Abstract
Background
During the COVID-19 pandemic, the provision of quality care for behavioral and psychological symptoms in older adults with dementia may have been impeded due to physical distancing and infection control measures. Of particular concern is whether psychotropic medication use has increased despite its limited efficacy and adverse effects. This systematic review described the trajectory of psychotropic use for older adults with dementia across various settings, from community living to healthcare settings during the pandemic. Also, psychotropic use was explored in relation to patients, caregivers, and environment-related factors along with the occurrence of the pandemic.
Methods
We conducted a comprehensive search across five databases: Embase, PubMed, PsycINFO, CINAHL, and Cochrane Library. Methodological quality was assessed using Joanna Briggs Institute Critical Appraisal tools. A random-effects model was used to estimate the pooled risk ratios (RRs) of psychotropic use in older adults with dementia, comparing the pandemic period to the pre-pandemic period. Subgroup analyses based on the class of psychotropics and sensitivity analyses also were conducted. A funnel plot and Egger’s regression test were used to detect potential publication bias.
Results
Of the 3,123 screened articles, 15 studies were included in this systematic review, with 10 of them being part of the meta-analysis. Our meta-analysis yielded an RR of 1.16 (95% CI = 1.05–1.26) for overall psychotropic medication use. Further subgroup analysis based on the type of psychotropic medication revealed a significantly greater prevalence in the use of antipsychotics (RR = 1.19, 95% CI = 1.08–1.30). However, no significant differences were observed in the use of anxiolytics and/or hypnotics (including benzodiazepines), antidepressants, and mood stabilizers. Among psychotropics, some studies on antipsychotic use additionally explored patients, caregivers, and environmental-related factors during the pandemic.
Conclusions
The review indicates a higher risk of psychotropic use, especially antipsychotics, during the pandemic. Nonetheless, underlying reasons for the increased psychotropic use are not fully available from the reviewed studies. Therefore, further research is needed to identify the factors driving psychotropic use during the pandemic and facilitate the development of quality improvement interventions that can be implemented to minimize inappropriate psychotropic prescribing in future pandemics.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05563-4.
Keywords: Dementia, Behavioral and psychological symptoms, Psychotropic medication use, COVID-19 pandemic
Brief summary
This review explored the trajectory of psychotropic use for older adults with behavioral and psychological symptoms of dementia across community living and healthcare settings during the pandemic. Also, psychotropic use was explored in relation to patients, caregivers, and environment-related factors along with the occurrence of the pandemic.
Background
Behavioral and psychological symptoms of dementia (BPSD) are a major aspect of dementia care and decrease the well-being of people with dementia. Non-pharmacological interventions are generally recommended as a first-line option for BPSD [1–3]. Psychotropics can be used for concerns about harm to self and/or others associated with psychosis or aggression [1, 3]. However, despite limited efficacy and severe adverse effects, psychotropics are often used to treat challenging behaviors with a lack of monitoring for BPSD or the application of non-pharmacological interventions [4–6]. Particularly, concerns about antipsychotic use in long-term care (LTC) settings (e.g., nursing homes (NHs), assisted living (ALs)) have been raised. For example, in the US, the Centers for Medicare and Medicaid (CMS) initiated policies to reduce the unnecessary use of antipsychotics in NHs [7], and a gradual decline has been noted since the initiative, with an average use of 14.5% of NH residents nationally [8]. In Canada, potentially inappropriate prescribing of antipsychotics among LTC settings has been monitored, 24.5% from 2022 to 2023 compared to 27.5% from 2014 to 2015 [4, 9].
In late 2019, a new respiratory syndrome, now known as coronavirus disease 2019 (COVID-19), was reported in China, and the COVID-19 infection spread globally, becoming a pandemic on March 11, 2020 [10]. The pandemic extensively disrupted the daily life of older adults with dementia because confinement and isolation were widely applied as infection control precautions to limit COVID-19 spread. Older adults with dementia were disproportionately vulnerable to severe illness following COVID-19 infection [11]. Those with dementia often had a lack of understanding of basic infection control measures. In addition, they were susceptible to the adverse effects of enforced quarantine [12], as they strongly relied upon community and social support systems due to their dependence for their activities of daily living (ADLs) [13].
In community environments, most home-based rehabilitation interventions and/or outpatient rehabilitation services were postponed or canceled. Physical distancing and infection control measures limited recreational activities, close contact with healthcare providers, and visits from family and friends, all of which contributed to social isolation in older adults with dementia [14]. In LTC settings, the measures imposed during the pandemic impeded the implementation of non-pharmacological interventions in older adults with dementia [14].
Changes in clinical care provisions in healthcare settings and restrictions during the pandemic may have worsened BPSD in older adults with dementia [15, 16], which could have led to increased reliance on psychotropic use [17–19]. Moreover, the inability to review drug dosages and monitor the efficacy of prescribed psychotropics, due to the disruption of routine assessments may have aggravated adverse consequences of psychotropics [10]. Thus, a systematic review of trends of psychotropic use to manage BPSD during the COVID-19 pandemic among older adults with dementia is greatly needed, to guide the appropriate management of BPSD in future pandemics and/or public health crises.
This review aims to describe empirical evidence on the trajectory of psychotropic use for the management of BPSD across community living, LTC settings, and hospital units for older adults with dementia during the pandemic. In addition, this review explored psychotropic use in relation to patients, caregivers, and environment-related factors along with the occurrence of the pandemic. The pandemic brought enormous changes in patients’ psychosocial status, availability of formal/informal caregivers, and clinical practices in acute- and long-term healthcare settings [14, 20–22].
Methods
The systematic review was conducted in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [23].
Search strategies
We used the following databases to identify potentially eligible articles: Embase, PubMed, PsycINFO, CINAHL, and Cochrane Library. The search terms included a combination of keywords such as (“dementia*” OR “Alzheimer*”) AND (“COVID-19” OR “SARS-Cov-2” OR “pandemic*” OR “corona*”) AND (“psychotropic*” OR “antipsychotic*” OR “antianxi*” OR “hypnotic*” OR “benzodiazepine*” OR “antidepress*” OR “anticonvulsant*” OR “antiepileptic*” OR “cholinesterase*” OR “memantine*” OR “behavio*” OR “psycho*”), as well as their subject headings from each database (e.g., MeSH terms in PubMed) and related synonyms. A database search was performed on March 20, 2024. Full search strategies can be found in the online Supplementary Materials (see Additional file 1).
Inclusion and exclusion criteria
Inclusion criteria
This review included articles that met the following criteria:
Population: Studies with all or most participants (≥ 90%) diagnosed with dementia. No limits were placed on the type or stage of dementia.
Outcome: Studies that addressed changes in psychotropic use for BPSD during the COVID-19 pandemic. Psychotropics were defined as antipsychotics, anxiolytics/hypnotics (including benzodiazepines), antidepressants, mood stabilizers (anticonvulsants/antiepileptics), cholinesterase inhibitors, and memantine, based on existing literature [1, 24, 25].
Setting: Studies across any settings, from community living to healthcare settings.
Study design and source: Empirical observational studies conducted with quantitative and/or qualitative research methodologies and published in peer-reviewed journals to ensure comprehensive and credible data would be reviewed.
Publication dates: Articles published between January 1, 2020, and December 31, 2023.
Exclusion criteria
Articles were excluded if they met the following criteria:
Studies focusing on mental health disorders (e.g., schizophrenia, bipolar disorders) other than dementia.
Studies not written in English.
Review papers, case reports, correspondence, or instrument development articles.
Abstract-only papers.
Study selection and data extraction process
Two reviewers (JMY and EK) independently conducted title and abstract screening for all records obtained from the database and manual searches, and then a full-text review to determine eligibility. Any discrepancies during the study selection process were resolved through discussion.
The following data were extracted from the included studies: authors, publication year, country, study design, data source, comparison period, characteristics of study setting and subjects, measures used, and main findings. Of the 15 included studies, 10 included data on psychotropic use for meta-analysis and were used to estimate risk ratios (RRs) and 95% confidence intervals (CIs) for psychotropic medication use. From the nine studies, we extracted the exact number of people with psychotropic use when available, or we used crude monthly, yearly, or mean percentages of those patients relative to the sample size for the comparison periods in each study. For one article that presented prevalence ratios and plots for the percentage of each psychotropic use [26], we contacted the author and obtained quarterly percentages. We then calculated and used the average number of people who were prescribed or administered psychotropics, as well as the average sample size before and during the pandemic period from each article.
Quality assessment
The final 15 selected articles were then rated for quality using Joanna Briggs Institute (JBI) Critical Appraisal tools for prevalence studies [27], analytical cross-sectional studies [28], cohort studies [28], or qualitative research [29]. A full review was independently rated by two raters (JMY and EK) to evaluate methodological quality in identifying characteristics of samples and their conditions, describing settings, and measuring outcomes using rigorous statistical evaluations Additional file 2 shows the summary of the quality appraisal of the included studies.
Statistical analysis
We used the “meta” package in R version 4.3.1 to perform the meta-analysis. Pooled estimates of RRs and 95% CIs were calculated using a random-effects model and the Mantel–Haenszel method. Heterogeneity was assessed using the Higgins Index (I2). Subgroup analyses were performed based on the class of psychotropics. To assess the robustness of the synthesized results, we conducted sensitivity analyses by sequentially omitting studies and observing changes in the pooled effect size and heterogeneity statistics. A funnel plot and Egger’s regression test were used to detect potential publication bias [30].
Results
Study selection results
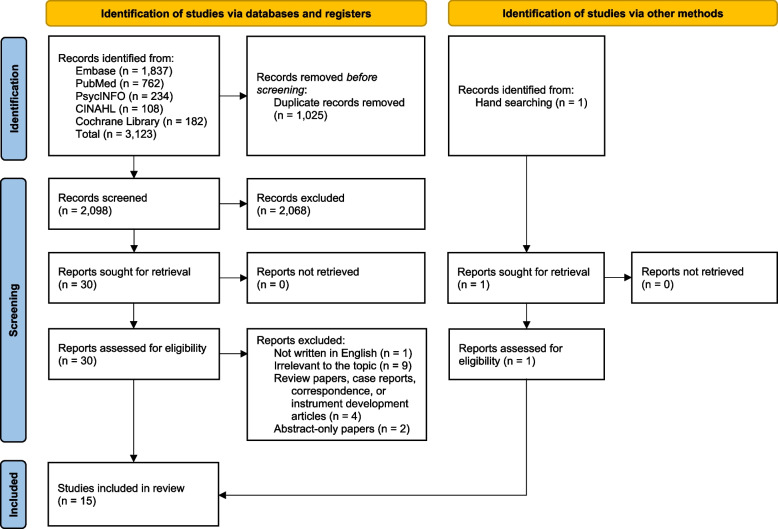
Overall, 3,123 articles were identified from the searched databases. After removing 1,024 duplicates, 2,099 articles were screened for title and abstract. After excluding 2,068 articles irrelevant to the topic through title and abstract screening, a full-text review was conducted on 30 articles. After removing 16 studies that met the exclusion criteria and adding one article from the manual search, 15 studies were finally selected for this review. A flowchart for the study selection process (Fig. 1) is presented according to the PRISMA guidelines [23].
Fig. 1.
Flow diagram of the study selection process
Study characteristics
Additional file 3 provides an overview of the included studies. Out of the 15 studies, eight investigated changes among residents with dementia in LTC settings, while two assessed changes in community-dwelling patients. Four studies used data from a mixture of healthcare settings. The included studies covered 10 countries, with three conducted in the US [31–33], three in the UK [20, 34, 35], two in Canada [26, 36], and one study each in Germany [37], Italy [38], the Netherlands [39], Spain [17], and Argentina [40]. Two studies were multinational; one included data from France, Germany, Italy, South Korea, the UK, and the US [41], while the other used global federated data, mainly from the US [42]. The research periods ranged from 2015 to January 2022, including pre-pandemic and pandemic periods.
According to the JBI critical appraisal assessment, this review included five prevalence studies [17, 20, 26, 31, 37], four analytical cross-sectional studies [33, 34, 36, 40], five cohort studies [35, 38, 39, 41, 42], and one qualitative study [32]. The critical appraisal assessment, as shown in Additional file 2, indicated that one-third of reviewed studies scored lower than 70% out of the total scores, mainly due to a lack of clearly identified sample conditions and incompletely addressed confounding variables.
Main findings
Antipsychotics
Among the 15 studies included in this review, 12 articles investigated changes in antipsychotic use during the COVID-19 pandemic. The study settings encompassed LTC settings in seven studies; communities in two studies; and a combination of healthcare settings in the remaining three studies. Overall, as shown in Additional file 3, 10 of the 12 studies (83%) reported an increase in antipsychotic drug use during the pandemic across settings [26, 31, 33–36, 38, 40–42].
Varying patterns in antipsychotic use were shown among the three studies that included NH residents with severe dementia as the majority of study subjects: one reported a significant increase in the average proportion of residents with prescriptions, from 18% (2015–16) to 32% (2020–22) (p< 0.001) [34]; another study found a significant but small decrease in the prescription proportion, from 80.5% (April 2018 to March 2020) to 78.2% (April 2020 to March 2021) (absolute difference [AD] = −2.31, 95% CI = −3.68–−0.93, p< 0.001) [17]; and in the third study, a stable pattern was noted throughout the initial phase of the pandemic (February to August 2020) [39].
Two studies explored changes in antipsychotic use associated with patient-related factors, along with the occurrence of the pandemic. For example, Schnier and colleagues [35] conducted age-standardized time-series analyses using population-scale health data from Wales. They found that those in the youngest age group (60–64 years) compared to other age groups, had increased prescribing rates of antipsychotics during the pandemic [35]. Additionally, people with all-cause dementia or a subgroup with vascular dementia had fluctuations in prescribing rates, whereas antipsychotic prescriptions in people with Alzheimer’s disease steadily increased [35]. A survey-based study on patients with dementia living at home found no difference in the proportions of increased or new-onset antipsychotic use in relation to levels of dementia severity [40].
McDermid and colleagues [34] examined antipsychotic prescription rates in NHs in relation to caregiver-related factors. They categorized NHs into tertiles according to antipsychotic prescription rates (low: 0–14%; medium: 14–36%; high: > 36%) and found no significant differences in staff sick days due to COVID-19, total staff sick days, or temporary staff shifts among the three groups [34].
Three studies explored environmental factorsin relation to antipsychotic use during the pandemic. A multinational study involving various healthcare settings explored the relationship between the strictness of lockdown policies and the prescribing rate of antipsychotic drugs for people with dementia [42]. They found significant associations across the majority of countries with databases included [42]. For example, a 10-point elevation in the COVID-19 Stringency Index score was related to a 10.2% increase (rate ratio = 1.10, 95% CI = 1.08–1.13) in prescription rates in the South Korean KUN database, and to a 3.3% increase (rate ratio = 1.03, 95% CI = 1.01–1.05) in the UK IMRD database [42]. Yan and colleagues [33] observed a 0.7 percentage-points increase in antipsychotic use among low-minority NHs (p < 0.001), and an additional 2.9 percentage-points increase in very-high minority NHs (p= 0.005) in the US at the beginning of the pandemic. They also found no significant differences in the impact of the pandemic on antipsychotic use by NH size (beds ≥ 120 vs. smaller), ownership (for-profit vs. not-for-profit) or community location in disadvantaged versus less-disadvantaged communities [33]. Similarly, McDermid and colleagues [34] observed no significant differences in NH size or number of residents with dementia across the low, medium, and high antipsychotic use tertiles in their pandemic sample.
Anxiolytics and/or hypnotics (including benzodiazepines)
Eight studies assessed changes in the use of anxiolytic and/or hypnotic drugs, including benzodiazepines. Among these, two studies conducted in communities reported increased prescriptions of anxiolytics and/or hypnotics including benzodiazepines [38, 40]. However, findings from studies in LTC settings or a combination of community and LTC settings were mixed. A study using AL settings, found decreased benzodiazepine use in 2021 compared to 2018–19: (prevalence ratio [PR] = 0.86, 95% CI = 0.78–0.95; p< 0.05) [26]. Also, a population-scale study in the UK in primary care and care homes observed a downward trend in benzodiazepine use throughout the study period from 2016 to 2021 [35]. Two other studies in NHs noted no significant differences in benzodiazepine use between pre-pandemic and pandemic periods [17, 39]. In contrast, another NH study reported an increase in anxiolytic drug use (slope change [SC] = 0.17, 95% CI = 0.13–0.21, p< 0.001) but no difference in hypnotic drug use [31], while another NH study reported increased PRN lorazepam injections [36].
Additionally, regarding patient-related factors, Cohen et al. [40] reported no significant relationship between an increase or onset of benzodiazepine and hypnotic prescriptions and dementia severity. Whereas no studies explored the use of anxiolytics and/or hypnotics in relation to caregivers and environmental-related factors.
Antidepressants
Among the five studies examining antidepressants, four studies (three in LTC settings, and one in the community) reported an increase in antidepressant use as shown in Table S3 [17, 26, 31, 40]. However, Sizoo et al. [39] found no significant changes in antidepressant use among NH residents. Regarding patient-related factors, Cohen et al. [40] reported no significant associations between increased or initiated antidepressant prescriptions and dementia severity. However, there was no study on the use of antidepressants in relation to caregivers and environmental-related factors.
Mood stabilizers
Two studies investigated changes in mood stabilizer use in LTC settings before and during the pandemic. Ferro Uriguen and colleagues [17] examined antiepileptic drug prescription rates among NH residents and found a significant increase in the average prevalence from 36.3% to 42.4% (AD = 6.10, 95% CI = 3.20–9.00, p< 0.001), while another study reported no significant change in dispensing rates of anticonvulsants among AL setting residents throughout the pandemic [26]. Among the reviewed studies, no studies explored the use of mood stabilizers in relation to patients, caregivers, and environmental-related factors.
Cholinesterase inhibitors and memantine
No studies were found regarding changes in the use of cholinesterase inhibitors and memantine during the COVID-19 pandemic.
All types of psychotropics
Two mixed-methods studies explored BPSD occurrence and all types of psychotropic use during the pandemic. Hoel and colleagues [37] found a low increase in pharmacological therapy for BPSD among 5.6% of German NHs along with increased occurrence of depression, anxiety, and appetite loss. Harding and colleagues [20] reported that about one quarter (26%) of 184 formal/informal caregivers for people with rarer dementias reported an increase or initiation of psychotropic use in those they were caring for, and two-thirds stated people with dementia experienced worsening of cognitive symptoms, ability to do things, and well-being.
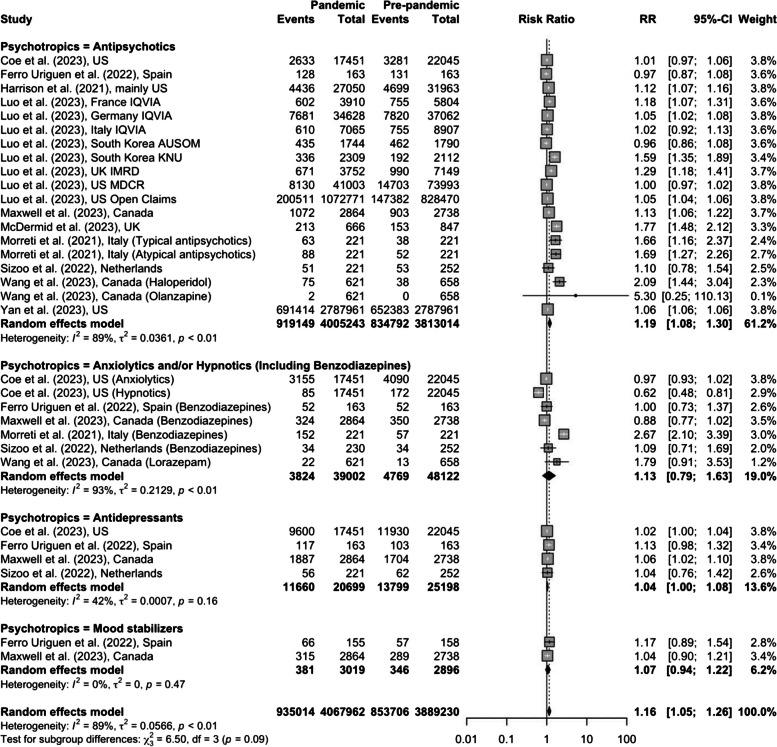
Meta-analysis
Figure 2 shows the pooled RRs of psychotropic use in individuals with dementia during the pandemic period compared to the pre-pandemic period. Our meta-analysis yielded an RR of 1.16 (95% CI = 1.05–1.26) for overall psychotropic medication use, with high heterogeneity (I2 = 89%). Further subgroup analysis revealed that the COVID-19 pandemic was associated with a significantly higher prevalence of antipsychotic use (RR = 1.19, 95% CI = 1.08–1.30, I2 = 89%), while no significant changes were observed for anxiolytics and/or hypnotics (including benzodiazepines) (RR = 1.13, 95% CI = 0.79–1.63, I2 = 93%), antidepressants (RR = 1.04, 95% CI = 1.00–1.08, I2 = 42%), and mood stabilizers (RR = 1.07, 95% CI = 0.94–1.22, I2 = 0%). Sensitivity analyses revealed consistent results on the pooled RR of psychotropic use for BPSD (RR = 1.15, 95% CI = 1.05–1.26, p < 0.01) (see Additional file 4). Visual inspection of the funnel plot demonstrated a symmetrical distribution (see Additional file 5). This observation was confirmed by Egger’s regression test, suggesting an absence of potential publication bias (p = 0.26).
Fig. 2.
RRs of psychotropic use for BPSD during the COVID-19 pandemic compared to the pre-pandemic period
Discussion
Overall, the review indicates slightly higher risks of increased psychotropic use in relation to the pandemic period from the meta-analysis, although some studies showed non-significant changes in the use of psychotropic medications. Subgroup analysis for each type of psychotropics indicated a small but significant likelihood of an increase in antipsychotic use.
Most reviewed studies and their meta-analyses reported an increase in the use of antipsychotics during the pandemic. It is not surprising to expect an increase in antipsychotic use given an increased prevalence of agitation, aggression, and psychosis during the pandemic [43–46]. Despite the efficacy of atypical antipsychotics for anger, aggression, and paranoid ideas, careful evaluation is needed because these agents have little efficacy for wandering and vocalizations and carry significant adverse effects [47–49]. Moreover, antipsychotics may worsen respiratory function and increase the risk of thromboembolism for those with COVID-19 infections [50].
The second most frequently used psychotropics were anxiolytic and hypnotic drugs and antidepressant medications. However, some LTC settings experienced a decreased use of benzodiazepines throughout the pandemic [17, 26], possibly due to increased use of other psychotropics, and such trends should be carefully monitored [51]. Benzodiazepines can be used for agitation and anxiety, but should not be routinely used due to dependence and adverse effects among older adults [2, 52]. Compared to benzodiazepines, most reviewed studies reported an increase in antidepressant use during the pandemic. The increase in antidepressant use coincides with an increased prevalence of depression, apathy, and agitation during the pandemic [46, 51, 53, 54]. Whilst antidepressants are relatively safe for the management of BPSD [55], the evidence of efficacy in the treatment of depression and agitation is mixed [48, 55–58].
Noted was a predominance of studies of antipsychotic use in LTC settings. Despite a higher proportion of older adults with dementia, ranging from 40 to 90% [9, 59, 60], LTC settings often lack sufficient professional staff, have insufficient dementia care training, and poorer environmental resources, all of which were related to a greater prevalence of psychotropic use compared to acute healthcare settings [60–64]. Especially, among the reviewed studies, a greater increase in antipsychotic use and a higher decrease in nurse staffing occurred in NHs with a larger proportion of racial and ethnic minority residents [33]. High minority LTC settings, even before the pandemic, lacked appropriate mental health-related services and had higher antipsychotic use [65, 66]. Thus, greater attention needs to be paid to vulnerable LTC settings to ameliorate pre-existing environmental conditions and help them cope with the challenges of providing quality dementia care in the post-pandemic era.
This review implies the need for consideration of patients, caregivers, and environment-related determinants of psychotropic use. Among reviewed studies, only two reported higher antipsychotic prescriptions in relation to environmental factors, such as stricter lockdown policies and having larger racial/ethnic minorities [33, 42]. Despite no relationship between psychotropic use and caregiver-related factors [34], higher cancellation rates of social activities in NHs were directly related to the proportion of staff with COVID-19 infection and to staff shortages [37]. Several pre-pandemic studies have examined factors influencing psychotropic use in older adults with dementia including patient factors (e.g., age, dementia severity), caregiver factors (e.g., caregiver’s burnout, BPSD care knowledge, nurse staffing), and environment-related factors (e.g., urban location, socioeconomic status, bed size) and can provide important pre-pandemic data on psychotropic use-related factors [6, 66–70].
The importance of exploring multiple factors of psychotropic use other than the occurrence of the pandemic is highlighted in comparing between- or within- countries' results. For example, large differences in the prevalence of antipsychotic use for NH residents with dementia between these two multinational studies were noted [17, 34] (18% [34] vs. 80.5% [17] in the pre-pandemic period and 32% [34] vs. 78.2% [17] in the pandemic period) and a consistently higher prevalence throughout both periods could be due to data collection from psychogeriatric NHs with high-intensity BPSD related to severe cognitive impairment [17]. However, both studies lacked information on dementia types, BPSD severity, and caregiver- or facility-related factors to compare determinants of antipsychotic use. Also, different studies conducted within the same country reported significantly heterogeneous prevalences of psychotropics use (e.g., South Korea AUSOM vs. South Korea KUN [42] and studies in Canada [26, 36]). Although different study sample sizes and settings, such as locations (e.g., urban areas vs. others [26, 36, 42]), LTC types (AL [26] vs. NHs [36]), and regular and PRN psychotropic use assessment [26] vs. PRN use only [36] can lead to different prevalence rates, it is still challenging to compare within countries’ results due to a lack of patient, caregiver, and environmental-related factors.
Limitations
Limitations in this review can be a lack of methodological rigor in defining samples’ characteristics and conditions as indicated by JBI quality appraisal. Further research needs well-characterized samples with cognitive impairment levels, types of dementia, and frequency and severity of BPSD. Among the reviewed studies, although Cohen et al. [40] found no significant relationship between psychotropic use and dementia severity, anxiety, depression, and insomnia were more prevalent in people with mild or moderate dementia compared to those with severe dementia. Regarding dementia types, Schnier and colleagues [35] found the highest proportion of prescribed antipsychotic medications among those with Alzheimer’s disease compared to other types, consistent with the research of Xiong and colleagues [71]. Also important is to assess any changes in the provision of non-pharmacological interventions for those with dementia during the pandemic.
Because psychotropics are also used to manage behavioral symptoms related to psychiatric or neurological disorders (e.g., schizophrenia, bipolar disorders, Huntington's disease), the lack of patient assessment for these indications for psychotropic use should be noted as a limitation. Furthermore, some studies relied on self-reported rates of psychotropic use by caregivers or others, thus responses could be affected by recall or subjective biases. Finally, there is little research on the use of other types of psychotropics. Given that mood stabilizers (e.g., valproic acid) are often used as an alternative to antipsychotics, more research is needed to explore their consequences, given their more serious and potentially life-threatening side effects compared to antipsychotics [72].
Moreover, regarding the review process, only published articles written in English were included, which might have led to the omission of potentially relevant studies. As COVID-19 rapidly became a pandemic, some publications written in languages of significantly affected countries (e.g., China, Italy) might have been missed [73]. Meta-analysis was conducted with 10 articles of the 15 selected because some studies used qualitative and mixed-methods so psychotropic use prevalence rates were unavailable.
Implications
This review highlights the importance of healthcare professionals as well as formal/informal caregivers to understand that care for BPSD may be more challenging during the pandemic in relation to national-level lockdowns, compromised delivery of regular rehabilitation, and the withdrawal of medical consultants [20, 40, 74]. There may have been a greater reliance upon psychotropic use among older adults with dementia from acute healthcare settings to those living in the community. Thus, policies are needed to ensure medical counsel on a regular basis, social service support, and widespread sharing of resources in the event of a pandemic. In LTC settings, protocols to review drug dosages and monitor the efficacy of prescribed psychotropics should be developed to facilitate regular assessments and reduce the adverse effects of psychotropics. Strategies to reduce unnecessary psychotropic use and provide non-pharmacological interventions are needed, such as alternative interventions in online or virtual formats, to promote appropriate BPSD care [75].
Conclusions
This systematic review and meta-analysis explored changes in psychotropic prescriptions during the pandemic. This review showed slightly increased psychotropic use in relation to the pandemic, specifically indicating higher risks of antipsychotic use compared to other psychotropic medications. The review suggests more prevalent psychotropic prescribing during the pandemic, but the underlying reasons in terms of patients, caregivers, and environmental-related factors are not fully available from the reviewed studies. Some studies lacked methodological rigor in identifying sample characteristics. As previous studies examined specific factors related to psychotropic use, there is a need to develop targeted research to clearly understand the driving factors of psychotropic use along with the pandemic crisis. Also, further research needs to be conducted in the post-pandemic period (after May 5, 2023) [76] to determine whether elevated psychotropic use has been sustained.
Supplementary Information
Additional file 2. Quality appraisal of included studies based on JBI (Joanna Briggs Institute) Critical Appraisal tools.
Additional file 3. Overview of included studies on changes in psychotropic use for BPSD during the COVID-19 pandemic.
Additional file 4. Sensitivity analyses on the pooled RR of psychotropic use for BPSD during the COVID-19 pandemic compared to the pre-pandemic period.
Additional file 5. Funnel plot of risk ratios and standard errors among the studies included in meta-analysis.
Additional file 6. PRISMA 2020 Checklist.
Acknowledgements
Not applicable.
Abbreviations
- AD
Absolute difference
- ADL
Activities of daily living
- AL
Assisted living
- AUSOM
Ajou University School of Medicine database
- BPSD
Behavioral and psychological symptoms of dementia
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- IMRD
IQVIA Medical Research Data
- JBI
Joanna Briggs Institute
- KUN
Kangwon National University
- LTC
Long-term care
- MDCR
IBM MarketScan Medicare Supplemental and Coordination of Benefits Database
- NH
Nursing home
- PR
Prevalence ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta Analyses
- RR
Risk ratio
- SC
Slope change
Authors’ contributions
JMY contributed to the conception and design of the study. JMY and EK performed the literature search, quality assessment, extraction, analysis and interpretation of the data. All authors (JMY, EK, and AMT) were involved in drafting the manuscript and revising it critically for important intellectual content. All authors approved the submitted version of the final manuscript.
Funding
This study was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (Grant number: RS-2023–00277604, PI: Jung Min Yoon). Also, this study was supported by the Ewha Womans University Research Grant of 2023.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015;350:h369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94. [DOI] [PubMed]
- 3.National Institute for Health and Care Excellence. Dementia: assessment, management and support for people living with dementia and their carers. 2018. http://www.nice.org.uk/guidance/ng97. Accessed 21 Sept 2024. [PubMed]
- 4.Kirkham J, Sherman C, Velkers C, Maxwell C, Gill S, Rochon P, et al. Antipsychotic use in dementia: is there a problem and are there solutions? Can J Psychiatry. 2017;62(3):170–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2018;30(3):295–309. [DOI] [PubMed] [Google Scholar]
- 6.Yoon JM, Trinkoff AM, Galik E, Storr CL, Lerner NB, Brandt N, et al. Deficiency citations on inappropriate psychotropics use related to care for behavioral symptoms of dementia. J Am Med Dir Assoc. 2022;23(11):1772–9. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid. Request to convey information: partnership to improve dementia care in nursing homes. 2012. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/SC-Letter-12-42-Introduction-National-Partnership.pdf. Accessed 21 Sept 2024.
- 8.Centers for Medicare and Medicaid. National Partnership to Improve Dementia Care in Nursing Homes: Antipsychotic Medication Use Data Report (April 2022). 2022. https://www.cms.gov/files/document/antipsychotic-medication-use-data-report-2021q4-updated-07292022.pdf. Accessed 21 Sept 2024.
- 9.Canadian Institute for Health Information. Potentially inappropriate use of antipsychotics in long-term care. 2022. https://yourhealthsystem.cihi.ca/hsp/inbrief?lang=en#!/indicators/008/potentially-inappropriate-use-of-antipsychotics-in-long-term-care/;mapC1;mapLevel2;/. Accessed 21 Sep 2024.
- 10.Brown EE, Kumar S, Rajji TK, Pollock BG, Mulsant BH. Anticipating and mitigating the impact of the COVID-19 pandemic on Alzheimer’s disease and related dementias. Am J Geriatr Psychiatry. 2020;28(7):712–21. [DOI] [PMC free article] [PubMed]
- 11.Goldstein MR, Poland GA, Graeber CW. Does apolipoprotein E genotype predict COVID-19 severity? QJM. 2020;113:529–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodman-Casanova J, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J Med Internet Res. 2020;22(5):e19434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Austrom MG, Boustani M, Lamantia MA. Ongoing medical management to maximize health and well-being for persons living with dementia. Gerontologist. 2014;2018(58):S48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keng A, Brown EE, Rostas A, Rajji TK, Pollock BG. Effectively caring for individuals with behavioral and psychological symptoms of dementia during the COVID-19 pandemic. Front Psychiatry. 2020;11:573367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Canevelli M, Valletta M, Toccaceli Blasi M, Remoli G, Sarti G, Nuti F, et al. Facing dementia during the COVID-19. J Am Geriatr Soc. 2020;68:1673–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cagnin A, Di Lorenzo R, Marra C, Bonanni L, Cupidi C, Laganà V, et al. Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front Psychiatry. 2020;11:578015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferro Uriguen A, Laso Lucas E, Sannino Menicucci C, Iturrioz Arrechea I, Alaba Trueba J, Echevarría Orella E, et al. Psychotropic drug prescription in nursing homes during the COVID-19 pandemic. Drugs Aging. 2022;39(6):467–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soysal P, Smith L, Trott M, Alexopoulos P, Barbagallo M, Tan SG, et al. The effects of COVID-19 lockdown on neuropsychiatric symptoms in patients with dementia or mild cognitive impairment: A systematic review and meta-analysis. Psychogeriatrics. 2022;22(3):402-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toniolo S, Scarioni M, Di Lorenzo F, Hort J, Georges J, Tomic S, et al. Dementia and COVID-19, a bidirectional liaison: risk factors, biomarkers, and optimal health care. J Alzheimers Dis. 2021;82(3):883-98. [DOI] [PubMed] [Google Scholar]
- 20.Harding E, Rossi-Harries S, Gerritzen EV, Zimmerman N, Hoare Z, Proctor D, et al. “I felt like I had been put on the shelf and forgotten about” – lasting lessons about the impact of COVID-19 on people affected by rarer dementias. BMC Geriatr. 2023;23(1):392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davidson PM, Szanton SL. Nursing homes and COVID-19: we can and should do better. J Clin Nurs. 2020;29(15–16):2758–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Numbers K, Brodaty H. The effects of the COVID-19 pandemic on people with dementia. Nat Rev Neurol. 2021;17:69–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kindstedt J, Sjölander M, Lövheim H, Gustafsson M. Psychotropic drug use among older people with major neurocognitive disorder: a cross-sectional study based on Swedish national registries. Eur J Clin Pharmacol. 2022;78(3):477–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Medicare and Medicaid. State Operations Manual Appendix PP - Guidance to surveyors for long term care facilities. 2024. https://www.cms.gov/medicare/provider-enrollment-and-certification/guidanceforlawsandregulations/downloads/appendix-pp-state-operations-manual.pdf. Accessed 21 Sept 2024.
- 26.Maxwell CJ, Dampf H, Alkabbani W, Cotton CA, Gamble JM, Hogan DB, et al. Psychotropic, anticonvulsant, and opioid use in assisted living residents before and during the COVID-19 pandemic. J Am Med Dir Assoc. 2024;25(1):121–9. [DOI] [PubMed] [Google Scholar]
- 27.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Healthc. 2015;13(3):147–53. [DOI] [PubMed] [Google Scholar]
- 28.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI. 2020. https://synthesismanual.jbi.global. Accessed 1 Mar 2024.
- 29.Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179–87. [DOI] [PubMed] [Google Scholar]
- 30.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coe AB, Montoya A, Chang CH, Park PS, Bynum JP, Shireman TI, et al. Behavioral symptoms, depression symptoms, and medication use in Michigan nursing home residents with dementia during COVID-19. J Am Geriatr Soc. 2023;71(2):414–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richards KC, Radhakrishnan K, Britt KC, Vanags-Louredo A, Park E, Gooneratne NS, et al. “Please don’t forget us”: a descriptive qualitative study of caregivers of older adults with Alzheimer’s disease and related dementias during the COVID-19 pandemic. Res Gerontol Nurs. 2022;15(5):217–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yan D, Temkin-Greener H, Cai S. Did the COVID-19 pandemic affect the use of antipsychotics among nursing home residents With ADRD? Am J Geriatr Psychiatry. 2023;31(2):124–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McDermid J, Ballard C, Khan Z, Aarsland D, Fox C, Fossey J, et al. Impact of the Covid-19 pandemic on neuropsychiatric symptoms and antipsychotic prescribing for people with dementia in nursing home settings. Int J Geriatr Psychiatry. 2023;38(1):e5878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schnier C, McCarthy A, Morales DR, Akbari A, Sofat R, Dale C, et al. Antipsychotic drug prescribing and mortality in people with dementia before and during the COVID-19 pandemic: a retrospective cohort study in Wales. UK Lancet Healthy Longev. 2023;4(8):e421–30. [DOI] [PubMed] [Google Scholar]
- 36.Wang HJ, Kusumo RW, Kiss A, Tennen G, Marotta G, Viaje S, al. Characterizing PRN use of psychotropic medications for acute agitation in Canadian long-term care residents with dementia before and during COVID-19. J Alzheimers Dis Rep. 2023;7(1):575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoel V, Seibert K, Domhoff D, Preuß B, Heinze F, Rothgang H, et al. Social health among German nursing home residents with dementia during the COVID-19 pandemic, and the role of technology to promote social participation. Int J Environ Res Public Health. 2022;19(4):1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moretti R, Caruso P, Giuffré M, Tiribelli C. COVID-19 lockdown effect on not institutionalized patients with dementia and caregivers. Healthcare. 2021;9(7):893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sizoo EM, Thunnissen JA, van Loon AM, Brederveld CL, Timmer H, Hendriks S, et al. The course of neuropsychiatric symptoms and psychotropic drug use in Dutch nursing home patients with dementia during the first wave of COVID-19: a longitudinal cohort study. Int J Geriatr Psychiatry. 2022;37(3):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cohen G, Russo MJ, Campos JA, Allegri RF. COVID-19 epidemic in Argentina: worsening of behavioral symptoms in elderly subjects with dementia living in the community. Front Psychiatry. 2020;11:866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harrison SL, Buckley BJR, Lane DA, Underhill P, Lip GY. Associations between COVID-19 and 30-day thromboembolic events and mortality in people with dementia receiving antipsychotic medications. Pharmacol Res. 2021;167:105534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luo H, Lau WCY, Chai Y, Torre CO, Howard R, Liu KY, et al. Rates of antipsychotic drug prescribing among people living with dementia during the COVID-19 pandemic. JAMA Psychiat. 2023;80(3):211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trinkoff AM, Yoon JM, Storr CL, Lerner NB, Yang BK, Han K. Comparing residential long-term care regulations between nursing homes and assisted living facilities. Nurs Outlook. 2020;68(1):114–22. [DOI] [PubMed] [Google Scholar]
- 44.Custodio N, Castro-Suárez S, Montesinos R, Failoc-Rojas VE, Cruz del Castillo R, Herrera-Perez E. Neuropsychiatric symptoms in patients with Alzheimer’s disease duringpandemic in Peru. Am J Alzheimers Dis Other Demen. 2021;36:15333175211039088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.El Haj M, Larøi F, Gallouj K. Hallucinations and COVID-19: increased occurrence of hallucinations in patients with Alzheimer’s disease during lockdown. Psychiatr Q. 2021;92:1531–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Manini A, Brambilla M, Maggiore L, Pomati S, Pantoni L. The impact of lockdown during SARS-CoV-2 outbreak on behavioral and psychological symptoms of dementia. Neurol Sci. 2021;42:825–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ballard C, Day S, Sharp S, Wing G. Neuropsychiatric symptoms in dementia: Importance and treatment considerations. Int Rev Psychiatry. 2008;20:396–404. [DOI] [PubMed] [Google Scholar]
- 48.Gauthier S, Cummings J, Ballard C, Brodaty H, Grossberg G, Robert P, et al. Management of behavioral problems in Alzheimer’s disease. Int Psychogeriatr. 2010;22:346–72. [DOI] [PubMed] [Google Scholar]
- 49.Sultzer DL, Davis SM, Tariot PN, Dagerman KS, Lebowitz BD, Lyketsos CG, et al. Clinical symptom responses to atypical antipsychotic medications in Alzheimer’s disease: phase 1 outcomes from the CATIE-AD effectiveness trial. Am J Psychiatry. 2008;165:844–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ostuzzi G, Papola D, Gastaldon C, Schoretsanitis G, Bertolini F, Amaddeo F, et al. Safety of psychotropic medications in people with COVID-19: evidence review and practical recommendations. BMC Med. 2020;18:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Coe AB, Zhang T, Zullo AR, Gerlach LB, Thomas KS, Daiello LA, et al. Psychotropic medication prescribing in assisted living and nursing home residents with dementia after the National Partnership. J Am Geriatr Soc. 2022;70:3513–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Franchi B. Pharmacological management of behavioural and psychological symptoms of dementia. J Pharm Pract Res. 2016;46(3):277–85. [Google Scholar]
- 53.El Haj M, Boutoleau-Bretonnière C, Allain P, Kapogiannis D, Chapelet G, Gallouj K. On Covid-19 and mental health: an observational study on depression, anxiety, and loneliness during the second lockdown in patients with Alzheimer disease. Medicine. 2022;101:e29145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lara B, Carnes A, Dakterzada F, Benitez I, Piñol-Ripoll G. Neuropsychiatric symptoms and quality of life in Spanish patients with Alzheimer’s disease during the COVID-19 lockdown. Eur J Neurol. 2020;27:1744–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hsu TW, Stubbs B, Liang CS, Chen TY, Yeh TC, Pan CC, et al. Efficacy of serotonergic antidepressant treatment for the neuropsychiatric symptoms and agitation in dementia: a systematic review and meta-analysis. Ageing Res Rev. 2021;69:101362. [DOI] [PubMed] [Google Scholar]
- 56.Henry G, Williamson D, Tampi RR. Efficacy and tolerability of antidepressants in the treatment of behavioral and psychological symptoms of dementia, a literature review of evidence. Am J Alzheimers Dis Other Demen. 2011;26:169–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Porsteinsson AP, Drye LT, Pollock BG, Devanand DP, Frangakis C, Ismail Z, et al. Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA. 2014;311:682–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Husain M, Roiser JP. Neuroscience of apathy and anhedonia: a transdiagnostic approach. Nat Rev Neurosci. 2018;19(8):470–84. [DOI] [PubMed] [Google Scholar]
- 59.Harris-Kojetin L, Sengupta M, Lendon JP, Rome V, Valverde R, Caffrey C. Long-term care providers and services users in the United States, 2015–2016. National Center for Health Statistics. Vital Health Stat. 2019;3(43). https://stacks.cdc.gov/view/cdc/76253. Accessed 21 May 2024. [PubMed]
- 60.Zimmerman S, Carder P, Schwartz L, Silbersack J, Temkin-Greener H, Thomas KS, et al. The imperative to reimagine assisted living. J Am Med Dir Assoc. 2022;23(2):225–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hoben M, Li W, Dampf H, Hogan DB, Corbett K, Chamberlain SA, et al. Caregiver involvement and concerns with care of residents of assisted living before and during the COVID-19 pandemic. Gerontology. 2023;69(7):839–51. [DOI] [PubMed] [Google Scholar]
- 62.Schwartz LB, Lieblich C, Laxton CE, Kaes L, Barnett DP, Port C, et al. COVID-19 in assisted living: protecting a critical long-term care resource. J Am Med Dir Assoc. 2023;24:134–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Candon M, Strominger J, Gotlieb E, Maust DT. Nursing home characteristics associated with high and low levels of antipsychotic, benzodiazepine, and opioid prescribing to residents with Alzheimer’s disease and related dementias: a cross-sectional analysis. J Am Med Dir Assoc. 2022;23:1780–6.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.U.S. Department of Health and Human Services, Office of Inspector General (Christi A. Grimm). Long-term trends of psychotropic drug use in nursing homes. https://oig.hhs.gov/oei/reports/OEI-07-20-00500.pdf. Accessed 21 May 2023.
- 65.Cioltan H, Alshehri S, Howe C, Lee J, Fain M, Eng H, et al. Variation in use of antipsychotic medications in nursing homes in the United States: a systematic review. BMC Geriatr. 2017;17(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lucas JA, Chakravarty S, Bowblis JR, Gerhard T, Kalay E, Paek EK, et al. Antipsychotic medication use in nursing homes: a proposed measure of quality. Int J Geriatr Psychiatry. 2014;29(10):1049–61. [DOI] [PubMed] [Google Scholar]
- 67.Loftus KL, Wand APF, Breen JL, Hunt GE, Peisah C. Factors associated with psychotropic medication use in people living with dementia in the community: a systematic review and meta-analysis. Drugs Aging. 2023;40(12):1053–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Resnick B, Kolanowski A, Van Haitsma K, Galik E, Boltz M, Ellis J, et al. Current psychotropic medication use and contributing factors among nursing home residents with cognitive impairment. Clin Nurs Res. 2021;30(1):59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Walsh KA, Sinnott C, Fleming A, Mc Sharry J, Byrne S, Browne J, et al. Exploring antipsychotic prescribing behaviors for nursing home residents with dementia: a qualitative study. J Am Med Dir Assoc. 2018;19(11):948–58.e12. [DOI] [PubMed] [Google Scholar]
- 70.Yoon JM, Trinkoff AM, Galik E, Storr CL, Lerner NB, Brandt N, et al. Nurse staffing and deficiency of care for inappropriate psychotropic medication use in nursing home residents with dementia. J Nurs Scholarsh. 2022;54(6):728–37. [DOI] [PubMed] [Google Scholar]
- 71.Xiong GL, Filshtein T, Beckett LA, Hinton L. Antipsychotic use in a diverse population with dementia: a retrospective review of the National Alzheimer’s Coordinating Center Database. J Neuropsychiatry Clin Neurosci. 2015;27(4):326–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Candon M, Strominger J, Gerlach LB, Maust DT. Antiepileptic prescribing to persons living with dementia residing in nursing homes: a tale of two indications. J Am Geriatr Soc. 2023;71(1):89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen J, Lu H, Melino G, Boccia S, Piacentini M, Ricciardi W, al. COVID-19 infection: the China and Italy perspectives. Cell Death Dis. 2020;11(6):438. [DOI] [PMC free article] [PubMed]
- 74.Sriram V, Jenkinson C, Peters M. Impact of COVID-19 restrictions on carers of persons with dementia in the UK: a qualitative study. Age Ageing. 2021;50(6):1876–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McDermid J, Henley W, Corbett A, Williams G, Fossey J, Clare L, et al. Impact of the iWHELD digital person-centered care program on quality of life, agitation and psychotropic medications in people with dementia living in nursing homes during the COVID-19 pandemic: a randomized controlled trial. Alzheimers Dement. 2024;20(3):1797–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wise J. Covid-19: WHO declares end of global health emergency. BMJ. 2023;381:1041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Quality appraisal of included studies based on JBI (Joanna Briggs Institute) Critical Appraisal tools.
Additional file 3. Overview of included studies on changes in psychotropic use for BPSD during the COVID-19 pandemic.
Additional file 4. Sensitivity analyses on the pooled RR of psychotropic use for BPSD during the COVID-19 pandemic compared to the pre-pandemic period.
Additional file 5. Funnel plot of risk ratios and standard errors among the studies included in meta-analysis.
Additional file 6. PRISMA 2020 Checklist.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.