Trends in pain prevalence have implications for disability, healthcare utilization, productivity, and population health. These findings are not optimistic but align with other population-wide studies, suggesting a global trend of rising pain prevalence.
Keywords: pain, Europe, cross-national analysis, trends, aging
Introduction
There is limited research investigating trends in chronic pain among aging populations, especially within the European context, even though understanding pain trends is critical for assessing and improving population health. Chronic pain is among “the leading causes of global disability” (Blyth & Schneider, 2018) and a leading cause of healthcare utilization (Elliott et al., 1999; Song et al., 2016). It is closely connected to functional health problems that increase the need for formal and informal support (Andrews et al., 2013; Covinsky et al., 2009; Mäntyselkä et al., 2003). The economic costs of pain, including those related to lost productivity, are enormous and arguably greater than those for any other single health condition (Coyte et al., 1998; Gaskin & Richard, 2012; Wenig et al., 2009). Understanding trends in pain is also crucial for health equity; the social distribution of pain is highly unequal, with women and the socioeconomically disadvantaged experiencing substantially higher prevalence (Anderson et al., 2009; Andersson et al., 1993; Fillingim et al., 2009; Wijnhoven et al., 2006). Therefore, documenting the trends in pain is important for health, well-being, and equity in populations.
Today, the proportion of the population aged 50 and older is higher in Europe (about 38%) than in any other world region—higher still when considering Northern and Western Europe only—and continuing to rise rapidly (United Nations, 2018). Since prevalence of chronic pain increases with age, chronic pain may pose a particularly significant challenge for population health in Europe (Blyth, 2010; Breivik et al., 2013; European Commission, 2018). There are some examinations of pain levels, or prevalence, although most rely on cross-sectional, single-country, and small-sample data (Achterberg et al., 2010; Ahacic & Kåreholt, 2010; Breivik et al., 2006; Cimas et al., 2018; Croda, 2015; Farioli et al., 2014; Harkness et al., 2005; Heistaro et al., 1998; Hüppe et al., 2007; Todd et al., 2019). Furthermore, it is difficult to find a unifying message from these studies. While most confirm extensive effects of pain on individuals across Europe, they also collectively suggest variations in prevalence exist across countries.
Studies on temporal trends in European pain prevalence are particularly few and far between, and report mixed findings. Ahacic and Kåreholt (2010) found increases in prevalence among Swedish cohorts born in 1940 or later, Harkness et al. (2005) found very large increases in musculoskeletal pain prevalence in England, and Hüppe et al. (2007) and Heistaro et al. (1998) found little change in prevalence over time in Germany and Finland. The overall trends for European countries thus remain unclear.
Another knowledge gap pertains to correlates of the trends. Studies mentioned above tend to account for age and sex. Other factors associated with pain prevalence that might drive population-level trends are frequently absent. These include changes in social and economic factors such as marital and educational status, or changes in underlying health characteristics such as specific chronic conditions or obesity.
The Survey of Health, Ageing, and Retirement in Europe (SHARE) is a panel survey started in 2004 and comprises over 20 European countries, with the aim of producing cross-national panel data for the population aged 50 and older on health and other topics of interest to aging scholars and policymakers. SHARE contains questions that allow for pain prevalence estimates across a number of countries (Croda, 2015), but these data have not been previously analyzed with the aim of evaluating trends in pain. The present study is thus the first analysis to explore temporal trends in pain drawing on SHARE data, while taking into consideration concomitant changes in socioeconomic and health-related factors. Previous research suggests that pain prevalence may be reported differently across different countries and languages (Breivik et al., 2006; Farioli et al., 2014). Therefore, rather than directly comparing prevalence across countries or providing a unified prevalence estimate for Europe, which could be impacted by the reporting differences, we analyze within-country trends. This is accomplished by analyzing trends in individual countries separately and by pooling countries and using multilevel models with country-level random effects to adjust for the country-level idiosyncratic tendencies to differentially report pain.
Applying such techniques to SHARE data and considering the combination of acute and chronic pain, this study addresses three specific questions: (1) Has the prevalence of pain been increasing or decreasing across Europe net of changes in the age distribution? (2) Are the increasing or decreasing trends consistent across countries? (3) Do a set of correlates, commonly considered predictors of pain prevalence (e.g., age and sex), account for the increasing or decreasing trends? Answers to these questions will clarify how pain—an important but understudied aspect of population health—contributes to the changing health profiles of the 50 and older European population.
Methods
Data
Data are from SHARE (Börsch-Supan et al., 2013). SHARE provides cross-national longitudinal micro-data on health, socioeconomic status, social and family networks, and other topics associated with multidisciplinary aspects of aging. Participants are aged 50+. Data are collected primarily by computer-assisted personal interviews. Wave 1 collection occurred in 2004/5 in 11 European countries plus Israel and involved over 22,000 respondents. Waves 2 through 7 were collected in 2006/7, 2008/9, 2011, 2013, 2015, and 2017, respectively. New countries came on board over time, while others dropped out or did not participate in specific waves. Individuals were added in each wave to bolster samples, backfill younger ages, and replace dropouts. At the time of writing, SHARE had completed about 380,000 interviews with around 140,000 individuals. SHARE data have been cited in over 2,300 publications. Further details can be found on their website [http://www.share-project.org/].
Waves 3 and 7, titled “SHARELIFE,” concentrated on life course data and did not include questions needed for the current analysis. Therefore, we use data from Waves 1, 2, 4, 5, and 6, which cover years 2004–2015, and include the 15 countries: Austria, Belgium, the Czech Republic, Denmark, Estonia, France, Germany, Italy, Luxembourg, the Netherlands, Poland, Spain, Slovenia, Sweden, and Switzerland. In our analyses, each wave in each country is treated as a cross section. Table 1 shows sample sizes by country and survey wave/year. The total number of valid cases across waves and countries for this analysis is 207,701.
Table 1.
Countries, Country Abbreviations, and Unweighted Valid Sample Sizes by Survey Wave/Year.
| Abbreviation | Wave 1 (2004/5) | Wave 2 (2006/7) | Wave 4 (2011) | Wave 5 (2013) | Wave 6 (2015) | |
|---|---|---|---|---|---|---|
|
| ||||||
| Country | ||||||
| Austria | AUS | 1525 | 1178 | 5017 | 4262 | 3343 |
| Belgium | BEL | 3614 | 3107 | 5118 | 5492 | 5673 |
| Czech Republic | CZE | — | 2642 | 5320 | 5503 | 4782 |
| Denmark | DEN | 1611 | 2519 | 2206 | 4032 | 3647 |
| Estonia | EST | — | — | — | 5658 | 5520 |
| France | FRA | 2909 | 2832 | 5532 | 4392 | 3855 |
| Germany | GER | 2925 | 2562 | 1608 | 5548 | 4326 |
| Italy | ITA | 2497 | 2905 | 3512 | 4635 | 5184 |
| Luxembourg | LUX | — | — | — | 1582 | 1542 |
| Netherlands | NET | 2854 | 2622 | 2735 | — | — |
| Poland | POL | — | 2400 | 1713 | — | — |
| Slovenia | SLO | — | — | — | 2903 | 4169 |
| Spain | SPA | 2262 | 2364 | 3632 | 6537 | 5550 |
| Sweden | SWE | 2990 | 2751 | 1956 | 4492 | 3868 |
| Switzerland | SWI | 950 | 1445 | 3642 | 2984 | 2767 |
| Total (all waves) | 207,701 | |||||
Measuring Pain
In Waves 1, 2, and 4 of SHARE, all respondents were asked if they were “bothered by… pain in the back, knees, hips, or any other joint” (SHARE question PH010). In Wave 5, however, questions about pain changed. An initial question asked individuals if they are “troubled with pain” (SHARE question PH085). Those responding in the affirmative were asked about affected parts of the body (including back, knees, hips, and other locations). If the response to the first question was negative, respondents were not asked about specific pain sites. Because of this change, prevalence from Waves 1, 2, and 4 is not comparable to prevalence from Waves 5 and 6. Therefore, the analysis is divided into two periods. The first examines trends across the earlier period (Waves 1, 2, and 4 or between years 2004 and 2011) and the second across the later period (Waves 5 and 6 or between years 2013 and 2015). For the earlier period, individuals are coded as having pain if they responded affirmatively to the question about site-specific pain. For the later period, individuals are coded as having pain if they responded in the affirmative to the global question about being troubled by pain. Because the questions do not reference a length of time during which pain has been experienced, the measures account for the combination of acute and chronic pain. For the earlier period, 53.9% of weighted respondents reported pain; for the later period, it is 45.1%.
Modeling Trends in Pain
To model trends, we construct a variable called “time.” This variable is centered on the midpoint year of the period. For the earlier period, we subtract 2007.5, the midpoint between the earliest and latest survey years, from the year of the observation. For instance, the time for observations taken in 2004 is −3.5 and in 2011 is +3.5. For the second period, 2012 is the midpoint and is subtracted from the year of observation. Measured in this way, time represents the annual change in prevalence and can be interpreted as a trend.
Our selection of covariates derives from two considerations. First, we draw upon a social determinants of pain framework (Craig & Fashler, 2013), which recognize that the reporting of pain is a function of three types of factors: distal, such as socioeconomic and demographic characteristics that shape exposure; intermediate, such as psychological characteristics that moderate the impact of health conditions; and proximate, such as pain-producing chronic conditions that are direct causes of pain. Next, we examined previous literature on population level on pain prevalence and chose factors that concur with a social determinant framework and have been shown in the past to be predictors of pain (Blyth, 2010; Institute of Medicine, 2012). Besides time, our models include age in years, sex, whether the respondent lives with a spouse or partner (Fillingim et al., 2009; Flor et al., 1989; Rubin & Zimmer, 2015; Wade et al., 2013), education (Dionne et al., 2001; Grol-Prokopczyk, 2017; Riskowski, 2014), six major self-reported chronic physical conditions (arthritis, heart disease, diabetes, lung disease, cancer, and stroke), risk of depression (Currie & Wang, 2005; Tsang et al., 2008), and obesity (Deyo & Bass, 1989; McCarthy et al., 2009; Shiri et al., 2010).
While the link between arthritis and pain is particularly strong, all of the chronic conditions, including those that are physical and psychological in nature, have been found to have independent influences on pain (Hooten, 2016; Janevic et al., 2017; Kennedy et al., 2014; Nahin, 2015). Note that while there is clearly a bidirectional association between chronic pain and mental health, there is a wide body of research showing that depression predicts chronic pain, partly due to shared neural mechanisms and partly through mediating behaviors such as smoking and alcohol use (Gatchel et al., 2007; Goosby, 2013; Gureje et al., 2008; Hooten, 2016; Janevic et al., 2017; Van Hecke et al., 2013). Each chronic condition and risk of depression is measured dichotomously. Obesity is based on self-reported height and weight and is defined as a BMI of 30+. Education is based on the ISCED standardized scale (UNESCO Institute for Statistics, 2012). For this study, we recode the scale into three groups and treat education as a categorical variable as follows: Education Level 1 (comparison category)—no more than lower secondary or second stage education; Education Level 2—upper secondary; and Education Level 3—higher than upper secondary. The risk of clinical depression is defined as having a score of 4+ on the Euro-D, a scale of mental health (Castro-Costa et al., 2007).
Descriptive statistics are shown by wave/year in Table 2. The table also shows whether means or percentages statistically differ across any two consecutive waves. Some of the covariates change in a way that could be expected to be associated with higher pain prevalence. For instance, there are increases in the percent of respondents with arthritis. But there are also decreases in cancer and increases in education, both of which might be expected to predict lower pain prevalence.
Table 2.
Descriptive Statistics for Covariates: Weighted Means and Percent Distributions, by Wave/Survey Year.1
| Wave 1 (2004) | Wave 2 (2005/6) | Wave 4 (2011) | Wave 5 (2013) | Wave 6 (2015) | |
|---|---|---|---|---|---|
|
| |||||
| Mean age (years) | 65.5 | 65.8** | 66.3** | 66.4 | 66.6 |
| % Female | 54.3 | 54.4 | 54.2 | 54.5 | 54.3 |
| % Married | 64.6 | 64.6 | 64.9 | 62.3** | 61.9 |
| % Education level 1 | 51.6** | 47.8** | 42.5** | 38.9** | 37.1** |
| % Education level 2 | 27.4 | 30.6** | 34.0** | 34.5 | 35.3* |
| % Education level 3 | 21.1 | 21.6 | 23.5** | 26.5** | 27.6** |
| % Arthritis | 20.0 | 21.9** | 23.3** | 24.7** | 24.3 |
| % Heart disease | 15.1 | 15.7‡ | 14.5** | 11.2** | 10.3** |
| % Diabetes | 9.7 | 10.6** | 11.9** | 12.3 | 12.4 |
| % Lung disease | 5.5 | 5.5 | 6.3** | 6.0* | 6.1 |
| % Cancer | 5.9 | 4.1** | 5.0** | 5.3* | 4.2** |
| % Stroke | 4.0 | 3.8 | 3.8 | 4.0 | 3.4** |
| % Obese | 16.2 | 18.1** | 18.7* | 20.5** | 21.6** |
| % Depressed | 25.7 | 26.0 | 26.9* | 27.0 | 26.1* |
Note.
p < .01
.05 < p < .10
.01 < p < .05.
Significance tests are for differences between any two consecutive waves (Wave 2 vs. 1, Wave 4 vs. 2, Wave 5 vs. 4, and Wave 6 vs. 5).
Statistical Analysis
Estimates incorporate SHARE observational weights, which make results generalizable to within-country populations aged 50+, and SHARE’S complex multistage survey design. As noted, due to changes in the survey instrument, we divide the data into an earlier and later period and conduct separate analyses for each. We begin with descriptive analyses that show country-by-country weighted pain prevalence for the total population aged 50+ and separately by sex for three broad age-groups (50–59, 60–69, and 70 and older). Prevalence is defined as the percentage reporting pain, regardless of the specific measure of pain being used in any particular wave. For the descriptive analyses of the earlier time period, we pool data from Waves 1 and 2 and compare the pooled Wave 1/2 prevalence to prevalence in Wave 4; analyses of the later time period compare prevalence in Waves 5 and 6.
Next, we present multivariate models assessing the pain trends, that is, evaluating the association of “time” with pain prevalence. Results are presented two ways. First, we test a series of multilevel logistic regression models that pool data across countries (Raudenbush & Bryk, 2002). Second, we use data from individual countries and examine the effect of time in each.
The multilevel models provide coefficients for time with the assumption that there is unmeasured heterogeneity in country-specific prevalence and in the country-specific effect of time. This assumption is satisfied by providing coefficients for time, the variation in prevalence across countries, and the variation in the effect of time across countries. This can be specified in two equations labeled Level 1 (the individual level) and Level 2 (the country level)
The Level 1 equation indicates that the probability that person in country reports pain is a function of a grand intercept reflecting overall prevalence, a fixed effect that time has on person , a set of fixed-effect covariates , and an error term . The Level 2 equation indicates the grand intercept is a function of an overarching intercept which varies across countries according to which is a random effect, and is the difference between the overall prevalence and prevalence within individual countries. The effect of time is considered to also vary across countries. It is equal to the average effect of time plus the idiosyncratic effect of time in each country . We do not assume that the prevalence of pain or the effect of time on this prevalence is the same in each country, and we report on a trend with the condition that prevalence and effect of time differ in ways that cannot be explained by fixed effects. We fit seven multilevel models. Each includes the variable time plus a combination of covariates. A base model begins with time, age, and sex. Other models add specific covariates (marriage, education, chronic conditions, obesity, or risk of depression). The final model adds all covariates simultaneously as a full model. Results presented are the log odds and significance levels. Complete results including standard errors, z-values, p-values, and confidence intervals are provided in Supplementary Materials.
In the next procedure, country-by-country logistic regression models show the log odds associated with a one-year change in time on the probability of reporting pain in each country. The coefficients based on baseline and full models (controlling for age and sex, and for all covariates, respectively) are presented herein as figures. Complete findings from these models are provided in the Supplementary Materials.
We conducted sensitivity tests. We tested quadratic terms for time, but they were not significant, indicating trends in pain are better modeled linearly. We constructed dummy variables for countries and entered these into fixed-effect models. The difference between the fixed only and random effect treatments was minimal, but the random effect model is preferred since it provides more robust statistical tests when prevalence is dependent on country (Hox et al., 2018). Also, the multilevel treatment is supported by standard tests for assessing validity such as Hausman tests and interclass correlation. We treated time categorically, creating dummy variables for wave in which the SHARE survey was completed. This treatment of time was either not statistically different or statistically inferior to a linearized treatment of time based on log-likelihood tests. To assess if repeated observations affect results, we ran models only using observations that were responding to their first SHARE questionnaire. This sensitivity test did not alter the nature of the findings reported herein. Finally, rather than treating each chronic condition as a separate measure, we created indices for any and number of chronic conditions. These models were found to provide similar findings, but the explanatory powers were somewhat lower based on log-likelihood tests.
Coefficients are presented as log-odds, so exponentiation provides odds ratios of reporting pain for each unit increase in a predictor variable. Log-odds are preferred for trend models since they center on zero, and, therefore, a positive coefficient is interpreted as an increasing trend in prevalence and a negative coefficient as a decreasing trend.
Results
Unadjusted Trends in Pain Prevalence
Table 3 compares pooled Wave 1/2 prevalence with Wave 4 for individual countries, for the total population, and by age and sex. For each comparison, there is an indication of whether differences across waves are statistically significant Standard errors are provided in Supplementary Materials. There is substantial variation in pain prevalence across European countries, as has been shown in other studies (Achterberg et al., 2010; Breivik et al., 2006; Cimas et al., 2018; Farioli et al., 2014). In Wave 1/2, prevalence ranged from a low of 40.7% in the Netherlands to a high of 56.2% in Italy. In Wave 4, the range was from 42.6% in the Netherlands to 65.7% in Germany. Overall, pain prevalence increased substantially and significantly at p < .05, or nearing this significance level, in half of the 12 countries [Belgium (53.2–60.4; p < .01), France (54.7–62.0; p < .01), Germany (54.4–65.7; p < .01), the Netherlands (40.7–42.6; p < .10), Spain (52.4–56.3; p < .01), and Switzerland (42.3–45.9; p < .01)]. The change in the other countries was positive but nonsignificant, with the exception of Italy, which was the only country to experience a (nonsignificant) decline in prevalence.
Table 3.
Weighted Percentage Reporting Pain in Wave 1/2 (2004/5 and/or 2006/7) versus Wave 4 (2011) by Country, Age, and Sex, Showing Statistical Significance of Change across Waves.
| AUS |
BEL |
CZE |
DEN |
|||||
|---|---|---|---|---|---|---|---|---|
| Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | Wave 1/2 | Wave 1/2 | Wave 1/2 | Wave 4 | |
|
| ||||||||
| Total | 53.2 | 53.4 | 53.2 | 60.4** | 47.5 | 47.5 | 47.5 | 48.8 |
| Men (years) | ||||||||
| 50–59 | 52.6 | 48.2 | 49.5 | 56.5** | 48.3 | 48.3 | 48.3 | 45.9 |
| 60–69 | 47.9 | 58.0 | 47.1 | 55.8** | 41.8 | 41.8 | 41.8 | 46.6 |
| 70+ | 46.3 | 54.3** | 45.7 | 52.7** | 43.8 | 43.8 | 43.8 | 44.7 |
| Women (years) | ||||||||
| 50–59 | 52.9 | 50.0 | 52.8 | 62.1** | 50.0 | 50.0 | 50.0 | 51.7 |
| 60–69 | 56.2 | 53.6 | 55.5 | 63.3** | 49.0 | 49.0 | 49.0 | 47.8 |
| 70+ | 59.2 | 62.4 | 63.5 | 68.2** | 50.1 | 50.1 | 50.1 | 54.8 |
|
| ||||||||
| FRA |
GER |
ITA |
NET |
|||||
| Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | |
|
| ||||||||
| Total | 54.7 | 62.0** | 54.4 | 65.7** | 56.2 | 54.6 | 40.7 | 42.6* |
| Men (years) | ||||||||
| 50–59 | 50.5 | 61.3** | 46.8 | 62.3** | 42.2 | 34.6** | 37.2 | 38.5 |
| 60–69 | 48.4 | 56.4** | 50.5 | 65.9** | 49.1 | 46.8 | 35.3 | 38.0 |
| 70+ | 53.7 | 60.1** | 47.4 | 56.7 | 51.3 | 53.5 | 31.4 | 35.4 |
| Women (years) | ||||||||
| 50–59 | 54.1 | 58.8** | 51.4 | 68.3** | 53.0 | 42.1** | 41.5 | 45.4 |
| 60–69 | 56.5 | 63.7** | 53.2 | 68.7** | 61.6 | 63.1 | 45.9 | 45.7 |
| 70+ | 61.8 | 68.6** | 64.3 | 70.1* | 71.7 | 75.1‡ | 49.5 | 50.1 |
|
| ||||||||
| POL |
SPA |
SWE |
SWI |
|||||
| Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | Wave 1/2 | Wave 4 | |
|
| ||||||||
| Total | 47.7 | 53.5 | 52.4 | 56.3** | 51.6 | 53.0 | 42.3 | 45.9** |
| Men (years) | ||||||||
| 50–59 | 51.4 | 53.8 | 34.4 | 36.3 | 44.0 | 52.9** | 38.1 | 36.5 |
| 60–69 | 61.9 | 59.7 | 42.7 | 41.4 | 47.2 | 47.6 | 38.1 | 45.4* |
| 70+ | 54.7 | 52.1 | 47.8 | 51.8 | 46.0 | 48.7 | 40.1 | 45.1 |
| Women (years) | ||||||||
| 50–59 | 64.7 | 63.2 | 51.4 | 56.5‡ | 54.9 | 58.6 | 40.5 | 44.4 |
| 60–69 | 75.5 | 72.5 | 62.9 | 64.9 | 55.7 | 53.7 | 46.2 | 48.6 |
| 70+ | 59.4 | 59.8 | 68.3 | 76.7** | 59.4 | 56.9 | 49.2 | 53.7 |
Note.
p < .01
.01 < p < .05
.05 < p < .10.
Table 4 shows the change in pain prevalence from Wave 5 to Wave 6 for individual countries. Wave 5 prevalence ranged from a low of 27.1 in Switzerland to a high of 56.9 in France. For Wave 6, the range was from 29.6 to 55.7 in the same two countries. Six countries experienced increases that are significant or nearing significance (Belgium, the Czech Republic, Denmark, Estonia, Slovenia, and Switzerland). Italy experienced a significant decline.
Table 4.
Percentage Reporting Pain in Wave 5 (2013) versus Wave 6 (2015) by Country, Age, and Sex, Showing Statistical Significance of Change across Waves.
| AUS |
BEL |
CZE |
DEN |
|||||
|---|---|---|---|---|---|---|---|---|
| Wave 5 | Wave 6 | Wave 5 | Wave 6 | Wave 5 | Wave 6 | Wave 5 | Wave 6 | |
|
| ||||||||
| Total | 29.6 | 31.4 | 41.1 | 46.0** | 45.1 | 52.3** | 31.3 | 33.1* |
| Men (years) | ||||||||
| 50–59 | 28.9 | 30.2 | 34.8 | 42.7* | 31.8 | 54.2* | 25.3 | 29.5* |
| 60–69 | 34.0 | 33.7 | 35.1 | 39.7‡ | 40.7 | 46.2 | 25.7 | 30.8‡ |
| 70+ | 31.0 | 33.4 | 34.8 | 34.8 | 47.1 | 50.3* | 26.6 | 25.7 |
| Women (years) | ||||||||
| 50–59 | 32.3 | 37.3‡ | 43.8 | 52.3** | 39.6 | 45.0* | 35.3 | 38.2 |
| 60–69 | 47.7 | 50.8 | 44.7 | 48.5 | 47.5 | 52.4 | 35.5 | 36.4 |
| 70+ | 29.6 | 31.4 | 49.8 | 54.1* | 61.8 | 62.7** | 37.5 | 37.0 |
|
| ||||||||
| EST |
FRA |
GER |
ITA |
|||||
| Wave 5 | Wave 6 | Wave 5 | Wave 6 | Wave 5 | Wave 6 | Wave 5 | Wave 6 | |
|
| ||||||||
| Total | 49.6 | 54.2** | 56.9 | 55.7 | 39.5 | 38.5 | 54.1 | 51.7* |
| Men (years) | ||||||||
| 50–59 | 45.0 | 45.9 | 52.7 | 45.3** | 34.6 | 34.5 | 33.8 | 29.3‡ |
| 60–69 | 47.5 | 49.3 | 44.2 | 48.1 | 32.1 | 33.7 | 40.0 | 38.0 |
| 70+ | 49.2 | 54.3‡ | 58.4 | 54.5 | 33.6 | 31.9 | 53.5 | 54.2 |
| Women (years) | ||||||||
| 50–59 | 45.3 | 50.9** | 52.8 | 52.8 | 38.6 | 42.4 | 46.6 | 42.2‡ |
| 60–69 | 49.9 | 56.8** | 58.9 | 61.0 | 41.0 | 38.0 | 61.9 | 60.0 |
| 70+ | 56.1 | 62.6** | 69.0 | 67.7 | 51.0 | 46.7* | 75.5 | 73.7 |
|
| ||||||||
| LUX |
SLO |
SPA |
SWE |
|||||
| Wave 5 | Wave 6 | Wave 5 | Wave 6 | Wave 5 | Wave 6 | Wave 5 | Wave 6 | |
|
| ||||||||
| Total | 43.5 | 44.6 | 49.8 | 52.8* | 50.6 | 50.7 | 37.8 | 37.0 |
| Men (years) | ||||||||
| 50–59 | 40.3 | 33.8‡ | 30.6 | 39.6** | 31.1 | 30.5 | 31.1 | 27.5 |
| 60–69 | 36.1 | 34.1 | 40.4 | 45.2 | 38.5 | 37.3 | 29.9 | 29.0 |
| 70+ | 36.0 | 37.0 | 54.0 | 56.2 | 47.0 | 48.8 | 28.7 | 30.2 |
| Women (years) | ||||||||
| 50–59 | 46.9 | 52.2 | 52.5 | 49.4 | 43.3 | 45.8 | 41.9 | 40.1 |
| 60–69 | 49.6 | 53.8 | 52.7 | 54.4 | 60.5 | 56.6 | 42.1 | 44.2 |
| 70+ | 49.5 | 54.7 | 64.9 | 68.2 | 74.0 | 75.7 | 49.4 | 47.1 |
|
| ||||||||
| SWI | ||||||||
|
|
||||||||
| Wave 5 | Wave 6 | Wave 5 | Wave 6 | |||||
|
| ||||||||
| Total | 27.1 | 29.6* | ||||||
| Men (years) | Women (years) | |||||||
| 50–59 | 20.7 | 24.7 | 50–59 | 27.9 | 27.5 | |||
| 60–69 | 20.0 | 23.7 | 60–69 | 25.8 | 34.3** | |||
| 70+ | 25.8 | 26.9 | 70+ | 38.7 | 37.7 | |||
Note.
p < .01
.01 < p < .05
.05 < p < .10.
Tables 3 and 4 also show that pain prevalence increases were consistent across sex and age-groups in countries where overall prevalence increased. For instance, comparing Waves 1/2 with 4, all age-/sex groups experienced increasing prevalence in Belgium, France, Germany, and the Netherlands, and most of these within–age-/sex group comparisons are statistically significant. In countries with no significant total rise in prevalence, there was nevertheless an increase among some age/sex subgroups. For instance, in Sweden, comparing Waves 1/2 with Wave 4, there was a large increase in prevalence for men aged 50–59 (44.0–52.9; p < .01). There was also a decline in prevalence among a few subgroups. In Table 4, prevalence dropped considerably for women aged 70+ in Germany (51.0–46.7; p < .01), for men aged 50–59 in Luxembourg (40.3–33.8; p < .10), and among men aged 50–59 in France (52.7–45.3; p < .01).
Multilevel Models
The base model in Table 5 (Model 1) demonstrates that, net of age and sex, time is associated with a statistically significant increase in the log-odds of reporting pain (β = .022; p < .01). Across countries, the odds of reporting pain increased on average by a factor of 1.022 or 2.2% per year between 2004 and 2011. Models 2 through 7 indicate that the upward trend remains statistically significant and roughly similar in size net of controls. Model 7 indicates that after adjusting for all covariates, the log-odds of an individual reporting pain increased by .022 per year (just as in Model 1). Supplementary Materials show standard errors and 95% confidence intervals for the time coefficient and provide evidence of no statistical difference in the coefficients across models.
Table 5.
Multilevel Logistic Regression Models for Effect of Time (One Year) on the Log Odds of Reporting Pain in 12 European Countries from Wave 1 (2004) through Wave 4 (2011) (N = 95,455).
| Model (Base) | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 (Full) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time | .022** | .022** | .025** | .020** | .021** | .023** | .022** |
| Age | .015** | .014** | .012** | .001 | .015** | .012** | −.000 |
| Female | .386** | .377** | .364** | .245** | .389** | .288** | .166** |
| Married | −.051* | .036‡ | |||||
| Education level 2 (vs. 1) | −.143** | −.057 | |||||
| Education level 3 (vs. 1) | −.354** | −.219** | |||||
| Arthritis | 2.087** | 2.018** | |||||
| Heart disease | .348** | .256** | |||||
| Diabetes | .266** | .143** | |||||
| Lung disease | .374** | .281** | |||||
| Cancer | .034 | −.013 | |||||
| Stroke | .169** | .075 | |||||
| Obesity | .523** | .369** | |||||
| Depression | .779** | .582** | |||||
| Constant | −1.029 | −.959 | −.714 | −.513 | −1.169 | −1.014 | −.525 |
| Variance (Intercept) | .060** | .059** | .057** | .060** | .054** | .049* | .063** |
| Variance (slope) | .00044** | .00043** | .00044** | .00056** | .00045** | .00040** | .00056** |
| Pseudo-log-likelihood | 64,354.7 | 64,348.5 | 64,168.0 | 58,042.6 | 63,249.4 | 61,614.7 | 55,273.3 |
| Δ-2LL1 | 12.4** | 373.4** | 12,624.2 | 2210.6** | 5480.0** | 18,162.8** | |
Note.
p < .01
.01 < p < .05
.05 < p < .10. Supplementary Materials contain complete results including standard errors, z-value, p-values, and CIs.
Likelihood-ratio test compared with base model.
Control variables display the expected associations. Age is positively associated with pain, although this association disappears in models controlling for chronic conditions. Being female predicts higher odds. Being married and having higher education reduce the likelihood of reporting pain. Each of the six chronic diseases, with the exception of cancer, increases the likelihood, as do obesity and risk of depression. Among the six conditions, arthritis is, as expected, particularly prominent as a predictor of pain.
The multilevel models in Table 6 indicate that the trend of increasing pain prevalence across Europe continued between 2013 and 2015. When moving from the base to the full model, the coefficient representing the effect of time gets larger (β = .036; p < .05 to β = .060; and p < .01), suggesting that once we take into account the changing distribution of covariates known to influence pain, the trends become steeper. In particular, addition of chronic conditions such as heart disease and stroke to the model increases the trend, indicating that the trend would have risen more had there not been some decline in these chronic conditions between 2013 and 2015. Standard errors and 95% confidence intervals provided in Supplementary Materials indicate changes in the magnitude of the time coefficient across models are, however, not statistically significant. Exponentiation of the result from full Model 7 indicates that Europeans aged 50+ experienced an annual increase in the odds of reporting pain between 2013 and 2015 of 1.06% or 5.8% (even larger than what was found for the earlier time period). Results for covariates are consistent with those shown for the earlier period.
Table 6.
Multicountry Logistic Regression Models for Effect of Time (One Year) on the Log-Odds of Reporting Pain In 13 European Countries from Wave 5 (2013) to Wave 6 (2015), including Country Random Effects (N = 112,246).
| Model 1 (Base) | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 (Full) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time | .036** | .036** | .042** | .056** | .034* | .040* | .059** |
| Age | .021** | .020** | .016** | .005 | .021** | .017** | .001 |
| Female | .485** | .472** | .466** | .366** | .489** | .369** | .251** |
| Married | −.077* | .005 | |||||
| Education level 2 (vs. 1) | −.279** | −.189** | |||||
| Education level 3 (vs. 1) | −.565** | −.391** | |||||
| Arthritis | 1.811** | 1.754** | |||||
| Heart disease | .449** | .329** | |||||
| Diabetes | .448** | .299** | |||||
| Lung disease | .518** | .371** | |||||
| Cancer | .364** | .276** | |||||
| Stroke | .437** | .281** | |||||
| Obesity | .579** | .384** | |||||
| Depression | 1.090** | .915** | |||||
| Constant | −1.880 | −1.786 | −1.325 | −1.374 | −2.070 | −1.878 | −1.154 |
| Variance (Intercept) | .128** | .129** | .101** | .156** | .122** | .100** | .110** |
| Variance (slope) | .0028** | .0028** | .0029** | .0038‡ | .0026** | .0035** | .0046** |
| Pseudo-log-likelihood | 74,224.0 | 74,207.3 | 73,676.7 | 66,444.5 | 73,354.0 | 68,780.3 | 61,676.6 |
| Δ-2 LL1 | 33.4** | 1094.6** | 15,594.0 | 1740.0** | 10887.4** | 25,094.8** | |
Note.
p < .01
.01 < p < .05
.05 < p < .10. Supplementary Materials contain complete results including standard errors, z-value, p-values, and CIs.
Likelihood-ratio test compared with base model.
In both tables, the random coefficients indicate that variation exists across countries in the intercept. This means that the overall level of pain varies significantly by country. In addition, the random slope effect is significant, and so there is significant variation in the effect of time across countries.
Country-Specific Models
Given significant random effects across countries, a country-by-country analysis helps to understand how trends vary for each specific country. Figure 1 presents the effect of time on country-specific log-odds of reporting pain between 2004 and 2011. Complete model findings are shown in Supplementary Materials. Results are presented for two models: the base and the full. Looking for instance at the lull model findings, the majority of countries experience rising pain prevalence. Adjusting for all covariates, a significant positive association is found in Belgium, Denmark, France, Germany, and the Netherlands. Relatively robust positive associations that are near significance are found in Poland, Spain, and Sweden. No specific direction is detected in the trends in Austria, the Czech Republic, Italy, and Switzerland.
Figure 1.
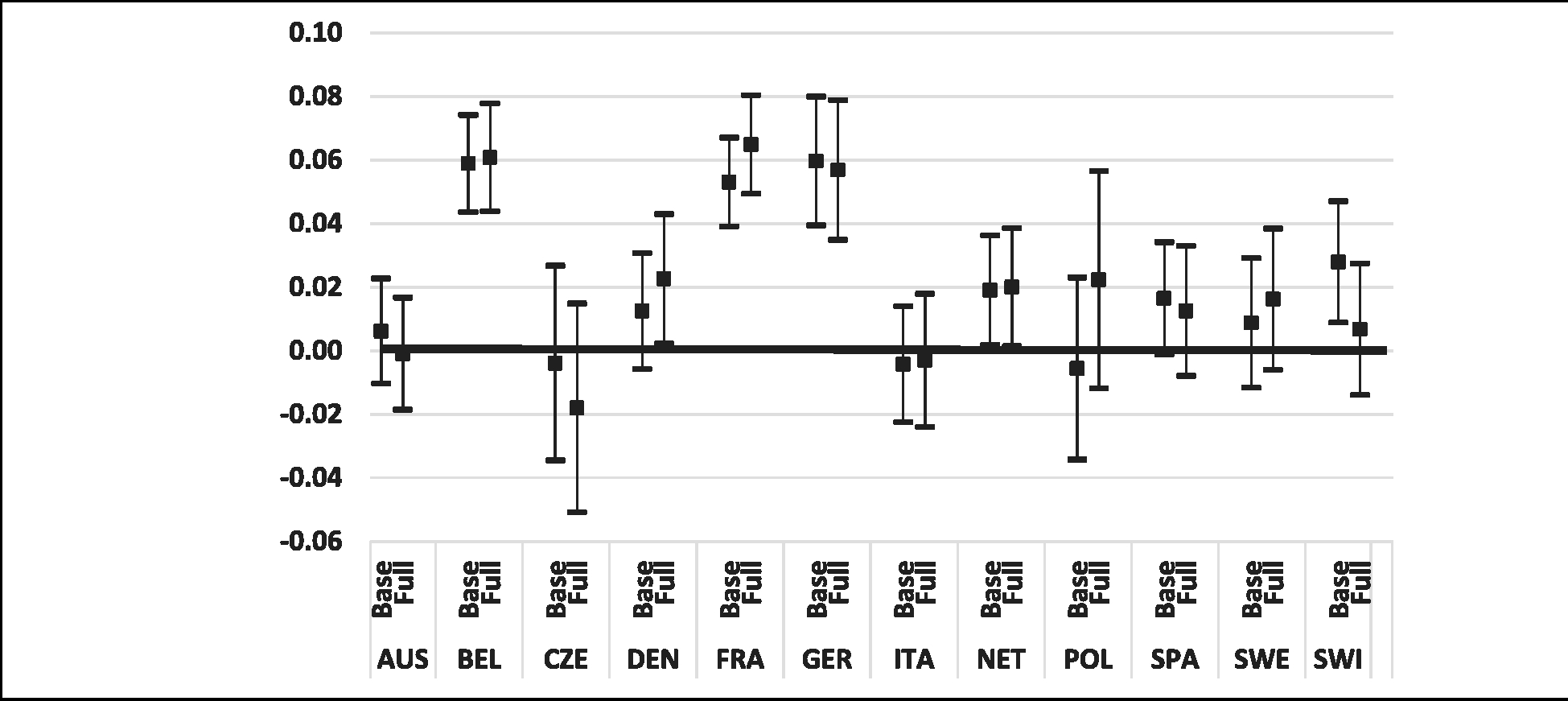
Country-specific point estimates and 95% confidence intervals for the effect of one year of time on the log-odds of reporting pain across Waves 1, 2, and 4.
Note. Data from Survey of Health and Retirement in Europe, 2004–2011, ages 50+, for models predicting pain as a function of time, from the base model that adjusts for age and sex, and the full model that adjusts for age, sex, marital status, education, six chronic conditions, obesity, and depression.
Country-specific findings for the later period are displayed in Figure 2. Again, referring to the full model results, positive and statistically significant country-specific associations are found in the Czech Republic, Denmark, Estonia, Luxembourg, and Switzerland. Results near significance and suggestive of a positive trend are found in Belgium, Slovenia and Sweden. Negative but nonsignificant associations appear in France and Germany. Associations in Austria, Italy, and Spain are nonsignificant and do not suggest any direction of change. Note that because relative annual changes in prevalence are greater in the later period, there is a scale difference in the presentation of results in Figures 1 and 2.
Figure 2.
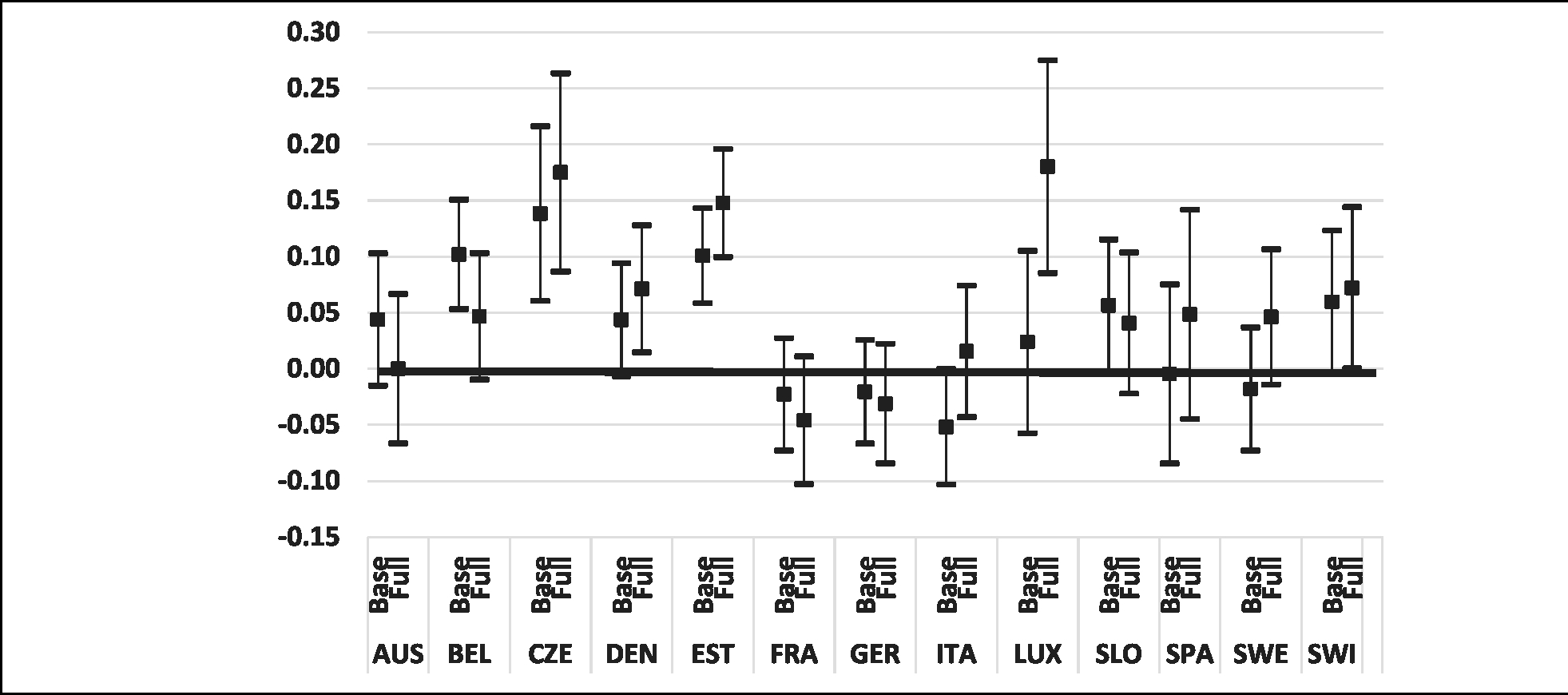
Country-specific point estimates and 95% confidence intervals for the effect of one year of time on the log-odds of reporting pain across Waves 5 and 6.
Note. Data from the Survey of Health and Retirement in Europe, 2013–2015, ages 50+, for models predicting pain as a function of time, from the base model that adjusts for age and sex, and the full model that adjusts for age, sex, marital status, education, six chronic conditions, obesity, and depression.
Discussion
We examined trends in the prevalence of pain in 15 European countries among those aged 50+ from 2004 to 2015. The population 50 and older is growing rapidly in Europe, as it is in most of the world. Moreover, life expectancy has been rising, and those that reach age 50 can expect to live increasingly long lives. The combination of population aging and rising longevity raises critical questions regarding whether these demographic changes are accompanied by improvements or deteriorations in health (Crimmins & Beltrán-Sánchez, 2011; Jagger, 2006). This question has been addressed frequently by referencing trends in disability and other physical functioning outcomes (Freedman, 2018; Martin et al., 2010). In contrast, there have been very few such studies that have considered pain prevalence, despite pain’s inextricable links to physical Sanctioning and disability (not to mention pain’s links to other aspects of well-being such as mental health). The current investigation therefore fills a high-priority gap.
Due to changes in how SHARE measured pain, this study examined trends separately in two periods: 2004–2011 and 2013–2015. Between 2004 and 2011, the relative increase in the odds of reporting pain is 2.2% in each year across 12 observed countries. Between 2013 and 2015, the relative increase in the odds was even greater, 5.8% across 13 observed countries. Thus, although specific countries and measures differed between the earlier and later periods, our study suggests an accelerating trend. All increases were adjusted for age; thus, increases in pain prevalence were not simply reflections of population aging but indications of declining health net of age.
At the same time, there is variation across countries. We took this into account by not mechanically pooling countries but instead estimating multilevel and country-specific models. The former indicated a significant random effect of time, which suggests significant unobserved heterogeneity exists in trends across countries. Country-specific regressions showed that despite this heterogeneity, most countries, but not all, witnessed increases in prevalence over time. Summarizing trends in prevalence based on country-specific results, 9 of 15 countries (Belgium, the Czech Republic, Denmark, Estonia, France, Germany, Luxembourg, the Netherlands, and Switzerland) showed a statistically significant increase in either the earlier or later period based on fully adjusted models. No country experienced a statistically significant decrease in either period in the fully adjusted model.
Our conclusion, based on the combination of multilevel and country-specific regressions, is that among adults aged 50+ in 15 European countries, there was a general increase in pain prevalence of relatively large magnitude between 2004 and 2015. There are some studies of pain trends using data from individual European countries or from the United States that report opposing findings, although these tend to rely on smaller and/or geographically limited samples (Deyo et al., 2006; Freburger et al., 2009; Heistaro et al., 1998; Hüppe et al., 2007; Shen et al., 2015). The current study is more in line with recent large-scale population-level studies in North America. Nahin and colleagues (Nahin et al., 2019) examined data from the U.S. medical expenditure panel survey over 18 years and reported considerable increases in the number and percent reporting pain. Using data from the well-recognized Health and Retirement Study, Zimmer & Zajacova (2018) reported increases in chronic pain prevalence among Americans aged 55 and older in the order of about 2% per year between 1992 and 2014. Shupler et al. (2019), using Canadian Community Health Survey data, identified significant increases in pain prevalence across all Canadian provinces, among all age-groups, among both men and women, across socioeconomic characteristics, and among those without any reported chronic health conditions. When paired with these prior studies, our current findings raise the possibility of a more global trend of rising pain prevalence.
This is the first study to report on the general trend in pain across Europe, and it is beyond the study’s scope to attempt to understand or explain specific trends in each country. No doubt variations in social, economic, and political contexts may be relevant. It is puzzling, however, that in the current study, temporal trends changed minimally even after we controlled for other characteristics, such as chronic diseases and obesity. The way in which pain is reported across cohorts is one possible explanation (Ahacic & Kåreholt, 2010; Grol-Prokopczyk, 2017; Shupler et al., 2019). This could occur if there has been an increased openness to reporting pain, reflecting a societal shift in how pain is interpreted, diagnosed, and treated. While this possibility needs to be examined more carefully in future studies, so do other mechanisms that also might explain the increases in prevalence. Among these, we suggest changes in the severity of chronic conditions and the degree to which specific conditions lead to pain symptoms, changes in physical activity, and a host of psychosocial factors, such as social support, locus of control, and psychological health that we were unable to control for in the current study. Moreover, the connection between opioid use and pain prevalence, while complicated, should be explored. Increases in pain prevalence suggest intriguing questions regarding the extent to which increases in pain are responsible for or are a consequence of rising availability of opioids in some settings (Chu et al., 2008; Morasco et al., 2017).
Also puzzling is the degree to which studies documenting robust national-level increases in pain prevalence are diverging from studies that have been monitoring trends in physical functioning and disability. For instance, using SHARE data, Verropoulou and Tsimbos (2017) found improvements in mild and moderate activity restriction and functional limitation across a number of European countries and some minor declines in more severe activities of daily living. Studies in the United States, for some time now, have been indicating overall improvements in disability within some, although not all, age-groups. Crimmins et al. (2016) recently reported relatively large long-term gains in disability-free life expectancy, while Martin and Schoeni (2014) reported on decreases in functional limitation among Americans 65 and older. Indeed, there are reasons trends in pain and trends in disability may diverge. For instance, disability is a function of both physical ability and the environmental circumstance in which functional tasks are conducted (Verbrugge & Jette, 1994). If the environment and accommodations within are improved, for instance, if personal support improves or devices that help to complete activities are enhanced, one might see pain levels increase without a concomitant change in disability. Furthermore, pain and disability, although clearly related, are functions of a different set of mechanisms. Pain is highly subjective but tied closely to certain types of pathological conditions, such as arthritis. Disability may be a function of a different set of conditions that can include both mental and physical dysfunction. There are other possible explanations for this divergence, which underscores the need to further examine the causal connections between pain and disability, whether the link has been weakening over time, and the mechanisms through which pain translates into disability.
There are limitations to the current study. SHARE does not collect data on pain severity, duration, or specific cause, which limits our ability to explore the nature of our trends and potentially clarify the causes. The change in SHARE’S measurement of pain limits the ability to draw firm conclusions across the entire time period. A number of European countries that are part of SHARE were not included in the current study because they did not contain data across enough waves for temporal comparison. Future waves of SHARE data will enable assessment of the described trends across a broader range of countries and will help to verify if the accelerating trend found across the earlier and later time periods in the current study is genuine. Variation in pain trends across countries is difficult to explain without additional detailed analysis. Future research should assess the role of national-level predictors such as differences in work disability and healthcare policies. Such analyses are likely to be particularly valuable with longer term data collection. Future studies should consider additional covariates like other chronic disorders and sociodemographic characteristics in an attempt to better understand the factors driving increases in pain prevalence.
In sum, this study has expanded our understanding of trends in pain prevalence among those 50 and older across a number of European countries. Pain is common and has high societal costs, including loss of productivity, increases in disability and healthcare utilization, and reductions in quality of life. Yet, there have been very few examinations of trends in pain prevalence, especially in Europe. While there are well-recognized challenges of combining survey responses from multiple countries, including unexplained variation across countries, the findings here are sufficiently robust to suggest that older Europeans have generally experienced rising pain prevalence that may be accelerating and not explained by population aging alone.
Supplementary Material
Authors’ Note
The lead author acknowledges funding from the Social Sciences and Humanities Research Council of Canada and their Canada Research Chairs program.
This study uses data from SHARE Waves 1, 2, 4, 5, and 6 (DOIs 10.6103/SHARE.wl .611, 10.6103/SHARE.w2.611, 10.6103/SHARE.w4.611, 10.6103/SHARE.w5.611, 10.6103/SHARE.w6.611), see Börsch-Supan et al. (2013) for methodological details. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-13: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARETJFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: No. 211909, SHARE-LEAP: No. 227822, SHARE M4: No. 261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Yl-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071Q, and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Social Sciences and Humanities Research Council of Canada (Canada Research Chairs Program).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- Achterberg WP, Gambassi G, Finne-Soveri H, Liperoti R, Noro A, Frijters DHM, Cherubini A, Dell’Aquila G, & Ribbe MW (2010). Pain in European long-term care facilities: Cross-national study in Finland, Italy and the Netherlands. Pain, 148(1), 70–74. [DOI] [PubMed] [Google Scholar]
- Ahacic K, & Kåreholt I (2010). Prevalence of musculoskeletal pain in the general Swedish population from 1968 to 2002: Age, period, and cohort patterns. Pain, 151(1), 206–214. [DOI] [PubMed] [Google Scholar]
- Anderson KO, Green CR, & Payne R (2009). Racial and ethnic disparities in pain: Causes and consequences of unequal care. The Journal of Pain, 10(12), 1187–1204. [DOI] [PubMed] [Google Scholar]
- Andersson HI, Ejlertsson G, Leden I, & Rosenberg C (1993). Chronic pain in a geographically defined general population. The Clinical Journal of Pain, 9(3), 174–182. [DOI] [PubMed] [Google Scholar]
- Andrews JS, Cenzer IS, Yelin E, & Covinsky KE (2013). Pain as a risk factor for disability or death. Journal of the American Geriatrics Society, 61(4), 583–589. doi: 10.1111/jgs.12172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blyth FM (2010). The demography of chronic pain: An overview. In Croft P, Blyth FM, & Van der Windt D (Eds.), Chronic Pain Epidemiology From Aetiology to Public Health (pp. 19–29). Oxford University Press. [Google Scholar]
- Blyth FM, & Schneider CH (2018). Global burden of pain and global pain policy-creating a purposeful body of evidence. Pain, 159, S43–S48. [DOI] [PubMed] [Google Scholar]
- Börsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, Schaan B, Stuck S, & Zuber S 2013). Data resource profile: The survey of health, ageing and retirement in europe (SHARE). International Journal of Epidemiology, 42(4), 992–1001. doi: 10.1093/ije/dyt088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breivik H, Collett B, Ventafridda V, Cohen R, & Gallacher D (2006). Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. European Journal of Pain, 10(4), 287. [DOI] [PubMed] [Google Scholar]
- Breivik H, Eisenberg E, & O’Brien T (2013). The individual and societal burden of chronic pain in Europe: The case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health, 13(1), 1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro-Costa E, Dewey M, Stewart R, Banerjee S, Huppert F, Mendonca-Lima C, Bula C, Reisches F, Wancata J, Ritchie K, Tsolaki M, Mateos R, & Prince M (2007). Prevalence of depressive symptoms and syndromes in later life in ten European countries. British Journal of Psychiatry, 191(5), 393–401. [DOI] [PubMed] [Google Scholar]
- Chu LF, Angst MS, & Clark D (2008). Opioid-induced hyperalgesia in humans. The Clinical Journal of Pain, 24(6), 479–496. [DOI] [PubMed] [Google Scholar]
- Cimas M, Ayala A, Sanz B, Agulló-Tomás MS, Escobar A, & Forjaz MJ (2018). Chronic musculoskeletal pain in European older adults: Cross-national and gender differences. European Journal of Pain, 22(2), 333–345. [DOI] [PubMed] [Google Scholar]
- Covinsky KE, Lindquist K, Dunlop DD, & Yelin E (2009). Pain, functional limitations, and aging. Journal of the American Geriatrics Society, 57(9), 1556–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyte PC, Asche CV, Croxford R, & Chan B (1998). The economic cost of musculoskeletal disorders in Canada. Arthritis Care & Research, 11(5), 315–325. [DOI] [PubMed] [Google Scholar]
- Craig KD, & Fashler SR (2013). Social determinants of pain. In Griensven HV, Strong J, & Unruh AM (Eds.), Pain. A textbook for health professionals (2nd ed., pp. 21–34). Churchill Livingstone. [Google Scholar]
- Crimmins EM, & Beltran-Sanchez H (2011). Mortality and morbidity trends: Is there compression of morbidity? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66B(1), 75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Zhang Y, & Saito Y (2016). Trends over 4 decades in disability-free life expectancy in the United States. American Journal of Public Health, 106(7), 1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croda E (2015). Pain and social exclusion among the European older people. In Borsch-Supan A, Kneip T, Litwin H, Myck M, & Weber G (Eds,), Ageingin Europe: Supporting policies for an inclusive society (pp. 313–320). De Gruyter. [Google Scholar]
- Currie SR, & Wang J (2005). More data on major depression as an antecedent risk factor for first onset of chronic back pain. Psychological Medicine, 35(09), 1275–1282. [DOI] [PubMed] [Google Scholar]
- Deyo RA, & Bass JE (1989). Lifestyle and low-back pain. Spine, 14(5), 501–506. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Mirza SK, & Martin BI (2006). Back pain prevalence and visit rates, 2002. Spine, 31(23), 2724–2727. doi: 10.1097/01.brs.0000244618.06877.cd [DOI] [PubMed] [Google Scholar]
- Dionne CE, Von Korff M, Koepsell T, Deyo R, Barlow W, & Checkoway H (2001). Formal education and back pain: A review. Journal of Epidemiology & Community Health, 55(7), 455–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott AM, Smith BH, Penny KI, Cairns Smith W, & Alastair Chambers W (1999). The epidemiology of chronic pain in the community. The Lancet, 354(9186), 1248–1252. [DOI] [PubMed] [Google Scholar]
- European Commission. (2018). 2018 Ageing Report: Policy Challenges for Ageing Societies. Brussels: European Commission. December 17, 2019. https://ec.europa.eu/info/news/economy-finance/policy-implications-ageing-examined-new-report-2018-may-25_en [Google Scholar]
- Farioli A, Mattioli S, Quaglieri A, Curti S, Violante FS, & Coggon D (2014). Musculoskeletal pain in Europe: The role of personal, occupational, and social risk factors. Scandinavian Journal of Work, Environment & Health, 40(1), 36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, & Riley JL (2009). Sex, gender, and pain: A review of recent clinical and experimental findings. The Journal of Pain, 10(5), 447–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flor H, Turk DC, & Rudy TE (1989). Relationship of pain impact and significant other reinforcement of pain behaviors: The mediating role of gender, marital status and marital satisfaction. Pain, 38(1), 45–50. [DOI] [PubMed] [Google Scholar]
- Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, & Carey TS (2009). The rising prevalence of chronic low back pain. Archives of Internal Medicine, 169(3), 251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA (2018). The demography of late-life disability. In Majmundar MK & Hayward MD (Eds.), Future directions for the demography of aging: Proceedings of a workshop (pp. 269–305). National Academies Press. [PubMed] [Google Scholar]
- Gaskin DJ, & Richard P (2012). The Economic costs of pain in the United States. The Journal of Pain, 13(8), 715–724. doi: 10.1016/j.jpain.2012.03.009 [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, & Turk DC (2007). The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin, 133(4), 581–624. [DOI] [PubMed] [Google Scholar]
- Goosby BJ (2013). Early life course pathways of adult depression and chronic pain. Journal of Health and Social Behavior, 54(1), 75–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol-Prokopczyk H (2017). Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain, 158(2), 313–322. doi: 10.1097/j.pain.0000000000000762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gureje O, Von Korff M, Kola L, Demyttenaere K, He Y, Posada-Villa J, Lepine JP, Angermeyer MC, Levinson D, De Girolamo G, Iwata N, Karam A, Borges G, De Graaf R, Browne M, Stein D, Haro J, Bromet E, Kessler R, & Alonso J (2008). The relation between multiple pains and mental disorders: Results from the world mental health surveys. Pain, 135(1–2), 82–91. [DOI] [PubMed] [Google Scholar]
- Harkness EF, Macfarlane GJ, Silman AJ, & McBeth J (2005). Is musculoskeletal pain more common now than 40 years ago?: Two population-based cross-sectional studies. Rheumatology, 44(7), 890–895. doi: 10.1093/rheumaiology/keh599 [DOI] [PubMed] [Google Scholar]
- Heistaro S, Vartiainen E, Heliovaara M, & Puska P (1998). Trends of back pain in eastern Finland, 1972–1992, in relation to socioeconomic status and behavioral risk factors. American Journal of Epidemiology, 148(7), 671–682. doi: 10.1093/aje/148.7.671 [DOI] [PubMed] [Google Scholar]
- Hooten WM (2016). Chronic pain and mental health disorders: Shared neural mechanisms, epidemiology, and treatment. Mayo Clinic Proceedings, 91(7), 955–970. [DOI] [PubMed] [Google Scholar]
- Hox JJ, Moerbeek M, & van de Schoot R (2018). Multilevel analysis: Techniques and applications. Routledge. [Google Scholar]
- Huppe A, Muller K, & Raspe H (2007). Is the occurrence of back pain in Germany decreasing? Two regional postal surveys a decade apart. The European Journal of Public Health, 17(3), 318–322. doi: 10.1093/eurpub/ckl231 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2012). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. The National Academies Press. [PubMed] [Google Scholar]
- Jagger C (2006). Can we live longer, healthier lives? In Zeng Y (Ed.), Longerlife and healthy aging (pp. 7–22). Springer. [Google Scholar]
- Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, & Piette JD (2017). Racial and socioeconomic disparities in disabling chronic pain: Findings from the health and retirement study. The Journal of Pain, 18(12), 1459–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy J, Roll JM, Schraudner T, Murphy S, & McPherson S (2014). Prevalence of persistent pain in the US adult population: New data from the 2010 national health interview survey. The Journal of Pain, 15(10), 979–984. [DOI] [PubMed] [Google Scholar]
- Mäntyselkä PT, Turunen JH, Ahonen RS, & Kumpusalo EA (2003). Chronic pain and poor self-rated health. JAMA, 290(18), 2435–2442. [DOI] [PubMed] [Google Scholar]
- Martin LG, & Schoeni RF (2014). Trends in disability and related chronic conditions among the forty-and-over population: 1997–2010. Disability and Health Journal, 7(1), S4–S14. doi: 10.1016/j.dhjo.2013.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin LG, Schoeni RF, & Andreski PM (2010). Trends in health of older adults in the United States: Past, present, future. Demography, 47(S1), S17–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy LH, Bigal ME, Katz M, Derby C, & Lipton RB (2009). Chronic pain and obesity in elderly people: Results from the Einstein aging study. Journal of the American Geriatrics Society, 57(1), 115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morasco BJ, Yarborough BJ, Smith NX, Dobscha SK, Deyo RA, Perrin NA, & Green CA (2017). Higher prescription opioid dose is associated with worse patient-reported pain outcomes and more health care utilization. The Journal of Pain, 18(4), 437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin RL (2015). Estimates of pain prevalence and severity in adults: United States, 2012. The Journal of Pain, 16(8), 769–780. doi: 10.1016/j.jpain.2015.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin RL, Sayer B, Stussman BJ, & Feinberg TM (2019). Eighteen-year trends in the prevalence of, and health care use for, noncancer pain in the United States: Data from the medical expenditure panel survey. The Journal of Pain, 20(7), 796–809. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (Vol. 1). Sage. [Google Scholar]
- Riskowski JL (2014). Associations of socioeconomic position and pain prevalence in the United States: Findings from the National Health and Nutrition Examination Survey. Pain Medicine, 15(9), 1508–1521. doi: 10.1111/pme.l2528 [DOI] [PubMed] [Google Scholar]
- Rubin S, & Zimmer Z (2015). Pain and self-assessed health: Does the association vary by age? Social Science & Medicine, 130, 259–267. doi: 10.1016/j.socscimed.2015.02.024 [DOI] [PubMed] [Google Scholar]
- Shen X, Zuckerman IH, Palmer JB, & Stuart B (2015). Trends in prevalence for moderate-to-severe pain and persistent pain among medicare beneficiaries in nursing homes, 2006–2009. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 70(5), 598–603. doi: 10.1093/gerona/glu226 [DOI] [PubMed] [Google Scholar]
- Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, & Viikari-Juntura E (2010). The association between obesity and low back pain: A meta-analysis. American Journal of Epidemiology, 171(2), 135–154. [DOI] [PubMed] [Google Scholar]
- Shupler MS, Kramer JK, Cragg JJ, Jutzeler CR, & Whitehurst DGT (2019). Pan-Canadian estimates of chronic pain prevalence from 2000 to 2014: A repeated cross-sectional survey analysis. The Journal of Pain, 20(5), 557–565. [DOI] [PubMed] [Google Scholar]
- Song M, Jin X, Ko HN, & Tak SH (2016). Chief complaints of elderly individuals on presentation to emergency department: A retrospective analysis of South Korean national data 2014. Asian Nursing Research, 10(4), 312–317. doi: 10.1016/j.anr.2016.10.001 [DOI] [PubMed] [Google Scholar]
- Todd A, McNamara CL, Balaj M, Huijts T, Akhter N, Thomson K, Kasim A, Eikemo TA, & Bambra C (2019). The Europain epidemic: Pain prevalence and socioeconomic inequalities in pain across 19 European countries. European Journal of Pain, 23(8), 1425–1436 [DOI] [PubMed] [Google Scholar]
- Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, Borges GLG, Bromet EJ, de Girolamo G, de Graaf R, Gureje O, Lepine J-P, Haro JM, Levinson D, Oakley Browne MA, Posada-Villa J, Seedat S, & Watanabe M (2008). Common chronic pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression-anxiety disorders. The Journal of Pain, 9(10), 883–891. [DOI] [PubMed] [Google Scholar]
- UNESCO Institute for Statistics. (2012). International standard classification of education: ISCED 2011.
- United Nations. (2018). World population prospects: The 2018 revision.
- Van Hecke O, Torrance N, & Smith BH (2013). Chronic pain epidemiology - where do lifestyle factors fit in? British Journal of Pain, 7(4), 209–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, & Jette AM (1994). The Disablement Process. Social Science & Medicine, 38(1), 1–14. [DOI] [PubMed] [Google Scholar]
- Verropoulou G, & Tsimbos C (2017). Disability trends among older adults in ten European countries over 2004–2013, using various indicators and survey of health, ageing and retirement in Europe (SHARE) data. Ageing and Society, 37(10), 2152–2182. [Google Scholar]
- Wade JB, Hart RR, Wade JH, Bajaj JS, & Price DD (2013). The relationship between marital status and psychological resilience in chronic pain. Pain Research and Treatment, 2013, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenig CM, Schmidt CO, Kohlmann T, & Schweikert B (2009). Costs of back pain in Germany. European Journal of Pain, 13(3), 280–286. [DOI] [PubMed] [Google Scholar]
- Wijnhoven HAH, de Vet HCW, & Picavet SJH (2006). Explaining sex differences in chronic musculoskeletal pain in a general population. Pain, 124(1), 158–166. [DOI] [PubMed] [Google Scholar]
- Zimmer Z, & Zajacova A (2018). Persistent, consistent, and extensive: The trend of increasing pain prevalence in older Americans. The Journals of Gerontology: Series B, 75(2), 436–447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


